
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health, 19 September 2023
Sec. Public Mental Health
Volume 11 - 2023 | https://doi.org/10.3389/fpubh.2023.1231326
This article is part of the Research TopicMental Health in Healthcare Workers and its Associations with Psychosocial Work ConditionsView all 32 articles
 Hien Thu Pham1
Hien Thu Pham1 Tung Viet Cao2
Tung Viet Cao2 Ngoc Bich Le3*
Ngoc Bich Le3* Nhung T-T Nguyen3
Nhung T-T Nguyen3 Bich Thi Ngoc Vuong1
Bich Thi Ngoc Vuong1 Linh Vu Dieu Pham1
Linh Vu Dieu Pham1 Trang Thu Hoang1
Trang Thu Hoang1 Trang Thi Hanh Pham1
Trang Thi Hanh Pham1 Thuy Ngoc Nguyen1
Thuy Ngoc Nguyen1 Huong Thi Thu Bui1
Huong Thi Thu Bui1 Tho Van Tran4
Tho Van Tran4 Linh Thuy Vu5
Linh Thuy Vu5 Phuong Thi Le1
Phuong Thi Le1Introduction: The outbreak of coronavirus severe acute respiratory syndrome coronavirus 2 (SARS-CoV2) had significant effects on the mental well-being in general, particularly for healthcare professionals. This study examined the prevalence of depression, anxiety, and stress, and identified the associated risk factors amongst healthcare workers during the COVID-19 outbreak in a tertiary hospital located in Vietnam.
Methods: We conducted a cross-sectional study at a tertiary-level hospital, where the Depression Anxiety and Stress Scale 21 (DASS-21) web-based questionnaire was employed. We analyzed the determinant factors by employing multivariate logistic models.
Results: The prevalence of depression, anxiety, and stress symptoms were 19.2%, 24.7%, and 13.9%, respectively. Factors such as engaging in shift work during the pandemic, taking care of patients with COVID-19, and staff’s health status were associated with mental health issues among health professionals. In addition, having alternate rest periods was likely to reduce the risk of stress.
Conclusion: The prevalence of mental health problems in healthcare workers during the COVID-19 pandemic was relatively high. Having resting periods could potentially mitigate the development of stress among health professionals. Our findings could be taken into account for improving mental health of the health professional population.
The surge in the number of Coronavirus (COVID 19) cases strongly impacted public health around the world. Since the initial case in Wuhan, China, in December 2019, COVID-19 spread rapidly worldwide, quickly becoming a global health threat. As of 30 July 2023, there were over 768 million confirmed cases and over 6.9 million deaths reported globally (1). Over the same period of time, the total number of COVID-19 cases in Vietnam reached over 11.6 million confirmed cases and over 43,000 deaths (2). As a result, governments adopted a variety of measures to mitigate the spread of the virus. In Vietnam, the government enforced compulsory quarantine for people returning from abroad and patients with COVID-19; people worked from home, non-essential services were shut down, schools were suspended, there were travel restrictions, and lockdown in some locations. Such measures changed daily life and impacted incomes. Consequently, these factors affected the mental health of the population.
It is reasonable to assume that the COVID-19 pandemic was and is stressful for health workers. They had a higher risk of being infected with COVID-19 or were always fearful of being infected (3, 4). They also worked long hours, increased workloads, a shortage of personal protective equipment, faced social stigma, and lacked incentives to continue working (5–7). As a result, studies showed that this led to a significantly higher incidence of insomnia among healthcare workers as compared to non-healthcare workers during the pandemic (8, 9). However, unlike other professional groups, healthcare workers were not diagnosed and their health issues were not cared for during the pandemic. Indeed, they may not have realized that they had health problems, especially those related to mental health. This influenced the health of health care professionals and their levels of motivation. Subsequently, patient care was negatively affected.
Studies from many countries reported a prevalence of depression and anxiety in healthcare workers during the pandemic. For instance, Chen et al. (10) reported that the overall prevalence of anxiety and depression among frontline healthcare workers was 43% and 45%, respectively. Pappa et al. (11) reported that the prevalence of insomnia was 34.32% in 2020. A study in five major hospitals in Singapore and India reported that the prevalence of depression, anxiety, and stress symptoms was 10.6%, 15.7%, and 5.2%, respectively (12). A study among 1,090 medical staff in China revealed that the self-reported prevalence of anxiety symptoms, depression symptoms were 13.3%, 18.4%, and 23.9%, respectively (13). However, the percentages vary depending on the country and culture. In Vietnam, some previous studies reported the prevalence rates (14–17). For instance, Nguyen et al. reported 22.6% of participants had psychosocial problems (14). Nguyen et al. observed that 90.3% of participants felt that their job put them at risk of COVID-19 infection and 85.7% of participants expressed fear of potential infections (14). However, no study examined the associated risk factors carefully.
Vietnam experienced a challenging period of epidemic outbreaks and deployed several special strategies. For instance, mobilizing doctors from low risk countries to support high risk countries. Moreover, the healthcare staff from the studied hospital, a pediatric hospital, have worked and supported treatment on adults’ patients. These factors can contribute to an increase in the workload as well as the anxiety of healthcare workers.
The objectives of this study were to investigate the prevalence of depression, anxiety, and stress, as well as the associated risk factors, among healthcare workers at a tertiary hospital for children in Northern Vietnam during the COVID-19 outbreak. These findings will help identify strategies to support counseling services, implement stress management programs, and promote work-life balance for a particular population.
We conducted this cross-sectional study at a tertiary-level children’s hospital in Hanoi. This is a multi-disciplinary hospital and the largest pediatric hospital in Northern Vietnam.
We recruited all permanent hospital staff in July 2022, just after the COVID-19 pandemic’s peak, to participate in the investigation. There were 1,001 staff who responded to the questionnaire (about 65% of the total hospital staff). We collected data through an online self-administered survey using an anonymous questionnaire distributed to all healthcare workers via email address. Only one response per person was permitted. The study was approved by the institutional ethics board of the Vietnam National Children’s Hospital (Number 1925/BVNTW_HĐĐĐ).
Depression, anxiety, and stress were assessed by the Depression Anxiety and Stress Scale 21 (DASS-21). The scale consists of three subscales that are depression, anxiety, and stress. Each subscale includes seven questions which are graded on a 4-point Likert scale from 0 to 3 (0 “Did not apply to me at all,” 1 “Applied to me to some degree, or some of the time,” 2 “Applied to me to a considerable degree, or a good part of time,” 3 “Applied to me very much, or most of the time”). The Vietnamese version of the DASS-21 scale has been translated and validated by the National Institute of Mental Health (18) with a reported Cronbach Alpha of 0.88, sufficiently reliable for the Vietnam population.
The questions also included demographic characteristics (age, gender, education, marital status, years of working, health status before COVID-19 pandemic); and working conditions during COVID-19, shift work during the pandemic, including number of working hours, having alternate rest periods, having direct contact with COVID-19 patients, incomes, number of days away from home per month, and number of sick days.
We extracted data and performed quality control by checking the missing values and cross-checked the information. Fortunately, we did not find duplicated records and missing records. Levels of depression, anxiety and stress were coded based on the total score as the guideline (19). For depression, total score from 0 to 9 was considered as normal, from 10 to 13 was mild, from 14 to 20 was moderate, from 21 to 27 were considered as severe, above 28 was considered extremely severe. The anxiety subscales were considered as normal (0–7), mild (8, 9), moderate (10–14), severe (15–19), and extremely severe (20–42). The total stress subscale was considered as normal (0–14), mild (15–18), moderate (19–25), severe (26–33), and extremely severe (34–42).
We employed the logistic model to investigate the associated risk factors of total depression scores equal and higher than 10, total anxiety scores equal and higher than 8, and total stress scores equal and higher than 15. Variables with p value above 0.2 would be included for final logistic regression models. We also conducted t-test and ANOVA to compare scores by participants’ characteristics, which is in the appendix. The significant level was set at 0.05.
The mean age (standard deviation—SD) was 35.7 (± 13.5) years. More than 75% of participants were female and most participants were married (84%). Approximately 23.9% were doctors and 56.2% were nurses or medical technologists. More than half of the study participants had more than 10 years of experience in their respective fields (Table 1).
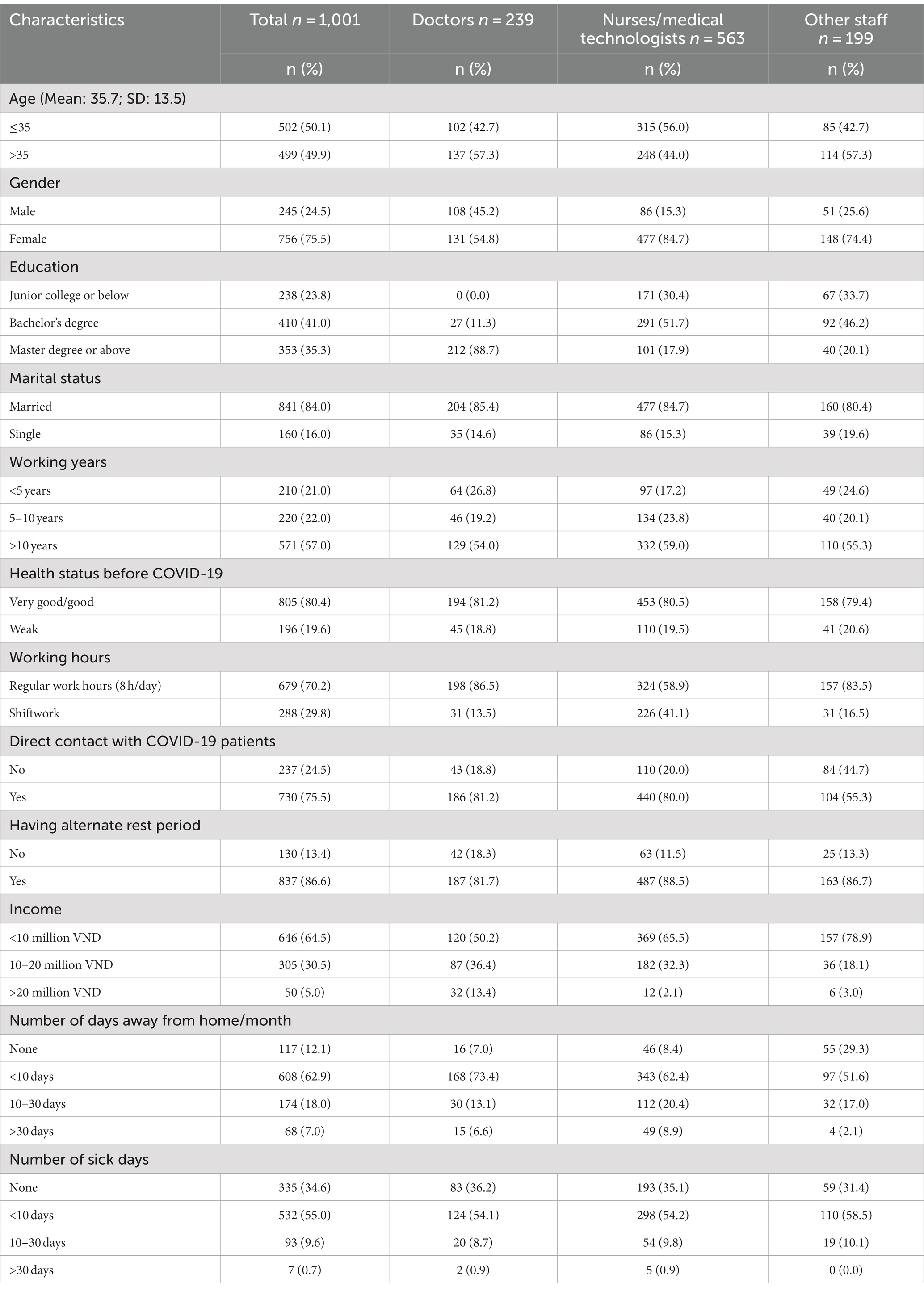
Table 1. Participants’ characteristics of an children’s hospital, location in Northern Vietnam all and by type of professional, 2022.
In relation to working conditions of healthcare workers during the COVID-19 pandemic, about 70.2% of respondents had normal work hours (8 h per day) and 29.8% were shift workers. Most participants (86.6%) had alternate rests. About 75.5% of the staff had direct contact with COVID-19 patients. On average, 64.5% had income less than 10 million VND, and 30.5% had income from 10 to 20 million VND.
Table 2 shows the percentage of depression, anxiety, and stress among healthcare workers. 24.7% of respondents reported having symptoms of anxiety, of which 11.7% had moderate symptoms and 5.4% had extremely severe symptoms. 19.2% of respondents reported having symptoms of depression, of which 8.3% had mild symptoms and 6.5% had mild symptoms. 13.9% of respondents reported having symptoms of stress, of which 5.4% had mild symptoms and 3.8% had moderate symptoms.
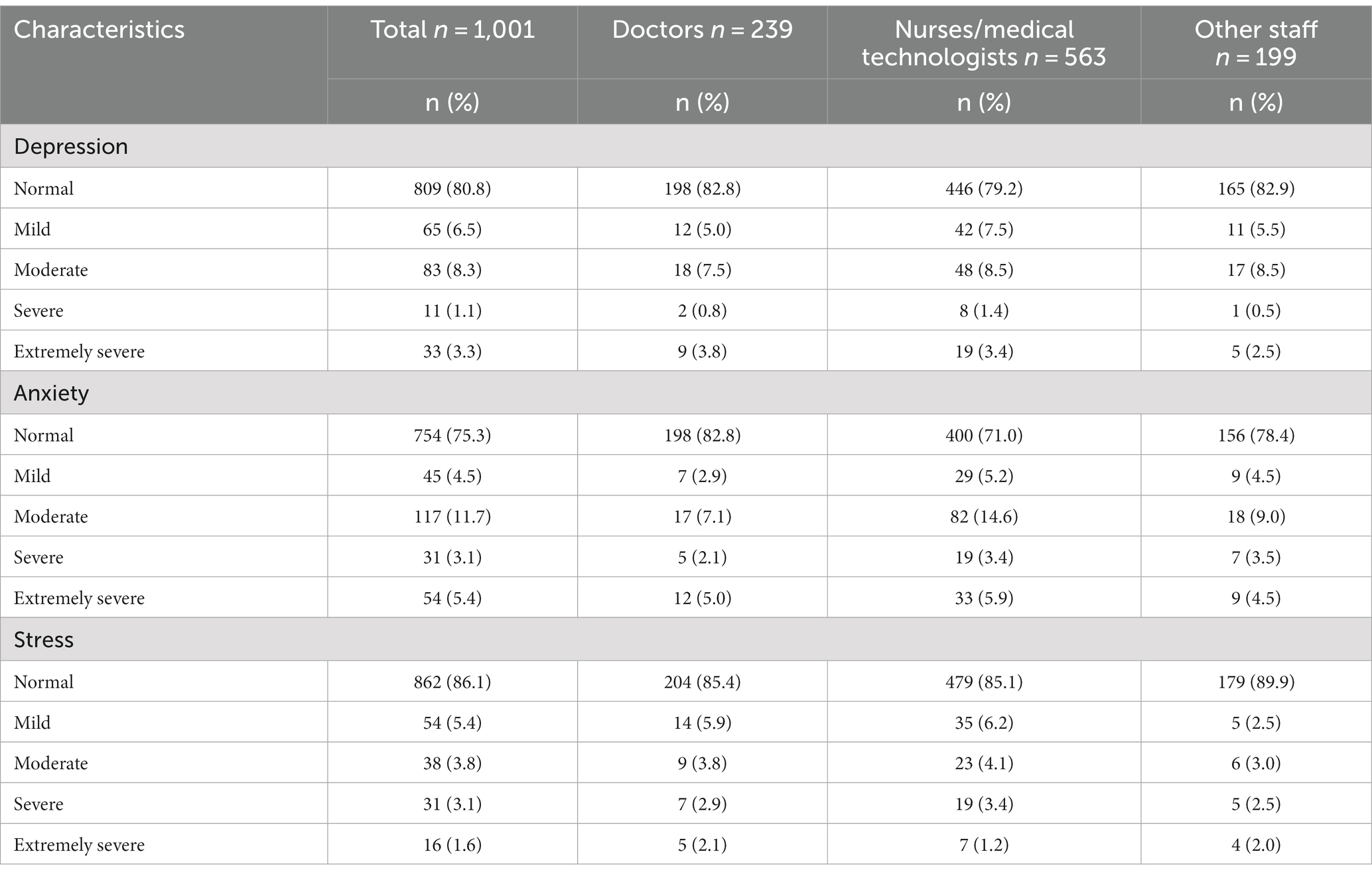
Table 2. Levels of depression, anxiety and stress symptoms among the staff in a children hospital located in the Northen Vietnam, in total and by professionals.
The associated factors of depression, anxiety, and stress are presented in Tables 3–5, respectively. Sociodemographic characteristics (i.e., age, gender, education, marital status, year of experience) were not associated with symptoms of depression, anxiety, and stress. The odds of having depression were significantly higher among those having weak health status before the outbreak of COVID-19 (OR = 1.87, 95% CI 1.28–2.73). Similarly, high proportions of those suffering from anxiety among health professionals were those with shift work during the pandemic (OR = 1.48, 95% CI 1.06–2.07) and having weak health status before the outbreak of COVID-19 (OR = 1.67, 95% CI 1.16–2.40). High risk stress was observed in those in direct contact with COVID-19 patients (OR = 1.94, 95%CI 1.13–3.32) and shift work during the pandemic (OR = 2.22, 95%CI 1.47–3.37). Healthcare workers having alternate rest periods significantly decreased the odds of having stress (OR = 0.42, 95%CI 0.26–0.67).
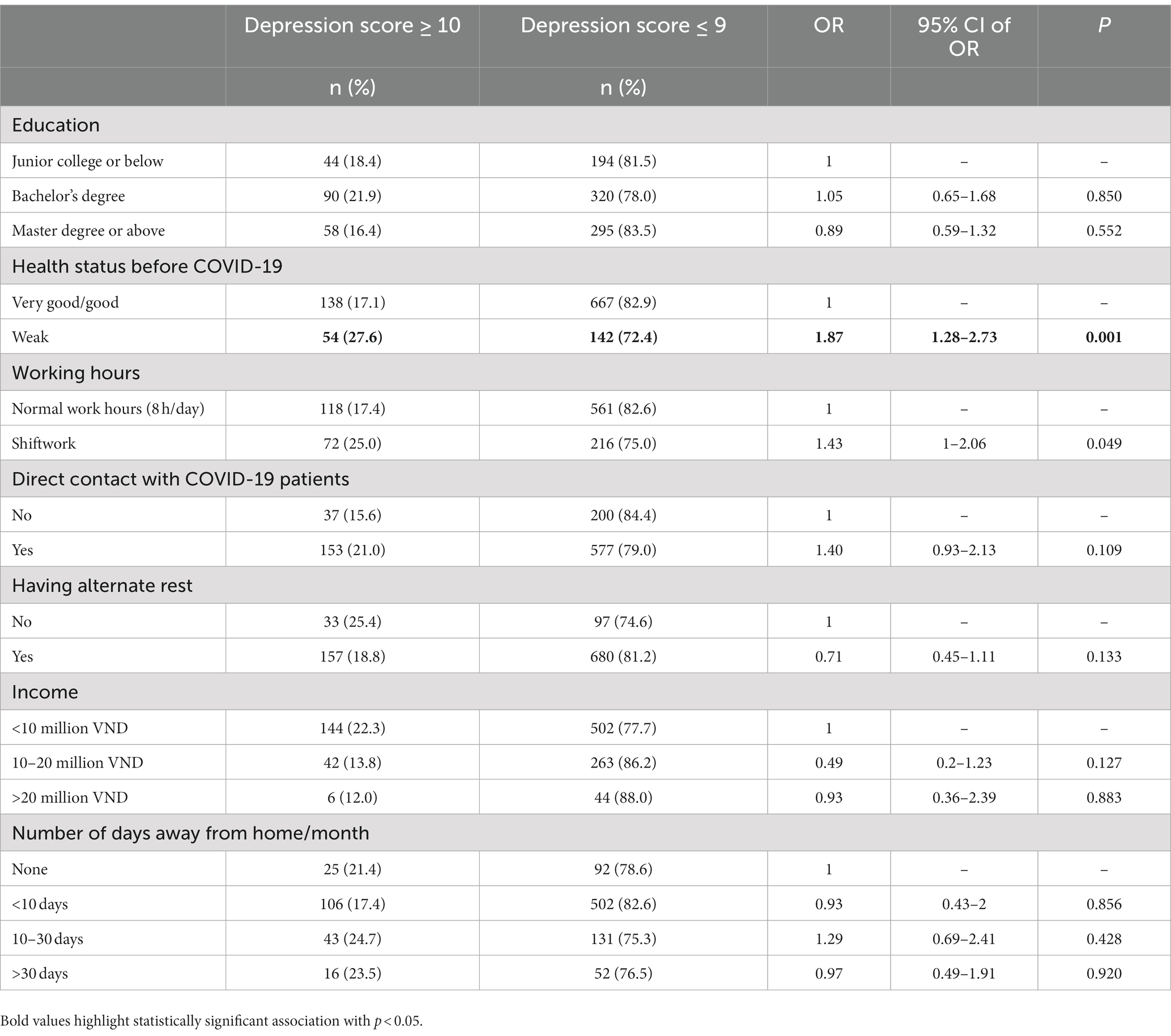
Table 3. Associations between participants’ characteristics and depression’s prevalence in a children hospital located in Northern Vietnam, 2022.
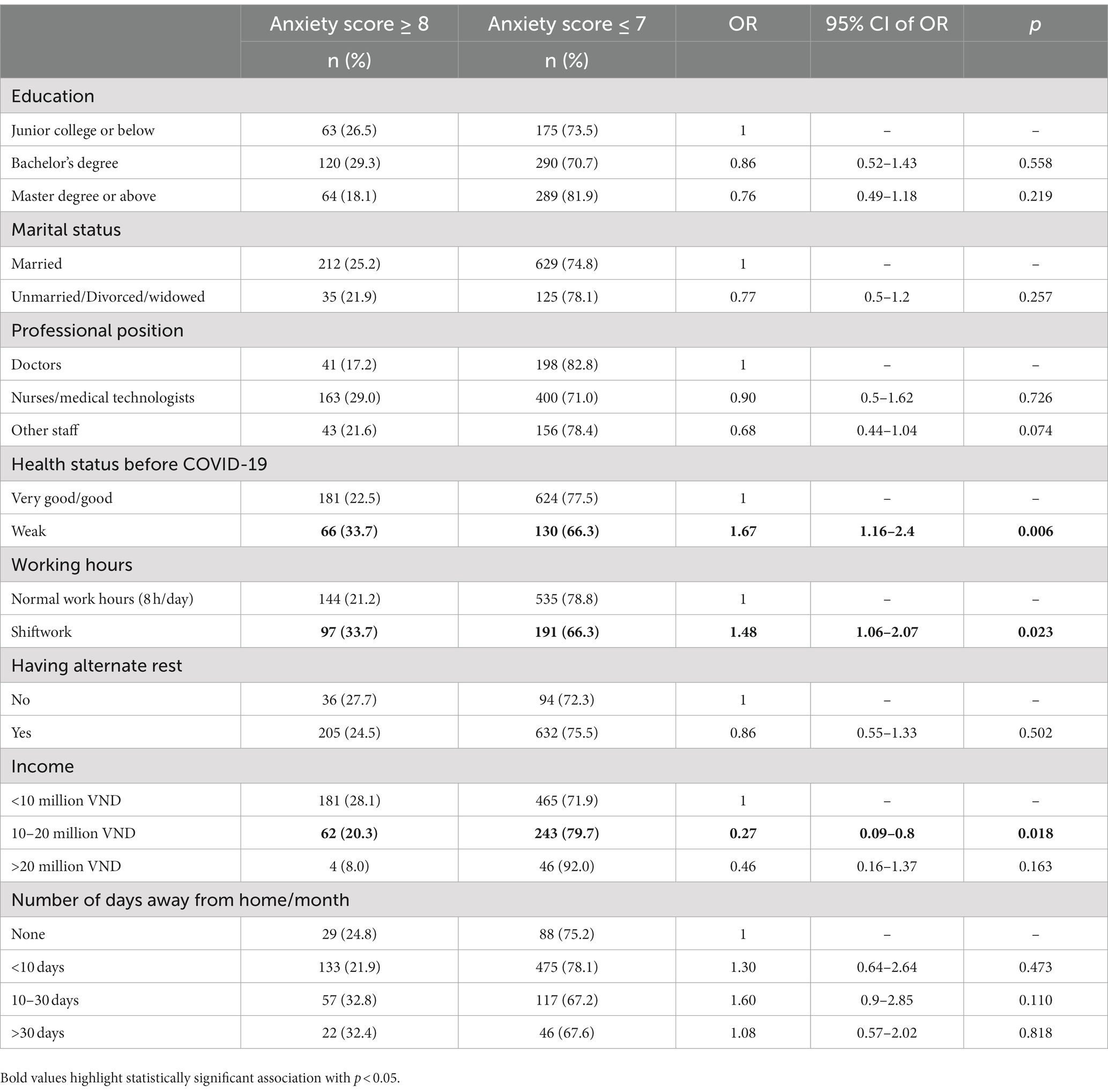
Table 4. Associations between participants’ characteristics and anxiety’s prevalence in a children hospital located in Northern Vietnam, 2022.
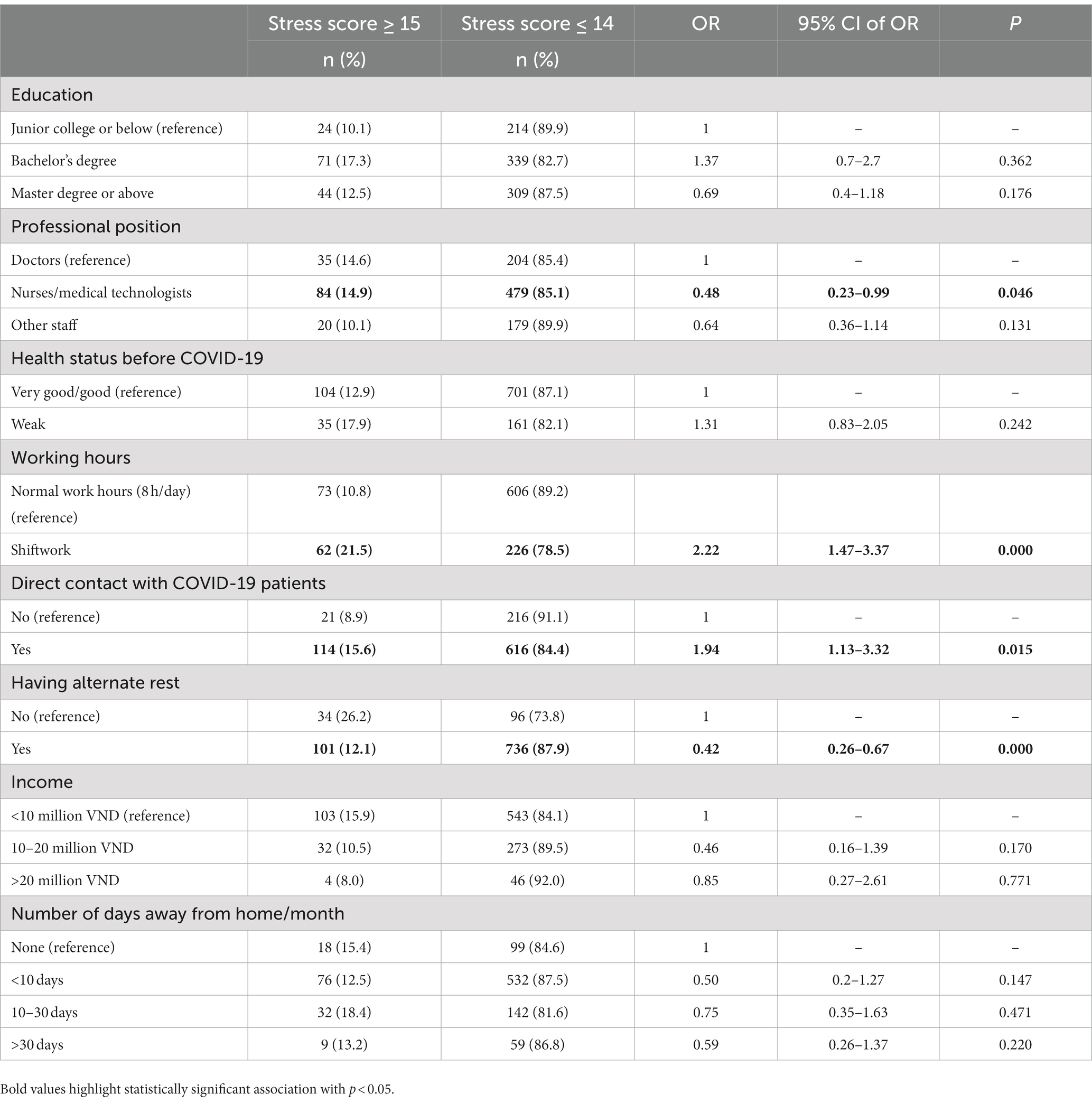
Table 5. Associations between participants’ characteristics and Stress’s prevalence in a children hospital located in Northern Vietnam, 2022.
Mental health problems among healthcare worker can lead to high levels of job dissatisfaction and increased turnover (20). So, the evidence of the mental health problems concern can help address the issue by creating a supportive work environment and promoting staff retention. Consequently this contributes to better continuity of care for patients and hospital performance (21). In this study, the prevalence of depression, anxiety and stress among healthcare workers were 19.2%, 24.7%, and 13.9%, respectively. Those were slightly higher than figures reported by some other studies in Vietnam (16, 17). However, figures in our study were lower than those in a study conducted during the fourth wave of COVID-19 (22). The prevalence of depression, anxiety, and stress among healthcare workers in this study was lower than figures in many countries, including China (23.6%, 27.4%, and 16.3% respectively) (23), South Korea (30.6%, 41%, and 19.4% respectively) (24), Italy (35.9%, 25.5%, 33.3%, respectively) (25), Brazil (38.4%, 53.8%, and 40.3%, respectively) (26), and Northwest Ethiopia (55.3%, 69.6%, and 20.5%, respectively) (27). The prevalence of depression, anxiety, and stress among healthcare workers in this study was higher than figures in Singapore and India (12). Nonetheless, in line with the other countries, these prevalence rates in health providers in Vietnam during COVID-19 were higher than in the larger community.
During the pandemic, health professionals experienced many psychosocial stressors such as the disruption of routine life, travel restrictions, shortage of necessities, separation from family members and friends, and salary reduction. Indeed, during the COVID-19 pandemic, several frontline healthcare workers such as doctors working with COVID-19 patients or laboratories, were isolated with other staff in the hospital and isolated with families and communities due to incomplete information and fear associated with COVID-19 (16). In the beginning of pandemic, Holmes et al. (28) had called for actions to address the mental health in vulnerable groups including healthcare providers and emphasized the long term psychological impact. In this study, even at the end of the peak wave of pandemic when life was gradually returning to normal, the prevalence remained high. Therefore, further studies on mental health issues in health workers need to be conducted in order to promote the healthcare sector.
The lower prevalence of depression, anxiety, and stress observed among healthcare workers in our study may be attributed to several factors. Firstly, our study was conducted once the pandemic had ended and life had returned to a more normal state. During this time, there was a clearer understanding of virus transmission and spread, which likely reduced the fear and uncertainty experienced by healthcare workers. As mentioned by Singh and Subedi (29) health workers initially faced fear, threats, and eviction from their homes due to concerns about bringing the virus home in the beginning stage of pandemic. Such experiences often led to stigma, discrimination, and social isolation. Secondly, Vietnam adopted several effective strategies to control COVID-19 in the last stage (30). These strategies likely contributed to a lower number of cases and reduced the burden on healthcare workers, resulting in less psychological distress. Thirdly, the staff studied were in a children’s hospital where the number of COVID-19 hospitalized cases was small. Some staff had to mobilize to support other hospitals, but this was a small number. During the outbreak in Ho Chi Minh City and the southern provinces, 195 healthcare workers of a studied hospital traveled south to help deal with the pandemic. Healthcare workers at the hospital took alternate breaks from 7 to 14 days per month. Incomes were cut based on the number of actual working days. Healthcare workers with COVID-19 infections are entitled to 7–10 days of paid quarantine leave according to the social insurance regime.
In conclusion, our study supported the fact that mental health depends on the healthcare workers’ emotional response under pressurized situations (31) or adaptation to contextual demands (32). We suggest using the context sensitivity index (CSI) to measuring the ability to identify the presence and absence of stressor context cues in Vietnam.
Our study revealed that those with shiftwork were more likely to suffer from anxiety and stress than those with regular work hours (8 h/day). A study from Korea showed that female nurses or nursing assistants who did shift work had a higher risk of anxiety (33). Another study revealed that nurses working night shifts were at twice the risk of developing stress than those working the day shifts (27). In hospitals, clinical staff members often do shiftwork, whereas the administrative staff work regular hours. Hence we observed a higher prevalence of stress amongst the healthcare workers working directly with patients.
Healthcare workers in direct contact with patients with COVID-19 were more likely to have stress. Previous findings from other countries also showed that healthcare workers in direct exposure to patients with COVID-19 were at a higher risk of mental health problems (34–37). A study conducted in the fourth wave of COVID-19 in Vietnam reported that healthcare workers treating moderate and severe COVID-19 patients were at increased risk for anxiety (22).
Our study also found that those having alternate rest periods significantly decreased the risk of having stress. A study conducted by Robles et al. with 5,938 healthcare workers found that over 30% of frontline healthcare workers reported a lack of rest time, and those with a lack of rest time were at a 3.1 times higher risk of having insomnia (38). Several qualitative studies revealed that healthcare workers desired adequate rest during COVID-19. They would like more support and attention toward their psychological well-being from leaders (39, 40). We also suggest special implement intervention for clinical staff in Vietnam.
Some intervention programs to cope with new psychosocial issues resulting from COVID-19 for healthcare workers have been introduced. For example, the Institute of Mental Health and the Medical Psychology Research Center of the Second Xiangya Hospital provided psychological support by examining of immediate needs from the staff and adjusting the measures afterward (20). In this study, the hospital provided a place for rest, protective supplies, and training on psychological skills to deal with patients’ emotional problems such as anxiety or depression during the pandemic. The trial entitled “RECHARGE” mainly focuses on psychoeducation by teaching people techniques on problem-solving skills and managing worries in Australia, Switzerland (41). A program in Canada had been using a Virtual Peer Support Platform to guide healthcare workers to build resilience against burnout by group therapy (42). Regardless of the methodology, all studies emphasized the significance of multidisciplinary collaboration. However, most past programs were implemented in university associated hospitals, which prevents us from applying the findings to other types of hospital or “lack a rigorous protocol” impedes finding out the best way to go (21). Therefore, the World Health Organization is still calling to develop a tailored psychological intervention for healthcare workers worldwide (43).
Though DASS-21 has been widely used to assess levels of depression, anxiety, and stress in various research, it has certain limitations that can lead to subscale overlap and interaction. In the current study, we found strong positive correlations between depression and anxiety (r = 0.85, p < 0.05), depression and stress (r = 0.88, p < 0.05), and anxiety and stress (r = 0.84, p < 0.05). Indeed, we observed the consistent determinant factors for each subscale (Tables 3–5). The reasons might be attributed to the scale reliance on self-reporting, in other words, it is influenced by individual socially desirable response. Furthermore, there is the potential of bias due to cultural factors in the questionnaire (44, 45). Therefore, findings from this study could be considered as preliminary results. Future comprehensive studies should combine its findings with other assessment methods, taking account of the cultural context. This can help mitigate some limitations of the scale.
This study is subject to several limitations. Firstly, the research design was a cross-sectional study, so causal relationships are inconclusive. Secondly, given that the study took place after the pandemic, there could have been recall bias involved when obtaining information.
Finally, it is important to note that the study was conducted at a single center, which may limit the scope of the findings. Nonetheless, our sample size is high (above 1,000), hence, the interpreting findings are reliable.
The prevalence of depression, anxiety, and stress among healthcare workers were notably high. Additionally, staff with adverse working conditions, such as shift work, direct contact with COVID-19 patients, and income level, and psychological status before the pandemic, were more likely to have a high risk of mental health problems. Having alternate rest periods and limiting time away from home to no more than 10 days per month during COVID-19 pandemic might reduce risk of stress development. The findings of the study can help promote adequate measures to protect the mental health of pediatric health staff during pandemics.
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
The studies involving humans were approved by the Institutional Review Board at the Vietnam National Children’s Hospital (IRB number:1925/BVNTW-HDDD dated August 22, 2022). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
HTP: conceptualization, methodology, and writing—review and editing. TV: conceptualization, methodology, and review and editing. NT-T and NB: writing—original draft and writing—review and editing. LV, BT, LT, TV, TT, PT, TTH, HTTB, and TN: data curation, formal analysis and writing - original draft. All authors contributed to the article and approved the submitted version.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2023.1231326/full#supplementary-material
1. World_Health_Organizations. Weekly epidemiological update on COVID-19-3 August 2023 (2023). Available at: https://www.who.int/publications/m/item/weekly-epidemiological-update-on-covid-19---3-august-2023.
2. World_Health_Organizations. Viet Nam situation on COVID-19 (2023). Available at: https://covid19.who.int/region/wpro/country/vn.
3. Nguyen, LH, Drew, DA, Graham, MS, Joshi, AD, Guo, CG, Ma, W, et al. Risk of COVID-19 among front-line health-care workers and the general community: a prospective cohort study. Lancet Public Health. (2020) 5:e475–83. doi: 10.1016/S2468-2667(20)30164-X
4. Mutambudzi, M, Niedwiedz, C, Macdonald, EB, Leyland, A, Mair, F, Anderson, J, et al. Occupation and risk of severe COVID-19: prospective cohort study of 120 075 UK biobank participants. Occup Environ Med. (2020) 78:307–14. doi: 10.1136/oemed-2020-106731
5. Razu, SR, Yasmin, T, Arif, TB, Islam, MS, Islam, SMS, Gesesew, HA, et al. Challenges faced by healthcare professionals during the COVID-19 pandemic: a qualitative inquiry from Bangladesh. Front Public Health. (2021) 9:647315. doi: 10.3389/fpubh.2021.647315
6. De Kock, JH, Latham, HA, Leslie, SJ, Grindle, M, Munoz, S-A, Ellis, L, et al. A rapid review of the impact of COVID-19 on the mental health of healthcare workers: implications for supporting psychological well-being. BMC Public Health. (2021) 21:104. doi: 10.1186/s12889-020-10070-3
7. Shahbaz, S, Ashraf, MZ, Zakar, R, and Fischer, F. Psychosocial, emotional and professional challenges faced by female healthcare professionals during the COVID-19 outbreak in Lahore, Pakistan: a qualitative study. BMC Womens Health. (2021) 21:197. doi: 10.1186/s12905-021-01344-y
8. Sheraton, M, Deo, N, Dutt, T, Surani, S, Hall-Flavin, D, and Kashyap, R. Psychological effects of the COVID 19 pandemic on healthcare workers globally: a systematic review. Psychiatry Res. (2020) 292:113360. doi: 10.1016/j.psychres.2020.113360
9. Deng, Y, Chen, Y, and Zhang, B. Different prevalence trend of depression and anxiety among healthcare workers and general public before and after the peak of COVID-19 occurred in China: a meta-analysis. Asian J Psychiatr. (2021) 56:102547. doi: 10.1016/j.ajp.2021.102547
10. Chen, Y, Wang, J, Geng, Y, Fang, Z, Zhu, L, Chen, Y, et al. Meta-analysis of the prevalence of anxiety and depression among frontline healthcare workers during the COVID-19 pandemic. Front Public Health. (2022) 10:984630. doi: 10.3389/fpubh.2022.984630
11. Pappa, S, Ntella, V, Giannakas, T, Giannakoulis, VG, Papoutsi, E, and Katsaounou, P. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: a systematic review and meta-analysis. Brain Behav Immun. (2020) 88:901–7. doi: 10.1016/j.bbi.2020.05.026
12. Chew, NWS, Lee, GKH, Tan, BYQ, Jing, M, Goh, Y, Ngiam, NJH, et al. A multinational, multicentre study on the psychological outcomes and associated physical symptoms amongst healthcare workers during COVID-19 outbreak. Brain Behav Immun. (2020) 88:559–65. doi: 10.1016/j.bbi.2020.04.049
13. Liu, Y, Chen, H, Zhang, N, Wang, X, Fan, Q, Zhang, Y, et al. Anxiety and depression symptoms of medical staff under COVID-19 epidemic in China. J Affect Disord. (2021) 278:144–8. doi: 10.1016/j.jad.2020.09.004
14. Nguyen, TT, Le, XTT, Nguyen, NTT, Nguyen, QN, Le, HT, Pham, QT, et al. Psychosocial impacts of COVID-19 on healthcare workers during the Nationwide partial lockdown in Vietnam in April 2020. Front Psych. (2021) 12:562337. doi: 10.3389/fpsyt.2021.562337
15. Pham, QT, Le, XTT, Phan, TC, Nguyen, QN, Ta, NKT, Nguyen, AN, et al. Impacts of COVID-19 on the life and work of healthcare workers during the Nationwide partial lockdown in Vietnam. Front Psychol. (2021) 12:563193. doi: 10.3389/fpsyg.2021.563193
16. Nguyen, TK, Tran, NK, Bui, TT, Tran, LT, Tran, NT, Do, MT, et al. Mental health problems among front-line healthcare workers caring for COVID-19 patients in Vietnam: a mixed methods study. Front Psychol. (2022) 13:858677. doi: 10.3389/fpsyg.2022.858677
17. Le Thi, NA, Dang Van, C, Nguyen Thanh, P, Lewycka, S, and Van Nuil, JI. Depression, anxiety, and stress among frontline health workers during the second wave of COVID-19 in southern Vietnam: a cross-sectional survey. PLoS Glob Publ Health. (2022) 2:e0000823. doi: 10.1371/journal.pgph.0000823
18. Tran, TD, Tran, T, and Fisher, J. Validation of the depression anxiety stress scales (DASS) 21 as a screening instrument for depression and anxiety in a rural community-based cohort of northern Vietnamese women. BMC Psychiatry. (2013) 13:24. doi: 10.1186/1471-244X-13-24
19. Lovibond, SH, and Lovibond, PF. Manual for the depression anxiety stress scales. 2nd edn. Sydney: Psychology Foundation of Australia (1995).
20. Chen, Q, Liang, M, Li, Y, Guo, J, Fei, D, Wang, L, et al. Mental health care for medical staff in China during the COVID-19 outbreak. Lancet Psychiatry. (2020) 7:e15–6. doi: 10.1016/S2215-0366(20)30078-X
21. Buselli, R, Corsi, M, Veltri, A, Baldanzi, S, Chiumiento, M, Lupo, ED, et al. Mental health of health care workers (HCWs): a review of organizational interventions put in place by local institutions to cope with new psychosocial challenges resulting from COVID-19. Psychiatry Res. (2021) 299:113847. doi: 10.1016/j.psychres.2021.113847
22. Doan, QH, Tran, NN, Than, MH, Nguyen, HT, Bui, VS, Nguyen, DH, et al. Depression, anxiety and associated factors among frontline hospital healthcare Workers in the Fourth Wave of COVID-19: empirical findings from Vietnam. Trop Med Infect Dis. (2021) 7:3. doi: 10.3390/tropicalmed7010003
23. Ning, L, Jia, H, Yu, J, Gao, S, Shang, P, Cao, P, et al. Mental health among healthcare workers during the prolonged COVID-19 pandemic: a cross-sectional survey in Jilin Province in China. Front Public Health. (2022) 10:1030808. doi: 10.3389/fpubh.2022.1030808
24. Kim, MY, and Yang, YY. Mental health status and its influencing factors: the case of nurses working in COVID-19 hospitals in South Korea. Int J Environ Res Public Health. (2021) 18:6531. doi: 10.3390/ijerph18126531
25. Demartini, B, Nisticò, V, D'Agostino, A, Priori, A, and Gambini, O. Early psychiatric impact of COVID-19 pandemic on the general population and healthcare Workers in Italy: a preliminary study. Front Psych. (2020) 11:561345. doi: 10.3389/fpsyt.2020.561345
26. Appel, AP, Carvalho, A, and Santos, RPD. Prevalence and factors associated with anxiety, depression and stress in a COVID-19 nursing team. Rev Gaucha Enfermagem. (2021) 42:e20200403. doi: 10.1590/1983-1447.2021.20200403
27. Mekonen, E, Shetie, B, and Muluneh, N. The psychological impact of COVID-19 outbreak on nurses working in the northwest of Amhara regional state referral hospitals, Northwest Ethiopia. Psychol Res Behav Manag. (2020) 13:1353–64. doi: 10.2147/PRBM.S291446
28. Holmes, EA, O'Connor, RC, Perry, VH, Tracey, I, Wessely, S, Arseneault, L, et al. Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. Lancet Psychiatry. (2020) 7:547–60. doi: 10.1016/S2215-0366(20)30168-1
29. Singh, R, and Subedi, M. COVID-19 and stigma: social discrimination towards frontline healthcare providers and COVID-19 recovered patients in Nepal. Asian J Psychiatr. (2020) 53:102222. doi: 10.1016/j.ajp.2020.102222
30. Toan, DTT, Pham, TH, Nguyen, KC, Pham, QT, Ha, QD, Nguyen, HL, et al. Shift from a zero-COVID strategy to a new-normal strategy for controlling SARS-CoV-2 infections in Vietnam. Epidemiol Infect. (2023) 151:e117. doi: 10.1017/S0950268823001048
31. Burton, CL, and Bonanno, GA. Measuring ability to enhance and suppress emotional expression: the flexible regulation of emotional expression (FREE) scale. Psychol Assess. (2016) 28:929–41. doi: 10.1037/pas0000231
32. Bonanno, GA, Maccallum, F, Malgaroli, M, and Hou, WK. The context sensitivity index (CSI): measuring the ability to identify the presence and absence of stressor context cues. Assessment. (2020) 27:261–73. doi: 10.1177/1073191118820131
33. Park, S, Lee, Y, Kim, T, and Jung, SJ. Anxiety and COVID-19 related stressors among healthcare workers who performed shift work at four COVID-19 dedicated hospitals in Korea. J Occup Environ Med. (2021) 63:875–80. doi: 10.1097/JOM.0000000000002250
34. Lai, J, Ma, S, Wang, Y, Cai, Z, Hu, J, Wei, N, et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw Open. (2020) 3:e203976. doi: 10.1001/jamanetworkopen.2020.3976
35. van Elk, F, Robroek, SJW, Burdorf, A, and Oude Hengel, KM. Impact of the COVID-19 pandemic on psychosocial work factors and emotional exhaustion among workers in the healthcare sector: a longitudinal study among 1915 Dutch workers. Occup Environ Med. (2023) 80:27–33. doi: 10.1136/oemed-2022-108478
36. Rossi, R, Socci, V, Pacitti, F, Di Lorenzo, G, Di Marco, A, Siracusano, A, et al. Mental health outcomes among frontline and second-line health care workers during the coronavirus disease 2019 (COVID-19) pandemic in Italy. JAMA Netw Open. (2020) 3:e2010185. doi: 10.1001/jamanetworkopen.2020.10185
37. Weilenmann, S, Ernst, J, Petry, H, Pfaltz, MC, Sazpinar, O, Gehrke, S, et al. Health care workers' mental health during the first weeks of the SARS-CoV-2 pandemic in Switzerland-a cross-sectional study. Front Psych. (2021) 12:594340. doi: 10.3389/fpsyt.2021.594340
38. Robles, R, Rodríguez, E, Vega-Ramírez, H, Álvarez-Icaza, D, Madrigal, E, Durand, S, et al. Mental health problems among healthcare workers involved with the COVID-19 outbreak. Rev Bras Psiquiatr. (2021) 43:494–503. doi: 10.1590/1516-4446-2020-1346
39. Billings, J, Ching, BCF, Gkofa, V, Greene, T, and Bloomfield, M. Experiences of frontline healthcare workers and their views about support during COVID-19 and previous pandemics: a systematic review and qualitative meta-synthesis. BMC Health Serv Res. (2021) 21:923. doi: 10.1186/s12913-021-06917-z
40. Poh, LW, Teo, I, Tewani, K, Tan, HK, Yoon, S, and Sung, SC. Understanding the needs of health care workers in Singapore during the COVID-19 outbreak: a qualitative analysis. Am J Infect Control. (2022) 50:1133–9. doi: 10.1016/j.ajic.2022.06.004
41. Morina, N, Weilenmann, S, Dawson, K, Ernst, J, Zanitti, Z, von Känel, R, et al. RECHARGE – a brief psychological intervention to build resilience in health care workers during the COVID-19 pandemic: study protocol for a randomized controlled trial. (2021) Research Square: Blenheim Chalcot Company.
42. Samaan, Z.Z The role of virtual peer support platforms for reducing stress and burnout among frontline healthcare workers during COVID-19: a randomized controlled trial (clinical trial registration no. NCT04474080). Available at: https://clinicaltrials.gov/study/NCT04474080 (2020).
43. World_Health_Organization. Occupational health (2021). Available at: https://www.who.int/health-topics/occupational-health.
44. Oei, TP, Sawang, S, Goh, YW, and Mukhtar, F. Using the depression anxiety stress scale 21 (DASS-21) across cultures. Int J Psychol. (2013) 48:1018–29. doi: 10.1080/00207594.2012.755535
Keywords: depression, anxiety, stress, DASS 21, healthcare workers, COVID-19, Vietnam
Citation: Thu Pham H, Viet Cao T, Bich Le N, T-T Nguyen N, Thi Ngoc Vuong B, Vu Dieu Pham L, Thu Hoang T, Thi Hanh Pham T, Ngoc Nguyen T, Thi Thu Bui H, Van Tran T, Thuy Vu L and Thi Le P (2023) Depression, anxiety and stress among healthcare workers in the context of the COVID-19 pandemic: a cross-sectional study in a tertiary hospital in Northern Vietnam. Front. Public Health. 11:1231326. doi: 10.3389/fpubh.2023.1231326
Received: 30 May 2023; Accepted: 15 August 2023;
Published: 19 September 2023.
Edited by:
Juan Jesús García-Iglesias, University of Huelva, SpainReviewed by:
Rahim Badrfam, Alborz University of Medical Sciences, IranCopyright © 2023 Thu Pham, Viet Cao, Bich Le, T-T Nguyen, Thi Ngoc Vuong, Vu Dieu Pham, Thu Hoang, Thi Hanh Pham, Ngoc Nguyen, Thi Thu Bui, Van Tran, Thuy Vu and Thi Le. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ngoc Bich Le, bGJuQGh1cGguZWR1LnZu
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.