- 1Department of Rehabilitation Medicine, The First Affiliated Hospital of Gannan Medical University, Ganzhou, Jiangxi Province, China
- 2Ganzhou Key Laboratory of Rehabilitation Medicine, Ganzhou, Jiangxi Province, China
- 3Ganzhou Intelligent Rehabilitation Technology Innovation Center, Ganzhou, Jiangxi Province, China
- 4Shaanxi Rehabilitation Hospital, Xi'an, Shaanxi Province, China
- 5School of Public Health and Health Management, Gannan Medical University, Ganzhou, Jiangxi Province, China
- 6Department of Rehabilitation Medicine, Xi’an Children’s Hospital, Xi’an, Shaanxi Province, China
Objective: This study aimed to investigate the use intention and influencing factors of telerehabilitation in people with rehabilitation needs.
Methods: This cross-sectional survey recruited a total of 183 participants with rehabilitation needs from May 2022 to December 2022. Sociodemographic and medical data were collected by a structured questionnaire. The factors influencing the use intention of telerehabilitation were measured by the extended Unified Theory of Acceptance and Use of Technology (UTAUT) model. Multiple hierarchical regression analyses were performed.
Results: A total of 150 valid questionnaires were included for analysis. The results indicated that the use intention of telerehabilitation was overall high in people with rehabilitation needs. Health condition (β = −0.21, p = 0.03), performance expectancy (β = 0.21, p = 0.01), facilitating conditions (β = 0.25, p = 0.03), perceived trust (β = 0.25, p < 0.01), and self-efficacy (β = 0.19, p = 0.04) were significant factors influencing the use intention of telerehabilitation.
Conclusion: Overall, the use intention of telerehabilitation is high in individuals with rehabilitation needs. Health conditions, performance expectancy, facilitating conditions, perceived trust, and self-efficacy are important factors influencing the use intention of telerehabilitation in individuals with rehabilitation needs.
Introduction
With the aging of the population and the rising incidence of disabling diseases, the number of people with rehabilitation needs is rapidly growing worldwide (1, 2). These people with severe functional impairment often require long-term and persistent rehabilitation services to improve their functional limitations and quality of life, which results in a huge health and economic burden on their families and society (3, 4). The World Health Organization indicates that the globe is facing challenges related to the increasing unmet rehabilitation needs in this century, especially in some low-income and middle-income countries (5). According to a survey, the rehabilitation needs of Chinese older adult have increased more than 70% in the past 30 years, which is much higher than the world average (6).
In order to redress the imbalance between the supply and demand of rehabilitation services, some healthcare organizations or countries attempted to use telerehabilitation to provide professional rehabilitation services for people with rehabilitation needs, including consultation, education, assessment, monitoring, and treatment (7–10). However, telerehabilitation is currently still in the early stages of implementation in most areas (11). The use intention and influencing factors of telerehabilitation remain unclear in people with rehabilitation needs. Therefore, a comprehensive understanding of the use intention and influencing factors of telerehabilitation is a prerequisite to facilitate its application.
The Unified Theory of Acceptance and Use of Technology (UTATU) model is one of the most widely used models for exploring behavioral intention (BI) to use new technologies, and it explains approximately 70% of the variance in behavioral intentions (12). The UTAUT model includes four core predictors: Performance expectancy (PE), effort expectancy (EE), social influence (SI), and facilitating conditions (FC) (13). Currently, several studies have applied the UTAUT model in the context of telemedicine to analyze the underlying factors influencing users’ behavioral intentions to adopt telemedicine (14–16). However, some studies suggest that the variables of the UTAUT model cannot fully explain users’ BI to telemedicine (17). Therefore, some studies have extended the original UTAUT model by integrating context-specific determinants to improve its predictive power. For example, Zhu et al. (14), Breil et al. (18), and Li et al. (19) extended the UTAUT model by applying perceived risk (PR), perceived trust (PT), and self-efficacy (SE) and concluded that these are also important factors that influence users’ use of telemedicine. In addition, a recent review indicated that patient characteristics (e.g., age, gender, educational level, and occupation) and health conditions were also important factors influencing patient’s use of telemedicine (20).
Therefore, this study aimed to investigate the use intention and influencing factors of telerehabilitation in people with rehabilitation needs in terms of three aspects: patients’ sociodemographic characteristics, medical characteristics, and an extended UTAUT theoretical model.
Methods
Study design and participants
A cross-sectional survey was conducted to investigate the behavioral intentions to use telerehabilitation among people with rehabilitation needs. Participants were recruited in the Department of Rehabilitation Medicine, First Affiliated Hospital of Gannan Medical University from May 2022 to December 2022. The department covers a wide range of the most common rehabilitation populations: cerebrovascular diseases, musculoskeletal chronic pain, post-operative fracture, etc.
The inclusion criteria of participants in this study were patients aged 14 years or older, who had completed at least 1 week of rehabilitation therapy. This questionnaire was completed on-site by the participants or their direct relatives in a paper form. Before the start of the survey, the researchers introduced the background, content, and objectives of this survey to each participant to ensure their informed consent, and this questionnaire was anonymous and voluntary. This study was approved by the Ethics Committee of the First Affiliated Hospital of Gannan Medical University.
Measures
The first section of this survey questionnaire used a structured questionnaire to collect the sociodemographic data (e.g., gender, age, occupation, and educational level) and medical data (e.g., diagnosis, impact of health condition on one’s life, and telerehabilitation experience) of the participants. The second section was to identify the factors influencing users’ behavioral intention to use telerehabilitation using an extended UTAUT model. The 28-item extended UTAUT questionnaire consists of eight constructs that influence behavioral intention to use telerehabilitation: PE, EE, SI, FC, PR, PT, SE, and BI. We defined each variables based on the specific context of telerehabilitation: PE was defined as the extent to which individuals believe that using the telerehabilitation will help them to improve in functional performance; EE was defined as the degree of ease associated with the use of the telerehabilitation; SI was defined as the extent to which individuals are impacted by the opinions of surrounding groups; FC was defined as the extent to which an individual believes that an organizational and technical infrastructure exists to support the use of the telerehabilitation; PR was defined as an individual’s expectation of the impact of uncertainty or loss resulting from the use of telerehabilitation; PT was defined as the extent to which individual perceives telerehabilitation to be reliable and trustworthy; SE was defined as the extent to which individual perceives that he or she can successfully use telerehabilitation; BI was defined as the extent to which individuals tendency to use or recommend an telerehabilitation. All items are measured with a 5-point Likert scale, ranging from (1) “strongly disagree” to (5) “strongly agree.”
To ensure the reliability and validity of this questionnaire, all items were adopted or modified from previous studies. The test results showed the Cronbach’s alpha for each construct ranged from 0.754 to 0.882, the average variance extracted (AVE) ranged from 0.619 to 0.765, and the square root of AVE for each construct was greater than the correlation coefficient between other constructs and itself, indicating good reliability and validity (17). This survey questionnaire is detailed in Appendix 1.
Statistical analysis
SPSS 25.0 (SPSS Inc., Chicago, IL, United States) was used for descriptive, univariate, and multivariate statistical analysis. Between-group differences in sociodemographic and medical characteristics at BI were analyzed using analysis of variance and independent t-tests. Correlations for the eight constructs of the extended UTAUT were analyzed using Pearson correlation coefficients. Multiple hierarchical regression analysis was performed to investigate the possible predictors of the adoption intention of telerehabilitation. With all regression assumptions satisfied, BI was considered as the dependent variable and the independent variables were sequentially entered into the regression model in three modules: (1) sociodemographic data, (2) medical data, and (3) extended UTAUT predictors. A two-tailed value of p < 0.05 was considered as statistically significant.
We used Smart-PLS 4.0 (free trial version) to test the reliability and validity. A Cronbach’s alpha higher than 0.7 indicates higher internal consistency. The average variance extracted (AVE) higher than 0.5 and the square root of AVE for each construct greater than the correlation coefficient between other constructs and itself indicate a good convergent validity (17).
Results
Sociodemographic and medical characteristics
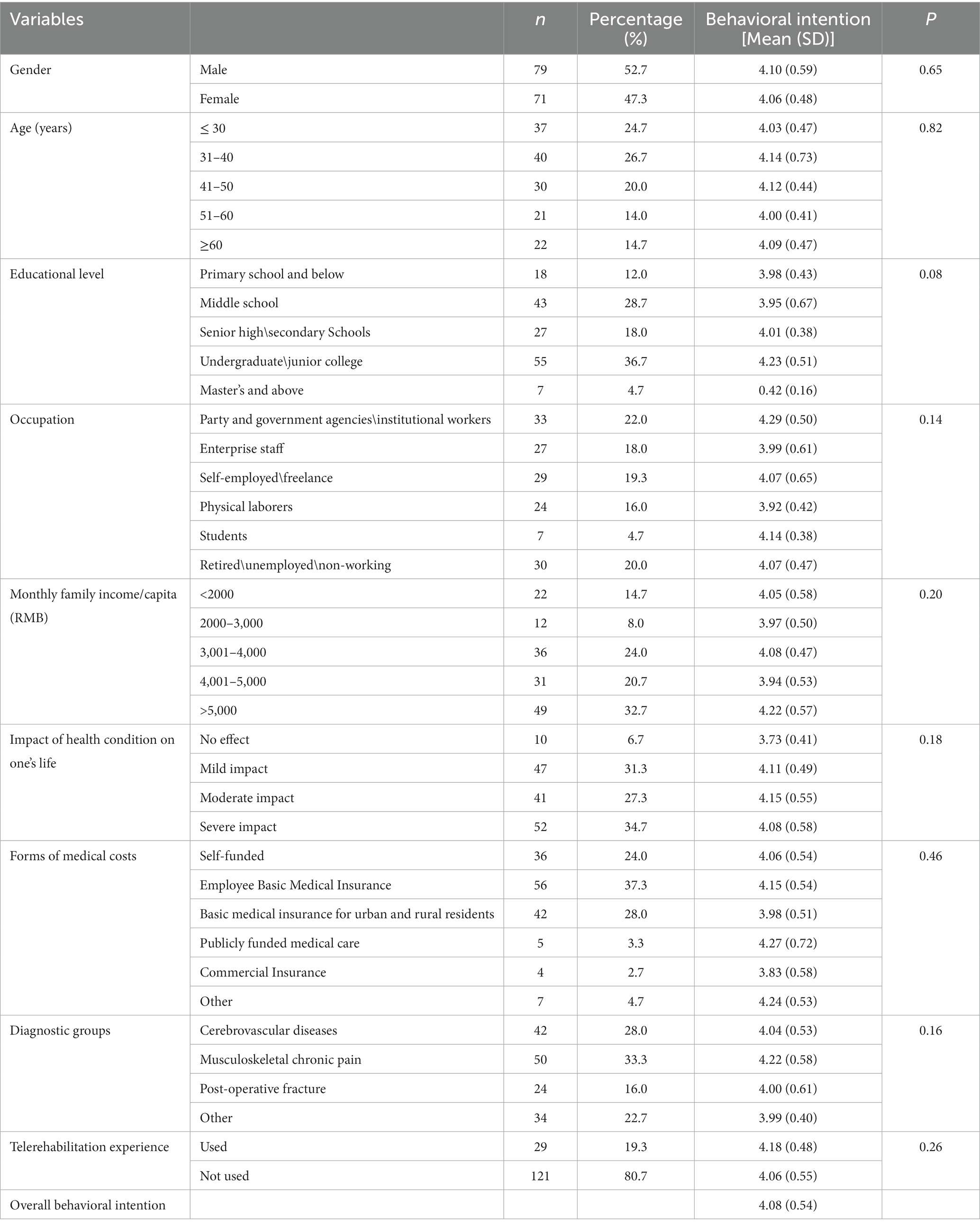
A total of 183 questionnaires were collected, including 150 valid questionnaires and 33 invalid questionnaires (15 were completed in less than 1 min, 13 had the same obvious answer, 5 had unfilled options in the questionnaire), with a validity rate of 81.97%. The sociodemographic and medical characteristics of 150 participants are shown in Table 1. The majority of participants stated that they had not previously used telerehabilitation, and only 29 (19.3%) had previously used telerehabilitation.
Adoption of telerehabilitation
The use intention of telerehabilitation was overall high in patients with rehabilitation needs with a mean of 4.08 (SD 0.54; Table 1) (21). There were no statistical differences in BI for all groups of sociodemographic and medical characteristics (Table 1; p > 0.05).
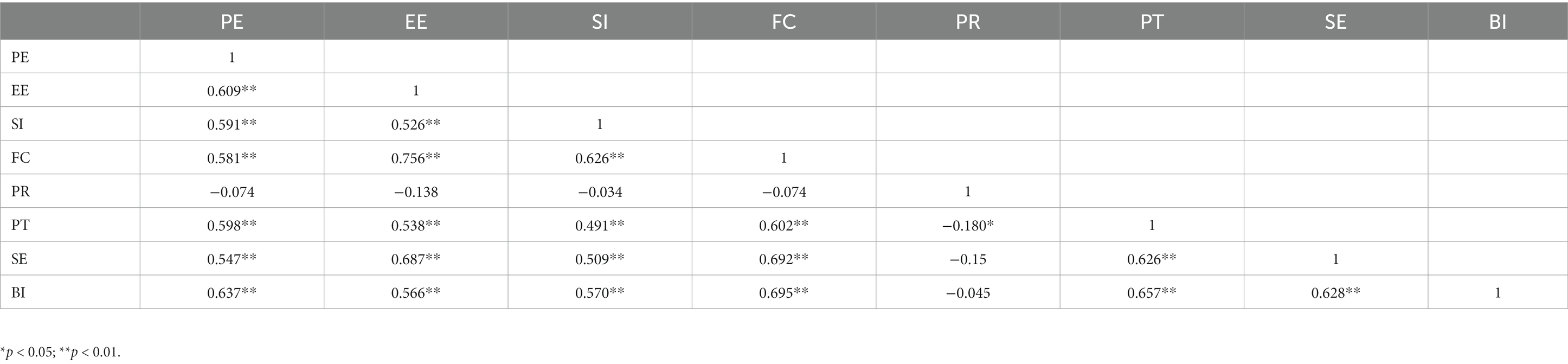
Correlation between constructs
Table 2 indicates that PE, EE, SI, FC, PR, PT, and SE had a significant positive correlation with BI. However, no significant correlation was found between BI and PR.
Multiple hierarchical regression analysis
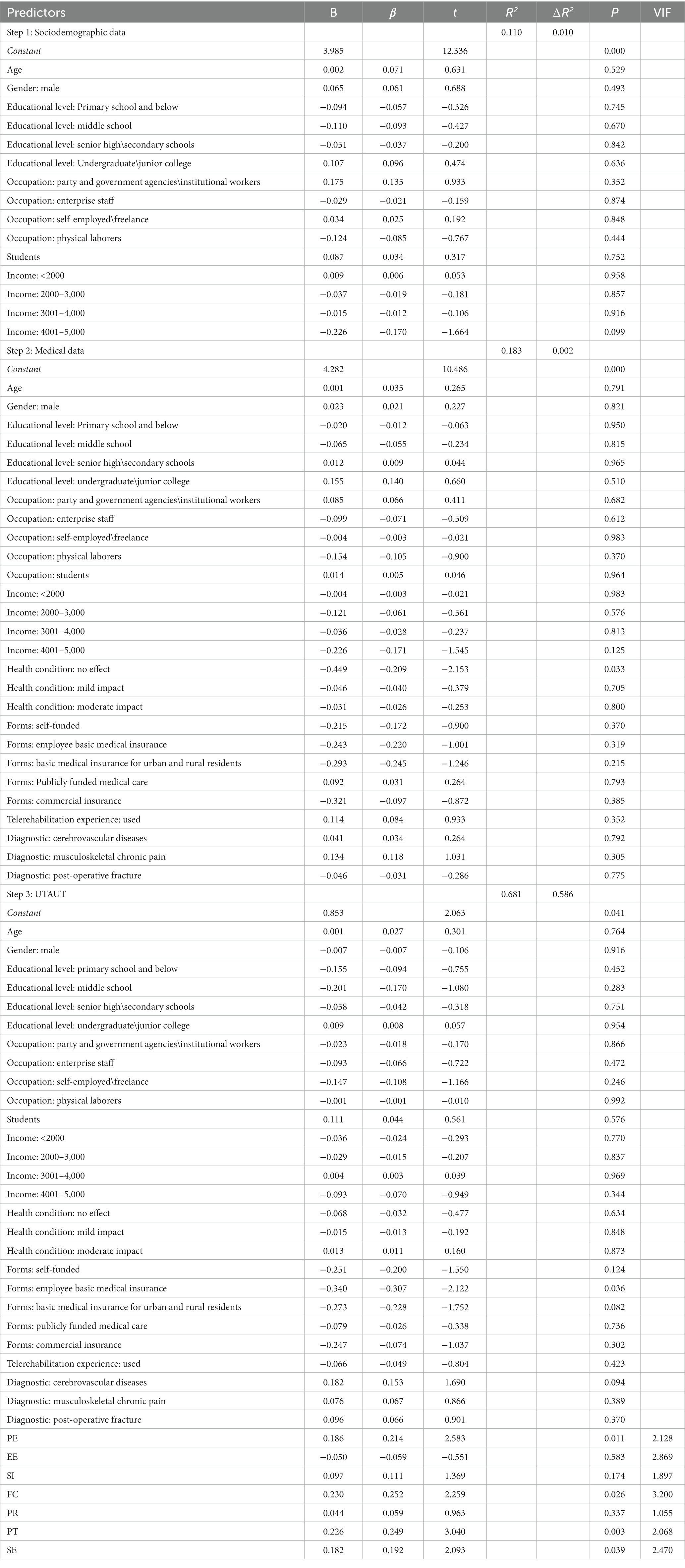
Table 3 summarizes the results of multiple hierarchical regression analysis. Sociodemographic data were included in the first step (R2 = 0.110, ∆R2 = 0.01, F = 1.10, p = 0.36) and explained 11% of the variance of BI. Sociodemographic characteristics were not significant factors influencing BI for telerehabilitation.
The second step included medical data as predictors (R2 = 0.183, ∆R2 = 0.002, F = 1.01, p = 0.46), and explained 18.3% of the variance of BI. In this step, a significant factor influencing BI was health condition: no effect (β = −0.21, p = 0.03).
The extended UTAUT predictors were included in the third step of hierarchical regression analysis (R2 = 0.68, ∆R2 = 0.59, F = 7.21, p < 0.001) and explained 68% of the variance of BI. PE (β = 0.21), FC (β = 0.25), PT (β = 0.25), and SE (β = 0.19) were significant factors influencing the intention to use telerehabilitation (p < 0.05). There was no multicollinearity found between the constructs because the variance inflation factor (VIF) values were all ⩽ 3 (22).
Discussion
This study investigated the BI and potential factors influencing the use of telerehabilitation by people with rehabilitation needs. Overall, the individuals’ use intention telerehabilitation is high. Our results indicated that individuals with severe self-assessed health conditions have higher use intentions for telerehabilitation, and PE, FC, PT, and SE are important factors influencing the intention to adopt telerehabilitation for individuals with rehabilitation needs.
Inconsistent with our findings, some previous studies indicated that the other user group (e.g., diabetic, chronic pain, and hospitalized) acceptance of telemedicine was only low-moderate (21, 23, 24). This may be because these studies were done 7 years ago, during which time telemedicine has gradually entered the public’s life with the rapid development of communication technology and the popularization of smart devices and has received increasing attention from a growing number of patients. On the other hand, the COVID-19 pandemic has hindered the traditional face-to-face medical service model, which in turn has promoted the development of telemedicine.
Our study findings show that the sociodemographic characteristics (e.g., age, gender, education, and occupation) had no significant effect on BI, which is similar to the findings of Yousef et al. (25) and Bäuerle et al. (26). However, it is worth noting that the findings indicated that individuals with self-assessed health conditions that severely impacted their lives had a higher adoption intention for telerehabilitation than individuals who were not affected. This may be because individuals with severe self-assessed health conditions have a stronger motivation to rehabilitate, and they are more eager to try this new and effective form of rehabilitation medical service. Meanwhile, individuals with rehabilitation needs are often required to have long-term and continuous rehabilitation medical services, whereas the traditional face-to-face rehabilitation medical services require them to travel frequently between their residence and the hospital, so they are more willing to adopt the convenient telerehabilitation.
The results of the study indicated that the main constructs of UTAUT, PE, and FC significantly influenced the public’s intention to adopt telerehabilitation. Some previous studies that have applied the UTAUT model to identify the important factors influencing the use of telemedicine have also established similar results (27–29). The findings suggested that the individuals’ foremost focus when using telerehabilitation remains on whether telerehabilitation can meet their actual rehabilitation needs. Telerehabilitation has the ability to provide tailored interventions to their needs and preferences, which is important for individuals with rehabilitation needs. FC was categorized into internal and external factors. External factors depend mainly on network conditions, device support, and so on. Internal factors include timely technical support and assistance (14). A key characteristic of telemedicine was the need for an infrastructure to match it. A previous study showed that the recipients of telemedicine were concentrated in urban areas with better infrastructure, while 91–99% of rural areas did not have telemedicine (30). Population groups who have higher needs for healthcare services and have the potential to benefit most from telemedicine are the ones who will encounter the greatest barriers to accessing telemedicine services (31). In other words, the essence of telemedicine is the application of advanced communication technologies in the medical field, so individuals first need to have the infrastructure and technical support of these advanced telecommunication technologies in order to access telerehabilitation rehabilitation medical services. However, our study found that EE and SI had no significant effect on adoption intention for telerehabilitation, which is inconsistent with the findings of some previous studies (21, 32, 33). This may be because with the prolonged use of telecommunication technologies and the improving smart mobile devices and technologies for people, users have become proficient in using applications related to telecommunication technology. This makes the issue of ease of use of telerehabilitation services less problematic. Our opinion gained support from Yuan et al. (34), who stated that the improvements in the ease of use of smartphone interfaces have reduced the difficulties that citizens may encounter when using telemedicine services. In addition, only 19.3% of the surveys in this sample had telerehabilitation experience; in other words, telerehabilitation is not widely used in the surveyed area. Therefore, individuals may not be able to obtain a proper understanding of telerehabilitation from important people around them (family, friends, medical workers, etc.). This may be the reason why SI is not significant in the adoption intention for telerehabilitation.
In addition, our findings revealed that PT and SE had a significant positive effect on the adoption intention for telerehabilitation. This is consistent with the results of Zhu et al. (14) and Mensah et al. (35). Telemedicine is closely related to an individual’s health; when individuals are using the process of telerehabilitation, they should be provided with accurate and reliable professional telerehabilitation medical services to enhance their trust in telerehabilitation and thus promoting the user’s intention to adopt. Absolutely, SE also plays an important role in the adoption of telerehabilitation as individuals seek to access and enjoy quality telerehabilitation medical services.
Limitations
There are several limitations of this study. First, this study is a single-center survey research, and the sample size was not very large, so there may be a sample bias. In addition, only 19.3% of the participants in this survey had experience in the use of telerehabilitation, and most of them may not have a good understanding of telerehabilitation, which may affect the accuracy of the results in this case. Finally, this study only investigated the use intention of telerehabilitation but not the actual usage behavior. Although use intention is a predictor of actual usage, there is an “intention-behavior gap” (36). Therefore, the actual use of telerehabilitation needs to be further examined in future studies.
Conclusion
This study investigated the use intention of telerehabilitation for individuals with rehabilitation needs and potential influencing factors. Our findings indicate that individuals’ overall use intentions for telerehabilitation are high. Health conditions, PE, FC, PT, and SE are important factors influencing the intention to adopt telerehabilitation for individuals with rehabilitation needs. Telerehabilitation is a new model of rehabilitation medicine that can provide long-term and professional rehabilitation medical services for individuals with rehabilitation needs. When promoting the use of telerehabilitation in clinical settings, relevant clinicians or healthcare organizations need to consider the important influencing factors observed. In future, large-scale investigations are still needed to gain a comprehensive understanding of the influencing factors of the intention to use telerehabilitation.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by the Ethics Committee of the First Affiliated Hospital of Gannan Medical University. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
M-YW: Writing – review & editing. HC: Data curation, Methodology, Writing – original draft. CG: Investigation, Project administration, Writing – original draft. X-MP: Writing – original draft. Y-BZ: Writing – original draft. C-MW: Supervision, Writing – review & editing. YL: Writing – review & editing. Y-QW: Data curation, Investigation, Methodology, Writing – original draft.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This study was supported by the Key Research and Development Project of Jiangxi Province (20203BBGL73127) to M-YW.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2023.1274080/full#supplementary-material
References
1. Kamenov, K, Mills, JA, Chatterji, S, and Cieza, A. Needs and unmet needs for rehabilitation services: a scoping review. Disabil Rehabil. (2019) 41:1227–37. doi: 10.1080/09638288.2017.1422036
2. Krug, E, and Cieza, A. Strengthening health systems to provide rehabilitation services. Am J Phys Med Rehabil. (2017) 96:438–9. doi: 10.1097/phm.0000000000000753
3. Fong, JH. Disability incidence and functional decline among older adults with Major chronic diseases. BMC Geriatr. (2019) 19:323. doi: 10.1186/s12877-019-1348-z
4. Bickenbach, J, Rubinelli, S, Sabariego, C, and Stucki, G. The learning rehabilitation system: strengthening an Intersectoral strategy to improve functioning of an ageing population. Heal policy (Amsterdam, Netherlands). (2023) 135:104866. doi: 10.1016/j.healthpol.2023.104866
5. Gimigliano, F, and Negrini, S. The World Health Organization "rehabilitation 2030: a call for action". Eur J Phys Rehabil Med. (2017) 53:155–68. doi: 10.23736/s1973-9087.17.04746-3
6. Guo, X, Huo, J, Dai, W, Wang, Z, Du, J, Zheng, X, et al. Current state and challenges of rehabilitation needs among elderly - China, 1990-2019. China CDC weekly. (2022) 4:871–4. doi: 10.46234/ccdcw2022.180
7. Giesbrecht, E, Major, ME, Fricke, M, Wener, P, van Egmond, M, Aarden, JJ, et al. Telerehabilitation delivery in Canada and the Netherlands: results of a survey study. JMIR Rehab Assistive Technol. (2023) 10:e45448. doi: 10.2196/45448
8. Rabanifar, N, Hoseini, MA, and Abdi, K. Exploring barriers to implementing Telerehabilitation from experiences of managers, policymakers, and providers of rehabilitation Services in Iran: a qualitative study. Med J Islam Repub Iran. (2022) 36:157. doi: 10.47176/mjiri.36.157
9. Nizeyimana, E, Joseph, C, Plastow, N, Dawood, G, and Louw, QA. A scoping review of feasibility, cost, access to rehabilitation services and implementation of Telerehabilitation: implications for low- and middle-income countries. Digital Heal. (2022) 8:20552076221131670. doi: 10.1177/20552076221131670
10. Wu, YQ, Long, Y, Peng, WJ, Gong, C, Liu, YQ, Peng, XM, et al. The efficacy and safety of Telerehabilitation for fibromyalgia: systematic review and Meta-analysis of randomized controlled trials. J Med Internet Res. (2023) 25:e42090. doi: 10.2196/42090
11. Li, L, and Sun, Y. Research hotspots and trends of the tele-rehabilitation for stroke survivors based on Citespace: a review. Medicine. (2023) 102:e33398. doi: 10.1097/md.0000000000033398
12. Venkatesh, V, Morris, MG, Davis, GB, and Davis, FD. User acceptance of information technology: toward a unified view. MIS Q. (2003) 27:425–78. doi: 10.2307/30036540
13. Rouidi, M, Elouadi, A, and Hamdoune, A. Acceptance and use of telemedicine technology by health professionals: development of a conceptual model. Digital Heal. (2022) 8:205520762210816. doi: 10.1177/20552076221081693
14. Zhu, Y, Zhao, Z, Guo, J, Wang, Y, Zhang, C, Zheng, J, et al. Understanding use intention of Mhealth applications based on the unified theory of acceptance and use of technology 2 (Utaut-2) model in China. Int J Environ Res Public Health. (2023) 20:3139. doi: 10.3390/ijerph20043139
15. Shiferaw, KB, Mengiste, SA, Gullslett, MK, Zeleke, AA, Tilahun, B, Tebeje, T, et al. Healthcare Providers' acceptance of telemedicine and preference of modalities during Covid-19 pandemics in a low-resource setting: an extended Utaut model. PloS One. (2021) 16:e0250220. doi: 10.1371/journal.pone.0250220
16. Serrano, KM, Mendes, GHS, Lizarelli, FL, and Ganga, GMD. Assessing the telemedicine acceptance for adults in Brazil. Int J Health Care Qual Assur. (2020) 34:35–51. doi: 10.1108/ijhcqa-06-2020-0098
17. Zhang, Q, Zhang, R, Lu, X, and Zhang, X. What drives the adoption of online health communities? An empirical study from patient-centric perspective. BMC Health Serv Res. (2023) 23:524. doi: 10.1186/s12913-023-09469-6
18. Breil, B, Salewski, C, and Apolinário-Hagen, J. Comparing the acceptance of Mobile hypertension apps for disease management among patients versus clinical use among physicians: cross-sectional survey. JMIR Cardio. (2022) 6:e31617. doi: 10.2196/31617
19. Li, W, Gui, J, Luo, X, Yang, J, Zhang, T, and Tang, Q. Determinants of intention with remote health management service among urban older adults: a unified theory of acceptance and use of technology perspective. Front Public Health. (2023) 11:1117518. doi: 10.3389/fpubh.2023.1117518
20. van Kessel, R, Roman-Urrestarazu, A, Anderson, M, Kyriopoulos, I, Field, S, Monti, G, et al. Mapping factors that affect the uptake of digital therapeutics within health systems: scoping review. J Med Internet Res. (2023) 25:e48000. doi: 10.2196/48000
21. Hennemann, S, Beutel, ME, and Zwerenz, R. Drivers and barriers to acceptance of web-based aftercare of patients in inpatient routine care: a cross-sectional survey. J Med Internet Res. (2016) 18:e337. doi: 10.2196/jmir.6003
23. Baumeister, H, Seifferth, H, Lin, J, Nowoczin, L, Lüking, M, and Ebert, D. Impact of an acceptance facilitating intervention on Patients' acceptance of internet-based pain interventions: a randomized controlled trial. Clin J Pain. (2015) 31:528–35. doi: 10.1097/ajp.0000000000000118
24. Baumeister, H, Nowoczin, L, Lin, J, Seifferth, H, Seufert, J, Laubner, K, et al. Impact of an acceptance facilitating intervention on diabetes Patients' acceptance of internet-based interventions for depression: a randomized controlled trial. Diabetes Res Clin Pract. (2014) 105:30–9. doi: 10.1016/j.diabres.2014.04.031
25. Yousef, CC, Salgado, TM, Farooq, A, Burnett, K, McClelland, LE, Thomas, A, et al. Predicting Patients' intention to use a personal health record using an adapted unified theory of acceptance and use of technology model: secondary data analysis. JMIR Med Inform. (2021) 9:e30214. doi: 10.2196/30214
26. Bäuerle, A, Mallien, C, Rassaf, T, Jahre, L, Rammos, C, Skoda, EM, et al. Determining the acceptance of digital cardiac rehabilitation and its influencing factors among patients affected by cardiac diseases. J Cardiovascular Develop Dis. (2023) 10:174. doi: 10.3390/jcdd10040174
27. Hoque, R, and Sorwar, G. Understanding factors influencing the adoption of Mhealth by the elderly: an extension of the Utaut model. Int J Med Inform. (2017) 101:75–84. doi: 10.1016/j.ijmedinf.2017.02.002
28. Adjei, TK, Mohammed, A, Acheampong, PR, Acquah-Gyan, E, Sylverken, A, Twumasi-Ankrah, S, et al. Determinants of a Mobile phone-based interactive voice response (Mivr) system for monitoring childhood illnesses in a Rural District of Ghana: empirical evidence from the Utaut model. PloS One. (2021) 16:e0248363. doi: 10.1371/journal.pone.0248363
29. Tian, XF, and Wu, RZ. Determinants of the Mobile health continuance intention of elders with chronic diseases: an integrated framework of Ecm-Isc and Utaut. Int J Environ Res Public Health. (2022) 19:9980. doi: 10.3390/ijerph19169980
30. Fast, N, van Kessel, R, Humphreys, K, Ward, NF, and Roman-Urrestarazu, A. The evolution of Telepsychiatry for substance use disorders during Covid-19: a narrative review. Curr Addict Rep. (2023) 10:187–97. doi: 10.1007/s40429-023-00480-9
31. van Kessel, R, Kyriopoulos, I, Wong, BLH, and Mossialos, E. The effect of the Covid-19 pandemic on digital health-seeking behavior: big data interrupted time-series analysis of Google trends. J Med Internet Res. (2023) 25:e42401. doi: 10.2196/42401
32. Rój, J. What determines the acceptance and use of Ehealth by older adults in Poland? Int J Environ Res Public Health. (2022) 19:15643. doi: 10.3390/ijerph192315643
33. Stoppok, P, Teufel, M, Jahre, L, Rometsch, C, Müßgens, D, Bingel, U, et al. Determining the influencing factors on acceptance of Ehealth pain management interventions among patients with chronic pain using the unified theory of acceptance and use of technology: cross-sectional study. JMIR Format Res. (2022) 6:e37682. doi: 10.2196/37682
34. Yuan, S, Ma, W, Kanthawala, S, and Peng, W. Keep using my health apps: discover Users' perception of health and fitness apps with the Utaut2 model. Telemed J e-heal: Official J American Telemed Assoc. (2015) 21:735–41. doi: 10.1089/tmj.2014.0148
35. Mensah, IK, Zeng, G, and Mwakapesa, DS. The behavioral intention to adopt Mobile health services: the moderating impact of Mobile self-efficacy. Front Public Health. (2022) 10:1020474. doi: 10.3389/fpubh.2022.1020474
Keywords: telerehabilitation, UTAUT, use intention, influencing factors, rehabilitation needs
Citation: Wang M-Y, Chen H, Gong C, Peng X-M, Zhong Y-B, Wu C-M, Luo Y and Wu Y-Q (2023) Understanding the use intention and influencing factors of telerehabilitation in people with rehabilitation needs: a cross-sectional survey. Front. Public Health. 11:1274080. doi: 10.3389/fpubh.2023.1274080
Edited by:
Ik-Whan Kwon, Saint Louis University, United StatesReviewed by:
Robin van Kessel, Maastricht University, NetherlandsChang Won Lee, Hanyang University, Republic of Korea
Copyright © 2023 Wang, Chen, Gong, Peng, Zhong, Wu, Luo and Wu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Chun-Mei Wu, d3VjaHVubWVpODJAcXEuY29t; Yun Luo, NzM1MDgzNTY2QHFxLmNvbQ==; Yong-Qiang Wu, Mzg2MzE2Mjc1QHFxLmNvbQ==
†These authors have contributed equally to this work and share first authorship
 Mao-Yuan Wang
Mao-Yuan Wang Hong Chen
Hong Chen Cheng Gong
Cheng Gong Xu-Miao Peng
Xu-Miao Peng Yan-Biao Zhong
Yan-Biao Zhong Chun-Mei Wu
Chun-Mei Wu Yun Luo
Yun Luo Yong-Qiang Wu
Yong-Qiang Wu