- 1Public Health, Societies and Belonging, Human Sciences Research Council, Pretoria, South Africa
- 2Aquity Innovations, Port Elizabeth, South Africa
- 3eResearch Knowledge Centre, Human Sciences Research Council, Pretoria, South Africa
- 4College of Humanities, University of KwaZulu-Natal, Durban, South Africa
Background: Amidst widespread public health recommendations and availability of COVID-19 vaccinations, half of South African adults are vaccinated against COVID-19. This study investigated the socio-behavioral determinants of vaccine hesitancy in South Africa, where vaccine hesitancy was separated into unwilling ness and uncertainty to take a COVID-19 vaccine.
Methods: Data was collected from a large-scale public survey during June–October 2021 that included online and telephonic surveys. Vaccination hesitancy was based on the question “When available, would you take the COVID 19 vaccine?,” with responses categorized into those who were willing, unwilling, and uncertain about taking a COVID-19 vaccine. Multinomial regression examined the association between socio-behavioral variables and vaccine hesitancy.
Results: Overall, 73.8% reported they would definitely or probably take the vaccine, 16.4% were uncertain and 9.9% reported they probably or definitely would not (n = 16,988). Younger age, White and Colored population groups, no influenza vaccination history, previous vaccination refusal, knowing someone who experienced a serious vaccination side-effect, misperceptions about vaccine benefits, cultural or religious discouragement from taking a COVID-19 vaccination, lack of governmental confidence, concerns about side-effects, perceived lack of safety information, and lack of trust in the pharmaceutical industry and in the information from health care providers were all associated with higher odds of being uncertain and unwilling to take a COVID-19 vaccination. Strengths of association for unwillingness and uncertainty varied by the explanatory variables. Concern about effectiveness due to fast development was associated with uncertainty to take the vaccine but not with unwillingness. Concerns about side-effects had stronger associations with uncertainty than with unwillingness, while previous vaccine refusal, misperceptions of the protective benefits of vaccines, White population group, religious/cultural discouragement, and lack of trust in the pharmaceutical industry and health care providers’ information had stronger associations with unwillingness than uncertainty.
Conclusion: The determinants of COVID-19 vaccine hesitancy should be addressed in interventions to improve vaccine uptake. Public health interventions and health communication can be prioritized and tailored to the different forms of vaccination hesitancy.
Introduction
Vaccine hesitancy, defined by the World Health Organization as the “delay in acceptance or refusal of vaccination despite availability of vaccination services,” was among the top 10 global health threats in 2019 (1). There is a continuum of vaccine hesitancy between complete acceptance and absolute refusal of all vaccines (2).
Despite COVID-19 vaccinations being one of the most effective strategies to control the pandemic, vaccination acceptance and uptake rates vary significantly globally (3). By January 2023, 64% of people worldwide were fully vaccinated against COVID-19 and 70% had received at least one vaccine dose (4, 5), with the African continent having far lower vaccination coverage (4). An in-depth understanding of the socio-behavioral determinants of COVID-19 vaccination hesitancy and the characteristics of people who are more likely to be uncertain about or refuse a COVID-19 vaccine is required for comprehensive and effective vaccination strategies. Interventions to improve vaccine uptake can be tailored to the various positions held along the vaccine acceptance continuum.
South Africa’s national vaccination program began in February 2021 with a staggered approach starting with healthcare workers and then age groups from oldest to youngest eligible. Amidst public health recommendations and wide availability of COVID-19 vaccinations in the country, only half of South African adults and 35% of children aged 12–17 had been vaccinated by March 2023 (6). Adults aged 30 or older and females had higher vaccination rates than young adults and males. Vaccination rates have stagnated since mid-2022.
Vaccine hesitancy, in general, is influenced by an array of cognitive, socio-demographic, psychologic, political and cultural factors (7). The literature on factors associated with COVID-19 vaccine hesitancy identifies issues around vaccine safety and efficacy, risk perceptions of COVID-19 infection and its severity, and concerns about the rapid development of the COVID-19 vaccines as prominent factors (7–13). Given that the COVID-19 vaccines were developed faster than other vaccines in the past, this has evidently contributed to hesitancy (7). Issues of trust play a key role in regulating vaccine acceptance, including trust in governments, health professionals, scientists and the pharmaceutical industry (14, 15). Sources of information about the pandemic and vaccinations (16) are another contributing factor. Misinformation and disinformation can diminish vaccine acceptance (17, 18). The flood of information about the pandemic and COVID-19 vaccines, often termed the COVID “infodemic,” included both factual and misleading or false information, that complicates access to reliable information about vaccination (19). Poor influenza-vaccination history also resulted in hesitancy to take a COVID-19 vaccination in several studies (11, 15, 18). In terms of socio-demographic factors, vaccine hesitancy was found to be higher in individuals with lower education levels and awareness, minority race groups, younger age groups, some women, and lower income groups (7, 15, 18).
This study investigated the socio-behavioral factors associated with COVID-19 vaccine hesitancy among South African adults aged 18 years and older during the third quarter of 2021, using data from a national survey. While the majority of studies on vaccine hesitancy in South Africa and internationally have focused on vaccine hesitancy as a homogenous group, this study aims to bridge that gap by separating hesitancy into individuals who were unwilling or did not want to be vaccinated and those who were uncertain about their intentions to be vaccinated. It was hypothesized that the identified factors and their strengths of association would differ for those who were unwilling versus those who were uncertain to receive the vaccination.
Materials and methods
Study design and setting
Data were collected using an online survey questionnaire and telephone facilitated interviews between 25 June and 11 October 2021. South Africans aged ≥18 years in all nine provinces were eligible to participate. During this data collection period, the country was experiencing its third wave of COVID-19 infections, with higher hospitalization rates than the previous two waves (20). A strict lockdown was implemented during July 2021. The country’s vaccination program was also underway, where vaccinations became available to persons aged 60 and older from mid-May 2021, to those aged 50–59 by July 2021, to those aged 35–49 from 1 August 2021; and by the end of August 2021, vaccinations were available to all adults aged 18 and older. Children aged 12 and older followed from October 2021. Furthermore, some employment categories such as educators and police service employees were prioritized during June and July 2021 (21).
Information about the survey and the invitation to participate were distributed on a data-free mobile messaging platform as well as on social media platforms, national and local radio, national television, local websites and communication networks in government, education, faith-based and community organizations, non-profit organizations and private sector organizations. The data-free mobile messaging platform has a substantial user-base of over 4 million South Africans, and it is accessible from most application stores. The data-free platform facilitated survey completion without incurring user data costs. This methodology was used previously by the authors (22, 23). The questionnaire and telephonic interviews were available to complete in six of South Africa’s languages; namely, English, Afrikaans, isiZulu, TshiVenda, xiTsonga and isiXhosa.
Telephonic interviews supplemented the online survey approach in order to include participants that would not typically participate in online surveys. Interns employed by the Human Sciences Research Council were selected to work as telephone interviewers. The interns were aged between 20 and 35 years, had attained a graduate degree and were enrolled in an experiential training program in social sciences research at the Human Sciences Research Council (HSRC). The interviewers were trained in procedures for obtaining informed consent and administering telephone interviews. The interviewers were collectively fluent in the six languages in which the survey could be completed. An anonymized list of telephone numbers of over 1 million people residing in predominantly densely populated areas such as informal settlements and townships (urban residential settlements) was used to recruit participants in the telephone survey, where 16,000 people from the list were selected and telephonically contacted and 7,962 participated.
Questionnaire development
The questionnaire was developed by a research team at the HSRC that constituted epidemiologists, and public health and behavioral scientists. The questionnaire development was informed by previous public online survey research conducted by the HSRC research team during the emergence of the COVID-19 pandemic (22–25) as well as previous a multi-country survey (26), and the questionnaire development was conducted in consultation with the South African National Department of Science and Technology. The questionnaire was refined using inputs from stakeholders in scientific and civil society networks. The thematic areas included in the questionnaire covered demographic characteristics, attitudes and experiences of vaccinations; culture, context and communications regarding the COVID-19 vaccinations, opinions on South Africa’s vaccination plan, grief and coping during the pandemic, social distancing behavior, the socio-economic impact of COVID-19, and family relationship dynamics during the COVID-19 pandemic. The questionnaire items were predominantly close ended.
Measures
The primary outcome variable, COVID-19 vaccination hesitancy, was derived from the question “When available, would you take the COVID 19 vaccine?” with five possible response options 1 = “Yes definitely, I would take the vaccine,” 2 = “Yes probably, I would take the vaccine,” 3 = “I am uncertain at this stage,” 4 = “No, probably I would NOT take the vaccine” and 5 = “No definitely, I would NOT take the vaccine.” The responses were recoded into three categories where 1 = “Willing: Would take the vaccine” (coded from options 1 and 2 above); 2 = “Uncertain” and 3 = “Unwilling: Would not take the vaccine” (coded from options 4 and 5 above).
The selection of explanatory variables was informed by the literature on COVID-19 vaccine hesitancy [7–16]. The explanatory variables used can be categorized as socio-demographic (gender, age group, population group, province, community type, educational attainment, employment), experiences and perceptions related to other vaccines or vaccines in general (having ever taken the influenza vaccine, having ever refused to take any vaccine, knowing anyone who experienced a serious side-effect to any vaccine, thinking that vaccines are a good way to protect communities from disease), information on the COVID-19 vaccinations (main source of information on the COVID-19 vaccinations, having heard conflicting or confusing information about the COVID-19 vaccinations), religious/cultural influence (feeling that one’s religion or culture would discourage one from receiving a COVID-19 vaccination), trust/confidence in governments and health and scientific institutions (level of confidence in how the national government was handling the pandemic, trust in the pharmaceutical industry with developing the COVID-19 vaccine, trust in the information from one’s health care provider about the COVID-19 vaccinations), perceptions of risk, safety and efficacy (concerned about side-effects related to the COVID-19 vaccines, thinking that there is adequate safety information related to the COVID-19 vaccination program, perception that the effectiveness of the COVID-19 vaccine will be in question due to its fast development and having lost anyone close to you during the lockdown period).
The questions from which these variables are based are presented in Supplementary File S1. Population group was reported in alignment with Statistics South Africa’s standard classification categories (27).
Statistical analysis
Data were analyzed on participants who responded to the question on vaccine hesitancy. Analyses were performed using Stata 15.0 (Stata Corporation, College Station, Texas, United States). The data were benchmarked using the South African adult mid-year population estimates for 2021 by age, sex, population group and province (27) in order to increase generalizability of the estimates at national level. The percentages of participants who did want to receive a COVID-19 vaccine, who were uncertain at the time, and who did not want to receive the vaccine were tabulated by the explanatory variables of interest, with Pearson Chi-square tests used to identify significant differences in estimates.
Multivariate multinomial logistic regression was used to determine the explanatory variables associated with being uncertain and unwilling to receive the COVID-19 vaccine, where “would take the vaccine” was used as the reference category. The explanatory variables that exhibited a significant univariate association with the outcome variable, as determined by Chi-square tests, were included in the multivariate multinomial model. Pairwise correlations between the explanatory variables were used to check for multicollinearity. However, all pairwise correlation coefficients were less than 0.35. Odds ratios and their 95% confidence intervals measured the strength and direction of the associations in the multinomial regression model. All statistical tests were considered significant at p < 0.05.
Results
Description of the weighted sample
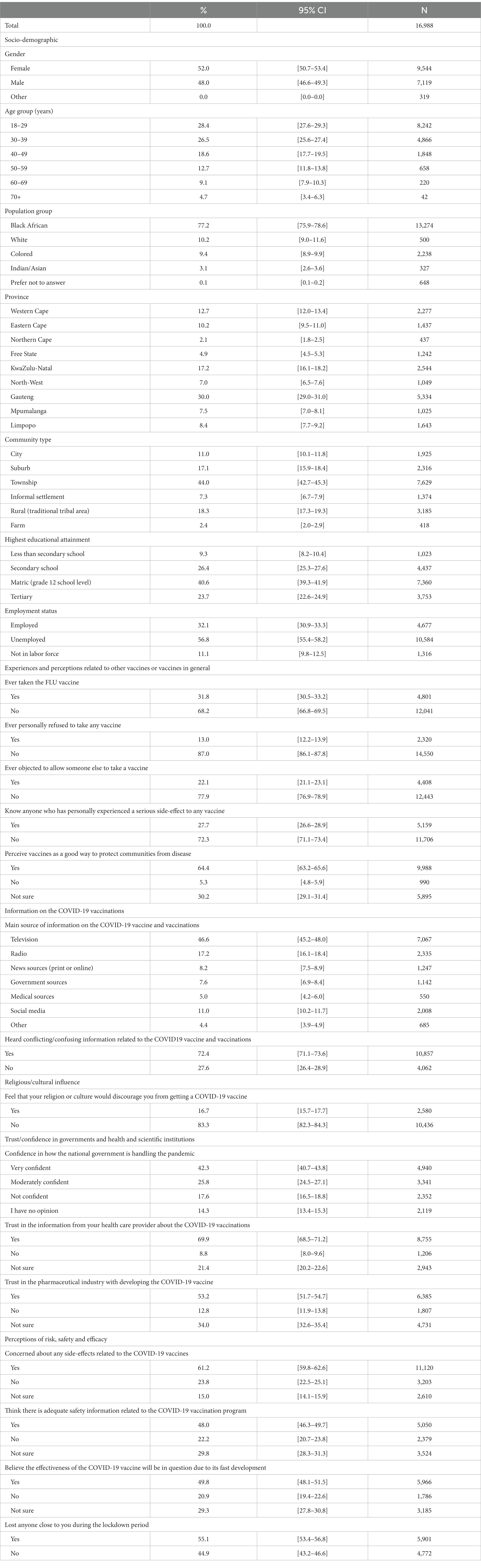
The sample comprised 52% females and the mean age was 40.1 years (Standard. error = 0.355) (Table 1). Over three-quarters (77.2%) identified as Black African. Over 64% had completed secondary school and 56.8% were employed. Regarding previous experiences with vaccines in general, almost a third (31.8%) had ever taken an influenza vaccination, 13.0% had ever refused to receive any vaccination, 22.1% had objected to allow someone else to receive a vaccination, 27.7% knew someone who had experienced a serious side-effect to any vaccine and 64.4% thought that vaccines were a good way to protect communities from disease. The most prevalent responses to the main source of information on the COVID-19 vaccine and vaccinations were television (46.6%), followed by radio (17.2%) and social media (11.0%). Almost three in four people (72.4%) reported hearing conflicting or confusing information about the COVID-19 vaccine and vaccinations and 16.7% felt that their religion or culture would discourage them from taking a COVID-19 vaccine. Moderate or high confidence in the government’s handling of the pandemic was reported by 68.1% of participants, while 69.9% trusted the information from their health care providers about the COVID-19 vaccinations and 53.2% trusted the pharmaceutical industry with developing the vaccine. Over 60% were concerned about side-effects from the COVID-19 vaccine, 48.0% thought there was adequate safety information about the COVID-19 vaccination program and 49.8% thought the effectiveness of the vaccinations would be in question due to their fast development.
Vaccine hesitancy by explanatory variables
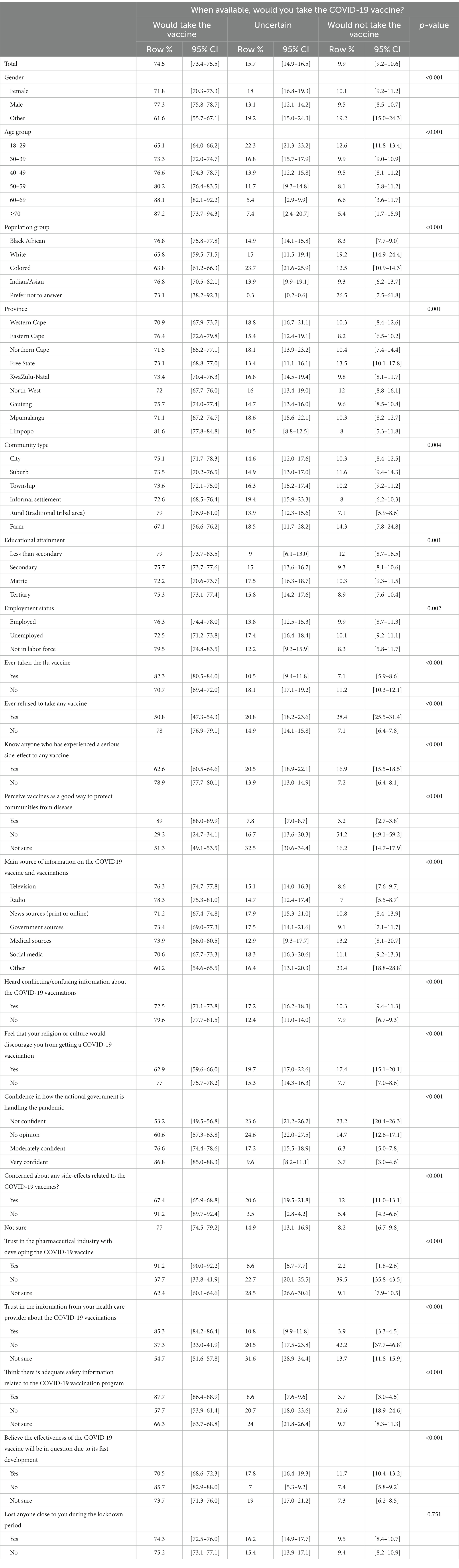
Overall, 74.5% of the eligible participants reported that they would take a COVID-19 vaccine, 15.7% were uncertain at the time and 9.9% would not take the vaccine.
The percentages of participants who were willing, uncertain and unwilling to take a vaccine varied significantly with all the explanatory variables (Table 2). We highlight the characteristics of people who were uncertain or unwilling to vaccinate. Vaccine hesitancy, that is, the prevalence of being uncertain or unwilling to take a vaccine, were both higher among 18–29-year-olds, those who had never received an influenza vaccination, those who had previously refused to take a vaccine, who knew someone who experienced a vaccine-related side-effect, who heard conflicting information about the COVID-19 vaccinations, who were not confident in the government’s handling of the pandemic, who did not trust or were unsure of their trust in the pharmaceutical industry with vaccine development and in the information from their health care providers, who felt religious or cultural discouragement about the vaccinations, and among those who had concerns about side-effects, safety and effectiveness.
Factors associated with vaccine hesitancy
Characteristics of those who were uncertain about taking a COVID-19 vaccination
The adjusted odds of being uncertain about taking a COVID-19 vaccination, compared to being willing to take a vaccination, were significantly higher for the following groups: adults who identified as White (Adjusted Odds Ratio (AOR) = 2.78 [1.80–4.29]) or Colored (AOR = 2.12 [1.57–2.86]) than those who identified as Black African; who had ever refused to take any vaccine (AOR = 1.89 [1.38–2.6]) than those who had not refused; who did not think that or were unsure about whether vaccines were a good way to protect communities from disease (AOR = 4.05 [2.62–6.26], AOR = 3.38 [2.75–4.16], respectively); who felt that their religion or culture would discourage them from getting a COVID-19 vaccination (AOR = 1.39 [1.03–1.9]); who were not confident in the national government’s handling of the pandemic (AOR = 1.43 [1.1–1.86]) compared to those who were very confident; who had concerns about side-effects of the COVID-19 vaccines or were unsure if they had concerns about side-effects (AOR = 6.32 [4.3–9.29] and AOR = 2.92 [1.91–4.46], respectively) than those with no concerns about side-effects; who did not trust or were not sure if they trusted the pharmaceutical industry with developing COVID-19 vaccines (AOR = 3.07 [2.24–4.21] and AOR = 2.53 [1.97–3.25], respectively); who did not trust or were unsure if they trusted the information from their health care provider about the COVID-19 vaccinations (AOR = 1.7 [1.25–2.38] and AOR = 1.89 [1.48–2.42], respectively); who did not think or were unsure about whether there was adequate safety information about the COVID-19 vaccination program (AOR = 1.45 [1.1–1.91] and AOR = 1.44 [1.14–1.82], respectively) and those who believed that the effectiveness of the COVID 19 vaccine would be questionable due to its fast development (AOR = 1.66 [1.2–2.31]) (Table 3).
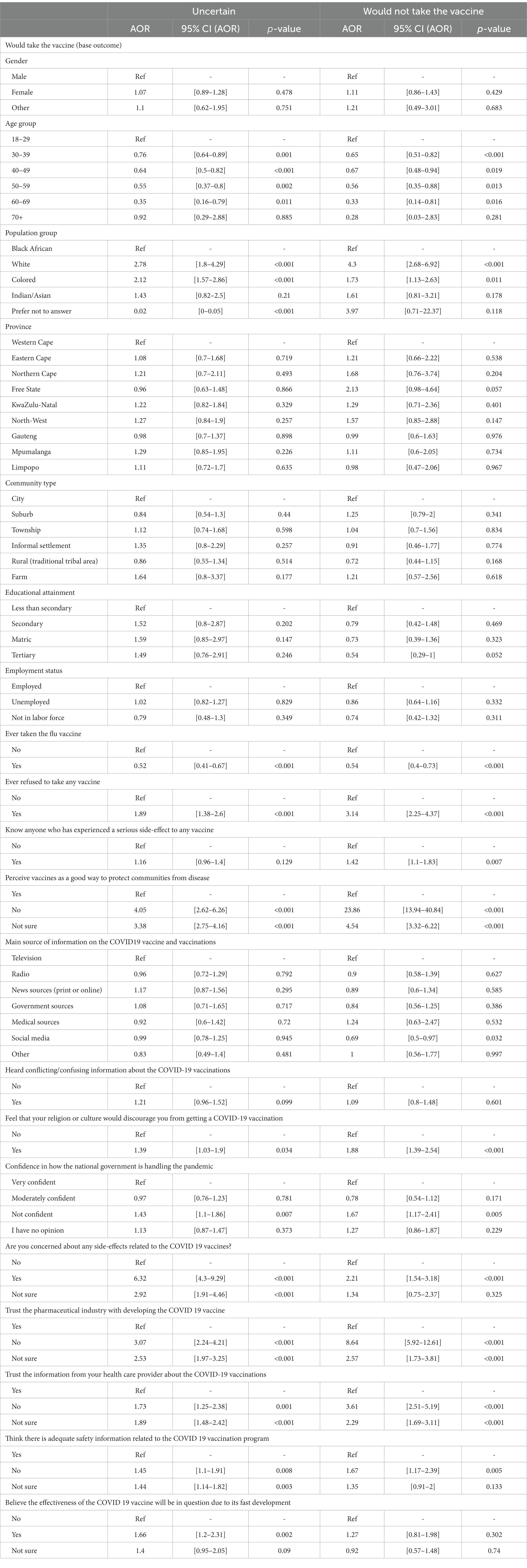
Table 3. Socio-behavioral factors associated with vaccination hesitancy—multiple multinomial regression model.
In addition, the odds of being uncertain about taking a COVID-19 vaccination, compared to being willing to take a vaccination, were significantly lower for older adults aged 30–39, 40–49, 50–59 and 60–69 years (AOR = 0.76 [0.64–0.89], AOR = 0.64 [0.5–0.82], AOR = 0.55 [0.37–0.8] and AOR = 0.35 [0.16–0.79], respectively) than those aged 18–29; those who preferred not to report their population group (AOR = 0.02 [0–0.05]) than those who identified as Black African and among those who had ever received an influenza vaccination (AOR = 0.52 [0.41–0.67]) than those who had not.
Characteristics of those who were unwilling to take a COVID-19 vaccination
The adjusted odds of being unwilling to take a COVID-19 vaccination, compared to being willing to take one, were significantly higher for adults who identified as White or Colored (AOR = 4.3 [2.68–6.92], AOR = 1.73 [1.13–2.63]) than those who identified as Black African; among those who had ever refused to receive any vaccine (AOR = 3.14 [2.25–4.37]); who knew anyone who experienced a serious side-effect to a vaccine (AOR = 1.42 [1.1–1.83]); who did not perceive or were unsure if they perceived vaccines as being a good way to protect communities from diseases (AOR = 23.86 [13.94–40.84] and AOR = 4.54 [3.32–6.22], respectively); who felt religious or cultural discouragement from taking a COVID-19 vaccine (AOR = 1.88 [1.39–2.54]); who expressed no confidence in the national government’s handling of the pandemic (AOR = 1.67 [1.17–2.41]); who had concerns about side-effects of the COVID-19 vaccines (AOR = 2.21 [1.54–3.18]); who did not trust or were unsure if they trusted the pharmaceutical industry with developing the vaccines (AOR = 8.64 [5.92–12.61] and AOR = 2.57 [1.73–3.81], respectively); who did not trust or were unsure if they trusted the information from their health care provider about the COVID-19 vaccines (AOR = 3.61 [2.51–5.19] and AOR = 2.29 [1.69–3.11], respectively); and who did not think there was adequate safety information about the COVID-19 vaccination program (AOR = 1.67 [1.17–2.39]) (Table 3).
Unwillingness to take a COVID-19 vaccination, compared to willingness to take one, were significantly lower for older adults aged 30–39, 40–49, 50–59 and 60–69 years (AOR = 0.65 [0.51–0.82], AOR = 0.67 [0.48–0.94], AOR = 0.56 [0.35–0.88], AOR = 0.33 [0.14–0.81], respectively) than 18–29 year-olds; for those who had ever received an influenza vaccination (AOR = 0.54 [0.4–0.73]); and whose main source of information on the COVID-19 vaccinations were from social media (AOR = 0.69 [0.5–0.97]).
The socio-demographic factors (gender, education, province, community type and employment status) and having heard conflicting information about the COVID-19 vaccinations, which had significant bivariate associations with vaccine hesitancy, were no longer significantly associated with unwillingness and uncertainty about receiving a vaccination in the regression model which adjusted for all the explanatory variables.
Discussion
The current study identified several socio-behavioral factors associated with vaccine hesitancy among South African adults, including being of younger age, being of the White and Colored population groups, no history of influenza vaccination, previous vaccination refusal, and knowing someone who experienced a serious vaccination side-effect. Other factors such as misperceptions about vaccinations being beneficial in protecting communities, experiencing cultural or religious discouragement from taking a COVID-19 vaccination, no confidence in the government’s handling of the pandemic, and having concerns about side-effects of the COVID-19 vaccinations were also found. The perceived lack of safety information about the COVID-19 vaccinations and lack of trust in the pharmaceutical industry and in the information from health care providers also contributed to vaccine hesitancy. The following items had stronger associations with unwillingness to take a COVID-19 vaccination than with uncertainty to take the vaccinations: previous refusal to receive any vaccination, not perceiving vaccines as beneficial for protecting communities from disease, individuals from the White population group, religious or cultural discouragement, and lack of trust in the pharmaceutical industry and in the information from health care providers. Concerns about effectiveness of the COVID-19 vaccines due to their fast development was associated with being uncertain about taking the vaccine but not with being unwilling. Having concerns about side-effects had stronger associations with uncertainty to take the vaccine than with unwillingness.
As vaccine-hesitant individuals are a heterogeneous group with varying levels of indecision and apprehensions (19), individuals who are uncertain about their intentions to take a COVID-19 vaccination lie more toward the center of the continuum compared to those who are unwilling. These individuals could be viewed as more amenable to changing their vaccination intentions if their apprehensions are sufficiently addressed than those who reported that they would not take a vaccination, thereby providing key opportunities for public health action. Interventions to improve vaccine uptake should address the identified determinants of vaccine hesitancy. However, interventions can be tailored for those uncertain and unwilling to take a COVID-19 vaccination by addressing the respective determinants of these two types of hesitancy. Therefore, addressing concerns about effectiveness, rapid vaccine development and side-effects need to be focused on more intensively for individuals who are more uncertain about their decision to vaccinate. In comparison, reliable information about why vaccines are protective at population-level, addressing the influence of religious or cultural social norms and attitudes on vaccine behavior and addressing issues of trust in pharmaceutics and the health system are important for individuals who are leaning more toward refusing a COVID-19 vaccination. Furthermore, in the case of adamant vaccine refusers, public health programs should seek to curtail the effect of their anti-vaxxer discourses on other individuals rather than convincing them to change their stance (19).
The finding of higher vaccine hesitancy among young South Africans is consistent with other South African (13, 28, 29) and international studies (15) and evidenced by the lower rates of vaccination coverage among youth in the country (6). Younger individuals tend to be more vaccine hesitant due to their lower risk perceptions regarding severity of COVID-19 in their age group (15). Increasing youth vaccination uptake is important for immunizing communities, due to South Africa having a relatively young population where many youths live in multigenerational households with exposure to older adults. White race was also a predictor of vaccine hesitancy in the United States and Brazil (13, 30, 31). Earlier South African studies confirmed vaccine hesitancy to be highest among White followed by Colored individuals (12, 13). In fact, one study showed that between January to July 2021, vaccine hesitancy increased among white adults, while it decreased for black African adults. It found that concerns about side-effects and vaccine effectiveness were more pronounced among White adults (12).
Favorable experiences with other vaccines can enhance and reinforce trust, self-efficacy and intention regarding taking a COVID-19 vaccination. Having an influenza vaccine and having not refused other vaccines in the past were predictors of vaccine hesitancy. However, as in many developing countries, the majority of the population do not take influenza vaccinations (32). Moreover, Makoae et al. (33) found that South African parents who had never taken an influenza vaccine were significantly less likely to have taken their children for their scheduled vaccinations. Perceptions of vaccines being beneficial for protecting communities was strongly associated with hesitancy, but particularly so with unwillingness to take the vaccination. Lee et al. (34) found that healthcare professionals and community stakeholders who thought that the vaccine could strengthen their immunity against COVID-19, that vaccination was an effective way to prevent COVID-19, that the benefits of COVID-19 vaccination outweighed its harm, and that the vaccine could lower the risk of transmitting the viruses to their family and friends were significantly more likely to get vaccinated. Transparent information, effective science communication strategies and health provider and community discourses are needed to build a greater understanding of why vaccines are needed, how they work in creating herd and population immunity, and how they are developed.
Given that feeling religious or cultural discouragement from taking a COVID-19 vaccine was associated more with unwillingness than uncertainty to take the vaccine; involving religious, traditional and community leaders in vaccine and risk communication and community engagement campaigns can help raise awareness and change social norms (35). Katoto et al. (28) found that many South African community members expressed the desire for religious leaders to be involved in vaccination education programs. Discourses between community members and trusted leaders can help individuals reconcile their vaccination decisions with their values and beliefs. Sharing of personal experiences with vaccines among community members is important.
This study showed that individuals who expressed no confidence in the national government’s handling of the pandemic were more likely to be unwilling or uncertain to take a COVID-19 vaccination. Distrust of government was one of the major predictors of vaccine hesitancy in other South African studies (28, 36). Lack of confidence in government’s handling of the pandemic was also associated with lower engagement in transmission reducing behaviors like social distancing (25). This distrust in government may be due to probes of corruption and fraud related to COVID-19 contracts issued by the South African government (37). Initiatives to address corruption and promote transparent concise communication from government are required.
Mistrust in the pharmaceutical industry, the manufacturers of the COVID-19 vaccines, was a strong predictor of vaccine hesitancy and especially unwillingness to take a COVID-19 vaccine. In 2019, pharmaceutical companies were perceived as the most poorly regarded industry in the United States (38); a perception which is likely to have filtered through to the rest of the world. As such, there has always been public concern over commercial profiteering from the COVID-19 vaccine production (14). Risk and uncertainty are fundamental assumptions of trust (14). Trust in the pharmaceutical industry is therefore inherently linked to concerns over the development process, and hence effectiveness, safety and side-effects.
Health care providers have a responsibility to engage with patients and relay clear, concise and transparent information regarding the vaccines, so that individuals can make informed health decisions. In addition, healthcare providers need to spend sufficient time discussing vaccines with patients, should not deride their concerns, and need to provide satisfactory responses to questions. Mistrust in the information from health providers was associated with vaccine hesitancy in this study. Lower levels of trust in the healthcare system allow individuals to become more sensitive to misinformation about the COVID-19 vaccine (39). In this study, almost half of participants reported being exposed to conflicting information about the COVID-19 vaccines. The finding of lower unwillingness to take a COVID-19 vaccine among those whose main source of vaccine-related information was social media requires further investigation as it is contradictory to previous work (13), where higher vaccine hesitancy was observed among South Africans who had high trust in social media sources. Furthermore there is need to be cognizant of the reality that behavior change cannot be changed by a single intervention such as correct messaging. Therefore, long term multi-level and contextually relevant interventions needs to be designed to address vaccine hesitancy not only for COVID-19, but that straddle across many diseases that requires routine vaccination.
A limitation of this study is that the variables are subject to self-report bias. Furthermore, online surveys are subject to selection bias because individuals who interact more frequently with the internet and smart phones are more likely to participate in an online survey. However, the online surveys were supplemented with telephonic interviews that targeted South Africans in lower-income, high-density areas who have lower internet access, and the data was benchmarked to the general population to increase generalizability of the findings.
Conclusion
Public health officials and vaccination campaigns need to involve health providers and community and religious leaders in developing and implementing contextually relevant interventions for vaccine hesitancy. Communication campaigns and community engagement strategies need to relaying transparent and concise information about the COVID-19 vaccines, and discuss beliefs, attitudes and barriers and facilitators for vaccine acceptance. It is also critical for health interventions to be designed in such a way that they are culturally relevant and take into consideration the social context of the setting. The health system and public and medical institutions need to demonstrate their trustworthiness to citizens. Ultimately, individuals need to make health care decisions that are aligned with their values (2). In this regard, interventions such as motivational interviewing have been successful in changing vaccination intentions. Comprehensive communication strategies should include issues about side-effects, safety risks, and effectiveness of the vaccines so as to address public concerns about risks of taking a COVID-19 vaccine. This is particularly important for individuals who are uncertain about their vaccine intentions, as it will aid them in making an informed vaccination decision.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
Ethical approval to conduct the study was received from the Human Sciences Research Council Research Ethics Committee (HSRC REC) (Protocol number: REC 5/03/20), which is aligned with the principles of the Declaration of Helsinki. Consent for participation was obtained from all participants before they proceeded to the survey questions. Participants were informed of voluntary participation, the anonymity of their responses, and the right to withdraw from the survey at any time.
Author contributions
RS, SR, SS, and RG: conceptualization and methodology. RS: formal analysis. SR and SS: supervision. TM and IN: validation. RS, RG, IN, and TM: writing original draft. RS, RG, TM, IN, SR, and SS: review and editing of draft manuscript. All authors have read the manuscript and agreed to its submission.
Funding
This study was supported by the South African Department of Science and Technology.
Acknowledgments
We thank the participants for taking their time to complete the survey. We acknowledge the research team from the Human Sciences Research Council (HSRC) who coordinated the COVID-19 socio-behavioral research surveys; including Yolande Shean, Saahier Parker, Adlai Davids, Shandir Ramlagan, and Thabang Manyaapelo.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2023.1233031/full#supplementary-material
References
1. World Health Organization . Ten threats to global health in 2019. (2019). Available at: https://www.who.int/news-room/spotlight/ten-threats-to-global-health-in-2019 (Accessed March 15, 2023).
2. MacDonald, NE . Vaccine hesitancy: definition, scope and determinants. Vaccine. (2015) 33:4161–4. doi: 10.1016/j.vaccine.2015.04.036
3. Lazarus, JV , Wyka, K , White, TM , Picchio, CA , Rabin, K , Ratzan, SC, et al. Revisiting COVID-19 vaccine hesitancy around the world using data from 23 countries in 2021. Nat Commun. (2022) 13:3801. doi: 10.1038/s41467-022-31441-x
4. Our World in Data . Coronavirus (COVID-19) vaccinations 2023. Available at: https://ourworldindata.org/covid-vaccinations?country=~OWID_WRL.
5. Coronavirus pandemic (COVID-19). (2020). Available at: https://ourworldindata.org/coronavirus.
6. South African Department of Health . COVID-19 online resource and news portal (2023). Available at: https://sacoronavirus.co.za/latest-vaccine-statistics/.
7. Cascini, F , Pantovic, A , Al-Ajlouni, Y , Failla, G , and Ricciardi, W . Attitudes, acceptance and hesitancy among the general population worldwide to receive the COVID-19 vaccines and their contributing factors: a systematic review. EClinicalMedicine. (2021) 40:101113. doi: 10.1016/j.eclinm.2021.101113
8. Bono, SA , de Moura, F , Villela, E , Siau, CS , Chen, WS , Pengpid, S, et al. Factors affecting COVID-19 vaccine acceptance: an international survey among low- and middle-income countries. Vaccines. (2021) 9:515. doi: 10.3390/vaccines9050515
9. Grossman, VA . The COVID-19 vaccine: why the hesitancy? J Radiol Nurs. (2021) 40:116–9. doi: 10.1016/j.jradnu.2021.02.011
10. Caserotti, M , Girardi, P , Rubaltelli, E , Tasso, A , Lotto, L , and Gavaruzzi, T . Associations of COVID-19 risk perception with vaccine hesitancy over time for Italian residents. Soc Sci Med. (2021) 272:113688. doi: 10.1016/j.socscimed.2021.113688
11. Roy, DN , Biswas, M , Islam, E , and Azam, MS . Potential factors influencing COVID-19 vaccine acceptance and hesitancy: a systematic review. PLoS One. (2022) 17:e0265496. doi: 10.1371/journal.pone.0265496
12. Runciman, C , Roberts, B , Alexander, K , Bohler-Muller, N , and Bekker, M . Willingness to take a COVID-19 vaccine: a research briefing. UJ-HSRC COVID-19 democracy Survey2021. Available at: https://www.uj.ac.za/wp-content/uploads/2022/02/2022-02-02-r5-vaccine-acceptance-and-hesitancy.pdf.
13. Burger, R , Köhler, T , Golos, A , Buttenheim, A , English, R , Tameris, M, et al. COVID-19 vaccine hesitancy in South Africa: results from NIDS-CRAMWave 4. (2021). Available at: https://cramsurvey.org/wp-content/uploads/2021/05/3.-Burger-R.-Buttenheim-A.-English-R.-Maughan-Brown-B.-Kohler-T.-_-Tameris-M.-2021.-COVID-19-vaccine-hesitancyin-South-Africa-Results-from-NIDS-CRAM-Wave-4.pdf.
14. Sapienza, A , and Falcone, R . The role of trust in COVID-19 vaccine acceptance: considerations from a systematic review. Int J Environ Res Public Health. (2022) 20:665. doi: 10.3390/ijerph20010665
15. Pires, C . Global predictors of COVID-19 vaccine hesitancy: a systematic review. Vaccines. (2022) 10:1349. doi: 10.3390/vaccines10081349
16. Viswanath, K , Bekalu, M , Dhawan, D , Pinnamaneni, R , Lang, J , and McLoud, R . Individual and social determinants of COVID-19 vaccine uptake. BMC Public Health. (2021) 21:818. doi: 10.1186/s12889-021-10862-1
17. Loomba, S , de Figueiredo, A , Piatek, SJ , de Graff, K , and Larson, HJ . Measuring the impact of COVID-19 vaccine misinformation on vaccination intent in the UK and USA. Nat Hum Behav. (2021) 5:337–48. doi: 10.1038/s41562-021-01056-1
18. Shakeel, CS , Mujeeb, AA , Mirza, MS , Chaudhry, B , and Khan, SJ . Global COVID-19 vaccine acceptance: a systematic review of associated social and behavioral factors. Vaccines. (2022) 10:110. doi: 10.3390/vaccines10010110
19. Dubé, E , and MacDonald, NE . COVID-19 vaccine hesitancy. Nat Rev Nephrol. (2022) 18:409–10. doi: 10.1038/s41581-022-00571-2
20. Wadvalla, B-A . How South Africa is dragging its vaccine rollout back from the brink. BMJ. (2021) 374:n1949. doi: 10.1136/bmj.n1949
21. Health Justic Initiative . Timeline of key South Africa COVID-19 related developments and health justice Initiative’s engagement with government on vaccine access for south Africa. (2023). Available at: https://healthjusticeinitiative.org.za/vaccine-equity/vaccine-timeline/#:~:text=Phase%201%3A%20February%20%E2%80%93%20April%202021.in%20Phases%201%20and202.
22. Ramlagan, S , Shean, YL , Parker, S , Trollip, K , Davids, A , and Reddy, SP . Pushing the boundaries: adapting research methodology to document the COVID-19 pandemic from a socio-behavioural perspective in a low/middle level income country: the case of South Africa. Int J Soc Res Methodol. (2022) 25:323–9. doi: 10.1080/13645579.2021.1883538
23. Reddy, SP , Sewpaul, R , Mabaso, M , Parker, S , Naidoo, I , Jooste, S, et al. South Africans' understanding of and response to the COVID-19 outbreak: an online survey. S Afr Med J. (2020) 110:894–902. doi: 10.7196/SAMJ.2020.v110i9.14838
24. Naidoo, I , Mabaso, M , Moshabela, M , Sewpaul, R , and Reddy, SP . South African health professionals' state of well-being during the emergence of COVID-19. S Afr Med J. (2020) 110:13104. doi: 10.7196/SAMJ.2020.v110i10.15250
25. Sewpaul, R , Mabaso, M , Dukhi, N , Naidoo, I , Vondo, N , Davids, AS, et al. Determinants of social distancing among south Africans from 12 days into the COVID-19 lockdown: a cross sectional study. Front Public Health. (2021) 9:632619. doi: 10.3389/fpubh.2021.632619
26. Ipsos . Coronavirus: opinion and reaction results from a multi-country poll. Paris, France: Ipsos (2020).
27. Statistics South Africa . Mid-year population estimates. Pretoria: Statistics South Africa (2021).
28. Katoto, P , Parker, S , Coulson, N , Pillay, N , Cooper, S , Jaca, A, et al. Predictors of COVID-19 vaccine hesitancy in south African local communities: the VaxScenes study. Vaccines. (2022) 10:353. doi: 10.3390/vaccines10030353
29. Kollamparambil, U , Oyenubi, A , and Nwosu, C . COVID19 vaccine intentions in South Africa: health communication strategy to address vaccine hesitancy. BMC Public Health. (2021) 21:2113. doi: 10.1186/s12889-021-12196-4
30. Hao, F , and Shao, W . Understanding the influence of political orientation, social network, and economic recovery on COVID-19 vaccine uptake among Americans. Vaccine. (2022) 40:2191–201. doi: 10.1016/j.vaccine.2022.02.066
31. Moore, DCBC , Nehab, MF , Camacho, KG , Reis, AT , Junqueira-Marinho, MF , Abramov, DM, et al. Low COVID-19 vaccine hesitancy in Brazil. Vaccine. (2021) 39:6262–8. doi: 10.1016/j.vaccine.2021.09.013
32. Solanki, G , Cornell, M , and Lalloo, R . Uptake and cost of influenza vaccines in a private health insured south African population. S Afr J Infect Dis. (2018) 33:a138. doi: 10.4102/sajid.v33i5.138
33. Makoae, M , Mokhele, T , Naidoo, I , Sifunda, S , and Sewpaul, R . Determinants of parents taking their children for scheduled vaccinations during COVID-19 pandemic in South Africa. Vaccine. (2023) 11:389. doi: 10.3390/vaccines11020389
34. Lee, RLT , Chien, WT , Stubbs, M , Cheng, WLS , Chiu, DCS , Fung, KHK, et al. Factors associated with COVID-19 vaccine acceptance among healthcare professionals and community stakeholders in Hong Kong: a cross-sectional study. Int J Environ Res Public Health. (2022) 19:14499. doi: 10.3390/ijerph192114499
35. Volpp, KG , Loewenstein, G , and Buttenheim, AM . Behaviorally informed strategies for a national COVID-19 vaccine promotion program. JAMA. (2021) 325:125–6. doi: 10.1001/jama.2020.24036
36. Engelbrecht, M , Heunis, C , and Kigozi, G . COVID-19 vaccine hesitancy in South Africa: lessons for future pandemics. Int J Environ Res Public Health. (2022) 19:6694. doi: 10.3390/ijerph19116694
37. Reuters . South African corruption probe flags COVID contracts worth $137 million. (2022). Available at: https://www.reuters.com/world/africa/safrican-corruption-probe-flags-covid-contracts-worth-137-million-2022-01-25/
38. McCarthy, J . Big pharma sinks to the bottom of US industry rankings. Washington, DC: Gallup Inc (2019).
Keywords: COVID-19 vaccinations, vaccine hesitancy, trust, side-effects, influenza vaccination, South Africa
Citation: Sewpaul R, Sifunda S, Gaida R, Mokhele T, Naidoo I and Reddy SP (2023) Vaccine hesitancy and related factors among South African adults in 2021: unpacking uncertainty versus unwillingness. Front. Public Health. 11:1233031. doi: 10.3389/fpubh.2023.1233031
Edited by:
Joao Sollari Lopes, National Statistical Institute of Portugal, PortugalReviewed by:
Ana Afonso, NOVA University of Lisbon, PortugalRafael Obregon, UNICEF United Nations International Children's Emergency Fund, United States
Copyright © 2023 Sewpaul, Sifunda, Gaida, Mokhele, Naidoo and Reddy. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ronel Sewpaul, cnNld3BhdWxAaHNyYy5hYy56YQ==
 Ronel Sewpaul
Ronel Sewpaul Sibusiso Sifunda1
Sibusiso Sifunda1 Tholang Mokhele
Tholang Mokhele Inbarani Naidoo
Inbarani Naidoo Sasiragha Priscilla Reddy
Sasiragha Priscilla Reddy