
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health , 03 November 2023
Sec. Life-Course Epidemiology and Social Inequalities in Health
Volume 11 - 2023 | https://doi.org/10.3389/fpubh.2023.1265071
This article is part of the Research Topic Delay in Cancer Diagnosis and Factors Affecting Outcomes View all 5 articles
 Sixia Chen1
Sixia Chen1 Shirley A. James1*
Shirley A. James1* Spencer Hall1
Spencer Hall1 Julie H. Dang2
Julie H. Dang2 Janis E. Campbell1
Janis E. Campbell1 Moon S. Chen Jr.2†
Moon S. Chen Jr.2† Mark P. Doescher3†
Mark P. Doescher3†Objectives: Assess the percentage of cancer-related appointment delays, cancelations, and the unavailability of medications experienced by American Indian participants during the COVID-19 pandemic.
Methods: This cross-sectional survey study was completed between October 2020 and July 2021 by 360 individuals with cancer who lived in California and Oklahoma. Binary and multivariate logistic regression analysis was completed in SAS 9.4.
Results: During the initial Covid-19 pandemic, almost one-third (30%) of respondents delayed cancer-related appointments, 42% canceled cancer-related appointments, and one-quarter (24%) were unable to access prescription medications or over-the-counter medications (27%) due to COVID-19. People who underwent testing for COVID-19 were five times more likely to delay a medical appointment [adjusted odds ratio (aOR) = 5.3, 95% CI:2.4, 11.7] and people who followed three or more social distancing measures were more than six times more likely to cancel medical appointments (aOR:6.3, 95% CI:2.9, 13.9).
Conclusion: This study identifies delays, cancelations, and medication inaccessibility people identifying as American Indian faced during the coronavirus pandemic. Disparities in healthcare delivery could contribute to increased morbidity and mortality rates of cancer.
The Coronavirus caused a variety of medical care delays, but perhaps none as critical as in the field of oncology. Additionally, the impact of COVID-19 was especially devastating for members of the American Indian population. Widespread fear of the pandemic and of spreading and contracting COVID-19 before the vaccine was readily available caused patients to avoid crowded places and delay critical cancer screenings (1). Patt and associates, in a study of the impact of the pandemic on senior citizens, reported that when comparing cancer screenings in 2020 to pre-covid levels, screenings decreased between 56 and 85% (2). Other studies have corroborated this finding, and note that screening delays have led to the diagnoses of serious cancer conditions at later disease stages, when they were less responsive to intervention (1–6).
In addition to screening delays, delays occurred around outpatient visits required for evaluation, intervention, and management of cancer (2–4). Inability to be in public because of exposure to COVID-19, fear of crowds due to altered immunity, and clinic staff shortages all contributed to appointment delays and cancelations (1–6). In a systematic review, Riera and associates (3) reported delays in cancer care in 38 categories, with significant decreases in cancer screenings, cancer surgeries, and radiation therapy visits. Furthermore, patients with urgent follow-up ancillary cancer screening appointments were forced to reschedule outpatient visits (3).
Other ancillary areas of cancer care were delayed for patients, resulting in undesirable consequences, including heightened mortality rates (4). Examples include chemotherapy drug delay or discontinuation, radiation or proton therapy delay, and surgical treatment delay (3–7). Many of these delays occurred in higher rates among African American patients, people of Hispanic ethnicity, and members of other racial and ethnic minority groups (8). Drug stores also reported an unprecedented increase in demand for over-the-counter medications used to treat the symptoms of COVID-19, making these medications difficult to obtain and expensive to purchase during the pandemic (9). Pain relieving drugs, nausea medication, and anti-inflammatories are all required to alleviate the symptoms, not only of cancer, but also of cancer intervention including chemotherapy and radiation therapy. Their unavailability made these symptoms unavoidable (9).
While COVID-19 associated disruptions to health care pose a risk to all patients affected by cancer, there was a disproportionate burden on the Black, Hispanic, and American Indian (AI) communities (10–13). The Centers for Disease Control and Prevention report that minority populations experienced disproportionately higher COVID-19 mortality rates when compared to Whites and other races (8). Researchers report that compared with the Black, Latino, and White populations, AI populations have a higher prevalence of socioeconomic and health-related COVID-19 risk factors (14). Moreover, AI individuals are also at higher risk for COVID-19 compared to members of the non-Hispanic White race (15–17).
Because the focus of this study was to report delays in medical care among people reporting AI race, data were collected from California and Oklahoma, two states with large AI populations (18). Data were collected during 2020–2021 and analyzed during 2022–2023. Study aims were to assess the percentage of cancer-related medical appointment delays, cancelations made by patients, unavailability of prescription medications, and unavailability of over-the-counter medications experienced by AI participants with cancer. The secondary aim was to identify factors associated with these delays, cancelations, and shortages.
The “Impact of COVID-19 on the Cancer Continuum Consortium” (IC-4), was established to develop and agree upon a set of core survey questions administered by 17 National Cancer Institute (NCI)-Designated Cancer Centers (Centers) across the U.S. The purpose of this survey was to assess the impact of COVID-19 on cancer prevention, control, and survivorship. This paper reports responses from a subset of survey questions administered by the University of California-Davis, Comprehensive Cancer Center (UCD), and the University of Oklahoma, Stephenson Cancer Center (OUHSC). Both Centers used a cross-sectional, non-probability-based survey design. This study was approved by the University Institutional Review Board (IRB) at each Center; in Oklahoma it was also approved by the Oklahoma City Area Indian Health Service IRB, the Choctaw Nation IRB, and the Cherokee Nation IRB. Each survey participant consented to participate in this study via telephone or by answering the consent question in the written online survey.
This convenience sample included 360 AI adults. The OUHSC sample comprised AI adults diagnosed with cancer who were purposefully recruited through the Oncology Research Information Exchange Network (ORIEN) and the OU Health Sciences Center cancer registry (n = 328). The UCD utilized two partnering tribal health centers to recruit and administer the survey (n = 32). Data were collected between October 2020 and July 2021. Staff administered the 20-min surveys online, through phone interviews, and in person. Participants received gift cards as partial compensation for their time.
Sociodemographic questions included Hispanic ethnicity (yes; no), sex (female; male), age group (18–39; 40–59; ≥60), rural vs. urban setting, marital status (single and never married; married or living together; separated, divorced or widowed), educational attainment (any post-secondary education; high school education/GED or less), income level (< $35,000; ≥ $35,000), minors residing in household (yes; no), health status (good; poor), pre-existing medical conditions other than cancer (zero; one; two; three or more), employment status before COVID-19 (full or part-time employment; unemployed or other occupation), household financial situation (have enough or more than enough; cutting back or never enough), health insurance status (yes; no), tested for COVID-19 (yes; no), time of the survey (October 2020–January 2021, February–April 2021 or May–July, 2021), number of social distancing measures followed during the pandemic (0–2; 3 or more) (social distancing measures given for participants to “check off” included wearing a face mask in public, maintaining six feet of distance between yourself and others, avoiding crowded public places, working from home instead of the office, attending conferences or large meetings online, and not inviting relatives, friends or neighbors into your home, and “other”), past 30-day close physical contact with a person who tested positive for COVID-19 (yes; no), attendance at gatherings of two or more people not living with, or regularly associated with you during the pandemic (yes; no), importance of social distancing during the pandemic (very or somewhat; a little or not), frequency of support during the pandemic (frequent; not supported).
Four dependent variables were included in the survey. Each dependent variable was independent of each other and was binary (yes; no) in nature; “Have you ever delayed a cancer-related appointment due to the pandemic?” “Have you canceled a clinic, doctor, or outpatient cancer-related medical appointment to avoid being around others due to the pandemic?” “Have you been unable to access cancer-related prescription medications due to the pandemic?” and “Have you been unable to access over-the-counter medications due to the pandemic?”
Descriptive statistics were calculated for each categorical variable. Binary associations between covariate variables and outcome were examined using the chi-square test or Fisher’s exact test when cell counts were less than five. Multivariable logistic regression was conducted, analyzing the associations between each outcome variable and the series of independent variables. Binary logistic regression modeling was first used to select the set of significant predictors for each outcome variable. After that, collinearity and interactions were examined among the selected set of significant predictors in building the final model. A stepwise model-selection procedure was used to select the final model. Tables 1, 2 present the independent variables included in the final model for each outcome variable. Adjusted odds ratios were obtained for the association between dependent (i.e., outcome) variables and independent (i.e., “predictor”) variables. Respondents with missing outcome values and predictors were excluded from bivariate and multivariate analysis. All statistical analyses were conducted using SAS® 9.4 (19) with an alpha = 0.05.
This sample consisted of 360 AI adults with a history of cancer. More participants were female (60%), were over 59 years (38%), lived in an urban setting (61%), were married (61%), had a post-secondary education (73%), had a household income level of $35,000 or above (63%), had no minors in the household (59%), reported being in good health (61%), and reported having three or more pre-existing medical conditions other than cancer (43%). Additionally, most were employed prior to the pandemic (56%), felt that they were financially stable (71%), and were covered by health insurance or a health plan (81%). At the time of the survey, most respondents had received testing for COVID-19 (73%), taking the survey May–July 2021 (58%), that is, at a time when the vaccine was widely available, followed three or more social distancing measures (81%), and had not had past 30-day close physical contact with a person who had tested positive for COVID-19 (74%) (Table 1).
Almost one third (30%) of participants had a delay in a cancer-related medical appointment. Binary analysis revealed males (55%) were more likely than females to experience a delay in their cancer-related appointments (p = 0.0001), as were those in the 18–39-year age group (49%, p < 0.0001). Participants who had received COVID-19 testing (93%) were also more likely to experience a delay in a cancer-related medical appointment (p < 0.0001) (Table 2).
Many participants (42%) canceled a clinic, doctor, or dental appointment to avoid being around others because of COVID-19. Binary analysis revealed that participants in the 18–39 year age group (42%, p = 0.0003), who took the survey May–July 2021 (65%, p = 0.0121), and who followed three or more social distancing measures (92%, p = 0.0001) were more likely to cancel a medical or dental appointment to avoid being around others because of COVID-19 (Table 2).
Respondents also had difficulty getting prescription medications related to cancer (24%), as well as over the counter medications (27%). Binary analysis revealed AI participants in the 18–39-year age group (58%, p < 0.0001), with past 30-day close physical contact with a person who tested positive for COVID-19 (51%, p < 0.0001) and who took the survey May–July 2021 (83%, p < 0.0001) were more likely to have had difficulty obtaining prescription medications because of the pandemic (Table 2). Respondents aged 18–39 years (51%, p < 0.0001), who took the survey May–July 2021 (79%, p < 0.0001), and who had close physical contact within the past 30-days with someone who had tested positive for the coronavirus (51%, p < 0.0001) were more likely to have had difficulty obtaining over-the-counter medications because of the pandemic (Table 2).
Multivariate analysis revealed that after adjusting for other variables in the model, the odds of having an appointment delayed due to the pandemic were higher for those 18–39 years compared to those aged 60 years or older (aOR:2.6, 95% CI:1.4, 4.9), and were higher for those aged 40–59 years compared to those aged 60 years or older (aOR:2.1, 95% CI:1.1, 4.1). Additionally, the odds of a male having an appointment delayed due to the pandemic were higher than those of a female (aOR:2.2, 95% CI:1.3, 3.6) and odds were higher for those who received testing for COVID-19 than for those who did not (aOR:5.0, 95% CI:2.4, 11.7) (Table 3).
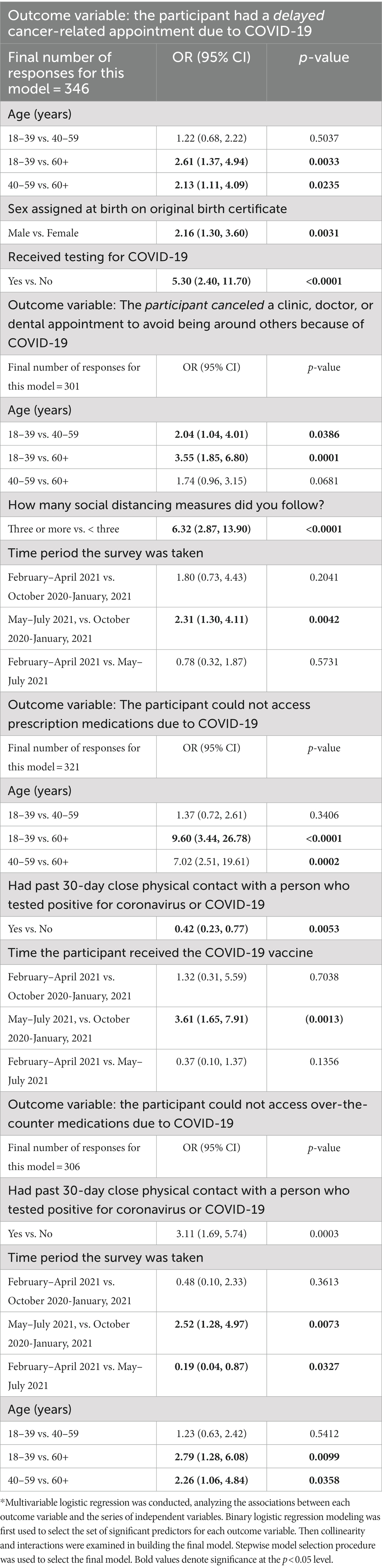
Table 3. Multivariate regression with predictors of cancer related appointment delays, participant cancelation of appointments, inaccessibility of prescription medications, and Inaccessibility of over-the-counter medications (n = 360)*.
Multivariate analysis revealed that after adjusting for other variables in the model, the odds of a participant canceling an appointment to avoid being around others because of COVID-19 were higher for those 18–39 years compared to those 40–59 years (aOR:2.0, 95% CI:1.0, 4.0), and for those 18–39 years compared to those aged 60 years or older (aOR:3.6, 95% CI:1.9, 6.8). The odds of a participant who followed three or more social distancing precautions canceling an appointment to avoid being around others because of COVID-19 were higher than those who followed fewer than three social distancing precautions (aOR:6.3, 95% CI:2.9, 13.9), as well as for those who took the survey May–July 2021 compared to those who took the survey October 2020–January 2021 (aOR:2.31, 95% CI:1.3, 4.1) (Table 3).
Multivariate analysis revealed that after adjusting for other variables in the model, the odds of having difficulty obtaining prescription medications during the pandemic were higher for those 18–39 years compared to those who were 60 years or older (aOR:9.6, 95% CI = 3.4, 26.8), were higher for those who took the survey May–July 2021 compared to those taking the survey October 2020-Jaunary 2021 (aOR:3.6, 95% CI:1.7, 7.9) and were lower for those who had past 30-day close physical contact with a person who tested positive for COVID-19 compared to those who did not (aOR:0.4, 95% CI = 0.2, 0.8) (Table 3).
Multivariate analysis revealed that after adjusting for other variables in the model, the odds of having difficulty obtaining over-the-counter medications during the pandemic were higher for those who had 30-day contact with a person who tested positive for the coronavirus compared to those who did not (aOR:3.1, 95% CI = 1.7, 5.7), and for those who took the survey May–July 2021 compared to those who took the survey October 2020–January 2021 (aOR:2.5, 95% CI:1.3, 5.0). However, the odds were lower for those who took the survey from February to April 2021 compared to those who took the survey from May to July 2021 (aOR:0.2, 95% CI:0.04, 0.9). Finally, the odds of having difficulty obtaining prescription medications during the pandemic were higher for those 18–39 years compared to those aged 60 years or older (aOR:2.8, 95% CI = 1.3, 6.1), and for those 40–59 years compared to those aged 60 years or older (aOR:2.3, 95% CI:1.1, 4.8) (Table 3).
In this survey of American Indian participants with a history of cancer, almost one-third delayed a cancer-related appointment, 42% canceled a clinic, doctor, or dental appointment to avoid being around others due to COVID-19, and about one-quarter were unable to access prescription or over-the-counter medications due to the COVID-19 pandemic. As other studies have suggested, these delays, cancelations, and inaccessibility of medications could all contribute to long-term heightened morbidity and mortality from cancer resulting from the pandemic (2–6). California and Oklahoma are among states with the largest number of AIs (18). Our ability to collect data on a sizable number of AI individuals from these states helps to fill a gap in the collection of data on AI populations that national surveys are typically forced to avoid or neglect due to small numbers (10–13).
In this study, the most significant factor associated with a cancer-related appointment delay was being tested for COVID-19. After adjusting for both age and sex, individuals who were tested for COVID-19 were five times more likely to experience appointment delays. These results are like those discussed by Riera and associates (3); participants in their study who tested positive for COVID-19 were forced to wait for care until they tested negative, or until the isolation period passed. This study separated delays in medical care from cancelations, different from other studies that have only reported cancelations (2–6), a factor unique and important in the study of COVID-19.
Additionally, in this study more than two out of five individuals with a history of cancer canceled a clinic, doctor, or dental appointment to avoid being around others (2–6). Not surprisingly, these participants, who exercised enough caution to follow three or more social distancing precautions, were more than six times more likely to cancel one or more doctor appointments. While this finding characterizing AI participants has not been reported in the literature, this observation aligns well with several studies suggesting that social distancing during the COVID-19 pandemic was especially important for patients with chronic conditions including cancer (10–13, 15, 17). One study suggested fear of contracting COVID-19 may be at least partially responsible, particularly in patients with cancer (1).
This fear is warranted. Compared to other racial groups, the American Indian population has experienced the highest morbidity and mortality rates from COVID-19 (20–25). Musshafen et al. (15), in a study of American Indian people in Mississippi, found that the probability of death for those with the highest number of comorbidity risk factors was 69% in the AI, compared with 28% in the Black, and 25% in the non-Hispanic White population (15, 16).
Participants in our study also had difficulty obtaining prescription drugs related to their cancer intervention, as well as over-the counter medications required for physical symptoms resulting from cancer, cancer intervention, or minor medical conditions. Findings from our study were similar to others reporting chemotherapy drug delay or discontinuation because of the pandemic (7), which occurred more frequently among minorities (7). Additionally, in a survey of 68 members of the US hematology/oncology pharmacy association, 63% reported one or more chemotherapy drug shortages during the pandemic. Three quarters (75%) of the pharmacists in the study reported the need to delay chemotherapy treatment, reduce dosage, or use alternative drug regimens during the pandemic (7). Over-the-counter medications used to treat the symptoms of COVID-19 were also difficult to obtain. Drug stores reported an unprecedented increase in demand, making the most basic cold, flu, and anti-inflammatory medications difficult to obtain and expensive to purchase during the pandemic, particularly among underserved populations (9).
COVID-19 placed an immediate burden on AI communities in terms of mortality and morbidity (15–18) exacerbated by appointment delays and cancelations (1–4). One study suggests that these delays were present prior to the pandemic, although not within a subset of the population who also had a diagnosis of cancer. In 2016, Shimotsu and associates reported the odds of missed appointments were 1.8 times higher for Black/African Americans and two times higher for American Indian/Alaskan Natives and Hispanic/Latinos when compared with White non-Hispanic patients (26).
While the reasons for heightened morbidity and mortality during COVID-19 is beyond the scope of this study, accessing quality health care is difficult for people who are a part of the American Indian population, despite provision of partial health care service from the Indian Health Service (10). American Indians living within reservations often experience crowded, multigenerational, and poverty-stricken housing conditions, food insecurity, poor or no health insurance, and low incomes (10, 26). Many are employed in front-line occupations, making them more at risk of exposures (10). A clear understanding behind the reasons for gaps in quality health care for the AI population is important for preventing the heightened COVID-19 morbidity and mortality that occurred in this population from recurring.
This study was a convenience, cross-sectional sample in which participants’ self-reported appointment delays, cancelations, and inability to access medications. There is potential for reporting bias and non-response bias. While we collected information about the nature of missed appointments, these are not reported due to small numbers in each category. Analysis revealed that all were cancer-related appointments. Participants in the study were in various stages of cancer intervention, from new diagnoses to those requiring appointments to assess potential recurrence. Stratification by stage of intervention was also not possible due to low numbers in each category.
A control group consisting of cancer patients of other racial and ethnic groups would have allowed stratification by race, allowing us to confirm the existence of disparities in care. Conversely, a control group of patients with diagnoses other than cancer would have allowed us to stratify by diagnosis and determine whether cancer patients were treated differently or behaved differently than those with other diagnoses. These items are important for future study investigators who are forced to respond quickly to pandemic situations.
Finally, because this sample consisted of individuals with cancer recruited through the Oncology Research Information Exchange Network (ORIEN) and the OU Health Sciences Center cancer registry, as opposed to a random sample of the American Indian population, it does not represent the Choctaw or the Cherokee Nation (CN) populations accurately. Those populations are largely rural, live in a higher level of poverty, and with far less education than that reflected in Table 1. Their challenges in accessing health care are far greater than this sample of patients already receiving intervention for cancer actually reflects. Despite these limitations, this study had several strengths. First, this is the largest study to investigate the influence of Covid-19 on delays in medical care among AI adults with cancer, specifically associated with the Covid-19 pandemic. Second, the survey questions queried delays or postponements in medical care separately from the cancelations. Third, the delays and cancelations reported in this study were initiated by the patient and not by the medical clinic. This provides a clearer picture of the impact of the virus on the patients receiving healthcare during the pandemic, as opposed to clinic-related shortages.
COVID-19 placed an immediate burden on AI communities in terms of mortality and morbidity (15–18) exacerbated by appointment delays and cancelations (1–4). While we hope to never experience another pandemic, lessons learned suggest that we must overcome institutional barriers causing treatment delays and explore alternative options such as telehealth visits to ensure continuation of care, especially to those vulnerable to racial disparity.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving humans were approved by the University of Oklahoma Health Sciences Center IRB, University of California-Davis IRB, Oklahoma City Area Indian Health Service IRB, the Choctaw Nation IRB and the Cherokee Nation IRB. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
SC: Writing – review & editing, Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration. SJ: Writing – review & editing, Writing – original draft. SH: Data curation, Formal analysis, Writing – review & editing. JD: Conceptualization, Methodology, Supervision, Validation, Writing – review & editing. JC: Conceptualization, Investigation, Methodology, Supervision, Writing – review & editing. MC: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Supervision, Validation, Visualization, Writing – review & editing. MD: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Supervision, Validation, Visualization, Writing – review & editing.
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This project was supported by grants P30CA225520 and P30CA093373 from the National Institute of Health. JD was funded by the National Institute of Health, Building Interdisciplinary Research Careers in Women’s Health at UC Davis through Grant Number: 5K12HD051958–17. SC was partially supported by grant P30CA225520 from the National Institutes of Health and the Oklahoma Shared Clinical and Translational Resources (U54GM104938) with an Institutional Development Award (IDeA) from NIGMS.
We would like to acknowledge our tribal and community partners: Northern Valley Indian Health, Feather River Tribal Health, Choctaw Nation of Oklahoma, and Cherokee Nation of Oklahoma. The content is the sole responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Erdoğan, AP, Ekinci, F, Acar, Ö, and Göksel, G. Level of COVID-19 fear in cancer patients. Middle East Curr Psychiatry. (2022) 29:9. doi: 10.1186/s43045-022-00181-5
2. Patt, D, Gordan, L, Diaz, M, Okon, T, Grady, L, Harmison, M, et al. Impact of COVID-19 on cancer care: how the pandemic is delaying cancer diagnosis and treatment for American seniors. JCO Clin Cancer Inform. (2020) 4:1059–71. doi: 10.1200/CCI.20.00134.33253013
3. Riera, R, Bagattini, ÂM, Pacheco, RL, Pachito, DV, Roitberg, F, and Ilbawi, A. Delays and disruptions in cancer health care due to COVID-19 pandemic: systematic review. JCO Glob Oncol. (2021) 7:311–23. doi: 10.1200/GO.20.00639.33617304
4. Mullangi, S, Aviki, EM, Chen, Y, Robson, M, and Hershman, DL. Factors associated with Cancer treatment delay among patients diagnosed with COVID-19. JAMA Netw Open. (2022) 5:e2224296. doi: 10.1001/jamanetworkopen.2022.24296
5. Rucinska, M, and Nawrocki, S. COVID-19 pandemic: impact on cancer patients. Int J Environ Res Public Health. (2022) 19:12470. doi: 10.3390/ijerph191912470.36231769
6. Wenger, NS, Stanton, AL, Baxter-King, R, Sepucha, K, Vavreck, L, and Naeim, A. The impact of COVID-19 on routine medical care and cancer screening. J Gen Intern Med. (2022) 37:1450–6. doi: 10.1007/s11606-021-07254-x
7. McBride, A, Hudson-DiSalle, S, Pilz, J, Hamm, M, Boring, B, Buie, LW, et al. National survey on the effect of oncology drug shortages in clinical practice: a hematology oncology pharmacy association survey. JCO Oncol Pract. (2022) 18:e1289–96. doi: 10.1200/OP.21.00883
8. CDC Available at: https://www.cdc.gov/nchs/nvss/vsrr/covid19/health_disparities.htm
9. Badreldin, HA, and Atallah, B. Global drug shortages due to COVID-19: impact on patient care and mitigation strategies. Res Social Adm Pharm. (2021) 17:1946–9. doi: 10.1016/j.sapharm.2020.05.017
10. Wang, Q, Berger, NA, and Xu, R. Analyses of risk, racial disparity, and outcomes among US patients with cancer and COVID-19 infection. JAMA Oncol. (2021) 7:220–7. doi: 10.1001/jamaoncol.2020.6178
11. Schmidt, AL, Bakouny, Z, Bhalla, S, Steinharter, JA, Tremblay, DA, Awad, MM, et al. Cancer care disparities during the COVID-19 pandemic: COVID-19 and cancer outcomes study. Cancer Cell. (2020) 38:769–70. doi: 10.1016/j.ccell.2020.10.023
12. Llanos, AAM, Ashrafi, A, Ghosh, N, Tsui, J, Lin, Y, Fong, AJ, et al. Evaluation of inequities in cancer treatment delay or discontinuation following SARS-CoV-2 infection. JAMA Netw Open. (2023) 6:e2251165. doi: 10.1001/jamanetworkopen.2022.51165
13. Zavala, VA, Bracci, PM, Carethers, JM, Carvajal-Carmona, L, Coggins, NB, Cruz-Correa, MR, et al. Cancer health disparities in racial/ethnic minorities in the United States. Br J Cancer. (2021) 124:315–32. doi: 10.1038/s41416-020-01038-6
14. Hathaway, ED. American Indian and Alaska native people: social vulnerability and COVID-19. J Rural Health. (2021) 37:256–9. doi: 10.1111/jrh.12505
15. Musshafen, LA, El-Sadek, L, Lirette, ST, Summers, RL, Compretta, C, and Dobbs, TE 3rd. In-hospital mortality disparities among American Indian and Alaska native, black, and white patients with COVID-19. JAMA Netw Open. (2022) 5:e224822. doi: 10.1001/jamanetworkopen.2022.4822
16. Leggat-Barr, K, Uchikoshi, F, and Goldman, N. COVID-19 risk factors and mortality among native Americans. Demogr Res. (2021) 45:1185–218. doi: 10.4054/DemRes.2021.45.39
17. Gross, CP, Essien, UR, Pasha, S, Gross, JR, Wang, SY, and Nunez-Smith, M. Racial and ethnic disparities in population-level COVID-19 mortality. J Gen Intern Med. (2020) 35:3097–9. doi: 10.1007/s11606-020-06081-w
18. U.S. Census Bureau (2022). American community survey. 2021: ACS 1-year estimates selected population profiles, table 20201. Available at: https://data.census.gov/cedsci/table?q=S0201&t=009&g=0100000US%240400000_0400000US06&tid=ACSSPP1Y2021.S0201 (Accessed November 3, 2022).
19. SAS Institute Inc. SAS/ACCESS® 9.4 Interface to ADABAS: reference. Cary, NC: SAS Institute Inc. (2013).
20. Parolin, Z, and Lee, EK. The role of poverty and racial discrimination in exacerbating the health consequences of COVID-19. Lancet Reg Health Am. (2022) 7:100178. doi: 10.1016/j.lana.2021.100178
21. Boserup, B, McKenney, M, and Elkbuli, A. Disproportionate impact of COVID-19 pandemic on racial and ethnic minorities. Am Surg. (2020) 86:1615–22. doi: 10.1177/0003134820973356
22. Hatcher, SM, Agnew-Brune, C, Anderson, M, Zambrano, LD, Rose, CE, Jim, MA, et al. COVID-19 among American Indian and Alaska native persons - 23 states, January 31-July 3, 2020. MMWR Morb Mortal Wkly Rep. (2020) 69:1166–9. doi: 10.15585/mmwr.mm6934e1
23. Owen, MJ, Sundberg, MA, Dionne, J, and Kosobuski, AW. The impact of COVID-19 on American ‘Indian and Alaska native communities: a call for better relational models. Am J Public Health. (2021) 111:801–3. doi: 10.2105/AJPH.2021.306219
24. Williamson, LL, Harwell, TS, Koch, TM, Anderson, SL, Scott, MK, Murphy, JS, et al. COVID-19 incidence and mortality among American Indian/Alaska native and white persons - Montana, march 13-November 30, 2020. MMWR Morb Mortal Wkly Rep. (2021) 70:510–3. doi: 10.15585/mmwr.mm7014a2
25. Acquati, C, Chen, TA, Martinez Leal, I, Connors, SK, Haq, AA, Rogova, A, et al. The impact of the COVID-19 pandemic on cancer care and health-related quality of life of non-Hispanic black/African American, Hispanic/Latina and non-Hispanic white women diagnosed with breast cancer in the US: a mixed-methods study protocol. Int J Environ Res Public Health. (2021) 18:13084. doi: 10.3390/ijerph182413084
Keywords: COVID-19, coronavirus, American Indian, medical delays, appointment cancelations, cancer, disparities
Citation: Chen S, James SA, Hall S, Dang JH, Campbell JE, Chen MS Jr and Doescher MP (2023) Avoidance of medical care among American Indians with a history of cancer during the coronavirus pandemic. Front. Public Health. 11:1265071. doi: 10.3389/fpubh.2023.1265071
Received: 21 July 2023; Accepted: 23 October 2023;
Published: 03 November 2023.
Edited by:
Sara Haddadi, University of Miami, United StatesReviewed by:
Valentina Possenti, National Institute of Health (ISS), ItalyCopyright © 2023 Chen, James, Hall, Dang, Campbell, Chen and Doescher. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Shirley A. James, c2hpcmxleS1qYW1lc0BvdWhzYy5lZHU=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.