
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health , 13 November 2023
Sec. Aging and Public Health
Volume 11 - 2023 | https://doi.org/10.3389/fpubh.2023.1282461
Aims: This research sought to assess the perceived levels of participation and autonomy in senior patients who had received total hip arthroplasty (THA) or total knee arthroplasty (TKA) in Hangzhou, China. Furthermore, the study aimed to identify the factors linked to these outcomes.
Study design: This investigation will utilize a cross-sectional study design to assess perceived participation and autonomy among older adults total hip arthroplasty (THA) and total knee arthroplasty (TKA) patients. The research was conducted in Hangzhou, China, at a tertiary hospital.
Methods: Convenient sampling was utilized to select 139 patients who underwent THA or TKA between March 2022 and March 2023 and met the inclusion criteria at a tertiary hospital in Hangzhou. The Impact on Participation and Autonomy Questionnaire, Hip/Knee Injury and Osteoarthritis Outcome Score (HOOS/KOOS), 5-Item Geriatric Depression Scale, Multidimensional Scale of Perceived Social Support, and Elders Health Empowerment Scale were used to assess perceived participation, hip/knee-related symptoms and functional restrictions, depression symptoms, social support, and health empowerment.
Results: The mean score for perceived participation and autonomy was 22.554 (SD: 13.042). The mean scores for participation in indoor autonomy, outdoor autonomy, family roles, and social relations were 0.654 (SD: 0.608), 1.324 (SD: 0.792), 1.053 (SD: 0.657), and 0.664 (SD: 0.542), respectively. Negative correlations were observed between perceived participation/autonomy scores and HOOS/KOOS, social support, and health empowerment scores. Conversely, a positive correlation was found between perceived participation/autonomy scores and depression scores. The detrimental effect of HOOS/KOOS, social support, and health empowerment scores on perceived participation and autonomy was notable, while the impact of depressive symptoms was comparatively minor.
Conclusion: Older Chinese patients, at first six months post THA/TKA surgery, reported higher levels of perceived participation compared to individuals with other conditions, such as stroke patients. Functional limitations resulting from hip/knee-related symptoms, as well as social support and health empowerment, emerged as significant influencing factors for perceived participation and autonomy. This research enhances our comprehension of the elements influencing perceived participation among older adults individuals who have undergone THA/TKA procedures.
The frequency of Total Hip Arthroplasty (THA) and Total Knee Arthroplasty (TKA) procedures has surged rapidly, driven by the significant growth of the older adults population in China and other countries. Model forecasts project a staggering 176% increase in THA cases and a 139% rise in TKA cases by the year 2040 (1). However, despite this surge in surgeries, many patients exhibit disappointingly modest levels of postoperative activity. Following the surgical procedures, a substantial 20% of patients experience social isolation, and a range of 7 to 23% encounter persistent long-term discomfort (2). Furthermore, individuals requiring THA or TKA are increasingly concerned about their ability to return to work and actively participate in society (3).
A more complete approach to recovery will involve looking at a lot of different outcome measures that show physical and mental impairments, activity limitations, and participation restrictions, as shown in the International Classification of Functioning (ICF) model at different follow-up points (4).
Therefore, there is a pressing need for research into factors associated with involvement in order to encourage full participation of patients following TKA or THA.
Until now, the focus has predominantly been on assessing hip or knee function and a limited set of activities such as mobility and walking. The majority of studies have primarily examined the connections between participation and rehabilitation outcomes in the assessment of THA or TKA participation (5, 6). Factors influencing patients’ participation have often been investigated using objective indicators, such as different surgical approaches and physiological function (6–8). However, participation after a THA or TKA can be influenced by a number of factors. Sergooris et al. (9) indicated depression, social support, self-efficacy, and other characteristics may be connected to activities and engagement after total hip arthroplasty (THA). Maxwell et al. (10) showed that reduced participation was linked to females, depressed symptoms, and significant knee pain in either knee. Hylkema et al. (11) illustrated that among working-age TKA patients, activity, mental, and physical limitations have a substantial impact on participation constraints. Overall, it is significant to highlight that the evidence for those relationship varies at different periods among different articles. Diverse research have shown inconsistent results.
The long-term effects of psychological and social functioning are crucial for postoperative patients, according to the biopsychosocial model, in addition to the physical recovery (12, 13). Especially in empowerment, Patients who have a high level of health empowerment frequently have greater self-care skills and self-efficacy in rehabilitation (14). Caillouet et al. (15) discovered that health empowerment could encourage positive health behaviors, such as exercise, among community-dwelling older adults individuals.
In conclusion, there is a need for exploratory studies focusing on participation among THA or TKA patients following surgery, with health empowerment, depression, and perceived social support potentially shedding light on participation dynamics. However, the majority of existing research on participation recovery after THA or TKA predominantly centers on Western populations. Hence, the aim of this study is to identify the variables associated with perceived participation among THA or TKA patients at first six months post-surgery in China.
The main aim of this study was to evaluate the perceived levels of participation and autonomy among Chinese patients who had undergone Total Hip Arthroplasty (THA) or Total Knee Arthroplasty (TKA).
This study employed an exploratory cross-sectional research design.
Subjects were enlisted from the orthopedic division of a hospital graded as 3A, in accordance with the Hospital Grading Management Measures and pertinent regulations governing medical establishments in mainland China. Eligibility criteria for potential participants were as follows: (a) age 60 years or older, (b) underwent primary THA or TKA surgery, (c) which is at first 6-month had passed since the surgery, (d) capable of completing the surveys in Chinese both physically and cognitively, and (e) provided informed consent to participate in the study after being duly informed and signing the informed consent form. Exclusion criteria encompassed patients who: (a) underwent contralateral TKA or contralateral THA within six months prior to the surgery, (b) had various ailments that impeded walking, (c) were significantly organ dysfunctional or critically ill, and (d) were diagnosed with mental illnesses. Sample size = number of dimensions for main variable * (5–10)/(100%–10%) =14 * (5–10)/(100%–10%) = [78 ~ 156] (16).
Data collection was conducted between March 2022 and March 2023 at a tertiary hospital located in Hangzhou. Prior to commencing the investigation, all investigators underwent a comprehensive briefing regarding the study’s inclusion and exclusion criteria, effective communication techniques, and data collection procedures. Following obtaining informed consent, participants were provided with survey instructions. Subsequently, communication was established with the patients through phone calls or WeChat, a widely-used social media and messaging application in China, to gain insights into their condition and arrange outpatient follow-up appointments. Surveys were administered and data was collected from participants through a combination of phone or WeChat communication and in-person visits to the hospital.
This research design, participant recruitment criteria, and data collection methods aimed to comprehensively explore the perceived participation and autonomy levels among Chinese THA and TKA patients, shedding light on their experiences and factors influencing their postoperative outcomes.
The IPA, developed by Dutch researchers Cardol et al. (17), was employed to gauge patients’ perceived participation and autonomy. In this study, the Chinese version of IPA (C-IPA) was utilized to assess patients’ perceived participation levels. C-IPA comprises four dimensions: autonomy indoors (seven items), autonomy outdoors (five items), social life and relations (six items), and family role (seven items). Respondents rate each item on a 5-point Likert scale ranging from 0 (completely consistent) to 4 (completely inconsistent). Higher scores indicate greater levels of perceived participation, generating a total score between 0 and 100 (18). The Cronbach’s alpha values for each domain of IPA-Chinese have been reported to range from 0.81 to 0.91 across diverse demographics, including stroke and burns patients (19, 20).
The HOOS and KOOS instruments are self-administered questionnaires employed for evaluating symptoms and functional limitations related to the hip or knee. The HOOS, consisting of 40 items, assesses five patient-centered domains: pain (10 items), symptoms encompassing stiffness and range of motion (5 items), activity limitations in daily living (17 items), sport and recreational function (4 items), and hip-related quality of life (4 items) (21). Similarly, the KOOS consists of five domains: pain (9 items), symptoms (7 items), activities of daily living (17 items), sport and leisure function (5 items), and knee-related quality of life (4 items) (22). The score for each domain is calculated by summing individual item scores, which range from 0 to 4. These subscale scores are then transformed to a scale of 0 (indicating no issues) to 100 (indicating severe problems). Notably, the HOOS has demonstrated strong reliability, as indicated by intra-class correlations ranging from 0.75 to 0.97 and Cronbach’s alpha values of 0.82 to 0.98 (23–26). Each HOOS-Chinese dimension has a Cronbach’s alpha value between 0.865 to 0.968 (27). The Cronbach’s alpha values for each KOOS-Chinese dimension range from 0.80 to 0.94 (28).
The GDS-5, derived from the GDS-15, evaluates depressive symptoms in the older adults. Respondents provide scores of 0 or 1 for each of the five items, which are then summed to indicate symptom intensity. Scores of 2 or higher indicate the presence of symptoms, while scores of 0 or 1 suggest their absence (29). GDS-5 has strong test–retest and interrater reliability, with scores of 0.88 and 0.84, respectively (29). The Cronbach’s alpha coefficient of GDS-5 in Chinese was between 0.603–0.61 (30, 31).
The MSPSS, comprising 12 items, evaluates individuals’ perceptions of their social networks, encompassing family support (items 3, 4, 8, and 11), friend support (items 6, 7, 9, and 12), and significant other support (items 1, 2, 5, and 10). Using a 7-point Likert scale to gauge agreement, higher scores (ranging from 12 to 94) denote stronger perceived social support (32). The Chinese version of the MSPSS has consistently demonstrated reliability across diverse samples (33).
The EHES, developed by Park and Park (34), is designed to assess the older adults’s capacity to manage health-related matters. The Chinese version of EHES (C-EHES) consists of eight items, representing seven health empowerment facets: control, problem-solving, decision-making, self-motivation, psychosocial coping, resource utilization, and self-efficacy. C-EHES items are rated on a 5-point Likert scale, where higher scores (ranging from 8 to 40) indicate greater levels of health empowerment. The EHES has exhibited a Cronbach’s alpha value of 0.80 (34). The Cronbach’s alpha coefficient of Chinese version of EHES is 0.838 (35).
A custom-designed questionnaire was utilized to gather demographic and clinical information, encompassing gender, age, educational attainment, marital status, place of residence, sources of income, monthly income, type of surgery, existing comorbidities, apprehension about falling, additional complications, and presence of painful joints in other regions.
The Ethics Review Board of Zhejiang Provincial People’s Hospital granted approval for this study. Participants were assured that their involvement would have no adverse repercussions for them or their loved ones and that participation was entirely voluntary. All participants provided written consent before participating.
Statistical analysis was performed using SPSS 26.0 software, encompassing descriptive analysis, Spearman/Pearson correlation analysis, and multiple linear regression. Mean and standard deviation (SD) for each IPA domain were calculated. Relationships between perceived participation and quantitative factors (hip/knee-related symptoms and functional restrictions, depressive symptoms, social support, and health empowerment) were assessed through Spearman/Pearson correlation analysis. Correlational variables were incorporated into multiple linear regression analysis.
All researchers, nursing major in graduate students, received training on research ethics, participant recruitment, and standard operating procedures. Confidentiality and anonymity were maintained to minimize self-reported bias. Questionnaires were promptly reviewed for completeness after each administration. To ensure accuracy, two researchers independently cross-checked interview data entry. Data were coded for analysis purposes and the data’s consistency was examined.
A total of 139 patients participated in the study (see Table 1). With 65.25% more female participants than male participants, there is a sizable gender gap. According to the participants’ age distribution, 48.20% are between the ages of 60 and 69, followed by 42.45% between the ages of 70 and 79, and just 9.35% are 80 or older. Indicating poorer educational attainment, a sizable portion of participants (35.25%) are illiterate and 34.53% have only finished elementary school. The proportion of participants who are single, divorced, or widowed is smaller than the proportion who are married (82.01%) 0.33.09% of participants live in urban regions, compared to 66.91% who live in rural areas. Among the surgical treatments, total knee arthroplasty is slightly more frequent (56.83%) than total hip arthroplasty. The majority of individuals (62.59%) report having a fear of falling, compared to 37.41% who do not.87.05% of patients had no extra issues, compared to 12.95% who did. Fewer people (69.06%) report having one or more additional joint pains, with the remainder reporting none at all.
Table 2 descriptive statistics are presented in the format “Mean Standard Deviation (Min, Max),” with corresponding variable descriptions. The mean score for perceived participation and autonomy was 22.554 (SD: 13.042), in contrasting their mean results, the highest one is participation in autonomy outdoors followed by participation in family role, participation in social relations, and participation in autonomy indoors, representing a ranking of involvement level in reverse. The average HOOS/KOOS score was 390.052 (SD: 62.962), while depression symptom scores averaged 0.583 (SD: 1.221). Social support received a mean score of 58.165 (SD: 8.984), and health empowerment yielded a mean score of 28.849 (SD: 5.595).
Table 3 outlines the correlations between IPA scores and various factors. Noteworthy IPA-significant correlations were observed with factors including HOOS/KOOS (r = −0.587, p < 0.01). Depression symptoms (r = 0.426, p < 0.01), Social support (r = −0.477, p < 0.01), and Health empowerment (r = −0.565, p < 0.01).
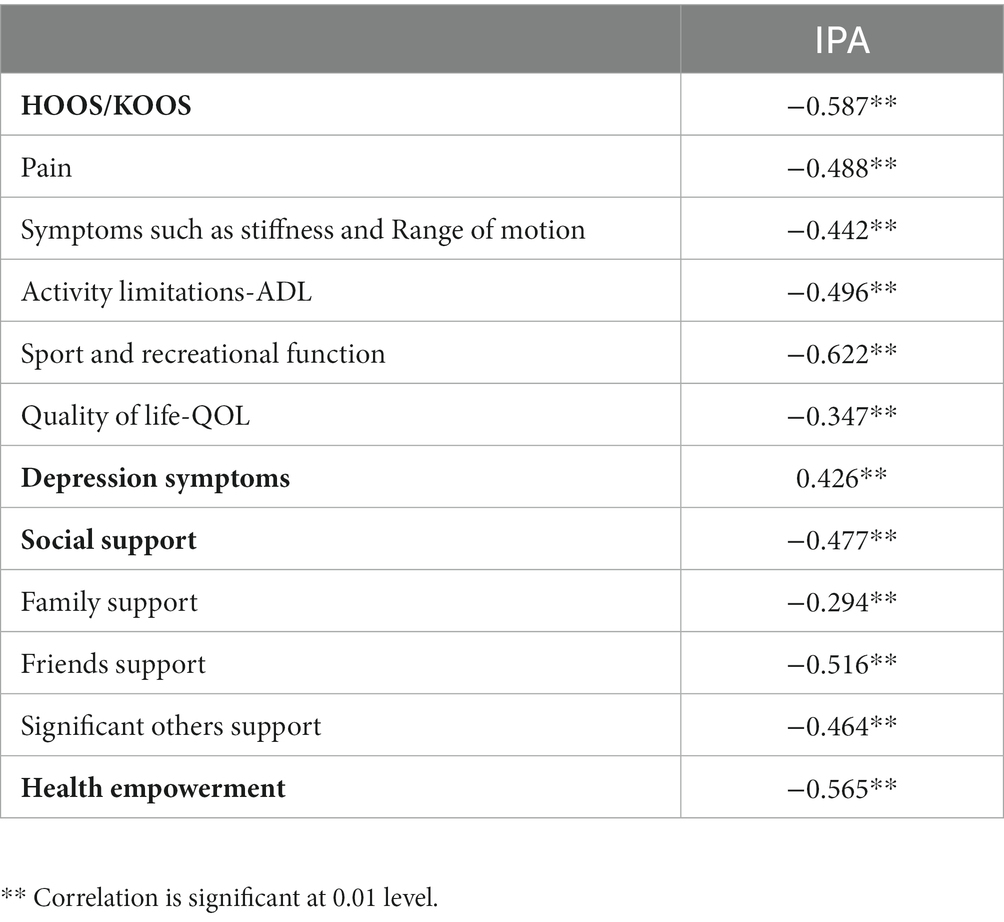
Table 3. Correlation between the perceived participation and HOOS/KOOS, depression systems, social support, and health empowerment.
Table 4 predictors of perceived participation were analyzed through multiple linear regression. Notable predictors included HOOS/KOOS (β = −0.446, p < 0.01), Social support (β = −0.217, p = 0.002), and Health empowerment (β = −0.266, p < 0.01).
The study’s results reveal significant associations and predictors of perceived participation and autonomy among older adults THA & TKA patients, offering insights into the factors influencing their postoperative experiences.
Following THA & TKA, an examination of perceived participation was conducted, encompassing its levels and potential determinants.
The average score for perceived participation and autonomy was lower than the findings in Chen et al.’s study (20).
Six months post-surgery, patients in our study demonstrated improved perceived participation compared to research outcomes pertaining to other conditions. Within our study, THA & TKA patients reported higher levels of perceived participation in social interactions and indoor autonomy in comparison to their reported participation in family roles and outdoor autonomy. This discrepancy can be attributed to a combination of factors. On one hand, the older adults patients who underwent hip and knee joint replacement in this study may be more socially engaged due to their enhanced self-esteem and the fulfillment of their desire for respect through positive interactions with family, neighbors, and friends. On the other hand, limitations in joint flexibility and stiffness resulting from hip and knee joint replacement surgery, particularly among older patients, could affect their ability to engage in outdoor activities. Concerns related to safety and the fear of falling might lead patients to prioritize lower-intensity activities that align with their sense of self-identity and value, such as childcare and housekeeping. Consequently, their participation in outdoor activities might decrease (36).
Healthy providers require a reliable resource to identify factors indicative of participation following THA & TKA, aiding in the efficient assessment of high-risk patients with limited participation and guiding care provision. As anticipated, the occurrence of symptoms, functional limitations and Infectious complication associated with the hip and knee stood out as strong indicators of participation (11, 37–38). Therefore, in the context of fostering participation, it is crucial to focus on the early restoration of hip/knee-related symptoms, functional limitations and infectious prevention post-THA & TKA surgery. Orthopedic nursing should encompass teaching THA & TKA-related rehabilitation techniques to facilitate swift and sustained recovery. Besides, the use of prophylactic antibiotics prior to surgery, the application of the asepsis principle throughout the procedure, and the symptoms of postoperative infection should all be thoroughly monitored. It is also important to acknowledge that partial two-stage revision procedures have a beneficial effect on persistent joint replacement infections (38).
Health empowerment is another determinant of patients’ degree of perceived participation and autonomy.
Aligning with findings from studies involving older adults individuals engaged in physical activity within community settings (15). An exploration of causative factors suggests that older adults patients who have undergone hip and knee joint replacement surgery experience an increased motivation for self-health management and participation six months after achieving substantial recovery of physical function and structure. This enhanced motivation propels greater engagement in physical activity, subsequently boosting social interaction levels (15, 39).
Therefore, healthcare providers can learn more about their patients’ post-operative experiences by using qualitative research techniques. Mindfulness treatment and psychological simulation training (including motor imagery and motor observation) can be effectively administered after surgery with the help of honest patient feedback (40, 41). The patient’s sense of agency and ability to care for themselves may increase as a result.
Our conclusion regarding the relationship between social support and engagement resonates with existing research, encompassing studies involving stroke patients (42) and other populations (43). This relationship could stem from the material and emotional support provided by family, friends, and relatives, satisfying patients’ emotional needs and bolstering treatment adherence. Consequently, their confidence in social interaction is heightened (43). As licensed healthcare professionals, nurses play a pivotal role in offering patients nursing care and education, while acting as a crucial link to medical practitioners such as surgeons, physical therapists, home healthcare providers, and social services (44). Therefore, nurses must comprehend how social support from diverse sources impacts the level of social engagement among older adults patients who have undergone hip and knee joint replacement surgery (42, 43). However, the potential impact of host-related factors in these situations must be taken into account. Doctors must unavoidably tell patients to the fullest extent practicable about all relevant risks and potential benefits associated with the procedure, as well as any potential challenges in the management of postoperative recovery. The choice of joint materials and the possibility of postoperative joint wear are also included in this (45).
Additionally, healthy providers can perform proper clinical management and risk stratification to prevent postoperative infection, which can also help to minimize medical litigation (37). Furthermore, nurses can enhance health education guidance for family members, elevating disease and recovery awareness among older patients’ families and caregivers, thereby strengthening internal family support. Consequently, they can better manage the condition collectively, ultimately boosting patients’ confidence in social interaction. Alongside knowledge about the social support system, nurses can also furnish accessible information and educational materials regarding social services. They can effectively harness community resources while actively organizing community events. By guiding patients towards senior activity centers or local parks, nurses can further harness social support and enhance social contact and communication (39). Notably, depression symptoms were not observed to impact patients’ participation levels six months post-surgery in this investigation. This might be attributed to the fact that individuals with pre-existing depression who underwent joint replacement surgery reported diminished depressive symptoms. This improvement could be attributed to the surgery-induced enhancement in joint function and reduction of unfavorable symptoms such as pain (11, 46).
Furthermore, this study included remote follow-up for patients who had joint replacements. In addition to ensuring continuity of treatment, remote healthcare offers a fresh approach to addressing patients’ post-operative recovery demands and consequently raising their post-operative satisfaction. Therefore, in the future, it will be crucial to integrate and foster synergy among financial, organisational, human, and technological resources through national or regional digital health initiatives, under well-structured strategic leadership (47). To ensure the applicability and efficacy of remote healthcare, special emphasis should be given to the creation of pertinent rules and regulations and adherence to ethical standards (48).
Limitations of this study include a sample drawn from a single center, potential subjective biases due to assistance needed from family members for data collection, and a focus on a less educated older adults population. Future research could explore perceived participation among patients with different joint replacements through a stratified approach and develop detailed relationship descriptions using trajectory models.
Following THA & TKA, participation and autonomy encompass intricate concepts influenced by multiple factors. The recuperation of hip/knee-related symptoms, functional limitations, social support, and health empowerment assumes pivotal significance. In nursing practice, heightened focus should be placed on older patients vulnerable to reduced engagement. By addressing patient concerns through interventions like health empowerment, bolstering social support, and imparting comprehensive hip and knee knowledge through health education, nurses can play a more proactive role in advancing the rehabilitation of THA and TKA among the older adults.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving humans were approved by Department of Orthopedics, Zhejiang Provincial People’s Hospital. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants’ legal guardians/next of kin.
LY: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Software, Writing – original draft, Writing – review & editing. QJ: Supervision, Writing – review & editing. JW: Data curation, Writing – original draft. YC: Conceptualization, Software, Writing – original draft. CG: Conceptualization, Methodology, Writing – original draft. YW: Conceptualization, Investigation, Writing – review & editing. KL: Validation, Writing – review & editing. ML: Formal analysis, Data curation, Writing – original draft.
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Shichman, I, Roof, M, Askew, N, Nherera, L, Rozell, JC, Seyler, TM, et al. Projections and epidemiology of primary hip and knee arthroplasty in medicare patients to 2040-2060. JBJS Open Access. (2023) 8:e22.00112. doi: 10.2106/JBJS.OA.22.00112
2. Bandholm, T, Wainwright, TW, and Kehlet, H. Rehabilitation strategies for optimisation of functional recovery after major joint replacement. J Exp Orthop. (2018) 5:44. doi: 10.1186/s40634-018-0156-2
3. Rondon, AJ, Tan, TL, Greenky, MR, Kheir, MM, Foltz, L, and Purtill, JJ. Return to Work After Total Joint 3. Arthroplasty: A Predictive Model. Orthopedics. (2020) 43:415–420. doi: 10.3928/01477447-20200619-12
4. Huang, SW, Chen, YW, Escorpizo, R, Liao, CD, and Liou, TH. Development international classification of functioning, disability and health core set for post total knee replacement rehabilitation program: Delphi-based consensus study in Taiwan. Int J Environ Res Public Health. (2021) 18:1630. doi: 10.3390/ijerph18041630
5. Meng, Y, Deng, B, Liang, X, Li, J, Li, L, Ou, J, et al. Effectiveness of self-efficacy-enhancing interventions on rehabilitation following total hip replacement: a randomized controlled trial with six-month follow-up. J Orthop Surg Res. (2022) 17:225. doi: 10.1186/s13018-022-03116-2
6. Arshi, A, Khan, IA, Ciesielka, KA, Cozzarelli, NF, and Fillingham, YA. Participation in sports and physical activities after total joint arthroplasty. J Arthroplast. (2023) 38:806–814.e5. doi: 10.1016/j.arth.2022.11.008
7. Latijnhouwers, D, Laas, N, Verdegaal, SHM, Nelissen, RGHH, Vliet Vlieland, TPM, Kaptijn, HH, et al. Activities and participation after primary total hip arthroplasty; posterolateral versus direct anterior approach in 860 patients. Acta Orthop. (2022) 93:613–22. doi: 10.2340/17453674.2022.3149
8. Matsunaga-Myoji, Y, Fujita, K, Makimoto, K, Tabuchi, Y, and Mawatari, M. Three-year follow-up study of physical activity, physical function, and health-related quality of life after total hip arthroplasty. J Arthroplast. (2020) 35:198–203. doi: 10.1016/j.arth.2019.08.009
9. Sergooris, A, Verbrugghe, J, de Baets, L, Meeus, M, Roussel, N, Smeets, RJEM, et al. Are contextual factors associated with activities and participation after total hip arthroplasty? A systematic review. Ann Phys Rehabil Med. (2023) 66:101712. doi: 10.1016/j.rehab.2022.101712
10. Maxwell, JL, Keysor, JJ, Niu, J, Singh, JA, Wise, BL, Frey-Law, L, et al. Participation following knee replacement: the most cohort study. Phys Ther. (2013) 93:1467–74. doi: 10.2522/ptj.20130109
11. Hylkema, TH, Brouwer, S, Stewart, RE, van Beveren, J, Rijk, PC, Brouwer, RW, et al. Two-year recovery courses of physical and mental impairments, activity limitations, and participation restrictions after total knee arthroplasty among working-age patients. Disabil Rehabil. (2022) 44:291–300. doi: 10.1080/09638288.2020.1766583
12. Edwards, RR, Campbell, C, Schreiber, KL, Meints, S, Lazaridou, A, Martel, MO, et al. Multimodal prediction of pain and functional outcomes 6 months following total knee replacement: a prospective cohort study. BMC Musculoskelet Disord. (2022) 23:302. doi: 10.1186/s12891-022-05239-3
13. Engel, GL. The clinical application of the biopsychosocial model. Am J Psychiatry. (1980) 137:535–44. doi: 10.1176/ajp.137.5.535
14. Huang, TT, Sung, CC, Wang, WS, and Wang, BH. The effects of the empowerment education program in older adults with total hip replacement surgery. J Adv Nurs. (2017) 73:1848–61. doi: 10.1111/jan.13267
15. Caillouet, KA, and Cosio-Lima, L. Association of health empowerment and handgrip strength with intention to participate in physical activity among community-dwelling older adults. Exp Gerontol. (2019) 121:99–105. doi: 10.1016/j.exger.2019.04.001
16. Ni, P, Chen, JL, and Liu, N. The sample size estimation in quantitative nursing research. Chinese J Nurs. (2010) 45:378–80.
17. Berenschot, L, and Grift, Y. Validity and reliability of the (adjusted) impact on participation and autonomy questionnaire for social-support populations. Health Qual Life Outcomes. (2019) 17:41. doi: 10.1186/s12955-019-1106-0
18. Cardol, M, de Haan, RJ, van den Bos, GA, de Jong, BA, and de Groot, IJM. The development of a handicap assessment questionnaire: the impact on participation and autonomy (ipa). Clin Rehabil. (1999) 13:411–9. doi: 10.1191/026921599668601325
19. Li, L, Wu, XL, and Xu, L. Factors affecting self-perceived participation and autonomy among patients with burns: a follow-up study. Burns. (2018) 44:2064–73. doi: 10.1016/j.burns.2018.07.008
20. Chen, X, He, Y, Meng, X, Gao, C, Liu, Z, and Zhou, L. Perceived participation and its correlates among first-stroke survivors at six months after discharge from a tertiary hospital in China. Arch Phys Med Rehabil. (2018) 99:667–75. doi: 10.1016/j.apmr.2017.09.120
21. Nilsdotter, AK, Lohmander, LS, Klässbo, M, and Roos, EM. Hip disability and osteoarthritis outcome score (hoos)--validity and responsiveness in total hip replacement. BMC Musculoskelet Disord. (2003) 4:10. doi: 10.1186/1471-2474-4-10
22. Roos, EM, Roos, HP, Lohmander, LS, Ekdahl, C, and Beynnon, BD. Knee injury and osteoarthritis outcome score (koos)--development of a self-administered outcome measure. J Orthop Sports Phys Ther. (1998) 28:88–96. doi: 10.2519/jospt.1998.28.2.88
23. Klässbo, M, Larsson, E, and Mannevik, E. Hip disability and osteoarthritis outcome score. An extension of the western Ontario and mcmaster universities osteoarthritis index. Scand J Rheumatol. (2003) 32:46–51. doi: 10.1080/03009740310000409
24. de Groot, IB, Reijman, M, Terwee, CB, Bierma-Zeinstra, SMA, Favejee, M, Roos, EM, et al. Validation of the dutch version of the hip disability and osteoarthritis outcome score. Osteoarthr Cartil. (2007) 15:104–9. doi: 10.1016/j.joca.2006.06.014
25. Gojło, MK, and Paradowski, PT. Polish adaptation and validation of the hip disability and osteoarthritis outcome score (hoos) in osteoarthritis patients undergoing total hip replacement. Health Qual Life Outcomes. (2020) 18:135. doi: 10.1186/s12955-020-01390-4
26. Machado, RK, Casagrande, AA, Pereira, GR, Vissoci, JRN, Pietrobon, R, and Ferreira, APB. Hip disability and osteoarthritis outcome score (hoos): a cross-cultural validation of the brazilian portuguese version study. Rev Bras Ortop (São Paulo). (2019) 54:282–7. doi: 10.1055/s-0039-1691764
27. Wei, X, Wang, Z, Yang, C, Wu, B, Liu, X, Yi, H, et al. Development of a simplified chinese version of the hip disability and osteoarthritis outcome score (hoos): cross-cultural adaptation and psychometric evaluation. Osteoarthr Cartil. (2012) 20:1563–7. doi: 10.1016/j.joca.2012.08.018
28. Cheng, ASK, Chan, KC, Chan, SY, Fan, MK, Fung, MK, Lee, OY, et al. Cross-cultural adaptation and validation of the Hong Kong version of the knee injury and osteoarthritis outcome score (hk-koos) for patients with knee osteoarthritis. Occup Ther Int. (2019) 2019:1–9. doi: 10.1155/2019/8270637
29. Rinaldi, P, Mecocci, P, Benedetti, C, Ercolani, S, Bregnocchi, M, Menculini, G, et al. Validation of the five-item geriatric depression scale in elderly subjects in three different settings. J Am Geriatr Soc. (2003) 51:694–8. doi: 10.1034/j.1600-0579.2003.00216.x
30. Liu, X, Wang, C, Qiao, X, Si, H, and Jin, Y. Sleep quality, depression and frailty among chinese community-dwelling older adults. Geriatr Nurs. (2021) 42:714–20. doi: 10.1016/j.gerinurse.2021.02.020
31. Qiao, X, Ji, L, Si, H, Jin, Y, Bian, Y, Wang, W, et al. Validation and comparison of three short depression screening tools among chinese community-dwelling older adults. Res Gerontol Nurs. (2022) 15:283–91. doi: 10.3928/19404921-20220929-01
32. Brugnoli, AVM, Gonçalves, TR, Silva, R, and Pattussi, MP. Evidence of the validity of the multidimensional scale of perceived social support (mspss) in university students. Cien Saude Colet. (2022) 27:4223–32. doi: 10.1590/1413-812320222711.08592022
33. Guan, NC, Seng, LH, Hway Ann, AY, and Hui, KO. Factorial validity and reliability of the malaysian simplified chinese version of multidimensional scale of perceived social support (mspss-scv) among a group of university students. Asia Pac J Public Health. (2015) 27:225–31. doi: 10.1177/1010539513477684
34. Park, C, and Park, YH. Validity and reliability of korean version of health empowerment scale (k-hes) for older adults. Asian Nurs Res (Korean Soc Nurs Sci). (2013) 7:142–8. doi: 10.1016/j.anr.2013.07.004
35. Zhang, S, Wu, Y, Fu, Z, Lu, Y, Wang, Q, and Liu, M. Reliability and validity of the Chinese version of the simplified elders health empowerment ScalelJ. J Nurs Sci. (2018) 33:83–5.
36. Hawke, LJ, Taylor, NF, Dowsey, MM, Choong, PFM, and Shields, N. In the dark about physical activity – exploring patient perceptions of physical activity after elective total knee joint replacement: a qualitative study. Arthritis Care Res (Hoboken). (2022) 74:965–74. doi: 10.1002/acr.24718
37. Davis, AM, Perruccio, AV, Ibrahim, S, Hogg-Johnson, S, Wong, R, Streiner, DL, et al. The trajectory of recovery and the inter-relationships of symptoms, activity and participation in the first year following total hip and knee replacement. Osteoarthr Cartil. (2011) 19:1413–21. doi: 10.1016/j.joca.2011.08.007
38. Moreno-Romero, M, Ordas-Bayon, A, Gomez-Rice, A, Ortega, MA, and de la Torre Escuredo, BJ. Partial two-stage exchange for infected total hip arthroplasty: a treatment to take into account. J Pers Med. (2023) 13:137. doi: 10.3390/jpm13010137
39. Kim, YR, and Jung, HS. Effects of social interaction and depression on homeboundness in community-dwelling older adults living alone. Int J Environ Res Public Health. (2022) 19:3608. doi: 10.3390/ijerph19063608
40. Paravlic, AH, Tod, D, and Milanovic, Z. Mental simulation practice has beneficial effects on patients' physical function following lower limb arthroplasty: a systematic review and meta-analysis. Arch Phys Med Rehabil. (2020) 101:1447–61. doi: 10.1016/j.apmr.2020.04.004
41. Pester, BD, Wilson, JM, Yoon, J, Lazaridou, A, Schreiber, KL, Cornelius, M, et al. Brief mindfulness-based cognitive behavioral therapy is associated with faster recovery in patients undergoing total knee arthroplasty: a pilot clinical trial. Pain Med. (2023) 24:576–85. doi: 10.1093/pm/pnac183
42. Li, Y, Zhang, W, Ye, M, and Zhou, L. Perceived participation and autonomy post-stroke and associated factors: an explorative cross-sectional study. J Adv Nurs. (2021) 77:1293–303. doi: 10.1111/jan.14670
43. Evangelista, DG, Malaguti, C, Meirelles, FA, de Jesus, LAS, José, A, Cabral, LF, et al. Social participation and associated factors in individuals with chronic obstructive pulmonary disease on long-term oxygen therapy. COPD. (2021) 18:630–6. doi: 10.1080/15412555.2021.2005012
44. Goldsmith, LJ, Suryaprakash, N, Randall, E, Shum, J, MacDonald, V, Sawatzky, R, et al. The importance of informational, clinical and personal support in patient experience with total knee replacement: a qualitative investigation. BMC Musculoskelet Disord. (2017) 18:127. doi: 10.1186/s12891-017-1474-8
45. González-Bravo, C, Ortega, MA, Buján, J, de la Torre, B, and Barrios, L. Wear risk prevention and reduction in total hip arthroplasty. A personalized study comparing cement and cementless fixation techniques employing finite element analysis. J Pers Med. (2021) 11:780. doi: 10.3390/jpm11080780
46. Vajapey, SP, McKeon, JF, Krueger, CA, and Spitzer, AI. Outcomes of total joint arthroplasty in patients with depression: a systematic review. J Clin Orthop Trauma. (2021) 18:187–98. doi: 10.1016/j.jcot.2021.04.028
47. World Health Organization. Global strategy on digital health 2020–2025. Available at: https://www.who.int/health-topics/digital-health/#tab=tab_1 (Accessed September 1, 2022).
Keywords: aged, arthroplasty, replacement, participation, rehabilitation, daily living activities, psychological well-being
Citation: Yao L, Jia Q, Wu J, Chai Y, Gao C, Wang Y, Li K and Lai M (2023) Assessing perceived participation among older adults total hip arthroplasty and total knee arthroplasty patients six months post-surgery: a cross-sectional study. Front. Public Health. 11:1282461. doi: 10.3389/fpubh.2023.1282461
Received: 24 August 2023; Accepted: 26 October 2023;
Published: 13 November 2023.
Edited by:
Miguel A. Ortega, University of Alcalá, SpainReviewed by:
Begoña Polonio-López, University of Castilla-La Mancha, SpainCopyright © 2023 Yao, Jia, Wu, Chai, Gao, Wang, Li and Lai. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Qin Jia, anExMjI3QDE2My5jb20=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.