- 1Centre for Palliative and Cancer Care in Conflict (CPCCC), King Hussein Cancer Centre (KHCC), Amman, Jordan
- 2Centre of Research Shared Resources, King Hussein Cancer Centre (KHCC), Amman, Jordan
- 3Faculty of Medicine, The University of Jordan, Amman, Jordan
- 4Florence Nightingale Faculty of Nursing, Midwifery and Palliative Care, King’s College London, Cicely Saunders Institute, London, United Kingdom
- 5Faculty of Health Sciences, Cancer Care and Epidemiology, Queen's University, Kingston, ON, Canada
- 6Institute of Cancer Policy, King’s College London, London, United Kingdom
- 7Nursing Department, King Hussein Cancer Center, Amman, Jordan
- 8Director General’s Office, King Hussein Cancer Center, Amman, Jordan
- 9Department of Palliative Care, King Hussein Cancer Centre (KHCC), Amman, Jordan
Background: The coronavirus pandemic has potential implications for stress levels and resilience among oncology healthcare professionals (HCPs). This study aims to assess perceived stress, resilience, and moral distress levels among oncology HCPs in Jordan during the pandemic and identify associated risk factors.
Methods: An online cross-sectional survey was conducted among oncology HCPs in Jordan using three validated tools: Perceived Stress Scale (PSS), Connor-Davidson Resilience Scale (CD-RSIC), and Moral Distress Thermometer (MDT). Seven items were used to assess sources of stress.
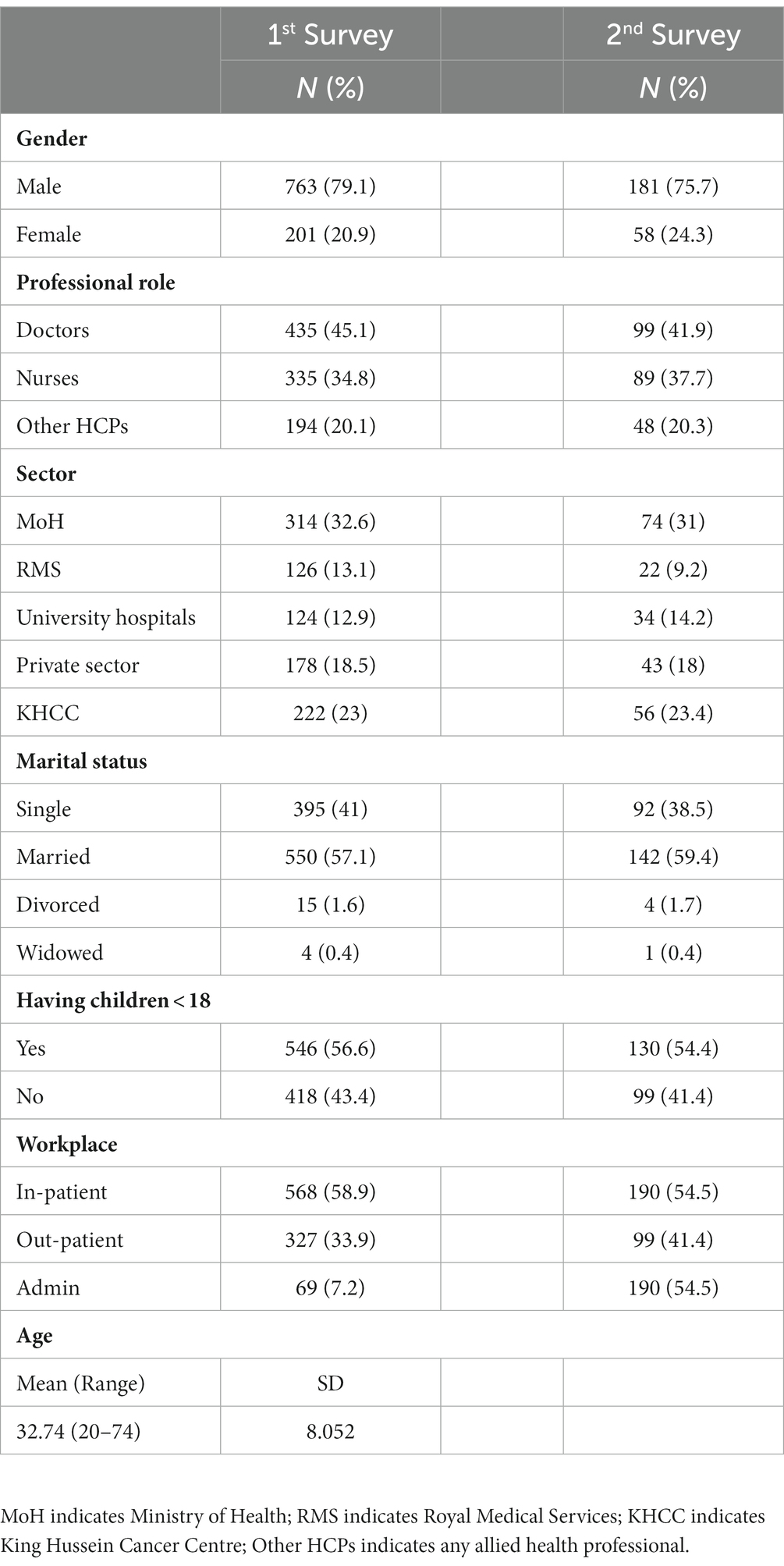
Results: A total of 965 participants enrolled with a 74% response rate. The participants’ ages ranged from 20 to 74 (mean = 32.74, SD = 5.197), with 79.1% males, 45.1% were physicians, 32.6% were public hospital workers, 57.1% were married, and 56.6% had children below 18 years. Findings indicated moderate perceived stress (Mean = 15.87, SD = 5.861), low resilience (Mean = 29.18, SD = 5.197), and high moral distress (Mean = 4.72, SD = 2.564). Females, unmarried individuals, and younger age groups exhibited higher PSS (p = 0.009, p < 0.001, and P<0.001) and lower resilience (p = 0.024, p = 0.034, and p = 0.001). Not having children below 18 years correlated with higher perceived stress (P < 0.001). In linear regression analysis, age and gender emerged as significant predictors of both perceived stress and resilience. Female participants reported stress related to the risk of contracting COVID-19 (p = 0.001), transmitting it to others (p = 0.017), social isolation (P < 0.001), and having children at home due to school closures (p = 0.000). A cohort of 239 participants repeated the survey within a two-month interval, revealed a statistically significant decrease in the CD-RISC scores (p < 0.001).
Conclusion: Oncology HCPs in Jordan experienced moderate stress, high moral distress, and poor resilience during the COVID-19 pandemic. These factors may negatively affect the quality of oncology care. Urgent measures are necessary to support HCPs in coping with unforeseen circumstances in the future.
1 Introduction
1.1 Overview of the COVID-19 situation in Jordan
Jordan, which was recently downgraded as a lower-middle-income country at the close of 2022 (1), boasted a population of 11,285,869 (2). The demographic landscape in Jordan skews towards a predominantly youthful population. In 2021, approximately 71% of the inhabitants fell within the age bracket of 15–65; while a 3.7% were aged 65 and older (3). Jordan’s experience with COVID-19 has seen several waves and government responses. The first case emerged in March 2020, with initial success in containment. However, by October 2020, the first wave hit, peaking in November with over 26,000 cases and 468 deaths (4). The virus was initially contained in refugee camps, with a high recovery rate among affected refugees (5). Recovery began in May 2021, with low daily cases until November when a third wave occurred, peaking in December 2021 with 34,735 cases and 226 deaths. Despite these waves (4), intensive care unit capacity remained manageable (6).
In January 2022, Jordan faced a fourth wave, with a significant portion linked to the Omicron variant. By February 2022, Jordan reported 1,490,473 cases and 13,532 deaths (4), but ICU and ventilator occupancy remained below alarming levels (6).
Jordan’s response to COVID-19 has been characterized by proactive measures, vaccination campaigns, and policies aimed at restoring normalcy while managing the evolving challenges of the pandemic. Early on, safety measures were implemented, including quarantine, lockdowns, and curfews (7, 8). A vaccination campaign began in January 2021, prioritizing high-risk groups (9). By June 2021, over 2 million adults received the first dose, with additional funding from international partners to accelerate vaccination efforts, including refugees (10).
1.2 Understanding COVID-19 impact on healthcare providers
Healthcare providers (HCPs) worldwide have faced numerous challenges and stressors in response to the COVID-19 pandemic since its initial outbreak in China in December 2019 (11, 12). These challenges and stressors are often related to patient care, including limited healthcare resources, difficulties in providing the usual level of care, and patients being isolated without family support. Additionally, HCPs may experience work-related stressors such as long working hours, frequent policy and guideline changes related to COVID-19, uncertainty regarding protocols, and fear of infection, especially when there is insufficient protective equipment. Furthermore, HCPs may encounter additional challenges due to social isolation, lockdowns, and the need to care for their own children at home due to school closures (11–13).
The specific challenges faced by HCPs can vary depending on their involvement in the care of COVID-19 patients. For instance, frontline and intensive care unit HCPs may experience higher levels of stress and challenges compared to others (14, 15). Moreover, HCPs involved in cancer care may face additional and significant challenges that are compounded by pandemic-related issues such as medication and HCP shortages. Healthcare systems need to carefully balance the benefits of providing cancer treatment against the risk of COVID-19 transmission in the hospital environment, taking into account the vulnerability of cancer patients with compromised immunity (16).
Various studies have examined stress levels and mental well-being among HCPs in stable environments using different assessment tools. For example, Abraham et al. (17) assessed stressors, morale, and coping mechanisms among staff working in emergency units. Magnavita et al. (18) examined mental and physical well-being in cancer units using the needs questionnaire and positivity scale. While several studies have explored stressors in rapidly evolving environments like COVID-19, William and Lancee (19) found that HCPs reported long-term stress during the SARS outbreak but their mental status remained unaffected. These studies have contributed to the development of strategies to enhance resilience and reduce stress by promoting safety measures, comfort, and social connections (20).
Marjanovic et al. (20) conducted an online survey among 333 nurses to assess the association of the working environment with psychosocial variables. The study focused on predictors of coping attitudes, emotional exhaustion, and anger using validated tools such as the State–Trait Anger Expression Inventory and the Maslach Burnout Inventory. Results showed that lower emotional exhaustion levels were predicted by higher institutional support, less contact with SARS patients, and shorter quarantine times. Maunder et al. (21) surveyed staff members from 13 hospitals in Toronto, Canada, to assess the impact of SARS on their psychological and occupational well-being 13–26 months after the outbreak. The study revealed higher levels of stress and burnout among staff working in SARS treatment hospitals, reduced working hours, and stress-related behavioral consequences.
In their study, Motahedi et al. (22) underscored the significance of addressing the mental health challenges encountered by HCPs during the COVID-19 pandemic. They conducted an investigation involving 140 HCPs in an urban region of Iran. The findings revealed the presence of moderate anxiety levels alongside concurrent moderate to severe depression among the HCPs. Notably, gender, a history of COVID-19-related quarantine, and previous exposure to COVID-19 were identified as factors associated with elevated levels of both anxiety and depression. Given that working in institutions treating COVID-19 patients may expose HCPs to stress and mental health issues, it is important to identify potential stressors and challenges specific to oncology HCPs in Jordan. Tracking changes over time can provide preliminary baseline data to inform future policies and studies, particularly considering the scarcity of research in this area in Jordan. The objectives of this survey are: (1) to describe the impact of COVID-19 on oncology HCPs in Jordan by assessing self-reported perceived stress levels, resilience, and moral distress, (2) to compare these findings within different HCP groups (e.g., nurses vs. doctors, ambulatory vs. in-patient care), and (3) to conduct longitudinal assessments of these mental wellness dimensions over time as the COVID-19 environment evolves.
2 Materials and methods
2.1 Study design and participants
The study employed a cross-sectional survey with a longitudinal assessment to quantify perceived stress, its sources, resilience, and moral distress among oncology healthcare professionals (HCPs) in Jordan. Data collection was conducted using the Survey Monkey platform from November 9, 2020, to April 28, 2021. The study included frontline HCPs (e.g., doctors, nurses, pharmacists, psychosocial workers) who worked full-time or part-time during the pandemic in COVID-19-designated hospitals in Jordan, encompassing in-patient, ambulatory, and administrative care settings. HCPs who did not work in COVID-19-designated hospitals, did not work at least part-time during the pandemic, or were on vacation were excluded from the study.
2.2 Data collection
Data was collected through a structured survey instruments that incorporated both validated psychological scales and demographic information. The data collection process aimed to capture the experiences and mental well-being of oncology HCPs in Jordan during the COVID-19 pandemic.
2.3 Data collection instruments
2.3.1 Perceived Stress Scale (PSS-10)
The PSS is a validated self-reported tool used to measure stress levels in individuals who perceive their lives to be unpredictable, uncontrollable, and burdensome over the past month (23). Originally introduced in 1983 by Cohen and colleagues (23), where the PSS initially comprised 14 items. Participants are required to rate the frequency of their experiences of emotions and thoughts associated with life events and situations over the preceding month using a five-point scale, ranging from (0) “Never” to (4) “Very Often.” The cumulative score derived from the PSS serves as a comprehensive measure of perceived stress. A short version of the PSS (PSS-10) was developed by Cohen and Williamson (24) in 1988. This adaptation was created by excluding four items with the lowest factor loadings from the original scale. The psychometric characteristics of the PSS-10 were initially assessed in a large national sample in the United States. The PSS-10 demonstrated satisfactory internal consistency reliability (α = 0.78). Furthermore, moderate concurrent criterion validity, as indicated by significant positive correlations with the level of stress experienced during an average week (r = 0.39, p < 0.001) and the frequency of stressful life events in the past year (r = 0.32, p < 0.001). Additionally, it exhibited adequate convergent validity, as evidenced by its associations with measures of both physical and mental health. The developers endorsed the use of the PSS-10 in future research due to its comparable psychometric properties with the original version. Furthermore, subsequent studies consistently reaffirmed these findings (25–27).
The scale consists of 4 positively worded items (4, 5, 7, and 8) and 6 negatively worded items (1, 2, 3, 6, 9, and 10), which are rated on a 5-point Likert scale (0 = never, 1 = almost never, 2 = sometimes, 3 = fairly often, or 4 = very often). The total score ranges from 0 to 40, with scores of 0–13, 14–26, and 27–40 indicating low, moderate, and high levels of stress, respectively (28, 29).
Seven Source of Stress items were added, rated on a 5-point Likert scale (0–4; 0 = not at all stressful, 4 = majorly stressful), to capture responses related to the PSS. These items were designed to assess the significance of each source of stress, including work environment, patient care, personal safety, home life, social isolation, financial toxicity, and having children at home due to school closures.
In our study, we employed both the validated English version (30) and the Arabic versions (31, 32) of the questionnaire.
2.3.2 Connor-Davidson Resilience Scale (CD-RISC-10)
The CD-RISC-10 is a validated self-reported tool used to measure resilience in individuals with post-traumatic stress disorder (PTSD) or other types of anxiety. Derived from the CD-RISC-25 (33), a 25-item scale gauging the ability to cope with adversity, respondents rate items on a five-point scale ranging from 0 (not true at all) to 4 (true nearly all the time) reflecting their feelings and experiences over the course of the past month. The total score ranges from 0 to 40 with higher scores reflecting greater resilience. Preliminary investigations into the psychometric properties of the CD-RISC in both the general population and patient samples have substantiated its internal consistency, test–retest reliability, and convergent and divergent validity (33). In a study conducted by Campbell-Sills and Stein (34), the psychometric properties of the CD-RISC-25 were examined. Their research identified an unstable factor structure in the CD-RISC across two equivalent samples via exploratory factor analysis (EFA). Following a series of modifications, a 10-item unidimensional scale was developed, exhibiting robust internal consistency and construct validity. Multiple study’s results underscore the excellent psychometric qualities of the 10-item version, affirming its reliability as a tool for assessing resilience (35–37). The new version uses a five-point scale (0–4). The total score ranges from 0 to 40, with score ranges of 0–29, 30–32, 33–36, and 37–40, indicating lower to higher levels of resilience, with the median score for the general population residing at 32 (38). In our study, we employed the original English version (34) and the validated Arabic version (39) of the questionnaire.
2.3.3 Moral Distress Thermometer (MDT)
Moral distress refers to distress experienced when individuals know the morally right thing to do but are unable to do so due to perceived obligations (40, 41). In their study, Wocial and Weaver (42) initially developed and assessed the psychometric properties of a novel tool designed for detecting moral distress, referred to as the Moral Distress Thermometer (MDT). In their cross-sectional investigation, they presented compelling evidence supporting the MDT’s validity as a subjective measure of moral distress among HCPs when compared to the more comprehensive Moral Distress Scale (MDS) 2009. The validation process of the MDT involved its comparison with the more extensive Moral Distress Scale (MDS) 2009, a tool specifically designed for assessing moral issues (43). The MDT utilizes an 11-point scale, spanning from 0 to 10, along with associated verbal descriptors. Respondents are required to rate the level of moral distress they have experienced in relation to their work over the past 2 weeks. The study findings indicated a moderate correlation between the MDT and the MDS 2009, thereby confirming convergent validity. Concurrent validity was established by comparing MDT scores among different groups of nurses based on their experiences with leaving positions due to moral distress, and these results were consistent with the findings obtained using the MDS 2009. Given the dynamic and subjective nature of moral distress, the authors determined that reliability testing for the MDT was impractical. In our study, Participants are asked to circle the number that best describes the extent to which they experienced work-related moral distress over the past 2 weeks. A score of 4 and above indicates high moral distress. Both the validated English (42) and Arabic (44) versions were used.
In response to the rapidly evolving pandemic circumstances, we made the decision to shorten the recall period to 7 days (45). This adjustment aimed to capture immediate and contextually relevant stressors and experiences encountered by HCPs in their demanding roles within the healthcare system. Given that the importantly, we maintained this consistent 7-day recall period for HCPs in both the initial and subsequent survey waves. This deliberate approach enabled us to longitudinally evaluate stress level, resilience and moral distress while taking into account the dynamic nature of the pandemic’s impact on HCPs.
2.3.4 Socio-demographic data
Socio-demographic data included gender (male or female), occupation (e.g., doctor, nurse, other HCP), age group (≤ 33, > 33), marital status, having children below the age of 18, workplace (in-patient, out-patient, administration), and health sector (MOH, RMS, Private Sector, University hospitals, KHCC).
2.4 Measurement translation
Systematic and culturally sensitive translations of the three validated measurements into Arabic for use in the context of Jordan, This comprehensive process strictly adhered to the EORTC (European Organisation for Research and Treatment of Cancer) translation procedures (46). This involved independent forward translations by two bilingual speakers with End-of-Life Care (EoLC) knowledge, professional back translation, and harmonization of all versions.
Then, we systematically compared our reconciled Arabic version with the Arabic-validated questionnaires for PSS, CD-RISC and MDT. This meticulous comparison revealed that there were no disparities between our translated versions and the established and validated Arabic tools designed for these measurements. Consequently, we decided to utilize the three previously validated Arabic versions of the questionnaires (PSS-10, CD-RISC-10, and MDT).
2.5 Data collection procedure
The survey was primarily conducted through an online survey platform to ensure participant anonymity and safety during the pandemic. Participants were provided with secure links to the surveys, which were accessible on various devices. The survey was available in Arabic and English language to accommodate the diverse backgrounds of the participants. The eligible participants were identified and contacted by their managers, who informed them about the voluntary nature of participation and clarified that their decision would not affect their performance evaluation. Subsequently, the participants received an invitation and a survey information letter via their official emails. Interested participants contacted the research team, and those who wished to participate or obtain more information were provided with a survey link via their official emails.
A follow-up assessment was performed on a subsample of participants who agreed to repeat the measurement within 2 months of the initial survey to evaluate changes in their responses to the three validated tools over time.
2.6 Ethical considerations
Data collection was carried out in a structured and standardized manner. All participants provided informed consent before participating in the study. And were explicitly informed that their consent was implied by reading the survey information letter and completing the survey. They were also assured that they could withdraw from the study at any time without providing a reason until they submitted their completed questionnaires, after which data withdrawal would not be possible.
Ethical approval for the study protocol, including data collection procedures, was obtained from the Institutional Review Board at the King Hussein Cancer Centre (KHCC) under the reference number EC/Ref No: 20 KHCC 123.
2.7 Statistical analysis
2.7.1 Sample size estimation
In this study, we employed the Krejcie and Morgan table (47), a well-established and widely accepted method for estimating survey sample sizes. This approach prescribes a minimum sample size of 384 respondents to ensure adequate representation and randomness when dealing with a population size of 10,000.
2.7.2 Statistics
Data were collected using Survey Monkey and exported to SPSS software (V.26) for analysis. Missing data of no more than 10% were accepted by the research team using the Pairwise deletion approach. The responses were analyzed and summarized, and correlations were run with the answered items, resulting in different sample sizes per item.
The significance level was set at p < 0.05. The original scores of the three validated tools were presented as mean with standard deviation. The ranked data derived from the counts of each level for PSS, CD-RISC, and MDT were presented as numbers and percentages, likely indicating the distribution of responses across different levels. Independent t-tests and one-way ANOVA tests were used to find associations between different variables such as gender, age group, marital status, professional role, workplace, health sector, and having children below the age of 18. A paired t-test was performed in a subsample to evaluate responsiveness to change. Variables that showed significance in the analysis were entered into linear regression model. Adjusted p-values were reported, indicating the significance of each variable while controlling for the influence of other variables in the model.
3 Results
A total of 1,310 healthcare professionals (HCPs) participated in the survey, with 965 completing the initial survey, resulting in a response rate of 74%. Among these respondents, 340 expressed their willingness to participate in a follow-up survey within 2 months, and 239 completed the second survey.
3.1 Participant characteristics
Participant characteristics revealed that the majority of participants were male (763, 79.1%). The mean age was 32.74 years (range: 20–74). Among the participants, 435 (45.1%) were doctors, 314 (32.6%) worked in Ministry of Health Hospitals, 550 (57.1%) were married, 546 (56.6%) had children below the age of 18, and 568 (58.9%) worked in an in-patient care setting (Table 1).
3.2 Outcome measurements
Figure 1 summarizes the scores for the Perceived Stress Scale (PSS), Connor-Davidson Resilience Scale (CD-RSIC), and Moral Distress Thermometer (MDT) over 25 weeks. The mean scores were 15.87 for PSS, 29.18 for resilience, and 4.72 for MDT.
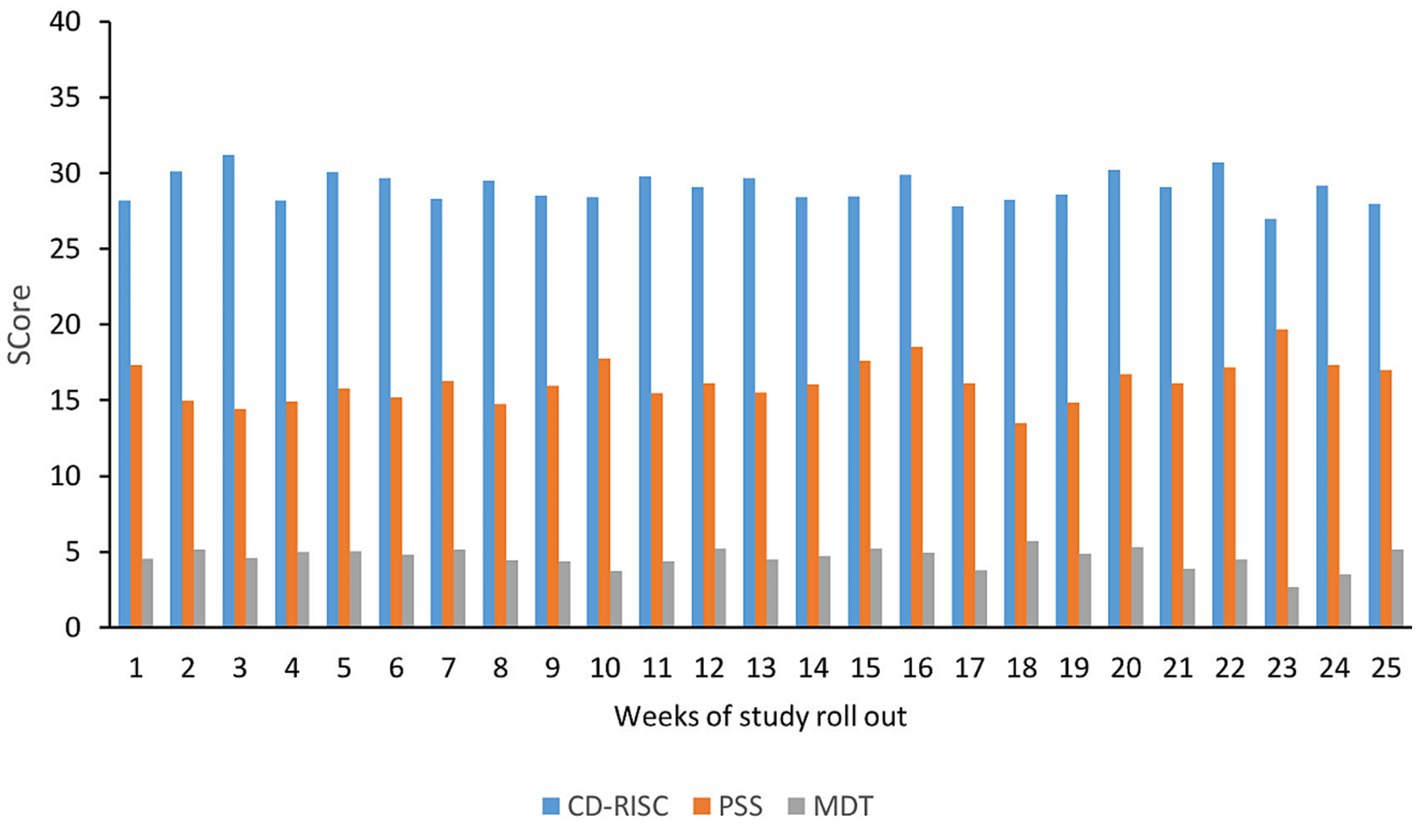
Figure 1. PSS, CD-RISC, and MDT scores in the initial survey: the figure illustrates the Perceived Stress Scale (PSS), Connor-Davidson Resilience Scale (CD-RISC), and Moral Distress Thermometer (MDT) scores on the vertical axis. The horizontal axis represents the week of the study rollout. PSS scores are categorized as low (0–13), moderate (14–26), and high (27–40) levels of stress. CD-RISC scores range from 0 to 29, 30 to 32, 33 to 36, and 37 to 40, with higher scores indicating greater resilience levels. MDT scores range from 0 to 10, with a score of 4 and above indicating high moral distress.
3.2.1 The Perceived Stress Scale (PSS)
The analysis using the Perceived Stress Scale (PSS) indicated that being female (p = 0.009), unmarried (p = 0.001), having no children below the age of 18 (p = 0.000), and being younger (p < 0.001) were significantly associated with higher PSS scores. However, occupation (p = 0.254), health sector (p = 0.637), and workplace (p = 0.357) did not have a significant impact on PSS scores. In the summary linear regression analysis involving independent variables and PPS-10 scores, it was observed that gender and age emerged as significant predictors for PPS-10, with p = 0.002 and p < 0.001, respectively (Table 2).

Table 2. Participants’ characteristics with respect to the three validated tools of the first survey.
3.2.1.1 Source of stress
The sources of stress were categorized as follows: “Not at all stressful” or “Almost never stressful” (indicating minor stress), “Sometime stressful” (indicating moderate stress), and “Fairly often stressful” or “A major cause of stress” (indicating major stress).
3.2.1.2 Gender
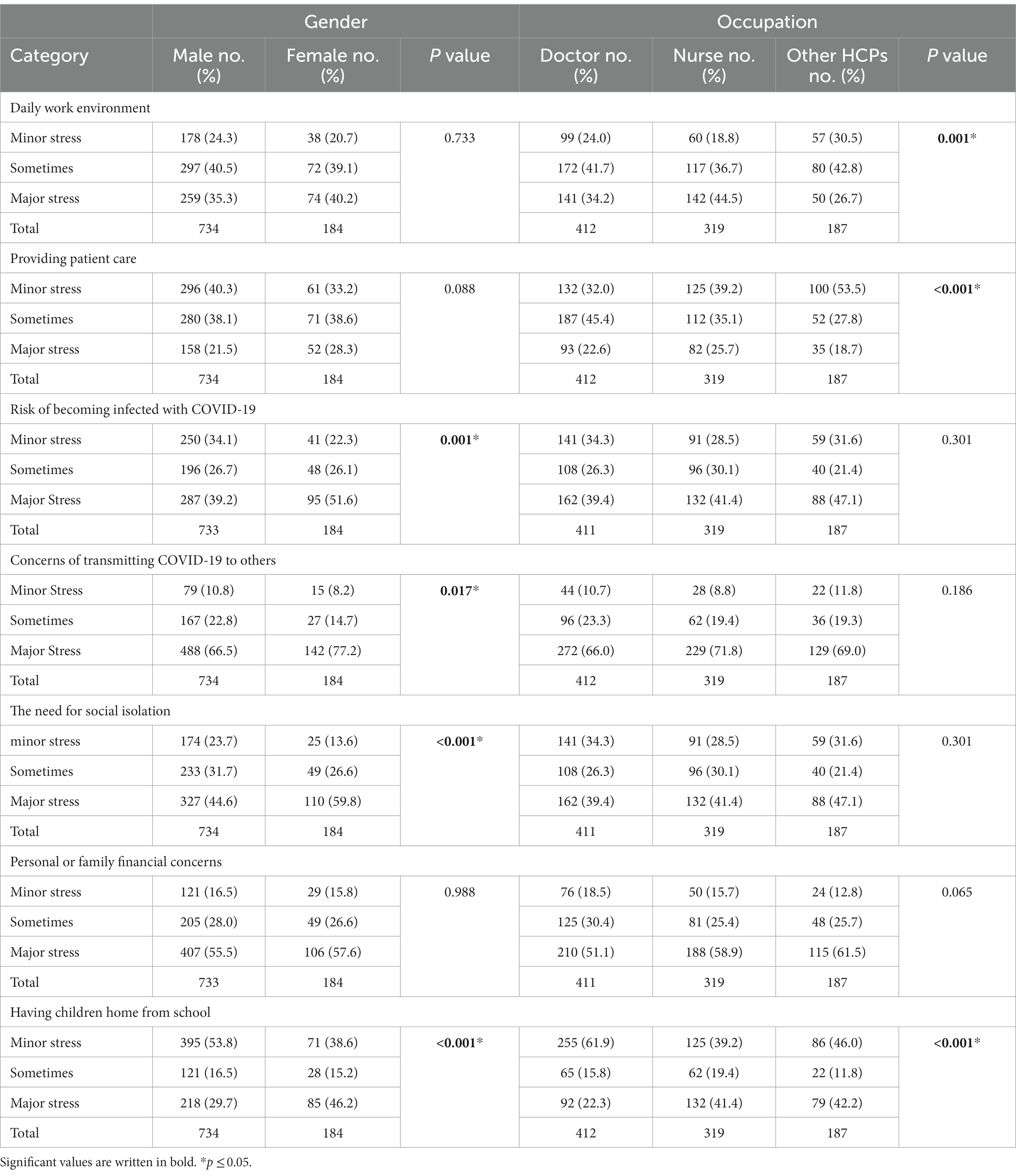
Significant associations were observed between gender and sources of stress. Females reported higher levels of major stress from the imposed social isolation (59.7% vs. 44.5% for males, p = 0.000), the risk of contracting COVID-19 (51.6% vs. 39.2% for males, p = 0.001), the risk of transmitting COVID-19 to others (77.2% vs. 66.2% for males, p = 0.017), and having children home from school (46.2% vs. 29.7% for males, p = 0.000). No significant association was found between gender and stress related to providing patient care (p = 0.088), the daily work environment (p = 0.733), or personal or familial financial concerns (p = 0.988) (Table 3).
3.2.1.3 Occupation
Profession (doctors, nurses, and other HCPs) also showed a significant correlation with certain sources of stress. Other HCPs reported minor stress from providing patient care more frequently (53.0% vs. 39.2% for nurses and 32.1% for doctors, p = 0.000). Nurses demonstrated higher levels of major stress from the daily work environment compared to doctors and other HCPs (44.5% vs. 34.3% for doctors and 26.7% for other HCPs, p = 0.001). Other HCPs showed minor stress from the need for social isolation more frequently (55.6% vs. 42.3% for doctors and 49.8% for nurses, p = 0.023). Doctors reported minor stress from having children home from school more often (61.9% vs. 46.0% for other HCPs and 39.2% for nurses, p = 0.000).
However, the model did not show a significant association between occupation and other sources of stress, such as the risk of contracting COVID-19 (p = 0.301), transmitting COVID-19 to others (p = 0.186), or personal or familial financial concerns (p = 0.065) (Table 3).
3.2.2 The Connor-Davidson Resilience Scale (CD-RISC)
Resilience significantly decreased in females (p = 0.024), unmarried individuals (p = 0.034), and those of younger age (p = 0.001). However, occupation (p = 0.494), health sector (p = 0.114), having children below the age of 18 (p = 0.440), and workplace (p = 0.907) did not show any significant effects on resilience. In the summary of the linear regression analysis that incorporated independent variables alongside CD-RISC-10 scores, both gender and age emerged as statistically significant predictors for CD-RISC-10, with p-values of 0.01 and p = 0.020, respectively (Table 2).
3.2.3 The Moral Distress Thermometer (MDT)
Throughout the entire survey period of 25 weeks, no statistically significant relationship was observed between the participants’ demographic characteristics and the levels of perceived moral distress (Table 2).
3.2.4 Paired data
The statistical model revealed a significant decline only in the CD-RISC scores (p < 0.001) for participants in the second survey, while other outcomes remained unaffected (Figure 2).
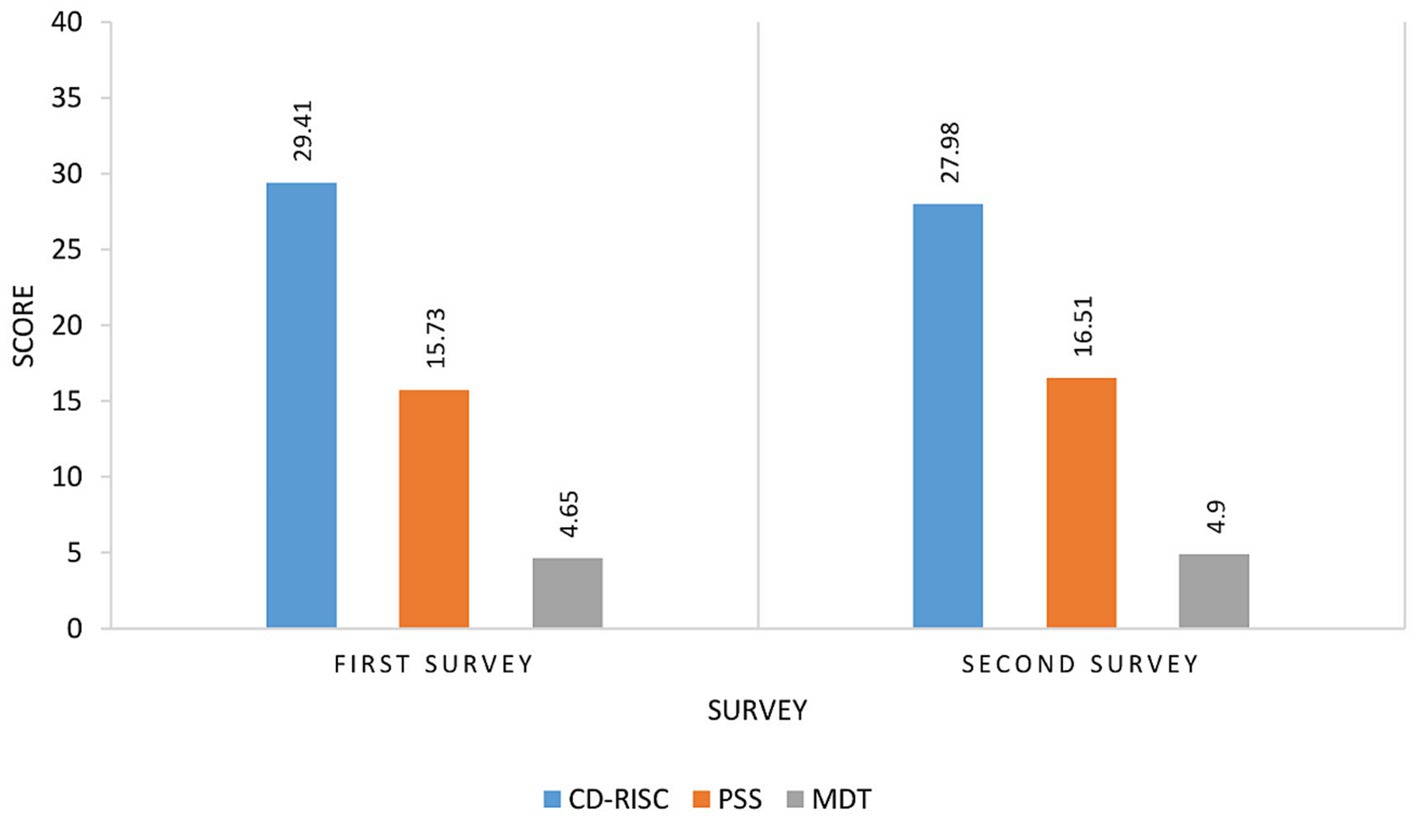
Figure 2. Comparison of CD-RISC, PSS, and MDT between Paired Sample (n = 239). PSS, Perceived Stress Scale; CD-RISC, Connor-Davidson Resilience Scale; MOT, The Moral Distress Thermometer. The scores of CD-RISC, PSS, and MDT are shown on the vertical line, and the horizontal line represents the paired surveys during the study roll-out. The PSS scores range from 0 to 13, 14 to 26, and 27 to 40, indicating low, moderate, and high stress levels, respectively. The CD-RISC scores range from 0 to 29, 30 to 32, 33 to 36, and 37 to 40, with a higher score indicating higher resilience. The MDT scores range from 0 to 10, with a score of 4 and above indicating high moral distress.
4 Discussion
In the midst of the COVID-19 pandemic, healthcare professionals (HCPs) have faced unprecedented challenges that have significantly impacted their mental well-being. The present study aimed to assess the impact of the COVID-19 pandemic on the stress, resilience, and moral distress levels of healthcare professionals (HCPs) in Jordan over a period of 25 weeks.
The findings of the study indicate that oncology HCPs in Jordan reported moderate levels of perceived stress, low resilience, and high levels of perceived moral distress. These results are consistent with previous studies conducted during the COVID-19 pandemic (11, 12, 48, 49). The waves and peaks of the pandemic in Jordan between 2020 and 2021 likely contributed to the sustained levels of stress and distress experienced by the participants (50).
The Perceived Stress Scale (PSS) scores indicated that being female (22), unmarried (51–57), having no children below the age of 18 (51, 54), and being younger (56, 58–62) were significantly associated with higher stress levels. This aligns with previous research that has shown females and younger individuals experiencing higher stress levels during the pandemic due to factors like increased caregiving responsibilities, work demands, and concerns about personal health and safety (22, 54, 63–65). However, the lack of significant association between occupation groups, health sector, and workplace with stress scores is surprising (52, 55, 66–69). Indicating that the pandemic’s stressors were pervasive across various healthcare professions and settings (66). These findings suggest that the mental well-being of all HCPs should be prioritized, irrespective of their specific roles, and targeted interventions should be implemented to provide adequate support (22).
The sources of stress reported by the participants also showed interesting patterns. Females experienced higher stress levels related to social isolation, the risk of contracting and transmitting COVID-19 (13, 22, 54, 70–73), and having children home from school. This could be attributed to gender-specific societal expectations, such as women shouldering more responsibilities related to caregiving and household tasks during the pandemic (13, 22, 70, 71, 74).
However, stress related to patient care, the daily work environment, and financial concerns was not differentiated by gender (54).
Occupation was also linked to specific stressors such as patient care, the work environment, social isolation, and having children at home (54). While other HCPs reported more stress from providing patient care, Frontline healthcare professionals such as nurses experienced higher stress from the daily work environment, which could be linked to their direct patient care responsibilities and exposure to stressful healthcare settings (13, 57, 75–77). These findings shed light on the unique stressors faced by nurses during the pandemic. Addressing these stressors through targeted interventions, such as mental health support and flexible work arrangements, may be essential in reducing their stress levels and improving overall well-being (13). Although the results did not indicate a statistically significant difference in the Perceived Stress Scale (PSS) scores among HCPs groups regarding stress from personal or family financial concerns, it is worth mentioning that a considerable proportion of them rated it as a major source of stress. This contrasts with the findings of a recent Italian study (54). Its likely influenced by the negative economic impact on families and the national economy (78). The finding that doctors reported more stress from having children home from school is surprising and warrants further investigation. These findings underscore the importance of recognizing the distinct challenges faced by different healthcare professionals and customizing support mechanisms accordingly.
Resilience, as measured by the Connor-Davidson Resilience Scale (CD-RISC), although the participants reported low resilience levels in both surveys, which were below the average resilience score of the general population (38). The decline in resilience scores for participants in the second survey is a noteworthy finding. It suggests that prolonged exposure to the challenges of the pandemic may have eroded participants’ resilience over time, potentially leaving them more vulnerable to stress and burnout (11, 54). The lack of significant changes in stress and moral distress levels may indicate that these factors are relatively stable over the 25-week period or that other external factors such as direct patient care, and the absence of effective vaccines or drugs during the study period may have contributed to a decrease in resilience among HCPs (79).
The Connor-Davidson Resilience Scale (CD-RISC) also showed a significant decline in females, unmarried individuals, and younger participants (56, 58–62). This suggests that certain demographic groups may be more vulnerable to decreased resilience during the pandemic, which could have implications for their mental health and coping abilities (80).
Contrary to some studies, no significant relationship was found between the participants’ demographic characteristics and perceived moral distress levels (52, 55, 67–69), indicating that moral distress may be a universal experience among healthcare professionals during the pandemic, irrespective of their individual characteristics. This highlights the collective challenges faced by healthcare professionals in navigating ethical dilemmas and moral concerns during times of crisis (67–69).
The longitudinal analysis highlighted a significant decline in resilience scores over time. This finding emphasizes the need for continuous mental health support and interventions to sustain HCPs’ well-being throughout the prolonged duration of the pandemic. Implementing resilience-building programs and providing resources for stress management can aid in mitigating potential long-term effects on HCPs’ mental health.
Furthermore, the lack of significant changes in stress and moral distress levels over the two-time point test may indicate that these factors are relatively stable over the 25-week period or that other external factors are compensating for the effects of the pandemic on these outcomes.
5 Strengths and limitations
The study had several strengths. First, it included a substantial sample size of 965 healthcare professionals, which enhances the representativeness of the findings. Second, a longitudinal design was employed, allowing for the examination of changes in perceived stress, resilience, and moral distress over time, providing valuable insights into the evolving psychological responses during the pandemic. Third, validated tools were used to measure perceived stress, resilience, and moral distress, increasing the reliability and validity of the study findings.
However, there were also limitations to consider. The initial survey had a cross-sectional design, limiting the ability to establish causal relationships and providing only a snapshot of participants’ psychological responses. Self-report measures were utilized, which may be influenced by response biases such as social desirability bias, potentially affecting the accuracy of reported levels of stress, resilience, and moral distress. The study focused on healthcare professionals in COVID-19-designated hospitals in Jordan, potentially limiting the generalizability of the findings to other healthcare settings or regions. The absence of a control group of healthcare professionals not directly involved in COVID-19 care prevented comparisons and a deeper understanding of the unique stressors and psychological responses associated with the pandemic.
A another limitation of this study is the skewed gender representation, with the majority of participants being male. The low female participation rate may be attributed to cultural and religious factors in Jordanian society, where females may be reluctant to participate in surveys involving direct communication with unrelated males due to cultural norms and preferences for female respondents (81, 82).
Despite these limitations, the study provides valuable insights into the psychological well-being of healthcare professionals during the COVID-19 pandemic. The findings contribute to the existing literature on the subject and highlight the importance of targeted interventions and support strategies to address stress, enhance resilience, and mitigate moral distress among healthcare professionals in similar contexts.
6 Conclusion
This study sheds light on the impact of the COVID-19 pandemic on the stress, resilience, and moral distress levels of healthcare professionals in Jordan. The findings highlight the need for targeted support and interventions for vulnerable groups, such as females, unmarried individuals, and younger professionals, to bolster their resilience and mitigate the negative effects of prolonged stress. Healthcare organizations and policymakers should be aware of the sources of stress experienced by different occupational groups to tailor support measures accordingly and promote the well-being of their frontline workers.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by King Hussein Cancer Center Institutional Review Board. The studies were conducted in accordance with the local legislation and institutional requirements. The ethics committee/institutional review board waived the requirement of written informed consent for participation from the participants or the participants’ legal guardians/next of kin because the survey was conducted over Survey Monkey.
Author contributions
WA: Conceptualization, Data curation, Funding acquisition, Methodology, Project administration, Supervision, Writing – original draft, Writing – review & editing, Formal analysis. GA: Conceptualization, Data curation, Formal analysis, Funding acquisition, Methodology, Project administration, Supervision, Writing – original draft, Writing – review & editing. KA: Formal analysis, Writing – review & editing. AS: Writing – review & editing. RH: Conceptualization, Methodology, Writing – review & editing. CB: Conceptualization, Methodology, Writing – review & editing. RS: Conceptualization, Methodology, Writing – review & editing. MA-r: Project administration, Resources, Validation, Writing – review & editing. AM: Project administration, Resources, Validation, Writing – review & editing. OS: Conceptualization, Formal analysis, Funding acquisition, Methodology, Project administration, Supervision, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. The research is part of the RH4C-MENA project that received funding through a four-year grant (ES/P010962/1) from the Economic and Social Research Council (ESRC) spanning from 2017 to 2021. This financial support was instrumental in facilitating the enhancement of capabilities, the establishment of partnerships, and the execution of research initiatives within the Middle and Near East region, aligning with the project’s overarching objectives.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1 The World Bank . Jordan | Data [Internet]. World Bank National Accounts Data (2022). Available at: https://data.worldbank.org/country/jordan
2 Department of Statistics . Department of Statistics, Jordan [internet]. Department of Statistics web. Available at: https://dosweb.dos.gov.jo/
3 Department of Statistics . Jordan in Figures 2021 [Internet]. 9th ed. Amman: Department of Statistics (Jordan) (2021).
4 WHO . WHO coronavirus disease (COVID-19) dashboard with vaccination data [Internet]. (2022). p. 1–5. Available at: https://covid19.who.int/region/emro/country/jo (Accessed September 24, 2023).
5 UNHCR . Document – Jordan: COVID-19 response (17 March 2021) [internet] (2021). Available at: https://data2.unhcr.org/en/documents/details/85614
6 Xinhua News Agency . Jordan enters 3rd wave of COVID-19 pandemic: Health ministry-Xinhua [internet]. Xinhua. (2021). Available at: https://english.news.cn/20211015/C99FC984F1100001D8311D2D5D201B78/c.html
7 HRW . Jordan: state of emergency declared [Internet]. Human Rights Watch (2020). Available at: https://www.hrw.org/news/2020/03/20/jordan-state-emergency-declared
8 The World Bank (2020). Jordan Economic Monitor – Spring: weathering the storm [internet]. The World Bank Data; p. 1–26. Available at: http://documents.worldbank.org/curated/en/895901594653936142/Jordan-Economic-Monitor-Spring-2020-Weathering-the-Storm
9 Jordan Ministry of Health . Additional financing to the COVID emergency response project stakeholder engagement plan (SEP). (2021)
10 The World Bank . US$63.75 million additional financing to support COVID-19 vaccination in Jordan [Internet]. The World Bank Data (2021). Available at: https://www.worldbank.org/en/news/press-release/2021/06/23/us-63-75-million-additional-financing-to-support-covid-19-vaccination-in-jordan (Accessed February 3, 2022)
11 Banerjee, S, Lim, KHJ, Murali, K, Kamposioras, K, Punie, K, Oing, C, et al. The impact of COVID-19 on oncology professionals: results of the ESMO Resilience Task Force survey collaboration. ESMO Open [Internet]. (2021) 6:100058. doi: 10.1016/j.esmoop.2021.100058
12 Du, J, Dong, L, Wang, T, Yuan, C, Fu, R, Zhang, L, et al. Psychological symptoms among frontline healthcare workers during COVID-19 outbreak in Wuhan. Gen Hosp Psychiatry [Internet]. (2020) 67:144–5. doi: 10.1016/j.genhosppsych.2020.03.011
13 Nikbakht Nasrabadi, A, Abbasi, S, Mardani, A, Maleki, M, and Vlaisavljevic, Z. Experiences of intensive care unit nurses working with COVID-19 patients: a systematic review and meta-synthesis of qualitative studies. Front Public Health. (2022) 10:1034624. doi: 10.3389/fpubh.2022.1034624
14 Billings, J, Ching, BCF, Gkofa, V, Greene, T, Bloomfield, M, Chi Fung Ching, B, et al. Experiences of frontline healthcare workers and their views about support during COVID-19 and previous pandemics: a systematic review and qualitative meta-synthesis. BMC Health Serv Res [Internet]. (2021) 21:1–17. doi: 10.1186/s12913-021-06917-z
15 Han, S, Choi, S, Cho, SH, Lee, J, and Yun, JY. Associations between the working experiences at frontline of COVID-19 pandemic and mental health of Korean public health doctors. BMC Psychiatry. (2021) 21:298. doi: 10.1186/s12888-021-03291-2
16 Datta, SS, Mukherjee, A, Ghose, S, Bhattacharya, S, and Gyawali, B. Addressing the mental health challenges of cancer care workers in LMICs during the time of the COVID-19 pandemic. JCO Glob Oncol [Internet]. (2020) 6:1490–3. doi: 10.1200/GO.20.00470
17 Abraham, LJ, Thom, O, Greenslade, JH, Wallis, M, Johnston, ANNB, Carlström, E, et al. Morale, stress and coping strategies of staff working in the emergency department: a comparison of two different-sized departments. EMA – Emerg Med Australas. (2018) 30:375–81. doi: 10.1111/1742-6723.12895
18 Magnavita, N, Sestili, C, Mannocci, A, Ercoli, E, Boccia, A, Bonaga, G, et al. Mental and physical well-being in oncology-hematology–unit personnel. Arch Environ Occup Heal [Internet]. (2018) 73:375–80. doi: 10.1080/19338244.2017.1361901
19 Lancee, WJ, Maunder, RG, and Goldbloom, DS. Prevalence of psychiatric disorders among Toronto hospital workers one to two years after the SARS outbreak. Psychiatric services. (2008) 59:91–5. doi: 10.1176/ps.2008.59.1.91
20 Marjanovic, Z, Greenglass, ER, and Coffey, S. The relevance of psychosocial variables and working conditions in predicting nurses’ coping strategies during the SARS crisis: an online questionnaire survey. Int J Nurs Stud. (2007) 44:991–8. doi: 10.1016/j.ijnurstu.2006.02.012
21 Maunder, RG, Lancee, WJ, Balderson, KE, Bennett, JP, Borgundvaag, B, Evans, S, et al. Long-term psychological and occupational effects of providing hospital healthcare during SARS outbreak. Emerg Infect Dis. (2006) 12:1924–32. doi: 10.3201/eid1212.060584
22 Motahedi, S, Aghdam, NF, Khajeh, M, Baha, R, Aliyari, R, Bagheri, H, et al. Anxiety and depression among healthcare workers during COVID-19 pandemic: a cross-sectional study. Heliyon [Internet]. (2021) 7:e08570. doi: 10.1016/j.heliyon.2021.e08570
23 Cohen, S, Kamarck, T, and Mermelstein, R. A global measure of perceived stress. J Health Soc Behav. (1983) 24:385–96. doi: 10.2307/2136404
24 Cohen, S, and Williamson, GM. Perceived stress in a probability sample of the United States In: S Spacapan and S Oskamp, editors. The social psychology of health. Newbury Park, CA: Sage (1988). 31–67.
25 Reis, RS, Hino, AA, and Añez, CR. Perceived stress scale. J Health Psychol. (2010) 15:107–14. doi: 10.1177/1359105309346343
26 Barbosa-Leiker, C, Kostick, M, Lei, M, McPherson, S, Roper, V, Hoekstra, T, et al. Measurement invariance of the perceived stress scale and latent mean differences across gender and time. Stress Heal. (2013) 29:253–60. doi: 10.1002/smi.2463
27 Wu, SM, and Amtmann, D. Psychometric evaluation of the perceived stress scale in multiple sclerosis. Int Sch Res Not. (2013) 2013:1–9. doi: 10.1155/2013/608356
28 Roberti, JW, Harrington, LN, and Storch, EA. Further psychometric support for the 10-item version of the perceived stress scale. J Coll Couns. (2006) 9:135–47. doi: 10.1002/j.2161-1882.2006.tb00100.x
29 Cohen: the social psychology of health – Google scholar [Internet] . Available at: https://scholar.google.com/scholar_lookup?title=The+Social+Psychology+of+Health&author=S+Cohen&author=G+Williamson&author=S+Spacapam&author=S+Oskamp&publication_year=1988& (Accessed February 28, 2022)
30 Cohen, S, and Williamson, G. Perceived stress in a probability sample of the United States. Soc Psychol Heal [Internet]. (1988) 13:31–67. Available at: http://doi.apa.org/psycinfo/1988-98838-002
31 Chaaya, M, Osman, H, Naassan, G, and Mahfoud, Z. Validation of the Arabic version of the Cohen perceived stress scale (PSS-10) among pregnant and postpartum women. BMC Psychiatry. (2010) 10:111. doi: 10.1186/1471-244X-10-111
32 Ben Loubir, D, Serhier, Z, Battas, O, Agoub, M, and Bennani Othmani, M. Evaluation of psychometric properties of the Arabic version of PSS stress measuring scale in the Moroccan population. Sage Open. (2014) 4:2158244014564353.
33 Connor, KM, and Davidson, JRT. Development of a new resilience scale: the Connor-Davidson resilience scale (CD-RISC). Depress Anxiety. (2003) 18:76–82. doi: 10.1002/da.10113
34 Campbell-Sills, L, and Stein, MB. Psychometric analysis and refinement of the Connor-Davidson resilience scale (CD-RISC): validation of a 10-item measure of resilience. J Trauma Stress [Internet]. (2007) 20:1019–28. doi: 10.1002/jts.20271
35 Yu, X, and Zhang, J. Factor analysis and psychometric evaluation of the Connor-Davidson resilience scale (CD-RISC) with Chinese people. Soc Behav Personal Int J. (2007) 35:19–30. doi: 10.2224/sbp.2007.35.1.19
36 Baek, HS, Lee, KU, Joo, EJ, Lee, MY, and Choi, KS. Reliability and validity of the Korean version of the Connor-Davidson resilience scale. Psychiatry Investig. (2010) 7:109–15. doi: 10.4306/pi.2010.7.2.109
37 Elkudssiah Ismail, N, Hui, WM, Goh, KW, Jimam, NS, Hermansyah, A, and Ming, LC. Resilience among Malaysian community pharmacists and general medical practitioners using the 10-item Connor-Davidson resilience scale (CD-RISC): the first national survey. Behav Sci (Basel). (2022) 12:1–11. doi: 10.3390/bs12080272
38 Campbell-Sills, L, Forde, DR, and Stein, MB. Demographic and childhood environmental predictors of resilience in a community sample. J Psychiatr Res [Internet]. (2009) 43:1007–12. doi: 10.1016/j.jpsychires.2009.01.013
39 Toma, G, Guetterman, TC, Yaqub, T, Talaat, N, and Fetters, MD. A systematic approach for accurate translation of instruments: experience with translating the Connor–Davidson resilience scale into Arabic. Methodol Innov [Internet]. (2017) 10:2059799117741406. doi: 10.1177/2059799117741406
40 American Association of Critical Care Nurses . Moral Distress – AACN [Internet]. AACN Position Statement: Moral Distress and Moral Residue. Aliso Viejo, CA; (2019). Available at: https://www.aacn.org/clinical-resources/moral-distress
41 Hamric, AB, and Epstein, EG. A health system-wide moral distress consultation service: development and evaluation. HEC Forum. (2017) 29:127–43. doi: 10.1007/s10730-016-9315-y
42 Wocial, LD, and Weaver, MT. Development and psychometric testing of a new tool for detecting moral distress: the moral distress thermometer. J Adv Nurs. (2013) 69:167–74. doi: 10.1111/j.1365-2648.2012.06036.x
43 Corley, MC, Elswick, RK, Gorman, M, and Clor, T. Development and evaluation of a moral distress scale. J Adv Nurs [Internet]. (2001) 33:250–6. doi: 10.1111/j.1365-2648.2001.01658.x
44 Alosaimi, FD, Abdel-Aziz, N, Alsaleh, K, AlSheikh, RRRR, AlSheikh, RRRR, and Abdel-Warith, A. Validity and feasibility of the Arabic version of distress thermometer for Saudi cancer patients. PLoS One [Internet]. (2018) 13:1–14. doi: 10.1371/journal.pone.0207364
45 Latif, A, Yaqub, S, Anwar Dar, Q, Sultan Awan, U, Farhat, H, and Abbas, KM. Stress, resilience and moral distress among health care providers during COVID-19 pandemic. Esculapio. (2021) 17:79–82. doi: 10.51273/esc21.2517116
46 Kulis, D, Bottomley, A, Velikova, G, Greimel, E, and Koller, M. EORTC quality of life group translation procedure. Eur Organ Res Treat Cancer. (2017) 2017:1–26. Available at: https://www.eortc.org/app/uploads/sites/2/2018/02/translation_manual_2017.pdf
47 Krejcie, RV, and Morgan, DW. Determining sample size for research activities. Educ Psychol Meas. (1970) 30:607–10. doi: 10.1177/001316447003000308
48 Simione, L, and Gnagnarella, C. Differences between health workers and general population in risk perception, behaviors, and psychological distress related to COVID-19 spread in Italy. Front Psychol. (2020) 11:2166. doi: 10.3389/fpsyg.2020.02166
49 Couarraze, S, Delamarre, L, Marhar, F, Quach, B, Jiao, J, Dorlhiac, RA, et al. The major worldwide stress of healthcare professionals during the first wave of the COVID-19 pandemic – the international COVISTRESS survey. PLoS One [Internet]. (2021) 16:e0257840. doi: 10.1371/journal.pone.0257840
50 WHO . WHO coronavirus disease (COVID-19) dashboard with vaccination data [internet]. (2021). Available at: https://covid19.who.int/%0Ahttps://covid19.who.int/region/searo/country/bd (Accessed February 28, 2022)
51 Flesia, L, Monaro, M, Mazza, C, Fietta, V, Colicino, E, Segatto, B, et al. Predicting perceived stress related to the Covid-19 outbreak through stable psychological traits and machine learning models. J Clin Med. (2020) 9. doi: 10.3390/jcm9103350
52 Vyas, KJ, Delaney, EM, Webb-Murphy, JA, and Johnston, SL. Psychological impact of deploying in support of the U.S. response to ebola: a systematic review and meta-analysis of past outbreaks. Mil Med [Internet]. (2016) 181:e1515–31. doi: 10.7205/MILMED-D-15-00473
53 Barzilay, R, Moore, TM, Greenberg, DM, DiDomenico, GE, Brown, LA, White, LK, et al. Resilience, COVID-19-related stress, anxiety and depression during the pandemic in a large population enriched for healthcare providers. Transl Psychiatry [Internet]. (2020) 10:1–8. doi: 10.1038/s41398-020-00982-4
54 Babore, A, Lombardi, L, Viceconti, ML, Pignataro, S, Marino, V, Crudele, M, et al. Psychological effects of the COVID-2019 pandemic: perceived stress and coping strategies among healthcare professionals. Psychiatry Res [Internet]. (2020) 293:113366. doi: 10.1016/j.psychres.2020.113366
55 Liu, S, Yang, L, Zhang, C, Xu, Y, Cai, L, Ma, S, et al. Gender differences in mental health problems of healthcare workers during the coronavirus disease 2019 outbreak. J Psychiatr Res [Internet]. (2021) 137:393–400. doi: 10.1016/j.jpsychires.2021.03.014
56 Liu, X, Kakade, M, Fuller, CJ, Fan, B, Fang, Y, Kong, J, et al. Depression after exposure to stressful events: lessons learned from the severe acute respiratory syndrome epidemic. Compr Psychiatry. (2012) 53:15–23. doi: 10.1016/j.comppsych.2011.02.003
57 Spoorthy, MS . Mental health problems faced by healthcare workers due to the COVID-19 pandemic–a review. Asian J Psychiatr. (2020) 51:102119–21. doi: 10.1016/j.ajp.2020.102119
58 Croghan, IT, Chesak, SS, Adusumalli, J, Fischer, KM, Beck, EW, Patel, SR, et al. Stress, resilience, and coping of healthcare workers during the COVID-19 pandemic. J Prim Care Community Health [Internet]. (2021) 12:215013272110084. doi: 10.1177/21501327211008448
59 Liu, N, Zhang, F, Wei, C, Jia, Y, Shang, Z, Sun, L, et al. Prevalence and predictors of PTSS during COVID-19 outbreak in China hardest-hit areas: gender differences matter. Psychiatry Res. (2020) 287:112921. doi: 10.1016/j.psychres.2020.112921
60 Qiu, J, Shen, B, Zhao, M, Wang, Z, Xie, B, and Xu, Y. A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: implications and policy recommendations. Gen Psychiatry [Internet]. (2020) 33:100213. doi: 10.1136/gpsych-2020-100213
61 Mazza, C, Ricci, E, Biondi, S, Colasanti, M, Ferracuti, S, Napoli, C, et al. A nationwide survey of psychological distress among Italian people during the COVID-19 pandemic: immediate psychological responses and associated factors. Int J Environ Res Public Heal. (2020) 17:3165. doi: 10.3390/ijerph17093165
62 Alhalaiqa, FN, Khalifeh, AH, Al Omari, O, Yehia, DB, and Khalil, MMH. Psychological problems in a sample of Jordanian healthcare workers involved in caring for patients with COVID-19: a cross-sectional study. Front Psychol. (2021) 12:3626. doi: 10.3389/fpsyg.2021.679785
63 O’Connor, RC, Wetherall, K, Cleare, S, McClelland, H, Melson, AJ, Niedzwiedz, CL, et al. Mental health and well-being during the COVID-19 pandemic: longitudinal analyses of adults in the UK COVID-19 Mental Health & Wellbeing study. Br J Psychiatry. (2021) 218:326–33. doi: 10.1192/bjp.2020.212
64 Son, C, Hegde, S, Smith, A, Wang, X, and Sasangohar, F. Effects of COVID-19 on college students’ mental health in the United States: interview survey study. J Med Internet Res. (2020) 22:1–14. doi: 10.2196/21279
65 Sareen, J, Erickson, J, Medved, MI, Asmundson, GJG, Enns, MW, Stein, M, et al. Risk factors for post-injury mental health problems. Depress Anxiety [Internet]. (2013) 30:321–7. doi: 10.1002/da.22077
66 The World Bank . The World Bank Jordan COVID-19 emergency response additional financing (P176862). (2021). Available at: https://corona.moh.gov.jo/en
67 Schneider, JN, Hiebel, N, Kriegsmann-Rabe, M, Schmuck, J, Erim, Y, Morawa, E, et al. Moral distress in hospitals during the first wave of the COVID-19 pandemic: a web-based survey among 3,293 healthcare workers within the German network university medicine. Front Psychol. (2021) 12:5295. doi: 10.3389/fpsyg.2021.775204
68 Pergert, P, Bartholdson, C, Blomgren, K, and Af Sandeberg, M. Moral distress in paediatric oncology: contributing factors and group differences. Nurs Ethics [Internet]. (2019) 26:2351–63. doi: 10.1177/0969733018809806
69 Mehlis, K, Bierwirth, E, Laryionava, K, Mumm, FHA, Hiddemann, W, Heußner, P, et al. High prevalence of moral distress reported by oncologists and oncology nurses in end-of-life decision making. Psychooncology [Internet]. (2018) 27:2733–9. doi: 10.1002/pon.4868
70 Verma, R, Balhara, YPS, and Gupta, CS. Gender differences in stress response: role of developmental and biological determinants. Ind Psychiatry J [Internet]. (2011) 20:4. doi: 10.4103/0972-6748.98407
71 Calvarese, M . The effect of gender on stress factors: an exploratory study among university students. Soc Sci. (2015) 4:1177–84. Available at: https://www.mdpi.com/2076-0760/4/4/1177/htm
72 Wu, PE, Styra, R, and Gold, WL. Mitigating the psychological effects of COVID-19 on health care workers. CMAJ [Internet]. (2020) 192:E459–60. doi: 10.1503/cmaj.200519
73 Abdel Wahed, WY, Hefzy, EM, Ahmed, MI, and Hamed, NS. Assessment of knowledge, attitudes, and perception of health care workers regarding COVID-19, a cross-sectional study from Egypt. J Community Health [Internet]. (2020) 45:1242–51. doi: 10.1007/s10900-020-00882-0
74 Racine, N, Hetherington, E, McArthur, BA, McDonald, S, Edwards, S, Tough, S, et al. Maternal depressive and anxiety symptoms before and during the COVID-19 pandemic in Canada: a longitudinal analysis. Lancet Psychiatry [Internet]. (2021) 8:405–15. doi: 10.1016/S2215-0366(21)00074-2
75 Alshekaili, M, Hassan, W, Al Said, N, Al Sulaimani, F, Jayapal, SK, Al-Mawali, A, et al. Factors associated with mental health outcomes across healthcare settings in Oman during COVID-19: frontline versus non-frontline healthcare workers. BMJ Open [Internet]. (2020) 10:e042030. doi: 10.1136/bmjopen-2020-042030
76 Lai, J, Ma, S, Wang, Y, Cai, Z, Hu, J, Wei, N, et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw Open [Internet]. (2020) 3:e203976–6. doi: 10.1001/jamanetworkopen.2020.3976
77 Tselebis, A, Lekka, D, Sikaras, C, Tsomaka, E, Tassopoulos, A, Ilias, I, et al. Insomnia, perceived stress, and family support among nursing staff during the pandemic crisis. Healthcare [Internet]. (2020) 8:434. doi: 10.3390/healthcare8040434
78 The World Bank . Jordan: modest economic contraction but private sector and equality suffer [internet]. The World Bank Data (2021). Available at: https://www.worldbank.org/en/news/press-release/2021/06/28/jordan-modest-economic-contraction-but-private-sector-and-equality-suffer
79 Lin, J, Ren, Y, Gan, H, Chen, Y, Huang, Y, and You, X. Factors influencing resilience of medical workers from other provinces to Wuhan fighting against 2019 novel coronavirus pneumonia. Research Square. (2020):1–13. doi: 10.21203/rs.3.rs-17931/v1
80 Arrogante, O, and Aparicio-Zaldivar, E. Burnout and health among critical care professionals: the mediational role of resilience. Intensive Crit Care Nurs. (2017) 42:110–5. doi: 10.1016/j.iccn.2017.04.010
81 Al Subeh, ZY, and Alzoubi, KH. Cultural and religious barriers influencing the participation of women in research: a study from Jordan. Gender Issues [Internet]. (2020) 37:173–86. doi: 10.1007/s12147-019-09235-1
Keywords: coronavirus pandemic, stress levels, resilience, oncology healthcare professionals, Perceived Stress Scale (PSS), Connor-Davidson Resilience Scale (CD-RSIC), Moral Distress Thermometer (MDT), Jordan
Citation: Alrjoub W, Alarjeh G, Ammar K, Shamieh A, Harding R, Booth C, Sullivan R, Al-ruzzieh M, Mansour A and Shamieh O (2023) Stress, resilience, and moral distress among health care providers in oncology during the COVID-19 pandemic. Front. Public Health. 11:1288483. doi: 10.3389/fpubh.2023.1288483
Edited by:
Reza Lashgari, Shahid Beheshti University, IranReviewed by:
Abbas Mardani, Iran University of Medical Sciences, IranFahad M. Alhowaymel, Shaqra University, Saudi Arabia
Copyright © 2023 Alrjoub, Alarjeh, Ammar, Shamieh, Harding, Booth, Sullivan, Al-ruzzieh, Mansour and Shamieh. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Omar Shamieh, T3NoYW1pZWhAa2hjYy5qbw==
 Waleed Alrjoub
Waleed Alrjoub Ghadeer Alarjeh
Ghadeer Alarjeh Khawlah Ammar2
Khawlah Ammar2 Richard Sullivan
Richard Sullivan Omar Shamieh
Omar Shamieh