- 1Department of Angiology, HELIOS Klinikum Krefeld, Krefeld, Germany
- 2Department of Behavioural Science and Health, University College London, London, United Kingdom
- 3Department for Vascular and Thoracic Surgery, Städtisches Klinikum Karlsruhe gGmbH, Karlsruhe, Germany
1 Introduction
Considering the health harms of tobacco smoking, the primary aim of individual and population-level interventions should always be cigarette cessation [i.e., “tobacco use pattern which involves the cessation of smoking cigarettes,” defined by ADDICTO:0000649 (1)]. However, many smokers struggle to quit, and therefore replacing cigarettes with less harmful electronic nicotine delivery systems (ENDS) such as e-cigarettes can be helpful as a harm reduction strategy. While some people may switch completely, others might prefer dual use of combustible cigarettes and ENDS. Temporary dual use is not an argument against using ENDS as a smoking cessation aid. There is no clear scientific evidence that dual use either increases or decreases harmfulness beyond the level of combustible cigarette use. German guidelines on smoking and tobacco addiction recommend harm reduction through products with low toxicants emission, such as e-cigarettes, for people who smoke combustible cigarettes and are unable to quit smoking or do not want to (2). However, the guidelines also state that dual use leads to much less pronounced reduction in exposure to toxicants compared with completely switching to e-cigarettes. The authors conclude that there is a lack of evidence demonstrating the health impact of dual use due to limited studies in this area, which mostly suffer from methodological problems such as small sample sizes (2).
2 Add-on vs. displacement dual use
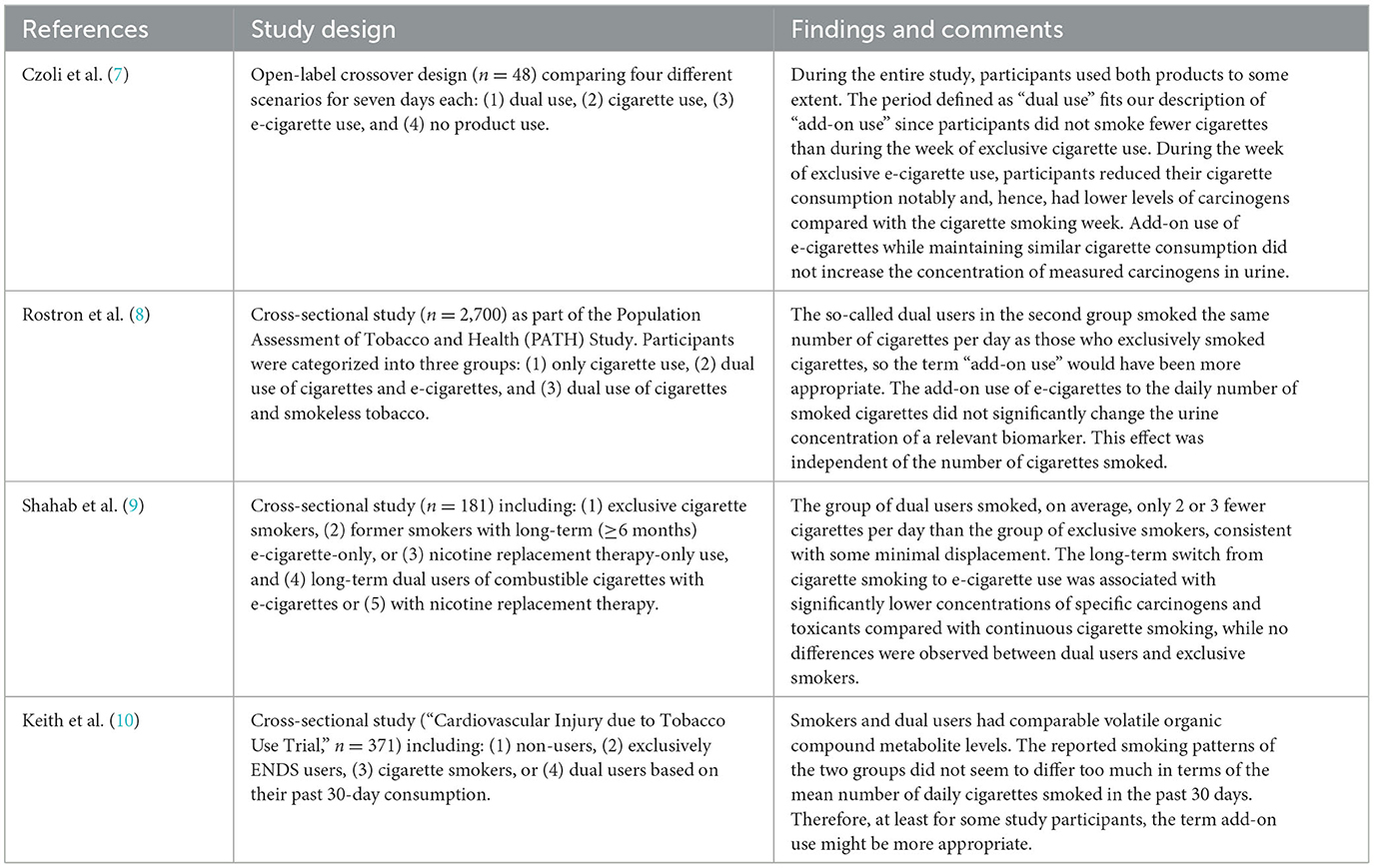
In contrast to the German guidelines' conclusions on dual use (2), Stokes et al. (3) observed no difference between dual users and those who exclusively smoked cigarettes based on biomarker data (inflammation and oxidative stress) of 7,130 US American adults who used combustible cigarettes, e-cigarettes, both, or none. Further, the researchers found no difference between adults who exclusively vaped and those who did not smoke or vape. Compared with regular cigarette smokers, vapers had significantly lower levels for almost all inflammatory and oxidative stress biomarkers (3). A secondary analysis of a Cochrane systematic review of trials of e-cigarettes for cigarette cessation also demonstrated that the biomarkers are lower when switching to e-cigarettes or dual use compared to combustible cigarette smoking (4). Nevertheless, critics of harm reduction repeatedly portray dual use as dangerous, and sometimes even more so than continued exclusive cigarette smoking (5, 6). By using the term “dual use,” guidelines suggest that there is a generally recognized definition of dual use that forms the basis of these studies and thus for guideline recommendations. However, this is not the case, as we will show below using the studies cited in the German guidelines [(7–10), see Table 1]. Rather, a distinction should be made between add-on use (where cigarette consumption is maintained but topped up with e-cigarettes, e.g., in situations that require temporary abstinence or similar) and displacement dual use (where some cigarettes are actually replaced by e-cigarettes) (11).
As the studies by Rostron et al. (8), Shahab et al. (9), and Keith et al. (10) were cross-sectional, it is unclear whether the behavior of dual users changed over time. It is possible that more dependent smokers may be more likely to become dual users and so actually reduce their higher cigarette consumption to levels similar to that of less dependent exclusive smokers. Longitudinal comparisons to assess changes in biomarkers have the advantage that researchers can follow up smokers before they start dual using. For example, Pasquereau et al. (12) followed up smokers (exclusive tobacco and dual use of tobacco and e-cigarettes) for 6 months. Those who used both products at baseline were more likely to reduce their cigarette consumption and attempt to quit smoking during the study than those who only smoked cigarettes at baseline. Kasza et al. (13) found that among smokers who were not intending to quit at baseline, those who started using e-cigarettes were more likely to stop smoking within 6 months than those who continued exclusively cigarette smoking. The same effect was observed with nicotine replacement therapy—when offered to smokers, even if they did not intend to quit, they were more likely to make a quit attempt than when not offered nicotine replacement therapy (14).
Using data from the Population Assessment of Tobacco and Health (PATH) Study conducted in the US between 2013 and 2014, Goniewicz et al. (15) observed two distinct usage groups among 792 dual users. One group smoked cigarettes and used e-cigarettes daily. This group could be labeled as add-on users. Another group used e-cigarettes daily but only smoked cigarettes on some days, so could be described as displacement dual users. The former group had significantly higher biomarker concentrations compared with the latter group. The authors concluded that the frequency of cigarette use among those consuming both products was positively correlated with nicotine and toxicant exposure (15). A study funded by Juul labs (an e-cigarette company) using the same PATH Study, but data collected in 2018/19, compared dual users who smoked <10 cigarettes per day (“displacement dual users”) to those who smoked at least 10 cigarettes per day (“add-on users”) (16). Toxicant levels of displacement dual users were lower than those of add-on users, while the levels of add-on users were comparable to exclusive cigarette smokers (16).
ENDS use is associated with a significant reduction in toxicants compared with the consumption of combustible cigarettes. The WHO, known to be rather critical of e-cigarettes, stated in its report on electronic nicotine and non-nicotine delivery systems (EN&NNDS): “There is conclusive evidence that: completely substituting EN&NNDS for combustible tobacco cigarettes reduces users' exposure to numerous toxicants and carcinogens present in combustible tobacco cigarettes; …” (17). The International Agency for Research on Cancer, which forms part of the WHO, states on their website (18): “E-cigarettes have the potential to reduce the enormous burden of disease and death caused by tobacco smoking if most smokers switch to e-cigarettes and public health concerns are properly addressed.” Despite this encouraging assessment, many consider the simultaneous consumption of combustion cigarettes and ENDS as harmful, and the risk of so-called dual use is cited as a strong argument against recommending ENDS use (5, 6). As stated above, the term dual use is not generally well-defined and negative effects of dual use beyond those of exclusive cigarette smoking have not been scientifically substantiated. One can speak of dual use in a completely neutral way when two products are used side by side. However, this is not suitable for scientific evaluation. It is important to distinguish between smokers who have not changed their cigarette smoking pattern but who additionally started using ENDS and those who replaced some of their combustible cigarette consumption through ENDS use. The former could be defined as “add-on use” and the latter as “displacement dual use.”
Add-on use, commonly associated with higher nicotine dependence (19, 20), is not recommended as it does not reduce the level of toxicants inhaled. In contrast, displacement dual use reduces the inhaled concentration of toxicants compared with obtaining the same amount of nicotine by smoking cigarettes exclusively (3, 4, 7–10). The idea of harm reduction in the context of smoking means that people should reduce their cigarette consumption as much as possible by switching to alternatives that contain less harmful toxicants. The publications summarized above have demonstrated that add-on use is not generally associated with an increased concentration of biomarkers (3, 4, 7–10). The measured values correlated with the number of combustible cigarettes consumed. With displacement dual use, on the other hand, the concentration of carcinogens in the urine decreased in line with the decrease in the number of combustible cigarettes smoked, suggesting that ENDS use did not measurably contribute to additional toxicant intake.
3 Displacement dual use as a cigarette cessation aid
The European Union and its member states have been trying for years to curb the consumption of tobacco and related products through different measures, including regulations, restrictions on advertising and sponsorship, smoke-free zones, and anti-smoking campaigns. The European Commission regularly conducts opinion polls to gauge Europeans' attitudes toward tobacco-related issues. These polls showed that e-cigarettes and heated tobacco products did not contribute to smoking uptake. A US study (21) using data from the Tobacco Use Supplement to Current Population Surveys and the National Health Interview Survey found that from 2014/2015 to 2018/2019, exclusive ENDS use increased while exclusive cigarette and dual use of ENDS and cigarettes decreased [in the US, dual use primarily fits our definition of add-on use (22, 23)]. In agreement with studies (12, 13) cited above, a 24-month study on the consumption of tobacco and e-cigarettes among young adult binge drinkers showed that dual use is often a transitional phase between cigarette smoking and cessation (24). The latent transition analysis revealed four distinct user patterns among young adults from the US and Canada: (1) exclusive e-cigarette use, (2) dual use, (3) exclusively combustible cigarette smoking, and (4) non-use. Most of the dual users switched to complete abstinence or to the exclusive consumption of e-cigarettes. For smokers who used only combustible cigarettes, the most common transition was abstinence, followed by those who remained in the group of combustible cigarette smoking. After 24 months, 63% of exclusive e-cigarette users transitioned to abstinence, 37% continued to use e-cigarettes, and none transitioned to dual or combustible cigarette use (24).
The German DEBRA study showed that e-cigarette use was associated with higher odds of successful quitting than nicotine replacement therapy use or no aid (25). A study from New Zealand assessed smoking and vaping patterns in people who smoked cigarettes but were not currently using ENDS or were using them less than once a week, not currently attempted to quit, and had never tried to quit through using ENDS for 30 days or more (26). Participants received an ENDS device at the beginning of the study and were asked to report their use over 20 weeks. Most participants reported different consumption levels of combustible cigarettes and ENDS throughout the study period, which also included phases of dual use. The authors concluded that the considerable diversity in alternate use observed within and between study participants suggests that the high variability is typical rather than exceptional. The transition from smoking to ENDS use may involve significant periods of dual use that are likely to be dynamic and may span several months (26).
In qualitative interviews, Notley et al. (27) found that some former smokers started using e-cigarettes without attempting to quit combustible cigarette smoking but slowly transitioned by replacing some of their cigarettes through e-cigarette use, and eventually found more pleasure in e-cigarettes than in combustible cigarettes. Because e-cigarette use, unlike other nicotine replacement products, can substitute psychological, psychosocial, and social aspects of combustible cigarette smoking, it may be more suitable to help some smokers quit cigarettes than other nicotine replacement products. In addition, e-cigarettes offer unique features for smoking relapse prevention (27, 28).
4 Conclusions
Unfortunately, there is no recognized definition of dual use in the scientific literature that differentiates between what we term add-on and displacement use dual use. The studies on the topic of dual use listed in the German guidelines on smoking and tobacco dependence illustrate this dilemma clearly. In most of these studies, what is referred to as dual use likely represents add-on use. At the same time, however, these studies also show that even add-on use, regardless of the form in which it is practiced, does not lead to higher levels of toxicant exposure for the consumer than consumption of combustible cigarettes alone. Dual use and add-on use are not the goals of cigarette cessation strategies. The primary goal is the complete cessation of cigarettes. From a health perspective, people would ideally quit all nicotine-containing products. However, for those who cannot achieve this, a full switch to ENDS makes sense, and temporary dual use is not a good argument against using ENDS as an aid to achieve abstinence from cigarette smoking, especially if it leads to later cessation of all nicotine-containing products. There is no scientific evidence that dual use is more harmful than combustible cigarette use if the number of cigarettes smoked remains the same. Therefore, we suggest that the adoption of agreed standards would help to evaluate the consequences of add-on and displacement dual use, respectively. A clearer differentiation would not just be of scientific value but could guide decision-making in clinical practice. Temporary displacement dual use should be evaluated differently than permanent displacement dual use or even add-on dual use. These dual users likely require a different approach to successfully achieve cigarette cessation. If research continues to show that displacement dual use reduces exposure to harmful toxicants compared to exclusive cigarette smoking and potentially increases chances of quit success, it should be recommended by guidelines as a harm reduction tool. After all, the aim of interventions should be to reduce the harm, with abstinence as an ultimate ideal but not a requirement.
Author contributions
KK: Conceptualization, Writing—original draft. VB: Writing—review & editing. LS: Writing—review & editing. MS: Writing—review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
LS reports receiving honoraria for talks, receiving an unrestricted research grant and travel expenses to attend meetings and workshops by pharmaceutical companies that make smoking cessation products (Pfizer and Johnson & Johnson), and acting as a paid reviewer for grant-awarding bodies and as a paid consultant for health care companies. He has never received personal fees or research funding of any kind from alcohol, electronic cigarette or tobacco companies.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. AddictOvocab. Cigarette Cessation [Internet]. London: AddictO (2020). Available online at: https://addictovocab.org/ADDICTO:0000649 (accessed October 23, 2023).
2. Andreas S, Batra A, Brüggmann D, Effertz T, Geyer D, Gohlke H, et al. S3-Leitlinie Rauchen und Tabakabhängigkeit: Screening, Diagnostik und Behandlung. Berlin (2021).
3. Stokes AC, Xie W, Wilson AE, Yang H, Orimoloye OA, Harlow AF, et al. Association of cigarette and electronic cigarette use patterns with levels of inflammatory and oxidative stress biomarkers among US adults. Circulation. (2021) 143:869–71. doi: 10.1161/CIRCULATIONAHA.120.051551
4. Hartmann-Boyce J, Butler AR, Theodoulou A, Onakpoya IJ, Hajek P, Bullen C, et al. Biomarkers of potential harm in people switching from smoking tobacco to exclusive e-cigarette use, dual use or abstinence: secondary analysis of Cochrane systematic review of trials of e-cigarettes for smoking cessation. Addiction. (2023) 118:539–45. doi: 10.1111/add.16063
5. Pankow W, Andreas S, Rupp A, Pfeifer M. Tabakentwöhnung mit E-zigarette? Eine ad-hoc-stellungnahme der deutschen gesellschaft für pneumologie und beatmungsmedizin e. v. (DGP). Pneumologie. (2021) 75:31–2. doi: 10.1055/a-1323-6045
6. Deutsche Gesellschaft für Pneumologie und Beatmungsmedizin. Empfehlungen zum Umgang mit der elektronischen Zigarette (E-Zigarette). Pneumologie. (2022) 76:473–78. doi: 10.1055/a-1862-3112
7. Czoli CD, Fong GT, Goniewicz ML, Hammond D. Biomarkers of exposure among “dual users” of tobacco cigarettes and electronic cigarettes in Canada. Nicotine Tobacco Res. (2018) 21:1259–66. doi: 10.1093/ntr/nty174
8. Rostron BL, Corey CG, Chang JT, van Bemmel DM, Miller ME, Chang CM. Associations of cigarettes smoked per day with biomarkers of exposure among U.S. adult cigarette smokers in the Population Assessment of Tobacco and Health (PATH) study wave 1 (2013–2014). Cancer Epidemiol Biomark Prevent. (2019) 28:1443–53. doi: 10.1158/1055-9965.EPI-19-0013
9. Shahab L, Goniewicz ML, Blount BC, Brown J, McNeill A, Alwis KU, et al. Nicotine, carcinogen, and toxin exposure in long-term e-cigarette and nicotine replacement therapy users. Ann Intern Med. (2017) 166:390–400. doi: 10.7326/M16-1107
10. Keith RJ, Fetterman JL, Orimoloye OA, Dardari Z, Lorkiewicz PK, Hamburg NM, et al. Characterization of volatile organic compound metabolites in cigarette smokers, electronic nicotine device users, dual users, and nonusers of tobacco. Nicotine Tobacco Res. (2019) 22:264–72. doi: 10.1093/ntr/ntz021
11. Kröger K. E-Zigaretten, Tabakerhitzer: Dual Use Oder Add On – Derzeit Ohne Definition. (2022). Available online at: https://www.der-niedergelassene-arzt.de/medizin/kategorie/gefaessmedizin-1/e-zigaretten-tabakerhitzer-dual-use-oder-add-on-derzeit-ohne-definition (accessed December 11, 2023).
12. Pasquereau A, Guignard R, Andler R, Nguyen-Thanh V. Electronic cigarettes, quit attempts and smoking cessation: a 6-month follow-up. Addiction. (2017) 112:1620–28. doi: 10.1111/add.13869
13. Kasza KA, Hammond D, Gravely S, O'Connor RJ, Meng G, East K, et al. Associations between nicotine vaping uptake and cigarette smoking cessation vary by smokers' plans to quit: longitudinal findings from the International Tobacco Control Four Country Smoking and Vaping Surveys. Addiction. (2023) 118:340–52. doi: 10.1111/add.16050
14. Moore D, Aveyard P, Connock M, Wang D, Fry-Smith A, Barton P. Effectiveness and safety of nicotine replacement therapy assisted reduction to stop smoking: systematic review and meta-analysis. BMJ. (2009) 338:b1024. doi: 10.1136/bmj.b1024
15. Goniewicz ML, Smith DM, Edwards KC, Blount BC, Caldwell KL, Feng J, et al. Comparison of nicotine and toxicant exposure in users of electronic cigarettes and combustible cigarettes. JAMA Netw Open. (2018) 1:e185937. doi: 10.1001/jamanetworkopen.2018.5937
16. Holt NM, Shiffman S, Black RA, Goldenson NI, Sembower MA, Oldham MJ. Comparison of biomarkers of exposure among US adult smokers, users of electronic nicotine delivery systems, dual users and nonusers, 2018–2019. Sci Rep. (2023) 13:7297. doi: 10.1038/s41598-023-34427-x
17. World Health Organization. Regional Office for Europe. Electronic Nicotine and Non-Nicotine Delivery Systems: A Brief. Copenhagen: World Health Organization; Regional Office for Europe (2020). p.14.
18. International Agency for Research on Cancer. Are E-Cigarettes Less Harmful Than Conventional Cigarettes?: International Agency for Research on Cancer. (2016). Available online at: https://cancer-code-europe.iarc.fr/index.php/en/ecac-12-ways/tobacco/247-are-e-cigarettes-less-harmful-than-conventional-cigarettes2023 (accessed May 4, 2023).
19. Snell LM, Barnes AJ, Nicksic NE. A longitudinal analysis of nicotine dependence and transitions from dual use of cigarettes and electronic cigarettes: evidence from waves 1–3 of the PATH Study. J Stud Alcohol Drugs. (2020) 81:595–603. doi: 10.15288/jsad.2020.81.595
20. Jackson SE, Shahab L, West R, Brown J. Associations between dual use of e-cigarettes and smoking cessation: a prospective study of smokers in England. Addict Behav. (2020) 103:106230. doi: 10.1016/j.addbeh.2019.106230
21. Mattingly DT, Zavala-Arciniega L, Hirschtick JL, Meza R, Levy DT, Fleischer NL. Trends in exclusive, dual and polytobacco Use among U.S. adults, 2014-2019: results from two nationally representative surveys. Int J Environ Res Publ Health. (2021) 18:13092. doi: 10.3390/ijerph182413092
22. Reid JL, Hammond D, Burkhalter R, Rynard VL. Tobacco Use in Canada: Patterns and Trends. Waterloo, ON (2022).
23. Coleman BN, Rostron B, Johnson SE, Ambrose BK, Pearson J, Stanton CA, et al. Electronic cigarette use among US adults in the population assessment of tobacco and health (PATH) study, 2013–2014. Tobacco Control. (2017) 26:e117–26. doi: 10.1136/tobaccocontrol-2016-053462
24. Martinez-Loredo V, González-Roz A, Dawkins L, Singh D, Murphy JG, MacKillop J. Is E-cigarette use associated with persistence or discontinuation of combustible cigarettes? A 24-month longitudinal investigation in young adult binge drinkers. Nicotine Tobacco Res. (2022) 24:962–69. doi: 10.1093/ntr/ntac049
25. Kotz D, Jackson S, Brown J, Kastaun S. The effectiveness of E-cigarettes for smoking cessation. Deutsches Ärzteblatt Int. (2022) 119:297–301. doi: 10.3238/arztebl.m2022.0162
26. Conner TS, Zeng J, Blank M-L, He V, Hoek J. A descriptive analysis of transitions from smoking to electronic nicotine delivery system (ENDS) use: a daily diary investigation. Int J Environ Res Public Health. (2021) 18:6301. doi: 10.3390/ijerph18126301
27. Notley C, Ward E, Dawkins L, Holland R. The unique contribution of e-cigarettes for tobacco harm reduction in supporting smoking relapse prevention. Harm Reduct J. (2018) 15:1–12. doi: 10.1186/s12954-018-0237-7
Keywords: smoking cessation, electronic nicotine delivery system, harm reduction, dual use, tobacco
Citation: Kroeger K, Buss VH, Shahab L and Storck M (2024) Use of electronic nicotine delivery systems and cigarette smoking—Add-on vs. displacement dual use. Front. Public Health 11:1281999. doi: 10.3389/fpubh.2023.1281999
Received: 25 August 2023; Accepted: 06 December 2023;
Published: 04 January 2024.
Edited by:
Julia Dickson-Gomez, Medical College of Wisconsin, United StatesReviewed by:
Jannie Hugo, University of Pretoria, South AfricaCopyright © 2024 Kroeger, Buss, Shahab and Storck. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Knut Kroeger, a251dC5rcm9lZ2VyQGhlbGlvcy1nZXN1bmRoZWl0LmRl; Vera Helen Buss, di5idXNzQHVjbC5hYy51aw==
 Knut Kroeger
Knut Kroeger Vera Helen Buss
Vera Helen Buss Lion Shahab
Lion Shahab Martin Storck3
Martin Storck3