- 1School of Nursing, Yunnan University of Chinese Medicine, Kunming, Yunnan, China
- 2The First People's Hospital of Yunnan Province, Kunming, Yunnan, China
- 3Postdoctoral Research Station of Public Administration, Yunnan University, Kunming, Yunnan, China
Objective: Cognitive frailty (CF) is characterized by physical frailty and potentially reversible cognitive impairment without Alzheimer’s disease and other dementias. Clarifying the prevalence and related factors of cognitive frailty can help researchers understand its epidemiological status and formulate intervention measures. This study aims to conduct a systematic review and meta-analysis of the prevalence and related factors of CF in diabetic patients in Chinas to better understand the current status of CF in diabetic patients in China and develop effective intervention measures for related factors.
Methods: PubMed, Web of Science, Embase, Cochrane Library, CNKI, Weipu(VIP), WANFANG, China Biology Medicine (CBM) and DUXIU were searched to collect epidemiological data on Chinese diabetic patients. Articles published through May 29, 2023, were searched. The number of diabetes with CF and the total number of diabetes in the included studies were extracted to estimate the prevalence of diabetes with CF. For factors related to diabetes with CF, odds ratios (OR) and 95% confidence intervals (CI) were used for estimation.
Results: A total of 248 records were screened, of which 18 met the inclusion criteria. The results of meta-analysis showed that the prevalence of Chinese diabetic patients with CF was 25.8% (95% CI = 19.7 to 31.9%). Subgroup analysis showed that hospital prevalence was higher than in the community and in women than in men. Combined estimates showed that depression, malnutrition, advanced age (≥70, ≥80), combined chronic diseases ≥4 and glycated hemoglobin ≥8.5 were risk factors for CF in diabetics patients in China, with regular exercise and high education level (≥ college) as protective factors.
Conclusion: Cognitive frailty was common in diabetic patients in China. Such populations should be screened early and intervened with relevant factors.
Systematic review registration: A systematic review of this study evaluated the registered websites as https://www.crd.york.ac.uk/PROSPERO/, CRD42023431396.
1. Introduction
Diabetes is a common chronic disease. The latest data from the International Diabetes Federation (IDF) in 2021 showed that the number of people with diabetes in the world was 537 million, which is expected to increase to 643 million by 2030 (1), and the related expenditure was US $966 billion, accounting for 11.5% of the total global health expenditure. The health problems of patients with diabetes deserve the attention of medical and health professionals in all countries. Population aging will increase the expected prevalence of diabetes by 16%. As the country with the largest number of diabetes patients, China will face certain medical pressure, and the health problems of diabetes patients will be more prominent.
Physical frailty and cognitive impairment are common symptoms in the older adults (2). Frailty refers to a physiological syndrome in which multiple systems of the body are dysfunctional, resulting in decreased physiological reserve and increased susceptibility to stimulation (3). Cognitive impairment is considered to be the early stage of dementia, and the lack of cognitive ability will lead to the impairment of daily function of patients (4). With the progress of research, more studies have found that there is a certain correlation between physical frailty and cognitive impairment (5). Therefore, the concept of CF has been proposed. The concept of CF was first proposed in 2013 (6) and is defined as the coexistence of physical frailty and cognitive impairment in the absence of other neurological diseases such as Alzheimer’s disease. Ruan et al. proposed two subtypes of CF in 2015 (7): reversible CF, which refers to the existence of subjective cognitive decline and/or related markers on the basis of physical frailty; and potentially reversible CF refers to physical frailty accompanied by mild cognitive impairment. The concept of CF is more conducive to the transformation of the assessment method of the older adults from single-dimensional to multidimensional and the maintenance of the physical and mental health of older adults individuals.
In the mechanism of CF, there is a bidirectional relationship between physical frailty and cognitive impairment, which affect and promote each other, forming a vicious circle of decline in physical function and cognitive function of the older adults (8, 9). On this basis, hypoglycemic events and sarcopenia in diabetic patients can be used as facilitating and linking links in this process. Hypoglycemic events: Abdelhafiz et al. (10) suggested a bidirectional relationship between hypoglycemia and physical frailty and cognitive impairment. In terms of cognitive function, hypoglycemia events can increase the risk of cognitive dysfunction in patients, and cognitive dysfunction may reduce self-care and rational drug use and increase the risk of blood glucose fluctuation. In terms of physical frailty, diabetic patients with frequent hypoglycemia are often complicated with diseases, malnutrition, weight loss and have potential physical frailty. Diabetic patients with physical frailty have a higher risk of hypoglycemia due to reduced physiological reserve. Sarcopenia: Hormone deficiency (11), neuropathy (12) and chronic inflammation (13) caused by diabetes can affect the growth and metabolism of skeletal muscle cells, reduce muscle mass and delay muscle regeneration, leading to an increased risk of sarcopenia. Sarcopenia can also lead to an increased risk of physical frailty and cognitive impairment in patients (14, 15).
CF can not only predict adverse health outcomes in the older adults but also increase the risk of adverse health outcomes. A 7-year follow-up study found that older adults people with CF had increased cumulative length of hospital stay compared with healthy older adults people (OR = 1.48) (16). A study of older adults in an Italian community showed that people with CF had more severe physical activity impairments than healthy older adults (17). Rivan et al. (18) showed that CF was not only an influencing factor for falls in the older adults (OR = 2.98, 95% CI: 1.78–4.99) but also significantly predicted the incidence of disability (OR = 5.17, 95% CI: 1.11–24.21). The results of another meta-analysis showed that CF may be an early sign of the onset of dementia and is an important predictor of dementia (19). Feng et al. used a 3-year prospective cohort study and concluded that CF significantly increased the risk of death in the older adults (OR = 5.12, 95% CI: 3.00–8.74) (20). However, CF is reversible (7). Early screening and intervention of diabetic CF patients will help patients restore normal cognitive function, maintain self-care ability, delay or prevent dementia, and reduce the occurrence of adverse health events.
Since the concept of CF was systematically proposed in 2013, the number of related studies has been increasing, while the research progress in China is relatively backward. Although many epidemiological studies have been conducted to further understand the prevalence and associated factors of CF, there are currently insufficient studies on the prevalence and associated factors of CF in diabetic patients. To improve the attention of Chinese medical workers and facilitate the promotion of related research progress, it is necessary to conduct a meta-analysis on the current epidemiological status of CF in diabetic patients in China. Based on the reversibility of CF, clarifying the related factors between diabetic patients and CF will help to carry out relevant intervention research to improve the coping ability of this group to maintain their own health.
Many epidemiological studies have been conducted in China to further understand the prevalence and related factors of CF, but there are still insufficient studies on the prevalence and related factors of CF in diabetic patients. Therefore, this study aims to systematically evaluate the current status of CF in diabetic patients in China and analyze the prevalence of CF in diabetic patients by gender, age, region and education level to provide evidence for the development of health intervention measures and the government to formulate relevant public health strategies.
2. Method
This systematic review and meta-analysis was conducted according to the Preferred Reporting Item (PRISMA) updated guidelines for systematic reviews and meta-analyses (21). The protocol has been registered in the International Prospective Register of Systematic Reviews (PROSPERO) and the registration number is CRD42023431396.
2.1. Search strategy
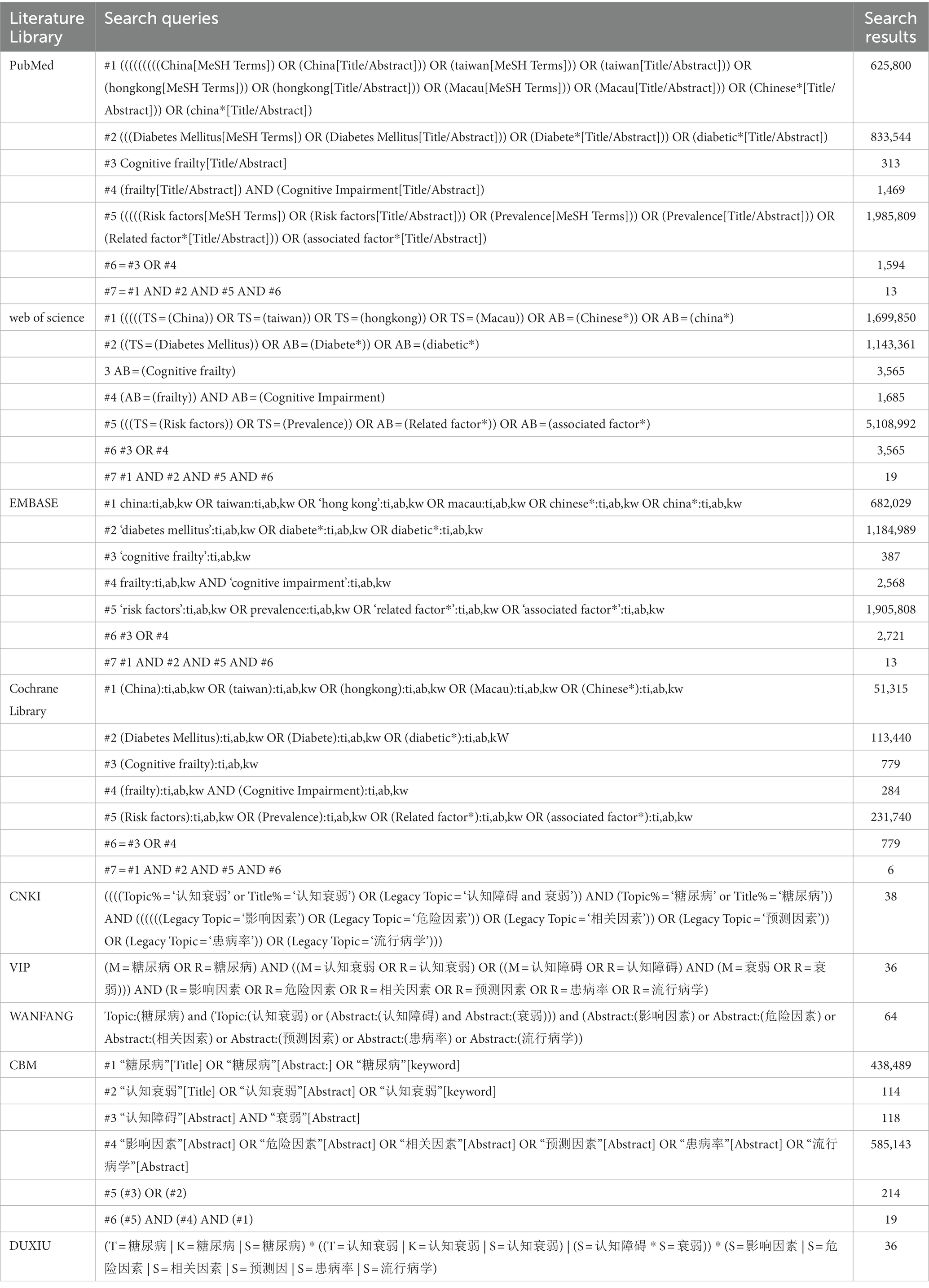
PubMed, Web of Science, Cochrane Library, Embase, CNKI, Wanfang (VIP), China Biology Medicine disc (CBM), and DUXIU were searched for articles published up to May 29, 2023. Because CF topics are relatively new in the scientific literature, no time limits were used. The search was conducted using Medical Subject Headings (MeSH) and free terms, including Diabetes Mellitus, Diabete*, Cognitive Frailty, frailty, Cognitive Impairment. In addition, the search was extended by handsearching the reference lists of relevant studies, including reviews and included studies. The search strategy is shown in Table 1.
2.2. Inclusion and exclusion criteria
Inclusion criteria were based on the PICO process: (1) The patient was diagnosed with diabetes; (2) Cross-sectional, case–control, or cohort studies; (3) There are clear diagnostic criteria for CF, which are both physical frailty and cognitive dysfunction, and other neuropathic diseases such as Alzheimer’s disease are excluded; (4) The article provides the prevalence of CF in diabetic patients or provides corresponding data that can calculate the prevalence; (5) Research is carried out in China.
The exclusion criteria: (1) duplicate publications; (2) data on outcome indicators could not be extracted; (3) review articles, case reports and letters to the editor; (4) documentation from the same region in the same year.
2.3. Literature screening and data extraction
Import records identified in databases and manual retrievals into Endnote X9.0. Based on the inclusion and exclusion criteria, two review authors independently assessed and screened the titles and abstracts recorded in Endnote X9.0 for inclusion. If there was disagreement, we consulted and discussed or listened to the opinions of third-party evidence-based medicine experts. Data from the included studies were extracted by the same two reviewers using a data extraction table in Excel, including author, year of publication, country, study design, sample size, participant characteristics (age and sex), CF assessment tool, prevalence (numerator and denominator), and relevant factors.
2.4. Qualitative evaluation
Literature quality assessment was conducted by two review authors according to the criteria, and disagreements were resolved by consultation or discussion with a third investigator. The cross-sectional study used the evaluation criteria recommended by the Agency (22), and the AHRQ criteria included 11 items with “yes,” “no” or “unclear.” The cohort study adopted the NOS evaluation criteria of the cohort study (23), and the NOS evaluated the literature through the method of three blocks with a total of 8 items. The evaluation of the quality of the literature adopted the semiquantitative principle of the star system, with a maximum score of 9 stars. The quality of each study was classified as poor, fair, or good.
2.5. Statistical analysis
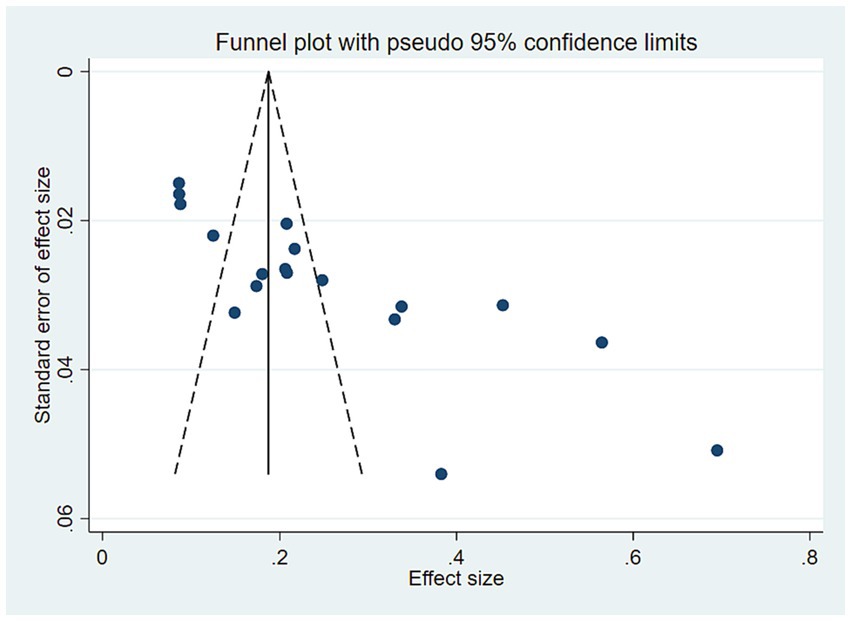
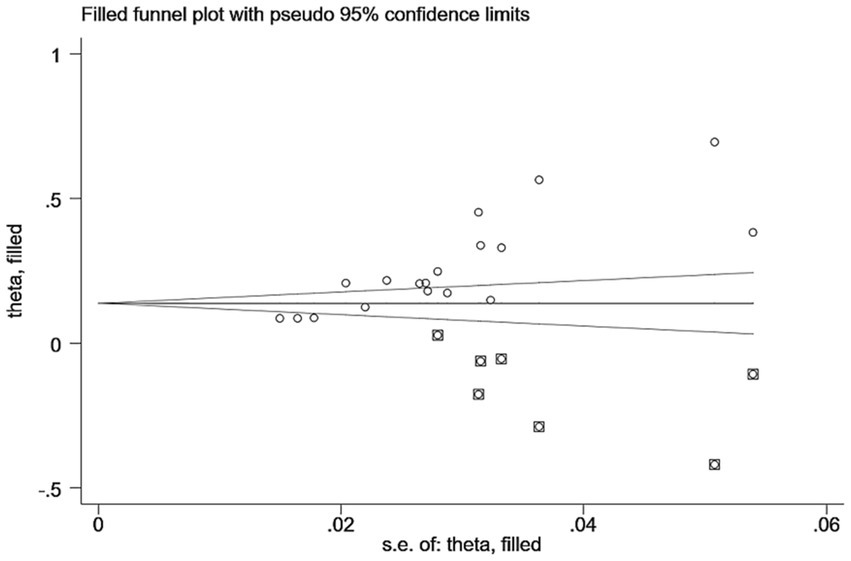
EndNote X9 software was used for file management, an Excel table was used to extract data, and Stata 15.0 was used for analysis. The primary outcomes were the pooled prevalence and 95% confidence interval (CI) of CF in people with diabetes in China, and the factors associated with CF were estimated using the pooled odds ratio (OR) and 95% CI. Cochran’s Q and I2 statistics were used to examine statistical heterogeneity between studies. If the test for heterogeneity detected a statistically significant difference (I2 > 50%), we used a random-effects model; otherwise, we used a fixed-effect model. Begg’s test, Egger’s test, and funnel plots were used to assess publication bias. The significance level of the tests was considered less than 0.05.
3. Results
3.1. Literature screening process and results
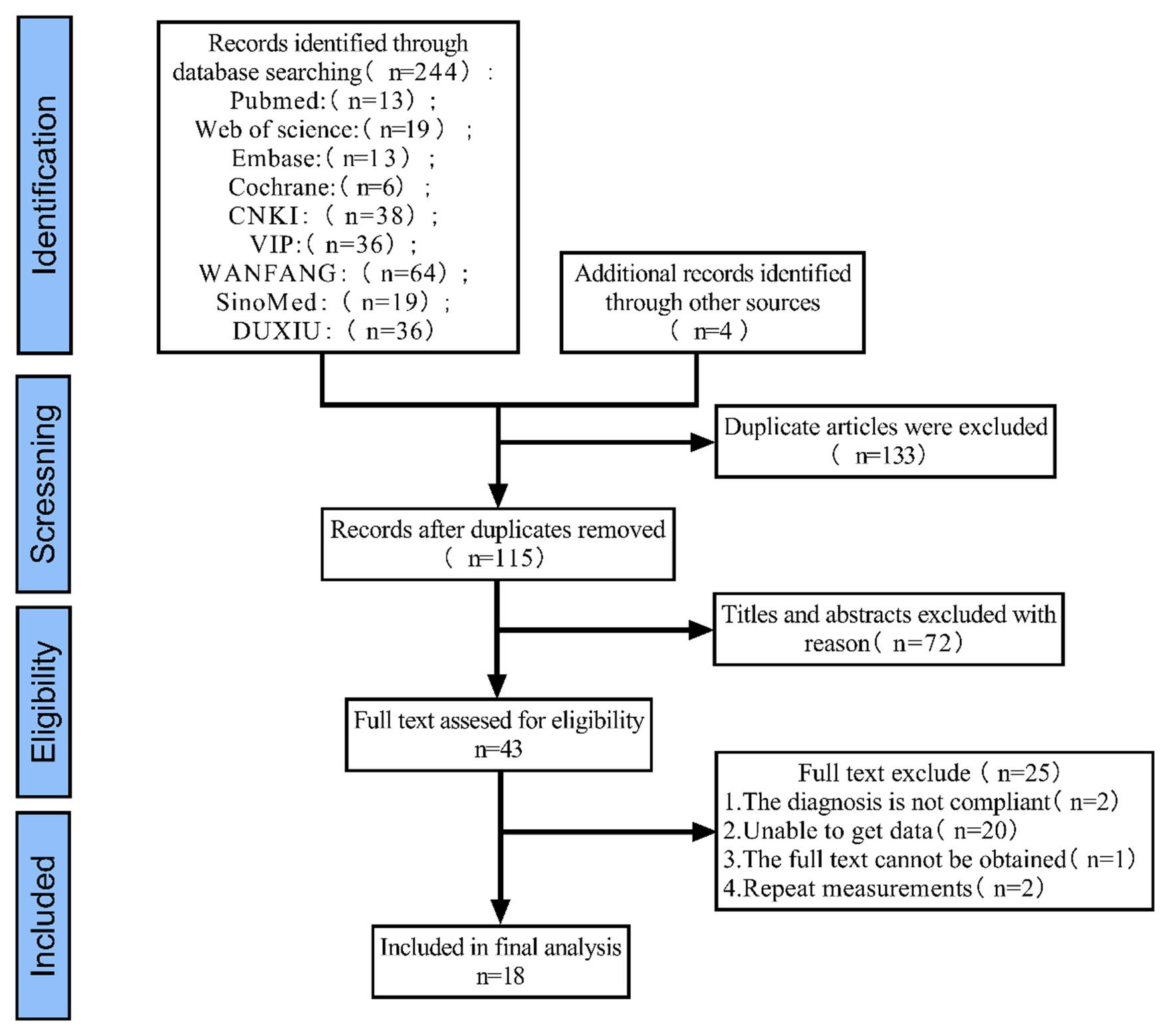
The results are shown in Figure 1, where a database search identified 248 records (the number of studies retrieved was small, which may be related to the fact that there are few studies on CF in diabetic patients in China), of which 133 were duplicates. By reading the title and abstract, 72 studies were eliminated and 43 studies were retained for full-text reading to assess eligibility. Ultimately, 18 studies were included.
3.2. Characteristics and quality evaluation results of the included literature
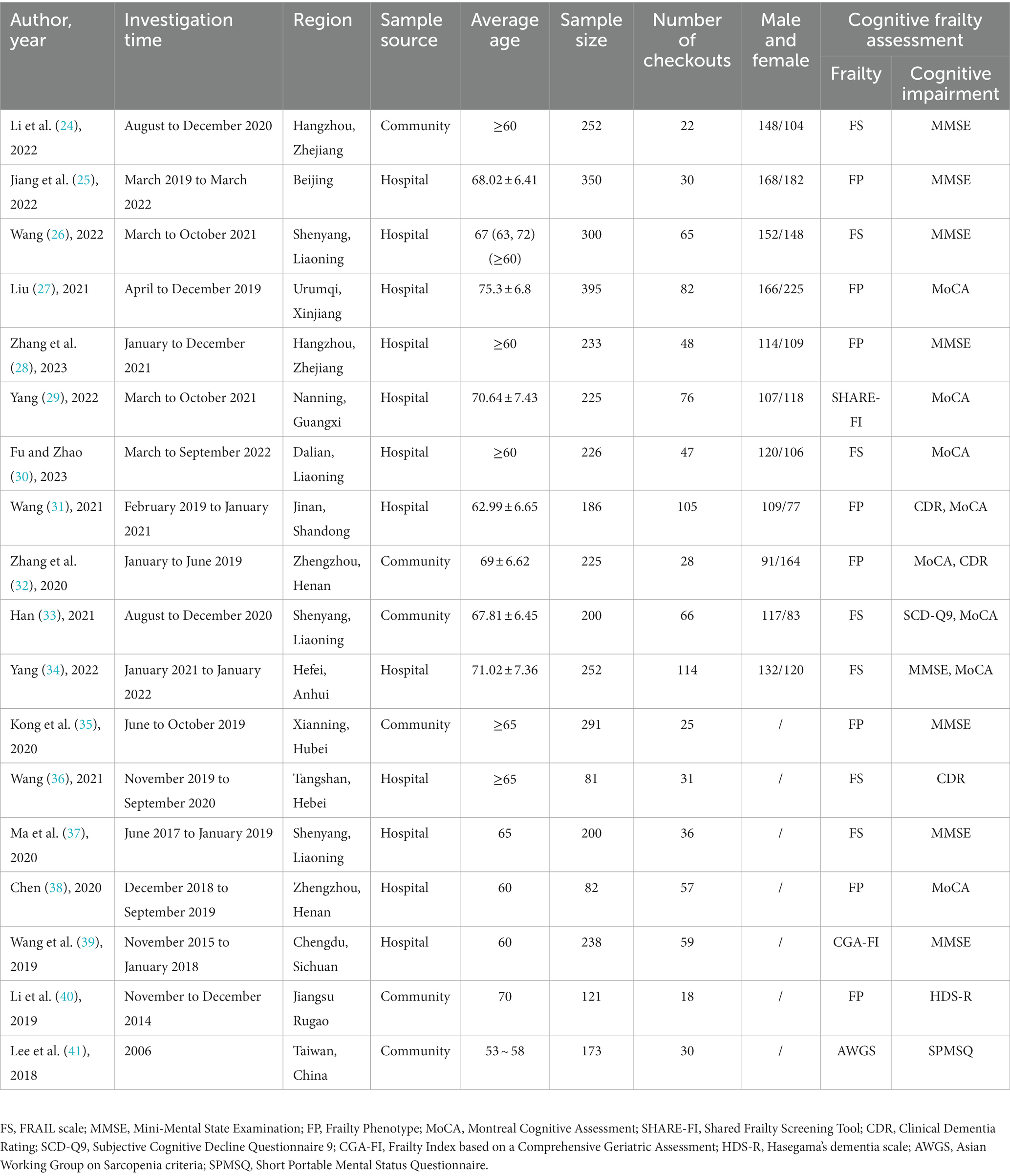
The characteristics of the study are shown in Table 2. A total of 18 studies included 4,030 Chinese people with diabetes, 16 studies had a cross-sectional design, and two studies had a cohort design. Sample sizes ranged from 81 to 395. In the areas where the survey was conducted, there were 8 in the south and 10 in the north. In terms of sample sources, there were 12 hospital sources and 6 community sources. In the diagnosis of CF, the evaluation tools of physical frailty were mainly FS and FP, with 7 and 8, respectively, and others such as SHARE-FI, CGA-FI and AWGS accounted for one each. Four of the cognitive function assessment tools used two different evaluation tools, and the rest were single evaluation tools, 8 studies used MMSE, 8 used MoCA, 3 studies used CDR, and one each used SCD-Q9, HDS-R and SPMSQ. The most commonly used combinations by researchers are FS or FP, MMSE or MoCA.
3.3. Quality appraisal
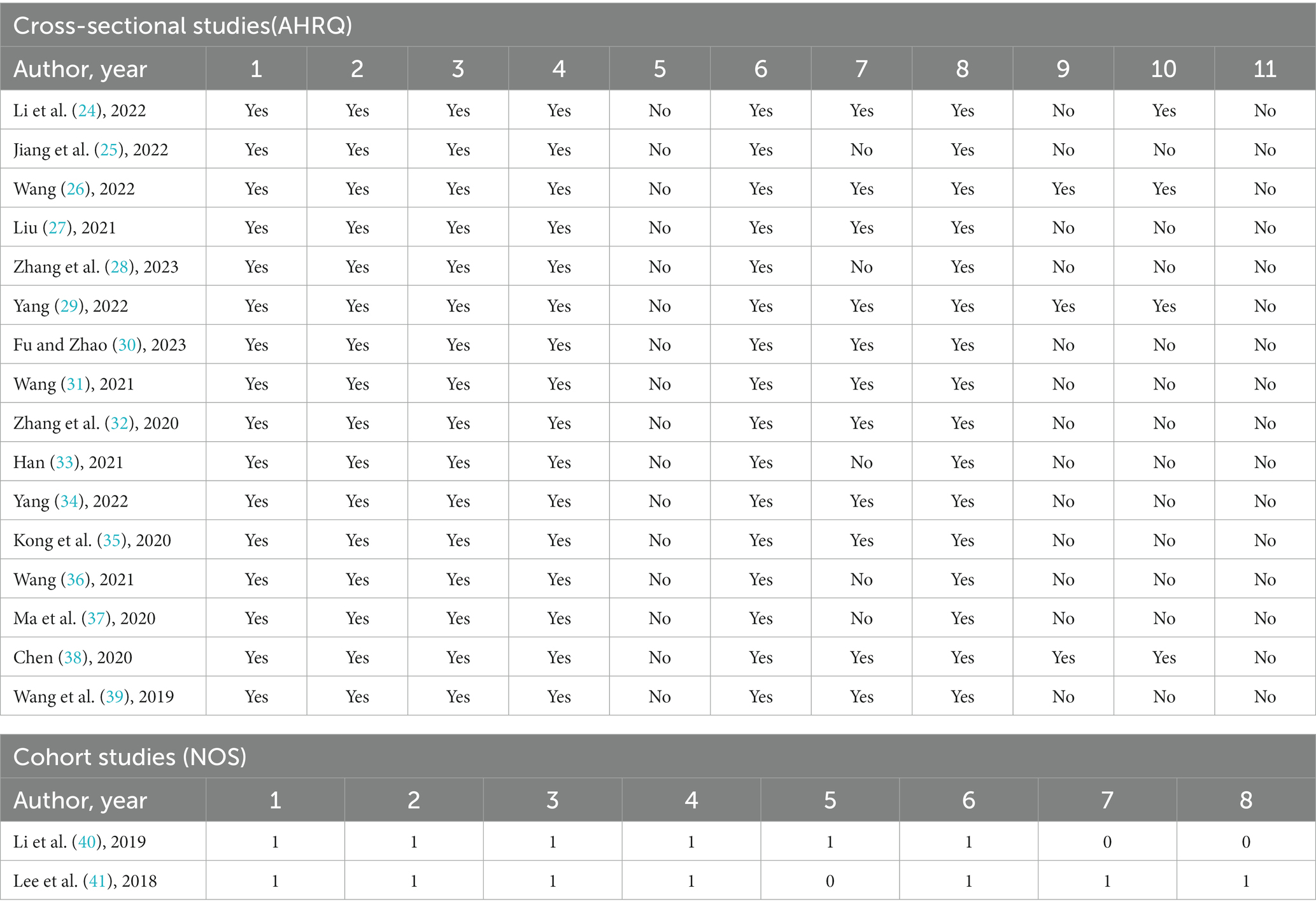
Table 3 lists the assessment of methodological quality of all 18 studies included in this review. Of the cross-sectional studies, four studies were judged to be ‘good’ and 12 to be of ‘fair’ quality. Of the cohort studies, one was considered ‘good’ and one was classified as ‘fair’.
3.4. Meta-analysis
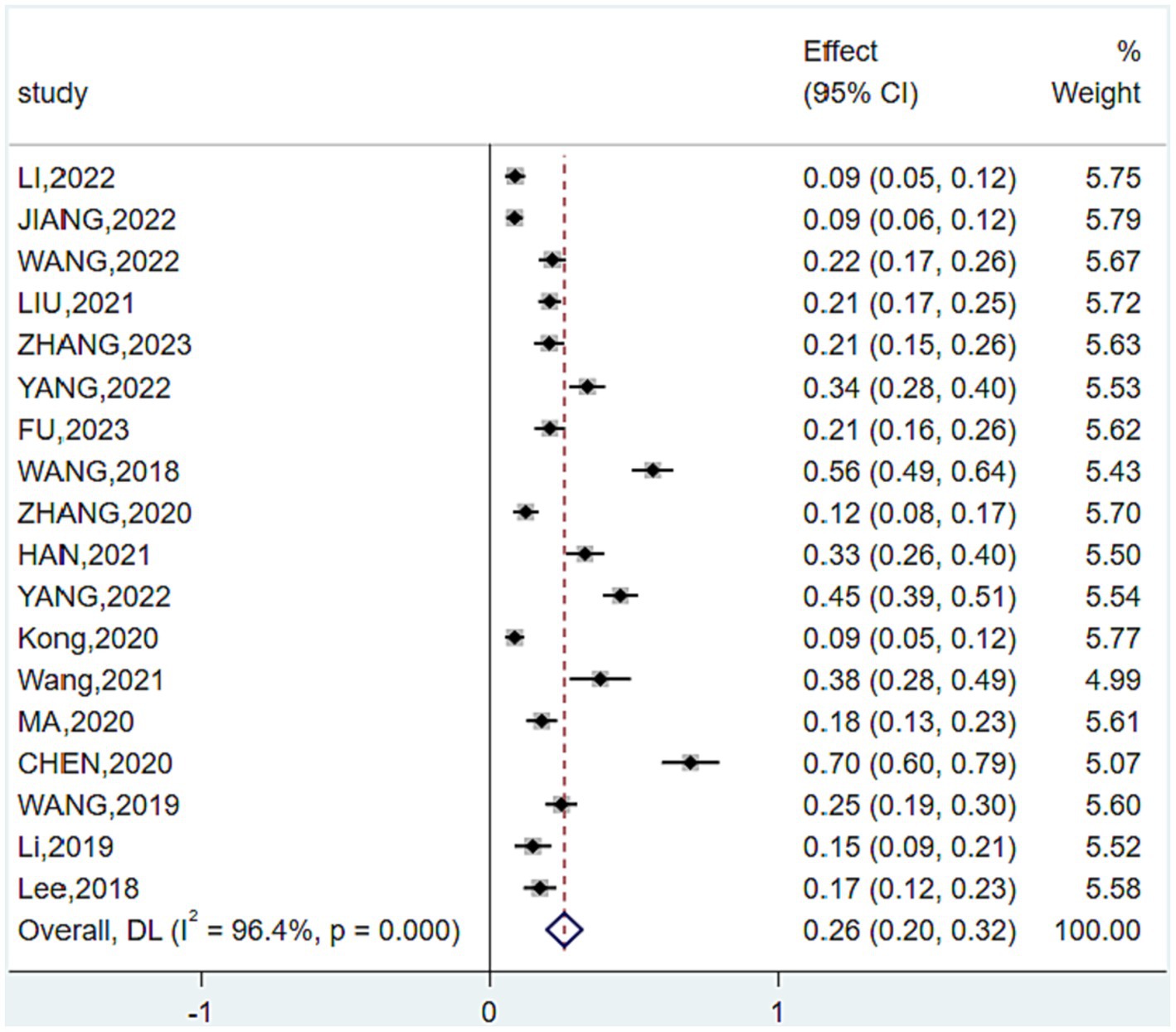
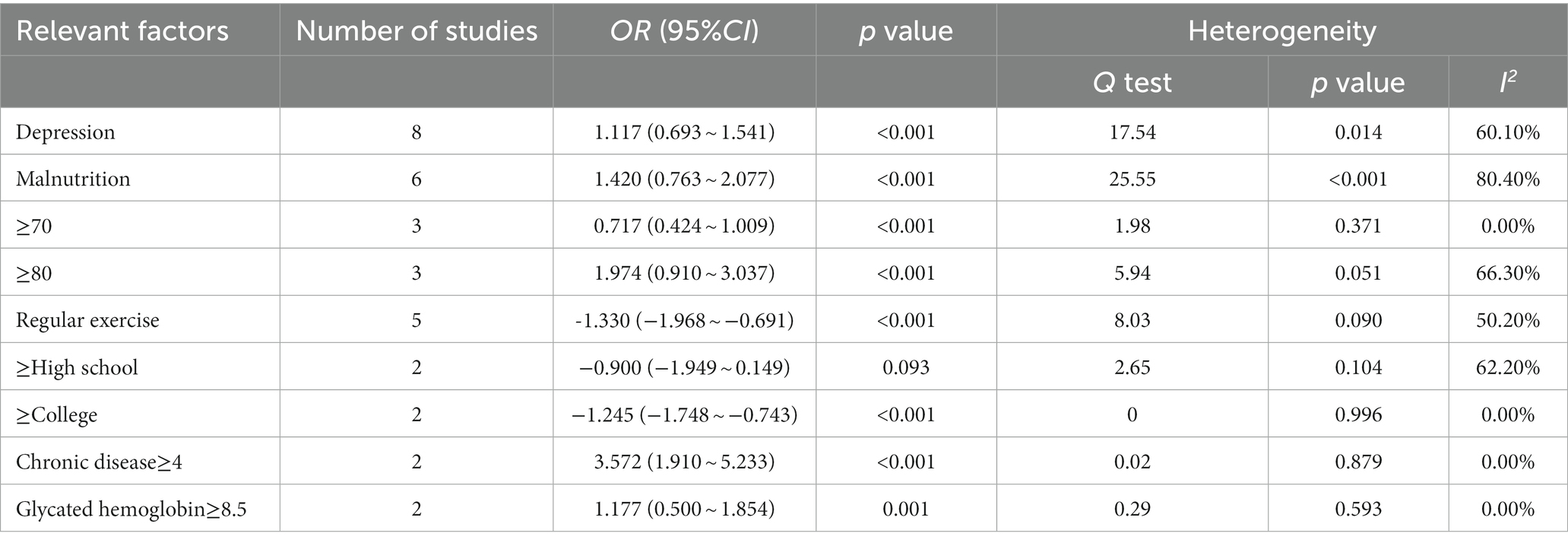
Meta-analysis showed some heterogeneity in the included studies (I2 = 96.4%, p < 0.001), so a random-effects model was used and subgroup analyses were performed to analyze sources of heterogeneity. The forest chart is shown in Figure 2, and the analysis results are shown in Table 4.
Overall prevalence of CF in patients with diabetes in China. A total of 4,030 older adults diabetic patients in China were included in the 18 studies of this study, and 939 diabetic patients with CF were detected. The prevalence of the included studies was 8.60–56.50%. The total number of patients with diabetes and the number of CF patients were compared, and the overall prevalence of CF in Chinese patients with diabetes was 25.8% (95% CI (19.7 to 31.9%)).
Prevalence by sex. A total of 11 studies reported the prevalence of CF in both men and women, men and women prevalence was 23.2% (95% CI (15.1 to 31.3%)) and 26.7% (95% CI (18.3 to 35.1%)); 8 study carried out in the hospital, the hospital male and female CF prevalence was 26.7% (95% CI (1.66 to 3.69%)) and 29.5% (95% CI (4.11 to 5.89%)); 3 study in community, CF men and women with diabetes prevalence was 13.9% (95% CI (0.24 to 2.55%)) and 19.2% (95% CI (0.42 to 3.42%)).
3.4.1. Prevalence by region
Two studies were included in hospitals and 6 were included in the community. The prevalence was 31.1% (95% CI (22.6 to 39.6%)) in hospitals and 25.8% (95% CI (19.7 to 31.9%)) in the community. There were 8 studies in the south and 10 studies in the north, and the prevalence was 29.4% (95% CI (2.01–3.87%)) and 21.6% (95% CI (1.32–3.00%)) in the north and south, respectively. According to hospital location, the prevalence was 31.2% (95% CI (1.99% CI 1.99 to 4.25%)) in northern hospitals and 31.0% (95% CI (2.04–4.16%)) in southern hospitals.
3.4.2. Prevalence by age
There were 7 studies involving patients aged 60 ~ 69 years with a prevalence of 14.7% (95% CI (0.90–2.05%)), 8 studies involving patients aged 70 ~ 79 years with a prevalence of 32.2% (95% CI (1.99–4.45%)), 8 studies involving patients ≥80 years with a prevalence of 57.3% (95% CI (1.13–3.24%)), and a total of 16 studies involving older adults patients aged 60 years ≥ with a prevalence of 24.4%(95% CI(1.85–3.03%)).
3.4.3. Prevalence by educational level
A total of 9 studies included patients with a primary school education and below, with a prevalence of 44.5% (95% CI (2.76 to 6.13%)), 8 included patients with a junior high school degree, with a prevalence of 27.2% (95% CI (1.77 to 3.68%)), 8 included patients with a high school education, with a prevalence of 21.8% (95% CI (1.99 to 4.45%)), and 9 studies included patients with a college education or above, with a prevalence of 0.69% (95% CI (0.15 to 1.22%)).
According to the course. A total of 7 studies included CF in diabetic patients with a course of 1 ~ 9 years, with a prevalence of 26.1% (95% CI (1.37–3.86%)), and a total of 8 studies contained data on diabetic patients with a course of ≥10 years, with a prevalence of 36.2% (95% CI (2.29–4.94%)).
According to the stratified number of combined chronic diseases. A total of 6 studies included data on diabetes patients with 0 ~ 1 chronic diseases, with a prevalence of 21.7% (95% CI (0.82–3.51%)), and a total of 6 studies included data on diabetic patients with ≥2 combined chronic diseases, with a prevalence of 31.5% (95% CI (1.86–4.43%)).
Analysis results of other subgroups. A total of 9 studies included data on diabetic patients with depression, with a prevalence of 41.4% (95% CI (2.55–5.72%)), and 6 studies included data on diabetic patients with malnutrition, with a prevalence of 39.0% (95% CI (2.39–5.40%)).
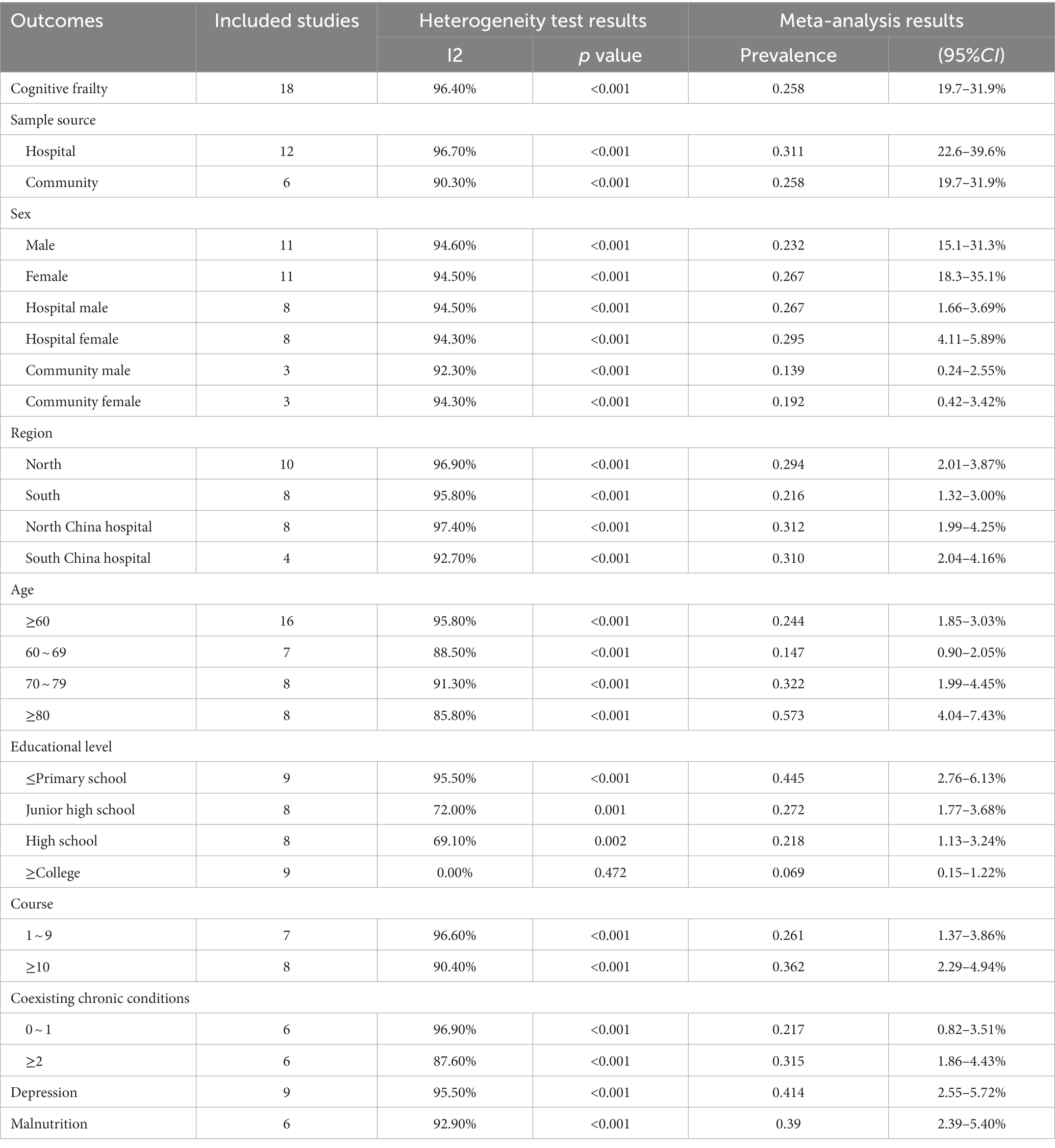
3.5. Analysis of CF related factors in diabetic patients in China
The analysis results of CF related factors in diabetic patients in China are shown in Table 5. The combined estimates showed that depression (OR = 1.117, 95% CI = 0.693 ~ 1.541, p < 0.001), malnutrition (OR = 1.420, 95% CI = 0.763 ~ 2.0771, p < 0.001), age (≥70) (OR = 0.717, 95% CI = 0.424 ~ 1.009, p < 0.001), age (≥80) (OR = 1.974, 95% CI = 0.910 ~ 3.037, p < 0.001), chronic disease≥4 (OR = 3.572, 95% CI = 1.910 ~ 5.233, p < 0.001) and glycated hemoglobin ≥8.5 (OR = 1.177, 95% CI = 0.500 ~ 1.8543, p = 0.001) were risk factors for CF. Education level (college or above) (OR = -1.245, 95% CI = -1.748 ~ −0.743, p < 0.001) and regular movement (OR = -1.330, 95% CI = -1.968 ~ −0.6919, p < 0.001) were protective factors. The pooled data showed that there was no significant difference in the association between education level (high school and above) (p > 0.05).
3.6. Sensitivity analyses and publication bias
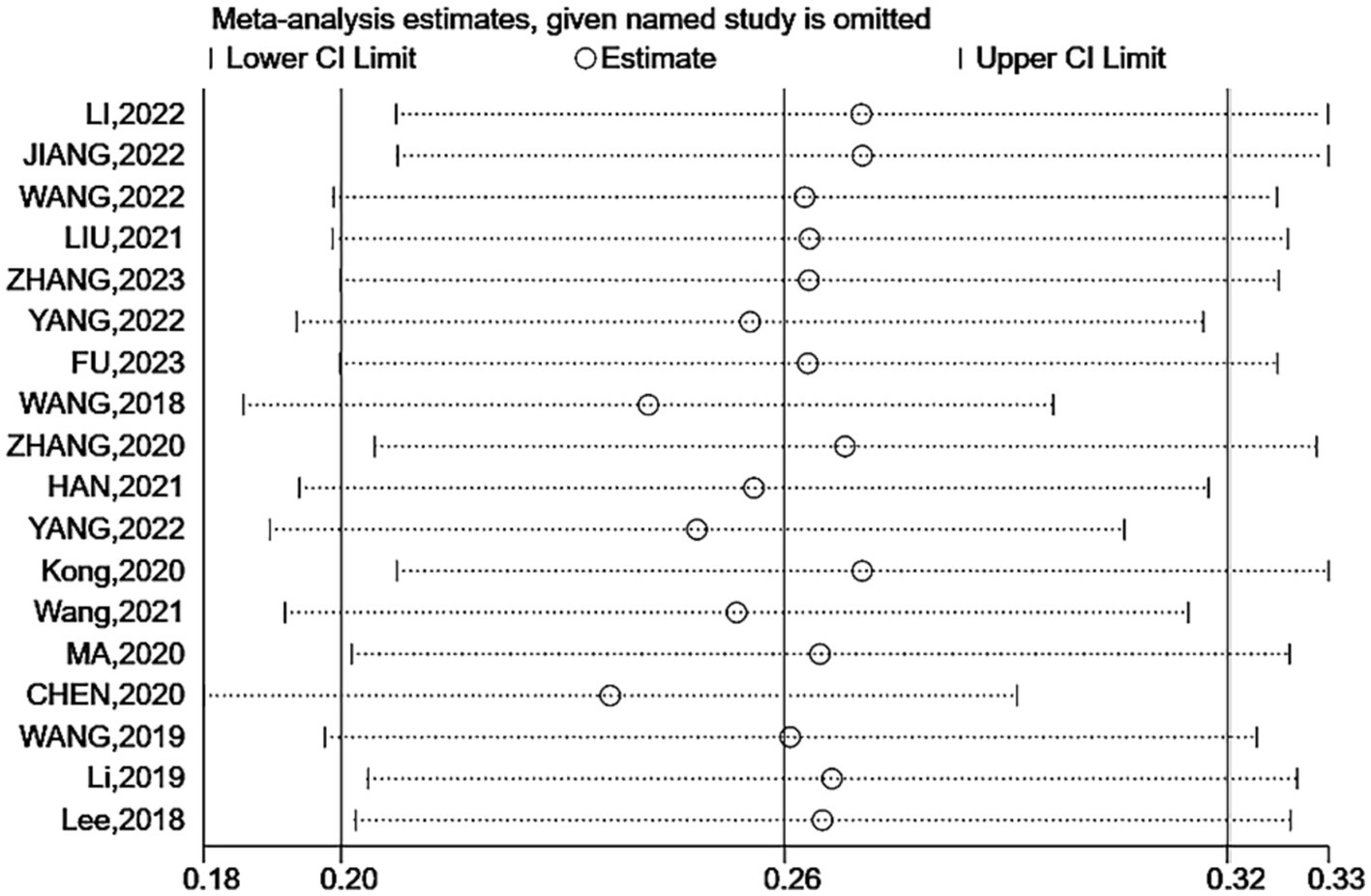
Sensitivity analysis showed no significant change in the combined prevalence of CF after excluding individual studies (Figure 3), indicating stable pooled prevalence results. The funnel shape of the CF prevalence study is essentially symmetrical (Figure 4). Based on the results of the Egger test (p < 0.001) and the Begg test (p = 0.001), it was suggested that the article may have some publication bias. Using the scissification method, it was determined that seven further studies would need to be included in this study to eliminate publication bias (Figure 5).
4. Discussion
Based on 18 studies (4,030 patients), the overall prevalence of CF in diabetic patients in China was 25.8%, and the prevalence of CF in diabetic patients ≥60 years old was 24.4%(the lower prevalence of CF in diabetic patients ≥60 years old may be related to the exclusion of Wang’s study (31) (the study could not extract data ≥60 years old)). The prevalence of CF varies in different countries and institutions according to the survey population and the assessment tool used. The general population prevalence of CF in other countries ranges from 1.0 to 8.9% (17, 20, 42–44), which is much higher in our study. The reasons may include a certain gap between China and developed countries in per capita medical resource occupancy. This generation of Chinese older adults individuals is more likely to engage in manual labor when they are young, have lower education level, are more prone to potential injuries and are less likely to use resources to maintain their health. Patients with diabetes are affected by diseases, and their physical health is more fragile and prone to unhealthy states.
In comparison with the prevalence of their disease CF: one study showed that the prevalence of CF in patients with chronic kidney disease was 15.2% (46), another Chinese study showed that the prevalence of CF in patients with hypertension was 9.8% (47), and this figure was 20.8% in patients with diabetes and hypertension (48), both of which were lower than the 25.8% prevalence of CF in diabetic patients in this study. In terms of more severe diseases, a survey of Korean patients with heart failure showed that the prevalence of CF in patients with heart failure was 34.5% (49), and another study mentioned that the prevalence of CF in older adults patients on dialysis was 35.9% (50), both of which were higher than the results of this study. This suggests that compared with more serious diseases, the physical health of patients with diabetes is relatively better, but compared with other long-term chronic diseases, the impact of diabetes on the occurrence of CF should be given more attention.
In the comparison of the prevalence of CF in patients with diabetes in the community, except for one study in India, which reached 21.8% (51), the prevalence of CF in other countries did not exceed 10% (52–55). The rate of 25.8% in our study was higher than that in other countries, but only India had a similar result. Both China and India have large populations, so this may be related to the per capita occupancy of health care resources. The results of this study suggest that the prevalence of CF in diabetic patients in China is high and that prevalence of CF in older adults diabetic patients is higher than that in the general older adults population. Therefore, it is necessary to improve the attention of medical staff and older adults diabetic patients.
Subgroup analyses showed that the prevalence varied by range. From the perspective of sample sources, the prevalence of CF in diabetic patients in Chinese communities is 25.8%, and the detection rate of CF in older adults hospitalized diabetic patients is 31.1%, indicating that the prevalence of CF in hospitals is higher than that in communities. The conclusion is the same as that of Liu et al. (56), which may be related to the poor health status of hospitalized patients compared with community patients. They are prone to negative emotions such as loneliness and depression, their daily activities in the hospital are limited, and their physical and mental work is reduced. In terms of sex, the prevalence of CF in women was higher than that in men, and the prevalence of CF in women was higher than that in men in both the community and hospital, consistent with the findings of Liu et al. (56). Whitson et al. (57) found that older women generally have more comorbidities than men, which may lead to a higher prevalence than men. In addition, vitamin D deficiency in older adults women after menopause may also be one of the causes. In terms of regional distribution, the detection rate of CF in southern patients was 21.6%, and the detection rate of CF in northern patients was 29.4%, indicating that the prevalence of southern patients was higher than that of northern patients, and the conclusion was the same as that of Liu et al. (56). The reason may be that the economic level of the south is relatively higher, the medical and health services are better, and diabetics patients can more easily access higher quality medical services and higher health standards. In terms of age distribution, the prevalence of CF in patients aged 60 ~ 69, 70 ~ 79, and ≥ 80 years increased gradually, suggesting that the prevalence of CF in patients with diabetes increases with age, which is consistent with previous studies (56, 58, 59). The reason for this may be that with increasing age, the physical function of the older adults gradually declines, accompanied by muscle loss, which promotes the occurrence and development of CF. The results suggest that there are differences in the prevalence of CF among diabetic patients in China in terms of sample source and regional distribution, and more longitudinal studies are needed to explore the reasons for the difference in prevalence between different regions. Targeted interventions need to be used for different regions and different patient groups in treatment.
This study showed that depression, malnutrition, age (≥70) (≥80), regular exercise, educational level (college or above), chronic disease ≥4 and high glycated hemoglobin (≥8.5) were the main factors related to CF in diabetic patients in China.
4.1. Depression
This study showed that depression was a protective factor for CF in diabetic patients in China. A study from Korea showed that patients’ depression was associated with CF (49). In addition, studies on patients with hypertension (47), chronic kidney disease (45), and dialysis (50) also showed the same conclusion, which may be related to the severity of the disease, high medical costs, and heavy burden of care, which make patients prone to pessimism. The mechanism of depression in CF may affect patients by slowing cognitive ability (60), reducing feeding and exercise initiative (61), and reducing social activities (62). At the same time, depression is also associated with the risk of adverse health outcomes such as suicide (63). Therefore, relevant medical personnel should put psychotherapy in the same important position as physical therapy and carry out psychotherapy under the guidance of professional psychologists.
4.2. Malnutrition
Malnutrition, according to the results of this study is a risk factor for diabetic patients with CF. This is in line with the findings of Chen et al. (50), a study of 340 maintenance hemodialysis patients, and may be related to the problems of metabolism and nutrient utilization in both diabetic and dialysis patients. Research has shown that insufficient nutrient intake is considered an important factor in physical frailty (64), while another study has shown that metabolic problems are also associated with cognitive decline in older people (64). For this, shall meet the needs of diabetes patients with CF, detailed in diabetes diet, nutrition, dietary intervention. At the same time, attention should be given to the potential malnutrition of low-income diabetic patients and corresponding interventions should be carried out to maintain their healthy nutritional status.
4.3. Age (≥70, ≥80)
This study shows that the age of diabetic patients in China is related to the prevalence of CF. This conclusion is consistent with previous studies (44, 45, 48, 50, 51), but age was not a relevant factor in a study of CF in hypertensive patients (47), which may be related to the fact that the population included in this study was mainly 60-79-years-old patients, and the age span was small. The study by Shimada et al. (65) showed that CF problems were more severe in patients older than 75 years. This suggests the need for interventions in accordance with age characteristics for patients of different ages. For example, older older adults patients may pay more attention to aerobic exercise and meditation, while younger older adults people may increase muscle strength and endurance training so that patients can obtain the maximum benefit from exercise therapy.
4.4. Regular exercise
The results of this study showed that regular exercise was a protective factor for CF in diabetic patients in China. Previous studies have suggested that exercise is not a protective factor for CF in hypertensive patients (47). The reason may be that diabetic patients have glucose utilization disorders, and they need to exercise regularly to stabilize postprandial blood glucose, reduce body weight, and improve insulin sensitivity, so they have higher exercise requirements than hypertensive patients. Other studies have concluded that physical exercises such as resistance exercise and aerobic exercise are beneficial for maintaining muscle strength, improving cognitive ability and reducing frailty in patients with diabetes (66–68). At the same time, studies have shown that long-term regular exercise is also conducive to relieving patients’ emotions and improving their quality of life. At the same time, studies have shown that muscle strength is related to the quality of life of the older adults individuals (69), and long-term regular exercise can also help the older adults individuals improve their quality of life (69, 70). People with diabetes are advised to exercise regularly to control blood sugar fluctuations. Diabetic patients with CF should carry out more targeted exercises that take into account both flexibility and coordination or add a certain proportion of cognitive training (such as meditation after exercise) to their daily exercise plan to take into account both physical and mental training.
4.5. High education level (college or above)
The results of this study suggest that a high level of education is a protective factor for CF in diabetic patients in China. This conclusion is consistent with previous studies (44, 50, 51), and another study showed that it is only an association factor but not an independent risk factor (45). The analysis may be related to the fact that people with higher education levels are more active in thinking, have stronger health concepts and are more likely to obtain disease-related knowledge and high-quality medical services. Although the education level of the individual is not a controllable factor, understanding the cultural level of the patients can help the relevant medical staff to carry out health education in a way that is easy for the patients to understand and formulate intervention measures in line with the patients’ educational level to improve their compliance with the intervention. Some studies have also built a risk prediction model by incorporating the patient’s cultural level into the model, which will help to predict the risk of CF in patients (71, 72).
4.6. Multimorbidity (chronic disease≥4)
Research shows that CF patients with diabetes risk factors include multimorbidity, in accordance with previous research results (47, 50). Kim et al. (73) showed a 6.419-fold increased risk of CF among community-dwelling older adults individuals with four or more chronic diseases. Multimorbidity can lead to a decline in physiological reserve, reduce the body’s resistance and tolerance, accelerate organ and system failure, and increase the potential risk of inappropriate medication in patients, leading to multiple factors acting on the body and increasing cognitive impairment and frailty (74). The treatment of older adults patients with multimorbidity needs to proceed from a systemic point of view and adopt the treatment modality that is most suitable for the patient’s condition.
4.7. High glycated hemoglobin (≥8.5)
High glycated hemoglobin is a risk factor for CF in diabetic patients in China, and a previous study on CF in diabetic patients with hypertension showed no correlation between high glycated hemoglobin and CF, but other laboratory indicators also showed no correlation with CF (48). The main reason is that the patient population is diabetic patients with hypertension, which is different from this study, and the survey area is a more developed area with better medical conditions.
Overall, we conducted a comprehensive search of the literature and maximized the collection of relevant studies to reduce selection bias. All study phases were independently assessed by two investigators, with discrepancies resolved through discussion. Data were pooled using a random-effects model to provide conservative estimates of the prevalence of CF in people with diabetes in China. Sensitivity and subgroup analyses were also performed to investigate possible causes of heterogeneity and to assess publication bias.
Our study still has some limitations. In our review, despite subgroup analyses of study participants, the source of heterogeneity was not identified, possibly from the study population and methodology. The differences in the population come from the differences in culture, diet, living habits, behavior patterns, etc. among the included groups. The differences in research methods mainly come from the differences in the combination of use scales. There is currently no optimal combination of the measurement scale for physical frailty and cognitive function, there are differences in the focus and scoring criteria between the scales used in each study, and there are different combinations and arrangements. At the same time, the included literature in this paper are all published literature, there may be some publication bias, and future studies need to include more high-quality literature to supplement the article conclusions.
5. Conclusion
In summary, the analysis results of this study showed that the prevalence of CF in Chinese diabetic patients was 25.8%, and the prevalence was high. Subgroup analysis showed that the prevalence was higher in hospitals than in the community, with women being more prevalent than men. With increasing age, course, and number of chronic diseases, the prevalence of CF gradually increases, and there are certain differences between the prevalence in different regions and cultural levels. Among the related factors, depression, malnutrition, advanced age, combined chronic diseases ≥4, and glycosylated hemoglobin ≥8.5 were risk factors for CF. A college education level or above education level and regular exercise are protective factors against CF. Future researchers should conduct standardized research on the assessment tools of CF, and medical workers should recognize the importance of CF in diabetic patients and actively take interventions to reduce the occurrence of diabetic CF and delay or prevent its progression.
Author contributions
JP conducts major thesis writing, data extraction and data analysis, and article proofreading. LM conducts thesis writing, data extraction and partial data analysis. JW, YL, and SY provided ideas. QL provides ideas for papers and reviews articles. All authors contributed to the article and approved the submitted version.
Funding
This investigation was supported by the Yunnan Province Natural Science Foundation Project (202001AU070117).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. International Diabetes Federation. IDF Diabetes Atlas [Internet] International Diabetes Federation (n.d.) Available at: https://diabetesatlas.org/atlas/tenth-edition/.
2. Okoro, CA, Hollis, ND, Cyrus, AC, and Griffin-Blake, S. Prevalence of disabilities and health care access by disability status and type among adults - United States, 2016. MMWR Morb Mortal Wkly Rep. (2018) 67:882–7. doi: 10.15585/mmwr.mm6732a3
3. Fried, LP, Tangen, CM, Walston, J, Newman, AB, Hirsch, C, Gottdiener, J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci. (2001) 56:M146–57. doi: 10.1093/gerona/56.3.M146
4. Patnode, CD, Perdue, LA, Rossom, RC, Rushkin, MC, Redmond, N, Thomas, RG, et al. Screening for cognitive impairment in older adults: updated evidence report and systematic review for the US preventive services task force. JAMA. (2020) 323:764–85. doi: 10.1001/jama.2019.22258
5. Armstrong, JJ, Godin, J, Launer, LJ, White, LR, Mitnitski, A, Rockwood, K, et al. Changes in frailty predict changes in cognition in older men: the Honolulu-Asia aging study. J Alzheimer's Dis. (2016) 53:1003–13. doi: 10.3233/JAD-151172
6. Kelaiditi, E, Cesari, M, Canevelli, M, van Kan, GA, Ousset, PJ, Gillette-Guyonnet, S, et al. Cognitive frailty: rational and definition from an (I.A.N.A./I.A.G.G.) international consensus group. J Nutr Health Aging. (2013) 17:726–34. doi: 10.1007/s12603-013-0367-2
7. Ruan, Q, Yu, Z, Chen, M, Bao, Z, Li, J, and He, W. Cognitive frailty, a novel target for the prevention of elderly dependency. Ageing Res Rev. (2015) 20:1–10. doi: 10.1016/j.arr.2014.12.004
8. Han, ES, Lee, Y, and Kim, J. Association of cognitive impairment with frailty in community-dwelling older adults. Int Psychogeriatr. (2014) 26:155–63. doi: 10.1017/S1041610213001841
9. Brigola, AG, Rossetti, ES, Dos Santos, BR, Neri, AL, Zazzetta, MS, Inouye, K, et al. Relationship between cognition and frailty in elderly: a systematic review. Dementia Neuropsychol. (2015) 9:110–9. doi: 10.1590/1980-57642015DN92000005
10. Abdelhafiz, AH, and Sinclair, AJ. Cognitive frailty in older people with type 2 diabetes mellitus: the central role of hypoglycaemia and the need for prevention. Curr Diab Rep. (2019) 19:15. doi: 10.1007/s11892-019-1135-4
11. Serra-Prat, M, Palomera, E, Clave, P, and Puig-Domingo, M. Effect of age and frailty on ghrelin and cholecystokinin responses to a meal test. Am J Clin Nutr. (2009) 89:1410–7. doi: 10.3945/ajcn.2008.27076
12. Tuttle, LJ, Sinacore, DR, Cade, WT, and Mueller, MJ. Lower physical activity is associated with higher intermuscular adipose tissue in people with type 2 diabetes and peripheral neuropathy. Phys Ther. (2011) 91:923–30. doi: 10.2522/ptj.20100329
13. Cesari, M, Penninx, BW, Pahor, M, Lauretani, F, Corsi, AM, Rhys Williams, G, et al. Inflammatory markers and physical performance in older persons: the InCHIANTI study. J Gerontol A Biol Sci Med Sci. (2004) 59:M242–8. doi: 10.1093/gerona/59.3.M242
14. Morley, JE, Malmstrom, TK, Rodriguez-Mañas, L, and Sinclair, AJ. Frailty, sarcopenia and diabetes. J Am Med Dir Assoc. (2014) 15:853–9. doi: 10.1016/j.jamda.2014.10.001
15. Chang, KV, Hsu, TH, Wu, WT, Huang, KC, and Han, DS. Association between sarcopenia and cognitive impairment: a systematic review and meta-analysis. J Am Med Dir Assoc. (2016) 17:1164.e7–1164.e15. doi: 10.1016/j.jamda.2016.09.013
16. Yu, R, Morley, JE, Kwok, T, Leung, J, Cheung, O, and Woo, J. The effects of combinations of cognitive impairment and pre-frailty on adverse outcomes from a prospective community-based cohort study of older Chinese people. Front Med. (2018) 5:50. doi: 10.3389/fmed.2018.00050
17. Roppolo, M, Mulasso, A, and Rabaglietti, E. Cognitive frailty in Italian community dwelling older adults: prevalence rate and its association with disability. J Nutr Health Aging. (2017) 21:631–6. doi: 10.1007/s12603-016-0828-5
18. Rivan, NFM, Singh, DKA, Shahar, S, Wen, GJ, Rajab, NF, Din, NC, et al. Cognitive frailty is a robust predictor of falls, injuries, and disability among community-dwelling older adults. BMC Geriatr. (2021) 21:593. doi: 10.1186/s12877-021-02525-y
19. Zheng, L, Li, G, Gao, D, Wang, S, Meng, X, Wang, C, et al. Cognitive frailty as a predictor of dementia among older adults: a systematic review and meta-analysis. Arch Gerontol Geriatr. (2019) 87:103997. doi: 10.1016/j.archger.2019.103997
20. Feng, L, Zin Nyunt, MS, Gao, Q, Feng, L, Yap, KB, and Ng, TP. Cognitive frailty and adverse health outcomes: findings from the Singapore longitudinal ageing studies (SLAS). J Am Med Dir Assoc. (2017) 18:252–8. doi: 10.1016/j.jamda.2016.09.015
21. Moher, D, Liberat, A, Tetzlaff, J, and Altman, DG, PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. (2009) 6:e1000097. doi: 10.1371/journal.pmed.1000097
22. Rostom, A, Dubé, C, Cranney, A, Saloojee, N, Sy, R, Garritty, C, et al. Celiac disease. Evid Rep Technol Assess (Summ). (2004) 104:1–6.
23. Stang, A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Euro J Epid. (2010) 25:603–5. doi: 10.1007/s10654-010-9491-z
24. Li, XY, Yang, XY, Wu, QQ, Kong, LP, and Zhu, QY. Analysis of related factors of cognitive decline in elderly patients with type 2 diabetes in Hangzhou community. Chin J Gen Pract. (2022) 20:274–7. doi: 10.16766/j.cnki.issn.1674-4152.002331
25. JIANG, MJ, FENG, TT, YAO, X, Ma, LY, and Liu, R. Logistic regression analysis of risk factors for cognitive frailty in elderly patients with type 2 diabetes mellitus and their impact on executive function and occurrence risk of fall fear. Prog Modern Biomed. (2022) 22:4076–80. doi: 10.13241/j.cnki.pmb.2022.21.013
26. Wang, HL. Current situation and influencing factors of cognitive frailty in elderly patients with type 2 diabetes mellitus (Master's thesis China Medical University (2022) Available at: https://kns.cnki.net/KCMS/detail/detail.aspx?dbname=CMFD202301&filename=1022731367.nh.
27. Liu, YX, Han, T, Yu, L, and Li, P. Cognitive frailty and influencing factors in seniors with type 2 diabetes mellitus. Chin J Prev Contr Chron Dis. (2021) 6:426–31. doi: 10.16386/j.cjpccd.issn.1004-6194.2021.06.006
28. Zhang, L, Yu, Z, Jia, QM, Ge, HY, and Kong, LP. Analysis of influencing factors of cognitive frailty in elderly hospitalized patients with type 2 diabetes. ZJITCWM. (2023) 30:267–70.
29. Yang, SH. Gender differences of cognitive frailty morbidity and influence factors analysis in elderly inpatients with type 2 diabetes mellitus (Master's thesis Guangxi University of Chinese Medicine (2022) Available at: https://kns.cnki.net/KCMS/detail/detail.aspx?dbname=CMFD202301&filename=1022081367.nh.
30. Fu, JN, and Zhao, H. Association between cognitive frailty and phobic disease progression in elderly hospitalized patients with type 2 diabetes. J Clin Nurs. (2023) 20:30–4.
31. Wang, YL. Analysis of related factors of senile diabetes cognitive frailty and research the distribution of TCM syndrome types. Master’s thesis Shandong University of Traditional Chinese Medicine. (2021) Available at: https://kns.cnki.net/KCMS/detail/detail.aspx?dbname=CMFD202201&filename=1021129909.nh.
32. Zhang, S, Chen, Y, Jiang, ZL, Sun, NY, and Zhang, WH. (2020). Study on cognitive frailty and the influencing factors in community aged with diabetes. Chinese Nursing Management. 383–388.
33. Han, SS. Study on the status and influencing factors of cognitive frailty in community-dwelling elderly patients with diabetes in Shenyang (Master's thesis China Medical University (2021) Available at: https://kns.cnki.net/KCMS/detail/detail.aspx?dbname=CMFD202201&filename=1021870133.nh.
34. Yang, GF. STUDY ON COGNITIVE FRAILTY STATUS AND INFLUENCING FACTORS IN ELDERLY HOSPITALIZED WITH TYPE 2 DIABETES (Master's thesis Anhui University of Chinese Medicine (2022) Available at: https://kns.cnki.net/KCMS/detail/detail.aspx?dbname=CMFD202301&filename=1022758278.nh.
35. Kong, LL, Zhao, HM, Liu, YT, Fan, JY, Wang, Q, Li, J, et al. Cognitive frailty and its influencing factors among the elderly with type 2 diabetes in community. J Nurs Sci. (2020) 70:89–92.
36. Wang, LW. Influencing factors of cognitive frailty in elderly patients with comorbidities (Master's thesis North China University of Science and Technology (2021) Available at: https://kns.cnki.net/KCMS/detail/detail.aspx?dbname=CMFD202201&filename=1021915964.nh.
37. Ma, N, Bian, O, Zhang, SH, Yan, SM, Hu, WS, Ding, L, et al. Risk factors analysis of cognitive dysfunction in elderly patients with frailty. Clin J Med Office. (2020) 30:264–6. doi: 10.16680/j.1671-3826.2020.03.07
38. Chen, J. The current situation and influential factors of cognitive frailty in elderly inpatients (Master's thesis Henan University (2020) Available at: https://kns.cnki.net/KCMS/detail/detail.aspx?dbname=CMFD202101&filename=1020107620.nh.
39. Wang, LX, Yang, YX, Guan, LJ, and Shen, J. Current status of cognitive frailty and its influencing factors in hospitalized elderly with comorbidities. Chin J Mult Organ Dis Elderly. (2019) 10:738–42.
40. Li, YX, Jiang, XY, Stone, C, Ma, YJ, Liu, Q, Hu, ZH, et al. A new physical-cognitive scale for assessment of frailty in Chinese Han elderly. Neurol Res. (2019) 41:728–33. doi: 10.1080/01616412.2019.1609164
41. Lee, WJ, Peng, LN, Liang, CK, Loh, CH, and Chen, LK. Cognitive frailty predicting all-cause mortality among community-living older adults in Taiwan: a 4-year nationwide population-based cohort study. PLoS One. (2018) 13:e0200447. doi: 10.1371/journal.pone.0200447
42. Feng, L, Nyunt, MS, Gao, Q, Feng, L, Lee, TS, Tsoi, T, et al. Physical frailty, cognitive impairment, and the risk of neurocognitive disorder in the Singapore longitudinal ageing studies. J Gerontol A Biol Sci Med Sci. (2017) 72:369–75. doi: 10.1093/gerona/glw050
43. Yi, J, and Yoon, JY. Cognitive frailty increases the risk of long-term care dependency in community-dwelling older adults: a nationwide cohort study in South Korea. Geriatr Gerontol Int. (2023) 23:117–23. doi: 10.1111/ggi.14534
44. Wongtrakulruang, P, Muangpaisan, W, Panpradup, B, Tawatwattananun, A, Siribamrungwong, M, and Tomongkon, S. The prevalence of cognitive frailty and pre-frailty among older people in Bangkok metropolitan area: a multicenter study of hospital-based outpatient clinics. J Frailty Sarcopenia Falls. (2020) 5:62–71. doi: 10.22540/JFSF-05-062
45. Shimada, H, Makizako, H, Lee, S, Doi, T, Lee, S, Wang, Y, et al. Impact of cognitive frailty on daily activities in older persons. J Nutr Health Aging. (2016) 20:729–35. doi: 10.1007/s12603-016-0685-2
46. Chang, J, Hou, W, Li, Y, Li, S, Zhao, K, Tsutsumimoto, K, et al. Prevalence and associated factors of cognitive frailty in older patients with chronic kidney disease: a cross-sectional study. BMC Geriatr. (2022) 22:681–10. doi: 10.1186/s12877-022-03366-z
47. Wang, C, Zhang, J, Hu, C, and Wang, Y. Prevalence and risk factors for cognitive frailty in aging hypertensive patients in China. Brain Sci. (2021) 11:1018. doi: 10.3390/brainsci11081018
48. Lu, S, Xu, Q, Yu, J, Yang, Y, Wang, Z, Zhang, B, et al. Prevalence and possible factors of cognitive frailty in the elderly with hypertension and diabetes. Front Cardiovasc Med. (2022) 9:1054208. doi: 10.3389/fcvm.2022.1054208
49. Seo, EJ, and Son, YJ. The prevalence of cognitive frailty and its association with sleep duration and depression among older adults with heart failure. Clin Gerontol. (2022) 1–10. doi: 10.1080/07317115.2022.2125858
50. Chen, G, Zhang, H, Du, X, Yin, L, Zhang, H, and Zhou, Q. Comparison of the prevalence and associated factors of cognitive frailty between elderly and middle-young patients receiving maintenance hemodialysis. Int Urol Nephrol. (2022) 54:2703–11. doi: 10.1007/s11255-022-03188-3
51. Das, S. Cognitive frailty among community-dwelling rural elderly population of West Bengal in India. Asian J Psychiatr. (2022) 70:103025. doi: 10.1016/j.ajp.2022.103025
52. Thein, FS, Li, Y, Nyunt, MSZ, Gao, Q, Wee, SL, and Ng, TP. Physical frailty and cognitive impairment is associated with diabetes and adversely impact functional status and mortality. Postgrad Med. (2018) 130:561–7. doi: 10.1080/00325481.2018.1491779
53. Aliberti, MJR, Cenzer, RS, Smith, AK, Lee, SJ, Yaffe, K, and Covinsky, KE. Risk assessment of adverse outcomes for older adults: the need to include both physical and cognitive elements. J Am Geriatr Soc. (2019) 67:477–83. doi: 10.1111/jgs.15683
54. Shimada, H, Makizako, H, Tsutsumimoto, K, Doi, T, Lee, S, and Suzuki, T. Cognitive frailty and incidence of dementia in older persons. J Prev Alzheimers Dis. (2018) 5:42–8. doi: 10.14283/jpad.2017.29
55. Alkhodary, AA, Aljunid, SM, Ismail, A, Nur, AM, and Shahar, S. Health care utilization and out-of-pocket payments among elderly with cognitive frailty in Malaysia. Int J Environ Res Public Health. (2022) 19:3361. doi: 10.3390/ijerph19063361
56. Liu, J, Xu, S, Wang, J, Yan, Z, Wang, Z, Liang, Q, et al. Prevalence of cognitive frailty among older adults in China: a systematic review and meta-analysis. BMJ Open. (2023) 13:e066630. doi: 10.1136/bmjopen-2022-066630
57. Whitson, HE, Landerman, LR, Newman, AB, Fried, LP, Pieper, CF, and Cohen, HJ. Chronic medical conditions and the sex-based disparity in disability: the cardiovascular health study. J Gerontol A Biol Sci Med Sci. (2010) 65:1325–31. doi: 10.1093/gerona/glq139
58. Zhang, T, Ren, Y, Shen, P, Jiang, S, Yang, Y, Wang, Y, et al. Prevalence and associated risk factors of cognitive frailty: a systematic review and meta-analysis. Front Aging Neurosci. (2022) 13:755926. doi: 10.3389/fnagi.2021.755926
59. Vatanabe, IP, Pedroso, RV, Teles, RHG, Ribeiro, JC, Manzine, PR, Pott-Junior, H, et al. A systematic review and meta-analysis on cognitive frailty in community-dwelling older adults: risk and associated factors. Aging Ment Health. (2022) 26:464–76. doi: 10.1080/13607863.2021.1884844
60. van den Kommer, TN, Comijs, HC, Aartsen, MJ, Huisman, M, Deeg, DJ, and Beekman, AT. Depression and cognition: how do they interrelate in old age? Am J Geriatr Psychiatry. (2013) 21:398–410. doi: 10.1016/j.jagp.2012.12.015
61. Soysal, P, Veronese, N, Thompson, T, Kahl, KG, Fernandes, BS, Prina, AM, et al. Relationship between depression and frailty in older adults: a systematic review and meta-analysis. Ageing Res Rev. (2017) 36:78–87. doi: 10.1016/j.arr.2017.03.005
62. Liu, Y, Meng, H, Tu, N, and Liu, D. The relationship between health literacy, social support, depression, and frailty among community-dwelling older patients with hypertension and diabetes in China. Front Public Health. (2020) 8:280. doi: 10.3389/fpubh.2020.00280
63. Elamoshy, R, Bird, Y, Thorpe, L, and Moraros, J. Risk of depression and suicidality among diabetic patients: a systematic review and meta-analysis. J Clin Med. (2018) 7:445. doi: 10.3390/jcm7110445
64. Panza, F, Solfrizzi, V, Barulli, MR, Santamato, A, Seripa, D, Pilotto, A, et al. Cognitive frailty: a systematic review of epidemiological and neurobiological evidence of an age-related clinical condition. Rejuvenation Res. (2015) 18:389–412. doi: 10.1089/rej.2014.1637
65. Shimada, H, Makizako, H, Doi, T, Yoshida, D, Tsutsumimoto, K, Anan, Y, et al. Combined prevalence of frailty and mild cognitive impairment in a population of elderly Japanese people. J Am Med Dir Assoc. (2013) 14:518–24. doi: 10.1016/j.jamda.2013.03.010
66. Yu, R, Leung, G, and Woo, J. Randomized controlled trial on the effects of a combined intervention of computerized cognitive training preceded by physical exercise for improving frailty status and cognitive function in older adults. Int J Environ Res Public Health. (2021) 18:1396. doi: 10.3390/ijerph18041396
67. Wang, R, Yan, W, Du, M, Tao, L, and Liu, J. The effect of physical activity interventions on cognition function in patients with diabetes: A systematic review and meta-analysis. Diabetes/metabolism research and reviews. (2021) 37:e3443.
68. Laudisio, A, Giovannini, S, Finamore, P, Loreti, C, Vannetti, F, Coraci, D, et al. Muscle strength is related to mental and physical quality of life in the oldest old. Arch Gerontol Geriatr. (2020) 89:104109. doi: 10.1016/j.archger.2020.104109
69. Lee, M, Lee, H, Song, K, and Lee, YM. Benefits of sustained physical activity from middle age to early old age on quality of life in early old age. Sci Rep. (2022) 12:16455. doi: 10.1038/s41598-022-20431-0
70. Choi, GW, and Chang, SJ. Correlation of health-related quality of life for older adults with diabetes mellitus in South Korea: theoretical approach. BMC Geriatr. (2023) 23:491. doi: 10.1186/s12877-023-04186-5
71. Peng, S, Zhou, J, Xiong, S, Liu, X, Pei, M, Wang, Y, et al. Construction and validation of cognitive frailty risk prediction model for elderly patients with multimorbidity in Chinese community based on non-traditional factors. BMC Psychiatry. (2023) 23:266. doi: 10.1186/s12888-023-04736-6
72. Luo, B, Luo, Z, Zhang, X, Xu, M, and Shi, C. Status of cognitive frailty in elderly patients with chronic kidney disease and construction of a risk prediction model: a cross-sectional study. BMJ Open. (2022) 12:e060633. doi: 10.1136/bmjopen-2021-060633
73. Kim, H, Awata, S, Watanabe, Y, Kojima, N, Osuka, Y, Motokawa, K, et al. Cognitive frailty in community-dwelling older Japanese people: prevalence and its association with falls. Geriatr Gerontol Int. (2019) 19:647–53. doi: 10.1111/ggi.13685
Keywords: cognitive frailty, diabetes, prevalence, relevant factors, meta-analysis
Citation: Peng J, Ming L, Wu J, Li Y, Yang S and Liu Q (2023) Prevalence and related factors of cognitive frailty in diabetic patients in China: a systematic review and meta-analysis. Front. Public Health. 11:1249422. doi: 10.3389/fpubh.2023.1249422
Edited by:
Roberta Zupo, University of Bari Aldo Moro, ItalyReviewed by:
Luisa Lampignano, Local Health Authority of Bari, ItalySilvia Giovannini, Catholic University of the Sacred Heart, Italy
Copyright © 2023 Peng, Ming, Wu, Li, Yang and Liu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Qin Liu, bGl1cWluQHludXRjbS5lZHUuY24=
 Junjie Peng
Junjie Peng Limei Ming1
Limei Ming1