- 1BRAVO VICTOR, Research, London, United Kingdom
- 2UCL, Institute of Ophthalmology, London, United Kingdom
Background: Despite an increased risk of certain eye conditions which can lead to visual impairment (V.I.), there is evidence of a greater delay to treatment-seeking among adults from minority ethnic communities (MEC). MEC adults may also be underrepresented on V.I. registers, within early intervention services, and among the beneficiaries of national V.I. charities. However, much of this evidence is outdated or anecdotal.
Methods: This secondary analysis of V.I. Lives survey data explored use of eye health and support services and mobility aids among a matched control sample of 77 MEC and 77 adults aged 18 and over from white communities (WC). Participants were matched on age, gender, UK region and urban/rural setting. Additional subgroup analysis was conducted for Asian (n = 46) and black participants (n = 22).
Results: There were no significant group differences in areas such as eye health service use, registration status, contact with charities, and level of practical support received. But MEC participants were significantly more likely than WC participants to have received direct payments from social services to cover their care needs, Χ2 (1, 154) = 8.27, p = 0.004, and to use apps on their mobile for mobility, Χ2 (1, 154) = 5.75, p = 0.017. In contrast, WC participants were significantly more likely to agree that they were getting the level of emotional support to get on with their life, U = 3,638, p = 0.010, to feel confident to ask their friends for support, U = 2,416, p = 0.040, and to have a guide dog for mobility, Χ2 (1, 154) = 3.62, p = 0.057, although the latter did not reach statistical significance. Within the MEC group, Asian participants were significantly more likely than black participants to use a long cane, Χ2 (1, 68) = 7.24, p = 0.007, but they were significantly less likely to agree that they had received the right level of support when they started to experience V.I., U = 236.5, p = 0.040.
Conclusion: The preliminary findings suggests that there is scope to increase support provided by V.I. charities and the V.I. register, although, contrary to existing evidence, there were no statistically significant differences in eye health service use, registration status and use of wider support services. Further research is required to confirm these findings and explore reasons for differences.
1 Introduction
The number of people living with visual impairment (V.I.) in the UK is estimated to increase from around 2 million to approximately 4 million by 2050 (1). Data from the 2021 UK Census shows that minority ethnic communities (MEC) make up an increasing proportion of the population in England and Wales (2). People from certain MEC have been found to be at increased risk of V.I. (3, 4) and certain eye conditions which can result in V.I. relative to people from white communities (WC). For instance, people from Afro-Caribbean communities have been found to be at increased risk of primary open-angle glaucoma across all age groups (5, 6), while people from Asian communities may be at increased risk and earlier onset of diabetic retinopathy (7), including sight-threatening diabetic retinopathy (8), and cataract (9). As such, they are projected to make up an increasing proportion of adults living with V.I. in the UK (10).
In the UK, the eyecare pathway usually commences with an initial appointment with a community optometrist or general practitioner (GP), who may refer patients for diagnosis to secondary or tertiary eyecare. Diagnosis by an ophthalmologist may be followed by a treatment or monitoring phase, which requires regular eye appointments usually with an ophthalmologist or specialist community optometrist. Despite the increased risk of V.I. and eye disease, there is evidence of a greater delay to treatment-seeking among MEC adults. Research in the field of diabetic eye disease found that there was a significantly longer delay in attending an appointment at an eye clinic following a referral among Asian people than Black and White people and there was a significantly longer delay from referral (and also first appointment) to receiving treatment for their diabetic eye disease among Black people than Asian and White people (11). This suggests that people from Black communities may be waiting longer for treatment, while people from Asian communities may be waiting longer to receive a diagnosis. Research with adults from Indian communities explored barriers to use of further eyecare services (12). These included dissatisfaction with prior health service experiences, including long waiting times, limited awareness of how to access services, limited acceptance of Western medicine resulting in treatment being sought abroad, lack of time, health not being seen as a priority, and language. In addition, unhelpful perceptions of sight loss and limited awareness and understanding of eye conditions may result in fear and treatment-seeking only once symptoms were no longer manageable. For instance, cataracts were thought to require an undetermined period of maturing or ‘ripening’ until the condition was no longer manageable before treatment was thought necessary. Similarly, due to perceptions of glaucoma as being associated with aging, the perceived risk of experiencing glaucoma was low among younger African-Caribbean adults (13).
V.I. has been associated with a negative impact on activities of daily living (14, 15), participation in sports and leisure activities (16, 17), quality of life, mental health outcomes and social functioning (18–23). A recent rapid evidence review found limited research on the impact of V.I. among different ethnic communities in the UK (24). People who have been diagnosed with a V.I. have several support options. In the UK, individuals with a moderate or severe V.I. can be registered as sight impaired (partially sighted) or severely sight impaired (blind). To join the register, people need to first be certified as sight impaired (partially sighted) or severely sight impaired (blind) by an ophthalmologist (25). Certification is based on best-corrected visual acuity and visual field (26). A copy of the certificate is sent to the patient’s local council which will contact individuals with the offer to join the register (27). Registering a V.I. with local social services has a number of practical benefits including access to a needs assessment and appropriate support to remain independent, as well as financial concessions on transport, television and health services. There is evidence that MEC adults (28), including Asian adults (7) are less likely to be registered than WC adults. This may be due to limited awareness and knowledge of the benefits and registration process resulting from inhibition, particularly among older adults, and/or communication difficulties with clinicians (28). Some eye clinics provide early interventions services such as the Eye Clinic Liaison Officer (ECLO). These can offer advice and support relating to hospital appointments, registering a V.I., benefits, education, employment, housing, low vision aids or training, travel and social networks, and refer or signpost patients and their families to social services, sight loss charities or support groups following a diagnosis of irreversible sight loss (29, 30). However, Slade (29) reports that only 3.6% of service users were from Black and other minority ethnic communities while 96.4% were from White communities, suggesting that MEC may be underrepresented in early intervention services. Finally, sight loss charities can provide vision rehabilitation and mental health support following diagnosis and beyond. But anecdotal evidence suggests that MEC adults may be less aware of support services and the benefits associated with them (31, 32). This may result in unmet needs. For instance, qualitative research with Somali refugees who had V.I. found that language barriers may prevent these individuals from accessing statutory and other support resulting in unmet needs for support with activities of daily living including housework, and social isolation where participants were unable to leave the house without support (33). Anecdotal evidence also suggests that MEC adults may prefer to receive support from V.I. groups specifically for their ethnic community rather than national sight loss charities (31). This may be due to the cultural appropriateness of these services. Johnson and Morjaria-Keval (32) recommend hiring MEC staff, providing information materials in different languages, drawing on community partners to disseminate information, and providing funding and resources to community partners who offer support services within their communities, among other. To overcome negative experiences, they recommend building relationships and providing a continuous service. Overall, this suggests that service use may be lower among MEC, although the evidence is limited and/or anecdotal. There is further anecdotal evidence that guide dogs may not be an acceptable mobility aid among Somali community (34) and Afro-Caribbean communities (35). This raises important questions around the acceptability of available mobility aids among different communities, which is yet to be explored.
The current article forms part of a series of articles which explore the wider experiences of MEC adults living with V.I. in the United Kingdom. This article explores awareness and use of health and support services among a sample of MEC adults, including those from Asian and Black communities.
2 Materials and methods
This article uses secondary data collected in the V I Lives survey (36), a telephone survey of people with V.I. commissioned by the Royal National Institute of the Blind (RNIB), the Thomas Pocklington Trust (TPT) and Guide Dogs for the Blind Association (Guide Dogs).
2.1 Data and sample
Details of the survey and sample have been described elsewhere (36, 37). Briefly, participants were recruited through a healthcare database, local and national charities, social media, and radio adverts. People without V.I. and those who did not speak English were excluded. Wave 1 of fieldwork took place from 17 December 2019 to 23 March 2020. Wave 2 of fieldwork ran from 14 August 2020 to 2 November 2020.
To control for the unequal subgroup sample sizes and statistically significant differences between MEC and WC participants, a matched control sample was drawn using R (38). WC participants were matched to MEC participants based on their age, gender, region and whether participant lived in rural areas vs. towns.
2.2 Materials
A questionnaire was developed for the survey covering a wide range of topics. V.I. severity was assessed using a participant’s self-reported registration status (sight impaired/partially sighted or severely sight impaired/blind). Where participants were not registered, V.I. severity was determined with a set of questions adapted from the Life Opportunities Survey. These assessed the extent to which participant’s had difficulties seeing ordinary newsprint at arm’s length (near vision), the face of someone across the room ca. 4 m/12 ft. away (distance vision), and people or things in the periphery of their vision (peripheral vision). Finally, participants were asked about their legal driving status. Those who reported wearing glasses or contact lenses, were asked to rate near, distance and peripheral vision difficulties with glasses or contact lenses. Individual cases were reviewed and discussed by a panel to ensure they met inclusion criteria and to resolve inconsistent responses.
Ethnicity: participants were asked to indicate how they would describe their ethnic background from a list including white British, white other, mixed/multiple ethnic groups, Asian/Asian British, black/African/Caribbean/black British and other ethnic group.
Use of health services: a single question asked participants if they remembered roughly when they last visited an eye clinic.
Registration status: participants were asked if, as far as they knew, they were registered as severely sight impaired or sight impaired. Further response categories included Registered but do not know which category and Not registered.
Awareness and use of charities: three questions asked participants to select from lists (1) the charities for people with V.I. they had heard of (2) the charities they had contacted or had contact with, and (3) the other charities that they had contacted or had contact with in relation to their V.I.
Support received: One question explored which types of support services participants had ever received in relation to their V.I. The extent to which participants’ support needs had been met was explored in three questions which asked participants to what extent they agreed or disagreed that they got the level of practical support (a) and emotional support (b) they needed to get on with their life, and that they had received the right level of support when they started to experience sight impairment (c). Participants who were born with V.I. were not asked the last question. Participants were also asked to indicate how confident they were in asking for support from personal networks (family, friends, neighbors, network of visually impaired people they knew), authorities (government agencies, local councils), social workers/NHS services, wider support (charities, volunteers who visit people in their home) and religious groups.
Use of mobility aids: participants were asked whether they normally used any kind of mobility aid, such as guide dog or long cane. Interviewers then coded all aids used from a list. Those who did not have a guide dog or dual assistance dog were asked to indicate why this was the case.
2.3 Data analysis
Although the survey was not specifically designed to compare subgroups and despite low subsample sizes, the data analysis explored status within and group differences between MEC (n = 77) and WC participants (n = 77), as well as between the two largest MEC subgroups, participants from Asian (n = 46) and Black communities (n = 22), to gain a preliminary insight into service use among these groups.
For all variables, response distributions were calculated as counts (n) and proportions (%) for each subgroup. Subgroup analysis was performed using Mann–Whitney U tests for ordinal and chi-square tests, or Fisher’s exact test where assumptions of expected cell counts were violated, for categorical variables. Data analysis was conducted using SPSS (39) except for Fishers’ exact tests which were conducted using R.
3 Results
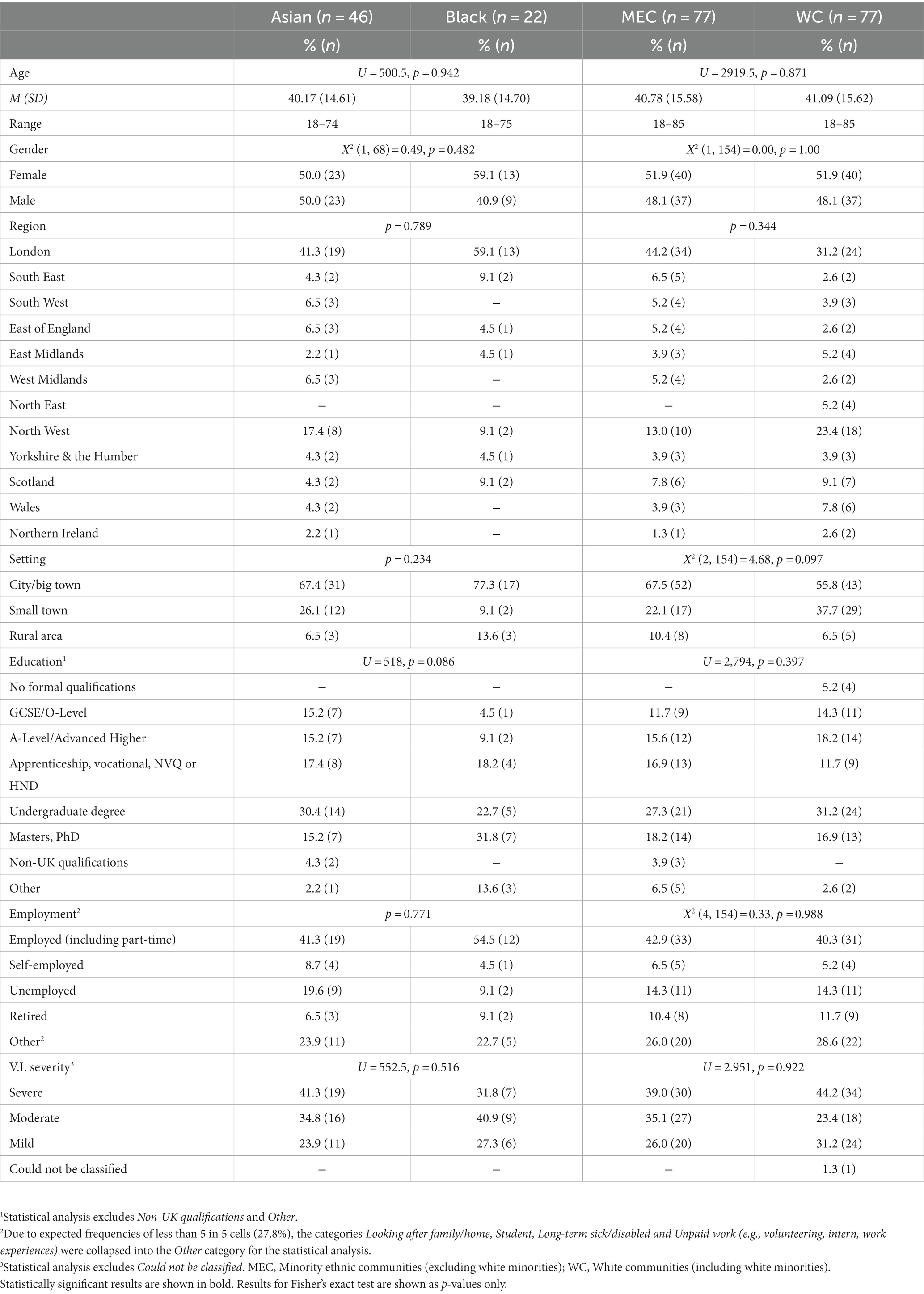
Table 1 provides an overview of participant characteristics by subgroup. Mean age was similar across all groups. A majority across all groups resided in a big town or city, specifically London, and were in employment. Around half of Asian, MEC and WC participants were female, and a majority were educated to degree-level and categorized as having severe V.I. In comparison, the proportion of females was higher among Black participants (59.1%), who were also more likely to be educated to Master’s level and to be categorized as having moderate V.I.
3.1 Eye health services
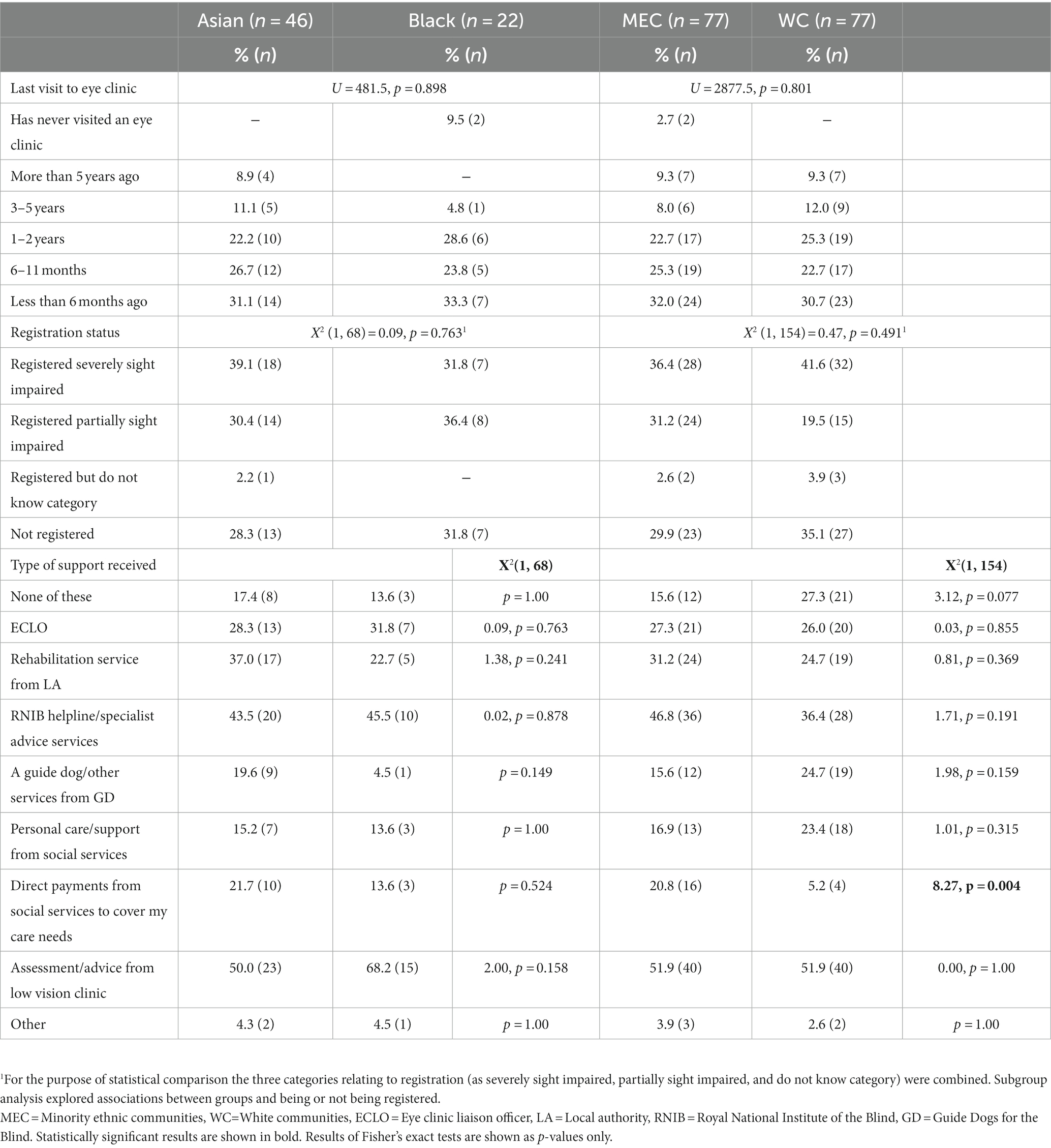
There were no statistically significant differences between MEC and WC participants, U = 2877.5, p = 0.801, nor between Asian and Black participants, U = 481.5, p = 0.898, in the use of eye health services (Table 2). A slightly lower proportion of WC (53.4%) than MEC participants (57.3%) attended an eye clinic in the last year. Similar proportions of Asian (57.8%) and Black participants (57.1%) visited an eye clinic within the last 12 months, with around a third in both groups attending an eye clinic in the last 6 months. Two Black participants reported that they had never visited an eye clinic. These had mild and moderate V.I., keratoconus/corneal dystrophy and nystagmus, and neither had registered their V.I.
3.2 Registration status
There were no statistically significant associations between ethnicity and being registered or not registered, neither when comparing Asian and Black, nor when comparing MEC and WC participants (Table 2). Being unregistered was most common among WC (35.1%) followed by Black (31.8%) and Asian participants (28.3%). In addition, three WC and one Asian participant were registered but did not know in which category. A majority of unregistered Asian, Black and WC participants had mild V.I. (84.6, 85.7 and 84.6% respectively). The primary cause of V.I. among unregistered Asian patients was keratoconus/corneal dystrophy (30.8%), while unregistered Black and WC participants primarily had “other”, unlisted conditions (28.6 and 37.0% respectively).
3.3 Support received
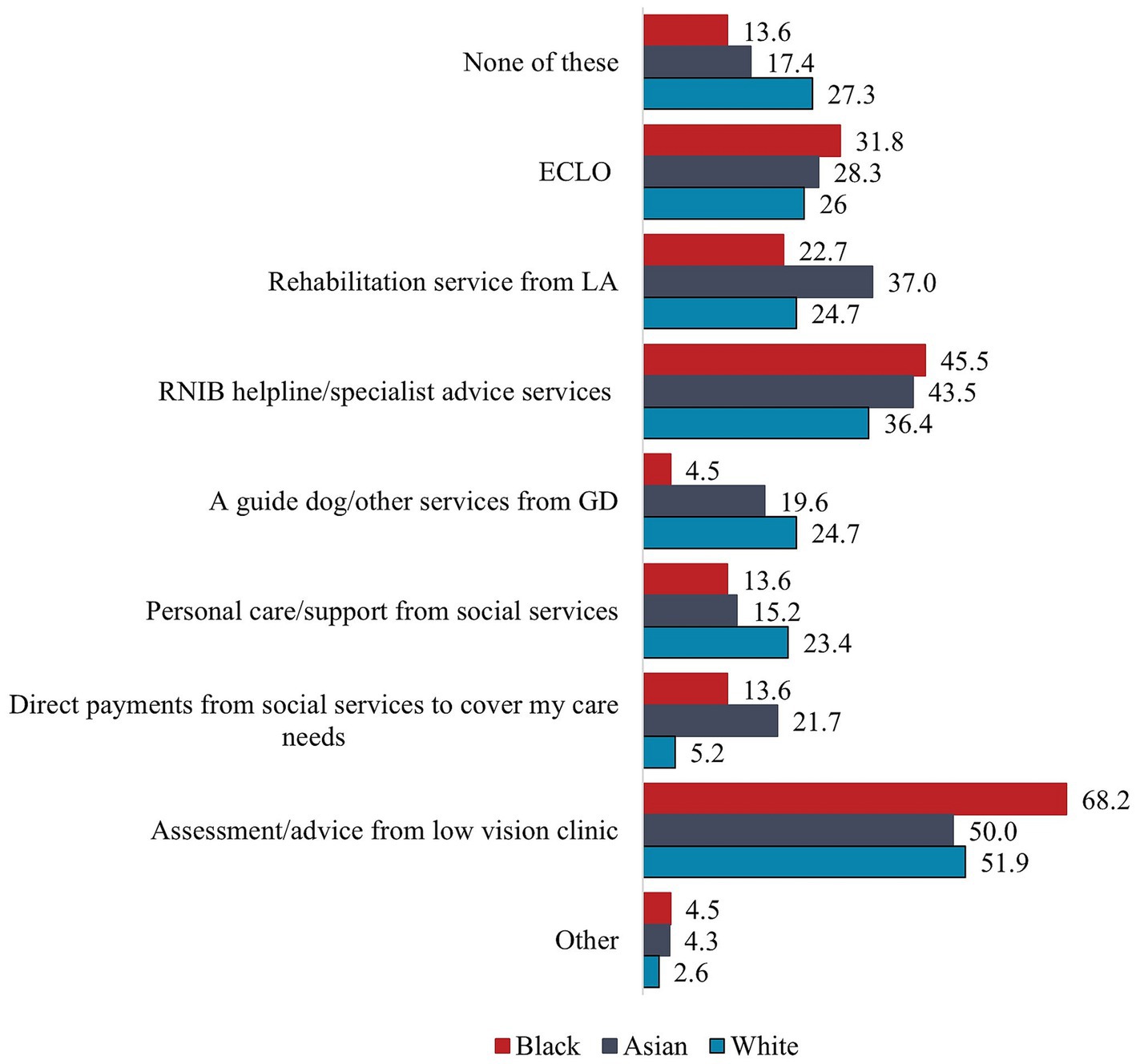
The survey assessed the types of support received, the adequacy of emotional, practical and initial support, as well as confidence in asking different sources for support. In terms of types of support received, MEC participants were four times more likely than WC participants to have received direct payments from social services to cover their care needs, 20.8% vs. 5.2%, Χ2 (1, 154) = 8.27, p = 0.004, Cramer’s V = 0.232. There were no further statistically significant associations between ethnicity and different support services available to people with V.I., neither for Asian and Black participants, nor for MEC and WC participants (Table 2). Although not statistically significant, WC participants (27.3%) were more likely to have received none of the listed support than MEC (15.6%), including Asian (17.4%) and Black participants (13.6%), but they were more likely than the MEC groups to have received a guide dog or other services from Guide Dogs as well as personal care and support from social services. All four WC participants who had been referred by Guide Dogs reported having received a guide dog or other support from Guide Dogs. In contrast, Black participants were more likely than other groups to have received support from a low vision clinic, the RNIB helpline or other specialist advice services and ECLOs, while Asian participants were more likely than other groups to have received rehabilitation services from their local authority and direct payments from social services (Figure 1). Assessment and advice from a low vision clinic followed by support from the RNIB helpline or other specialist advice services were the most common types of support received by participants in all groups. Half of Asian and WC participants and over two thirds of Black participants had received this.
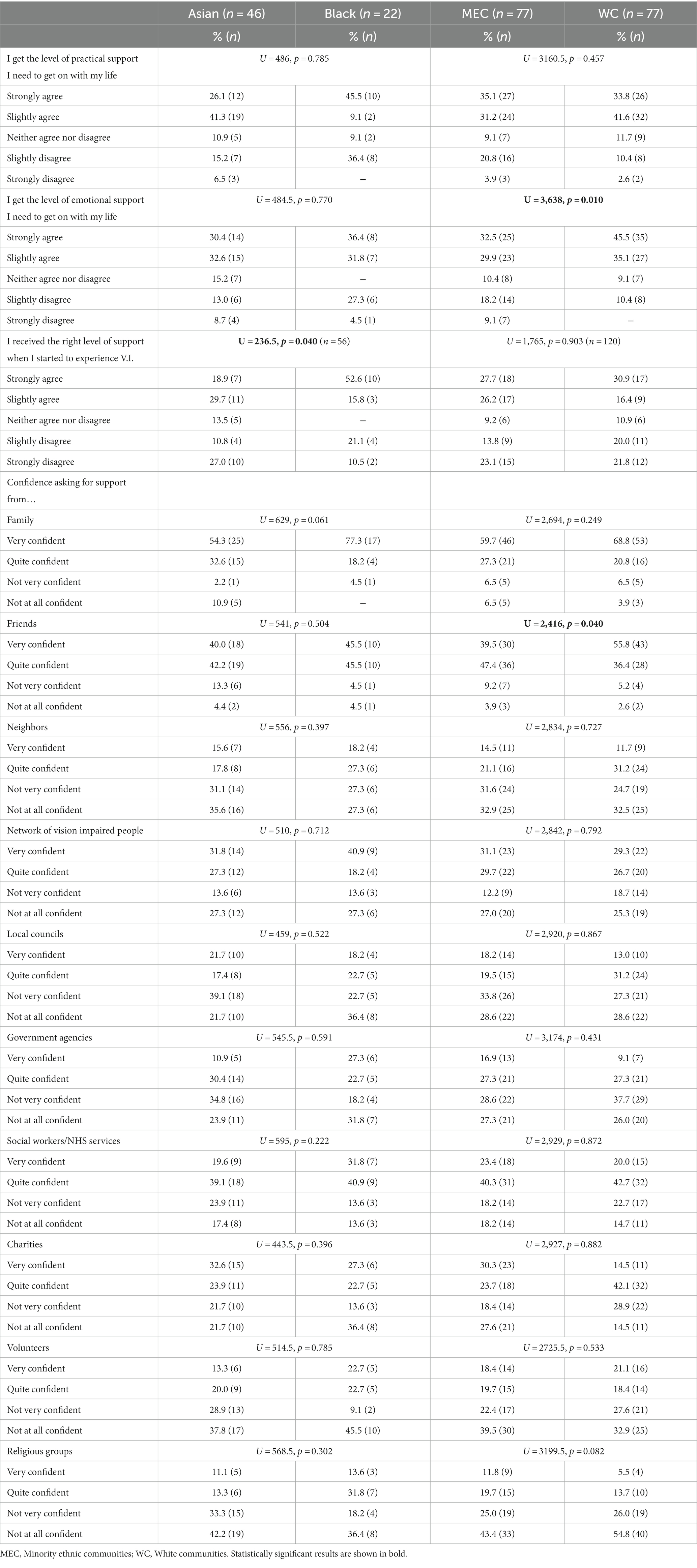
In terms of the extent to which the support received was adequate, MEC participants were significantly less likely to agree that they were getting the level of emotional support to get on with their life, U = 3,638, p = 0.010. Eight in ten WC participants agreed with this compared to just over six in ten MEC participants (Table 3). Although not statistically significant, MEC participants were also less likely to agree that they got the level of practical support they needed to get on with their life but slightly more likely to agree that they got the right level of support when they started to experience V.I. While similar levels of Asian and Black participants agreed that they received sufficient emotional support (63.0% vs. 68.2% respectively), 54.6% of Black participants agreed that they received sufficient practical support compared to 67.4% of Asian participants, but 45.5% of Black participants agreed strongly with this compared to just 26.1% of Asian participants. At the other end of the scale, 21.7% of Asian participants disagreed that they received sufficient practical support compared to 36.4% of Black participants, but none of the Black participants disagreed strongly compared to 6.5% of Asian participants. These differences were not statistically significant. However, Black participants were significantly more likely to agree and agree strongly than Asian participants that they had received the right level of support when they started to experience V.I., U = 236.5, p = 0.040. Overall, around a third of Asian and Black participants did not believe they had received the right support when they lost their sight, nor the practical or emotional support they needed at the time of the survey, although the proportion of Asian participants who did not receive sufficient emotional support was lower (21.7%).
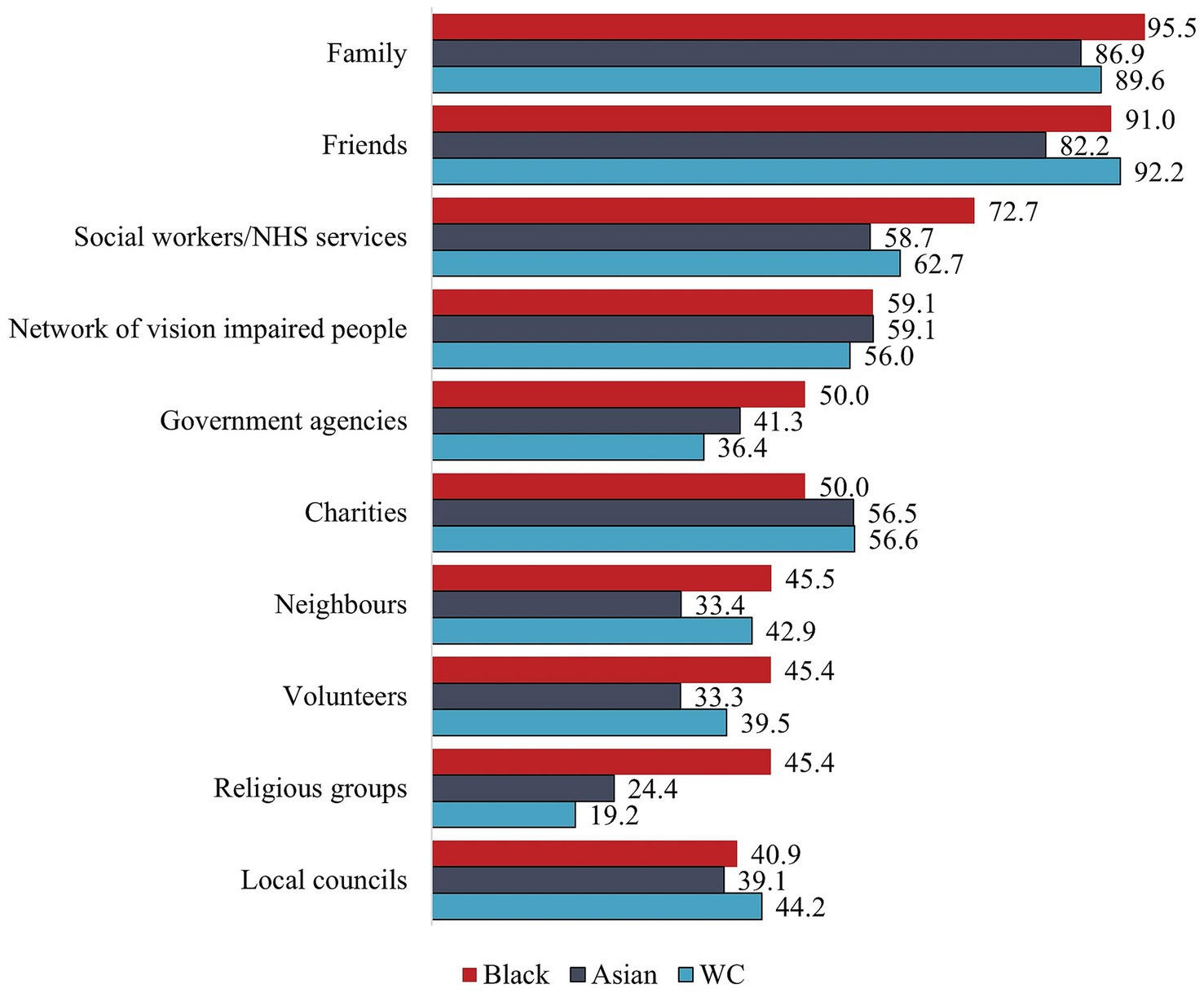
WC participants were significantly more likely to feel confident to ask their friends for support than MEC participants, U = 2,416, p = 0.040 (Figure 2). There were no further statistically significant differences in the extent to which participants felt confident to ask a range of sources for support. While Black participants were more confident than Asian participants to ask family for support, and MEC participants were more confident than WC participants to ask religious groups for support, these differences did not reach statistical significance. Asian participants were generally less confident than Black participants in asking for support, except for their network of people with V.I. and charities. Black and Asian participants felt most comfortable asking family and friends for support. While Asian and WC participants felt least confident to ask religious groups for support, Black participants felt least confident asking local councils for support.
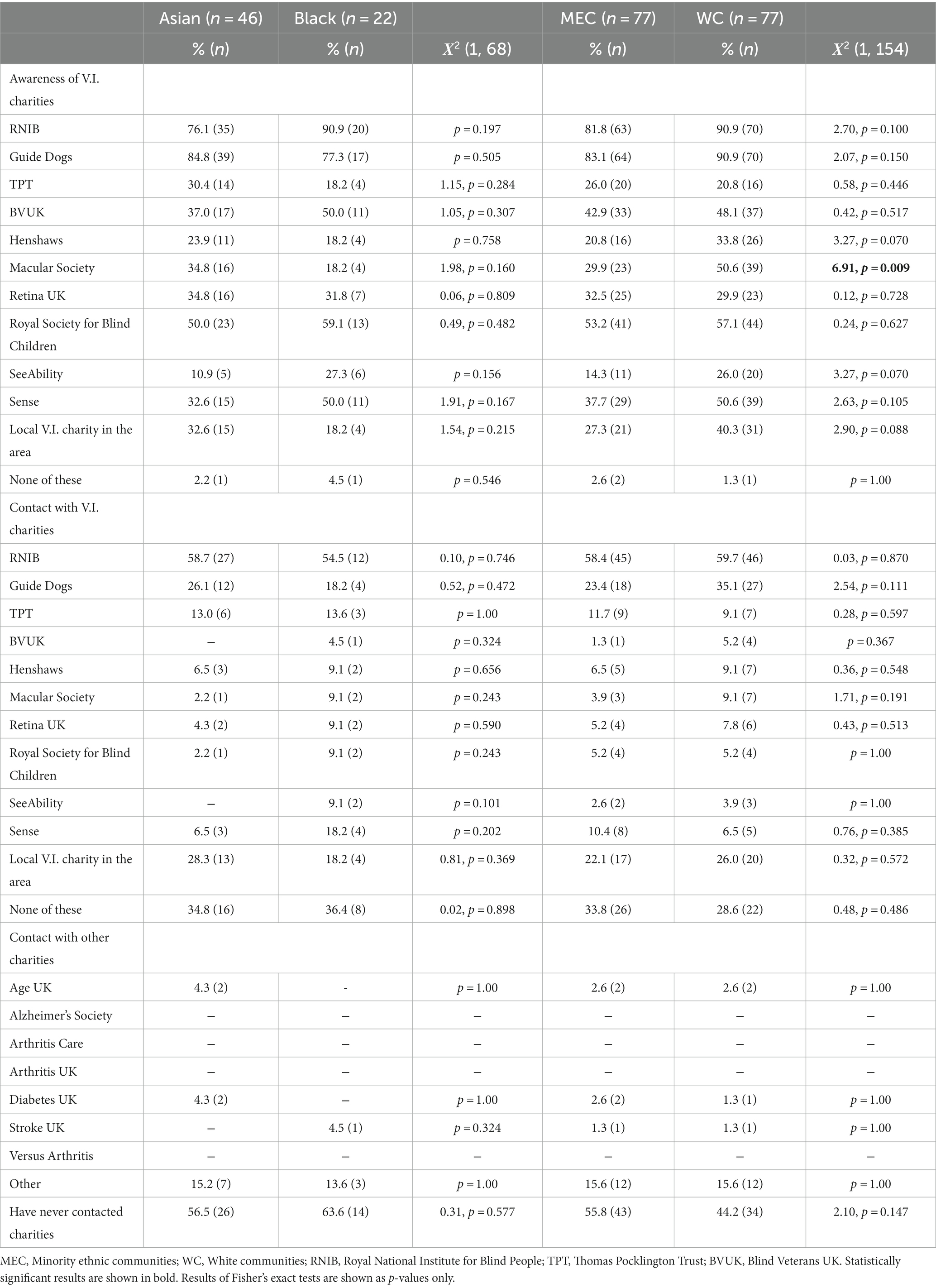
3.4 Awareness of and contact with charities
There were no statistically significant associations between ethnicity and contact with V.I. and other charities (Table 4). Support from V.I. charities was highest among WC and lowest among Black participants. Over a third of Black (36.4%) and Asian participants (34.8%) had not had any contact with any of the charities compared to 28.6% of WC participants. While the latter had had contact with an average of 1.78 (SD = 1.85, range 0–10) charities, this was slightly lower for Black (M = 1.73, SD = 2.33, range 0–10) and Asian participants (M = 1.50, SD = 1.63, range 0–5). Over half of participants in all groups had had contact with the RNIB, while contact with SeeAbility and Blind Veterans UK, who provide support for people with learning difficulties/autism and veterans with sight loss respectively, was low among all groups.
A similar pattern emerged for non-V.I. charities. Contact with these was again highest among WC and lowest among Black participants. Almost two thirds of Black (63.6%) and over half of Asian participants (56.5%) had not had contact with other charities. Most participants in all groups had contact with ‘other’, unlisted charities. A small number of participants also had contact with Stroke UK (Black and WC participants), Age UK and Diabetes UK (Asian and WC participants respectively).
Awareness of V.I. charities was higher than actual contact, but there were also no statistically significant associations between ethnicity and awareness of different sight loss charities, except for a significantly higher awareness of the Macular Society among WC (50.6%) compared to MEC participants (29.9%), Χ2 (1, 154) = 6.91, p = 0.009, Cramer’s V = 0.212. RNIB and Guide Dogs were the best-known charities among all groups, with Black participants being more aware of RNIB and Asian participants being more aware of Guide Dogs. The least-known charity among Asian participants was SeeAbility (10.9%), while comparatively lower proportions of Black participants (18.2% respectively) were aware of TPT, Henshaws, Macular Society and local V.I. charities. TPT was also the least-known charity among WC participants (20.8%). Except for RNIB, Guide Dogs and the Royal Society for Blind Children, fewer than half of Asian participants were aware of the other V.I. charities listed. While at least half of Black participants were also aware of Blind Veterans UK and Sense, awareness of the other charities was lower than for Asian participants except for SeeAbility. One Asian, Black and WC participant, respectively, had never heard of any of the V.I. charities listed.
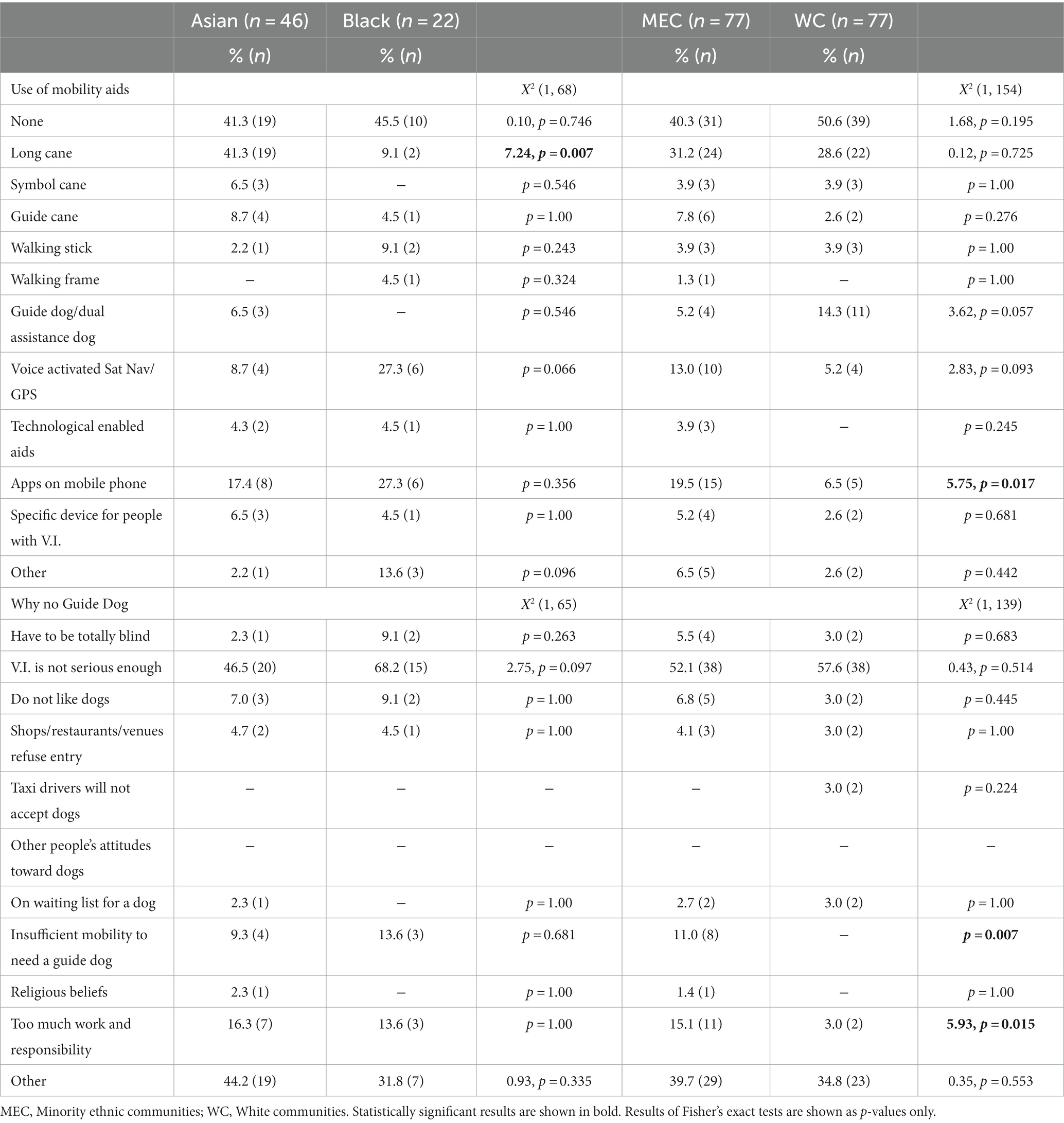
3.5 Use of mobility aids
A majority in all groups reported that they did not use any mobility aids (Table 5), although the same proportions of Asian participants reported using no aids as the long cane. Asian participants were over four times more likely to use a long cane (the most common aid among this group), Χ2 (1, 68) = 7.24, p = 0.007, Cramer’s V = 0.326, while Black participants were around three times more likely to use voice activated sat nav or GPS, but this did not reach statistical significance, p = 0.066. Voice-activated sat nav/GPS and apps on mobile phones were the most common mobility aids used by Black participants, while none used symbol canes or had a guide dog.
MEC participants were more likely than WC participants to use aids, but this was not statistically significant. MEC participants were three times more likely to use apps on their mobile, Χ2 (1, 154) = 5.75, p = 0.017, Cramer’s V = 0.193, while WC participants were just under three times more likely to have a guide dog,this did not reach statistical significance, p = 0.057. When asked why they did not have a guide dog, MEC participants were five times more likely to give too much work and responsibility as reasons, Χ2 (1, 139) = 5.93, p = 0.015, Cramer’s V = 0.206. In addition, 11.0% said they did not having sufficient mobility to need a guide dog, but none of the WC participants gave this as a reason.
A higher proportion of Black (68.2%) than Asian participants (46.5%) reported that their V.I. was not serious enough to need a guide dog, but this did not reach statistical significance, p = 0.097. The latter was the most common reason given among all groups. Only one person in the Asian group gave religious beliefs as a reason for not having a guide dog.
4 Discussion
This article provides a preliminary insight into awareness and use of V.I. services among a sample of MEC, including Asian and Black, participants.
Overall, there were few statistically significant differences between Black and Asian, and a matched control sample of MEC and WC participants in the support they had received. Among these, MEC participants were significantly more likely than WC participants to have received direct payments from social services to cover their care needs, but they were less likely to be aware of the Macular Society, agree that they got the level of emotional support they needed to get on with their life, and feel confident in asking friends for support. Within the MEC group, Black participants were significantly more likely than Asian participants to agree that they had received the right level of support when they started to experience V.I. Although neither was statistically significant, WC participants were more likely to agree that they received the practical support they needed, but they were least likely to agree that they had received the right level of support when they developed their V.I. There were further statistically significant differences between groups in the mobility aids they used: despite previous findings from qualitative research conducted in the UK that older MEC adults were less likely to have up-to-date technological devices (55), MEC participants in this sample were three times more likely to use apps on their mobile than WC participants, who, in turn, were just under three times more likely to have a guide dog. MEC participants were significantly more likely to give too much work and responsibility and not having sufficient mobility as reasons for not having a guide dog than WC participants. The lower uptake of guide dogs among MEC, particularly Black participants, is perhaps not surprising considering previous findings that guide dogs may not be appropriate among Afro-Caribbean (35) including Somali (34) communities. It has been suggested that this is due to religious or cultural beliefs which perceived dogs as wild animals rather than pets (33), but only one participant in the Asian group gave religious beliefs as a reason. Within the MEC group, Asian participants were over four times more likely than Black participants to use a long cane and, although not statistically significant, Black participants were around three times more likely to use voice activated sat nav or GPS. The comparatively higher use of technology versus mechanical mobility aids among Black participants reflects previous findings from the US which showed that use of assistive technologies (AT) was higher among African American (40, 41), but lower among Asian adults (41) compared to European American adults with disabilities. Indeed, African American adults with disabilities were 29% more likely to use AT than their European American counterparts (40). In contrast, Hispanic and African Americans were less likely to receive AT services than European Americans in the context of vocational rehabilitation (42). It is unclear to what extent these findings apply to the UK context, because research exploring ethnic group differences in the use of AT in the UK and among adults with V.I. is missing. This would be an interesting and important area of future research, first, to confirm if there are indeed ethnic group differences in AT and app usage, and second, to explore potential reasons for these. One reason for the higher use of apps among the Black participants in this particular sample may relate to preferences for more discreet AT. For example, other types of mobility assistance such as guide dogs and long canes were avoided due to their distinct association with V.I., whereas apps may be more convenient and easier to conceal. Invisible aids may be felt to be more appropriate among communities with particularly negative perceptions of people with V.I. which may make them reluctant to identify as having V.I. (13, 33). Indeed, none of the Black participants had a guide dog or used a symbol cane, which, contrary to the long cane, serves to notify others that the person has a V.I. rather than for mobility. Despite the preference for technological aids among Black participants, improving functioning and availability of technology was a bigger priority for Asian than Black participants in this sample (43). This may reflect a lack of awareness of available aids, suggesting that Asian communities may benefit from information and training about the different apps and technology that is available to support people living with V.I.
There were no statistically significant differences between groups in the last time they had visited an eye clinic nor in registration status. Contrary to existing evidence (7, 28), WC participants were slightly more likely to be unregistered (35.1%) than Black (31.8%) and Asian participants (28.3%). Although around 8 in 10 unregistered participants in all three groups had mild V.I. and may therefore not be eligible for registration, around 14% of unregistered participants in all groups had moderate or severe V.I.: of the 7 unregistered Black participants one was categorized as having moderate V.I., of the 13 unregistered Asian participants two were categorized as having moderate and two as having severe V.I., and of the 27 unregistered WC participants two were categorized as having moderate and two as having severe V.I. V.I. severity in this sample was assessed using self-reported registration status, near, distance and peripheral vision difficulties and driving status, rather than objective measures of vision status. It is possible that some participants were miscategorized, but there were no differences between groups in V.I. severity. It is unclear then if the higher proportion being unregistered among WC participants reflects an uptake of registrations among MEC adults or drop-off in registrations among WC adults since Pardhan and Mahomed (7) published their findings in 2002 and Barry and Murray (28) in 2005. Neither article provides proportions, but Barry and Murray (28) report that MEC adults were more than three times more likely to be unregistered (OR: 3.23, 95% CI: 1.56–6.65). Alternatively, the findings may reflect selection bias among MEC participants in this sample, whereby those who are in contact with services, including the V.I. register, and better supported were more likely to take part in the research. Considering the benefits associated with registration, it is important that evidence relating to uptake of registration among different communities is updated in a larger sample.
Existing evidence also suggests that MEC adults may be underrepresented among early intervention services such as ECLOs (29). However, MEC participants, particularly those from Black communities, were slightly more likely to have received support from ECLOs than WC participants in this sample, although this was not statistically significant. MEC participants were also more likely to have received some form of support, the most common among all groups being assessment and advice from a low vision clinic followed by support from specialist advice services including the RNIB helpline. The prevalence of support received from the RNIB hotline and similar specialist advice services may be expected considering that a proportion of the sample was recruited from lists provided by the RNIB. While all three Black participants referred by the RNIB had received this type of support, 8 of the 10 Asian participants and only 10 of the 18 WC participants referred by the RNIB reported that they had received support through the RNIB hotline or similar service.
The RNIB was also the best known V.I. charity. Although anecdotal evidence suggests that MEC adults may prefer to seek support from V.I. groups run by members of their community rather than national sight loss charities (31), there were no statistically significant differences for any of the charities listed including local V.I. charities in the area. Patterns of prevalence of contact with charities were similar for MEC and WC participants, though the proportion who have not had any contact with any of the V.I. charities listed was slightly higher among MEC than WC participants: over a third of Asian and Black participants have not had contact with any V.I. charities compared to over a quarter of WC participants. It is possible that this finding reflects a greater reluctance to approach charities for support. Indeed, the proportion of participants who were not at all confident in asking charities for support was much lower among WC than Asian and Black participants, but equal proportions of Asian and WC participants felt at least quite confident in asking charities for support. In contrast, half of Black participants felt not very or not at all confident in asking charities for support. Participants from Black communities also felt least confident asking their local council for support. This is of concern because it may impact on accessing vision rehabilitation, and emotional, financial and wider support available to this group. In addition, Asian participants, who were least likely to seek support from most sources, were less likely than the other groups to feel confident asking social and NHS services for support. This may impact on seeking an early diagnosis and treatment. Social services are not only responsible for the local V.I. register but can provide a range of practical and financial support to help people remain independent. Despite a higher proportion of WC participants receiving personal care and support from social services, Asian participants were most likely to receive direct payments from social services to cover their care needs. The lack of confidence in contacting social and NHS services could therefore relate to difficulties associated with the payment process. A lack of social care may also impact on the wider family with family members having to take the place of carers. Future research may need to explore the reasons for the lower confidence in medical and social services observed among Asian participants and how this impacts on eye health, care received and the wider family. While participants across all three groups felt most confident asking family and friends for support, there is some evidence that members of the Somali communities, for instance, may be reluctant to ask family for support or feel more comfortable asking a daughter than a son for support (33). Future research may need to explore gender roles and cultural differences in the extent to which people feel confident in seeking support from family members. At least half of participants in all three groups felt not very or not at all confident asking government agencies, local councils, neighbors, volunteers, and religious groups for support. Participants from Black communities were around twice as likely to feel at least quite confident in asking religious group for support, with the proportion being lowest among WC participants. The survey did not explore participants’ religious beliefs and affiliation. It is therefore not possible to explore if confidence was tied to specific religious groups or strength of religious beliefs. This may be a useful area of research as it may be possible to work with religious groups to disseminate information relating to eye health and available support.
4.1 Limitations
There are a number of sample-related limitations. Despite the cultural diversity of groups that tend to be categorized as “Asian” (44), it was not possible to compare more granular subgroups due to already small sample sizes. The relatively small sample size particularly among MEC subgroups may have impacted statistical power, resulting in the few statistically significant differences found in this study. The sample also does not include non-English speakers who may be less likely to access services or have access to services that are not provided in their mother tongue and therefore be in particular need of support. Conversely, although the majority of the sample were recruited through the Acumen health database, a small number were referred through sight loss charities such as RNIB and Guide Dogs. The participants in this study may therefore have been better supported than the general V.I. population in the UK. V.I. status was assessed using self-report, which relies on an honest and realistic response, including for a more objective measure such as registration status. Two articles (45, 46) compared subjective and objective measures of V.I. Both found some mismatches, including an overidentification of V.I. using self-report (46), nonetheless both concluded that self-report was a reasonable indicator of V.I. in surveys. While a full ophthalmic assessment would therefore be preferrable, self-reported V.I. continues to be used in V.I. research (45, 47–51).
The survey explored a wide range of topics. As a results, certain areas such as eye health service use, satisfaction with different aspects of wider support and areas where support and services were perceived to be missing were underexplored or not explored at all. As a result, future research with a bigger, representative sample will need to confirm the validity of the current findings and explore service use, support needs as well as barriers and facilitators.
5 Conclusion
This article provides a preliminary insight into the use of V.I. services and support among a sample of MEC, including Asian and Black, adults. Contrary to existing evidence, there were no statistically significant differences in eye health service use, registration of a V.I. and use of wider support services. The findings suggests that there is scope to increase uptake of support, including support provided by V.I. charities and through the V.I. register. Further research is required to understand the reasons why MEC participants felt less confident than WC participants in asking charities and their local council for support. Similarly, cultural differences in the acceptability of and resulting preferences for different types of mobility aids warrant further exploration to ensure that appropriate support can be provided.
Scope statement
Visual impairment (V.I.) has been associated with a negative impact on a wide range of life domains including activities of daily living, sports and leisure activities, social activities quality-of-life and mental health. There are various eye health and support services available to those living with V.I. in the UK. However, there is some evidence of inequalities relating to ethnicity and eye service use in the UK: adults from minority ethnic communities (MEC) may delay seeking a diagnosis or treatment, be underrepresented among services, which can provide vital support such as early intervention services, and the V.I. register, which can provide financial and functional support. However, much of the evidence requires confirmation or updating and/or relates to a BAME supergroup. This secondary analysis provides preliminary insights into the use of eye health and a range of support services among a sample of MEC, including Asian and Black, adults. Although there were few statistically significant differences, the findings provide practical insights into habits and patterns relating to service and mobility aid use among the different groups, highlighting, for instance, that there is scope to increase uptake of support provided by V.I. charities and through the V.I. register among MEC participants.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
Ethical approval was not required for the study involving humans in accordance with the local legislation and institutional requirements. Written informed consent to participate in this study was not required from the participants or the participants’ legal guardians/next of kin in accordance with the national legislation and the institutional requirements.
Author contributions
NH: Conceptualization, Data curation, Formal analysis, Methodology, Visualization, Writing – original draft. LJ: Methodology, Visualization, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This research was supported by the Thomas Pocklington Trust, grant number: FR-00380.
Acknowledgments
The authors would like to thank the Royal National Institute of the Blind (RNIB), Thomas Pocklington Trust (TβPT) and Guide Dogs for the Blind Association (Guide Dogs) for sharing “V.I. Lives” survey data with us for the purpose of this secondary analysis. A particular thank you to Hilary Ingleton at the RNIB for providing the data set and answering questions about the survey methods, data collection and individual variables.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
UK, United Kingdom; MEC, Minority ethnic communities; WC, White communities; V.I., Visual impairment; ECLO, Eye Clinic Liaison Officer.
References
1. Pezzullo, L, Streatfeild, J, Simkiss, P, and Shickle, D. The economic impact of sight loss and blindness in the UK adult population. BMC Health Serv Res. (2018) 18:1–13. doi: 10.1186/s12913-018-2836-0
2. ONS. Ethnic group. England and Wales: Census 2021 Office for National Statistics (2022). Available at: https://www.ons.gov.uk/peoplepopulationandcommunity/culturalidentity/ethnicity/bulletins/ethnicgroupenglandandwales/census2021 (Accessed August 14, 2023).
3. Cumberland, PM, and Rahi, JS. Visual function, social position, and health and life chances: the UK biobank study. JAMA Ophthalmol. (2016) 134:959–66. doi: 10.1001/jamaophthalmol.2016.1778
4. Dawes, P, Dickinson, C, Emsley, R, Bishop, PN, Cruickshanks, KJ, Edmondson-Jones, M, et al. Vision impairment and dual sensory problems in middle age. Ophthalmic Physiol Opt. (2014) 34:479–88. doi: 10.1111/opo.12138
5. Wormald, R, Basauri, E, Wright, L, and Evans, J. The African Caribbean eye survey: risk factors for glaucoma in a sample of African Caribbean people living in London. Eye. (1994) 8:315–20. doi: 10.1038/eye.1994.64
6. Rudnicka, AR, Mt-Isa, S, Owen, CG, Cook, DG, and Ashby, D. Variations in primary open-angle glaucoma prevalence by age, gender, and race: a Bayesian meta-analysis. Invest Ophthalmol Vis Sci. (2006) 47:4254–61. doi: 10.1167/iovs.06-0299
7. Pardhan, S, and Mahomed, I. The clinical characteristics of Asian and Caucasian patients on Bradford’s low vision register. Eye. (2002) 16:572–6. doi: 10.1038/sj.eye.6700164
8. Pardhan, S, Gilchrist, J, and Mahomed, I. Impact of age and duration on sight–threatening retinopathy in south Asians and Caucasians attending a diabetic clinic. Eye. (2004) 18:233–40. doi: 10.1038/sj.eye.6700629
9. Das, B, Thompson, J, Patel, R, and Rosenthal, A. The prevalence of eye disease in Leicester: a comparison of adults of Asian and European descent. J R Soc Med. (1994) 87:219.
10. Deloitte Access Economics. The economic impact of sight loss and blindness in the UK adult population, 2013. RNIB. (2014)
11. Kirthi, V, Reed, KI, Gunawardena, R, Alattar, K, Bunce, C, and Jackson, TL. Do black and Asian individuals wait longer for treatment? A survival analysis investigating the effect of ethnicity on time-to-clinic and time-to-treatment for diabetic eye disease. Diabetologia. (2021) 64:749–57. doi: 10.1007/s00125-020-05364-5
12. Patel, D, Baker, H, and Murdoch, I. Barriers to uptake of eye care services by the Indian population living in Ealing, West London. Health Educ J. (2006) 65:267–76. doi: 10.1177/0017896906067777
13. Cross, V, Shah, P, Bativala, R, and Spurgeon, P. Glaucoma awareness and perceptions of risk among African–Caribbeans in Birmingham, UK. Divers Health Soc Care. (2005) 2:81–90.
14. Alma, MA. Participation of the elderly after vision loss. Disabil Rehabil. (2011) 33:63–72. doi: 10.3109/09638288.2010.488711
15. Gopinath, B, Liew, G, Burlutsky, G, and Mitchell, P. Age-related macular degeneration and 5-year incidence of impaired activities of daily living. Maturitas. (2014) 77:263–6. doi: 10.1016/j.maturitas.2013.12.001
16. Jaarsma, EA, Dekker, R, Koopmans, SA, Dijkstra, PU, and Geertzen, JH. Barriers to and facilitators of sports participation in people with visual impairments. Adapt Phys Act Q. (2014) 31:240–64. doi: 10.1123/2013-0119
17. Phoenix, C, Griffin, M, and Smith, B. Physical activity among older people with sight loss: a qualitative research study to inform policy and practice. Public Health. (2015) 129:124–30. doi: 10.1016/j.puhe.2014.10.001
18. Fenwick, E, Rees, G, Pesudovs, K, Dirani, M, Kawasaki, R, Wong, TY, et al. Social and emotional impact of diabetic retinopathy: a review. Clin Exp Ophthalmol. (2012) 40:27–38. doi: 10.1111/j.1442-9071.2011.02599.x
19. Zhang, X, Bullard, KM, Cotch, MF, Wilson, MR, Rovner, BW, McGwin, G, et al. Association between depression and functional vision loss in persons 20 years of age or older in the United States, NHANES 2005-2008. JAMA Ophthalmol. (2013) 131:573–81. doi: 10.1001/jamaophthalmol.2013.2597
20. Fenwick, EK, Pesudovs, K, Khadka, J, Dirani, M, Rees, G, Wong, TY, et al. The impact of diabetic retinopathy on quality of life: qualitative findings from an item bank development project. Qual Life Res. (2012) 21:1771–82. doi: 10.1007/s11136-012-0110-1
21. van der Aa, HP, Comijs, HC, Penninx, BW, van Rens, GH, and van Nispen, RM. Major depressive and anxiety disorders in visually impaired older adults. Invest Ophthalmol Vis Sci. (2015) 56:849–54. doi: 10.1167/iovs.14-15848
22. Frank, CR, Xiang, X, Stagg, BC, and Ehrlich, JR. Longitudinal associations of self-reported vision impairment with symptoms of anxiety and depression among older adults in the United States. JAMA Ophthalmol. (2019) 137:793–00. doi: 10.1001/jamaophthalmol.2019.1085
23. Schliermann, R, Heydenreich, P, Bungter, T, and Anneken, V. Health-related quality of life in working-age adults with visual impairments in Germany. Disabil Rehabil. (2017) 39:428–37. doi: 10.3109/09638288.2016.1146353
24. Heinze, N, Jones, L, and Makwana, B. A rapid review of evidence relating to service use, experiences, and support needs of adults from minority ethnic communities along the eyecare pathway in the United Kingdom. Front. Public Health. (2023) 11:540. doi: 10.3389/fpubh.2023.1119540
25. RNIB. Registering as sight impaired London, UK: RNIB. Available at: https://www.rnib.org.uk/your-eyes/navigating-sight-loss/registering-as-sight-impaired/ (Accessed December 4, 2023).
26. RNIB. The criteria for certification: RNIB. Available at: https://www.rnib.org.uk/eye-health/registering-your-sight-loss/criteria-certification (Accessed December 4, 2023).
27. Department of Health and Social Care. Registering vision impairment as a disability UK: Department of Health and Social Care. (2018). Available at: https://www.gov.uk/government/publications/guidance-published-on-registering-a-vision-impairment-as-a-disability (accessed 19 November, 2018).
28. Barry, RJ, and Murray, PI. Unregistered visual impairment: is registration a failing system? Br J Ophthalmol. (2005) 89:995–8. doi: 10.1136/bjo.2004.059915
29. Slade, J. Early intervention support in eye clinics - an overview of emotional and practical support in UK eye clinics for the year 2012/13. London, UK: RNIB (2014).
30. Menon, V, Treen, T, Burdon, MA, and Batra, R. Impact of the eye clinic liaison officer at an NHS foundation trust: a retrospective study. BMJ Open ophthalmol. (2020) 5:e000587. doi: 10.1136/bmjophth-2020-000587
31. Peace, S, Katz, J, Holland, C, and Jones, R. The needs and aspirations of older people with vision impairment. UK: TPT (2016).
32. Johnson, MRD, and Morjaria-Keval, A. Ethnicity, sight loss and invisibility. Br J Vis Impair. (2007) 25:21–31. doi: 10.1177/0264619607071772
33. Higginbottom, GM, Rivers, K, and Story, R. Health and social care needs of Somali refugees with visual impairment (VIP) living in the United Kingdom: a focused ethnography with Somali people with VIP, their caregivers, service providers, and members of the horn of Africa blind society. J Transcult Nurs. (2014) 25:192–01. doi: 10.1177/1043659613515715
34. Biddyr, S, Molik, B, Garwood, P, Sheen, N, Griffiths, S, and Porter, T. Eye health Care in Black and Minority Ethnic Communities. UK: RNIB (2016).
35. Cross, V, Shah, P, Bativala, R, and Spurgeon, P. ReGAE 2: glaucoma awareness and the primary eye-care service: some perceptions among African Caribbeans in Birmingham UK. Eye. (2007) 21:912–20. doi: 10.1038/sj.eye.6702461
36. RNIB, Guide Dogs, TPT. VI lives-an in-depth understanding of the experiences of people living with vision impairment (VI) in the UK. London, UK: RNIB, Guide Dogs, TPT (2022).
37. Heinze, N, and Castle, CL. Exploring mental well-being, the emotional impact of visual impairment and experiences of prejudice and discrimination among adults from minority ethnic communities in the UK. Front Public Health. (2023) 11:1277341. doi: 10.3389/fpubh.2023.1277341
38. R Core Team. R: A language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing (2021).
40. Loggins, S, Alston, R, and Lewis, A. Utilization of assistive technology by persons with physical disabilities: an examination of predictive factors by race. Disabil Rehabil Assist Technol. (2014) 9:487–92. doi: 10.3109/17483107.2013.836683
41. Chan, KT-K, and Marsack-Topolewski, C. Examining social determinants in use of assistive technology for race/ethnic groups of older adults. Disability and rehabilitation. Assist Technol. (2022) 17:703–11.
42. Huang, IC, Cheing, G, Rumrill, P, Bengtson, K, Chan, F, Telzlaff, J, et al. Characteristics of people with disabilities receiving assistive technology services in vocational rehabilitation: a logistic regression analysis. J Vocat Rehabil. (2016) 45:63–72. doi: 10.3233/JVR-160811
43. Heinze, N, and Jones, L. Priority issues among a sample of adults from minority ethnic communities who are living with visual impairment in the UK. Submitted for publication. (2023).
45. Zimdars, A, Nazroo, J, and Gjonça, E. The circumstances of older people in England with self-reported visual impairment: a secondary analysis of the English longitudinal study of ageing (ELSA). Br J Vis Impair. (2012) 30:22–30. doi: 10.1177/0264619611427374
46. Whillans, J, and Nazroo, J. Assessment of visual impairment: the relationship between self-reported vision and ‘gold-standard’ measured visual acuity. Br J Vis Impair. (2014) 32:236–48. doi: 10.1177/0264619614543532
47. Horowitz, A, Brennan, M, and Reinhardt, JP. Prevalence and risk factors for self-reported visual impairment among middle-aged and older adults. Res Aging. (2005) 27:307–26. doi: 10.1177/0164027504274267
48. Jin, Y-P, and Wong, DT. Self-reported visual impairment in elderly Canadians and its impact on healthy living. Can J Ophthalmol. (2008) 43:407–13. doi: 10.3129/i08-077
49. Bekibele, CO, and Gureje, O. Impact of self-reported visual impairment on quality of life in the Ibadan study of ageing. Br J Ophthalmol. (2008) 92:612–5. doi: 10.1136/bjo.2007.124859
50. Ryskulova, A, Turczyn, K, Makuc, DM, Cotch, MF, Klein, RJ, and Janiszewski, R. Self-reported age-related eye diseases and visual impairment in the United States: results of the 2002 national health interview survey. Am J Public Health. (2008) 98:454–61. doi: 10.2105/AJPH.2006.098202
51. Crews, JE, Chou, C-F, Zhang, X, Zack, MM, and Saaddine, JB. Health-related quality of life among people aged≥ 65 years with self-reported visual impairment: findings from the 2006–2010 behavioral risk factor surveillance system. Ophthalmic Epidemiol. (2014) 21:287–96. doi: 10.3109/09286586.2014.926556
Keywords: visual impairment, sight loss, minority ethnic, BamE, service use, eye health, support, health inequalities scope statement
Citation: Heinze N and Jones L (2024) Access to eye care and support services among adults from minority ethnic communities living with visual impairment in the United Kingdom. Front. Public Health. 11:1277519. doi: 10.3389/fpubh.2023.1277519
Edited by:
Zhiqiang Feng, University of Edinburgh, United KingdomReviewed by:
Frouke Nienke Boonstra, Royal Dutch Visio, NetherlandsAneta Grochowska, University of Applied Sciences in Tarnow, Poland
Copyright © 2024 Heinze and Jones. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Nikki Heinze, Tmlra2kuaGVpbnplQGJyYXZvdmljdG9yLm9yZw==
 Nikki Heinze
Nikki Heinze Lee Jones
Lee Jones