- Department of 12 Ward, Huzhou Third Municipal Hospital, The Affiliated Hospital of Huzhou University, Zhejiang, Huzhou, China
Background: To document pooled evidence on the association between weekend hospital admissions and the potential risks of mortality, intensive care requirements, and readmission among patients with pneumonia.
Methods: We performed a systematic search across the PubMed, EMBASE, and Scopus databases. We collected observational studies exploring the association between weekend admissions and outcomes of interest in patients with pneumonia. To analyze the data, we used a random effects model and expressed the effect sizes as pooled odds ratios (ORs) accompanied by their respective 95% confidence intervals (CIs).
Results: The analysis comprised data from 13 retrospective studies. Compared to patients admitted on weekdays, those admitted during the weekend had a non-statistically significant marginally higher risk of in-hospital mortality (OR, 1.02; 95% CI, 1.00, 1.04) but similar 30-day mortality after admission (OR, 1.03; 95% CI, 0.97, 1.10), and similar risks of admission to intensive care unit (OR, 1.04; 95% CI, 0.98, 1.11) and re-admission (OR, 0.85; 95% CI, 0.65–1.12).
Conclusion: Our findings do not support the presence of a “weekend effect” in patients with pneumonia.
Systematic review registration: PROSPERO, identifier CRD42023425802, https://www.crd.york.ac.uk/prospero/.
Introduction
Pneumonia is a significant global health concern with substantial morbidity and mortality worldwide (1–3). Pneumonia is a leading cause of illness and death, particularly among vulnerable populations such as young children, older adult, and individuals with underlying health conditions (4, 5). Pneumonia is associated with significant healthcare use, including hospitalizations, intensive care unit (ICU) stays, and the need for respiratory support and antibiotics (6–8).
The idea of the “weekend effect” refers to the increased risk of mortality in patients admitted to hospitals on Saturdays or Sundays compared to the risks in patients admitted on weekdays (9, 10). Researchers, policymakers, and healthcare professionals have tried to understand the underlying mechanisms of the weekend effect, and several factors have been suggested as potential contributors, including differences in staffing levels, reduced availability of certain services or resources, delayed diagnostic tests, and limited access to specialized interventions during weekends (11–13). Studies have shed light on this intriguing pattern (9, 10, 14, 15). Zhou et al. performed a comprehensive meta-analysis of 140 studies to examine the association between admission during off-hours or on weekends and the risk of mortality across various diseases (16). Their findings revealed a substantial correlation between off-hour admissions and elevated mortality rates for specific conditions (aortic aneurysm, breast cancer, pulmonary embolism, arrhythmia, and cardiac arrest). No significant association was observed for other conditions such as hip fracture, pneumonia, intestinal obstruction, or trauma. However, when considering ~28 diseases together, off-hour admission demonstrated a consistent association with increased mortality (16). This above-mentioned review was published in 2016 and included seven unique studies on pneumonia. Since then, other studies looking at the effect of timing of admission on the survival of patients with pneumonia have been published. Thus, we decided to update the evidence with findings of newer studies. Our meta-analysis aims to pool findings from all available studies to present updated evidence on the impact of weekend admission on mortality, risk of admission to intensive care unit (ICU), and readmission in patients with pneumonia.
Methods
Process for selection of studies
We conducted a comprehensive search of three electronic databases (PubMed, Embase, and Scopus) to identify relevant studies for our analysis. The search encompassed articles published from the inception of these databases up to April 30, 2023. We designed the search strategy using a combination of medical subject headings (MeSH) and free-text terms, focusing on topics such as pneumonia, off-hours admission, weekend admission, and outcomes. The search strategy included the following entries: (off-hours admission OR, weekend admission OR, weekday admission) AND (pneumonia OR, respiratory infection OR, lung infection OR, pneum*) AND (clinical outcome OR, mortality OR, death OR, survival OR, readmission OR, intensive care). Moreover, we conducted a thorough screening of the reference lists of the relevant articles and systematic reviews to identify any additional studies that met our predefined inclusion criteria. This process allowed us to capture any potentially relevant studies. The need for ethical approval was waived due to the nature of this systematic review and meta-analysis based on existing literature. To ensure the transparency and completeness of our methodology and findings, we followed the guidelines set forth by PRISMA (17). This protocol was registered at PROSPERO, No. CRD42023425802.
To ensure the quality and reliability of our study, we implemented a robust process that involved two independent reviewers meticulously screening all identified studies for inclusion. This screening was carried out on the basis of predetermined eligibility criteria that were established prior to initiating the study. Our primary focus was on observational studies that specifically examined the association between weekend admission (as opposed to weekday admission) and various outcomes of interest in individuals admitted for pneumonia within healthcare facilities. These outcomes primarily encompassed mortality rates, the risk of admission to the intensive care unit (ICU), and the risk of readmission. To ensure consistency and adherence to our selection criteria, we identified studies reporting on at least one of the specified outcomes. Moreover, we limited our inclusion to studies published in English. During the literature search, we applied specific exclusion criteria to ensure the relevance and appropriateness of the selected studies. Any studies containing duplicate or overlapping data were excluded from consideration. In addition, we also excluded case reports, editorials, letters, and conference abstracts.
In case of disagreements between the two reviewers during the screening process, discussions were held to reach a consensus. If necessary, a third expert reviewer was consulted. Finally, after the initial screening, we retrieved and carefully assessed the full texts of the potentially eligible studies to ensure that only the most relevant and appropriate studies were incorporated into our analysis.
Extraction of relevant data from included studies
Two authors extracted the data independently using a standardized form to ensure consistency and uniformity. Any discrepancies during the data extraction phase were resolved through discussion between the two authors to reach a consensus. To assess the risk of bias within the included studies, we used the Newcastle-Ottawa Scale (NOS) (18), a widely accepted tool for evaluating the quality and potential bias of the selected studies. Again, disagreements were resolved during discussions or after consulting with a third expert. This collaborative approach ensured a comprehensive and reliable evaluation of the included studies, minimizing the potential for bias and enhancing the overall quality of our study.
Data analysis
To estimate the pooled effect sizes (odd's ratios, ORs) and their corresponding 95% confidence intervals (CIs) for each outcome of interest, we applied a random-effects model. This statistical approach considers both within-study and between-study variability (19). We calculated the overall effect estimate by first obtaining a weighted average of the effect sizes from each individual study. The weights were determined on the basis of the inverse of the variance of each effect size. This weighting scheme gives more emphasis to studies with smaller variances, and provides a precise estimate of the overall effect (19).
To assess the presence of statistical heterogeneity, we calculated the I2 statistic, which quantifies the proportion of total variability across studies that can be attributed to heterogeneity rather than chance (20). Moreover, we conducted an evaluation of publication bias using Egger's test and visual inspection of funnel plots (21). We considered P-values lower than 0.05 as indicative of statistically significant publication bias.
Results
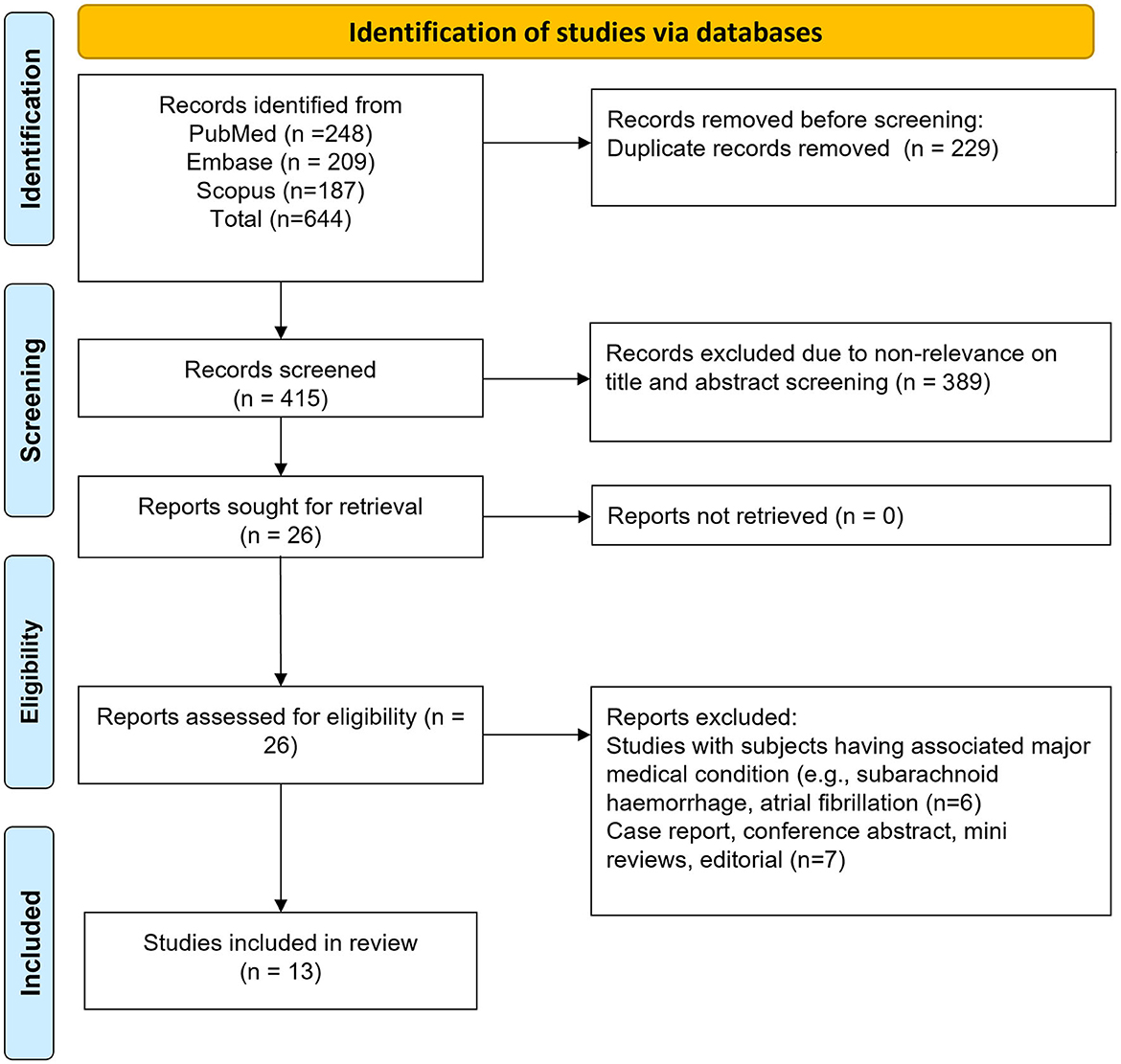
We initially identified 644 studies through our search strategy. After removing 229 duplicates, we were left with 415 unique studies. We further screened the titles and abstracts of these studies and excluded 389 of them. We proceeded to the detailed review of the full texts of the remaining 26 studies, leading to the exclusion of an additional 13 studies. Ultimately, our meta-analysis included 13 studies, as illustrated in Figure 1 (22–34).
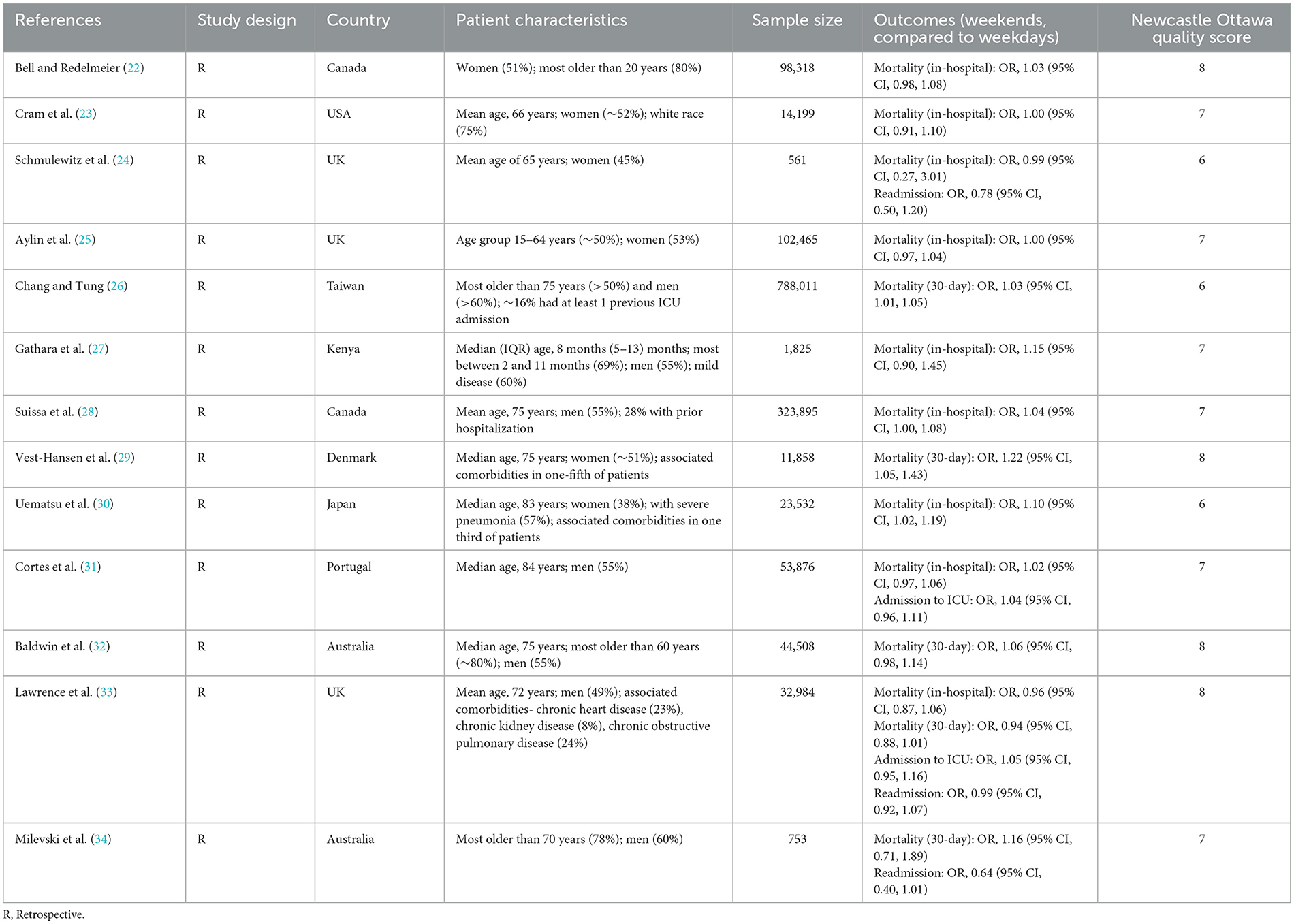
The 13 retrospective studies included comprised data from 14,56,735 patients (Table 1). Three studies were conducted in United Kingdom (UK), two in Australia and Canada, and one each in Kenya, USA, Japan, Taiwan, Denmark, and Portugal (Table 1). All studies, except one, included only adults. The quality assessment score varied between 6 and 8, out of the maximum attainable score of 9. The mean NOS score of the included studies was 7.1 (Table 1).
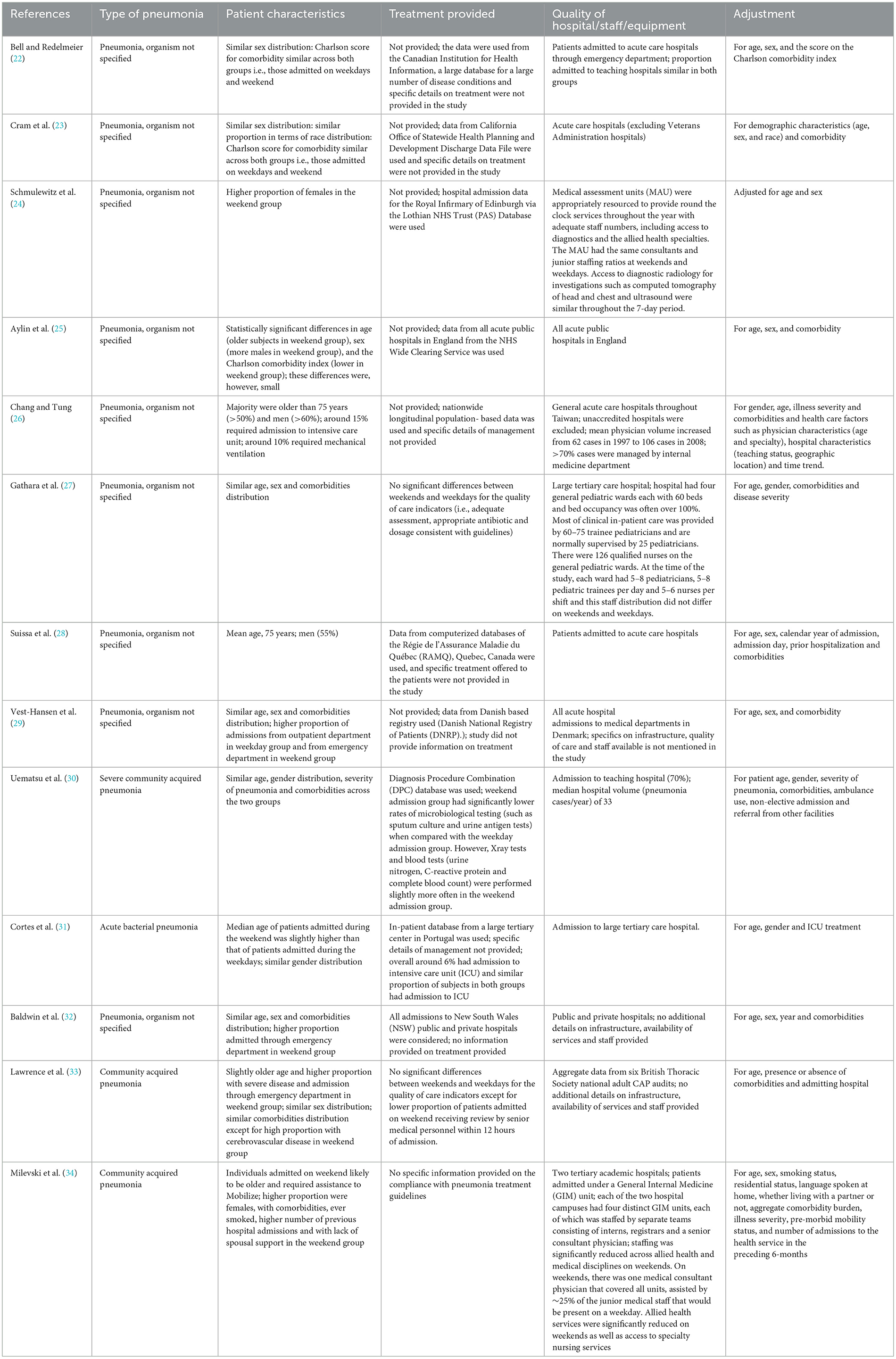
Table 2 provides additional insights into the included studies, particularly concerning the type of pneumonia, administered treatments, details about health facilities, and variables adjusted in the analytic model. Among the 13 studies, 9 simply specified “pneumonia” without differentiating between bacterial or viral origins. One study specifically identified cases as “acute bacterial pneumonia” (31), while the remaining three studies focused on “community-acquired pneumonia” (30, 33, 34). Regarding the treatment or quality of care given to pneumonia patients and whether there were distinctions between weekend and weekday admissions, a majority of studies did not furnish this information. One study reported no significant disparities in the quality of care indicators between weekends and weekdays (27). In contrast, another study noted that the weekend admission group exhibited significantly lower rates of microbiological testing, such as sputum culture and urine antigen tests, compared to the weekday admission group (30). This same study also revealed that X-ray tests and blood tests (urine nitrogen, C-reactive protein, and complete blood count) were marginally more frequent in the weekend admission group (30). Yet another study found no significant differences between weekends and weekdays in terms of quality of care indicators, except for a lower proportion of weekend-admitted patients receiving reviews by senior medical personnel within 12 h of admission (33). In terms of the study settings, six investigations were conducted in acute care hospitals, while four were carried out in large tertiary care or academic teaching hospitals.
Compared to patients admitted on a weekday, those with weekend admissions had a slightly higher risk of in-hospital mortality (OR, 1.02; 95% CI, 1.00, 1.04; n = 9; I2 = 6.7%), but similar risks of 30-day mortality (OR, 1.03; 95% CI, 0.97, 1.10; n = 5; I2 = 67%), admission to intensive care unit (OR, 1.04; 95% CI, 0.98, 1.11; n = 2; I2 = 0.0%), and being re-admitted (OR, 0.85; 95% CI, 0.65, 1.12; n = 3; I2 = 53.8%) (Figure 2). We found statistical evidence of publication bias for in-hospital mortality (P = 0.033), but not for other outcomes. The funnel plots for visual assessment of publication bias can be found in the Supplementary Figures 1–4.

Figure 2. Comparison of outcomes between patients with pneumonia admitted during weekend and those admitted during weekdays.
Discussion
In the current meta-analysis, we found that weekend admission for pneumonia was associated with a marginal increase in risk of in-hospital mortality, but not with risks of 30-day mortality, admission to intensive care unit, or being re-admitted. These findings confirm those reported by Zhou et al., who found no significant associations between off-hours admissions and the mortality risk in patients with pneumonia (16).
The weekend effect concept, which suggests that patients admitted during weekends experience poorer outcomes, may exhibit significant heterogeneity. The impact of the weekend effect probably depends on clinical conditions, hospital contexts, regional policies, and other factors that can differ considerably across geographical settings (11, 35–37). Studies have identified factors, including issues related to medical service accessibility and quality, limited access to specialized care, and reduced availability of certain procedures, which contribute to poor outcomes for patients admitted during off-hours or weekends (35–39). However, we found no elevated risk of mortality among patients with pneumonia admitted on weekends.
It is plausible that the weekend/off-hour effect is more pronounced for medical conditions that need additional specialized resources beyond standard care levels. The specialized healthcare resources level for the management of pneumonia is relatively low compared to the level needed for more critical conditions such as aortic aneurysms, pulmonary embolisms, arrhythmias, or cardiac arrests (40–42). Pneumonia can usually be readily diagnosed, and its treatment often follows standardized guidelines (40, 41). Therefore, pneumonia can be effectively managed by emergency medical staff without the immediate involvement of specialists. Thus, the impact of the weekend effect on patients with pneumonia may be less pronounced than the impact on conditions requiring a higher level of specialized care.
Most studies in our meta-analysis included vast amounts of routinely collected data as part of the patient care. By leveraging the information available on administrative data, researchers can gain deep insights into the weekend effect. However, improving coding standards and incorporating more refined parameters would help account for factors such as baseline disease severity, patient characteristics, and hospital workload (43, 44). The extensive datasets encompass various pre-defined fields, including demographic information, diagnoses, co-morbidities, and robust data on mortality and clinical outcomes (43, 44). While these data provide a valuable starting point, they offer limited specific information. Given the multifaceted nature of the weekend effect, researchers estimating mortality rates need to consider a multitude of factors, including the availability and quality of staff, as well as patient-level data. Research efforts need to shift focus from debating the mere existence of the weekend effect to delving deeper into its underlying causes and consequences to be able to implement innovative solutions and improve patient outcomes.
We are aware of certain limitations of the studies included. First, all of them were observational in nature, which makes them susceptible to potential confounding and bias. These studies cannot be used to establish a causal association between weekend admissions and outcomes in patients with pneumonia. Another potential limitation is the exclusion of unpublished studies and those published in languages other than English. With this decision, we may have introduced publication and language biases because we may have missed studies with negative or inconclusive results or those published in other languages. Incorporating a broader range of studies could provide a more comprehensive overview. Additionally, the underlying mechanisms that drive the association between weekend admissions and outcomes in patients with pneumonia remain unclear. The presence of high heterogeneity among some of the outcomes examined is worth noting, it could have arisen from differences in patient demographics, healthcare system characteristics, geographic locations, or other unaccounted factors. Further, performing statistical comparisons to analyze outcomes across various groups of hospitals, levels of staff arrangement, patients' characteristics, and types of pneumonia could have enhanced our understanding at a more detailed level. Unfortunately, not all studies furnished these essential details, and even among those that did, there was insufficient variation in relation to these factors. As a result, conducting statistical comparisons based on these variables was deemed unlikely to produce meaningful and actionable results. We acknowledge this limitation in our study. We recognize the importance of undertaking such an analysis, and to facilitate this, we advocate for future studies to present clear and comprehensive data on these variables. Finally, given that the analysis spans the pre- and during COVID-19 infection era, it is crucial to acknowledge this temporal context. Some of the included studies were published since the year 2019 and could have incorporated data from COVID-19 patients, thereby, introducing a unique aspect to the analysis. The nature of pneumonia cases, treatment protocols, and hospital resources may have been substantially altered to accommodate the challenges posed by the pandemic. Factors such as changes in healthcare infrastructure, and variations in treatment guidelines could have influenced the outcomes being studied. Healthcare systems worldwide underwent significant adaptations to address the surge in COVID-19 cases, potentially impacting the standardization of care and the comparability of results across different time points. Therefore, it is imperative to recognize this limitation when comparing findings across diverse publications with varying timeframes.
Conclusion
Our findings do not support the presence of the weekend effect for patients with pneumonia. This suggests that outcomes in patients with pneumonia are probably not significantly influenced by the timing of admission. Therefore, healthcare providers and policymakers can focus on developing strategies that optimize care delivery and enhance patient outcomes consistently, regardless of the day or time of admission.
Data availability statement
Publicly available datasets were analyzed in this study. This data can be found here: The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Author contributions
JL, XC, and JY wrote the manuscript and made the figures and approved the final revisions of the manuscript submitted for publication. JL and JY conducted the literature search, study selection, and analysis. All authors contributed to the article and approved the submitted version.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2023.1248952/full#supplementary-material
Supplementary Figure 1. Forest plot for in-hospital mortality.
Supplementary Figure 2. Forest plot for mortality at 30-day follow up.
Supplementary Figure 3. Forest plot for admission to ICU.
Supplementary Figure 4. Forest plot for readmission as an outcome.
References
1. GBD 2016 Lower Respiratory Infections Collaborators. Estimates of the global, regional, and national morbidity, mortality, and aetiologies of lower respiratory infections in 195 countries, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Infect Dis. (2018) 18:1191–1210. doi: 10.1016/S1473-3099(18)30310-4
2. Eshwara VK, Mukhopadhyay C, Rello J. Community-acquired bacterial pneumonia in adults: an update. Indian J Med Res. (2020) 151:287–302. doi: 10.4103/ijmr.IJMR_1678_19
3. Mandell LA. Epidemiology and etiology of community-acquired pneumonia. Infect Dis Clin North Am. (2004) 18:761–776. doi: 10.1016/j.idc.2004.08.003
4. McAllister DA, Liu L, Shi T, Chu Y, Reed C, Burrows J, et al. Global, regional, and national estimates of pneumonia morbidity and mortality in children younger than 5 years between 2000 and 2015: a systematic analysis. Lancet Glob Health. (2019) 7:e47–57. doi: 10.1016/S2214-109X(18)30408-X
5. GBD 2015 LRI Collaborators. Estimates of the global, regional, and national morbidity, mortality, and aetiologies of lower respiratory tract infections in 195 countries: a systematic analysis for the Global Burden of Disease Study 2015. Lancet Infect Dis. (2017) 17:1133–1161. doi: 10.1016/S1473-3099(17)30396-1
6. Niederman MS. Pneumonia: considerations for the critically ill patient. Crit Care Med. (2008) 867–883. doi: 10.1016/B978-032304841-5.50045-5
7. Zhang S, Sammon PM, King I, Andrade AL, Toscano CM, Araujo SN, et al. Cost of management of severe pneumonia in young children: systematic analysis. J Glob Health. (2016) 6:010408. doi: 10.7189/jogh.06.010408
8. Al Dallal SAM, Farghaly M, Ghorab A, Elaassar M, Haridy H, Awad N, et al. Real-world evaluation of costs of illness for pneumonia in adult patients in Dubai-A claims database study. PLoS One. (2021) 16:e0256856. doi: 10.1371/journal.pone.0256856
9. Shih P-C, Liu S-J, Li S-T, Chiu A-C, Wang P-C, Liu LY-M. Weekend effect in upper gastrointestinal bleeding: a systematic review and meta-analysis. PeerJ. (2018) 6:e4248. doi: 10.7717/peerj.4248
10. Honeyford K, Cecil E, Lo M, Bottle A, Aylin P. The weekend effect: does hospital mortality differ by day of the week? A systematic review and meta-analysis. BMC Health Serv Res. (2018) 18:870. doi: 10.1186/s12913-018-3688-3
11. Zampieri FG, Lisboa TC, Correa TD, Bozza FA, Ferez M, Fernandes HS, et al. Role of organisational factors on the “weekend effect” in critically ill patients in Brazil: a retrospective cohort analysis. BMJ Open. (2018) 8:e018541. doi: 10.1136/bmjopen-2017-018541
12. Chen Y-F, Armoiry X, Higenbottam C, Cowley N, Basra R, Watson SI, et al. Magnitude and modifiers of the weekend effect in hospital admissions: a systematic review and meta-analysis. BMJ Open. (2019) 9:e025764. doi: 10.1136/bmjopen-2018-025764
13. Bray BD, Steventon A. What have we learnt after 15 years of research into the “weekend effect”? BMJ Qual Saf. (2017) 26:607–10. doi: 10.1136/bmjqs-2016-005793
14. Yang T-Y, Wen Y-W, Chao Y-K. Impact of weekend effect on short- and long-term survival of patients undergoing esophagectomy for cancer: a population-based, inverse probability of treatment-weighted analysis. Ann Surg Oncol. (2023) 30:3790–8. doi: 10.1245/s10434-023-13280-2
15. Fabbian F, De Giorgi A, Di Simone E, Cappadona R, Lamberti N, Manfredini F, et al. Weekend effect and in-hospital mortality in elderly patients with acute kidney injury: a retrospective analysis of a national hospital database in Italy. J Clin Med. (2020) 9:1815. doi: 10.3390/jcm9061815
16. Zhou Y, Li W, Herath C, Xia J, Hu B, Song F, et al. Off-hour admission and mortality risk for 28 specific diseases: a systematic review and meta-analysis of 251 cohorts. J Am Heart Assoc. (2016) 5:e003102. doi: 10.1161/JAHA.115.003102
17. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. (2021) 372:n71. doi: 10.1136/bmj.n71
18. Well G, Shea B, O'Connell D, Peterson J, Welch V, Losos M, et al. The Newcastle-Ottawa (NOS) for assessing the quality of nonrandomized studies in meta-analysis. Ottawa Hospital Research Institute. Available online at: https://www.ohri.ca/programs/clinical_epidemiology/oxford.asp (accessed January 5, 2023).
19. Dettori JR, Norvell DC, Chapman JR. Fixed-effect vs random-effects models for meta-analysis: 3 points to consider. Global Spine J. (2022) 12:1624–6. doi: 10.1177/21925682221110527
20. Higgins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. (2003) 327:557–60. doi: 10.1136/bmj.327.7414.557
21. Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. (1997) 315:629–34. doi: 10.1136/bmj.315.7109.629
22. Bell CM, Redelmeier DA. Mortality among patients admitted to hospitals on weekends as compared with weekdays. N Engl J Med. (2001) 345:663–8. doi: 10.1056/NEJMsa003376
23. Cram P, Hillis SL, Barnett M, Rosenthal GE. Effects of weekend admission and hospital teaching status on in-hospital mortality. Am J Med. (2004) 117:151–7. doi: 10.1016/j.amjmed.2004.02.035
24. Schmulewitz L, Proudfoot A, Bell D. The impact of weekends on outcome for emergency patients. Clin Med (Lond). (2005) 5:621–5. doi: 10.7861/clinmedicine.5-6-621
25. Aylin P, Yunus A, Bottle A, Majeed A, Bell D. Weekend mortality for emergency admissions. A large, multicentre study. Qual Saf Health Care. (2010) 19:213–7. doi: 10.1136/qshc.2008.028639
26. Chang G-M, Tung Y-C. Factors associated with pneumonia outcomes: a nationwide population-based study over the 1997-2008 period. J Gen Intern Med. (2012) 27:527–33. doi: 10.1007/s11606-011-1932-1
27. Gathara D, Irimu G, Kihara H, Maina C, Mbori-Ngacha D, Mwangi J, et al. Hospital outcomes for paediatric pneumonia and diarrhoea patients admitted in a tertiary hospital on weekdays versus weekends: a retrospective study. BMC Pediatr. (2013) 13:74. doi: 10.1186/1471-2431-13-74
28. Suissa S, Dell'Aniello S, Suissa D, Ernst P. Friday and weekend hospital stays: effects on mortality. Eur Respir J. (2014) 44:627–33. doi: 10.1183/09031936.00007714
29. Vest-Hansen B, Riis AH, Sørensen HT, Christiansen CF. Out-of-hours and weekend admissions to Danish medical departments: admission rates and 30-day mortality for 20 common medical conditions. BMJ Open. (2015) 5:e006731. doi: 10.1136/bmjopen-2014-006731
30. Uematsu H, Kunisawa S, Yamashita K, Fushimi K, Imanaka Y. Impact of weekend admission on in-hospital mortality in severe community-acquired pneumonia patients in Japan. Respirology. (2016) 21:905–10. doi: 10.1111/resp.12788
31. Cortes MB, Fernandes SR, Aranha P, Avô LB, Falcão LM. Association between weekend and holiday admission with pneumonia and mortality in a tertiary center in portugal: a cross-sectional study. Acta Med Port. (2017) 30:361–7. doi: 10.20344/amp.8029
32. Baldwin HJ, Marashi-Pour S, Chen H-Y, Kaldor J, Sutherland K, Levesque J-F. Is the weekend effect really ubiquitous? A retrospective clinical cohort analysis of 30-day mortality by day of week and time of day using linked population data from New South Wales, Australia. BMJ Open. (2018) 8:e016943. doi: 10.1136/bmjopen-2017-016943
33. Lawrence H, McKeever TM, Lim WS, on behalf of British Thoracic Society. Admission to hospital in the UK at a weekend does not influence the prognosis of adults with community-acquired pneumonia. Thorax. (2020) 75:594–6. doi: 10.1136/thoraxjnl-2019-214318
34. Milevski SV, Lloyd M, Janus E, Maguire G, Karunajeewa H. Impact of weekend admission and changes in treating team on patient flow and outcomes in adults admitted to hospital with community-acquired pneumonia. Intern Med J. (2021) 51:1681–90. doi: 10.1111/imj.15252
35. Mathew A, Fyyaz SA, Carter PR, Potluri R. The enigma of the weekend effect. J Thorac Dis. (2018) 10:102–5. doi: 10.21037/jtd.2017.12.115
36. Becker DJ. Do hospitals provide lower quality care on weekends? Health Serv Res. (2007) 42:1589–612. doi: 10.1111/j.1475-6773.2006.00663.x
37. Liu C-Y, Kung P-T, Chang H-Y, Hsu Y-H, Tsai W-C. Influence of admission time on health care quality and utilization in patients with stroke: analysis for a possible July effect and weekend effect. Int J Environ Res Public Health. (2021) 18:12362. doi: 10.3390/ijerph182312362
38. Saposnik G, Baibergenova A, Bayer N, Hachinski V. Weekends: a dangerous time for having a stroke? Stroke. (2007) 38:1211–5. doi: 10.1161/01.STR.0000259622.78616.ea
39. Black N. Is hospital mortality higher at weekends? If so, why? Lancet. (2016) 388:108–11. doi: 10.1016/S0140-6736(16)30505-0
40. Corrêa R de A, Costa AN, Lundgren F, Michelin L, Figueiredo MR, Holanda M, et al. 2018 recommendations for the management of community acquired pneumonia. J Bras Pneumol. (2018) 44:405–23. doi: 10.1590/s1806-37562018000000130
41. Grief SN, Loza JK. Guidelines for the evaluation and treatment of pneumonia. Prim Care. (2018) 45:485–503. doi: 10.1016/j.pop.2018.04.001
42. Plouffe JF, Martin DR. Pneumonia in the emergency department. Emerg Med Clin North Am. (2008) 26:389–411. doi: 10.1016/j.emc.2008.02.005
43. Johnson EK, Nelson CP. Values and pitfalls of the use of administrative databases for outcomes assessment. J Urol. (2013) 190:17–8. doi: 10.1016/j.juro.2013.04.048
44. Mazzali C, Paganoni AM, Ieva F, Masella C, Maistrello M, Agostoni O, et al. Methodological issues on the use of administrative data in healthcare research: the case of heart failure hospitalizations in Lombardy region, 2000 to 2012. BMC Health Serv Res. (2016) 16:234. doi: 10.1186/s12913-016-1489-0
Keywords: pneumonia, weekend effect, mortality, readmission, intensive care, systematic review, meta-analysis
Citation: Lu J, Yang J and Cai X (2024) Weekend admissions and outcomes in patients with pneumonia: a systematic review and meta-analysis. Front. Public Health 11:1248952. doi: 10.3389/fpubh.2023.1248952
Received: 27 June 2023; Accepted: 29 December 2023;
Published: 17 January 2024.
Edited by:
Marc Leone, Aix Marseille Université, FranceReviewed by:
Deska Dimitrievska, PHIU Clinic of Pulmology and Allergy-Skopje, North MacedoniaGordana Krljanac, University of Belgrade, Serbia
Copyright © 2024 Lu, Yang and Cai. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jing Yang, WWFuZ2ppbmdkb2NAMTI2LmNvbQ==
 Jiayao Lu
Jiayao Lu Jing Yang
Jing Yang