- 1West China School of Public Health and West China Fourth Hospital, Sichuan University, Chengdu, China
- 2West China-PUMC C.C. Chen Institute of Health, Sichuan University, Chengdu, China
- 3Department of Emergency and Critical Care Medicine, West China School of Public Health and West China Fourth Hospital, Sichuan University, Chengdu, China
- 4Duke Kunshan University, Suzhou, China
- 5Department of Occupational Health, West China School of Public Health and West China Fourth Hospital, Sichuan University, Chengdu, China
- 6Institute for Disaster Management and Reconstruction (IDMR), Sichuan University, Chengdu, China
- 7International Institute of Spatial Life Course Epidemiology (ISLE), Wuhan University, Wuhan, China
- 8Teaching and Research Section of General Practice, The General Practice Medical Center, West China Hospital of Sichuan University, Chengdu, China
Background: Non-suicidal self-injury (NSSI) is a common psychological and behavioral problem among adolescents. The COVID-19 pandemic has had a significant impact on people’s mental health. To date, few studies have documented the temporal changes in adolescents’ psychological status during the pandemic, as well as the impact of large-scale public health intervention strategies. This study contributes to the existing evidence on the subject.
Methods: Participants were 6,023 adolescents aged 10 years and older, with data from two waves of longitudinal surveys, including data for a 7-month interval before and during the pandemic. A cross-lagged model was used to test the bidirectional relationship between NSSI and depressive symptoms in adolescents; logistic regression analysis was used to explore the predictors of NSSI implementation in adolescents with depressive symptoms.
Results: In this study, 32.69% participants reported depressive symptoms at baseline and 34.27% at follow-up; 44.34% participants with depressive symptoms reported NSSI at baseline and 53.44% at follow-up. The duration of the online class, depressed affect, and somatic and related activity were the risk factors for NSSI; sleep duration and positive mood were the protective factors. The lag effect of depression symptoms on NSSI is significant, and so is NSSI on depressive symptoms.
Conclusion: During the COVID-19 pandemic, adolescents’ mental health has worsened, resulting in an increase in the prevalence of NSSI among those with depressive symptoms compared to pre-pandemic levels. Early screening for depression is crucial in preventing or decreasing NSSI in adolescents.
1 Introduction
The outbreak of the COVID-19 pandemic has presented significant challenges to people’s mental well-being (1). After the outbreak, countries, including China, implemented lockdown or semi-lockdown measures, disrupting the normal routines of daily life. The uncertainty and concerns surrounding contracting the virus have intensified the psychological health crisis (2, 3). A systematic review of studies on COVID-19-related psychological distress in countries such as China, Italy, and the United States revealed high prevalence rates of anxiety (6.3 to 50.9%), depression (14.6 to 48.3%), post-traumatic stress disorder (7 to 53.8%), psychological distress (34.4 to 38%), and stress (8.1 to 81.9%) among the general population (4).
The global mental crisis coronavirus disease 2019 (COVID-19) had created a challenging situation for all, especially adolescents. Adolescence is characterized by prominent relationships with peers. Research suggests that friends provide companionship and social and emotional support as adolescents pursue independent development (5). However, home isolation, maintaining social distancing, and closing schools hindered peer interactions, especially school closures, and reduced students’ accessibility to external psychosocial protective resources during COVID-19. Therefore, it is necessary to study the influence of the COVID-19 pandemic on adolescent mental health. Adolescence is a time when the incidence of psychological problems is high, with approximately 50% of psychological disorders, including anxiety, depression, and other negative feelings, appearing before the age of 14 years (6, 7). Data on adolescents before the COVID-19 pandemic in China suggest that 19.9% of adolescents had already experienced depressive symptoms, and 13.99% had experienced anxiety disorders (8). A systematic review and meta-analysis revealed that 28.6 and 25.5% of adolescents experienced symptoms of depression and anxiety, respectively, during the COVID-19 pandemic (9). The COVID-19 pandemic has affected the mental health of adolescents.
Adolescence is also a critical period for mental health issues and risky behaviors such as non-suicidal self-injury (NSSI), which refers to the direct intentional destruction of one’s body without suicidal intent, including cutting, scratching, burns, stabbing, and biting, but is not life-threatening (10, 11). Adolescents are at a high risk of NSSI, with a lifetime prevalence of 17.2% (12). The prevalence of NSSI in Chinese adolescents was 21.9% (13) and 27.4% among middle school students (14). Some data show that the prevalence of NSSI among Chinese adolescents has been on the rise in recent years (15). NSSI not only causes harm to one’s body, but also adversely affects family and interpersonal relationships, and NSSI is also a risk factor for subsequent suicidal behavior (16). There is evidence that NSSI is associated with a range of psychological difficulties, including depression, anxiety, and post-traumatic stress disorder (17). A meta-analysis of factors related to NSSI among Chinese adolescents showed that adolescents with mental health problems were more than 1.5 times more likely to develop NSSI than those without mental health problems (18). A systematic evaluation of 39 studies pointed out that, based on adolescents’ depressive symptoms, one can predict their chances of committing NSSI in the future (19). A longitudinal study with a sample of 813 Chinese adolescents also showed that higher levels of depressive symptoms were associated with an increase in NSSI one year later (20). However, the long-term effects of depressive symptoms on NSSI in adolescents remain unknown in the context of COVID-19.
The WHO emphasized the need for people to study the psychological impact COVID-19 has caused (21). Thus far, there is a relatively small record of longitudinal change in adolescents’ psychological status during the COVID-19 pandemic as well as with the implementation of large-scale public health intervention methods (22–24). To investigate the influence of depressive symptoms on NSSI among adolescents and the occurrence rate of NSSI among adolescents with depressive symptoms, we performed this follow-up study. Furthermore, to assess the bidirectional association between depressive symptoms and NSSI to provide more evidence for a follow-up study of NSSI in Chinese adolescents. Therefore, we hypothesized that during COVID-19, there will be an increase in NSSI behaviors and the incidence of depressive symptoms. In addition, psychological health among adolescents deteriorated, and the prevalence of NSSI among adolescents with depressive symptoms increased compared with that before the pandemic.
2 Methods
2.1 Design and participants
Five schools in Chengdu were selected for this study using multi-stage stratified cluster sampling. Stage 1: The city of Chengdu was divided into high, medium, and low levels according to the level of economic development, with one district randomly selected from each level; Stage 2: One school was randomly selected in each district (county); and Stage 3: all students in the school were included in the study. In this way, we selected one school in the center of Chengdu City and two schools in each of the two suburban counties to the north and south. Among these schools, two schools included both primary and secondary students, two were primary school and one was middle school. All students in the selected schools were included in the survey. Before conducting the targeted school surveys, the researchers coded all students in all schools individually and created survey manuals to train classroom teachers and quality controllers (QC). Then the school was organized to conduct the questionnaire survey and all respondents were grouped into classes, each class was assigned a classroom teacher and a QC. The class teacher led the students to fill in the questionnaire and explained the content of the questionnaire according to the student’s cognitive ability. When the classroom teacher encounters a student question that cannot be answered, the QC will explain.
There are two waves of data collection. The Wave 1 survey was carried out between December 23, 2019, and January 13, 2020 (before the pandemic, at baseline). We did an on-site survey and distributed questionnaires from December 23, 2019 until the end of December. We collected questionnaires and processed data from the beginning of January through January 13, 2020. This was before the outbreak of COVID-19 in Wuhan, China, and the school closure. A year following the baseline survey, a wave 2 survey was planned. It was, however, carried out 6 months ahead of schedule to record the immediate impact of the COVID-19 pandemic. So, from June 16 to July 8, 2020 (during the pandemic, at follow-up), wave 2 data was obtained when schools reopened following the COVID-19 outbreak.
We received 6,190 and 6,654 completed questionnaires in Wave 1 and Wave 2 surveys, respectively, from adolescents aged 10 and up. Finally, 6,023 valid respondents were included after excluding questionnaires with more missing (variable missing more than 20%), not answering attentively, and inconsistent personal information in the two surveys.
2.2 Ethics approval and consent to participate
The study was conducted by the Declaration of Helsinki. The schools, students, and parents participating in the survey provided written informed consent, whereas the children provided parental informed consent before inclusion in the study. The study protocol was approved by the Medical Ethics Committee of Sichuan University (Ethics No. K2020025).
2.3 Measuring tools
2.3.1 Deliberate self-harm inventory, DSHI
The Deliberate Self-Harm Inventory (DSHI) was used to measure the NSSI. Gratz (2) created and verified a scale that Lundh et al. (25, 26) reduced and shortened. The Chinese version of the DSHI has also been proven to have high reliability and validity when applied to Chinese children and adolescents (27, 28). Adolescents were asked if they had ever experienced self-injury, including cuts, burns, scratches, bites, stabbing, or other types of NSSI. To measure the existence or absence of NSSI behaviors, a scoring system was employed, and the frequency of each NSSI was designed as 0 points for “never,” 1 point for “1 time,” 2 points for “2 times,” and 3 points for “3 times or more.” The NSSI scores were categorized into dichotomous “yes” and “no” variables. “Without” refers to a cumulative total score of 0, and “with” refers to a cumulative score of ≥1 for each of the 8 NSSI modalities. Cronbach’s α for the surveyed sample was 0.875.
2.3.2 Center for epidemiologic studies depression scale for children, CES-DC
The Center for Epidemiological Studies for Children (CES-DC) (29) was used to assess depressive symptoms in participants during the past week. Dimensionality and factorial invariance were also investigated (30). Radloff (31) designed the scale. In addition to being widely used worldwide, the CES-DC has been applied to Chinese adolescents with good reliability and validity (32). The CES-DC includes four dimensions: depressed affect (8 items), positive affect (4 items), somatic symptoms and related activity (6 items), and interpersonal (2 items). Each item is answered on a four-point scale (0 = very little or no time, 1 = some or a little time, 2 = moderate or most of the time, and 3 = most or all of the time). A total score of 15 shows no depression symptoms, a total score of 16 to 27 suggests the possibility of depressed symptoms, and a total score greater than 27 indicates confirmed depressive symptoms. Participants who had both the likelihood of and definite depression symptoms were deemed to have depressive symptoms (33). The Cronbach’s α of this study is 0.84.
2.3.3 Demographics and COVID-19 infection history
The demographic data consists of nine items: age (year), gender (boy or girl), self-evaluation of caregiver relationship (Do you have a good relationship with your caregivers? “1 “means very bad,” 10 “means very good”), place of residence (urban and rural), sleep duration, exercise time, and duration of online classes during the pandemic (From the COVID-19 Pandemic to the Back-to-School Period, how long were your daily sleep/exercise time and duration of online classes respectively?), history of COVID-19 infection (Have you or your family members been infected by COVID-19?).
2.4 Data analysis
SPSS (version 22.0) and Mplus (version 7.3) were used to analyze the data. Descriptive statistics include mean and standard deviation (SD) for continuous variables, whereas categorical variables include frequency and percentage. T-test, Chi-square, and logistic regression models were used to analyze the connection between depression symptoms and NSSI. Data that do not follow a normal distribution are represented by the median and quartile, replace the t-test with the Wilcoxon signed rank sum test. Cross-lagged analysis was utilized to explore the bidirectional relationship between depressive symptoms and NSSI. To assess overall model quality and path significance, a variety of fit indices were used, including χ2/df (degrees of freedom), Root Mean Square Error of Approximation (RMSEA), CFI (Comparative Fit Indices), and TLI (Tucker Lewis Index). When χ2/df is less than 5.0, the CFI and TLI are all greater than 0.95 and the RMSEA is less than 0.05, as a good fit, the longitudinal cross-lagged route model is supported (34). Furthermore, the model demonstrates that the proposed model can accurately reproduce the observed longitudinal data. All statistical tests used were two-sided, and a p value of less than 0.05 was considered statistically significant.
3 Results
3.1 Demographic profile of study participants
The study used two waves of data-complete samples, with 6,023 adolescents aged 10 years and older included in the survey. The oldest was 17(Mean age = 11.63, SD = 1.54, at Wave 1). 3,121 boys (51.82%) and 2,902 girls (48.18%) were included. 5,048 adolescents (89.78%) assessed their relationship with caregivers as good (≥ 5 points), and 615 adolescents (10.21%) assessed such relationship as bad (< 5 points). 3,679 (61.08%) of all adolescents included resided in urban areas, while the rest 2,344 (38.92%) lived in rural regions. During the pandemic, adolescents’ average daily sleep duration was 8.64 (1.50) hours, their average physical exercise duration was 1.55 (1.41) hours, and their average online class duration was 5.64 (2.92) hours. COVID-19 infected 111 people (1.84%) and 732 households (12.15%) lost their jobs.
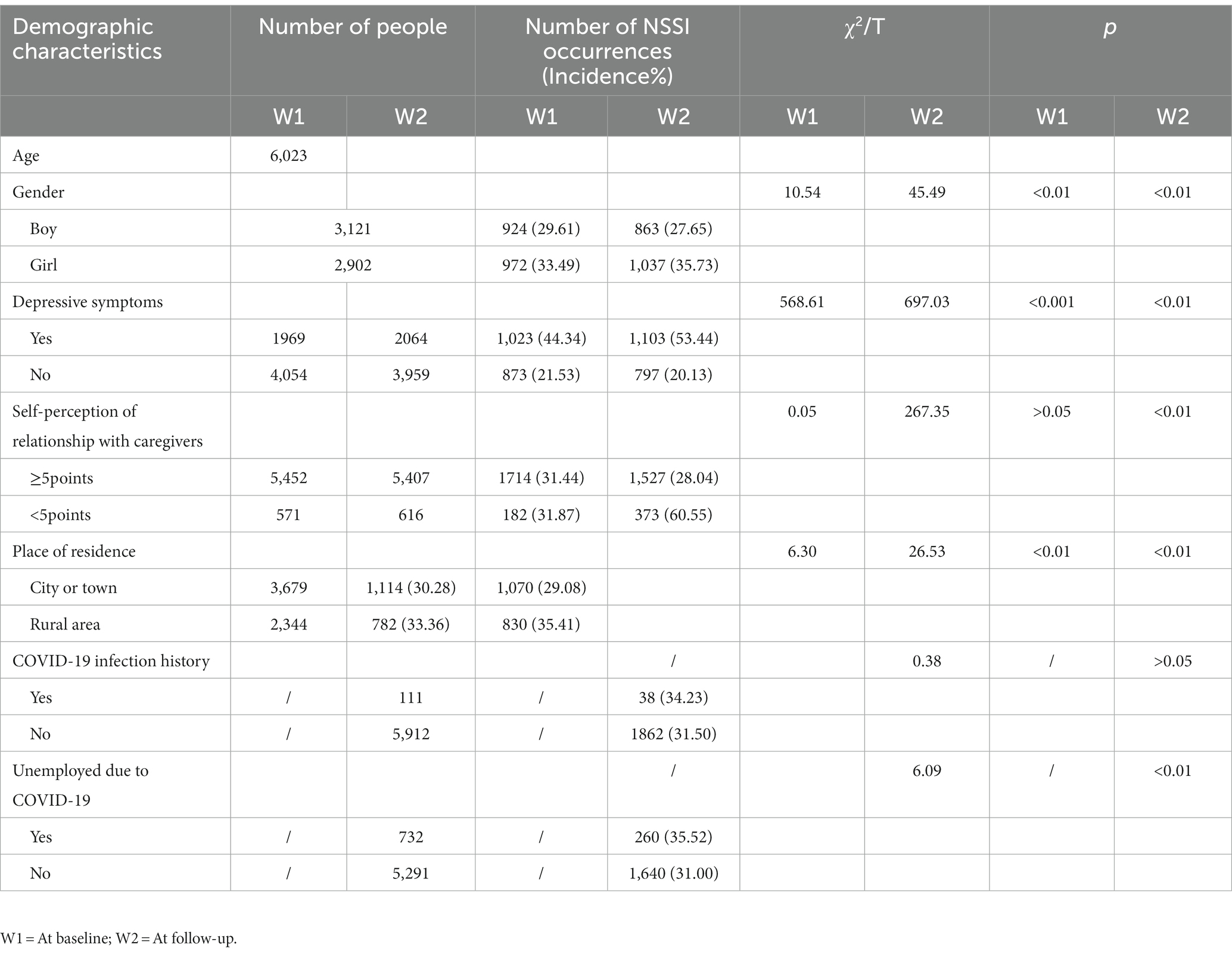
After performing a normality test, we found that the NSSI data did not meet the requirements. Therefore, logarithmic transformation was performed on the NSSI data. At baseline, 29.61% of boys and 27.65% of girls reported NSSIs; at follow-up, the statistics were 33.49 and 35.73%, respectively. Among students with depressive symptoms, the occurrence rate of NSSI was 44.34 and 53.44%, respectively, and the occurrence rate of NSSI increased in both surveys. The occurrence of NSSI decreased among students without depressive symptoms (Table 1).
3.2 The alteration of NSSI and depressive symptoms at baseline and follow-up
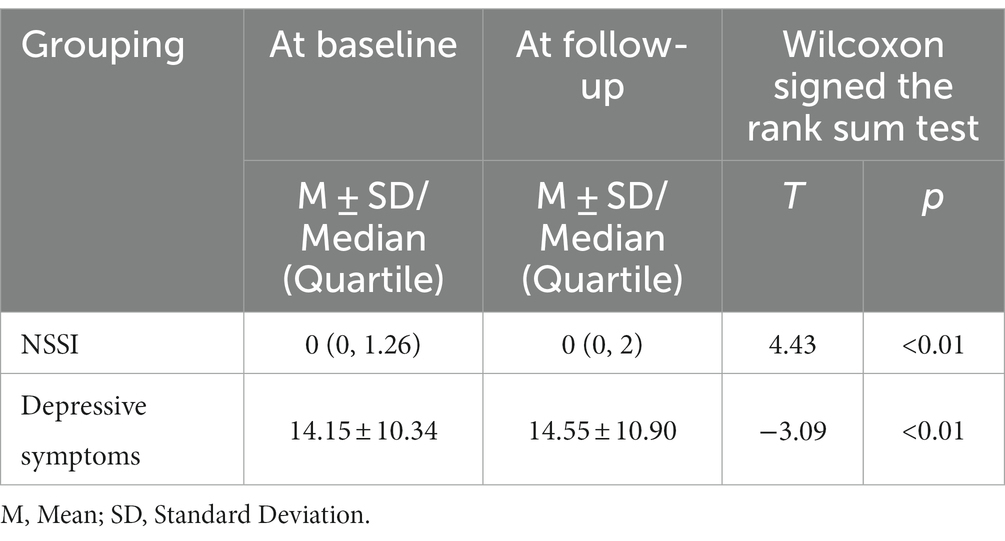
A paired t-test of depressive symptoms was conducted to assess the differences between baseline and follow-up. The Wilcoxon signed-rank sum test was used for NSSI. The NSSI scores showed a statistically significant difference between the baseline and follow-up periods, and the same was observed for depression symptoms, with an increase in scores compared to the previous period (p < 0.01) (Table 2).
McNemar et al. suggested an increase in the incidence of NSSI in adolescents (37.71 to 38.32%); however, the difference was not statistically significant (p > 0.05). The occurrence rate of depressive symptoms among adolescents was higher than that at baseline (32.69–34.27%, p < 0.01) (Table 3).

Table 3. The alteration of the occurrence rate of depression in adolescents at baseline and follow-up.
3.3 The alteration of depression symptoms scores in different dimensions at baseline and follow-up
The test of normality for the four dimensions of depressive symptoms showed that the vast majority of points could be distributed on a straight line with a clear linear trend, and the continuous data could be considered as obeying a normal distribution. Data analysis using independent samples T-test. According to the analysis from the independent sample test, differences exist in the scores of depressed affect, positive affect, somatic and related activity, and interpersonal relationships between the NSSI group and the Non-NSSI group (p < 0.01) (Table 4).

Table 4. The alteration of depression symptoms scores in different dimensions at baseline and follow-up.
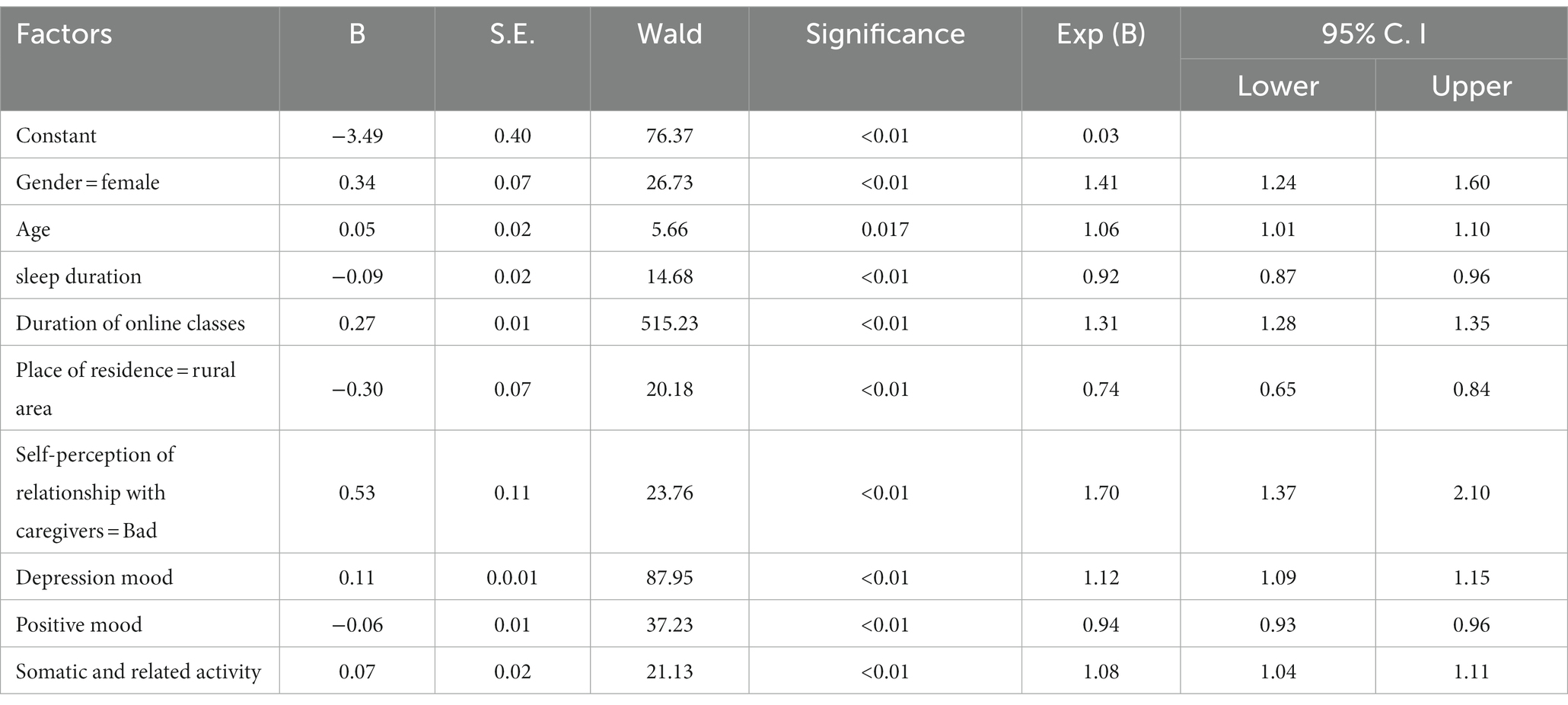
3.4 Binary logistic regression analysis revealing effect on NSSI
Taking whether adolescents commit NSSI as a dependent variable while considering gender, age, depression measurement factors, duration of sleep, duration of exercise, duration of online class, self-perception of relationship with caregivers, residence, and whether unemployed due to COVID-19 as the independent variables, a binary logistic regression analysis (forward: LR method) was conducted. The introduction level was 0.05 and the exclusion level was 0.1. The statistical results showed that among adolescents, females, age, duration of the online class, self-perceived poor relationship with caregivers, depression mood, somatic and related activity were the risk factors for NSSI (or > 1, β > 0), living in rural area, sleep duration and positive mood was the protective factor (or < 1, β < 0) (Table 5).
3.5 Longitudinal, bilateral relations between NSSI and depressive symptoms
A cross-lagged model was used to explore the longitudinal relationship between depressive symptoms and self-injury, with gender and age as control variables. Variables were non-normal data and parameter estimation was performed using the MLM, provided a good fit (χ2/df = 2.74<3, CFI = 0.996>0.95, TLI = 0.993>0.95, RMSEA = 0.017<0.05).
Figure 1 illustrates the normalized coefficients for all model paths. At seven-month intervals, NSSI and depression symptoms were associated, with correlation coefficients of 0.77 (p < 0.05) and 0.27 (p < 0.01), respectively. A steady association was found between pre-pandemic NSSI and post-pandemic NSSI, implying that pre-existing NSSI can predict subsequent (β = 0.43, p < 0.05). The same was true for depression symptoms (β = 0.53, p < 0.05). There was a significant lag effect of adolescents’ depressive symptoms on NSSI, meaning that the deeper the adolescents were depressed, the more frequent their NSSI was, controlling for the adolescents’ baseline NSSI (β = 0.26, p < 0.01). There was also a lag effect of NSSI on depressive symptoms (β = 0.02, p < 0.01). However, depressive symptoms were more predictive.

Figure 1. The cross-lagged model between NSSI and depressive symptoms. Using sex and age as control variables, the two-way arrow in the chart indicates the result of correlation analysis, with the data of correlation coefficient; the one-way arrow indicates the result of path analysis, with the data of standardized regression coefficient (β). *p < 0.05. **p < 0.01. Depression W1: depressive symptoms at baseline; Depression W2: depressive symptoms at follow-up; NSSI W1: NSSI behavior at baseline; NSSI W2: NSSI behavior at follow-up.
4 Discussion
To our knowledge, the hypothesis that “an increase in the prevalence of depressive symptoms and prevalence of NSSI with depressive symptoms” was confirmed. Adolescents had relatively high rates of depressive symptoms (32.69 to 34.27%) and NSSI with depressive symptoms (44.34 to 53.44%). These findings enrich theoretical research on teenage mental health and NSSI in the context of the COVID-19 pandemic. First, this study did not find an increased incidence of NSSI during the COVID-19 pandemic. Nevertheless, the NSSI scores showed statistically significant differences between baseline and follow-up. Prolonged exposure to the uncertainty of infection may trigger vulnerability in adolescents and lead to changes in NSSI from the pre-pandemic period to several months later. There was an increased incidence of NSSI among adolescents with depressive symptoms. This suggests that adolescents with preexisting mental distress perceived the negative events that occurred during COVID-19 as more stressful, which may have contributed to their increased likelihood of participating in NSSI (6, 35). Specifically, adolescents with prior depressive symptoms, relatively high rates of internalizing problem behaviors, and poorer emotional regulation experienced more COVID-19-related stress and were at a higher risk of engaging in NSSI.
NSSI and depressive symptoms in adolescents before COVID-19 predicted these issues after COVID-19. Studies have shown that underlying psychological and psychiatric problems usually occur after disasters, the most common being depression (36, 37). If this theory were applied to the pandemic, we could infer that adolescents who had never experienced mental illness before COVID-19 may experience psychiatric symptoms such as depression, distress, stress, and anxiety. Groups that had previously suffered psychological distress may have exacerbated preexisting mental and emotional distress (38, 39). However, adolescents are emotionally vulnerable and easily stimulated by negative life events to experience emotional outbursts, which, in turn, produce several negative emotions. When there is an inability to regulate negative emotions, they may resort to NSSI to transfer them. According to the experiential avoidance model proposed by Chapman et al., NSSI can provide temporary relief from adolescents’ negative emotions. Nevertheless, when adolescents are again exposed to negative emotional stimuli, they tend to use NSSI for relief, which continuously facilitates the occurrence of NSSI (40). Based on this theory, adolescents with pre-existing vulnerabilities may be more stressed in the face of the COVID-19 pandemic and are at a higher risk of engaging in NSSI. This study also found that NSSI was a predictor of depressive symptoms. NSSIs such as cuts or burns may be a coping mechanism for those experiencing emotional distress or mental health problems. These behaviors may provide temporary relief; nonetheless, they do not address the root cause of distress and can instead lead to feelings of guilt, shame, or despair—common symptoms of depression. Thus, adolescents participating in NSSI are more likely to experience depressive symptoms.
Data from this study found that adolescents who had engaged in the NSSI scored higher on all dimensions of depressive symptoms than those who had not participated in the NSSI; the highest and lowest scores were for depressed affect and interpersonal, respectively. Depression symptoms are primarily defined as emotional problems characterized by a predominantly depressed state of mind, ranging from mildly negative emotional experiences to severe mood disorders (41). In turn, depressive symptoms are associated with chronic dopamine downregulation, which can be accompanied by psychomotor inhibition, and may have a synergistic effect on clinical deficits in adolescents’ affective, cognitive, and motor behaviors, leading to unresponsiveness, reduced speech and movement, reluctance to communicate with others, and enjoyment of solitude, all of which are harmful to adolescents’ interpersonal development (42, 43). Regression analyses revealed that depressed mood and somatic and related activities were risk factors for NSSI. Adverse life events that are usually capable of directly causing negative emotional experiences are risk factors for prompting and maintaining NSSI in adolescents (44).
Adolescents’ self-perceptions of their relationship with their caregivers are predictors of NSSI, and adolescents who perceive themselves as having a poor relationship with their caregivers are more likely to engage in NSSI. Studies have shown that dysfunctional family environments increase the risk of NSSI and that parental conflict and parent–child conflict are associated with a range of psychological problems in adolescents (45, 46). The duration of online classes during the pandemic was also a predictor of NSSI, and the fact that parents had to support their children’s homeschooling while working at home may have increased the risk of parent–child conflict. Past theories on the psychological effects of an approaching disaster have predicted how the place of residence will affect mental health, namely “psychological typhoon eye” (47). The results of this study support the psychological typhoon-eye effect, as adolescents living in rural areas have a lower risk of developing NSSI than those living in urban areas, regardless of whether or not these adolescents have depressive symptoms. The potential explanation was a decrease in social contact. During the pandemic, adolescents have been forced to reduce their social contacts, and involuntary reductions in social contact may cause more suffering among socially active urban adolescents than among rural adolescents. NSSI may also increase as a result of limited social contact, especially among those who are mentally vulnerable. Gender was one of the predictors of adolescent NSSI during the pandemic, consistent with previous findings (48).
Positive emotions were also found to be positive predictors. Evidence from previous studies suggests that disasters and pandemics can stimulate social cohesion and solidarity (49, 50). For example, after the outbreak of severe acute respiratory syndrome in Hong Kong in 2003, residents’ sense of belonging to friends and family increased (51, 52). Therefore, we believe that, in the context of the pandemic, the widely shared experience of combating the pandemic may enhance social cohesion and intimacy, which may change adolescents’ views on death and health. Adolescents who develop psychological disorders may experience a climate of social support during difficult pandemic prevention. During the COVID-19 pandemic, people supported the government’s strategies and measures to prevent and control the pandemic, the community provided help for survival and medical supplies for the sealed control area, and healthcare workers stood firm on the frontline of the fight against the pandemic. Such positive feedback may promote adolescents’ psychological functioning and lead to positive psychological changes. This study also found that sleep duration has an important protective effect against NSSI. Previous studies have identified poor sleep quality and frequent nightmares as important risk factors for NSSI. A study of 223 adolescents with self-harming behaviors found that 2% had serious sleep problems (53). However, adolescents with sleep disorders usually experience NSSI mediated by mood disorders. Shorter sleep duration is directly related to depression (54). Lack of sleep can lead to decreased mood regulation, and chronic sleep deprivation may increase the risk of depression and trigger NSSI.
To conclude, adolescents with NSSI have worse depressive symptoms, and adolescents with depressive symptoms are at higher risk for NSSI; they should be the primary group for attention and intervention. Timely attention should be paid to the negative emotions of adolescents, and screening for depression, as well as their assessment and treatment, should be conducted. For adolescents with NSSI, it is important to intervene as early as possible and provide effective psychological support from schools, families, and society to help them realize the value of life. Finally, it is necessary to develop the mental toughness of young people and improve their abilities to withstand stress and adversity.
5 Limitations
This study had several limitations. To begin, the duration of the follow-up research was 7 months, which is short but fair because we collected data before and after the school shutdown in Chengdu. Furthermore, the Center for Epidemiological Studies for Children (CES-DC) instrument is a self-report screening scale rather than a diagnostic tool, which may be a major limitation. It assesses the intensity of depressive symptoms over the previous week, which is also a short timeframe for making a diagnosis. Finally, as this study collected data using a self-administered questionnaire, there may be some confounding issues, such as remembrance bias and report bias, which could have affected the stability of our study’s longitudinal connection. Further advancements are required in future research. Additionally, the sampling technique for this study was divided geographically, while the discussion was held in urban and rural areas. The use of sample data is insufficient, and there may be conflicting data.
6 Conclusion
Reciprocal effects between depression symptoms and NSSI among Chinese adolescents were found in our study. The increasing trend in the incidence of depressive symptoms and NSSI with depressive symptoms before and during the pandemic, demonstrates that COVID-19 may have had some impact on the mental health of adolescents. The current study also reveals that sleep duration and positive emotions are protective factors for NSSI. Sleep duration is essentially a modifiable influence on depressive symptoms and can also alter the NSSI. Positive emotion, as an intrinsic psychological trait, suggests that future research could already be conducted from a positive psychology perspective, focusing on the positive traits of adolescents.
Data availability statement
The datasets generated and/or analyzed during the study are not publicly available due to reasons of sensitivity e.g. human data. Anonymized data can be made available from the corresponding author on reasonable request.
Ethics statement
The studies involving humans were approved by The study protocol was approved by the Medical Ethics Committee of Sichuan University (Ethics No. K2020025). The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants' legal guardians/next of kin.
Author contributions
RH: writing original draft, writing- reviewing and editing, methodology, data curation, investigation, and formal analysis. L-LP: writing - original draft, writing- reviewing and editing, and data curation. YD, Y-WF, L-SX, and PJ: writing - review & editing. WS: writing - review & editing, methodology, language editing. L-HJ: writing - review & editing, supervision. LZ: conceptualization, methodology, project administration, and funding acquisition. All authors contributed to the article and approved the submitted version.
Funding
This work was supported by The Hong Kong Polytechnic University (19H0642); Research of the 14th Five-Year Plan (2021–2025) for Mental Health Development in Sichuan Province (WJW20211001); Research 0f the 14th Five-Year Plan (2021–2025) for the Mental Health Development in Chengdu (SKZX20220511).
Acknowledgments
We thank Professor Daniel T. L. Shek of Hong Kong Polytechnic University for their research support.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
NSSI, Non-suicidal self-injury; CPCD, Chengdu Positive Child Development; DSHI, Deliberate Self-Harm Inventory; CES-DC, Center for Epidemiologic Studies Depression Scale for Children; M, Mean; SD, Standard deviation; CFI, Comparative fit index; RMSEA, Root Mean Square Error of Approximation; TLI, Tucker-Lewis Index.
References
1. Shek, D, Zhao, L, Dou, D, Zhu, X, and Xiao, C. The impact of positive youth development attributes on posttraumatic stress disorder symptoms among Chinese adolescents under COVID-19. J Adolesc Health. (2021) 68:676–82. doi: 10.1016/j.jadohealth.2021.01.011
2. Gratz, KL. Measurement of deliberate self-harm: preliminary data on the deliberate self-harm inventory. J Psychopathol Behav. (2001) 23:253–63. doi: 10.1023/A:1012779403943
3. Ornell, F, Schuch, JB, Sordi, AO, and Kessler, F. Pandemic fear ' and COVID-19: mental health burden and strategies. Braz J Psychiatry. (2020) 42:333. doi: 10.1590/1516-4446-2020-0011
4. Xiong, J, Lipsitz, O, Nasri, F, Lui, L, Gill, H, Phan, L, et al. Impact of COVID-19 pandemic on mental health in the general population: a systematic review. J Affect Disord. (2020) 277:55–64. doi: 10.1016/j.jad.2020.08.001
5. Fahs, SC, Ulberg, R, Dahl, HJ, and Hoglend, PA. Parental bonding and relationships with friends and siblings in adolescents with depression. Int J Environ Res Public Health. (2022) 19:6530. doi: 10.3390/ijerph19116530
6. De Luca, L, Giletta, M, Nocentini, A, and Menesini, E. Non-suicidal self-injury in adolescence: the role of pre-existing vulnerabilities and COVID-19-related stress. J Youth Adolesc. (2022) 51:2383–95. doi: 10.1007/s10964-022-01669-3
7. World Health Organization. Mental health of adolescents. (2021). Available at: https://www.who.int/news-room/fact-sheets/detail/adolescent-mental-health
8. Rao, W, Xu, D, Cao, X, Wen, S, Che, W, Ng, CH, et al. Prevalence of depressive symptoms in children and adolescents in China: a meta-analysis of observational studies. Psychiatry Res. (2019) 272:790–6. doi: 10.1016/j.psychres.2018.12.133
9. Holmes, EA, O'Connor, RC, Perry, VH, Tracey, I, Wessely, S, Arseneault, L, et al. Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. Lancet Psychiatry. (2020) 7:547–60. doi: 10.1016/S2215-0366(20)30168-1
10. Di Pierro, R, Sarno, I, Perego, S, Gallucci, M, and Madeddu, F. Adolescent nonsuicidal self-injury: the effects of personality traits, family relationships and maltreatment on the presence and severity of behaviours. Eur Child Adolesc Psychiatry. (2012) 21:511–20. doi: 10.1007/s00787-012-0289-2
11. Park, MJ, Paul, MT, Adams, SH, Brindis, CD, and Irwin, CJ. The health status of young adults in the United States. J Adolesc Health. (2006) 39:305–17. doi: 10.1016/j.jadohealth.2006.04.017
12. Swannell, SV, Martin, GE, Page, A, Hasking, P, and St, JNJ. Prevalence of nonsuicidal self-injury in nonclinical samples: systematic review, meta-analysis and meta-regression. Suicide Life Threat Behav. (2014) 44:273–303. doi: 10.1111/sltb.12070
13. Shuangyu, G, du Meijie, L, Xiaorong, SX, Chan, P, and Wanzhu, Z. Meta analysis of the detection rate of non-suicidal self-injury in Chinese adolescents. Modern Prev Med. (2023) 50:26371. doi: 10.20043/j.cnki.MPM.202209070
14. Azhu, HAN, Geng, XU, and Puyu, SU. Meta analysis of epidemic characteristics of non-suicidal self-injury among Chinese mainland middle school students. School Health China. (2017) 38:1665–70. doi: 10.16835/j.cnki.1000-9817.2017.11.019
15. Lang, J, and Yao, Y. Prevalence of nonsuicidal self-injury in chinese middle school and high school students a meta-analysis. Medicine. (2018) 97:e12916. doi: 10.1097/MD.0000000000012916
16. Ribeiro, JD, Franklin, JC, Fox, KR, Bentley, KH, Kleiman, EM, Chang, BP, et al. Self-injurious thoughts and behaviors as risk factors for future suicide ideation, attempts, and death: a meta-analysis of longitudinal studies. Psychol Med. (2016) 46:225–36. doi: 10.1017/S0033291715001804
17. Taylor, PJ, Jomar, K, Dhingra, K, Forrester, R, Shahmalak, U, and Dickson, JM. A meta-analysis of the prevalence of different functions of non-suicidal self-injury. J Affect Disord. (2018) 227:759–69. doi: 10.1016/j.jad.2017.11.073
18. Fan, YY, Liu, J, Zeng, YY, Conrad, R, and Tang, YL. Factors associated with non-suicidal self-injury in Chinese adolescents: a meta-analysis. Front Psych. (2021) 12:747031. doi: 10.3389/fpsyt.2021.747031
19. Fatima, V, Georgina, CB, Lourdes, E, and Tami, K. Nonsuicidal self-injury in community adolescents: a systematic review of prospective predictors, mediators and moderators. J Adolesc. (2018) 65:25–38. doi: 10.1016/j.adolescence.2018.02.012
20. Wu, N, Hou, Y, Chen, P, and You, J. Peer acceptance and non-suicidal self-injury among Chinese adolescents: a longitudinal moderated mediation model. J Youth Adolesc. (2019) 48:1806–17. doi: 10.1007/s10964-019-01093-0
21. World Health Organization. Mental health and psychosocial considerations during the COVID-19 outbreak, Report. (2020). Available at: https://www.who.int/publications/i/item/WHO-2019-nCoV-MentalHealth-2020.1
22. Vindegaard, N, and Benros, ME. COVID-19 pandemic and mental health consequences: systematic review of the current evidence. Brain Behav Immun. (2020) 89:531–42. doi: 10.1016/j.bbi.2020.05.048
23. Wang, C, Pan, R, Wan, X, Tan, Y, Xu, L, McIntyre, RS, et al. A longitudinal study on the mental health of general population during the COVID-19 epidemic in China. Brain Behav Immun. (2020) 87:40–8. doi: 10.1016/j.bbi.2020.04.028
24. Robinson, E, Sutin, AR, Daly, M, and Jones, A. A systematic review and meta-analysis of longitudinal cohort studies comparing mental health before versus during the COVID-19 pandemic in 2020. J Affect Disord. (2022) 296:567–76. doi: 10.1016/j.jad.2021.09.098
25. Bjarehed, J, and Lundh, LG. Deliberate self-harm in 14-year-old adolescents: how frequent is it, and how is it associated with psychopathology, relationship variables, and styles of emotional regulation? Cogn Behav Ther. (2008) 37:26–37. doi: 10.1080/16506070701778951
26. Lundh, LG, Karim, J, and Quilisch, E. Deliberate self-harm in 15-year-old adolescents: a pilot study with a modified version of the deliberate self-harm inventory. Scand J Psychol. (2007) 48:33–41. doi: 10.1111/j.1467-9450.2007.00567.x
27. Lan, T, Jia, X, Lin, D, and Liu, X. Stressful life events, depression, and non-suicidal self-injury among Chinese left-behind children: moderating effects of self-esteem. Front Psych. (2019) 10:244. doi: 10.3389/fpsyt.2019.00244
28. Ming, Wei, and Xia, Liu. A follow-up study on the effects of bullying on self-injury behavior in adolescents: the mediating effect of depression and loneliness. The 20th National Conference on psychology-psychology and National Mental Health; Chongqing, China. (2017). P.2.
29. Radloff, L. The CES-D scale; a self-report depression studies-depression scale with older adults. Clin Gerontol. (1986) 5:119–36. doi: 10.1300/J018v05n01_06
30. Dou, D, Shek, D, Zhu, X, and Zhao, L. Dimensionality of the Chinese CES-D: is it stable across gender, time, and samples? Int J Environ Res Public Health. (2021) 18:11818. doi: 10.3390/ijerph182211818
31. Radloff, LS. The CES-D scale: a self-report depression scale for research in the general population. Appl Psychol Meas. (1977) 1:385–401. doi: 10.1177/014662167700100306
32. Zhou, M, Zhang, G, Rozelle, S, Kenny, K, and Xue, H. Depressive symptoms of Chinese children: prevalence and correlated factors among subgroups. Int J Environ Res Public Health. (2018) 15:283. doi: 10.3390/ijerph15020283
33. Qi, S, Jingyi, Y, Jing, Y, and Huaqing, L. The relationship between adolescent trauma, stress perception, psychological capital and depression. Monthly J Psychol. (2022) 17:32–4.
34. Bentler, PM. Comparative fit indexes in structural models. Psychol Bull. (1990) 107:238–46. doi: 10.1037/0033-2909.107.2.238
35. Guessoum, SB, Lachal, J, Radjack, R, Carretier, E, Minassian, S, Benoit, L, et al. Adolescent psychiatric disorders during the COVID-19 pandemic and lockdown. Psychiatry Res. (2020) 291:113264. doi: 10.1016/j.psychres.2020.113264
36. Mamun, MA, Huq, N, Papia, ZF, Tasfina, S, and Gozal, D. Prevalence of depression among Bangladeshi village women subsequent to a natural disaster: a pilot study. Psychiatry Res. (2019) 276:124–8. doi: 10.1016/j.psychres.2019.05.007
37. Mamun, MA, and Griffiths, MD. PTSD-related suicide six years after the Rana plaza collapse in Bangladesh. Psychiatry Res. (2020) 287:112645. doi: 10.1016/j.psychres.2019.112645
38. Shigemura, J, Ursano, RJ, Morganstein, JC, Kurosawa, M, and Benedek, DM. Public responses to the novel 2019 coronavirus (2019-nCoV) in Japan: mental health consequences and target populations. Psychiatry Clin Neurosci. (2020) 74:281–2. doi: 10.1111/pcn.12988
39. Khan, KS, Mamun, MA, Griffiths, MD, and Ullah, I. The mental health impact of the COVID-19 pandemic across different cohorts. Int J Ment Health Addict. (2020) 20:380–6. doi: 10.1007/s11469-020-00367-0
40. Angelakis, I, and Gooding, P. Experiential avoidance in non-suicidal self-injury and suicide experiences: a systematic review and meta-analysis. Suicide Life Threat Behav. (2021) 51:978–92. doi: 10.1111/sltb.12784
41. Xuliang, S, Xiaofei, Q, Xiaojun, Z, and Ya, Z. Heterogeneous development of depressive symptoms in junior high school students and its relationship with psychological resilience and unsafe attachment. Chin J Clin Psych. (2023) 31:955–9. doi: 10.16128/j.cnki.1005-3611.2023.04.037
42. Damme, K, Park, JS, Vargas, T, Walther, S, Shankman, SA, and Mittal, VA. Motor abnormalities, depression risk, and clinical course in adolescence. Biol Psychiatry Glob Open Sci. (2022) 2:61–9. doi: 10.1016/j.bpsgos.2021.06.011
43. Robison, AJ, Thakkar, KN, and Diwadkar, VA. Cognition and reward circuits in schizophrenia: synergistic, not separate. Biol Psychiatry. (2020) 87:204–14. doi: 10.1016/j.biopsych.2019.09.021
44. Aghamohammadi, S, Mazaheri, MA, Fata, L, and Mootabi, F. The relationship between nonsuicidal self-injury and attachment: protocol for a systematic review and meta-analysis. Jmir Res Protoc. (2023) 12:e40808. doi: 10.2196/40808
45. Nemati, H, Sahebihagh, MH, Mahmoodi, M, Ghiasi, A, Ebrahimi, H, Barzanjeh Atri, S, et al. Non-suicidal self-injury and its relationship with family psychological function and perceived social support among Iranian high school students. J Res Health Sci. (2020) 20:e469. doi: 10.34172/jrhs.2020.04
46. Shao, C, Wang, X, Ma, Q, Zhao, Y, and Yun, X. Analysis of risk factors of non-suicidal self-harm behavior in adolescents with depression. Ann Palliat Med. (2021) 10:9607–13. doi: 10.21037/apm-21-1951
47. Li, S, Rao, LL, Bai, XW, Zheng, R, Ren, XP, Li, JZ, et al. Progression of the "psychological typhoon eye" and variations since the Wenchuan earthquake. PLoS One. (2010) 5:e9727. doi: 10.1371/journal.pone.0009727
48. Wilkinson, PO, Qiu, T, Jesmont, C, Neufeld, S, Kaur, SP, Jones, PB, et al. Age and gender effects on non-suicidal self-injury, and their interplay with psychological distress. J Affect Disord. (2022) 306:240–5. doi: 10.1016/j.jad.2022.03.021
49. Calo-Blanco, A, Kovarik, J, Mengel, F, and Romero, JG. Natural disasters and indicators of social cohesion. PLoS One. (2017) 12:e176885. doi: 10.1371/journal.pone.0176885
50. James, H, and John, R. Social relations that generate and sustain solidarity after a mass tragedy. Soc Forces. (2011) 89:1363–84. doi: 10.1093/sf/89.4.1363
51. Lau, ALD, Chi, I, Cummins, RA, Lee, TMC, Chou, K, and Chung, LWM. The SARS (severe acute respiratory syndrome) pandemic in Hong Kong: effects on the subjective wellbeing of elderly and younger people. Aging Ment Health. (2008) 12:746–60. doi: 10.1080/13607860802380607
52. Lau, JTF, Yang, X, Tsui, HY, Pang, E, and Wing, YK. Positive mental health-related impacts of the SARS epidemic on the general public in Hong Kong and their associations with other negative impacts. J Infect. (2006) 53:114–24. doi: 10.1016/j.jinf.2005.10.019
53. Mcglinchey, ELCEAG. The role of sleep disturbance in suicidal and non-suicidal self-injurious behavior among adolescents. Suicide Life Threat Behav. (2017) 47:103–11. doi: 10.1111/sltb.12268
Keywords: non-suicidal self-injury, depressive symptoms, adolescence, follow-up study, COVID-19
Citation: Hu R, Peng L-L, Du Y, Feng Y-W, Xie L-S, Shi W, Jia P, Jiang L-H and Zhao L (2024) Reciprocal effect between non-suicidal self-injury and depressive symptoms in adolescence. Front. Public Health. 11:1243885. doi: 10.3389/fpubh.2023.1243885
Edited by:
Wulf Rössler, Charité University Medicine Berlin, GermanyReviewed by:
Santiago Resett, Conicet- universidad austral, ArgentinaHongyu Zou, South China Normal University, China
Copyright © 2024 Hu, Peng, Du, Feng, Xie, Shi, Jia, Jiang and Zhao. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Li-Hua Jiang, bGhqaWFuZ0BzY3UuZWR1LmNu
†These authors have contributed equally to this work and share first authorship
 Rui Hu
Rui Hu Li-Li Peng
Li-Li Peng Yu Du
Yu Du Yi-Wei Feng
Yi-Wei Feng Lin-Shen Xie
Lin-Shen Xie Wei Shi
Wei Shi Peng Jia
Peng Jia Li-Hua Jiang
Li-Hua Jiang Li Zhao
Li Zhao