
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
BRIEF RESEARCH REPORT article
Front. Public Health, 18 December 2023
Sec. Children and Health
Volume 11 - 2023 | https://doi.org/10.3389/fpubh.2023.1250259
This article is part of the Research TopicInternational Day of Persons with Disabilities – Children’s DisabilitiesView all 25 articles
American Academy of Pediatrics (AAP) recommendations for Autism Spectrum Disorder (ASD) screening do not specifically address safety-net clinics, which provide multidisciplinary healthcare services to underserved patients. This project explored the potential for ASD screening in safety-net clinics by assessing parental perceived knowledge of ASD at JayDoc Free Clinic, a student-run safety-net clinic in Wyandotte County, Kansas. May through December 2022, patients who reported to be the parent of a minor received a demographic survey and a Likert-style questionnaire assessing perceived knowledge of ASD, including understanding the importance of ASD screening and ASD signs and symptoms. Responses were categorized into positive, negative, and unsure. Demographic variables included the minor’s primary care provider (PCP) status. Results were analyzed using bivariate analysis, with chi-square tests for significance (p-value ≤ 0.05). Of the 52 participants who completed at least one Likert response, 55.8% reported their child had a PCP. Responses were somewhat balanced with 44.2% positive for understanding the importance of ASD screening and 53.8% positive for understanding ASD signs and symptoms. For understanding the signs and symptoms of ASD, an unsure response (32.7% of responses) was statistically associated with a lack of PCP (p = 0.017). The balance of positive with negative and unsure responses could reflect lack of ASD knowledge and may relate to healthcare inaccessibility. This is consistent with the significant association between lack of PCP and unsure responses for understanding ASD signs and symptoms. ASD screening and education in safety-net clinics like JayDoc could be valuable, particularly for children without a PCP.
Autism Spectrum Disorder (ASD) is a developmental disorder affecting social communication and interaction and accompanied by restricted repetitive behavior (1). With a prevalence of 1 in 59 children, early diagnosis and treatment of this disorder is crucial for children and their families (2). The American Academy of Pediatrics (AAP) advises ASD screening at the 18 and 24-month well-child checks, which are regularly scheduled visits with primary care providers (PCP) to screen for development and growth. As a result, most ASD screening occurs at primary health care visits for children (2).
However, there is a gap in advice for those receiving care at safety-net clinics. These clinics are places that provide healthcare to uninsured and other vulnerable populations, regardless of their ability to pay (3). State health insurance through Medicaid is available to all children born in the United States. Yet, people born outside of the United States often do not qualify for state-funded health insurance and therefore frequently access healthcare through safety-net clinics (4). In a rural Hispanic community that has access to safety-net clinics, patients still felt their preventative health needs were not being met (5). Thus, infrequent access to preventative healthcare for uninsured families could create a knowledge gap on general preventative services such as ASD screening.
Past literature has shown how screening correlates to more diagnoses of ASD among different socioeconomic statuses. In the United States, ASD rates are higher in families with higher socioeconomic status (6). However, in countries like Sweden with universal access to healthcare, lower socioeconomic status correlated with higher rates of ASD (7). This discrepancy suggests that in the United States, children of higher socioeconomic status receive appropriate ASD screening, while those of lower socioeconomic status may be falling through cracks in ASD identification and care.
With an understanding of the healthcare disparities associated with ASD, this project aimed to assess parental self-rated knowledge of ASD screening in a free clinic setting, with the goal of discerning the potential gaps in healthcare for this patient population.
During May through December 2022, participants were recruited from JayDoc Free Clinic, a free, student-run safety-net clinic affiliated with the University of Kansas School of Medicine in Wyandotte County, Kansas City, Kansas. Patients were recruited from the JayDoc’s walk-in and specialty clinics on Mondays, Tuesdays, and Wednesdays from 5 to 9 p.m.
Patients who had a child under 18 and were willing to participate in the study were given a two-part form, available in English and Spanish, to fill out and hand back at the end of their visit. The form contained a demographics survey including zip code, county of residence, ethnicity, marital status, education level, employment status, household language, insurance status, household income, number of children, and primary care provider status of their children. It also contained a Likert questionnaire of eight questions written by the study authors about the patient’s self-perceived knowledge of ASD and the importance of ASD screening. Response options included strongly agree, agree, disagree, strongly disagree, and not sure. Participants were not offered compensation and assured that their choice to participate would not affect their care. This project was approved by the University of Kansas IRB for a quality improvement (QI) study.
Following data collection, responses were categorized into positive (strongly agree, agree), negative (strongly disagree, disagree), and unsure. After data collection, the authors chose three questions for data analysis to focus the study on the impact of PCPs on ASD awareness. The authors did not analyze the other five questions. Responses to the three questions were examined closely in association with the child’s PCP status. Analysis occurred via R-studio using Pearson’s Chi-square (ꭓ2) test for independence. All tests were ran assuming a significance level α = 0.05.
Of 73 participants who initiated surveys, 52 completed at least one Likert response. Of the 52 participants, 29 (55.8%) reported their child had a PCP. 69.8% of patients selected Wyandotte County, Kansas as their county of residence. Most surveyed identified as Hispanic or Latino (n = 39, 75%) and selected Spanish as their primary household language (n = 32, 61.5%). Additionally, 59.6% of participants reported their insurance status as “uninsured/none.” However, this question had a 26.9% non-response rate. Demographic data is reported in Table 1.
When responding to whether participants’ knowledge on ASD comes from healthcare providers, Figure 1 indicates those whose children do not have a PCP chose mostly unsure responses, followed by positive and negative responses (52.2, 39.1 and 8.7%, respectively) with a p-value of 0.098. Responses for understanding the importance of ASD screening showed that those with no PCP had balanced responses between unsure (47.8%) and positive (43.5%), as shown in Figure 2. Those with a PCP responded with more positive responses overall (44.8%) with even balance between negative and unsure responses (27.6% each) with a p-value of 0.148. Finally, the child’s PCP status was examined in relation to parental awareness of the signs and symptoms of ASD. For this, those without a PCP reported mostly unsure and positive responses (52.2 and 43.5%, respectively). For those with a PCP there was a 62.1% rate of positive responses, resulting in a significant difference between the groups of PCP vs. no PCP (p = 0.017), reported in Figure 3.
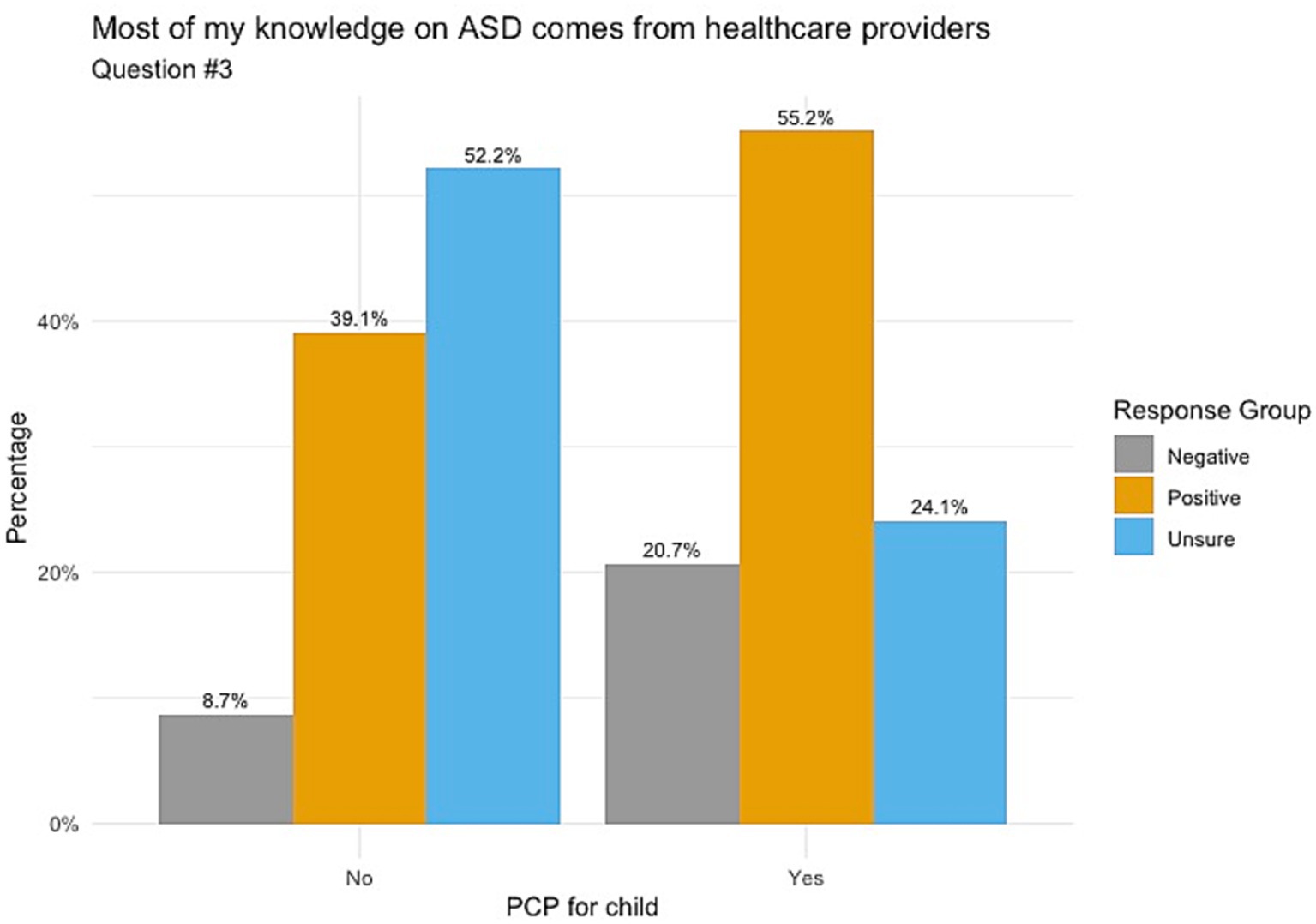
Figure 1. Knowledge of ASD from healthcare providers correlated with child’s PCP status. Non-significance between these groups was found with a p-value of 0.098.
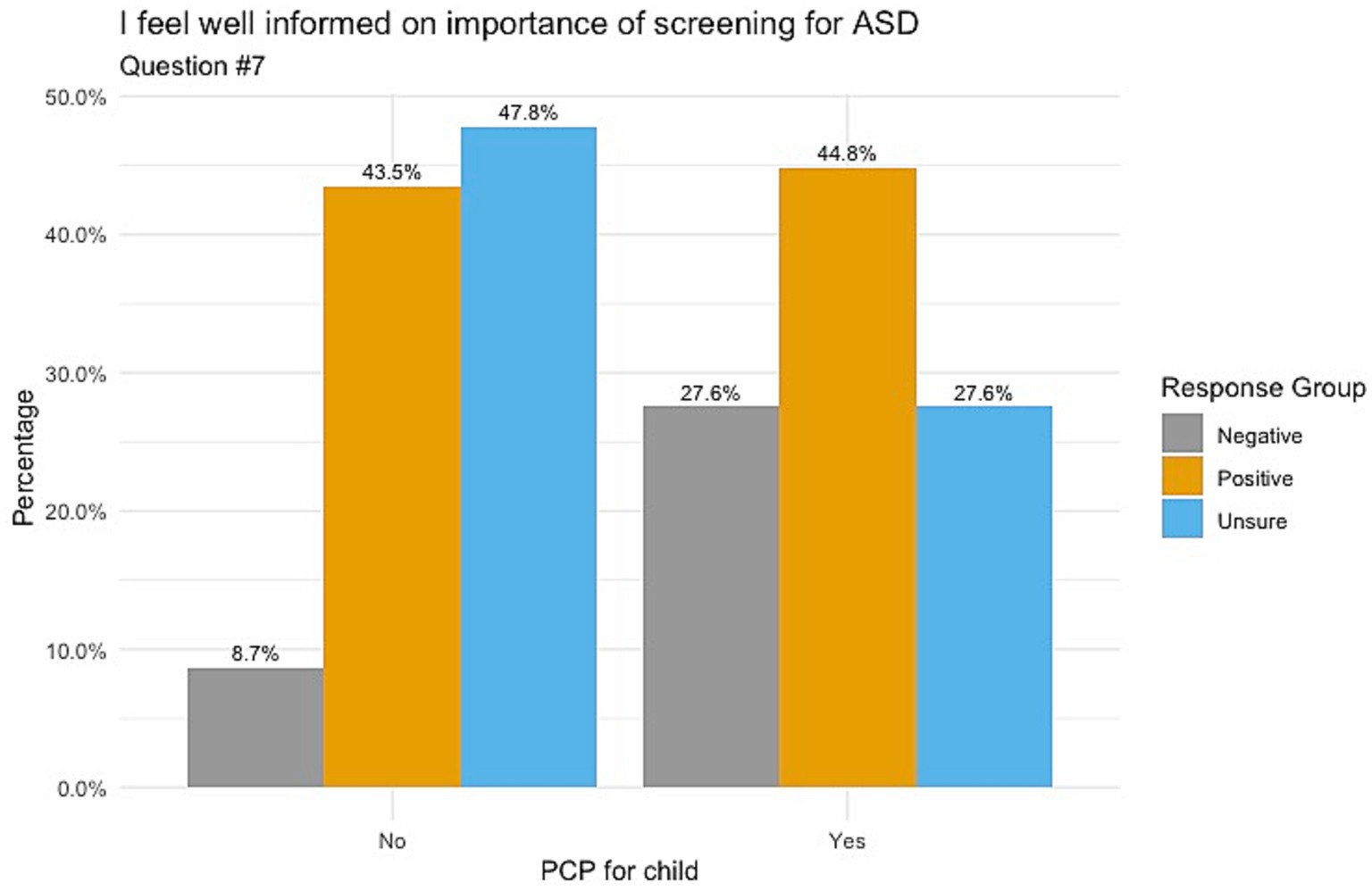
Figure 2. Feeling informed on the importance of ASD screening correlated with child’s PCP status. Non-significance between these groups was found with a p-value of 0.148.
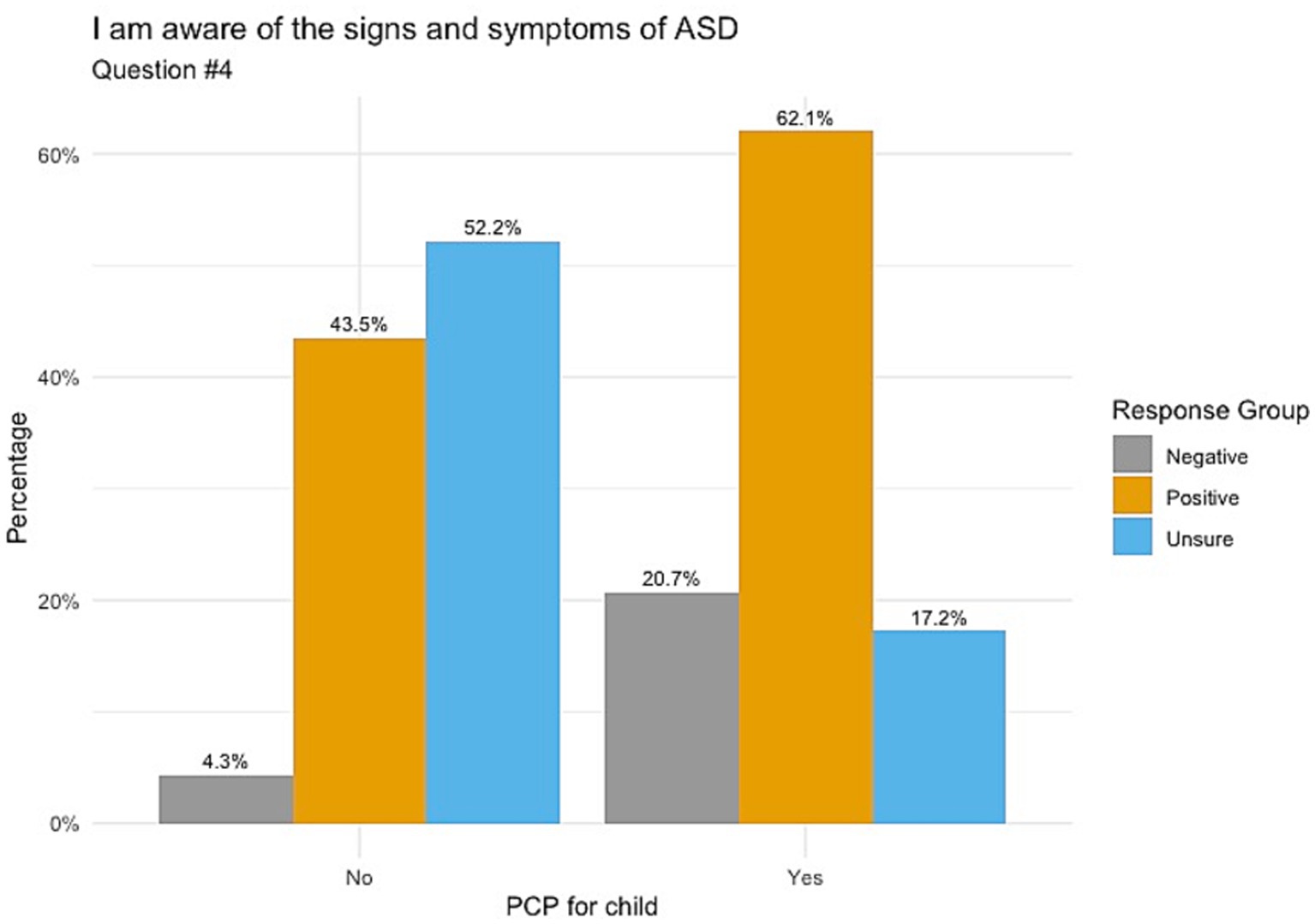
Figure 3. Awareness of signs and symptoms of ASD correlated with child’s PCP status. Significance between these groups was found to give a p-value of 0.017.
Overall, these results indicate adults with children who access safety-net clinics feel unsure about their knowledge of ASD and autism screening, particularly if their child lacks a PCP. As a result, their children may be missing out on this crucial screen, resulting in a lack of access to services.
Given the intrinsic nature of safety-net clinics in caring for underserved populations, it is not surprising that 59.6% of participants lacked health insurance, and 26.9% of participants left the question blank altogether. The insurance status of the participants may help explain why only 55.8% of participants reported having a PCP for their child. While children are generally more likely to have health insurance than their parents, socioeconomic barriers affect whether children can access healthcare even with insurance (8). Those of low socioeconomic status are more likely to rely on safety-net clinics for primary care needs than traditional physician offices (9). Thus our finding that many participants did not have a PCP for their child points to the socioeconomic circumstances that lead people to safety-net clinics such as JayDoc. Additionally, the percentage of children with a PCP at JayDoc Clinic (55.8%) was not significantly different than that of the United States (47.0%) or Kansas (51.9%) as a whole (10).
The balance of positive responses with negative and unsure responses to questions about ASD could reflect lack of ASD knowledge and may relate to healthcare inaccessibility. Additionally, the significant association between a lack of PCP and unsure responses for understanding ASD signs and symptoms points to the importance of providers in promoting awareness and screening. This finding is in accordance with a previous study conducted in a safety-net clinic that examined barriers to colorectal cancer screening and found that provider communication impacts frequency of screening (11). While safety-net clinics can sometimes serve as PCPs, there is often discordance in the services they can typically provide. JayDoc, for example, is not able to provide longitudinal care to patients with the same healthcare provider due to rotating volunteer physicians. Benefits of PCPs, as indicated by our findings, include increased awareness of ASD among parents.
Limitations of this study include generalizability to populations outside the United States. Insurance status in the United States for adults under age 65 depends on citizenship and employment. Lacking health insurance makes regularly accessing healthcare unaffordable for many, causing these people to access healthcare through safety-net and free clinics. Many other countries have systems that prevent this care gap which could lead to better access to primary care providers. Another limitation is that survey distribution depended on cooperation from front-office staff. Dependence on front-office staff may have led to bias and consistency in the distribution of the surveys. Thirdly, of the 73 patients surveyed, 52 respondents submitted at least one answer. This lack of response suggests that some respondents missed a large portion of the survey due to printing on two sides of the paper or needing more time to complete the survey. Finally, the authors conducted this survey in Wyandotte County, Kansas, which ranks at 103rd out of 104 counties in Kansas for health outcomes, including life expectancy (12). These differences in health outcomes may be due to a lack of health literacy. The lack of awareness regarding ASD may be from poor health literacy in addition to poor access to primary care.
Our findings demonstrate that the assessment of PCP status of patient’s children could be helpful in guiding referrals to PCPs from safety-net clinics. Most patients who are seen at JayDoc are adults, thus JayDoc primary care referrals are currently focused on adult providers. The discovery that a significant number of participants lacked a designated primary care physician for their child, coupled with the observation that pediatric PCPs enhance ASD awareness, underscores the importance of advocating for referrals to pediatric PCPs. Asking about patients’ children and assessing socioeconomic barriers to PCPs could improve referral to pediatric providers. Additionally, ASD screening and education at JayDoc could be valuable, particularly for children without a PCP.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
RS and MO’D contributed to conception and design of the study. MO’D created the data-file. RS performed the statistical analysis. FB provided significant guidance throughout the study. RS, MO’D, and FB wrote the first draft of the manuscript. All authors contributed to the article and approved the submitted version.
The article processing charges related to the publication of this article were supported by The University of Kansas (KU) One University Open Access Author Fund sponsored jointly by the KU Provost, KU Vice Chancellor for Research, and KUMC Vice Chancellor for Research and managed jointly by the Libraries at the Medical Center and KU - Lawrence.
This paper and the research behind it would not have been possible without the members of the 2022 executive board of JayDoc Free Clinic, and Allen Keith Greiner, MD at the University of Kansas School of Medicine for their assistance with data collection and guidance throughout the project. We would also like to acknowledge and thank the patients of JayDoc Free Clinic who were willing to participate in the research behind this paper.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: DSM-5-TR. 5th ed. Washington, DC: American Psychiatric Association Publishing (2022).
2. Hyman, SL, Levy, SE, and Myers, SM. Identification, evaluation, and management of children with autism spectrum disorder. Pediatrics. (2020, 2020) 145:e20193447. doi: 10.1542/peds.2019-3447
3. Lewin, ME, and Altman, SH., Institute of Medicine (U.S.). America’s Health Care Safety Net: Intact but Endangered. Washington, DC: Institute of Medicine: National Academy Press (2000).
4. Staiti, AB, Hurley, RE, and Katz, A. Stretching the Safety Net to Serve Undocumented Immigrants: Community Responses to Health Needs. Issue Brief Cent Stud Health Syst Change. (2006):1–4.
5. Leon, JJ, Guthrie, KK, Rueda, C, De la Cruz, D, and Montoya-Williams, D. Pediatric healthcare needs and barriers self-reported by a rural hispanic community. Cureus. (2020) 12:e11999. doi: 10.7759/cureus.11999
6. Durkin, MS, Maenner, MJ, Baio, J, Christensen, D, Daniels, J, Fitzgerald, R, et al. Autism spectrum disorder among US children (2002-2010): socioeconomic, racial, and ethnic disparities. Am J Public Health. (2017) 107:1818–26. doi: 10.2105/AJPH.2017.304032
7. Rai, D, Lewis, G, Lundberg, M, Araya, R, Svensson, A, Dalman, C, et al. Parental socioeconomic status and risk of offspring autism spectrum disorders in a swedish population-based study. J Am Acad Child Adolesc Psychiatry. (2012) 51:467–476.e6. doi: 10.1016/j.jaac.2012.02.012
8. Lazar, M, and Davenport, L. Barriers to health care access for low-income families: a review of literature. J Community Health Nurs. (2018) 35:28–37. doi: 10.1080/07370016.2018.1404832
9. Hussein, M, Diez Roux, AV, and Field, RI. Neighborhood socioeconomic status and primary health care: usual points of access and temporal trends in a major US urban area. J Urban Health. (2016) 93:1027–45. doi: 10.1007/s11524-016-0085-2
10. KFF “Percent of Children with a Medical Home,” KFF (blog) (2022). Available at: https://www.kff.org/other/state-indicator/children-with-a-medical-home/ (Accessed December 2, 2022).
11. Nagelhout, E, Comarell, K, Samadder, NJ, and Wu, YP. Barriers to colorectal cancer screening in a racially diverse population served by a safety-net clinic. J Community Health. (2017) 42:791–6. doi: 10.1007/s10900-017-0319-6
12. University of Wisconsin Population Health Institute. Kansas | County Health Rankings & Roadmaps 2023. Available at: https://www.countyhealthrankings.org/explore-health-rankings/kansas?year=2023&tab=0.
Keywords: autism spectrum disorder, developmental screening, primary health care, physicians, primary care, free clinics, perception, safety-net providers
Citation: O’Donnell MT, Schmidt RB and Butler FM (2023) The impact of primary care access on autism spectrum disorder awareness in an underserved population. Front. Public Health. 11:1250259. doi: 10.3389/fpubh.2023.1250259
Received: 29 June 2023; Accepted: 24 November 2023;
Published: 18 December 2023.
Edited by:
Olaf Kraus de Camargo, McMaster University, CanadaReviewed by:
Mackenzie Salt, McMaster University, CanadaCopyright © 2023 O’Donnell, Schmidt and Butler. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Randall B. Schmidt, cnNjaG1pZHQ4QGt1bWMuZWR1
†These authors have contributed equally to this work and share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.