- 1Johns Hopkins School of Nursing, Baltimore, MD, United States
- 2Fort Belknap Reservation Community, Agency, MT, United States
- 3Montana Family Planning, Bozeman, MT, United States
- 4Fort Belknap Tribal Health Department, Harlem, MT, United States
- 5Auckland University of Technology, Auckland, New Zealand
Introduction: Suicide and suicide clusters within Native American Reservation communities are devastating to the entire community and increase individuals’ risk for suicide over the lifespan. The objective of this paper is to describe the Indigenous community-based participatory research protocol implemented in partnership with the Fort Belknap Indian Community in Montana, United States. The study protocol was developed to understand suicide risk and protective factors, and community-derived solutions, in a reservation community with history of a suicide cluster and high rates of youth suicide.
Methods: In this mixed-methods study, qualitative data from youth, adults, and service providers and quantitative data from 200 adolescents and young adults (aged 14–24 years) were collected in Fort Belknap, Montana from May – December of 2022. Qualitative data were collected first via in-depth interviews and focus groups. Survey questions included validated and pre-tested measures of factors youth experience across socio-ecological levels. Thematic analysis was applied to the qualitative data; and logistic regression models were used to examine relationships within the quantitative data.
Discussion: This study will add a multi-dimensional perspective to our current understanding of (1) risk and protective factors for suicide, community-derived postvention solutions, and insights on community assets, and (2) the current health and psychosocial status of youth in the Fort Belknap community. This study may serve as an exemplar of co-created, culturally safe solutions designed to address mental health resource gaps. Next steps include development of a suicide crisis response tool kit and a culturally aligned postvention intervention that will enhance individual, family, and community survivance.
1 Introduction
Native Americans (inclusive of American Indians and Alaska Natives in the United States; more broadly referred to as Indigenous Peoples, globally) have been exposed, collectively and historically, to an array of traumatic experiences stemming from settler colonialist systems. Actions involved attempts to systematically erase Indigenous peoples and culture through forced displacement from traditional and sacred land bases, depopulation through starvation, military action, forced boarding school experiences and family separation (1–6). The impact of these historical exposures is long-lasting and intergenerational (7, 8). Decades of research has shown that Native American communities experience profound distress and health inequities, including higher rates of mortality and suicide (9–11). Suicide has been a leading cause of death for Native American youth aged 15–24 years for over 40 years (12–14), and this population has the highest rate of death by suicide of any ethno-racial group in the United States (US) (15). Particular communities bear the burden of suicide, including suicide point clusters. In general, little is known about why suicide clusters form—and at times persist. Research regarding suicide clusters among Native Americans shows increased risk among rural reservations and Alaska villages (16, 17). Native American youth aged 10–24 years accounted for approximately 35% of all deaths by suicide in the Native American community (14). A suicide cluster is defined as a group of suicides, suicide attempts, or self-harm events that occur closer together in time and space than would normally be expected in a community. While rare, suicide clusters tend to occur in remote and tight-knit communities (such as reservations), where mental health resources are scarce and unemployment and economic hardships are common (18). The increased number of deaths and fear of additional losses associated with suicide clusters can have a profound impact on Native American families and communities. It can also exacerbate collective and intergenerational trauma (19). Literature has documented the stark disparities in suicide-related deaths among reservation-based Native American youth compared to their non-Native American counterparts (10). However, there remains a limited understanding of differences that exist across Native American communities and tribes, particularly in the context of existing community-based suicide response systems, assets, and infrastructures (18, 19). Among the subgroup of Native Americans (2.2 million) who receive their healthcare through the Indian Health Service (IHS)—described as “having the worst health outcomes” of any ethnic group in the US—there are vast differences in suicides (20). Among the 12 IHS Areas, suicide rates are highest among those in the Alaska Area, at 38.9 per 100,000 people, a rate 3.6 times the US national rate of 10.9 and 7 times higher than the California Area, which possesses a rate of 5.5 per 100,000. Suicide is highest among remote IHS Areas, underscoring the impact social determinants of health have on suicide, and that suicide is not race related (21).
Native American reservations, established by treaty during the Reservation Era (1851–1887) following the enactment of the Indian Appropriations Act, are areas of concentrated poverty, high distress, and increased morbidity and mortality (10, 22, 23). The risk of suicide among reservation-based Native American youth is nearly six times higher compared to those living in other areas (13). Reservations, such as Fort Belknap, experience concentrated poverty and segregation, which limits access to resources and contributes to increased morbidity and mortality (24–26). Furthermore, the persistent underfunding of IHS, coupled with the failure to allocate resources based upon need, has created limited access to resources and networks required to meet residents’ full potential, including challenges accessing health care and mental health resources (27). The gap in access to mental health care and culturally appropriate services has further exacerbated the suicide crisis across reservation-based Native American communities (10, 27–29).
As of 2020, the state of Montana had the third highest suicide mortality rate in the US, with a crude rate of 26.1 deaths per 100,000 – ranking among the top five states with the highest suicide mortality rates for over 30 years (30). Between 2011 and 2020, the nine Tribes located in Montana had the highest rate of suicide, with a crude rate of 32.0 deaths per 100,000, despite comprising only 6% of the total state population (30, 31). The Fort Belknap Reservation is extremely remote and has an average population density of <4 persons per square mile, compared to the national average of 94 persons per square mile (32). Fort Belknap also ranks among the poorest areas in Montana and in the US with approximately 50% of children under the age of 18 years living in poverty (33). In terms of educational attainment, <25% of Fort Belknap residents hold college degrees (33).
Despite these alarming disparities, Fort Belknap demonstrates considerable community support and mastery during crises, potentially resulting from strong family and community ties, connection to culture, language, and land. These distinct social and cultural assets can promote psychological resilience and collective well-being and foster psychosocial resources that can protect Native American communities against suicide and suicide clusters (25, 34, 35). For example, studies have shown interconnectedness among Native American families, systems, and communities can enhance available networks and sources of social support, thereby buffering the risk of suicide – even in the presence of potent community risk factors (36–38). Native American communities across North America are also leading culture and language revitalization efforts to reclaim traditional knowledge and practices that were formally eradicated through centuries of cultural genocide – promoting connection to tribal and cultural identity, and spiritual and traditional practices (39, 40). Increasingly, Native American communities are nurturing these cultural strengths to develop community-driven responses and interventions to address and prevent suicide (39, 41, 42).
1.1 Objective
This paper outlines the protocol for an ongoing study to understand suicide risk and protective factors, and community-derived solutions in a reservation community. With three main components, the study aims are to: (Aim 1) Explore environmental, cultural, spiritual, and relational factors (e.g., opportunities for belonging, connectedness) in the Fort Belknap community to understand how they contribute to, or protect against, youth suicide via qualitative focus groups and interviews; (Aim 2) Identify risk and protective factors for youth suicide at the individual, familial, communal, and societal levels among Aaniiih and Nakoda youth aged 14–24 years using survey methodology; and (Aim 3) Identify resources for mitigating suicides and natural helpers for the development of accessible, relevant, and effective suicide postventions on the Fort Belknap reservation through cultural and community asset mapping.
2 Methods and analysis
2.1 Conceptual model
The conceptual model (Figure 1) that guides this work was adapted from the Social-Ecological Model: A Framework for Prevention (43), in collaboration with the study’s Tribal Advisory Board (TAB) and informed by lessons learned from over 10 years of work with the neighboring Fort Peck Assiniboine and Sioux Reservation (11). Rooted in socio-ecological principles, the model encompasses two key concepts: (a) There are multiple levels of individual, relationship, community, and societal factors that contribute to suicide and thus, it is necessary to intervene at multiple levels; and (b) reciprocal causation—individual behaviors shape and are shaped by the social environment. The model guided questions asked in Aim 1 and the selection of measures for Aim 2.

Figure 1. An adapted conceptual model of multilevel factors associated with risk of and protection for reservation-based youth suicide.
2.2 Study design
We used a sequential exploratory mixed-methods design, which was implemented for the purpose of triangulation and corroboration of research findings. In alignment with this design, the qualitative focus groups and individual interviews were conducted for Aim 1. Preliminary analysis of the qualitative data informed development, refinement, and selection of the subsequent quantitative survey components. A 251-item questionnaire, including demographics and 17 measures was utilized to collect data from an estimated 200 Aaniiih and Nakoda youth aged 14–24 years. Analysis of the qualitative and quantitative data was conducted sequentially and independently to explore consistency and/or divergence across findings. Following completion of both qualitative and quantitative research, two points of integration will have occurred: (1) a priori (aligned with survey guide) flexible coding and index analysis informed design and selection of the quantitative measures; and (2) during phase two of qualitative inductive thematic analysis (primary indexing and secondary thematic) confirmed findings of the quantitative results while offering thematic insights on experiences of the community.
2.3 Setting
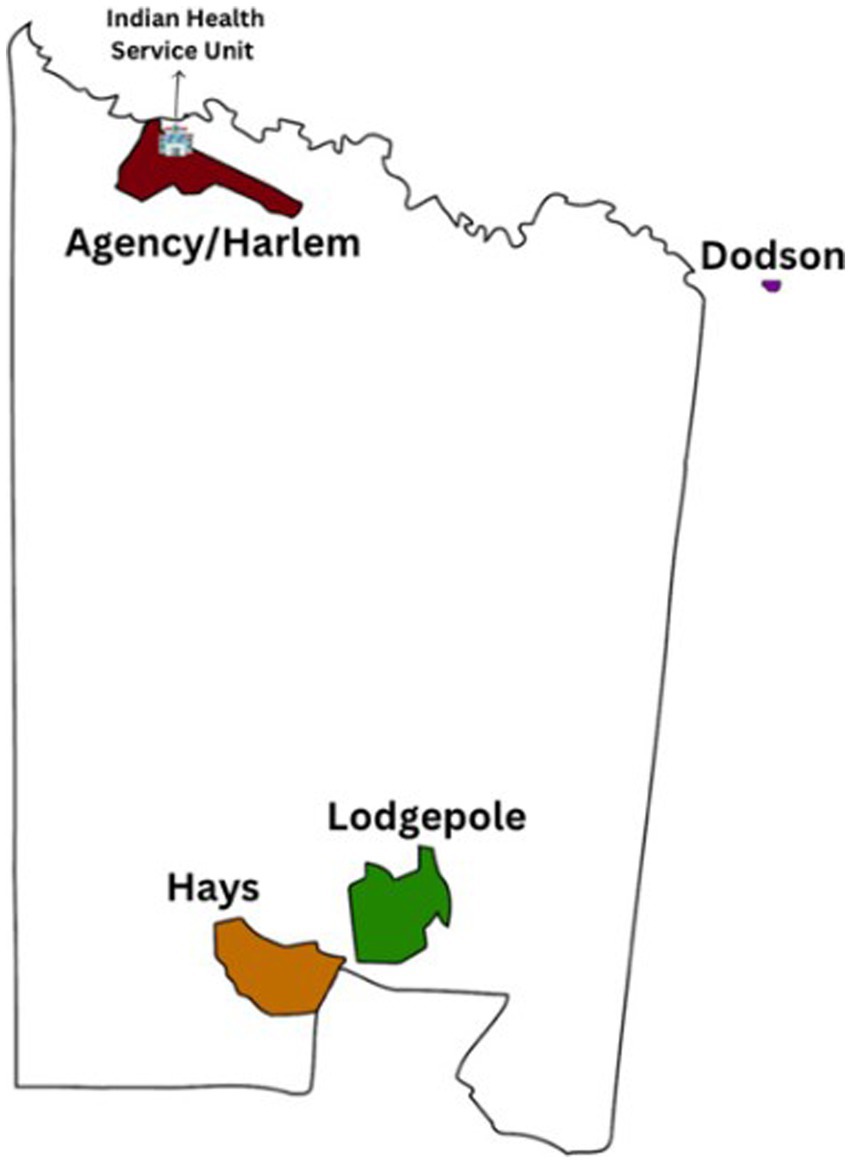
The Fort Belknap Indian Reservation was established by treaty in 1885 and is governed by the elected Fort Belknap Community Council. The Fort Belknap Reservation is part of the Billings IHS Area, which services 11 Tribal Nations that encompass one reservation in Wyoming and seven reservations in Montana. Fort Belknap is in northcentral Montana and spans 675,147 acres (about half the area of Delaware) and is home to approximately 7,000 enrolled Aaniiih and Nakoda members (44, 45). There are four distinct communities in Fort Belknap (Hays, Lodgepole, Agency/Harlem, and Dodson), each with varying strengths, resources, and community characteristics (Figure 2). The IHS Service Unit provides health services to the Fort Belknap community by treaty and is in Fort Belknap Agency, Montana (44).
In 2019, Tribal leaders declared a state of emergency following three youth deaths by suicide in 1 month (26). The increasing urgency to address youth suicide as a public health crisis led to the development of a research-practice partnership between the Fort Belknap Tribes, Aaniiih Nakoda College (ANC), and the Johns Hopkins University (JHU) School of Nursing in 2020.
2.4 Community-based participatory research approach
Our study leverages Indigenous and community-based participatory research methodologies to center partnerships and capacity building, which is critical to promoting evidence-based advocacy and health equity for Indigenous communities (23, 46–48). The Fort Belknap-JHU partnership encompasses partners from the Tribal Health Department and Public Health Nursing Department, who are a powerfully engaged team of public health nurse leaders and advocates who address the public health needs of the community while prioritizing a culturally aligned health care delivery model. Another essential partner is ANC, one of 35 tribal colleges in the U.S., whereby education is grounded in Indigenous ways and knowledge (49).
A critical step in establishing trusting partnerships with tribal communities includes the formation of a Tribal Advisory Board (TAB) (50). Our TAB served as the voice of the community, providing input in study design and recruitment (identification of key stakeholders and community leaders), qualitative interview guide development, selection of quantitative measures, data interpretation, and dissemination. This level of engagement directly infuses the voices of community members into the research process and strengthens the relevance and impact of study findings. Team members also participated in traditional ceremonies with community members, which served to establish and strengthen relationships, appropriately acknowledged the importance of data collection, and supported our collective healing given the sensitive nature of the study topic. Additionally, we engaged local leaders who work with youth in the community, hereafter referred to as “community champions,” to plan, promote, and support research efforts. The in-depth processes utilized to develop and leverage our relationships with the Fort Belknap community will be reported in a future publication.
2.5 Recruitment
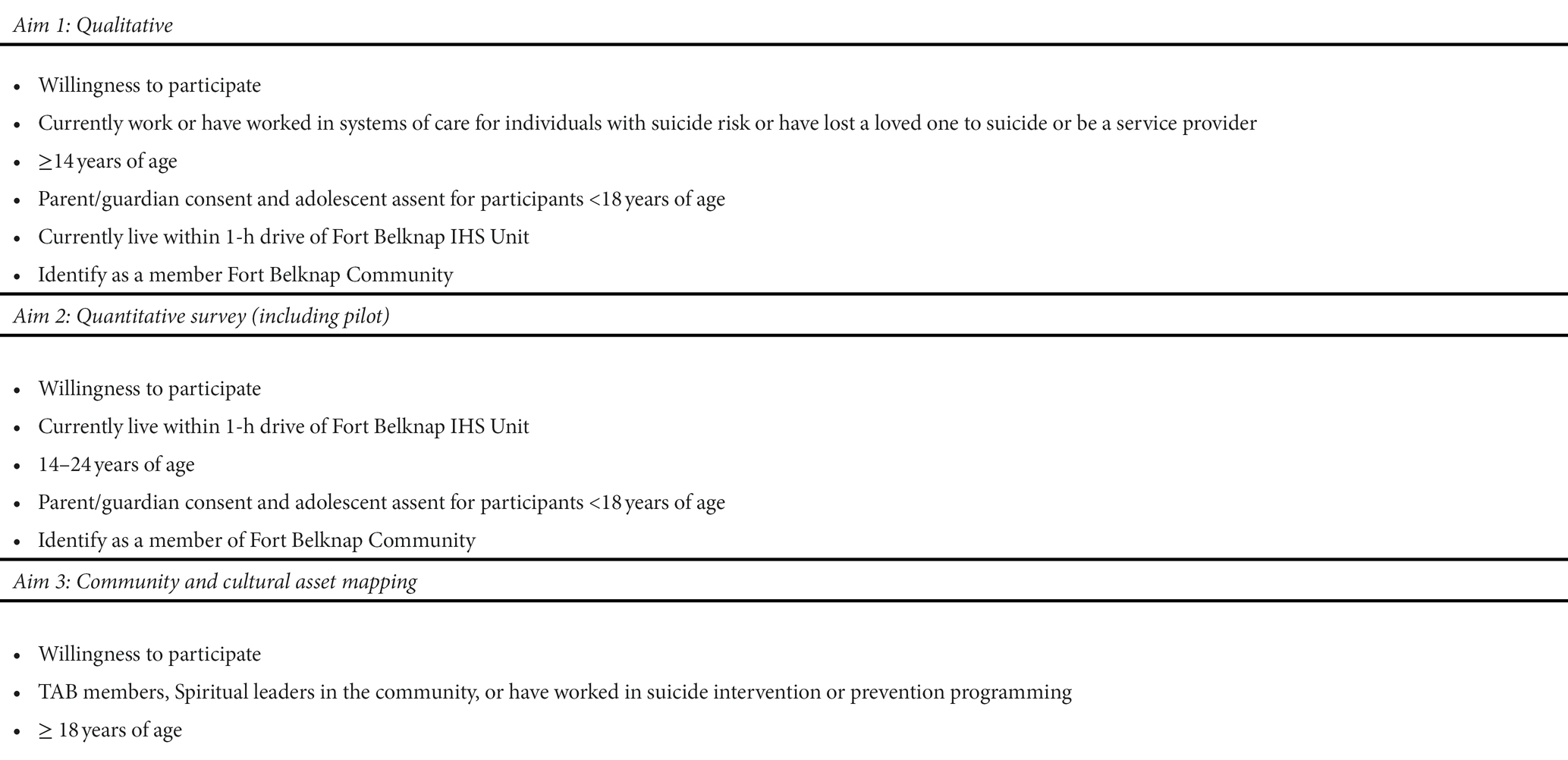
Recruitment for our focus groups, in-depth interviews, and survey were initiated by the local community research coordinator in collaboration with community champions. We recruited participants in all four communities through word-of-mouth, flyers, and radio public service announcements. For asset mapping (Aim 3), we will recruit participants who have been involved in suicide intervention and prevention programming and research through established networks. The Fort Belknap community and TAB were also engaged in providing recommendations for participant recruitment. Utilizing snowball sampling, we asked participants to identify additional contacts for potential participation. Community champions facilitated community engagement activities such as sharing recruitment materials at local events, booking meeting facilities, and gathering food, supplies and equipment, highlighting the importance of involving community. Table 1 depicts inclusion and exclusion criteria for the study. Living within a 1-h drive of the Fort Belknap IHS Unit was a component of our safety protocol to ensure participants had adequate access to care and/or could be referred for follow-up as needed following study participation.
2.6 Participant incentives and debriefing
At the end of each data collection segment all participants received an honorarium for their time and knowledge contributions. Participant incentives were as follows: Aim 1 and survey pilot participants received a $40 Visa gift card; Aim 2 participants received $30 cash. Additionally, all participants received a local mental health resource card and smudge was offered after all study activities for culturally appropriate debrief spiritual centering, cleansing, and calming (48, 51) Every Aim 2 participant was engaged in cultural debrief and mental health screening, with referrals provided if indicated, upon survey completion.
2.7 Aim 1
2.7.1 Sample size
Sample size centered on maximizing inclusion of diverse perspectives from across the four Fort Belknap communities (52, 53). Sample sizes were estimated using the following parameters: community size, suicide risk level, and TAB feedback. We drew on guidance from content and methodological experts to determine number of focus groups and their make-up (i.e., 5–10 participants per group, with separate groups for youth, adults, and service providers) (54).
2.7.2 Data collection
We conducted theoretically grounded, semi-structured focus groups and individual interviews with a diverse sample of community stakeholders and members impacted by suicide (N = 79). We offered individual interviews in the event participants felt uncomfortable in a focus group setting, given the sensitive nature of the topic. Data collection occurred in-person on the Fort Belknap Reservation—in adherence with local COVID-19 safety protocols (e.g., room capacity limits, temperature checks, masks, etc.). Participants completed a brief anonymous demographic questionnaire before their session. Interviews and focus groups were audio recorded, professionally transcribed, de-identified, and reviewed by the research team for accuracy. We used an in-depth interview guide, which was developed based on feedback and input from our TAB, subject matter experts, and community members.
2.7.3 Analysis
In phase one of the qualitative analysis, index analysis was conducted by performing flexible coding in f4Analyse® (version 2.5.2), a qualitative analysis software. The index analysis was framed by the survey guides and allowed the team of reviewers to become familiar with the data. The team coded and indexed data into a priori index code categories (risk factors, protective factors, grief experience, and postvention solutions) (53, 55). The COREQ criteria were used for structuring our analysis (56). The indexed data will be further analyzed to generate meaningful themes in phase two of qualitative analysis. The resulting themes—and the relationships among them—will be harnessed for designing a postvention response and reported in a separate manuscript.
2.8 Aim 2
2.8.1 Sample size
We used data from the neighboring Fort Peck Reservation to estimate the prevalence of suicide (7). Based on this data, we estimated that 45% of participants would screen positive for lifetime suicidal ideation and 35% would report a lifetime suicide attempt. Our goal was to detect odds ratios of approximately 1.50 or greater for each one unit increase in the predictor variable. With statistical power = 0.80 and alpha = 0.05, we can detect significant OR > 1.49 for suicide ideation and OR > 1.52 for attempts with a sample size of 200. As such, recruitment targets were 75 participants from both Hays and Agency/Harlem, and 25 each from the Lodge Pole and Dodson communities, respectively, to reach this total.
2.8.2 Data collection
Survey pilot: Prior to implementation, the survey was piloted with 11 participants to ensure participant acceptability, usability, and cultural relevance. Participants provided informed consent and for those <18 years, parental consent and participant assent were achieved. Each individual completed the survey via tablet in REDCap, a HIPPA-compliant data management software, or via paper-based copy. Participants then completed an individual interview about their experience completing the survey. Interviews were audio recorded, and trained interviewers also took detailed notes.
Survey implementation: For survey administration, the study team collaborated with community champions across the four communities to schedule data collection sites and dates, which took place in schools and community centers. Cell phone usage was not allowed in the computer labs being used for survey conduction and participants were seated at every other computer for safety and privacy purposes. These protocols were implemented as part of our Standard Operating Procedures to promote overall fidelity for data collection and reduce the potential for social desirability bias. Paper copies of the survey were available if needed to troubleshoot any technology issues, though the need for this ultimately did not arise.
2.8.3 Measures
Quantitative data were collected using pre-tested and psychometrically validated questionnaires that have previously been used with Native American populations and/or validated in cross-cultural settings (Table 2). As noted above, measures were revised based on Aim 1 preliminary findings, survey pilot findings, and feedback from TAB members and experts in youth suicide research. At a later point, three measures (polysubstance use, traumatic grief, and racial discrimination) were added at the request of the TAB and content experts so were not pilot tested with Fort Belknap youth. Aligning with our conceptual model, the 17 measures are grouped into four domains: individual, relationship/family, community, and society and are described in depth below.
2.8.3.1 Primary outcome
The primary outcome of interest for this study was lifetime suicidal ideation and attempts. Suicide risk was measured with five dichotomous Yes/No items from the Columbia Suicide Severity Rating Scale (CSSR-S), which has been used widely to identify suicide risk among diverse populations (61). Items included were those that assessed suicide risk based on severity of ideation, intensity of ideation, behavior, and lethality.
2.8.3.2 Individual level variables
Tribal identity was assessed with an adapted version of the Orthogonal Cultural Identification Scale (57). This 6-item scale uses a 4-point response scale (None to A Lot) and was modified based on pilot feedback to measure cultural identification with Aaniiih and Nakoda tribal identity. The original version of this scale was utilized with Indigenous youth (α = 0.90) (58). Depression symptoms were assessed with the 10-item Center for Epidemiologic Studies Depression Scale-Revised (CESD-R-10), which uses a 4-point response scale (Rarely or None of the time to All of the time) (59). The CESD-R-10 is an abbreviated version of the CESD which has been validated among Native American populations (75, 76). Positive childhood experiences (between birth to age 18), including perceived feelings of safety, support, and predictability, were measured using 10-items, with dichotomous (yes or no) response options from the Benevolent Childhood Experiences Scale (60). Emotional intelligence was measured by the 33-item Schutte Self-Report Emotional Intelligence Test (SSEIT) with a 5-point response scale (Strongly disagree to Strongly agree) that includes four subscales: emotion perception, utilizing emotions, managing self-relevant emotions, and managing others’ emotions (62). Trauma symptoms were measured by the 4-item Short Form – Post-traumatic Stress Disorder (PTSD) Checklist for Diagnostic and Statistical Manual of Mental Disorders DSM-5 (PCL-5) with a 5-point response scale (Not at all to Extremely) (63). Cyberbullying experiences, and frequency of experiences, were measured by 27 items on a 5-point response scale (Not at all to Very often) from the Cyberbullying Victimization Scale (64). Adverse childhood experiences occurring in the first 18 years of life and related to the community, family, and the individual were measured by 22 items from the Philadelphia Adverse Childhood Experience (ACE) Questionnaire (65). This scale uses a combination of dichotomous (Yes/No) and Likert scale items capturing adverse childhood experiences. High-risk substance use, first use, lifetime, and current use of substances and binge drinking were assessed with selected questions from the CDC Youth Risk Behavior Surveillance (YRBS) Survey (66). Additionally, polysubstance use, or the concurrent use of substances over the past 12 months was assessed using an adapted version of Midanik et al. (67) polysubstance use scale. Perceived discrimination was measured with the 11-item Racial Discrimination Scale with a 3-point response scale (Never, A few times, Always), which was originally developed to assess discrimination experienced by Native Americans (7, 68).
2.8.3.3 Relationship/family level variables
Family relationships were assessed using 25 items with a 3-point response scale (Not at all, Somewhat, A lot) from the Brief Family Relationship Scale (BFRS): The BFRS was adapted from the 27-item Relationship dimension of the Family Environment Scale (77) and was utilized to assess family relationship domains of Cohesion, Expressiveness, and Conflict subscales (9 items each). Subscales were developed with Native American youth (69). Traumatic grief was assessed using the 19 items from the Traumatic Grief Inventory Self Report (TGI-SR): the first part of the questionnaire asks about the death of the loved one and the second part asks about symptoms related to loss of a loved one, using a 5-point Likert scale (“Never” to “Always”) (70). The first part was removed after pilot testing. Lifetime exposure to domestic violence was assessed using one item: “In your whole life, have you ever seen your mother get hit, slapped, punched, or beaten up?” and lifetime victimization to domestic violence using one item: “In your whole life, have you been hit, slapped, kicked or otherwise physically hurt?,” using dichotomous (Yes or No) responses (7, 71).
2.8.3.4 Community level variables
Communal mastery was assessed with the 10-item Communal Mastery Scale with a 4-point response scale (Strongly Disagree to Strongly Agree) (34). The scale was developed from two commonly employed measures of mastery and self-efficacy and adapted for more collectivist communities including Native American populations (34, 72) and Alaskan Native youth (73).
2.8.3.5 Societal level variables
Historical trauma was measured using three Yes/No questions developed from our previous work (78): (1) “That you know of, did any of your great-great-grandparents or elders attend mandatory boarding school?” (2) “Was their attendance and experience in boarding school talked about in your home?” and (3) “In your opinion, was their experience in mandatory boarding school negative, positive, or neutral?” (74). Historical loss was measured by the 12-item Historical Loss Scale with a 6-point response scale (Several times a day to Never) (79). This scale was used to quantify the types of losses that Native Americans might have experienced in the past and how often they are thought about in the present (79). This scale uses a 6-point Likert scale (“Several times a day” to “Never”) to measure losses and has been used in our previous study (α = 0.93) (74).
2.8.4 Analysis
All variables were summarized descriptively (means, standard deviations, interquartile range, and percentages) and distributions examined to determine if they met the assumptions of the underlying analytical models. The pattern of missing data was examined to determine if it was missing at random. Multiple imputations were used to handle missing data at the scale level. Model building was conducted by examining the bivariate relationship between each of the predictor variables and suicide attempt/ideation using logistic regression. Variables significant at the 0.05 level were moved into a multivariable logistic regression model and the area under the curve (AUC), sensitivity, and specificity was estimated to determine model fit. Next, a multinomial model was estimated with three levels of the outcome (no ideation/attempt, ideation without an attempt, suicide attempt). Suicide ideation without an attempt was the reference category utilized to explore the factors that may distinguish between suicide ideation and attempt. We began using a bivariate model and moved significant variables forward to the multivariable model. Results were also graphically displayed using forest plots. Findings from this analysis will be reported in a separate manuscript.
2.9 Aim 3
2.9.1 Sample size
We will recruit 10–12 individuals from the Fort Belknap community with expertise in suicide prevention and intervention via our existing networks to participate in roundtable discussions.
2.9.2 Data collection
We will utilize a roundtable discussion format to conduct asset mapping with community experts to identify natural helpers and resources to inform development of postvention interventions and a suicide cluster response plan. Community Asset Mapping consists of six steps: (1) defining community boundaries; (2) identifying and involving partners; (3) determining what type of assets/resources are available; (4) generating lists of organizations, associations, and institutions in the community; (5) generating lists of individuals in the community; and (6) organizing a visual map or diagram about where these resources, organizations and individuals are and how they communicate with each other (80). Together with our TAB, community leaders, and stakeholders, we will develop a Fort Belknap Community Crisis Management Plan for Preventing and Responding to Suicide Clusters. This plan will present reigning national recommendations, promising practices, and guidelines for community response. Collaborative consultation with reservation stakeholders in the design of such a plan will ensure maximum community and cultural validity for the locally developed postvention plans.
2.9.3 Analysis
The data-derived themes from Aim 1 will be particularly vital to this analysis, highlighting participant perspectives, cultural insights, and culturally aligned approaches—therein identifying community assets. Integration and comparison of qualitative (Aim 1) and quantitative (Aim 2) results will allow for triangulation to confirm areas of consistency or convergence. The resulting themes will be summarized in written form and circulated to the TAB and other community stakeholders for comments and recommendations for further improvement. Once finalized, the blueprint of the resulting community-driven postvention response will be passed along to tribal leaders for consideration of implementation and further planning.
3 Quality control and safety procedures
The study team performed internal quality management of study conduct and data collection, storage, documentation, and completion. All research staff were trained in and followed the Standard Operating Procedures to ensure study fidelity and participant safety. Quality control procedures were implemented as outlined below.
3.1 Informed consent
Study staff completed a review of completed consent form documents to ensure signature, date, time, and any optional participation notes (such as future contact) were correctly completed. The Program Coordinator reviewed each form and provided feedback to the study team to ensure proper consenting procedures were followed.
3.2 Recruitment report
The Program Coordinator produced a report each week to share at study progress meetings. This included: number of active participants, eligible individuals who required follow-up, conflicts of interest, number of participants who enrolled/declined/consented/undecided, and the number of focus groups/interviews/surveys completed overall.
3.3 Team training
The Program Coordinator facilitated training for all data collection team members on the Standard Operating Procedures and strategies for collecting data with safety and validity at the forefront. Expert trainers provided team trainings on the following topics: Qualitative Data Collection: Recruitment, Asking, Listening and Ethical Considerations; Keeper of Stories: The Responsibility of Storytellers in an Indigenous Research Context; Psychiatric Diagnostic Criteria and Cultural Safety; Working with Youth; QPR (Question, Persuade, Refer) Suicide Prevention; Safety Planning and Mandated Reporting, REDCap Basics; and Minimizing Bias in Quantitative Data.
3.4 Data management and storage
Audio recordings and transcripts were saved to the JHU OneDrive platform. Survey data were stored in REDCap (81). Hard copy documents were stored both in double locked file cabinets at the JHU School of Nursing office and in a standardized filing system in OneDrive. Survey data were reviewed at regular meetings by the Data Manager to ensure participant responses were correctly captured. All records will be kept in a secure location for a minimum of 7 years and to age 23 for pediatric participants, in accordance with Johns Hopkins Medicine Record Retention policy. Only key study team members (PI, study coordinator, and on-site coordinator) have access to the master list of participant names and IDs.
3.5 Participant safety and referrals
At completion of each survey, participants were flagged if their assessment scores indicated clinical levels of depression (a CESD-R score of 10 or above), moderate active trauma symptoms (a PCL-5 score of 8 or above), and/or suicide risk (any “yes” response to question number 1, 3 and 4 in the Adapted CSSR-S scale). A trained study staff member with a nursing background performed a debrief during which clinical flags were reviewed with each participant. In addition, referrals to local mental health providers were offered and participants were provided a mental health and referral resource card. Cultural debriefing and smudge were also offered before and after data collection to maximize participants’ safety, comfort, and healing.
4 Discussion
This study will provide multi-dimensional perspectives on the risk and protective factors for youth suicide and community-derived postvention solutions grounded in community assets and strengths. It will also enhance our understanding of the current health and psychosocial status of youth in the Fort Belknap community. Findings may be useful for addressing behavioral health needs for reservation communities across Indian Country. The US Government’s lack of resource investment and failure to address the physical and psychosocial health needs of Native Americans living on reservations established by treaty demonstrates little progress has been (and is likely to be) made towards developing context-specific suicide interventions in these communities. The variations in suicidal activity, risk factors, and mental health access across the 12 IHS geographical areas indicate tribal differences that require distinct exploration and tailored co-creation of culturally informed and community-derived interventions. To eliminate geographic disparities in suicide-related deaths and suicide clusters impacting reservation-based Native American communities, it is vital to focus research and resource allocation on Native American communities that experience disproportionately high suicide rates. In addition, the complexity of compounded trauma (individual, familial, community, historical, and intergenerational), the mental health treatment gap, and psychosocial stressors experienced by underfunded reservation communities require a multi-faceted, culturally aligned approach that prioritizes equity of voice and power between the research team and the community.
The contribution of this work will showcase the ongoing need to prioritize finding solutions to address the disproportionate mental health comorbidities (depression, anxiety, substance use disorder, complex trauma, and grief) in Fort Belknap. This work will inform a suicide crisis response tool kit and the development of meaningful culturally aligned, and safe solutions and interventions that will enhance individual, family, and community survivance (82). Overall, our study will serve as an exemplar of co-created, culturally safe solutions designed to address mental health resource gaps, which may be useful for other research-practice partnership teams.
5 Ethics and dissemination
This study was authorized by Fort Belknap Tribal Resolution #182–2020 and received Human Subjects approval from the Johns Hopkins School of Medicine (00305879) and Aaniiih Nakoda College Institutional Review Boards (IRBs). Protocol amendments were submitted as an amendment to both IRBs. All manuscripts and presentations are submitted to ANC IRB for review and approval. We obtained a Certificate of Confidentiality (CoC) through the National Institutes of Health (NIH), which further protects the privacy of study participants. Due to the CoC, investigators and others who have access to research records will not disclose identifying information except when the participant consents or in certain instances when federal, state, or local law or regulation requires disclosure. NIH expects investigators to inform research participants of the protections and limits to protections provided by a Certificate issued through this Policy.
Ethics statement
The studies involving humans were approved by Fort Belknap Tribal Resolution #182-2020 and received human subjects approval from Johns Hopkins School of Medicine (00305879) and Aaniiih Nakoda College Institutional Review Boards. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participant if 18 years of age or older; if under 18, participants provided assent and participants’ legal guardians/next of kin” provided written consent.
Author contributions
TBr: Conceptualization, Funding acquisition, Investigation, Methodology, Resources, Supervision, Writing – original draft, Writing – review & editing. MK-J: Formal analysis, Investigation, Methodology, Writing – original draft, Writing – review & editing. LM: Investigation, Writing – original draft, Writing – review & editing. EB: Investigation, Writing – review & editing. TrB: Investigation, Writing – review & editing. TeB: Writing – review & editing. ED: Project administration, Supervision, Writing – original draft, Writing – review & editing. NG: Conceptualization, Formal analysis, Funding acquisition, Methodology, Writing – review & editing. HH: Validation, Writing – review & editing. KH: Validation, Writing – review & editing. NM: Investigation, Methodology, Writing – review & editing. MK: Investigation, Methodology, Project administration, Writing – original draft, Writing – review & editing. RP-M: Validation, Writing – review & editing. AM: Investigation, Project administration, Validation, Writing – review & editing. KN: Investigation, Writing – original draft, Writing – review & editing. AR: Conceptualization, Investigation, Methodology, Writing – review & editing. TaR: Funding acquisition, Resources, Writing – review & editing. TeR: Investigation, Writing – review & editing. DW: Investigation, Writing – original draft, Writing – review & editing. KY: Funding acquisition, Resources, Writing – review & editing. NP: Formal analysis, Investigation, Methodology, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. The primary funder of this research is the William T. Grant Foundation (WTGF-201485) and Doris Duke Foundation (DDCF-2021175) these funders provided 3 years of funding for the project and personnel related to this study. It was awarded to PI, TBr at Johns Hopkins School of Nursing and Co-PI, KY at Fort Belknap Indian Community/Tribal Health.
Acknowledgments
The authors gratefully acknowledge the Aaniiih and Nakoda Tribes of the Fort Belknap Community, including participants and leaders, for their support of the research.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
ACE(s), adverse childhood experience(s); ANC, Aaniiih Nakoda College; CoC, certificate of confidentiality; COREQ, consolidated criteria for reporting qualitative research; HIPPA, Health Insurance Portability and Accountability Act of 1996; IRB, Institutional Review Board; IHS, Institutional Health Service; JHU, Johns Hopkins School of Nursing; NIH, National Institutes of Health; PI, principal investigator; TAB, Tribal Advisory Board; US, United States
References
1. Grover, LL . The Vermilion Lake Indian School: from assimilation to termination. Minn. Hist. (2002) 58:224–40.
2. Duran, E , Duran, B , Heart, MYHB , and Horse-Davis, S . Healing the American Indian soul wound In: Y Danieli , editor. International Handbook of Multigenerational Legacies of Trauma. Boston, MA: Springer US (1998). 341–54.
3. Adams, DW . Education for Extinction: American Indians and the Boarding-School Experience, 1875–1928. 2nd ed. Lawrence: University Press of Kansas (1995).
4. Heart, MYHB . The historical trauma response among natives and its relationship with substance abuse: a Lakota illustration. J Psychoactive Drugs. (2003) 35:7–13. doi: 10.1080/02791072.2003.10399988
5. Gone, JP . “We never was happy living like a Whiteman”: mental health disparities and the postcolonial predicament in American Indian communities. Am J Community Psychol. (2007) 40:290–300. doi: 10.1007/s10464-007-9136-x
6. Settler Colonialism . (2023). Available at: https://www.law.cornell.edu/wex/settler_colonialism. (Accessed February 03, 2023).
7. Brockie, T . Historical and Contemporary Factors Influencing Non-Lethal Suicidal Behavior among Reservation-Based Native American Youth. Baltimore, MD: The Johns Hopkins University (2012).
8. Gone, JP . A community-based treatment for native American historical trauma: prospects for evidence-based practice. J Consult Clin Psychol. (2009) 77:751–62. doi: 10.1037/a0015390
9. Friedman, J , Hansen, H , and Gone, JP . Deaths of despair and indigenous data genocide. Lancet. (2023) 401:874–6. doi: 10.1016/S0140-6736(22)02404-7
10. Jones, DS . The persistence of American Indian health disparities. Am J Public Health. (2006) 96:2122–34. doi: 10.2105/AJPH.2004.054262
11. Brockie, TN , Dana-Sacco, G , Wallen, GR , Wilcox, HC , and Campbell, JC . The relationship of adverse childhood experiences to PTSD, depression, poly-drug use and suicide attempt in reservation-based native American adolescents and Young adults. Am J Community Psychol. (2015) 55:411–21. doi: 10.1007/s10464-015-9721-3
12. Mental and Behavioral Health – American Indians/Alaska Native (2021). Available at: https://minorityhealth.hhs.gov/omh/browse.aspx?lvl=4&lvlid=39. (Accessed February 06, 2023).
13. Frederick, CJ . Suicide, Homicide, and Alcoholism among American Indians: Guidelines for Help. Bethesda, MD: National Institute of Mental Health (DHEW) (1973).
14. Leavitt, RA , Ertl, A , Sheats, K , Petrosky, E , Ivey-Stephenson, A , and Fowler, KA . Suicides among American Indian/Alaska Natives — National Violent Death Reporting System, 18 States, 2003–2014. Report No.: 67. United States: Center for Surveillance, Epidemiology, and Laboratory Services, Centers for Disease Control and Prevention (CDC), U.S. Department of Health and Human Services (2018).
15. SAMHSA . To Live to see the Great Day that Dawns: Preventing Suicide by American Indian and Alaska Native Youth and Young Adults/U.S. Department of Health and Human Services. Maryland: Center for Mental Health Services, Substance Abuse and Mental Health Services Administration (2010).
16. SAMHSA . Substance Abuse and Mental Health, Services Administration. Preventing and Responding to Suicide Clusters in American Indian and Alaska Native Communities. Rockville, MD: Department of Health and Human Services (2014).
17. Goldston, DB , Molock, SD , Whitbeck, LB , Murakami, JL , Zayas, LH , and Hall, GCN . Cultural considerations in adolescent suicide prevention and psychosocial treatment. Am Psychol. (2008) 63:14–31. doi: 10.1037/0003-066X.63.1.14
18. Lazzarini, TA , Gonçalves, C , Maymone, C , Benites, WM , Silva, LF , Tsuha, DH, et al. Suicide in Brazilian indigenous communities: clustering of cases in children and adolescents by household. Rev Saude Publica. (2018) 52:56. doi: 10.11606/S1518-8787.2018052000541
19. Forum on Mental Health and Substance . Use Disorders, Forum for Children's Well-Being, Board on Health CS, Board on Children Y, and Families, Health and MD, Division of Behavioral and Social Sciences, and Education, et al. Suicide Prevention in Indigenous Communities: Proceedings of a Workshop. Washington, D.C.: National Academies Press (2022).
20. U.S. Commission on Civil Rights . Broken Promises: Continuing Federal Funding Shortfall for Native Americans. Washington, DC: United States Commission on Civil Rights. (2018). Available from: https://www.usccr.gov/pubs/2018/12-20-Broken-Promises.pdf
21. Roubideaux, Y , Frazier, F , and Greenway, K . Regional Differences in Indian Health 2012 Edition [Internet]. Rockville, MD: U.S. Department of Health and Human Services, Indian Health Service. (2016). Available from: https://www.ihs.gov/sites/dps/themes/responsive2017/display_objects/documents/RegionalDifferences2012Edition.pdf
22. Native Voices: Native Peoples' Concepts of Health and Illness . (2023). Available at: https://www.nlm.nih.gov/nativevoices/timeline/index.htmll. (Accessed March 09, 2023).
23. National Academies of Sciences, Engineering, and Medicine, Health and Medicine Division, Board on Population Health and Public Health Practice; Committee on Community-Based Solutions to Promote Health Equity in the United States In: A Baciu, Y Negussie, and A Geller, editors. Communities in Action: Pathways to Health Equity. Washington, DC: National Academies Press (US) (2017)
24. Byerly, J . The residential segregation of the American Indian and Alaska native population in US metropolitan and micropolitan areas, 2010. DemRes. (2019) 40:963–74. doi: 10.4054/DemRes.2019.40.33
25. Brockie, T , Decker, E , Barlow, A , Cwik, M , Ricker, A , Aguilar, T, et al. Planning for implementation and sustainability of a community-based suicide surveillance system in a native American community. Implementat. Sci. Commun. (2023) 4:1. doi: 10.1186/s43058-022-00376-1
26. Sukut, J. Fort Belknap declares emergency over suicide crisis, lack of resource [Internet]. Billings, MT: Billings Gazette. (2019). Available from: https://billingsgazette.com/news/state-and-regional/fort-belknap-declares-emergency-over-suicide-crisis-lack-of-resources/article_4912efa5-6c8a-50c7-b55b-836cd9e050b6.html
27. Warne, D , and Frizzell, LB . American Indian health policy: historical trends and contemporary issues. Am J Public Health. (2014) 104:S263–7. doi: 10.2105/AJPH.2013.301682
28. National Academies of Sciences, Engineering, and Medicine, Division HaM, Practice, Board on Population Health and Public Health, States, Committee on Community-Based Solutions to Promote Health Equity in the United In: A Baciu and Y Negussie, editors. Communities in Action. Washington, D.C.: National Academies Press (2017)
29. Substance Abuse and Mental Health Services Administration . Suicide Clusters within American Indian and Alaska Native Communities: A Review of the Literature and Recommendations. Rockville, MD: Center for Mental Health Services, Substance Abuse and Mental Health Services Administration. (2017).
30. Montana Department of Health and Human Service (DPHHS) . 2016 Suicide Mortality Review Team Report [Internet]. Helena, MT (2016). Available from: https://dphhs.mt.gov/assets/suicideprevention/2016suicidemortalityreviewteamreport.ppf (Accessed December 20, 2023).
31. Rosston, K. Suicide in Montana: Facts, Figures and Formulas for Prevention [Internet]. Helena, MT: Montana Department of Health and Human Services (DPHHS).(2022). Available from: https://dphhs.mt.gov/assets/suicideprevention/SuicideinMontana.pdf (Accessed December 20, 2023).
32. Census Reporter Profile Page for fort Belknap Reservation (2021). Available at: https://censusreporter.org/profiles/25200US1150R-fort-belknap-reservation/. (Accessed March 09, 2023).
34. Hobfoll, SE , Jackson, A , Hobfoll, I , Pierce, CA , and Young, S . The impact of communal-mastery versus self-mastery on emotional outcomes during stressful conditions: a prospective study of native American women. Am J Community Psychol. (2002) 30:853–71. doi: 10.1023/A:1020209220214
35. Allen, J , Mohatt, GV , Fok, CCT , Henry, D , and Burkett, R . A protective factors model for alcohol abuse and suicide prevention among Alaska native youth. Am J Community Psychol. (2014) 54:125–39. doi: 10.1007/s10464-014-9661-3
36. Lyons, RF , Mickelson, KD , Sullivan, MJL , and Coyne, JC . Coping as a communal process. J Soc Pers Relat. (1998) 15:579–605. doi: 10.1177/0265407598155001
37. Joiner, TE . The clustering and contagion of suicide. Curr. Direct. Psychol. Sci. (1999) 8:89–92. doi: 10.1111/1467-8721.00021
38. Roh, S , Burnette, CE , Lee, KH , Lee, Y , Easton, SD , and Lawler, MJ . Risk and protective factors for depressive symptoms among American Indian older adults: adverse childhood experiences and social support. Aging Ment Health. (2015) 19:371–80. doi: 10.1080/13607863.2014.938603
39. Barker, B , Goodman, A , and DeBeck, K . Reclaiming indigenous identities: culture as strength against suicide among indigenous youth in Canada. Can J Public Health. (2017) 108:e208–10. doi: 10.17269/CJPH.108.5754
40. Tatsch, S . Language revitalization in native North America--issues of intellectual property rights and intellectual sovereignty. Coll Antropol. (2004) 28:257–62.
41. Bassett, D , Tsosie, U , and Nannauck, S . “Our culture is medicine”: perspectives of native healers on posttrauma recovery among American Indian and Alaska native patients. Perm J. (2012) 16:19–27. doi: 10.7812/TPP/11-123
42. Gone, JP , and Trimble, JE . American Indian and Alaska native mental health: diverse perspectives on enduring disparities. Annu Rev Clin Psychol. (2012) 8:131–60. doi: 10.1146/annurev-clinpsy-032511-143127
43. McLeroy, KR , Bibeau, D , Steckler, A , and Glanz, K . An ecological perspective on health promotion programs. Health Educ Q. (1988) 15:351–77. doi: 10.1177/109019818801500401
44. Welcome to Fort Belknap Indian Community . (2023). Available at: https://ftbelknap.org/. (Accessed January 20, 2023)
45. Census profile: Fort Belknap Reservation (2021). Available at: https://censusreporter.org/profiles/25200US1150R-fort-belknap-reservation/. (Accessed August 21, 2023).
46. Minkler, M , Garcia, AP , Rubin, V , and Wallerstein, N . Community-Based Participatory Research: A Strategy for Building Healthy Communities and Promoting Health through Policy Change [Internet]. Berkeley, CA: U.C. Berkeley Public Health & Policy Link (2012). (A Report to The California Endowment). Available from: https://www.policylink.org/sites/default/files/CBPR.pdffiles/1399/CBPR.pdf
47. Wallerstein, N , Duran, B , Oetzel, JG , and Minkler, M . Community-Based Participatory Research for Health. 3rd ed. Hoboken, NJ: Jossey-Bass & Pfeiffer Imprints, Wiley (2018).
48. Brockie, TN , Dana-Sacco, G , López, MM , and Wetsit, L . Essentials of research engagement with native American tribes: data collection reflections of a tribal research team. Prog Community Health Partnersh. (2017) 11:301–7. doi: 10.1353/cpr.2017.0035
49. Aaniiih Nakoda College (2023). Available at: https://www.ancollege.edu/. (Accessed August 21, 2023).
50. Brockie, T , Azar, K , Wallen, G , O’Hanlon Solis, M , Adams, K , and Kub, J . A conceptual model for establishing collaborative partnerships between universities and native American communities. Nurse Res. (2019) 27:27–32. doi: 10.7748/nr.2019.e1613
51. Brockie, TN , Hill, K , Davidson, PM , Decker, E , Krienke, LK , Nelson, KE, et al. Strategies for culturally safe research with native American communities: an integrative review. Contemp. Nurse. (2022) 58:8–32. doi: 10.1080/10376178.2021.2015414
52. Hennink, M , and Kaiser, BN . Sample sizes for saturation in qualitative research: a systematic review of empirical tests. Soc Sci Med. (2022) 292:114523. doi: 10.1016/j.socscimed.2021.114523
53. Deterding, NM , and Waters, MC . Flexible coding of in-depth interviews: a twenty-first-century approach. Sociol. Methods Res. (2018) 50:708–39. doi: 10.1177/0049124118799377
54. Carlsen, B , and Glenton, C . What about N? A methodological study of sample-size reporting in focus group studies. BMC Med Res Methodol. (2011) 11:26. doi: 10.1186/1471-2288-11-26
55. Gale, NK , Heath, G , Cameron, E , Rashid, S , and Redwood, S . Using the framework method for the analysis of qualitative data in multi-disciplinary health research. BMC Med Res Methodol. (2013) 13:117. doi: 10.1186/1471-2288-13-117
56. Tong, A , Sainsbury, P , and Craig, J . Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. (2007) 19:349–57. doi: 10.1093/intqhc/mzm042
57. Oetting, ER . Orthogonal cultural identification: theoretical links between cultural identification and substance use. NIDA Res Monogr. (1993) 130:32–56.
58. Oetting, E , and Beauvais, F . Orthogonal cultural identification theory: the cultural identification of minority adolescents. Int J Addict. (1991) 25:655–85. doi: 10.3109/10826089109077265
59. Eaton, WW , Smith, C , Ybarra, M , Muntaner, C , and Tien, A . Center for Epidemiologic Studies Depression Scale: Review and Revision (CESD and CESD-R). In ME Maruish (Ed.), The use of psychological testing for treatment planning and outcomes assessment: Instruments for adults. Hillsday, NJ: Lawrence Erlbaum Associates Publishers. 363–77. (2004).
60. Narayan, AJ , Rivera, LM , Bernstein, RE , Harris, WW , and Lieberman, AF . Positive childhood experiences predict less psychopathology and stress in pregnant women with childhood adversity: a pilot study of the benevolent childhood experiences (BCEs) scale. Child Abuse Negl. (2018) 78:19–30. doi: 10.1016/j.chiabu.2017.09.022
61. Posner, K , Brown, GK , Stanley, B , Brent, DA , Yershova, KV , Oquendo, MA, et al. The Columbia–suicide severity rating scale: initial validity and internal consistency findings from three multisite studies with adolescents and adults. Am J Psychiatry. (2011) 168:1266–77. doi: 10.1176/appi.ajp.2011.10111704
62. Schutte, NS , Malouff, JM , Hall, LE , Haggerty, DJ , Cooper, JT , Golden, CJ, et al. Development and validation of a measure of emotional intelligence. Personality and Individual Differences. (1998) 25:167–77. doi: 10.1016/S0191-8869(98)00001-4
63. Zuromski, KL , Ustun, B , Hwang, I , Keane, TM , Marx, BP , Stein, MB, et al. Developing an optimal short-form of the PTSD checklist for DSM-5 (PCL-5). Depress Anxiety. (2019) 36:790–800. doi: 10.1002/da.22942
64. Lee, J , Abell, N , and Holmes, JL . Validation of measures of cyberbullying perpetration and victimization in emerging adulthood. Res Soc Work Pract. (2017) 27:456–67. doi: 10.1177/1049731515578535
65. Pachter, LM , Lieberman, L , Bloom, SL , and Fein, JA . Developing a community-wide initiative to address childhood adversity and toxic stress: a case study of the Philadelphia ACE task force. Acad Pediatr. (2017) 17:S130–5. doi: 10.1016/j.acap.2017.04.012
66. Centers for Disease Control and Prevention (CDC) . Youth Risk Behavior Surveillance System (YRBSS) Questionnaire Content 1991–2017 [Internet]. Atlanta, GA: Centers for Disease Control and Prevention (CDC). (2016). Available from: https://www.cdc.gov/healthyyouth/data/yrbs/pdf/2017/YRBS_questionnaire_content_1991-2017.pdf
67. Midanik, LT , Tam, TW , and Weisner, C . Concurrent and simultaneous drug and alcohol use: results of the 2000 National Alcohol Survey. Drug Alcohol Depend. (2007) 90:72–80. doi: 10.1016/j.drugalcdep.2007.02.024
68. Whitbeck, LB , Hoyt, DR , McMorris, BJ , Chen, X , and Stubben, JD . Perceived discrimination and early substance abuse among American Indian children. J Health Soc Behav. (2001) 42:405–24. doi: 10.2307/3090187
69. Fok, CCT , Allen, J , Henry, D , and Team, PA . The brief family relationship scale: a brief measure of the relationship dimension in family functioning. Assessment. (2014) 21:67–72. doi: 10.1177/1073191111425856
70. Boelen, PA , and Smid, GE . The traumatic grief inventory self-report version (TGI-SR): introduction and preliminary psychometric evaluation. J Loss Trauma. (2017) 22:196–212. doi: 10.1080/15325024.2017.1284488
71. Brennan, RT , Molnar, BE , and Earls, F . Refining the measurement of exposure to violence (ETV) in urban youth. J Community Psychol. (2007) 35:603–18. doi: 10.1002/jcop.20167
72. Hobfoll, SE , Schröder, KEE , Wells, M , and Malek, M . Communal versus individualistic construction of sense of mastery in facing life challenges. J Soc Clin Psychol. (2002) 21:362–99. doi: 10.1521/jscp.21.4.362.22596
73. Fok, CCT , Allen, J , Henry, D , and Mohatt, GV . Multicultural mastery scale for youth: multidimensional assessment of culturally mediated coping strategies. Psychol Assess. (2012) 24:313–27. doi: 10.1037/a0025505
74. Brockie, T , Wetsit, L , Ricker, A , and Wallen, G . A Tribal Partnership to Address Violence and Suicide: Building Tribal Research Evidence and Increasing Tribal Research Capacity. Washington, DC: Society for Prevention Research 22nd Annual Meeting. (2013).
75. Barlow, A , Mullany, B , Neault, N , Compton, S , Carter, A , Hastings, R, et al. Effect of a paraprofessional home-visiting intervention on American Indian teen mothers’ and infants’ behavioral risks: a randomized controlled trial. Am J Psychiatry. (2013) 170:83–93. doi: 10.1176/appi.ajp.2012.12010121
76. Brockie, T , Haroz, EE , Nelson, KE , Cwik, M , Decker, E , Ricker, A, et al. Wakȟáŋyeža (little holy one) – an intergenerational intervention for native American parents and children: a protocol for a randomized controlled trial with embedded single-case experimental design. BMC Public Health. (2021) 21:2298. doi: 10.1186/s12889-021-12272-9
77. Moos, RH , and Moos, BS . Family Environment Scale Manual. 3rd ed. Palo Alto, CA: Consulting Psychologists Press (1994).
78. Brave Heart, M , and DeBruyn, LM . The American Indian holocaust: healing historical unresolved grief. Am Indian Alsk Native Ment Health Res. (1998) 8:60–82. doi: 10.5820/aian.0802.1998.60
79. Whitbeck, L . Conceptualizing and measuring historical trauma among American Indian people. Am J Community Psychol. (2004) 33:119–30. doi: 10.1023/B:AJCP.0000027000.77357.31
80. Turin, TC , Shahid, M , and Vaska, M . Asset mapping as a tool for identifying resources in community health: a methodological overview. J Biomed Anal. (2019) 2:13–25. doi: 10.30577/jba.2019.v2n1.22
81. Project REDCap . (2023). Available at: https://projectredcap.org/about/. (Accessed August 21, 2023).
Keywords: suicide cluster, Native American, youth, reservation, protective factors, risk factors, mixed-methods
Citation: Brockie T, Kahn-John M, Mata Lopez L, Bell E, Brockie T, Brockie T, Decker E, Glass N, Has Eagle H, Helgeson K, Main NJ, Kazemi M, Perez-Monteau R, Myrick A, Nelson KE, Ricker A, Rider T, Roberts T, Wilson DH, Yazzie K and Perrin N (2024) A mixed-methods study protocol on factors contributing to suicide clusters among Native American youth in a northern plains reservation. Front. Public Health. 11:1281109. doi: 10.3389/fpubh.2023.1281109
Edited by:
Wulf Rössler, Charité University Medicine Berlin, GermanyReviewed by:
Justin Reedy, University of Oklahoma, United StatesMarlyn Bennett, University of Manitoba, Canada
Copyright © 2024 Brockie, Kahn-John, Mata Lopez, Bell, Brockie, Brockie, Decker, Glass, Has Eagle, Helgeson, Main, Kazemi, Perez-Monteau, Myrick, Nelson, Ricker, Rider, Roberts, Wilson, Yazzie and Perrin. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Teresa Brockie, dGJyb2NraTFAamh1LmVkdQ==
 Teresa Brockie
Teresa Brockie Michelle Kahn-John
Michelle Kahn-John Laura Mata Lopez1
Laura Mata Lopez1 Ellie Decker
Ellie Decker Nancy Glass
Nancy Glass Mina Kazemi
Mina Kazemi Teeah Roberts
Teeah Roberts Deborah H. Wilson
Deborah H. Wilson Nancy Perrin
Nancy Perrin