- ICMR-National Institute of Research in Tribal Health, Jabalpur, India
Tuberculosis (TB) is a significant public health problem among the Saharia community, an underprivileged tribal group in the west-central part of India. There are several challenges for India’s TB control program to curtail TB in the Saharia tribe. Malnutrition, poor health sector facilities, lower socio-economic status, and substance abuse are interconnected and synergistic factors contributing to a high burden of TB in the Saharia tribe. In this review, efforts are made to collate the findings of previous studies discussing the causes of high burden of TB in the Saharia tribe, social gaps for mitigating these preventable risk factors of TB in the Saharia tribe, and the plausible solutions for closing these gaps. The concept of Health in All Policies and intersectoral co-ordination is needed for the reduction of TB in the Saharia tribe and to make India TB-free by the year 2025.
1. Background
Tuberculosis (TB) is an airborne infectious disease, and its persistent morbidity and mortality remains one of the major public health challenges in developing countries such as India (1). Three countries, namely India, Indonesia, and the Philippines, shoulder the 67% global burden of TB (2). It is estimated that, globally, 10.6 million people developed TB in the year 2021 as compared to 10.1 million in the preceding year (3). TB is the 13th leading cause of death and second leading infectious disease globally after coronavirus (4).
India contributes 30% of the global TB cases, which is the highest in the world (2, 5, 6). The incidence of TB in India for the year 2022 was 172 per 100,000 people. A sharp rise in TB cases of 13% was recorded in 2022 as compared with 2021 (6, 7). The prevalence of TB is lowest in Kerala (67 per 100,000) whereas it is highest (546 per 100,000) in the state of Delhi (6–8).
The Saharia community is a particularly vulnerable tribal group (PVTG) (9). The prevalence of pulmonary TB in Saharia PVTG is alarmingly high (about 7–10 times higher than the national average in previous studies). The prevalence of TB in the Saharia tribe has been reported as 1518/100,000 in Sheopur (10), 1504/100,000 in Shivpuri (11), and 3294/100,000 in Gwalior districts (12) in previous surveys conducted at different time points. Various demographic and socio-economic factors as well as nutritional status, availability of health amenities in the vicinity, and lifestyle patterns may be responsible for the high prevalence of TB in Saharia tribe (13).
India is planning to eradicate TB by the year 2025, Five years ahead of the global End TB timeline (1, 14). TB-free initiatives at state levels are being carried out to achieve a 90% reduction in the prevalence of TB by the year 2025 from a baseline prevalence of the year 2015 (3, 15). To attain the goal of END-TB by 2025, it is urgent to mitigate the risk factors associated with TB. In previous studies, various determinants of health associated with the high burden of TB in Saharia PVTG have been identified, which are summarized in this article. In addition, several gaps and challenges for reducing the risk factors in previous studies are also discussed in this article.
2. Risk factors associated with the high prevalence of TB among the Saharia tribe
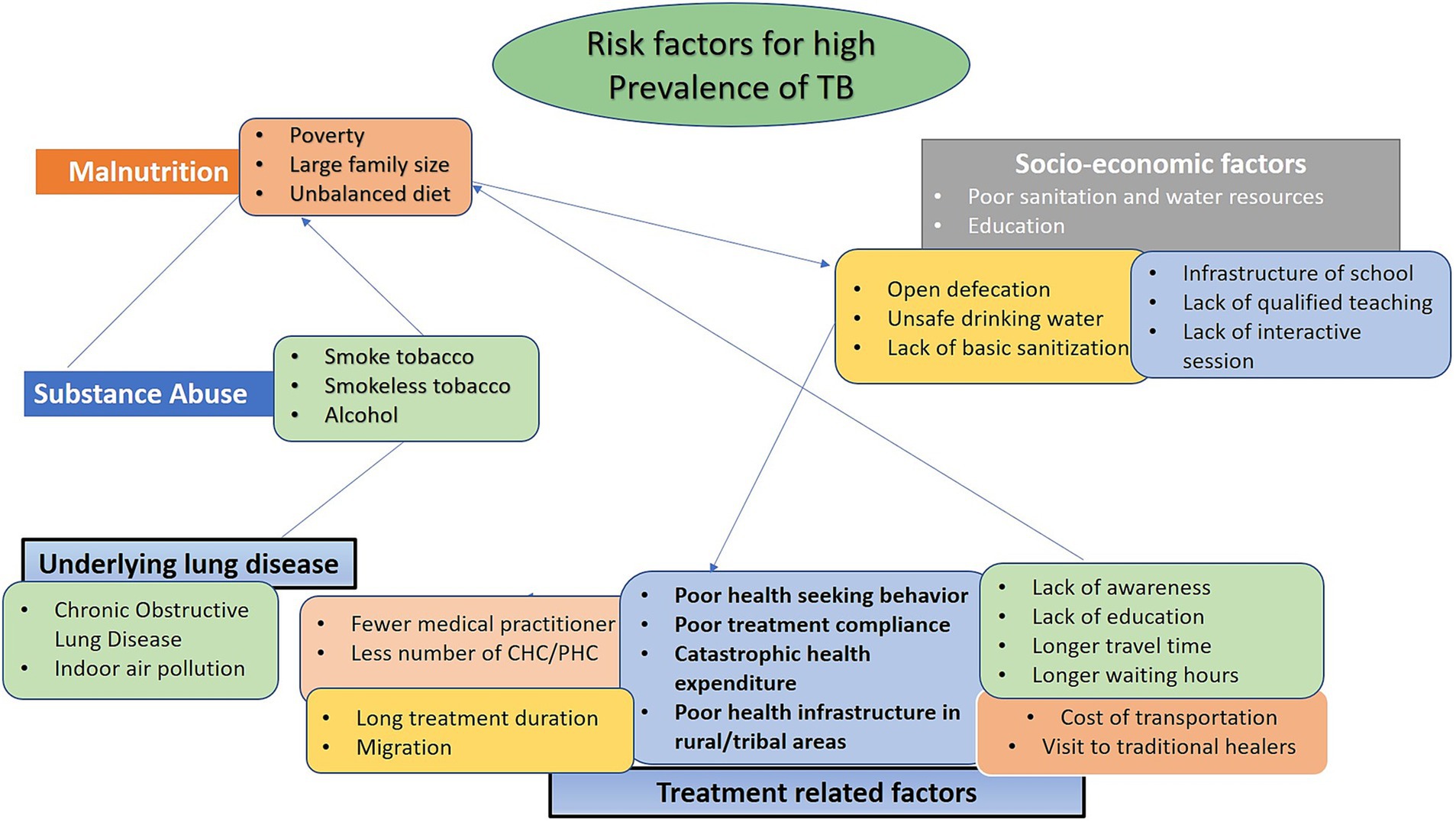
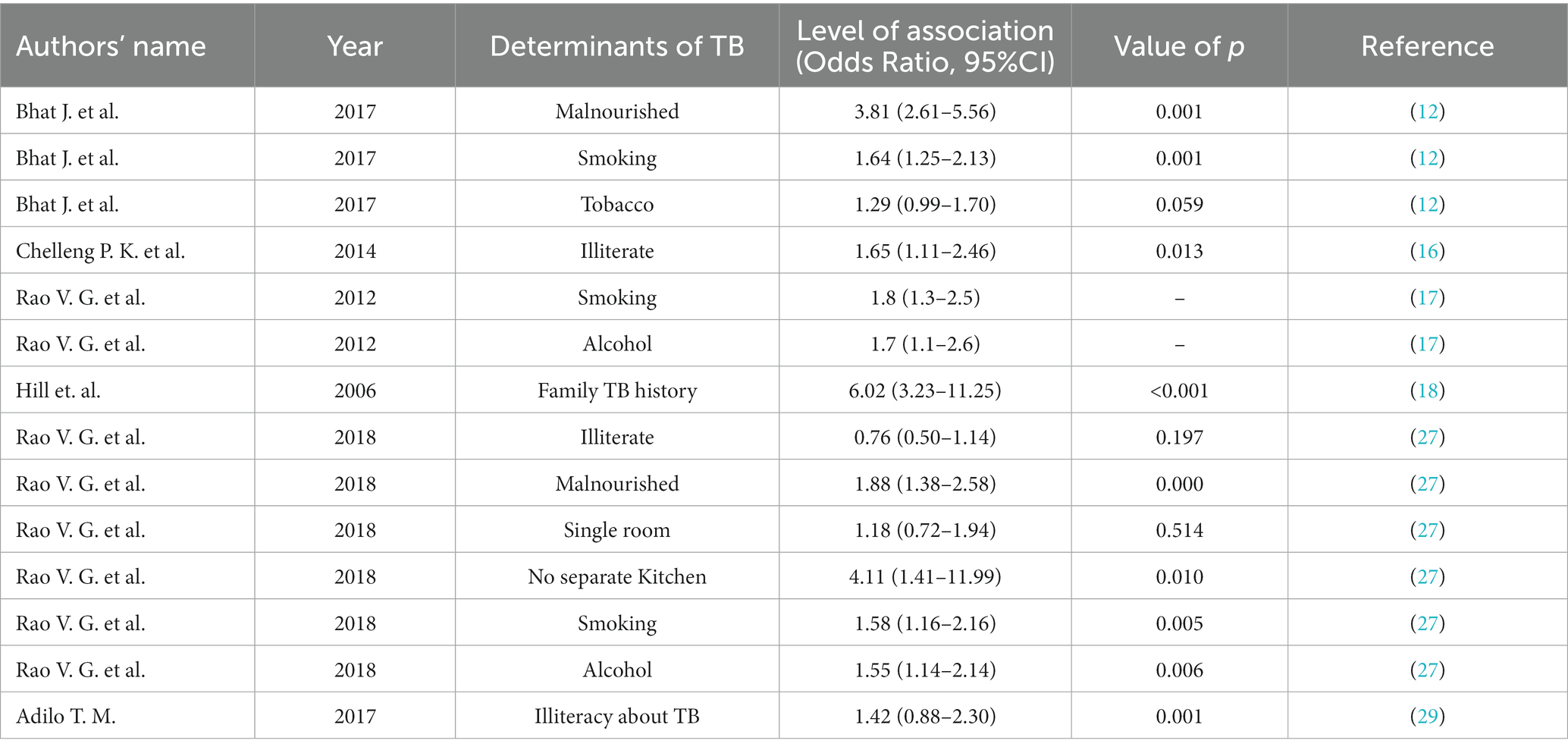
As discussed above, the Saharia tribe exhibit a high burden of TB. Various factors such as malnutrition, underlying lung disease(s), substance abuse, treatment-related factors, and low-socio-economic status have been found to be linked with TB [(12, 16–18); Figure 1]. These factors need to be addressed in the context of Saharia PVTG.
2.1. Malnutrition
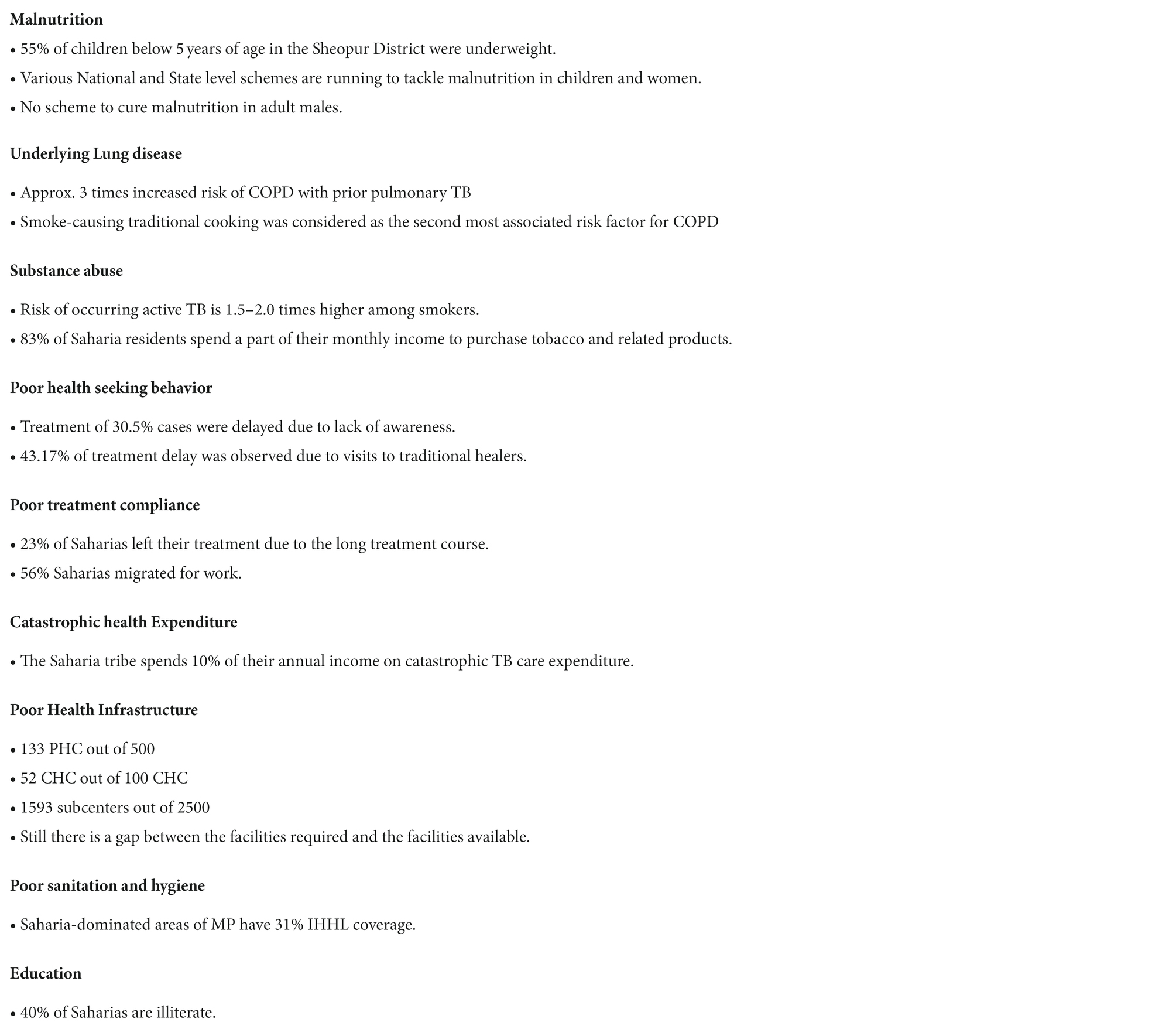
Undernutrition and TB form a vicious cycle. Malnourished individuals are more susceptible to the development of active TB, while TB exacerbates malnutrition [Figure 2; (19, 20)]. Cell-mediated immunity, which is the principal defense against Mycobacterium tuberculosis, is selectively compromised by undernutrition, and thereby increases the risk of reactivation of latent infection to disease (21). Various evidence generated from ecological studies, case series, and large population-based cohort studies have shown the association between nutritional status and the incidence of TB among humans (19, 22, 23). Previous systematic reviews and meta-analysis have shown that the TB incidence reduces by 13.8% with per unit increase in body mass index (BMI) (23, 24). Furthermore, malnutrition also affects the outcome of TB treatment (20). A study conducted in rural Chhattisgarh state, India, by following up 1,179 active TB cases, showed that severe undernutrition at the time of diagnosis was associated with two times higher risk of death (25). There are high chances of relapse of TB in patients who are underweight before the start of treatment (22, 26). Furthermore, TB infection increases the anabolic process and consumes additional energy and therefore TB patients are at increasing risk of becoming underweight (25).
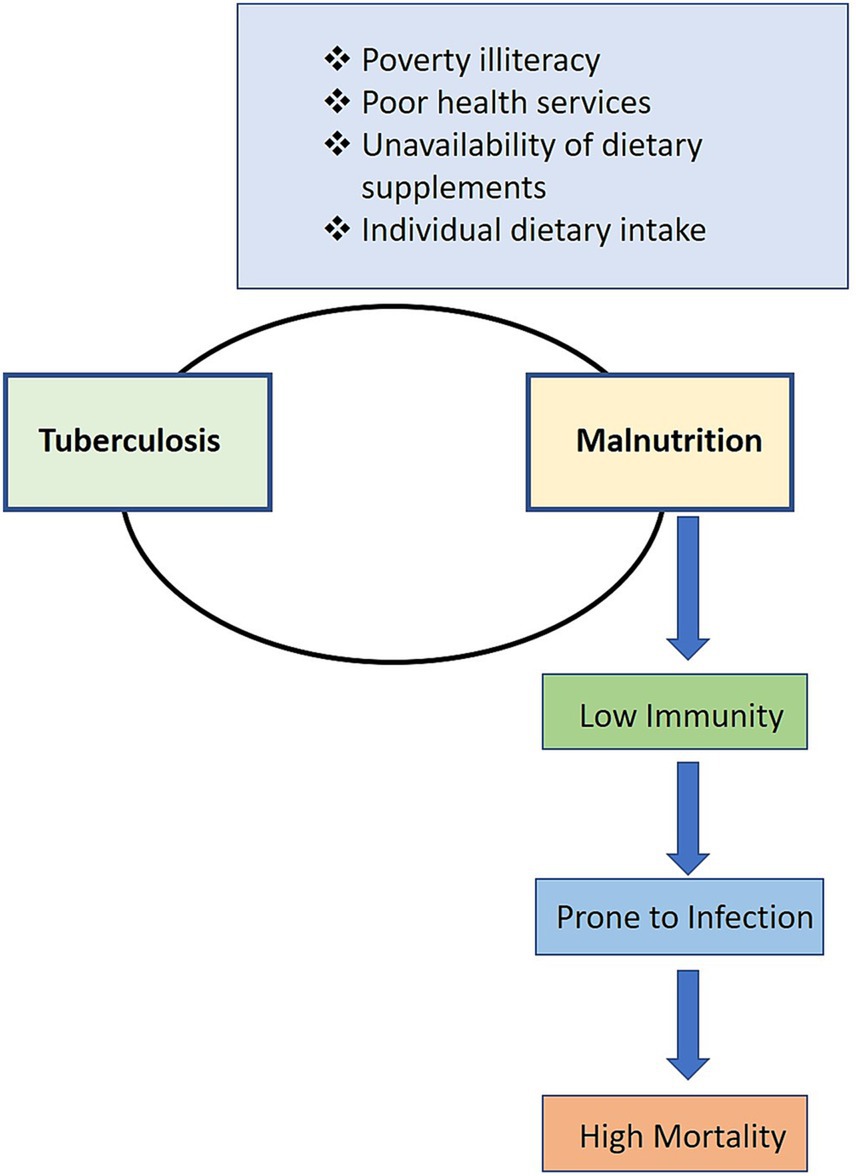
Figure 2. Relationship between TB and malnutrition: Due to TB and malnutrition, the affected person has generally lower immunity and is more prone to infection, which leads to high mortality (19–28).
The Saharia tribe have an exorbitantly high rate of malnutrition (12, 27). Previous reports indicate 32–60% of children below 5 years of age are underweight whereas stunting was observed in 40 to 65% of children belonging to Saharia PVTG. Previous studies have also shown that 93% of Saharia children suffered from malnourishment at some age and 15% of them were almost on the verge of death due to malnourishment (28). The high prevalence of undernutrition in the Saharia tribe is also supported by the fact that more than 75.2% non-pregnant non-lactating (NPNL) and 74.6% pregnant women have anemia. Out of these, 4–15% have severe anemia (28). Furthermore, 64% of TB cases were attributed to malnutrition in Saharia PVTG. Additionally, Saharia people with BMI <18.5 kg/m2 have a high risk of pulmonary TB [Table 1; (12)].
2.2. Underlying lung diseases and other predisposing factors/conditions
Chronic Obstructive Pulmonary Disease (COPD) is a chronic inflammatory lung disease that causes obstructed airflow from the lungs. The relationship between TB and COPD is complex due to similar symptoms of breathing difficulty, cough, mucus, sputum production, and wheezing. Previous studies showed that patients with chronic COPD have a three times higher risk of developing active TB as compared to the general population (30). The growing global burden of COPD is alarming, especially in highly endemic TB settings (30, 31). Various risk factors such as lower socioeconomic status, air pollution, and exposure to environmental or occupational dust are the major contributing factors for lung diseases like COPD in India (32–34). Exposure to indoor smoke by cooking inside the house using firewood or kerosene is considered the second-most common risk factor associated with COPD (35–38).
In the Saharia tribe, 12–18% of people with pulmonary TB also have asthma [Table 1; (16, 28)]. The people of the Saharia tribe usually live in one-room houses with no proper ventilation and cook inside the house using firewood (Figures 3A,B). Therefore, they are exposed to a higher amount of toxic air pollutants and microscopic fine particles produced by biofuels. Frequent exposure to this smoke may lead to burning eyes, bronchitis, COPD, and asthma. Previous studies have shown that cooking inside the house using traditional methods is associated with the occurrence of TB [(27); Table 1].
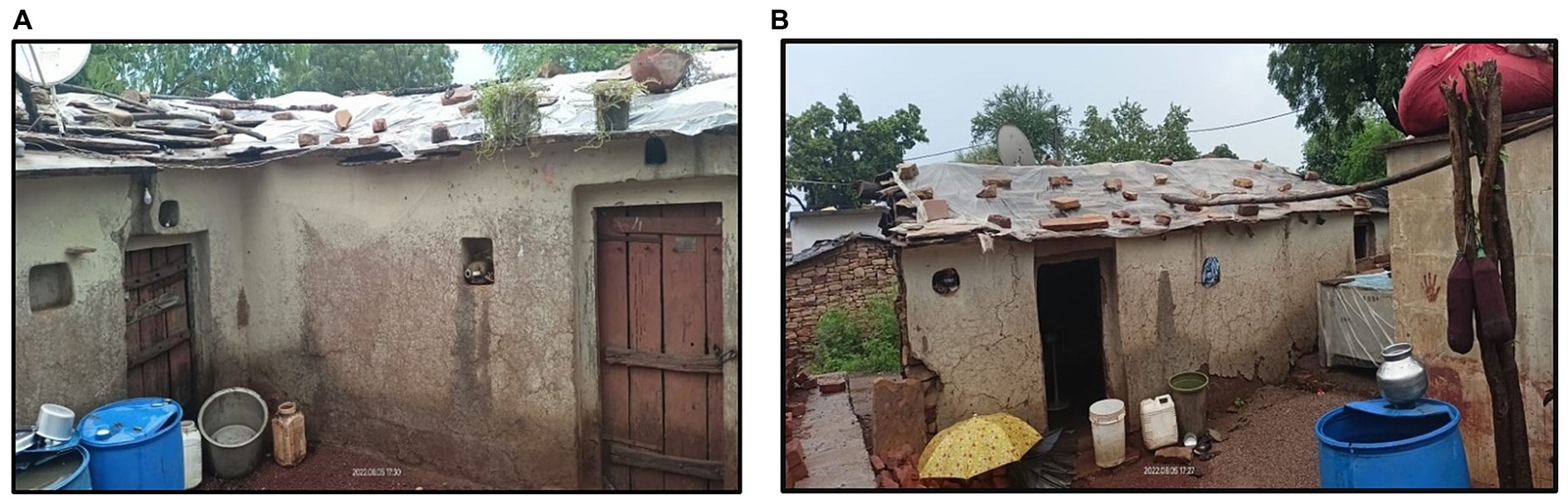
Figure 3. Traditional designs of Saharia houses (A and B) (lack of ventilation increases the chances of indoor transmission from an index case to other members of the family) (Photos are captured by the authors during field activities).
Furthermore, the majority of the Saharia community works as migratory laborers in rice fields where they are exposed to rice husk dust. Previous studies showed that exposure to rice husk dust is associated with decreased lung function. Long-term exposure may lead to the development of COPD (39–42).
2.3. Substance abuse
Substance abuse is a significant risk factor for TB infection and disease (Table 1). Substance abusers present unique challenges for TB diagnosis and control (43). They are more likely to be infectious, take longer to become culture-negative for TB bacilli, and remain at increased risk of TB-related mortality. The physiological effects of substance abuse may contribute to the high prevalence of TB among substance abusers. In-vitro studies have shown deleterious effects on the immune system, with biological evidence supporting direct impairment of the cell-mediated immune response using opium-derived drugs (opiates) (44).
Tobacco smoking is a major factor in the loss of lung function and causes lung diseases like TB, COPD, and asthma. Risk of occurring active TB is 1.5 to 2 times higher among smokers (34, 41, 42). Smoking suppresses innate as well as adaptive immunity and reduces the activity of alveolar macrophages, dendritic cells, and natural killer cells. This in turn increases the susceptibility to pulmonary bacterial infection (45). Furthermore, several studies demonstrated alcohol consumption to be a major risk factor for TB (46–49).
Comparative studies have explained that heavy episodic drinking is associated with higher rates of treatment failure, relapse, and death (48). Additionally, alcohol is a factor for default and non-compliance in TB. Moreover, alcohol intake increases the risk of active TB among TB patients. Alcohol and alcohol-related conditions are reported to influence the immune system and contribute to the increase risk of TB in individuals with alcohol use disorders (47).
High rates of tobacco smoking and alcohol consumption in the Saharia tribe may be one of the contributing factors for the high burden of TB. The Saharia tribe have a high rate of alcohol and tobacco consumption which can be exemplified by the fact that around 83% of the Saharia people spend a significant amount of their regular monthly income on alcohol/tobacco products (28). Furthermore, groups of Saharia people often share bidi (a cheaper alternative to cigarettes for tobacco smoking, made with Tendu leaves locally), which are wet with saliva and thus can contribute to increased transmission of Mycobacterium tuberculosis among the social groups (9), considering the already high prevalence of TB in Saharia community members. Previous studies conducted in the Saharia tribe have shown that alcohol consumption and tobacco smoking increase the risk for development of pulmonary TB (27). Studies have shown that the prevalence of respiratory disease remains higher among the members who are involved in the occupation of bidi making (50). Other studies revealed that hazardous exposure to tobacco among children is associated with symptoms of ill health, poor nutritional status, and higher risk of infectious diseases, including TB and HIV (51). Despite the source of substitutional income through bidi making, it causes hazardous health impacts on the workers, especially children, involved in this trade. During the process of making bidi, tobacco powder needs to undergo heat treatment, vaporizing it into air, and the persons working in these areas are inevitably exposed to tobacco smoke through their skin and respiratory tracts. Many members of the Saharia community are engaged in the occupation of ‘bidi making’ in their improperly ventilated houses, which makes them even more vulnerable to tobacco exposure (50).
2.4. Treatment-related factors
2.4.1. Poor health-seeking behavior
Like other tribes, Saharia also has poor health-seeking behavior due to various factors (Figure 4): (i) socio-cultural beliefs in traditional healers (called ‘Gunias’), (ii) lack of awareness and faith in modern treatment facilities, (iii) lack of health facilities in their vicinity, and (iv) lack of public transport and health illiteracy (52, 53). Saharia community members generally use take-home remedies to cure diseases and usually prefer to visit traditional healers. Belief in local practices and Gunias indirectly affects health outcomes adversely, thereby further contributing to transmission of TB bacilli [(1, 53); Table 1].
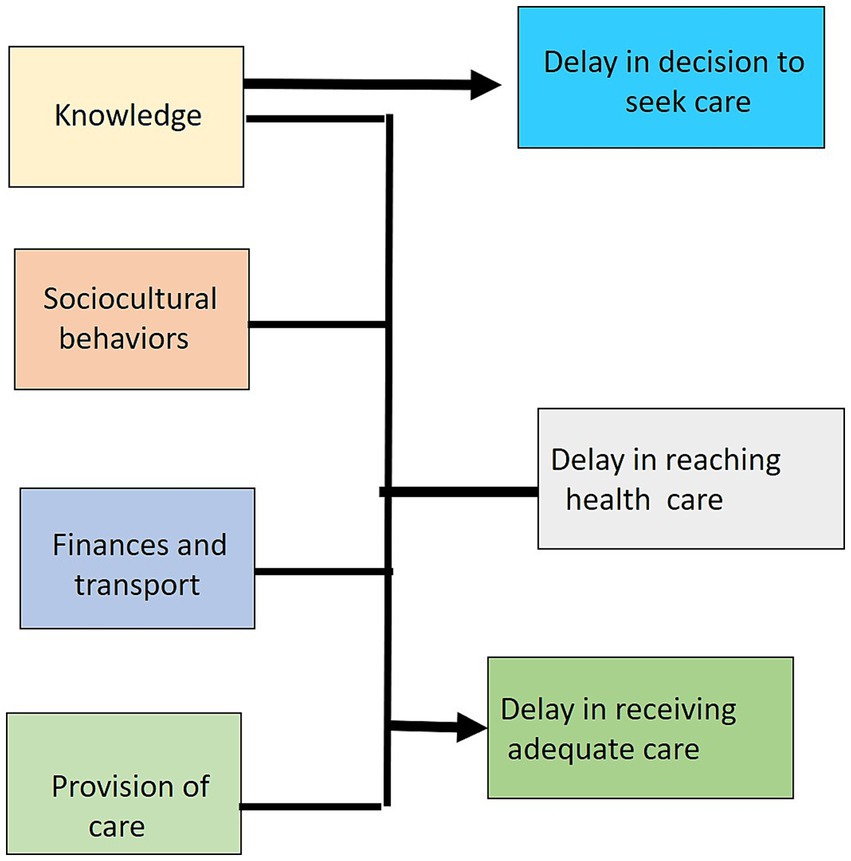
Figure 4. Interconnected factors for poor health-seeking behavior: Various factors like lack of awareness, longer travel time to reach hospitals, and catastrophic expenditure on TB treatment are responsible for poor health-seeking behavior (52–54).
Since TB is an airborne disease, early treatment is crucial for preventing transmission. Various factors are responsible for the delay in diagnosis and treatment of TB patients. Poor health seeking behavior is one of the major risk factors associated with high transmission of TB. The treatment of 30.5% of TB cases is delayed due to lack of awareness. Another major reason for delay in treatment initiation among 43.17% of TB cases is due to their visit to traditional healers/private practitioners after TB diagnosis in tribes of the Odisha state (52). However, similar information in the Saharia tribe living in Madhya Pradesh state is lacking. Various factors like illiteracy, lack of awareness, and treatment expenditure are contributing to poor health-seeking behavior of the Saharia tribe [(52–54); Figure 4].
2.4.2. Poor treatment compliance
Longer treatment duration with various side effects for anti-tubercular therapy (ATT) may be a responsible factor for poor treatment compliance (29, 54, 55). Previous studies reported that 23% of patients left their treatment early because of the long time duration (28). Most of the Saharia are daily wage earners. Among the Saharia households, approximately 56% migrated for work while only 12% of those from non-Saharia households migrated for work (28). Due to this migration, the Saharia tribe has poor treatment compliance and, therefore, increased transmission of Mycobacterium tuberculosis (55).
2.4.3. Catastrophic health expenditure
Despite having free diagnosis and treatment of TB from the National Tuberculosis Elimination Program (NTEP), various out-of-pocket expenditures are incurred by the families affected with TB. The Saharia tribe face catastrophic TB care expenditures that can amount to roughly 10% of their annual income (28). Catastrophic cost includes the loss of daily wages and travel costs to healthcare facility. Moreover, treatment and hospitalization in severe cases exert a higher economic burden on TB patients (56). Expenditure caused by TB and its treatment can be catastrophic for households (57).
2.4.4. Poor health infrastructure in rural/tribal areas
Among the barriers that restrict TB control in Saharia is poor healthcare facilities. Nine Saharia-inhabited districts of Madhya Pradesh have a total population of approx. 1.07 crores. These nine districts have only 52 Community Health Centers, which is half of the required CHC as per NHM guidelines (58). Similarly, there are only 25% of the necessary Primary Healthcare Centers (PHCs) compared to the recommended number.
2.5. Socio-economic factors
2.5.1. Poor housing and overcrowding
The End TB Strategy and UN Sustainable Development Goals recognize the interdependence between social determinants and health, particularly in low-and middle-income countries where most TB cases are clustered among economically and socially disadvantaged groups. Furthermore, previous studies carried out in the Saharia community have reported that poor housing quality and overcrowding correlate with increased TB prevalence, while higher ‘social capital’ (detailed below) was associated with lower TB prevalence within a household (59). ‘Social capital’ refers to the value of social networks and connections, which may promote dissemination of TB-related awareness, leading to increase knowledge and TB-preventive behavior. Furthermore, overcrowding and roof leakage significantly contributed to the increased probability of TB (59, 60). Due to limited resources, Saharia PVTG are living in small, non-ventilated houses with a large number of family members, making them more prone to TB infection. These findings suggest that socioeconomic factors play a significant role in the high prevalence of TB in the Saharia community. Socioeconomic status is a crucial determinant of differential exposure, vulnerability to disease-causing agents, and differential consequences of ill health.
2.5.2. Poor sanitation and water resources
The Saharia are a vulnerable population with limited access to health resources and services, and they are particularly at risk of TB due to poor sanitation and water resources. Sanitation and water resources are essential for preventing and treating TB, and the lack of access to these resources is a major contributing factor to the high prevalence of TB among the Saharia. Improving access to sanitation and water resources is essential for reducing the prevalence of TB among this population. The unhygienic living conditions increase the likelihood of contracting and spreading the disease, as well as other infectious diseases. Studies have shown the high prevalence of TB in areas with poor sanitation (61). Saharia-inhabited areas of Madhya Pradesh have 35% individual household latrine (IHHL) coverage (62) and most of them continue to defecate in the open (63).
2.5.3. Education
TB is associated with low education levels and reflects the complex interaction between non-communicable disease, urbanization, and a changing economic climate (48, 62). Low education or illiteracy has been found to be associated with TB among the Saharia tribe (64, 65).
Despite the occurrence of many government and private schools in Saharia-inhabited districts of Madhya Pradesh, approximately 40% of the population is still illiterate. The Saharia community has 11% more illiterate people than the non-Saharia community (28).
3. Strategies for reduction of preventable risk factors associated with TB
As discussed earlier, there are several risk factors (Box 1) which may be attributed to the high prevalence of TB in the Saharia tribe. To eliminate TB in high endemic settings, these risk factors need be addressed. Most of these factors are associated with initiatives for mitigating the above-mentioned risk factors and are discussed below.
To overcome malnutrition in tribes, various national-level programs are continuously running such as the “Pradhan Mantri Matru Vandana Yojana” (66) and the Scheme for Adolescent Girls under the umbrella of the Integrated Child Development Services Scheme (ICDS) (67). Recently, the POSHAN 2.0 Abhiyaan (Prime Minister’s Overarching Scheme for Holistic Nutrition) has also been initiated to curb malnutrition and improve nutritional outcomes for children, pregnant women, and lactating mothers.
Madhya Pradesh is the first state in the country where the community-based Nutrition Management (C-SAM) (66–69) was launched in the form of a two-phase campaign to identify severely malnourished children. Apart from these, various innovative schemes like “Tiranga Thali,” “Dastak Programme,” and “Seven (7) days Seven (7) plots” were started to create awareness, and provide a balanced diet to reduce malnutrition by the Madhya Pradesh government (66). In addition, to tackle the problem of malnutrition in TB patients, the Government of India is supporting the nutritional requirement of all TB patients through Nikshay Poshan Yojna for the entire duration of TB treatment (69).
Similarly, to control indoor as well as outdoor environmental pollution and minimize the respiratory health issues that occur due to coal, firewood, and cow dung smoke used for cooking, Pradhan Mantri Ujjwala Yojana (70) was launched by the Government of India. Ujjwala Yojana provides LPG connections to the remotest and poorest parts of the country to provide a smoke-free cooking environment. However, due to the high cost involved in cooking gas, the majority of Saharia people are still dependent on traditional cooking methods (Figures 5A,B).
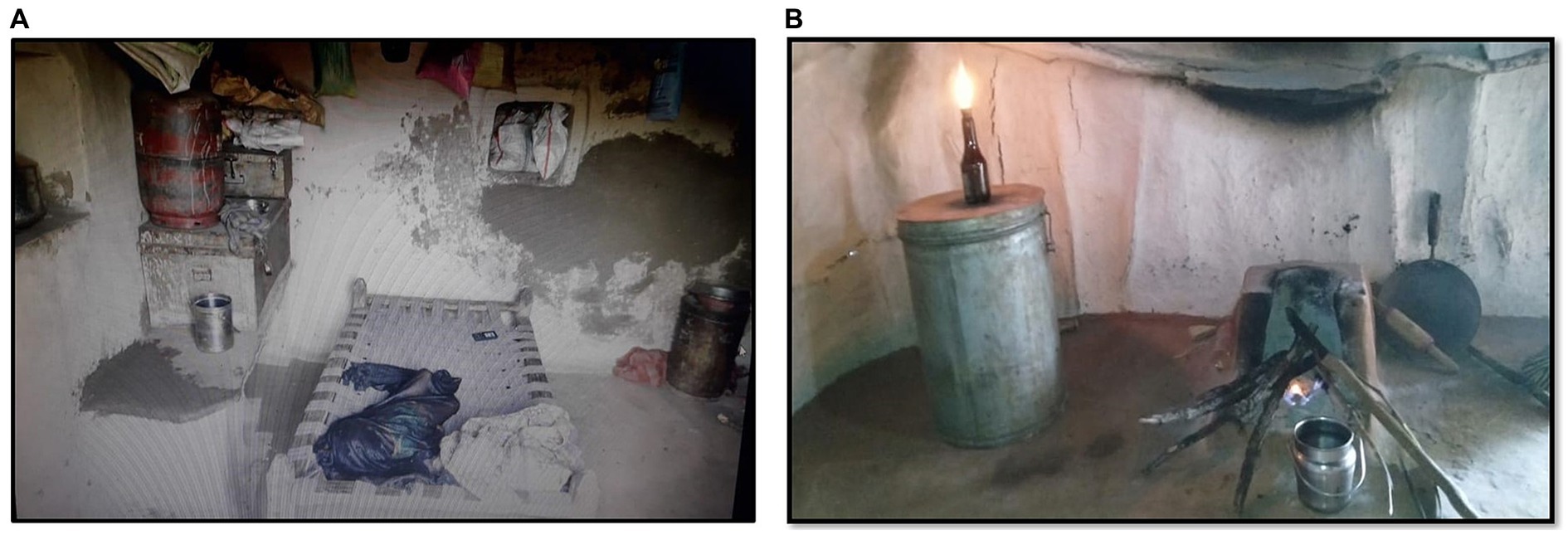
Figure 5. Negligence of LPG cylinders over basic cooking using wood-based smoke Chulha: Refilling of gas cylinders is not a routine practice in tribal areas owing to cost constraints (A) or distance/supply at home and the easy availability of firewood material from adjoining forests. It encourages more frequent use of smoke fuel and negligible use of LPG (B) (Photos are captured by the authors during field activities).
Tobacco consumption exerts hazardous direct effect on an individual’s health. At the same time, it also puts creates a high cost burden due to the cost of treatment of tobacco-related diseases. To create awareness about the harmful effects of tobacco consumption and to reduce the production and supply of tobacco products, in the year 2007–2008 the Government of India initiated the National Tobacco Control Programme (NTCP) (71). The program works at the national, state, and district levels.
The Government of India initiated several awareness schemes to prevent irregularity and poor treatment compliance. Migration certificates through the NIKSHAY portal is being provided to migrant people on ATT drug to minimize poor treatment compliance among migratory workers. Despite this, most of the patients become defaulters due to their sudden migration and are lost to follow-up. Regular work opportunity in their areas is the key to reducing migration and related poor treatment compliance.
The loss of daily income and frequently unaffordable expense of treatment push marginalized Saharia TB patients and their families deeper into poverty. For reduction of out-of-pocket expenditure, NTEP initiated doorstep diagnosis and provides treatment through ASHA. Further, NTEP is also providing travel costs for treatment initiation in tribal communities. Policies for reducing catastrophic costs may help in better treatment compliance. In addition to this, the Government of India introduced Ayushman Bharat-Health and Wellness Centers (HWC) in Feb 2018, to make the healthcare services available to out-of-reach patients. These HWCs cover around 3,000–5,000 people (72). Integrating TB services with these HWCs decentralizes the healthcare services and increases patient’s footfall for seeking treatment. It reduces the time for start of treatment after diagnosis, improves treatment compliance, and reduces out-of-pocket expenditure.
India has made tremendous progress in ending open defecation which significantly improves Water, Sanitation, and Hygiene (WASH). A tremendous achievement is possible because of the Government’s flagship program, the Swachh Bharat Mission (SBM) (Clean India Campaign), with the partnership of UNICEF (73). It has also been observed that there is a reduction in undernutrition in children under five after the increase in household toilet availability (74).
All these policies and programs initiated by the government are not directly benefiting Saharia PVTG. Other programs are indirectly benefiting Saharia such as Nikshay Poshan Yojna supporting malnourished TB patients. Similarly, Ujjwala Yojna provides gas cylinder connections to enable smoke-free cooking, as cooking-related smoke exposure is a major risk factor of TB. However, studies related to the effect of these initiatives on the reduction of TB in the Saharia tribe are lacking.
4. Existing gaps need to be considered
Despite various programs and schemes, Saharias remain among the most marginalized population in Madhya Pradesh and many of these government schemes remain underutilized by the Saharia community. Malnutrition continues to be a persisting challenge and will remain so until the underlying causes of malnutrition in Saharia are resolved. The policymakers and stakeholders consider malnutrition as a health-related issue. However, poverty, unemployment, and lifestyle are also important factors responsible for undernutrition due to an unbalanced diet. Currently, a major focus of various programs is on malnutrition in children and women. Malnutrition among adult males and older people often remains neglected, and these populations are also more susceptible to developing TB (75). Nutrition in adults may be improved through targeted supplementation of micronutrients and protein where diet alone is not sufficient to meet the age-specific requirements (76, 77). Still, there are many challenges for the treatment of malnutrition in adults due to various underlying age-related chronic disease (76).
Despite awareness about the health hazards of tobacco, reduction in tobacco consumption and substance abuse at the periphery is challenging. Clinicians and public health practitioners should be aware of special considerations and the latest evidence concerning TB management among people who are addicted to substances (43, 44). Strong political will is required to control tobacco consumption which is lacking at present due to the large economical factor involved in the tobacco industry. It is estimated that 20 million people are working in the tobacco industry, in which 0.74 million get employment for about three months through the collection of tendu leaves (Figure 6) and 4.16 million people earn their living by making bidis from Tendu leaves (78). Of these 4.16 million people, nearly 90% are women and children as this group often works for lower wages and yet remains proficient in rolling bidis (78, 79), thereby increasing the profit margin of the bidi manufacturers.

Figure 6. Collection of Tendu Patta by Saharia tribe: Bidi making process requires filling of tobacco inside Tendu Patta leaves which is collected by all age groups including young children. Bidi smoking is also a common practice among the workers, especially among adolescents and children from a young age (Photos are captured by the authors during field activities).
Timely and accurate diagnosis is the first and foremost requirement for the eradication of TB. Access to medical services should be provided to ensure that every case of TB can be properly diagnosed and treated. Without this assistance, the Saharia tribe will continue to face a high risk of developing TB and associated morbidity and mortality. Additionally, treatment strategies should incorporate the use of directly observed therapy (DOT) with deaddiction program for substance abuse (43, 44). Despite higher expenditure on the treatment of tobacco-related diseases (Rs 177,340 crore) than the average annual revenue collection from tobacco products (Rs 53,750 crore), the reduction of tobacco consumption seems far-sighted (78, 79). Commercial tobacco control strategies like increasing tobacco prices and anti-tobacco mass media campaigns can be effective in reducing the consumption of tobacco products. Deaddiction programs at workplaces may prevent direct as well as involuntary exposure to smoke. There is a high priority to focus on deaddiction and individual-level counseling in tribal areas.
To resolve the problem of open defecation, several toilets have been constructed in tribal and rural areas under the ‘Swachh Bharat Mission’ (SBM). However, most of the toilets constructed under this mission are being used as store rooms or to wash utensils by the Saharia tribe and they continue to defecate in the open. There is a need to adopt Behavioral Change Communication (BCC) strategies for the effective utilization of toilets and to stop open defecation.
To reduce the illiteracy rate, the education awareness strategy should be revised. There should be a separate strategy for each community. Campaigns for education through interactive meetings with the target community giving examples of successful educated persons belonging to similar communities may be an effective strategy for improving the literacy rate. A small contribution from every educated person to creating awareness toward education may be key to increasing awareness and literacy. Regular monitoring activities by the higher authorities in the schools situated in remote areas may increase attendance at school and improve the quality. Apart from the awareness, adapting the curriculum to suit specific areas may help in the reduction of preventable diseases such as TB. Since TB is a major problem of the Saharia tribe, awareness generation through educational programs at the school level will help in the elimination of TB.
5. Conclusion and the way forward
Morbidity and mortality due to TB are unacceptable considering the availability of highly effective early diagnostic and therapeutic options. Various aspects among particularly vulnerable tribal groups such as malnutrition, poor socio-economic status, high rate of substance abuse, and unequal access to diagnosis and treatment pose obstacles to TB elimination programs. Additionally, the increase in COVID-19 combined with the intermittence of health services during the pandemic has led to a predicted increase in the TB burden worldwide (80). To achieve the END TB goal by 2025, there is an urgent need to mitigate these obstacles along with active case finding and prompt treatment in vulnerable tribal groups, which have a high prevalence of TB at present. A context-specific, tailor-made policy and implantation plan based on existing and new scientific evidence is the need of the hour for the elimination of TB in the Saharia tribe. Intersectoral coordination is needed with the concept of Health in All Policies for making India TB-free. All concerned ministries, i.e., the Ministry of Health and Family Welfare, Ministry of Tribal Affairs, Ministry of Agriculture, Ministry of Women and Child Development, Ministry of Education, Ministry of Labour and Employment, and the Ministry of Social Justice and Empowerment may come forward and work together to mitigate all possible risk factors associated with TB and eventually eliminate TB from India.
Author contributions
PG did the literature search and wrote the first draft of the manuscript. RK and AD designed the study and revised the manuscript. PS provided important intellectual suggestions for improving the manuscript. All authors contributed to the article and approved the submitted version.
Acknowledgments
The authors thank the Secretary, Department of Health Research and Director General, Indian Council of Medical Research, New Delhi for providing facilities and support. PG is thankful to ICMR, New Delhi for the Research Associate fellowship.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Sachdeva, KS. Accelerating progress towards ending tuberculosis in India. Indian J Med Res. (2020) 151:266–8. doi: 10.4103/ijmr.IJMR_407_20
2. Kanabus, A. Information about tuberculosis, GHE (2022). Available at: www.tbfacts.org (Accessed March 31, 2023).
3. Chakaya, J, Petersen, E, Nantanda, R, Mungai, BN, Migliori, GB, Amanullah, F, et al. The WHO Global Tuberculosis 2021 report – not so good news and turning the tide back to End TB. Int J Infect Dis. (2022) 124:S26–9. doi: 10.1016/j.ijid.2022.03.011
4. TB/COVID-19 Global Study Group. Tuberculosis and COVID-19 co-infection: description of the global cohort. Eur Respir J. (2022) 59:2102538. doi: 10.1183/13993003.02538-2021
5. Khan, MK, Islam, MN, Ferdous, J, and Alam, MM. An overview on epidemiology of tuberculosis. Mymensingh Med J. (2019) 28:259–66.
6. Bagcchi, S. WHO's global tuberculosis report 2022. Lancet Microbe. (2023) 4:e20. doi: 10.1016/S2666-5247(22)00359-7
7. Central, TB Division, Ministry of Health and Family Welware, Government of India. India TB Report 2023. Coming Together to End TB Altogether. Available at: TBAnnaulReport 2023.pdf (tbcindia.gov.in) (Accessed September 4, 2023).
8. ICMR-National Institute for Research in Tuberculosis. National TB prevalence survey in India. 2019–2021. Available at: https://tbcindia.gov.in/showfile.php?lid=3659 (Accessed March 29, 2023).
9. Das, A. Aiming for a tuberculosis-free India: perspective of a highly endemic Particularly Vulnerable Tribal Group (PVTG). Clin Epidemiol Global Health. (2021) 9:69–70. doi: 10.1016/j.cegh.2020.07.001
10. Thomas, BE, Thiruvengadam, K, Vedhachalam, C, A, S, Rao, VG, Vijayachari, P, et al. Prevalence of pulmonary tuberculosis among the tribal populations in India. PLoS One. (2021) 16:e0251519. doi: 10.1371/journal.pone.0251519
11. Bhat, J, Sharma, RK, Yadav, R, Mishra, P, Nigam, S, Lingala, MA, et al. Persistent high prevalence of pulmonary tuberculosis in a resource-limited setting: threat to India's TB Free campaign. Trans R Soc Trop Med Hyg. (2022) 116:564–70. doi: 10.1093/trstmh/trab181
12. Bhat, J, Rao, VG, Sharma, RK, Muniyandi, M, Yadav, R, and Bhondley, MK. Investigation of the risk factors for pulmonary tuberculosis: a case-control study among Saharia tribe in Gwalior district, Madhya Pradesh, India. Indian J Med Res. (2017) 146:97–104. doi: 10.4103/ijmr.IJMR_1029_16
13. Taye, H, Alemu, K, Mihret, A, Wood, JLN, Shkedy, Z, Berg, S, et al. Global prevalence of Mycobacterium bovis infections among human tuberculosis cases: systematic review and meta-analysis. Zoonoses Public Health. (2021) 68:704–18. doi: 10.1111/zph.12868
14. Pai, M, Bhaumik, S, and Bhuyan, SS. India's plan to eliminate tuberculosis by 2025: converting rhetoric into reality. BMJ Glob Health. (2016) 2:e000326. doi: 10.1136/bmjgh-2017-000326
15. Fukunaga, R, Glaziou, P, Harris, JB, Date, A, Floyd, K, and Kasaeva, T. Epidemiology of tuberculosis and progress toward meeting global targets-worldwide, 2019. MMWR Morb Mortal Wkly Rep. (2021) 70:427–30. doi: 10.15585/mmwr.mm7012a4
16. Chelleng, PK, Devi, KR, Borbora, D, Chetia, M, Saikia, A, Mahanta, J, et al. Risk factors of pulmonary tuberculosis in tea garden communities of Assam, India. Indian J Med Res. (2014) 140:138–41.
17. Rao, VG, Gopi, PG, Bhat, J, Yadav, R, Selvakumar, N, and Wares, DF. Selected risk factors associated with pulmonary tuberculosis among Saharia tribe of Madhya Pradesh, Central India. Eur J Pub Health. (2012) 22:271–3. doi: 10.1093/eurpub/ckr009
18. Hill, P, Jackson-Sillah, D, Donkor, S, Otu, J, Adegbola, R, and Lienhardt, C. Risk factors for pulmonary tuberculosis TB: a clinic-based case control study in the Gambia. BMC Public Health. (2006) 6:156. doi: 10.1186/1471-2458-6-156
19. Sinha, P, Lönnroth, K, Bhargava, A, Heysell, SK, Sarkar, S, Salgame, P, et al. Food for thought: addressing undernutrition to end tuberculosis. Lancet Infect Dis. (2021) 21:e318–25. doi: 10.1016/S1473-3099(20)30792-1
20. Sinha, P, Davis, J, Saag, L, Wanke, C, Salgame, P, Mesick, J, et al. Undernutrition and tuberculosis: public health implications. J Infect Dis. (2019) 219:1356–63. doi: 10.1093/infdis/jiy675
21. McMurray, DN, Loomis, SA, Casazza, LJ, Rey, H, Miranda, R, et al. Development of impaired cell-mediated immunity in mild and moderate malnutrition. Am J Clin Nutr. (1981) 34:68–77. doi: 10.1093/ajcn/34.1.68
22. Martin, SJ, and Sabina, EP. Malnutrition and associated disorders in tuberculosis and its therapy. J Diet Suppl. (2019) 16:602–10. doi: 10.1080/19390211.2018.1472165
23. Choi, H, Yoo, JE, Han, K, Choi, W, Rhee, SY, Lee, H, et al. Body mass index, diabetes, and risk of tuberculosis: a retrospective cohort study. Front Nutr. (2021) 8:739766. doi: 10.3389/fnut.2021.739766
24. Lönnroth, K, Williams, BG, Cegielski, P, and Dye, C. A consistent log-linear relationship between tuberculosis incidence and body mass index. Int J Epidemiol. (2010) 39:149–55. doi: 10.1093/ije/dyp308
25. Bhargava, A, Chatterjee, M, Jain, Y, Chatterjee, B, Kataria, A, Bhargava, M, et al. Nutritional status of adult patients with pulmonary tuberculosis in rural Central India and its association with mortality. PLoS One. (2013) 8:e77979. doi: 10.1371/journal.pone.0077979
26. Yen, YF, Chuang, PH, Yen, MY, Lin, SY, Chuang, P, Yuan, MJ, et al. Association of body mass index with tuberculosis mortality: a population-based follow-up study. Medicine (Baltimore). (2016) 95:e2300. doi: 10.1097/MD.0000000000002300
27. Rao, VG, Bhat, J, Yadav, R, Sharma, RK, and Muniyandi, M. A comparative study of the socio-economic risk factors for pulmonary tuberculosis in the Saharia tribe of Madhya Pradesh, India. Trans R Soc Trop Med Hyg. (2018) 112:272–8. doi: 10.1093/trstmh/try052
28. Atal Bihari Vajpayee Institute of Good Governance & Policy Analysis. Study of malnutrition among under-6 children of Sheopur district with special focus on Saharia tribe Bhopal, Madhya Pradesh. (2018). Available at: https://aiggpa.mp.gov.in/uploads/project/Study_Report-Study_of_malnutrition_among_under-6_children_of_Sheopur_district_with_special_focus_on_Saharia_tribe.pdf (Accessed March 29, 2023).
29. Adilo, TM. Determinants of TB stigma, and its effects on health care seeking behaviour and treatment adherence among TB patients in Addis Ababa, Ethiopia. EC Microbiol. (2017) 12:37–51.
30. Inghammar, M, Ekbom, A, Engström, G, Ljungberg, B, Romanus, V, Löfdahl, CG, et al. COPD and the risk of tuberculosis – a population-based cohort study. PLoS One. (2010) 5:e10138. doi: 10.1371/journal.pone.0010138
31. Yakar, HI, Gunen, H, Pehlivan, E, and Aydogan, S. The role of tuberculosis in COPD. Int J Chron Obstruct Pulmon Dis. (2017) 12:323–9. doi: 10.2147/COPD.S116086
32. Gudi, N, Mahmood, A, Roy, MP, Ravishankar,, Nayak, P, and Verma, A. Burden of COPD among population above 30 years in India: protocol for a systematic review and proposed meta-analysis. Can J Respir Ther. (2021) 57:14–7. doi: 10.29390/cjrt-2020-040
33. Postma, DS, Bush, A, and van den Berge, M. Risk factors and early origins of chronic obstructive pulmonary disease. Lancet. (2015) 385:899–909. doi: 10.1016/S0140-6736(14)60446-3
34. Yang, IA, Jenkins, CR, and Salvi, SS. Chronic obstructive pulmonary disease in never-smokers: risk factors, pathogenesis, and implications for prevention and treatment. Lancet Respir Med. (2022) 10:497–511. doi: 10.1016/S2213-2600(21)00506-3
35. Smith, KR, and Pillarisetti, A. Household air pollution from solid cookfuels and its effects on health In: CN Mock, R Nugent, O Kobusingye, and KR Smith, et al., editors. Injury prevention and environmental health. Washington, DC: The International Bank for Reconstruction and Development, The World Bank (2017).
36. Raju, S, Siddharthan, T, and McCormack, MC. Indoor air pollution and respiratory health. Clin Chest Med. (2020) 41:825–43. doi: 10.1016/j.ccm.2020.08.014
37. Qiu, AY, Leng, S, McCormack, M, Peden, DB, and Sood, A. Lung effects of household air pollution. J Allergy Clin Immunol Pract. (2022) 10:2807–19. doi: 10.1016/j.jaip.2022.08.031
38. Gordon, SB, Bruce, NG, Grigg, J, Hibberd, PL, Kurmi, OP, Lam, KBH, et al. Respiratory risks from household air pollution in low and middle income countries. Lancet Respir Med. (2014) 2:823–60. doi: 10.1016/S2213-2600(14)70168-7
39. Biswas, M, Pranav, PK, and Nag, PK. Effect on pulmonary functions of dust exposed rice mill workers in comparison to an unexposed population. Work. (2023) 74:945–53. doi: 10.3233/WOR-205146
40. Singh, SK, Nishith, SD, Tandon, GS, Shukla, N, and Saxena, SK. Some observations on pulmonary function tests in rice mill workers. Indian J Physiol Pharmacol. (1988) 32:152–7.
41. Salvi, SS, and Barnes, PJ. Chronic obstructive pulmonary disease in non-smokers. Lancet. (2009) 374:733–43. doi: 10.1016/S0140-6736(09)61303-9
42. Park, HY, Kang, D, Shin, SH, Choi, H, Jang, SH, Lee, CH, et al. Pulmonary tuberculosis and the incidence of lung cancer among patients with chronic obstructive pulmonary disease. Ann Am Thorac Soc. (2022) 19:640–8. doi: 10.1513/AnnalsATS.202010-1240OC
43. Deiss, RG, Rodwell, TC, and Garfein, RS. Tuberculosis and drug use: review and update (2009) 48:72–82. doi: 10.1086/594126
44. Necho, M, Tsehay, M, Seid, M, Zenebe, Y, Belete, A, Gelaye, H, et al. Prevalence and associated factors for alcohol use disorder among tuberculosis patients: a systematic review and meta-analysis study. Subst Abuse Treat Prev Policy (2021) 16:2. doi: 10.1186/s13011-020-00335-w
45. Qiu, F, Liang, CL, Liu, H, Zeng, YQ, Hou, S, Huang, S, et al. Impacts of cigarette smoking on immune responsiveness: up and down or upside down?. Oncotarget. (2017) 8:268–84. doi: 10.18632/oncotarget.13613
46. Simou, E, Britton, J, and Leonardi-Bee, J. Alcohol consumption and risk of tuberculosis: a systematic review and meta-analysis. Int J Tuberc Lung Dis. (2018) 22:1277–85. doi: 10.5588/ijtld.18.0092
47. Imtiaz, S, Shield, KD, Roerecke, M, Samokhvalov, AV, Lönnroth, K, and Rehm, J. Alcohol consumption as a risk factor for tuberculosis: meta-analyses and burden of disease. Eur Respir J. (2017) 50:1700216. doi: 10.1183/13993003.00216-2017
48. Rehm, J, Samokhvalov, AV, Neuman, MG, Room, R, Parry, C, Lönnroth, K, et al. The association between alcohol use, alcohol use disorders and tuberculosis (TB). A systematic review. BMC Public Health. (2009) 9:450. doi: 10.1186/1471-2458-9-450
49. Weiangkham, D, Umnuaypornlert, A, Saokaew, S, Prommongkol, S, and Ponmark, J. Effect of alcohol consumption on relapse outcomes among tuberculosis patients: a systematic review and meta-analysis. Front Public Health. (2022) 10:962809. doi: 10.3389/fpubh.2022.962809
50. Kim, J, Rana, S, Lee, W, Haque, SE, and Yoon, JH. How the bidi tobacco industry harms child-workers: results from a walk-through and quantitative survey. Saf Health Work. (2020) 11:143–51. doi: 10.1016/j.shaw.2020.02.002
51. Vonasek, BJ, Radtke, KK, Vaz, P, Buck, WC, Chabala, C, McCollum, ED, et al. Tuberculosis in children with severe acute malnutrition. Expert Rev Respir Med. (2022) 16:273–84. doi: 10.1080/17476348.2022.2043747
52. Basa, S, and Venkatesh, S. Patient and healthcare system delays in the start of pulmonary tuberculosis treatment among tribal patients registered under DOTS, Odisha. J Clin Diagn Res. (2016) 10:Lc21-Lc24. doi: 10.7860/JCDR/2016/20136.8567
53. Muniyandi, M, Rao, VG, Bhat, J, Yadav, R, Sharma, RK, and Bhondeley, MK. Health literacy on tuberculosis amongst vulnerable segment of population: special reference to Saharia tribe in Central India. Indian J Med Res. (2015) 141:640–7. doi: 10.4103/0971-5916.159566
54. Muture, BN, Keraka, MN, Kimuu, PK, Kabiru, EW, Ombeka, VO, and Oguya, F. Factors associated with default from treatment among tuberculosis patients in Nairobi province, Kenya: a case control study. BMC Public Health. (2011) 11:696. doi: 10.1186/1471-2458-11-696
55. Mishra, P, Sharma, RK, Yadav, R, Rao, VG, Nigam, S, Lingala, MA, et al. Reasons for loss to follow-up (LTFU) of pulmonary TB (PTB) patients: A qualitative study among Saharia, a particularly vulnerable tribal group of Madhya Pradesh, India. PLoS One. (2021) 16:e0261152. doi: 10.1371/journal.pone.0261152
56. Yadav, J, John, D, and Menon, G. Out of pocket expenditure on tuberculosis in India: do households face hardship financing? Indian J Tuberc. (2019) 66:448–60. doi: 10.1016/j.ijtb.2019.02.016
57. Prasad, BM, Tripathy, JP, Muraleedharan, VR, and Tonsing, J. Rising catastrophic expenditure on households due to tuberculosis: is India moving away from the END-TB goal? Front Public Health. (2021) 9:614466. doi: 10.3389/fpubh.2021.614466
58. Directorate General of Health Services Ministry of Health and Family Welfare Government of India. Indian public health standard (IPHS) community health centres level. Available at: http://nhmmp.gov.in/NHM_Old/nrhm/draft%20iphs.pdf (Accessed March 30, 2023).
59. Cramm, JM, Koolman, X, Møller, V, and Nieboer, AP. Socio-economic status and self-reported tuberculosis: a multilevel analysis in a low-income township in the Eastern Cape, South Africa. J Public Health Afr. (2011). 2:e34. doi: 10.4081/jphia.2011.e34
60. Nidoi, J, Muttamba, W, Walusimbi, S, Imoko, JF, Lochoro, P, Ictho, J, et al. Impact of socio-economic factors on Tuberculosis treatment outcomes in north-eastern Uganda: a mixed methods study. BMC Public Health. (2021) 21:2167. doi: 10.1186/s12889-021-12056-1
61. Bishwajit, G, Ide, S, and Ghosh, S. Social determinants of infectious diseases in South Asia. Int Sch Res Notices. (2014) 2014:135243:1–10. doi: 10.1155/2014/135243
62. Atal Bihari Vajpayee Institute of Good Governance & Policy Analysis. Tribal health in Madhya Pradesh. A road map. Available at: http://aiggpa.mp.gov.in/uploads/project/tribal_health.pdf (Accessed August 14, 2023).
63. Hindustan Times. (2017). Available at: https://www.hindustantimes.com/bhopal/put-o-by-faulty-designs-tribals-in-mp-turn-govt-toilets-into-storerooms/story-IXP4buUyuB9Y8iJDhGYaWI.html
64. Shetty, N, Shemko, M, Vaz, M, and D'Souza, G. An epidemiological evaluation of risk factors for tuberculosis in South India: a matched case control study. Int J Tuberc Lung Dis. (2006) 10:80–6.
65. Nigam, S, Sharma, RK, Yadav, R, Rao, VG, Mishra, P, Lingala, MA, et al. Experiences and needs of patients with MDR/XDR-TB: a qualitative study among Saharia tribe in Madhya Pradesh, Central India. BMJ Open. (2021) 11:e044698. doi: 10.1136/bmjopen-2020-044698
66. von Haaren, P, and Klonner, S. Lessons learned? Intended and unintended effects of India's second-generation maternal cash transfer scheme. Health Econ. (2021) 30:2468–86. doi: 10.1002/hec.4390
67. Minstry of Women and Child Development. Government of India. Umbrella ICDS. Available at: https://wcd.nic.in/schemes-listing/2404 (Accessed March 30, 2023).
68. Challa, S. Innovative way to combat malnutrition in MP. Buisness line. (2022). Available at: https://www.thehindubusinessline.com/profile/author/Sreekar--Challa-15797/ (Accessed on 30 March 2023).
69. Central TB Division, Governemnt of India National strategic plan for TB: 2017–25 elimination by 2025 (2017). Available at: https://tbcindia.gov.in/WriteReadData/National%20Strategic%20Plan%202017-25.pdf
70. Ministry of Petrolium and Natural Gas, Government of India. Pradhan Mantri Ujjwala Yojana 2.0. Avaialbe at: https://www.pmuy.gov.in/about.html (Accessed March 30, 2023).
71. Nazar, GP, Chang, KC, Srivastava, S, Pearce, N, Karan, A, and Millett, C. Impact of India's National Tobacco Control Programme on bidi and cigarette consumption: a difference-in-differences analysis. Tob Control. (2020) 29:103–10. doi: 10.1136/tobaccocontrol-2018-054621
72. Lahariya, C. Health & Wellness Centers to strengthen primary health care in India: concept, progress and ways forward. Indian J Pediatr. (2020) 87:916–29. doi: 10.1007/s12098-020-03359-z
73. Patel, K, Kalpana, P, Trivedi, P, Yasobant, S, and Saxena, D. Assessment of water, sanitation and hygiene in HCFs: which tool to follow? Rev Environ Health. (2019) 34:435–40. doi: 10.1515/reveh-2019-0001
74. Singh, P, Shah, M, and Bruckner, TA. Child undernutrition following the introduction of a large-scale toilet construction campaign in India. J Nutr. (2021) 151:2455–64. doi: 10.1093/jn/nxab150
75. Shankar, PS. Viewpoint on tuberculosis in elderly in India. Indian J Tuberc. (2022) 69:S198–201. doi: 10.1016/j.ijtb.2022.10.004
76. Feleke, BE, Feleke, TE, and Biadglegne, F. Nutritional status of tuberculosis patients, a comparative cross-sectional study. BMC Pulm Med. (2019) 19:182. doi: 10.1186/s12890-019-0953-0
77. Bauer, J, Biolo, G, Cederholm, T, Cesari, M, Cruz-Jentoft, AJ, Morley, JE, et al. Evidence-based recommendations for optimal dietary protein intake in older people: a position paper from the PROT-AGE Study Group. J Am Med Dir Assoc. (2013) 14:542–59. doi: 10.1016/j.jamda.2013.05.021
78. Arora, M, Datta, P, Barman, A, Sinha, P, Munish, VG, Bahl, D, et al. The Indian bidi industry: trends in employment and wage differentials. Front Public Health. (2020) 8:572638. doi: 10.3389/fpubh.2020.572638
79. Ministry of Commerce & Industry, Government of India. Economic Burden of Tobacco Related Diseases in India (2022). Available at: https://pqars.nic.in/annex/256/AU370.pdf (Accessed March 30, 2023).
Keywords: malnutrition, public health, Saharia, tobacco, tuberculosis, catastrophic expenditure
Citation: Gupta P, Singh P, Das A and Kumar R (2023) Determinants of tuberculosis: an example of high tuberculosis burden in the Saharia tribe. Front. Public Health. 11:1226980. doi: 10.3389/fpubh.2023.1226980
Edited by:
P. Bernard Fourie, University of Pretoria, South AfricaReviewed by:
Melese Abate Reta, University of Pretoria, South AfricaMariana Araújo-Pereira, Gonçalo Moniz Institute (IGM), Brazil
Copyright © 2023 Gupta, Singh, Das and Kumar. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ravindra Kumar, cmF2aW5kcmEua3VtQGljbXIuZ292Lmlu
 Parul Gupta
Parul Gupta Pushpendra Singh
Pushpendra Singh Ravindra Kumar
Ravindra Kumar