
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health , 14 February 2024
Sec. Aging and Public Health
Volume 11 - 2023 | https://doi.org/10.3389/fpubh.2023.1303137
Background: China has by far one of the fastest-aging populations in the world. Increasing age is often accompanied by an increasing prevalence of chronic diseases and impaired Activities of Daily Living (ADL). The aim of this study was to analyze the effects of chronic diseases on ADL in Chinese middle-aged and older adults and to provide a scientific basis for delaying the impairment of ADL and prolonging the self-care life expectancy of middle-aged and older adults.
Methods: This investigation utilized the survey information of 10,096 middle-aged and older adults from the China Health and Aging Tracking Survey (CHARLS) of 2011 as baseline data, then followed up this cohort until 2018, and performed multifactorial analyses using Cox proportional risk models to explore the strength of the associations between chronic diseases and the risk of impaired ADL in middle-aged and older adults.
Results: Among the middle-aged and older adult population, the presence of hypertension was associated with a 38% higher risk of impaired ADL compared to those without the condition (HR = 1.38,95% CI:1.24–1.54); the involvement of heart disease was associated with a 27% higher risk of impaired ADL compared to those without the condition (HR = 1.27,95% CI:1.10- 1.46); the existence of arthritis was associated with a 38% higher risk of impaired ADL in middle-aged and older adults compared to those without arthritis (HR = 1.38,95% CI:1.25–2.08); additionally, the risk of impaired ADL with one or ≥ 2 chronic diseases was increased by 34% (HR = 1.34, 95% CI:1.18–1.52) and 84% (HR = 1.84, 95% CI:1.63–2.08) in middle-aged and older adult individuals, respectively.
Conclusion: Hypertension is a risk factor for impaired ADL at any age in the subjects of this study. Examining the association between the number of chronic diseases and impairment in activities of daily living, it was revealed that the risk of ADL impairment increased with the number of chronic diseases in both the middle-aged (45–59 years) and older adult (60–74 years) groups.
Population aging has become a major global problem, and China has the world's largest older adult population and one of the fastest-aging populations in the world (1). In 2022, 14.9% of the country's population was 65 years of age or older. It is expected that by 2050, China's older adult population aged 65 and above will reach 382 million, accounting for 32.5% of the total population (2). As we age, all organs and functions of the human body weaken, and the ability to perform activities of daily living (ADL) declines.
ADL refers to the fundamental duties that are necessary for a person to carry out on a daily basis. These activities include using the restroom, eating, clothing, grooming, walking, and taking a bath. ADL impairment indicates a person's inability to perform these necessary tasks on their own, which exerts a heavy load on the person, their family, and society at large (3). As of 2021, approximately 16% of the world's population are affected by ADL impairment, with 34.4% of those aged 60 years and older affected (4). The ADL indicator has been officially recognized by the World Health Organization (WHO) and is widely used (5). There are many factors that influence ADL impairment in middle-aged and older adults, and previous studies have shown that low socioeconomic status, low education, cerebral hemorrhage (6), absence of a spouse, physical inactivity, low social activity, experience of falls, cognitive decline (7), being female, admission to a nursing home for ≥5 years, and impaired consciousness (8) are all factors contributing to ADL impairment.
However, there is a paucity of research on the relationship between chronic conditions and impaired ADL. A study published in 2023 noted that the negative impact of chronic diseases on the quality of life of older adults is not limited to physical health, but also involves psychological and social aspects (9). Approximately 70% of the total disease burden experienced by the Chinese population in 2019 was attributable to chronic diseases. The health damage caused by chronic diseases is immeasurable and has become the most important cause of death among Chinese residents, accounting for approximately 88.5% of deaths (10). Chronic diseases have demonstrated an aging trend in recent years. The high prevalence of chronic diseases aggravates the physical deterioration and daily life dysfunction of middle-aged and older adults, which in turn leads to a continuous decline in the self-care ability and quality of life of middle-aged and older adults, and imposes a heavy disease burden on individuals, families and society (11).
Few studies have been conducted both nationally and internationally to investigate the relationship between chronic diseases and impaired ADL, and the studies that have been carried out have utilized primarily cross-sectional data (12, 13). Limited studies have examined the impact of co-morbidities and chronic diseases interacting with other risk variables on ADL in middle-aged and older adults using cohort data. Therefore, this study utilized data from the China Health and Retirement Longitudinal Study (CHARLS) to analyze the effects of chronic diseases on ADL in middle-aged and older adults in China, using a retrospective cohort study design to provide a scientific basis for delaying the impairment of ADL and improving the quality of life in middle-aged and older adults.
Data were obtained from the CHARLS database. The database is designed to study the issue of aging in China and to facilitate corresponding research. The CHARLS study used a multistage stratified random sample of 450 village-level units in 150 counties (districts) in 28 provinces (autonomous regions and municipalities directly under the central government). Survey weights were considered in all our analyses as follows. The product of the basic and adjusted weights was used to obtain a combined weight for each individual to represent the probability of its true occurrence in the aggregate. To make the data a better representation, the weighting considers a number of factors, including the sampling design, missingness, non-response rate, non-coverage, geographical location, gender, age, and socioeconomic characteristics (14). The ethical approval for the CHARLS project was received from the Ethics Review Committee of Peking University, and informed consent was obtained from all participants during the data collection.
A total of 17,683 samples were collected for the survey at the 2011 baseline. After excluding 396 individuals under 45 years old and 2,870 who had already experienced ADL impairment at the time of the baseline survey, 14,417 middle-aged and older adults who were eligible for the study were ultimately included in the study. As a result of death, withdrawal, loss of visits, etc., the sample reported 11,301 individuals at the end of the follow-up in 2018. However, due to missing data and other factors, a valid sample of 10,096 individuals was finally included. Of these, 8,346 did not have an ADL loss, and 1,750 individuals in the group had an ADL injury. Prior to and during sample removal, there was no statistically significant difference between middle-aged and older adults with and without ADL injury within the cohort, indicating a low likelihood of bias from lost visits, data cleaning, and other reasons. Figure 1 depicts the particular sample screening procedure.
This study used a cohort study method, with 14,417 middle-aged and older adults aged ≥45 years obtained from the 2011 survey as the baseline population. The exclusion criteria for the study population were: respondents with impaired ADL at the time of the baseline survey; and age under 45 years. Inclusion criteria were: respondents did not meet the exclusion criteria; no key variables were missing. The study variables of this survey are basic demographic factors (age, gender, region, residence, marital status, education level), lifestyle that may be associated with impaired ADL (smoking status, alcohol consumption status, social activity status) (15), personal health status (ability to perform activities of daily living, physical pain status, fall status), and chronic disease prevalence (cardiovascular disease, respiratory disease, digestive disease, metabolic disease, neurological disease, arthritis or rheumatism, and kidney disease). Data on these study variables were collected using a validated, reliable questionnaire on subjects previously diagnosed with chronic diseases by health-care providers (16).
According to WHO standards, middle-aged and older adult individuals were divided into three groups for this study: middle-aged individuals 45–59 years old, young older adult individuals 60–74 years old, and older adult individuals 75 years of age and older. Also investigated was how various groups' ADL was affected by their status with chronic diseases. Hypertension, dyslipidemia, heart disease, gastric or digestive diseases, arthritis, and other conditions with prevalence in the top five were chosen as the study factors based on the chronic disease parity of middle-aged and older adults, as reported in the 2018 CHARLS data analysis report. The quantity of prevalence outside of these five categories of chronic diseases was used as the control number. In this study, the number of chronic diseases suffered by middle-aged and older adults was divided into three categories (0, 1, and 2). The majority of these individuals had several co-morbidities. Furthermore, there are significant differences in middle-aged and older adult health status between age groups.
The ADL impairment status of the middle-aged and older adult cohorts was followed up in 2013, 2015, and 2018, respectively. The outcome events were categorized as “occurrence of ADL impairment” and “deletion.” Middle-aged and older adults who were lost during the follow-up, who died before the end of the follow-up without ADL impairment, and who did not have ADL impairment at the end of the last follow-up in 2018 were labeled as censored. The definition of impaired ability to perform activities of daily living includes using the restroom, eating, clothing, grooming, walking, and taking a bath. Each question is rated on a four-point scale (1: no difficulty). 2: difficulty but still can be completed. 3: difficulty and need help. 4: cannot be completed.). A total score equal to 6 is considered completely normal; a score greater than 6 represents a middle-aged or older adult person with varying degrees of ADL impairment. A score of 1 for a single question is considered normal, and a score of 2–4 is considered a decrease in functioning; if two or more scores are greater than or equal to 3, or if the total score is greater than or equal to 12, it represents a significant impairment of the ADL. Some studies have shown that the ADL scale has high reliability and validity in reflecting the mental and health status of Chinese older adults (15).
In this study, the distribution of categorical variables was described using n (%), and the log-rank one-way test was used to analyze whether there was a statistical association between exposure factors and the risk of developing impaired ADL in the middle-aged and older adult population; multifactorial analysis using Cox proportional risk models to explore the strength of the association between hypertension, dyslipidaemia, heart disease, gastric or digestive disorders, arthritis, and the number of chronic illnesses suffered and the risk of impaired ADLs in middle-aged and older adults; Finally, the VIF variance inflation factor was used to test for variable covariance. All analyses were performed using the statistical software Stata 16.0, and a two-tailed P value < 0.05 was considered statistically significant.
Sixty-eight percent of the 10,096 sample population that was included in the survey was between the ages of 45 and 59, thirty-nine percent was between the ages of 60 and 74, and four percent was above the age of 75. The following factors were found by the log-rank test to be statistically significant in the difference between the ADL impaired group and the ADL intact group in the 45–59-year age group: gender, place of residence, marital status, education level, smoking, drinking, physical pain status, fall status, arthritis, heart disease, dyslipidemia, number and region of chronic diseases, and hypertension. Moreover, in the subgroup 60–74 years, hypertension, heart disease, stomach or digestive disease, arthritis, number and gender of chronic diseases, place of residence, marital status, education, smoking status, alcohol consumption status, social activity status, physical pain status, and fall status showed statistically significant differences between the ADL impaired group and the ADL intact group by the log-rank test. Besides, the ADL impaired and ADL intact groups differed statistically significantly in alcohol consumption status, gender, and hypertension in the 75 and over subgroup (Table 1).
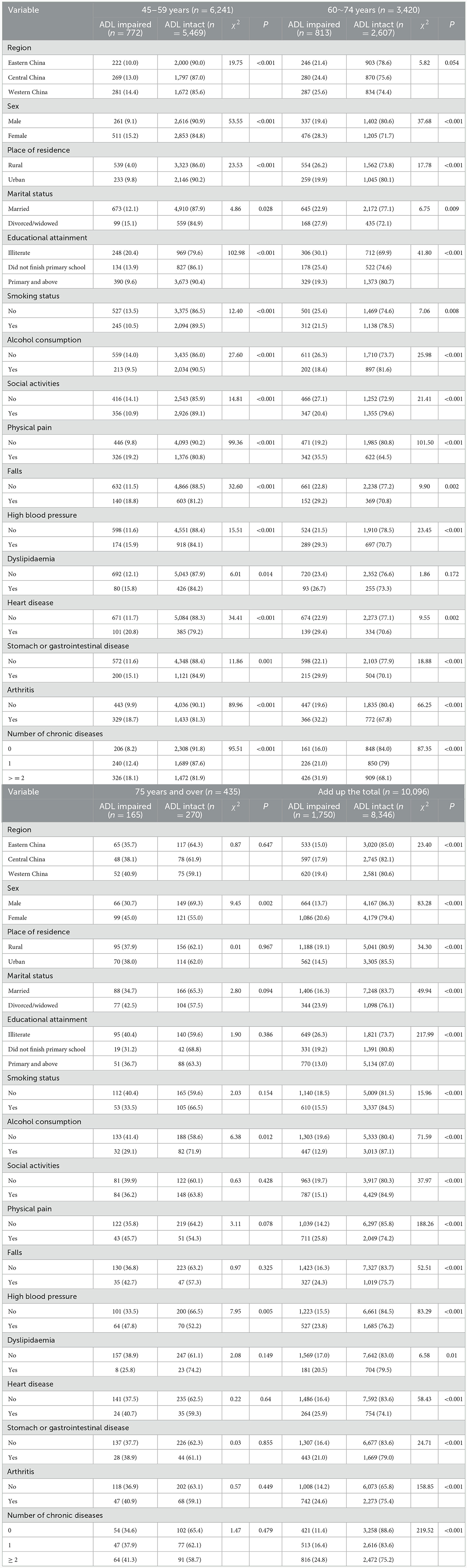
Table 1. Descriptive analysis of demographic characteristics and baseline exposure factors in the middle-aged and older adult population (%).
Furthermore, a Variance Inflation Factor (VIF) test was conducted to assess the multicollinearity between the independent variables in the model. The VIF value measures the degree of multicollinearity between the independent variables, and in general, a VIF value of < 10 means that it is acceptable (17). In Table 2, the mean VIF values for the four models are 2.35, 2.13, 2.12, and 2.23 from left to right, and the VIF values for all variables are < 5, which indicates that there is no multicollinearity among the variables. In Table 3, the mean values of VIF for the four models are 2.63, 2.38, 2.33, and 2.48 from left to right, and the VIF values of all variables are < 6, which indicates that there is no multicollinearity among the variables.
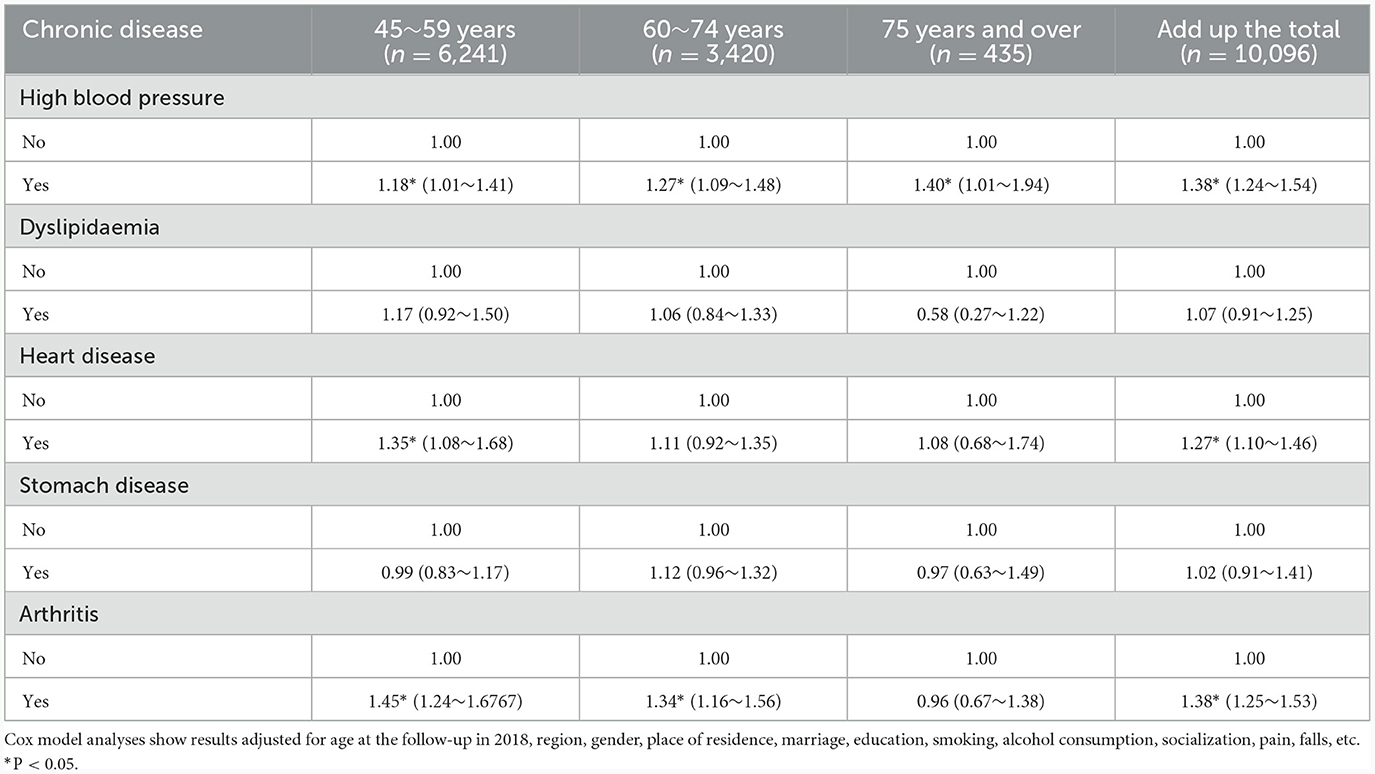
Table 2. Cox model analysis of factors influencing the risk of impaired ability to perform activities of daily living for five categories of high prevalence chronic diseases (HR 95% CI).
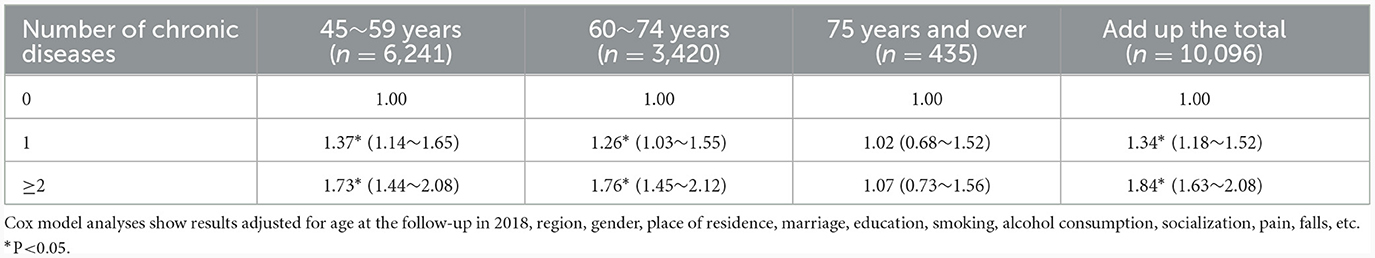
Table 3. Cox model analysis of the factors influencing the number of chronic diseases on the risk of impaired ability to perform daily activities (HR 95% CI).
In the overall sample, subjects with heart disease had a 27% higher risk of impaired ADLs than people without heart disease (HR = 1.27, 95% CI: 1.20–1.46), individuals with arthritis had a 38% higher risk of ADL impairment than persons without arthritis (HR = 1.38, 95% CI: 1.25–1.53), and subjects with hypertension had a 38% higher risk of impaired ADLs compared to subjects without hypertension. Age subgroup analyses of the entire sample revealed that the 45–59-year-old subgroup had a 21% (HR = 1.21, 95% CI: 1.01–1.45), 37% (HR = 1.37, 95% CI: 1.09–1.71), and 47% (HR = 1.47, 95% CI: 1.26–1.71) higher risk of impaired ADL, respectively, due to hypertension, heart disease, and arthritis. In the 60–74-year-old subgroup, hypertension and arthritis increased the risk of impaired ADLs by 28% (HR = 1.28, 95% CI: 1.10–1.49) and 34% (HR = 1.34, 95% CI: 1.16–1.55), respectively; in the 75–year-old and older subgroups, suffering from hypertension increased the risk of impaired ADLs by 40% (HR = 1.40, 95% CI: 1.01–1.94). Moreover, the several cox regression analyses expressed, neither dyslipidaemia nor stomach disease was found to be statistically significantly associated with impaired ADL in the entire sample (Table 2). Compared to those without chronic diseases, the risk of impaired ADL was higher in the overall sample for those with one or more chronic conditions by 34% (HR = 1.34, 95% CI: 1.18–1.52) and 84% (HR = 1.84, 95% CI: 1.63–2.08), respectively. The results of the age subgroup analyses indicated that, in the 45–59-year-old subgroup, the probability of impaired ADL was raised by 40% (HR = 1.40, 95% CI: 1.16–2.59) and 79% (HR = 1.79, 95% CI: 1.48–2.15), respectively, if one or more chronic diseases were present. Having one or more chronic illnesses increased the likelihood of impaired ADL by 26% (HR = 1.26, 95% CI: 1.03–1.55) and 77% (HR = 1.77, 95% CI: 1.47–24.14) in the subgroup of people aged 60–74 years, respectively (Table 3).
This study investigated the relationship between demographic characteristics, health status, types of chronic diseases, and impaired ADL among middle-aged and older adults in China who were 45 years of age and older. It was based on a large-scale population-based survey that used a nationally representative cohort. The results of this research revealed that among China's middle-aged and older population, having multiple chronic diseases, heart disease, arthritis, and hypertension are risk factors for impaired ADL. The likelihood of having impaired ADL also increases with the number of chronic diseases a person possesses.
The results of this present study found that hypertension increases the risk of impaired ADL in middle-aged and older adults, which is consistent with the results of previous studies (18, 19). Moreover, data from the 2011–2015 China Health and Retirement Longitudinal Study (CHARLS) of middle-aged and older adults aged 45 years and older in China found that hypertension was a risk factor for impaired ADL in middle-aged and older adults (18). Further 7-year cohort research carried out in the United States similarly discovered that older persons with hypertension had an increased probability of having impaired ADL (19). About half of China's yearly fatalities from cardiovascular and cerebrovascular disorders are attributable to hypertension, which is well recognized to be extremely hazardous and a significant risk factor for many of these conditions (20). Moreover, studies indicate that the number of fatalities from hypertension and disability-adjusted life years (DALYs) is rising annually (21). The Report on Nutrition and Chronic Disease Status of Chinese Residents (22), states that among Chinese residents who are 18 years of age and older, the prevalence of hypertension is 27.5%; however, the control rate is only around 16.8%. The study's findings indicated that middle-aged and older adults in three distinct age groups: 45–59, 60–74, and 75 years and older, were prone to having impaired ADL due to hypertension. Considering the serious harm and high prevalence of hypertension, it is recommended that middle-aged and older adults with hypertension receive scientifically grounded, comprehensive management that includes early detection, early diagnosis, and early control in order to minimize its effects on ADL impairment.
The results of the study also showed a significant association between the presence of heart disease and impaired ADL in Chinese middle-aged and older adults. Heart disease may have a serious impact on heart function, including ischemia and hypoxia in the myocardial tissues, which in turn leads to a decline in heart function and affects the patients' ADL. Secondly, heart disease may trigger a range of psychological and emotional problems, such as anxiety, depression, and fear, which in turn affect their motivation, willingness, and confidence in performing daily tasks, leading to impaired ADL. This is consistent with the findings of Akasaki et al., who examined older people with and without heart disease using data from community health surveys and discovered a substantial correlation between social vulnerability and heart disease (23). Furthermore, Liperoti et al. conducted a systematic review that yielded similar findings. They searched for relevant papers in PubMed, Web of Science, and Embase. The eligible papers were then subjected to a meta-analysis. The study found that older patients with ischemic heart disease frequently had frailty. Thus, it is critical to take into account the frailty state of older people with ischemic heart disease in order to establish individualized strategies for cardiovascular prevention and treatment (24). Heart diseases, which include congenital heart disease, coronary heart disease, and various forms of heart disease, are collectively referred to as heart disease (25). Ischemia and hypoxia of the myocardial tissues can result from cardiac disease, which can have a major impact on heart function, perhaps even on a normal life. China's aging population continues to grow rapidly, and the burden of heart disease is becoming more and more serious, posing a great challenge to prevention and control (26). Therefore, prevention, diagnosis, treatment, and control of heart disease in middle-aged and older adults are crucial in delaying ADL damage.
Moreover, the investigation's findings indicate that arthritis increases middle-aged and older people's risk of ADL impairment and this is similar to previous findings (27, 28). Arthritis is currently the most disabling disease worldwide (29). Arthritis is an inflammatory disease that occurs in the joints and surrounding tissues of the body and is characterized by redness, swelling, heat, pain, dysfunction, and joint deformity. Common types of arthritis include rheumatoid arthritis, osteoarthritis, reactive arthritis, infectious arthritis, and traumatic arthritis (30, 31). Studies have found that the prevalence of arthritis in China is as high as 50% in people over 60 years of age. The disease is associated with an inability to exert force during movement, and the associated muscles become increasingly atrophied, ultimately leading to impaired daily activities (29). Based on the severity of arthritis, middle-aged and older adults should have early prevention, diagnosis, control, and scientific comprehensive management of arthritis in order to alleviate its impact on ADL impairment.
By examining subgroups of middle-aged and older persons, the research revealed that only the middle-aged group suffered from heart disease and that only the middle-aged and young older adult groups were at higher risk of developing impaired ADL. This clue indicates that younger people with heart disease and arthritis are more likely to have impaired ADL, and previous studies have also reached similar conclusions (32, 33). In the future, the preventive intervention of heart disease and arthritis among the younger population should be further strengthened to reduce the incidence of the diseases in order to delay and control ADL impairment. Heart disease and arthritis were not significantly associated with impaired ADL in the older age group, this may be due to the health-selective effect of death on older age group, and those who manage to live to an advanced age are usually the healthier older people in their cohort. In addition, the study found that middle-aged and older adults with chronic diseases were at increased risk of impaired ADL, and that the risk increased with the number of diseases, which is consistent with previous findings (8). Middle-aged and older adults with impaired functioning and multiple chronic diseases require more health care services and financial support (34), which imposes a significant financial, illness, and emotional burden on individuals, families, and society. Therefore, prevention, diagnosis, treatment, and management of chronic diseases in middle-aged and older adults are necessary to delay ADL impairment.
Unlike previous studies that used a cross-sectional study design (16), the present study used a large-scale population as the study population and adopted a prospective cohort study method to dynamically collect ADL impairment in middle-aged and older adults, to more reasonably evaluate the relationship between suffering from chronic diseases and ADL impairment from a temporal perspective, and to provide reliable evidence for slowing down and controlling ADL impairment in middle-aged and older adults in China. This study also has some limitations; information on the prevalence of chronic diseases and ADL impairment was obtained by self-report, which may be subject to recall bias. However, the present study was able to reduce recall bias to a greater extent by using a scientific and well-recognized scale to measure ADL impairment in middle-aged and older adults and by using self-reported illnesses diagnosed by healthcare institutions as the study factor (14). Therefore, the likelihood of recall bias is small, and the results have a certain degree of reliability.
In summary, this study found that hypertension is a risk factor for impaired ADL in all age groups, so increasing the rate of awareness, treatment, and control of hypertension is very important for delaying impaired ADL and improving the quality of life in middle-aged and older adults. Additionally, it was discovered in the investigation of the association between the number of chronic diseases and ADL impairment that the presence of chronic diseases increased the risk of ADL impairment in both the middle-aged group (45–59 years old) and the older adult group (60–74 years old), and that the risk increased as the number of diseases increased. Therefore, the prevention and management of chronic diseases in middle-aged and older adults should be strengthened, which is of great public health significance in reducing the risk of ADL impairment.
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
The studies involving human participants were reviewed and approved by Ethical Review Committee of Peking University. The patients/participants provided their written informed consent to participate in this study. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required from the participants or the participants' legal guardians/next of kin because the large-scale study organized by the government obtained informed consent from the participants. Written informed consent was not obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article because the large-scale study organized by the government obtained informed consent from the participants.
ZA: Conceptualization, Data curation, Formal analysis, Methodology, Software, Writing—original draft. CT: Formal analysis, Methodology, Writing—review & editing. XW: Data curation, Writing—review & editing. ST: Funding acquisition, Resources, Supervision, Validation, Visualization, Writing—review & editing. KK: Formal analysis, Methodology, Writing—review & editing.
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This study was funded by the Comprehensive Research on the Integrated Prevention and Control Strategy of the COPD (Chronic Obstructive Pulmonary Disease) Population Medicine Model in Yunnan Province (No. 2022-DFZD-30) and Specialty Discipline Development Plan of Kunming Medical University - Public Health and Preventive Medicine (No. J1301902).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Dan L. Developmental status, causes and countermeasures of population ageing in China. Chin J Gerontol. (2022) 42:4123–6.
2. Xia W, Feng P. Strengthening the construction of geriatrics to actively promote healthy aging. China Contemp Med. (2023) 30:4–6.
3. Huang J, Choi EPH, Chau PH. The impact of unmet needs for assistance with activities of daily living on the self-rated health and life satisfaction of Chinese community-dwelling older adults. Aging Ment Health. (2023) 27:803–10. doi: 10.1080/13607863.2022.2045563
4. The World Health Organization. Global Report on Health Equity for Persons With Disabilities. (2022). Available online at: https://www.who.int/publications/i/item/9789240063600 (accessed December 17, 2023).
5. The World Health Organization. WHO launches free OpenWHO.org training on rehabilitation for COVID-19. (2021). Available online at: https://www.who.int/news/item/05-02-2021-who-launches-free-openwho.org-training-on-rehabilitation-for-covid-19 (accessed December 17, 2023).
6. Liu H, Wang M. Socioeconomic status and ADL disability of the older adults: Cumulative health effects, social outcomes and impact mechanisms. PLoS ONE. (2022) 17:e0262808. doi: 10.1371/journal.pone.0262808
7. Zhang Y, Xiong Y, Yu Q, Shen S, Chen L, Lei X. The activity of daily living (ADL) subgroups and health impairment among Chinese elderly: a latent profile analysis. BMC Geriatr. (2021) 21:30. doi: 10.1186/s12877-020-01986-x
8. Böhner ES, Spek B, Joling KJ, Zwaagstra Y, Gerridzen IJ. Factors associated with ADL dependence in nursing home residents with Korsakoff's syndrome and other alcohol-related disorders: an explorative cross-sectional study. J Clin Med. (2023) 12:2181. doi: 10.3390/jcm12062181
9. Jiang H, Liu Z. Community home elderly care services, multidimensional health and social participation of chronically ill Elderly-Empirical analysis based on propensity score matching and multiple mediation analysis. Front Public Health. (2023) 11:1121909. doi: 10.3389/fpubh.2023.1121909
10. Xuan Z, Aiyun C. Implications of foreign classical chronic disease management models for chronic disease management in China. Chin Fam Med. (2023) 26:21–6.
11. Ng M, Fleming T, Robinson M, Thomson B, Graetz N, Margono C, et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. (2014) 384:766–81. doi: 10.1016/S0140-6736(14)60460-8
12. He Y, Gao YL, Jin YX Yu B, Zhang XH, Huang J, Hu Y, et al. Analysis of factors associated with impaired daily living ability in hospitalised elderly patients. Chin J Geriatric Multiorgan Dis. (2018) 17:53–6.
13. Prasad A, Shellito N, Alan Miller E, Burr JA. Association of chronic diseases and functional limitations with subjective age: the mediating role of sense of control. J Gerontol B Psychol Sci Soc Sci. (2023) 78:10–9. doi: 10.1093/geronb/gbac121
14. Ai Z, Tang C, Peng P, Wen X, Tang S. Prevalence and influencing factors of chronic pain in middle-aged and older adults in China: results of a nationally. Front Public Health. (2023) 11:1110216. doi: 10.3389/fpubh.2023.1110216
15. Katz S. Assessing self-maintenance: activities of daily living, mobility, and instrumental activities of daily living. J Am Geriatr Soc. (1983) 31:721–7. doi: 10.1111/j.1532-5415.1983.tb03391.x
16. Jing C, Caohui D. Factors influencing daily activity ability of Chinese older adults-analysis based on CHARLS data. Public Health Prev. Med. (2017) 3:68–71.
17. Wan HY. Application of Bayesian Network to Establish a Benign and Malignant Prediction Model for Isolated Pulmonary Nodules. Jinzhong: Shanxi Medical University (2022).
18. Wang RF, Luo Y, Chen ZS, Huang ZT, Su HX, Xu HW, et al. Relationship between cardiac metabolic co-morbidities and disability in Chinese middle-aged and elderly people. J Jilin Univ. (2021) 47:761–9.
19. Caskie GI, Sutton MC, Margrett JA. The relation of hypertension to changes in ADL/IADL limitations of Mexican american older adults. Gerontol B Psychol Sci Soc Sci. (2010) 65B:296-305. doi: 10.1093/geronb/gbq001
21. Danaei G, Finucane MM, Lin JK, Singh GM, Paciorek CJ, Cowan MJ, et al. National, regional, and global trends in systolic blood pressure since 1980: systematic analysis of health examination surveys and epidemiological studies with 786 country-years and 2,000 years: systematic analysis of health examination surveys and epidemiological studies with 786 country-years and 5-4 million participants. Lancet. (2011) 377:568–77. doi: 10.1016/S0140-6736(10)62036-3
22. National Health Commission. Report on nutrition and chronic disease status of Chinese residents 2020. J Nutr. (2020) 42:521.
23. Akasaki Y, Tabira T, Maruta M, Makizako H, Miyata M, Han G, et al. Social frailty and meaningful activities among community-dwelling older adults with heart disease. Int J Environ Res Public Health. (2022) 19:15167. doi: 10.3390/ijerph192215167
24. Liperoti R, Vetrano DL, Palmer K, Targowski T, Cipriani MC, Lo Monaco MR, et al. association between frailty and ischemic heartdisease: a systematic review and meta-analysis. BMC Geriatr. (2021) 21:357. doi: 10.1186/s12877-021-02304-9
25. Junbo G. Definition and scope of structural heart disease and its present and future. Shanghai Med. (2021) 4:217–20.
26. Wang T, Zhao Z, Yu X, Zeng T, Xu M, Xu Y, et al. Age-specific modifiable risk factor profiles for cardiovascular disease and all-cause mortality: a nationwide, population-based, prospective cohort study. Lancet Reg Health West Pac. (2021) 17:100277. doi: 10.1016/j.lanwpc.2021.100277
27. Li-Rong C, Wu R, Zheng J-J, Pan Y-K, An B-C. Effect of knee osteoarthritis on balance in older adults. Nurs Res. (2016) 11:1385–7.
29. Ching ai J. The Dangers of Arthritis Should Not Be Ignored. The Danger of Arthritis Cannot Be Ignored. Hebei Daily (2015).
30. De Matos O, Ruthes EMP, Lenardt BCC, Beira de Andrade A, PetroskiCA, de Mello MF, et al. Relationship between postural changes, osteoarthritis and bone mineral density in postmenopausal women. Gynecol Endocrinol. (2022) 38:983–7. doi: 10.1080/09513590.2022.2126454
31. Michelena X, Poddubnyy D, Marzo-Ortega H. Axial psoriatic arthritis: a distinct clinical entity in search of a definition. Rheum Dis Clin North Am. (2020) 46:327–41. doi: 10.1016/j.rdc.2020.01.009
32. Zhang B, Zhang H, Xu H, Wu Y. P2744Age distribution of valvular heart disease in China: from a national multicenter prospective cohort study. Eur Heart J. (2019) 40 (Suppl. 1). doi: 10.1093/eurheartj/ehz748.1061
33. Cao F, Li DP, Wu GC, He YS, Liu YC, Hou JJ, et al. Global, regional and national temporal trends in prevalence for musculoskeletal disorders in women of childbearing age, 1990-2019: an age-period-cohort analysis based on the Global Burden of Disease Study 2019. Ann Rheum Dis. 83:121–32. doi: 10.1136/ard-2023-224530
Keywords: chronic diseases, activities of daily living, middle-aged and older adults, cohort study, China
Citation: Ai Z, Tang C, Wen X, Kartheepan K and Tang S (2024) Examining the impact of chronic diseases on activities of daily living of middle-aged and older adults aged 45 years and above in China: a nationally representative cohort study. Front. Public Health 11:1303137. doi: 10.3389/fpubh.2023.1303137
Received: 27 September 2023; Accepted: 19 December 2023;
Published: 14 February 2024.
Edited by:
Evelyn Frias-Toral, Catholic University of Santiago de Guayaquil, EcuadorReviewed by:
Tania Abril, Universidad Católica de Santiago de Guayaquil, EcuadorCopyright © 2024 Ai, Tang, Wen, Kartheepan and Tang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Songyuan Tang, dHN5dGhhaWxhbmRAaG90bWFpbC5jb20=
†These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.