
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health , 12 October 2023
Sec. Aging and Public Health
Volume 11 - 2023 | https://doi.org/10.3389/fpubh.2023.1226642
This article is part of the Research Topic Molecular and Physiological Aspects of Sarcopenia in the Older Person: Mechanisms, Diagnostics and Therapy View all 12 articles
Background: While the potential of physical performance tests as screening tools for sarcopenia is evident, limited information on relevant reference values for sarcopenia detection. In this study, we aimed to establish the prospective relationship between physical performance tests, including time up and go (TUG), functional reach (FR), gait speed (GS), and hand grip strength (HGS) with five-year sarcopenia risk and to determine suitable cut-off values for screening activities.
Method: This was a prospective study utilizing data from the Malaysian Elders Longitudinal Research (MELoR) study, which involved community-dwelling older adults aged 55 years and above at recruitment. Baseline (2013–2015) and wave 3 (2019) data were analyzed. Sarcopenia risk was determined using the strength, assistance walking, rising from a chair, climbing stairs, and falls (SARC-F) tool, with SARC-F ≥ 4 indicating sarcopenia. Baseline physical performance test scores were dichotomized using ROC-determined cut-offs.
Result: Data were available from 774 participants with mean age of 68.13 (SD = 7.13) years, 56.7% women. Cut-offs values for reduced GS, TUG, FR, and HGS were: <0.7 m/s (72.9% sensitivity and 53% specificity), >11.5 s (74.2%; 57.2%), <22.5 cm (73%; 54.2%) and HGS male <22 kg (70.0%; 26.7%) and female <17 kg (70.0%; 20.3%) respectively. Except for FR = 1.76 (1.01–3.06), GS = 2.29 (1.29–4.06), and TUG = 1.77 (1.00–3.13) were associated with increased sarcopenia risk after adjustments for baseline demographics and sarcopenia.
Conclusion: The defined cut-off values may be useful for the early detection of five-year sarcopenia risk in clinical and community settings. Despite HGS being a commonly used test to assess strength capacity in older adults, we advocate alternative strength measures, such as the sit-to-stand test, to be included in the assessment. Future studies should incorporate imaging modalities in the classification of sarcopenia to corroborate current study findings.
Sarcopenia has been reported in up to 29 percent of community-dwelling older persons worldwide, though prevalence varies according to definitions, study setting, and population selection (1). The prevalence of sarcopenia is higher among nursing home residents with a 33 percent prevalence previously reported (2, 3). Among older persons with disabilities or those who receive rehabilitation, the prevalence rises to 78 percent (4, 5). The highest prevalence of sarcopenia has been reported in low- and middle-income countries (LMICs) (6) with a 7 to 44 percent prevalence reported in Malaysia (7).
Sarcopenia negatively impacts afflicted older adults’ quality of life. The reduction in muscle quality and quantity leads to decreased mobility, and in the longer term, increased dependency. Moreover, sarcopenia has been recognized as an independent condition by the World Health Organization through its listing in the International Classification of Diseases ICD-10 suggesting the need for early prevention and management strategies (8). Loss of functional capacity in older adults manifests as greater difficulties in completing basic tasks such as walking at a regular pace, loss of muscle strength, and mobility impairments. Poor physical performance is associated with sarcopenia (9–11), frailty (12, 13), and cognitive impairment (14–16).
While sarcopenia is a common age-related issue with calls for opportunistic screening in the primary care setting (17), the availability of published cut-off scores for physical performance tests commonly used to predict sarcopenia remains limited. Further, healthcare practitioners currently lack the knowledge or training necessary to identify and manage physical capacity losses as people age (18). Previous studies have utilized short physical performance battery (SPPB), hand grip strength (HGS), and timed up-and-go TUG tests to predict the risk of sarcopenia (11, 19). Poor physical performance in older persons is also related to adverse outcomes in older persons such as falls (12, 20) disability (21) and poor quality of life (22).
In the Asian population, physical performance test cut-off values are largely determined from published studies conducted in the East Asian population (23). Further research from other parts of the continent is needed. In addition, previous studies have addressed cross-sectional detection of the presence of sarcopenia rather than prediction of future risk of sarcopenia. Thus, in this study, we sought to evaluate and establish the predictive ability of the prospective relationship between physical performance tests, including time up and go (TUG), functional reach (FR), gait speed (GS), and hand grip strength (HGS) with five-year sarcopenia for adults aged 55 years and over in Malaysia, using newly established cut-off values. We formulated a hypothesis that the physical performance tests (HGS, TUG, GS, and FR) could accurately predict the risk of sarcopenia after 5-years of follow-up.
This prospective observational study utilized baseline (2013 to 2015) and wave 3 follow-up (2019) data from the Malaysian Elders and Longitudinal Research (MELoR) study. The MELoR study is now the Transforming Cognitive Frailty to Later Life Self-sufficiency (AGELESS) study, which was funded by the Ministry of Higher Education Malaysia Long Term Research Grant Scheme (LR005-2019) LRGS/1/2019/UM//1/1.
The study population comprised community-dwelling individuals aged 55 years and above identified from the electoral rolls of three neighboring parliamentary constituencies using simple stratified sampling. Further details on recruitment strategies for the MELoR study have been published elsewhere (24). Baseline measurements of physical performance and potential influencing factors were utilized in this study. A total of 1,311 participants (n = 1,311) were initially collected for this study at the baseline. Following a 5-year follow-up period, 537 participants were lost to follow-up, declined or died. Out of the 774 data initially managed for follow-up, 21 were found to be incomplete. We collected a total of 747 complete data entries for analysis. Telephone follow-up was conducted in 2019 by trained interviewers. Sarcopenia outcomes were obtained from the telephone follow-up interviews (Figure 1).
Figure 1 depicts a flowchart of participants and recruitment. The socio-demographic data of age, gender, marital status, medical history, comorbidities, and anthropometric data were collected at baseline (n = 1,311). Weight was measured using a digital scale (TANITA type TBF-400). Height was measured using a calibrated standing stadiometer into the nearest centimeter. The body mass index (BMI) was then calculated by weight divided by the body weight in kilograms with the height in meters (kg/m2). Waist and hip circumference were obtained in the standing position using a measuring tape and the waist-to-hip ratio was calculated by dividing the waist measurements with the hip measurements. Older adults aged 55 years and above, residing in the community, demonstrated the ability to stand independently for at least 1 min without any support, walk 7 meters, and have the capability to get in and out of a chair with or without an assistive device were included in the study. However, older adults who were unable to comprehend and follow the instructions for the physical performance tests, those experiencing acute illnesses, and individuals taking medications that could potentially impact their balance during the assessment were excluded from the study.
In this study, Sarcopenia was determined during telephone follow-up using the SARC-F tool, which consists of the five questions: Strength (S), Assistance walking (A), Rising from a chair (R), Climbing stairs (C), and Falls (F), rated from “not at all” to “extremely difficult” on a scale of 0 to 2. The suggested cut-off for the presence of sarcopenia is four points out of the maximal total score of 10 (25, 26). SARC-F scores were determined both at baseline and at five-year follow-up for all participants. SARC-F at baseline involved the substitution of sex-specific lowest quintile for hand grip strength for strength, as the question was not available for the baseline questionnaire.
A 10-meter walking path (2-meter acceleration, 6-meter walk, and 2-meter deceleration) was used in this study. The participant was asked to walk using their casual walking speed. The stopwatch was started when the foot first crossed the marked acceleration point and stopped when the foot crossed the first marked deceleration point. The time taken was recorded in seconds. The test was then repeated and the mean of two trials was taken as the result (27).
To conduct the TUG test, a wooden solid chair with its seat at a height of 46 cm above the ground was used. The participant was given verbal instruction prior to the test. The stopwatch is started as soon as the participant’s bottom leaves the chair. Participants then walked three meters at their usual walking speed, turned around, and walked back to the chair and sat down. The stopwatch stopped when the participant’s bottom touched the chair once again. The average time (in seconds) of two performances was used as the result (28).
The functional reach test was performed in the standing position. The participant stood against the wall with one arm positioned at 90° of forward flexion with a measuring tape placed at shoulder height. Participant was instructed to maintain their base of support with legs shoulder width apart while trying to reach forward as far as they could. The difference in length between the initial position of the tip of the middle finger (in cm) and the furthest position was considered the FR (29).
To assess HGS, a Jamar™ hand dynamometer (Patterson Medical, United States) was used. Participants were seated with shoulders adducted, elbow flexed to 90 degrees, with the forearm and the wrist maintained in neutral position, while the hand gripping the dynamometer. The best result from the dominant hand was taken as the result for the present study (30).
Statistical analyses were conducted using the Statistical Package for Social Science for Windows, version 2,626 (IBM Corp., Armonk, N.Y., United States). The Independent t-test was used to generate descriptive characteristics for continuous variables while the Chi-squared test was used for categorical variables. The association between physical performance tests and the risk of sarcopenia was assessed using multiple logistic regressions. The physical performance test data were dichotomized based on the outcome value of the receiver operating characteristic curve (ROC) analysis. By categorizing participants as having or not having a risk of sarcopenia at 5 years, this approach creates a plot of sensitivity (true positive rate) vs. 1-specificity (false positive rate) at each test value. The test value with the highest sensitivity and specificity was then selected as a cut-off to classify whether the participant has the condition (31, 32). The SARC-F cumulative incidence was calculated by dividing new cases of SARC-F during the follow-up period by the number of participants at risk in the population at baseline. The incidence rate was obtained by dividing new cases of SARC-F by the total-person-time observed between the two assessments.
Baseline and follow-up SARC-F scores were available for 747 participants. Participants’ baseline characteristics are presented in Table 1. Eighty-six (11.1%) fulfilled the SARC-F cut-off of four or more points and were classified as sarcopenic at baseline while 6.8% (n = 51) women from the total population were categorized as sarcopenia group, mean age (SD) 72.0 ± 6.98, p < 0.001. From the data analysis at follow-up, 632 (84.6%) participants were categorized as normal (SARC-F < 4), and 115 (15.4%) participants were in the sarcopenia category (SARC-F ≥ 4). The mean age for normal group participants was 67.5 ± 6.52 years, and 54.7% (n = 346) were women. The participant’s age range in the sarcopenic group was 70.8 ± 8.84 years, of which 67% (n = 77) were women. There were significant differences in body mass index (BMI), educational level, and presence of diabetes mellitus (DM) between groups (p < 0.001) (Table 1). The five-year incidence of possible sarcopenia according to SARC-F was 17 per 100 person-years.
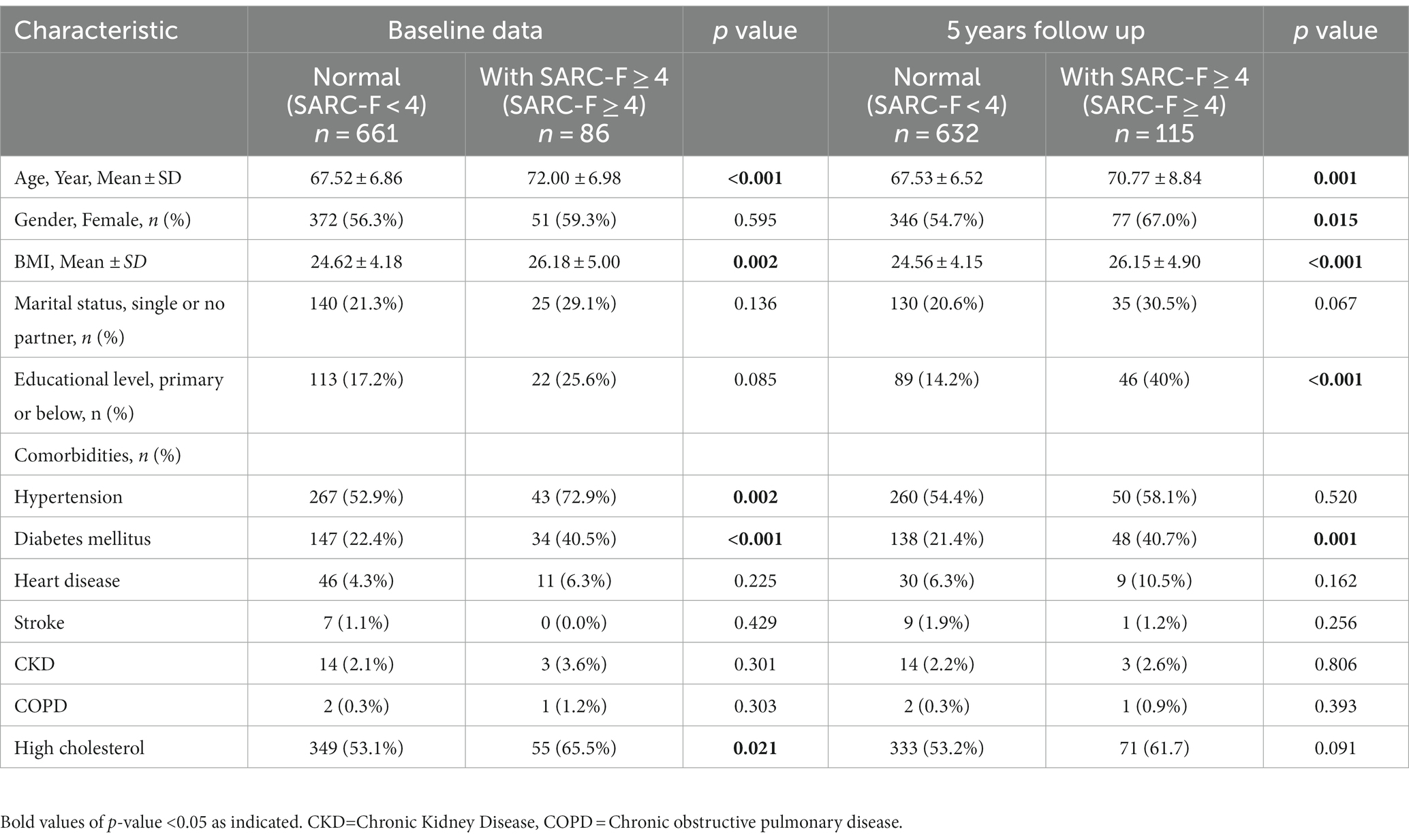
Table 1. Characteristics of participants with SARC-F ≥ 4 and SARC-F < 4 at Baseline and 5 Years follow up (N = 747).
Physical performance among participants with and without sarcopenia in the baseline and after five years of follow-up is summarized in Table 2. The TUG, GS, and FR were significantly correlated with the SARC-F scores (p < 0.001) at the baseline and follow-up. However, HGS in this study was not significant in predicting the risk of sarcopenia in both groups (Table 2; Figure 2).
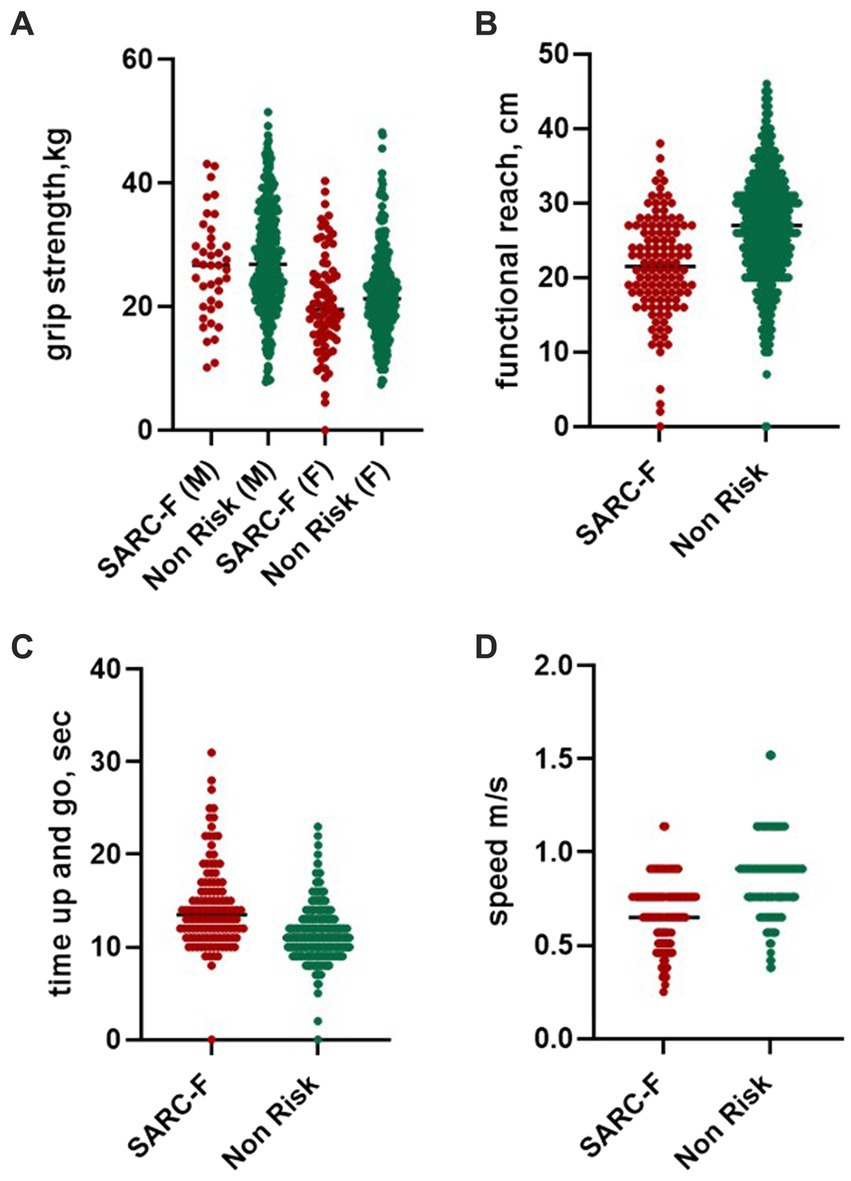
Figure 2. Physical performance score in non-risk participants and with a SARC-F score of 4 and above. Graph figure of physical performance in participants with SARC-F ≥ 4. SARC-F: S=Strength, A = Assistance in walking, R = Rising from a chair, C=Climbing stairs, F = Falls history.
The area under the ROC curve (AUC) was used to assess the performance of baseline GS, TUG, HGS, and FR in predicting probable sarcopenia in 5 years. The reference values set for GS were ≤ 0.7 m/s (72.9% sensitivity and 53% specificity). Meanwhile, ≥11.5 s was set for TUG (74.2% sensitivity and 57.2% specificity). We proposed a cut-off value of ≤22.5 cm for FR (73% sensitivity and 54.2% specificity). The cut-off values for male and female HGS proposed were < 22 kg and < 17 kg, respectively, (70% sensitivity for both genders, 26.7% specificity for male HGS, and 20.3% for female HGS) (Table 3).
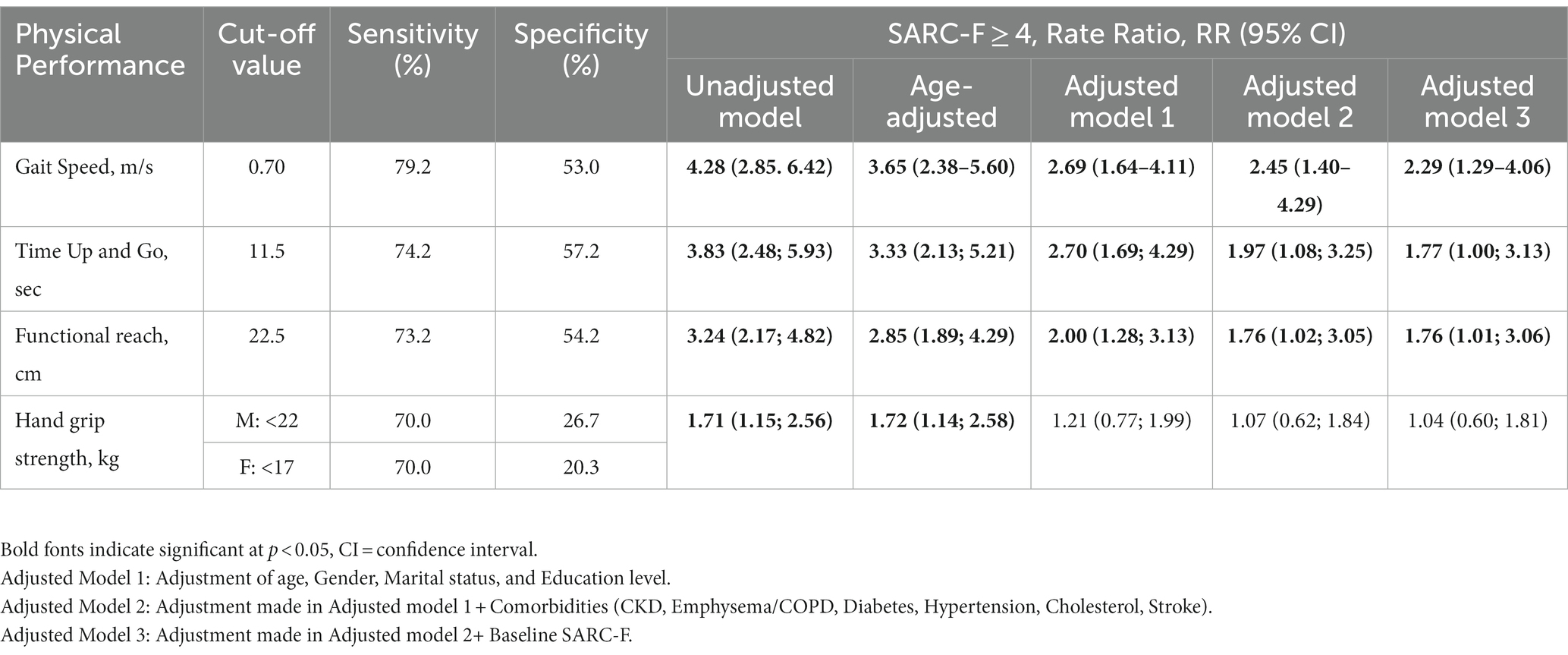
Table 3. Rate ratio of SARC-F ≥ 4 at 5 years follow up among older people with poor physical performance measured using different type of test.
The association was significant for TUG, GS, and FR even after adjustment for baseline sarcopenia except for HGS. The rate Ratio (RR) of sarcopenia at five years follow-up among older people with poor physical performance was measured by an unadjusted model, adjusted Model 1 (model adjusted for age, gender, marital status, and educational level), adjusted Model 2 [adjustment made in adjusted model 1 + comorbidities (chronic kidney disease (CKD), emphysema/chronic objective pulmonary disease (COPD), diabetes, hypertension, cholesterol, stroke)] and adjusted Model 3 (adjustment made in adjusted model 2 + baseline SARC-F) as depicted in Table 3. The unadjusted model of GS was 4.28 (2.85; 6.42); TUG was 3.83 (2.48; 5.93) meanwhile FR 3.24 (2.17;4.82) and HGS 1.71 (1.15; 2.56). The HGS was the only parameter that was not significant after being adjusted with models 1, 2, and 3: 1.21 (0.77;1.99), 1.07 (0.62;1.84), and 1.04 (0.60;1.81) consecutively (Table 3).
Aging is associated with balance impairment, and it is estimated that 13% of older people ages 65–69 and 46% of older adults ages 85 and above self-report having balance deficits (33). Lack of balance, unsteadiness while walking, and weak muscles are the main internal factors that increase the risk of falling in older adults (34). Older individuals with sarcopenia often experience weakened muscles, which can significantly impact their balance while walking. Early detection of sarcopenia is crucial in mitigating the progression of muscle loss and maintaining better health outcomes for older individuals. Implementing straightforward physical performance assessments in clinical practice becomes imperative to effectively prevent the occurrence of sarcopenia. Knowing the cut-off value of physical performance will empower health practitioners to establish targeted sarcopenia prevention programs effectively. Research conducted by Pepera et al. in 2021 revealed compelling evidence regarding the efficacy of a two-month multicomponent exercise training (MCEP) program in enhancing mobility among older adults. This comprehensive exercise regimen encompasses a combination of balance and muscle-strengthening exercises, strategically designed to amplify both balance performance and gait ability. Sarcopenia notably exerted a significant impact on these aspects in older adults.
This study identified the cut-off values for physical performance tests to predict the risk of sarcopenia in 5-years among individuals aged 55 years and over in Malaysia. The proposed cut-off value of gait speed was at ≤0.7 m/s, ≤11.5 s for TUG, and < 22.5 cm for FR. The cut-off of sex-specific hand grip strength for men was <22 kg women was <17 kg. Several studies have been conducted to predict probable sarcopenia utilizing SARC-F but were focused mainly on studying prevalence (35–39) and were not focused on the physical performance’s cut off values to predict sarcopenia risk in the Southeast Asian population.
The ability of TUG to predict sarcopenia has been mentioned in one study (11) with the cut-off set at 10.85 s (sensitivity of 67% and specificity of 88.7%). This result was slightly different from the present study which set the cut-off at ≤11.5 s (sensitivity of 74.2% and specificity of 57.2%). As physical performance is correlated with physiological and anthropometric measurements such as height and limb length that vary according to ethnicity, body morphology differences between European and Asian populations probably play a role in the dissimilarity of step length and walking speed resulting in the majority of the older Asian population having slower TUG (40).
In terms of gait speed, the cut-off point set in this study ≤0.7 m/s (sensitivity 79.2% and specificity 53%) was lower than the value set by the Asian Working Group of Sarcopenia (AWGS) which is <0.8 m/s (41). However, this cut-off was within a range value presented by Cawthon in his study which set the cut-off points in walking speed of 0.60 m/s and 0.75 m/s discriminated older adults with mobility limitation related to sarcopenia (42). Another study by Kang et al. (43) denoted healthy older adult walking speed was 1.23 ± 0.26 m/s, which is 0.08 m/s faster compared to sarcopenic people (1.15 ± 0.25 m/s, value of p <0.001).
In this study, the specificity for HGS cut-offs was quite low. This cut-off value of HGS was the lowest among the cut-off set by other working definition sarcopenia such as AWGS (<26 kg for men and < 18 kg for women) and EWGSOP (<30 kg for men and < 20 kg for women). The lack of association between HGS and sarcopenia defined using SARC-F at 5-year follow-up may be attributed to the limitation of SARC-F. A previous study has, however, suggested that SARC-F showed a high level of overlap with established definitions of sarcopenia of up to 54% with the IWGS definition (36). In addition, in the more recent study, it was suggested that SARC-F is better suited to rule out sarcopenia in case-finding. Since HGS just measures upper body strength, its value in determining whole-body strength is probably limited (44). However, according to research conducted by Laudisio et al. (45), a correlation exists between muscle strength, as quantified through handgrip strength, and the overall physical and mental well-being of older adults. Furthermore, enhancing muscle performance has the potential to contribute to an improved quality of life for this population.
This study represents the first longitudinal investigation into the relationship between physical performance measures (PPMs) including GS, TUG, HGS, and FR, and adverse health namely Sarcopenia in older Malaysian adults. However, this study lacked objective measurements of body composition and imaging (i.e., dual-energy X-ray absorptiometry and magnetic resonance imaging) to classify sarcopenia, which may have led to inaccuracies. Various imaging techniques, encompassing both qualitative and quantitative approaches, are utilized for evaluating muscle mass and body composition. These methods include computed tomography (CT), nuclear magnetic resonance (MRI), dual-energy X-ray absorptiometry (DXA), bioelectrical impedance analysis (BIA), and muscle ultrasound. CT and MRI are regarded as the benchmark due to their ability to provide accurate assessments of distinct body tissues, but a consensus regarding the specific cutoff values for defining sarcopenia remains absent (46). Secondly, the MELoR study targeted Malaysian adults living in an urban area which will limit the generalization to those living in rural areas whose occupations and lifestyles may be different. Future studies should include older people living in rural areas and compare their performance to evaluate whether geographical factors may affect the results. Finally, no physical assessment was conducted during the follow-up visit. Hence, we were not able to evaluate the influence of changes in physical performance on sarcopenia. Nevertheless, this study revealed the temporal associations between physical performance tests on five-year sarcopenia risk in older adults in Malaysia.
This study proposed the cut-off values for physical performance tests that may be useful for early detection of sarcopenia risk within the older Malaysian population. Future studies should seek to confirm our findings using more accurate sarcopenia measurements which should ideally include imaging modalities. In addition, the value of screening for five-year sarcopenia risk using physical performance tests should also be evaluated.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving humans were approved by the research ethics committee of the university of Malaya. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required from the participants or the participants’ legal guardians/next of kin in accordance with the national legislation and institutional requirements.
IM, SM, DKAS, and MPT conceived the study, contributed to the study design, obtained the funding for the study and were responsible for the conduct of the study. IM was involved in data collection. SM and MPT contributed to data analysis. All authors contributed to the writing of the manuscript and approved the final submitted version.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Meier, NF, and Lee, DC. Physical activity and sarcopenia in older adults. Aging Clin Exp Res. (2020) 32:1675–87. doi: 10.1007/s40520-019-01371-8
2. Beaudart, C, McCloskey, E, Bruyere, O, Cesari, M, Rolland, Y, Rizzoli, R, et al. Sarcopenia in daily practice: assessment and management. BMC Geriatr. (2016) 16:170. doi: 10.1186/s12877-016-0349-4
3. Cruz-Jentoft, AJ, Landi, F, Schneider, SM, Zúñiga, C, Arai, H, Boirie, Y, et al. Prevalence of and interventions for sarcopenia in ageing adults: a systematic review. Report of the international sarcopenia initiative (EWGSOP and IWGS). Age Ageing. (2014) 43:748–59. doi: 10.1093/ageing/afu115
4. Doi, T, Tsutsumimoto, K, Ishii, H, Nakakubo, S, Kurita, S, and Shimada, H. Association between sarcopenia, its defining indices, and driving cessation in older adults. J Nutr Health Aging. (2021) 25:462–6. doi: 10.1007/s12603-020-1554-6
5. Shimokata, H, Shimada, H, Satake, S, Endo, N, Shibasaki, K, Ogawa, S, et al. Chapter 2 epidemiology of sarcopenia. Geriatr Gerontol Int. (2018) 18:13–22. doi: 10.1111/ggi.13320
6. Smith, L, Jacob, L, Barnett, Y, Butler, LT, Shin, JI, López-Sánchez, GF, et al. Association between food insecurity and sarcopenia among adults aged ≥65 years in low- and middle-income countries. Nutrients. (2021) 13. doi: 10.3390/nu13061879
7. Af, ML, Clark, B, Shahar, S, Abdul Manaf, Z, DKA, Singh, Lau, H, et al. Characterisation of sarcopenia in Malaysian elders using the Asian working group on sarcopenia and the European working group on sarcopenia in older people consensus definitions introduction figure 1. Prevalence of sarcopenia among Malaysian elderly according to Asian working Group for Sarcopenia References (2015).
8. Anker, S, Morley, J, and von Haehling, S. Welcome to the ICD-10 code for sarcopenia. J Cachexia Sarcopenia Muscle. (2016) 7:512–4. doi: 10.1002/jcsm.12147
9. Bahat, G, Kilic, C, Eris, S, and Karan, MA. Power versus sarcopenia: associations with functionality and physical performance measures. J Nutr Health Aging. (2021) 25:13–7. doi: 10.1007/s12603-020-1544-8
10. Frisoli, A, Paes, AT, Borges, J, Ingham, SM, Cartocci, MM, Lima, E, et al. The association between low lean mass and osteoporosis increases the risk of weakness, poor physical performance and frailty in Brazilian older adults: data from SARCOS study. Eur J Clin Nutr. (2021) 75:446–55. doi: 10.1038/s41430-020-00753-w
11. Martinez, BP, Gomes, IB, de Oliveira, CS, Ramos, IR, Rocha, MDM, Júnior, LAF, et al. Accuracy of the timed up and go test for predicting sarcopenia in elderly hospitalized patients. Clinics. (2015) 70:369–72. doi: 10.6061/clinics/2015(05)11
12. Binotto, MA, Lenardt, MH, and Rodríguez-Martínez, MDC. Physical frailty and gait speed in community elderly: a systematic review. Rev Esc Enferm USP. (2018) 52:e03392. doi: 10.1590/s1980-220x2017028703392
13. Menezes, K, Auger, C, Barbosa, JFS, Gomes, CS, Menezes, WRS, and Guerra, RO. Trajectories and predictors of functional capacity decline in older adults from a Brazilian northeastern hospital. J Geriatr Phys Ther. (2021) 44:82–7. doi: 10.1519/jpt.0000000000000255
14. Chang, KV, Hsu, TH, Wu, WT, Huang, KC, and Han, DS. Association between sarcopenia and cognitive impairment: a systematic review and Meta-analysis. J Am Med Dir Assoc. (2016) 17:1164.e7–1164.e15. doi: 10.1016/j.jamda.2016.09.013
15. Peng, TC, Chen, WL, Wu, LW, Chang, YW, and Kao, TW. Sarcopenia and cognitive impairment: a systematic review and meta-analysis. Clin Nutr. (2020) 39:2695–701. doi: 10.1016/j.clnu.2019.12.014
16. Sui, SX, Williams, LJ, Holloway-Kew, KL, Hyde, NK, and Pasco, JA. Skeletal muscle health and cognitive function: a narrative review. Int J Mol Sci. (2020) 22. doi: 10.3390/ijms22010255
17. Lenchik, L, and Boutin, RD. Sarcopenia: beyond muscle atrophy and into the new Frontiers of opportunistic imaging, precision medicine, and machine learning. Semin Musculoskelet Radiol. (2018) 22:307–22. doi: 10.1055/s-0038-1641573
18. Beaudart, C, Rolland, Y, Cruz-Jentoft, AJ, Bauer, JM, Sieber, C, Cooper, C, et al. Assessment of muscle function and physical performance in daily clinical practice: a position paper endorsed by the European Society for Clinical and Economic Aspects of osteoporosis, osteoarthritis and musculoskeletal diseases (ESCEO). Calcif Tissue Int. (2019) 105:1–14. doi: 10.1007/s00223-019-00545-w
19. Choi, KM. Sarcopenia and sarcopenic obesity. Korean J Intern Med. (2016) 31:1054–60. doi: 10.3904/kjim.2016.193
20. Hicks, C, Levinger, P, Menant, JC, Lord, SR, Sachdev, PS, Brodaty, H, et al. Reduced strength, poor balance and concern about falls mediate the relationship between knee pain and fall risk in older people. BMC Geriatr. (2020) 20:94. doi: 10.1186/s12877-020-1487-2
21. Aartolahti, E, Lönnroos, E, Hartikainen, S, and Häkkinen, A. Long-term strength and balance training in prevention of decline in muscle strength and mobility in older adults. Aging Clin Exp Res. (2020) 32:59–66. doi: 10.1007/s40520-019-01155-0
22. Groessl, EJ, Kaplan, RM, Rejeski, WJ, Katula, JA, Glynn, NW, King, AC, et al. Physical activity and performance impact long-term quality of life in older adults at risk for major mobility disability. Am J Prev Med. (2019) 56:141–6. doi: 10.1016/j.amepre.2018.09.006
23. Chen, LK, Liu, LK, Woo, J, Assantachai, P, Auyeung, TW, Bahyah, KS, et al. Sarcopenia in Asia: consensus report of the Asian working Group for Sarcopenia. J Am Med Dir Assoc. (2014) 15:95–101. doi: 10.1016/j.jamda.2013.11.025
24. Alex, D, Khor, HM, Chin, AV, Hairi, NN, Othman, S, Khoo, SPK, et al. Cross-sectional analysis of ethnic differences in fall prevalence in urban dwellers aged 55 years and over in the Malaysian elders longitudinal research study. J BMJ Open. (2018) 8:e019579. doi: 10.1136/bmjopen-2017-019579
25. Nishikawa, H, Asai, A, Fukunishi, S, Takeuchi, T, Goto, M, Ogura, T, et al. Screening tools for sarcopenia. In Vivo. (2021) 35:3001–9. doi: 10.21873/invivo.12595
26. Vidal-Cuellar, C, Mas, G, Ayamamani-Torres, P, Yazawa, T, Rosas-Carrasco, O, and Tello, T. Identification of probable sarcopenia based on SARC-F and SARC-CalF in older adults from a low-resource setting. J Frail Sarcop Falls. (2022) 7:222–30. doi: 10.22540/JFSF-07-222
27. Karpman, C, Lebrasseur, NK, Depew, ZS, Novotny, PJ, and Benzo, RP. Measuring gait speed in the out-patient clinic: methodology and feasibility. Respir Care. (2014) 59:531–7. doi: 10.4187/respcare.02688
28. Ziegl, A, Hayn, D, Kastner, P, Löffler, K, Weidinger, L, Brix, B, et al. Quantitative falls risk assessment in elderly people: results from a clinical study with distance based timed up-and-go test recordings. Physiol Meas. (2020) 41:115006. doi: 10.1088/1361-6579/abc352
29. Scena, S, Steindler, R, Ceci, M, Zuccaro, SM, and Carmeli, E. Computerized functional reach test to measure balance stability in elderly patients with neurological disorders. J Clin Med Res. (2016) 8:715–20. doi: 10.14740/jocmr2652w
30. Abdul Mutalib, S, Mace, M, Seager, C, Burdet, E, Mathiowetz, V, and Goldsmith, N. Modernising grip dynamometry: inter-instrument reliability between GripAble and Jamar. BMC Musculoskelet Disord. (2022) 23:80. doi: 10.1186/s12891-022-05026-0
31. Hajian-Tilaki, K. Receiver operating characteristic (ROC) curve analysis for medical diagnostic test evaluation. Caspian J Intern Med. (2013) 4:627–35.
32. Zweig, MH, and Campbell, G. Receiver-operating characteristic (ROC) plots: a fundamental evaluation tool in clinical medicine. Clin Chem. (1993) 39:561–77. doi: 10.1093/clinchem/39.4.561
33. Osoba, MY, Rao, AK, Agrawal, SK, and Lalwani, AK. Balance and gait in the elderly: a contemporary review. Laryngosc Investig Otolaryngol. (2019) 4:143–53. doi: 10.1002/lio2.252
34. Lacroix, A, Kressig, RW, Muehlbauer, T, Gschwind, YJ, Pfenninger, B, Bruegger, O, et al. Effects of a supervised versus an unsupervised combined balance and strength training program on balance and muscle power in healthy older adults: a randomized controlled trial. Gerontology. (2016) 62:275–88. doi: 10.1159/000442087
35. Bahat, G, Yilmaz, O, Kiliç, C, Oren, MM, and Karan, MA. Performance of SARC-F in regard to sarcopenia definitions muscle mass and functional measures. Berlin: Springer Science and Business Media LLC (2018).
36. Kemmler, W, Sieber, C, Freiberger, E, and von Stengel, S. The SARC-F questionnaire: diagnostic overlap with established sarcopenia definitions in older German men with sarcopenia. Gerontology. (2017) 63:411–6. doi: 10.1159/000477935
37. Malmstrom, TK, Miller, DK, Simonsick, EM, Ferrucci, L, and Morley, JE. SARC-F: a symptom score to predict persons with sarcopenia at risk for poor functional outcomes. J Cachexia Sarcopenia Muscle. (2016) 7:28–36. doi: 10.1002/jcsm.12048
38. Piotrowicz, K, Głuszewska, A, Czesak, J, Fedyk-Łukasik, M, Klimek, E, Sánchez-Rodríguez, D, et al. SARC-F as a case-finding tool for sarcopenia according to the EWGSOP2. National validation and comparison with other diagnostic standards. Aging Clin Exp Res. (2021) 33:1821–9. doi: 10.1007/s40520-020-01782-y
39. Sacar, DE, Kilic, C, Karan, MA, and Bahat, G. Ability of SARC-F to find probable sarcopenia cases in older adults. J Nutr Health Aging. (2021) 25:757–61. doi: 10.1007/s12603-021-1617-3
40. Ibrahim, A, Singh, DKA, and Shahar, S. 'Timed up and Go' test: age, gender and cognitive impairment stratified normative values of older adults. PLoS One. (2017) 12:e0185641. doi: 10.1371/journal.pone.0185641
41. Locquet, M, Beaudart, C, Reginster, J-Y, Petermans, J, and Bruyere, O. Comparison of the performance of five screening methods for sarcopenia. Clin Epidemiol. (2018) 10:71–82. doi: 10.2147/CLEP.S148638
42. Cawthon, PM, Patel, SM, Kritchevsky, SB, Newman, AB, Santanasto, A, Kiel, DP, et al. What cut-point in gait speed best discriminates community-dwelling older adults with mobility complaints from those without? A pooled analysis from the sarcopenia definitions and outcomes consortium. J Gerontol A Biol Sci Med Sci. (2021) 76:e321–7. doi: 10.1093/gerona/glab183
43. Kang, M-G, Kim, K-I, Kang, JK, Kang, S-J, Roh, H-K, and Jung, H-Y. Association between gait speed measured using a wearable device and sarcopenia. Innov Aging. (2019) 3:S885–6. doi: 10.1093/geroni/igz038.3242
44. Bohannon, RW. Grip Strength: An Indispensable Biomarker For Older Adults. Clin Interv Aging. (2019) 14:1681–91. doi: 10.2147/cia.S194543
45. Laudisio, A, Giovannini, S, Finamore, P, Loreti, C, Vannetti, F, Coraci, D, et al. Muscle strength is related to mental and physical quality of life in the oldest old. Arch Gerontol Geriatr. (2020) 89:104109. doi: 10.1016/j.archger.2020.104109
Keywords: sarcopenia, physical performance test, SARC-F, older adults, cut-off value
Citation: Megasari IM, Mat S, Singh DKA and Tan MP (2023) Prospective sarcopenia outcomes associated with physical performance in individuals aged 55 years and over in Malaysia. Front. Public Health. 11:1226642. doi: 10.3389/fpubh.2023.1226642
Received: 22 May 2023; Accepted: 19 September 2023;
Published: 12 October 2023.
Edited by:
Colette Joy Browning, Federation University Australia, AustraliaReviewed by:
Revital Feige Gross Nevo, Independent Researcher, Jerusalem, IsraelCopyright © 2023 Megasari, Mat, Singh and Tan. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Sumaiyah Mat, c3VtYWl5YWgubWF0QHVrbS5lZHUubXk=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.