
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health , 06 October 2023
Sec. Public Mental Health
Volume 11 - 2023 | https://doi.org/10.3389/fpubh.2023.1257943
This article is part of the Research Topic Community Series in Mental Illness, Culture, and Society: Dealing with the COVID-19 Pandemic, volume VIII View all 63 articles
 Jian Liu1†
Jian Liu1† Tong Leong Si2,3†
Tong Leong Si2,3† Pan Chen2,3†
Pan Chen2,3† Yue-Ying Wang3
Yue-Ying Wang3 Zhaohui Su4
Zhaohui Su4 Teris Cheung5
Teris Cheung5 Todd Jackson6
Todd Jackson6 Yu-Tao Xiang2,3*
Yu-Tao Xiang2,3* Yuan Feng7*
Yuan Feng7*Background: In December 2022, China terminated its dynamic zero-COVID policy. To date, however, no research has been conducted upon mental health issues and their relationship with quality of life (hereafter QoL) among fire service recruits since the dynamic zero-COVID policy ended. This study explored fear of COVID-19 (FOC) prevalence and correlates as well as its network structure and interconnections with QoL among fire service recruits.
Methods: A cross-sectional survey design was used to assess fire service recruits in Beijing and Sichuan, Guangxi and Guizhou provinces of China between February 13 and 16, 2023. Fear of COVID-19 was measured using the Fear of COVID-19 Scale, depression was assessed with the Patient Health Questionnaire, anxiety was examined using the Generalized Anxiety Disorder scale, and QOL was evaluated with the World Health Organization Quality of Life-brief version. Univariate and multivariate analyses were used to explore correlates of COVID-19 fear. Network analysis assessed the structure of fear of COVID-19 and its associations with QoL.
Results: A total of 1,560 participants were included in this study. The overall prevalence of fear of COVID-19 was 38.85% (n = 606; 95% CI = 36.42–41.32%). Being afraid of COVID-19 was significantly related to depression (OR = 1.084; p < O.OO1) and physical fatigue (OR = 1.063; p = 0.026). Fire service recruits with more fear of COVID-19 had lower QOL (F = 18.061 p < 0.001) than those with less fear of COVID-19 did. The most central symptoms included FOC6 (“Sleep difficulties caused by worry about COVID-19”), FOC7 (“Palpitations when thinking about COVID-19”) and FOC2 (“Uncomfortable to think about COVID-19”). The top three symptoms negatively associated with QoL were FOC4 (“Afraid of losing life because of COVID-19”), FOC6 (“Sleep difficulties caused by worry about COVID-19”) and FOC2 (“Uncomfortable to think about COVID-19”).
Conclusion: Over one-third of fire service recruits reported fear of COVID-19 after China’s dynamic zero-COVID policy had terminated. Poorer QoL was related to fear of COVID-19. Targeting core symptoms of the fear network structure could help improve the physical and mental health of fire service recruits during public health crises.
In late January 2020, the COVID-19 outbreak rapidly spread, causing global concern (1). China lifted its almost three-year dynamic zero-COVID policy in December 2022, leaving Omicron variants in wide circulation across the country (2). Thereafter, rapid spread of the virus led to increased mental health problems among many people due to fear of getting sick, social isolation and economic uncertainty as well as reduced quality of life (QoL) (3). In addition, lockdowns and other pandemic control measures have resulted in widespread job losses, business closures, and economic hardship for many individuals and communities (4).
Fire service recruits are individuals who receive specialized training to acquire skills and competencies required by the fire service (5). According to relevant regulations and policies in China, the national comprehensive fire and rescue team is open to the community and new entry firefighters are required to participate in a one-year induction training program. If recruits fail the training and assessment, they will be dismissed (6). Fire service recruits undergo technical and operational training as well as training in mental health and stress management (7). The mental health of firefighters has been subject to significant challenges during and following the pandemic. In response to the pandemic, the Chinese government implemented policies and measures to combat COVID-19. As a result, training for fire service recruits occurred within specific premises, from which they were not permitted to leave freely, increased risk of loneliness, depression and fear were possible consequences of this policy (8, 9). Therefore, understanding mental health problems of fire service recruits could help to reduce distress and promote mental well-being for this population.
Fear, an emotion associated with physiological arousal and emotional avoidance of specific stimuli, is linked to clinical phobias and anxiety disorders when expressed in extreme form (10). Previous research (11) estimated the prevalence of fear of COVID-19 was 18, 19, and 33.7% in general population samples from Bosnia and Herzegovina (12), Brazil (13), and Lebanon (14), respectively. Potential widespread public fear brought on by the COVID-19 pandemic could result in severe emotional distress and a variety of coping responses to perceived dangers of infectious disease (15). Moreover, chronic fear can be emotionally exhausting, leading to feelings of helplessness and hopelessness that are characteristic of depression (16, 17). Prolonged activation of stress responses associated with fear and anxiety can also contribute to disruptions in the regulation of stress hormones and affect brain regions involved in mood regulation (18). Other research has found significant associations between higher fear of COVID-19 levels and perceived job insecurity, decreased job satisfaction and poor quality of life (QoL) (19).
Network analysis has emerged as a novel approach to conceptualizing psychological phenomena including fear of COVID-19 (20). Core concepts of network analysis include nodes, that reflect individual symptoms, and edges that represent associations between symptoms (21). Based on network theory, psychological disorders or syndromes can be viewed as networks of interacting symptoms (20). Network models can help to elucidate the most central nodes in a network structure as well as the edges that reflect the strongest relationships between symptoms; such central symptoms serve as plausible targets for prevention or intervention (22).
Network analysis has been applied to numerous mental disorders in samples of the general population (23), adolescents (24), older adults (25), nurses (26), and firefighters (27) during the COVID-19 pandemic. Due to the nature of their work, fire service recruits must learn how to deal with various emergencies including public health crises such as virus outbreaks. Therefore, fire service recruits may be more prone to fear of emergent viruses including COVID-19 compared to the general population. However, to date, no network model of fear of COVID-19 has been evaluated among fire service recruits during or after any virus pandemic, although understanding the pattern of fear and its network structure is important for developing effective psychosocial interventions for those confronted with ongoing and future virus outbreaks.
This study examined the prevalence and correlates of fear of COVID-19 among fire service recruits following the cessation of China’s dynamic zero-COVID policy. In addition, we explored the network structure of COVID-19 fear and identified symptoms having the strongest relationships with QoL.
This cross-sectional study was carried out during February 13–16, 2023. Due to risk of contagion and a continuing closed management policy for fire service recruits (8), face-to-face interviews were not conducted in this study. Following other published studies (28, 29), self-report survey data were collected using the WeChat-embedded “Questionnaire Star” software program which is widely used in survey research. Study invitation and data collection forms were linked to a Quick Response code (QR code) that was distributed to all fire service recruits who attended training courses in Beijing (North China) and Sichuan (Southwest China), Guangxi (South China) and Guizhou (Southwest China) provinces via a major social media platform (WeChat) during the study period. Fire service recruits were required to report their health status during the COVID-19 pandemic; therefore, all recruits used WeChat. Fire service recruits who fulfilled the following criteria were included in this study: (1) adult age (18 years or older), (2) ability to speak and understand Chinese, and (3) status as a fire service recruit during the pandemic. Electronic written informed consent was provided by participants on a voluntary and confidential basis. The ethics committee of China Emergency General Hospital approved the study protocol.
Socio-demographic information was collected. Perceived physical pain and physical fatigue present in the current COVID-19 wave were recorded using self-reported Numeric Rating Scales (NRS) comprising horizontal lines marked with integers from 0 to 10, with “0” and “10” representing “no suffering” and “unbearable suffering,” respectively. NRS are reliable tools for evaluating severity of pain and fatigue (30).
Fear of COVID-19 was measured by the seven-item, self-report Fear of COVID-19 Scale (FCV-19S) (11). The FCV-19 Scale was originally published in English but has been translated and validated in many countries and areas (31), including China (32). FCV-19S items comprise both a physical dimension (i.e., FOC3: Clammy when think about COVID-19; FOC6: Sleep difficulties caused by worry about COVID-19; FOC7: Palpitations when thinking about COVID-19) and a psychological dimension (FOC1: Afraid of COVID-19; FOC2: Uncomfortable to think about COVID-19; FOC4: Afraid of losing life because of COVID-19; FOC5: Nervous when watching news about COVID-19) (33). Each item was rated from 1 (“Strongly Disagree”) to 5 (“Strongly Agree”), with the total scores ranging from 7 to 35. Following previous research (32), we adopted a FCV-19S cut-off value of 16. Hence, participants with a FCV-19S total score of ≥16 were classified as “those with fear of COVID-19,” while those with a FCV-19S total score of <16 were classified as “those with less fear of COVID-19.”
Depression was measured with the nine-item Patient Health Questionnaire (PHQ-9) (34), a self-report measure of depression; items were rated on a 4-point frequency scale and total scores ranged between 0 and 27. Self-reported anxiety was assessed using the seven-item Generalized Anxiety Disorder scale (GAD-7) (35). Each GAD-7 item was rated from 0 (not at all) to 3 (nearly every day); total scores range from 0 to 21. Following previous research (28), the sum of the first two items of another self-report scale, the World Health Organization Quality of Life-brief version (WHOQOL-BREF) (36), was used to measure global quality of life (QoL). Higher total scores reflected better QoL.
Data analyses were performed using R software (37). Differences in socio-demographic and clinical characteristics of participants “with fear of COVID-19” versus those with “low fear of COVID-19” were assessed using univariate analyses. QoL differences between these subgroups were compared using analysis of covariance (ANCOVA) after controlling for other significant differences identified from univariate analysis. Factors independently associated with fear of COVID-19 status were examined using a binary logistic regression analysis with “Enter” method. The significance level was set at p < 0.05 for all tests (two-tailed).
Estimation and visualization of the fear of COVID-19 network model were conducted with R-packages “qgraph” (21), “bootnet” (38), the least absolute shrinkage and selection operator (LASSO) and extended Bayesian information criteria (EBIC) (38). Node relationships in green color reflected positive correlations while red color edges reflected negative correlations. To examine the most central nodes, Expected Influence (EI) was adopted as a centrality index (39). R package “mgm” (40) estimated the predictability of each node. Individual fear of COVID-19 symptoms that were directly related to QoL were identified using the “flow” function in R package “qgraph” (21). In addition, 1,000 case-dropping bootstraps were used to estimate stability of the network model, which was graphically represented by calculating the correlation stability coefficient (CS-C).
Of the 1,564 fire service recruits invited to participate, 1,560 (99.74%) met the study selection criteria and were included in analyses. The sample comprised men only with 874 (56.03%) reporting an education level of undergraduate/college degree or above.
The overall prevalence of fear of COVID-19 (FCV-19S total score ≥ 16) was 38.85% (n = 606; 95% CI = 36.42–41.32%). The fear of COVID-19 mean score for fire service recruits also approached this cut-off (M = 14.52) (SD = 5.64). Table 1 presents demographic data of participants.
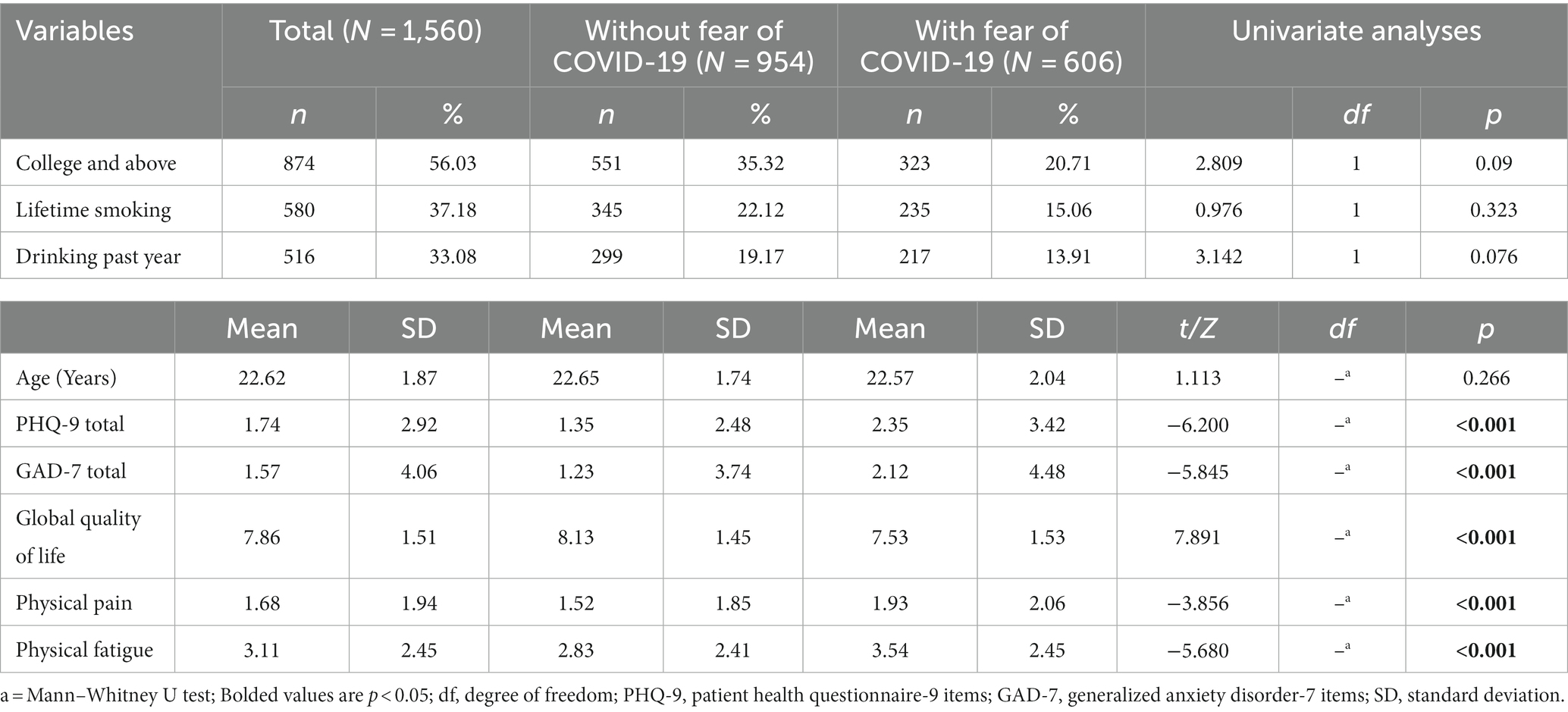
Table 1. Comparison of demographic and clinical characteristics between fire service recruits with fear of COVID-19 and those with no fear of COVID-19.
Univariable analyses revealed a statistical trend indicating fire service recruits with fear of COVID-19 were more likely to have a college or above degree (p = 0.09). Compared with those who reported lower fear of COVID-19, fire service recruits with fear of COVID-19 had higher mean total PHQ-9 (p < 0.001), GAD-7 (p < 0.001) perceived physical pain (p < 0.001) and perceived physical fatigue (p < 0.001) scores in addition to a lower average QoL rating (p < 0.001). An ANCOVA found a significantly lower mean QOL score for fire service recruits with fear of COVID-19 compared to those with lower fear of COVID-19 (F = 18.061 p < 0.001), even after controlling for other significant differences identified from univariate analysis. A binary logistic regression analysis revealed that participants with fear of COVID-19 also reported comparatively more severe depressive symptoms (OR = 1.084; p < 0.001) and fatigue (OR = 1.063; p = 0.026) (Table 2).
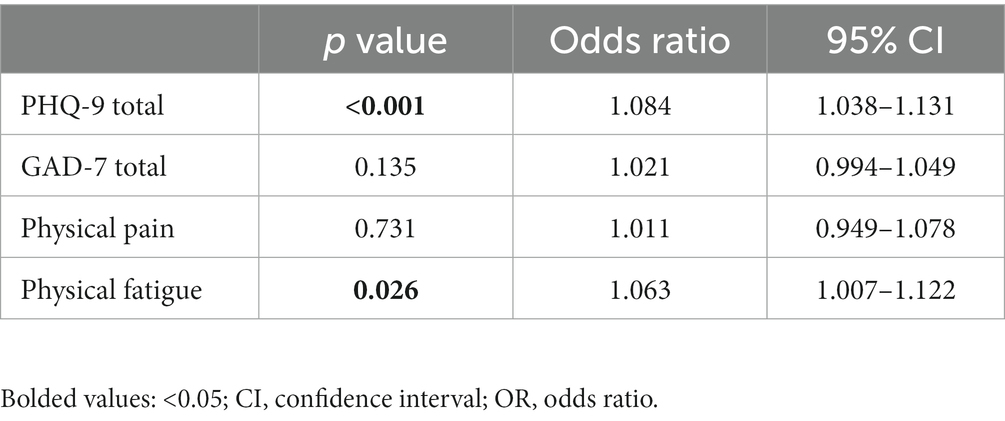
Table 2. Independent correlates among fire service recruits during the COVID-19 pandemic (N = 1,560).
Figure 1 shows the network structure for fear of COVID-19 symptoms as measured by FCV-19S items. The three most central symptoms with the highest EI values were nodes FOC6 (“Sleep difficulties caused by worry about COVID-19”) and FOC7 (“Palpitations when thinking about COVID-19”) from the FCV-19S physical dimension, and FOC2 (“Uncomfortable to think about COVID-19”) from the FCV-19S psychological dimension. The mean predictability of nodes was 0.775, which showed that, on average, 77.5% of the variance in each node could be accounted for by other nodes in the network model. Supplementary Table S1 presents network centrality indices for each fear of COVID-19 symptom. Figure 2 shows results of the flow network model. FOC2 (“Uncomfortable to think about COVID-19”; average edge weight = −0.0497) and FOC1 (“Afraid of COVID-19”; average edge weight = −0.0421) from the FCV-19S psychological dimension, and FOC6 (“Sleep difficulties caused by worry about COVID-19”; average edge weight = −0.0314) from the FCV-19S physical dimension had the strongest negative relationships with QoL.
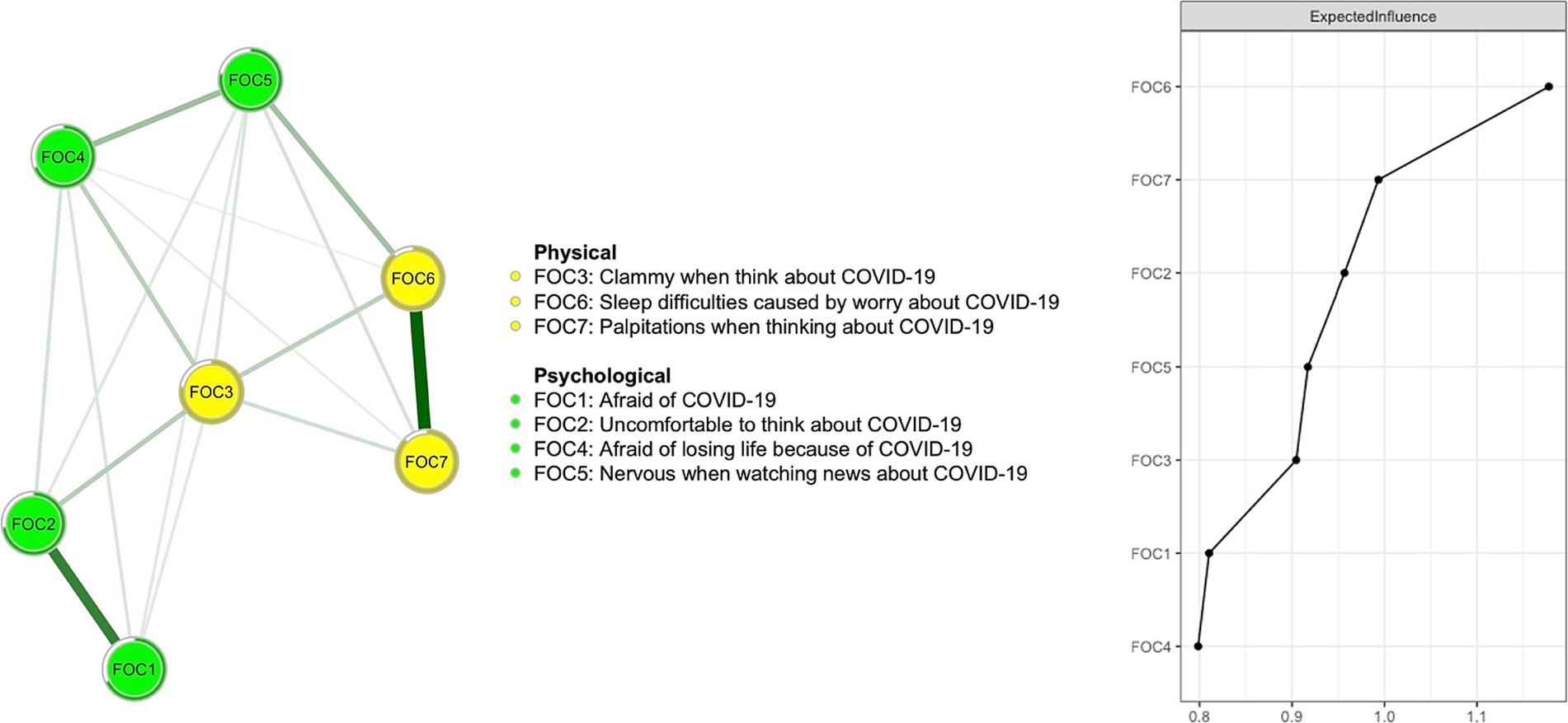
Figure 1. The fear of COVID-19 network structure among fire service recruits during the COVID-19 pandemic.
As shown in Figure 3, based on the case-dropping bootstrap procedure, the network model was highly stable. In addition, bootstrap 95% CIs for edge weights used to estimate network accuracy reflected a limited range, with most edge weights being non-zero (Supplementary Figure S1). As such, most edges were stable and accurate. These comparisons were statistically significant, underscoring sound reliability of the network model (Supplementary Figure S2).
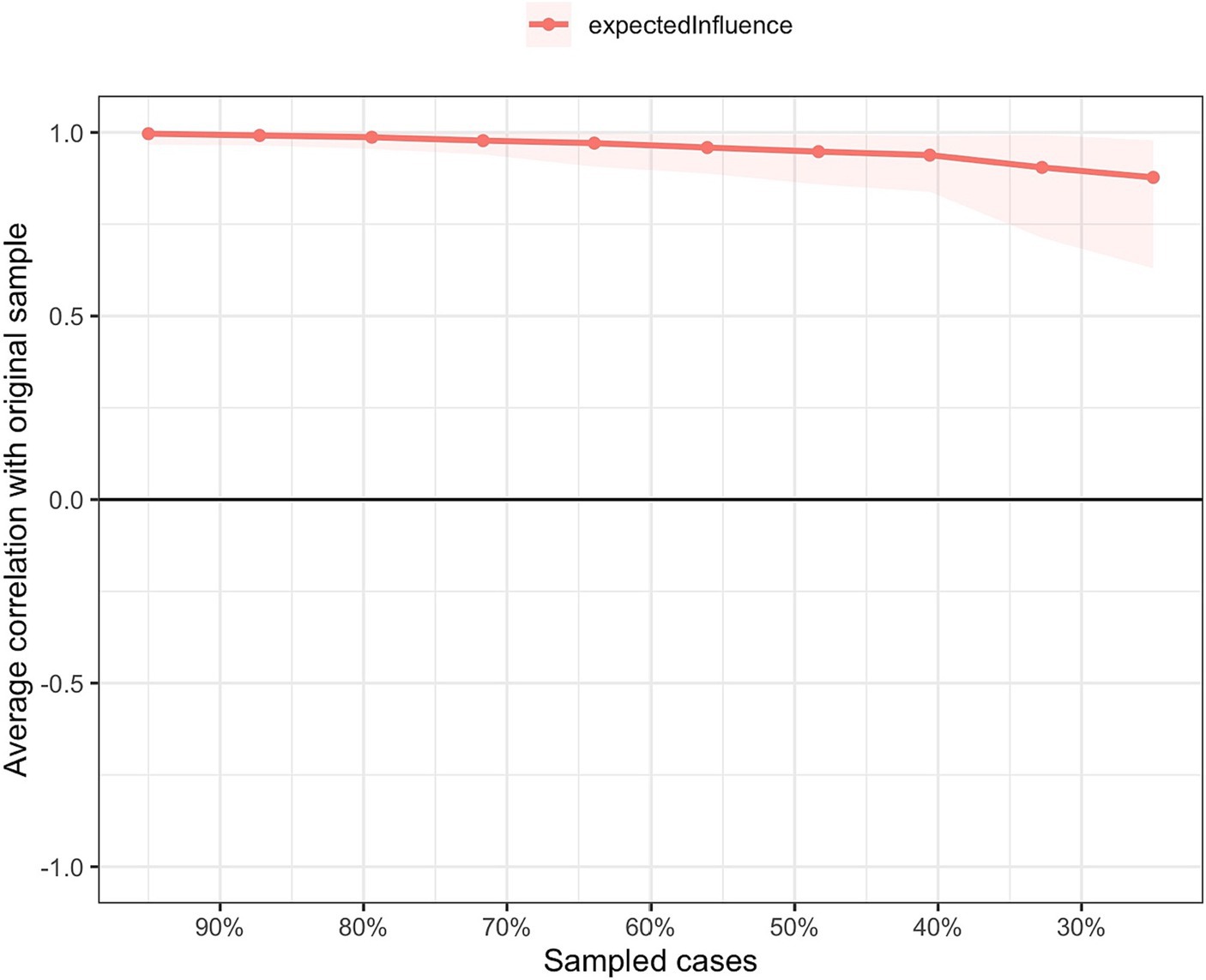
Figure 3. Network stability of the fear of COVID-19 among fire service recruits during the COVID-19 pandemic.
To our knowledge, this study is the first to examine the prevalence, correlates, and network structure of COVID-19 fear as well as its relationship with QoL among fire service recruits following the cessation of China’s dynamic zero-COVID policy. The prevalence of COVID-19 fear in this sample was 38.85% (95% CI = 36.42–41.32%). This rate was higher than corresponding figures of 18% among residents in Bosnia and Herzegovina (12), and 33.7% for a general population sample in Lebanon (14), each of which used measures with no clear objective cut-off scores. Conversely, the current rate was lower than the rate of 43.8% found within a Hamburg sample of homeless people, based on a single item COVID-19 fear measure (41). Due to study differences in sample characteristics and assessment methods for examining fear of COVID-19, implications based on direct comparisons between these studies should be drawn with caution. However, in the context of their training during the COVID-19 pandemic, fire service recruits have been required to live in a group environment away from their families for an extended period and face strict training assessments that can cause significant stress (42). Our prevalence results align with the meta-analysis finding of a positive relationship between fear of COVID-19 and stress (43).
We found that more severe depression was associated with a higher level of COVID-19 fear among fire service recruits. After the dynamic zero-COVID policy ceased and a full-blown outbreak followed in China, fire service recruits were trained in a lockdown environment. Similarly, previous studies have found a positive correlation between isolation and depression (44, 45). For example, in a study of Turkish adults, fear of COVID-19 was positively correlated with depression (46). The association between depression and COVID-19 fear may be due, in part, to impaired emotion regulation. People who are depressed may experience more emotional dysregulation (47), which contributes to fear by interfering with the capacity to manage emotions effectively as well as increased sensitivity to perceived threats or stressors (48). A study on fear of COVID-19 and psychiatric comorbidities in the United States also reported significant bivariate associations between fear and symptoms of anxiety and depression (49).
We also found that fire service recruits with fear of COVID-19 were more prone to severe physical fatigue. Fire service recruits must undergo long hours of physical fitness and skill training that may be detrimental to their immediate physical and mental well-being. Fatigue refers to a persistent feeling of tiredness that may affect physical and cognitive performance to the point of increasing fear (50, 51). Previous research (52) has highlighted the interplay between cognitive functions and fear. In addition, when people experience fear of COVID-19, they may show heightened stress responding (53) that exacerbates physical fatigue over time (54).
In the network model of fear of COVID-19, “Sleep difficulties caused by worry about COVID-19” (FOC6) in the FCV-19S physical dimension was the most central symptom. Fire service recruits undergo intense training and testing that can cause psychological stress (6, 8). During the pandemic, recruits may be concerned about their own or others’ health, increasing their stress levels and leading to sleep difficulties or other physical and psychological problems (55). The COVID-19 pandemic has led to global uncertainty (56), so fire service recruits may worry about its effects on their jobs, personal lives, and future career development, leading to anxiety and sleep difficulties (57), that may, in turn, lower QOL. Decreased social support associated with quarantine measures may also contribute to feelings of isolation and sleep disturbances (58). The centrality of “Sleep difficulties caused by worry about COVID-19″ in the network structure highlights potential pandemic effects on mental health of fire service recruits, who are particularly susceptible to pandemic-related stressors.
Another central symptom of COVID-19 fear from the FCV-19S physical dimension was “Palpitations when thinking about COVID-19” (FOC7). While palpitations are commonly associated with cardiovascular diseases, previous studies have found that psychiatric disturbances such as panic, anxiety, depression, and somatoform disorders are frequently observed in patients with palpitations (59). Fire service recruits may experience worry about infecting themselves or others, being unable to perform their job effectively or protecting themselves and others. Palpitations are a psychological and physiological response to perceived threats that often emerge in the context of significant life stressors (60). The centrality of “Palpitations when thinking about COVID-19” suggested that physiological symptoms present in severe anxiety states such as panic (61) warrant attention and may be amenable to interventions based on exposure and learning to realistically reappraise specific physiological reactions (62).
“Uncomfortable to think about COVID-19” (FOC2) from the FCV-19S psychological dimension was another central symptom in the network model among fire service recruits, consistent with findings in a study of Latin American countries (63). Worry and stress about viruses such as COVID-19 may lead to physical reactions such as heart palpitations (61), muscle tension (64), upset stomach (65), and fatigue (54) that contribute to more general experiences of discomfort. To ensure the safety and improve well-being of fire service recruits in the context of virus outbreaks or pandemics, it is important to implement a range of measures that include providing comprehensive training and instruction, establishing safety protocols, offering psychological support and promoting physical fitness.
The top three symptoms that were negatively associated with QoL in the flow network model of QoL and Fear of COVID-19 included “Afraid of losing life because of COVID-19” (FOC4) and “Uncomfortable to think about COVID-19” (FOC2) from the FCV-19S psychological dimension and “Sleep difficulties caused by worry about COVID-19” (FOC6) from the FCV-19S physical dimension. After the dynamic zero-COVID policy ceased, Chinese social media was flooded with news about the pandemic; reports of fever and other symptoms were common thereafter. Consequently, many people, including some fire service recruits, may have experienced increased fear of disability or death from COVID-19. While phobias and anxiety disorders are characterized by excessive and persistent worry, fear and apprehension related to external stimuli or bodily sensations (66), death anxiety pertains specifically to fear and distress associated with death and dying (67). Research has contended that fear of death or death anxiety are common and can become more pronounced in situations where mortality risk is prominent (68). Excessive dread of dying can cause psychiatric illnesses and maladjustment (69) that impair QoL (70). Other possible mechanisms underlying death anxiety (71) include regrets about past events and a lack of meaning in life. Fire service recruits will have demanding, risky, psychologically taxing jobs that require long and arduous training to meet required standards. However, during pandemics, the confinement of their training may cause recruits to question the meaning of their lives and their preparedness to meet job demands. A significant negative association between death anxiety and QoL has been shown in previous studies (72, 73).
Strengths of this study included its assessment of a unique, understudied population, and reliable results from the associated network model. However, the research also had several limitations. First, fear of COVID-19 (FCVS-19) was based on a self-report measure and was susceptible to possible response biases (e.g., social desirability bias and recall biases). Second, since this was a cross-sectional study, causal relations between fear of COVID-19 and other factors cannot be demonstrated. Third, to maintain reasonable assessment burdens on unpaid participants, the survey was highly focused and potentially important influences such as workload, personal life characteristics and use of psychotropic medications were not recorded in this study. Furthermore, potentially salient psychiatric conditions such as post-traumatic stress disorder were not assessed and warrant inclusion in future studies. Fourth, specific sources of COVID-19 related fear (e.g., the virus versus vaccines) could not be determined using the FCV-19S.
In conclusion, more than one third of fire service recruits reported fear of COVID-19 after China’s dynamic zero-COVID policy was terminated and a full-blown outbreak followed. Increased fear of COVID-19 was associated with other mental health concerns including elevations in depression, anxiety, pain and physical fatigue in addition to diminished QoL. As the most central symptoms in the network structure of COVID-19 fear, “Sleep difficulties caused by worry about COVID-19,” “Palpitations when thinking about COVID-19” and “Uncomfortable to think about COVID-19” appear to be plausible targets for psychosocial interventions among fire service recruits with heightened fear of COVID-19. Based on the core symptoms negatively correlated with QoL (“Afraid of losing life because of COVID-19,” “Sleep difficulties caused by worry about COVID-19” and “Uncomfortable to think about COVID-19”), maintaining physical and mental health during closed training, improving professional training quality and knowledge (74), keeping in touch with family and friends (75), and participating in recreational activities are viable strategies for helping fire service recruits to maintain or improve their QoL (6).
The data analyzed in this study is subject to the following licenses/restrictions: the datasets presented in this article are not readily available because The Institutional Review Board (IRB) of the China Emergency General Hospital that approved the study prohibits the authors from making publicly available the research dataset of clinical studies. Requests to access these datasets should be directed to Y-TX, eHl1dGx5QGdtYWlsLmNvbQ==.
The studies involving humans were approved by the ethics committee of China Emergency General Hospital. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
JL: Conceptualization, Data curation, Formal analysis, Funding acquisition, Writing – review & editing. TS: Data curation, Formal analysis, Methodology, Validation, Writing – original draft, Writing – review & editing. PC: Data curation, Methodology, Writing – review & editing. Y-YW: Data curation, Writing – review & editing. ZS: Data curation, Writing – review & editing. TC: Data curation, Writing – review & editing. TJ: Writing – review & editing. Y-TX: Conceptualization, Funding acquisition, Writing – original draft, Writing – review & editing. YF: Conceptualization, Funding acquisition, Writing – review & editing.
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. The study was supported by Beijing High Level Public Health Technology Talent Construction Project (Discipline Backbone-01-028) and the University of Macau (MYRG2019-00066-FHS; MYRG2022-00187-FHS).
The authors are grateful to all participants and clinicians involved in this study.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2023.1257943/full#supplementary-material
1. Li, W, Yang, Y, Liu, ZH, Zhao, YJ, Zhang, Q, Zhang, L, et al. Progression of mental health services during the COVID-19 outbreak in China. Int J Biol Sci. (2020) 16:1732–8. doi: 10.7150/ijbs.45120
2. Burki, T. Moving away from zero COVID in China. Lancet Respir Med. (2023) 11:132. doi: 10.1016/S2213-2600(22)00508-2
3. Ferreira, LN, Pereira, LN, da Fé, BM, and Ilchuk, K. Quality of life under the COVID-19 quarantine. Qual Life Res. (2021) 30:1389–405. doi: 10.1007/s11136-020-02724-x
4. Gostin, LO, and Wiley, LF. Governmental public health powers during the COVID-19 pandemic: stay-at-home orders, business closures, and travel restrictions. JAMA. (2020) 323:2137–8. doi: 10.1001/jama.2020.5460
5. Lan, F-Y, Scheibler, C, Hershey, MS, Romero-Cabrera, JL, Gaviola, GC, Yiannakou, I, et al. Effects of a healthy lifestyle intervention and COVID-19-adjusted training curriculum on firefighter recruits. Sci Rep. (2022) 12:10607. doi: 10.1038/s41598-022-10979-2
6. Ma, HR. Study on the mechanism of combat-oriented training for newly recruited firefighters. China Acad J Electron Publ House. (2020) 24:52–3. doi: 10.16859/j.cnki.cn12-9204/tu.2020.24.031
7. Chen, X, Zhang, L, Peng, Z, and Chen, S. Factors influencing the mental health of firefighters in Shantou City, China. Psychol Res Behav Manag. (2020) 13:529–36. doi: 10.2147/PRBM.S249650
8. Ministry of Emergency Management of the People's Republic of China. (2022). National Comprehensive Fire Rescue Team 2022 Annual Examination Recruitment Cadre Interview Announcement. Available at: https://www.mem.gov.cn/gk/zfxxgkpt/fdzdgknr/202201/t20220120_407031.shtml (Accessed June 27, 2023).
9. Tang, Y-M, Wu, T-L, and Liu, H-T. Causal model analysis of the effect of formalism, fear of infection, COVID-19 stress on firefighters’ post-traumatic stress syndrome and insomnia. Int J Environ Res Public Health. (2023) 20:1097. doi: 10.3390/ijerph20021097
10. Krueger, RF, Kotov, R, Watson, D, Forbes, MK, Eaton, NR, Ruggero, CJ, et al. Progress in achieving quantitative classification of psychopathology. World Psychiatry. (2018) 17:282–93. doi: 10.1002/wps.20566
11. Ahorsu, DK, Lin, C-Y, Imani, V, Saffari, M, Griffiths, MD, and Pakpour, AH. The fear of COVID-19 scale: development and initial validation. Int J Ment Heal Addict. (2022) 20:1537–45. doi: 10.1007/s11469-020-00270-8
12. Šljivo, A, Kačamaković, M, Quraishi, I, and Džubur, KA. Fear and depression among residents of Bosnia and Herzegovina during COVID-19 outbreak-internet survey. Psychiatr Danub. (2020) 32:266–72. doi: 10.24869/psyd.2020.266
13. Meller, FO, Schäfer, AA, Quadra, MR, Demenech, LM, Paludo, SDS, da Silva, PA, et al. Fear of Covid-19 and health-related outcomes: results from two Brazilian population-based studies. Psychiatry Res. (2022) 313:114596. doi: 10.1016/j.psychres.2022.114596
14. Chalhoub, Z, Koubeissy, H, Fares, Y, and Abou-Abbas, L. Fear and death anxiety in the shadow of COVID-19 among the Lebanese population: a cross-sectional study. PLoS One. (2022) 17:e0270567. doi: 10.1371/journal.pone.0270567
15. Usher, K, Durkin, J, and Bhullar, N. The COVID-19 pandemic and mental health impacts. Int J Ment Health Nurs. (2020) 29:315–8. doi: 10.1111/inm.12726
16. Salcioglu, E, Urhan, S, Pirinccioglu, T, and Aydin, S. Anticipatory fear and helplessness predict PTSD and depression in domestic violence survivors. Psychol Trauma. (2017) 9:117–25. doi: 10.1037/tra0000200
17. Liu, RT, Kleiman, EM, Nestor, BA, and Cheek, SM. The hopelessness theory of depression: a quarter century in review. Clin Psychol (New York). (2015) 22:345–65. doi: 10.1111/cpsp.12125
18. Chrousos, G, and Gold, P. The concepts of stress and stress system disorders: overview of behavioral and physical homeostasis, vol. 267. Bethesda, MD: National Institutes of Health (1991). 1244 p.
19. Gasparro, R, Scandurra, C, Maldonato, NM, Dolce, P, Bochicchio, V, Valletta, A, et al. Perceived job insecurity and depressive symptoms among Italian dentists: the moderating role of fear of COVID-19. Int J Environ Res Public Health. (2020) 17:5338. doi: 10.3390/ijerph17155338
20. Mertens, G, Duijndam, S, Smeets, T, and Lodder, P. The latent and item structure of COVID-19 fear: a comparison of four COVID-19 fear questionnaires using SEM and network analyses. J Anxiety Disord. (2021) 81:102415. doi: 10.1016/j.janxdis.2021.102415
21. Epskamp, S, Cramer, AO, Waldorp, LJ, Schmittmann, VD, and Borsboom, D. Qgraph: network visualizations of relationships in psychometric data. J Stat Softw. (2012) 48:1–18. doi: 10.18637/jss.v048.i04
22. Cramer, AO, Van Borkulo, CD, Giltay, EJ, Van Der Maas, HL, Kendler, KS, Scheffer, M, et al. Major depression as a complex dynamic system. PLoS One. (2016) 11:e0167490. doi: 10.1371/journal.pone.0167490
23. Si, TL, Chen, P, Zhang, L, Sha, S, Lam, MI, Lok, KI, et al. Depression and quality of life among Macau residents in the 2022 COVID-19 pandemic wave from the perspective of network analysis. Front Psychol. (2023) 14:1164232. doi: 10.3389/fpsyg.2023.1164232
24. Cai, H, Chow, IH, Lei, S-M, Lok, GK, Su, Z, Cheung, T, et al. Inter-relationships of depressive and anxiety symptoms with suicidality among adolescents: a network perspective. J Affect Disord. (2023) 324:480–8. doi: 10.1016/j.jad.2022.12.093
25. Jin, Y, Sun, HL, Lam, SC, Su, Z, Hall, BJ, Cheung, T, et al. Depressive symptoms and gender differences in older adults in Hong Kong during the COVID-19 pandemic: a network analysis approach. Int J Biol Sci. (2022) 18:3934–41. doi: 10.7150/ijbs.69460
26. Tokac, U, and Razon, S. Nursing professionals' mental well-being and workplace impairment during the COVID-19 crisis: a network analysis. J Nurs Manag. (2021) 29:1653–9. doi: 10.1111/jonm.13285
27. Yuan, H, Ren, L, Ma, Z, Li, F, Liu, J, Jin, Y, et al. Network structure of PTSD symptoms in Chinese male firefighters. Asian J Psychiatr. (2022) 72:103062. doi: 10.1016/j.ajp.2022.103062
28. Chen, P, Zhang, L, Sha, S, Lam, MI, Lok, KI, Chow, IHI, et al. Prevalence of insomnia and its association with quality of life among Macau residents shortly after the summer 2022 COVID-19 outbreak: a network analysis perspective. Front Psych. (2023) 14:1113122. doi: 10.3389/fpsyt.2023.1113122
29. Cai, H, Bai, W, Sha, S, Zhang, L, Chow, IHI, Lei, SM, et al. Identification of central symptoms in internet addictions and depression among adolescents in Macau: a network analysis. J Affect Disord. (2022) 302:415–23. doi: 10.1016/j.jad.2022.01.068
30. Oldenmenger, WH, de Raaf, PJ, de Klerk, C, and van der Rijt, CCD. Cut points on 0–10 numeric rating scales for symptoms included in the Edmonton symptom assessment scale in Cancer patients: a systematic review. J Pain Symptom Manag. (2013) 45:1083–93. doi: 10.1016/j.jpainsymman.2012.06.007
31. Luo, F, Ghanei Gheshlagh, R, Dalvand, S, Saedmoucheshi, S, and Li, Q. Systematic review and meta-analysis of fear of COVID-19. Front Psychol. (2021) 12:661078. doi: 10.3389/fpsyg.2021.661078
32. Feng, Q-y, Huang, C-w, Jia, Y-p, Liu, T, Jia, H-y, Wang, K-c, et al. Reliability and validity of the Chinese version of fear of coronavirus disease 2019 scale (Chinese). Acad J Second Mil Univ. (2021) 42:778–82.
33. Lecuona, O, Lin, C-Y, Rozgonjuk, D, Norekvål, TM, Iversen, MM, Mamun, MA, et al. A network analysis of the fear of COVID-19 scale (FCV-19S): a large-scale cross-cultural study in Iran, Bangladesh, and Norway. Int J Environ Res Public Health. (2022) 19:6824. doi: 10.3390/ijerph19116824
34. Chen, M, Sheng, L, and Qu, S. Diagnostic test of screening depressive disorders in general hospital with the patient health questionnaire. Chin Ment Health J. (2015) 12:241–5.
35. He, X, Li, C, Qian, J, Cui, H, and Wu, W. A study on the reliability and validity of generalized anxiety scale in general hospitals. Shanghai Psychiatry. (2010) 22:200–3.
36. The WHOQOL Group. Development of the World Health Organization WHOQOL-BREF quality of life assessment. Psychol Med. (1998) 28:551–8. doi: 10.1017/S0033291798006667
37. R Core Team. R: a language and environment for statistical computing. R Foundation for Statistical Computing. Vienna, Austria: (2013) Available at: http://www.R-project.org/
38. Epskamp, S, Borsboom, D, and Fried, EI. Estimating psychological networks and their accuracy: a tutorial paper. Behav Res Methods. (2018) 50:195–212. doi: 10.3758/s13428-017-0862-1
39. Robinaugh, DJ, Millner, AJ, and McNally, RJ. Identifying highly influential nodes in the complicated grief network. J Abnorm Psychol. (2016) 125:747–57. doi: 10.1037/abn0000181
40. Haslbeck, J, and Waldorp, LJ. (2015). Mgm: estimating time-varying mixed graphical models in high-dimensional data. arXiv preprint arXiv:151006871.
41. Hajek, A, Bertram, F, van Rüth, V, Kretzler, B, Püschel, K, Heinrich, F, et al. Prevalence and factors associated with fear of COVID-19 among homeless individuals during the COVID-19 pandemic: evidence from the Hamburg survey of homeless individuals. Risk Manag Healthc Policy. (2021) 14:2689–95. doi: 10.2147/RMHP.S317039
42. Sun, H, Yang, F, and Li, C-X. Study on the mental health status and social influencing factors of newly recruited firefighters during the intensive training period. China Acad J Electron Publ House. (2022) 41:1155–59.
43. Şimşir, Z, Koç, H, Seki, T, and Griffiths, MD. The relationship between fear of COVID-19 and mental health problems: a meta-analysis. Death Stud. (2022) 46:515–23. doi: 10.1080/07481187.2021.1889097
44. Brooks, SK, Webster, RK, Smith, LE, Woodland, L, Wessely, S, Greenberg, N, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. (2020) 395:912–20. doi: 10.1016/S0140-6736(20)30460-8
45. Ruan, J, Xu, Y-M, and Zhong, B-L. Loneliness in older Chinese adults amid the COVID-19 pandemic: prevalence and associated factors. Asia Pac Psychiatry. (2023):e12543. doi: 10.1111/appy.12543
46. Satici, B, Gocet-Tekin, E, Deniz, ME, and Satici, SA. Adaptation of the fear of COVID-19 scale: its association with psychological distress and life satisfaction in Turkey. Int J Ment Heal Addict. (2021) 19:1980–8. doi: 10.1007/s11469-020-00294-0
47. Hilt, LM, Hanson, JL, and Pollak, SD. Emotion dysregulation In: BB Brown and MJ Prinstein, editors. Encyclopedia of adolescence. San Diego: Academic Press (2011). 160–9.
48. Berking, M, and Wupperman, P. Emotion regulation and mental health: recent findings, current challenges, and future directions. Curr Opin Psychiatry. (2012) 25:128–34. doi: 10.1097/YCO.0b013e3283503669
49. Fitzpatrick, KM, Harris, C, and Drawve, G. Fear of COVID-19 and the mental health consequences in America. Psychol Trauma Theory Res Pract Policy. (2020) 12:S17–21. doi: 10.1037/tra0000924
50. Tanaka, M, Tajima, S, Mizuno, K, Ishii, A, Konishi, Y, Miike, T, et al. Frontier studies on fatigue, autonomic nerve dysfunction, and sleep-rhythm disorder. J Physiol Sci. (2015) 65:483–98. doi: 10.1007/s12576-015-0399-y
51. Foa, EB, and Kozak, MJ. Emotional processing of fear: exposure to corrective information. Psychol Bull. (1986) 99:20–35. doi: 10.1037/0033-2909.99.1.20
52. Phelps, EA, and LeDoux, JE. Contributions of the amygdala to emotion processing: from animal models to human behavior. Neuron. (2005) 48:175–87. doi: 10.1016/j.neuron.2005.09.025
53. Bakioğlu, F, Korkmaz, O, and Ercan, H. Fear of COVID-19 and positivity: mediating role of intolerance of uncertainty, depression, anxiety, and stress. Int J Ment Heal Addict. (2021) 19:2369–82. doi: 10.1007/s11469-020-00331-y
54. Kocalevent, RD, Hinz, A, Brähler, E, and Klapp, BF. Determinants of fatigue and stress. BMC Res Notes. (2011) 4:238. doi: 10.1186/1756-0500-4-238
55. Blix, I, Birkeland, MS, and Thoresen, S. Worry and mental health in the Covid-19 pandemic: vulnerability factors in the general Norwegian population. BMC Public Health. (2021) 21:928. doi: 10.1186/s12889-021-10927-1
56. Koffman, J, Gross, J, Etkind, SN, and Selman, L. Uncertainty and COVID-19: how are we to respond? J R Soc Med. (2020) 113:211–6. doi: 10.1177/0141076820930665
57. Wu, D, Yang, T, Hall, DL, Jiao, G, Huang, L, and Jiao, C. COVID-19 uncertainty and sleep: the roles of perceived stress and intolerance of uncertainty during the early stage of the COVID-19 outbreak. BMC Psychiatry. (2021) 21:306. doi: 10.1186/s12888-021-03310-2
58. Choi, H, Irwin, MR, and Cho, HJ. Impact of social isolation on behavioral health in elderly: systematic review. World J Psychiatry. (2015) 5:432–8. doi: 10.5498/wjp.v5.i4.432
59. Ehlers, A, Mayou, RA, Sprigings, DC, and Birkhead, J. Psychological and perceptual factors associated with arrhythmias and benign palpitations. Psychosom Med. (2000) 62:693–702. doi: 10.1097/00006842-200009000-00014
60. Dong, M, and Zheng, J. Letter to the editor: headline stress disorder caused by Netnews during the outbreak of COVID-19. Health Expect. (2020) 23:259–60. doi: 10.1111/hex.13055
61. Alijaniha, F, Noorbala, A, Afsharypuor, S, Naseri, M, Fallahi, F, Mosaddegh, M, et al. Relationship between palpitation and mental health. Iran Red Crescent Med J. (2016) 18:e22615. doi: 10.5812/ircmj.22615
62. Margraf, J, Barlow, DH, Clark, DM, and Telch, MJ. Psychological treatment of panic: work in progress on outcome, active ingredients, and follow-up. Behav Res Ther. (1993) 31:1–8. doi: 10.1016/0005-7967(93)90036-T
63. Caycho-Rodríguez, T, Ventura-León, J, Valencia, PD, Vilca, LW, Carbajal-León, C, Reyes-Bossio, M, et al. Network analysis of the relationships between conspiracy beliefs towards COVID-19 vaccine and symptoms of fear of COVID-19 in a sample of Latin American countries. Curr Psychol. (2022):1–16. doi: 10.1007/s12144-022-03622-w
64. Pluess, M, Conrad, A, and Wilhelm, FH. Muscle tension in generalized anxiety disorder: a critical review of the literature. J Anxiety Disord. (2009) 23:1–11. doi: 10.1016/j.janxdis.2008.03.016
65. Creed, F, Craig, T, and Farmer, R. Functional abdominal pain, psychiatric illness, and life events. Gut. (1988) 29:235–42. doi: 10.1136/gut.29.2.235
66. Craske, MG, Rauch, SL, Ursano, R, Prenoveau, J, Pine, DS, and Zinbarg, RE. What is an anxiety disorder? Focus. (2011) 9:369–88. doi: 10.1176/foc.9.3.foc369
67. Lonetto, R, and Templer, DI. (1986). Death anxiety. Washington, DC, US: Hemisphere Publishing Corp. p. 7–37.
68. Greenberg, J, Pyszczynski, T, Solomon, S, Rosenblatt, A, Veeder, M, Kirkland, S, et al. Evidence for terror management theory II: the effects of mortality salience on reactions to those who threaten or bolster the cultural worldview. J Pers Soc Psychol. (1990) 58:308–18. doi: 10.1037/0022-3514.58.2.308
69. Sarfraz, M, Waqas, H, Ahmed, S, Rurush-Asencio, R, and Mushtaque, I. Cancer-related stigmatization, quality of life, and fear of death among newly diagnosed cancer patients. Omega (Westport). (2022) 003022282211406. doi: 10.1177/00302228221140650
70. Thomson, L, Sheehan, KA, Meaney, C, Wnuk, S, Hawa, R, and Sockalingam, S. Prospective study of psychiatric illness as a predictor of weight loss and health related quality of life one year after bariatric surgery. J Psychosom Res. (2016) 86:7–12. doi: 10.1016/j.jpsychores.2016.04.008
71. Tomer, A, and Eliason, G. Toward a comprehensive model of death anxiety. Death Stud. (1996) 20:343–65. doi: 10.1080/07481189608252787
72. Maddahi, ME, Khalatbari, J, Samadzadeh, M, Amraei, M, Ahmadi, R, and Keikhafarzaneh, M. The study of quality of life and personality traits of NEO five factors concerning death anxiety in Shahed university students. Int J Sci Eng Res. (2011) 2:1–4.
73. Sherman, DW, Norman, R, and McSherry, CB. A comparison of death anxiety and quality of life of patients with advanced cancer or AIDS and their family caregivers. J Assoc Nurses AIDS Care. (2010) 21:99–112. doi: 10.1016/j.jana.2009.07.007
74. Ding, Y, Du, X, Li, Q, Zhang, M, Zhang, Q, Tan, X, et al. Risk perception of coronavirus disease 2019 (COVID-19) and its related factors among college students in China during quarantine. PLoS One. (2020) 15:e0237626. doi: 10.1371/journal.pone.0237626
Keywords: COVID-19 pandemic, fire service recruits, fear of COVID-19, network analysis, quality of life
Citation: Liu J, Si TL, Chen P, Wang Y-Y, Su Z, Cheung T, Jackson T, Xiang Y-T and Feng Y (2023) Prevalence of COVID-19 fear and its association with quality of life among fire service recruits after ceasing the dynamic zero-COVID policy in China. Front. Public Health. 11:1257943. doi: 10.3389/fpubh.2023.1257943
Received: 13 July 2023; Accepted: 20 September 2023;
Published: 06 October 2023.
Edited by:
Mohammadreza Shalbafan, Iran University of Medical Sciences, IranReviewed by:
Vida Imani, Tabriz University of Medical Sciences, IranCopyright © 2023 Liu, Si, Chen, Wang, Su, Cheung, Jackson, Xiang and Feng. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yu-Tao Xiang, eHl1dGx5QGdtYWlsLmNvbQ==; Yuan Feng, MTk1NTgwNTFAcXEuY29t
†These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.