- 1Department of Integrated Care Management Center, West China Hospital, Sichuan University, Chengdu, Sichuan, China
- 2Public Affairs Department, West China Hospital, Sichuan University, Chengdu, Sichuan, China
- 3Department of Nursing/Evidence-based Nursing Center, West China Hospital, Sichuan University, Chengdu, Sichuan, China
Background: Chronic kidney disease (CKD) is a major public health problem worldwide. Periodic surveys are essential for monitoring the prevalence of CKD and its risk factors. We assessed the prevalence of CKD and its risk factors in Mianzhu City in 2020.
Method: The Natural Population Cohort Study surveyed 7,770 individuals aged>20 years in Mianzhu City of Sichuan province in 2020. Our investigation encompassed the measurement of CKD prevalence, the evaluation of various renal function indicators, and comparisons based on age, gender, and hukou status. Additionally, some metabolic indices were also measured to identify the underlying causes of CKD.
Results: (1) Overall, the prevalence of reduced renal function (eGFR<60 mL/min/1.73m2), albuminuria, and CKD were 1.3, 10.0, and 10.4%, respectively, (2) the overall prevalence of CKD was higher among men than among women (14.5% vs. 8.6%). Similarly, the prevalence of CKD was higher among men than women in most age groups, (3) among urban residents, the prevalence of CKD was higher among middle-aged individuals and lower among young individuals and older adults, and (4) considering eGFR, the albuminuria and CKD for group definition, Blood pressure, triglyceride, high-density lipoprotein, blood sugar, and BMI were all statistically different among between normal groups and abnormal groups s in the albuminuria and CKD.
Conclusion: The incidence of CKD greatly varied between Mianzhu City and other regions in China and other countries. The differences in risk factors of CKD should be explored in the future. The gender difference in the prevalence of CKD in this study was markedly different from that in previous studies. More high-quality studies are needed to further explore this controversy. Based on the different prevalence of CKD and metabolism-related indices in rural and urban areas in this study, we speculated that the high incidence of CKD in Mianzhu City might be related to diet, lifestyle, and availability of healthcare services.
1 Introduction
Chronic kidney disease (CKD) is a progressive condition characterized by structural and functional changes in the kidney. Chronic kidney disease is typically defined as reduced kidney function, estimated glomerular filtration rate (eGFR) of less than 60 mL/min per 1.73m2, or imaging evidence or laboratory markers of kidney damage, such as albuminuria, hematuria that persist at least for 3 months (1). CKD is globally recognized as a public health problem. It is associated with an increased risk of end-stage kidney disease. Additionally, it is an independent risk factor for cardiovascular diseases and premature death (2, 3). The prevalence and associated burden of CKD are rising worldwide, with the fastest growth occurring in low-income and middle-income countries (4–6). According to an epidemiological survey in 2012, the overall prevalence of CKD was 10.8% in China. The number of Chinese patients with CKD is estimated to be nearly 119.5 million (5).
CKD is usually insidious, and most affected individuals remain asymptomatic until the disease progresses. Early detection and secondary prevention of CKD by modifying major risk factors and using inexpensive medications are cost-effective solutions for developing countries. Hyperglycemia, hypertension, hyperlipidemia, and obesity are major contributors to the global burden of disease and are the most common risk factors of CKD (7–11). Therefore, in addition to determining the kidney function of the general population, we explored the prevalence of these risk factors in this study. We identified individuals at high risk of CKD, which can help implement preventive strategies.
This study was conducted based on data from the Natural Population Cohort Study (NPCS). Previous studies have indicated that the prevalence of CKD substantially differs between different regions worldwide (12–14). This heterogeneity might be related to differences in lifestyles and economic conditions (15, 16). Mianzhu is close to Chengdu, the capital city of Sichuan province. Because of its poor economy and frequent natural disasters, it was included in many medical investigations (17–19). We collected the demographic data of residents in Mianzhu from the NPCS. We preliminarily measured the renal function of residents in Mianzhu, which can primarily help design subsequent cohort studies.
2 Methods
2.1 Participants
Data for this study were derived from NPCS. The NPCS is a population-based multicenter cohort study conducted by the Clinical Research Group at WCH/SCU. This study was approved by the Ethics Committee of the WCH/SCU [NO. (2020)145] and the Ministry of Science and Technology of China [No. (2020) CJ0150]. This study used the cluster sampling method (community or village) to recruit participants. Adult participants and their relatives who (1) aged ≥20 years and (2) had local household registration or non-local household registration but lived in the area for more than 6 months were invited to participate. The NPCS began in 2020 and will continue for at least 5 years.
2.2 Data collection
A questionnaire was used to collect demographic characteristics, such as gender, age, marital status, education, health insurance, commercial insurance, smoking, and alcohol drinking. Data were collected by face-to-face interviews with respondents and their family members. Height and weight were measured by nurses in the field. The subjects were asked to sit still for 20 min before blood pressure measurement. The left upper limb was taken for measurement with the help of trained evaluators. Blood pressure was measured between 8 and 10 a.m. with an empty stomach. Blood samples (4 mL in ethylenediaminetetraacetic acid (EDTA; plasma) and 1.5 mL in serum separator tube (SST; serum)) were collected for measuring complete blood count between 8 and 10 a.m. with an empty stomach. Random urine samples were collected between 8 and 10 a.m.
2.3 Laboratory measurement and specimen collection
(1) Chronic kidney disease (CKD) was defined as eGFR less than 60 mL/min per 1.73m2 or the presence of albuminuria (20). We used CKD-EPI to estimate eGFR. According to the Kidney Disease Outcomes Quality Initiative (K/DOQI) guidelines, we divided eGFR into five levels. eGFR class one was defined as eGFR ≥60 and was considered normal kidney function; eGFR class two was defined as eGFR between 45 and 59 and was considered a mild decline in kidney function; eGFR class three was defined as eGFR between 30 and 44, and was considered a moderate decline in kidney function; eGFR class four was defined as eGFR<30, and was considered a severe decline in kidney function (21).
Albuminuria was classified into -, +, ++, and +++ in urine analysis. Albuminuria ≥1+ was considered positive.
(2) Hypertension was defined as the presence of average systolic blood pressure ≥ 140 mmHg or diastolic blood pressure ≥ 90 mmHg, previous diagnosis of hypertension, or use of antihypertensive medication. Hypertension was divided into three stages: stage 1 hypertension (SBP 140–159 mmHg and/or DBP 90–99 mmHg); stage 2 hypertension (SBP 160–179 mmHg and/or DBP 100–109 mmHg); and stage 3 hypertension (SBP>180 mmHg and/or DBP>110 mmHg) (22).
(3) Diabetes was defined based on the following criteria: average fasting blood glucose (FBG) ≥ 7.0 mmol/L, currently taking anti-diabetic medications, or the previous diagnosis of diabetes (23).
(4) Dyslipidemia was defined as an abnormal lipid profile characterized by increased levels of total cholesterol (TC), low-density lipoprotein cholesterol (LDL-C), and triglyceride (TG) and decreased levels of high-density lipoprotein cholesterol (HDL-C). The specific criteria were as follows: TC higher than 6.2 mmol/L; LDL-C higher than 4.1 mmol/L; TG higher than 2.3 mmol/L; and HDL-C lower than 1.0 mmol/L (24, 25).
2.4 Statistics analysis
We excluded 869 participants with missing values. In addition, all participants (156) from a survey site with extremely poor-quality data on blood pressure were excluded, leaving 7,770 individuals for final analysis.
Demographic characteristics of patients and risk factors of CKD were determined. Quantitative variables are presented as mean and standard deviation (SD), and qualitative variables are presented as numbers and percentages. We used the χ2 test and t-test to compare groups. All analyzes were performed using SPSS version 25. value of p (two-tailed)<0.05 was considered statistically significant.
3 Results
3.1 Demographic characteristics
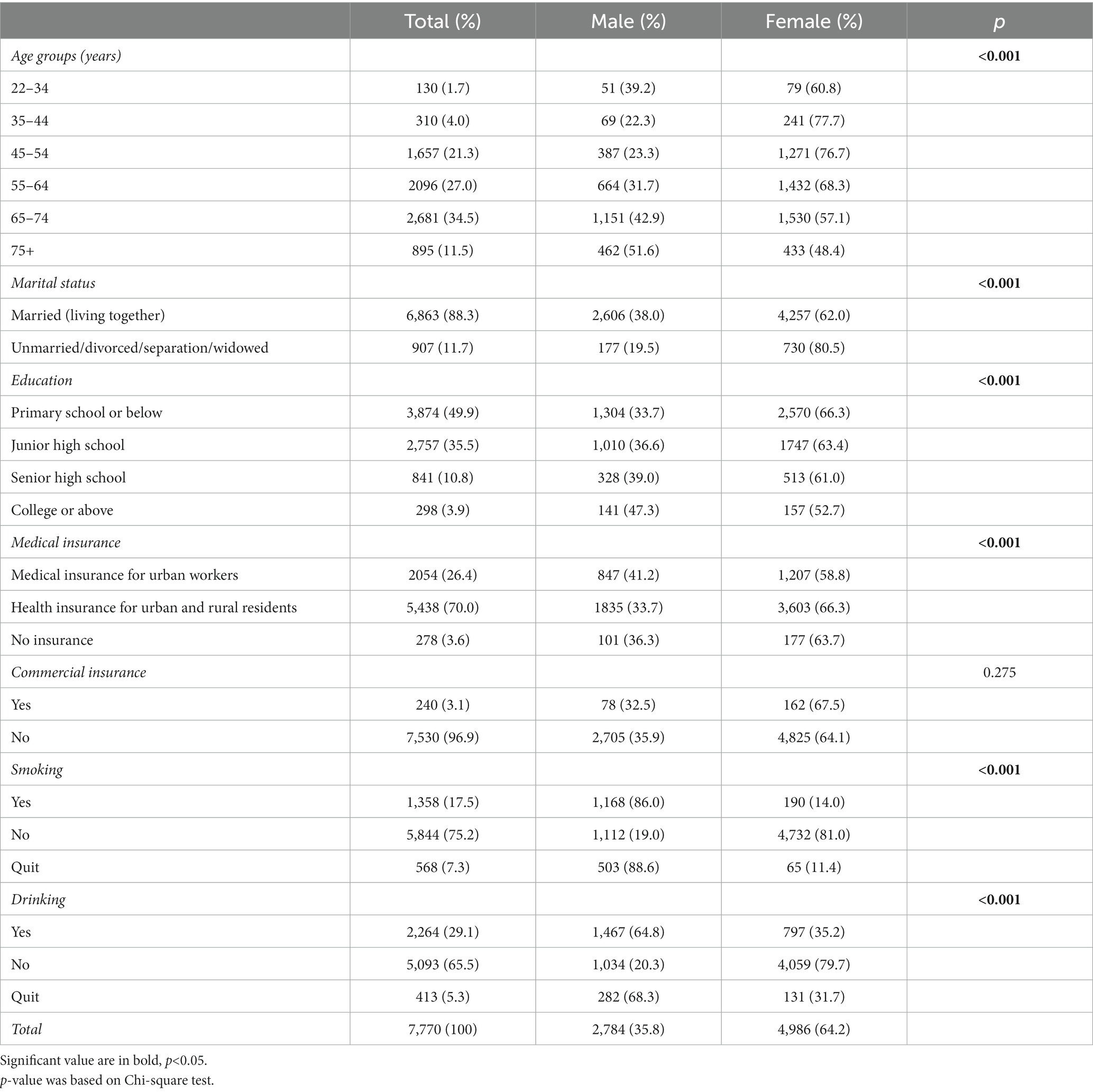
Of 7,770 participants, 35.8% were men and 64.2% were women. Most of the participants were > 45 years old and married. Their education level was mostly junior high school or below. The majority of urban and rural residents had health insurance, but most of them did not have commercial insurance. In addition, 15% of participants were current smokers and 20% drank alcohol. Except for commercial insurance, other variables were significantly and differently distributed among males and females (Table 1).
3.2 Renal function tests
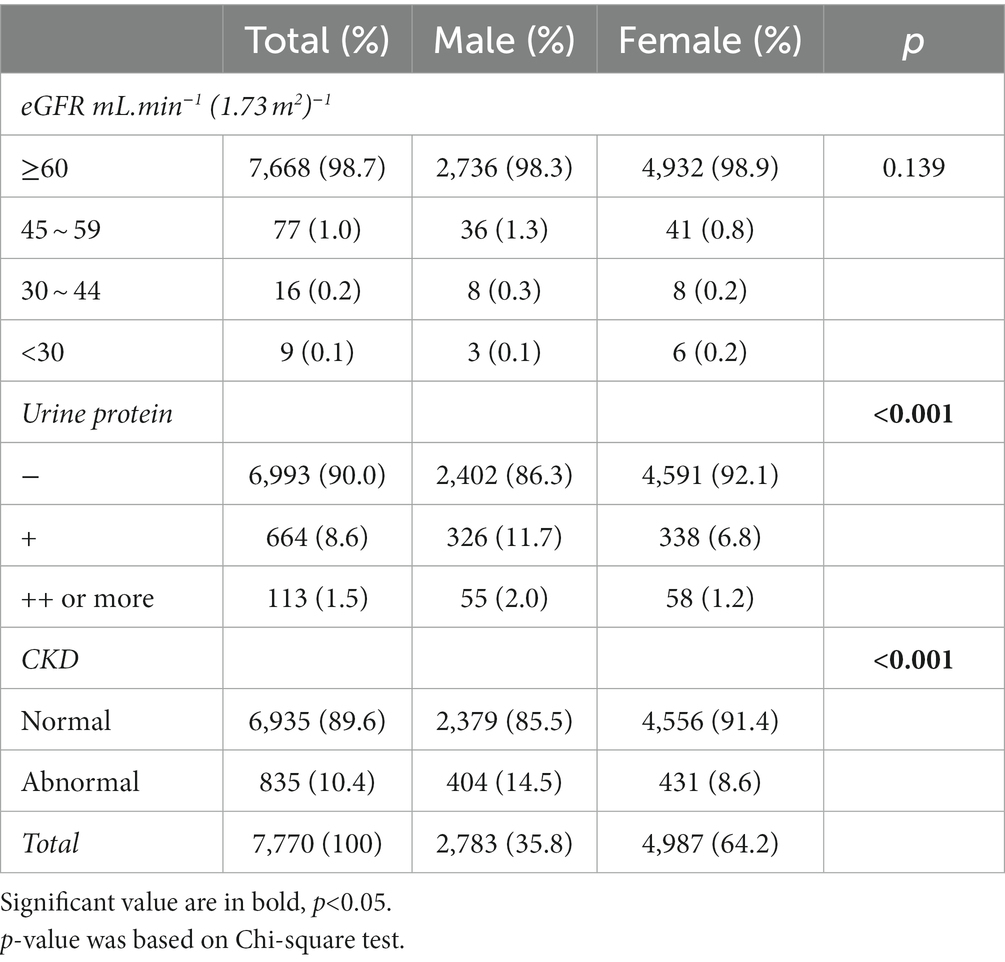
Table 2 shows that only 1.3% of participants had abnormal eGFR [<60 mL.min−1(1.73 m2)−1]. Most of them had an eGFR of between 45 and 59 mL.min−1(1.73 m2)−1. In addition, 10.1% of participants had positive urine protein tests. We found that 10.4% of participants had CKD. Decreased eGFR, positive urine protein result, and CKD were all more common among men. Positive urine protein and CKD were statistically different between men and women (P<0.001).
3.3 The prevalence of CKD by gender and hukou
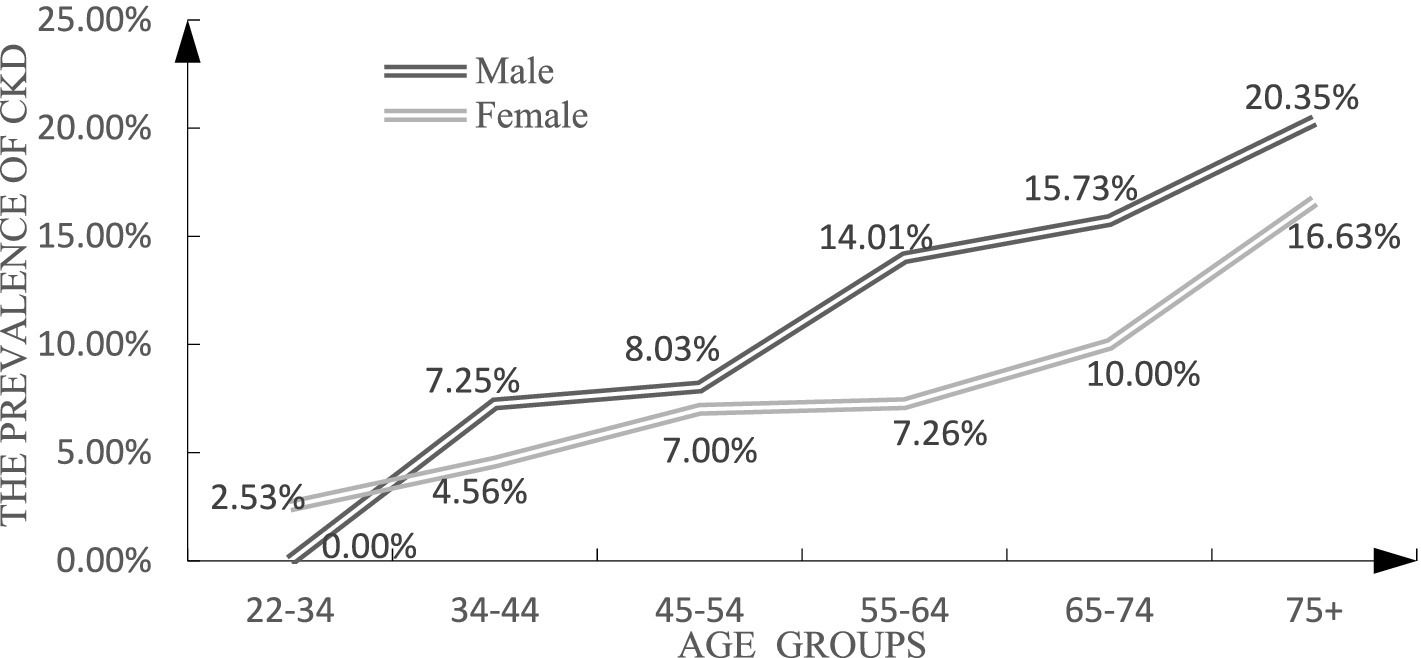
Figure 1 shows that the prevalence of CKD was higher among males than among females in most age groups. The gap between males and females gradually decreased in older ages.
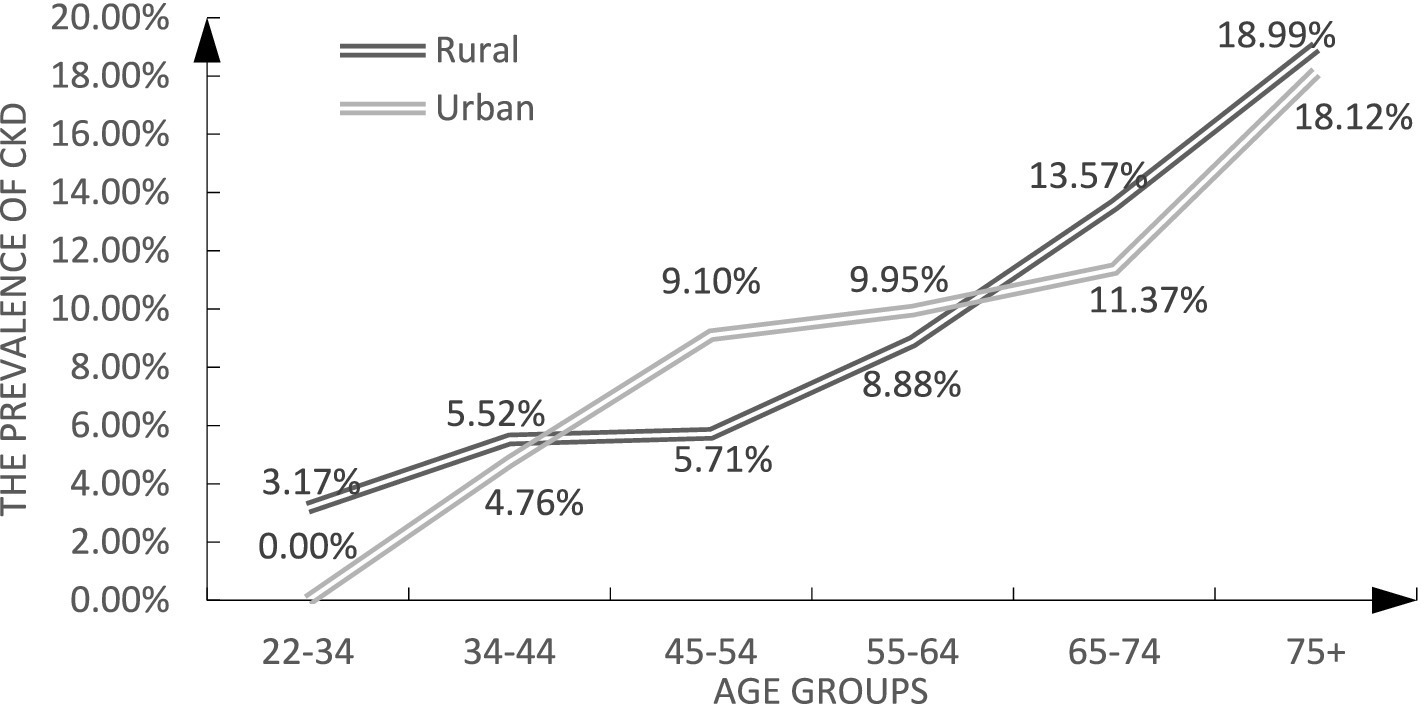
Figure 2 illustrates that among urban residents, the prevalence of CKD was elevated among middle-aged participants and declined among both younger and older individuals.
3.4 The relationship between indicators of kidney injury and risk factors of CKD
Table 3 indicates that 34% of participants suffered from hypertension, 8.7% of participants suffered from prediabetes, 1.8% of participants suffered from diabetes, and 10.8% of participants had a BMI of more than 28.
Hypertension was positively correlated with proteinuria and CKD (p<0.001). In addition, hypertension was positively correlated with the prevalence of patients with eGFR<60 mL.min−1(1.73 m2)−1, but the difference was not statistically significant (p>0.05).
Higher levels of TC, TG, and LDL-C and lower levels of HDL-C were observed among participants with proteinuria and CKD. TC, LDL-C, and HDL-C levels were lower in participants with eGFR<60. TG levels were higher in participants with normal eGFR<60. However, statistical significance was only observed for TG and HDL-C (p<0.001).
Prediabetes and diabetes were more common among patients with eGFR<60 mL.min−1(1.73 m2)−1, proteinuria, and CKD (p<0.001). Abnormal eGFR, proteinuria, and CKD were all more frequent in patients with BMI>24 than in the normal population (p<0.001).
Prediabetes, diabetes, and BMI were all more common among those with decreased eGFR, proteinuria, and CKD, and there was a significant difference between groups (p<0.001).
4 Discussion
In this study, there were more women than men, and most participants were > 50 years old. This may be due to the fact that men constitute the main proportion of the labor force, and older adults people and women are neglected in the non-developed cities of China. The educational level of participants was not high, and 85.3% of them had only completed junior high school or less. The coverage rate of health insurance in Mianzhu City was similar to that reported by a national survey (96.42% vs. 96.45%) (26). We found that only 3% of participants had commercial insurance. According to the 2020 China Household Wealth Index Survey Report, 10.8% of Chinese households are covered by commercial insurance (27). The low rate of commercial insurance indicates that the economy of Mianzhu is not prosperous.
We collected data on CKD stage, albuminuria, and eGFR. The prevalence of reduced renal function (eGFR<60 mL/min/1.73 m2) was 1.3%, the prevalence of albuminuria was 10.0%, and the overall prevalence of CKD was 10.4% in this study. We found that only the prevalence of reduced renal function in Mianzhu was lower than that in other regions. For instance, the prevalence of eGFR<60 mL/min/1.73m2, albuminuria, and CKD were 1.83, 8.65, and 9.88% in Zhejiang province, respectively (28). Using the same definition of CKD, a cross-section national survey in China showed that the prevalence of CKD was 10.8%, and the highest prevalence of CKD was found in Southwest China (18.3%) (20). The global estimated prevalence of CKD is 13.4% (29). CKD has various risk factors, including developmental, physical, social, cultural, structural, environmental, and genetic factors (30). Therefore, the difference in the prevalence of CKD between Mianzhu city and other regions may be due to the different prevalence of these risk factors.
Consistent with studies from Japan and Singapore (31, 32), the prevalence of CKD was higher among men than among women in our study. However, in most other geographical regions, the prevalence of CKD was higher among women (33–36). Some studies showed that despite including sex in the estimation, the CKD-EPI formula may overestimate eGFR in women (37). We used this formula, but the prevalence of CKD among men was still higher than that among women in this study. Chronic kidney disease resulting from hypertension or diabetes is more prevalent in men while autoimmune kidney disease or infectious urinary tract disease prevail in female (38). And in this study, we found that some metabolic risk factors, such as high blood pressure, dyslipidemia, diabetes, and high BMI were more common among men. Similarly, some national studies reported that the prevalence of hypertension (39), hyperglycemia (40), dyslipidemia (41), and obesity (42) were all higher among men than among women. We hypothesized that CKD is closely associated with metabolic factors in Mianzhu. In addition, as in Ciarambino’s study, the physiological differences in tubular absorption and secretory function between men and women may also account for the higher prevalence of CKD in men (38).
Among middle-aged residents, the prevalence of CKD was lower in rural areas than in urban areas. The main career of Minazhu citizens is agriculture, lacking a prosperous economy. Therefore, many rural residents migrate in their early adulthood to obtain better jobs. Existing studies have shown that the incidence of CKD is related to the Western lifestyle (15). Migrant workers do not have the sufficient economic power to maintain a high-oil, high-fat, and high-sugar diet and are, therefore, less likely to become obese and metabolically ill. Old immigrants return to the countryside, where public health services and medical resources are not abundant, which may increase the risk of CKD.
5 Limitation
We lost some participants who were migrant workers. Minority groups avoided participation due to their living habits and religious beliefs. In addition, there are many combinations of indicators for CKD. In this study, we referred to the previous large-scale cross-sectional survey on the prevalence of kidney disease in China, which only used eGFR and proteinuria to evaluate CKD. Since our data comes from the natural population, we only collected on eGFR and proteinuria for a single time point. These limitations may affect the measured rates of CKD. In future cohort studies, we may need to improve the relevant indicators and plans to obtain more reliable data on the prevalence of CKD. Finally, because of the cross-sectional design, this study cannot demonstrate a causal relationship between metabolic risk factors and CKD.
Data availability statement
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
Ethics statement
The studies involving humans were approved by Ethics Committee of West China Hospital, Sichuan University. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
YJ and MW: conceptualization, methodology, and writing, review & editing. FC: formal analysis, data visualization, and writing the original draft. All authors contributed to the article and approved the submitted version.
Funding
We are supported by Science and Technology Department of Sichuan Province Project 2020YFS0229.
Acknowledgments
The authors would like to express their gratitude to EditSprings (https://www.editsprings.cn) for the expert linguistic services provided.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Kalantar-Zadeh, K, Jafar, TH, Nitsch, D, Neuen, BL, and Perkovic, V. Chronic kidney disease. Lancet. (2021) 398:786–802. doi: 10.1016/S0140-6736(21)00519-5
2. Hill, NR, Fatoba, ST, Oke, JL, Hirst, JA, O’Callaghan, CA, Lasserson, DS, et al. Global prevalence of chronic kidney disease – a systematic review and meta-analysis. PLoS One. (2016) 11:e0158765. doi: 10.1371/journal.pone.0158765
3. Mills, KT, Xu, Y, Zhang, W, Bundy, JD, Chen, CS, Kelly, TN, et al. A systematic analysis of worldwide population-based data on the global burden of chronic kidney disease in 2010. Kidney Int. (2015) 88:950–7. doi: 10.1038/ki.2015.230
4. GBD 2015 Disease and Injury Incidence and Prevalence Collaborators. GBD 2015 Disease and injury incidence and prevalence collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990-2015: a systematic analysis for the global burden of Disease study 2015 published correction appears in lancet. 2017. Lancet. (2016) 388:1545–602. doi: 10.1016/S0140-6736(16)31678-6
5. Martinez, R, Lloyd-Sherlock, P, Soliz, P, Ebrahim, S, Vega, E, Ordunez, P, et al. Trends in premature avertable mortality from non-communicable diseases for 195 countries and territories, 1990-2017: a population-based study. Lancet Glob Health. (2020) 8:e511–23. doi: 10.1016/S2214-109X(20)30035-8
6. Levey, AS, de Jong, PE, Coresh, J, Nahas, ME, Astor, BC, Matsushita, K, et al. The definition, classification, and prognosis of chronic kidney disease: a KDIGO controversies conference report. Kidney Int. (2011) 80:17–28. doi: 10.1038/ki.2010.483
7. Xie, Y, Bowe, B, Mokdad, AH, Xian, H, Yan, Y, Li, T, et al. Analysis of the global burden of Disease study highlights the global, regional, and national trends of chronic kidney disease epidemiology from 1990 to 2016. Kidney Int. (2018) 94:567–81. doi: 10.1016/j.kint.2018.04.011
8. Zhang, L, Long, J, Jiang, W, Shi, Y, He, XX, Zhou, ZY, et al. Trends in chronic kidney Disease in China. N Engl J Med. (2016) 375:905–6. doi: 10.1056/NEJMc1602469
9. Pugh, D, Gallacher, PJ, and Dhaun, N. Management of Hypertension in chronic kidney Disease. Drugs. (2019) 79:365–79. doi: 10.1007/s40265-019-1064-1
10. Nehus, E. Obesity and chronic kidney disease. Curr Opin Pediatr. (2018) 30:241–6. doi: 10.1097/MOP.0000000000000586
11. Chen, Y, Dabbas, W, Gangemi, A, Benedetti, E, Lash, J, Finn, PW, et al. Obesity management and chronic kidney disease. Semin Nephrol. (2021) 41:392–402. doi: 10.1016/j.semnephrol.2021.06.010
12. Li, G, Huang, J, Wang, J, Zhao, M, Liu, Y, Guo, X, et al. Long-term exposure to ambient PM2.5 and increased risk of CKD prevalence in China published correction appears. J Am Soc Nephrol. (2021) 32:448–58. doi: 10.1681/ASN.2020040517
13. Liyanage, T, Toyama, T, Hockham, C, Ninomiya, T, Perkovic, V, Woodward, M, et al. Prevalence of chronic kidney disease in Asia: a systematic review and analysis. BMJ Glob Health. (2022) 7:e007525. doi: 10.1136/bmjgh-2021-007525
14. Wang, F, He, K, Wang, J, Zhao, MH, Li, Y, Zhang, L, et al. Prevalence and risk factors for CKD: a comparison between the adult populations in China and the United States. Kidney Int Rep. (2018) 3:1135–43. doi: 10.1016/j.ekir.2018.05.011
15. Hu, FB, Liu, Y, and Willett, WC. Preventing chronic diseases by promoting healthy diet and lifestyle: public policy implications for China. Obes Rev. (2011) 12:552–9. doi: 10.1111/j.1467-789X.2011.00863.x
16. Liang, Z, Wang, W, Yang, C, Wang, Y, Shen, J, Li, P, et al. Residential greenness and prevalence of chronic kidney disease: findings from the China National Survey of chronic kidney Disease. Sci Total Environ. (2022) 806:150628. doi: 10.1016/j.scitotenv.2021.150526
17. Guo, S, Liu, S, Peng, L, and Wang, H. The impact of severe natural disasters on the livelihoods of farmers in mountainous areas: a case study of Qingping township, Mianzhu City. Nat Hazards. (2014) 73:1679–96. doi: 10.1007/s11069-014-1165-9
18. Reinhardt, J, Zhang, X, Chen, S, Li, JN, Zhou, MW, and Khan, F. Long-term effectiveness of rehabilitation services delivery for Wenchuan earthquake survivors with impairments over a 4-year period: a prospective cohort study. BMJ Open. (2022) 12:e057158. doi: 10.1136/bmjopen-2021-057158
19. Wei, YY, Lin, JL, and Pu, FF. Current situation analysis of dietary patterns among middle-aged and elderly with different obesity metabolic phenotypes in Sichuan area. J Army Med Univ. (2023) 45:1596–603. doi: 10.16016/j.2097-0927.202304062
20. Zhang, L, Wang, F, Wang, L, Wang, W, Liu, B, Liu, J, et al. Prevalence of chronic kidney disease in China: a cross-sectional survey published correction appears in lancet. Lancet. (2012) 379:815–22. doi: 10.1016/S0140-6736(12)60033-6
21. Stevens, PE, Levin, A, and Disease, K. Improving global outcomes chronic kidney Disease guideline development work group members. Evaluation and management of chronic kidney disease: synopsis of the kidney disease: improving global outcomes 2012 clinical practice guideline. Ann Intern Med. (2013) 158:825–30. doi: 10.7326/0003-4819-158-11-201306040-00007
22. Williams, B, Mancia, G, Spiering, W, Rosei, EA, Azizi, M, Burnier, M, et al. 2018 ESC/ESH guidelines for the management of arterial hypertension. Eur Heart J. (2018) 39:3021–104. doi: 10.1093/eurheartj/ehy339
23. Chinese Diabetes Society. Guideline for the prevention and treatment of type 2 diabetes mellitus in China (2020 edition). Chin J Endocrinol Metab. (2021) 37:311–98. doi: 10.3760/cma.j.cn311282-20210304-00142
24. Joint committee issued Chinese guideline for the management of dyslipidemia in adults. Zhonghua Xin Xue Guan Bing Za Zhi. (2016) 44:833–53. doi: 10.3760/cma.j.issn.0253-3758.2016.10.005
25. Wang, TJ, Lien, AS, Chen, JL, Lin, CH, Yang, YS, and Yang, SH. A randomized clinical efficacy trial of red yeast Rice (Monascus pilosus) against hyperlipidemia. Am J Chin Med. (2019) 47:323–35. doi: 10.1142/S0192415X19500150
26. Central People’s Government. Central People’s Government of the People’s Republic of China: China has 1.36 billion people covered by basic medical insurance. Available at: http://www.gov.cn/zhengce/2021-07/13/content_5624486.htm
27. Survey and Research Center for China Household Finance. China Household Wealth Index Survey Report (2020Q2). Available at: https://chfs.swufe.edu.cn/zkcg/cgbg.htm
28. Lin, B, Shao, L, Luo, Q, Ou-yang, L, Zhou, F, Biao, D, et al. Prevalence of chronic kidney disease and its association with metabolic diseases: a cross-sectional survey in Zhejiang province, eastern China. BMC Nephrol. (2014) 15:36. doi: 10.1186/1471-2369-15-36
29. Lv, JC, and Zhang, LX. Prevalence and Disease burden of chronic kidney Disease. Adv Exp Med Biol. (2019) 1165:3–15. doi: 10.1007/978-981-13-8871-2_1
30. Levin, A, Tonelli, M, Bonventre, J, Coresh, J, Donner, JA, Fogo, AB, et al. Global kidney health summit participants. Global kidney health 2017 and beyond: a roadmap for closing gaps in care, research, and policy. Lancet. (2017) 390:1888–917. doi: 10.1016/S0140-6736(17)30788-2
31. Nagata, M, Ninomiya, T, Doi, Y, Yonemoto, K, Kubo, M, Hata, J, et al. Trends in the prevalence of chronic kidney disease and its risk factors in a general Japanese population: the Hisayama study. Nephrol Dial Transplant. (2010) 25:2557–64. doi: 10.1093/ndt/gfq062
32. National Health Survey 2010 MOH. Epidemiology & Disease control division, Ministry of Health, Singapore. Singapore: National Health Survey 2010 MOH (2011).
33. Vinhas, J, Gardete-Correia, L, Boavida, JM, Raposo, JF, Mesquita, A, Fona, MC, et al. Prevalence of chronic kidney disease and associated risk factors, and risk of end-stage renal disease: data from the PREVADIAB study. Nephron Clin Pract. (2011) 119:c35–40. doi: 10.1159/000324218
34. Gasparini, A, Evans, M, Coresh, J, Grams, ME, Norin, O, Qureshi, AR, et al. Prevalence and recognition of chronic kidney disease in Stockholm healthcare. Nephrol Dial Transplant. (2016) 31:2086–94. doi: 10.1093/ndt/gfw354
35. Murphy, D, McCulloch, CE, Lin, F, Banerjee, T, Bragg-Gresham, J, Eberhardt, M, et al. Trends in prevalence of chronic kidney Disease in the United States. Ann Intern Med. (2016) 165:473–81. doi: 10.7326/M16-0273
36. Shin, HY, and Kang, HT. Recent trends in the prevalence of chronic kidney disease in Korean adults: Korean National Health and nutrition examination survey from 1998 to 2013. J Nephrol. (2016) 29:799–807. doi: 10.1007/s40620-016-0280-y
37. Lewandowski, MJ, Krenn, S, Kurnikowski, A, Bretschneider, P, Sattler, M, Schwaiger, E, et al. Chronic kidney disease is more prevalent among women but more men than women are under nephrological care: analysis from six outpatient clinics in Austria 2019. Wien Klin Wochenschr. (2023) 135:89–96. doi: 10.1007/s00508-022-02074-3
38. Ciarambino, T, Crispino, P, and Giordano, M. Gender and renal insufficiency: opportunities for their therapeutic management? Cells. (2022) 11:3820. doi: 10.3390/cells11233820
39. Zhang, M, Shi, Y, Zhou, B, Huang, Z, Zhao, Z, Li, C, et al. Prevalence, awareness, treatment, and control of hypertension in China, 2004-18: findings from six rounds of a national survey. BMJ. (2023) 380:e071952. doi: 10.1136/bmj-2022-071952
40. Li, Y, Teng, D, Shi, X, Qin, G, Qin, Y, Quan, H, et al. Prevalence of diabetes recorded in mainland China using 2018 diagnostic criteria from the American Diabetes Association: national cross sectional study. BMJ. (2020) 369:m997. doi: 10.1136/bmj.m997
41. Li, XX, Zhao, Y, Huang, LX, Xu, HX, Liu, XY, Yang, JJ, et al. Effects of smoking and alcohol consumption on lipid profile in male adults in northwest rural China. Public Health. (2018) 157:7–13. doi: 10.1016/j.puhe.2018.01.003
Keywords: chronic kidney disease, diabetes, hypertension, hyperlipidemia, body mass index
Citation: Chen F, Wang M and Jiang Y (2024) Prevalence of chronic kidney disease and metabolic related indicators in Mianzhu, Sichuan, China. Front. Public Health. 11:1252110. doi: 10.3389/fpubh.2023.1252110
Edited by:
Laureline Berthelot, INSERM U1064 Centre de Recherche en Transplantation et Immunologie, FranceReviewed by:
Changchun Cao, Dapeng New District Nan’ao People’s Hospital, ChinaTiziana Ciarambino, Hospital of Marcianise, Italy
Copyright © 2024 Chen, Wang and Jiang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Miao Wang, ODU4OTMxNDFAcXEuY29t; Yan Jiang, aHhobGp5MjAxOEAxNjMuY29t
†These authors have contributed equally to this work
 Feng Chen
Feng Chen Miao Wang2*†
Miao Wang2*† Yan Jiang
Yan Jiang