- 1Ottawa Hospital Research Institute, Ottawa, ON, Canada
- 2School of Epidemiology and Public Health, University of Ottawa, Ottawa, ON, Canada
- 3Substance Use and Concurrent Disorders Program, Royal Ottawa Mental Health Centre, Ottawa, ON, Canada
- 4Department of Psychiatry, Faculty of Medicine, University of Ottawa, Ottawa, ON, Canada
- 5University of Ottawa Institute of Mental Health Research at the Royal, Ottawa, ON, Canada
- 6Department of Pharmacotherapy, College of Pharmacy, University of Utah, Salt Lake City, UT, United States
- 7Informatics, Decision Enhancement, and Analytics Sciences (IDEAS) Center, Veterans Affairs Salt Lake City Healthcare System, Salt Lake City, UT, United States
- 8Harrison College of Pharmacy, Auburn University, Auburn, AL, United States
- 9Department of Pharmaceutical Care, Pharmacoepidemiology and Statistics Research Center, Faculty of Pharmacy, Chiang Mai University, Chiang Mai, Thailand
- 10Mental Health Commission of Canada, Ottawa, ON, Canada
- 11School of Public Policy and Administration, Carleton University, Ottawa, ON, Canada
- 12Community Addictions Peer Support Association, Ottawa, ON, Canada
- 13Canadian Centre on Substance Use and Addiction, Ottawa, ON, Canada
- 14Children’s Hospital of Eastern Ontario Research Institute, Ottawa, ON, Canada
- 15Knowledge Institute on Child and Youth Mental Health and Addictions, Ottawa, ON, Canada
Introduction: Services to treat problematic alcohol use (PAU) should be highly accessible to optimize treatment engagement. We conducted a scoping review to map characteristics of services for the treatment of PAU that have been reported in the literature to be barriers to or facilitators of access to treatment from the perspective of individuals with PAU.
Methods: A protocol was developed a priori, registered, and published. We searched MEDLINE®, Embase, the Cochrane Library, and additional grey literature sources from 2010 to April 2022 to identify primary qualitative research and surveys of adults with current or past PAU requiring treatment that were designed to identify modifiable characteristics of PAU treatment services (including psychosocial and pharmacologic interventions) that were perceived to be barriers to or facilitators of access to treatment. Studies of concurrent PAU and other substance use disorders were excluded. Study selection was performed by multiple review team members. Emergent barriers were coded and mapped to the accessibility dimensions of the Levesque framework of healthcare access, then descriptively summarized.
Results: One-hundred-and-nine included studies reported an extensive array of unique service-level barriers that could act alone or together to prevent treatment accessibility. These included but were not limited to lack of an obvious entry point, complexity of the care pathway, high financial cost, unacceptably long wait times, lack of geographically accessible treatment, inconvenient appointment hours, poor cultural/demographic sensitivity, lack of anonymity/privacy, lack of services to treat concurrent PAU and mental health problems.
Discussion: Barriers generally aligned with recent reviews of the substance use disorder literature. Ranking of barriers may be explored in a future discrete choice experiment of PAU service users. The rich qualitative findings of this review may support the design of new or modification of existing services for people with PAU to improve accessibility.
Systematic Review Registration: Open Science Framework doi: 10.17605/OSF.IO/S849R.
1 Introduction
Alcohol consumption is a leading cause of death and disability, associated with numerous dose-dependent negative physical and mental health problems (1, 2) that contribute to a high global burden of disease (2). Despite disabling consequences at both individual and population levels, rates of treatment seeking for alcohol use disorder (AUD) and problematic alcohol use (PAU)—hereafter simply “PAU”—are remarkably low, globally, and have potentially declined over time (3, 4). In 2020, the COVID-19 pandemic exposed gaps in the continuum of PAU treatment services, raising concerns that reductions in treatment availability (5–10) would further decrease treatment seeking and engagement. To mitigate pandemic-related barriers, treatment delivery was modified in many countries to embrace telehealth options (11–18). However, for some treatment seekers, telehealth was challenging and was itself a barrier to treatment engagement (17). Comprehensive knowledge of the barriers to PAU treatment is necessary to develop mitigation strategies to improve the accessibility of existing treatment services, to guide future policy reform, and to establish resiliency in treatment accessibility during future unanticipated service disruptions.
Many factors can impede help-seeking and engagement in treatment for substance use problems, including individual, social, and structural barriers. At the individual level, lack of awareness or acceptance of the severity of the substance use problem (4, 19), belief in capacity to self-manage (4, 19), negative attitude toward treatment from past experience (4, 19), and negative emotional states, such as depression (20), can decrease the motivation to seek treatment. Social barriers, such as stigmatization of people who disclose their challenges with PAU (4, 19, 20), normalization of drinking (21), and sociocultural and gender norms regarding treatment seeking (4) also lower treatment seeking rates. Structural barriers to treatment accessibility encompass both policy-level barriers (e.g., coverage of PAU treatment by government and/or private insurance) and service-level barriers (e.g., fragmented treatment pathways, lengthy waiting periods (22–26)). Service-level barriers can be wide ranging, including treatment seekers not knowing where to access care; lack of treatment services in a given region; lack of sufficient service supply, which leads to long wait times; inappropriateness of services for some demographics; and a limited range of treatment options. Accessibility may be challenging due to practical issues, such as inflexible or inconvenient appointment times, and problems with cost, transportation, or childcare. Service restrictions to certain demographics (e.g., men-only mutual aid groups) and lack of cultural sensitivity and safety in treatment programs (e.g., for Indigenous people and other ethno-cultural groups) can further exclude or dissuade treatment seekers. Behavior change theories suggest that environmental factors, such as service-level barriers, can decrease engagement in treatment, even when the necessary positive attitude toward the behavior (i.e., engagement in treatment), social factors, and the skills and capacity required to perform the behavior are all present (27, 28). Thus, for people with PAU, real or perceived service-level barriers decrease treatment engagement, even when motivation to change drinking behavior is high (29). Identifying modifiable treatment barriers at the service level is important for developing strategies to improve treatment uptake among people with PAU. To address this important objective, we addressed the following question using a scoping review approach:
What characteristics of services for the treatment of PAU have been identified in the literature as barriers to or facilitators of access to the services from the perspective of the individuals with PAU?
2 Methods and analysis
We used a scoping review approach to identify and map existing evidence related to the review question above (30). The scoping review was underpinned by the Arskey and O’Malley (31) framework and was guided by methodology provided by the Joanna Briggs Institute (JBI) (32) and other sources (33–35). Reporting has been guided by the Preferred Reporting Items for Systematic reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR) (36) (Supplementary Table 1), as well as the Enhancing Transparency in Reporting the Synthesis of Qualitative Research (ENTREQ) guidelines (37) (Supplementary Table 1). The methods reported below include amendments that were made during the scoping review process. For transparency, we describe these amendments along with rationale in Supplementary Table 2.
2.1 Protocol and registration
A review protocol was published (38) and registered with the Open Science Framework (doi:10.17605/OSF.IO/S849R).
2.2 Eligibility criteria
Review eligibility criteria were based upon the PCC (Participants – Concept – Context) framework (32).
2.2.1 Participants
We included studies that enrolled service users, which were defined as adults (18+ years), with current or past PAU of any definition that requires/required treatment, as determined by the individual (i.e., treatment seeking) or another actor (e.g., study investigators, primary healthcare, criminal justice system). Subgroups of service users were of interest, including Indigenous peoples and other ethno-cultural groups, individuals with PAU and concurrent mental health conditions (“dual diagnoses”), sex and gender subgroups, older adults, and others. Because different factors may influence access to treatment for PAU, substance use disorders (SUDs), and mental health conditions, we excluded studies of (1) people with concurrent PAU and other SUDs, unless they also had a concurrent mental health condition; (2) mixed populations of (a) people with PAU and people with other SUDs and (b) people with and people without PAU, unless relevant findings were reported separately for the former. Studies of people with/without PAU were included if they assessed a PAU screening intervention. Studies including both service users and service providers were included if relevant findings specific to the service users were reported.
2.2.2 Concept
• Research design criteria: We included qualitative and cross-sectional primary research studies designed to identify modifiable characteristics (i.e., can be altered to mitigate a barrier) of PAU services that service users perceived to be barriers to or facilitators of access to the services.
“Access” was restricted to the search for treatment and initiation of treatment (or screening), including referral to specialist care. We did not consider either the period between a recognized desire for treatment and the subsequent search for care or the continuation of care once it had been initiated to be part of access (39).
• Intervention criteria: Both psychosocial and pharmacologic interventions were of interest.
o Psychosocial: Screening for PAU, either standalone or in combination with brief intervention and/or referral (i.e., SBIRT), brief interventions, mutual aid groups (e.g., 12-step groups), self-help (e.g., online programs, books), cognitive behavioral therapy (CBT), motivational interviewing, contingency management, family-based therapy, mindfulness-based interventions, motivational enhancement therapy, community reinforcement therapy, etc.
o Pharmacologic: Naltrexone, acamprosate, disulfiram, gabapentin, topiramate, baclofen, ondansetron.
Screening and SBIRT for PAU were considered relevant treatment services because they are often the initial point of access with the treatment system. Treatment of acute withdrawal symptoms was not relevant unless concurrent with a relevant psychosocial or pharmacologic intervention.
• Setting/context criteria: Service delivery could occur in any context, such as clinical (e.g., emergency department (ED), primary care, specialist clinics, live-in/hospital) or non-clinical (e.g., workplace settings, police custody/detention facilities, college/university) settings, including both in-person and virtual (i.e., telephone, video) services.
• Data criteria: To be eligible, studies must have reported at least one potentially modifiable characteristic of a PAU service that was perceived to be a barrier or facilitator of accessibility (e.g., appointment hours, cost, location) and that was identified through qualitative data (interview or focus group) or survey data analysis. Any primary study design was relevant; however, routinely collected administrative data and data from patient medical records were excluded. Interview studies with fewer than 13 participants were excluded, unless reporting a claim of data saturation (40).
• Barriers related to service users’ capacities were relevant if they corresponded to modifiable service-level factors (e.g., service user inability to afford treatment corresponded to treatment cost as a service-level barrier). However, factors related to the service user (e.g., readiness to change, lack of recognition/acknowledgment of a problem), the healthcare system/government (e.g., lack of government insurance coverage), and society (e.g., stigma, social norms of drinking) were not relevant.
• Studies were excluded if they reported only characteristics of specific interventions that could not be generalized to other interventions (e.g., elements of the user interface of mobile apps).
2.2.3 Context
We decided a priori to focus on literature published from 2010 to present (including pandemic-related studies), given that provision of PAU services has changed over time and these changes may have influenced the perceived barriers to and facilitators of access (e.g., increased provision of virtual care). All geographic areas were of interest; however, we limited inclusion to studies published in English and French due to time and resource constraints. We excluded conference abstracts, letters, and commentaries, given the low likelihood of sufficient reporting for our purposes. Systematic reviews, rapid reviews and scoping reviews were excluded.
2.3 Literature search
A pre-planned search approach was used, involving comprehensive search strategies to identify all available studies. Search strategies were developed by an experienced information specialist in consultation with the review team. Using the multifile option and deduplication tool available on the Ovid platform, we searched Ovid MEDLINE® ALL, Embase Classic + Embase, APA PsycInfo, EBM Reviews - Cochrane Central Register of Controlled Trials, and EBM Reviews - Cochrane Database of Systematic Reviews. CINAHL was searched on Ebsco. The MEDLINE strategy was peer reviewed by a second senior information specialist using the PRESS Checklist (41). Results were limited to English or French and to the publication years 2010 to the present. All searches were executed on April 5, 2022.
The strategies utilized a combination of controlled vocabulary (e.g., “Alcohol-Related Disorders,” “Mental Health Services,” “Health Services Accessibility”) and keywords (e.g., “PAU,” “counselling,” “social values”). Vocabulary and syntax were adjusted across the databases. Where possible, animal-only records, opinion pieces, case reports, books and book chapters were removed. Specific details regarding the strategies appear in Supplementary Table 3.
A targeted grey literature search of COVID-19-related sites was conducted, including the Cochrane COVID-19 Study Register, COVID-END, L-OVE, UNCOVER, and the WHO COVID-19 Database.
2.4 Study selection
Records were downloaded and deduplicated using EndNote version 9.3.3 (Clarivate Analytics) and uploaded to DistillerSR® online software where further duplicates were removed (DistillerSR. Version 2.38. Evidence Partners; 2022. https://www.evidencepartners.com). Two levels of screening were performed: citations included at initial screening of titles and abstracts were subsequently screened in full text. To calibrate the screening process, pilot testing of screening forms was conducted on batches of 50 citations at Level 1 and two citations at Level 2 until conflicts between reviewers were reduced to approximately 5% and reviewers were comfortable with the screening process.
To expedite screening, at Level 1, the artificial intelligence (AI) active-machine learning (AML) feature of DistillerSR® was used to prioritize screening of citations most likely to be relevant. A set of 200 citations that included both included and excluded studies was initially screened by two human reviewers to train the AML tool’s classification algorithm. Following this, the remaining citations were sorted for screening in order of highest to lowest likelihood of relevance, as perceived by the AML tool. The AML tool continued to learn as reviewers screened citations, resulting in re-ordering of citations with time as the classification algorithm became more accurate. Once 95% of the citations predicted to be relevant by the AML tool had been screened and included at Level 1 (454 of 473 predicted relevant citations in 5,665 citations screened), we implemented the AI reviewer in DistillerSR® to act as an independent reviewer to exclude the remaining 10,251 citations (highest remaining relevance probability score = 0.1279). These remaining citations were also screened by a human reviewer, and all conflicts were resolved with the aid of a second human reviewer. This approach aligns with recent guidance for the use of artificial intelligence in title/abstract screening (42).
All citations and full texts were screened in duplicate and independently by a team of seven reviewers (and the AI reviewer at Level 1, as described above). Conflicts were resolved via discussion and arbitration with a third reviewer, if necessary.
2.5 Data extraction
Data extraction was performed by two reviewers (DW and BH) in DistillerSR®. Data extraction forms were piloted on batches of five studies, with refinements made to the forms as needed, until both reviewers were comfortable with the data to be extracted and conflicts were minimized. Data verification was conducted on 50% of the included references. The following elements were extracted:
• Publication characteristics: First author’s last name, year of publication, country of study or first author’s country
• Study characteristics: Study objective, data collection methods
• Demographic data: Service user subgroup (e.g., people with concurrent mental health conditions, Indigenous people, people of specific gender/sex/sexual orientation subgroups)
• Study setting data: Where the interventions were delivered or where the participants were recruited, such as no context (e.g., national or online surveys, online self-help programs), primary care, community-based alcohol treatment services, emergency department, etc.
• Intervention data: No specific intervention (i.e., study focused on access to any treatment); interactive non-pharmacologic therapies (e.g., mutual aid groups, psychosocial interventions), plus the mode of delivery (e.g., in person, telemedicine); independent or technology-based therapies (e.g., self-help, web-based programs); pharmacologic therapies, care models (e.g., stepped care), adjuncts to therapy (e.g., body sensors).
• Barrier/facilitator data: Modifiable service-level factors reported to be barriers to or facilitators of accessibility to PAU treatment were extracted from the Results section of each paper as they emerged, without an a priori list of factors of interest. Concepts were copied and pasted electronically into DistillerSR® or paraphrased, if necessary due to length. As per our eligibility criteria, factors related to the service user, society, or the healthcare system were not extracted; however, factors related to service users’ capacities that correlated with service-level factors were extracted (e.g., an inability to pay was considered a service-level barrier related to the cost of the service). Service provider personality traits, knowledge/training, self-confidence, role responsibility, and the therapeutic relationship were not factors of interest because they were considered to impact treatment success and retention more than accessibility. However, certain service provider characteristics that were reported to be barriers of treatment accessibility were extracted (e.g., language, culture, sex/gender). Where available, we extracted service users’ “preferred levels” that could facilitate treatment accessibility (e.g., preferred appointment times).
Barrier data were coded during data extraction to the most appropriate barrier concept, with new barrier concepts added as they emerged (e.g., “Cost,” “Location,” “Appointment hours,” “Wait period”). Relevant text for each barrier was extracted to provide greater context and depth. Data could be coded to more than one concept; data could be recoded, if necessary, during data verification, cleaning, or synthesis.
Risk of bias assessment was not conducted, as per accepted scoping review methodology (32).
2.6 Mapping/synthesizing the evidence
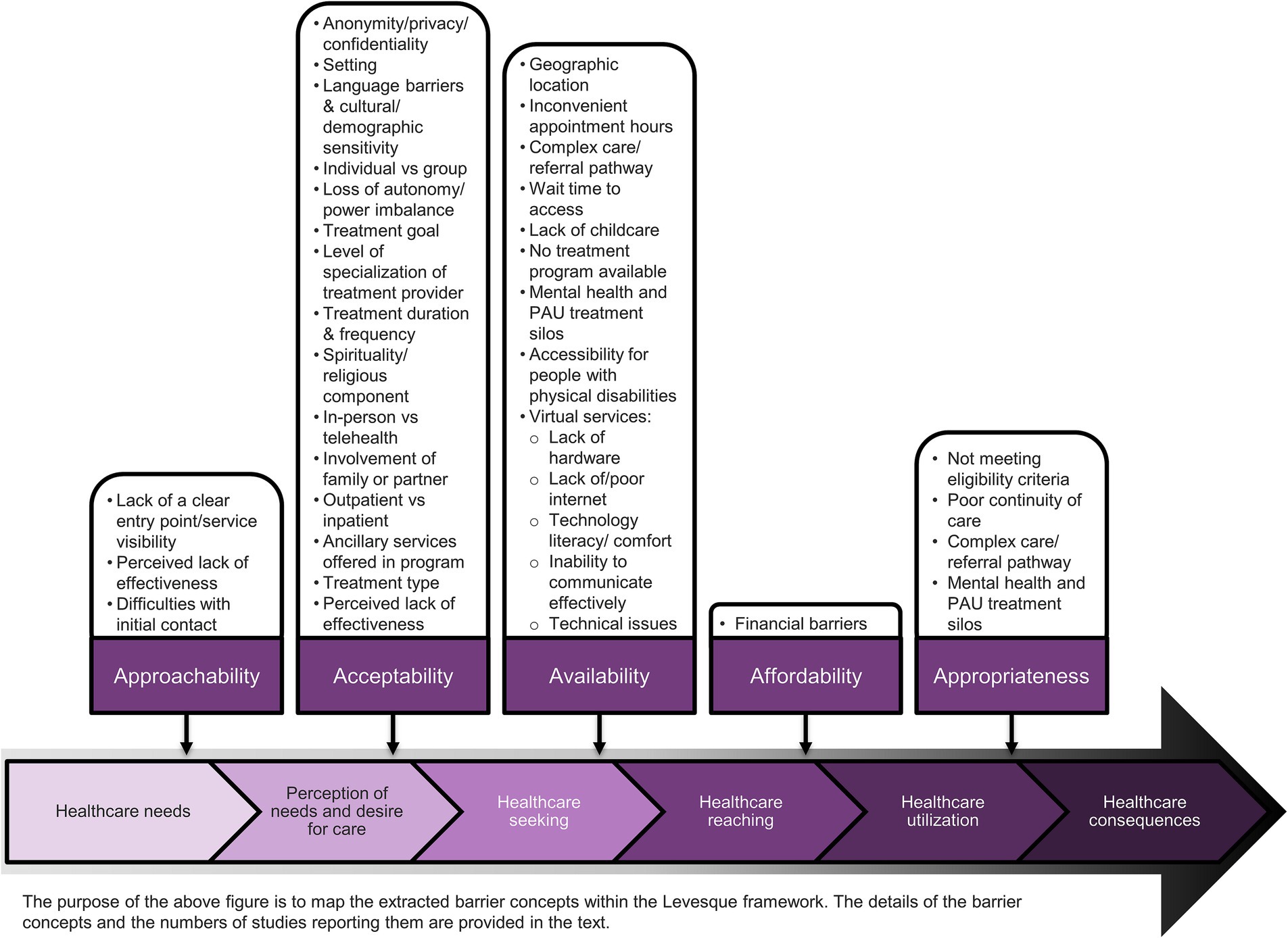
Data were cleaned and collated in Microsoft Excel by DW. Given the scoping review approach undertaken, the objective of our synthesis was to map barrier concepts rather than to synthesize them through a qualitative methodology [e.g., meta-ethnography (43, 44)] or to rank them according to importance. Barrier concepts were mapped by DW to dimensions of Levesque’s Conceptual Framework of Access to Healthcare (39) and verified by an independent reviewer (BH or KT) through discussion to overcome known challenges to the use of the framework (45). Levesque and colleagues defined healthcare access as “the possibility to identify healthcare needs, to seek healthcare services, to reach the healthcare resources, to obtain or use health care services, and to actually be offered services appropriate to the needs for care (39).” Within this framework, “access” is portrayed as an interplay between the “accessibility” of treatment services and the “abilities” (or “capacities,” a term preferred by our research team) of individual treatment seekers throughout the pathway of healthcare utilization (39). “Accessibility” relates to traits of treatment services and is conceptualized by Levesque et al. to have five dimensions: Approachability, Acceptability, Availability and accommodation, Affordability, and Appropriateness. Five corresponding dimensions of the “capacity” of individuals to interact with the accessibility dimensions to obtain access were also conceptualized: Capacity to perceive, Capacity to seek, Capacity to reach, Capacity to pay, and Capacity to engage (39). The focus of this review was on dimensions of accessibility and the service-level factors that they encompass.
After mapping to the Levesque framework, where possible, similar barrier concepts were amalgamated within an accessibility dimension. Synthesis of data from service user subgroups was explored within barrier concepts, where there was sufficient available data. An additional synthesis was conducted that incorporated studies focused on treatment accessibility barriers during the COVID-19 pandemic.
2.7 Involvement of people with lived experience and the public
We engaged people with lived experience during the planning and conduct of this research. Input was gathered from multiple organizations as represented in the make-up of our authorship team, to ensure findings are of relevance to multiple groups. Specifically, we engaged with the Community Addictions Peer Support Association, the Canadian Psychological Association, the Canadian Centre on Substance Use and Addiction and the Mental Health Commission of Canada, and we thank them for their valuable contributions to this work.
3 Results
3.1 Extent of the literature
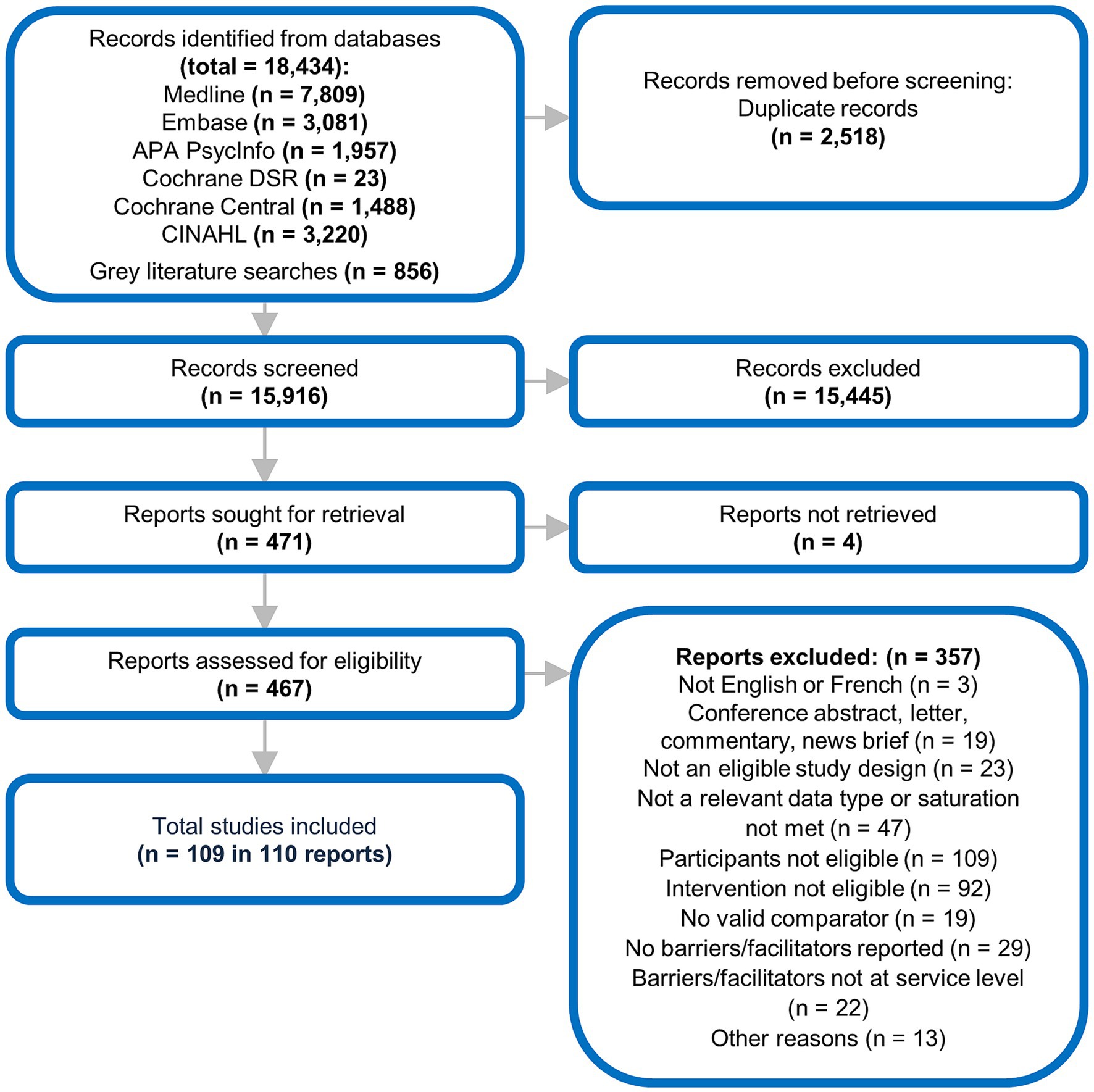
Following removal of duplicates, 15,916 references were screened at Level 1, with 471 references included for full-text screening at Level 2. Of these, 109 studies in 110 reports were retained in our review (Figure 1). References excluded at full-text screening (n = 284) and their reasons for exclusion have been provided in Supplementary Table 4.
3.2 Study characteristics
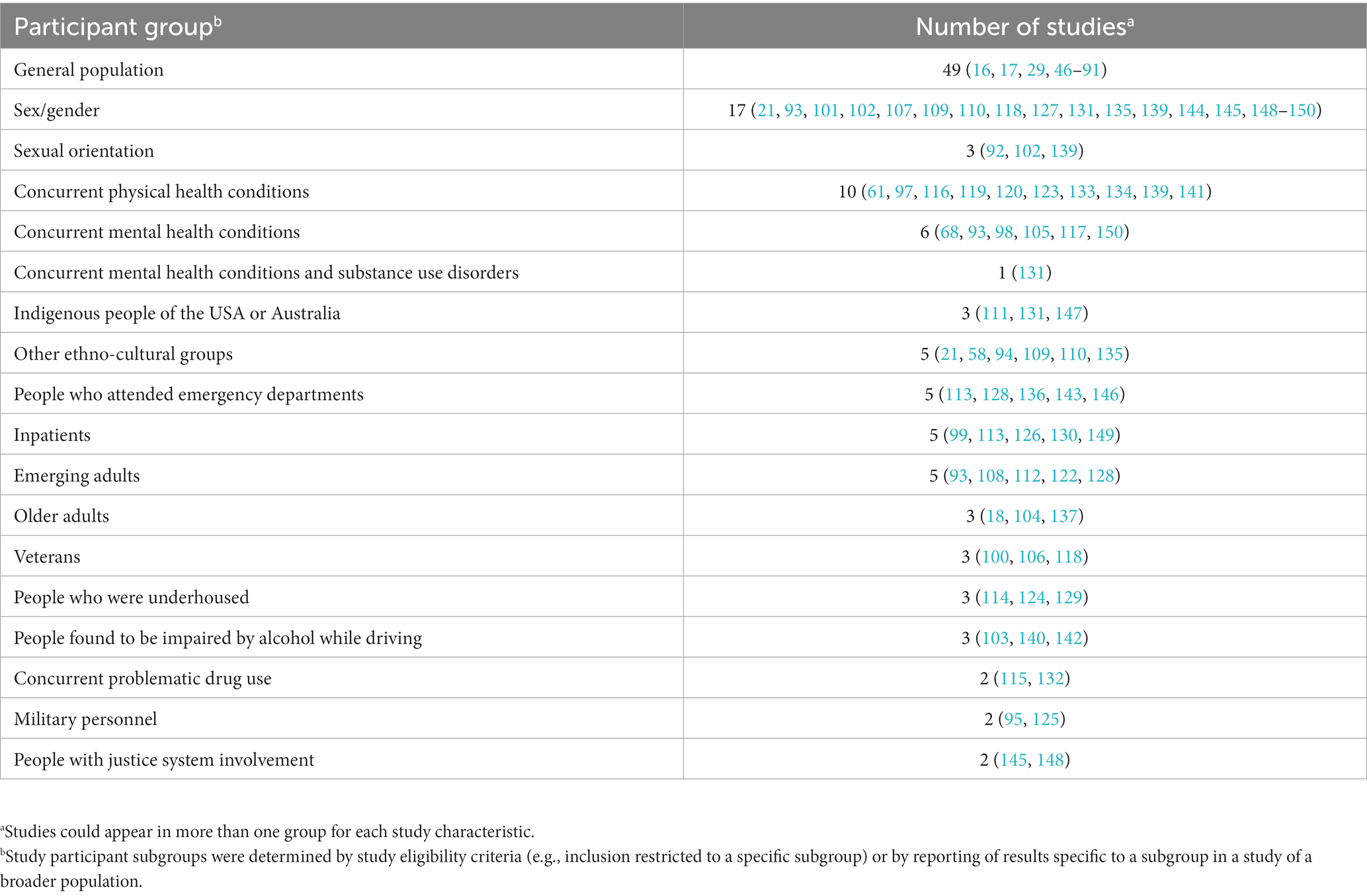
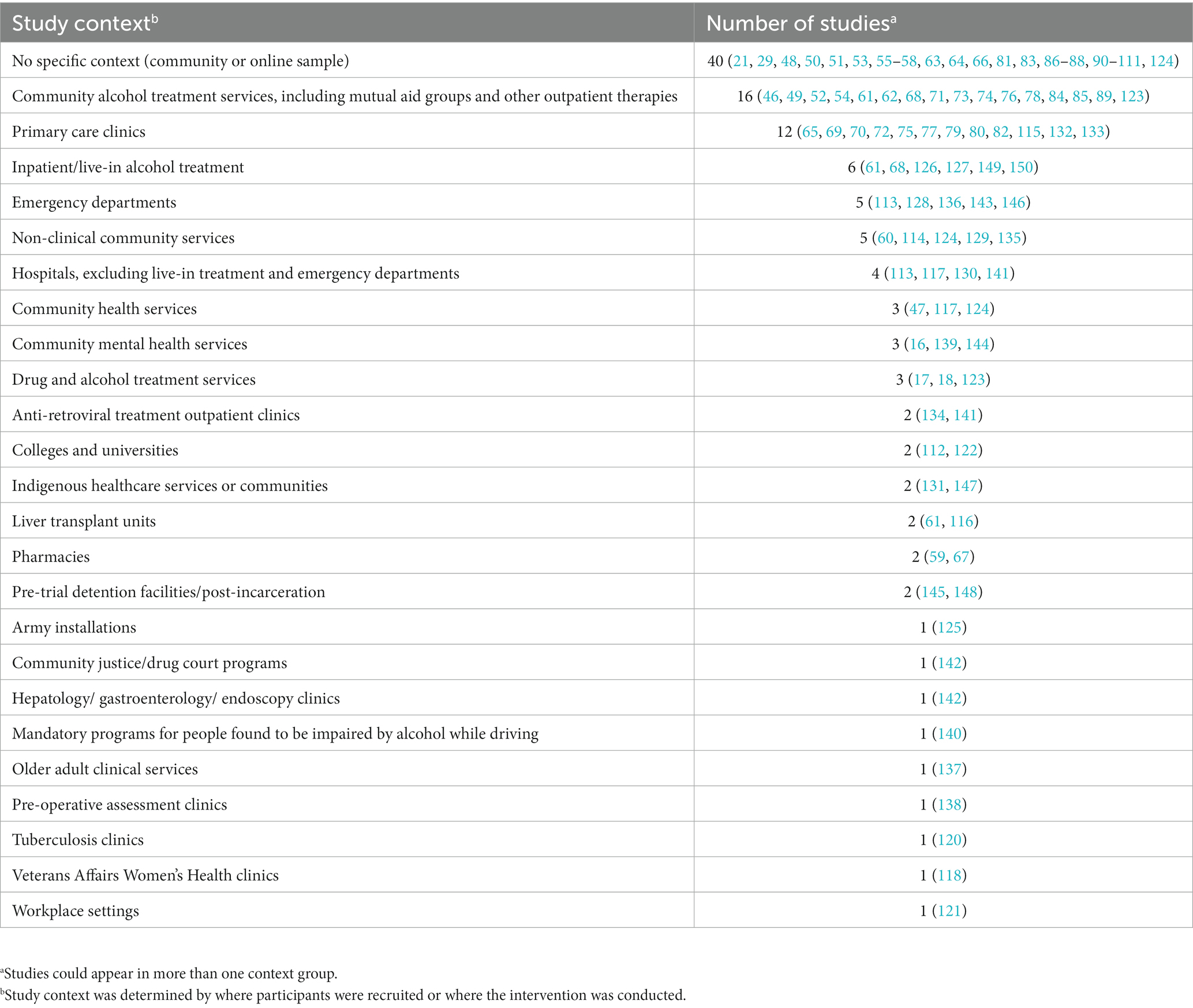
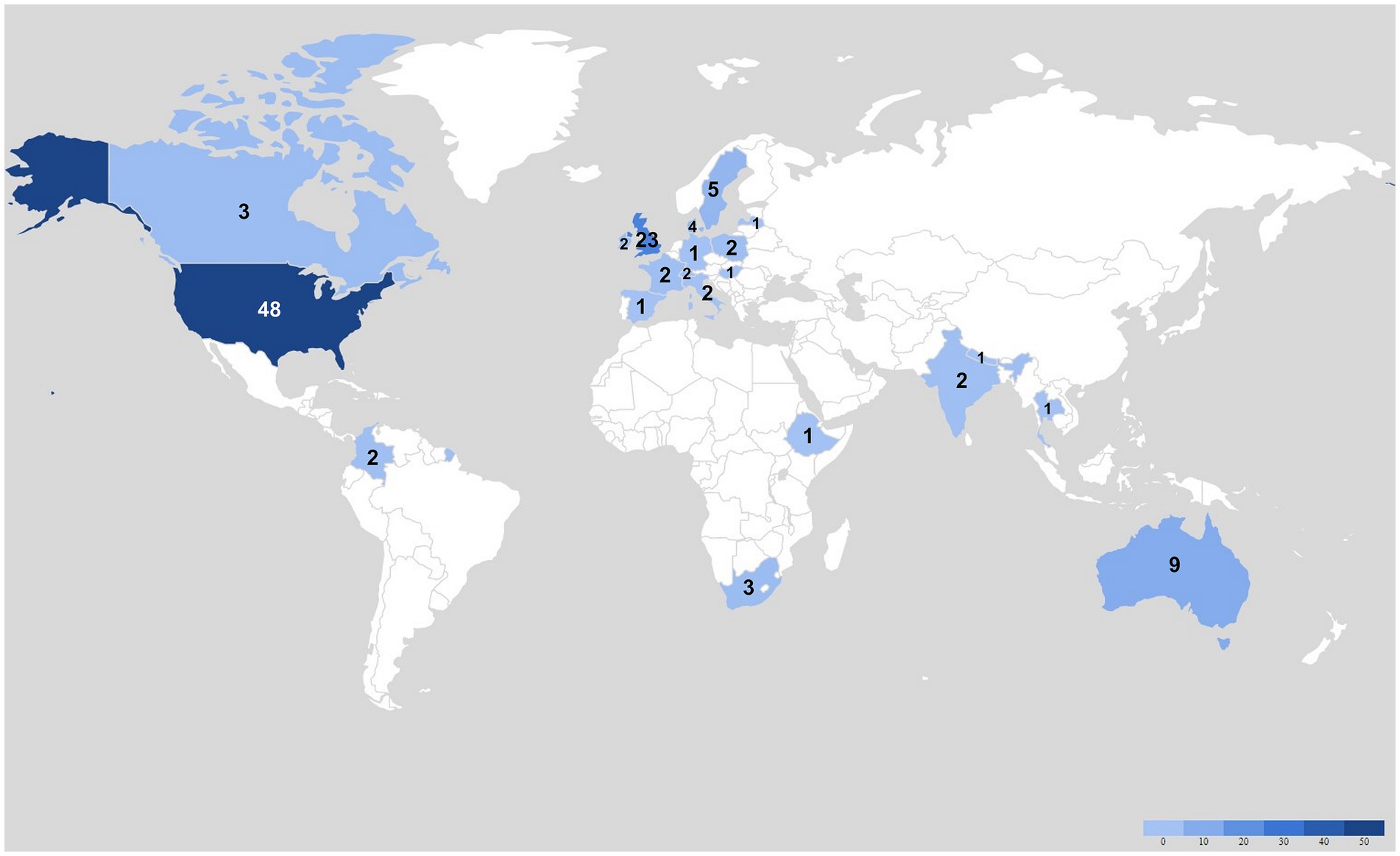
Characteristics of the 109 included studies are summarized in Tables 1–3, while individual study details are reported in Supplementary Table 5 (with further details in Supplementary Datasheet 1). The geographical distribution and frequency of the included studies are depicted in Figure 2. Years of publication ranged from 2010 to 2022. Forty-nine of the studies (45%) included participants of no specific subgroup (i.e., participants were selected based solely on their PAU status and/or because they were seeking treatment to reduce their alcohol intake) (16, 17, 29, 46–91). Forty studies were not conducted in a specific context (i.e., participants were recruited from the community or online and the intervention had no specific context) (21, 29, 48, 50, 51, 53, 55–58, 63, 64, 66, 81, 86–88, 90, 92–111). Thirty-four studies evaluated no specific intervention (e.g., evaluations of general treatment seeking or engagement) (17, 21, 29, 47, 51, 58, 61, 63, 65, 68, 74, 75, 88, 91, 92, 95, 97, 100–102, 105, 106, 109–120), while 59 studies evaluated some type of screening or non-pharmacologic psychosocial therapy. Independent or technology-based therapies were evaluated by 12 studies (48, 53, 55, 57, 63, 83, 94, 98, 108, 109, 121, 122), and two studies evaluated pharmacologic therapies (extended-release naltrexone (XR-NLT)) (123, 124); two evaluated models of care, including a military-based confidential care model (125) and a primary care collaborative care model (72); and four studies evaluated adjuncts to therapy (e.g., alcohol sensors and monitors, exercise therapy, mindfulness-based therapy) (46, 71, 78, 126, 127). Data collection methods among the 109 studies included interviews only (n = 57) (16–18, 21, 29, 48, 49, 52–56, 61–63, 68, 70–73, 75, 77, 78, 80, 85, 86, 89, 92, 93, 96–99, 101, 103, 105–107, 110, 113–118, 122, 128–139), focus groups only (n = 6) (50, 87, 108, 127, 140, 141), surveys only (n = 26) (46, 47, 57, 64–66, 74, 81, 83, 84, 90, 91, 94, 95, 100, 102, 112, 121, 123, 124, 126, 142–146), and combinations of methods (n = 20) (51, 58, 60, 67, 69, 76, 79, 82, 88, 104, 109, 111, 119, 120, 125, 147–150). Sample sizes ranged from 6 to 1,556 participants (median = 35), with larger studies tending to use survey designs. Three studies reported findings related to PAU telehealth service accessibility during the COVID-19 pandemic in Canada/USA (17), India (16), and the UK (18).
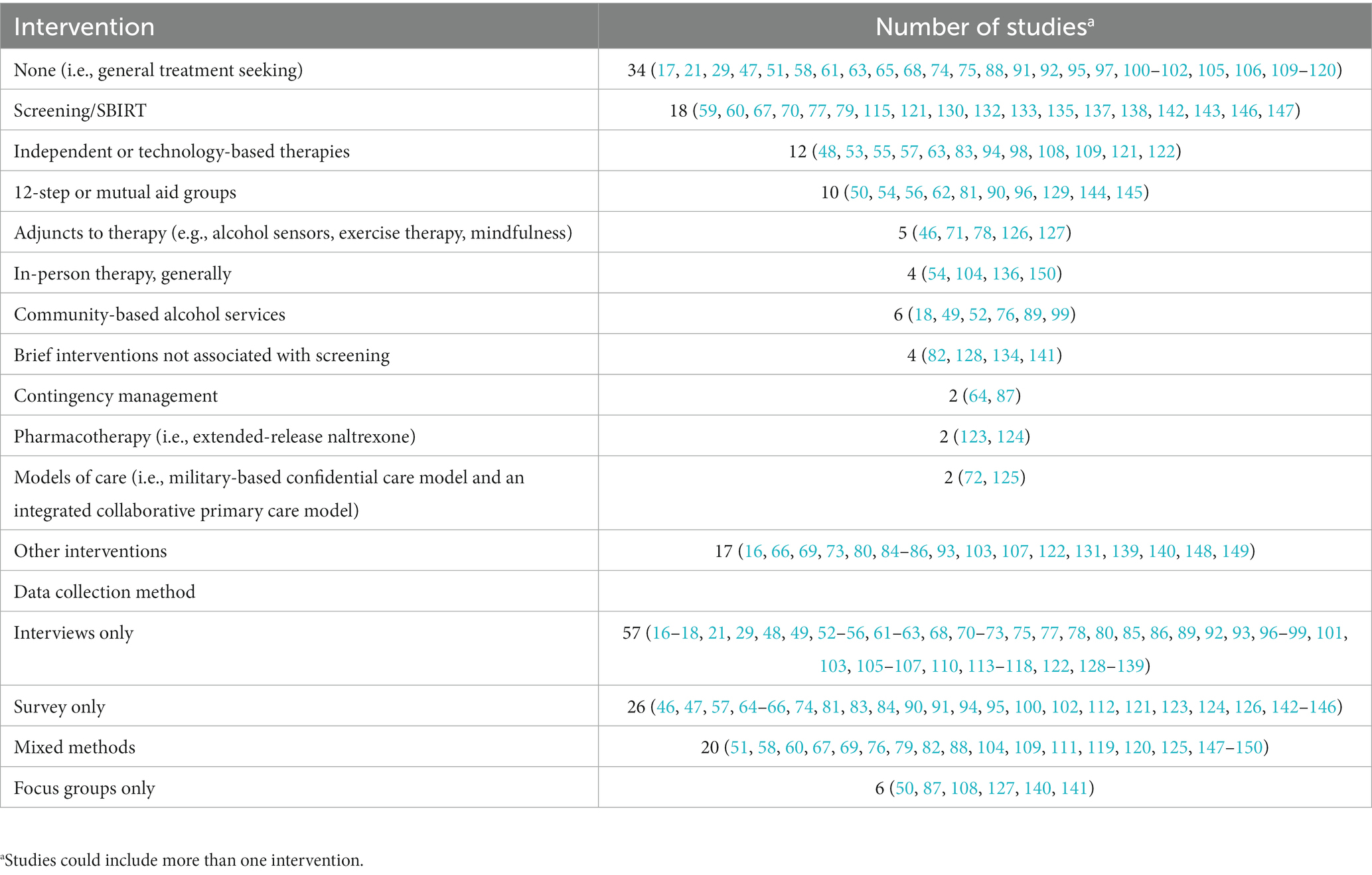
Table 3. Summary of the intervention characteristics and data collection methods in the 109 included studies.
3.3 Accessibility dimensions
The barrier concepts extracted are portrayed in Figure 3, mapped to the accessibility dimensions of the Levesque framework. The richest data were found in the acceptability dimension, which included 20 emergent barrier concepts of which at least one was reported in 84 studies (see Acceptability subsection below). Less rich data were found in the availability/accommodation (14 concepts in 64 studies), approachability (4 concepts in 40 studies), appropriateness (4 concepts in 28 studies), and affordability dimensions (1 concept 25 studies). The most frequently reported barrier concepts were service visibility (acceptability dimension; n = 35 studies), anonymity/privacy/confidentiality (acceptability dimension; n = 32), geographic location and transportation barriers (availability dimension; n = 29), inconvenient or inflexible appointment hours (availability dimension; n = 26), financial barriers (affordability dimension; n = 26), and the complexity of the care/referral pathway (availability and appropriateness dimensions; n = 23). All barrier concepts are described in detail in their respective accessibility dimension below.
3.3.1 Approachability of PAU services
This dimension reflects the capacity of treatment seekers to find and engage with services that they believe can help them (39).
3.3.1.1 Lack of a clear entry point/service visibility (n = 33 studies)
Treatment seekers expressed uncertainty regarding where to seek treatment or had sparse knowledge of services available to them. In surveys, not knowing where to go for treatment varied by country, with 49.2% of treatment seekers in Ethiopia (91), 35.8% in Nepal (75), and 8–19% in the USA (58, 101) endorsing it as a barrier to treatment. A greater proportion of men (9%) than women (4%) (101), the majority of people belonging to ethnic minority groups (21, 109–111, 131), and 9.4% of US military personnel with PAU did not know where to seek help (95). Inconsistent dissemination of information about a confidential military treatment program resulted in many military personnel only discovering its existence after self-referring to non-confidential treatment despite potential career implications (125). Similar proportions of people with and without concurrent mental health conditions did not “know where to go” for PAU treatment (100, 105); however, in one study, the majority of Australian Indigenous women with concurrent mental health conditions and SUDs had little knowledge of available services and felt that services were poorly promoted (131). Another study from the UK focusing on specialist community alcohol services reported “marketing and promotion were consistently seen as both important and lacking by service users (76).”
3.3.1.2 Perceived lack of effectiveness (n = 14 studies)
The perceived effectiveness of specific PAU interventions influenced treatment engagement for some study participants (21, 29, 47, 54, 66, 88, 98, 100, 104, 105, 110, 111, 124, 136, 145), though extent of endorsement varied substantially across subgroups. In two American survey studies, skepticism about the effectiveness of treatment, generally, was endorsed as a barrier to engagement by 46% of participants with AUD who wanted but did not receive treatment (47), and 75% of urban-dwelling Indigenous American participants felt treatment “would not do any good (111).” Among Americans with and without concurrent mental health conditions, 9.2 and 10.9%, respectively, expressed that they “Did not think anyone could help (105);” however, among US veterans with and without concurrent mental health conditions, 59.1 and 46.3%, respectively, did not think treatment would help (100). Previous unhelpful treatment experienced by themselves (136, 145) or by others (111) dissuaded some from seeking treatment. American Hispanic men generally perceived free treatment as less effective and unaffordable treatment as more effective (110). In a Swedish study, internet- and telephone-based treatments were seen as ineffective (88). Psychotherapy may be preferred over pharmacotherapy by some, including some older adults, because it allows one to understand the causes of problematic drinking (88, 104), whereas pharmacotherapy “merely targets the symptoms without addressing the underlying problems (88).” Low expectations of treatment success were a barrier to engagement with Alcoholics Anonymous (AA) for some American women in pre-trial detention facilities (145), while unrealistically high expectations of therapy may encourage initial engagement in some interventions (e.g., extended-release naltrexone (124) and online self-help (98)).
3.3.1.3 Difficulties with initial contact (n = 4 studies)
Some treatment seekers reported difficult initial contact with PAU services as a barrier to engagement (e.g., phone calls unanswered or not returned (29, 99, 117, 150), computer respondent that indicated a two-to-three-month waiting period (150)). Participants expressed feeling dismissed or ignored, and considerable assertiveness was required to obtain treatment (29), although others disengaged (29, 99, 117, 150). “Being able to speak directly to a counselor and having their calls returned was an important factor in not only coming to the treatment center but also in shaping a positive expectation about what they might gain from treatment (150).”
3.3.2 Acceptability of PAU services
The acceptability dimension covers cultural and social aspects of a service that influence a treatment seeker’s willingness to access it (39). We identified a wide range of factors within this dimension, including confidentiality and anonymity, language barriers, discordance in the treatment goals of the treatment seeker and provider, conflicts between a person’s religious or spiritual values and their medical care, restrictions to a person’s involvement in treatment decisions, and provider-patient power dynamics. “Perceived lack of effectiveness” was categorized in both the Acceptability and Approachability dimensions and has been addressed in the Approachability section to avoid redundancy.
3.3.2.1 Anonymity/privacy/confidentiality of service (n = 32 studies)
The desire and need for anonymity, privacy, and confidentiality appeared to be driven by fears of stigma and shame (111), deportation (135), and losses of children (53, 58), employment (58, 119, 121), and military careers (95, 125). Concepts related to anonymity, privacy, and confidentiality were frequently found in studies of small or rural communities (56, 89, 111), public non-clinical settings (e.g., pharmacy) (59, 60, 67, 130), the military (95, 125), peer-led groups (56, 62, 70, 74, 99, 111, 145), and text- (108) or internet-based interventions (48, 53, 56, 63, 70, 81, 84, 85, 96, 98). The need for anonymity tended to be highest for those seeking or initiating therapy (62, 63, 96, 108).
3.3.2.2 Setting (n = 19 studies)
The treatment setting could negatively influence treatment engagement through perceived stigmatization, triggering fear, first impressions of the condition of the treatment facility, and other factors. Some people with PAU felt stigmatized when treatment was offered in the same location as other drug services (49, 76) or human immunodeficiency virus (HIV) treatment (134); outpatient treatment at a hospital was more acceptable because they could be there for many reasons other than therapy for their PAU (99). Treatment facilities that appeared unsafe (99, 102, 104, 111) or were unfamiliar (136) also discouraged engagement, and locating services in safe (150) or familiar settings (67, 115, 135) may improve accessibility. Interventions set in the ED were preferred by many rather than waiting until the shock of an alcohol-related incident had dissipated (128); however, 30% of participants in the ED in another study were too ill to participate (143). In group settings, heterogeneity of participants with respect to treatment goal (e.g., abstinence or consumption reduction) (136) or reason for treatment (i.e., people with an alcohol-impaired driving conviction forced to attend AA) (140) could negatively impact engagement.
3.3.2.3 Language barriers and cultural/demographic sensitivity (n = 7 studies)
Lack of care sensitive to a person’s own ethno-cultural group or in the language of their choice was an accessibility barrier identified by Indigenous people (111, 131), other ethno-cultural groups (21, 58, 66, 107, 110, 135), people living with deafness (89), older adults (104), military personnel (106, 118), and people of different sexual orientations (102). When linguistic or cultural disconnects are present, service providers may be perceived as not fully understanding service users’ experiences (104, 106, 107, 110, 135), including the social norms of drinking within their culture (107, 135). People of cultural minority groups may also feel that service providers of the cultural majority are judgmental (107) or invasive (110). In peer-led groups of mixed cultures, people of cultural minorities may feel singled out (111) but feel comfortable in groups of people of their own culture (111, 151). Women also may prefer women-only groups due to content and style of communication (144), safety (144, 150), and the potential for men to trigger underlying mental health conditions (118).
3.3.2.4 Individual vs. group treatment (n = 17 studies)
Preference for individual or group therapy varied across participants within studies, potentially limiting accessibility, if the preferred treatment format was unavailable (53, 61, 89, 118, 120, 136, 145). Some who did not like to be singled out preferred a group format (53, 120), and many derived support from exchanging stories (29, 62, 119). Online mutual-aid groups were appreciated by those who enjoyed the flexibility of accessing support anytime and anywhere (62). However, groups were perceived negatively by some because of the lack of individualized attention (97, 110), triggering of social anxiety (99, 119), concerns about confidentiality (99, 119), focusing on other people’s problems (51), focus of sessions being devoted to those who were still drinking (99), and a preference to be in groups of people who were abstinent (119). Some people felt that group and individual therapy had differing purposes: group therapy supported recovery, whereas individual therapy was seen to deal with complex psychological issues (29), and treatment availability in concordance with their perceived needs may encourage engagement. Specifically, individual treatment provided an individualized connection for some that helped to maintain a sense of personal responsibility (17).
3.3.2.5 Loss of autonomy and power imbalance (n = 15 studies)
Many treatment seekers feared losing control of their lives with traditional prescribed “police-style” PAU interventions (53, 54, 63, 88, 111, 114) or with AA’s concepts of powerlessness and peer authority (54), causing some to access self-paced online treatment (53). Patient-centered care that involved participants in personal healthcare decision making (29, 68, 72, 85, 103) and provided flexibility in treatment delivery options (e.g., in-person or telehealth) (72) promoted feelings of empowerment, responsibility, and independence (54, 85). However, some people with PAU have preferred having less autonomy if they became overwhelmed by the onus of responsibility of treatment seeking when access to treatment is extremely difficult (29), or if therapist supervision would force them to engage more and be more accurate in reporting their alcohol consumption (53).
Power imbalances that negatively impacted treatment engagement were identified in group treatment settings, including the perceived paternalistic sponsorship model of AA and some other mutual aid groups (54, 73, 111), the authoritarian indoctrination of 12-step groups (73), and the abstinence hierarchy perceived in groups of people at all stages of recovery (104, 114). In other settings, power imbalances were found in the rules and reminders to follow in live-in treatment (150) and the need to comply with PAU treatment from a general practitioner (GP) who also provides individuals with methadone for their other substance use problems (115).
3.3.2.6 Treatment goal (abstinence vs. consumption reduction) (n = 16 studies)
Treatment engagement was reduced when disconnects existed between the treatment goal of a program (i.e., abstinence vs. consumption reduction) and the goal of the treatment seeker. When faced with forced abstinence, some did not enroll because they felt the treatment goal was too difficult to attain or maintain (72, 86, 88, 89, 104), and some opted out because they felt pressured to conform (99) or were antagonized by abstinent group members for preferring consumption reduction (96). However, for others, an abstinence commitment may make them feel a part of a group (96) and reinforce their self-esteem when met (86). Consumption reduction as a goal was preferred by many (79, 88) and was perceived as motivating and positive (104) and more easily attainable (86), providing an intermediate goal toward abstinence (54, 86). In some areas, there was a perceived gap in service provision for people wanting to moderate their drinking rather than abstain (63). Some programs appeared to support consumption reduction in principle, only to expel participants that perceived moderation to be an end and not an intermediate goal toward abstinence (29). Programs supporting both abstinence and consumption reduction goals were generally appreciated (49, 72, 86, 104); however, some seeking abstinence feel that such programs enable drinking (72).
3.3.2.7 Level of specialization of treatment provider (n = 14 studies)
The level of specialization of the provider of community-based PAU counselling influenced some treatment seekers’ engagement; some preferred to access treatment with their primary care clinic and others preferred a specialist. Treatment within primary care clinics may be preferred by many over specialist clinics (65, 72, 79, 115, 147) because of the pre-existing therapeutic relationship (79), the convenience and low cost (72), and primary care being perceived as a less drastic and stigmatizing step to take (88). Within primary care, in one study, nurses were preferred over doctors for screening and brief intervention (SBI) (79), but there was no preference between doctors and either computers (146) or telephone-based interactive voice recognition (77). Others preferred to access specialist PAU therapy due to perceptions that expert knowledge was needed to treat PAU (88) and primary care may not be able to access all diagnostic or treatment modalities (69). Regarding inpatient treatment, some accessing PAU treatment in general inpatient settings felt that their symptoms were often minimized and that they were not as accepted as they would be in a specialty inpatient program (88). However, some with complex mental health conditions appreciated general over specialist inpatient services (68). Finally, most pharmacy users found SBI acceptable, although a minority suggested that they preferred to discuss alcohol with their primary care doctor (59, 67).
3.3.2.8 Treatment duration and frequency (n = 9 studies)
The duration of a treatment program, whether too short or too long, impacted program engagement, depending on the treatment seeker’s perceived needs and abilities (53, 89, 108, 118, 128, 133, 134). Preferred program duration often varied among study participants (53, 89, 108, 118, 128, 134), with those with a history of higher-risk drinking perceiving programs as too short, while those with a history of lower-risk drinking perceiving programs as adequate or too long (134). Similarly, the frequency of therapy could impact engagement (29, 68, 89), with the preferred frequency varying across treatment seekers: high frequency of therapy required too great of a time commitment for some (68, 89), while low frequency of therapy potentially offered insufficient support for others (29).
3.3.2.9 Spiritual/religious component (n = 8 studies)
Spiritual or religious aspects of some PAU interventions were perceived negatively (53, 54, 68, 98, 114, 145, 150), depending on service users’ personal beliefs. Many perceived AA to have an oppressive approach, decreeing that participants surrender to a Higher Power and rely on belief rather than objective reasoning (54). Many participants expressed that such approaches were incompatible with their beliefs, even those who were religious or spiritual (54), or were offensive or triggering for those who were not (54, 150). Some chose secular online (53, 98) or in-person (54) alternatives to AA to separate recovery from religion.
3.3.2.10 In-person vs. telehealth (n = 6 studies)
In-person therapy was preferred over telehealth by service users in several studies (18, 76, 84), while preferences were mixed in others (17, 85). In-person face-to-face therapy felt “more genuine, more personable,” a better therapeutic relationship was developed, there was the potential for deeper conversations and to read body language, and it was easier to follow or to ask for help than by video (84, 85), telephone (18), or either virtual delivery method (17). As well, people using telehealth services may not be able to access the full suite of therapies that are provided through in-person care (76). Despite this potential limitation, telehealth minimized the need for some service users to cancel appointments (85), provided greater flexibility in timing (17, 18, 85), reduced the anxiety of initial engagement in group therapy (18), and enabled access during COVID lockdowns (16).
3.3.2.11 Involvement of partner or family (n = 4 studies)
Participants in some studies suggested that they would be more likely to engage in PAU treatment if a support person (e.g., spouse/partner, children, caregiver) could also attend (50, 116, 120, 137) to give them a better understanding of PAU, treatment, and how to foster abstinence (116). This concept was found mainly in studies of population subgroups such as people with concurrent alcohol-related liver disease/transplant (116) or tuberculosis (120) and older adults (137).
3.3.2.12 Outpatient vs. inpatient (n = 4 studies)
Many treatment seekers felt that inpatient therapy was “a last resort” and preferred outpatient to inpatient therapy (88, 92, 102), with a greater proportion of bisexual compared to heterosexual individuals being afraid of being placed in hospital if they sought treatment (92). For people with PAU who were underhoused, inpatient treatment offered a sense of stability and a time-out from “the hardships of life on the streets and from the 24-h job of obtaining, drinking, and recovering from the effects of alcohol (114).” However, inpatient therapy wasn’t seen as an effective form of therapy to maintain abstinence (114).
3.3.2.13 Ancillary services offered within the treatment program (n = 2 studies)
Service users in two studies suggested that they would be more likely to engage with PAU treatment if ancillary services were also offered, such as life-skills/employment training (68, 136) or free access to a gym (136).
3.3.2.14 Treatment type (n = 21 studies)
Numerous studies reported service user preferences for different types of treatments that have not been reported above. Barriers to treatment engagement could occur when treatment seekers could not access their preferred treatment [e.g., only AA available but preferred another intervention (97, 110, 111)]. A summary of participant treatment type preferences has been provided in Supplementary Table 7.
3.3.3 Availability of PAU services
The availability dimension suggests that PAU services are accessible if they can be reached where and when they are needed by the treatment seeker (39).
3.3.3.1 Geographic location and transportation barriers
The geographic location of PAU services or lack of transportation were common barriers to treatment accessibility (17, 18, 50, 53, 54, 58, 66, 74, 76, 85, 89, 95, 99–102, 105, 111, 119, 123, 126, 131, 136, 145, 150), especially for people living in rural areas or outside of the urban core (18, 76, 85, 89, 99, 131), people with physical disabilities (123, 136), and people with concurrent mental health conditions (100). Some preferred telehealth or internet-based treatment services because they overcame geographical considerations, transportation issues and logistical hassles, and were timesaving (17, 53, 85). Receiving PAU treatment from an existing service that people with PAU already attended (e.g., primary care clinic, liver transplant program, non-clinical community services) was preferred by many because of convenience (72, 116, 135).
3.3.3.2 Inconvenient or inflexible appointment hours (n = 26 studies)
Inconvenient or inflexible appointment hours were reported to be a barrier to accessibility by participants in many studies (17, 18, 29, 48, 53, 58, 66, 76, 85, 87, 89, 91, 92, 95, 100–102, 105, 111, 115, 125, 131, 133, 134, 141, 145), especially those who were employed (53, 66, 76, 85, 87, 89, 95, 100, 102, 111, 125, 133, 134). Telehealth options provided greater flexibility in timing and, therefore, greater accessibility (17, 18, 48, 53, 85). For people with PAU and concurrent mental health conditions, inflexible service hours resulted in poor accessibility at times of crisis (131). Military personnel appreciated appointments outside of duty hours because they were free to attend in civilian clothes, they did not need to ask superiors for time off (and so the treatment could remain off their record), and off-duty treatment occupied a time when they were more likely to drink, providing a distraction (125).
3.3.3.3 Complexity of the care/referral pathway (n = 22 studies)
Lack of communication, coordination, and agreements between care providers (e.g., hospital and community services, primary care and specialists) resulted in fragmented, time-consuming, and sometimes non-linear referral pathways that contributed to difficulties in navigation and accessibility for service users (21, 29, 51, 68, 69, 74, 75, 88, 89, 97, 104, 110, 113, 150). As well, referral providers’ lack of knowledge of or communication of the existence of available treatment options (54, 89, 118, 150), lack of provision of referral contact information to service users (118), and lack of scheduling of initial appointments for service users (117, 118) were expressed by service users as negatively affecting treatment accessibility. Integrated PAU treatment programming (e.g., within primary care) (72), outreach (76, 148) and in-reach (e.g., “locating potential service users [in hospital] and engaging them prior to formal enrolment” into a program) (76), the use of third-sector charities to aid service-user navigation (106); identification and coordination of services, teams, and clinicians (68, 135); and proactive scheduling of initial appointments for service users by referral providers (103, 113, 118) were all suggested as facilitators of referral pathway navigation and accessibility.
3.3.3.4 Wait time To access treatment (n = 17 studies)
The time between identification of a suitable PAU service (or referral to one) and initiation of treatment was a frequently cited barrier to treatment accessibility (21, 49, 58, 68, 74, 76, 89, 97, 101, 103–105, 110, 111, 113, 131, 136, 150). When wait times were prolonged, treatment seekers’ readiness to change could fade (89, 104, 111). Some who felt the need for immediate treatment presented at hospital if they were unable to wait for outpatient therapy (113, 150). However, if they presented in crisis with alcohol toxicity, their help-seeking was sometimes dismissed as hospital staff perceived them not to be serious about recovery (150). Services were suggested to be overburdened (21, 110) due to staff shortages (49) or funding cuts (76), exacerbating wait times.
3.3.3.5 Lack of childcare (n = 10 studies)
Lack of childcare was a barrier to PAU treatment that varied by country and subgroup. In general population surveys in the USA, “Could not arrange for child care” was endorsed infrequently as a barrier to accessing PAU treatment (0–2%) (58, 101, 105). However, surveys of Nepalese (66) and Ethiopian people (91) with AUD found 58 and 22%, respectively, reported problems with childcare as a barrier to PAU treatment. In specific US subpopulations, such as veterans (100) and Indigenous people (111), 10–30% expressed that difficulty obtaining childcare was a PAU treatment barrier. Among US veterans, women were significantly more likely than men to report lack of childcare as a PAU treatment barrier (26% vs. 18%), as were people with a concurrent mental health condition compared to those without (29% vs. 11%) (100). In US general population surveys, no differences in the proportion endorsing childcare as a barrier were found between US ethnic groups (58); however, event counts were too low to detect a difference between women and men (101) and those with and without concurrent mental health conditions (105). Online treatment programs were easier to engage in for some treatment seekers because they did not have to obtain childcare during the time they engaged with treatment (53).
3.3.3.6 No treatment program available (n = 8 studies)
An overt lack of existing treatment programs or interventions was identified as a barrier to PAU treatment, especially for those in rural areas (89, 99) and those seeking specific interventions, such as treatment integrated into primary care (80, 104), tuberculosis clinics (120), or liver transplant programs (116), or alcohol-specific treatment for people with opioid use disorder (OUD) (115). A minority of military personnel reported that there were no providers in their community, preventing them from obtaining treatment (95).
3.3.3.7 Mental health and PAU treatment silos (n = 5 studies)
Lack of treatment programs that offered both mental health and PAU interventions was reported as barrier in 5 of 7 studies that included people with concurrent mental health conditions (68, 76, 99, 117, 131). Siloed mental health and PAU services requiring abstinence to receive mental health therapy and stable mental health to receive PAU treatment resulted in people with concurrent disorders not being accepted for either program (68, 76, 99, 131). Some felt that the combined services available to them did not meet their individual needs, with one participant stating, “my psychiatrist’s way of looking at it was just to abstain from alcohol, all problems will be resolved (117).”
3.3.3.8 Accessibility for physically disabled (n = 2 studies)
People with PAU and concurrent physical disabilities reported that in-person treatment accessibility was impeded by lack of wheelchair lifts or platforms (89) and that those who could not physically use a computer could not access computer-based screening and treatment services (70).
3.3.3.9 Technology-based therapy: lack of hardware (n = 5 studies; published 2014–20)
For some attempting to access technology-based therapy, such as telehealth video appointments, text-messaging services, or mobile phone-based apps, engagement was contingent upon owning a computer or a mobile phone (17, 18, 55, 69, 94). Provision of a mobile phone by the service provider ensured accessibility to treatment in one study (55).
3.3.3.10 Technology-based therapy: lack of or poor internet (n = 5 studies; published 2012–22)
Not having access to the internet was a barrier to telehealth video appointments reported by older adults (18). Poor or unstable internet also forced some people with PAU to reject telehealth as a treatment option over in-person therapy (17, 85). Similarly, some could not complete computer based SBIs in venues such as the ED or primary care that had unstable internet (70, 143).
3.3.3.11 Technology-based therapy: low technology literacy or comfort (n = 8 studies; published 2010–22)
Technology-based therapies such as telehealth by videoconference, computer- or tablet-based PAU screening, and mobile phone apps were inaccessible for some due to low technology literacy or being uncomfortable with technical devices (17, 18, 69, 84, 85, 137, 142, 146). Subgroups that appeared to have low technology literacy included older adults (18, 69, 137), those with learning disabilities (18), and those with lower education or experience with computers in rural areas (69) or among people found impaired with alcohol while driving who were most vulnerable to unmet treatment needs (142). Some preferred not to engage with telehealth by videoconference despite being computer literate because they already spent enough time on the computer (84).
3.3.3.12 Technology-based therapy: inability to communicate effectively (n = 3 studies; published 2017–21)
Some found engagement with interventions delivered by email, telephone, or videoconference difficult (18, 57, 85). Weekly email guidance for an internet-based CBT program was difficult as a form of conversation (57). Older adults had difficulties both hearing and communicating via telehealth by phone, especially those with memory problems, speech or hearing impairments, or serious mental health issues (18). Videoconference was reported to be a poor medium to provide CBT, when cognitive exercises were drawn on a blackboard that could not be seen properly (85).
3.3.3.13 Technology-based therapy: technical issues (n = 3 studies; published 2013–22)
Minor and major technical issues could prevent engagement with computer-assisted SBIRT (143), cellular photo digital breathalyzers (71), and any telehealth intervention (17).
3.3.4 Affordability of PAU services
This dimension reflects a treatment seeker’s capacity to spend money and time on services. It results from direct service-associated costs and opportunity costs associated with lost income (39).
3.3.4.1 Financial barriers (n = 25 studies)
The out-of-pocket cost—determined by the amount charged by the service provider, non-treatment costs such as transportation, and the amount offset by any insurance coverage held by the service user—was found to be a substantial barrier to service accessibility in a large number of studies (n = 26) (21, 47, 58, 64, 66, 72, 75, 81, 91, 92, 95, 97, 100–102, 104, 105, 110, 111, 118–120, 126, 135, 141, 150). In US population-based surveys, 8–20% of respondents reported that they “could not afford to pay the bill” or that “health insurance did not cover it (58, 101, 105),” with people with concurrent mood or anxiety disorders being significantly more likely to express financial barriers to care compared to people without (19.2% vs. 9.8), at least in part attributable to differential insurance coverage between the groups (30.9% vs. 15.9% without insurance, respectively) (105). In US subpopulations, the proportions of people with PAU reporting financial barriers were higher than the general population for veterans (56.3% with concurrent mental health conditions and 45.7% without) (100), Indigenous people (55.4% could not afford and 51.8% had no insurance) (111), and people in the Hispanic community (21, 110), many of whom did not have health insurance due to employment or legal status (135). However, for people using services funded by the Health Resources and Services Administration (HRSA), low proportions expressed financial reasons as a barrier to treatment (2%) (47), and those using an online mutual aid group (81) and a collaborative care model based in primary care (72) found accessibility facilitated by affordable services. Financial barriers in other countries varied, endorsed by 4% of people surveyed in Italy, Germany, Hungary, Latvia, Poland, and Spain (75), 42.2% in Ethiopia (91), and 96.5% in Nepal (66).
Wide variations in insurance coverage drove inequalities in treatment accessibility. In Canada, a two-tiered healthcare system reduced treatment accessibility for those who relied on programs covered by government insurance: those willing to pay out of pocket could access more timely, longer, and more specialized treatment than that offered by insurance-covered programs (150). Similarly, some US Indigenous people felt that insurance would only cover a limited duration of treatment that was inadequate to their needs, and to go elsewhere was too expensive (111). Hispanic men in the USA felt that effective treatment was reserved for those who could afford it or were insured, and that the poor or uninsured could only access inadequate treatment (21, 110).
3.3.5 Appropriateness of PAU services
The appropriateness dimension refers to how well a service meets a treatment seeker’s needs, how quickly it is delivered, how thoroughly health problems are evaluated and treatments selected, and how high a service’s technical and interpersonal standards are (39). The complexity of the care/referral pathway and mental health and PAU treatment silos were also categorized in the Availability dimension and have been covered there.
3.3.5.1 Not meeting eligibility criteria (n = 11 studies)
Treatment seekers suggested that they had not met PAU treatment program eligibility criteria based on condition severity (29, 70, 99), capacity to achieve and sustain abstinence (104), readiness to change (150), immigration status (110), and stable mental health (68, 76, 99, 131), and that sometimes eligibility assessments had been incorrect (e.g., level of severity or readiness to change were misinterpreted) (99, 150). Some treatment seekers felt that PAU treatment was for those who were “really, really ill” or when all else fails (29), or that services were for people who had lost employment, relationships, and/or housing (99), and they therefore assumed that they did not meet eligibility criteria (29, 99).
3.3.5.2 Poor continuity of care (n = 6 studies)
Poor continuity of care within a treatment service negatively impacts the therapeutic relationship between service user and provider, and people with PAU may be less likely to engage with services with known poor continuity of care (29, 68, 104, 114). Staff turnover (29, 68, 104, 114) and inconsistency in providers between different phases of treatment (e.g., screening by a nurse followed by BI from a physician) (93, 138) disrupted existing therapeutic relationships.
3.4 Pau telehealth service accessibility during the COVID-19 pandemic
Three studies reported findings related to PAU telehealth service accessibility during the COVID-19 pandemic in Canada/USA (17), India (16), and the UK (18).
In Canada and the USA, virtual care resources, including online peer-support groups and individual telehealth psychosocial treatment, were embraced because in the process of reducing the risk of coronavirus transmission, they also eliminated the logistical hassles of driving to and from meetings or appointments and mutual aid groups could be accessed any time of the day or night in different locations around the world (17). Some service users felt that online mutual aid groups allowed them to connect and form relationships with others more easily; however, others expressed that online groups provided less meaningful conversations and made forming personal connections more difficult, preferring to have in-person meetings (17). Virtual services were difficult for some to access due to lack of awareness of the services in the community, lack of hardware or internet access, low technological literacy, and technical problems during sessions (17). Although group sessions were helpful toward recovery, some stated that they would appreciate having individual support options during the pandemic to help them maintain a sense of personal responsibility and because “they missed the individualized connection (17).”
In India, 35% of people with AUD sought treatment via telehealth phone calls compared to 2.6% of people with OUD, indicating possibly that those with AUD were less concerned about privacy issues (16). Unwillingness to use telehealth services was endorsed by a low proportion of people with SUDs (11%) (16).
In the UK, older adults with PAU found telehealth appointments by phone to be highly accessible and appreciated not having to travel to appointments, especially those in remote rural areas (18). Telehealth by phone offered greater flexibility in appointment hours, more frequent contact, and was perceived to have greater anonymity than in-person options (18). However, in-person options were preferred by some service users, given the ease of communication compared to the phone: in-person felt more genuine, more personable, easier to follow, and easier to ask for help and to express feelings (18). No participants in the study used telehealth by videoconference during the pandemic, some due to lack of hardware or access to the internet, some due to technological literacy, and others due to health issues or learning difficulties that prevented them from using technology effectively (18).
3.5 Facilitators of service accessibility and service-specific factors
Service users in some studies suggested approaches that could be adopted to overcome service-level barriers and facilitate service accessibility. These facilitators have been summarized in detail by barrier concept in Supplementary Table 8. Briefly, facilitators mainly reflected the barriers reported above, including the following:
• Approachability: participants suggested various media to increase the visibility of PAU services in different contexts and some commented that engagement with a counsellor initially by phone was instrumental in accessing a service.
• Acceptability: participants highlighted factors that increased anonymity (e.g., online services) and endorsed treatment providers/groups with similar demographics or culture to their own, involvement of family or supportive people in treatment, involvement in their own treatment decisions, and choice regarding treatment goal, level of specialization of treatment provider, and spiritual aspects of programs.
• Availability: participants valued telemedicine and treatment embedded into existing services that they regularly attended, flexible appointment hours, and help to navigate complex care pathways.
• Affordability: free treatment, low-fee online programs, and treatment embedded in primary care were considered to facilitate accessibility.
• Appropriateness: maintenance of continuity of care ensured trust between treatment provider and seeker, facilitating care.
Also, some studies focused on specific interventions for which barriers and facilitators were not generalizable to other PAU services (e.g., screening, pharmacotherapy, online programs or apps). These findings have been summarized in Supplementary Table 9.
4 Discussion
To our knowledge, this is the first scoping review to map recent literature regarding service-level barriers to and facilitators of accessibility of PAU treatment services from the perspective of treatment seekers and service users. Our review found numerous unique barriers that were classified to the Levesque framework dimensions of approachability, acceptability, availability, affordability, and appropriateness of PAU services. However, it should be noted that barriers to PAU treatment accessibility do not exist in isolation and multiple barriers from different dimensions may interact to decrease accessibility. For example, one of the barriers that was endorsed across a variety of subpopulations and contexts was that PAU treatment seekers did not know where to go: there was no readily available “door” through which one could access PAU services (Approachability). To find that access point, sometimes multiple disconnected doors must be identified and passed through before access to PAU treatment can be reached, if it’s geographically reachable (Availability). Ultimately, upon gaining access to PAU treatment, treatment seekers may discover that they do not meet eligibility criteria because they do not drink heavily enough, they have a concurrent mental health condition, or they have differing goals compared to those of the program (Appropriateness). Or they may find that the wait period is months long (Availability), the treatment is unaffordable (Affordability), or the program is not culturally appropriate (Acceptability). In being turned away, they may not be directed to a more appropriate treatment service, or that service may not exist. As the final door closes, they have nowhere to go.
As the above example illustrates, several barriers may act together to prevent treatment engagement, and the importance of any given barrier in the treatment seeking process may be difficult to discern. The objective of this scoping review was to map PAU treatment accessibility barriers and not to rank them in order of importance. Although tempting, ranking barriers across studies by vote counting (i.e., inferring that barriers reported more frequently in the literature are of greater importance than those reported less frequently) may be biased by the research questions, populations, contexts, survey tools, and years of conduct of the available primary research studies. The distributions of these study characteristics impact the frequency at which specific barriers may be reported. For example, a few studies (6%) in our review included people with PAU and concurrent mental health conditions. Accordingly, barriers related to concurrent mental health conditions were reported infrequently, including the segregation of mental health services and PAU treatment services, and the inability to meet eligibility criteria requiring the absence of co-existing mental health conditions. Given that the prevalence of co-occurring mental health conditions in people living with PAU is high (152), if vote counting were used, the importance of these barriers would be undervalued. Consequently, we have descriptively summarized the data, attributing equal weight to each barrier.
4.1 Contextualizing findings with other reviews
The service-level barriers to PAU treatment accessibility found in this review generally aligned with barriers identified in other recent systematic, scoping, and narrative reviews of the general SUD literature (153–160), some of which have focused on specific subgroups related to female sex or gender (154, 156, 157, 159) or specific treatment attributes (e.g., treatment goal (160), telehealth mode of delivery (153)).
A recent overview of reviews explored barriers and facilitators to SUD treatment (19). Many of the structural barriers to SUD treatment reported in that review (19) demonstrated a congruence with the PAU treatment barriers in our review, including lengthy waiting periods, lack of suitable services for people with concurrent mental health disorders, treatment affordability, lack of connectivity of referral pathway, lack of gender-suitable treatment, and issues with treatment goal and intensity. Lack of confidentiality, privacy, or anonymity was a frequently endorsed service-level barrier in the studies included in our review that caused fears of stigma (111), deportation (135), and losses of parental rights (53, 58), employment (58, 119, 121), and careers (95, 125). The previous overview of reviews classified these concerns about privacy and fears of stigma and loss of child custody as individual-level barriers (19); however, we considered these barriers as potentially modifiable service barriers. Similarly, we considered a lack of transportation to be a service-level barrier related to the geographic location of the treatment service. In the Levesque framework (39), the five dimensions of accessibility are countered by five corresponding dimensions of capacities of treatment seekers, with which they interact to generate access. Therefore, the service location is balanced by the treatment seeker’s capacity to reach the service, which may lead to inequities in access, if the service is located off public transit or in another city. Offering a treatment service in a more convenient location (i.e., modifying the service-level barrier) may improve access for treatment seekers with limited means of transportation.
Regarding subgroups related to female sex or gender, the accessibility barriers to SUD treatment among pregnant people and mothers reported in two reviews (154, 156) were similar to many in our review, including fear of loss of custody, lack of childcare, or childcare as a competing priority. Many sex-related barriers found in our review were amplified in a scoping review of studies of female veterans for whom mental healthcare in the predominantly male military environment was perceived as unwelcoming and insensitive, necessitating a sex-specific approach (157). Integrated gender-responsive approaches have also been advocated for women with SUD and concurrent mental health disorders to overcome many of the difficulties to treatment engagement faced by this very vulnerable group (159).
Two recent reviews reported barriers to treatment accessibility resulting from specific treatment attributes: non-abstinence approaches (160) and a telehealth delivery model (153). Our review found that abstinence-based PAU treatment may pose a barrier to initial engagement, with consumption reduction approaches being preferred by some treatment seekers. Although consumption reduction approaches have been proposed in the SUD treatment literature, limited empirical research has tested the hypothesis that offering goal choice earlier in the treatment process may increase treatment engagement (160). Barriers to virtual care, including unfamiliarity with technology, lack of internet access or hardware, and communication difficulties via telehealth that were endorsed in our review were also identified in a scoping review of barriers to virtual care in the health system, generally (153).
4.2 Impact of COVID-19 on PAU treatment accessibility
Globally, the availability of PAU treatment services was impacted by COVID-19 and associated public health restrictions (5–10); however, only three studies met our review eligibility criteria regarding COVID-19 impacts. Temporal constraints may account, in part, for the paucity of COVID-19 literature identified, as pandemic-related delays in the conduct and peer review of primary research may have precluded publication prior to our April 2022 search date. Additionally, our review eligibility requirement of service-level barriers meant that studies reporting only policy-level barriers related to the pandemic more broadly, such as lockdowns (7, 161), were ineligible for inclusion. Strategies to mitigate the effects of COVID-19 by substance use treatment facilities early in the pandemic were reported in a scoping review (12). That review identified several mechanisms by which substance use treatment services attempted to support service users, including telehealth, use of remote monitoring devices, altering prescription practices and distribution of medications, and extension or adjustment of appointment hours (12). However, despite attempts to facilitate substance use treatment service accessibility, COVID-19 restrictions and control measures ultimately acted to decrease the availability of care and service capacity by reducing employee working hours, appointment hours, care visits, live-in care beds, and group treatment offerings (12).
4.3 Strengths and limitations of the review methods and the available literature
We used rigorous scoping review methods to identify and synthesize data on a diverse and challenging topic in a replicable and transparent manner. Using a well-established framework, we distilled a large volume of rich qualitative data into a coherent narrative. We optimized qualitative validity and reliability through the use of strict eligibility criteria, a codebook of barriers, open discussion during data extraction/verification, and triangulation of data from multiple studies during synthesis (162). However, as in other studies that have used the Levesque framework (39, 45), our ability to categorize barriers to accessibility dimensions was sometimes limited by the level of detail of the barriers reported in the included studies. Few studies were conducted in low-to-middle-income countries and a large proportion were conducted in the USA, meaning that the findings from the review may have low generalizability outside of high-income countries. Finally, manuscript length prevented full presentation of the extracted data, and we encourage readers to view our Supplementary data sheets.
4.4 Strengths and limitations of the research question
We posed a highly focused research question that concentrated on service-level barriers and did not include person- or societal-level barriers to treatment. This allowed for greater attention to service-level factors that could be modified but did not provide a broad view of the barrier landscape, where cultural drinking norms, lack of awareness or acceptance of the severity of a problem (4, 19), and societal stigma substantively impact initiation of treatment seeking. A variety of sources of stigma are known to negatively influence treatment seeking, including structural stigma, stigma held by service providers, stigma in the community, and self-stigma. While we acknowledge these sources of stigma, they were not considered to be service-level factors and, therefore, were beyond the scope of our review. We also acknowledge that service provider factors, such as knowledge/training, role responsibility, and personality traits (e.g., empathy, self-confidence) can also substantively impact provision of care and retention in care. However, these factors mainly impact treatment accessibility indirectly (e.g., by reducing availability of care), and therefore we elected not to include these factors.
4.5 Future directions
Our review findings could be used to support the design and implementation of new treatment services or modification of existing services for people with PAU. The rich qualitative findings from our review will allow future discrete choice experiments (DCEs) to draw on the views of people with PAU, lessening the chance of misspecification of preferred service characteristics as a result of placing too much weight on the opinions of experts or researchers (163). We recognize that barriers to provision of care also negatively impact treatment availability and, therefore, treatment accessibility, and future research should consider this perspective.
5 Conclusion
In conclusion, modifiable service-level barriers to the accessibility of PAU treatment are rich in diversity and depth. While many different barrier concepts determined the acceptability of a treatment service from the perspective of people with PAU, the affordability and availability of the service also appeared prominently in primary studies. The results from this scoping review can be used to develop strategies to determine the importance of specific service-level barriers to PAU treatment accessibility within a given context or population, with an ultimate goal of targeted modification of existing treatment services and design of new diverse services to overcome accessibility issues.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
DW: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. BH: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. KC: Conceptualization, Funding acquisition, Investigation, Methodology, Validation, Writing – review & editing. NC: Conceptualization, Funding acquisition, Investigation, Methodology, Validation, Writing – review & editing. SNg: Conceptualization, Funding acquisition, Investigation, Methodology, Validation, Writing – review & editing. SNo: Data curation, Methodology, Resources, Validation, Writing – review & editing. JP: Conceptualization, Funding acquisition, Investigation, Methodology, Project administration, Validation, Writing – review & editing. AG: Data curation, Resources, Validation, Writing – review & editing. MD: Data curation, Resources, Validation, Writing – review & editing. AP: Data curation, Resources, Validation, Writing – review & editing. KS: Funding acquisition, Resources, Validation, Writing – review & editing. BS: Methodology, Project administration, Resources, Software, Writing – review & editing. MB: Funding acquisition, Validation, Writing – review & editing. GG: Funding acquisition, Validation, Writing – review & editing. LD: Funding acquisition, Validation, Writing – review & editing. AP: Funding acquisition, Validation, Writing – review & editing. BP: Funding acquisition, Validation, Writing – review & editing. SK: Conceptualization, Validation, Writing – review & editing. AE: Conceptualization, Methodology, Validation, Writing – review & editing. KT: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Supervision, Validation, Visualization, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. The authors declare that this study received funding from Canadian Institutes of Health Research (grant # EG7- 179464). The funder was not involved in the study design, collection, analysis, interpretation of data, the writing of this article, or the decision to submit it for publication.
Acknowledgments
We would like to kindly thank Leila Esmaeilisaraji, Marco Ghassemi, Candyce Hamel, Paul Khan, Danielle Rice, and Naazish Shariff for their contributions toward reference screening; Kaitryn Campbell for peer review of the MEDLINE search strategy; Karen Cohen for her expertise and support during the grant procurement process, and for knowledge dissemination; and Melanie Willows for her clinical expertise.
Conflict of interest
BH has previously received honoraria from Eversana Inc. for methodologic advice related to the performance of systematic reviews and meta-analysis.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
KT declares that they were an editorial board member of Frontiers, at the time of submission. This had no impact on the peer review process and the final decision.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2023.1296239/full#supplementary-material
Abbreviations
AA, Alcoholics Anonymous; AUD, alcohol use disorder; CBT, cognitive behavioral therapy; COVID-19, coronavirus disease 2019; DCE, discrete choice experiment; ED, emergency department; OUD, opioid use disorder; PAU, problematic alcohol use; SBI, screening and brief intervention; SBIRT, screening, brief intervention, and referral to therapy; SUD, substance use disorder.
References
1. Paradis, C, Butt, P, Shield, K, Poole, N, Wells, S, Naimi, T, et al. The low-risk alcohol drinking guidelines scientific expert panels. Canada's guidance on alcohol and health: Final report. Ottawa, ON: Canadian Centre on Substance Use and Addiction (2023). ISBN 978–1–77871-046-9.
2. GBD. Alcohol collaborators. Alcohol use and burden for 195 countries and territories, 1990-2016: a systematic analysis for the global burden of disease study 2016. Lancet. (2016) 392:1015–35. doi: 10.1016/s0140-6736(18)31310-2
3. Mekonen, T, Chan, GCK, Connor, J, Hall, W, Hides, L, and Leung, J. Treatment rates for alcohol use disorders: a systematic review and meta-analysis. Addiction. (2021) 116:2617–34. doi: 10.1111/add.15357
4. Venegas, A, Donato, S, Meredith, LR, and Ray, LA. Understanding low treatment seeking rates for alcohol use disorder: a narrative review of the literature and opportunities for improvement. Am J Drug Alcohol Abuse. (2021) 47:664–79. doi: 10.1080/00952990.2021.1969658
5. Abbas, MJ, Kronenberg, G, McBride, M, Chari, D, Alam, F, Mukaetova-Ladinska, E, et al. The early impact of the COVID-19 pandemic on acute care mental health services. Psychiatr Serv. (2021) 72:242–6. doi: 10.1176/appi.ps.202000467
6. Hoyer, C, Ebert, A, Szabo, K, Platten, M, Meyer-Lindenberg, A, and Kranaster, L. Decreased utilization of mental health emergency service during the COVID-19 pandemic. Eur Arch Psychiatry Clin Neurosci. (2021) 271:377–9. doi: 10.1007/s00406-020-01151-w
7. Swahn, MH, Balenger, A, Umenze, F, Aneja, R, Bureh, TA, and Obot, I. Impact of the COVID-19 pandemic on alcohol treatment access and harm prevention in West Africa: reports from NGOs and community-based organizations. J Epidemiol Glob Health. (2022) 12:160–7. doi: 10.1007/s44197-022-00035-7
8. Tromans, S, Chester, V, Harrison, H, Pankhania, P, Booth, H, and Chakraborty, N. Patterns of use of secondary mental health services before and during COVID-19 lockdown: observational study. BJPsych Open. (2020) 6:e117. doi: 10.1192/bjo.2020.104
9. Zielasek, J, Vrinssen, J, and Gouzoulis-Mayfrank, E. Utilization of inpatient mental health Care in the Rhineland during the COVID-19 pandemic. Front Public Health. (2021) 9:593307. doi: 10.3389/fpubh.2021.593307
10. World Health Organization. COVID-19 disrupting mental health services in most countries WHO survey [internet] (2020). Available at: https://www.who.int/news/item/05-10-2020-covid-19-disrupting-mental-health-services-in-most-countries-who-survey (accessed 5 May 2022).
11. Columb, D, Hussain, R, and O'Gara, C. Addiction psychiatry and COVID-19: impact on patients and service provision. Ir J Psychol Med. (2020) 37:164–8. doi: 10.1017/ipm.2020.47
12. de Vargas, D, Pereira, CF, Volpato, RJ, Lima, AVC, da Silva, FR, de Oliveira, SR, et al. Strategies adopted by addiction facilities during the coronavirus pandemic to support treatment for individuals in recovery or struggling with a substance use disorder: a scoping review. Int J Environ Res Public Health. (2021) 18:18. doi: 10.3390/ijerph182212094
13. Del Palacio-Gonzalez, A, Thylstrup, B, and Houborg, E. The impact of the COVID-19 lockdown on services for substance use in Denmark: implications for meeting users' needs and recommendations for the future. Nordisk Alkohol Nark. (2022) 39:175–89. doi: 10.1177/14550725211069229
14. Perri, M, Schmidt, RA, Guta, A, Kaminski, N, Rudzinski, K, and Strike, C. COVID-19 and the opportunity for gender-responsive virtual and remote substance use treatment and harm reduction services. Int J Drug Policy. (2022) 108:103815. doi: 10.1016/j.drugpo.2022.103815
15. Rodda, SN, Park, JJ, Wilkinson-Meyers, L, and King, DL. The impact of COVID-19 on addiction treatment in New Zealand. Addict Behav. (2022) 127:107230. doi: 10.1016/j.addbeh.2021.107230
16. Arya, S, Ghosh, A, Mishra, S, Swami, M, Prasad, S, Somani, A, et al. A multicentric survey among patients with substance use disorders during the COVID-19 lockdown in India. Indian J Psychiatry. (2022) 64:48–55. doi: 10.4103/indianjpsychiatry.indianjpsychiatry_557_21
17. Scarfe, ML, Haik, AK, Rahman, L, Todi, AA, Kane, C, Walji, A, et al. Impact of COVID-19 on alcohol use disorder recovery: a qualitative study. Exp Clin Psychopharmacol. (2022) 31:148–62. doi: 10.1037/pha0000560
18. Seddon, J, Trevena, P, Wadd, S, Elliott, L, Dutton, M, McCann, M, et al. Addressing the needs of older adults receiving alcohol treatment during the COVID-19 pandemic: a qualitative study. Aging Ment Health. (2021) 26:919–24. doi: 10.1080/13607863.2021.1910794
19. Farhoudian, A, Razaghi, E, Hooshyari, Z, Noroozi, A, Pilevari, A, Mokri, A, et al. Barriers and facilitators to substance use disorder treatment: an overview of systematic reviews. Subst Abuse. (2022) 16:1118462. doi: 10.1177/11782218221118462
20. Schober, R, and Annis, HM. Barriers to help-seeking for change in drinking: a gender-focused review of the literature. Addict Behav. (1996) 21:81–92. doi: 10.1016/0306-4603(95)00041-0
21. Valdez, LA, Garcia, DO, Ruiz, J, Oren, E, and Carvajal, S. Exploring structural, sociocultural, and individual barriers to alcohol abuse treatment among Hispanic men [research support, non-U.S. Gov't]. Am j. (2018) 12:1948–57. doi: 10.1177/1557988318790882
22. Glauser, W, Tepper, J, and Tierney, M. Health care system is failing people with alcohol addiction, say experts (2015). Available at: https://healthydebate.ca/2015/09/topic/alcohol-addiction-diagnosis-and-treatment/ (accessed 5 May 2022).
23. National Treatment Strategy Working Group. A Systems Approach to Substance Use in Canada: Recommendations for a National Treatment Strategy (2008). Canadian Centre on substance use and addiction. Available at: https://www.ccsa.ca/systems-approach-substance-use-canada-recommendations-national-treatment-strategy.
24. Pascoe, RV, Rush, B, and Rotondi, NK. Wait times for publicly funded addiction and problem gambling treatment agencies in Ontario. Canada BMC Health Serv Res. (2013) 13:483. doi: 10.1186/1472-6963-13-483
25. Posselt, M, McDonald, K, Procter, N, de Crespigny, C, and Galletly, C. Improving the provision of services to young people from refugee backgrounds with comorbid mental health and substance use problems: addressing the barriers. BMC Public Health. (2017) 17:280. doi: 10.1186/s12889-017-4186-y
26. Saitz, R, Larson, MJ, Labelle, C, Richardson, J, and Samet, JH. The case for chronic disease management for addiction. J Addict Med. (2008) 2:55–65. doi: 10.1097/ADM.0b013e318166af74
27. Cane, J, O'Connor, D, and Michie, S. Validation of the theoretical domains framework for use in behaviour change and implementation research. Implement Sci. (2012) 7:37. doi: 10.1186/1748-5908-7-37
28. Michie, S, van Stralen, MM, and West, R. The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implement Sci. (2011) 6:42. doi: 10.1186/1748-5908-6-42
29. Gilburt, H, Drummond, C, and Sinclair, J. Navigating the alcohol treatment pathway: a qualitative study from the service Users' perspective [research support, non-U.S. Gov't]. Alcohol Alcohol. (2015) 50:444–50. doi: 10.1093/alcalc/agv027
30. Campbell, F, Tricco, AC, Munn, Z, Pollock, D, Saran, A, Sutton, A, et al. Mapping reviews, scoping reviews, and evidence and gap maps (EGMs): the same but different- the "big picture" review family. Syst Rev. (2023) 12:45. doi: 10.1186/s13643-023-02178-5
31. Arksey, H, and O'Malley, L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. (2005) 8:19–32. doi: 10.1080/1364557032000119616
32. Peters, MDJ, Godfrey, C, McInerney, P, Munn, Z, Tricco, AC, and Khalil, H. Chapter 11: scoping reviews In: E Aromataris and Z Munn, editors. Joanna Briggs institute Reviewer's manual (2020). Available at: https://synthesismanual.jbi.global (Accessed May 5, 2022).
33. Levac, D, Colquhoun, H, and O'Brien, KK. Scoping studies: advancing the methodology. Implementat Sci. (2010) 5:69. doi: 10.1186/1748-5908-5-69
34. Peters, MDJ, Godfrey, CM, Khalil, H, McInerney, P, Parker, D, and Soares, CB. Guidance for conducting systematic scoping reviews. Int J Evid Based Healthc. (2015) 13:141–6. doi: 10.1097/xeb.0000000000000050
35. Thomas, A, Lubarsky, S, Durning, SJ, and Young, ME. Knowledge syntheses in medical education: demystifying scoping reviews. Acad Med. (2017) 92:161–6. doi: 10.1097/acm.0000000000001452
36. Tricco, AC, Lillie, E, Zarin, W, O'Brien, KK, Colquhoun, H, Levac, D, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. (2018) 169:467–73. doi: 10.7326/m18-0850
37. Tong, A, Flemming, K, McInnes, E, Oliver, S, and Craig, J. Enhancing transparency in reporting the synthesis of qualitative research: ENTREQ. BMC Med Res Methodol. (2012) 12:181. doi: 10.1186/1471-2288-12-181
38. Wolfe, D, Hutton, B, Corace, K, Chaiyakunapruk, N, Ngorsuraches, S, Nochaiwong, S, et al. Service-level barriers to and facilitators of access to services for the treatment of alcohol use disorder and problematic alcohol use: protocol for a scoping review. BMJ Open. (2022) 12:e064578. doi: 10.1136/bmjopen-2022-064578
39. Levesque, JF, Harris, MF, and Russell, G. Patient-centred access to health care: conceptualising access at the interface of health systems and populations. Int J Equity Health. (2013) 12:18. doi: 10.1186/1475-9276-12-18
40. Francis, JJ, Johnston, M, Robertson, C, Glidewell, L, Entwistle, V, Eccles, MP, et al. What is an adequate sample size? Operationalising data saturation for theory-based interview studies. Psychol Health. (2010) 25:1229–45. doi: 10.1080/08870440903194015
41. McGowan, J, Sampson, M, Salzwedel, DM, Cogo, E, Foerster, V, and Lefebvre, C. PRESS peer review of electronic search strategies: 2015 guideline statement. J Clin Epidemiol. (2016) 75:40–6. doi: 10.1016/j.jclinepi.2016.01.021
42. Hamel, C, Hersi, M, Kelly, SE, Tricco, AC, Straus, S, Wells, G, et al. Guidance for using artificial intelligence for title and abstract screening while conducting knowledge syntheses. BMC Med Res Methodol. (2021) 21:285. doi: 10.1186/s12874-021-01451-2
43. Campbell, R, Pound, P, Morgan, M, Daker-White, G, Britten, N, Pill, R, et al. Evaluating meta-ethnography: systematic analysis and synthesis of qualitative research. Health Technol Assess. (2011) 15:1–164. doi: 10.3310/hta15430
44. Noblit, G, and Hare, D. Meta-ethnography: Synthesiszing qualitative studies. Thousand Oaks, CA: Sage Publications (1988).
45. Cu, A, Meister, S, Lefebvre, B, and Ridde, V. Assessing healthcare access using the Levesque's conceptual framework- a scoping review. Int J Equity Health. (2021) 20:116. doi: 10.1186/s12939-021-01416-3
46. Alessi, SM, Barnett, NP, and Petry, NM. Experiences with SCRAMx alcohol monitoring technology in 100 alcohol treatment outpatients. Drug Alcohol Depend. (2017) 178:417–24. doi: 10.1016/j.drugalcdep.2017.05.031
47. Bearnot, B, Rigotti, NA, and Baggett, TP. Access to treatment for alcohol use disorder at US health centers: a National Study [letter research support, non-U.S. Gov't]. J Gen Intern Med. (2018) 33:2040–2. doi: 10.1007/s11606-018-4631-3
48. Black, N, Loomes, M, Juraskova, I, and Johnston, I. Engagement in a novel internet intervention for alcohol reduction: a qualitative study of user motivations and experiences. Cyberpsychol Behav Soc Netw. (2020) 23:225–33. doi: 10.1089/cyber.2019.0289
49. Carlebach, S, Wake, D, and Hamilton, S. Experiences of home detoxification for alcohol dependency [research support, non-U.S. Gov't]. Nurs Stand. (2011) 26:41–7. doi: 10.7748/ns2011.11.26.10.41.c8817
50. Chen, A, Smart, Y, Morris-Patterson, A, and Katz, CL. Piloting self-help groups for alcohol use disorders in Saint Vincent/Grenadines [research support, non-U.S. Gov't]. Ann Glob Health. (2014) 80:83–8. doi: 10.1016/j.aogh.2014.04.003
51. Costa, M, Barre, T, Coste, M, Yaya, I, Berenger, C, Tanti, M, et al. Screening and care for alcohol use disorder in France: expectations, barriers and levers using a mixed-methods approach. BMC Public Health. (2020) 20:358. doi: 10.1186/s12889-020-08495-x
52. Croxford, A, Notley, CJ, Maskrey, V, Holland, R, and Kouimtsidis, C. An exploratory qualitative study seeking participant views evaluating group cognitive behavioral therapy preparation for alcohol detoxification. J Subst Abus. (2015) 20:61–8. doi: 10.3109/14659891.2014.894590
53. Ekstrom, V, and Johansson, M. Choosing internet-based treatment for problematic alcohol use-why, when and how? Users' experiences of treatment online [research support, non-U.S. Gov't]. Addict Sci Clin Pract. (2020) 15. doi: 10.1186/s13722-020-00196-5
54. Falconer, BJ. (2015) An exploration of participants' experiences of the LifeRing secular recovery support group model in the management of chronic alcohol dependence [Psy.D dissertation]. [Berkeley, CA]: Wright Institute Graduate School of Psychology.
55. Giroux, D, Bacon, S, King, DK, Dulin, P, and Gonzalez, V. Examining perceptions of a smartphone-based intervention system for alcohol use disorders [research support, N.I.H., extramural]. Telemed J E Health. (2014) 20:923–9. doi: 10.1089/tmj.2013.0222
56. Green-Hamann, S, Campbell Eichhorn, K, and Sherblom, JC. An exploration of why people participate in second life social support groups [empirical study; interview; qualitative study]. J Comput-Mediat Commun. (2011) 16:465–91. doi: 10.1111/j.1083-6101.2011.01543.x
57. Hadjistavropoulos, HD, Chadwick, C, Beck, CD, Edmonds, M, Sundstrom, C, Edwards, W, et al. Improving internet-delivered cognitive behaviour therapy for alcohol misuse: patient perspectives following program completion. Internet Interv. (2021) 26:100474. doi: 10.1016/j.invent.2021.100474
58. Haeny, AM, Oluwoye, O, Cruz, R, Iheanacho, T, Jackson, AB, Fisher, S, et al. Drug and alcohol treatment utilization and barriers among Black, American Indian/Alaskan native, Latine, Asian/Pacific islander/native Hawaiian, and White adults: findings from NESARC-III [research support, N.I.H., extramural]. J Subst Abus Treat. (2021) 131:108569. doi: 10.1016/j.jsat.2021.108569
59. Hattingh, HL, Hallett, J, and Tait, RJ. 'Making the invisible visible' through alcohol screening and brief intervention in community pharmacies: an Australian feasibility study [evaluation study]. BMC Public Health. (2016) 16:1141. doi: 10.1186/s12889-016-3805-3
60. Herring, R, Thom, B, Bayley, M, and Tchilingirian, J. Delivering alcohol identification and brief advice (IBA) in housing settings: a step too far or opening doors? Drugs: education. Prevent Policy. (2016) 23:365–73. doi: 10.1080/09687637.2016.1176992
61. Heyes, CM, Baillie, AJ, Schofield, T, Gribble, R, and Haber, PS. The reluctance of liver transplant participants with alcoholic liver disease to participate in treatment for their alcohol use disorder: an issue of treatment matching? Alcohol Treat Q. (2016) 34:233–51. doi: 10.1080/07347324.2016.1148515
62. Ippolito, TA. Safe in the rooms of a.a.: how anonymity helps reduce the stigma of help-seeking and reinforces solidarity and group cohesiveness. Alcohol Treat Q. (2020) 38:2–20. doi: 10.1080/07347324.2019.1647772
63. Khadjesari, Z, Stevenson, F, Godfrey, C, and Murray, E. Negotiating the 'grey area between normal social drinking and being a smelly tramp': a qualitative study of people searching for help online to reduce their drinking [research support, non-U.S. Gov't]. Health Expect. (2015) 18:2011–20. doi: 10.1111/hex.12351
64. Koffarnus, MN, Kablinger, AS, Kaplan, BA, and Crill, EM. Remotely administered incentive-based treatment for alcohol use disorder with participant-funded incentives is effective but less accessible to low-income participants [randomized controlled trial]. Exp Clin Psychopharmacol. (2021) 29:555–65. doi: 10.1037/pha0000503
65. Lieberman, DZ, Cioletti, A, Massey, SH, Collantes, RS, and Moore, BB. Treatment preferences among problem drinkers in primary care. Int J Psychiatry Med. (2014) 47:231–40. doi: 10.2190/PM.47.3.d
66. Luitel, NP, Jordans, MJD, Kohrt, BA, Rathod, SD, and Komproe, IH. Treatment gap and barriers for mental health care: a cross-sectional community survey in Nepal. PLoS One. (2017) 12:e0183223. doi: 10.1371/journal.pone.0183223
67. Mackridge, AJ, Krska, J, Stokes, EC, and Heim, D. Towards improving service delivery in screening and intervention services in community pharmacies: a case study of an alcohol IBA service. J Public Health (Oxf). (2016) 38:92–8. doi: 10.1093/pubmed/fdv010
68. McCallum, SL, Mikocka-Walus, AA, Gaughwin, MD, Andrews, JM, and Turnbull, DA. 'I'm a sick person, not a bad person': patient experiences of treatments for alcohol use disorders [research support, non-U.S. Gov't]. Health Expect. (2016) 19:828–41. doi: 10.1111/hex.12379
69. Medina Ch, AM, Torrey, WC, Vargas, S, Uribe-Restrepo, JM, and Gomez-Restrepo, C. Network of actors involved in the identification, care, and follow-up of unhealthy alcohol use in primary care in Colombia. Rev Colomb Psiquiatr (Engl Ed). (2021) 50:83–90. doi: 10.1016/j.rcpeng.2021.06.007
70. Murray, E, Linke, S, Harwood, E, Conroy, S, Stevenson, F, and Godfrey, C. Widening access to treatment for alcohol misuse: description and formative evaluation of an innovative web-based service in one primary care trust [multicenter study research support, non-U.S. Gov't]. Alcohol Alcohol. (2012) 47:697–01. doi: 10.1093/alcalc/ags096
71. Nehlin, C, Carlsson, K, and Oster, C. Patients' experiences of using a cellular photo digital breathalyzer for treatment purposes. J Addict Med. (2018) 12:107–12. doi: 10.1097/ADM.0000000000000373
72. O'Grady, MA, Conigliaro, J, Levak, S, Morley, J, Kapoor, S, Ritter, M, et al. "I felt I was reaching a point with my health": understanding reasons for engagement and acceptability of treatment Services for Unhealthy Alcohol use in primary care. Journal of primary Care & Community. Health. (2021) 12:1–10. doi: 10.1177/21501327211003005
73. Parkman, T, and Lloyd, C. How intense is too intense? A qualitative exploration of a structured day treatment program for substance dependency in the United Kingdom. Alcohol Treat Q. (2016) 34:274–91. doi: 10.1080/07347324.2016.1182816
74. Pitman, K. (2016) Addiction recovery: A comparison of the perceptions of alcohol-dependent individuals and mental health professionals [Psy.D dissertation] [Philadelphia, PA]: Chestnut Hill College.
75. Probst, C, Manthey, J, Martinez, A, and Rehm, J. Alcohol use disorder severity and reported reasons not to seek treatment: a cross-sectional study in European primary care practices [research support, non-U.S. Gov't]. Subst Abuse Treat Prev Policy. (2015) 10. doi: 10.1186/s13011-015-0028-z
76. Roberts, E, Hillyard, M, Hotopf, M, Parkin, S, and Drummond, C. Access to specialist community alcohol treatment in England, and the relationship with alcohol-related hospital admissions: qualitative study of service users, service providers and service commissioners. BJPsych Open. (2020) 6:e94. doi: 10.1192/bjo.2020.80
77. Rose, GL, MacLean, CD, Skelly, J, Badger, GJ, Ferraro, TA, and Helzer, JE. Interactive voice response technology can deliver alcohol screening and brief intervention in primary care [comparative study research support, N.I.H., extramural]. J Gen Intern Med. (2010) 25:340–4. doi: 10.1007/s11606-009-1233-0
78. Sari, S, Muller, AE, and Roessler, KK. Exercising alcohol patients don't lack motivation but struggle with structures, emotions and social context - a qualitative dropout study. BMC Fam Pract. (2017) 18:45. doi: 10.1186/s12875-017-0606-4
79. Scholer, PN, Sondergaard, J, Barfod, S, and Nielsen, AS. Danish feasibility study of a new innovation for treating alcohol disorders in primary care: the 15-method. BMC Prim Care. (2022) 23:34. doi: 10.1186/s12875-022-01639-5
80. Shannon, CL, Bartels, SM, Cepeda, M, Castro, S, Cubillos, L, Suarez-Obando, F, et al. Perspectives on the implementation of screening and treatment for depression and alcohol use disorder in primary Care in Colombia [research support, N.I.H., extramural]. Community Ment Health J. (2021) 57:1579–87. doi: 10.1007/s10597-021-00781-1
81. Sinclair, JMA, Chambers, SE, and Manson, CC. Internet support for dealing with problematic alcohol use: a survey of the soberistas online community. Alcohol Alcohol. (2017) 52:220–6. doi: 10.1093/alcalc/agw078
82. Sturgiss, E, Lam, T, Russell, G, Ball, L, Gunatillaka, N, Barton, C, et al. Patient and clinician perspectives of factors that influence the delivery of alcohol brief interventions in Australian primary care: a qualitative descriptive study. Fam Pract. (2022) 39:275–81. doi: 10.1093/fampra/cmab091
83. Sundstrom, C, Gajecki, M, Johansson, M, Blankers, M, Sinadinovic, K, Stenlund-Gens, E, et al. Guided and unguided internet-based treatment for problematic alcohol use - a randomized controlled pilot trial [randomized controlled trial]. PLoS One. (2016) 11:e0157817. doi: 10.1371/journal.pone.0157817
84. Tarp, K, Mejldal, A, and Nielsen, AS. Videoconferencing-based treatment of alcohol use disorders: analyses of nonparticipation. JMIR Form Res. (2017) 1:e3. doi: 10.2196/formative.6715
85. Tarp, K, and Nielsen, AS. Patient perspectives on videoconferencing-based treatment for alcohol use disorders. Alcohol Treat Q. (2017) 35:344–58. doi: 10.1080/07347324.2017.1348785
86. Vasseur, C, Montariol, Y, Petregne, F, Fleury, B, and Castera, P. Place de l’abstinence et de la consommation contrôlée. Alcoologie et Addictologie. (2019) 41:5–13.
87. Villalba, K, Cook, C, Devieux, JG, Ibanez, GE, Oghogho, E, Neira, C, et al. Facilitators and barriers to a contingency management alcohol intervention involving a transdermal alcohol sensor. Heliyon. (2020) 6:e03612. doi: 10.1016/j.heliyon.2020.e03612
88. Wallhed Finn, S, Bakshi, AS, and Andreasson, S. Alcohol consumption, dependence, and treatment barriers: perceptions among nontreatment seekers with alcohol dependence. Subst Use Misuse. (2014) 49:762–9. doi: 10.3109/10826084.2014.891616
89. Wieczorek, L. Barriers in the access to alcohol treatment in outpatient clinics in urban and rural community. Psychiatr Pol. (2017) 51:125–38. doi: 10.12740/PP/60345
90. Zemore, SE, Kaskutas, LA, Mericle, A, and Hemberg, J. Comparison of 12-step groups to mutual help alternatives for AUD in a large, national study: differences in membership characteristics and group participation, cohesion, and satisfaction [comparative study]. J Subst Abus Treat. (2017) 73:16–26. doi: 10.1016/j.jsat.2016.10.004
91. Zewdu, S, Hanlon, C, Fekadu, A, Medhin, G, and Teferra, S. Treatment gap, help-seeking, stigma and magnitude of alcohol use disorder in rural Ethiopia [research support, non-U.S. Gov't]. Subst Abuse Treat Prev Policy. (2019) 14. doi: 10.1186/s13011-019-0192-7
92. Allen, JL, and Mowbray, O. Sexual orientation, treatment utilization, and barriers for alcohol related problems: findings from a nationally representative sample. Drug Alcohol Depend. (2016) 161:323–30. doi: 10.1016/j.drugalcdep.2016.02.025
93. Bedard-Gilligan, M, Masters, NT, Ojalehto, H, Simpson, TL, Stappenbeck, C, and Kaysen, D. Refinement and pilot testing of a brief, early intervention for PTSD and alcohol use following sexual assault. Cogn. (2020) 27:470–86. doi: 10.1016/j.cbpra.2019.10.003
94. Burner, E, Zhang, M, Terp, S, Ford Bench, K, Lee, J, Lam, CN, et al. Feasibility and acceptability of a text message-based intervention to reduce overuse of alcohol in emergency department patients: controlled proof-of-concept trial [clinical trial research support, non-U.S. Gov't research support, U.S. Gov't, P.H.S.]. JMIR Mhealth Uhealth. (2020) 8:e17557. doi: 10.2196/17557
95. Burnett-Zeigler, I, Ilgen, M, Valenstein, M, Zivin, K, Gorman, L, Blow, A, et al. Prevalence and correlates of alcohol misuse among returning Afghanistan and Iraq veterans [research support, non-U.S. Gov't research support, U.S. Gov't, non-P.H.S.]. Addict Behav. (2011) 36:801–6. doi: 10.1016/j.addbeh.2010.12.032
96. Chambers, SE, Canvin, K, Baldwin, DS, and Sinclair, JMA. Identity in recovery from problematic alcohol use: a qualitative study of online mutual aid. Drug Alcohol Depend. (2017) 174:17–22. doi: 10.1016/j.drugalcdep.2017.01.009
97. Clark, BJ, Jones, J, Reed, KD, Hodapp, R, Douglas, IS, Van Pelt, D, et al. The experience of patients with alcohol misuse after surviving a critical illness. A qualitative study. Ann Am Thorac Soc. (2017) 14:1154–61. doi: 10.1513/AnnalsATS.201611-854OC
98. Darvell, MJ, Kavanagh, DJ, and Connolly, JM. A qualitative exploration of internet-based treatment for comorbid depression and alcohol misuse. Internet Interv. (2015) 2:174–82. doi: 10.1016/j.invent.2015.03.003
99. Dorey, L, Lathlean, J, Roderick, P, and Westwood, G. Patient experiences of alcohol specialist nurse interventions in a general hospital, and onwards care pathways. J Adv Nurs. (2021) 77:1945–55. doi: 10.1111/jan.14777
100. Elbogen, EB, Wagner, HR, Johnson, SC, Kinneer, P, Kang, H, Vasterling, JJ, et al. Are Iraq and Afghanistan veterans using mental health services? New data from a national random-sample survey [research support, N.I.H., extramural research support, U.S. Gov't, non-P.H.S.]. Psychiatr Serv. (2013) 64:134–41. doi: 10.1176/appi.ps.004792011
101. Gilbert, PA, Pro, G, Zemore, SE, Mulia, N, and Brown, G. Gender differences in use of alcohol treatment services and reasons for nonuse in a National Sample [research support, N.I.H., extramural]. Alcohol Clin Exp Res. (2019) 43:722–31. doi: 10.1111/acer.13965
102. Green, KE. Barriers and treatment preferences reported by worried drinkers of various sexual orientations. Alcohol Treat Q. (2011) 29:45–63. doi: 10.1080/07347324.2011.538311
103. Gustafsson, S, Nyberg, J, and Hrelja, R. The Swedish joint action method against drink driving-a study of suspected drink drivers' own experiences [review]. Traffic Inj Prev. (2016) 17:558–63. doi: 10.1080/15389588.2015.1132417
104. Haighton, C, Wilson, G, Ling, J, McCabe, K, Crosland, A, and Kaner, E. A qualitative study of service provision for alcohol related health issues in mid to later life [research support, non-U.S. Gov't]. PLoS One. (2016) 11:e0148601. doi: 10.1371/journal.pone.0148601
105. Kaufmann, CN, Chen, LY, Crum, RM, and Mojtabai, R. Treatment seeking and barriers to treatment for alcohol use in persons with alcohol use disorders and comorbid mood or anxiety disorders [research support, N.I.H., extramural]. Soc Psychiatry Psychiatr Epidemiol. (2014) 49:1489–99. doi: 10.1007/s00127-013-0740-9
106. Kiernan, MD, Osbourne, A, McGill, G, Jane Greaves, P, Wilson, G, and Hill, M. Are veterans different? Understanding veterans' help-seeking behaviour for alcohol problems. Health Soc Care Community. (2018) 31:31. doi: 10.1111/hsc.12585
107. Pinedo, M, Zemore, S, Beltran-Giron, J, Gilbert, P, and Castro, Y. Women's barriers to specialty substance abuse treatment: a qualitative exploration of racial/ethnic differences. J Immigr Minor Health. (2020) 22:653–60. doi: 10.1007/s10903-019-00933-2
108. Suffoletto, B, Kristan, J, Person Mecca, L, Chung, T, and Clark, DB. Optimizing a text message intervention to reduce heavy drinking in Young adults: focus group findings. JMIR Mhealth Uhealth. (2016) 4:e73. doi: 10.2196/mhealth.5330
109. Taak, K, Brown, J, and Perski, O. Exploring views on alcohol consumption and digital support for alcohol reduction in UK-based Punjabi-Sikh men: a think aloud and interview study. Drug Alcohol Rev. (2020) 40:231–8. doi: 10.1111/dar.13172
110. Valdez, LA. (2018) Exploring the intersected influences of sociocultural norms and the social context on alcohol and substance abuse in Hispanic men [PhD dissertation]. [Tucson, AZ]: University of Arizona
111. Venner, KL, Greenfield, BL, Vicuna, B, Munoz, R, Bhatt, S, and O'Keefe, V. "I'm not one of them": barriers to help-seeking among American Indians with alcohol dependence [research support, N.I.H., extramural]. Cultur Divers Ethni Minor Psychol. (2012) 18:352–62. doi: 10.1037/a0029757
112. Buscemi, J, Murphy, JG, Martens, MP, McDevitt-Murphy, ME, Dennhardt, AA, and Skidmore, JR. Help-seeking for alcohol-related problems in college students: correlates and preferred resources [research support, N.I.H., extramural research support, non-U.S. Gov't]. Psychol Addict Behav. (2010) 24:571–80. doi: 10.1037/a0021122
113. Chambers, SE, Baldwin, DS, and Sinclair, JMA. Course and outcome of patients with alcohol use disorders following an alcohol intervention during hospital attendance: mixed method study. BJPsych Open. (2020) 7:e6. doi: 10.1192/bjo.2020.138
114. Collins, SE, Jones, CB, Hoffmann, G, Nelson, LA, Hawes, SM, Grazioli, VS, et al. In their own words: content analysis of pathways to recovery among individuals with the lived experience of homelessness and alcohol use disorders [research support, N.I.H., extramural research support, non-U.S. Gov't]. Int J Drug Policy. (2016) 27:89–96. doi: 10.1016/j.drugpo.2015.08.003
115. Field, CA, Klimas, J, Barry, J, Bury, G, Keenan, E, Smyth, BP, et al. Problem alcohol use among problem drug users in primary care: a qualitative study of what patients think about screening and treatment [research support, non-U.S. Gov't]. BMC Fam Pract. (2013) 14:98. doi: 10.1186/1471-2296-14-98
116. Heyes, CM, Schofield, T, Gribble, R, Day, CA, and Haber, PS. Reluctance to accept alcohol treatment by alcoholic liver disease transplant patients: a qualitative study. Transplant Direct. (2016) 2:e104. doi: 10.1097/TXD.0000000000000617
117. Klingemann, J, Welbel, M, Nicaise, P, Priebe, S, Matanov, A, Bird, V, et al. Assessment and treatment of patients with comorbidity of mental health problems and alcohol use disorders: experiences of clinicians and patients in the UK and Poland [empirical study; interview; qualitative study]. Alcohol Alcohol. (2019) 54:279–86. doi: 10.1093/alcalc/agz023
118. Lewis, ET, Jamison, AL, Ghaus, S, Durazo, EM, Frayne, SM, Hoggatt, KJ, et al. Receptivity to alcohol-related care among U.S. women veterans with alcohol misuse [research support, U.S. Gov't, non-P.H.S.]. J Addict Dis. (2016) 35:226–37. doi: 10.1080/10550887.2016.1171670
119. Mellinger, JL, Scott Winder, G, DeJonckheere, M, Fontana, RJ, Volk, ML, Lok, ASF, et al. Misconceptions, preferences and barriers to alcohol use disorder treatment in alcohol-related cirrhosis [research support, non-U.S. Gov't]. J Subst Abus Treat. (2018) 91:20–7. doi: 10.1016/j.jsat.2018.05.003
120. Thomas, B, Suhadev, M, Mani, J, Ganapathy, BG, Armugam, A, Faizunnisha, F, et al. Feasibility of an alcohol intervention programme for TB patients with alcohol use disorder (AUD)--a qualitative study from Chennai [research support, non-U.S. Gov't research support, U.S. Gov't, non-P.H.S.]. South India PLoS One. (2011) 6:e27752. doi: 10.1371/journal.pone.0027752
121. Khadjesari, Z, Newbury-Birch, D, Murray, E, Shenker, D, Marston, L, and Kaner, E. Online health check for reducing alcohol intake among employees: a feasibility study in six workplaces across England [research support, non-U.S. Gov't]. PLoS One. (2015) 10:e0121174. doi: 10.1371/journal.pone.0121174
122. Lewis, MA, Cadigan, JM, Cronce, JM, Kilmer, JR, Suffoletto, B, Walter, T, et al. Developing text messages to reduce community college student alcohol use. Am J Health Behav. (2018) 42:70–9. doi: 10.5993/AJHB.42.4.7
123. Chokron Garneau, H, Venegas, A, Rawson, R, Ray, LA, and Glasner, S. Barriers to initiation of extended release naltrexone among HIV-infected adults with alcohol use disorders [research support, N.I.H., extramural]. J Subst Abus Treat. (2018) 85:34–7. doi: 10.1016/j.jsat.2017.05.004
124. Collins, SE, Duncan, MH, Smart, BF, Saxon, AJ, Malone, DK, Jackson, TR, et al. Extended-release naltrexone and harm reduction counseling for chronically homeless people with alcohol dependence [research support, N.I.H., extramural research support, non-U.S. Gov't]. Subst Abus. (2015) 36:21–33. doi: 10.1080/08897077.2014.904838
125. Gibbs, DA, and Rae Olmsted, KL. Preliminary examination of the confidential alcohol treatment and education program [empirical study; interview; focus group; qualitative study]. Mil Psychol. (2011) 23:97–111. doi: 10.1080/08995605.2011.534418
126. Stoutenberg, M, Warne, J, Vidot, D, Jimenez, E, and Read, JP. Attitudes and preferences towards exercise training in individuals with alcohol use disorders in a residential treatment setting. J Subst Abus Treat. (2015) 49:43–9. doi: 10.1016/j.jsat.2014.08.008
127. Wongtongkam, N, Lampoo, S, Choocherd, P, and Chiangkuntod, S. Partial efficacy of Vipassana mindfulness approach in alcohol-dependent persons [empirical study; Followup study; interview; focus group; qualitative study; quantitative study]. Alcohol Treat Q. (2018) 36:3–14. doi: 10.1080/07347324.2017.1355224
128. Gaume, J, Grazioli, VS, Paroz, S, Fortini, C, Bertholet, N, and Daeppen, J-B. Developing a brief motivational intervention for young adults admitted with alcohol intoxication in the emergency department-results from an iterative qualitative design [clinical trial; empirical study; interview; qualitative study]. PLoS One. (2021) 16:16. doi: 10.1371/journal.pone.0246652
129. Grazioli, VS, Collins, SE, Daeppen, JB, and Larimer, ME. Perceptions of twelve-step mutual-help groups and their associations with motivation, treatment attendance and alcohol outcomes among chronically homeless individuals with alcohol problems [research support, non-U.S. Gov't]. Int J Drug Policy. (2015) 26:468–74. doi: 10.1016/j.drugpo.2014.10.009
130. Groves, P, Pick, S, Davis, P, Cloudesley, R, Cooke, R, Forsythe, M, et al. Routine alcohol screening and brief interventions in general hospital in-patient wards: acceptability and barriers [empirical study; qualitative study]. Drugs Educ Prevent Policy. (2010) 17:55–71. doi: 10.3109/09687630802088208
131. Lee, KS, Harrison, K, Mills, K, and Conigrave, KM. Needs of aboriginal Australian women with comorbid mental and alcohol and other drug use disorders [research support, non-U.S. Gov't]. Drug Alcohol Rev. (2014) 33:473–81. doi: 10.1111/dar.12127
132. McCombe, G, Henihan, AM, Klimas, J, Swan, D, Leahy, D, Anderson, R, et al. Enhancing alcohol screening and brief intervention among people receiving opioid agonist treatment: qualitative study in primary care. Drugs Alcohol Today. (2016) 16:247–58. doi: 10.1108/DAT-03-2016-0010
133. Myers, B, Joska, JA, Lund, C, Levitt, NS, Butler, CC, Naledi, T, et al. Patient preferences for the integration of mental health counseling and chronic disease care in South Africa. Patient Prefer Adherence. (2018) 12:1797–03. doi: 10.2147/PPA.S176356
134. Myers, B, Parry, CDH, Morojele, NK, Nkosi, S, Shuper, PA, Kekwaletswe, CT, et al. "Moving forward with life": acceptability of a brief alcohol reduction intervention for people receiving antiretroviral therapy in South Africa [research support, non-U.S. Gov't]. Int J Environ Res Public Health. (2020) 17:7. doi: 10.3390/ijerph17165706
135. Ornelas, IJ, Allen, C, Vaughan, C, Williams, EC, and Negi, N. Vida PURA: a cultural adaptation of screening and brief intervention to reduce unhealthy drinking among Latino Day laborers [research support, N.I.H., extramural research support, non-U.S. Gov't research support, U.S. Gov't, non-P.H.S.]. Subst Abus. (2015) 36:264–71. doi: 10.1080/08897077.2014.955900
136. Parkman, T, Neale, J, Day, E, and Drummond, C. How do people who frequently attend emergency departments for alcohol-related reasons use, view, and experience specialist addiction services? Subst Use Misuse. (2017) 52:1460–8. doi: 10.1080/10826084.2017.1285314
137. Randall-James, J, Wadd, S, Edwards, K, and Thake, A. Alcohol screening in people with cognitive impairment: an exploratory study [research support, non-U.S. Gov't]. J Dual Diagn. (2015) 11:65–74. doi: 10.1080/15504263.2014.992095
138. Snowden, C, Lynch, E, Avery, L, Haighton, C, Howel, D, Mamasoula, V, et al. Preoperative behavioural intervention to reduce drinking before elective orthopaedic surgery: the PRE-OP BIRDS feasibility RCT [multicenter study randomized controlled trial research support, non-U.S. Gov't]. Health Technol Assess. (2020) 24:1–176. doi: 10.3310/hta24120
139. Woolf-King, SE, Sheinfil, AZ, Babowich, JD, Siedle-Khan, B, Loitsch, A, and Maisto, SA. Acceptance and commitment therapy (ACT) for HIV-infected hazardous drinkers: a qualitative study of acceptability. Alcohol Treat Q. (2019) 37:342–58. doi: 10.1080/07347324.2018.1539630
140. Osilla, KC, Kulesza, M, and Miranda, J. Bringing alcohol treatment to driving under the influence programs: perceptions from first-time offenders. Alcohol. (2017) 35:113–29. doi: 10.1080/07347324.2017.1288484
141. Sorsdahl, K, Morojele, NK, Parry, CD, Kekwaletswe, CT, Kitleli, N, Malan, M, et al. 'What will it take': addressing alcohol use among people living with HIV in South Africa. Int J STD AIDS. (2019) 30:1049–54. doi: 10.1177/0956462419862899
142. Mullen, J, Ryan, SR, Mathias, CW, and Dougherty, DM. Feasibility of a computer-assisted alcohol screening, brief intervention and referral to treatment program for DWI offenders [research support, N.I.H., extramural research support, non-U.S. Gov't]. Addict Sci Clin Pract. (2015) 10:25. doi: 10.1186/s13722-015-0046-1
143. Murphy, MK, Bijur, PE, Rosenbloom, D, Bernstein, SL, and Gallagher, EJ. Feasibility of a computer-assisted alcohol SBIRT program in an urban emergency department: patient and research staff perspectives [research support, non-U.S. Gov't]. Addict Sci Clin Pract. (2013) 8:2. doi: 10.1186/1940-0640-8-2
144. Sanders, JM. Acknowledging gender in women-only meetings of alcoholics anonymous [empirical study; qualitative study]. J Groups Addict Recover. (2010) 5:17–33. doi: 10.1080/15560350903543766
145. Schonbrun, YC, Anderson, BJ, Johnson, JE, Kurth, M, Timko, C, and Stein, MD. Barriers to entry into 12-step mutual help groups among justice-involved women with alcohol use disorders. Alcohol Treat Q. (2019) 37:25–42. doi: 10.1080/07347324.2018.1424596
146. Vaca, F, Winn, D, Anderson, C, Kim, D, and Arcila, M. Feasibility of emergency department bilingual computerized alcohol screening, brief intervention, and referral to treatment [research support, non-U.S. Gov't]. Subst Abus. (2010) 31:264–9. doi: 10.1080/08897077.2010.514245
147. Clifford, A, and Shakeshaft, A. Evidence-based alcohol screening and brief intervention in aboriginal community controlled health services: experiences of health-care providers [research support, non-U.S. Gov't]. Drug Alcohol Rev. (2011) 30:55–62. doi: 10.1111/j.1465-3362.2010.00192.x
148. Johnson, JE, Schonbrun, YC, and Stein, MD. Pilot test of 12-step linkage for alcohol-abusing women in leaving jail [empirical study; quantitative study]. Subst Abus. (2014) 35:7–11. doi: 10.1080/08897077.2013.794760
149. Klingemann, H, and Gomez, V. Masculinity issues in addiction treatment in Swiss inpatient alcohol programs: bringing men's treatment needs back to the research agenda. J Men's Health. (2010) 7:211–20. doi: 10.1016/j.jomh.2010.04.003
150. Mulvihill, DG. (2010) Help-seeking for alcohol dependency by women with post-traumatic stress disorder and a history of intimate partner violence [PhD dissertation]. [London, ON]: University of Western Ontario
151. Lee, AW. Review of mixed treatment comparisons in published systematic reviews shows marked increase since 2009. J Clin Epidemiol. (2014) 67:138–43. doi: 10.1016/j.jclinepi.2013.07.014
152. Castillo-Carniglia, A, Keyes, KM, Hasin, DS, and Cerda, M. Psychiatric comorbidities in alcohol use disorder. Lancet Psychiatry. (2019) 6:1068–80. doi: 10.1016/S2215-0366(19)30222-6
153. Babaei, N, Zamanzadeh, V, Valizadeh, L, Lotfi, M, Samad-Soltani, T, Kousha, A, et al. A scoping review of virtual care in the health system: infrastructures, barriers, and facilitators. Home Health Care Serv Q. (2023) 42:69–97. doi: 10.1080/01621424.2023.2166888
154. Barnett, ER, Knight, E, Herman, RJ, Amarakaran, K, and Jankowski, MK. Difficult binds: a systematic review of facilitators and barriers to treatment among mothers with substance use disorders. J Subst Abus Treat. (2021) 126:108341. doi: 10.1016/j.jsat.2021.108341
155. Cernasev, A, Hohmeier, KC, Frederick, K, Jasmin, H, and Gatwood, J. A systematic literature review of patient perspectives of barriers and facilitators to access, adherence, stigma, and persistence to treatment for substance use disorder. Explor Res Clin Soc Pharm. (2021) 2:100029. doi: 10.1016/j.rcsop.2021.100029
156. Choi, S, Rosenbloom, D, Stein, MD, Raifman, J, and Clark, JA. Differential gateways, facilitators, and barriers to substance use disorder treatment for pregnant women and mothers: a scoping systematic review. J Addict Med. (2022) 16:e185–96. doi: 10.1097/ADM.0000000000000909
157. Godier-McBard, LR, Wood, A, Kohomange, M, Cable, G, and Fossey, M. Barriers and facilitators to mental healthcare for women veterans: a scoping review. J Ment Health. (2022) 32:951–61. doi: 10.1080/09638237.2022.2118686
158. Sarkar, S, Tom, A, and Mandal, P. Barriers and facilitators to substance use disorder treatment in low-and middle-income countries: a qualitative review synthesis. Subst Use Misuse. (2021) 56:1062–73. doi: 10.1080/10826084.2021.1908359
159. Johnstone, S, Dela Cruz, GA, Kalb, N, Tyagi, SV, Potenza, MN, George, TP, et al. A systematic review of gender-responsive and integrated substance use disorder treatment programs for women with co-occurring disorders. Am J Drug Alcohol Abuse. (2023) 49:21–42. doi: 10.1080/00952990.2022.2130348
160. Paquette, CE, Daughters, SB, and Witkiewitz, K. Expanding the continuum of substance use disorder treatment: nonabstinence approaches. Clin Psychol Rev. (2022) 91:102110. doi: 10.1016/j.cpr.2021.102110
161. Balhara, YPS, Singh, S, and Narang, P. Effect of lockdown following COVID-19 pandemic on alcohol use and help-seeking behavior: observations and insights from a sample of alcohol use disorder patients under treatment from a tertiary care center. Psychiatry Clin Neurosci. (2020) 74:440–1. doi: 10.1111/pcn.13075
162. Creswell, JW, and Plano Clark, VL. Designing and conducting mixed methods research. 2nd ed. Washington, DC: SAGE Publications Inc. (2011). 457 p.
Keywords: problematic alcohol use, alcohol use disorder, addiction medicine, scoping review, barriers, treatment, review, knowledge synthesis
Citation: Wolfe DM, Hutton B, Corace K, Chaiyakunapruk N, Ngorsuraches S, Nochaiwong S, Presseau J, Grant A, Dowson M, Palumbo A, Suschinsky K, Skidmore B, Bartram M, Garner G, DiGioacchino L, Pump A, Peters B, Konefal S, Eves AP and Thavorn K (2023) Service-level barriers to and facilitators of accessibility to treatment for problematic alcohol use: a scoping review. Front. Public Health. 11:1296239. doi: 10.3389/fpubh.2023.1296239
Edited by:
Julia Dickson-Gomez, Medical College of Wisconsin, United StatesReviewed by:
Jannie Hugo, University of Pretoria, South AfricaKarina Conde, CONICET Institute of Basic, Applied and Technology Psychology (IPSIBAT), Argentina
Copyright © 2023 Wolfe, Hutton, Corace, Chaiyakunapruk, Ngorsuraches, Nochaiwong, Presseau, Grant, Dowson, Palumbo, Suschinsky, Skidmore, Bartram, Garner, DiGioacchino, Pump, Peters, Konefal, Eves and Thavorn. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Brian Hutton, Ymh1dHRvbkBvaHJpLmNh
 Dianna M. Wolfe1
Dianna M. Wolfe1 Brian Hutton
Brian Hutton Nathorn Chaiyakunapruk
Nathorn Chaiyakunapruk Surapon Nochaiwong
Surapon Nochaiwong Kednapa Thavorn
Kednapa Thavorn