Abstract
Introduction:
During the pandemic, the Cognitive Disorders Unit of San Raffaele Hospital (Milan, Italy) offered patients the opportunity to undergo neuropsychological evaluations and cognitive training through telemedicine.
Method:
We conducted an investigation to assess how patients responded to this option and to determine if telemedicine could ensure continuity of care.
Results:
Between October 2019 and May 2022, a total of 5,768 telemedicine appointments and 8,190 in-person outpatient appointments were conducted, resulting in an increase in the rate of telemedicine activity from 16.81% in January 2020 to 23.21% in May 2022. Peaks in telemedicine activity reached 85.64% in May 2020 and 83.65% in February 2021, both representing a significant portion of the total activity. Interestingly, there was a notable positive correlation between telemedicine activity and the worsening of the Italian pandemic (r = 0.433, p = 0.027).
Discussion:
During the peaks of contagion, the total number of visits remained stable, highlighting that telemedicine effectively served as a valuable and efficient tool to ensure continuity of care for vulnerable patients. This was evident from the integration of remote visits with in-person appointments.
Introduction
During the COVID-19 pandemic, issues related to discontinuing care have arisen due to hospitals needing to close numerous clinical departments and allocate most beds to COVID-19 patients. Furthermore, because of the emergency, many outpatient clinics were either closed for months or limited their services to emergencies only. To address these interruptions, the use of telemedicine was expanded, alongside digital solutions and advanced technology interfaces (1, 2). Telemedicine, along with tools rooted in artificial intelligence, big data analytics, and mobile tracing apps for surveillance, was extensively utilized globally for diagnosing, preventing, monitoring, and treating individuals (3, 4). Concomitantly with the drastic reduction in outpatients appointments, there has been a surge in the utilization of remote consultations (5). Patients, caregivers and clinicians rated the use of telemedicine during the recent pandemic as highly satisfactory (6). Consequently, the majority of patients and healthcare providers expressed a willingness to continue using telemedicine even after the pandemic (7, 8).
In 2019, before the onset of the COVID-19 pandemic, the Cognitive Disorders Unit at San Raffaele Hospital (Milan, Italy) had established telemedicine services for conducting remote neuropsychological evaluations and cognitive training. This service was offered to patients already undergoing treatment at our Institute, primarily those receiving care for dementia and acquired brain injuries. Dementia currently stands as the seventh leading cause of death worldwide and significantly contributes to disability and dependency among older populations. The statistics regarding dementia and its impact on patients, their families, and the entire healthcare system are staggering (9). Evidence reveal escalating pressures on families and caregivers, both emotionally and financially, alongside substantial financial strains on the entire healthcare system (10). Hence, telemedicine services represent an innovative solution that lessens the burden on patients’ support networks, is more environmentally friendly, and incurs reduced costs compared to in-person appointments (11–13). While further investigations are necessary to gauge the environmental impact and social costs, telemedicine has been reported as a feasible approach to assist individuals with dementia stay connected to their service providers amid the pandemic (14). The usability and efficacy of teleneuropsychology assessments and training have already been investigated (15–18). Data reported in the litterature showed good evidence for the validity of teleneuropsychology assessments in older adults and an efficacy of telecognitive rehabilitation at least as strong as face-to-face cognitive training. Additionally, prior studies have already indicated that both patients and clinicians found teleneuropsychology services satisfactory during the COVID-19 pandemic (8, 19). It is now accepted that telemedicine is useful but not sufficient and should not replace in-patient services but should complement traditional visits (7). More information should be collected regarding the integration of teleneuropsychology services into traditional care and how patients might respond to such offerings, especially in challenging situations like during a pandemic.
In this study, our primary objectives were to assess patients’ receptiveness to telemedicine services provided by the Cognitive Disorders Unit during the COVID-19 pandemic, investigate potential disruptions in continuity of care due to the various pandemic waves, and determine patients’ preferences continued telemedicine use versus returning to in-person outpatient care. This was particularly considered in light of the pandemic’s reduced impact in Italy since spring 2022.
Materials and methods
Telemedicine and outpatients’ clinic activity
We performed a retrospective analysis of telemedicine and outpatient clinic appointments administered by the Cognitive Disorders Unit at the San Raffaele Scientific Institute in Milan, Italy, between October 1st, 2019, and May 30th, 2022, as our primary outcome. Throughout this entire period, patients were given the option to receive care either in the outpatient clinic or through telemedicine. Despite the closure of numerous outpatient clinics and the reduced activity of others within our Institute, the Neuropsychology Service remained accessible to patients throughout the pandemic. The only prerequisite for patients to qualify for telemedicine was that they had previously undergone at least one neurological visit and one neuropsychological evaluation in the outpatient clinic. The telemedicine and outpatient clinic appointments considered in this study encompassed neuropsychological evaluations for patients’ follow-up and cognitive training sessions.
Telemedicine appointments were conducted remotely using video-conferencing software provided by our Institute, ensuring utmost confidentiality and privacy in a designated private room. Notably, patients who had tested positive for SARS-CoV-2 within the last 14 days were temporarily restricted from accessing the outpatient clinic during this period to mitigate the risk of contagion. The study was approved by the local Ethics committee of the San Raffaele Hospital (protocol number: PROTECT-COVID).
Correlations with the pandemic severity
As a secondary outcome, we correlated the severity of the Italian pandemic situation, extracted from the number of symptomatic patients hospitalized with SARS-CoV-2 in Italy from February 2020 to May 2022 (20), with the numbers of telemedicine and outpatients’ clinic appointments.
Statistical analyzes
First, we calculated the monthly percentage change (MPC) for both the outpatients and telemedicine activity time series with respective bootstrapped confidence interval (CI 95%) to explore the temporal trend of the two time series during the COVID-19 pandemic (February 2020 to May 2022).
Second, to test whether observed variations in the number of cases in the telemedicine activity series and the number of cases outpatient activity series shared any temporal association, a cross-spectral analysis was performed. A bivariate model was fitted to the time series during the COVID-19 pandemic (February 2020 to May 2022) to quantify the frequency-related squared coherence (i.e., the strength of dependency between the two time series at a particular period) and phase shift between in person medicine (the independent variable) and telemedicine (the dependent variable). The spectral estimates were smoothed with a Hamming window of width 5.
Third, a bivariate correlation analysis with bootstrapping (n = 5,000 samples) was run to assess the relationships between the volume of telemedicine appointments and the severity of the pandemic,. To ensure the validity of our analyzes, we also performed analyzes of variance with the Levene Test for Equality of Variances. Statistical significance was determined at a threshold of p < 0.05. All data analyzes were carried out using the commercially available IBM SPSS Statistics version 23 (IBM Corp. ©) software.
Results
Between October 1st, 2019, and May 30th, 2022, 225 patients benefited from neuropsychological evaluations or cognitive training and were included in the analyzes (103 Female, mean age 71.53 ± 15.36 years). The patient’s population consisted in post-traumatic disorders (8%), post-stroke patients (23%) and dementia patients (69%) (Alzheimer’s disease, Mild Cognitive Impairment, Frontotemporal Dementia, Lewy Body Dementia).
A total of 13,958 treatments were included in the analyzes: 2,512 neuropsychological evaluations (18% of the total treatments) and 11,446 cognitive training (82% of the total treatments). Among these 13,958 treatments, 5,768 appointments were conducted in telemedicine and 8,190 in-person appointments were conducted in the outpatients’ clinic.
During this period, the rate of telemedicine activity increased from 16.81% in January 2020 to 23.21% in May 2022. Peaks in telemedicine activity reached 85.64% in May 2020 and 83.65% in February 2021 (Table 1).
Table 1
| Telemedicine | Outpatients clinic | |||
|---|---|---|---|---|
| Number of visits | Percentage of total activity (%) | Number of visits | Percentage of total activity (%) | |
| October ‘19 | 40 | 8.47 | 432 | 91.53 |
| November ‘19 | 60 | 11.67 | 454 | 88.33 |
| December ‘19 | 80 | 17.13 | 467 | 82.87 |
| January ‘20 | 80 | 16.81 | 396 | 83.19 |
| February ‘20 | 160 | 24.92 | 482 | 75.08 |
| March ‘20 | 161 | 38.80 | 254 | 61.20 |
| April ‘20 | 201 | 72.04 | 78 | 27.96 |
| May ‘20 | 310 | 85.64 | 52 | 14.36 |
| June ‘20 | 183 | 74.09 | 64 | 25.91 |
| July ‘20 | 123 | 64.40 | 68 | 35.60 |
| September ‘20 | 128 | 33.16 | 258 | 66.84 |
| October ‘20 | 132 | 29.01 | 323 | 70.99 |
| November ‘20 | 168 | 42.00 | 232 | 58.00 |
| December ‘20 | 270 | 71.05 | 110 | 28.95 |
| January ‘21 | 302 | 74.02 | 106 | 25.98 |
| February ‘21 | 440 | 83.65 | 86 | 16.35 |
| March ‘21 | 280 | 76.09 | 88 | 23.91 |
| April ‘21 | 228 | 71.47 | 91 | 28.53 |
| May ‘21 | 192 | 65.31 | 102 | 34.69 |
| June ‘21 | 242 | 48.21 | 260 | 51.79 |
| July ‘21 | 122 | 27.60 | 320 | 72.40 |
| September ‘21 | 142 | 33.18 | 286 | 66.82 |
| October ‘21 | 166 | 34.87 | 310 | 65.13 |
| November ‘21 | 263 | 52.29 | 240 | 47.71 |
| December ‘21 | 286 | 48.31 | 306 | 51.69 |
| January ‘22 | 181 | 30.83 | 406 | 69.17 |
| February ‘22 | 206 | 33.17 | 415 | 66.83 |
| March ‘22 | 180 | 29.80 | 424 | 70.20 |
| April ‘22 | 186 | 29.15 | 452 | 70.85 |
Telemedicine and outpatients’ clinic activity, over time.
In-person appointments in the outpatients’ clinic had a greater variability compared to telemedicine appointments, especially during the year 2020, as shown by the standard deviations analyzes (in-person appointments sd = 143.13 vs. telemedicine sd = 76.30, p = 0.017) (Figure 1).
Figure 1
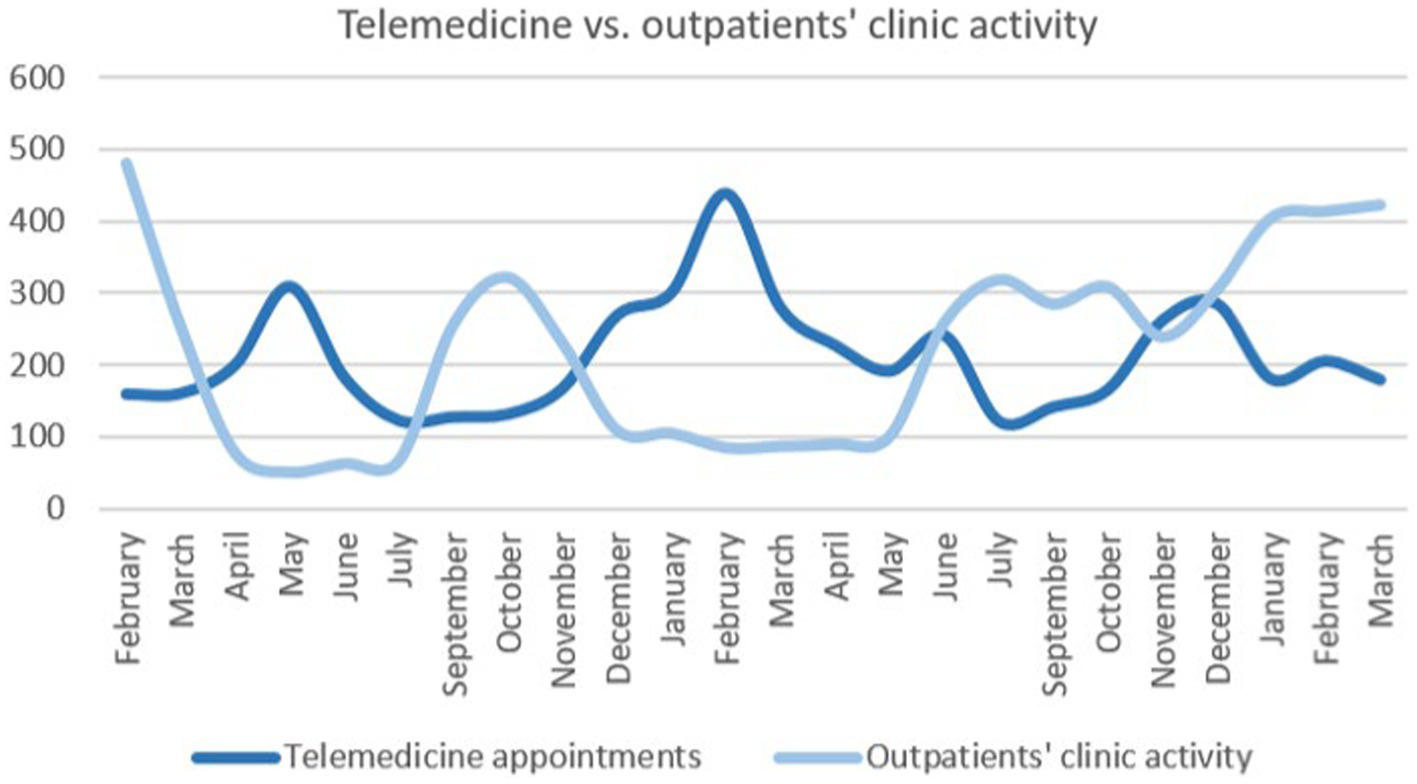
Telemedicine and outpatients’ clinic activity. It shows the evolution of telemedicine appointments (dark blue) and outpatients’ clinic activity (light blue) during the COVID-19 pandemic (February 2020 to May 2022).
The monthly percentage change index for the outpatients (mean percentage variation = 13.83; 95% CI: −8.58, 42.67) and telemedicine activity series (mean percentage variation = 5.14%; 95% CI: −6.43, 16.46) during the COVID-19 pandemic, shows a positive trend concerning telemedicine continuity and utility.
The bivariate spectral analysis yielded a significant common movement in the two series, with a significant peak involving a squared coherence of 0.421 (p = 0.032; phase angle, 3.03 radian) (see Figure 2), corresponding to a Fourier period of 5.2 months and with a 2.5-month lead relationship between the two time series.
Figure 2
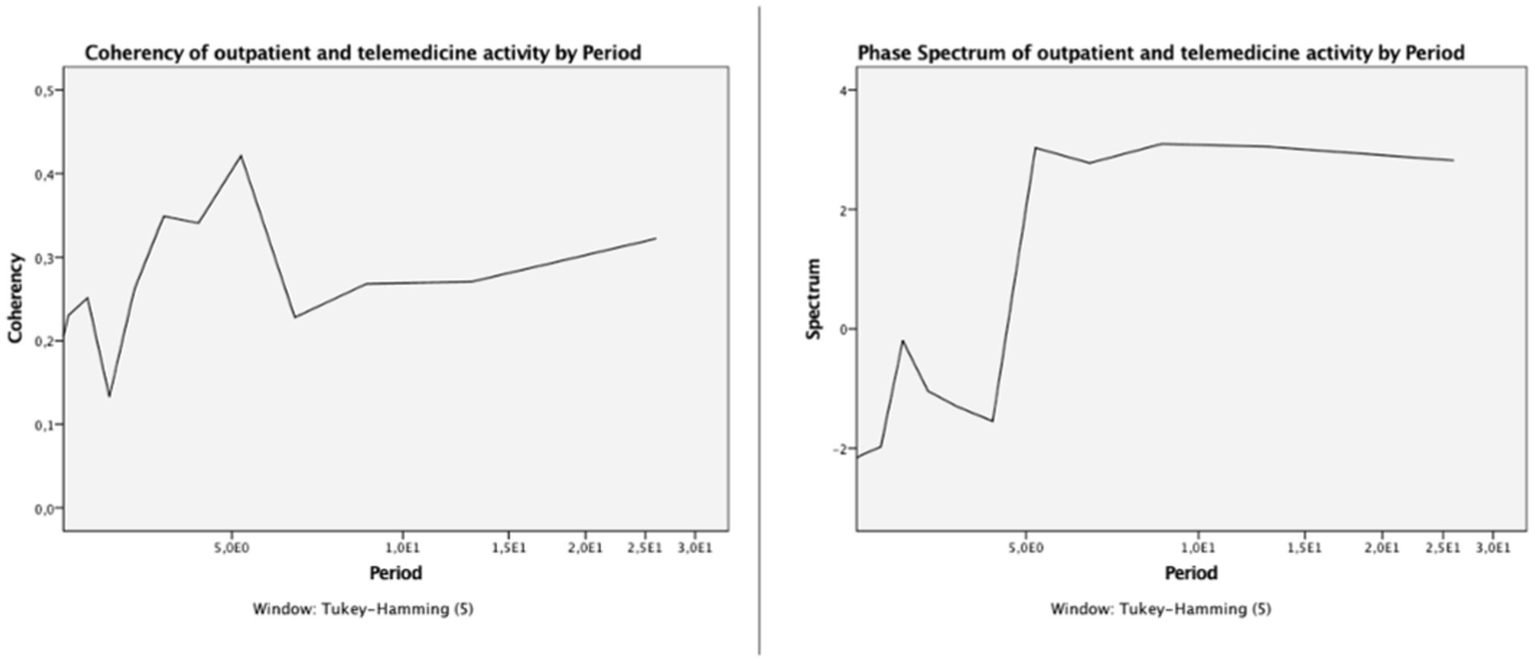
Coherency spectrum (left panel) and Phase Spectrum of outpatient and telemedicine activity during the COVID-19 pandemic (February 2020 to May 2022).
There was a significant positive correlation (r = 0.354, p = 0.038) between the number of telemedicine appointments and pandemic worsening expressed as the number of symptomatic patients hospitalized with SARS-CoV-2 in Italy (Figure 3).
Figure 3
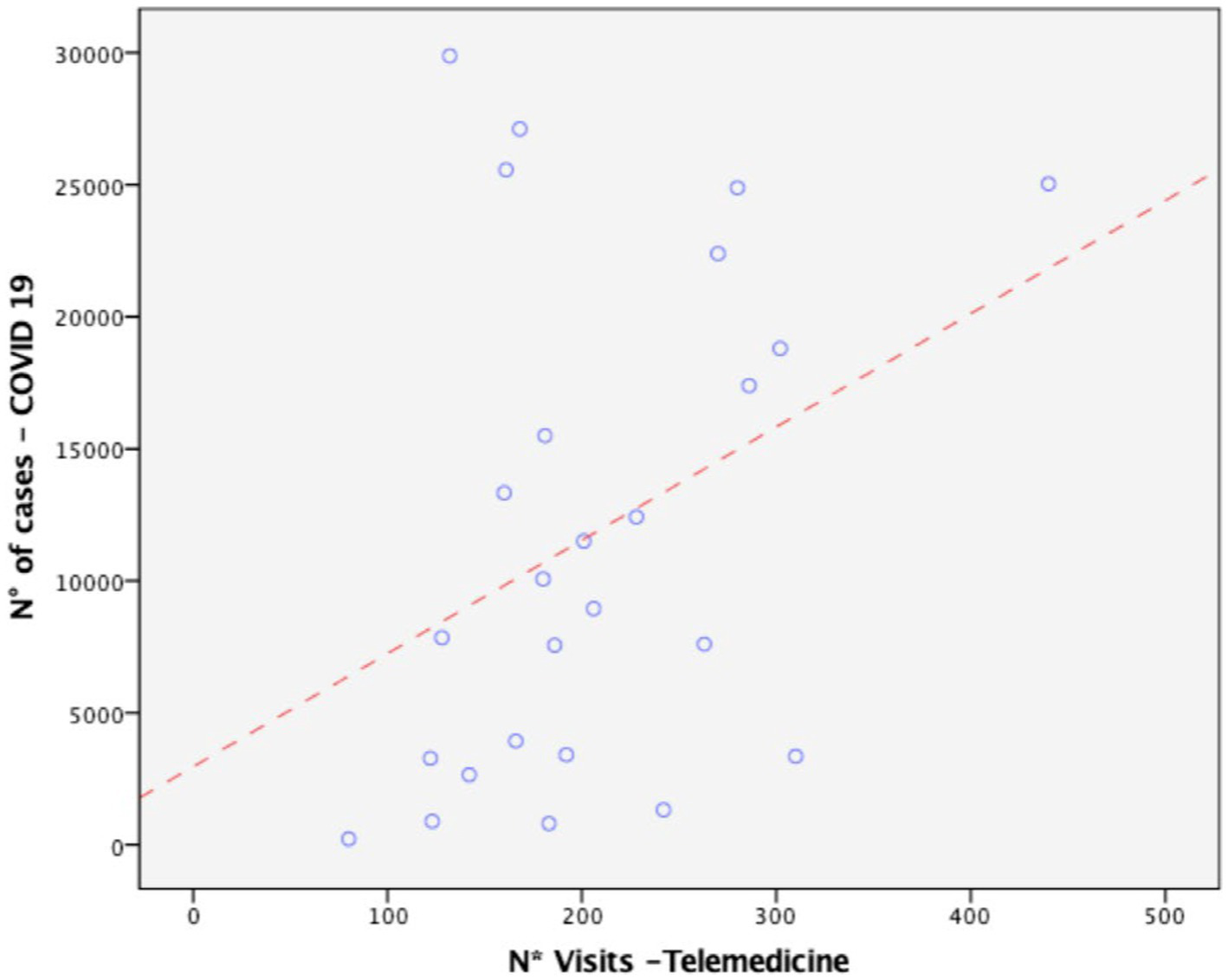
Positive association between telemedicine activity and the severity of the COVID-19 pandemic in Italy.
The first two peaks of SARS-CoV-2 contagion (March 2020 and November 2021) were immediately followed by an increase in telemedicine appointments. Strikingly, patients were faster to switch from in-person to telemedicine appointments at the third worsening of the Italian pandemic situation. This was reflected by the rise in telemedicine activity preceding the third peak of the pandemic, in Italy (Figure 4).
Figure 4
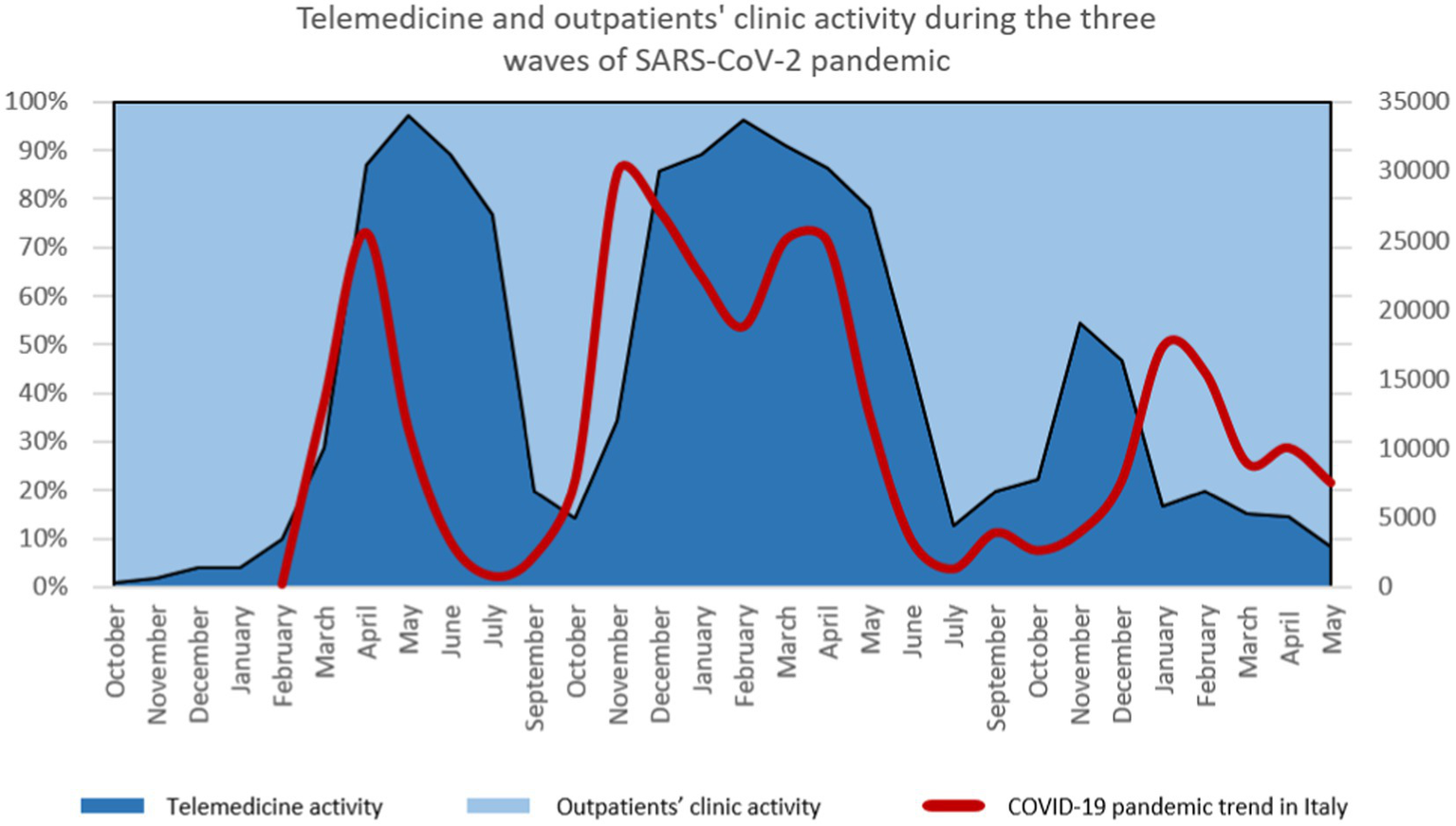
Telemedicine activity and pandemic trend in Italy. Percentages of telemedicine appointments (dark blue) and percentages of outpatients’ clinic appointments (light blue) are expressed and superimposed with the pandemic trend in Italy (red line), expressed as the numbers of hospitalized COVID-19 patients with symptoms over the national Italian territory.
Discussion
In recent years, teleneuropsychology has been recognized as a valid tool for patients’ assessments (16, 21, 22) and cognitive training (17, 18). we demonstrated how patients with dementia transitioned between modalities, moving from face-to-face visits to telemedicine and back to face-to-face appointments, depending on the severity of the pandemic situation. This suggests that telemedicine has the potential to become an integrated component of clinical practice for neuropsychology services. Our results showed that patients preferred telemedicine appointments during the difficult times of the pandemic, as reflected by a significant squared coherence peak and phase angle in the spectrum, mirroring a significant jointly cyclical variation between outpatients’ and telemedicine activity corresponding with the COVID-19 pandemic cycle. Importantly, our data revealed that the total number of patients under our Unit’s care remained consistent over the past 2 years. This suggests that telemedicine can facilitate continuity of care for these vulnerable and aging patients, especially during challenging periods when accessing outpatient clinics becomes difficult. Telemedicine activity increased in parallel with the severity of the pandemic, as shown by the positive association between telemedicine activity and the severity of the COVID-19 pandemic in Italy. Indeed, during the first two waves of the pandemic, the rise in telemedicine appointments immediately followed the pandemic curve. These data showed how fast the Cognitive Disorders Unit could propose alternative treatments’ modality to patients and how patients positively responded to these offers. During the peaks of contagion, our Institute restricted access to outpatient clinics, but the Cognitive Disorders Unit remained open to patients throughout the pandemic. Patients were consistently provided with the option to choose between in-person and telemedicine appointments. Between the pandemic waves, patients notably preferred returning to the hospital, continuing their treatments in person at the outpatient clinic. These findings demonstrate that even during the pandemic, every patient was able to continue their treatment plan, and patients adapted effectively to the new system, ensuring a consistent continuity of care.
Interestingly, during the third wave of the pandemic in Italy, patients anticipated the increase in contagions. They made the decision, as soon as the pandemic curve began to rise again, to transition back to telemedicine appointments. This data indicates that telemedicine has become a natural choice for patients when deciding the modality of their visits (23). Nowadays, telemedicine should not be viewed merely as a replacement for outpatient visits; rather, it should be integrated into regular clinical practice, helping to provide a continuity of care and protection for vulnerable patients (7). In the patients’ and healthcare professionals’ minds, telemedicine was often perceived as an alternative or substitution of in-person appointments. Such dichotomie might create barriers in the clinical practice and might lead patients to mistrust this system. Telemedicine should be integrated as a supplementary element in clinical practice. The intensity, timing and specificity of the use of telemedicine should be personalized according to the patients diagnosis and condition. In the case of neuropsychological assistance of patients with dementia, our study suggests that telemedicine can be integrated with outpatients clinic activity. Study limitations lie in the fact that we did not investigate patients’ and caregivers’ satisfaction of the telemedicine services. Future studies should incorporate satisfactory questionnaires for both patients and caregivers, assessing the quality of neuropsychological services delivered via telemedicine and evaluating the usability of such services, including the telehealth technology.
Many efforts remain to be achieved by the healthcare systems to recognize this modality of treatment as such and implement reimbursements and payments for patients (23). Moreover, more studies are needed to define the best use of telemedicine according to the pathology being addressed. Our study showed how patients positively adhered to remote treatments for cognitive disorders. The manner in which patients transitioned back to outpatient clinic visits implies that telemedicine could be seamlessly integrated into patients’ routine care alongside in-person visits, ensuring comprehensive continuity of care. However, it’s essential to acknowledge that telemedicine might not be suitable for all conditions and there is still the need to define its best application.
Conclusion
Our study suggests that telemedicine might constitute an effective tool to promote continuity of care for patients with dementia during the pandemic. We showed that in a short period of time, patients fully adopted this modality of treatment, switching between telemedicine and outpatients’ clinic depending on the pandemic situation. To facilitate healthcare systems in providing financial support to clinics and patients for promoting telemedicine, further studies are imperative. These studies should evaluate the amount of energy saving, the social contribution and the improvements in quality of life of patients and caregivers that might be correlated to the use of telemedicine.
Statements
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by Ethics committee of the San Raffaele Hospital. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
DE: Formal analysis, Writing – original draft. EH: Writing – original draft, Writing – review & editing. PR: Data curation, Writing – review & editing. AZ: Project administration, Writing – review & editing. LB: Writing – review & editing. PC: Writing – review & editing. JP: Writing – review & editing. AT: Writing – review & editing. SI: Conceptualization, Data curation, Investigation, Writing – review & editing. FA: Conceptualization, Data curation, Investigation, Methodology, Resources, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1.
Arshad Ali S Bin Arif T Maab H Baloch M Manazir S Jawed F et al . Global interest in telehealth during COVID-19 pandemic: an analysis of Google trends™. Cureus. (2020) 12:e10487. doi: 10.7759/cureus.10487
2.
Fiani B Siddiqi I Lee SC Dhillon L . Telerehabilitation: development, application, and need for increased usage in the COVID-19 era for patients with spinal pathology. Cureus. (2020) 12:e10563. doi: 10.7759/cureus.10563
3.
Golinelli D Boetto E Carullo G Nuzzolese AG Landini MP Fantini MP . Adoption of digital Technologies in Health Care during the COVID-19 pandemic: systematic review of early scientific literature. J Med Internet Res. (2020) 22:e22280. doi: 10.2196/22280
4.
Gunasekeran DV Tseng RMWW Tham YC Wong TY . Applications of digital health for public health responses to COVID-19: a systematic scoping review of artificial intelligence, telehealth and related technologies. NPJ Digit Med. (2021) 4:40. doi: 10.1038/s41746-021-00412-9
5.
Omboni S Padwal RS Alessa T Benczúr B Green BB Hubbard I et al . The worldwide impact of telemedicine during COVID-19: current evidence and recommendations for the future. Connect Health. (2022) 1:7–35. doi: 10.20517/ch.2021.03
6.
Emedoli D Alemanno F Houdayer E Brugliera L Iannaccone S Tettamanti A . Mobile application tool for remote rehabilitation after discharge from coronavirus disease-19 rehabilitation unit. Healthc Technol Lett. (2022) 9:70–6. doi: 10.1049/htl2.12033
7.
Nanda M Sharma R . A review of patient satisfaction and experience with telemedicine: a virtual solution during and beyond COVID-19 pandemic. Telemed J E-Health Off J Am Telemed Assoc. (2021) 27:1325–31. doi: 10.1089/tmj.2020.0570
8.
Andrews E Berghofer K Long J Prescott A Caboral-Stevens M . Satisfaction with the use of telehealth during COVID-19: an integrative review. Int J Nurs Stud Adv. (2020) 2:100008. doi: 10.1016/j.ijnsa.2020.100008
9.
Alzheimer’s Association . 2009 Alzheimer’s disease facts and figures. Alzheimers Dement J Alzheimers Assoc. (2009) 5:234–70. doi: 10.1016/j.jalz.2009.03.001
10.
Grabher BJ . Effects of Alzheimer disease on patients and their family. J Nucl Med Technol. (2018) 46:335–40. doi: 10.2967/jnmt.118.218057
11.
Pickard Strange M Booth A Akiki M Wieringa S Shaw SE . The role of virtual Consulting in Developing Environmentally Sustainable Health Care: systematic literature review. J Med Internet Res. (2023) 25:e44823. doi: 10.2196/44823
12.
Ruggiero F Zirone E Molisso MT Carandini T Fumagalli G Pietroboni A et al . Telemedicine for cognitive impairment: a telephone survey of patients’ experiences with neurological video consultation. Neurol Sci Off J Ital Neurol Soc Ital Soc Clin Neurophysiol. (2023) 44:3885–94. doi: 10.1007/s10072-023-06903-9
13.
Patel KB Turner K Alishahi Tabriz A Gonzalez BD Oswald LB Nguyen OT et al . Estimated indirect cost Savings of Using Telehealth among Nonelderly Patients with Cancer. JAMA Netw Open. (2023) 6:e2250211. doi: 10.1001/jamanetworkopen.2022.50211
14.
Elbaz S Cinalioglu K Sekhon K Gruber J Rigas C Bodenstein K et al . A systematic review of telemedicine for older adults with dementia during COVID-19: an alternative to in-person health services?Front Neurol. (2021) 12:761965. doi: 10.3389/fneur.2021.761965
15.
Brearly TW Shura RD Martindale SL Lazowski RA Luxton DD Shenal BV et al . Neuropsychological test administration by videoconference: a systematic review and meta-analysis. Neuropsychol Rev. (2017) 27:174–86. doi: 10.1007/s11065-017-9349-1
16.
Marra DE Hamlet KM Bauer RM Bowers D . Validity of teleneuropsychology for older adults in response to COVID-19: a systematic and critical review. Clin Neuropsychol. (2020) 34:1411–52. doi: 10.1080/13854046.2020.1769192
17.
Manenti R Gobbi E Baglio F Macis A Ferrari C Pagnoni I et al . Effectiveness of an innovative cognitive treatment and telerehabilitation on subjects with mild cognitive impairment: a Multicenter, randomized, Active-Controlled Study. Front Aging Neurosci. (2020) 12:585988. doi: 10.3389/fnagi.2020.585988
18.
Cotelli M Manenti R Brambilla M Gobbi E Ferrari C Binetti G et al . Cognitive telerehabilitation in mild cognitive impairment, Alzheimer’s disease and frontotemporal dementia: a systematic review. J Telemed Telecare. (2019) 25:67–79. doi: 10.1177/1357633X17740390
19.
Parsons MW Gardner MM Sherman JC Pasquariello K Grieco JA Kay CD et al . Feasibility and acceptance of direct-to-home tele-neuropsychology services during the COVID-19 pandemic. J Int Neuropsychol Soc JINS. (2022) 28:210–5. doi: 10.1017/S1355617721000436
20.
Dati COVID-19 Italia (2022). Presidenza del Consiglio dei Ministri - Dipartimento della Protezione Civile. Available at: https://github.com/pcm-dpc/COVID-19
21.
Parks AC Davis J Spresser CD Stroescu I Ecklund-Johnson E . Validity of in-home Teleneuropsychological testing in the wake of COVID-19. Arch Clin Neuropsychol. (2021) 36:887–96. doi: 10.1093/arclin/acab002
22.
Harrell KM Wilkins SS Connor MK Chodosh J . Telemedicine and the evaluation of cognitive impairment: the additive value of neuropsychological assessment. J Am Med Dir Assoc. (2014) 15:600–6. doi: 10.1016/j.jamda.2014.04.015
23.
Ahmed S Sanghvi K Yeo D . Telemedicine takes Centre stage during COVID-19 pandemic. BMJ Innov. (2020) 6:252–4. doi: 10.1136/bmjinnov-2020-000440
Summary
Keywords
telemedicine, telerehabilitation, cognitive disorders, cognitive training, neuropsychology, COVID-19, continuity of care
Citation
Emedoli D, Houdayer E, Della Rosa PA, Zito A, Brugliera L, Cimino P, Padul JD, Tettamanti A, Iannaccone S and Alemanno F (2024) Continuity of care for patients with dementia during COVID-19 pandemic: flexibility and integration between in-person and remote visits. Front. Public Health 11:1301949. doi: 10.3389/fpubh.2023.1301949
Received
25 September 2023
Accepted
22 December 2023
Published
08 January 2024
Volume
11 - 2023
Edited by
Lauren Moo, United States Department of Veterans Affairs, United States
Reviewed by
Asos Mahmood, University of Tennessee Health Science Center (UTHSC), United States; Wioletta Anna Medrzycka-Dabrowska, Medical University of Gdansk, Poland
Updates
Copyright
© 2024 Emedoli, Houdayer, Della Rosa, Zito, Brugliera, Cimino, Padul, Tettamanti, Iannaccone and Alemanno.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Federica Alemanno, alemanno.federica@hsr.it
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.