- 1Department of Radiotherapy, The First Hospital of China Medical University, Shenyang, Liaoning, China
- 2Department of Paediatrics, The First Hospital of China Medical University, Shenyang, Liaoning, China
Objective: To understand abnormal thyroid function and its associated factors among medical staff in radiotherapy departments.
Methods: Data related to medical staff in radiotherapy departments who met the inclusion and exclusion criteria were analyzed from September to December 2022 in Shenyang, Liaoning Province, including basic personal and lifestyle habits, work information, and scores on the Depression Self-Assessment Scale, Perception Stress Scale, and the Generalized Anxiety Scale. Data analysis was performed using the χ2 test and binary logistic regression.
Results: Among 484 medical staff in the radiotherapy department, 147 (30.4%) had abnormal thyroid function. Binary logistic regression analysis showed that age, years of work, smoking, occupational exposure, smoking, late-night snacking habits, depression, and stress perception were factors associated with abnormal thyroid function among medical staff in radiotherapy departments; on the other hand, physical exercise was a protective factor.
Conclusion: The positive rate of thyroid dysfunction among medical personnel in the radiology department is relatively high. It is necessary to strengthen health education and awareness among relevant practitioners and improve the coverage of occupational disease prevention and control education.
1. Introduction
Abnormal thyroid function is closely associated with prolonged occupational exposure, which is more common among medical staff in radiation therapy units (1). It is an endocrine disorder caused by insufficient synthesis secretion/biological effect or excessive release of thyroid hormones due to low or high thyroid action (2). Abnormal functional status increases the risk of anxiety, anger, obesity, diabetes, hypertension, and thyroid cancer among doctors and nurses (3), which adversely affects patient care, such as inappropriate protective measures leading to exposure to low-dose radiation, emotional instability of doctors and nurses leading to tension between doctors and patients, and long-term suboptimal health of doctors and nurses affecting the treatment plan (4, 5). Therefore, it is important to explore the abnormal thyroid function of medical staff in radiotherapy departments and its associated factors to promote harmony between doctors and patients and maintain the physical and mental health of medical and nursing staff.
Research studies have found that the incidence of thyroid function abnormalities among medical staff is between 4 and 30% (6, 7), showing an increasing trend year by year. Factors influencing thyroid function abnormalities include demographic factors (age, gender, education, etc.), work factors (level of protection, type of work, length of service, etc.), disease factors (coronary heart disease, diabetes, dyslipidemia, etc.), and lifestyle habits (smoking, drinking, dietary preferences, etc.) (8–11). However, studies on the association between factors such as psychological regulation, behavioral patterns, physical exercise, and thyroid function abnormalities among medical staff in radiotherapy departments are less common.
Currently, abnormal thyroid function is becoming an important public health and occupational health problem threatening the health of radiologists. Although medical staff are aware of the hazards of low-dose radiation and thyroid disease, they need to analyze potential risk factors and put interventions and preventive measures in place. This study investigates the association between abnormal thyroid function and its associated factors among medical staff in radiotherapy departments, especially exposure to lifestyle, psychological regulation, and behavioral patterns, to provide a scientific basis for preventing and controlling occupational disease hazards.
2. Methods
2.1. Study design
This study adopted a cross-sectional design, using the random number table method to randomly select 10 hospitals from 37 public tertiary A hospitals in Shenyang, Liaoning Province, from September to December 2022. Approximately 50 medical staff from the radiation therapy departments of the 10 hospitals were randomly sampled, and all individuals who met the standards were included in the target population.
2.2. Participant
The sample size of the study was calculated using the formula: N = 400 × Q/P (Q = 1-P and P was the incidence rate). Due to the lack of a unified incidence rate of abnormal thyroid hormone levels, after consulting Chinese domestic literature (12), the detection rate of abnormal levels of thyroid hormones among medical staff was set at 46.6%, and N = 458 people were calculated. Considering the possibility of invalid and missing questionnaires in the investigation process, 500 questionnaires were issued, of which 484 were recovered, with a recovery rate of 96.8%. All questionnaires were valid, so the target population of this study was set at 484 people. Inclusion criteria: (1) Aged ≥18 years; (2) Abnormal function as determined by two or more internists by thyroid color Doppler ultrasound and serum thyroid hormone tests [triiodothyronine (T3), thyroxine (T4), and thyrotropin (TSH)]; (3) Voluntary participation in this study and no participation in similar studies within 6 months; and (4) No mental disorders caused by cerebrovascular diseases, physical infections, or other physical diseases. Exclusion criteria: (1) Family history of thyroid disease, history or other autoimmune diseases; (2) Have a history of pituitary or hypothalamic diseases; (3) Have a history of severe parathyroid disease; (4) Chronic consumptive diseases (diabetes, abnormal liver function, abnormal kidney function, cardiac insufficiency, chronic infectious diseases, etc.) and malignant tumors; (5) Recent history of acute and severe infections; (6) Take or use drugs that affect thyroid hormones, such as phenytoin sodium, Carbamazepine, Amiodarone, Lithium carbonate, and iodine-containing contrast agent, and (7) Pregnant women. The study was approved by the hospital's ethical review committee, and all participants gave informed consent to the study content.
2.3. Instrumentation
2.3.1. General information survey
The questionnaire covered basic personal details, living habits, and work information. The basic personal information and living habits included gender, age, education, family history of thyroid disease, alcohol consumption, smoking, frequency of physical exercise, and whether there was a night snacking habit. The basic work information included years of work, title, type of occupation, whether the night shift was on rotation, and whether occupational exposure occurred.
2.3.2. Abnormal thyroid function
The five indicators of thyroid function included free triiodothyronine (CFT3), free thyroxine (CFT4), thyroid stimulating hormone (TSH), thyroglobulin antibody (TGAb), and thyroid peroxidase antibody (TPOAb). Approximately 3–5 ml of fasting peripheral blood was collected from the study participants and placed in a non-anticoagulant tube. It was let to stand at room temperature for 30 m and centrifuged at 3,500 rpm for 10 m, with a centrifugal force of 1,095*g. Approximately 500 uI of serum was collected and placed in an EP tube. Simultaneously, a backup was created and immediately frozen in a freezer at −20°C for testing. In this study, five indicators of thyroid function in the serum of the participants were detected by Roche E411 automatic electrochemiluminescence immune analyzer and its detection reagent. All experimental reagents were calibrated using a standard calibration solution, and those that passed the calibration were used on the machine. The products were tested daily for quality control before the experiments to ensure that each experiment was within the quality control range. The reference ranges of the blood biochemical indexes were: TSH 0.27–4.2 mIU/L, FT4 12–22 pmol/L, FT3 3.1–6.8 pmol/L, TPOAb 3–34 mIU/L, and TGAb 0–115 mIU/L. Two internists jointly determined whether the thyroid function was abnormal based on the blood biochemical index results according to the Chinese Guidelines for the Diagnosis and Treatment of Thyroid disease.
2.3.3. The Generalized Anxiety Disorder (GAD-7)
The scale consists of seven symptoms and one symptom-related degree of difficulty item that assessed the severity and functional impact of the seven anxiety symptoms over the past 2 weeks (13). Each symptom was rated on a 4-point Likert scale from 0 (not at all) to 3 (almost every day). The degree of difficulty degree item had four options (no difficulty at all, somewhat difficult, very difficult, and extremely difficult) but was not included in the score. The total score of the scale was 21, with 0–4 indicating no anxiety, 5–9 mild anxiety, 10–14 moderate anxiety, and ≥15 suggesting severe anxiety. This questionnaire has been widely used in the Chinese population and has good reliability and validity (14, 15). The Cronbach's alpha for this scale in this study was 0.851 (GFI = 0.982, RMSEA = 0.027, CFI = 0.995, NFI = 0.982).
2.3.4. Depression Self-Assessment Scale (PHQ-9)
The scale was developed based on the nine symptoms of DSM-IV depressive disorder and was widely used in scientific research and clinical practice because of its brevity and ease of use (16). The total score of the PHQ-9 ranges from 0 to 27, with scores of 5, 10, and 20 being the cut-off values for the degree of mild, moderate, and severe depression, respectively. The scale has good sensitivity and specificity in the screening and diagnosis of depression (17). This questionnaire has been widely used in the Chinese population and has good reliability and validity (14, 18). The Cronbach's alpha for this scale in this study was 0.910 (GFI = 0.964, RMSEA = 0.032, CFI = 0.988, NFI = 0.964).
2.3.5. The perceived stress scale
The perceived stress scale (PSS) was developed by Cohen et al. (19) in 1983 and is a more widely used tool for assessing perceived stress. This study used the Chinese version of the perceived stress scale (CPSS) based on PSS-14 (20). It is simple and easy to use and is mainly used to measure the level of stress in an individual's life. It consists of two dimensions: a sense of loss of control and a sense of tension, with 14 items, also known as the PSS-14. Each item is rated on a 5-point Likert scale, ranging from 0 to 4 on a scale of “strongly disagree” to “strongly agree.” Items 4, 5, 6, 7, 9, 10, and 13 were scored inversely, with a total score ranging between 0 and 56; higher scores indicated greater perceived stress. This questionnaire has been widely used in the Chinese population and has good reliability and validity (21, 22). The Cronbach's alpha for this scale in this study was 0.952 (GFI = 0.968, RMSEA = 0.020, CFI = 0.995, NFI = 0.968).
2.4. Statistical analysis
All collected data were analyzed using SPSS 26.0 software. The count variables were expressed as percentages, and comparisons between groups were made using the χ2 test. The measured variables were expressed as mean ± standard deviation, and a t-test was used for comparison between groups. Univariate and multivariate logistic regression were used to determine the factors influencing abnormal thyroid function.
3. Results
3.1. Basic information of the participants
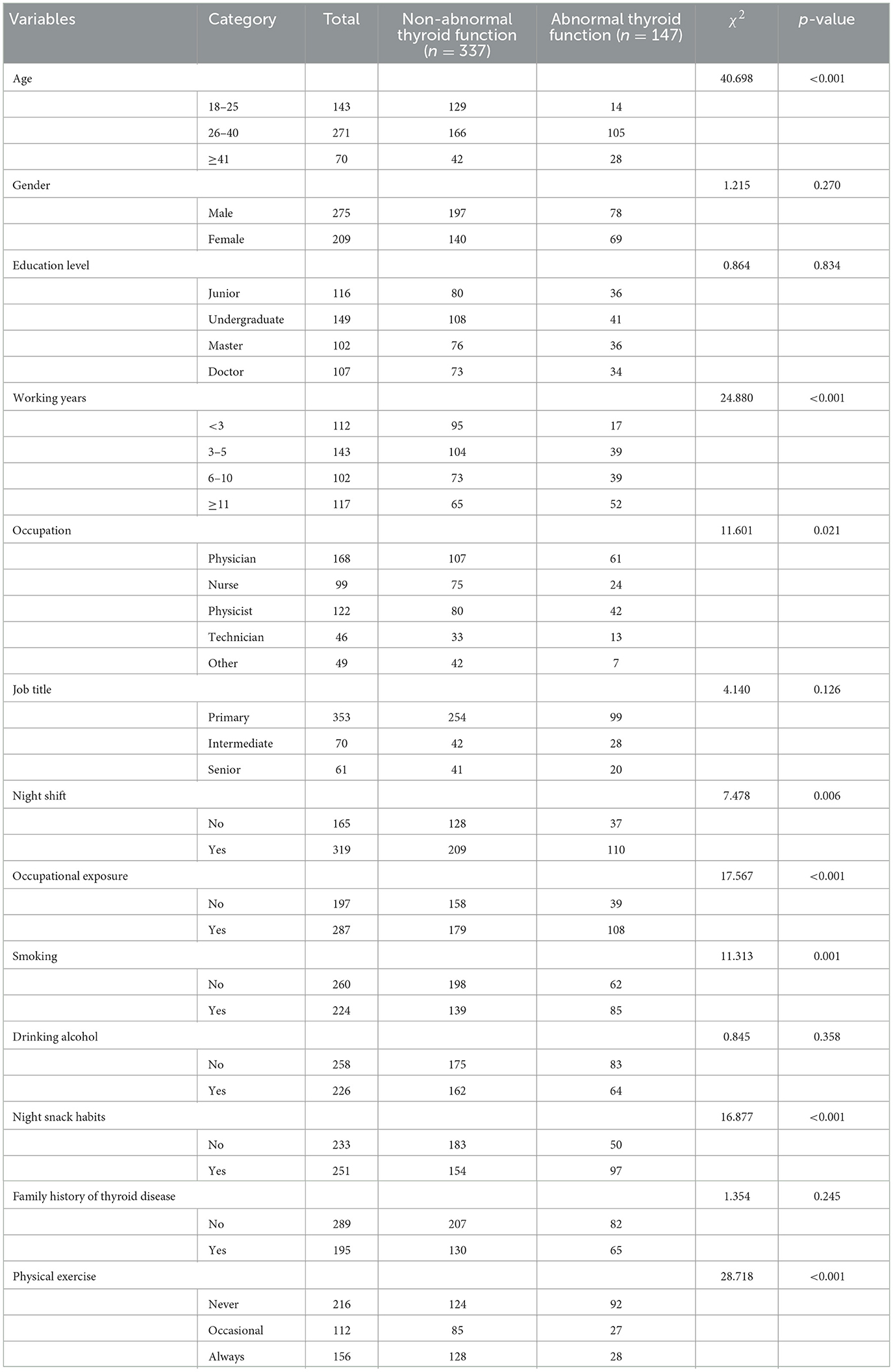
A total of 500 questionnaires were issued, and 484 valid questionnaires were returned, including 147 with abnormal thyroid function, with a detection rate of 30.4%. Hyperthyroidism, hypothyroidism, subclinical hyperthyroidism, and subclinical hypothyroidism were detected in 15, 28, 37, and 67 cases, with detection rates of 10.2%, 19.0%, 25.2%, and 45.6%, respectively. The age range of medical staff in the radiotherapy department was 21–37 years old, with an average of 29.0 ± 8.6 years. There were 283 (58.5%) female and 201 (41.5%) male staff. Approximately 289 participants mainly had irregular eating habits, accounting for 51.9%. In addition, 224 (46.3%) and 226 (46.7%) medical doctors had smoking and drinking habits, respectively. Approximately 216 (44.6%) participants never exercised, 112 (23.1%) occasionally exercised, and 156 (32.3%) always exercised. Their occupational types were predominantly physicians 168 (34.7%), in addition to 99 (20.5%) nurses, 122 (25.2%) physiatrists, 46 (9.5%) technicians, and 49 (10.1%) other staff. Approximately 287 (59.3%) of the staff had a history of occupational exposure. Most of the participants had worked for 5 years or less, and those with intermediate and below job titles were predominant. There were 319 (65.9%) medical staff involved in night shifts and 165 (34.1%) staff without night shifts. The details are shown in Table 1.
3.2. Anxiety, depression, and stress perceptions of medical staff in the radiotherapy department
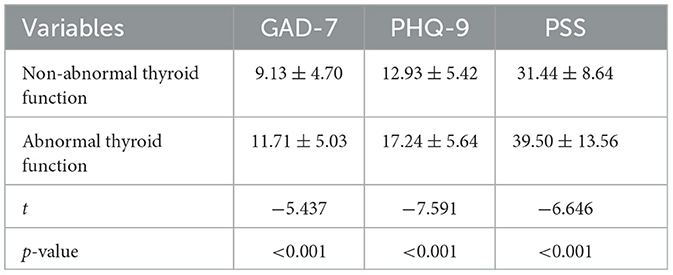
Reviewing the depression, anxiety, and stress assessments in both groups, the results showed that the PHQ-9, GAD-7, and PSS scores were significantly higher in the abnormal thyroid functioning group than in the non-abnormal group, and the differences were statistically significant. The details are shown in Table 2.
3.3. Univariate logistic regression analysis of factors associated with abnormal thyroid function among medical staff in radiotherapy departments
The results of univariate logistic regression analysis showed that age, years of work, type of occupation, job title, night shift, occupational exposure, late-night snacking habit, smoking, family history, physical exercise status, GAD-7, PHQ-9, and PSS were associated with abnormal thyroid function among medical staff in the radiotherapy department. The details are shown in Table 3.
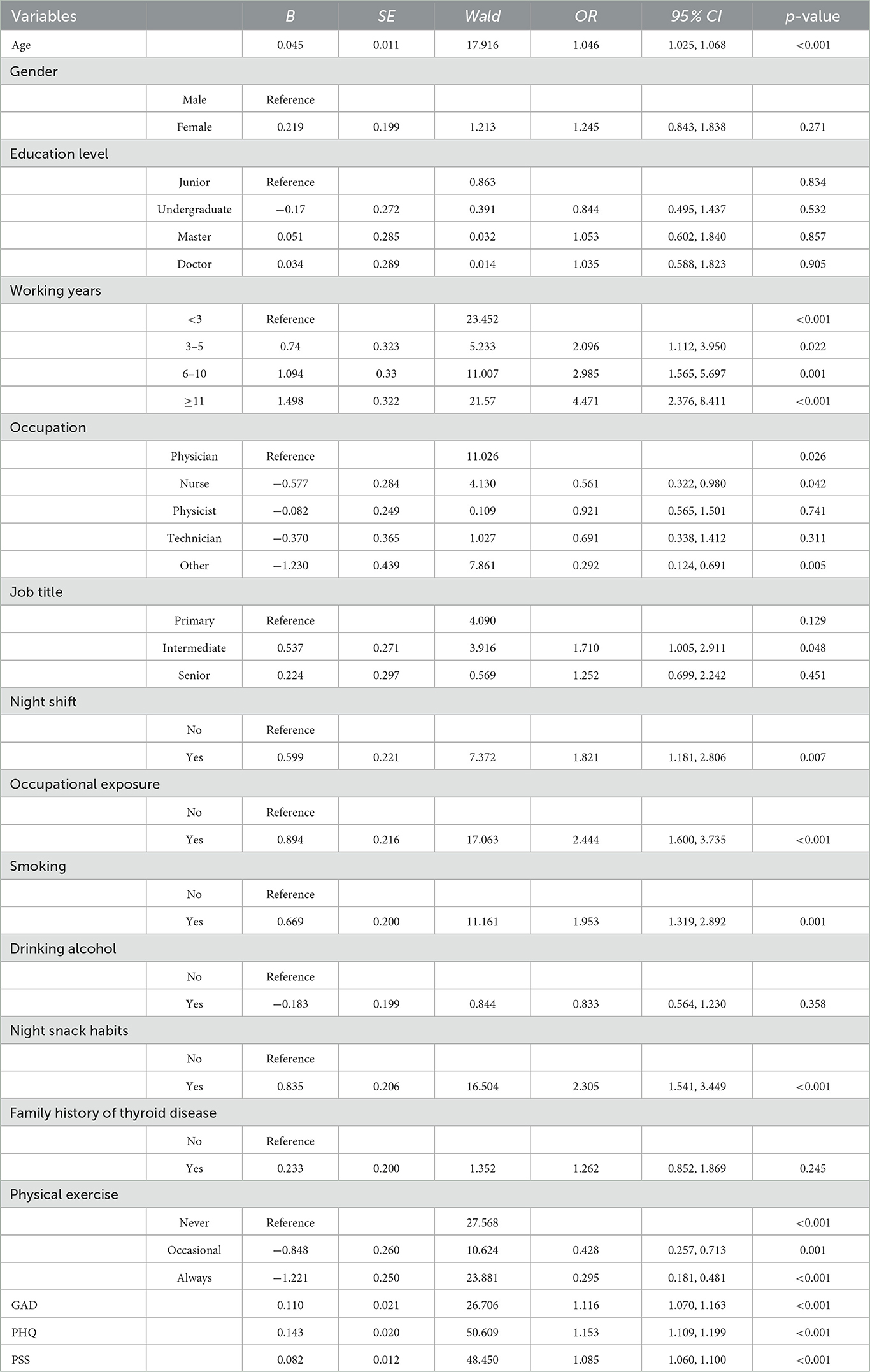
Table 3. Univariate logistic regression analysis of the factors associated with thyroid dysfunction in the radiotherapy department.
3.4. Multivariate logistic regression analysis of factors associated with abnormal thyroid function among medical staff in radiotherapy departments
A multivariate logistic regression analysis was performed with abnormal thyroid function (0 = no, 1 = yes) as the dependent variable and factors with p < 0.1 in the univariate logistic regression analysis as independent variables. The results showed that age, years of work, occupational exposure, smoking, late-night snacking habits, depression, and stress perception were associated factors for abnormal thyroid function among medical staff in the radiotherapy department: physical exercise, on the other hand, was a protective factor for abnormal thyroid function. For details, see Table 4.
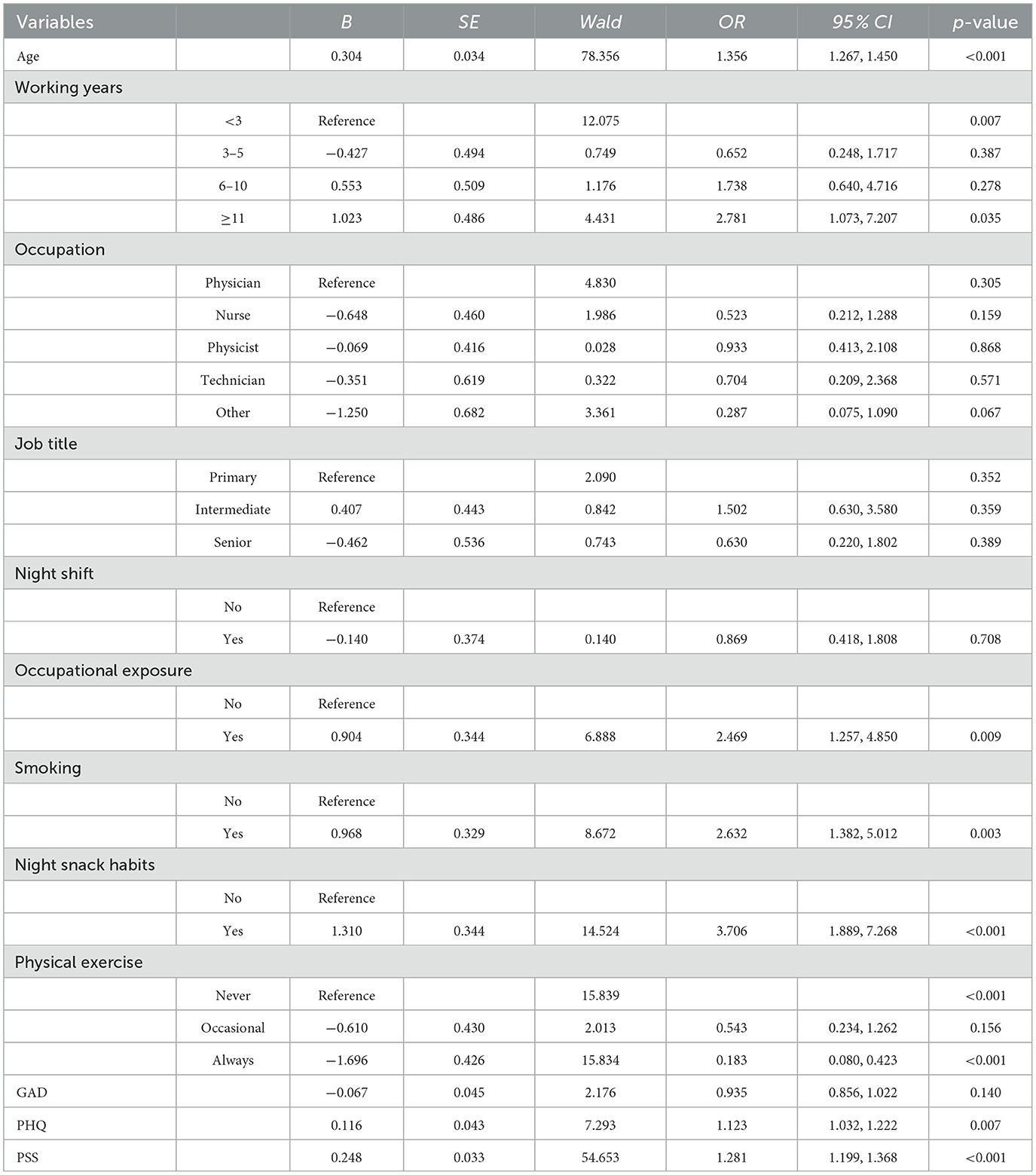
Table 4. Multivariate logistic regression analysis of factors associated with thyroid function abnormalities in the radiotherapy department.
4. Discussion
The thyroid gland is the largest endocrine gland in adults, which mainly regulates the growth and development of the human body, and affects emotions and the metabolism of sugar, fat, and protein. The prevalence of thyroid disease is increasing year by year (23). This study found that medical staff are more likely to suffer from thyroid disease than ordinary people (24). It also found that the detection rate of abnormal thyroid function was 30.4% based on the results of thyroid function testing and a questionnaire survey among 484 medical personnel in the radiotherapy department in Liaoning Province. The detection rate was significantly higher than the 6.6% surveyed in Europe and the United States (2) and higher than the 25% in the community-based older population aged 65 years and older in the United States (25). The positive rate of thyroid function abnormalities in this study was lower than the 39.4% reported by Zhang et al. (26) for medical radiologists in Nanjing but higher than the 12.3% reported by Santos et al. (27) for permanent residents aged 20 years and older in South America. The differences in study results may be due to differences in economic development, social environment, thyroid function measurement tools, and the participants included in different countries and regions. The literature search revealed that there are few studies on the factors associated with abnormal thyroid function in medical staff in radiotherapy departments, and most studies focus on physical and chemical indicators or functional changes in the thyroid gland but less on the influence of social, psychological, and behavioral factors on abnormal thyroid function (28–31).
The results of the multivariate analysis showed that age and working hours were associated factors for abnormal thyroid function in medical staff in radiation therapy units—the older the medical staff in radiation therapy units and the longer the working years, the higher the positive rate of abnormal thyroid function among them, which is generally consistent with previous studies (29, 32). The analysis suggests that with the accumulation of low-dose radiation exposure, thyroid peroxidase expression decreases, leading to inhibition of thyroid hormone synthesis (33), which, in turn, accelerates the incidence of thyroid dysfunction. The present study's results showed that the risk of thyroid function abnormalities among medical staff in radiotherapy departments with previous occupational exposure was 2.4 times higher than those without occupational exposure.
The thyroid gland is sensitive to ionizing radiation, and long-term exposure can lead to dysfunction and teratogenic effects (34). Radiation can cause vascular damage, parenchymal cell damage, and autoimmune cell response in the thyroid gland (35). Ron and Brenner (36) found that ionizing radiation increases the risk of goiter and thyroid nodules, and the incidence of benign thyroid nodules and follicular thyroid adenoma had a significant dose-effect relationship with ionizing radiation. The results of a cross-sectional survey based on the community population in Pomerania showed that occupational ionizing radiation exposure is related to the risk of autoimmune thyroid disease (37). The study found that medical staff did not take thyroid protection seriously during their prolonged professional practice and that staff who did not wear thyroid protection were frequently exposed to ionizing radiation, thus making the thyroid more vulnerable to radiation injury (31).
The results of this study showed that the risk of thyroid function abnormalities was higher in radiotherapy medical staff who smoked than in nonsmokers and that their serum TSH levels were significantly higher than in nonsmokers (38). This is probably because the alkaloids and nicotine in tobacco cause the body to be in a chronic inflammatory state and induce cellular mediators (produced by immune cells) that can accelerate the deterioration of thyroid function (39). Late-night snacking habits are also considered to be one of the risk factors affecting thyroid function. Studies have shown that regular and reasonably arranged intake of meat, staple foods, vegetables, and fruits are beneficial for preventing thyroid function disorders (40), which is consistent with the findings of this paper. A Mediterranean characteristic diet, low in animal foods and high in plant foods, is more protective for thyroid function than a high animal foods diet (41) and may be related to the balanced gain in nutrient intake from a good diet. Similarly, stress perception is a risk factor for abnormal thyroid function in radiotherapy medical staff, probably because acute or chronic stressful stress induces an imbalance in the body's immune system (42, 43), leading to an overproduction of glucocorticoids and catecholamines through activation of the thalamus-pituitary-adrenal axis, which, in turn, leads to the development of abnormal thyroid function. Depression has also been found to be a risk factor for abnormal thyroid function in medical staff in radiotherapy departments. The stimulation of adverse psychosomatic factors such as depression can cause disorders of the neuroendocrine system, affecting the abnormal function of the HPA axis, impeding thyroid hormone secretion, and affecting the normal functioning of the thyroid gland (28).
Medical staff who exercise daily are less likely to have abnormal thyroid function than those who exercise less than twice a week, which may be related to continuous and regular exercise reducing resting T4, T3, and thyroid-stimulating hormone levels. Further, it has been noted that exercise can alter the levels of zinc in the body, which is considered an important substance involved in synthesizing and processing thyroid hormones (44, 45).
5. Implications and limitations
This study is an important addition to the epidemiology of thyroid disorders. With the rising incidence of cancer, the issue of abnormal thyroid function among medical staff in radiotherapy units deserves attention and prevention. Age, years of work, smoking, occupational exposure, late-night snacking habits, depression, and perceived stress were found to be risk factors for abnormal thyroid function among radiotherapy medical staff, with physical activity as a protective factor. The study still has the following limitations. First, the sample size was limited, and all were from the same study center, subject to selection bias. Second, cross-sectional studies, which do not provide good evidence of causality, are necessary to conduct cohort studies to assess the effect of each factor more clearly on abnormal thyroid function.
6. Conclusions
In conclusion, the positive rate of thyroid dysfunction among medical personnel in the radiology department is relatively high. It is necessary to strengthen health education and awareness among relevant practitioners and improve the coverage of occupational disease prevention and control education. Hospitals should conduct regular training to enhance the radiation protection awareness of medical personnel, focusing on protecting the thyroid area and improving protective conditions. Medical staff should cultivate good living habits and maintain their mental health.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding authors.
Ethics statement
The studies involving humans were approved by the Ethics Committee of The First Hospital of China Medical University. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
ZR and PS: full access to all the data in the study, take data analysis, and supervision. YR: conceptualization, methodology, and writing—original draft. XB: software and validation. GL: writing—reviewing and editing. All authors approved the submitted version.
Funding
This research was funded by the National Natural Science Foundation of China (82272756).
Acknowledgments
We would like to thank our hospitals involved in the investigation for their cooperation.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2023.1225879/full#supplementary-material
References
1. Wong Y-S, Cheng Y-Y, Cheng T-J, Huang C-C, Yeh J-J, Guo H-R. The relationship between occupational exposure to low-dose ionizing radiation and changes in thyroid hormones in hospital workers. Epidemiology. (2019) 30:S32–8. doi: 10.1097/EDE.0000000000001004
2. Biondi B, Kahaly GJ, Robertson RP. Thyroid dysfunction and diabetes mellitus: two closely associated disorders. Endocr Rev. (2019) 3:789–824. doi: 10.1210/er.2018-00163
3. Wang JX, Zhang LA, Li BX, Zhao YC, Wang ZQ, Zhang JY, et al. Cancer incidence and risk estimation among medical X-ray workers in China, 1950–1995. Health Phys. (2002) 82:455–66. doi: 10.1097/00004032-200204000-00004
4. Karaman K, Mansiroglu K, Subasi O, Biricik A, Yirgin H, Kose E, et al. Thyroid hormone changes after sleeve gastrectomy with and without antral preservation. Obes Surg. (2020) 31:224–31. doi: 10.1007/s11695-020-04896-4
5. Heilmaier C, Mayor AC, Zuber N, Fodor P, Weishaupt D. Improving radiation awareness and feeling of personal security of non-radiological medical staff by implementing a traffic light system in computed tomography. Rofo. (2016) 188:280–7. doi: 10.1055/s-0041-110450
6. Canaris GJ, Manowitz NR, Mayor GH, Ridgway EC. The Colorado thyroid disease prevalence study. Arch Intern Med. (2000) 160:526–34. doi: 10.1001/archinte.160.4.526
7. Ragusa F, Fallahi P, Elia G, Gonnella D, Paparo SR, Giusti C, et al. Hashimotos' thyroiditis: epidemiology, pathogenesis, clinic and therapy. Best Pract Res Clin Endocrinol Metab. (2019) 33:101367. doi: 10.1016/j.beem.2019.101367
8. Pakdel F, Ghazavi R, Heidary R, Nezamabadi A, Parvizi M, Haji Safar Ali Memar M, et al. Effect of selenium on thyroid disorders: scientometric analysis. Iran J Public Health. (2019) 48:410–20. doi: 10.18502/ijph.v48i3.883
9. Mirian C, Grønhøj C, Jensen DH, Jakobsen KK, Karnov KKS, Jensen JS, et al. Trends in thyroid cancer: retrospective analysis of incidence and survival in Denmark 1980-2014. Cancer Epidemiol. (2018) 55:81–7. doi: 10.1016/j.canep.2018.05.009
10. Lerner A, Neidhöfer S, Reuter S, Matthias T. MMP3 is a reliable marker for disease activity, radiological monitoring, disease outcome predictability, and therapeutic response in rheumatoid arthritis. Best Pract Res Clin Rheumatol. (2018) 4:550–62. doi: 10.1016/j.berh.2019.01.006
11. Maniakas A, Davies L, Zafereo ME. Thyroid disease around the world. Otolaryngol Clin North Am. (2018) 3:631–42. doi: 10.1016/j.otc.2018.01.014
12. Hu W, Zhao J. Study on prevalence of thyroid nodules among medical staff. Occup Health Emer Rescue. (2018) 36:405. doi: 10.16369/j.oher.issn.1007-1326.2018.05.007
13. Spitzer RL, Kroenke K, Williams JBW, Löwe BJ. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. (2006) 166:1092–7. doi: 10.1001/archinte.166.10.1092
14. Tang L, Yu XT, Wu YW, Zhao N, Liang RL, Gao XL, et al. Burnout, depression, anxiety and insomnia among medical staff during the COVID-19 epidemic in Shanghai. Front Public Health. (2022) 10:1019635. doi: 10.3389/fpubh.2022.1019635
15. Zhou Y, Wang W, Sun Y, Qian W, Liu Z, Wang R, et al. The prevalence and risk factors of psychological disturbances of frontline medical staff in china under the COVID-19 epidemic: workload should be concerned. J Affect Disord. (2020) 277:510–4. doi: 10.1016/j.jad.2020.08.059
16. Manea L, Gilbody S, McMillan DJ. Optimal cut-off score for diagnosing depression with the Patient Health Questionnaire (PHQ-9): a meta-analysis. CMAJ. (2012) 184:E191–6. doi: 10.1503/cmaj.110829
17. Milette K, Hudson M, Baron M, Thombs BD. Comparison of the PHQ-9 and CES-D depression scales in systemic sclerosis: internal consistency reliability, convergent validity and clinical correlates. Rheumatology. (2010) 4:789–96. doi: 10.1093/rheumatology/kep443
18. Huo L, Zhou Y, Li S, Ning Y, Zeng L, Liu Z, et al. Burnout and its relationship with depressive symptoms in medical staff during the COVID-19 epidemic in China. Front Psychol. (2021) 12:616369. doi: 10.3389/fpsyg.2021.616369
19. Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. (1983) 24:385–96. doi: 10.2307/2136404
20. Yang TZ, Huang HT. [An epidemiological study on stress among urban residents in social transition period]. J. Epidemiol. (2003) 24:760–4.
21. Xu X, Chen L, Yuan Y, Xu M, Tian X, Lu F, et al. Perceived stress and life satisfaction among Chinese clinical nursing teachers: a moderated mediation model of burnout and emotion regulation. Front Psychiatry. (2021) 12:548339. doi: 10.3389/fpsyt.2021.548339
22. Tan T, Leung CW. Associations between perceived stress and BMI and waist circumference in Chinese adults: data from the 2015 China Health and Nutrition Survey. Public Health Nutr. (2021) 24:4965–74. doi: 10.1017/S1368980020005054
23. Taylor PN, Albrecht D, Scholz A, Gutierrez-Buey G, Lazarus JH, Dayan CM, et al. Global epidemiology of hyperthyroidism and hypothyroidism. Nat Rev Endocrinol. (2018) 14:301–16. doi: 10.1038/nrendo.2018.18
24. Desouky O, Ding N, Zhou G. Targeted and non-targeted effects of ionizing radiation. J Radiat Res Appl Sci. (2015) 8:247–54. doi: 10.1016/j.jrras.2015.03.003
25. Diab N, Daya NR, Juraschek SP, Martin SS, McEvoy JW, Schultheiss UT, et al. Prevalence and risk factors of thyroid dysfunction in older adults in the community. Sci Rep. (2019) 9:13156. doi: 10.1038/s41598-019-49540-z
26. Zhang PP, Zhu CH, Dong X. [Analysis of abnormal results of thyroid B-ultrasonography in medical radiological workers in Nanjing, China]. J. Indus. Hyg. Occup. Diseases. (2019) 12:940–2. doi: 10.3760/cma.j.issn.1001-9391.2019.12.017
27. Santos Palacios S, Llavero Valero M, Brugos-Larumbe A, Díez JJ, Guillén-Grima F, Galofré JC. Prevalence of thyroid dysfunction in a Large Southern European Population. Analysis of modulatory factors. The APNA study. Clin Endocrinol. (2018) 89:367–75. doi: 10.1111/cen.13764
28. Dai W, Liu J, Xie H, Teng Z, Luo W, Yuan H, et al. Association between subclinical hypothyroidism and psychotic features in Chinese young adults with first-episode and untreated major depressive disorder. J Affect Disord. (2023) 333:209–15. doi: 10.1016/j.jad.2023.04.067
29. Antonelli A, Silvano G, Bianchi F, Gambuzza C, Tana L, Salvioni G, et al. Risk of thyroid nodules in subjects occupationally exposed to radiation: a cross sectional study. Occup Environ Med. (1995) 52:500–4. doi: 10.1136/oem.52.8.500
30. Tsou MT, Chen JY. Burnout and metabolic syndrome among healthcare workers: is subclinical hypothyroidism a mediator? J Occup Health. (2021) 63:e12252. doi: 10.1002/1348-9585.12252
31. El-Benhawy SA, Fahmy EI, Mahdy SM, Khedr GH, Sarhan AS, Nafady MH, et al. Assessment of thyroid gland hormones and ultrasonographic abnormalities in medical staff occupationally exposed to ionizing radiation. BMC Endocr Disord. (2022) 22:287. doi: 10.1186/s12902-022-01196-z
32. Lee YK, Lee D-E, Hwangbo Y, Lee YJ, Kim HC, Lee EK. Long working hours are associated with hypothyroidism: a cross-sectional study with population-representative data. Thyroid. (2020) 30:1432–9. doi: 10.1089/thy.2019.0709
33. Albehairy A, Fathy S, Bahriz R. Thyroid peroxidase antibody (TPO) as a predictor of radiation induced thyroid dysfunction among nurses and technicians working in Mansoura specialized medical hospital: cross sectional study. Endocr Metab Immune Disord Drug Targets. (2020) 20:288–94. doi: 10.2174/1871530319666190626143301
34. Albi E, Cataldi S, Lazzarini A, Codini M, Beccari T, Ambesi-Impiombato FS, et al. Radiation and thyroid cancer. Int J Mol Sci. (2017) 18:911. doi: 10.3390/ijms18050911
35. Rao D, Shah S. Thyroid dysfunction following management of non-thyroid head and neck cancers. Indian J Otolaryngol Head Neck Surg. (2019) 71:447–52. doi: 10.1007/s12070-018-1347-y
36. Ron E, Brenner A. Non-malignant thyroid diseases after a wide range of radiation exposures. Radiat Res. (2010) 174:877–88. doi: 10.1667/RR1953.1
37. Völzke H, Werner A, Wallaschofski H, Friedrich N, Robinson DM, Kindler S, et al. Occupational exposure to ionizing radiation is associated with autoimmune thyroid disease. J Clin Endocrinol Metab. (2005) 90:4587–92. doi: 10.1210/jc.2005-0286
38. Wu K, Zhou Y, Ke S, Huang J, Gao X, Li B, et al. Lifestyle is associated with thyroid function in subclinical hypothyroidism: a cross-sectional study. BMC Endocr Disord. (2021) 21:112. doi: 10.1186/s12902-021-00772-z
39. Cho A, Chang Y, Ahn J, Shin H, Ryu SJ. Cigarette smoking and thyroid cancer risk: a cohort study. Br J Cancer. (2018) 119:638–45. doi: 10.1038/s41416-018-0224-5
40. Bellastella G, Scappaticcio L, Caiazzo FG, Tomasuolo M, Carotenuto RM, Caputo M, et al. Mediterranean diet and thyroid: an interesting alliance. Nutrients. (2022) 14:4130. doi: 10.3390/nu14194130
41. Ruggeri RM, Giovinazzo S, Barbalace MC, Cristani M, Alibrandi A, Vicchio TM, et al. Influence of dietary habits on oxidative stress markers in Hashimoto's thyroiditis. Thyroid. (2020) 31:96–105. doi: 10.1089/thy.2020.0299
42. Vaivode I, Zake T, Strele I, Upmale-Engela S, Gogins D, Gersone G, et al. Stress-related immune response and selenium status in autoimmune thyroid disease patients. Int J Mol Sci. (2023) 24:2440. doi: 10.3390/ijms24032440
43. Tsatsoulis A. The role of stress in the clinical expression of thyroid autoimmunity. Ann N Y Acad Sci. (2006) 1088:382–95. doi: 10.1196/annals.1366.015
44. Hackney AC, Saeidi A. The thyroid axis, prolactin, and exercise in humans. Curr Opin Endocr Metab Res. (2019) 9:45–50. doi: 10.1016/j.coemr.2019.06.012
Keywords: abnormal thyroid function, radiotherapy, depression, stress, occupation exposure
Citation: Ren Z, Ren Y, Bai X, Shang P and Li G (2023) Analysis of factors associated with abnormal thyroid function among medical staff in radiotherapy departments. Front. Public Health 11:1225879. doi: 10.3389/fpubh.2023.1225879
Received: 20 May 2023; Accepted: 27 July 2023;
Published: 17 August 2023.
Edited by:
Jessica García González, University of Almeria, SpainReviewed by:
Raúl Romero Del Rey, University of Almeria, SpainIrma Melyani Puspitasari, Padjadjaran University, Indonesia
Copyright © 2023 Ren, Ren, Bai, Shang and Li. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Puyu Shang, MzQyNDM4MjA3QHFxLmNvbQ==; Guang Li, MTM4MDQwNTg2MTZAMTYzLmNvbQ==
 Ziwei Ren
Ziwei Ren Yanwei Ren2
Yanwei Ren2