- 1Department of Emergency, Shandong Provincial Hospital Affiliated to Shandong First Medical University, Jinan, China
- 2Department of Pharmacy, Shandong Provincial Hospital Affiliated to Shandong First Medical University, Jinan, China
- 3Department of Emergency Internal Medicine, The Affiliated Hospital of Qingdao University, Qingdao, China
- 4Department of Emergency, Qilu Hospital of Shandong University Dezhou Hospital, Dezhou, China
- 5Department of Emergency, Shandong Public Health Clinical Center Affiliated to Shandong University, Jinan, China
Introduction: In the middle of December 2022, the Chinese government adjusted the lockdown policy on coronavirus disease 2019 (COVID-19), a large number of infected patients flooded into the emergency department. The emergency medical staff encountered significant working and mental stress while fighting the COVID-19 pandemic. We aimed to investigate the workload change, and the prevalence and associated factors for depression symptoms among emergency medical staff after the policy adjustment.
Methods: We conducted a cross-sectional online survey of emergency medical staff who fought against COVID-19 in Shandong Province during January 16 to 31, 2023. The respondents’ sociodemographic and work information were collected, and they were asked to complete the 9-item Patient Health Questionnaire (PHQ-9) then. Univariate and multivariate logistic regression analyses were applied to identify the potential associated factors for major depression.
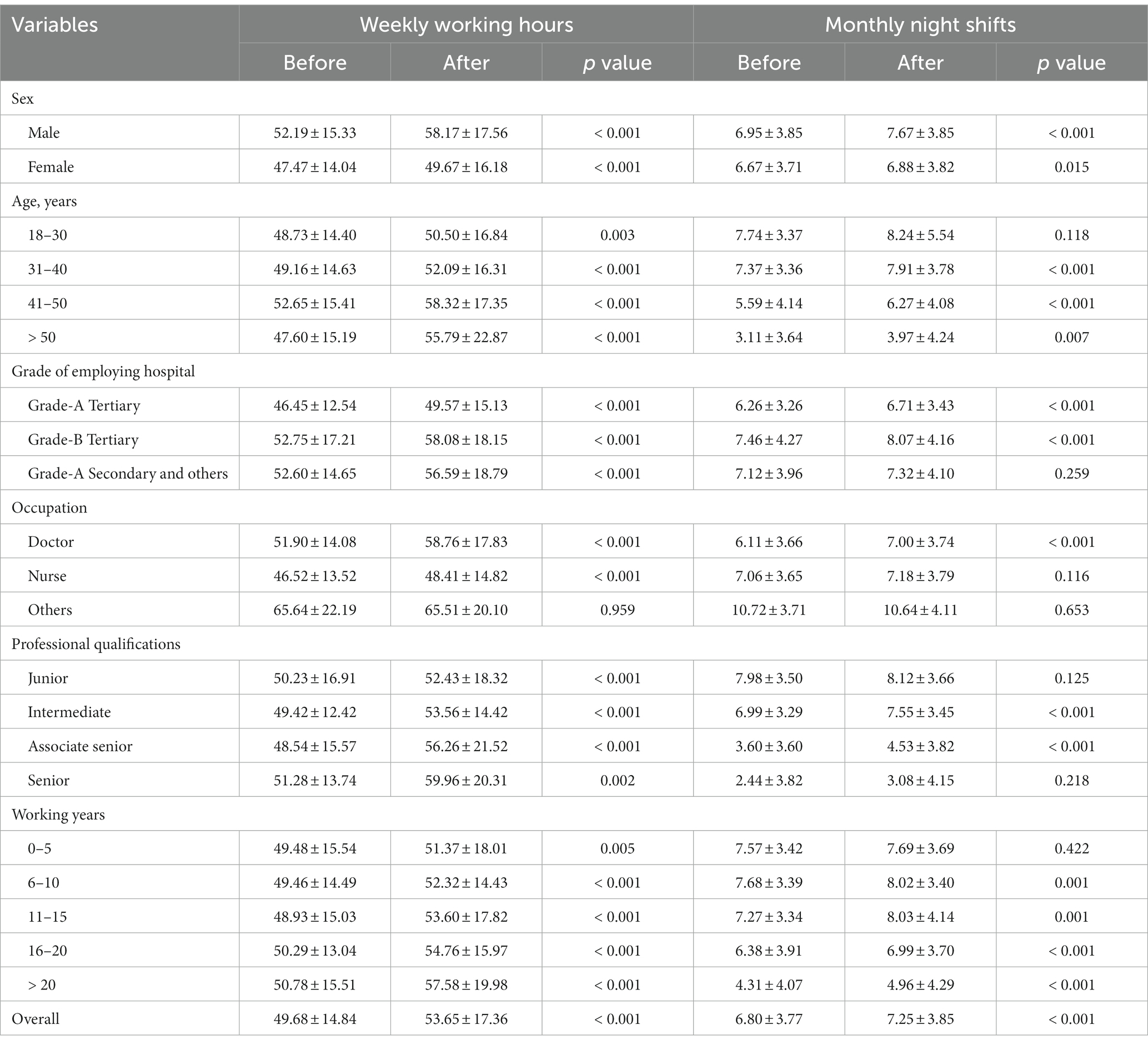
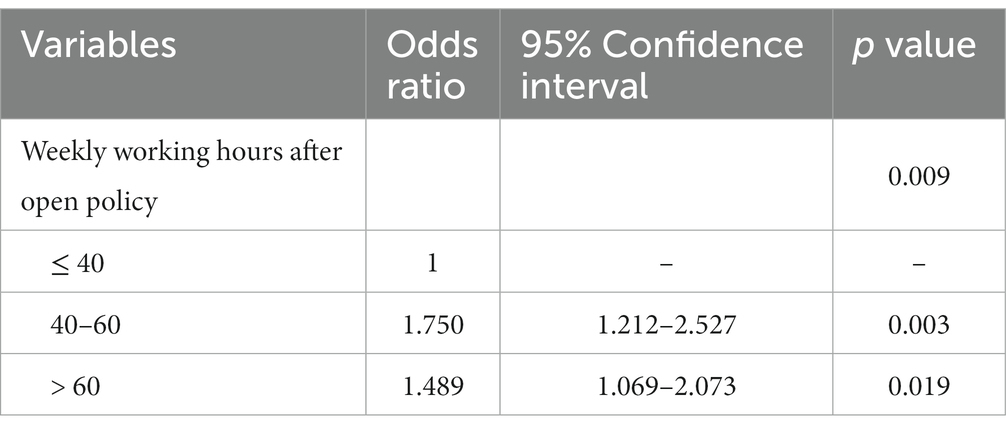
Results: Nine hundred and sixteen emergency medical personnel from 108 hospitals responded to this survey. The respondents’ weekly working hours (53.65 ± 17.36 vs 49.68 ± 14.84) and monthly night shifts (7.25 ± 3.85 vs 6.80 ± 3.77) increased after the open policy. About 54.3% of the respondents scored more than 10 points on the PHQ-9 standardized test, which is associated with depressive symptoms. In univariate analysis, being doctors, living with family members aged ≤16 or ≥ 65 years old, COVID-19 infection and increased weekly working hours after the open policy were significantly associated with a PHQ-9 score ≥ 10 points. In the multivariate analysis, only increased weekly working hours showed significant association with scoring ≥10 points.
Conclusion: Emergency medical staff’ workload had increased after the open policy announcement, which was strongly associated with a higher PHQ-9 scores, indicating a very high risk for major depression. Emergency medical staff working as doctors or with an intermediate title from grade-A tertiary hospitals had higher PHQ-9 scores, while COVID-19 infection and weekly working hours of 60 or more after the open policy were associated with higher PHQ-9 scores for those from grade-B tertiary hospitals. Hospital administrators should reinforce the importance of targeted emergency medical staff support during future outbreaks.
Introduction
The coronavirus disease 2019 (COVID-19) was first reported in Wuhan, China, in December 2019. It spread across the world and caused hundreds of millions infections since then. According to the World Health Organization (WHO), there have been 768,983,095 confirmed cases of COVID-19, including 6,953,743 deaths, by August 2nd, 2023 (1). In China, there have been 99,300,040 confirmed cases (including 121,563 deaths) by August 2nd, 2023 (1). Social distancing was recommended as one control option by the WHO to reduce the possibility of infection (2). However, hospital medical staff, especially those from emergency department who fight against COVID-19 on the front-lines, are unable to follow guidance on social distancing. In the middle of December 2022, the Chinese government adjusted the lockdown policy on COVID-19, a large number of infected patients flooded into the emergency department. Emergency medical staff were exposed to a high risk of coronavirus infection while suffering great working and mental stress. Previous infectious disease pandemics such as severe acute respiratory syndrome (SARS) and Middle East respiratory syndrome (MERS) have been reported to have a negative effect on people’s mental health, including medical staff (3, 4). COVID-19 pandemics have increased the prevalence of anxiety and depression among hospital medical staff (5–10). However, research exploring the mental health problems of front-line emergency medical staff after the open policy is limited. The aim of this research was to investigate the workload change, and the prevalence and associated factors for depressive symptoms among emergency medical staff during the policy adjustment period.
Methods
Study design and participants
This was a cross-sectional survey conducted in Shandong Province, China, between January 16 and January 31, 2023. The study was approved by the ethics committee of Shandong Provincial Hospital Affiliated to Shandong First Medical University (number SWYX:NO.2023–118), and all participants provided informed consent. Emergency medical staff (including doctors, nurses and pre-hospital emergency personnel) aged above 18 years who fought against COVID-19 between December 1, 2022 and January 15, 2023 were invited to participate. Those who were diagnosed with any mental illness previously or taking any anti-psychotic medications were excluded.
Survey instrument
An online questionnaire system (Wenjuanxing, Changsha Ranxing Information Technology Co., LTD, Changsha, China) was used as the platform for distributing our survey tool. We sent the survey out through emergency medicine groups on the WeChat messaging platform (Tencent Corporation, Shenzhen, China). Then the Wenjuanxing system was able to collect the survey data electronically. Our survey instrument began with collecting participants’ general characteristics, including sex, age, occupation, marital status, and whether they live with family members younger than 16 years or older than 65 years. Then the respondents were queried about work details including grade of employing hospital, professional qualifications, working years, vaccination and COVID-19 infection status. We then collected their weekly working hours and monthly night shifts information before and after the open policy. At last, we used the Patient Health Questionnaire-9 (PHQ-9) standardized questionnaire to ascertain the mental state of surveyed emergency medical staff, which was a self-rated version of the Primary Care Evaluation of Mental Disorders (PRIME-MD) patient questionnaire for depression (11, 12). The PHQ-9 is scored 0–27, with the cutoff score for major depression symptoms in prior studies was set at 10 (13, 14). We used the standard score of ≥10 as the critical value to divide those participants with or without depression in this study.
Statistical analysis
Continuous variables were presented as mean and standard deviation for normally distributed data or median and inter-quartile ranges for skewed data, while categorical variables were presented as frequency and percentages. Participants’ characteristics were compared according to PHQ-9 scoring ≥10 or not, using Student’s t-tests for quantitative variables and Chi-square tests for categorical variables. Univariate logistic regression analysis was performed to evaluate the relationships between variables and depressive symptoms. Variables associated with PHQ-9 ≥ 10 in univariate analysis (p < 0.10) were included in the multivariate model. p < 0.05 was considered statistically significant. All analyses were conducted using SPSS 20.0 software (IBM Inc., Armonk, NY, United States).
Results
Nine hundred and sixty-one respondents completed the questionnaires through the online survey system, of which 916 (95.32%) were valid. Respondents are emergency medical staff from 108 hospitals located in all 16 cities of Shandong Province. The average PHQ-9 score for all included medical staff was 11.18 ± 6.50, and 497 participants (54.26%) had a PHQ-9 score ≥ 10. The prevalence of major depression symptoms was high with a PHQ-9 score distribution of 10–14 (26.75%), 15–19 (15.17%), and 20–27 (12.34%).
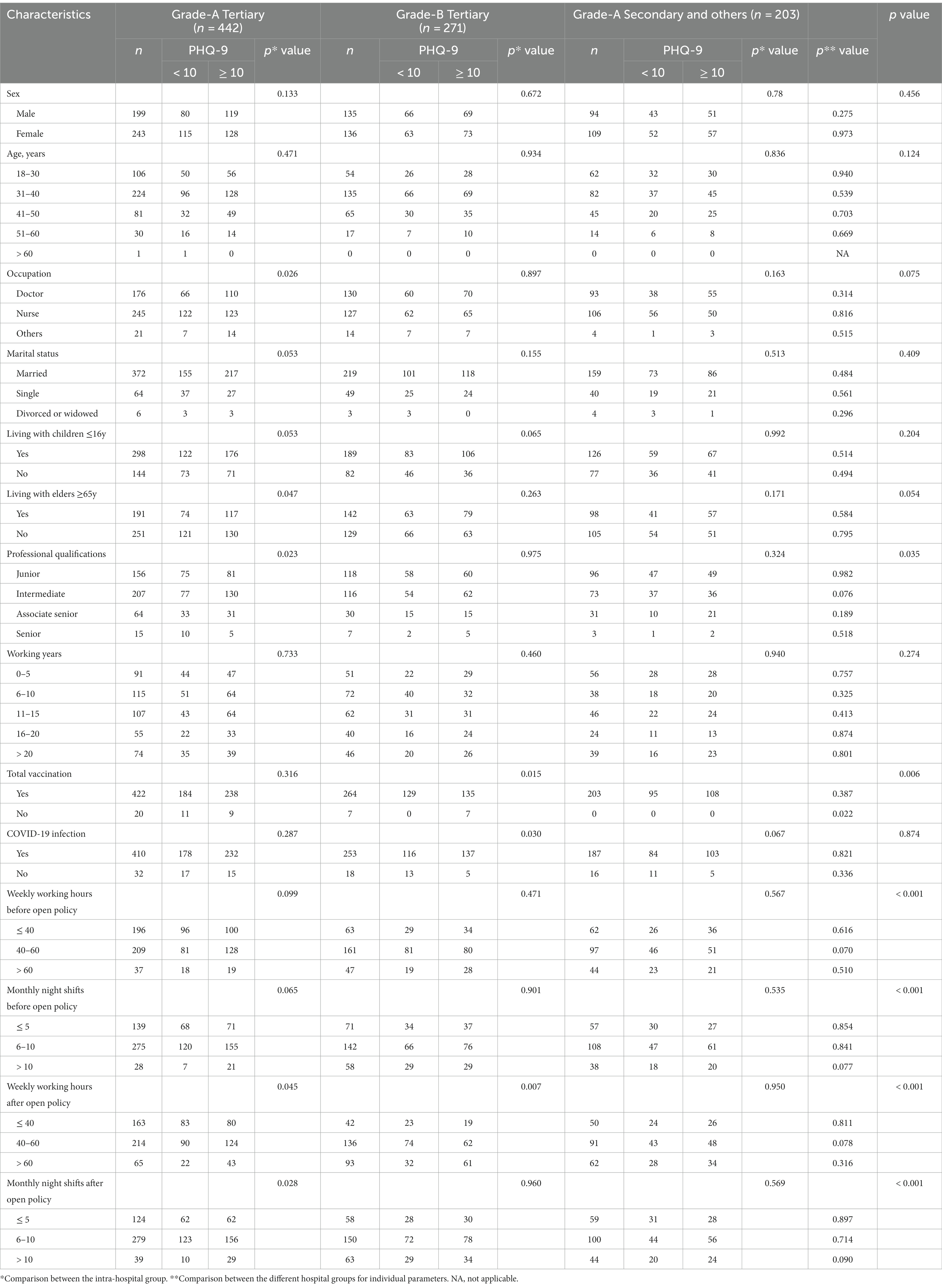
Participants’ characteristics
Participants’ characteristics are shown in Table 1. Among these respondents, 46.72% were male and most (72.38%) were ≤ 40 years old. Doctors and nurses accounted for 43.56 and 52.18%, respectively. About two thirds (66.92%) of the participants lived with children ≤16 years old, while 47.05% of them lived with elders ≥65 years old. Most of the participants (77.84%) worked in tertiary hospitals. Junior and intermediate level personnel accounted for 40.39 and 43.23% respectively, while associate senior and senior level personnel accounted for 13.65 and 2.73%, respectively.
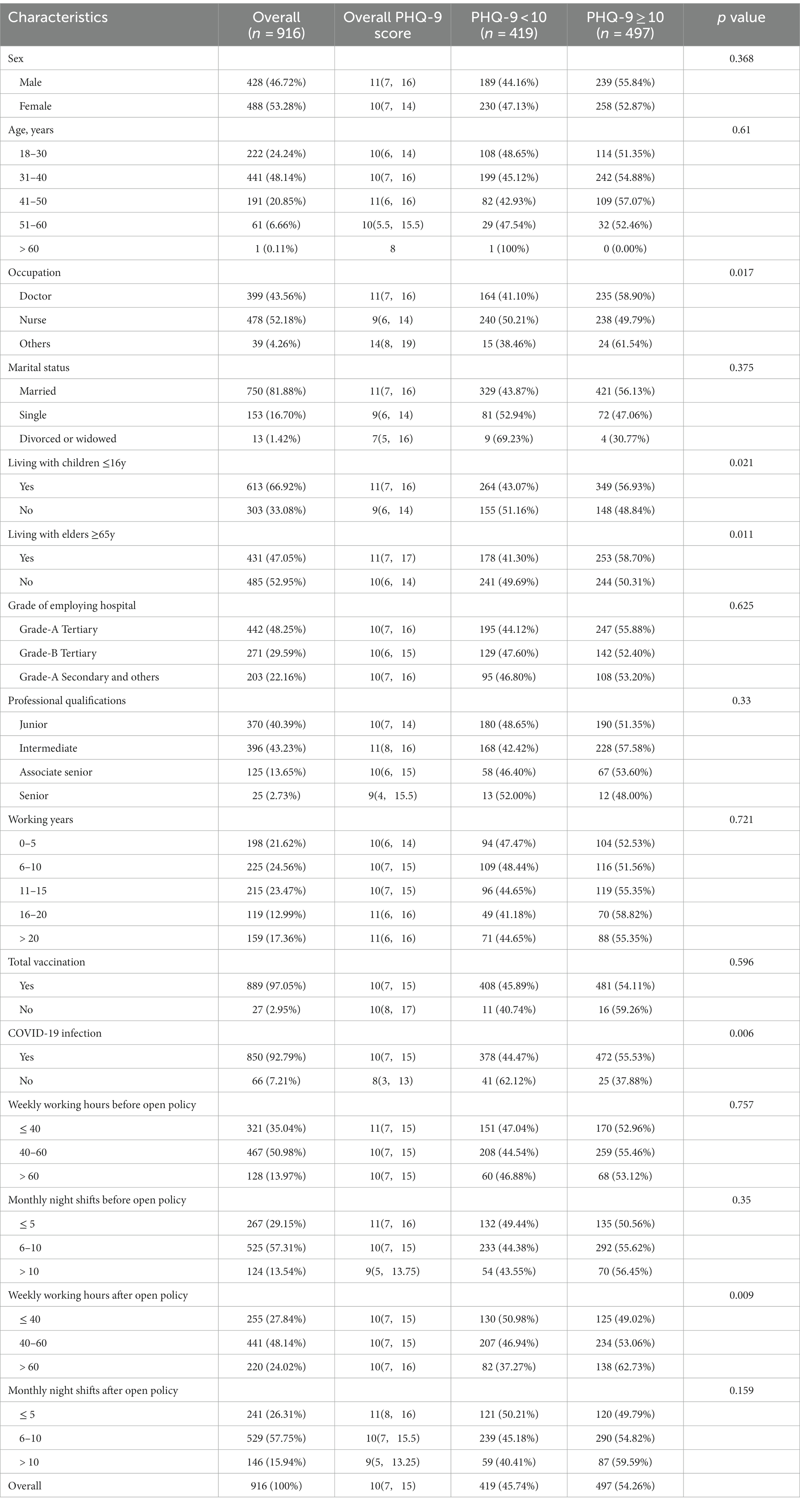
Table 1. Participants’ characteristics and univariate analysis results between the PHQ-9 < 10 and PHQ-9 ≥ 10 groups.
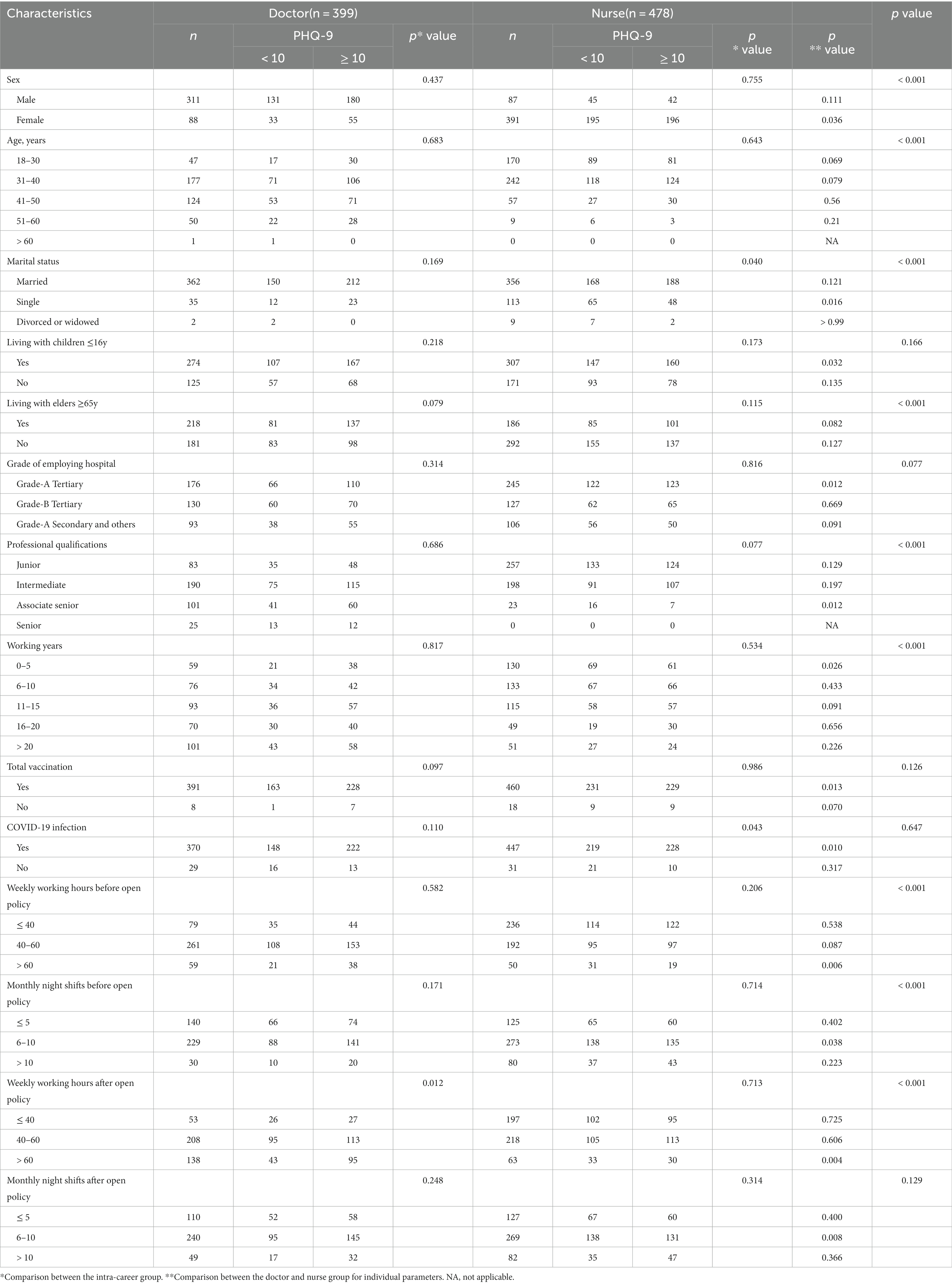
Workload before and after the open policy
The workload change during the open policy are shown in Table 2. Before the open policy, 321 (35.04%), 467 (50.98%) and 128 (13.97%) participants’ weekly working hours were ≤ 40, 40–60, and > 60 h, respectively. Of all the included participants, 267 (29.15%) had a monthly night shifts of ≤5, while 525 (57.31%) of them had a monthly night shifts of 6–10. After the open policy announcement, 441 (48.14%) participants’ weekly working hours were 40–60 h, while 220 (24.02%) participants’ were > 60 h. And 241 (26.31%) participants had a monthly night shifts of ≤5, while 529 (57.75%) of them had a monthly night shifts of 6–10. Overall, the participants’ weekly working hours increased after the open policy (53.65 ± 17.36 vs 49.68 ± 14.84, p < 0.001), which was the same for monthly night shifts(7.25 ± 3.85 vs 6.80 ± 3.77, p < 0.001). For different subgroups (sex, age, employing hospital, etc), the results were similar.
Male staff took more workload than female (eg. weekly working hours after the open policy among men vs. women: 58.17 ± 17.56 vs. 49.67 ± 16.18). Doctors had longer weekly working hours than nurses before and after the policy adjustment (eg. weekly working hours after the open policy among doctors vs. nurses: 58.76 ± 17.83 vs. 48.41 ± 14.82). Though doctors took less night shifts than nurses before the open policy (6.11 ± 3.66 vs. 7.06 ± 3.65), their night shifts increased to the same level as nurses after the open policy (7.00 ± 3.74 vs. 7.18 ± 3.79). The weekly working hours and monthly night shifts of grade A tertiary hospitals’ emergency medical staff were less than the other two hospital groups (both before and after the open policy).
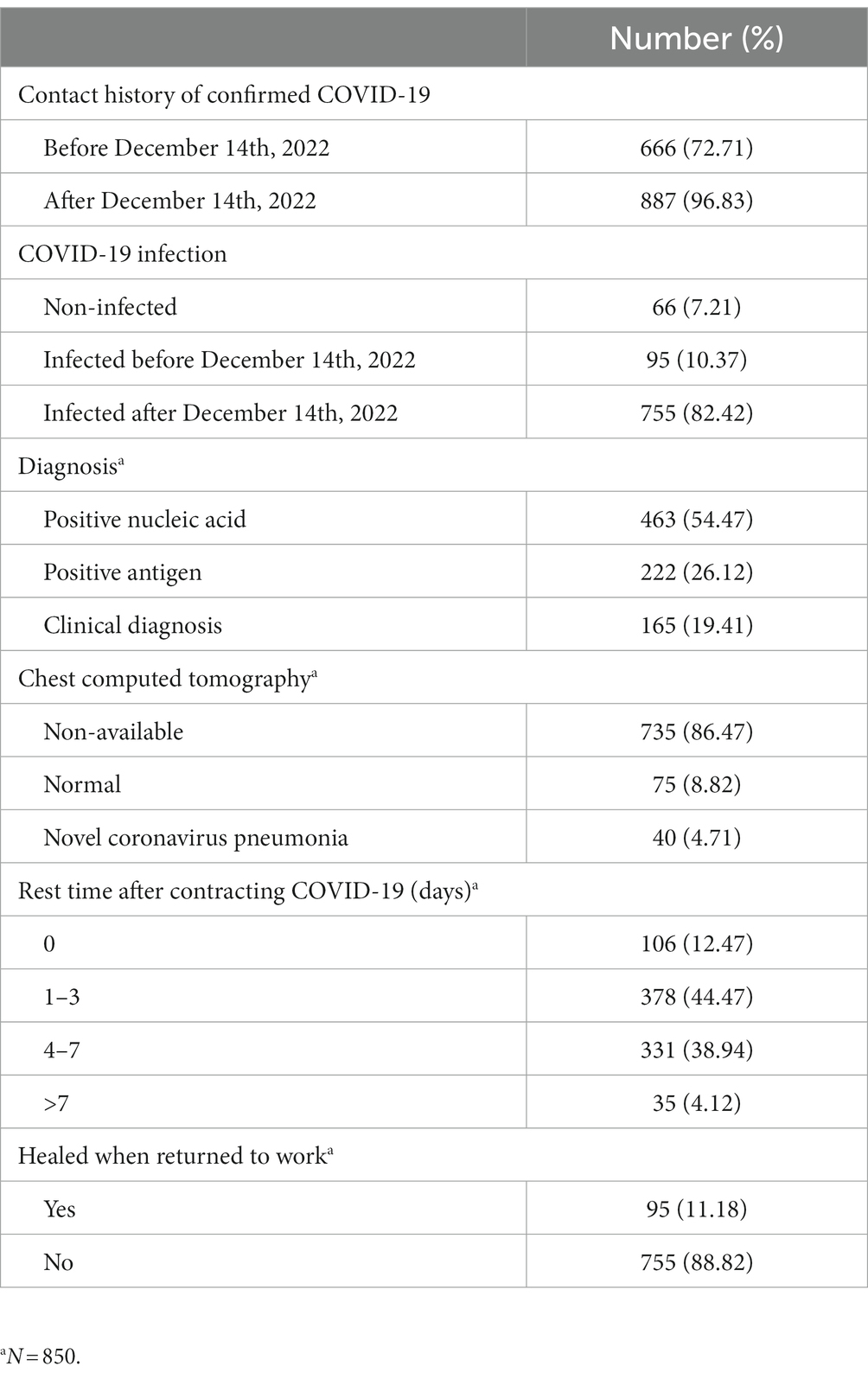
COVID-19 infection
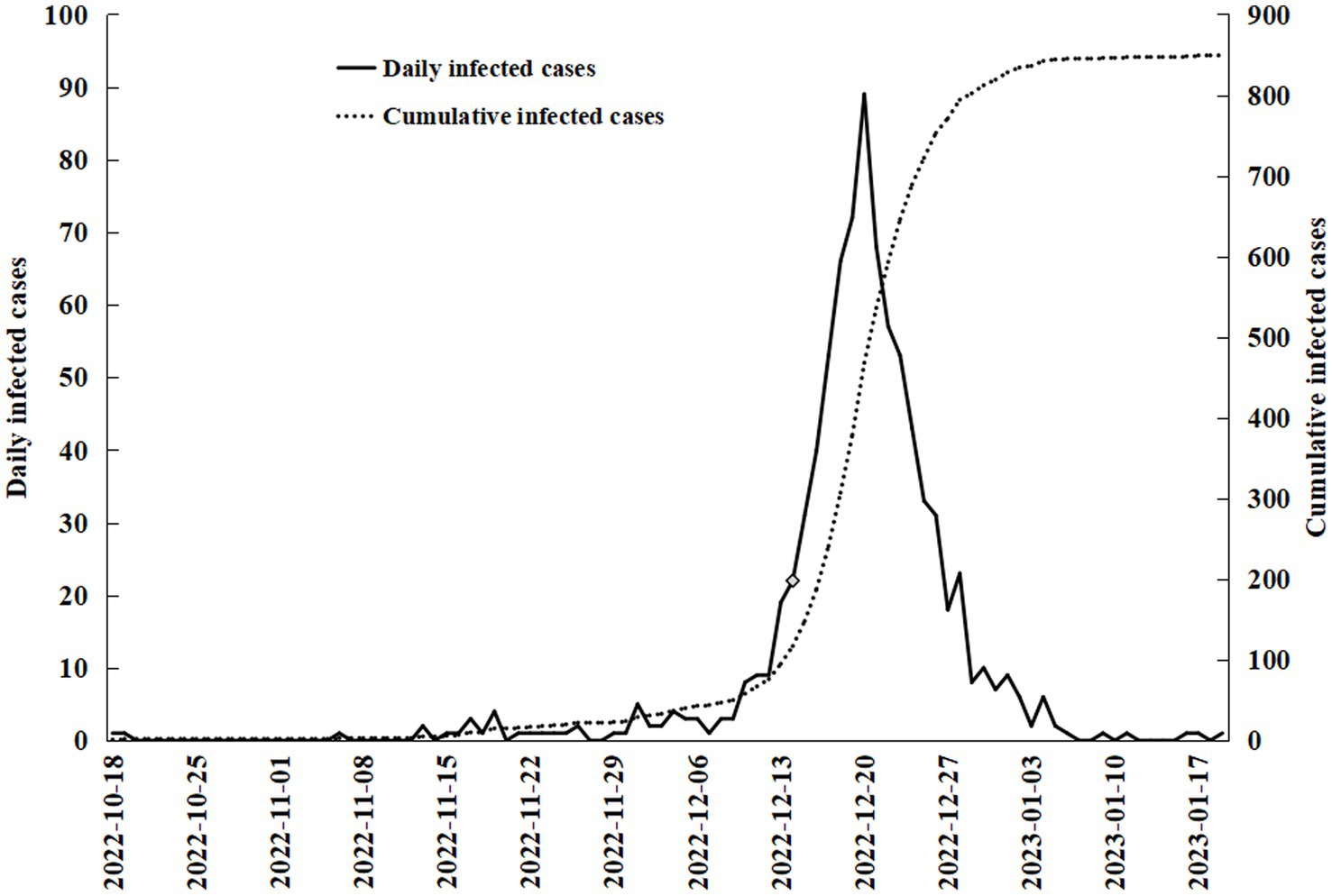
Almost all (97.05%) of the medical staff surveyed completed the full course of vaccination, but most of them (92.79%) were still infected with novel coronavirus. Before the government announced the open policy, infections with COVID-19 among health workers were at a low level. After the announcement of the open policy, a large number of infected patients flooded into the emergency department, and infections among emergency medical staff were skyrocketing (Figure 1).
Before December 14th, 2022, there were 95(10.37%) respondents who had been infected with COVID-19, while 666(72.71%) had a contact history of confirmed COVID-19 patients. Since then, the number of daily infections among emergency medical staff increased significantly, peaking at 89 on December 20th, 2022 (Figure 1). By January 19th, 2023, 887(96.83%) respondents reported a contact history of confirmed COVID-19 patients, 850(95.83%) of whom were infected with COVID-19 (Table 3). Most COVID-19 infections among emergency medical staff were confirmed by positive nucleic acid (54.47%) or antigen (26.12%). One hundred and fifteen participants took a chest computed tomography, among whom 40(34.78%) had image findings of COVID-19. After contracting COVID-19, most participants had to continue working due to the desperately shortage of medical personnel. There were 378(44.47%) respondents who left the work position to have a rest for 1–3 days, while 106(12.47%) respondents did not rest at all. Only 95(11.18%) participants returned to work after they had recovered.
Factors associated with depressive symptoms among emergency medical staff
Univariate analysis of factors associated with major depression symptoms among emergency medical staff are shown in Table 1. Being doctors, living with family members younger than 16 years or older than 65 years, COVID-19 infection and increased weekly working hours after the open policy showed statistical significance. There was no significant difference in the PHQ-9 scores divided by prevalence according to sex, age, marital status, grade of employing hospital, professional qualifications, working years and monthly night shifts. Multivariate logistic regression analysis showed that a PHQ-9 score ≥ 10 was significantly associated with increased weekly working hours after the open policy. Results of the multivariate logistic regression analysis are shown in Table 4.
Comparisons among hospitals of different grades
The results of comparisons among different hospital groups are shown in Table 5. For emergency medical staff working in grade A tertiary hospitals, being doctors, living with family member ≥65y, an intermediate professional qualifications, increased weekly working hours and monthly night shifts after the policy adjustment were associated with a higher PHQ-9 score. For those working in grade B tertiary hospitals, being unvaccinated, COVID-19 infection and increased weekly working hours after the open policy showed a strong relationship with PHQ-9 ≥ 10. No factors were found to be associated with a higher PHQ-9 score for those working in grade A secondary and other hospitals. When individual factors were compared among hospitals, those from grade A tertiary hospitals had a lower proportion of junior professional qualifications and vaccination than others. The weekly working hours and monthly night shifts of grade A tertiary hospitals’ medical staff were less than others (both before and after the open policy). Though no statistical significance among different groups was observed, medical staff with weekly working hours of 40 to 60 h and monthly night shifts of >10 from grade A tertiary hospitals tended to have a higher PHQ-9 score.
Multivariate logistic regression analysis showed that nurses and those with a senior title had a lower PHQ-9 score among emergency medical staff from grade A tertiary hospitals (Table 6). For those working in grade B tertiary hospitals, COVID-19 infection and increased weekly working hours (> 60) after the open policy were associated with higher PHQ-9 score (Table 7).
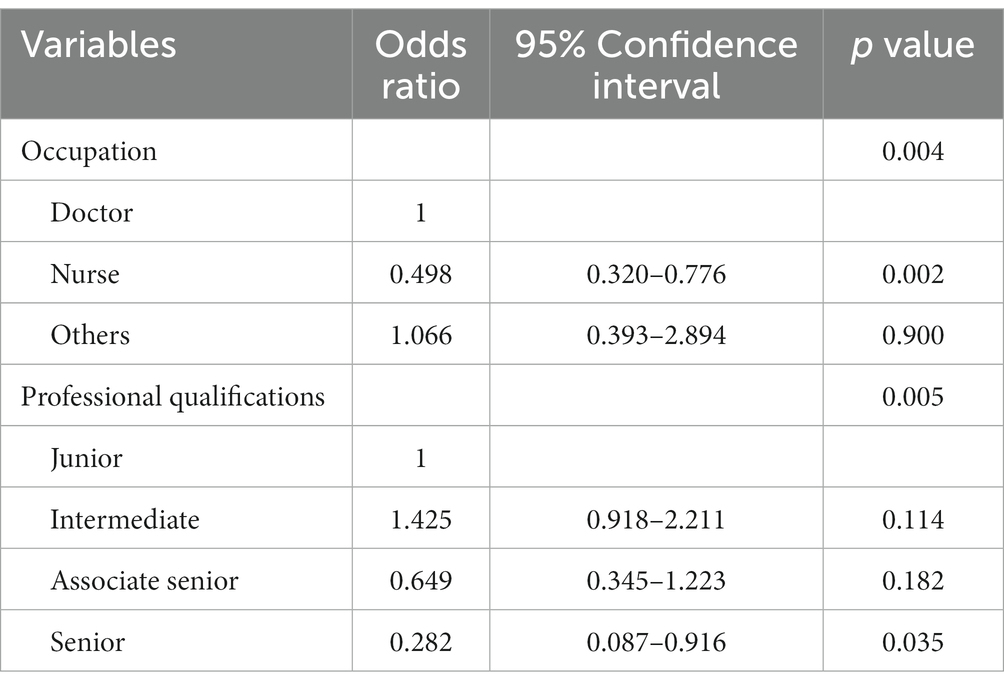
Table 6. Factors associated with depression symptoms by multivariate logistic regression analysis among emergency medical staff from grade-A tertiary hospitals.
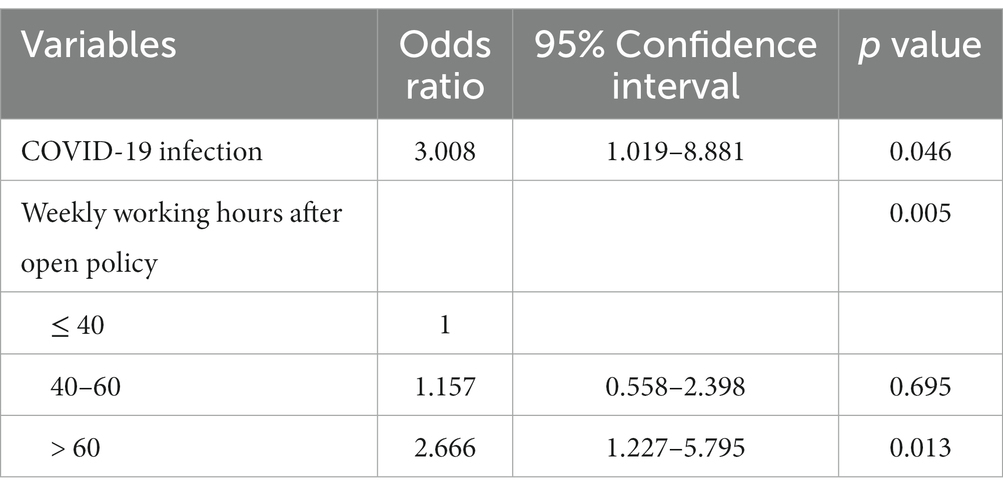
Table 7. Factors associated with depression symptoms by multivariate logistic regression analysis among emergency medical staff from grade-B tertiary hospitals.
Comparisons between doctors and nurses
Due to the small number of pre-hospital personnel and others, we made comparisons between doctors and nurses only (Table 8). Increased weekly working hours after the open policy were associated with PHQ-9 ≥ 10 for doctors, while marriage and COVID-19 infection showed a similar relationship with PHQ-9 ≥ 10 for nurses. Compared with nurses, doctors had a higher proportion of male sex, age of >40y, living with elders ≥65y, senior titles, long working years, and long weekly working hours. The unmarried rate and monthly night shifts before the open policy were higher for nurses. Interestingly, though nurses had more night shifts per month, their weekly working hours were lower than doctors (Table 2). The night shifts of doctors increased (7.00 ± 3.74 vs. 6.11 ± 3.66) after the open policy, while those of nurses did not change significantly (Table 2). When individual parameters were compared between doctors and nurses, doctors who were female, single, living with children ≤16y, working in grade A tertiary hospitals, having a senior title, infected with COVID-19, having longer weekly working hours and more night shifts were more prone to have a PHQ-9 ≥ 10 than nurses with the same conditions. Multivariate logistic regression analysis showed that nurses with associate senior titles had a lower PHQ-9 score than those with a junior or intermediate titles, though there was no statistical significance overall (Table 9). No factors were found to be associated with a higher PHQ-9 score among doctors in multivariate logistic regression analysis.
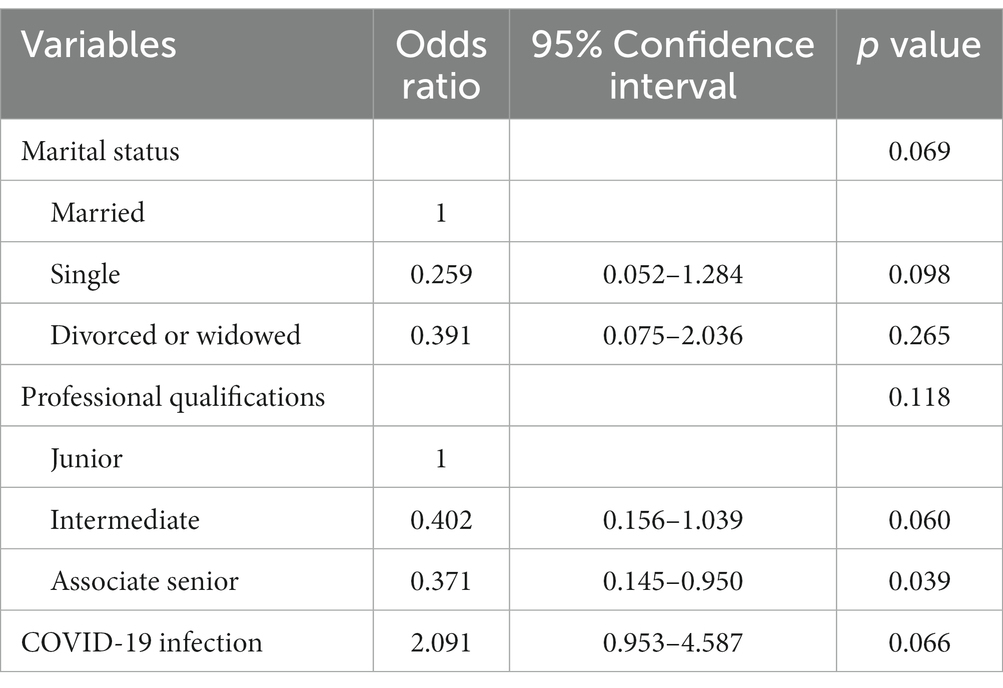
Table 9. Factors associated with depression symptoms by multivariate logistic regression analysis among nurses.
Discussion
This was a multi-center, cross-sectional study on the influence of policy adjustment on emergency medical staff, aiming to find the workload change, and the prevalence and risk factors for depression after the open policy during the COVID-19 pandemic in Shandong, China. The results showed that more than half of the surveyed respondents had a PHQ-9 score ≥ 10, which were consist with previous researches (9, 15). In our study, medical profession, living with juvenile or aged family members, COVID-19 infection and increased weekly working hours were associated with an increased PHQ-9 score in univariate analysis. However, only increased weekly working hours after the open policy showed a strong relationship with a PHQ-9 score ≥ 10 when multivariate analysis was carried out.
Previous study showed that the average working hours of all Chinese emergency medical staff were relatively long, with an average 12 h-long shift and 50 h of weekly working hours, which was consist with our survey results (9). Interestingly, the average working hours per week before COVID-19 pandemic were more than the average hours during COVID-19 in that study (8). The decreased working hours during COVID-19 pandemic might be explained by medical personnel support from other departments, national compulsory isolation policy or decreased emergency visits for other diseases other than fever (9, 16, 17). However, both weekly working hours and monthly night shifts of the respondents from our study had increased after the open policy announcement. There were several reasons for this. First, the emergency visits soared in a short time due to the rapid increasing infection. Second, since the lockdown policy had been lifted, patients with diseases other than fever came to emergency department seeking for care. Third, the emergency medical staff themselves were infected with COVID-19, some of whom had to leave their work position for several days due to poor physical conditions and the remaining ones shouldered their workloads. And increased workload was associated with higher rates of depression and other mental health outcomes, which had been verified in previous studies (18, 19).
Depression was one of the most common mental health problems among medial staff during COVID-19 pandemic and the reported prevalence varied from 13.4 to 53.9% in different researches (6, 7, 9, 10, 15, 20). There were different factors reported to be associated with depression, such as age, sex, marriage status, work position, etc. These factors might had a relationship with depression in a study, while not in another. However, front-line medical staff who participated in direct diagnosis, treatment and care of COVID-19 patients were reported to have a higher risk of depression in extensive literature (7, 9, 10, 15, 20). Emergency departments were the first presentation areas of patients before and during the COVID-19 pandemic period. Emergency medical staff working on the frontline during the pandemic experience more mental health problems than those working in other positions (4, 15, 21). Concur with our study, depression were detected in more than half of the participants in previous studies (4, 21).
Female, nurse and intermediate technical title were associated with worse mental health outcomes including depression, anxiety, and distress in a previous study (15). However, 76.7% of the participants were women, and 60.8% were nurses, there might be selection bias in that study (15). In our study, male accounted for nearly half (46.72%) of the whole participants, and 43.56% were doctors. The results showed that there was no difference between male and female for scores of depression, which was consist with a meta-analysis published in 2020 (20). Contrast with previous studies, doctors had higher PHQ-9 scores than nurses in our study. A meta-analysis of 26 studies investigating 31,447 doctors demonstrated that the prevalence of depression was 20.5% with the point prevalence ranged from 6.1 to 73.4% (22). Doctors, especially those working in grade A tertiary hospitals, had higher PHQ-9 scores than nurses in our study cohort. For front-line healthcare workers caring for COVID-19 patients, the prevalence of depression in doctors was much higher than nurses (40.4% vs. 28%), which was reported by a meta-analysis (5). As for our study cohort, the workload of doctors increased more significantly than that of nurses during the open policy, making them more stressed. They might experience poor job satisfaction, which was associated with higher prevalence of mental health problems (anxiety, depression and secondary traumatic stress) (23). For doctors from emergency department, the prevalence might be higher, since they need to make quick decisions on the diagnosis and treatment strategy when critically ill patients arrived in the emergency room, which make their occupational stress higher and result in psychological consequences such as depression and anxiety (24, 25). In our study cohort, emergency medical staff with associate senior (for nurses) or senior (for doctors) titles had a lower PHQ-9 score than those with an intermediate title. This could be explained by the fact that those with lower professional titles were more likely to work on the front-line.
Hospitals were the most common exposure sites, and medical staff have a higher risk for occupational COVID-19 compared with the general workforce (26). Researchers conducted an online survey on 1766 front-line nurses working in hospitals located in Shenzhen, China, after the open policy announcement. About 90.83% of the participants were infected with COVID-19, and 33.64% of them had to work while infected with COVID-19 (27). The overall prevalence of depressive symptoms was 69.20% (27). However, only 76 (4.3%) of the participants worked in the emergency departments (27). In our cohort, only 10.37% of the overall participants were infected before the adjustment of anti-epidemic policy at December 14th, 2022. Another 755 (82.42%) participants reported COVID-19 infection in the following month. Most of them (88.82%) had to return to work before getting healed due to the shortage of medical personnel.
A study surveying 1,103 emergency nurses showed that working in tertiary hospitals were significantly associated with depression (28). In another study, medical staffs in secondary hospitals reported higher scores for depression than those in tertiary hospitals (15). Despite of differences between studies, front-line medical staff from tertiary and secondary hospitals reported similar high PHQ-9 scores (15, 28), which was consist with our research. Emergency medical staff working in grade A tertiary hospitals undertook less weekly working hours and monthly night shifts than those working in the other two hospital groups, which could be explained by the concentration of medical resources. The higher proportion of medical personnel with intermediate titles in grade A tertiary hospitals also reflects the imbalance of medical resources. However, they did not have a lower PHQ-9 score, because they need to handle more patients with more complex and critical situations than those working in other hospitals.
Previous study has demonstrated that the ongoing stress have negative effects on medical staffs’ psychological well-being, especially when they face a great threat of public health emergencies (29). A longitudinal study conducted by Filippo Rapisarda and colleagues showed that psychological distress (a combination of severe post-traumatic, depressive and anxiety symptoms) tended to resolve within a few weeks, though it was present in 40% of healthcare workers (30). A Canadian study demonstrated similar result during one-year observation (31). Resilience and social support were predominant protective factors against depression over time (31). So health administrators should provide interventions to improve working conditions and reduce occupational stress of medical staffs to reduce or prevent prevalence of depression and other mental health problems.
Our study has some strengths. First, this study demonstrated the heavy workload and high prevalence of depression among emergency medical staff from China after the announcement of open policy, which highlighted the importance of targeted emergency medical staff support during future outbreaks. Second, the survey was conducted in a populous province. The population of Shandong is more than 100 million (about 7.19% of the total Chinese population), and the number of physicians accounts for 7.86% of the total number of physicians in China. Therefore, the research conducted in Shandong can be representative of China to a certain extent. Third, our study cohort included a higher proportion of male and doctors, which is less likely to be biased than previous studies that focused on female and nurses.
Our study has several limitations. First, the cross-sectional design only assessed individual status at the time the data were collected, which was not suitable for detecting intra-individual change across time and address causal associations. Second, there might be self-report bias since the participants completed the questionnaires online. Third, we only assessed depression in this study, other mental problems such as anxiety, insomnia and post-traumatic stress disorder were not included in the questionnaire. Too many questions included in the questionnaire might reduce the motivation of the respondents, since the survey was carried out during the peak of the epidemic after the open policy announcement. Fourth, the PHQ-9 scale is not accurate enough to make a definite diagnosis of depression. Scores above the threshold suggest a detailed psychological assessment. The prevalence estimates of common mental disorders such as anxiety and depression in medical staff were considerably lower when assessed using diagnostic interviews compared with screening tools (5). However, it was not realistic to conduct a diagnostic interview under the tense circumstances when the study was conducted. Fifth, the study included participants from Shandong Province only, and the results may not be applicable to other regions of China.
Conclusion
Our study demonstrates that emergency medical staff’ workload had increased after the open policy announcement, which was strongly associated with higher PHQ-9 scores, indicating a very high risk for major depression. Emergency medical staff working as doctors or with an intermediate title from grade-A tertiary hospitals had higher PHQ-9 scores, while COVID-19 infection and weekly working hours of 60 or more after the open policy were associated with higher PHQ-9 scores for those from grade-B tertiary hospitals. Hospital administrators should reinforce the importance of targeted emergency medical staff support during future outbreaks.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by the ethics committee of Shandong Provincial Hospital Affiliated to Shandong First Medical University. The studies were conducted in accordance with the local legislation and institutional requirements. The ethics committee/institutional review board waived the requirement of written informed consent for participation from the participants or the participants’ legal guardians/next of kin because The study was conducted online during the peak of the epidemic after the open policy announcement. The participants were asked to provide oral informed consent at the beginning of the online questionnaire. If they disagreed, they didn’t need to fill out a questionnaire.
Author contributions
BF: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Resources, Supervision, Validation, Writing – original draft, Writing – review & editing. HB: Data curation, Formal analysis, Supervision, Validation, Writing – review & editing. KZ: Data curation, Formal analysis, Supervision, Validation, Writing – review & editing. CM: Data curation, Formal analysis, Investigation, Writing – review & editing. XG: Data curation, Formal analysis, Investigation, Methodology, Writing – review & editing. XM: Investigation, Methodology, Validation, Writing – review & editing. CS: Data curation, Formal analysis, Investigation, Supervision, Writing – review & editing. MZ: Data curation, Formal analysis, Investigation, Validation, Writing – review & editing. JX: Data curation, Investigation, Methodology, Writing – review & editing. WZ: Data curation, Investigation, Methodology, Writing – review & editing. XZ: Data curation, Project administration, Supervision, Validation, Writing – review & editing. YZ: Conceptualization, Methodology, Project administration, Supervision, Writing – review & editing. DS: Conceptualization, Methodology, Project administration, Supervision, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
We are grateful to all the emergency medical staff who took their time to participate in the study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. World Health Organization. (n.d.) Coronavirus (COVID-19) dashboard (2023). Available at: https://covid19.who.int [Accessed August 5, 2023].
2. World Health Organization. (n.d.) Coronavirus disease 2019 (COVID-19) advice for the public. Available at: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public [Accessed January 5, 2023]
3. Jeong, H, Yim, HW, Song, YJ, Ki, M, Min, JA, Cho, J, et al. Mental health status of people isolated due to Middle East respiratory syndrome. Epidemiol Health. (2016) 38:e2016048. doi: 10.4178/epih.e2016048
4. Lu, YC, Shu, BC, Chang, YY, and Lung, FW. The mental health of hospital workers dealing with severe acute respiratory syndrome. Psychother Psychosom. (2006) 75:370–5. doi: 10.1159/000095443
5. Scott, HR, Stevelink, SAM, Gafoor, R, Lamb, D, Carr, E, Bakolis, I, et al. Prevalence of post-traumatic stress disorder and common mental disorders in health-care workers in England during the COVID-19 pandemic: a two-phase cross-sectional study. Lancet Psychiatry. (2023) 10:40–9. doi: 10.1016/S2215-0366(22)00375-3
6. Gustafson, DR, Yucel, R, Apple, SJ, Cirrone, G, Gao, H, Huang, AJ, et al. Mental health of emergency department healthcare workers during COVID-19 in Brooklyn, New York. Med Res Arch. (2022) 10:2903. doi: 10.18103/mra.v10i7.2903
7. Hill, JE, Harris, C, Danielle, LC, Boland, P, Doherty, AJ, Benedetto, V, et al. The prevalence of mental health conditions in healthcare workers during and after a pandemic: systematic review and meta-analysis. J Adv Nurs. (2022) 78:1551–73. doi: 10.1111/jan.15175
8. Aymerich, C, Pedruzo, B, Pérez, JL, Laborda, M, Herrero, J, Blanco, J, et al. COVID-19 pandemic effects on health worker’s mental health: systematic review and meta-analysis. Eur Psychiatry. (2022) 65:e10. doi: 10.1192/j.eurpsy.2022.1
9. Liu, S, Han, W, Shen, CY, Zhu, CJ, Wang, QF, Liang, XQ, et al. Depressive state in the emergency department during COVID-19: a national cross-sectional survey in China. Front Psych. (2021) 12:566990. doi: 10.3389/fpsyt.2021.566990
10. Wang, LQ, Zhang, M, Liu, GM, Nan, SY, Li, T, Xu, L, et al. Psychological impact of coronavirus disease (2019) (COVID-19) epidemic on medical staff in different posts in China: a multicenter study. J Psychiatr Res. (2020) 129:198–205. doi: 10.1016/j.jpsychires.2020.07.008
11. Tamburrino, MB, Lynch, DJ, Nagel, RW, and Smith, MK. Primary care evaluation of mental disorders (PRIME-MD) screening for minor depressive disorder in primary care. Prim Care Companion J Clin Psychiatry. (2009) 11:339–43. doi: 10.4088/PCC.08.m00711
12. Löwe, B, Kroenke, K, Herzog, W, and Gräfe, K. Measuring depression outcome with a brief self-report instrument: sensitivity to change of the patient health questionnaire (PHQ-9). J Affect Disord. (2004) 81:61–6. doi: 10.1016/S0165-0327(03)00198-8
13. Kroenke, K, Spitzer, RL, and Williams, JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. (2001) 16:606–13. doi: 10.1046/j.1525-1497.2001.016009606.x
14. Spitzer, RL, Kroenke, K, and Williams, JB. Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. JAMA. (1999) 282:1737–44. doi: 10.1001/jama.282.18.1737
15. Lai, J, Ma, S, Wang, Y, Cai, Z, Hu, J, Wei, N, et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw Open. (2020) 3:e203976. doi: 10.1001/jamanetworkopen.2020.3976
16. Walline, JH, Song, PP, Lim, AM, Hung, KK, and Graham, CA. Hong Kong emergency department attendance plummets during COVID-19. Emerg Med Australas. (2020) 32:1093–4. doi: 10.1111/1742-6723.13614
17. Ciarleglio, FA, Rigoni, M, Mereu, L, Tommaso, C, Carrara, A, Malossini, G, et al. The negative effects of COVID-19 and national lockdown on emergency surgery morbidity due to delayed access. World J Emerg Surg. (2021) 16:37. doi: 10.1186/s13017-021-00382-z
18. Torquati, L, Mielke, GI, Brown, WJ, Burton, NW, and Kolbe-Alexander, TL. Shift work and poor mental health: a meta-analysis of longitudinal studies. Am J Public Health. (2019) 109:e13–20. doi: 10.2105/AJPH.2019.305278
19. Lee, A, Myung, SK, Cho, JJ, Jung, YJ, Yoon, JL, and Kim, MY. Night shift work and risk of depression: meta-analysis of observational studies. J Korean Med Sci. (2017) 32:1091–6. doi: 10.3346/jkms.2017.32.7.1091
20. Serrano-Ripoll, MJ, Meneses-Echavez, JF, Ricci-Cabello, I, Fraile-Navarro, D, Fiol-deRoque, MA, Pastor-Moreno, G, et al. Impact of viral epidemic outbreaks on mental health of healthcare workers: a rapid systematic review and meta-analysis. J Affect Disord. (2020) 277:347–57. doi: 10.1016/j.jad.2020.08.034
21. Orrù, G, Marzetti, F, Conversano, C, Vagheggini, G, Miccoli, M, Ciacchini, R, et al. Secondary traumatic stress and burnout in healthcare workers during COVID-19 outbreak. Int J Environ Res Public Health. (2021) 18:337. doi: 10.3390/ijerph18010337
22. Johns, G, Samuel, V, Freemantle, L, Lewis, J, and Waddington, L. The global prevalence of depression and anxiety among doctors during the covid-19 pandemic: systematic review and meta-analysis. J Affect Disord. (2022) 298:431–41. doi: 10.1016/j.jad.2021.11.026
23. İlhan, B, and Küpeli, İ. Secondary traumatic stress, anxiety, and depression among emergency healthcare workers in the middle of the COVID-19 outbreak: a cross-sectional study. Am J Emerg Med. (2022) 52:99–104. doi: 10.1016/j.ajem.2021.11.051
24. Lv, C, Gan, Y, Feng, J, Yan, S, He, H, and Han, X. Occupational stress of physicians and nurses in emergency departments after contracting COVID-19 and its influencing factors: a cross-sectional study. Front Public Health. (2023) 11:1169764. doi: 10.3389/fpubh.2023.1169764
25. Yates, PJ, Benson, EV, Harris, A, and Baron, R. An investigation of factors supporting the psychological health of staff in a UK emergency department. Emerg Med J. (2012) 29:533–5. doi: 10.1136/emj.2010.099630
26. Bui, DP, Gibb, K, Fiellin, M, Rodriguez, A, Majka, C, Espineli, C, et al. Occupational COVID-19 exposures and illnesses among workers in California - analysis of a new occupational COVID-19 surveillance system. Int J Environ Res Public Health. (2023) 20:6307. doi: 10.3390/ijerph20136307
27. Xiao, J, Liu, L, Peng, Y, Wen, Y, Lv, X, Liang, L, et al. Anxiety, depression, and insomnia among nurses during the full liberalization of COVID-19: a multicenter cross-sectional analysis of the high-income region in China. Front Public Health. (2023) 11:1179755. doi: 10.3389/fpubh.2023.1179755
28. An, Y, Yang, Y, Wang, A, Li, Y, Zhang, Q, Cheung, T, et al. Prevalence of depression and its impact on quality of life among frontline nurses in emergency departments during the COVID-19 outbreak. J Affect Disord. (2020) 276:312–5. doi: 10.1016/j.jad.2020.06.047
29. Maharaj, S, Lees, T, and Lal, S. Prevalence and risk factors of depression, anxiety, and stress in a cohort of Australian nurses. Int J Environ Res Public Health. (2018) 16:61. doi: 10.3390/ijerph16010061
30. Rapisarda, F, Bergeron, N, Dufour, MM, Guay, S, and Geoffrion, S. Longitudinal assessment and determinants of short-term and longer-term psychological distress in a sample of healthcare workers during the COVID-19 pandemic in Quebec, Canada. Front Psych. (2023) 14:1112184. doi: 10.3389/fpsyt.2023.1112184
Keywords: COVID-19, overload, emergency medical staff, PHQ-9, open policy
Citation: Feng B, Bian H, Zhang K, Meng C, Gong X, Ma X, Su C, Zhou M, Xu J, Zhang W, Zhang X, Zhou Y and Shang D (2023) The workload change and depression among emergency medical staff after the open policy during COVID-19: a cross-sectional survey in Shandong, China. Front. Public Health. 11:1281787. doi: 10.3389/fpubh.2023.1281787
Edited by:
Samer El Hayek, Erada Center for Treatment and Rehab, United Arab EmiratesReviewed by:
Haidong Song, Hangzhou Seventh Peoples Hospital, ChinaCihad Dundar, Ondokuz Mayıs University, Türkiye
Agata Ewa Chudzicka-Czupała, University of Social Sciences and Humanities, Poland
Copyright © 2023 Feng, Bian, Zhang, Meng, Gong, Ma, Su, Zhou, Xu, Zhang, Zhang, Zhou and Shang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Baobao Feng, cm9iZXJ0X2ZlbmdAMTYzLmNvbQ==; Yi Zhou, eWl6aG91MTIwQHNpbmEuY29t; Deya Shang, c2RzbHl5c2R5QDEyNi5jb20=
 Baobao Feng
Baobao Feng Hongjun Bian
Hongjun Bian Ke Zhang1
Ke Zhang1