
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health , 08 January 2024
Sec. Disaster and Emergency Medicine
Volume 11 - 2023 | https://doi.org/10.3389/fpubh.2023.1276898
 Robiana Modjo1,2*
Robiana Modjo1,2* Fatma Lestari1,3*
Fatma Lestari1,3* Hendra Tanjung1,2
Hendra Tanjung1,2 Abdul Kadir1
Abdul Kadir1 Riskiyana Sukandhi Putra4
Riskiyana Sukandhi Putra4 Meilisa Rahmadani2,5
Meilisa Rahmadani2,5 Ali Syahrul Chaeruman2
Ali Syahrul Chaeruman2 Fetrina Lestari2
Fetrina Lestari2 Juliana Sutanto6
Juliana Sutanto6Introduction: The outbreak of SARS-CoV-2 in 2019 led to a global pandemic, posing unprecedented challenges to healthcare systems, particularly in hospitals.
Purpose: This study explores the intricacies of strategies employed for preventing and controlling COVID-19 in Indonesian hospitals, with a particular focus on the protocols, challenges, and solutions faced by healthcare professionals.
Methods: Using a cross-sectional analysis, we examined 27 hospitals and uncovered disparities in their preparedness levels. During our investigation, we observed the robust implementation of infection prevention measures, which encompassed stringent protocols, adequate ventilation, and proper use of personal protective equipment. However, shortcomings were identified in areas such as surveillance, mental health support, and patient management.
Discussion: This study underscores the importance of addressing these gaps, suggesting tailored interventions, and continuous training for healthcare staff. Effective leadership, positive team dynamics, and adherence to comprehensive policies emerge as pivotal factors. Hospitals should strengthen weak areas, ensure the ethical execution of emergency protocols, and integrate technology for tracking and improving standard operating procedures. By enhancing the knowledge and skills of healthcare workers and maintaining strong management practices, hospitals can optimize their efforts in COVID-19 prevention and control, thereby safeguarding the wellbeing of professionals, patients, and communities.
In December 2019, a novel coronavirus, known as SARS-CoV-2, surfaced in Wuhan, China, giving rise to a global pandemic recognized as COVID-19 (1, 2). The swift transmission of the virus posed an unprecedented challenge to healthcare systems worldwide, requiring immediate and effective responses to mitigate its consequences (3). Hospitals, situated at the forefront of the battle against COVID-19, encountered significant challenges in ensuring the safety of healthcare professionals who were tirelessly working to treat and care for patients.
One of the risks healthcare professionals faced was their susceptibility to infection due to prolonged direct exposure to COVID-19 patients or contact with virus-contaminated surfaces, potentially leading to subsequent contact with their facial areas, including the eyes, nose, and mouth. Furthermore, specific healthcare procedures, such as endotracheal intubation and noninvasive ventilation, had the potential to aerosolize the virus, making it an airborne pathogen. This circumstance significantly increased the risk encountered by healthcare professionals (4–6).
Ensuring the safety of healthcare workers is of utmost importance not only for their wellbeing but also for the welfare of patients, staff, and the community they serve. Furthermore, it is essential for maintaining the effectiveness of the healthcare system during a pandemic (3, 7, 8). Therefore, prioritizing health and safety in hospitals is crucial for providing high-quality patient care, supporting the wellbeing of health workers, complying with the regulations, optimizing resources, and preparing for emergency situations. Nevertheless, implementing safety and health in hospitals during the COVID-19 pandemic was challenging. Numerous challenges were encountered, including insufficient resources (9, 10), overwhelmed healthcare systems (11), and healthcare staff experiencing fatigue and burnout (12).
Indonesia, like many other countries, grappled with the immense burden posed by the pandemic. Tragically, during the COVID-19 pandemic, a total of 2,087 healthcare professionals lost their lives, including 751 doctors, 670 nurses, 398 midwives, and 46 dentists, underscoring the significant impact of the virus on the country’s medical community (13). In addition, a crucial aspect of Indonesia’s fight against COVID-19 is how infection prevention and control measures are implemented in hospitals to safeguard the health and wellbeing of healthcare workers. Interestingly, Indonesia, as a diverse archipelagic nation with a large population, faced distinctive challenges in managing the transmission of the virus within healthcare facilities (14, 15).
Therefore, this study examines the strategies, protocols, and experiences of hospital workers in Indonesia as they grappled with the complexities of managing COVID-19 infections while continuing to provide essential healthcare services. Understanding the challenges faced by hospital workers in Indonesia, as well as the innovative solutions and best practices developed in response, is essential for shaping future policies and practices. This study delves into the multifaceted aspects of infection prevention and control in Indonesian hospitals, examining leadership aspects, coordination and communication, surveillance, risk communication, human resources, training for healthcare workers, and infection prevention and control.
The research was conducted using a cross-sectional approach over a span of 6 months, from July to December 2020. The assessment of hospital workers’ protection was based on Ministry of Health Regulation No. 412 of the year 2020, which outlines guidelines for COVID-19 prevention and control, and Ministry of Health Regulation No. 327, which designates COVID-19 as a work-related disease for specific workers (7, 8). A total of 27 hospitals were selected from six provinces in Indonesia: West Java, Central Java, South Kalimantan, East Java, West Kalimantan, and West Sumatera. The distribution of hospitals across these provinces is as follows: West Java (4 hospitals), East Java (4 hospitals), Central Java (4 hospitals), South Kalimantan (4 hospitals), West Kalimantan (5 hospitals), and West Sumatera (6 hospitals). Figure 1 shows the locations of the selected hospitals in these six Indonesian provinces.
A non-probabilistic purposive sampling method was used in this study. The selected hospitals were all members of the network of the Indonesian Occupational Health Association (IOHA).
The selected hospitals were requested to complete a self-assessment evaluation form, which was distributed through the network of IOHA. These forms were filled out by key informants within the hospitals and then validated and verified through the local network of IOHA. The evaluation consisted of 12 elements, as detailed in Table 1. The scoring system was based on the degree of compliance with Ministry of Health Regulation No. 412 of the year 2020, which outlines guidelines for COVID-19 prevention and control, and Ministry of Health Regulation No. 327, which designates COVID-19 as a work-related disease for specific workers (16, 17). Compliance with these regulations was classified as “Very Good” if it exceeded 80%, “Good” if it ranged from 61 to 80%, “Sufficient” if it was between 41 and 60%, and “Poor” if it was ≤40%. The self-assessment evaluation form is available in Supplementary material.
Data were collected and analyzed using an Excel sheet. The analysis involved univariate analysis, which entailed presenting important information related to variables and assessing compliance with Indonesia’s Ministry of Health regulations. Data were then visualized through the use of bar charts, spider diagrams, and compliance-level presentations.
The study was reviewed and approved by the ethics committee of the Research and Community Engagement of the Faculty of Public Health, Universitas Indonesia, under Ethics Approval Letter No. Ket-435/UN2.F10.D11/PPM.00.02/2020. Informed consent procedures were explained in detail during the ethics approval process and obtained consent prior to the commencement of the study. All methods applied for this study were performed in compliance with the relevant guidelines and regulations of the ethical committee. It is important to note that no animals or human subjects were used or involved in this study.
The present study involves an analysis of diverse hospital parameters, including their class distinctions, bed capacity, ancillary amenities, and workforce composition, with a focus on their susceptibility to COVID-19. Furthermore, the assessment of COVID-19 management and control measures was conducted using a sample of hospitals categorized as Type A, Type B, Type C, and Type D. An examination of the acquired data reveals that Type A hospitals exhibit significantly superior metrics in terms of bed capacity, supporting facilities, and human resources compared to their counterparts in Type B, Type C, and Type D hospitals (Table 2).
Table 3 presents a comprehensive overview of COVID-19 incidence among the workforce in the 27 hospitals under scrutiny. MWS Hospital reported the highest number of positive cases, with 219 out of 2,316 total workers tested positive. Remarkably, three hospitals, namely, RS PBC, SJJ Hospital, and PTK Hospital, reported no instances of COVID-19 among their employees. Moreover, 11 hospitals had an equal number of workers who tested positive for COVID-19 and those who had recovered. This suggests that no fatalities occurred within these hospitals, and all affected workers had successfully recuperated by the time of data collection. Conversely, six hospitals documented cases of worker mortality due to COVID-19. Notably, DSS Hospital reported the highest fatality rate, with 10 individuals, including 4 healthcare workers and 6 non-healthcare workers, succumbing to the virus.
Table 4 presents the compliance percentages of various hospitals with the COVID-19 prevention and control guidelines established by the Indonesian Ministry of Health. RS RST exhibited the lowest compliance rate at 52.97%, while RS PTJ demonstrated the highest adherence, with a score of 98.51%. The data analysis revealed that 63% of the sampled hospitals achieved very good implementation, with a score exceeding 80%. Additionally, 33% of the hospitals were classified as having good implementation, with scores ranging from 60 to 80%. Conversely, a mere 4% of the hospitals demonstrated inadequate implementation, scoring below 60%, as illustrated in Figure 2.
Upon closer examination of each element of regulation within the areas of study, the data reveal that infection prevention and control exhibited the highest level of compliance, standing at an impressive 92%. Following closely behind are risk communication and community engagement and rapid identification and diagnosis, all at 80%. The lowest levels of compliance were observed in the areas of surveillance and information management; occupational health, mental health, and psychosocial support; and patient management, with scores of 69, 68, and 66%, respectively. When considering different geographic areas, East Java emerged as the leader, with a mean score of 83%. West Kalimantan secured the second position with a score of 77%, while South Kalimantan, West Java, and Central Java achieved scores of 71, 70, and 70%, respectively (Table 5). Figure 3 shows a radar plot analysis, providing an overview of COVID-19 prevention and control assessments in hospitals across the six areas. Strong performance is evident in the elements of infection prevention and control and risk communication and community engagement. In addition, the evaluation of COVID-19 preparedness for each element within the 27 hospitals is displayed, with red areas indicating a score below 60%, categorized as poor implementation Attachment S1.
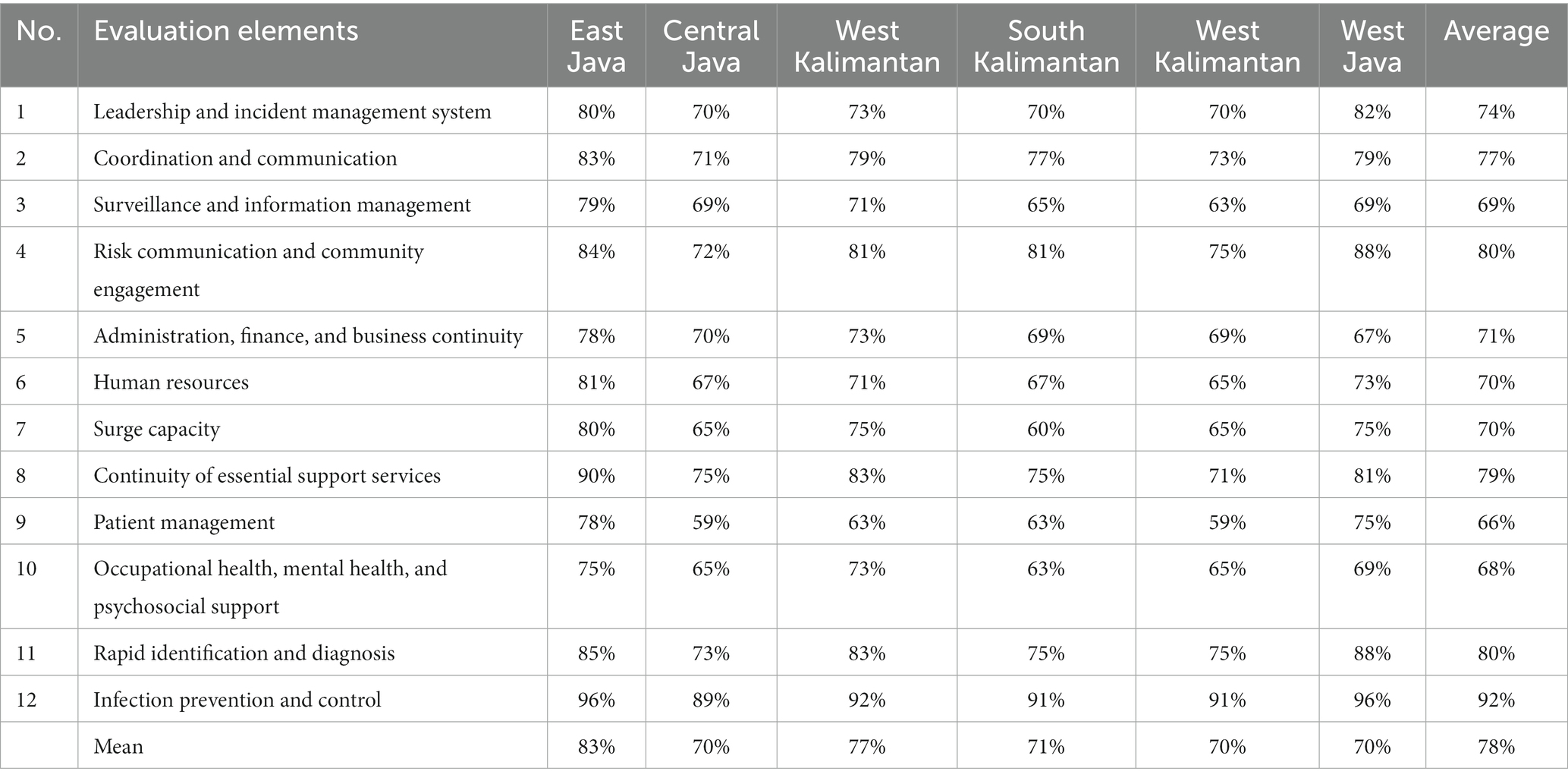
Table 5. Mean score evaluation for each element and area of COVID-19 prevention and control in hospitals.
The findings of this study have brought to light significant disparities in the preparedness and response capabilities of hospitals in the face of the COVID-19 pandemic. The World Health Organization (WHO) emphasized the escalating demand for healthcare systems, a direct consequence of the rising number of COVID-19 cases. This surge has particularly underscored the criticality of augmenting hospital bed capacities to cater to the exigencies of the most severe cases within the prevailing pandemic context (18). Addressing this challenge necessitates the implementation of a range of interventions aimed at curtailing and mitigating the virus’s transmission within healthcare facilities (19). In addition, the comprehensive analysis of various hospital parameters was crucial according to the implementation of COVID-19 prevention and control for hospital workers in Indonesia by referring to Ministry of Health Regulation Number 413 of 2020 and Indonesian Ministry of Health Regulation No. 327 of the year 2020, which provided valuable insights into the susceptibility of different hospitals to COVID-19. Our study categorized hospitals into four types—A, B, C, and D—based on the following parameters: leadership and incident management system; coordination and communication; surveillance and information management; risk communication and community engagement; administration, finance, and business continuity; human resources; surge capacity; sustainability of essential services; patient management; occupational health, mental health, and psychosocial support; rapid identification and diagnosis; and infection prevention and control.
Our study assessed a hospital’s compliance with COVID-19 regulations across various elements. Strong implementation was seen in infection prevention and control, rapid identification and diagnosis, and risk communication. However, areas needing improvement included surveillance and information management, occupational health, mental health, psychosocial support, and patient management.
In infection prevention, most hospitals ensure adequate PPE, ventilation, and hygiene measures. Moreover, hospitals effectively controlled the spread of COVID-19 through strategic measures. Occupational Health and Safety Officers ensured PPE availability, coordinating with units and monitoring usage. Given the airborne transmission risk during medical procedures and treatments, stringent precautions were advised, mandating the utilization of PPE, such as masks, coveralls, gloves, and goggles (20). Furthermore, standard operational procedures (SOPs) for prevention, control, and management were rigorously maintained and updated. Isolation areas with proper ventilation and clear instructions were established. The implementation of SOPs for COVID-19 prevention, control, and management was rigorously maintained. These SOPs, which are vital in preventing COVID-19 dissemination, were subject to periodic reviews and updates, accommodating the evolving nature of the pandemic (21). Hand hygiene stations were strategically placed, and multilingual educational posters were used. Staff were trained per WHO guidelines, emphasizing hand hygiene, social distancing, and proper PPE use. Beds were spaced 1 m apart regardless of COVID-19 status, ensuring infection prevention. Crucially, infection prevention and control were bolstered by the strategic allocation of isolation areas equipped with clear instructions, adequate supplies, and effective ventilation systems. Utilizing negative-pressure rooms with controlled airflow, especially when using mechanical ventilation, was imperative to prevent cross-contamination. Ventilation systems, maintaining optimal thermal conditions and adequate airflow, were acknowledged as fundamental in healthcare facilities by authoritative bodies, such as the Pan American Health Organization (PAHO). A ventilation rate of 6 to 12 air changes per hour, with 12 ACH being ideal for new constructions, was recommended (22).
In addition to these technical measures, the hospitals emphasized general preventive strategies. Entry and hospital areas were equipped with essential facilities for hand hygiene, including water, soap, tissue, hand sanitizers, and strategically placed trash cans. Encouragingly, the populace was educated on appropriate handwashing practices and advised to maintain social distancing (23). Hospitals disseminated information through multilingual posters, ensuring clarity and understanding and covering topics such as hand hygiene, respiratory etiquette, and social distancing. Furthermore, hospital staff underwent rigorous training in adherence to Regulation 413/WHO guidelines, focusing on meticulous hand hygiene, respiratory etiquette, social distancing, and the proper utilization of personal protective equipment. Policies mandating a minimum 1-m spacing between beds, irrespective of suspected COVID-19 cases, were established and diligently enforced.
Rapid identification involved staff training, communication systems, and sample handling. Risk communication protocols were effectively disseminated to staff, patients, and the community. Our study found that key indicators in rapid COVID-19 identification emphasized intensive staff training. Prompt diagnosis and reporting were crucial due to the virus’s novelty, necessitating swift screening to identify clinical symptoms (24). The hospital ensured comprehensive training, focusing on hygiene and workplace controls during outbreaks (25). A robust communication system covering entrances and patient areas facilitated rapid case reporting. Informative materials in labs aided safe sample handling and disseminated vital health information (26). In addition, emergency departments implemented efficient triage procedures, promptly isolating and assessing patients with respiratory symptoms. This comprehensive approach underscored the hospital’s commitment to efficient and accurate COVID-19 diagnosis and management. Furthermore, in a serious pandemic situation, there has been a shift in messaging, emphasizing the importance of supporting precautions when communicating about the crisis. Given these circumstances, it is crucial to assist organizations and institutions in achieving their goals and missions. Encouraging public trust and preventing harm and disruption are essential (27). Additionally, to ensure primary healthcare and promote people-centered services, it is crucial to consider community engagement within the healthcare sector. Involvement and participation among communities are viewed as critical in various sectors, including healthcare facilities. During the COVID-19 pandemic, the resilience of communities became a vital component in building trust and minimizing the spread of the virus (28, 29).
Surveillance and information management lacked in data reporting and integration. Hospital workers, both healthcare and non-healthcare workers, have been informed and trained on the definition of COVID-19 cases, including the definition of close contact and quarantine systems. Standard forms for reporting COVID-19 case information to a centralized health information system (Team/Task Force/Committee) within 24 h of identifying cases are available. SOPs for collecting, confirming, and validating COVID-19 data for designated workers are also in place. However, hospitals with low scores indicate a lack of several indicators in this element. According to Morgan et al. (30), the uncontrolled spread of the virus was due to the weak surveillance of cases and insufficient capacity of institutions or countries to integrate data for public health controls. It was also reported that some countries had poor data management and dissemination of data to residents. Furthermore, addressing infection prevention could be achieved by utilizing information technology in each phase of the crisis, such as a pandemic, especially for public health surveillance. Information technology has been employed to enhance the speed of diagnosis, improve epidemic management, monitor the situation, and deliver important information related to health promotion (31, 32).
Another concern in prevention and control programs in health settings is psychosocial issues. It was seen that occupational health and mental health support needed attention due to high stress levels among healthcare workers. It identified the profound issue of psychosocial challenges during pandemic situations. The research found a high prevalence of mental health problems among healthcare employees, particularly those dealing with COVID-19 patients. These problems encompass not only anxiety, insomnia, and depression but also somatization and post-traumatic stress symptoms (33). A study conducted in Toronto revealed alarming statistics: 30.4% of health professionals experienced burnout syndrome, 44.9% suffered from psychosocial distress, and 13.8% exhibited post-traumatic stress symptoms (34, 35). Visheh et al. (36) emphasized that healthcare workers face immense challenges due to highly infectious diseases. They often worked in isolated areas without adequate education and training, leading to a decline in their mental health. Consequently, it is crucial to implement appropriate measures to address these issues, including supportive interventions, encouragement, motivation, protective measures, and educational and training interventions.
Several fundamental indicators for preventing and controlling COVID-19 in hospitals include occupational health, mental health, and psychosocial support, including providing protection, training, and personal protective equipment (PPE) for hospital workers offering medical services to suspected, probable, or confirmed COVID-19 cases. This includes screening, resuscitation, initial stabilization, supportive therapy, and prevention of complications. A risk management process should be implemented in hospitals to prevent and control COVID-19 in every work area or location related to potential worker exposure. Policies and capacities for managing occupational safety and health, coupled with infection prevention and control measures, should be in place to safeguard hospital staff, suspected cases, their families, and close contacts.
The patient management aspect was the weakest element implemented in the study hospitals. Indicators in this category include hospitals updating protocols for essential care services for COVID-19 patients based on WHO guidelines, Ministry of Health regulations, regional policies, and hospital protocols. In addition, it is recommended to establish functioning procedures for receiving and transferring patients to isolation areas within the hospital, along with providing the necessary therapeutic and diagnostic support services.
Current best practices, such as placing all suspected patients in droplet masks during assessments and transit, restricting visitors, and implementing appropriate standard precautions, have been suggested for isolating and controlling infections in confirmed and suspected cases, as noted by Jamil et al. (37). Healthcare professionals should be familiar with these procedures to avoid mistakes (38). The WHO emphasizes that infection prevention and control are as critical as clinical patient management, healthcare professional safety, and preventing hospital-acquired infections. Therefore, implementing administrative, environmental, and engineering controls is crucial in healthcare facilities (39). Furthermore, healthcare facilities need to establish protocols for untested, trial, or emergency measures that have not been clinically approved, as well as ethically approved clinical trials or the Monitored Emergency Use of Unregistered Interventions (MEURI framework), all of which should be closely monitored. Hospitals must also ensure the implementation of infection prevention and control protocols, establish a safe hospital or health facility network, and provide transportation services for patient referrals, including transfers from home care services, if available.
Leadership and incident management systems were crucial, demanding effective policies and positive leader–team relationships to navigate the challenges posed by the pandemic. Effective leadership and incident management systems are vital for the success of COVID-19 prevention and control efforts (40). Rapid responses have been crucial in understanding and addressing COVID-19. The implementation of policies to combat COVID-19 has directly impacted institutional leadership, making them instrumental in guiding organizational teams. Therefore, fostering positive relationships between leaders and teams is essential (41). Positive social interactions in the workplace can nurture trust, respect, and support, enhancing employee performance (42). Furthermore, the COVID-19 pandemic poses challenges for leaders, testing their ability to handle cases and implement efficient incident management systems (IMSs) (43). It is crucial to design an IMS tailored for each country to bolster follow-up and support during crises, including pandemics (44).
It is important to acknowledge the strengths and limitations of this study. The in-depth analysis of hospital factors and adherence to regulations offers valuable insights into the pandemic-related challenges hospitals encounter. Nonetheless, it is essential to note that the study’s scope is limited to a particular area and might not apply universally. Moreover, relying on historical data may not reflect current, real-time changes in hospital readiness and responses. Future studies could benefit from additional analyses employing advanced methods. However, important implications and areas for further exploration according to our study are improving hospital preparedness through policy implementation by encouraging hospitals and healthcare systems to implement and adhere to comprehensive policies, particularly focusing on weak areas identified in our study, such as surveillance and information management, mental health support, and patient management protocols. In addition, enhancing skills related to rapid identification, information management, and patient care, especially for mental health support, are also crucial to be provided by healthcare institutions. To support the psychosocial aspects, designing interventions that address the mental health and psychosocial challenges faced by healthcare workers also needs to be considered. In terms of prevention and control, prevention programs should be implemented that integrate technology for better tracking of protocols and PPE usage, emphasize continuous improvement, regularly update SOPs, and ensure ethical considerations in emergency measures and protocols. Improving leadership and incident management and promoting positive team relationships for effective collaboration is vital for addressing the challenges presented by the pandemic.
This study examines the current state of COVID-19 prevention and control implementation in healthcare settings. In conclusion, the study reveals that the majority of hospitals achieved good scores, indicating full compliance with the regulations that minimize the spread of COVID-19 in the workplace and mitigate its impact on various aspects. The three elements that received the highest scores are infection prevention and control, risk communication and communication engagement, and rapid identification and diagnosis. However, the areas with the most room for improvement are surveillance and information management; occupational health, mental health, and psychosocial support; and patient management. Addressing these aspects necessitates a strong commitment to hospital management, ultimately safeguarding the health and wellbeing of healthcare professionals, patients, and communities from the threat of COVID-19. Providing healthcare workers with updated and regular training is vital to ensure their proficiency and procedures when dealing with individuals affected by COVID-19. This effort has yielded positive impacts, but it is important for hospital management to maintain focus on areas that received moderate scores, such as human resources; surge capacity; administration, finance, and business continuity; coordination and communication; and leadership and incident management systems. By addressing these areas, hospitals can attain the highest level of COVID-19 prevention and control implementation in the workplace.
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
RM: Conceptualization, Methodology, Resources, Validation, Visualization Writing – original draft, Writing – review & editing, Data curation, Formal analysis, Funding acquisition, Investigation, Supervision. FaL: Conceptualization, Data curation, Investigation, Methodology, Supervision, Validation, Writing – original draft, Writing – review & editing. HT: Conceptualization, Data curation, Investigation, Resources, Software, Validation, Writing – original draft, Writing – review & editing. AK: Conceptualization, Methodology, Resources, Software, Validation, Visualization, Writing – original draft, Writing – review & editing. RP: Investigation, Resources, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. MR: Investigation, Methodology, Project administration, Validation, Visualization, Writing – original draft, Writing – review & editing. AC: Investigation, Methodology, Project administration, Validation, Visualization, Writing – original draft, Writing – review & editing. FeL: Investigation, Methodology, Project administration, Resources, Visualization, Writing – original draft, Writing – review & editing. JS: Conceptualization, Methodology, Software, Validation, Visualization, Writing – review & editing.
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. All authors would like to thank the Indonesian Ministry of Health and the Directorate of Research and Development (Risbang) at the University of Indonesia for providing funding to conduct this study through the Q1 International Indexed Publication (PUTI) funding scheme (grant no. NKB-467/UN2.RST/HKP.05.00/2022). The authors would also like to thank all 27 hospitals for taking part in this study.
Researchers would like to thank the Disaster Risk and Reduction Center Universitas Indonesia (DRRC UI) for their support in completing this study.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2023.1276898/full#supplementary-material
1. Allegranzi, B, Tartari, E, and Pittet, D. “Seconds save Lives – Clean Your Hands”: The 5 May 2021 World Health Organization SAVE LIVES: Clean Your Hands Campaign. J. Hosp. Infect. (2021) 111:1–3.
2. Pérez-Campos Mayoral, L, Hernández-Huerta, MT, Mayoral-Andrade, G, Pérez-Campos Mayoral, E, and Pérez-Campos, E. A letter to the editor on "World Health Organization declares global emergency: A review of the 2019 novel coronavirus (COVID-19)". Int J Surg (2020) 79:163–4. doi: 10.1016/j.ijsu.2020.05.066
3. Filip, R, Gheorghita Puscaselu, R, Anchidin-Norocel, L, Dimian, M, and Savage, WK. Global challenges to public health care systems during the COVID-19 pandemic: A review of pandemic measures and problems. J Pers Med (2022) 12:1295. doi: 10.3390/jpm12081295
4. Chhablani, N, and Choudhari, SG. Behind the frontline: A review on the impact of COVID-19 pandemic on healthcare workers. Cureus (2022) 14:e29349. doi: 10.7759/cureus.29349
5. Alhouri, A, Shokor, MA, Marwa, K, Sharabi, A, and Nazir, DM. COVID-19 and its impact on healthcare workers: understanding stigma, stress, and quality of life. Cureus (2023) 15:e37846. doi: 10.7759/cureus.37846
6. Tran, K, Cimon, K, Severn, M, Pessoa-Silva, CL, and Conly, J. Aerosol generating procedures and risk of transmission of acute respiratory infections to healthcare workers: A systematic review. PLoS One (2012) 7:e35797. doi: 10.1371/journal.pone.0035797
7. Haileamlak, A. The impact of COVID-19 on health and health systems. Ethiop J Health Sci (2021) 31:1073–4. doi: 10.4314/ejhs.v31i6.1
8. Mahendradhata, Y, Andayani, NLPE, Hasri, ET, Arifi, MD, Siahaan, RGM, Solikha, DA, et al. The capacity of the Indonesian healthcare system to respond to COVID-19. Front Public Health (2021) 9:649819. doi: 10.3389/fpubh.2021.649819
9. Ceulemans, LJ, Van Slambrouck, J, De Leyn, P, Decaluwé, H, Van Veer, H, Depypere, L, et al. Successful double-lung transplantation from a donor previously infected with SARS-CoV-2. Lancet Respir Med (2021) 9:315–8. doi: 10.1016/S2213-2600(20)30524-5
10. Alhalaseh, YN, Elshabrawy, HA, Erashdi, M, Shahait, M, Abu-Humdan, AM, and Al-Hussaini, M. Allocation of the “already” limited medical resources amid the COVID-19 pandemic, an iterative ethical encounter including suggested solutions from a real life encounter. Front Med (2021) 7:616277. doi: 10.3389/fmed.2020.616277
11. Badalov, E, Blackler, L, Scharf, AE, Matsoukas, K, Chawla, S, Voigt, LP, et al. COVID-19 double jeopardy: the overwhelming impact of the social determinants of health. Int J Equity Health (2022) 21:76. doi: 10.1186/s12939-022-01629-0
12. Leo, CG, Sabina, S, Tumolo, MR, Bodini, A, Ponzini, G, Sabato, E, et al. Burnout among healthcare workers in the COVID 19 era: A review of the existing literature. Front Public Health (2021) 9:750529. doi: 10.3389/fpubh.2021.750529
13. Yayasan Warga Berdaya untuk Indonesia. STATISTIK Mereka yang gugur selama pandemi COVID-19. (2023) Available at: https://nakes.laporcovid19.org (Accessed 12 September 2023).
14. Harapan, BN, Harapan, T, Theodora, L, and Anantama, NA. From archipelago to pandemic battleground: unveiling Indonesia’s COVID-19 crisis. J Epidemiol Glob Health (2023) 13:591–603. doi: 10.1007/s44197-023-00148-7
15. Anindyajati, G, Mardiasmo, DR, Sekarasih, L, Susilaradeya, D, Takwin, B, Pelupessy, DC, et al. The right to health: COVID-19 pandemic and the opportunity to transform mental health inequalities in Indonesia. Front Public Health (2022) 10:844656. doi: 10.3389/fpubh.2022.844656
16. Kemenkes, R. I. Keputusan Menteri Kesehatan Republik Indonesia Nomor HK.01.07/MenKes/413/2020 Tentang Pedoman Pencegahan Dan Pengendalian Corona Virus Disease 2019 (Covid-19). MenKes/413/2020. Kementerian Kesehatan Republik Indonesia. (2020) 2019, 1–207.
17. Menteri Kesehatan, R. I. Keputusan Menteri Kesehatan Republik Indonesia Nomor HK.01.07/Menkes/327/2020 Tentang Penetapan Corona Virus Disease 2019 (COVID-19) Akibat Kerja Sebagai Penyakit Akibat Kerja Yang Spesifik Pada Pekerjaan Tertentu. Kementerian Kesehatan Republik Indonesia. (2020) 2019, 1–8.
19. Jefferson, T, Del Mar, CB, Dooley, L, Ferroni, E, Al-Ansary, LA, Bawazeer, GA, et al. Physical interventions to interrupt or reduce the spread of respiratory viruses. Cochrane Database Syst Rev (2011) 7:CD006207. doi: 10.1002/14651858.CD006207.pub4
20. World Health Organization (WHO). Rational use of personal protective equipment for coronavirus disease 2019 (COVID-19): Interim guidance, 6 April 2020. WHO (2020) 1–7. Available at: https://www.who.int/publications/i/item/rational-use-of-personal-protective-equipment-for-coronavirus-disease-(covid-19)-and-considerations-during-severe-shortages
21. WHO. Standard operating procedures (SOPs) for the movement of essential health and humanitarian supplies and personnel in the context of the COVID-19 pandemic in Africa. WHO (2020). Available at: https://www.afro.who.int/sites/default/files/Covid-19/Techinical%20documents/SOPs%20for%20the%20Movement%20of%20Essential%20Health%20and%20Humanitarian%20Supplies%20and%20Personnel.pdf
22. PAHO. Recommendations for heating, ventilation, and air conditioning in healthcare facilities. (2020) PAHO. 3–5. Available at: https://iris.paho.org/handle/10665.2/53303
23. Güner, R, Hasanoğlu, İ, and Aktaş, F. Covid-19: prevention and control measures in community. Turk J Med Sci (2020) 50:571–7. doi: 10.3906/sag-2004-146
24. Ghaderzadeh, M, and Asadi, F. Deep learning in the detection and diagnosis of COVID-19 using radiology modalities: A systematic review. J Healthc Eng (2021) 2021:1–10. doi: 10.1155/2021/6677314
25. OSHA. Guidance on preparing workplaces for COVID-19. United States of America: US Dep Labor (2020) 1–35.
26. Cereci, S., Tanyildizi, N. I., Yigit, M., and Erbas, S., Selected topics in communication. U.S. Department of Labor Occupational Safety and Health Administration. (2020).
27. Heydari, ST, Zarei, L, Sadati, AK, Moradi, N, Akbari, M, Mehralian, G, et al. The effect of risk communication on preventive and protective Behaviours during the COVID-19 outbreak: mediating role of risk perception. BMC Public Health (2021) 21:1–11. doi: 10.1186/s12889-020-10125-5
28. Rifkin, SB. Lessons from community participation in health Programmes: A review of the post Alma-Ata experience. Int Health (2009) 1:31–6. doi: 10.1016/j.inhe.2009.02.001
29. Gilmore, B, Ndejjo, R, Tchetchia, A, De Claro, V, Mago, E, Diallo, AA, et al. Community engagement for COVID-19 prevention and control: A rapid evidence synthesis. BMJ Glob Health (2020) 5:e003188. doi: 10.1136/bmjgh-2020-003188
30. Morgan, OW, Aguilera, X, Ammon, A, Amuasi, J, Fall, IS, Frieden, T, et al. Disease surveillance for the COVID-19 era: time for bold changes. Lancet (2021) 397:2317–9. doi: 10.1016/s0140-6736(21)01096-5
31. George, DB, Taylor, W, Shaman, J, Rivers, C, Paul, B, O’Toole, T, et al. Technology to advance infectious disease forecasting for outbreak management. Nat Commun (2019) 10:8–11. doi: 10.1038/s41467-019-11901-7
32. Asadzadeh, A, Pakkhoo, S, Saeidabad, MM, Khezri, H, and Ferdousi, R. Information Technology in Emergency Management of COVID-19 outbreak. Informatics Med Unlocked (2020) 21:100475. doi: 10.1016/j.imu.2020.100475
33. Kusumawardani, DA, Nurika, G, and Luthfiyana, NU. The mental health of medical workers during the Covid19 pandemic: how do we manage it? J Kesehat Lingkung (2020) 12:21. doi: 10.20473/jkl.v12i1si.2020.21-28
34. Lancee, WJ, Maunder, RG, and Goldbloom, DS. Prevalence of psychiatric disorders among Toronto hospital workers one to two years after the SARS outbreak. Psychiatr Serv (2008) 59:1–5. doi: 10.1176/ps.2008.59.1.91
35. Asnakew, S, Amha, H, and Kassew, T. Mental health adverse effects of COVID-19 pandemic on health Care Workers in North West Ethiopia: A multicenter cross-sectional study. Neuropsychiatr Dis Treat (2021) 17:1375–84. doi: 10.2147/ndt.s306300
36. Vizheh, M, Qorbani, M, Arzaghi, SM, Muhidin, S, Javanmard, Z, and Esmaeili, M. The mental health of healthcare workers in the COVID-19 pandemic: A systematic review. J Diabetes Metab Disord (2020) 19:1967–78. doi: 10.1007/s40200-020-00643-9
37. Jamil, S, Mark, N, Carlos, G, Dela Cruz, CS, Gross, JE, and Pasnick, S. Diagnosis and management of COVID-19 disease. Am J Respir Crit Care Med (2020) 201:P19–20. doi: 10.1164/rccm.2020C1
38. Shang, Y, Pan, C, Yang, X, Zhong, M, Shang, X, Wu, Z, et al. Management of Critically ill Patients with COVID-19 in ICU: statement from front-line intensive care experts in Wuhan, China. Ann Intensive Care (2020) 10:73. doi: 10.1186/s13613-020-00689-1
39. WHO. Clinical management clinical management living guidance COVID-19. Geneva: WHO (2021). Available at: https://iris.who.int/bitstream/handle/10665/372288/WHO-2019-nCoV-clinical-2023.2-eng.pdf?sequence=1
40. The Lancet. Emerging understandings of 2019-NCoV. Lancet (2020) 395:311. doi: 10.1016/S0140-6736(20)30186-0
41. Chen, JKC, and Sriphon, T. Perspective on COVID-19 pandemic factors impacting organizational leadership. Sustainability (2021) 13:3230. doi: 10.3390/su13063230
42. Houston, E. The importance of positive relationships in the workplace. (2021) Available at: https://positivepsychology.com/positive-relationships-workplace/ (Accessed 3 June 2021).
43. Fernandez, AA, and Shaw, GP. Academic leadership in a time of crisis: the coronavirus and COVID-19. J Leadersh Stud (2020) 14:39–45. doi: 10.1002/jls.21684
Keywords: COVID-19 infection prevention and control, implementation of OHS in hospitals, occupational health, protection of hospital workers, Indonesian Ministry of Health Regulations
Citation: Modjo R, Lestari F, Tanjung H, Kadir A, Putra RS, Rahmadani M, Chaeruman AS, Lestari F and Sutanto J (2024) COVID-19 infection prevention and control for hospital workers in Indonesia. Front. Public Health. 11:1276898. doi: 10.3389/fpubh.2023.1276898
Received: 13 August 2023; Accepted: 12 December 2023;
Published: 08 January 2024.
Edited by:
Tim Sandle, The University of Manchester, United KingdomReviewed by:
Ihab H. Sawalha, American University of Madaba, JordanCopyright © 2024 Modjo, Lestari, Tanjung, Kadir, Putra, Rahmadani, Chaeruman, Lestari and Sutanto. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Robiana Modjo, YmlhbkB1aS5hYy5pZA==; Fatma Lestari, ZmF0bWFAdWkuYWMuaWQ=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.