- 1Mianyang Central Hospital, School of Medicine, University of Electronic Science and Technology of China, Mianyang, China
- 2Department of neurosurgery, West China Hospital of Sichuan University, Chengdu, China
- 3College of Computer Science, Sichuan University, Chengdu, China
- 4School of Communication and Information Engineering, Chongqing University of Posts and Telecommunications, Chongqing, China
- 5Department of rehabilitation medicine, West China Hospital of Sichuan University, Chengdu, China
- 6The Fifth People’s hospital of Ningxia, Ningxia, China
Background: Minimally invasive surgery, in particular endoscopic surgery, has revolutionized the benefits for patients, but poses greater challenges for surgeons in terms of ergonomics. Integrating ergonomic assessments and interventions into the multi-stage endoscopic procedure contributes to the surgeon’s musculoskeletal health and the patient’s intraoperative safety and postoperative recovery.
Objective: The purpose of this study was to overview the objective assessment techniques, tools and assessment settings involved in endoscopic procedures over the past decade and to identify the potential factors that induce differences in high workloads in endoscopic procedures and ultimately to design a framework for ergonomic assessment in endoscopic surgery.
Methods: Literature searches were systematically conducted in the OVID, pubmed and web of science database before October 2022, and studies evaluating ergonomics during the process of endoscopic procedures or simulated procedures were both recognized.
Results: Our systematic review of 56 studies underscores ergonomic variations in endoscopic surgery. While endoscopic procedures, predominantly laparoscopy, typically incur less physical load than open surgery, extended surgical durations notably elevate ergonomic risks. Surgeon characteristics, such as experience level and gender, significantly influence these risks, with less experienced and female surgeons facing greater challenges. Key assessment tools employed include electromyography for muscle fatigue and motion analysis for postural evaluation.
Conclusion: This review aims to provide a comprehensive analysis and framework of objective ergonomic assessments in endoscopic surgery, and suggesting avenues for future research and intervention strategies. By improving the ergonomic conditions for surgeons, we can enhance their overall health, mitigate the risk of WMSDs, and ultimately improve patient outcomes.
1 Introduction
With the advancement of science and technology, the terminology of “minimally invasive” has penetrated into various fields of surgical procedures. Endoscopic surgery, in particular, has the tremendous benefits of a smaller incision, little discomfort, and a quick recovery (1), which optimizes the enhancement of patients’ quality of life and recovery and significantly lessens patients’ suffering. However, a crucial participant in this successful change, the surgeon, has borne considerable unforeseen costs and ergonomic constraints (2). Surveys on laparoscopic surgery, for instance, have revealed that 73 to 100% (3) of surgeons who conduct standard laparoscopic surgery have WMSDs (Work-related Musculoskeletal Disorders), with a range of 73 to 88% for complaints (4). This indicates a growing pandemic of patient benefit and physician misery. Unfortunately, endoscopic surgeons seldom come out to disclose injuries to their providers despite being aware of the higher physical demands and discomfort they encounter during surgery.
The development of WMSDs in endoscopic surgeons is complex and multifaceted. Unlike other occupations, several unique factors contribute to WMSDs in this group. Prolonged static positions commonly assumed during procedures lead to muscle fatigue and an elevated risk of WMSDs (5). The repetitive nature of endoscopic tasks, such as instrument manipulation and precise motor skills, can cause overuse injuries and musculoskeletal strain (6). Beyond physical strain, these procedures demand intense concentration and focus, leading to cognitive fatigue. This mental load can impair attention to proper body mechanics and temporarily mask muscle fatigue, contributing to a hazardous working environment. Furthermore, the interplay between physical and mental fatigue not only affects the surgeons but also poses a potential risk to patient safety. Fatigued surgeons operating in ergonomically challenging conditions are more likely to make errors, thereby compromising the safety of the procedures they perform (7). This connection underscores the urgent need for comprehensive strategies in healthcare that address both the physical and cognitive aspects of surgeon workload to enhance surgeon well-being and ensure patient safety.
Ergonomics is the scientific discipline which applies theory, principles, data and methods to design and optimize human well-being (the overall health and quality of life) and overall system performance (8). In the past, ergonomic assessment and intervention studies have typically focused on industrial manufacturing, however, it has recently been discovered that surgeons tend to work in harsher environments and working conditions than some industrial workers (9).
For endoscopic surgery, ergonomics can be integrated into all stages of the endoscopic surgery unit to provide a safe and comfortable ergonomic environment design for surgeons and patients (10), including preoperative surgeon scheduling, simulation training, and protocol planning; intraoperative layout and optimization of surgical instruments and patient position design; and postoperative safety care and interventions for occupational musculoskeletal disorders for endoscopic surgeons, as well as investment in construction of surgical instruments and surgical technology.
Ergonomics-based assessments assist in the early detection of environmental and individual potential factors on surgeons’ musculoskeletal health (11) and propose specific interventions. While workloads assessment has relied on paper-based subjective questionnaires over the years, with the development of information technology and human factors engineering, some objective assessment methods have emerged and have proven to be more thorough and sensitive to the identification of characterization of WMSDs (12). Motion analysis, force platform, and biochemical parameters such as surface EMG are beginning to be used in endoscopic surgery analysis of objective ergonomics for surgeons; and combined with subjective questionnaire collection to obtain high reliability assessment results.
Accordingly, given the explicit information extracted from the existing literature, the purpose of the work in this review is to analyze objective ergonomic assessment studies in endoscopic surgery to (a) ascertain the sources of heterogeneity and the threat of reproducibility, (b) identify and categorize the potential factors that induce differences in workloads, (c) summarize sound assessment frameworks, assessment instruments, assessment tools, and assessment settings, and (d) suggest future trends.
2 Methods
2.1 Search strategy and inclusion criteria
In order to achieve full coverage screening of the medical and scientific literature and to ensure that we capture a wide range of relevant research, literature searches were performed in the medical and engineering field, including pubmed, OVID databases of EMBASE, and Web of Science, for studies published from the earliest date until 2022, which ensures the reliability of included data by avoiding premature access to potentially unverified or incomplete research findings for 2023, safeguarding the robustness of our analysis while maintaining temporal consistency in our review process. Our search utilized a including of (1) Ergonomics, (2) Endoscopy, (3) Muscle strain, (4) workload, and (5) Surgeons as search strings. The inclusion and exclusion criteria of this review are listed as follows:
1. Studies had to be published with an accessible full text and written in either English, German, or Spanish.
2. The type of surgery involved in this review must be relevant to the surgical endoscopy and traditional open surgery and robotic-assisted surgery was not included in the review. When several different surgical procedures were performed in a study, at least one of those procedures is required to involve surgical endoscopy. For instance, it should be included when a study attempts to compare the ergonomic risk between endoscopic surgery and robot-assisted surgery.
3. Studies had to conclude statement about objective indicators, evaluation techniques, and conclusions, which were relevant to posture, electromyography and other physiological parameters. Studies that only based arbitrary questionnaires were disallowed.
2.2 Data extraction
Two researchers independently conducted the literature search, screening, and data extraction. Any disagreements regarding eligibility or data extraction were settled through discussion with an additional reviewer. A data extraction form was designed to store the data from the original literature, which included the following variables: publication year, sample characteristics (number of surgeons, age, and gender), type of surgery, study design, objective ergonomic risk assessment indicators, assessment sites and tools, Consolidation of subjective investigations and the outcome of the ergonomics.
3 Results
3.1 Literature search and selection
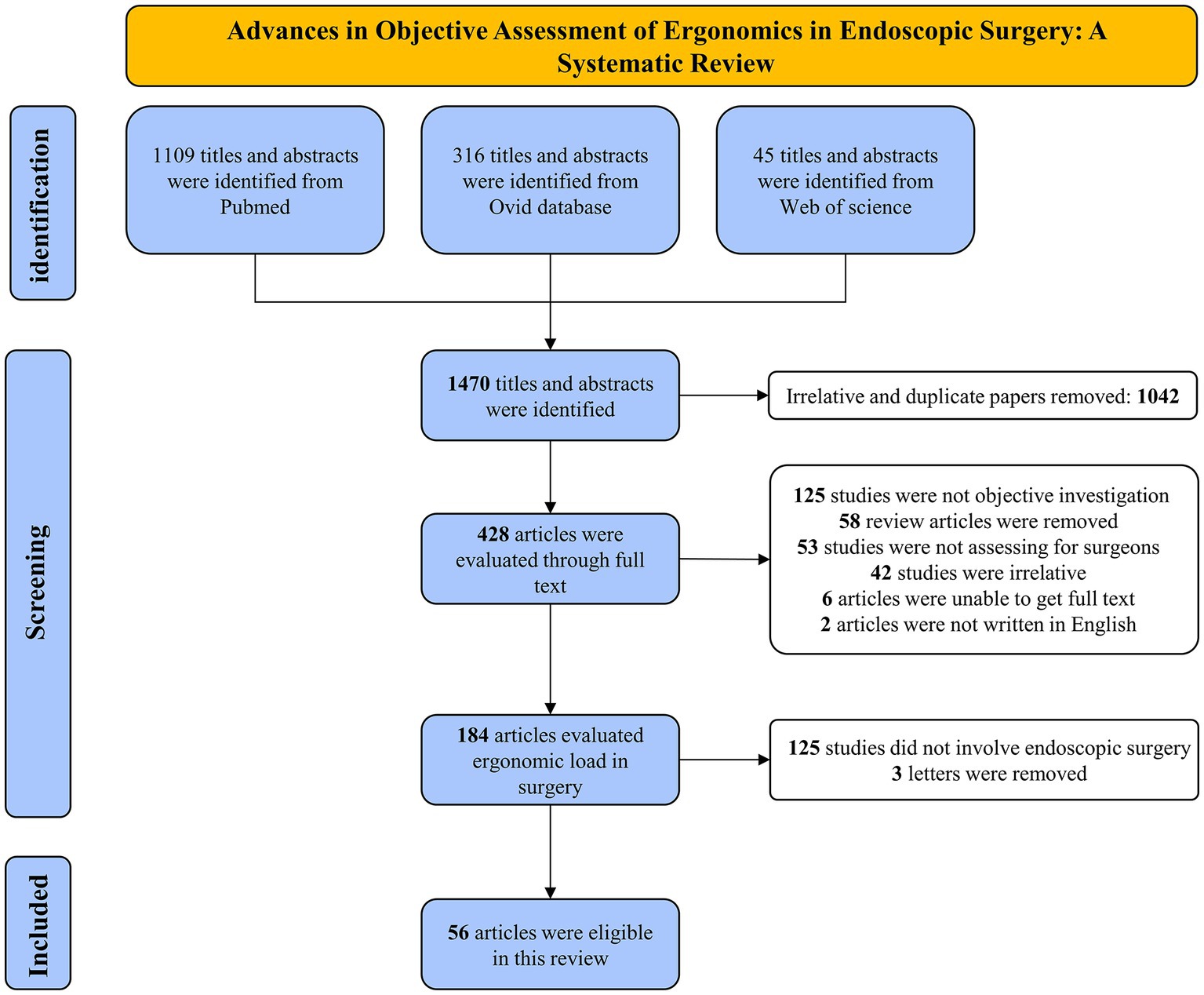
From our literature search, we identified 1,470 titles and abstracts. These were then methodically examined against specific inclusion and exclusion criteria, tailored to align with our research questions and objectives. The criteria focused on aspects like study design, target population, measured outcomes, and their pertinence to the surgical practice being studied. This rigorous examination led to the selection of 428 articles, which were then subjected to a detailed full-text analysis to further evaluate their relevance and contributions to our research. The following considerations led to the exclusion of a total of 362 articles: (1) There was no objective assessment employed; (2) It was a review of the literature; (3) The research participants were not surgeons; (4) Endoscopy was not used during the procedure; (5) The paper was not available; and (6) Language. Ultimately, a total of 56 studies were included in this systematic review (Figure 1).
3.2 Characteristics of studies
This review included 56 studies in total, 34 (60.7%) studies were from North America and 15 (26.8%) studies were from Europe. The preponderance of the publication years were from 2017 to 2022 (69.6%), with an upward trend. In addition, the number of surgeons participating were recorded with a median of 9.5.
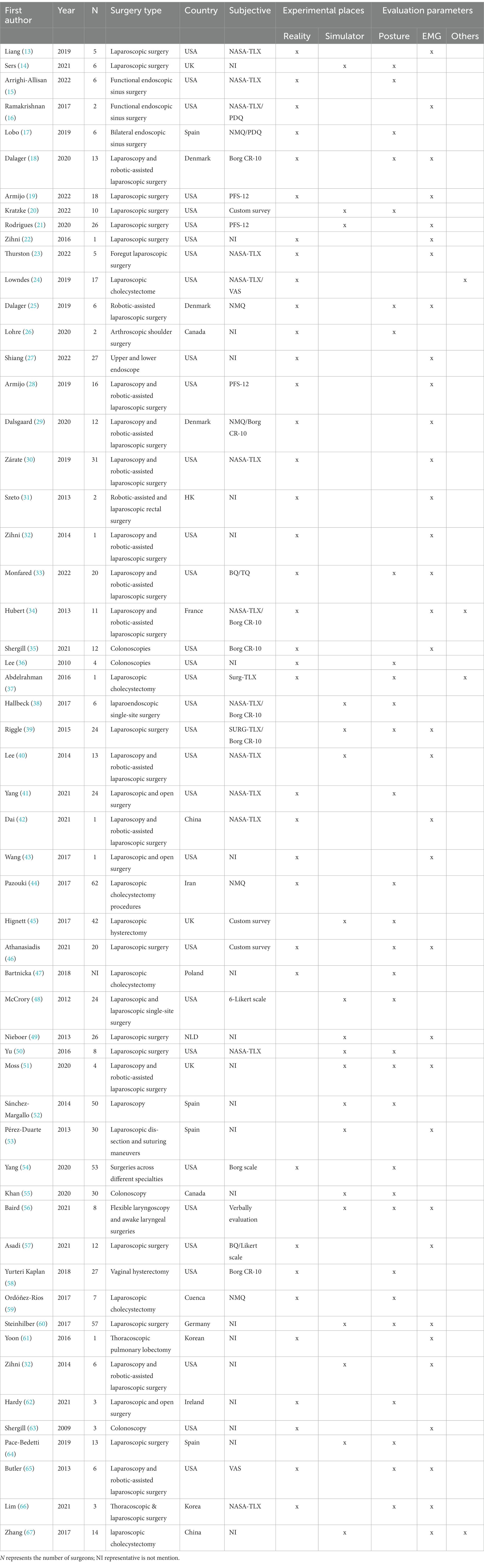
Table 1 offers a summary of the studies that were included. Of all the endoscopic surgical techniques employed in the surgeries, laparoscopy was the most frequent (n = 45), followed by, colonoscopy (n = 4), nasal endoscopy (n = 3), shoulder arthroscopy (n = 1), laryngoscopy (n = 1), thoracoscopy (n = 2), and hysteroscopy (n = 1). The types of surgeries primarily included conventional endoscopic surgeries, robot-assisted endoscopic surgeries with endoscopy (n = 14). Some open surgeries were incorporated in order to engage in comparisons (n = 3).
Although the objective of this systematic review focused on ergonomics quantitative methods for endoscopic surgeries, up to 62.5% (n = 35) of the studies used a conjunction analysis of subjective questionnaires to evaluate the ultimate results simultaneously. Eleven types of questionnaires were applied in these studies, consisting mainly of investigative questionnaires for musculoskeletal disorders/discomfort, and immediate questionnaires to evaluate workload or fatigue.
NASA Task Load Index (NASA-TLX) was the most utilized questionnaire in these studies (n = 13) which allows users to perform subjective workload in mental demand, physical demand, temporal demand, performance, effort and frustration (68).
Objective assessment of ergonomics was based on electromyographic (n = 34) and motion analysis (n = 30). Four studies used other tools such as heart rate and salivary cortisol as ergonomics indicators and 12 studies combined more than 2 instruments for the assessment of ergonomics study designs tended to be cross-sectional (n = 23) and cohort (n = 27), while RCT were utilized in 5 research and case–control was only employed in 1 interventional study.
3.3 Methodology of objective assessment in endoscopic ergonomics
3.3.1 Potential factors of ergonomic risk difference
Potential factors leading to a higher ergonomic risk were grouped into three categories: (1) Work task related factors; (2) Characteristics (surgeon and patient)-related factors; and (3) Environment-related factors.
3.3.1.1 Work task
The work task related load consists mainly of different types of surgeries, surgical equipment, assignment of surgical tasks, and duration and number of surgeries.
3.3.1.1.1 Surgery type
In the included literature, 20 studies focused on ergonomics differences between surgeons or surgeon teams due to different types of procedures, especially focus on the differences among open, endoscopic and robotic-assisted surgery. Among comparative studies of traditional open versus laparoscopic surgery, one study measured the activation of the upper body muscles during the laparoscopic and open phases of sigmoid colectomies and demonstrated that the laparoscopic surgery provides ergonomic benefits in several upper muscle groups compared to the open surgery (41). The average neck and trunk angle was shown to be considerably higher for open surgery than for laparoscopic surgery in two studies (41, 54) And when compared to laparoscopic surgery, open surgery involved much longer time spent in the physically taxing torso position (54). In contrast to these views, a study explored the sagittal and rotational movements of the neck in laparoscopic surgery versus open surgery. The results of the study showed that laparoscopic surgery required significantly less skin stretching during flexion and rotational movements compared to open surgery, which demonstrated that laparoscopic surgery requires a longer period of static neck position (62). Robot-assisted surgery can improve the flexibility of surgical operations, reduce tremors, and optimize the surgeon’s workload and physical strain based on ergonomic principles. Several studies have indicated superior performance in terms of postural stability (65), cumulative muscle strain (40), workload (34), and physical demands (29) for robot-assisted surgery compared to conventional endoscopic surgery. Notably, while robot-assisted surgery reduces postoperative discomfort and muscle strain in the upper extremity for the surgeon, it increases static neck positioning and back stiffness compared to endoscopy. Additionally, forearm muscles, particularly those that manage the ulnar offset movements of the wrist joint, exhibit a considerable level of muscle exertion during robot-assisted surgery (31).
3.3.1.1.2 Surgical equipment
A possible reason for the musculoskeletal symptoms reported by surgeons is the ergonomic limitations of the surgical handles designed for surgeon (69). All surgeons involved in such procedures are at risk for complications in the left and right wrist, right thumb, and left thumb. The left thumb and both wrists exceed the limits of movement and are at risk for repetitive motion injuries (63). Five studies explored handle settings in endoscopic surgery and examinations were included in this systematic review, and they focused on laparoscopic and colonoscopic handles. Some endoscopes that are more biomechanically compatible have been developed and have been shown to be beneficial in reducing the ergonomics on the surgeon (24, 39, 50). It is worth noting that the angular configuration of the endoscope (50), the height difference between the endoscope and the table, and the area of the operating field (60) all contribute to the occurrence of ergonomic risk differences. Veelen et al. have identified the ideal relationship between surgeon height and patient abdominal wall (PAW) location (70). The anterior claw’s tip need to be positioned between 70 and 80% of the surgeon’s elbow height. The suggested table height is deduced from the fact that the abdominal sagittal depth is contained at intervals of 30 to 40 cm. Furthermore, a study confirmed that laparoscopic tools with adjustable handle angles decrease the ergonomic risk of musculoskeletal strain and allow alternating tasks between floor and ceiling positions without compromising surgical performance (50).
3.3.1.1.3 Duration of surgery
Colonoscopy procedures, thoracoscopic lobectomies, and a comparative study of open and laparoscopic surgeries all highlight the relationship between surgical duration and ergonomics. In colonoscopies, which average about 19.5 min, significant muscle loads in the forearms and excessive pinch forces can pose ergonomic risks, suggesting that even shorter surgeries can be demanding due to repetitive tasks (63). Thoracoscopic lobectomies, lasting around 99 min, show notable muscle fatigue, especially in muscles like the lumbar erector spinae due to prolonged static postures, highlighting the cumulative effect of longer surgeries (61). Furthermore, a comparative study of open and laparoscopic surgeries reveals that longer procedures in both types lead to increased self-rated fatigue and pain, particularly in the neck and lower back. Open surgeries pose a higher postural risk due to larger neck and torso angles (41). This underscores the need for ergonomic interventions in surgeries, as surgeons often maintain high-risk postures for extended periods, affecting various body parts irrespective of the surgery type or duration.
3.3.1.2 Characteristics (surgeon and patient)
A comprehensive review of fourteen studies revealed several key findings regarding the impact of surgeons’ characteristics on their physical and psychological loads. These studies identified gender disparities, with results showing that women surgeons experience more physical load and fatigue during surgeries compared to their male counterparts (19). Variations in surgical experience also influence ergonomic loads, as surgeons with less experience or fewer years in their career were found to face higher physical strain (15, 23, 44). In addition, surgeon assistants and operating room nurses are subjected to severe ergonomic loads comparable to those experienced by surgeons (22, 44). The studies also examined the effect of surgical posture, revealing slight differences in ergonomic load between standing and sitting positions during endoscopic procedures. Specifically, in functional nasal endoscopy, surgeons face different workloads risks depending on whether they are standing or sitting, with sitting posing a greater risk to the upper extremity and standing to the legs (15, 16).
Furthermore, five studies investigated the relationship between patient characteristics and ergonomic load on surgeons. These studies focused on factors such as patient Body Mass Index (BMI) and positioning during surgery. It was found that performing laparoscopic surgery on patients with high BMI resulted in increased non-neutral postures and musculoskeletal discomfort for surgeons (14, 51). Contrarily, some studies reported no significant differences in ergonomic stress or workload when operating on obese versus non-obese patients (13). Additionally, the patient’s positioning during surgery was found to affect surgeon ergonomics, as demonstrated in a study where the lateral position during shoulder arthroscopy posed a higher ergonomic risk to orthopedic surgeons compared to the beach chair position (26).
3.3.1.3 Environment-related factors
Environment-related factors within the operating room (OR) significantly influence the ergonomic experience of endoscopic surgeons. The positioning of assistant surgeons, the arrangement of video displays, and the layout of surgical components and pedals are pivotal. Moreover, the height and design of operating beds and chairs, along with the ergonomics of surgical tools and handles, play a crucial role in surgeon performance and comfort (59). Head equipment, like headlamps and magnifiers, though essential, can contribute to musculoskeletal strain and ergonomic stress, necessitating careful design considerations to reduce the physical burden on surgeons during endoscopic procedures (3, 71).
3.3.2 Ergonomics assessment tools
3.3.2.1 Motion analysis-based
The optimum surgical posture aids in the optimization of the surgeon’s physical load and the evaluation and generalization of these postures lie under the purview of motion analysis. To objectively quantify postural load, 30 studies have tried to capture, track, and analyze surgeons’ actions intraoperatively, based on a perspective of motion analysis. Generally, intraoperative posture data acquisition relies on optical sensors and inertial sensors, the former including conventional cameras, depth structured light cameras, and optical tracking systems. Using a standard camera to record a surgeon’s surgery or taking interval photos is one of the most archaic techniques. One representative of a structured light camera sensor is the Kinect. The most recent version of Azure Kinect is outfitted with an orientation sensor for sophisticated computer vision model development, a 12 megapixel full HD camera, and a 1 megapixel improved depth camera. It has body segmentation capabilities that can produce an anatomically accurate skeleton that contains either the entire or the parts of the body.
A study used an optical tracking system to compare the kinematic differences between surgeons with straight and curved instruments (38). Optical tracking systems typically require participants to wear passive mirror-reflective markers or active LEDs and operate with the aid of high-speed cameras to reconstruct the virtual human body as a real-time action.
By integrating dispersed IMUs (Inertial Measurement Units) into the wearable accessory, the inertial sensor—which is made up of an angle meter, an accelerometer, and a gravimeter—allows for the capturing of human motion. IMUs from APDM Wearable Technologies was most frequently employed among the included researches (n = 5), and Perception Neuron from Noitom was also be employed (n = 1).
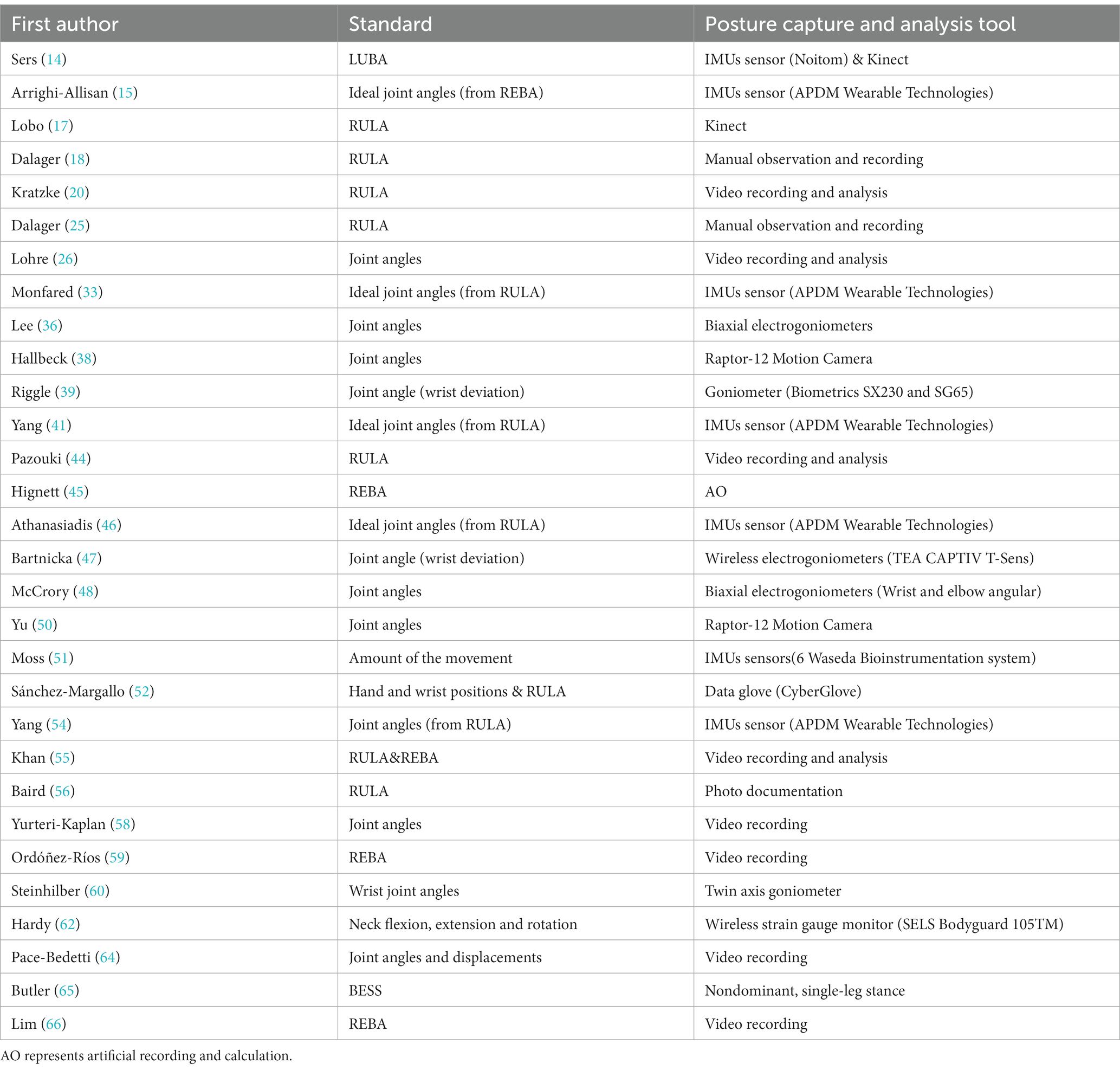
For angular motion capture of particular locations, the inertial measurement unit can also be utilized by itself. In order to detect motion tracking and body angles in the surgeon’s upper body, Monfared and Athanasiadia positioned the IMU sensors on the surgeon’s torso, head, chest, low back, and right and left biceps (33, 46) (Table 2).
Ergonomic assessment tools such as electrogoniometers are also widely used when researchers are more concerned with localized high loads on the human body (n = 4). Furthermore, when exploring the effects of laparoscopic handles on surgeon physical loads, researchers typically focus more on surgeon forearm, elbow, wrist, and finger activities. Hence, it is also desirable to capture the surgeon’s hands motion utilizing data gloves (n = 1), which are consists of a series of conductive sensors with sensitive resistive flow that detects changes in bending and is capable of recording the relative angle of deflection of the hand.
Commonly analyzed indicators include joint angles and ergonomics rating scales. Ergonomics scales incorporate joint angles of body subcomponents (e.g., trunk, neck, legs, upper arms, lower arms and wrist) and are evaluated in conjunction with the parameters of force, coupling, and duration. Of the included literature, RULA (Rapid upper larms assessment) is the most frequently used ergonomics rating scale (n = 12), followed by REBA (n = 5) and LUBA (n = 1). RULA, as the most widely used ergonomic scale, is created exclusively for light labor and concentrates on the classification of postural risk for the upper limb (72). REBA is a postural analysis system that is sensitive to musculoskeletal concerns in a variety of occupations, particularly in the health care and other service industries (73). Unlike RULA, REBA divides the joint movements of the entire body into several groups. One study measured ergonomics based on the LUBA scale, which was selected for the presence of prolonged low-risk postures and intermittent high-risk postures in laparoscopic surgery, which is consistent with the properties of LUBA for medium-risk settings (74). In general, higher ergonomics scores often indicate greater risk exposure and alertness to the need for urgent change.
When the motion data is being analyzed, ergonomists or occupational therapists can use intraoperative video/image data captured by the camera to manually generate ergonomics scores. Additionally, certain recent computer vision-based techniques can be utilized to extract human skeleton postures from videos and automatically determine ergonomic scores. A study was conducted to evaluate the body positioning of residents during laparoscopic surgery, and a computer vision algorithm based on Openpose and SMPL-X was designed for estimating the RULA score from 2D images/videos (20). To acquire the necessary joint angle data, the raw data captured by the inertial sensors typically needs to be filtered, smoothed, and denoised. These processes are carried out directly within the Matlab program, and some advanced IMUs solutions additionally offer software platforms for automated analysis. It is significant to mention that before any official measurements can be taken, all sensors must be calibrated beforehand in the environment.
3.3.2.2 sEMG-based
The endoscopic surgeon’s awkward posture, keeping the arm in an elevated position, and the use of high level strength instruments all cause an accumulation of muscle stresses that can cause microtrauma to the muscle tissues, leading to inflammation, pain, and ultimately, tissue damage. If the accumulated tissue damage exceeds the body’s ability to repair itself, it can lead to chronic musculoskeletal disease. Therefore, understanding muscle fatigue induced by surgical procedures in endoscopic surgeons can help guide the development of targeted interventions.
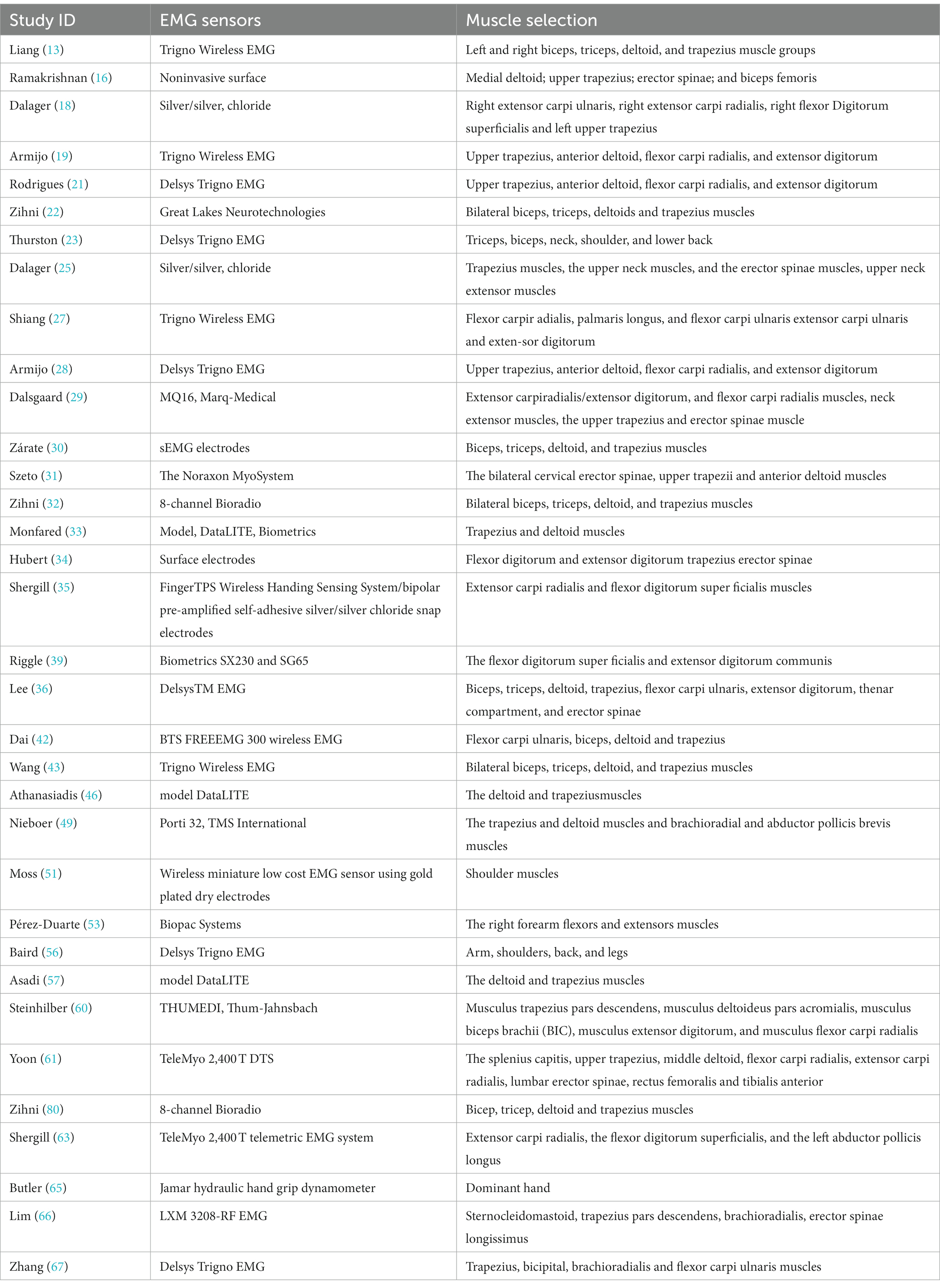
One of the important tools to measure muscle fatigue is electromyography (EMG), EMG signals are frequently used to assess muscle fatigue and ergonomics in occupational settings. Traditionally, invasive needle electrodes were used to obtain EMG signals, but recent advancements have made wireless surface EMG sensors the preferred method due to their convenience and accuracy.
EMG signals can be analyzed in both the time and frequency domains. Following signal acquisition, rectification, smoothing, and maximum voluntary contraction (MVC) normalization are typically performed. Commonly used metrics in the time domain include the integrated EMG value (iEMG) and root mean square (RMS). iEMG represents the intensity of muscle activity over a certain period, while RMS describes the average variation in surface EMG amplitude. In the frequency domain, median frequency (mDF) and mean power frequency (MPF) are commonly used metrics. MVC% is also a widely used EMG parameter that represents the percentage of actual EMG amplitude to the EMG amplitude at maximum voluntary contraction. Other metrics such as amplitude probability distribution function (APDF) and relative activation time (RAT) are also used.
Among the muscle groups involved in the included literature (Table 3), the most frequent EMG assessment regarding the trapezius muscle (n = 24) was followed only by the deltoid muscle (n = 19). In addition, the biceps, triceps erector spinae, radial wrist flexors, finger extensors, superficial finger flexors, cervical erector spinae, and wrist extensors were also frequently present. Interestingly, most of the included literature focused on Upper Extremity muscles, with only 1 study on thoracoscopic lobectomy and mediastinal lymph node dissection for lung cancer that included the rectus femoris and anterior tibialis muscles of the lower limb (61). A study quantifying and comparing surgeons’ ergonomic pressures during laparoscopic versus open access for sigmoid resection found that degree of surgical difficulty may have less impact laparoscopically compared to open access (43).Furthermore, a study to assess differences in physical load among surgeons with different surgical experience collected EMG activity of surgeons’ upper extremity muscles during laparoscopy, demonstrating higher RVC and MF levels intraoperatively for less experienced surgeons (23).
The muscle activation of the upper trapezius (UT), anterior deltoid (AD), and radial carpal flexor (FCR) muscles during the surgeon’s execution of the robot-assisted surgery phase showed a higher level of activation compared to performing a conventional laparoscopic procedure (28). In addition, one study found female had greater muscle effort than male in laparoscopic surgery (19).
3.3.2.3 Other tools-based
In addition to the feature of surface EMG signal as a biomarker of ergonomics, several other non-invasive biomarkers have been used to quantify the ergonomics of endoscopic surgeons. Previous studies have indicated that heart rate variability markers in the frequency domain, such as low frequency and high frequency, can give some indication of changes in physical and psychological loads. Moreover, mean heart rate and mean heart rate “cost” (intraoperative heart rate – resting heart rate) were also employed in a study to investigate the difference in workload between standard LAP and Robot-assisted surgery, and ultimately found that standard laparoscopic surgeons had increased heart rates compared to robot-assisted surgery (34). Salivary cortisol levels, a stress hormone, were employed in two trials to measure the ergonomics on laparoscopic surgeons. At various points during the process, they collected surgeon saliva using collection aid. The samples were then frozen, and at the conclusion of the trial, they were thawed and examined (24, 37), and both studies ultimately found that surgeons’ salivary cortisol levels were significantly higher during single-incision laparoscopic cholecystectomy than during conventional laparoscopic surgery. Eye tracking data, especially pupillary dilation, are typically sensitive to task difficulty and workload (75), and Zhang measured the psychological load on participants during the procedure by recording the physiological parameters of their eyes through an oculomotor while performing the task in the laparoscopic simulator (67).
3.3.3 Evaluation places
The integrity and validity of ergonomic assessment outcomes hold profound significance in surgical practice, demanding meticulous consideration of the chosen assessment site. Notably, 64.3% of the studies conducted meticulous trials within real operating room (OR) settings, while 35.7% (n = 20) employed surgical simulators to explore ergonomic intricacies. The authenticity of real-life OR surgery exposes surgeons to genuine occupational challenges, thereby rendering assessment outcomes more robust and clinically applicable.
Nonetheless, real-life OR surgery is not devoid of challenges that necessitate attention. Intrusion of ergonomic data capture instruments may inadvertently divert the surgeon’s focus; wearable instruments could contribute to an additional physical burden; the stringent requirement of sterilization for OR instruments might jeopardize the integrity of sophisticated equipment; and patient reluctance poses another practical hurdle. To circumvent these intricacies, the implementation of cadaveric surgery emerges as an attractive alternative. Intriguingly, nasal endoscopy studies based on cadaveric surgery, instead of clinical surgery, have discerned ergonomic disparities related to surgeon posture, ultimately yielding reliable conclusions (16, 17). Cadaveric surgery, although akin to real-life OR conditions, offers an exceptionally high-fidelity replication of clinical surgery’s tactile and visual aspects. It’s noteworthy that cost considerations have motivated certain researchers to compare robot-assisted laparoscopic surgery to traditional laparoscopic procedures using animal models (34, 42).
In parallel, surgical simulators emerge as instrumental tools, distinguished by their economic viability, controlled environmental factors, and ready accessibility. Within the realm of laparoscopy-related investigations, open-up simulators, box simulators, and virtual reality simulators are recurrently employed, primarily for training and preoperative assessment purposes. Open-up simulators cater to fundamental tasks encompassing handle movement, object manipulation, suturing, and cutting. Progressively complex, box simulators replicate realistic surgical settings, encompassing cannula needles, light sources, and real-time visual feedback. Virtual reality simulators, harnessed by panoramic computer vision and force feedback, simulate abdominal images with remarkable realism akin to genuine OR scenarios, affording opportunities for intricate surgical simulations.
Delving into the clinical realm, distinctions in upper extremity fatigue are perceptible between laparoscopic and robotic surgical training environments (40). In the study’s scope, a laparoscopic box simulator was juxtaposed against a robotic surgical training simulator, emulating the da Vinci system. Furthermore, investigations addressing surgeon postural load and muscle strain within box simulators employing foam of varying thicknesses to mimic patient BMI underscore the clinical relevance of ergonomic research (14, 51). Beyond laparoscopy, specialized simulators for nasal endoscopy and colonoscopy have been developed, enhancing training and assessment precision (55, 56).
In evaluating the ecological validity of simulations used in ergonomic assessments, it is crucial to recognize both their strengths and limitations in mimicking real surgical environments. Simulations offer a controlled, replicable setting for detailed ergonomic analysis, allowing researchers to isolate and study specific variables in depth. This controlled environment is particularly beneficial for initial training and for studying the ergonomic impact of specific tasks or equipment under standardized conditions. However, the ecological validity of these simulations is inherently limited by their inability to fully replicate the dynamic and often unpredictable nature of actual surgical procedures. Real-life surgeries involve variables such as patient-specific anatomical challenges, intraoperative complications, and varying team dynamics, which are difficult to reproduce in a simulated setting (76). Moreover, the stress and pressures experienced by surgeons in actual operations, which can significantly impact ergonomic load and cognitive function, are often attenuated in simulated environments.
3.3.4 Proposed framework for endoscopic ergonomics research
The comprehensive framework developed in this study, as depicted in Figure 2, is grounded in the critical evaluation of ergonomic assessment methodologies analyzed in previous sections. It systematically organizes the findings into a cohesive structure aimed at enhancing ergonomic evaluations. The “Identification of Factors” component draws from the diverse variables discussed earlier, such as surgeon’s posture and patient BMI, and situates them within a broader context affecting workload. “Selection of Evaluation Setting” takes into consideration the detailed examination of various settings, from ORs to simulations, acknowledging their respective strengths and limitations. The “Data Collection Methodology” integrates the diverse data types, from subjective questionnaires to objective measures like EMG, discussed throughout the review. This meticulously crafted framework thus serves as a testament to the synthesis of our findings, presenting a pathway for deploying these insights into practical, real-world applications that address the ergonomic challenges identified.
3.4 Interventions to reduce workload
Ergonomic assessment forms the bedrock for effective interventions. Common intervention approaches predominantly hinge on ergonomics education, encompassing expert presentations, lectures, and video modules. Simulation-based ergonomics training courses showcase potential benefits in mitigating work-related musculoskeletal injuries. Furthermore, real-time biofeedback presents a promising avenue for intervention, as does postural alignment to circumvent non-neutral postures that exacerbate musculoskeletal disorders. Emerging technologies like augmented reality glasses (ARG) and exoskeleton devices are indicative of the multifaceted approach required to address ergonomic challenges. In video-assisted surgery, the use of ARGs instead of conventional monitor devices can significantly reduce the surgeon’s workload and physical demands, especially for the upper body (66). Moreover, interventions like intraoperative targeted stretching micro breaks (TSMBs), which consisting of five standardized exercises for the neck, shoulders, upper back, lower back, wrists, hands, knees and ankles involving flexion, extension and lateral rotation (77), highlighting their potential in reducing surgeon discomfort while enhancing performance and focus. The current demand for ergonomic interventions signals the need for adequate supply, necessitating innovative integration of human factors engineering and human-machine interaction technologies for more effective and intelligent feedback mechanisms to optimize surgical safety (78).
4 Discussion
This review aimed to comprehensively synthesize the literature concerning the objective assessment and quantification of ergonomics in endoscopic surgery, with the goal of constructing a robust intraoperative assessment framework and extrapolating applicable evaluation techniques and settings. By categorizing and elucidating influencing factors, we also evaluated the evidence linking these factors to elevated ergonomics in endoscopic surgery. This pursuit aligns with the domain of human factors engineering, wherein research endeavors strive to understand, evaluate, and optimize human-environment interactions to enhance system performance without compromising human well-being. Modern minimally invasive techniques, like endoscopy, afford patients the advantages of convenience, efficiency, and reduced invasiveness. However, for endoscopic surgeons, particularly given the prevalence of work-related musculoskeletal disorders (WMSDs), the associated physical health risks are paramount. Notably, these risks extend beyond the individual surgeon, as discomfort resulting from human-machine system variables can reverberate into the surgical performance and patient safety (79). Thus, discerning the impact of evolving human-system dynamics on ergonomics and exhaustively quantifying workload and ergonomic factors within the surgical specialty become paramount.
This review takes a comprehensive approach by encompassing various endoscopic specialties, addressing a significant gap in the literature. This expansion beyond the prevailing focus on endoscopic procedures allows for a deeper understanding of ergonomic challenges in diverse surgical domains, including laryngoscopy, nasal endoscopy, thoracoscopy, arthroscopy, and gynecologic endoscopy. In contrast to past studies, our review stands out in its primary focus on “objective” ergonomics assessment, a distinctive feature that has been absent in many previous discussions. Thirdly, we categorize physical and psychological loads disparities into three overarching factors, providing a structured framework for understanding and addressing these issues, thus identifying specific areas for intervention. Fourthly, we underscore the integration of multiple assessment methods, such as motion analysis, surface electromyography, and heart rate variability, resulting in a multi-faceted analysis of ergonomic risks that enriches the evaluation of ergonomic well-being. Finally, our discussion of intervention strategies, including ergonomics education, simulation-based training, real-time biofeedback, and emerging technologies like augmented reality glasses and exoskeleton devices, not only identifies potential solutions but also acknowledges the dynamic nature of the field. In sum, our article offers a holistic understanding of ergonomic challenges, provides a structured framework, and offers practical insights for addressing these issues, making a significant contribution to the field of endoscopic surgery ergonomics.
The prevailing landscape of objective ergonomic evaluations predominantly centers around general surgical applications associated with laparoscopic procedures. Nevertheless, a notable paucity persists in the comprehensive and unbiased quantitative exploration of other endoscopic specialties, including laryngoscopy, nasal endoscopy, thoracoscopy, arthroscopy, and gynecologic endoscopy. These domains warrant further investigation to foster a holistic understanding of ergonomic challenges. Challenges persist in task design, data collection, and analysis complexity, underscoring the need for rigorous investigations that transcend opportunistic research designs characterized by limited sample sizes and short observation periods. Enhancing generalizability and reliability mandates robust study designs with larger cohorts and extended observation windows, across a wider spectrum of endoscopic procedures to capture the intricacies of diverse surgical specialties.
Ergonomics disparities are primarily shaped by three overarching factors: the work task, characteristics related variables, and environmental influences. Existing literature suggests the superiority of laparoscopic surgery over traditional open procedures in terms of both surgical performance and surgeon well-being. Furthermore, robotic-assisted endoscopic surgery emerges as a means to alleviate physical demands on surgeons. The selection of surgery type should align with patient needs, financial considerations, and potential muscle injuries. Delving into surgeon-related factors, optimizing for risk factors such as surgical posture becomes vital, with implications for improved performance distribution and strategic allowances. Gender disparities in ergonomic risks, as evidenced by higher physical loads endured by female surgeons during endoscopic surgeries, underscore the need for tailored interventions like additional breaks and performance considerations. In considering patient-related factors, meticulous preoperative planning must factor in physiological attributes like position and BMI, striving to minimize additional physical stress on the surgeon. Environmental factors, amenable to manipulation, offer opportunities to optimize surgical team arrangement, bed height, instrument positioning, and related parameters through anthropometric principles (Table 3).
The assessment phase mandates comprehensive evaluation encompassing both physiological and psychological burdens on the endoscopic surgeon. Commonly employed methods for objective ergonomic quantification include motion analysis and electromyographic signals. While traditional photogrametry is surpassed by motion analysis, advanced human skeleton prediction techniques rooted in computer visiozn or inertial sensing find broad application. Electromyography (EMG) signals enable the assessment of ergonomic compliance, while quantifying the mental load during endoscopy, vital given its association with WMSDs, relies on indicators such as EEG, ECG, EDA, and eye movement. Harmonizing physical and mental load assessment, coupled with in-depth comprehension of their intricate interplay, holds the potential to enhance overall ergonomic well-being among endoscopic surgeons. It’s worth noting that in the context of assessing the psychological burden on endoscopists, our review identifies a significant gap: the predominant reliance on subjective questionnaires to measure mental load. This is despite acknowledging that such approaches may not capture the full spectrum of cognitive demands. Notably, only one study within our reviewed literature incorporated an objective indicator of psychological load—HRV (37). This highlights a critical deficiency in current research and underscores the potential for future investigations to employ objective methods such as HRV. Advancing this direction could yield more accurate assessments of the mental burden on endoscopists, informing targeted strategies to alleviate this burden and enhance overall patient care.
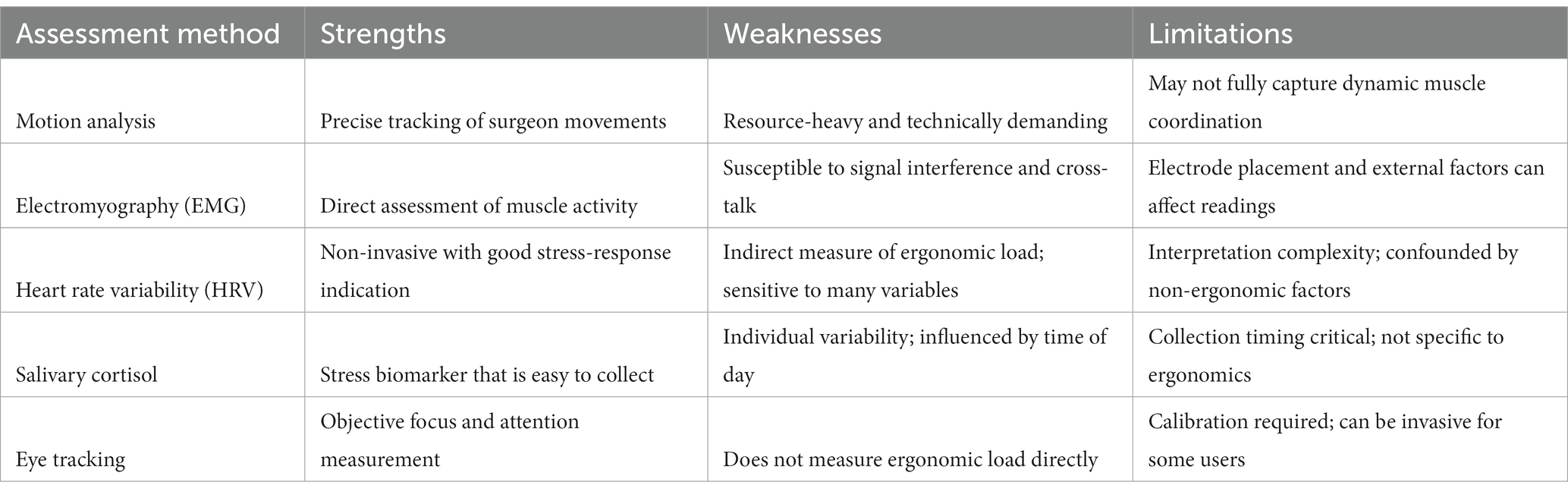
In our systematic review of ergonomic assessment methods in endoscopic surgery, we identified distinct strengths and limitations for each approach. Motion analysis stands out for its precision in tracking movements but is limited by its need for specialized environments and equipment (83, 84), potentially reducing its practicality in real surgical settings. Electromyography offers direct muscle exertion insights, yet is hindered by susceptibility to signal interference and the challenges of electrode placement in sterile conditions (85). Heart rate variability, while a useful non-invasive mental load indicator (86), lacks specificity to ergonomic stress due to its sensitivity to various factors (87). Similarly, salivary cortisol provides stress biomarkers but is affected by individual variability and diurnal patterns, limiting its immediate relevance to ergonomic assessment. Eye tracking technology, though valuable for measuring attentional focus, does not directly assess ergonomic load and requires careful calibration. These findings underscore the need for a multifaceted and practical approach in ergonomic assessment, integrating both objective measurements and subjective feedback to comprehensively address the ergonomic challenges in surgical environments. Table 4 summarizes the advantages, disadvantages, and limitations of these assessment tool.
Composite assessment methodologies integrating parameters like motion analysis, surface EMG, and heart rate variability have emerged as vital tools for ergonomic risk assessment. This multi-faceted analysis probes intraoperative ergonomics from diverse dimensions, enriching assessment comprehensiveness. While real-life OR surgery provides high reliability assessments, the associated surgical risks, including unpredictable intraoperative data collection and potential instrument damage, limit its feasibility. Similarly, while cadaveric surgery offers a high-fidelity assessment environment, practical constraints like expense and scarcity hamper its widespread application. Ergonomic evaluation within surgical simulator environments emerges as a viable alternative, albeit with a current focus on novice training rather than comprehensive ergonomic exploration. This gap warrants addressing for optimal integration into surgical practice.
5 Conclusion
The review identified three primary categories influencing ergonomic load in endoscopic surgery: environmental factors, characteristics-related factors and factors related to work task and proposed an overall research framework. The studies revealed that ergonomic challenges are prevalent in real and simulated surgical environments, with a significant impact on workloads. Our analysis underscores the multifaceted nature of ergonomic risks in endoscopic procedures. It highlights the importance of considering the entire surgical ecosystem, including the surgical team, equipment, patient characteristics, and the specific surgical procedure, to effectively address these challenges. The findings from this comprehensive review serve as a pivotal guide for future ergonomic assessments and interventions aimed at enhancing surgeon well-being and patient safety in endoscopic surgery.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding authors.
Author contributions
SL: Conceptualization, Data curation, Writing – original draft. Y-YL: Data curation, Visualization, Writing – original draft. DL: Data curation, Writing – original draft. F-YW: Writing – review & editing. L-JF: Writing – review & editing. L-xZ: Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
We are deeply grateful to Mianyang Central Hospital and Sichuan University for providing literature search support.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Sakai, P, and Faintuch, J. Evolving endoscopic surgery. J Gastroenterol Hepatol. (2014) 29:1132–8. doi: 10.1111/jgh.12577
2. Park, A, Lee, G, Seagull, FJ, Meenaghan, N, and Dexter, D. Patients benefit while surgeons suffer: an impending epidemic. J Am Coll Surg. (2010) 210:306–13. doi: 10.1016/j.jamcollsurg.2009.10.017
3. Catanzarite, T, Tan-Kim, J, Whitcomb, EL, and Menefee, S. Ergonomics in surgery: a review. Female Pelvic Med Reconstr Surg. (2018) 24:1–12. doi: 10.1097/SPV.0000000000000456
4. Alleblas, CCJ, de Man, AM, van den Haak, L, Vierhout, ME, Jansen, FW, and Nieboer, TE. Prevalence of musculoskeletal disorders among surgeons performing minimally invasive surgery: a systematic review. Ann Surg. (2017) 266:905–20. doi: 10.1097/SLA.0000000000002223
5. Szeto, G, Ho, P, Ting, A, Poon, J, Cheng, S, and Tsang, R. Work-related musculoskeletal symptoms in surgeons. J Occup Rehabil. (2009) 19:175–84. doi: 10.1007/s10926-009-9176-1
6. Davis, WT, Fletcher, SA, and Guillamondegui, OD. Musculoskeletal occupational injury among surgeons: effects for patients, providers, and institutions. J Surg Res. (2014) 189:207–212.e6. doi: 10.1016/j.jss.2014.03.013
7. Lowndes, BR, and Hallbeck, MS. Overview of human factors and ergonomics in the OR, with an emphasis on minimally invasive surgeries. Hum Factors Ergon Manuf Serv Ind. (2014) 24:308–17. doi: 10.1002/hfm.20383
8. International Ergonomics Association (IEA) Council . Definition and domains of ergonomics. Available at: http://www.iea.cc/whats/index.html (Accessed January 22, 2016).
9. Seagull, FJ . Disparities between industrial and surgical ergonomics. Work. (2012) 41:4669–72. doi: 10.3233/WOR-2012-0107-4669
10. Lipowska, AM, and Shergill, AK. Ergonomics of endoscopy. Gastrointest Endosc Clin N Am. (2021) 31:655–69. doi: 10.1016/j.giec.2021.05.003
11. Kim, SE, and Junggi Hong, PDATC. Ergonomic interventions as a treatment and preventative tool for work-related musculoskeletal disorders. Int J Caring Sci. (2013) 6:339.
12. David, GC . Ergonomic methods for assessing exposure to risk factors for work-related musculoskeletal disorders. Occup Med. (2005) 55:190–9. doi: 10.1093/occmed/kqi082
13. Liang, Z, Gerull, WD, Wang, R, Zihni, A, Ray, S, and Awad, M. Effect of patient body mass index on laparoscopic surgical ergonomics. Obes Surg. (2019) 29:1709–13. doi: 10.1007/s11695-019-03748-0
14. Sers, R, Forrester, S, Zecca, M, Ward, S, and Moss, E. The ergonomic impact of patient body mass index on surgeon posture during simulated laparoscopy. Appl Ergon. (2021) 97:103501. doi: 10.1016/j.apergo.2021.103501
15. Arrighi-Allisan, AE, Garvey, KL, Wong, A, Filip, P, Shah, J, Spock, T, et al. Ergonomic analysis of functional endoscopic sinus surgery using novel inertial sensors. Laryngoscope. (2022) 132:1153–9. doi: 10.1002/lary.29796
16. Ramakrishnan, VR, and Milam, BM. Ergonomic analysis of the surgical position in functional endoscopic sinus surgery. Int Forum Allergy Rhinol. (2017) 7:570–5. doi: 10.1002/alr.21911
17. Lobo, D, Anuarbe, P, López-Higuera, JM, Viera, J, Castillo, N, and Megía, R. Estimation of surgeons’ ergonomic dynamics with a structured light system during endoscopic surgery. Int Forum Allergy Rhinol. (2019) 9:857–64. doi: 10.1002/alr.22353
18. Dalager, T, Jensen, PT, Eriksen, JR, Jakobsen, HL, Mogensen, O, and Søgaard, K. Surgeons' posture and muscle strain during laparoscopic and robotic surgery. Br J Surg. (2020) 107:756–66. doi: 10.1002/bjs.11394
19. Armijo, PR, Flores, L, Pokala, B, Huang, CK, Siu, KC, and Oleynikov, D. Gender equity in ergonomics: does muscle effort in laparoscopic surgery differ between men and women? Surg Endosc. (2022) 36:396–401. doi: 10.1007/s00464-021-08295-3
20. Kratzke, IM, Zhou, G, Mosaly, P, Farrell, TM, Crowner, J, and Yu, D. Evaluating the ergonomics of surgical residents during laparoscopic simulation: a novel computerized approach. Am Surg. (2022) 89:1622–8. doi: 10.1177/00031348211047505
21. Rodrigues Armijo, P, Huang, CK, Carlson, T, Oleynikov, D, and Siu, KC. Ergonomics analysis for subjective and objective fatigue between laparoscopic and robotic surgical skills practice among surgeons. Surg Innov. (2020) 27:81–7. doi: 10.1177/1553350619887861
22. Zihni, AM, Cavallo, JA, Ray, S, Ohu, I, Cho, S, and Awad, MM. Ergonomic analysis of primary and assistant surgical roles. J Surg Res. (2016) 203:301–5. doi: 10.1016/j.jss.2016.03.058
23. Thurston, T, Dolan, JP, Husein, F, Stroud, A, Funk, K, Borzy, C, et al. Assessment of muscle activity and fatigue during laparoscopic surgery. Surg Endosc. (2022) 36:1–7. doi: 10.1007/s00464-021-08937-6
24. Lowndes, BR, Abdelrahman, AM, Thiels, CA, Mohamed, AO, McConico, AL, Bingener, J, et al. Surgical team workload comparison for 4-port and single-port laparoscopic cholecystectomy procedures. Appl Ergon. (2019) 78:277–85. doi: 10.1016/j.apergo.2018.06.005
25. Dalager, T, Jensen, PT, Winther, TS, Savarimuthu, TR, Markauskas, A, Mogensen, O, et al. Surgeons’ muscle load during robotic-assisted laparoscopy performed with a regular office chair and the preferred of two ergonomic chairs: a pilot study. Appl Ergon. (2019) 78:286–92. doi: 10.1016/j.apergo.2018.03.016
26. Lohre, R, Regan, W, and Goel, DP. Surgeon ergonomics during arthroscopic shoulder surgery. J Orthop Exp Innov. (2020) 1:13307. doi: 10.60118/001c.13307
27. Shiang, A, Wang, JS, Kushner, B, Panahi, AK, and Awad, MM. Smaller hands and less experience are associated with greater ergonomic strain during endoscopic procedures. Surg Endosc. (2022) 36:5104–9. doi: 10.1007/s00464-021-08876-2
28. Armijo, PR, Huang, CK, High, R, Leon, M, Siu, KC, and Oleynikov, D. Ergonomics of minimally invasive surgery: an analysis of muscle effort and fatigue in the operating room between laparoscopic and robotic surgery. Surg Endosc. (2019) 33:2323–31. doi: 10.1007/s00464-018-6515-3
29. Dalsgaard, T, Jensen, MD, Hartwell, D, Mosgaard, BJ, Jørgensen, A, and Jensen, BR. Robotic surgery is less physically demanding than laparoscopic surgery: paired cross sectional study. Ann Surg. (2020) 271:106–13. doi: 10.1097/SLA.0000000000002845
30. Zárate Rodriguez, JG, Zihni, AM, Ohu, I, Cavallo, JA, Ray, S, Cho, S, et al. Ergonomic analysis of laparoscopic and robotic surgical task performance at various experience levels. Surg Endosc. (2019) 33:1938–43. doi: 10.1007/s00464-018-6478-4
31. Szeto, GPY, Poon, JTC, and Law, WL. A comparison of surgeon’s postural muscle activity during robotic-assisted and laparoscopic rectal surgery. J Robot Surg. (2013) 7:305–8. doi: 10.1007/s11701-012-0374-z
32. Zihni, AM, Ohu, I, Cavallo, JA, Cho, S, and Awad, MM. Ergonomic analysis of robot-assisted and traditional laparoscopic procedures. Surg Endosc. (2014) 28:3379–84. doi: 10.1007/s00464-014-3604-9
33. Monfared, S, Athanasiadis, DI, Umana, L, Hernandez, E, Asadi, H, Colgate, CL, et al. A comparison of laparoscopic and robotic ergonomic risk. Surg Endosc. (2022) 36:1–6. doi: 10.1007/s00464-022-09105-0
34. Hubert, N, Gilles, M, Desbrosses, K, Meyer, JP, Felblinger, J, and Hubert, J. Ergonomic assessment of the surgeon's physical workload during standard and robotic assisted laparoscopic procedures. Int J Med Robot. (2013) 9:142–7. doi: 10.1002/rcs.1489
35. Shergill, AK, Rempel, D, Barr, A, Lee, D, Pereira, A, Hsieh, CM, et al. Biomechanical risk factors associated with distal upper extremity musculoskeletal disorders in endoscopists performing colonoscopy. Gastrointest Endosc. (2021) 93:704–711.e3. doi: 10.1016/j.gie.2020.11.001
36. Lee, D L, Rempel, D, Barr, A B, and Shergill, A Ergonomics of colonoscopy: wrist postures of gastroenterologists performing routine colonoscopy. Proceedings of the Human Factors and Ergonomics Society Annual Meeting. Los Angeles, CA: SAGE Publications, (2010), 54: 1205–1209.
37. Abdelrahman, AM, Bingener, J, Yu, D, Lowndes, BR, Mohamed, A, McConico, AL, et al. Impact of single-incision laparoscopic cholecystectomy (SILC) versus conventional laparoscopic cholecystectomy (CLC) procedures on surgeon stress and workload: a randomized controlled trial. Surg Endosc. (2016) 30:1205–11. doi: 10.1007/s00464-015-4332-5
38. Hallbeck, MS, Lowndes, BR, McCrory, B, Morrow, MM, Kaufman, KR, and LaGrange, CA. Kinematic and ergonomic assessment of laparoendoscopic single-site surgical instruments during simulator training tasks. Appl Ergon. (2017) 62:118–30. doi: 10.1016/j.apergo.2017.02.003
39. Riggle, JD, Miller, EE, McCrory, B, Meitl, A, Lim, E, Hallbeck, MS, et al. Ergonomic comparison of laparoscopic hand instruments in a single site surgery simulator with novices. Minim Invasive Ther Allied Technol. (2015) 24:68–76. doi: 10.3109/13645706.2014.946426
40. Lee, GI, Lee, MR, Clanton, T, Sutton, E, Park, AE, and Marohn, MR. Comparative assessment of physical and cognitive ergonomics associated with robotic and traditional laparoscopic surgeries. Surg Endosc. (2014) 28:456–65. doi: 10.1007/s00464-013-3213-z
41. Yang, L, Wang, T, Weidner, TK, Madura, JA II, Morrow, MM, and Hallbeck, MS. Intraoperative musculoskeletal discomfort and risk for surgeons during open and laparoscopic surgery. Surg Endosc. (2021) 35:6335–43. doi: 10.1007/s00464-020-08085-3
42. Dai, X, Fan, S, Hao, H, Yang, K, Shen, C, Xiong, G, et al. Comparison of KD-SR-01 robotic partial nephrectomy and 3D-laparoscopic partial nephrectomy from an operative and ergonomic perspective: a prospective randomized controlled study in porcine models. Int J Med Robot. (2021) 17:e2187. doi: 10.1002/rcs.2187
43. Wang, R, Liang, Z, Zihni, AM, Ray, S, and Awad, MM. Which causes more ergonomic stress: laparoscopic or open surgery? Surg Endosc. (2017) 31:3286–90. doi: 10.1007/s00464-016-5360-5
44. Pazouki, A, Sadati, L, Zarei, F, Golchini, E, Fruzesh, R, and Bakhtiary, J. Ergonomic challenges encountered by laparoscopic surgeons, surgical first assistants, and operating room nurses involved in minimally invasive surgeries by using RULA method. J Minim Invasive Surg Sci. (2017) 6:344–6. doi: 10.5812/minsurgery.60053
45. Hignett, S, Moss, E L, Gyi, D, Calkins, L, and Jones, LL. Save our surgeons: an ergonomics evaluation of laparoscopic hysterectomy. Loughborough University. Conference contribution (2017). Available at: https://hdl.handle.net/2134/23674
46. Athanasiadis, DI, Monfared, S, Asadi, H, Colgate, CL, Yu, D, and Stefanidis, D. An analysis of the ergonomic risk of surgical trainees and experienced surgeons during laparoscopic procedures. Surgery. (2021) 169:496–501. doi: 10.1016/j.surg.2020.10.027
47. Bartnicka, J, Zietkiewicz, AA, and Kowalski, GJ. An ergonomics study on wrist posture when using laparoscopic tools in four techniques in minimally invasive surgery. Int J Occup Saf Ergon. (2018) 24:438–49. doi: 10.1080/10803548.2018.1452666
48. McCrory, B, Lowndes, BR, Wirth, LM, de Laveaga, AE, LaGrange, CA, and Hallbeck, MS. Ergonomic evaluation of laparoendoscopic single-site surgery ports in a validated laparoscopic training model. Work. (2012) 41:1884–90. doi: 10.3233/WOR-2012-0402-1884
49. Nieboer, TE, Massa, M, Weinans, MJN, Vierhout, ME, Kluivers, KB, and Stegeman, DF. Does training of the nondominant upper extremity reduce the surgeon’s muscular strain during laparoscopy? Results from a randomized controlled trial. Surg Innov. (2013) 20:292–8. doi: 10.1177/1553350612456099
50. Yu, D, Lowndes, B, Morrow, M, Kaufman, K, Bingener, J, and Hallbeck, S. Impact of novel shift handle laparoscopic tool on wrist ergonomics and task performance. Surg Endosc. (2016) 30:3480–90. doi: 10.1007/s00464-015-4634-7
51. Moss, EL, Sarhanis, P, Ind, T, Smith, M, Davies, Q, and Zecca, M. Impact of obesity on surgeon ergonomics in robotic and straight-stick laparoscopic surgery. J Minim Invasive Gynecol. (2020) 27:1063–9. doi: 10.1016/j.jmig.2019.07.009
52. Sánchez-Margallo, FM, Pérez-Duarte, FJ, Sánchez-Margallo, JA, Lucas-Hernández, M, Matos-Azevedo, AM, and Díaz-Güemes, I. Application of a motion capture data glove for hand and wrist ergonomic analysis during laparoscopy. Minim Invasive Ther Allied Technol. (2014) 23:350–6. doi: 10.3109/13645706.2014.925928
53. Pérez-Duarte, FJ, Sánchez-Margallo, FM, Martín-Portugués, IDG, Sánchez-Hurtado, MA, Lucas-Hernández, M, Sánchez-Margallo, JA, et al. Ergonomic analysis of muscle activity in the forearm and back muscles during laparoscopic surgery: influence of previous experience and performed task. Surg Laparosc Endosc Percutan Tech. (2013) 23:203–7. doi: 10.1097/SLE.0b013e3182827f30
54. Yang, L, Money, SR, Morrow, MM, Lowndes, BR, Weidner, TK, Fortune, E, et al. Impact of procedure type, case duration, and adjunctive equipment on surgeon intraoperative musculoskeletal discomfort. J Am Coll Surg. (2020) 230:554–60. doi: 10.1016/j.jamcollsurg.2019.12.035
55. Khan, R, Scaffidi, MA, Satchwell, J, Gimpaya, N, Lee, W, Genis, S, et al. Impact of a simulation-based ergonomics training curriculum on work-related musculoskeletal injury risk in colonoscopy. Gastrointest Endosc. (2020) 92:1070–1080.e3. doi: 10.1016/j.gie.2020.03.3754
56. Baird, BJ, Tynan, MA, Tracy, LF, Heaton, JT, and Burns, JA. Surgeon positioning during awake laryngeal surgery: an ergonomic analysis. Laryngoscope. (2021) 131:2752–8. doi: 10.1002/lary.29717
57. Asadi, H, Monfared, S, Athanasiadis, DI, Stefanidis, D, and Yu, D. Continuous, integrated sensors for predicting fatigue during non-repetitive work: demonstration of technique in the operating room. Ergonomics. (2021) 64:1160–73. doi: 10.1080/00140139.2021.1909753
58. Yurteri-Kaplan, LA, Zhu, X, Iglesia, CB, Gutman, RE, Sokol, AI, Paquet, V, et al. Differences in postural loading between primary and assistant surgeons during vaginal surgery. Int J Ind Ergon. (2018) 65:60–7. doi: 10.1016/j.ergon.2018.01.003
59. Ordóñez-Ríos, M, Jara-Díaz, O, Salamea, J C, and Robles-Bykbaev, V. Ergonomic assessment and analysis of postural load of surgeons performing laparoscopic surgeries in Cuenca, Ecuador. International conference on applied human factors and ergonomics. Springer, Cham, (2017): 427–437.
60. Steinhilber, B, Reiff, F, Seibt, R, Rieger, MA, Martus, P, Kraemer, B, et al. Ergonomic benefits from a laparoscopic instrument with rotatable handle piece depend on the area of the operating field and working height. Hum Factors. (2017) 59:1048–65. doi: 10.1177/0018720817712597
61. Yoon, SH, Jung, MC, and Park, SY. Evaluation of surgeon’s muscle fatigue during thoracoscopic pulmonary lobectomy using interoperative surface electromyography. J Thorac Dis. (2016) 8:1162–9. doi: 10.21037/jtd.2016.04.16
62. Hardy, NP, Mannion, J, Johnson, R, Greene, G, and Hehir, DJ. In vivo assessment of cervical movement in surgeons—results from open and laparoscopic procedures. Ir J Med Sci. (2021) 190:269–73. doi: 10.1007/s11845-020-02255-x
63. Shergill, AK, Asundi, KR, Barr, A, Shah, JN, Ryan, JC, McQuaid, KR, et al. Pinch force and forearm-muscle load during routine colonoscopy: a pilot study. Gastrointest Endosc. (2009) 69:142–6. doi: 10.1016/j.gie.2008.09.030
64. Pace-Bedetti, HM, Dolz, JF, Martínez-de-Juan, JL, and Conejero, A. The effect of postural freedom to increase the neutral positions during laparoscopic surgery. Int J Interact Des Manuf. (2019) 13:627–31. doi: 10.1007/s12008-018-00527-6
65. Butler, KA, Kapetanakis, VE, Smith, BE, Sanjak, M, Verheijde, JL, Chang, YHH, et al. Surgeon fatigue and postural stability: is robotic better than laparoscopic surgery? J Laparoendosc Adv Surg Tech. (2013) 23:343–6. doi: 10.1089/lap.2012.0531
66. Lim, AK, Ryu, J, Yoon, HM, Yang, HC, and Kim, SK. Ergonomic effects of medical augmented reality glasses in video-assisted surgery. Surg Endosc. (2022) 36:988–98. doi: 10.1007/s00464-021-08363-8
67. Zhang, JY, Liu, SL, Feng, QM, Gao, JQ, and Zhang, Q. Correlative evaluation of mental and physical workload of laparoscopic surgeons based on surface electromyography and eye-tracking signals. Sci Rep. (2017) 7:1–7. doi: 10.1038/s41598-017-11584-4
68. Hart, SG, and Staveland, LE. Development of NASA-TLX (task load index): results of empirical and theoretical research In: PA Hancock and N Meshkati, editors. Human mental workload. Amsterdam: North Holland Press (1988)
69. Craven, R, Franasiak, J, Mosaly, P, and Gehrig, PA. Ergonomic deficits in robotic gynecologic oncology surgery: a need for intervention. J Minim Invasive Gynecol. (2013) 20:648–55. doi: 10.1016/j.jmig.2013.04.008
70. van Veelen, MA, Kazemier, G, Koopman, J, Goossens, RHM, and Meijer, DW. Assessment of the ergonomically optimal operating surface height for laparoscopic surgery. J Laparoendosc Adv Surg Tech. (2002) 12:47–52. doi: 10.1089/109264202753486920
71. Rodman, C, Kelly, N, Niermeyer, W, Banks, L, Onwuka, A, Mason, E, et al. Quantitative assessment of surgical ergonomics in otolaryngology. Otolaryngol Head Neck Surg. (2020) 163:1186–93. doi: 10.1177/0194599820932851
72. McAtamney, L, and Corlett, EN. RULA: a survey method for the investigation of work-related upper limb disorders. Appl Ergon. (1993) 24:91–9. doi: 10.1016/0003-6870(93)90080-S
73. Hignett, S, and McAtamney, L. Rapid entire body assessment (REBA). Appl Ergon. (2000) 31:201–5. doi: 10.1016/S0003-6870(99)00039-3
74. Kee, D, and Karwowski, W. LUBA: an assessment technique for postural loading on the upper body based on joint motion discomfort and maximum holding time. Appl Ergon. (2001) 32:357–66. doi: 10.1016/S0003-6870(01)00006-0
75. Beatty, J . Task-evoked pupillary responses, processing load, and the structure of processing resources. Psychol Bull. (1982) 91:276–92. doi: 10.1037/0033-2909.91.2.276
76. Bjerrum, F, Thomsen, ASS, Nayahangan, LJ, and Konge, L. Surgical simulation: current practices and future perspectives for technical skills training. Med Teach. (2018) 40:668–75. doi: 10.1080/0142159X.2018.1472754
77. Park, AE, Zahiri, HR, Hallbeck, MS, Augenstein, V, Sutton, E, Yu, D, et al. Intraoperative “micro breaks” with targeted stretching enhance surgeon physical function and mental focus. Ann Surg. (2017) 265:340–6. doi: 10.1097/SLA.0000000000001665
78. Epstein, S, Sparer, EH, Tran, BN, Ruan, QZ, Dennerlein, JT, Singhal, D, et al. Prevalence of work-related musculoskeletal disorders among surgeons and interventionalists: a systematic review and meta-analysis. JAMA Surg. (2018) 153:e174947–7. doi: 10.1001/jamasurg.2017.4947
79. Albanesi, B, Piredda, M, Bravi, M, Bressi, F, Gualandi, R, Marchetti, A, et al. Interventions to prevent and reduce work-related musculoskeletal injuries and pain among healthcare professionals. A comprehensive systematic review of the literature. J Saf Res. (2022) 82:124–43. doi: 10.1016/j.jsr.2022.05.004
80. Zihni, AM, Ohu, I, Cavallo, JA, Ousley, J, Cho, S, and Awad, MM. FLS tasks can be used as an ergonomic discriminator between laparoscopic and robotic surgery. Surg Endosc. (2014) 28:2459–65. doi: 10.1007/s00464-014-3497-7
81. Wade, L, Needham, L, McGuigan, P, and Bilzon, J. Applications and limitations of current markerless motion capture methods for clinical gait biomechanics. PeerJ. (2022) 10:e12995. doi: 10.7717/peerj.12995
82. Muro-De-La-Herran, A, Garcia-Zapirain, B, and Mendez-Zorrilla, A. Gait analysis methods: an overview of wearable and non-wearable systems, highlighting clinical applications. Sensors. (2014) 14:3362–94. doi: 10.3390/s140203362
83. al-Ayyad, M, Owida, HA, de Fazio, R, al-Naami, B, and Visconti, P. Electromyography monitoring Systems in Rehabilitation: a review of clinical applications, wearable devices and signal acquisition methodologies. Electronics. (2023) 12:1520. doi: 10.3390/electronics12071520
84. van Amelsvoort, LGPM, Schouten, EG, Maan, AC, Swenne, CA, and Kok, FJ. Occupational determinants of heart rate variability. Int Arch Occup Environ Health. (2000) 73:255–62. doi: 10.1007/s004200050425
85. Tiwari, R, Kumar, R, Malik, S, Raj, T, and Kumar, P. Analysis of heart rate variability and implication of different factors on heart rate variability. Curr Cardiol Rev. (2021) 17:74–83. doi: 10.2174/1573403X16999201231203854
86. Owlia, M, Kamachi, M, and Dutta, T. Reducing lumbar spine flexion using real-time biofeedback during patient handling tasks. Work. (2020) 66:41–51. doi: 10.3233/WOR-203149
Keywords: occupational health, endoscopic surgery, ergonomics, surgeon, review
Citation: Liu S, Li Y-y, Li D, Wang F-Y, Fan L-J and Zhou L-x (2024) Advances in objective assessment of ergonomics in endoscopic surgery: a review. Front. Public Health. 11:1281194. doi: 10.3389/fpubh.2023.1281194
Edited by:
Sara Rojas, University of Granada, SpainReviewed by:
Juan A. Sánchez-Margallo, Jesus Uson Minimally Invasive Surgery Centre, SpainSetia Hermawati, University of Nottingham, United Kingdom
Gyula Szabó, Óbuda University, Hungary
Copyright © 2024 Liu, Li, Li, Wang, Fan and Zhou. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Shuang Liu, bGl1c2h1YW5naW5tY2hAZ21haWwuY29t; Ling-Jie Fan, TGluZ2ppZUZhbkBmb3htYWlsLmNvbQ==
 Shuang Liu1*
Shuang Liu1* Ling-Jie Fan
Ling-Jie Fan Liang-xue Zhou
Liang-xue Zhou