
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health , 19 October 2023
Sec. Occupational Health and Safety
Volume 11 - 2023 | https://doi.org/10.3389/fpubh.2023.1283925
This article is part of the Research Topic Mental Health in Healthcare Workers and its Associations with Psychosocial Work Conditions View all 32 articles
 Ahmad R. Al-Qudimat1,2*†
Ahmad R. Al-Qudimat1,2*† Kalpana Singh3†
Kalpana Singh3† Emad Mustafa3
Emad Mustafa3 Abdulqadir J. Nashwan3†
Abdulqadir J. Nashwan3† Raed M. Al-Zoubi1,4,5†
Raed M. Al-Zoubi1,4,5† Aksam Yassin1,6†
Aksam Yassin1,6† Omar M. Aboumarzouk1,7†
Omar M. Aboumarzouk1,7† Abdulla Al-Ansari1†
Abdulla Al-Ansari1†Background: The COVID-19 pandemic has had a profound and global impact on healthcare systems worldwide, presenting unprecedented challenges for healthcare workers (HCWs) on the front. We aimed to evaluate the prevalence of anxiety and depression symptoms during the coronavirus pandemic among healthcare professionals in Qatar.
Methods: A cross-sectional study where an electronic questionnaire containing demographics, and psychosocial questions were made on Google Docs and Microsoft Team, and were sent through email and WhatsApp to healthcare workers, including doctors, nurses, allied health and others working at Hamad Medical Corporation in Qatar, from June 1, 2021, to January 1st 2023. ANOVA, t-test and multiple linear regression were used to see the association between the psychological factors and sociodemographic variables using STATA version 17 software.
Results: A total of 829 participants were included in this study (response rate: 55%). The average age of the participants is 36.0 ± 7.1; 65.9% were males; 2.3% were doctors and 53% were nurses, 38.7% were allied healthcare professionals and 6% were others. Psychological, social effects, and workplace were shown to significantly related to their marital status, career, and hospital setting (p < 0.01 for each). Similar to this, dealing with COVID-19 patients and their education level with the length of time working at the designated facility were all connected with the health professional safety score (p < 0.05).
Conclusion: During the COVID-19 epidemic, healthcare workers in Qatar experienced a high incidence of negative psychosocial symptoms. To alleviate these outcomes, it would be useful to implement screening procedures for such symptoms and to devise preventive measures accordingly.
The COVID-19 pandemic has had a profound and global impact on healthcare systems worldwide, presenting unprecedented challenges for healthcare workers (HCWs) on the front lines (1, 2). In response, various precautionary measures such as self-quarantine, social distancing, mandatory mask-wearing, and travel restrictions have been implemented to mitigate the spread of the highly contagious COVID-19 virus (3–8). However, these measures coupled with the suspension of elective medical procedures and strain on healthcare resources have significantly burdened HCWs and amplifying the pressure and presenting immense challenges (9–14).
Healthcare workers have faced not only an increased risk of infection but also prolonged periods of wearing cumbersome personal protective equipment (PPE), extended work shifts, and overwhelming patient caseloads (15–18). Furthermore, many studies reported the adverse effects of prolonged PPE usage. These effects include headaches, difficulty in breathing, and impaired cognition. Moreover, the continuous use of PPE interferes with vision, and communication, and disrupts thermal equilibrium (19–23). These demanding circumstances have taken a toll on the mental well-being of HCWs, leading to psychological distress, anxiety, sadness, and potential post-traumatic stress symptoms (24). Research conducted in countries such as the United States, Italy, and China has consistently reported high levels of anxiety, depression, and insomnia among HCWs during this unprecedented global health crisis (5, 25, 26).
On the other hand, several reports documented the diverse coping mechanisms adopted by healthcare workers. These strategies encompass seeking psychological support through counseling and therapy, engaging in stress-relieving activities such as physical exercise, meditation, and yoga, nurturing peer support from family and friends, as well as prioritizing effective self-care routines, and others. These endeavors played a critical role in preserving resilience and upholding an exceptional standard of patient care during this challenging period (27–30).
Despite the global recognition of the psychological impact on HCWs, limited research exists specifically examining the psychosocial effects of the COVID-19 pandemic on HCWs in the Gulf region, particularly in Qatar. To bridge this knowledge gap, the present study conducted a comprehensive cross-sectional examination of HCWs, encompassing various professional roles within significant hospitals under the Hamad Medical Corporation (HMC).
The study used descriptive, cross-sectional hospital-based study.
The study included a total of 829 healthcare workers (HCWs), including doctors, nurses, pharmacists, laboratory technicians, ambulance staff, and administrative personnel working in four major hospitals under Hamad Medical Corporation (HMC) in Qatar between January 2021 and December 2022. The response rate for this study was 78% across various hospitals, including Hamad General Hospital and HMGH. Incomplete surveys from HCWs were excluded from the study. We utilized a convenience sampling method, and the sample size was determined using the following equation: n = [(Z0.95)2 × p × (1 − p)]/(0.05)2, where n represents the sample size, Z: constant (1.96), p: is the estimated proportion or prevalence that meets our criteria.” p will be set as 0.5, as the proportion is not known. To attain a confidence level of 95% with a precision of +/− 0.05, the recommended calculated sample size is a minimum of 500 participants.
Data were collected using an anonymous online questionnaire. The use of an online survey form was conducted on Google Docs and Microsoft Team forms in English and sent to healthcare workers via email and WhatsApp. There was no direct contact or face-to-face interaction with the HCWs.
We developed a questionnaire using multiple English-language tools (31–33). The developed tools in consultation with mental health professionals. We conducted a pilot study involving 20 conveniently selected HWCs. We discussed with them the comprehensiveness, language, and grammar of the questions.
To assess the face and content validity of the questionnaire, we distributed it to four reviewers, consisting of two mental health professionals and two senior researchers. Each reviewer was asked to independently rate each item in the questionnaire and provide feedback on its readability, comprehensiveness, clarity, language, and grammar. Upon analyzing the results, we found that the questionnaire demonstrated accepted content validity.
The questionnaire consists of five sections, developed through an extensive literature review. The first section focuses on demographic characteristics and background information, such as age, sex, marital status, education level, nationality, specialty, hospital name, living status, family members, and other relevant details using multiple choice questions. The second section addresses 9 questions related to psychological impact, while the third section focuses on social impact with 5 questions. The fourth section delves into the workplace impact with 6 questions, and finally, the fifth section covers 4 questions on health professional safety. Likert scale (strongly disagree, disagree, neutral, agree, strongly agree) was used to answer questions for section 2 till section 5.
Descriptive statistics were calculated for the demographics and dependent variables of the study participants. Pearson correlations were used to examine the relationships between the four main variables, i.e., psychological impact, social impact, workplace and health professional safety. We used Q–Q plot and P–P plot and Schapiro Wilk test to check the normal distribution of psychological impact, social impact, workplace and health professional safety variables. ANOVA and t-tests were conducted to compare the level of psychological well-being, needs, resources, and job support satisfaction between the sector and socio-demographic characteristics (age, gender, education level, nationality, specialty, working with COVID-19 patient). A multiple linear regression was used to see the association between the psychological well-being, social impact, workplace and health professionals’ safety with the different sociodemographic variables. All statistical analysis was done using STATA 17 software with statistical significance level p < 0.05.
This study was conducted in accordance with the principles of the Declaration of Helsinki. Ethical approval for the study was obtained from HMC (Ethical Approval Number: MRC-01-21-235), and consent was obtained from all participants. Participants were provided with information about the study’s objectives, and assurance of the confidentiality of all shared information was given.
The questionnaire was distributed via email and WhatsApp, and 829 people responded in total. The age of healthcare professionals was 36 ± 7.1. Moreover, 65.9% of the population were men, 70.8% were married, and 76% had a bachelor’s degree. Eighty-three percent (83.2%) of the participants were Asian, with 58.1% of them working at Hamad General Hospital and 35.6% at Hazm Mebaireek General Hospital (HMGH) (Table 1).
In this sample, physicians made up 2.3% of the workforce, nurses (53%), allied healthcare workers including pharmacists, rehabilitation staff, dentists, dietitians, educators, researchers, technicians, respiratory therapists made up 38.7%, and other hospital staff such as administrative staff and engineers made up 6%. Most of the healthcare workers (70%) had direct contact with a COVID-19 positive patient and 67% were working in the COVID-19 facility last 12 months. About 76% of healthcare workers lived with their families, and 57.3% had three to five family members. 76% of healthcare workers who had the PCR test done at least four times or more had 71% of their relatives, co-workers or friends who tested positive.
Figure 1 shows the correlation between all four variables, i.e., psychological, social, workplace and health professional safety.
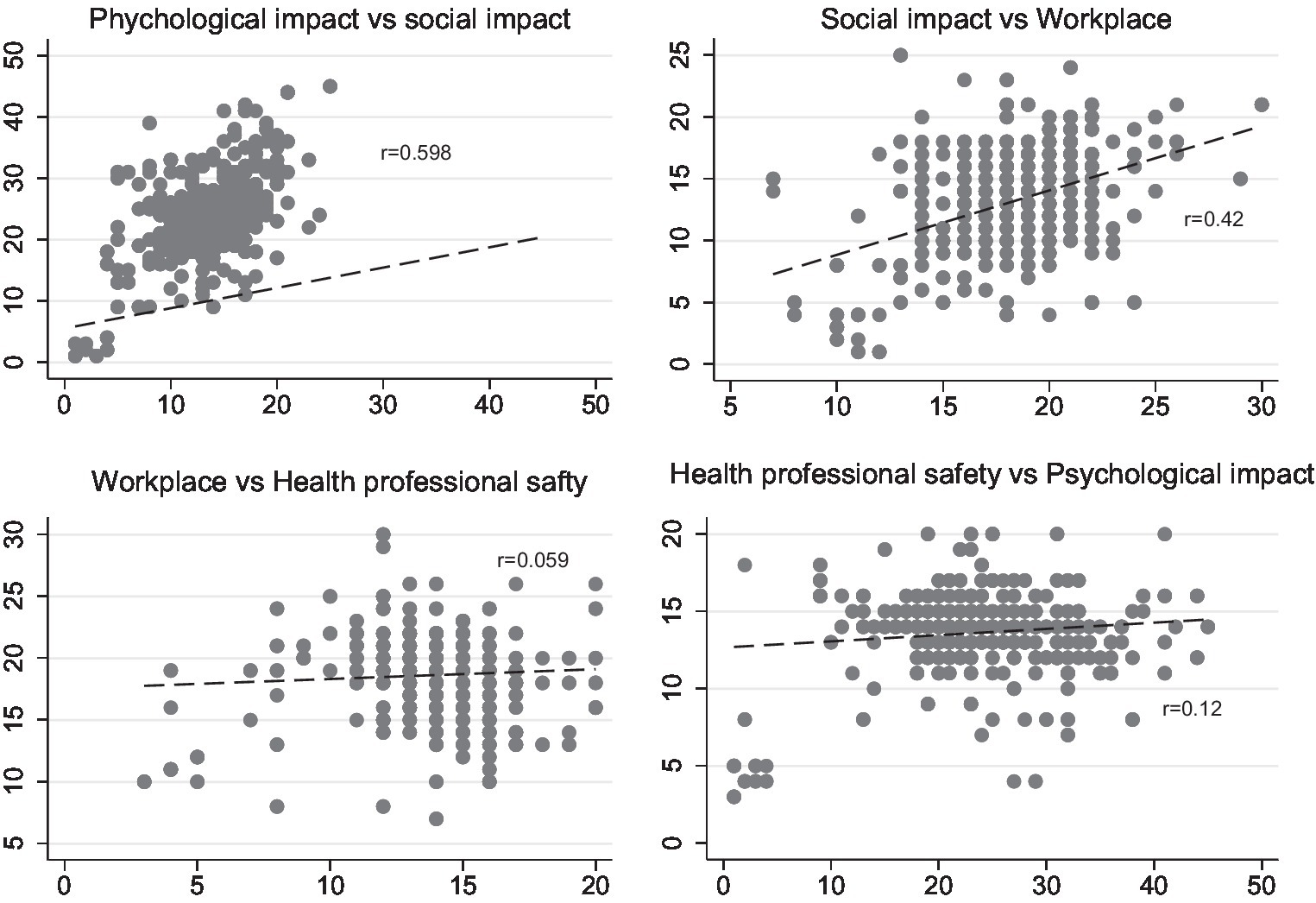
Figure 1. Correlation between psychosocial impact, social impact, workplace and health profession safety.
The mean of psychological impact, social impact, workplace and health professional safety scores of the participants were 23.6 ± 7.37, 13.3 ± 4.0, 18.5 ± 3.3 and 13.6 ± 2.4, respectively.
Females had considerably greater (13.9 ± 1.7) health professional safety as compared to males (13.5 ± 2.7, p = 0.03), while males had a significantly larger (24.2 ± 8.3) psychological impact as compared to females (22.4 ± 4.9, p ≤ 0.001).
When compared to married and widowed/divorced individuals, those who were single had a considerably higher psychological and social impact (p = 0.004 and p = 0.022), respectively. Married people (18.6 ± 3.5), followed by single people (18.5 ± 2.9), had stronger workplace impacts than widowed or divorced people (14.9 ± 3.4), p = 0.013. As comparison to individuals who earned a bachelor’s, master’s, or diploma, healthcare practitioners who earned a Ph.D. had better psychological, social impact, and health professional safety (p < 0.001, p < 0.001 and p = 0.01), respectively. North Americans (30.2 ± 8.0) were more psychologically affected than Europeans (24.7 ± 13.5) and Asians (23.7 ± 8.0) in terms of nationality p = 0.035.
Compared to nurses, allied health professionals, physicians, and others had greater psychological, social, and occupational effects (p < 0.001), respectively.
Other factors like indirect exposure with COVID-19 patients, those are not having any experience with COVID-19 had significantly higher psychological and social impact p < 0.001, p < 0.001 and p < 0.001, p = 0.002, respectively. Those were living with others had greater psychological and social impact as compared to those who were with family and single p < 0.001 and p < 0.001, respectively.
In terms of family members those were having 6–7 family members and their family members, relatives and colleagues tested positive had significantly higher psychological impact p < 0.001 and p = 0.02 (Table 2).
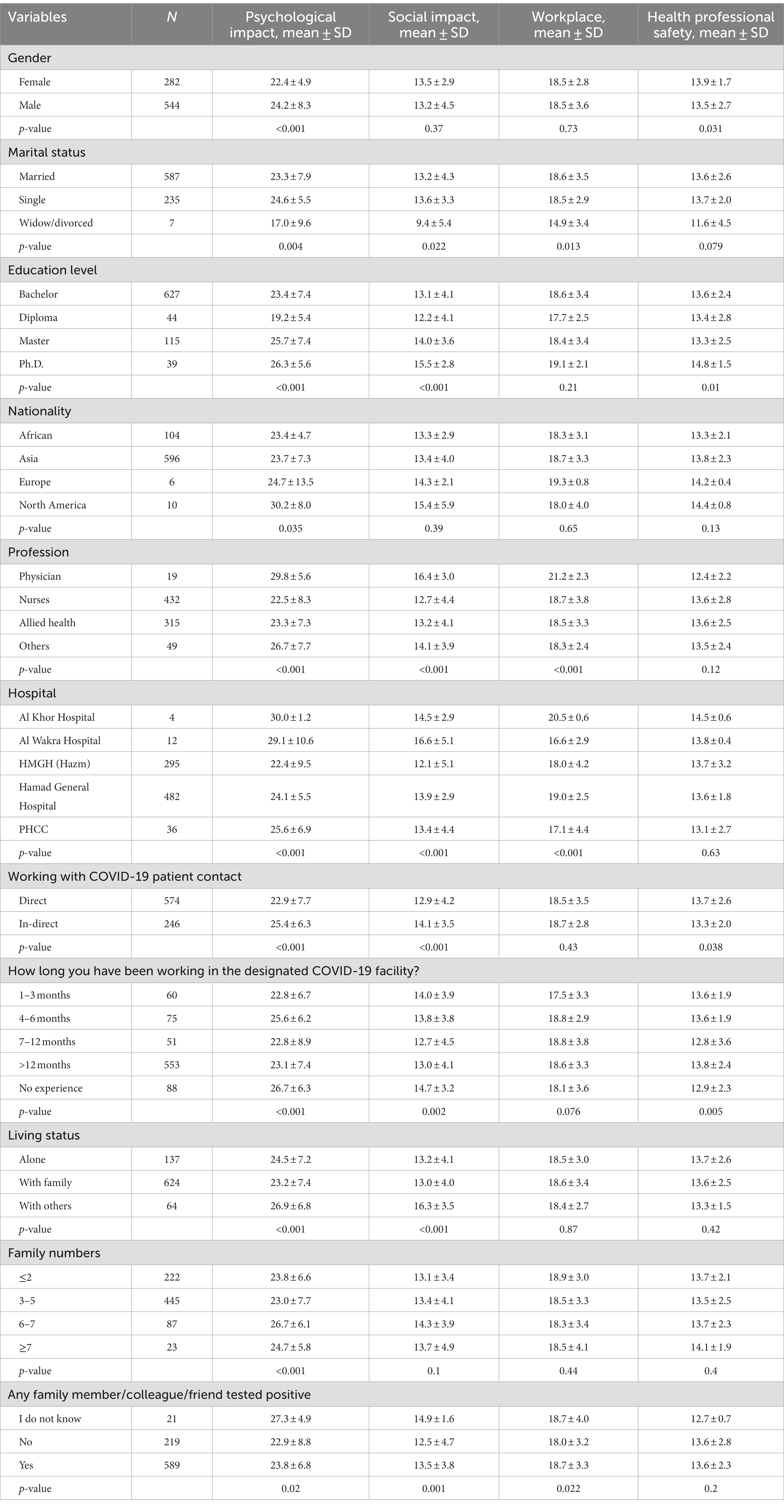
Table 2. The association between socio demographic factors, psychological, social, workplace and health professional safety.
Table 3 shows the adjusted relationship between sociodemographic characteristics, workplace, social, and health professional safety. Age was significantly associated with psychological impact Coef. 0.25: 95% CI (0.16, 0.35). Men had more of an emotional influence Coef. 2.28: 95% CI (0.94, 3.61); p = 0.001 and lower health professional safety Coef. −0.49: 95% CI (−0.83, −0.12); p = 0.009 as compared to females.
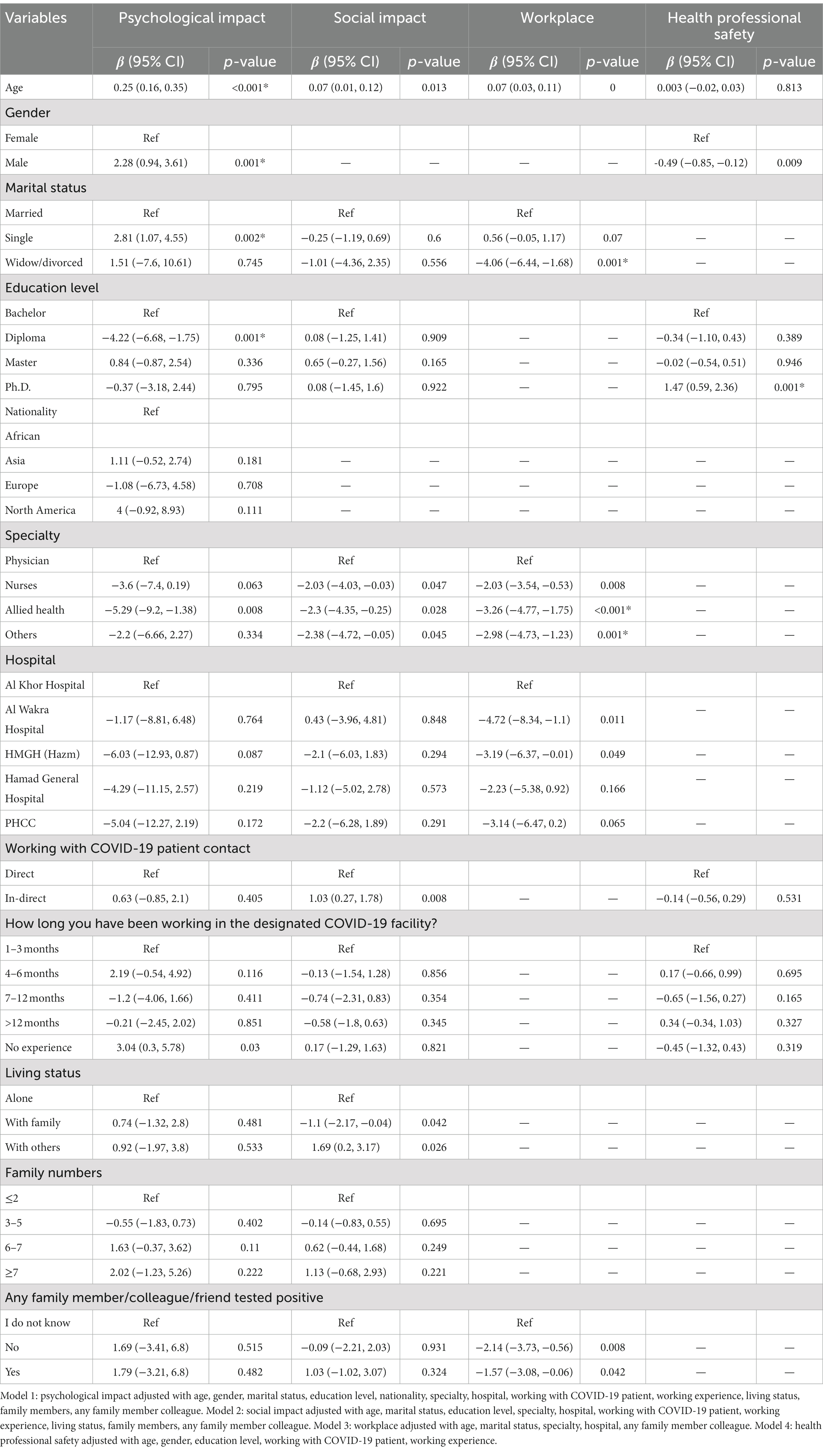
Table 3. Multiple linear regression for psychological impact, social impact, workplace and health professional safety.
In comparison to married, being single had higher psychological impact Coef. 2.81 95% CI (1.07, 4.55); p = 0.002 and being widow/divorced had lower workplace impact Coef. −4.06: 95% CI (−6.44, −1.68); p = 0.001. When compared to those who earned a bachelor’s degree, those with a diploma had a significantly lower psychological effect Coef. −4.22: 95% CI (−6.68, −1.75); p = 0.001 and those who completed a Ph.D. had higher health professional safety Coef. 1.47: 95% CI (0.59, 2.37), p = 0.001.
The psychological effect was lower among the allied health professionals Coef. −5.29: 95% CI (−9.2, −1.38); p = 0.008; nurses Coef. −2.03: 95% CI (−4.03, −0.03); p = 0.047; allied health professionals Coef. −2.3: 95% CI (−4.35, −0.25); p = 0.028; and others Coef. −2.38: 95% CI (−4.72, −0.05); p = 0.045 had lower social impact as compared to physicians. As compared to physicians, nurses Coef. −2.03: 95% CI (−3.54, −0.53), p = 0.008, allied health professional Coef. −3.26: 95% CI (−4.77, −1.75), p = <0.001 and others Coef. −2.98: 95% CI (−4.73, −1.23), p = 0.001 had lower workplace impact. Alwakra hospital also had lower workplace impact Coef. −4.72 95% CI (−8.34, −1.1), p = 0.011 as compared to Alkhor hospital.
Those who worked with COVID-19 patients indirectly had greater social impacts Coef. 1.03 95% CI (0.27, 1.78), p = 0.008 compared to those working directly with COVID-19 patients. Health workers who lived with families had a lower social impact on Coef. −1.20: 95% CI (−2.17, −0.04), p = 0.042, and those living with others had a higher social impact Coef. 1.70: 95% CI (0.2, 3.17), p = 0.026 compared to those living alone.
Those who know that their family members, co-workers or friends tested positive had a lower social impact Coef. −1.57: 95% CI (−3.08, −0.06), p = 0.042, and those who have no friends, colleagues, or family members had a lower social impact Coef. −2.14: 95% CI (−3.73, −0.56), p = 0.008 compared to those who were unaware that their friends, co-workers and family members have tested positive.
As previously mentioned, numerous reports have detailed the various coping strategies adopted by healthcare professionals. These approaches include seeking psychological support through counseling and therapy, engaging in stress-reduction activities like physical exercise, meditation, and yoga, fostering peer support from family and friends, and prioritizing effective self-care routines, among others. These efforts played a pivotal role in maintaining resilience and upholding an exceptional standard of patient care during this challenging period (27–30). Additionally, some scholars have highlighted individual and environmental factors, such as incidents of violence or psychiatric illnesses, prolonged wait times, understaffing in emergency rooms, a history of drug or alcohol abuse, and unrestricted public movement, as contributing to the challenges faced in healthcare settings (34).
This study aimed to elucidate the psychosocial experiences of HCWs who worked undergone the COVID-19 crisis. Drawing from the accounts of the participants, various domains were explored, including the psychological impact, social consequences, safety, and workplace.
In this study, healthcare workers (HCWs) experienced moderate psychological distress, which aligns with international research showing high levels of anxiety and depression among HCWs during the COVID-19 pandemic. The unprecedented challenges posed by the pandemic, such as increased work demands, fear of infection, and concerns about transmitting the virus, contribute to the psychological burden on HCWs (5, 35–43).
The social impact observed among HCWs in Qatar indicates a moderate disruption to social connections, consistent with international studies highlighting social isolation and loneliness experienced by HCWs (44–48). Implementing physical distancing measures and reducing social interactions have contributed to a sense of isolation among HCWs (48).
The findings indicate a high perception of workplace safety among participants, reflecting their confidence in the safety measures implemented by healthcare institutions in Qatar. This finding confirms that healthcare institutions have prioritized the safety of HCWs in the region. Studies conducted in Taiwan (49) and Saudi Arabia (50) have emphasized the importance of personal protective equipment (PPE) and infection control measures in reducing the risk of COVID-19 transmission among HCWs. Adequate provision of PPE, adherence to infection control guidelines, regular testing protocols, and vaccination have contributed to the high safety perception among participants.
Regular testing programs in Qatar enable early detection of COVID-19 cases among HCWs, facilitating prompt isolation and reducing the risk of transmission within healthcare settings (50, 51). Vaccination is another crucial factor in ensuring the safety of HCWs, and Qatar has made significant efforts to provide COVID-19 vaccines to its healthcare workforce (42, 52). Prioritizing immunization helps minimize the risk of infection and associated complications. This approach aligns with international best practices, as studies conducted in countries like the United States (53) and Canada (54) have also emphasized the importance of regular testing and vaccination in protecting HCWs from COVID-19.
These findings support the global understanding of the benefits of vaccination and regular testing as essential measures for safeguarding the health and safety of HCWs.
Our findings imply that age significantly impacts how the pandemic affects HCWs psychologically. Older HCWs may have heightened concerns about their vulnerability to the virus due to age-related health conditions, leading to increased psychological distress (55). Additionally, their professional experience and knowledge may contribute to higher levels of responsibility and pressure, further impacting their psychological well-being (56). International studies have also reported similar associations between age and psychological impact among HCWs. For instance, a study conducted in Jordan found higher levels of psychological distress among older HCWs compared to younger individuals (57). Conversely, a study in Saudi Arabia indicated that younger HCWs experienced more psychological distress (58). These findings underscore the importance of considering age-related factors when addressing the psychological well-being of HCWs during the COVID-19 pandemic.
Our findings indicate that females perceived higher levels of safety, while males reported a more significant psychological impact. The higher perception of safety among females may be attributed to their greater compliance with infection control measures and adherence to safety protocols (59). Additionally, female HCWs may possess a heightened awareness of COVID-19 risks and a stronger sense of responsibility toward their safety and that of their colleagues. On the other hand, males may experience additional stress and emotional burden due to societal expectations related to strength, resilience, and leadership in their professional roles (60). These unique challenges male HCWs face may contribute to their higher reported psychological impact. Therefore, it is crucial to consider these gender-specific factors when addressing the well-being of HCWs during the pandemic.
Furthermore, the results of this study are consistent with those of a study by Alhofaian et al. (61) carried out in Saudi Arabia, which also revealed that female HCWs perceived higher levels of safety than males. This suggests that gender differences in safety perception may transcend the specific context of this study. However, studies conducted in other regions, such as the US (53), have yielded different results, indicating that gender differences in safety perception may vary across cultural, social, and organizational contexts. Therefore, it is essential to consider these contextual factors when interpreting and generalizing the findings of this study.
The study findings revealed significant associations between marital status, educational level, and nationality, and the psychological, social, workplace, and health professional safety impacts experienced by HCWs during the pandemic. For example, single individuals reported higher psychological and social impacts than married and widowed/divorced individuals (62, 63). Married individuals, on the other hand, reported more substantial workplace impacts compared to widowed or divorced individuals (64). These findings suggest that marital status can influence the experiences and challenges faced by HCWs during the pandemic. In addition, the study findings indicate that HCWs with a Ph.D. qualification demonstrated better psychological and social impact and health professional safety than those with lower educational levels (65). This suggests that higher levels of education contribute to better coping strategies and a greater sense of control among HCWs.
On the other hand, the study discovered that North Americans suffered more significant psychological effects than Europeans and Asians, possibly due to cultural variations, healthcare systems, and the severity of the pandemic in various regions. When comparing the findings of this study with international, Middle Eastern, and Arabic studies, several similarities and differences emerge. For instance, Tan’s et al. (66) study in Singapore found similar results regarding the higher psychological impact single HCWs experience. This suggests that the association between marital status and psychological impact extends beyond regional boundaries. Additionally, studies conducted in Turkey (67) and India (68) showed that higher educational qualifications are associated with better psychological well-being and coping mechanisms among HCWs, aligning with the findings of this study.
However, limited research comparing North Americans, Europeans, and Asians regarding psychological impact among HCWs during the pandemic was found, making this finding regarding nationality a novel contribution that warrants further investigation.
Physicians in this study experienced more significant psychological, social, and occupational impacts than nurses, allied health professionals, and others. The higher psychological impact among physicians can be attributed to their direct involvement in diagnosing and treating COVID-19 patients, which exposes them to higher stress levels and emotional burdens. Difficult decisions regarding patient care, resource allocation, and ethical dilemmas further contribute to their psychological distress. The demanding nature of their profession, long working hours, and limited social engagement outside of work also play a role. Similar patterns have been observed in studies conducted in the United States (69) and Belgium (70), highlighting the global nature of physicians’ challenges. These findings underscore the importance of targeted interventions to support physicians’ well-being.
Participants without any prior experience with COVID-19 had significantly higher psychological and social impacts than those with previous exposure (71). This can be attributed to limited knowledge and understanding of the virus, increased anxiety, and uncertainty. The fear of contracting the virus and its potential consequences for personal and loved ones’ health further contribute to the observed impact. Moreover, individuals living with others, such as roommates or colleagues, experienced more significant psychological and social impacts than those living with their families or being single (72). This suggests that the dynamics of shared living spaces and interactions with others may contribute to increased stress and emotional burden. The challenges of maintaining physical distance, addressing potential conflicts, and navigating shared spaces could all contribute to the observed impact.
While these findings provide valuable insights, comparing them with international, Middle Eastern and Arabic studies is challenging due to the novelty of this specific discovery. Therefore, this finding represents a novel discovery and highlights the need for further research to understand the underlying mechanisms and explore potential interventions.
In spite of the findings presented in this study, it is important to acknowledge several limitations. The first limitation of this study is that the measurements, they were conducted after a peak of COVID-19. This timing may have influenced the psychosocial working conditions experienced during the data collection period. It is worth considering that the results might have varied if the measurements had been taken during peak hospitalization periods. The second limitation is that only participants who had given permission in 2019 were contacted to participate. This approach introduces the possibility of selection bias, as the sample may not accurately represent the entire population of interest.
The findings of this study have several implications for the healthcare sector in Qatar and beyond. First, acknowledging the psychological distress that HCWs experience emphasizes the need for extensive mental health support services and interventions. Therefore, healthcare organizations in Qatar should prioritize providing resources, such as access to mental health services and tailored coping mechanisms, to address the specific needs of HCWs. Additionally, efforts should be made to foster supportive environments, promote peer support programs, and facilitate opportunities for HCWs to maintain social connections while adhering to safety protocols.
The study’s findings regarding the perceived safety of HCWs highlight the effectiveness of infection control measures, PPE, regular testing, and vaccination in protecting HCWs. These measures should continue to be implemented and prioritized in Qatar’s healthcare institutions to ensure the safety of HCWs. Furthermore, these findings are consistent with international best practices, emphasizing the importance of regular testing and vaccination in protecting HCWs from COVID-19. Qatar’s adherence to these practices aligns with global recommendations and demonstrates its commitment to the safety and well-being of its healthcare workforce.
In conclusion, this study examined anxiety, depression, insomnia, psychological impact, social impact, workplace safety, and health professional safety among HCWs in Qatar during the COVID-19 pandemic. The findings revealed moderate levels of psychological distress, disruption to social connections, and perceived safety among HCWs. In addition, age, gender, marital status, educational level, nationality, and designation were identified as significant factors influencing the psychological and social impacts experienced by HCWs. The study also highlighted the importance of robust infection control measures, adequate PPE, regular testing, and vaccination in ensuring the safety and well-being of HCWs.
The raw data supporting the conclusions of this article will be made available by the corresponding author upon request.
The studies involving humans were approved by Medical Research Center (MRC)/Hamad Medical Corporation/Qatar. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants’ legal guardians/next of kin.
AA-Q: Conceptualization, Investigation, Methodology, Supervision, Writing – original draft, Writing – review & editing. KS: Formal analysis, Writing – review & editing. EM: Writing – review & editing. AN: Writing – review & editing. RA-Z: Writing – review & editing. AY: Supervision, Writing – review & editing. OA: Supervision, Writing – review & editing. AA-A: Supervision, Writing – review & editing.
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
The publication of this article was funded by Qatar National Library (QNL).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Bong, CL, Brasher, C, Chikumba, E, McDougall, R, Mellin-Olsen, J, and Enright, A. The COVID-19 pandemic: effects on low- and middle-income countries. Anesth Analg. (2020) 131:86–92. doi: 10.1213/ANE.0000000000004846
2. Christopher, DJ, Isaac, BT, Rupali, P, and Thangakunam, B. Health-care preparedness and health-care worker protection in COVID-19 pandemic. Lung India. (2020) 37:238–45. doi: 10.4103/lungindia.lungindia_189_20
3. Bruinen de Bruin, Y, Lequarre, AS, McCourt, J, Clevestig, P, Pigazzani, F, Zare Jeddi, M, et al. Initial impacts of global risk mitigation measures taken during the combatting of the COVID-19 pandemic. Saf Sci. (2020) 128:104773. doi: 10.1016/j.ssci.2020.104773
4. Shanka, MS, and Menebo, MM. When and how trust in government leads to compliance with COVID-19 precautionary measures. J Bus Res. (2022) 139:1275–83. doi: 10.1016/j.jbusres.2021.10.036
5. Chen, J, Liu, X, Wang, D, Jin, Y, He, M, Ma, Y, et al. Risk factors for depression and anxiety in healthcare workers deployed during the COVID-19 outbreak in China. Soc Psychiatry Psychiatr Epidemiol. (2021) 56:47–55. doi: 10.1007/s00127-020-01954-1
6. Varghese, GM, John, R, Manesh, A, Karthik, R, and Abraham, OC. Clinical management of COVID-19. Indian J Med Res. (2020) 151:401–10. doi: 10.4103/ijmr.IJMR_957_20
7. Tong, KK, Chen, JH, Yu, EW, and Wu, AMS. Adherence to COVID-19 precautionary measures: applying the health belief model and generalised social beliefs to a probability community sample. Appl Psychol Health Well Being. (2020) 12:1205–23. doi: 10.1111/aphw.12230
8. Sharun, K, Tiwari, R, Natesan, S, Yatoo, MI, Malik, YS, and Dhama, K. International travel during the COVID-19 pandemic: implications and risks associated with “travel bubbles”. J Travel Med. (2020) 27:taaa184. doi: 10.1093/jtm/taaa184
9. Sarac, NJ, Sarac, BA, Schoenbrunner, AR, Janis, JE, Harrison, RK, Phieffer, LS, et al. A review of state guidelines for elective orthopaedic procedures during the COVID-19 outbreak. J Bone Joint Surg Am. (2020) 102:942–5. doi: 10.2106/JBJS.20.00510
10. Zarrintan, S. Surgical operations during the COVID-19 outbreak: should elective surgeries be suspended? Int J Surg. (2020) 78:5–6. doi: 10.1016/j.ijsu.2020.04.005
11. Black, JRM, Bailey, C, Przewrocka, J, Dijkstra, KK, and Swanton, C. COVID-19: the case for health-care worker screening to prevent hospital transmission. Lancet. (2020) 395:1418–20. doi: 10.1016/S0140-6736(20)30917-X
12. Boserup, B, McKenney, M, and Elkbuli, A. The financial strain placed on America’s hospitals in the wake of the COVID-19 pandemic. Am J Emerg Med. (2021) 45:530–1. doi: 10.1016/j.ajem.2020.07.007
13. Badrfam, R, Zandifar, A, and Arbabi, M. Mental health of medical workers in COVID-19 pandemic: restrictions and barriers. J Res Health Sci. (2020) 20:e00481. doi: 10.34172/jrhs.2020.16
14. Vizheh, M, Qorbani, M, Arzaghi, SM, Muhidin, S, Javanmard, Z, and Esmaeili, M. The mental health of healthcare workers in the COVID-19 pandemic: a systematic review. J Diabetes Metab Disord. (2020) 19:1967–78. doi: 10.1007/s40200-020-00643-9
15. Park, SH. Personal protective equipment for healthcare workers during the COVID-19 pandemic. Infect Chemother. (2020) 52:165–82. doi: 10.3947/ic.2020.52.2.165
16. Kluger, DM, Aizenbud, Y, Jaffe, A, Parisi, F, Aizenbud, L, Minsky-Fenick, E, et al. Impact of healthcare worker shift scheduling on workforce preservation during the COVID-19 pandemic. Infect Control Hosp Epidemiol. (2020) 41:1443–5. doi: 10.1017/ice.2020.337
17. Huang, L, Wang, Y, Liu, J, Ye, P, Chen, X, Xu, H, et al. Factors influencing anxiety of health care workers in the radiology department with high exposure risk to COVID-19. Med Sci Monit. (2020) 26:e926008. doi: 10.12659/MSM.926008
18. Sharun, K, Rahman, CKF, Haritha, CV, Jose, B, Tiwari, R, and Dhama, K. COVID-19 vaccine acceptance: beliefs and barriers associated with vaccination among the general population in India. J Exp Biol Agric Sci. (2020) 8:S210–8. doi: 10.18006/2020.8(Spl-1-SARS-CoV-2).S210.S218
19. Santoro, PE, Borrelli, I, Gualano, MR, Proietti, I, Skroza, N, Rossi, MF, et al. The dermatological effects and occupational impacts of personal protective equipment on a large sample of healthcare workers during the COVID-19 pandemic. Front Public Health. (2021) 9:815415. doi: 10.3389/fpubh.2021.815415
20. Davey, SL, Lee, BJ, Robbins, T, Randeva, H, and Thake, CD. Heat stress and PPE during COVID-19: impact on healthcare workers’ performance, safety and well-being in NHS settings. J Hosp Infect. (2021) 108:185–8. doi: 10.1016/j.jhin.2020.11.027
21. Johnson, AT. Respirator masks protect health but impact performance: a review. J Biol Eng. (2016) 10:4. doi: 10.1186/s13036-016-0025-4
22. Lim, EC, Seet, RC, Lee, KH, Wilder-Smith, EP, Chuah, BY, and Ong, BK. Headaches and the N95 face-mask amongst healthcare providers. Acta Neurol Scand. (2006) 113:199–202. doi: 10.1111/j.1600-0404.2005.00560.x
23. Nashwan, AJ, Villar, RC, Al-Qudimat, AR, Kader, N, Alabdulla, M, Abujaber, AA, et al. Quality of life, sleep quality, depression, anxiety, stress, eating habits, and social bounds in nurses during the coronavirus disease 2019 pandemic in Qatar (the PROTECTOR study): a cross-sectional, comparative study. J Pers Med. (2021) 11:918. doi: 10.3390/jpm11090918
24. Rodríguez, BO, and Sánchez, TL. The psychosocial impact of COVID-19 on health care workers. Int Braz J Urol. (2020) 46:195–200. doi: 10.1590/s1677-5538.ibju.2020.s124
25. Pearman, A, Hughes, ML, Smith, EL, and Neupert, SD. Mental health challenges of United States healthcare professionals during COVID-19. Front Psychol. (2020) 11:2065. doi: 10.3389/fpsyg.2020.02065
26. Di Tella, M, Romeo, A, Benfante, A, and Castelli, L. Mental health of healthcare workers during the COVID-19 pandemic in Italy. J Eval Clin Pract. (2020) 26:1583–7. doi: 10.1111/jep.13444
27. Rossi, MF, Gualano, MR, Magnavita, N, Moscato, U, Santoro, PE, and Borrelli, I. Coping with burnout and the impact of the COVID-19 pandemic on workers’ mental health: a systematic review. Front Psychiatry. (2023) 14:1139260. doi: 10.3389/fpsyt.2023.1139260
28. Smith, GD, Ng, F, and Ho Cheung Li, W. COVID-19: emerging compassion, courage and resilience in the face of misinformation and adversity. J Clin Nurs. (2020) 29:1425–8. doi: 10.1111/jocn.15231
29. Maben, J, and Bridges, J. COVID-19: supporting nurses’ psychological and mental health. J Clin Nurs. (2020) 29:2742–50. doi: 10.1111/jocn.15307
30. Pappa, S, Ntella, V, Giannakas, T, Giannakoulis, VG, Papoutsi, E, and Katsaounou, P. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: a systematic review and meta-analysis. Brain Behav Immun. (2020) 88:901–7. doi: 10.1016/j.bbi.2020.05.026
31. Bai, Y, Lin, CC, Lin, CY, Chen, JY, Chue, CM, and Chou, P. Survey of stress reactions among health care workers involved with the SARS outbreak. Psychiatr Serv. (2004) 55:1055–7. doi: 10.1176/appi.ps.55.9.1055
32. Reagu, S, Wadoo, O, Latoo, J, Nelson, D, Ouanes, S, Masoodi, N, et al. Psychological impact of the COVID-19 pandemic within institutional quarantine and isolation centres and its sociodemographic correlates in Qatar: a cross-sectional study. BMJ Open. (2021) 11:e045794. doi: 10.1136/bmjopen-2020-045794
33. Brooks, SK, Webster, RK, Smith, LE, Woodland, L, Wessely, S, Greenberg, N, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. (2020) 395:912–20. doi: 10.1016/S0140-6736(20)30460-8
34. Rossi, MF, Beccia, F, Cittadini, F, Amantea, C, Aulino, G, Santoro, PE, et al. Workplace violence against healthcare workers: an umbrella review of systematic reviews and meta-analyses. Public Health. (2023) 221:50–9. doi: 10.1016/j.puhe.2023.05.021
35. Trumello, C, Bramanti, SM, Ballarotto, G, Candelori, C, Cerniglia, L, Cimino, S, et al. Psychological adjustment of healthcare workers in Italy during the COVID-19 pandemic: differences in stress, anxiety, depression, burnout, secondary trauma, and compassion satisfaction between frontline and non-frontline professionals. Int J Environ Res Public Health. (2020) 17:8358. doi: 10.3390/ijerph17228358
36. Hummel, S, Oetjen, N, Du, J, Posenato, E, Resende de Almeida, RM, Losada, R, et al. Mental health among medical professionals during the COVID-19 pandemic in eight European countries: cross-sectional survey study. J Med Internet Res. (2021) 23:e24983. doi: 10.2196/24983
37. Husky, MM, Villeneuve, R, Tabue Teguo, M, Alonso, J, Bruffaerts, R, Swendsen, J, et al. Nursing home workers’ mental health during the COVID-19 pandemic in France. J Am Med Dir Assoc. (2022) 23:1095–100. doi: 10.1016/j.jamda.2022.04.001
38. Adeyemo, OO, Tu, S, and Keene, D. How to lead health care workers during unprecedented crises: a qualitative study of the COVID-19 pandemic in Connecticut, USA. PLoS One. (2021) 16:e0257423. doi: 10.1371/journal.pone.0257423
39. Souza, DO. Health of nursing professionals: workload during the COVID-19 pandemic. Rev Bras Med Trab. (2021) 18:464–71. doi: 10.47626/1679-4435-2020-600
40. Shoja, E, Aghamohammadi, V, Bazyar, H, Moghaddam, HR, Nasiri, K, Dashti, M, et al. COVID-19 effects on the workload of Iranian healthcare workers. BMC Public Health. (2020) 20:1636. doi: 10.1186/s12889-020-09743-w
41. Cawcutt, KA, Starlin, R, and Rupp, ME. Fighting fear in healthcare workers during the COVID-19 pandemic. Infect Control Hosp Epidemiol. (2020) 41:1192–3. doi: 10.1017/ice.2020.315
42. Taylor, S, Landry, CA, Rachor, GS, Paluszek, MM, and Asmundson, GJG. Fear and avoidance of healthcare workers: an important, under-recognized form of stigmatization during the COVID-19 pandemic. J Anxiety Disord. (2020) 75:102289. doi: 10.1016/j.janxdis.2020.102289
43. Ehrlich, H, McKenney, M, and Elkbuli, A. Protecting our healthcare workers during the COVID-19 pandemic. Am J Emerg Med. (2020) 38:1527–8. doi: 10.1016/j.ajem.2020.04.024
44. Giardino, DL, Huck-Iriart, C, Riddick, M, and Garay, A. The endless quarantine: the impact of the COVID-19 outbreak on healthcare workers after three months of mandatory social isolation in Argentina. Sleep Med. (2020) 76:16–25. doi: 10.1016/j.sleep.2020.09.022
45. Hwang, TJ, Rabheru, K, Peisah, C, Reichman, W, and Ikeda, M. Loneliness and social isolation during the COVID-19 pandemic. Int Psychogeriatr. (2020) 32:1217–20. doi: 10.1017/S1041610220000988
46. Debnath, PR, Islam, MS, Karmakar, PK, Sarker, R, Zhai, ZW, and Potenza, MN. Mental health concerns, insomnia, and loneliness among intern doctors amidst the COVID-19 pandemic: evidence from a large tertiary Care Hospital in Bangladesh. Int J Ment Health Addict. (2021) 21:1799–819. doi: 10.1007/s11469-021-00690-0
47. Stubbs, JM, and Achat, HM. Are healthcare workers particularly vulnerable to loneliness? The role of social relationships and mental well-being during the COVID-19 pandemic. Psychiatry Res Commun. (2022) 2:100050. doi: 10.1016/j.psycom.2022.100050
48. Smaling, HJA, Tilburgs, B, Achterberg, WP, and Visser, M. The impact of social distancing due to the COVID-19 pandemic on people with dementia, family carers and healthcare professionals: a qualitative study. Int J Environ Res Public Health. (2022) 19:19. doi: 10.3390/ijerph19010519
49. Schwartz, J, King, CC, and Yen, MY. Protecting healthcare workers during the coronavirus disease 2019 (COVID-19) outbreak: lessons from Taiwan’s severe acute respiratory syndrome response. Clin Infect Dis. (2020) 71:858–60. doi: 10.1093/cid/ciaa255
50. Aljondi, R, Alghamdi, SS, Abdelaziz, I, Bushara, L, Alghamdi, S, Aljehani, A, et al. Knowledge of COVID-19 infection control among healthcare workers in radiology departments in Saudi Arabia. Med Sci. (2021) 14:51–60. doi: 10.1080/16878507.2020.1856587
51. Wee, LE, Sim, XYJ, Conceicao, EP, Aung, MK, Goh, JQ, Yeo, DWT, et al. Containment of COVID-19 cases among healthcare workers: the role of surveillance, early detection, and outbreak management. Infect Control Hosp Epidemiol. (2020) 41:765–71. doi: 10.1017/ice.2020.219
52. Kumar, R, Alabdulla, M, Elhassan, NM, and Reagu, SM. Qatar healthcare workers’ COVID-19 vaccine hesitancy and attitudes: a national cross-sectional survey. Front Public Health. (2021) 9:727748. doi: 10.3389/fpubh.2021.727748
53. Shekhar, R, Sheikh, AB, Upadhyay, S, Singh, M, Kottewar, S, Mir, H, et al. COVID-19 vaccine acceptance among health care workers in the United States. Vaccines. (2021) 9:119. doi: 10.3390/vaccines9020119
54. MacDonald, NE, Comeau, J, Dubé, È, Graham, J, Greenwood, M, Harmon, S, et al. Royal society of Canada COVID-19 report: enhancing COVID-19 vaccine acceptance in Canada. Facets. (2021) 6:1184–246. doi: 10.1139/facets-2021-0037
55. Driggin, E, Madhavan, MV, Bikdeli, B, Chuich, T, Laracy, J, Biondi-Zoccai, G, et al. Cardiovascular considerations for patients, health care workers, and health systems during the COVID-19 pandemic. J Am Coll Cardiol. (2020) 75:2352–71. doi: 10.1016/j.jacc.2020.03.031
56. Nohl, A, Afflerbach, C, Lurz, C, Brune, B, Ohmann, T, Weichert, V, et al. Acceptance of COVID-19 vaccination among front-line health care workers: a nationwide survey of emergency medical services personnel from Germany. Vaccines. (2021) 9:9. doi: 10.3390/vaccines9050424
57. Shahrour, G, and Dardas, LA. Acute stress disorder, coping self-efficacy and subsequent psychological distress among nurses amid COVID-19. J Nurs Manag. (2020) 28:1686–95. doi: 10.1111/jonm.13124
58. Al-Hanawi, MK, Mwale, ML, Alshareef, N, Qattan, AMN, Angawi, K, Almubark, R, et al. Psychological distress amongst health workers and the general public during the COVID-19 pandemic in Saudi Arabia. Risk Manag Healthc Policy. (2020) 13:733–42. doi: 10.2147/RMHP.S264037
59. Carlucci, L, D’Ambrosio, I, and Balsamo, M. Demographic and attitudinal factors of adherence to quarantine guidelines during COVID-19: the Italian model. Front Psychol. (2020) 11:559288. doi: 10.3389/fpsyg.2020.559288
60. Regenold, N, and Vindrola-Padros, C. Gender matters: a gender analysis of healthcare workers’ experiences during the first COVID-19 pandemic peak in England. Soc Sci. (2021) 10:43. doi: 10.3390/socsci10020043
61. Alhofaian, A, Tunsi, A, Alaamri, MM, Babkair, LA, Almalki, GA, Alsadi, SM, et al. Perception of heath care providers about COVID-19 and its vaccination in Saudi Arabia: cross-sectional study. J Multidiscip Healthc. (2021) 14:2557–63. doi: 10.2147/JMDH.S327376
62. Al-Sowygh, ZH. Academic distress, perceived stress and coping strategies among dental students in Saudi Arabia. Saudi Dent J. (2013) 25:97–105. doi: 10.1016/j.sdentj.2013.05.002
63. Peterson, BD, Pirritano, M, Block, JM, and Schmidt, L. Marital benefit and coping strategies in men and women undergoing unsuccessful fertility treatments over a 5-year period. Fertil Steril. (2011) 95:1759–1763.e1. doi: 10.1016/j.fertnstert.2011.01.125
64. Lee, Y, and Tang, F. More caregiving, less working: caregiving roles and gender difference. J Appl Gerontol. (2015) 34:465–83. doi: 10.1177/0733464813508649
65. Patel, N, Trikha, A, Aggarwal, R, Bhatia, R, Kumar, S, Ganesh, R, et al. Coping strategies among healthcare workers directly involved in coronavirus disease-2019 Care in a Tertiary Care Hospital in India. Ind J Priv Psychiatry. (2023) 17:4–9. doi: 10.5005/jp-journals-10067-0126
66. Tan, BYQ, Chew, NWS, Lee, GKH, Jing, M, Goh, Y, Yeo, LLL, et al. Psychological impact of the COVID-19 pandemic on health care workers in Singapore. Ann Intern Med. (2020) 173:317–20. doi: 10.7326/M20-1083
67. Özçevik Subaşi, D, Akça Sümengen, A, Şimşek, E, and Ocakçı, AF. Healthcare workers’ anxieties and coping strategies during the COVID-19 pandemic in Turkey. Perspect Psychiatr Care. (2021) 57:1820–8. doi: 10.1111/ppc.12755
68. Ali, A, and Kumar, S. Indian healthcare workers’ issues, challenges, and coping strategies during the COVID-19 pandemic: a cross-sectional study. Int J Environ Res Public Health. (2023) 20:3661. doi: 10.3390/ijerph20043661
69. Linzer, M, Stillman, M, Brown, R, Taylor, S, Nankivil, N, Poplau, S, et al. Preliminary report: US physician stress during the early days of the COVID-19 pandemic. Mayo Clin Proc Innov Qual Outcomes. (2021) 5:127–36. doi: 10.1016/j.mayocpiqo.2021.01.005
70. Somville, F, Vanspringel, G, De Cauwer, H, Franck, E, and Van Bogaert, P. Work stress-related problems in physicians in the time of COVID-19. Int J Occup Med Environ Health. (2021) 34:373–83. doi: 10.13075/ijomeh.1896.01674
71. Du, J, Dong, L, Wang, T, Yuan, C, Fu, R, Zhang, L, et al. Psychological symptoms among frontline healthcare workers during COVID-19 outbreak in Wuhan. Gen Hosp Psychiatry. (2020) 67:144–5. doi: 10.1016/j.genhosppsych.2020.03.011
Keywords: COVID-19, healthcare, workers, psychosocial, impact, Qatar
Citation: Al-Qudimat AR, Singh K, Mustafa E, Nashwan AJ, Al-Zoubi RM, Yassin A, Aboumarzouk OM and Al-Ansari A (2023) Psychosocial impact of COVID-19 pandemic: experience of healthcare workers in Qatar. Front. Public Health. 11:1283925. doi: 10.3389/fpubh.2023.1283925
Received: 27 August 2023; Accepted: 28 September 2023;
Published: 19 October 2023.
Edited by:
Juan Gómez-Salgado, University of Huelva, SpainReviewed by:
Assis Kamu, Universiti Malaysia Sabah, MalaysiaCopyright © 2023 Al-Qudimat, Singh, Mustafa, Nashwan, Al-Zoubi, Yassin, Aboumarzouk and Al-Ansari. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ahmad R. Al-Qudimat, YWFscXVkaW1hdEBoYW1hZC5xYQ==
†ORCID: Ahmad R. Al-Qudimat, https://orcid.org/0000-0003-1161-7244
Kalpana Singh, https://orcid.org/0000-0002-2273-5062
Abdulqadir J. Nashwan, https://orcid.org/0000-0003-4845-4119
Raed M. Al-Zoubi, https://orcid.org/0000-0002-0548-429X
Aksam Yassin, https://orcid.org/0000-0001-5457-3443
Omar M. Aboumarzouk, https://orcid.org/0000-0002-7961-7614
Abdulla Al-Ansari, https://orcid.org/0000-0002-6242-5667
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.