- 1School of Public Health, Cheeloo College of Medicine, Shandong University, Jinan, China
- 2Department of Poisoning and Occupational Diseases, Emergency Medicine, Qilu Hospital of Shandong University, Cheeloo College of Medicine, Shandong University, Jinan, China
This paper summarizes and analyzes the clinical data of a patient with Occupational hydrogen sulfide poisoning admitted to our hospital on March 4, 2023. On the morning of March 2, 2023, the patient worked at an environmental energy company (waste treatment plant) in Shandong Province for the first time, The job was to flush the sludge from the walls of the sludge treatment tank (anaerobic tank) with a water gun, which can release hydrogen sulfide gas. When the patient was about to start work after entering the tank for about 1 min, he suddenly smelled a harsh and pungent odor, felt dizzy and weak, and then the patient suddenly fainted. After hearing the sound of the patient fainting, the workman waiting at the entrance of the tank immediately called someone to go into the tank and quickly pull the patient out, and sent to the local hospital. In the local hospital, the patient was confused, accompanied by irritability, convulsion and other manifestations, and was treated with sedation and nutritional support. Two days later, the patient’s condition did not improve. For further diagnosis and treatment, the patient was transferred to the Department of Poisoning and Occupational Diseases in our hospital. After comprehensive treatment in our hospital, the patient got better and was discharged. Subsequent reexamination and follow-up showed that the patient recovered well. The work unit of the patient did not provide any personal protective equipment. According to the field investigation after the accident, the pipeline around the sludge treatment tank was blocked by sludge, resulting in a large amount of high concentration of H2S accumulated in the tank, causing the patient to faint soon after entering the tank, and his worker should be in the tank for a short time, and no health abnormalities were found. Hydrogen sulfide has a strong irritation to the human body, which can lead to asphyxia or even death in severe cases. The safety prevention and prevention knowledge of hydrogen sulfide poisoning should be popularized among enterprises and workers to reduce the occurrence of such incidents.
1. Introduction
Hydrogen sulfide, whose chemical formula is H2S, is one of the major toxic gases (1), and has the characteristic odor of rotten eggs (2). H2S can be found in the oil and gas industries. It is used in activities such as food processing, paper mills, and tanneries. H2S could damage one’s eyes, respiratory system and central nervous system when inhaled at a low concentration (3). However, it could cause permanent brain damage at a higher concentration, even death because of a respiratory failure (4, 5). It is the most common cause of occupational gas exposure deaths rank only second to carbon monoxide, particularly in the oil and gas, sanitation and so on (6, 7). The production speed of H2S is very fast, and in a closed environment, such as a car or a small room, it can reach a fatal concentration (7). H2S poisoning is usually related to the operation accidents in the confined space. That is because, in the confined space, due to the limited into the hole and adverse natural ventilation, produce poisonous gas material will be the breakdown and fermentation processes (8). Environmental Protection Agency’s (EPA) toxicological review of hydrogen sulfide reported that multiple occupational exposures led to rapid toxicity and sudden but reversible loss of consciousness, which was called “knockout” (9). At present, there is no antidote for sulfide poisoning, and the treatment is supportive to a great extent (10). No matter the severity of the initial coma, there were no obvious long-term adverse reactions among the survivors (11).
2. Case description
The patient was a male, 46 years old. On the morning of March 2, 2023, he worked in an environmental protection energy company in Shandong Province for the first time, which was a waste treatment power plant. His job was to flush the sludge from the inner wall of the sludge treatment tank (Figure 1, anaerobic tank, 4 m high, 3 m diameter) with a water gun, and the sludge could release hydrogen sulfide gas. According to his and his co-workers, the patient was about to start work after entering the tank for about 1 min, when he suddenly smelt a harsh, pungency smell, and felt dizzy and weak, then the patient suddenly fainted. After hearing the sound of his fainting, the workers waiting at the entrance of the tank immediately called someone to enter the tank and quickly pulled him out, and then sent to the local hospital. At the local hospital, the patient was confused, accompanied by irritability, convulsions and other manifestations, and was treated with sedation (Midazolam and Diprivan) and nutritional support [Structured fat emulsion (20%)/amino acid (16%), glucose injection (13%)]. Two days later (2023.3.4), the patient’s condition did not improve. For further diagnosis and treatment, the patient was transferred to the Department of Poisoning and Occupational Diseases in our hospital. The patient awoke in the ambulance while being transferred to this hospital with gradual improvement in consciousness but no recollection of the events that followed. After investigation, the causes of this accident were as follows: the labor unit of the patient did not provide any personal protective equipment, and the patient only wore an ordinary raincoat into the tank; The pipeline around the sludge treatment tank was blocked by sludge, resulting in the accumulation of a large number of high-concentration hydrogen sulfide gas in the tank, causing the patient to faint soon after entering the tank. Although there is an exhaust fan on the tank wall, the volume of the exhaust fan is too small to have any effect. Due to the very short time in the tank, the worker pulled out the patient immediately after entering the tank, and no health abnormalities were found. He was admitted to our hospital with a “disturbance of consciousness for 2 days,” and physical examination findings were as follows: temperature was 37°C; pulse was 95 times/min; respiratory rate was 18 times/min; blood pressure was 131/79 mmHg; and SPO2 was 96%. The patient had blurred consciousness, poor spirit, and autonomous posture; he was cooperative during cooperation. The skin mucosa of the whole body was not yellow, and the superficial lymph nodes were not large. His bilateral pupils were large and round, reflecting light, and the size of the pupil was 3 mm. There was no cyanosis or congestion in the pharynx. The patient had a soft neck with no resistance, bilateral thorax movement, clear lung sounds when breathing, and no dry and wet rales. The rhythm was normal and there was no pathological murmur in the valve area. The abdomen is soft, there is no tenderness and rebound pain in the whole abdomen, liver, spleen, and ribs, and there is no tapping pain in the liver and kidney areas. No deformity of spine and limbs. The patient had physiological reflex and no pathological reflex. The results of the patient’s blood draw after admission from 2023/3/6 to 2023/3/26, as shown in Table 1, were basically normal except for a higher number of inflammatory cells (neutrophils ratio was high on Day 1 and Day 3, and the total number of white blood cells was high on Day 1), which indicated an inflammatory response in this patient. Magnetic resonance imaging (MRI) after admission (2023/3/6), as shown in Figure 2, patchy long TI and long T2 signal shadows were seen in the left basal ganglia, and T2 FLAIR showed medium-low peripheral hyperintensity with clear boundaries. The left frontal lobe showed a speckle-like long TI and long T2 signal shadow, T2 FLAIR hyperintensity, and DWI isointensity. The examination concluded that abnormal signals in the left basal ganglia, considering softening foci (Figure 2A); There were a few abnormal signals in the left frontal lobe, considering non-specific signals or degenerative lesions around the perivascular space (Figure 2B). And the subsequent reexamination on 2023/3/26 revealed a slight reduction in the extent of the lesion (Figures 2C,D). On CT on 2023/3/6, as shown in Figure 3, there was a little exudation in the lower lobe of the right lung, with localized interstitial changes (Figure 3A), which were relieved on the second examination on 2023/3/26 (Figure 3C). There was localized thickening of the right pleura (Figure 3B), which were also relieved on the second examination (Figure 3D). According to the diagnostic criteria of occupational acute hydrogen sulfide poisoning of the People’s Republic of China (12), the patient had a history of exposure to a large amount of inhaled hydrogen sulfide in a short period of time, and the clinical manifestations of the central nervous system and respiratory system appeared. The on-site labor hygiene investigation also supported the above exposure history, so the patient was diagnosed with occupational acute hydrogen sulfide poisoning. As a consequence, the following management regimen was applied. Dexamethasone (10 mg, ivdrip, qd) was given to reduce the inflammatory reaction, and the drug was discontinued on the 4th day. Salvianolate (200 mg, ivdrip, qd) to improve microcirculation; Torasemide (20 mg, iv, bid) to reduce edema and speed up the excretion of poison; Nalmefene (0.1 mg, iv, bid) to alleviate the symptoms of consciousness disorder and promoting the recovery of consciousness in the patient and was discontinued on Day 3. Flucloxacillin (1 g, ivdrip, q6h) for infection prevention; In addition, he was treated with sedation (Midazolam and Diprivan) and nutritional support [Structured fat emulsion (20%)/amino acid (16%), glucose injection (13%)]. After comprehensive treatment in our hospital, the patient got better and was discharged on the 7th day of admission (2023/3/10), and then came for reexamination on 2023/3/26. Studies involving human subjects were reviewed and approved by the Ethics Committee of Qilu Hospital of Shandong University. The patient provided written informed consent to participate in this study. Personal written informed consent has been obtained for the release of any potentially identifiable images or data contained in this article.
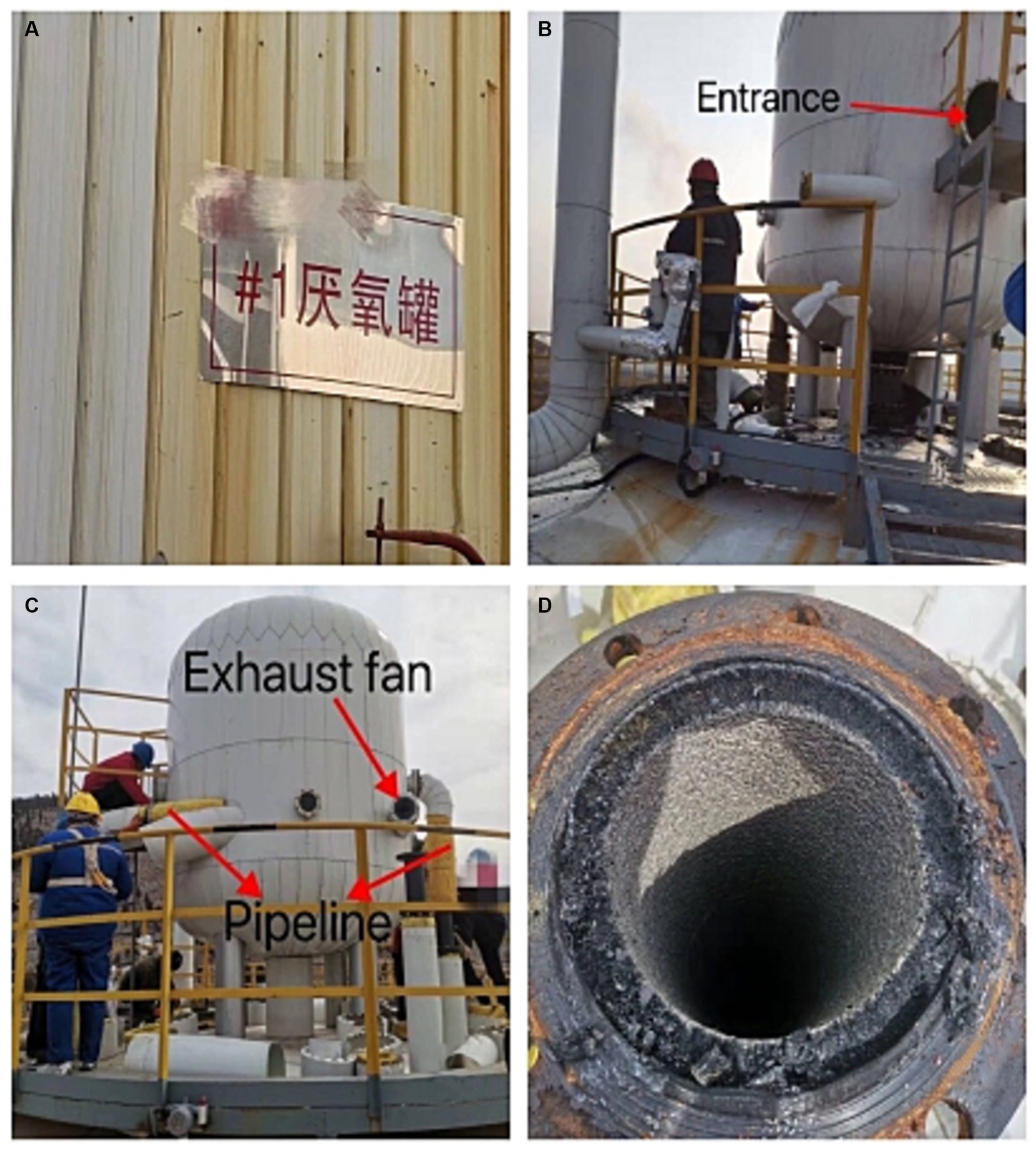
Figure 1. (A) Signs in Chinese for anaerobic tanks. (B,C) Exterior view of sludge treatment tank. (D) Interior view of sludge treatment tank.
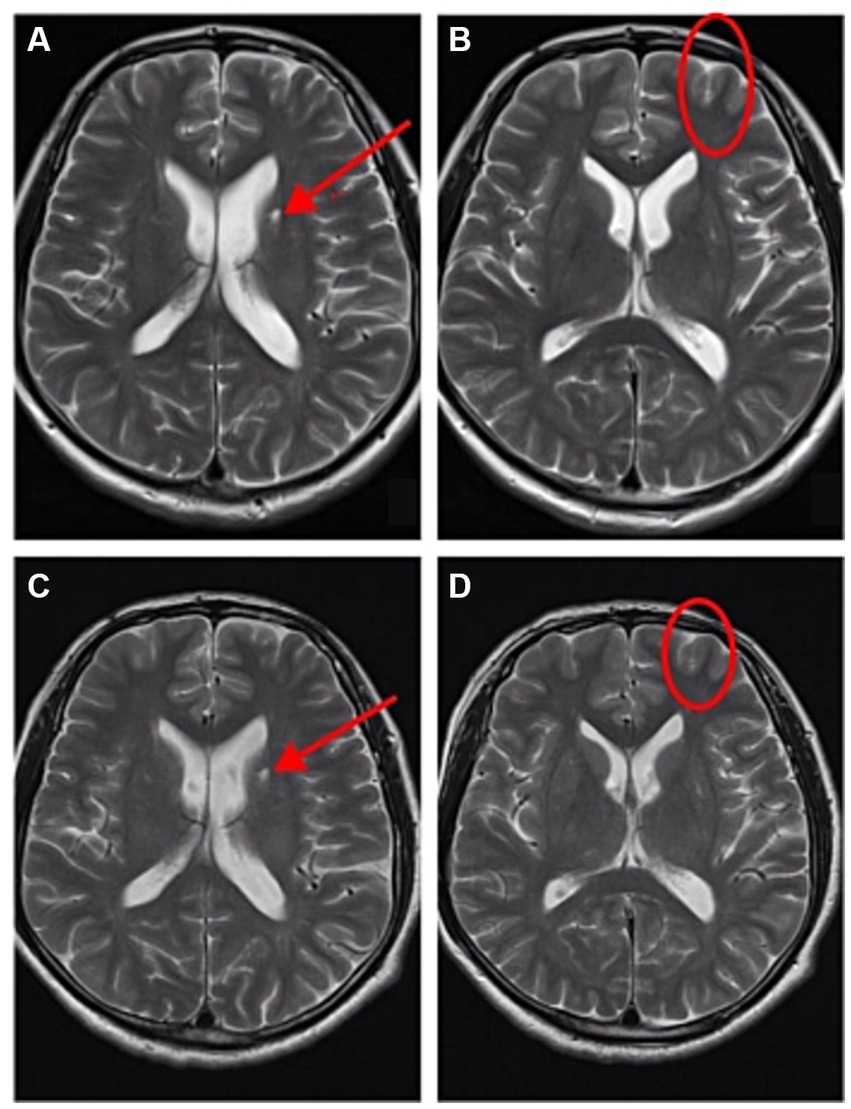
Figure 2. The patient underwent Brain MRI on 2023/3/6 (A,B) and 2023/3/26 (C,D). (A) There were abnormal signals in the left basal ganglia, considering softening foci. (B) There were a few abnormal signals in the left frontal lobe, considering non-specific signals or degenerative lesions around the perivascular space. (C) There were still abnormal signals in the left basal ganglia, considering softening foci, but the extent of the lesion was reduced compared with (A). (D) There were still a few abnormal signals in the left frontal lobe, considering non-specific signals or degenerative lesions around the perivascular space, but the extent of the lesion was reduced compared with (B).
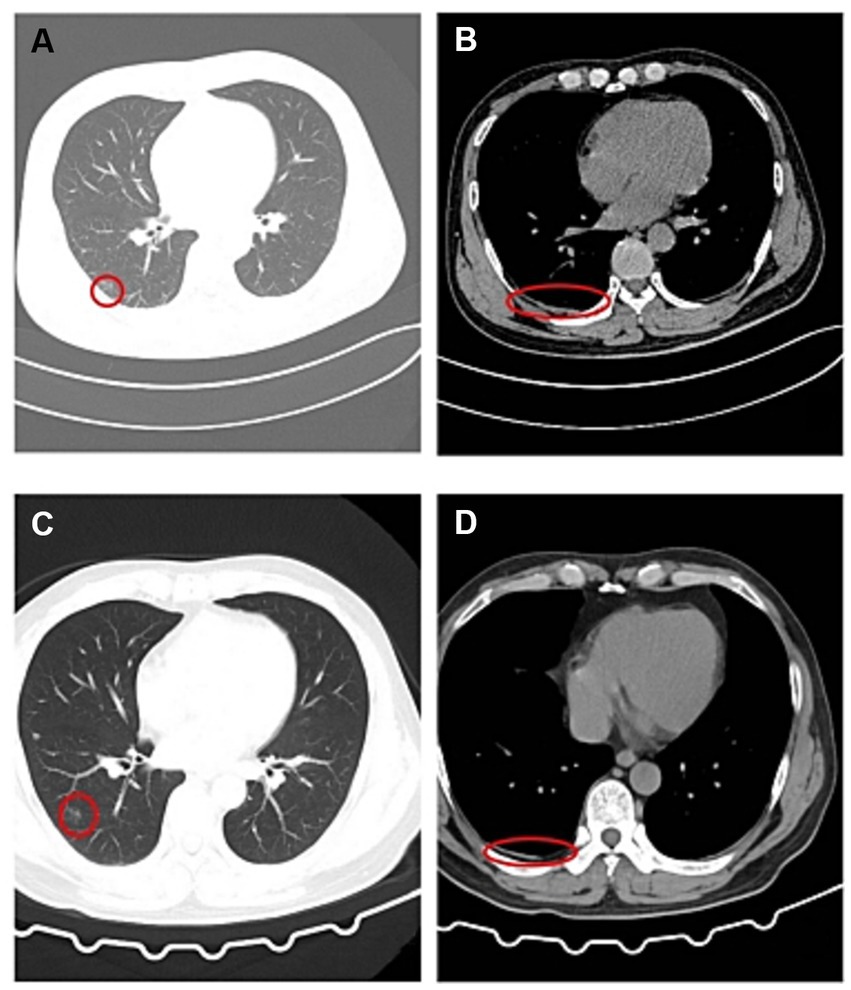
Figure 3. The patient underwent Chest CT on 2023/3/6 (A,B) and 2023/3/26 (C,D). (A) There was a little exudation in the lower lobe of the right lung, with localized interstitial changes. (B) There was localized thickening of the right pleura. (C) There was still exudation in the lower lobe of the right lung, but the extent of the lesion was reduced compared with (A). (D) There was still localized thickening of the right pleura, but the extent of the lesion was reduced compared with (B).
3. Discussion
H2S is poisonous, and accidents may occur on exposure to natural gas, volcanic gas, and industrial waste (13), this patient was also poisoned after exposure to industrial sludge. Accidents have been reported in chemical processing plants (14, 15) and sewage disposal facilities (16–19) and with the ingestion of sulfur products (20, 21). The same as reported by Jack et al. (16–19), This patient’s H2S poisoning accident occurred at a sewage disposal facility. The acute toxicity of H2S mainly involves the central nervous system and lungs (22), which is consistent with this patient’s clinical presentation. The oxidation of H2S after exogenous exposure is not complete, and the remaining H2S in vivo exists in a dissolved and bound form (23). The dissolved forms are H2S gas and sulfhydryl anion; both forms can diffuse between blood and tissue. The dissolved forms are H2S gas and sulfhydryl anion; both forms can diffuse between blood and tissue (24). Bound, insoluble sulfide forms include acid-labile sulfides and sulfated proteins (23). Both forms capture sulfide in an insoluble state and play a role in toxicity (23). For example, sulfide can bind to the iron atoms of the electron transport chain complex IV to inhibit cytochrome c oxidase (2, 25). Jiang et al. (10) described the direct toxicity to neurons derived from human induced pluripotent stem cells, leading to apoptosis. Cellular damage by reactive oxygen species, such as the increase in protein kinase (JNK and Erk) activity and the production of f2-isoprostane (a prostaglandin-like compound as a marker of oxidative stress), occurs after exposure to sulfide (26). Exposure to high concentrations of H2S can cause various neurological symptoms, such as dizziness, headache, poor coordination, and transient loss of consciousness. If exposure is transient, recovery is usually complete and rapid (27). A unique feature of this toxic gas is that sudden exposure to high concentration will lead to “knocking down” (28). This is a kind of incapacitating influence, which makes the victim unable to escape (29). For the same reason with Wang et al. (27), Anantharam et al. (28), and Guidotti et al. (29), the patient fainted after being exposed to high concentration of H2S and stayed in an anaerobic tank with poor ventilation for some time without personal protective equipment, resulting in H2S poisoning. Fortunately, after the accident, his workmates were able to find and rescue the patient in time, and immediately sent him to the hospital for treatment. The final result was that the patient recovered quickly without affecting the quality of life of the patient. The most frequently involved site in the brain is bilateral basal ganglia nuclei; because these nuclei need a lot of oxygen, the imaging features are symmetrical low density/high signal around bilateral basal ganglia and lateral ventricle; The lesions were distributed in bilateral frontoparietal white matter, oval center, lateral ventricle periphery, and basal ganglia nuclei (30). In patients with severe clinical symptoms, brain CT/MRI showed all four signs (systemic brain edema, symmetrical low density/abnormal signal around bilateral basal ganglia and lateral ventricle, subarachnoid hemorrhage or intracerebral hemorrhage, and cerebellar tonsil hernia) within 2 months; Systemic brain edema and symmetrical low density/abnormal signals around bilateral basal ganglia and lateral ventricles are the main findings (30). In contrast to the findings reported by Tang et al. (30), the imaging findings in this patient were unilateral rather than bilateral, probably because of the less severe degree of poisoning in this patient, which resulted in an atypical lesion. Lancia et al. (31) reported a fatal case of a factory worker who died after breathing H2S while performing a job for which he was not trained. Goolam et al. (32) described a 30-year-old sewer worker with a history of severe unexpected occupational exposure to inhaled H2S, and ultimately death due to acute respiratory distress syndrome and rapid respiratory depression. Sheikh et al. (33) reported a case of a fisherman exposed to a high concentration of H2S in a fish garbage room, and eventually, the patient survived and was discharged with a full recovery. The case we reported was clinically cured. Through telephone follow-up, we learned that the patient had no health abnormalities and has been transferred from his original post. However, this paper also has limitations, we did not obtain measurement data of H2S in the blood, nor did we obtain data of H2S in the field environment. We will continue to improve our work in the future.
Based on this accident, I have gained the following enlightenment to prevent occupational poisoning. The government and employers should work together to provide a safe and comfortable working environment for workers. It is suggested to reinforce the government’s responsibility for occupational disease prevention and control the occurrence of occupational disease hazards from the source. Establish an effective supervision mechanism for occupational disease prevention departments and an evaluation system for occupational disease prevention; Enhance occupational health supervision and law enforcement; Carry out in-depth publicity and training on occupational health laws and knowledge, give full play to the role of media publicity and public opinion guidance, continuously improve workers’ awareness of health protection and self-awareness of occupational disease prevention and control, and effectively prevent and control the occurrence of occupational diseases (34). Employers should adhere to the basic principle of people-oriented, always put the safety and health of workers in the first place, provide workers with a good working environment and personal protective equipment, strengthen the personal protection of workers, regularly carry out health education, carry out occupational health examination, eliminate potential safety hazards, and try to replace toxic or highly toxic substances with non-toxic or low-toxic substances. Implement occupational safety operation procedures. Workers should strengthen personal protection and work in accordance with occupational safety operating procedures.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
AG and MS designed the study and wrote the manuscript. XZ drafted the manuscript. XJ revised the manuscript. All authors contributed to the article and approved the submitted version.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Maebashi, K, Iwadate, K, Sakai, K, Takatsu, A, Fukui, K, Aoyagi, M, et al. Toxicological analysis of 17 autopsy cases of hydrogen sulfide poisoning resulting from the inhalation of intentionally generated hydrogen sulfide gas. Forensic Sci Int. (2011) 207:91–5. doi: 10.1016/j.f.Orsciint2010.09.008
2. Reiffenstein, RJ, Hulbert, WC, and Roth, SH. Toxicology of hydrogen sulfide. Annu Rev Pharmacol Toxicol. (1992). 32:109–134. doi: 10.1146/annurevpa.32.040192.000545
3. Ding, Y, Li, X, Chen, C, Ling, J, Li, W, Guo, Y, et al. A rapid evaluation of acute hydrogen sulfide poisoning in blood based on DNA-cu/ag nanocluster fluorescence probe. Sci Rep. (2017) 7:9638. doi: 10.1038/s41598-017-09960-1
4. Zeng, Z. A retrievable and highly selective fluorescent probe for monitoring sulfide and imaging in living cells. Inorg Chem. (2012) 51:2454–60. doi: 10.1021/ic2024082
5. Peng, H, Cheng, Y, Dai, C, King, AL, Predmore, BL, Lefer, DJ, et al. A fluorescent probe for fast and quantitative detection of hydrogen sulfide in blood. Angew Chem Int Ed Eng. (2011) 50:9672–5. doi: 10.1002/anie.201104236
6. Burnett, WW, King, EG, Grace, M, and Hall, WF. Hydrogen sulfide poisoning: review of 5 years' experience. Can Med Assoc J. (1977) 117:1277–80.
7. Arnold, IM, Dufresne, RM, Alleyne, BC, and Stuart, PJ. Health implication of occupational exposures to hydrogen sulfide. J Occup Med. (1985) 27:373–6. doi: 10.1097/00043764-198505000-00018
8. Ventura Spagnolo, E, Romano, G, Zuccarello, P, Laudani, A, Mondello, C, Argo, A, et al. Toxicological investigations in a fatal and non-fatal accident due to hydrogen sulphide (H2S) poisoning. Forensic Sci Int. (2019) 300:e4–8. doi: 10.1016/j.forsciint.2019.04.026
9. Strickland, J, Cummings, A, Spinnato, JA, Liccione, JJ, and Foureman, GL (2003). Toxicological review of hydrogen sulfide. U.S. Environmental Protection Agency, Washington, DC. Available at: https://cfpub.epa.gov/ncea/iris/iris_documents/documents/toxreviews/0061tr.pdf (Accessed March 30, 2019)
10. Jiang, J, Chan, A, Ali, S, Saha, A, Haushalter, KJ, Lam, WL, et al. Hydrogen sulfide--mechanisms of toxicity and development of an antidote. Sci Rep. (2016) 6:20831. doi: 10.1038/srep20831
11. Haouzi, P, Sonobe, T, and Judenherc-Haouzi, A. Hydrogen sulfide intoxication induced brain injury and methylene blue. Neurobiol Dis. (2020) 133:104474. doi: 10.1016/j.bd2019.05.013
12. Code of China (2002). Diagnostic standard of management of occupational acute hydrogen sulfide poisoning [S] GBZ 31-2002.
13. Guidotti, TL. Hydrogen sulphide. Occup Med (Lond). (1996) 46:367–71. doi: 10.1093/occmed/46.5.367
14. Tanaka, S, Fujimoto, S, Tamagaki, Y, Wakayama, K, Shimada, K, and Yoshikawa, J. Bronchial injury and pulmonary edema caused by hydrogen sulfide poisoning. Am J Emerg Med. (1999) 17:427–9. doi: 10.1016/s0735-6757(99)90102-x
15. Gabbay, DS, De Roos, F, and Perrone, J. Twenty-foot fall averts fatality from massive hydrogen sulfide exposure. J Emerg Med. (2001) 20:141–4. doi: 10.1016/s0736-4679(00)00301-2
16. Snyder, JW, Safir, EF, Summerville, GP, and Middleberg, RA. Occupational fatality and persistent neurological sequelae after mass exposure to hydrogen sulfide. Am J Emerg Med. (1995) 13:199–203. doi: 10.1016/0735-6757(95)90094-2
17. Kage, S, Takekawa, K, Kurosaki, K, Imamura, T, and Kudo, K. The usefulness of thiosulfate as an indicator of hydrogen sulfide poisoning: three cases. Int J Legal Med. (1997) 110:220–2. doi: 10.1007/s004140050071
18. Kage, S, Ikeda, H, Ikeda, N, Tsujita, A, and Kudo, K. Fatal hydrogen sulfide poisoning at a dye works. Leg Med. (2004) 6:182–6. doi: 10.1016/j.l.Egalmed2004.04.004
19. Knight, LD, and Presnell, SE. Death by sewer gas: case report of a double fatality and review of the literature. Am J Forensic Med Pathol. (2005) 26:181–5. doi: 10.1097/01.paf.0000163834.87968.08
20. Kage, S, Nagata, T, and Kudo, K. Determination of thiosulfate in body fluids by GC and GC/MS. J Anal Toxicol. (1991) 15:148–50. doi: 10.1093/jat/15.3.148
21. Nagata, T, Kage, S, Kimura, K, Kudo, K, and Imamura, T. How to diagnose polysulphide poisoning from tissue samples. Int J Legal Med. (1994) 106:288–90. doi: 10.1007/BF01224772
22. Ago, M, Ago, K, and Ogata, M. Two fatalities by hydrogen sulfide poisoning: variation of pathological and toxicological findings. Leg Med. (2008) 10:148–52. doi: 10.1016/j.l.Egalmed2007.11.005
23. Ng, PC, Hendry-Hofer, TB, Witeof, AE, Brenner, M, Mahon, SB, Boss, GR, et al. Hydrogen sulfide toxicity: mechanism of action, clinical presentation, and countermeasure development. J Med Toxicol. (2019) 15:287–94. doi: 10.1007/s13181-019-00710-5
24. Haouzi, P, Sonobe, T, Torsell-Tubbs, N, Prokopczyk, B, Chenuel, B, and Klingerman, CM. In vivo interactions between cobalt or ferric compounds and the pools of sulphide in the blood during and after H2S poisoning. Toxicol Sci. (2014) 141:493–504. doi: 10.1093/toxsci/kfu140
25. Haouzi, P, Sonobe, T, and Judenjerc-Haouzi, A. Developing effective countermeasures against acute hydrogen sulfide intoxication: challenges and limitations. Ann NY Acad Sci. (2016) 1374:29–40. doi: 10.1111/nyas.13015
26. Eghbal, MA, Pennefather, PS, and O’Brien, PJ. H2S cytotoxicity mechanism involves reactive oxygen species formation and mitochondrial depolarisation. Toxicology. (2004) 203:69–76. doi: 10.1016/j.tox.2004.05.020
27. Wang, X, Chen, M, Chen, X, Ma, J, Wen, C, Pan, J, et al. The effects of acute hydrogen sulfide poisoning on cytochrome P450 isoforms activity in rats. Biomed Res Int. (2014) 2014:209393. doi: 10.1155/2014/209393
28. Anantharam, P, Kim, DS, Whitley, EM, Mahama, B, Imerman, P, Padhi, P, et al. Midazolam efficacy against acute hydrogen sulfide-induced mortality and neurotoxicity. J Med Toxicol. (2018) 14:79–90. doi: 10.1007/s13181-017-0650-4
29. Guidotti, TL. Hydrogen sulfide intoxication. Handb Clin Neurol. (2015) 131:111–33. doi: 10.1016/B978-0-444-62627-1.00008-1
30. Tang, D, Tian, N, Cai, J, Ma, J, Wang, T, Zhang, H, et al. Analysis of CT and MR imaging features of the brain in patients with hydrogen sulfide poisoning based on clinical symptom grading. BMC Neurol. (2022) 22:413. doi: 10.1186/s12883-022-02956-z
31. Lancia, M, Panata, L, Tondi, V, Carlini, L, Bacci, M, and Rossi, R. A fatal work-related poisoning by hydrogen sulfide: report on a case. Am J Forensic Med Pathol. (2013) 34:315–7. doi: 10.1097/PAF.0000000000000055
32. Goolam, N, Bhikoo, R, Koegelenberg, CFN, and Lalla, U. Fatal sequelae of hydrogen sulphide poisoning. Respirol Case Rep. (2023) 11:e01144. doi: 10.1002/rcr2.1144
33. Sheikh, S, Baig, MA, Ali, N, and Khan, N. Hydrogen sulfide gas poisoning in fish garbage room: a report of a fisherman. J Pak Med Assoc. (2017) 67:1097–9.
Keywords: waste treatment plant, hydrogen sulfide poisoning, sludge treatment tank, analysis of the case, self-protection
Citation: Genjiafu A, Shi M, Zhang X and Jian X (2023) Case report: Analysis of a case of hydrogen sulfide poisoning in a waste treatment plant. Front. Public Health. 11:1226282. doi: 10.3389/fpubh.2023.1226282
Edited by:
Francesco Violante, University of Bologna, ItalyReviewed by:
Pietro Zuccarello, University of Catania, ItalyMingyang Zhang, Soochow University, China
Copyright © 2023 Genjiafu, Shi, Zhang and Jian. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xiangdong Jian, amlhbnhpYW5nZG9uZ3ZpcEB2aXAuMTYzLmNvbQ==
†These authors have contributed equally to this work
‡ORCID: Xiangdong Jian, https://orcid.org/0000-0002-2277-6817
 Aerbusili Genjiafu1†
Aerbusili Genjiafu1† Xiangxing Zhang
Xiangxing Zhang Xiangdong Jian
Xiangdong Jian