- 1Department of Epidemiology, International School of Public Health and One Health, Hainan Medical University, Haikou, China
- 2Department of Geriatric Center, Hainan General Hospital, Haikou, China
- 3School of Basic Medicine and Life Science, Hainan Medical University, Haikou, China
Objective: Asthma is a major public health problem that affects both children and adults, and its prevalence varies among people with different climatic characteristics and living habits. However, few studies have investigated the prevalence and risk factors for asthma among tropical residents in China. Therefore, this study aims to investigate the correlation between individuals’ living environment and daily habits in Hainan Province, and the occurrence of asthma.
Methods: This cross-sectional study collected data from 1021 participants in three regions of the Hainan Province. A questionnaire derived from the European Community Respiratory Health Survey was used to collect data on demographics, living habits, self-reported asthma, and respiratory system-related symptoms. Logistic regression was used for univariate and multivariate analyses to screen for relative risk factors associated with asthma.
Results: Among the 1,021 subjects investigated, the prevalence rate of self-reported asthma was 18.6%. Significant risk factors for asthma include hair dyeing, longer living time in Hainan, higher BMI, and living in a damp and musty room. Protective factors included fruit intake, years of higher education, and indoor timing of natural ventilation.
Conclusion: Higher frequency of hair dyeing, higher body mass index (BMI), longer living in Hainan, lower frequency of fruit intake, fewer years of education, a damp and musty room, and no indoor timing natural ventilation were associated with an increased risk of asthma.
1. Introduction
Asthma is a prevalent chronic, non-communicable disease that affected approximately 272.68 million people globally in 2017 (1). It is a prevalent respiratory disease characterized by airflow obstruction, airway inflammation, and airway hyperresponsiveness. These symptoms lead to wheezing, coughing, chest tightness, and shortness of breath in patients (2). This is a significant contributor to disability, health resource usage, and a diminished quality of life worldwide. Treatment of asthma with leukotriene receptor antagonists, either as monotherapy or in combination with inhaled corticosteroids (ICS), can effectively reduce asthma exacerbation. Additionally, biotherapy and macrolide antibiotics have emerged as potential treatment options in recent years (3).
The estimated global prevalence of doctor-diagnosed asthma in adults was 4.3% (95%CI: 4.2 ~ 4.4). However, there are significant variations between countries, with the highest prevalence rate found in developed countries such as Australia (21.5%) and the lowest in developing countries such as Vietnam (1.0%) (4). Using standardized data obtained from the World Health Organization (WHO) World Health Survey (WHS), we estimated that the global prevalence of clinical asthma in adults was 4.5% (4). A national cross-sectional study showed that the overall prevalence rate of asthma in China was 4.2% (5), implying a low diagnostic rate of asthma in the Chinese population and probably underestimating the true prevalence of the disease. Asthma is a complex condition characterized by variable respiratory symptoms and airflow limitations. Asthma exacerbations are typically associated with exposure to environmental allergens or upper respiratory tract infections, such as viruses (6). Previous studies have identified several risk factors for asthma, including age, exposure to mold, living in damp housing, smoking, exposure to mite mix, and cockroach allergens (5, 7–10).
Although allergies have traditionally been associated with western countries, they are also prevalent in developing countries.
Recent reports indicate that in the Asia-Pacific region, the prevalence of allergic diseases has reached its highest level in the last 50 years (7), a trend also observed in the tropical region of Southeast Asia. Furthermore, research has shown that in tropical regions, poly sensitization and seasonal variations complicate the management of allergic diseases. The causative agents of allergy in the tropics differ significantly from those observed in temperate countries (11). For example, Allergenic fungi are frequently present in Asian countries located in the tropics, where high levels of humidity and warm climates provide favorable conditions for their growth (12). As a result, a large number of fungal spores are airborne (13). These environmental conditions can potentially impact asthma symptoms.
Hainan province is the only province in China located entirely in tropical areas, and it possesses unique climate characteristics and dietary habits. This study aimed to investigate the prevalence rate of self-reported asthma in Hainan Province and explore the association of living habits, indoor humidity, and ventilation with asthma. A comprehensive understanding of the interrelationship between the factors under study can assist in the development of targeted interventions aimed at improving lifestyle habits, reducing the occurrence of asthma, and enhancing the quality of life in Hainan, China.
2. Materials and methods
2.1. Study design
From April to August 2021, this cross-sectional study was conducted in three administrative districts with varying humidity in Hainan Province, including Haikou, Chengmai, and Dongfang City. The study utilized stratified cluster random sampling to select subjects more than 18 years old from two universities in Haikou and Chengmai City, with a small portion of ordinary residents in Dongfang City.
2.2. Data collection
Data were collected using questionnaires derived from the European Community Respiratory Health Survey (ECRHS). This study investigated the basic demographic characteristics of subjects, including age, sex, ethnicity, years of education, whether parents had asthma, living time in Hainan, and BMI. In addition, the questionnaire covered the dietary information of subjects, whether animals were raised, whether the room was damp and musty, and whether there was indoor timing of natural ventilation. “There were more than three wheezing episodes during the past any time and there was wheezing when breathing out” was used as the standard for self-reported asthma.
The clinical features of self-reported asthma patients were also investigated, such as whether there were repeated attacks (more than three times) in the past 12 months, how many wheezing attacks occurred in the past 12 months, how long the repeated attacks of suffocation and wheezing symptoms lasted in the past 12 months, and whether the most severe stages in the past included inability to sleep, walk, suffocation at night.
Before the survey began, the questionnaire was reviewed and all relevant staff participating in the survey received training to ensure consistency. All participants completed the questionnaire anonymously with informed consent. The study was approved by the Ethics Review Committee of Hainan Medical University.
2.3. Statistical analysis
Basic demographic information and clinical characteristics of self-reported asthma patients were described using frequency and percentage. The prevalence rate of self-reported asthma was displayed according to the characteristics of the different populations, and univariate analysis was performed using the chi-square test. The compared variables included sex, age, living time in Hainan Province, ethnicity, years of education, BMI, whether pets were kept in the home, whether there was damp and musty in the room, whether there was timing natural ventilation in the room, whether parents had asthma, fruit intake frequency, vegetable intake frequency, meat intake frequency, exercise frequency, hair dyeing frequency, smoking frequency, drinking frequency, and mattress cleaning frequency. Self-reported asthma was used as the dependent variable, and the statistically significant indicators in the univariate analysis were used as independent variables. Binary logistic regression conditional forward method was used to screen for risk factors. The multifactorial regression model used in this study considered a wide range of factors, including general demographic characteristics, parental history of asthma, living environment, and local dietary behaviors. By identifying the risk factors through this model, we can develop targeted asthma prevention and control measures that cater to the needs of tropical residents. Statistical analyses were performed using IBM SPSS Statistics version 26.0(IBM SPSS Inc., Chicago, IL, United States). A significance level of p < 0.05 was used for all analyses. Figures were conducted using R software version 4.0.3 (R Development Core Team, Vienna, Austria).
3. Results
3.1. Characteristics of the study subjects
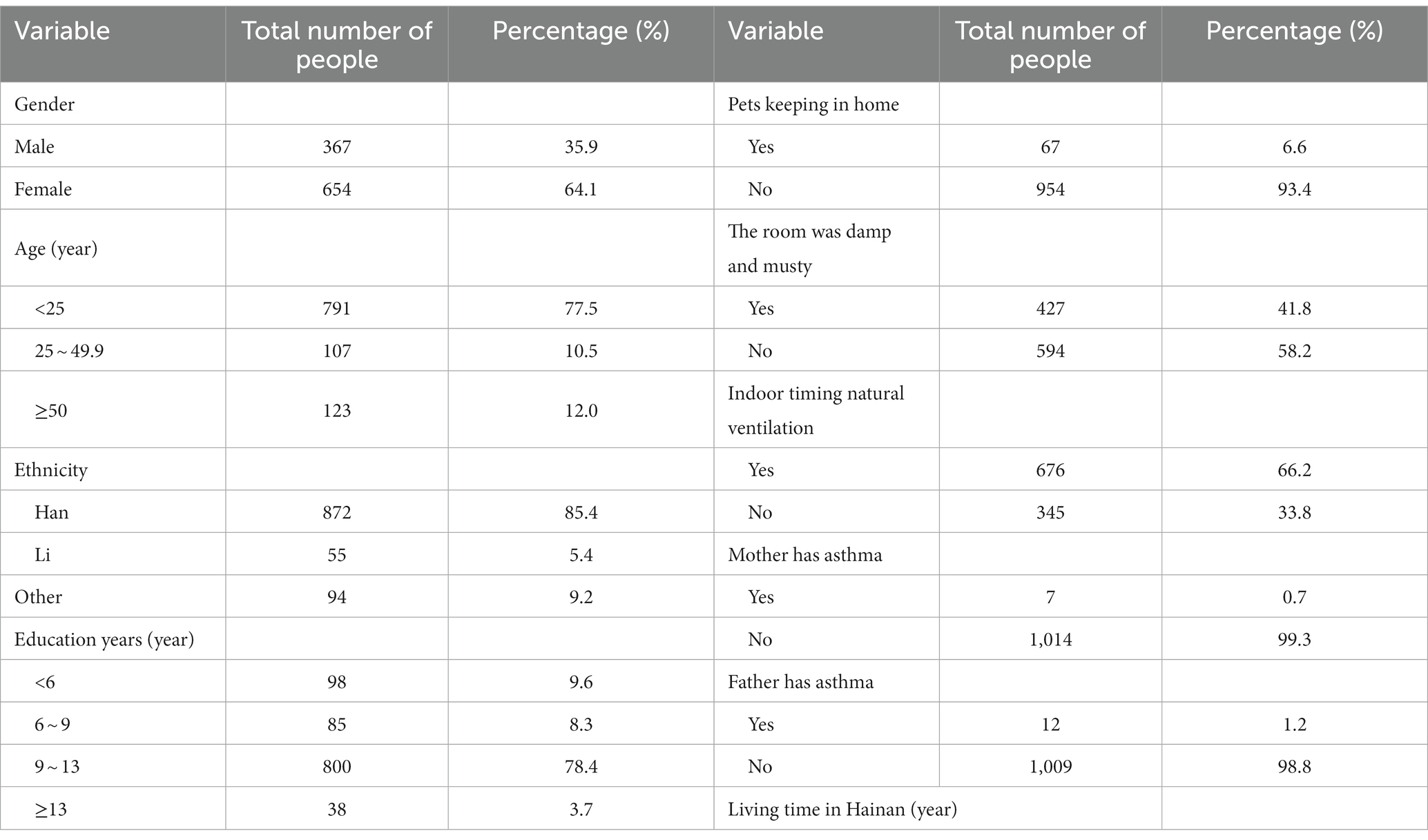
A total of 1,033 subjects were included in this survey, and 1,021 (98.8%) subjects were included for further analysis. Among the participants investigated, 367 were male (35.9%) and 654 were female (64.1%). The majority of the participants (77.5%) were range from 18 to 25 years of age. The Han ethnicity accounted for the largest proportion (85.4%) of 872 subjects, followed by the Li ethnicity (55 subjects, 5.4%) and other ethnicities (94 subjects, 9.2%). The largest period of education was 9–13 years, with 800 participants (78.4%). A total of 329 participants (32.2%) had lived in Hainan for more than 20 years. A total of 67 people (6.6%) kept pets, 427 subjects (41.8%) lived in damp and musty rooms, and 676 subjects (66.2%) had indoor timing natural ventilation. Seven mothers (0.7%) and 12 fathers (1.2%) had asthma (Table 1).
3.2. Basic clinical feature of asthma patients
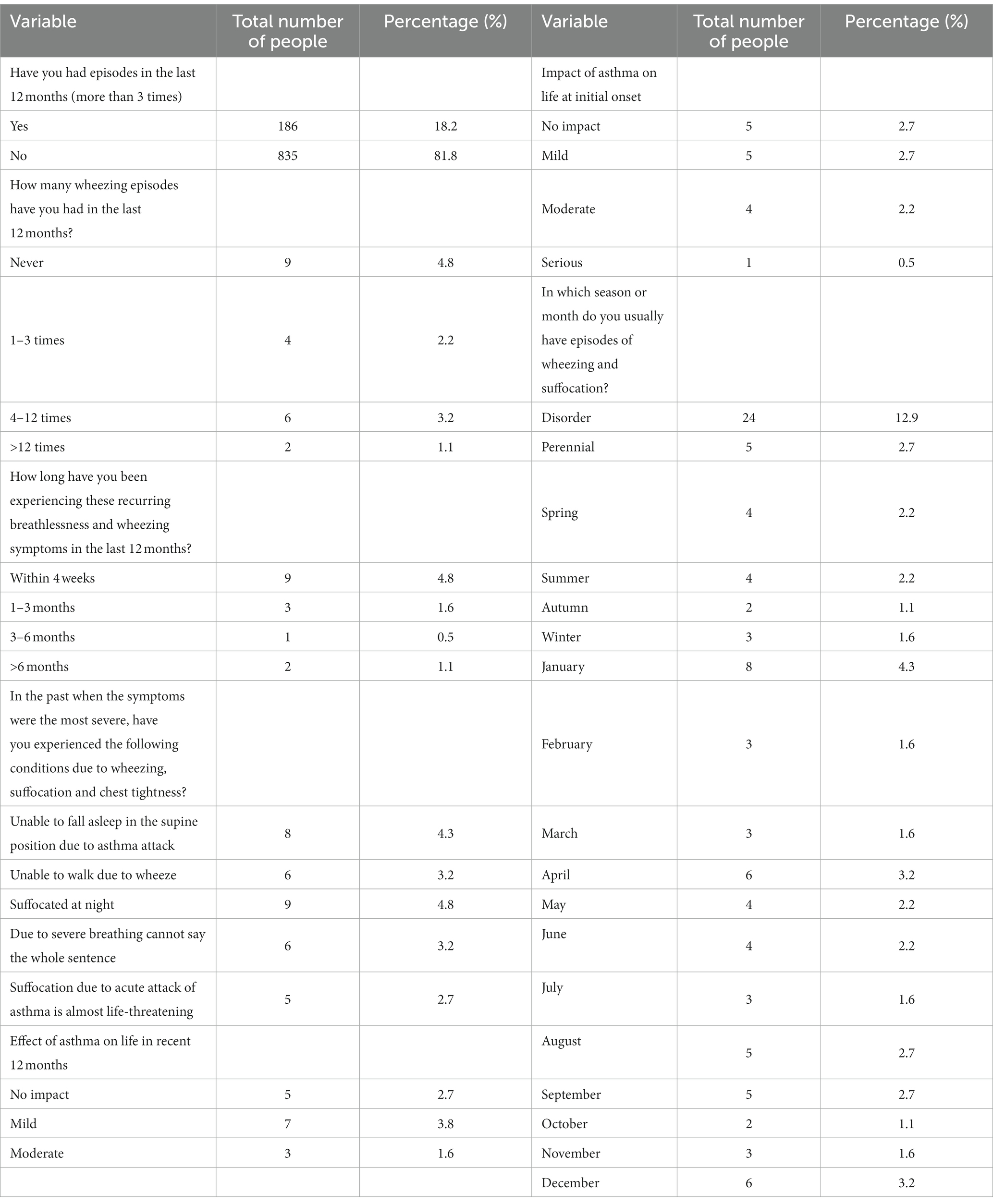
A total of 186 out of 1,021 subjects self-reported asthma, with a prevalence rate of 18.2%. Among the self-reported asthma patients in this survey, 15.6% had repeated episodes in the last 12 months, 4.8% had breathlessness and wheezing lasting less than four weeks, and 12.9% had irregular symptoms that could occur in any season or within 12 months. The other clinical characteristics are shown in Table 2.
3.3. Univariate analysis
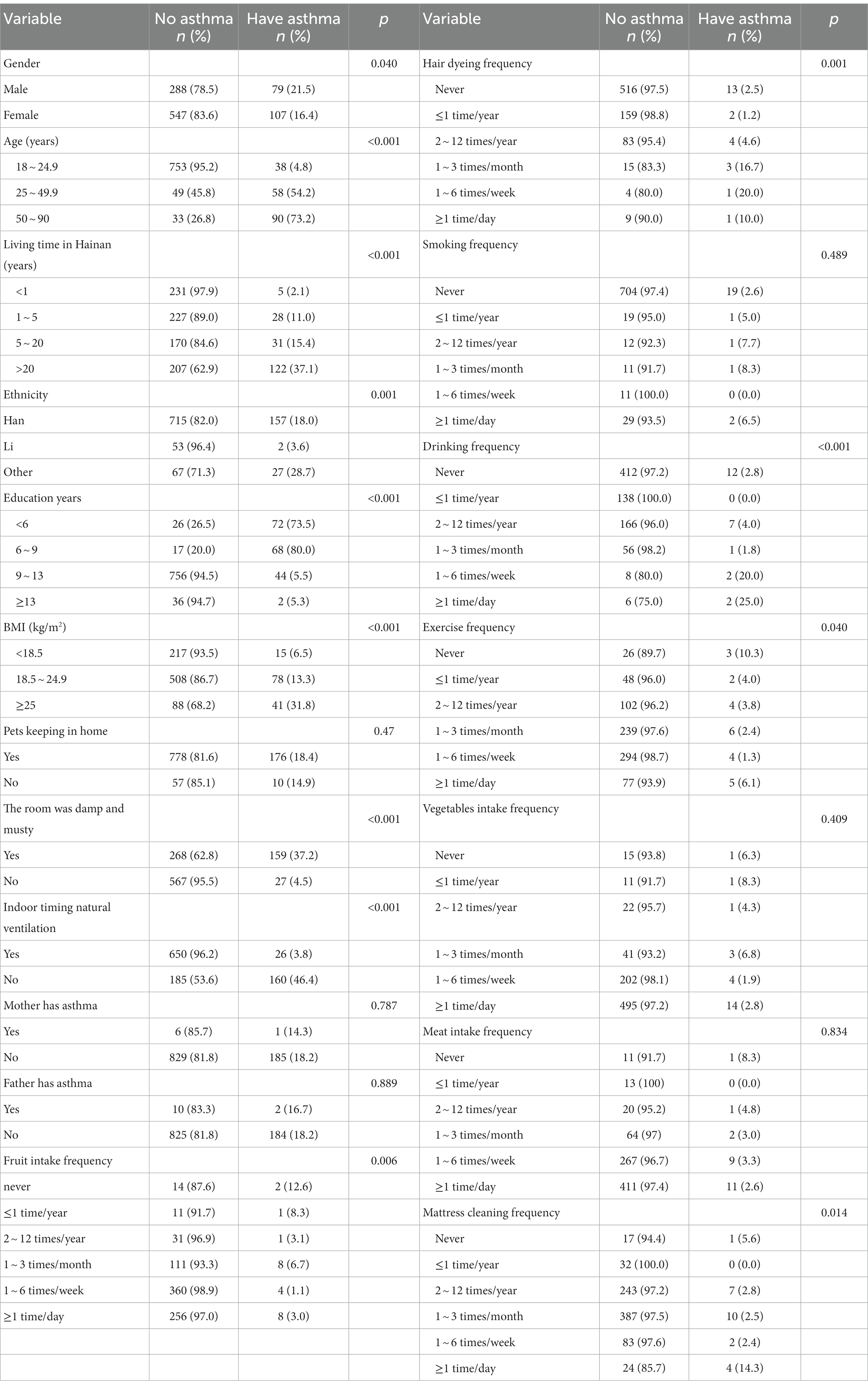
The results of the univariate analysis showed that there were significant differences in different groups of sex, age, living time in Hainan, ethnicity, years of education, BMI, hair dyeing frequency, drinking frequency, fruit intake frequency, exercise frequency, mattress cleaning frequency, whether the room was damp and musty, and whether the room was timing natural ventilation (p < 0.05). The prevalence rate of self-reported asthma in male was higher than that in female (p < 0.05). The prevalence increased with age, living time in Hainan, and BMI (p < 0.05). Indoor humidity and a musty environment, hair dyeing, and drinking were risk factors (p < 0.05). In contrast, years of education, indoor timing of natural ventilation, higher fruit intake frequency, and exercise frequency appropriately decreased the prevalence rate of asthma (p < 0.05) (Table 3).
3.4. Multivariate analysis
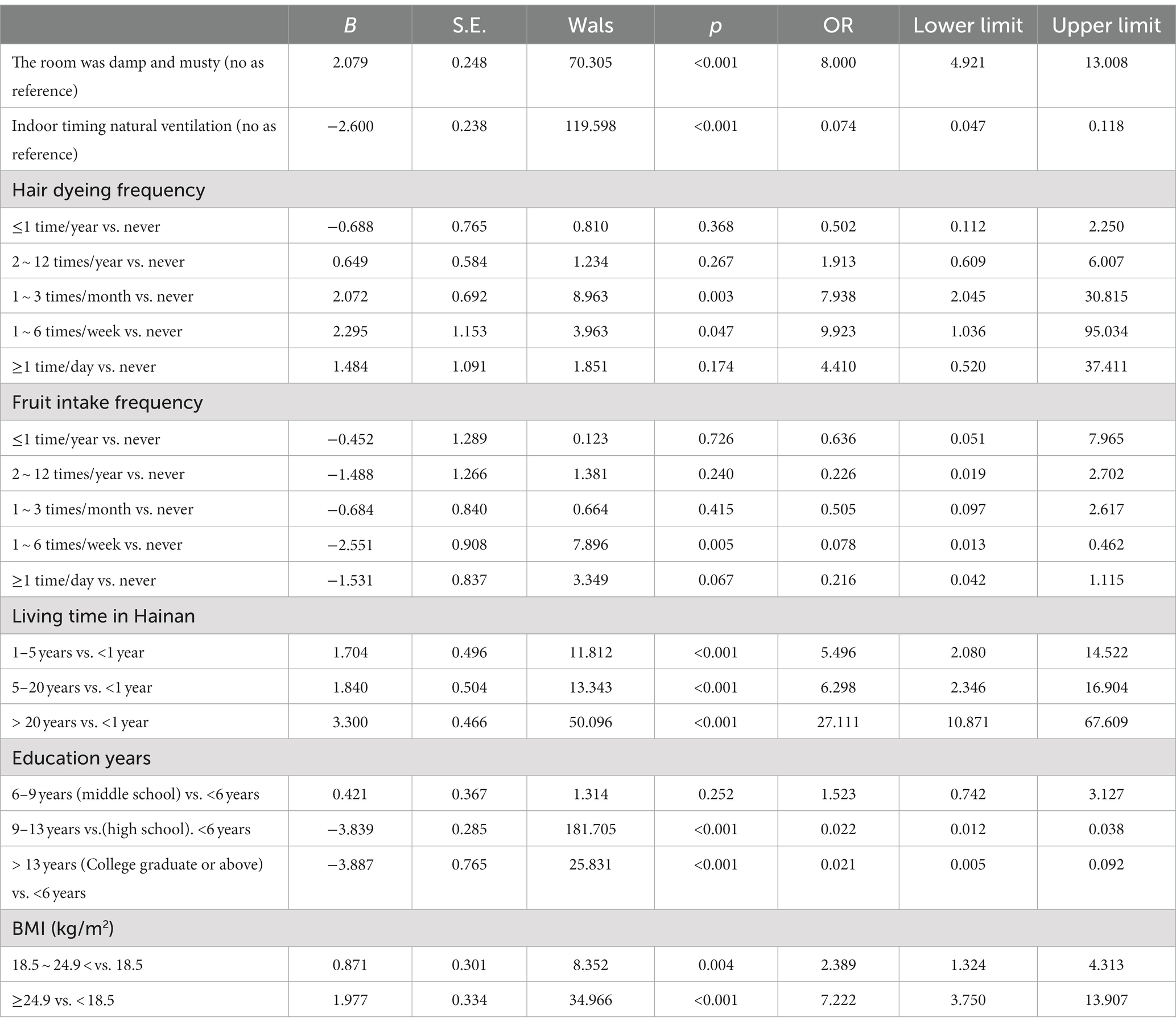
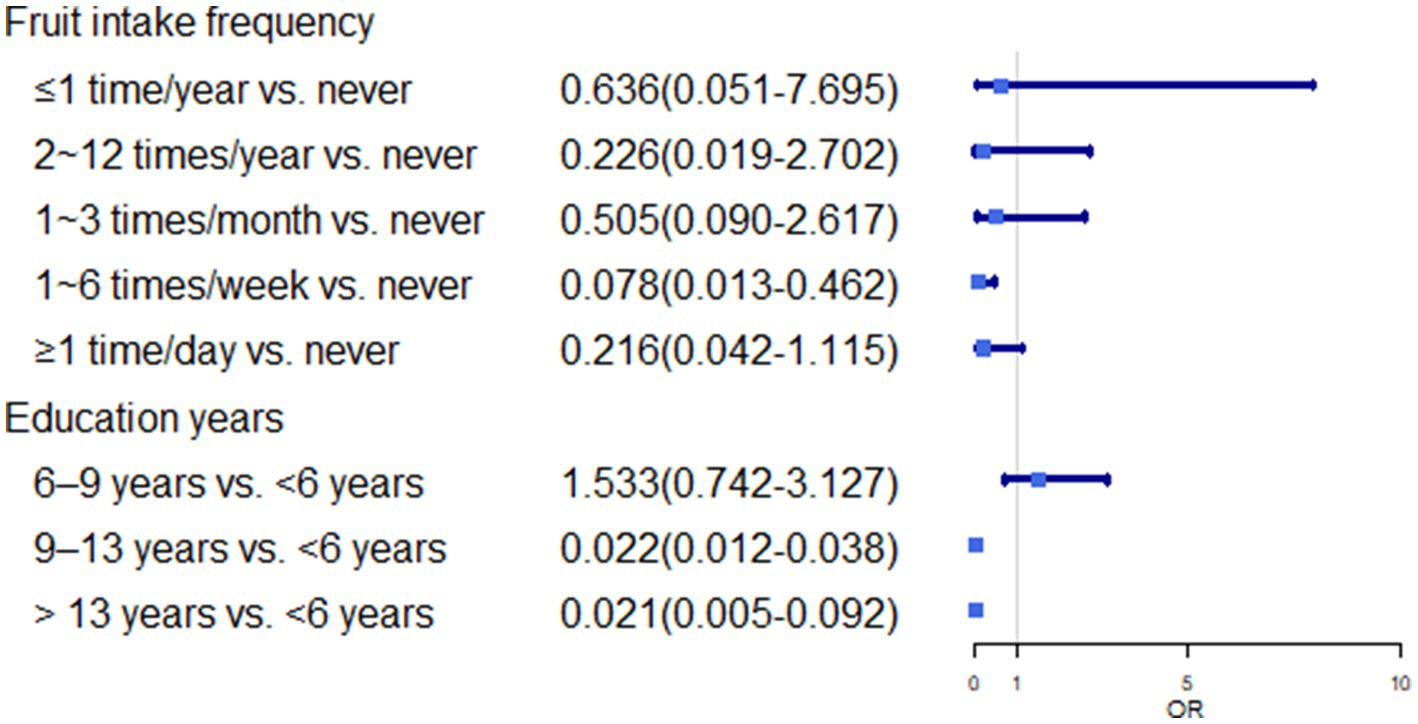
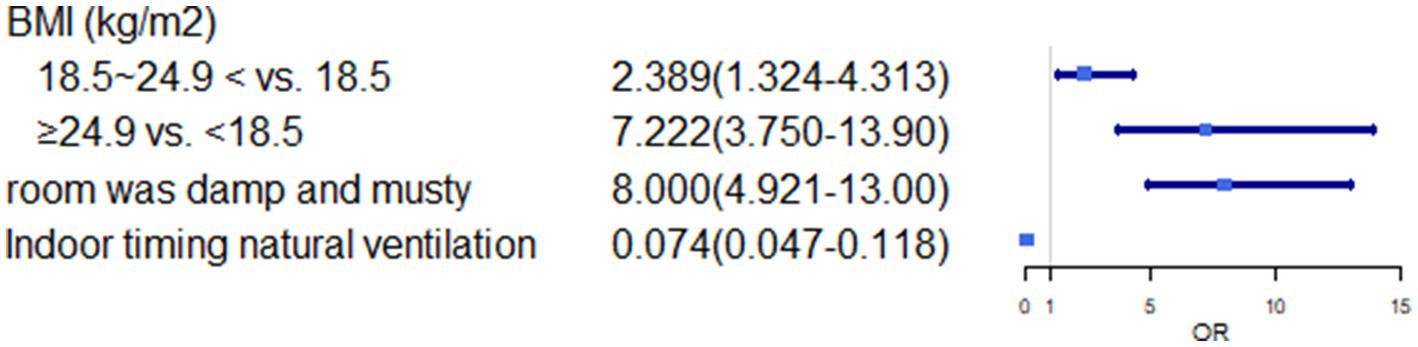
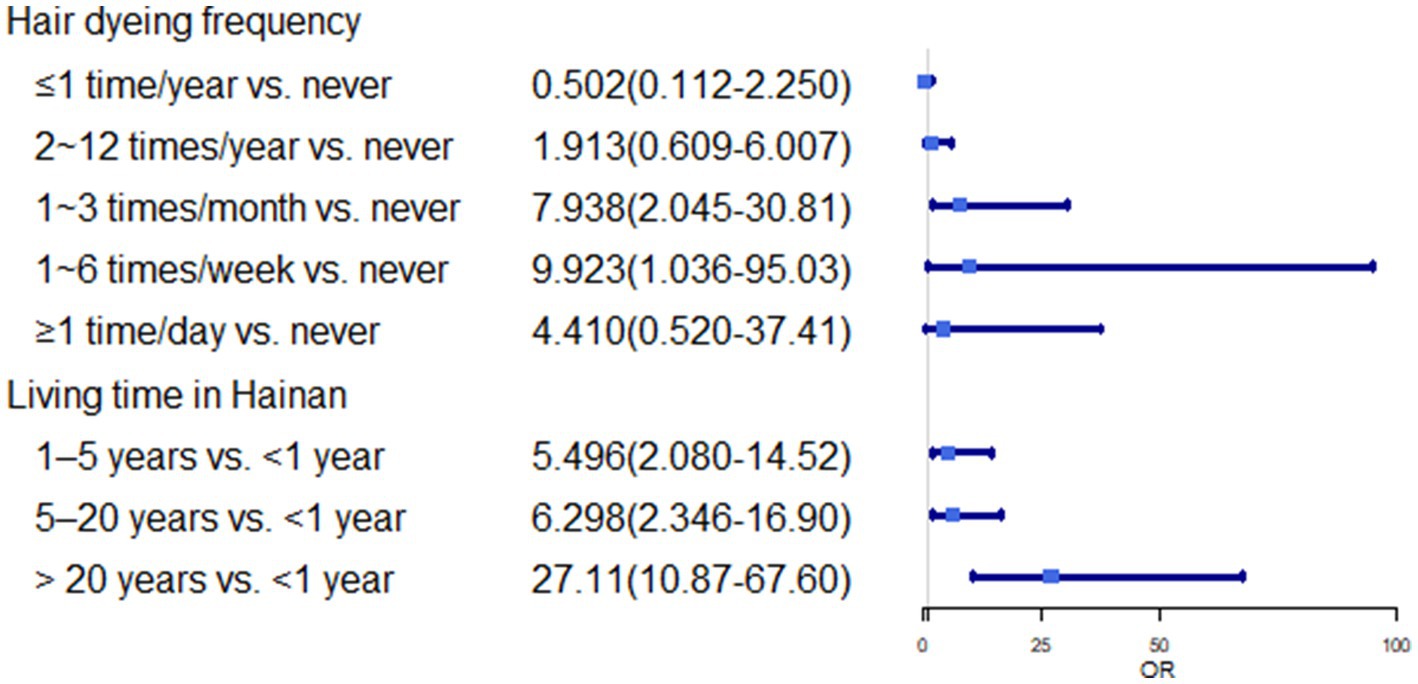
In multivariate analysis, we found some risk factors positively associated with the higher prevalence rate of asthma including longer living time in Hainan (>20 years vs. <1 year: OR, 27.111; 95%CI, 10.871 ~ 67.609), BMI (≥24.9 kg/m2 vs. <18.5 kg/m2: OR, 7.222; 95%CI, 3.750 ~ 13.907), hair dyeing (1 ~ 6 times/week vs. never: OR, 9.923; 95%CI, 1.036 ~ 95.034), the room was damp and musty (Yes vs. No: OR, 8.000; 95%CI, 4.921 ~ 13.008) (p < 0.05). Additionally, fruit intake (1–6 times/week vs. never: OR, 0.078; 95%CI, 0.013–0.462), years of education (>13 years vs. <6 years: OR, 0.021; 95%CI, 0.005–0.092), and indoor timing of natural ventilation (yes vs. No: OR 0.074; 95%CI, 0.047–0.118) showed a negative correlation with the prevalence rate of self-reported asthma (p < 0.05) (Table 4; Figures 1–3).
4. Discussion
In this study, univariate and multivariate analyses showed that higher fruit intake frequency, years of education, and indoor timing of natural ventilation were negatively correlated with the prevalence rate of self-reported asthma (p < 0.05). Conversely, living in a damp and musty room, a higher frequency of hair dyeing, longer living time in Hainan, and higher BMI were positively correlated with the prevalence of self-reported asthma (p < 0.05). The prevalence rate of self-reported asthma in this study was 18.2%. Similarly, according to Pagán et al. (4), the five countries with the highest prevalence rates of clinical asthma were Australia (21.5%), Sweden (20.2%), the UK (18.2%), the Netherlands (15.3%), and Brazil (13.0%). This indicates that asthma is a serious public health concern. However, our estimated prevalence rate of asthma based on questionnaires was higher than the value of 5.8% reported by Wang et al. in a phone interview study of adults aged 16–65 years from 18 major cities in China (14) and also higher than that reported by Huang et al. (5) in a cross-sectional study (4.2%).
In this study, we also found that living in damp and musty rooms was a risk factor for asthma (p < 0.05). The tropics are regions of the Earth surrounding the equator, delimited in latitude by the Tropic of Cancer in the Northern Hemisphere and the Tropic of Capricorn in the Southern Hemisphere. Haikou and Chengmai have a tropical monsoon climate with high-temperature and high-humidity environments. The annual average temperature ranges from 23.1 to 27.0°C, and the annual average humidity is greater than 70% (15, 16). These conditions provide an ideal warm and humid environment (25–30°C with a relative humidity of 70%) for the growth and multiplication of house dust mites (HDMs) (8). Average annual temperature is the main outdoor factor that correlates with higher mite concentrations (4). Humidity is a significant limiting factor for HDMs growth and has a profound influence on reproduction (17, 18). Intensive rain and flooding induce dampness and mold proliferation in affected households, thereby affecting the quality of indoor air (19, 20). Numerous epidemiological studies have shown that the number of house dust mites in dwellings increases with increasing indoor air humidity (21). Dampness facilitates the growth of microorganisms such as bacteria and molds (22, 23). Many studies have shown that fungi and mold are associated with an increased risk of asthma (24, 25). Therefore, the climate in Hainan may have a positive impact on the production and reproduction of mold and dust mites, resulting in a higher asthma rate among local residents. Sun et al. compared the concentrations of house dust mite allergens in China and Europe and found that indoor dust mite allergen concentrations were lower in the north than in the south, both in China and Europe (26). Therefore, although the loose diagnostic criteria in this study may increase the estimated prevalence of asthma, given the unique geographical location and environment of this study and the fact that 41.8% of subjects expressed damp and musty rooms, it is possible that the prevalence of asthma in this region is indeed higher than that in other regions, and the longer living time in Hainan is associated with a higher risk of asthma. Furthermore, the prevalence of asthma in China is likely to increase rapidly due to rapid changes in the environment and lifestyle, as well as the aging population (27).
Hair dyeing was identified as a risk factor for asthma (p < 0.05). Para-phenylenediamine (PDD) and other members of the aromatic amine family have been extensively used as primary agents in permanent hair dyes. Presently, over two-thirds of hair dyes in the market contain PPD (28). Hairdressers are at a high risk of occupational rhinitis and asthma because, in daily work, they are frequently exposed to irritants and allergens such as persulfate and PDD in hair dyes (29, 30). In vitro experiments involve the use of substances, such as PDD and hydrogen peroxide, in stains to reduce the acetylation of keratinocytes. This ultimately leads to the development of allergy asthma (26). Moreover, Haltia et al. (31) showed that vegetable hair dye containing indigo powder should be considered a causative agent for occupational asthma. Therefore, reducing the frequency of hair dyeing could increase the risk of asthma.
In this study, there was a positive association between asthma and BMI (p < 0.05), which is consistent with the findings of Kumar (32), who reported that the prevalence of asthma was higher in overweight respondents than in those with normal weight, indicating that body weight could be a key modifiable risk factor. Similarly, A meta-analysis of several prospective studies involving more than 300,000 adults found a dose–response relationship between obesity and asthma: the odds ratio of incident asthma was 1.5 in the overweight and 1.9 in the obese groups compared with the lean group (33). Epidemiological evidence has established a relationship between obesity and asthma (33, 34). The association between asthma and BMI is particularly relevant in the context of the increasing obesity rates worldwide. Previous studies have demonstrated that obesity is correlated with the enhanced secretion of inflammatory cytokines, including IL-6, IL-1β, and TNF-α. Consequently, this leads to lower levels of systemic inflammation and higher susceptibility to worsened asthma (35). Therefore, attention should be paid to the adverse effects of obesity on asthma.
In contrast, we found a negative correlation between years of education and the prevalence rate of self-reported asthma (p < 0.05), which is consistent with the findings of Anto et al. (35) and Fazlollahi et al. (36). This may be because subjects with higher education levels have better health knowledge and behaviors that can help reduce the risk of asthma. Our survey also found that increased fruit intake reduced the risk of asthma (p < 0.05). Similarly, an overview of systematic reviews showed evidence of the beneficial effects of fresh fruits and antioxidant vitamins on asthma (37). Several studies in adults have linked high fruit and vegetable intake to a lower risk of asthma (38–41). Airways are particularly vulnerable to oxidative damage (42). In experiments, oxidants can induce many symptoms of asthma by inducing the release of proinflammatory mediators, including cytokines and chemokines (43). The fruits contain several antioxidants. Therefore, fruit intake is associated with reduced risk of asthma. Additionally, our study found that the indoor timing of natural ventilation was associated with a lower risk of asthma (p < 0.05). Sun et al. (26) suggested that indoor ventilation can reduce the concentration of HDMs. Vardoulakis et al. (44) believed that ventilation is a key factor affecting the indoor air quality (chemical and microbial) and moisture-related allergens (mold and dust mites) in dwellings. Therefore, indoor ventilation is often conducive to reducing the incidence of asthma allergens, thereby reducing the occurrence of asthma in the local population.
5. Limitations and recommendations
This study represents the first investigation of the prevalence rate of asthma and its associated influencing factors in tropical Chinese regions, and the screening factors were comprehensive. There are still shortcomings in this study. Firstly, this was a cross-sectional study, no causal inference can be made. Secondly, The research subjects in this study were mainly college students and there were fewer community residents. Therefore, the generalizability of the research conclusion is limited; it is relevant to young and middle-aged groups. Studies should appropriately expand sample populations, such as including children and adolescents, and increase the number of follow-up studies to provide sufficient information to support clinical treatment and prevention. However, this study provides important insights for subsequent analytical studies. Our study suggests that medical practitioners should educate individuals who suffer from allergies on methods to reduce the frequency of hair coloring, maintain a healthy body weight, increase fruit consumption, and regularly open windows to keep indoor humidity low. Additionally, they may consider purchasing dehumidifiers to reduce indoor humidity. These interventions aim to prevent or reduce the occurrence of allergic diseases. Then, local hospitals can educate the public about the occurrence mechanisms of allergic diseases and prevention methods, among other things to enhance the general knowledge of allergic diseases among the public.
6. Conclusion
The prevalence of self-reported asthma in the tropical regions of China was 18.2%. Factors such as higher frequency of hair dyeing, higher BMI, longer living in Hainan, lower frequency of fruit intake, lower years of education, a damp and musty room, and no indoor timing natural ventilation were found to increase the risk of asthma. Therefore, These findings could help raise awareness among residents of asthma and its associated risk factors. Additionally, Hainan Province is the only region in China situated in the tropics. This study offers diagnostic and treatment assistance in the field of tropical medicine, while also serving as the foundation for allergy prevention in Southeast Asia. Future studies should explore further information about the risk factors and underlying causes of asthma in tropical residents.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by RZ, a member of our unit, has applied for the 2021 of the National Natural Science Foundation of China. After preliminary examination by the Ethics Review Committee of Hainan Medical University. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
MC: Writing – original draft, Writing – review & editing. XZ: Writing – review & editing. KZ: Conceptualization, Writing – review & editing. JG: Writing – original draft. RZ: Writing – original draft, Writing – review & editing. XW: Writing – review & editing. WC: Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This work was funded by the Hainan Provincial Natural Science Foundation of China (821RC583), Hainan Provincial Natural Science Foundation of China (820CXTD438), and National Natural Science Foundation of China (82160634).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
BMI, body mass index; WHS, world health survey; WHO, world health organization; ECRHS, the European community respiratory health survey; HDMs, house dust mites.
References
1. James, SL, Abate, D, Abate, KH, Abay, SM, Abbafati, C, Abbasi, N, et al. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: a systematic analysis for the global burden of disease study 2017. Lancet. (2018) 392:1789–858. doi: 10.1016/S0140-6736(18)32279-7
2. Im, D, Kishikawa, J, Shiimura, Y, Hisano, H, Ito, A, Fujita-Fujiharu, Y, et al. Structural insights into the agonists binding and receptor selectivity of human histamine H receptor. Nat Commun. (2023) 14:6538. doi: 10.1038/s41467-023-42260-z
3. Mayoral, K, Lizano-Barrantes, C, Zamora, V, Pont, A, Miret, C, Barrufet, C, et al. Montelukast in paediatric asthma and allergic rhinitis: a systematic review and meta-analysis. European respiratory review: an official journal of the European respiratory. Society. (2023) 32:170. doi: 10.1183/16000617.0124-2023
4. Pagán, JA, Huertas, AJ, Iraola, V, Pinto, H, Martínez, R, Ramírez, M, et al. Mite exposure in a Spanish Mediterranean region. Allergol Immunopathol (Madr). (2012) 40:92–9. doi: 10.1016/j.aller.2011.02.008
5. Huang, K, Yang, T, Xu, J, Yang, L, Zhao, J, Zhang, X, et al. Prevalence, risk factors, and management of asthma in China: a national cross-sectional study. Lancet. (2019) 394:407–18. doi: 10.1016/S0140-6736(19)31147-X
6. Nur Husna, S, Tan, H, Md Shukri, N, Mohd Ashari, N, and Wong, K. Allergic rhinitis: A clinical and pathophysiological overview. Front Med. (2022) 9:874114. doi: 10.3389/fmed.2022.874114
7. Gunnbjornsdottir, MI, Franklin, KA, Norback, D, Bjornsson, E, Gislason, D, Lindberg, E, et al. Prevalence and incidence of respiratory symptoms in relation to indoor dampness: the RHINE study. Thorax. (2006) 61:221–5. doi: 10.1136/thx.2005.057430
8. Acevedo, N, Zakzuk, J, and Caraballo, L. House dust mite allergy under changing environments. Allergy Asthma Immunol Res. (2019) 11:450–69. doi: 10.4168/aair.2019.11.4.450
9. Lin, J, Wang, W, Chen, P, Zhou, X, Wan, H, Yin, K, et al. Prevalence and risk factors of asthma in mainland China: the CARE study. Respir Med. (2018) 137:48–54. doi: 10.1016/j.rmed.2018.02.010
10. Wang, XA, Zhou, L, Wei, GX, Zhang, H, and Yang, B. Prevalence of allergen-specific IgE in southern China: a multicenter research. Aging (Albany NY). (2021) 13:18894–911. doi: 10.18632/aging.203341
11. Andiappan, AK, Puan, KJ, Lee, B, Nardin, A, Poidinger, M, Connolly, J, et al. Allergic airway diseases in a tropical urban environment are driven by dominant mono-specific sensitization against house dust mites. Allergy. (2014) 69:501–9. doi: 10.1111/all.12364
12. Sangngam, J, Prasopkittikun, T, Nookong, A, Pacharn, P, and Chamchan, C. Causal relationships among self-management behaviors, symptom control, health-related quality of life and the influencing factors among Thai adolescents with asthma. Int J Nurs Sci. (2023) 10:309–17. doi: 10.1016/j.ijnss.2023.06.001
13. Chakrabarti, A, HarsimranSavio, JR, MPatel, S, AtulShastri, PP, UmabalaKarthik, RB, SanjayKindo, AJB, et al. Epidemiology and clinical outcomes of invasive mould infections in Indian intensive care units (FISF study). J Crit Care. (2019) 51:64–70. doi: 10.1016/j.jcrc.2019.02.005
14. Wang, XD, Zheng, M, Lou, HF, Wang, CS, Zhang, Y, Bo, MY, et al. An increased prevalence of self-reported allergic rhinitis in major Chinese cities from 2005 to 2011. Allergy. (2016) 71:1170–80. doi: 10.1111/all.12874
15. Long, HX, Dai, SP, Li, MF, and Xie, ZH. Characterization of climate change on Hainan Island 1959-2015. Jiangsu Agric Sci. (2018) 12:268. doi: 10.15889/j.1ssn.1002-1302.2018.15.066
16. Wu, SA, Xin, CY, and Zhu, JJ. Characterization of the climate of Hainan Island. J Trop Biol. (2022) 15:315–21. doi: 10.15886/j.cnki.rdswxb.2022.04.001
17. Hart, BJ. Life cycle and reproduction of house-dust mites: environmental factors influencing mite populations. Allergy. (1998) 53:13–7. doi: 10.1111/j.1398-9995.1998.tb04990.x
18. Arlian, LG, and Platts-Mills, TA. The biology of dust mites and the remediation of mite allergens in allergic disease. J Allergy Clin Immunol. (2001) 107:S406–13. doi: 10.1067/mai.2001.113670
19. Katelaris, CH, and Beggs, PJ. Climate change: allergens and allergic diseases. Intern Med J. (2018) 48:129–34. doi: 10.1111/imj.13699
20. D'Amato, G, Annesi-Maesano, I, Cecchi, L, and D'Amato, M. Latest news on relationship between thunderstorms and respiratory allergy, severe asthma, and deaths for asthma. Allergy. (2019) 74:9–11. doi: 10.1111/all.13616
21. Korsgaard, J. Epidemiology of house-dust mites. Allergy. (1998) 53:36–40. doi: 10.1111/j.1398-9995.1998.tb04994.x
22. Bjornsson, E, Norback, D, Janson, C, Widstrom, J, Palmgren, U, Strom, G, et al. Asthmatic symptoms and indoor levels of micro-organisms and house dust mites. Clin Exp Allergy. (1995) 25:423–31. doi: 10.1111/j.1365-2222.1995.tb01073.x
23. Munir, AK, Bjorksten, B, Einarsson, R, Ekstrand-Tobin, A, Moller, C, Warner, A, et al. Mite allergens in relation to home conditions and sensitization of asthmatic children from three climatic regions. Allergy. (1995) 50:55–64. doi: 10.1111/j.1398-9995.1995.tb02483.x
24. Thacher, JD, Gruzieva, O, Pershagen, G, Melen, E, Lorentzen, JC, Kull, I, et al. Mold and dampness exposure and allergic outcomes from birth to adolescence: data from the BAMSE cohort. Allergy. (2017) 72:967–74. doi: 10.1111/all.13102
25. Sharpe, RA, Bearman, N, Thornton, CR, Husk, K, and Osborne, NJ. Indoor fungal diversity and asthma: a meta-analysis and systematic review of risk factors. J Allergy Clin Immunol. (2015) 135:110–22. doi: 10.1016/j.jaci.2014.07.002
26. Sun, Y, Cui, L, Hou, J, Luo, S, Norback, D, and Sundell, J. Role of ventilation and cleaning for controlling house dust mite allergen infestation: A study on associations of house dust mite allergen concentrations with home environment and life styles in Tianjin area, China. Indoor Air. (2022) 32:e13084. doi: 10.1111/ina.13084
27. Brusselle, GG, and Ko, FW. Prevalence and burden of asthma in China: time to act. Lancet. (2019) 394:364–6. doi: 10.1016/S0140-6736(19)31349-2
28. McFadden, JP, White, IR, Frosch, PJ, Sosted, H, Johansen, JD, and Menne, T. Allergy to hair dye. BMJ. (2007) 334:220. doi: 10.1136/bmj.39042.643206.BE
29. Moscato, G, Pignatti, P, Yacoub, MR, Romano, C, Spezia, S, and Perfetti, L. Occupational asthma and occupational rhinitis in hairdressers. Chest. (2005) 128:3590–8. doi: 10.1378/chest.128.5.3590
30. Helaskoski, E, Suojalehto, H, Virtanen, H, Airaksinen, L, Kuuliala, O, Aalto-Korte, K, et al. Occupational asthma, rhinitis, and contact urticaria caused by oxidative hair dyes in hairdressers. Ann Allergy Asthma Immunol. (2014) 112:46–52. doi: 10.1016/j.anai.2013.10.002
31. Haltia, T, Jungewelter, S, Airaksinen, L, Suomela, S, Lindstrom, I, and Suojalehto, H. Occupational asthma, rhinitis, and contact urticaria from indigo (Indigofera tinctoria) hair dye. J Allergy Clin Immunol Pract. (2021) 9:3500–2. doi: 10.1016/j.jaip.2021.04.047
32. Kumar, P, and Ram, U. Patterns, factors associated and morbidity burden of asthma in India. PLoS One. (2017) 12:e0185938. doi: 10.1371/journal.pone.0185938
33. Peters, U, Dixon, AE, and Forno, E. Obesity and asthma. J Allergy Clin Immunol. (2018) 141:1169–79. doi: 10.1016/j.jaci.2018.02.004
34. Beuther, DA, and Sutherland, ER. Overweight, obesity, and incident asthma: a meta-analysis of prospective epidemiologic studies. Am J Respir Crit Care Med. (2007) 175:661–6. doi: 10.1164/rccm.200611-1717OC
35. Anto, JM, Sunyer, J, Basagana, X, Garcia-Esteban, R, Cerveri, I, de Marco, R, et al. Risk factors of new-onset asthma in adults: a population-based international cohort study. Allergy. (2010) 65:1021–30. doi: 10.1111/j.1398-9995.2009.02301.x
36. Fazlollahi, MR, Najmi, M, Fallahnezhad, M, Sabetkish, N, Kazemnejad, A, Bidad, K, et al. The prevalence of asthma in Iranian adults: the first national survey and the most recent updates. Clin Respir J. (2018) 12:1872–81. doi: 10.1111/crj.12750
37. Garcia-Larsen, V, Del Giacco, SR, Moreira, A, Bonini, M, Charles, D, Reeves, T, et al. Asthma and dietary intake: an overview of systematic reviews. Allergy. (2016) 71:433–42. doi: 10.1111/all.12800
38. Patel, BD, Welch, AA, Bingham, SA, Luben, RN, Day, NE, Khaw, KT, et al. Dietary antioxidants and asthma in adults. Thorax. (2006) 61:388–93. doi: 10.1136/thx.2004.024935
39. Shaheen, SO, Sterne, JA, Thompson, RL, Songhurst, CE, Margetts, BM, and Burney, PG. Dietary antioxidants and asthma in adults: population-based case-control study. Am J Respir Crit Care Med. (2001) 164:1823–8. doi: 10.1164/ajrccm.164.10.2104061
40. Romieu, I, Varraso, R, Avenel, V, Leynaert, B, Kauffmann, F, and Clavel-Chapelon, F. Fruit and vegetable intakes and asthma in the E3N study. Thorax. (2006) 61:209–15. doi: 10.1136/thx.2004.039123
41. Garcia, V, Arts, IC, Sterne, JA, Thompson, RL, and Shaheen, SO. Dietary intake of flavonoids and asthma in adults. Eur Respir J. (2005) 26:449–52. doi: 10.1183/09031936.05.00142104
42. Yang, W, Yang, Y, He, L, Zhang, M, Sun, S, Wang, F, et al. Dietary factors and risk for asthma: A Mendelian randomization analysis. Front Immunol. (2023) 14:e1126457. doi: 10.3389/fimmu.2023.1126457
43. Caramori, G, and Papi, A. Oxidants and asthma. Thorax. (2004) 59:170–3. doi: 10.1136/thorax.2002.002477
Keywords: asthma, damp and musty, living time, hair dyeing, education years
Citation: Chen M, Zhang K, Zhang X, Gao J, Zhang R, Wei X and Cao W (2023) Association between living habits, indoor humidity, ventilation and asthma among residents in the tropical regions of China. Front. Public Health. 11:1294115. doi: 10.3389/fpubh.2023.1294115
Edited by:
Jianbang Xiang, Sun Yat-sen University, ChinaReviewed by:
Penpatra Sripaiboonkij, University College Dublin, IrelandAhmed Samour, Near East University, Cyprus
Copyright © 2023 Chen, Zhang, Zhang, Gao, Zhang, Wei and Cao. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Rongguang Zhang, enJnQHp6dS5lZHUuY24=; Xiaoli Wei, eGlhb2xpQGhhaW5tYy5lZHUuY24=; Wenting Cao, Q2Fvd2VudGluZ0BoYWlubWMuZWR1LmNu
†These authors have contributed equally to this work and share first authorship
 Mingming Chen
Mingming Chen Kun Zhang2†
Kun Zhang2† Rongguang Zhang
Rongguang Zhang Xiaoli Wei
Xiaoli Wei Wenting Cao
Wenting Cao