
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health , 19 February 2024
Sec. Public Mental Health
Volume 11 - 2023 | https://doi.org/10.3389/fpubh.2023.1295627
This article is part of the Research Topic Neurological and Neuropsychiatric Disorders Affecting Military Personnel and Veterans View all 17 articles
 Nicholas A. Rattray1,2,3*
Nicholas A. Rattray1,2,3* Mindy Flanagan1
Mindy Flanagan1 Allison Mann1,4
Allison Mann1,4 Leah Danson1,4
Leah Danson1,4 Ai-Nghia Do1
Ai-Nghia Do1 Diana Natividad1
Diana Natividad1 Katrina Spontak1,4
Katrina Spontak1,4 Gala True5,6
Gala True5,6Background: People who support Veterans as they transition from their military service into civilian life may be at an increased risk of psychological distress. Existing studies focus primarily on paid family caregivers, but few studies include spouses and informal non-family “care partners.” We sought to identify key challenges faced by care partners of Veterans with invisible injuries.
Methods: Semi-structured interviews were conducted with 36 individuals involved in supporting a recently separated US military Veteran enrolled in a 2-year longitudinal study. CPs completed validated measures on perceived stress, caregiving burden, quality of their relationship, life satisfaction, and flourishing. Independent t-tests were used to compare cases in these groups on caregiving burden, quality of their relationship, life satisfaction, and flourishing. Care partners were categorized as reporting high and low levels of stress. Exemplar cases were used to demonstrate divergences in the experiences of CPs with different levels of stress over time.
Results: Care partners reported shifts in self-perception that occurred from supporting a Veteran, emphasizing how they helped Veterans navigate health systems and the processes of disclosing health and personal information in civilian contexts. Exemplar cases with high and low burdens demonstrated divergent experiences in self-perception, managing multi-faceted strain, and coping with stress over time. Case studies of specific care partners illustrate how multi-faceted strain shifted over time and is affected by additional burdens from childcare, financial responsibilities, or lack of education on mental health issues.
Conclusions: Findings suggest the unique needs of individuals who support military Veterans with invisible injuries, highlighting variations and diachronic elements of caregiving. This sample is younger than the typical caregiver sample with implications for how best to support unpaid care partners caring for Veterans in the early to mid-period of their use of VA and civilian health services.
Since 2001, there has been increased focus on the “invisible wounds of war,” which refers to mental health issues and cognitive impairments resulting from military service in the twenty-first century (1). Longer deployments as well as advances in combat medicine (2), have led a significant proportion of returning soldiers to report high levels of psychological and physical distress (3), and difficulties in reintegrating into civilian society (4–6). Compared to past eras, there is greater emphasis on diagnosing Post Traumatic Stress Disorder (PTSD), traumatic brain injuries, and depressive symptoms in post-9/11 Veterans. However, the effects of these conditions are still poorly understood compared to injuries categorized as physical wounds. The medical costs for invisible conditions alone are ~$2–3 billion per year (7), and families bear a significant “private burden” of uncompensated costs related to service-connected disabilities (8).
The effects of caregiving by family members are well-established in medical literature but are largely based on geriatric populations (9). Caregivers for military and Veteran populations are more likely to be younger, have dependents, and face longer periods of care for individuals with higher disability burdens (10). For Veterans enrolled in health care with the US Department of Veterans Affairs (VA), studies have suggested that caregivers who support Veterans have higher depression and burden compared to civilian counterparts and more financial strain over time (11). This mirrors wider findings that caregiving can lead to negative impacts on the health, wellbeing, economic security, and careers of family caregivers (12–14).
Within the literature on people who are caregivers for Veterans, studies tend to focus on caregivers for military servicemembers (15, 16), enrollees in the paid VA caregiver program (17), or caregivers who support patients with a specific diagnostic condition (e.g., cancer, diabetes, etc.). Abraham et al. have demonstrated less visible forms of “emotional work” of Veteran caregivers (18), while others have examined how caregivers enrolled in VA support programs perceive their uncompensated work (19). In the wake of the two million US troops that were deployed to Iraq and Afghanistan, researchers called for more treatments focused on Veterans and their whole support system. These include family-centered interventions that account for caregiver burden and deal with psychological distress experienced by Veterans and their families (20), with greater attention paid to the early period of post-deployment adjustment (21) and the effects on spouses and children (22).
Caregivers of Veterans, specifically Veterans with invisible injuries, have unique sets of needs (23). Due to the complex nature of invisible injuries, these Veterans' care requires increased effort from caregivers (22) and associated burden (24). Previous research revealed that family and social resources available for caregivers of Veterans aid in mitigating their overall psychological distress (25). Studies have demonstrated the unique consequences of PTSD on family functioning, such as emotional numbing and withdrawal (26), how spouses are often responsible for maintaining normalcy (27), and lower levels of life satisfaction (28). Many Veteran caregivers' needs, such as emotional support, understanding Veterans' benefits, locating Veteran services, and more, go unfulfilled (16).
Research partnerships in recent years have been developed to establish a clear research agenda for US military and Veteran caregivers based on existing studies from RAND and efforts from the Elizabeth Dole Foundation (29). Extant studies tend to focus on paid caregivers in the VHA Program of Comprehensive Assistance for Family Caregivers (PCAFC), leaving gaps in knowledge about unpaid caregivers and Veterans who are not enrolled in VHA health care.
Direct engagement with military and Veteran caregivers has contributed to the development of the “Military and Veteran Caregiver Experience Map,” a conceptual model designating stages in caregivers' “journeys” (30). More recent research has focused on suicidal ideation among military caregivers (31) and on evaluating existing programs, such as a study showing that a VA caregiver program was effective in reducing anxiety, depression, caregiver burden, and overall stress (32).
In this study, we adopted the term “care partner,” (CP) which aligns with recent calls for an inclusive approach to caregiving that recognizes the wide range of activities and roles individuals may perform in support of those they care for (33, 34). In addition to spouses, this term enabled us to recruit friends, siblings, parents, or others who might be nominated by Veteran study participants. Although CPs play a significant role in the reintegration processes of post-9/11 Veterans with invisible injuries, less is known about how they subjectively view the burden and stress of caregiving, as well as how it impacts their wellbeing. More specifically, we build on an existing conceptual definition of burden (35) to incorporate the distinct perspectives of CPs for military Veterans. This conceptualization of caregiver burden incorporates the following three attributes: self-perception (perceived negative and positive feelings or aspects related to the caregiving role), multifaceted strain (multiple types of strain associated with caregiving, such as health problems, psychological stress, social isolation, or financial problems), and time (change in caregiving burden over time). Incorporating temporality from repeated interviews and analysis of personal history aligns with a life course perspective attentive to continuity and provides context to change in caregivers' experiences (36, 37) and shifts common in Veterans' lives (38). We adopt a mixed methods approach to understand why some caregivers report greater strain and burden and how their narratives diverge.
This study examines the role that informal CPs play in the lives of military Veterans with invisible injuries (mental or cognitive health conditions) in the early phase of their adjustment to civilian life. We do so by using a mixture of quantitative and qualitative methods to offer a more comprehensive view of caregiving and discover potential ways to assist Veteran CPs. The specific aims are to (1) examine associations between CP characteristics and outcomes (flourishing, stress, burden); (2) to describe CP perspectives on how they support the Veteran in their life; and (3) through mixed method analysis, to understand patterns of convergence or divergence between CPs reporting high and low levels of burden.
We adopted a mixed methods approach to offer breadth and depth of understanding beyond what qualitative or quantitative methods would allow alone (39). Specifically, our mixed method design was an explanatory unidirectional approach (40) where questionnaire data merged with qualitative findings from thematic analysis and in-depth case study analysis. Interview data was reported using a qualitative descriptive design with narratives (41). The study was approved by the Indiana University Institutional Review Board and VA Research and Development Committee.
This study included a sample of CPs participating in a 2-year longitudinal study that examined community reintegration among military Veterans with an invisible injury (42), which includes clinical diagnosis of post-traumatic stress disorder, depression, anxiety, traumatic brain injury, or other mental or cognitive health condition and their care partners. As reported elsewhere, 91% of these Veteran participants had a disability rating (43). A CP is defined by the Veteran as someone who supports him/her in an area considered important to reintegration (family/social life, school, work, rehabilitation, etc.), typically a family member, partner, friend, or neighbor (33). Following the baseline visit, Veterans were encouraged to nominate an individual who currently supports their adjustment to civilian life. Nominated individuals were contacted via phone to describe the study and inquire about their interest in study participation. Of the 75 Veterans, 48 nominated a CP, which led to a convenience sample of 36 CPs enrolled in the study.
Before collecting any data, a member of the research team discussed the study aims with CPs and obtained consent and HIPAA authorization. Data collection included a mix of quantitative and qualitative data. The qualitative data collection involved semi-structured open-ended interviews. CPs received a $25 gift card for each assessment. The quantitative data collection included demographic information and self-administered close-ended questionnaires.
Following a semi-structured interview guide, CPs were asked about their role in supporting the Veterans and how the Veteran's reintegration impacts their own health and wellbeing. Specific topics that were covered included the CP's role in the Veteran's transition experience, family or social issues, financial/economic issues, and their perceptions on the overall reintegration experience. CPs were interviewed at baseline, 12 months, and 24 months and each interview lasted 60–90 min. Interviews were conducted individually and were either face-to-face in a private room or virtually by phone or videoconferencing, depending upon participant preference and in accordance with protocols adopted during the COVID-19 pandemic period. The digitally recorded interviews were transcribed verbatim, checked for accuracy by listening to the tapes and comparing them with the transcripts, and de-identified.
The Zarit Burden Interview (ZBI) assesses the perceived burden of caregiving (i.e., the extent to which caregiving causes stress, and interferes with the caregiver's health and other relationships or responsibilities). This 12-item questionnaire includes a 5-point Likert scale (0 = Never, 4 = Nearly always). Summed scores range from 0 to 48, such that a higher perceived burden is indicated by higher scores (44). The cutoff between low and high burden has been reported as 12 (45), 13 (46), and 19 (47). A high burden was defined as 13 points and higher for this study. Studies have suggested that the caregiving burden is multi-dimensional, including role strain (how caregiving conflicts with other roles) and personal strain (individualized stress) (48, 49).
The Perceived Stress Scale (PSS) is a 10-item measure that assesses stress on a 0 (Never) to 4 (Very Often) scale (50). Items include “In the last month, how often have you felt that you were unable to control the important things in your life?” and “In the last month, how often have you felt difficulties were piling up so high that you could not overcome them?” Scores range from 0 to 40 where normative scores are 12.1 (SD = 5.9) for men and 13.7 (SD = 6.6) for women. For this study, high stress was operationalized as a score of 14 or higher.
The “Flourishing measure” includes six domains that contribute to sustained wellbeing (51) and has been validated in a cross-cultural study (52). The Flourishing measure includes the following six domains: happiness, health (mental and physical), meaning and purpose, character, social relationships, and financial stability, an enabler to the other five domains. The response set ranges from 1 (Strongly disagree) to 7 (Strongly agree). The Secure Flourishing Index (SFI) is an average of all 12 items, where higher scores indicate higher levels of flourishing.
The Satisfaction with Life Scale (SWLS) assesses an individual's quality of life as they experience and evaluate it. When completing the SWLS, respondents indicate the extent to which they agree or disagree with five items (1 = Extremely dissatisfied, 7 = Highly satisfied) (53). The SWLS has good validity and temporal stability (54). Scores are summed for the five items. Extreme dissatisfaction is operationalized as a score in the 5–9 range, neutral satisfaction is a score of 20, and extreme satisfaction is a score in the 31–35 range.
The Quality of Relationship Scale assesses the CP's relationship with the Veteran, which is adapted from the mutual communal relationship scale (55–57). This scale has 10 items with responses that range from 1 (Never) to 4 (Always), with five questions focused on the giving aspect and five questions on the receiving aspects of the relationship (58).
A list of 14 resources available to CPs was included to determine the extent to which CPs access these resources. Based on previous studies (59), this list of resources included informal sources of information, religious networks, health care, mental health care, wellness activities, financial support, case management, and support groups. Respondents indicated whether they had used the resource and the extent to which it was helpful (1 = “Not at all,” 2 = “Somewhat,” 3 = “Very”).
The overall mixed methods approach is described in Figure 1. First, a qualitative thematic analysis combined with matrix analysis (60) was undertaken to develop cross-cutting patterns from interviews with CPs. Three coders independently read interview transcripts in “open coding,” where each analyst inductively identified relevant excerpts with a provisional label (61). Analytic memos were written regularly during open coding to connect emergent content related to community reintegration. Case summaries were compared using a data matrix to further identify themes and achieve data saturation. A codebook was developed and refined until a shared understanding was achieved. Next, at least two team members independently coded each transcript; pairs met in person to review the double-coded transcripts and resolve discrepancies through consensus. Qualitative data was coded and analyzed using NVivo (62). Subsequently, themes were aligned with concepts from the caregiver burden model (i.e., self-perception, multi-faceted strain, disclosure, navigation, resources, needs, and strategies).
Consistent with the study aims, cases were sorted using baseline ZBI scores. Cases were categorized into high burden (ZBI score ≥ 13, 10/34, 29.4%) and low burden (ZBI score <13, 24/34, 70.6%) groups for focused analysis of interview transcripts according to their baseline burden score. Combining 12-month scores for burden with baseline burden scores, cases were categorized as staying high (4/27, 14.8%), low (17/27, 63.0%), shifting from high to low burden (4/27, 14.8%), or low to high burden (2/27, 7.4%). Seven CPs did not complete surveys at 12 months.
For the quantitative measures, descriptive statistics (e.g., mean, frequencies) were calculated to characterize the sample in terms of demographic variables and psychosocial outcomes. To examine associations between CP characteristics and outcomes, Pearson correlations were calculated among PSS, SFI, SWLS, Zarit Burden, and Quality of Relationship Scale scores. Additionally, to compare CPs reporting high burden with those reporting low burden, independent t-tests were used to compare these groups on PSS, SFI, SWLS, and Quality of Relationship Scale scores. To account for multiple comparisons increasing the possibility of a Type I error, a False Discovery rate adjustment was made (63).
In the next stage of analysis, baseline ZBI scores were used to categorize cases into high-burden (ZBI score ≥ 13, 10/34, 29.4%) and low-burden (ZBI score <13, 24/34, 70.6%) groups. Combining 12-month scores for burden with baseline burden scores, cases were categorized as staying high (4/27, 14.8%), low (17/27, 63.0%), shifting from high to low burden (4/27, 14.8%), or low to high burden (2/27, 7.4%). Seven CPs did not complete surveys at 12 months. In the last phase of analysis, we selected exemplar cases that illustrated cross-cutting findings and changes in burden over time.
Of the 36 CPs, a majority were women (72.2%) and married or partners (72.2%) to the Veteran for whom they provided care (see Table 1). Consequently, most CPs lived with the Veteran (63.9%) and, on average, had known the Veteran for a considerable length of time, mean = 15.1 years (SD = 10.0, range = 0.8, 34). Only 11.1% of CPs had been caregiving for the Veteran for less than a year, while 52.8% had been a caregiver for more than 5 years. Also, 58.3% of CPs were parents or guardians to a child under the age of 18 years. Over a third (36.%) reported military service. One respondent reported participation as a paid caregiver in the VHA PCAFC.
As expected, burden was significantly positively correlated to perceived stress (r = 0.50, p = 0.003). Additionally, burden was significantly inversely related to secure flourishing (r = −0.60, p < 0.001) and relationship quality (r = −0.45, p = 0.008). Though an inverse trend between burden and life satisfaction was observed, this correlation was non-significant (r = −0.26, p = 0.14).
Descriptive statistics are shown in Table 2 for survey measures completed by CPs. As expected, CPs with high burden had significantly higher stress (p = 0.02), lower secure flourishing (p = 0.02), and marginally significantly lower life satisfaction (p = 0.08) and relationship quality (p = 0.06).
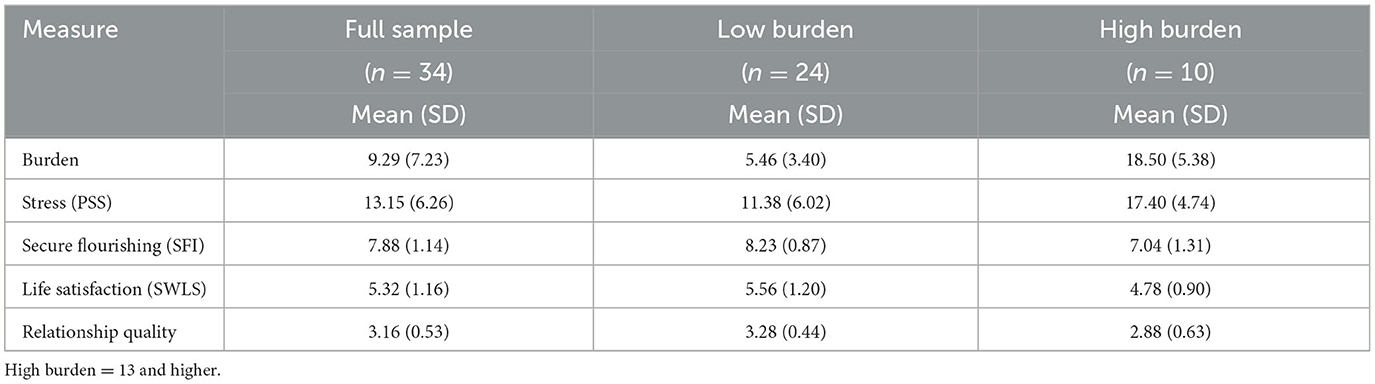
Table 2. Descriptive statistics of baseline survey measures assessed in the care partner sample by burden level.
As shown in Table 3, CPs did not access many of the resources available. The most frequently accessed resources were a religious or spiritual network and informal information sources, such as websites and articles. In contrast, formal, structured programs and resources, such as loans, support groups, case managers, caregiving training, and stipends, were rarely accessed.
Based on the themes and case descriptions that follow, Figure 2 depicts how burden was conceptualized in this study. The diagram retains the dynamic relationship between self-perception, multi-faceted strain, and change over time but adds factors that increase or decrease the burdens that are specific to CPs to Veterans.
CPs expressed a wide range of feelings and perceptions associated with their caregiving role. Negative emotions named included stress, anger, overwhelmed, frustrated, tired, or drained. For example, P4032 stated, “I feel like I run around like a chicken with my head cut off. So as a spouse, I feel like it's very overwhelming;” P4004 explained, “So yeah, I get stressed out. Do I know everything about what to do about everything all of the time? Absolutely not.”
However, CPs described their own qualities that were helpful in managing their caregiver role. These qualities included being adaptable, understanding the military experience, accepting their situation, being solution-focused, staying calm, and being a positive, caring person. As an example of adaptability being an asset, P4021 described, “I'm used to being flexible… it was always important to me for my husband to be happy with whatever job he's working for after the military, so if that meant we need to move a certain city, that's okay. I work in healthcare, so it's not as hard for me to find jobs.” Similarly, another CP relied on her acceptance and adaptability for managing the caregiver role. P4017 stated, “It's not a pity thing… When you sign on and you know that this is a lifestyle, you are choosing, and the choice was made that our marriage and we know that like his Marine Corps job is what's going to drive. And we were in that together. So but as a result, that means that I am not going to have a career… There is a lot of fluidity, and you have to be willing to just go with the flow and let his stuff drive it and not yours, if that makes sense.” P4006 described herself as a “fixer” meaning she will “try to figure out well, how can we fix this? Well, how can we make it better?” She viewed this as a strength in her role as a caregiver. Similarly, P4038 described herself as “a person that loves to take care of people” and “the bubbly, cheery, happy-go-lucky person. Day in and day out, will find the positive in everything.”
As noted by Liu et al. (30), CPs manage caregiving responsibilities alongside their other social roles. CPs reported that they helped their Veteran with daily medications, medical appointments, physical safety (i.e., falling), emotional support, and meals. One CP described monitoring her husband's mood and providing support when he appeared to need it. P4006 stated, “So at this point, that's what I really feel like that my role is really just to make sure that he has a loving support at home and that he knows that he's accepted no matter what and… recognize that oh okay, something is a little off… Either he's not communicating, or he seems a little withdrawn and then just trying to gently talk to him about are you just tired.” Similarly, when asked “Are you like worried about him?” P4012 responded, “It's kind, it's almost like a motherly worried. Because I can tell that he's anxious and that he's feeling that anxiety.” P4011 described her caregiving stress in the following way: “It can be a very, very tiring struggle sometimes to help everybody and make sure that he is still okay and still on the schedule that he needs or making it to the appointment or remembering to eat.” In addition to monitoring emotional changes, CPs reported that Veterans had angry outbursts that were hard to manage. P4020 explained: “I'm trying to keep him calm. You know… It's upsetting because he'll get angry and be upset more, which can cause the kids to get upset. Yeah, it's stressful.” Some of these CPs primarily managed household finances, daily household decisions, and household moves, or were the only driver in the household. For example, P4003 stated “So I take care of all of the financial stuff at our house.” Similarly, P4011 explained, “And I'm like the stick in the middle that controls everything (laughter). Yes. Very much so. I kind of rule everything, and I didn't like to take that spot, but I do pretty good at it (laughter).”
CPs played a crucial role in supporting help-seeking behavior, including encouraging Veterans to disclose information with appropriate timing and context. P4016 explained how her husband “was so closed off” that he did not respond to initial mental health outreach, but that her presence at therapy appointments was beneficial: “I was able to kind of explain certain situations… that he maybe he didn't even realize was happening.”
CPs describe how they helped Veterans navigate through challenges related to accessing health services, scheduling appointments, and paying for health services. One CP expressed how it “was easier to navigate with two brains than one” (P4013). This CP emphasized caring for his spouse: “No, it's not a burden. I'm not even stressed either, because of the way I deal with stress, which is another thing that she is mad about, how I'm different from her on that aspect.”
P4025, a CP with high self-reported stress, described in detail attempts to help:
“I'd come home and say so when's your appointment? Oh, I couldn't do that. And so I would be encouraging and say, okay, want me to call? No, I can do it. I'll do it tomorrow. And it took the initial phone call took 5 or 6 days and then the initial appointment, there was a lot of anxiety leading up to the appointment, and the day of the appointment, there's anxiety, and so it's, which the cultural stuff?”
This CP explained the importance of persistent monitoring coupled with empathy about the Veteran's anxiety about attending scheduled appointments. Other CPs discussed how they witnessed “getting the runaround” (P4011) when trying to access services; P4004 explained that it was necessary to reach out to the Patient Advocate for assistance.
In terms of resources that would aid CPs, respondents discussed a range of needs and strategies that they used. Several CPs suggested that focused courses or workshops delivered after military separation occurs would be beneficial with specific courses dedicated to CPs supporting Veterans. Topics that were suggested included communication skills, awareness of mental health issues, and support in navigating the VA healthcare system. P4020 suggested a coupled-focused course: “No, nobody ever contacted me and said this is what PTSD looks like—like I think that it should be mandatory for couples to go through classes before deployments and after deployments, and you know.” Other CPs expressed the need for consistency when it comes to health care services and courses to understand VA benefits, including disability and insurance from a CP perspective. P4002 proposed presentations about supporting a Veteran be held at local community centers to aid in caring efforts.
Table 3 summarizes which types of resources CPs found useful. The most accessed resources, structured wellness activities, informal information sources, and participation in spiritual or religious networks, were reported to be helpful.
The following offer exemplar cases that illustrate high and low burdens. To demonstrate within-case changes, we likewise offer cases that remained as either high or low burden or changed their burden-level at 12 months.
Among CPs reporting high levels of burden, P4019 was a spousal CP who himself served nearly three decades in the Navy and has a 70% service-connected disability. He left service prior to his wife, which was when they “reversed roles” and he was the primary caretaker of their children while she was deployed. He supported his wife primarily through cooking and cleaning but expressed how he wished he could provide more support for his wife but that they have communication issues. This CP scored higher for “role strain” than for “personal strain,” which converges with evidence from his interviews.
P4009 was also a Veteran who served in the Air Force for 6 years. Her husband struggled with mental health (depression, PTSD), which was a major stressor in their relationship. As a result, she felt “almost like a single parent,” caring for their four children while working as a mental health professional. This CP was categorized as having a high burden at baseline and at 12 months. She described stress from coping with the volatility of her spouse's mood, explaining how he “shuts off” and “self-isolates” from her and their children, leaving her feeling less hope for the future.
P4026 was a case where at baseline, the CP was struggling to support his girlfriend due to her own challenges with civilian reintegration, PTSD, and migraines. The CP was also a Veteran but had a smoother transition into higher education following his military service. The couple temporarily separated when the Veteran decided to move to a new state, but the CP changed his mind and moved in with her in her new residence. Though the CP had a high burden at baseline, at 12 months, the CP was categorized as low burden and had higher scores for flourishing.
Reporting low burden, P4004 was the sole CP who had been in the VA's “Program of Comprehensive Assistance for Family Caregivers” (PCAFC) for 5 years. This CP quit her job in oral hygiene to become a full-time caregiver to her husband, a Veteran who was medically discharged and had memory problems, several physical issues, and PTSD. P4004 navigates VHA health services, taking him to multiple weekly appointments, as well as managing medication and paperwork. Despite some lost earnings from her prior career, she reported low levels of stress and burden and a good quality of life.
P4020 had four children and had been married to the Veteran for 14 years. She had witnessed significant physical (back and shoulder pain) and mental health changes (increased anger and isolation) after his first combat deployment. Like P4004, P4020 assisted with her husband's medical care and engaged in couples counseling. P4020 remained a low-burden case at baseline and 12 months. Despite being the sole support for him outside of the mental health care team, she had a strong social network, including family, friends, and coworkers, and engages in self-care through meditation, traveling, and receiving massages.
In this study, we draw on self-reported caregiver burden in addition to interviews spaced 12 months apart to capture the experiences of CPs of US military Veterans. The objective was to use a mixed methods approach to categorize 36 CPs into discernible groups through a conceptual framework that posits three aspects of burden: multi-faceted strain, self-perception, and change over time. We demonstrated how CPs were categorized as high or low burden initially, but also how some cases shifted categories based on changing circumstances and factors exacerbating or diminishing personal strain. A life course perspective developed for military households can address the unique challenges of managing civilian-military cultural issues, the strain of emotional dysregulation among recently separated Veterans, and intertwined physical and mental health conditions (38, 64). These findings offer longitudinal evidence that supports the broader framework promoted by the Dole Foundation's caregiver journey map (30). In particular, our findings reinforce how the process of self-identifying as a caregiver can be a gradual process, followed by critical points where burden and wellbeing may fluctuate.
Drawing on an existing conceptual model for caregiver burden (35), we closely examine specific cases to identify antecedents and consequences of CP burden that are specific to providing support for military Veterans. Existing studies tend to focus on either the potentially positive aspects of caregiving or emphasize the emotional distress (65) but are less likely to describe financial strain or the opportunity costs of caregiving (66). This sample was notable for its relatively small use of available resources; a single CP was enrolled in a formal caregiver program, and CPs reported little training or preparation for support tasks. CPs in this study described how they supported Veterans who were dealing with emotional dysregulation. Likewise, CPs play an integral role in monitoring how their partners interact with civilians in stressful environments, often shielding them from potentially challenging spaces or repairing conversations where Veterans encountered communication problems with civilians.
In contrast to the preponderance of caregiving studies with older participants, these findings highlight the disruptions that occur for those in the early adult stage (ages 17–45), as they shift careers, manage childcare responsibilities, and transition from military service. CPs discussed balancing support for their partner alongside caring for children and pursuing their own career. Consistent with other studies (67), spousal caregivers reported a lack of confidence in their ability to support their partners and also described difficulties with intimacy. Male spouses in particular reported more issues with role strain—that is, feeling unsure or inadequate in their ability to support their spouse. Multi-faceted strain in the context of the challenges of early adulthood reinforces the importance of a life course perspective (31, 32).
Limitations of these findings should be noted. CPs were recruited based on being nominated by a participating Veteran, which likely limited the heterogeneity of the sample. Most participating Veterans were male, whereas 72% of CPs were female, and most had been caring for the Veterans for more than 5 years. More research is needed to better understand how findings might apply across different sociodemographic groups. The study included multiple data collection points which offered a window into how CPs changed over a 12-month period.
Few studies have examined how the experiences of unpaid caregivers support military Veterans with invisible injuries such as post-traumatic stress disorder and traumatic brain injuries. Findings suggest the unique needs of individuals who support military Veterans with invisible injuries, highlighting variations and diachronic elements of caregiving. Distinguishing between the experiences of CPs who report high and low burden offers insight into how unpaid caregivers are affected by childcare, financial responsibilities, or incomplete knowledge of appropriate mental health care.
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
The studies involving humans were approved by Indiana University IRB and Roudebush VA Medical Center. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
NR: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. MF: Conceptualization, Investigation, Resources, Visualization, Writing – original draft, Writing – review & editing, Project administration. AM: Data curation, Formal analysis, Visualization, Writing – original draft, Writing – review & editing. LD: Data curation, Writing – review & editing. A-ND: Writing – review & editing. DN: Writing – review & editing. KS: Writing – review & editing. GT: Funding acquisition, Conceptualization, Writing – review & editing.
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. Support was provided by a Career Development Award-2 (NR) from the US Department of Veterans Affairs, Rehabilitation Research and Development (D2642-W).
We acknowledge the contributions of Dr. Marina Kukla and Dr. Richard Frankel. We appreciate study support from Sean Baird and Dr. Michelle Salyers.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Tanielian TL, Jaycox L. Invisible Wounds of War: Psychological and Cognitive Injuries, Their Consequences, and Services to Assist Recovery. Santa Monica, CA: RAND (2008).
2. Ling GS, Rhee P, Ecklund JM. Surgical innovations arising from the Iraq and Afghanistan wars. Annu Rev Med. (2010) 61:457–68. doi: 10.1146/annurev.med.60.071207.140903
3. Spelman JF, Hunt SC, Seal KH, Burgo-Black AL. Post deployment care for returning combat veterans. J Gen Intern Med. (2012) 27:1200–9. doi: 10.1007/s11606-012-2061-1
4. Sayer NA, Carlson KF, Frazier PA. Reintegration challenges in US service members and veterans following combat deployment. Soc Iss Pol Rev. (2014) 8:33–73. doi: 10.1111/sipr.12001
5. Dillahunt-Aspillaga C, Powell-Cope G. Community reintegration, participation, and employment issues in veterans and service members with traumatic brain injury. Archiv Phys Med Rehabil. (2018) 99(2Suppl.):S1–S3. doi: 10.1016/j.apmr.2017.04.013
6. Smith RT, True G. Warring identities: identity conflict and the mental distress of American veterans of the wars in Iraq and Afghanistan. Soc Ment Health. (2014) 4:147–61. doi: 10.1177/2156869313512212
7. Geiling J, Rosen JM, Edwards RD. Medical costs of war in 2035: long-term care challenges for veterans of Iraq and Afghanistan. Mil Med. (2012) 177:1235–44. doi: 10.7205/MILMED-D-12-00031
8. Bilmes L. The Long-Term Costs of United States Care for Veterans of the Afghanistan and Iraq Wars. Providence, RI: Brown University-Watsons Institute for Institutional and Public Affairs (2021).
9. Tanielian T, Ramchand R, Fisher MP, Sims CS, Harris RS, Harrell MC. Military caregivers: cornerstones of support for our nation's wounded, ill, and injured veterans. Rand health Quart. (2013) 3:3. doi: 10.7249/RR244
10. Ramchand R, Tanielian T, Fisher MP, Vaughan CA, Trail TE, Epley C, et al. Hidden Heroes: America's Military Caregivers. Santa Monica, CA: Rand Corporation (2014).
11. Miller KEM, Lindquist JH, Olsen MK, Smith V, Voils CI, Oddone EZ, et al. Invisible partners in care: snapshot of well-being among caregivers receiving comprehensive support from Veterans Affairs. Health Sci Rep. (2019) 2:e112. doi: 10.1002/hsr2.112
12. George LK, Gwyther LP. Caregiver well-being: a multidimensional examination of family caregivers of demented adults. Gerontologist. (1986) 26:253–9. doi: 10.1093/geront/26.3.253
13. Raina P, O'Donnell M, Schwellnus H, Rosenbaum P, King G, Brehaut J, et al. Caregiving process and caregiver burden: conceptual models to guide research and practice. BMC Pediatr. (2004) 4:1. doi: 10.1186/1471-2431-4-1
14. Pinquart M, Sörensen S. Differences between caregivers and noncaregivers in psychological health and physical health: a meta-analysis. Psychol Aging. (2003) 18:250–67. doi: 10.1037/0882-7974.18.2.250
15. Stuttaford M. Unpaid public work is not cost free: military spouses performing emotional labor. Milit Behav Health. (2020) 8:139–47. doi: 10.1080/21635781.2020.1734511
16. Brickell TA, Lippa SM, French LM, Gartner RL, Driscoll AE, Wright MM, et al. Service needs and health outcomes among caregivers of service members and veterans following TBI. Rehabil Psychol. (2019) 64:72–86. doi: 10.1037/rep0000249
17. Smith VA, Lindquist J, Miller KEM, Shepherd-Banigan M, Olsen M, Campbell-Kotler M, et al. Comprehensive family caregiver support and caregiver well-being: preliminary evidence from a pre-post-survey study with a non-equivalent control group. Front Publ Health. (2019) 7:122. doi: 10.3389/fpubh.2019.00122
18. Abraham TH, Ono SS, Moriarty H, Winter L, Bender RE, Facundo R, et al. Revealing the invisible emotion work of caregivers: a photovoice exploration of informal care provided by family caregivers for post-9/11 veterans with traumatic brain injuries. J Head Trauma Rehabil. (2021) 36:25–33. doi: 10.1097/HTR.0000000000000589
19. Wyse JJ, Ono SS, Kabat M, True G. Supporting family caregivers of veterans: participant perceptions of a federally-mandated caregiver support program. Healthcare. (2020) 2020:100441. doi: 10.1016/j.hjdsi.2020.100441
20. Link PE, Palinkas LA. Long-term trajectories and service needs for military families. Clin Child Fam Psychol Rev. (2013) 16:376–93. doi: 10.1007/s10567-013-0145-z
21. Sayer N, Noorbaloochi S, Frazier P, Carlson K, Gravely A, Murdoch M. Reintegration problems and treatment interests among Iraq and Afghanistan combat veterans receiving VA medical care. Psychiat Serv. (2010) 61:589–97. doi: 10.1176/ps.2010.61.6.589
22. MacDermid SRDS. Military Deployment and Its Consequences for Families. New York, NY: Springer (2014).
23. Patel BR. Caregivers of veterans with “invisible” injuries: what we know and implications for social work practice. Soc Work. (2015) 60:9–17. doi: 10.1093/sw/swu043
24. Brickell TA, French LM, Lippa SM, Lange RT. Burden among caregivers of service members and veterans following traumatic brain injury. Brain Injury. (2018) 32:1541–8. doi: 10.1080/02699052.2018.1503328
25. Griffin JM, Lee MK, Bangerter LR, Van Houtven CH, Friedemann-Sánchez G, Phelan SM, et al. Burden and mental health among caregivers of veterans with traumatic brain injury/polytrauma. Am J Orthopsychiatry. (2017) 87:139. doi: 10.1037/ort0000207
26. Ray SL, Vanstone M. The impact of PTSD on veterans' family relationships: an interpretative phenomenological inquiry. Int J Nurs Stud. (2009) 46:838–47. doi: 10.1016/j.ijnurstu.2009.01.002
27. Yambo TW, Johnson ME, Delaney KR, Hamilton R, Miller AM, York JA. Experiences of military spouses of veterans with combat-related posttraumatic stress disorder. J Nurs Scholarsh. (2016) 48:543–51. doi: 10.1111/jnu.12237
28. Vogt D, Smith BN, Fox AB, Amoroso T, Taverna E, Schnurr PP. Consequences of PTSD for the work and family quality of life of female and male US Afghanistan and Iraq War veterans. Soc Psychiatr Psychiatr Epidemiol. (2017) 52:341–52. doi: 10.1007/s00127-016-1321-5
29. Tanielian T, Bouskill KE, Ramchand R, Friedman EM, Trail TE, Clague A. Improving support for america's hidden heroes: a research blueprint. Rand Health Quart. (2018) 7:9. doi: 10.7249/RR1873
30. Military Veteran Caregiver Experience Map. (2021). Available online at: https://caregiverjourney.elizabethdolefoundation.org/wp-content/themes/caregiver-child/images/Caregiver-Journey-Map.pdf (accessed December 10, 2022).
31. Delgado RE, Peacock K, Wang CP, Pugh MJ. Phenotypes of caregiver distress in military and veteran caregivers: suicidal ideation associations. PLoS ONE. (2021) 16:e0253207. doi: 10.1371/journal.pone.0253207
32. Martindale-Adams JL, Zuber J, Graney MJ, Burns R, Nichols LO. Effect of a behavioral intervention on outcomes for caregivers of veterans with PTSD. Milit Behav Health. (2021) 9:357–67. doi: 10.1080/21635781.2021.1927916
33. Boucher NA, Shepherd-Banigan M, McKenna K, Delgado RE, Peacock K, Van Houtven CH, et al. Inclusion of caregivers in veterans' care: a critical literature review. Med Care Res Rev. (2020) 78:463–74. doi: 10.1177/1077558720944283
34. Manheim C, Haverhals L, Gilman C, Karuza J, Olsan T, Edwards S, et al. VA home based primary care teams: partnering with and acting as caregivers for veterans. Home Health Care Serv Q. (2021) 40:1–15. doi: 10.1080/01621424.2020.1869634
35. Liu Z, Heffernan C, Tan J. Caregiver burden: a concept analysis. Int J Nurs Sci. (2020) 7:438–45. doi: 10.1016/j.ijnss.2020.07.012
36. Turner MJ, Killian TS, Cain R. Life course transitions and depressive symptoms among women in midlife. Int J Aging Hum Dev. (2004) 58:241–65. doi: 10.2190/4CUU-KDKC-2XAD-HY0W
37. Wethington E. An overview of the life course perspective: implications for health and nutrition. J Nutr Educ Behav. (2005) 37:115–20. doi: 10.1016/S1499-4046(06)60265-0
38. Segal MW, Lane MD, Fisher A. Conceptual model of military career and family life course events, intersections, and effects on well-being. Milit Behav Health. (2015) 3:107–95. doi: 10.1080/21635781.2015.1009212
39. Johnson RB, Onwuegbuzie AJ, Turner LA. Toward a definition of mixed methods research. J Mix Methods Res. (2007) 1:112–33. doi: 10.1177/1558689806298224
40. Moseholm E, Fetters MD. Conceptual models to guide integration during analysis in convergent mixed methods studies. Methodol Innov. (2017) 10:2059799117703118. doi: 10.1177/2059799117703118
41. Sandelowski M. Whatever happened to qualitative description? Res Nurs Health. (2000) 23:334–40. doi: 10.1002/1098-240X(200008)23:4<334::AID-NUR9>3.0.CO;2-G
42. Sayer NA, Orazem RJ, Noorbaloochi S, Gravely A, Frazier P, Carlson KF, et al. Iraq and Afghanistan war veterans with reintegration problems: differences by veterans affairs healthcare user status. Adm Policy Ment Health. (2015) 42:493–503. doi: 10.1007/s10488-014-0564-2
43. Rattray NA, Flanagan M, Salyers M, Natividad D, Do A, Frankel RM, Spontak K, Kukla M. The association between reintegration, perceptions of health and flourishing during transition from military to civilian life among veterans with invisible injuries. J Vet Stud. (2023) 9:224–34. doi: 10.21061/jvs.v9i1.432
44. Bédard M, Molloy DW, Squire L, Dubois S, Lever JA, O'Donnell M. The Zarit Burden Interview: a new short version and screening version. Gerontologist. (2001) 41:652–7. doi: 10.1093/geront/41.5.652
45. Higginson IJ, Gao W, Jackson D, Murray J, Harding R. Short-form Zarit Caregiver Burden Interviews were valid in advanced conditions. J Clin Epidemiol. (2010) 63:535–42. doi: 10.1016/j.jclinepi.2009.06.014
46. Gratão ACM, Brigola AG, Ottaviani AC, Luchesi BM, Souza É N, Rossetti ES, et al. Brief version of Zarit Burden Interview (ZBI) for burden assessment in older caregivers. Dement Neuropsychol. (2019) 13:122–9. doi: 10.1590/1980-57642018dn13-010015
47. Yu J, Yap P, Liew TM. The optimal short version of the Zarit Burden Interview for dementia caregivers: diagnostic utility and externally validated cutoffs. Aging Ment Health. (2019) 23:706–10. doi: 10.1080/13607863.2018.1450841
48. Whitlatch CJ, Zarit SH, von Eye A. Efficacy of interventions with caregivers: a reanalysis. Gerontologist. (1991) 31:9–14. doi: 10.1093/geront/31.1.9
49. Hébert R, Bravo G, Préville M. Reliability, validity and reference values of the Zarit Burden Interview for assessing informal caregivers of community-dwelling older persons with dementia. Can J Aging. (2000) 19:494–507. doi: 10.1017/S0714980800012484
50. Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. (1983) 24:385–96. doi: 10.2307/2136404
51. VanderWeele TJ. On the promotion of human flourishing. Proc Nat Acad Sci USA. (2017) 114:8148–56. doi: 10.1073/pnas.1702996114
52. Wȩziak-Białowolska D, McNeely E, VanderWeele TJ. Human flourishing in cross cultural settings. Evidence from the United States, China, Sri Lanka, Cambodia, and Mexico. Front Psychol. (2019) 10:1269. doi: 10.3389/fpsyg.2019.01269
53. Diener E, Emmons RA, Larsen RJ, Griffin S. The satisfaction with life scale. J Pers Assess. (1985) 49:71–5. doi: 10.1207/s15327752jpa4901_13
54. Pavot W, Diener E. Review of the satisfaction with life scale. Psychol Assess. (1993) 5:164–72. doi: 10.1037/1040-3590.5.2.164
55. Williamson GM, Schulz R. Caring for a family member with cancer: past communal behavior and affective reactions. J Appl Soc Psychol. (1995) 25:93–116. doi: 10.1111/j.1559-1816.1995.tb01586.x
56. Williamson GM, Schulz R. Relationship orientation, quality of prior relationship, and distress among caregivers of Alzheimer's patients. Psychol Aging. (1990) 5:502. doi: 10.1037/0882-7974.5.4.502
57. Williamson GM, Shaffer DR. Relationship quality and potentially harmful behaviors by spousal caregivers: how we were then, how we are now. Psychol Aging. (2001) 16:217. doi: 10.1037/0882-7974.16.2.217
58. Winter L, Moriarty HJ. Quality of relationship between veterans with traumatic brain injury and their family members. Brain Injury. (2017) 31:493–501. doi: 10.1080/02699052.2017.1283534
59. True G, Rigg KK, Butler A. Understanding barriers to mental health care for recent war veterans through photovoice. Qual Health Res. (2015) 25:1443–55. doi: 10.1177/1049732314562894
60. Averill JB. Matrix analysis as a complementary analytic strategy in qualitative inquiry. Qual Health Res. (2002) 12:855–66. doi: 10.1177/104973230201200611
61. Miles MB, Huberman AM, Saldaña J. Qualitative Data Analysis: A Methods Sourcebook. Thousand Oaks, CA: Sage (2014).
63. Benjamini Y, Hochberg Y. Controlling the false discovery rate: a practical and powerful approach to multiple testing. J Royal Stat Soc. (1995) 57:289–300. doi: 10.1111/j.2517-6161.1995.tb02031.x
64. Segal MW, Lane MD. Conceptual model of military women's life events and well-being. Mil Med. (2016) 181:12–9. doi: 10.7205/MILMED-D-15-00345
65. Brouwer WBF, Exel NJAv, Berg Bvd, Bos GAMvd, Koopmanschap MA. Process utility from providing informal care: the benefit of caring. Health Pol. (2005) 74:85–99. doi: 10.1016/j.healthpol.2004.12.008
66. Lin E, Durbin J, Guerriere D, Volpe T, Selick A, Kennedy J, et al. Assessing care-giving demands, resources and costs of family/friend caregivers for persons with mental health disorders: a scoping review. Health Soc Care Community. (2018) 2018:hsc.12546. doi: 10.1111/hsc.12546
Keywords: military Veterans, caregiver burden, caregiving, mixed methods, health services, veteran reintegration
Citation: Rattray NA, Flanagan M, Mann A, Danson L, Do A-N, Natividad D, Spontak K and True G (2024) Conceptualizing care partners' burden, stress, and support for reintegrating Veterans: a mixed methods study. Front. Public Health 11:1295627. doi: 10.3389/fpubh.2023.1295627
Received: 18 September 2023; Accepted: 07 December 2023;
Published: 19 February 2024.
Edited by:
Mary Jo Pugh, The University of Utah, United StatesReviewed by:
Roxana Delgado, The University of Texas Health Science Center at San Antonio, United StatesCopyright © 2024 Rattray, Flanagan, Mann, Danson, Do, Natividad, Spontak and True. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Nicholas A. Rattray, bnJhdHRyYXlAaXVwdWkuZWR1
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.