- 1Faculty of Sports Science, Ningbo University, Ningbo, China
- 2Research Academy of Medicine Combining Sports, Ningbo No.2 Hospital, Ningbo, China
- 3Department of Government and International Studies, Hong Kong Baptist University, Kowloon Tong, Hong Kong SAR, China
- 4Section of General Internal Medicine, Yale School of Medicine, Yale University, New Haven, CT, United States
- 5Center for Pain, Research, Informatics, Medical Comorbidities and Education Center (PRIME), VA Connecticut Healthcare System, West Haven, CT, United States
- 6Department of Neurology, The First Affiliated Hospital, Sun Yat-Sen University, Guangzhou, China
- 7Department of Sports, Physical Education and Health, Hong Kong Baptist University, Kowloon Tong, Hong Kong SAR, China
- 8School of Sports and Health, Nanjing Sport Institute, Nanjing, China
- 9Centre for Health and Exercise Science Research, Hong Kong Baptist University, Kowloon Tong, Hong Kong SAR, China
Objectives: In this review, we aim to highlight the evidence base for the benefits of exercise in relation to the treatment of noncommunicable diseases (NCDs), draw on the Health Triangular Policy Framework to outline the principal facilitators and barriers for implementing exercise in health policy, and make concrete suggestions for action.
Methods: Literature review and framework analysis were conducted to deal with the research questions.
Results: Exercise prescription is a safe solution for noncommunicable diseases prevention and treatment that enables physicians to provide and instruct patients how to apply exercise as an important aspect of disease treatment and management. Combining exercise prescription within routine care, in inpatient and outpatient settings, will improve patients’ life quality and fitness levels.
Conclusion: Inserting exercise prescription into the healthcare system would improve population health status and healthy lifestyles. The suggestions outlined in this study need combined efforts from the medical profession, governments, and policymakers to facilitate practice into reality in the healthcare arena.
1. Introduction
The 2011 United Nations Declaration on Noncommunicable Diseases (NCDs) recognized the importance of NCDs as a global health issue, particularly for low- and middle-income countries (1). NCDs are highly prevalent, costly, and are responsible for more than 74% of deaths worldwide, totaling 41 million people each year (2). In all but 20 countries, prior to the Covid-19 pandemic individuals were at a greater risk of premature death from NCDs than from all communicable diseases, maternal problems, perinatal issues, and poor nutrition combined (3). An estimated 17 million people die globally from NCDs before the age of 70, and 86% of these recorded premature deaths occur in low- and middle-income countries (4, 5). The four main groups of NCDs are cardiovascular diseases, cancers, chronic respiratory diseases, and diabetes. These diseases are responsible for over 80% of premature NCD deaths. Disease onset has several underlying modifiable risk factors, including using tobacco, the use of excessive alcohol, sedentary behavior, and unhealthy diets (6). The patient suffering and family economic burden resulting from NCDs is associated with profound negative consequences for families, health care systems and countries (7). The United Nations has estimated that the burden of chronic disease cumulative cost to the global economy may reach $47 trillion by 2030 if current trends do not change (8). NCDs have been included in the Sustainable Development Goal (SDG) Target 3.4. This target has been established to reduce premature mortality by one-third by 2030, through improved NCDs treatment and prevention, in addition to promoting mental health and well-being (3, 9).
The beneficial impact of exercise on health has been well documented since the 5th century BC; this relationship has been investigated, defined and reinforced by many years of scientific research. The evidence indicates a strong and consistent positive association between exercise participation and health status (10–14). Many systematic reviews and meta-analyses have revealed the comprehensive benefits that can be obtained from physical exercise (15–19). Exercise as a validated methodology has endured the test of time and can help individuals develop healthy lifestyles (20). Exercise is also a proven applied intervention for addressing illness and improving health and wellness (21). For example, exercise has been used in both the prevention and treatment of many chronic conditions such as pulmonary disease, heart disease, obesity, and diabetes (22, 23). Each year, hundreds of billions of dollars are invested in healthcare provision for NCDs; exercise interventions can often provide similar and/or greater health benefits as those provided by pharmaceutical interventions, without most of the associated expenses or the problematic side-effects (24, 25). In some instances, exercise can complement and influence traditional medicine treatments while enhancing the medicinal positive effect (26). The World Health Organization provides general exercise guidelines and recommendations for different age groups and specific populations. These groups include postpartum and pregnant women, individuals that have chronic conditions, and the disabled. The guidelines outline in brief the quantity of physical activity that is required for health benefits (27). However, the guidance is not targeted for individual NCD patients and cannot be used to prescribe individualized specific exercise programmes.
Exercise prescription (EP), based on the findings of previous studies, can be defined as: written and structured instruction by supervised/medical staff that establishes and uses supported exercise programmes that are clearly defined and contain elements of exercise advice stating exercise type, intensity, duration and frequency. Prescribing exercise should also include the patient’s health, exercise ability and cardio-pulmonary function based on medical examination and treatment outcomes (24, 25). Exercise prescription can be implemented by clinical exercise physiologist and qualified exercise professional physicians in a variety of settings (28). However, an interview study completed at the national level in the United States revealed that only 32% of patients received advice about exercise or the benefits of continuing to be physically active during visits with a physician (29). Physician counselling and exercise prescription referrals may be helpful for reducing morbidity and mortality rates from NCDs (30). Unfortunately, most physicians, who are traditionally trained (pharmaceutically or medically) to manage noncommunicable disease have not been extensively trained in exercise prescription at their associated medical schools or healthcare institutions (30).
Enhancing primary health care using exercise prescription is a low-risk, cost-effective approach to maximize health benefits at population levels. For this to be achieved there is a requirement for medical systems to create the necessary infrastructure and environment to ensure that supervised exercise can be prescribed as medicine. Exercise prescription is an additional healthcare provision that enables physicians to support their patients to engage in exercise as part of their disease prevention and treatment (22). Realizing these benefits to health care needs to be facilitated by large-scale investment from governments, non-government organizations, and the private sectors (2). Healthcare systems around the world are highly disparate, and vary according to the level of development in a particular country, and in local and national public health service provision. For example, inequality in health services coverage is common across South Asia, and the service does not achieve the key global target of at least 80% of essential health care service coverage (2). A 2020 World Health Organization survey revealed that the ongoing COVID-19 pandemic was disrupting NCD services in 122 of 159 countries; the combination of COVID-19 and NCDs has had devastating consequences for many patients’ access to health systems (5). There needs to be a stronger political commitment, the development of institutional and human capacity, and creative sustainable solutions to finance health systems that offer the widespread provision of exercise prescription within medical services at affordable rates (2).
Most intervention and review studies designed around physical activity and exercise therapy are terminated at the efficacy trial stage, without transfer as best practices for clinical provision systems and public health policy-making processes (16, 18, 31–34). As the available evidence indicates that exercise is effective as a treatment for NCDs, exercise treatment should be sufficiently recognized as a stimulating and beneficial policy change in the healthcare and wellness agenda. In the previous two decades, numerous health policy studies have focused on how to manage and improve treatment performance and outcomes (35). However, public health policy changes can also be implemented to provide a strategy to create better conditions for population health.
Based on the narrative provided above, this article aims to provide evidence, and outline a feasible plan for consideration, to implement exercise as medicine for future NCDs medical treatment provision. This article has been divided into three main sections. First, the article outlines the evidence base underpinning exercise as a medicine for NCDs. Second, the article discusses the health policy-making process, drawing on the Health Triangular Policy Framework. Third, the article presents specific suggestions for exercise prescription in the medical provision system.
2. Methods
2.1. Literature review
A structured comprehensive search strategy was conducted using PubMed, Google Scholar, Embase, Web of Science, Scopus and ProQuest to identify publications in English using search terms in the titles and abstracts (search strategies were adjusted to fit different databased setting): ‘exercise prescription’, ‘exercise treatment’, ‘health policy’, ‘medical system’, ‘clinical provision’, ‘healthcare’, ‘inpatient’, ‘outpatient’, ‘noncommunicable diseases’, ‘cardiovascular diseases’, ‘cancer’, ‘respiratory diseases’, ‘diabetes’. The search process was focused on original studies and reviews articles (in peer-reviewed journals) over the last 15 years. Further related articles were identified from reference lists of retrieved articles; and authority data (e.g., WHO) that were also considered. A total of 76 articles were finally included and the literature search was completed on November 16, 2022.
2.2. Framework analysis
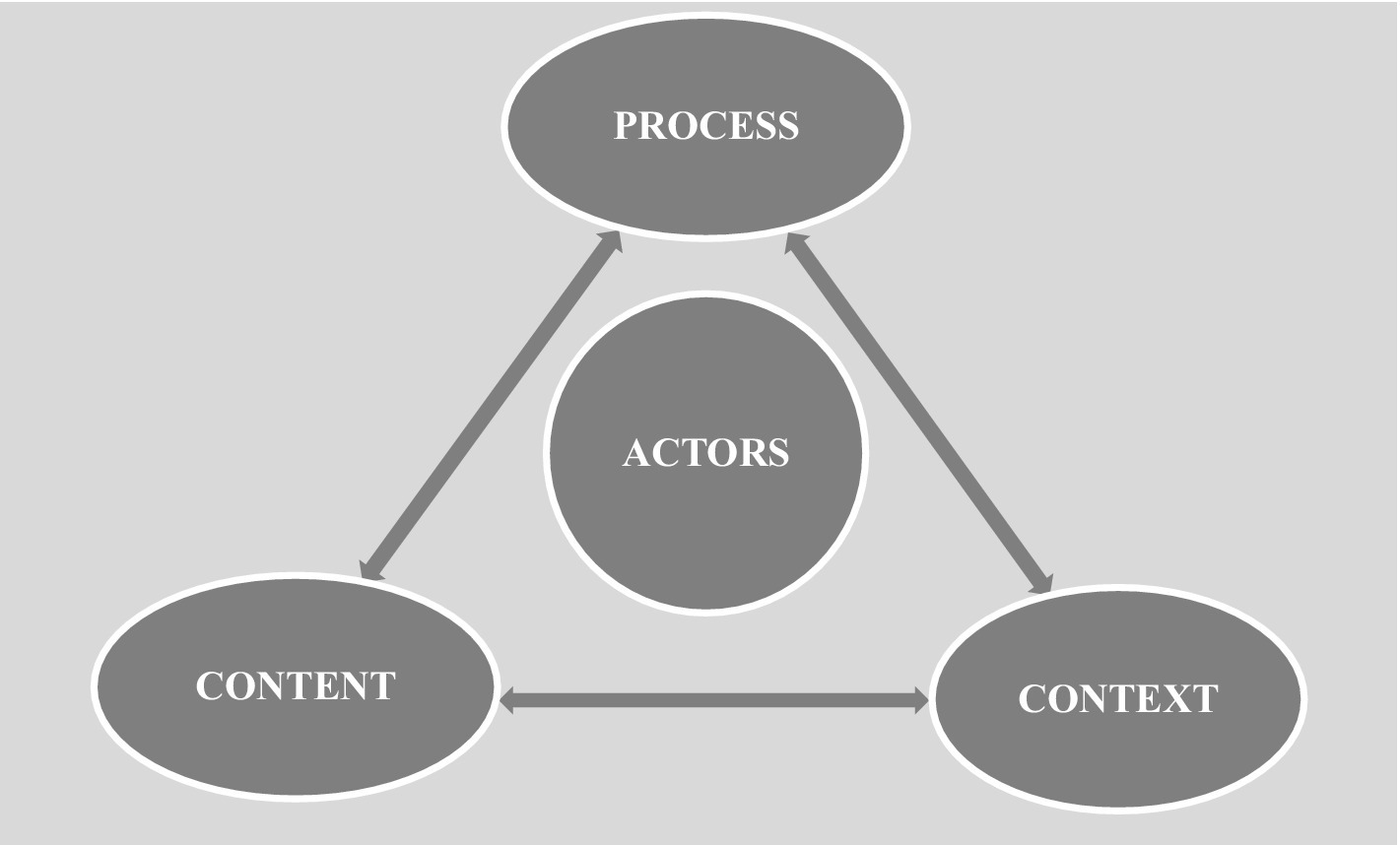
Our health policy-making analysis below is based around the Health Triangular Policy Framework (HPF) (36). The HPF was developed in 1994 by Wall and Gilson, and has been used in a retrospective or prospective manner to analyze many health-related policy issues (37). The framework highlights how policy implementation is influenced by the elements of policy Content, Context, and Process, and also emphasizes the influence of Actors on these three elements in the policy-making process (38). In the HPF, Content includes policy objectives, operational policies, legislation, regulations, and guidelines. Context refers to systemic factors: social, economic, political, cultural, and other environmental conditions. Process refers to the way in which policies are initiated, developed or formulated, negotiated, communicated, implemented, and evaluated. Actors refer to influential individuals (such as senior policy- and decision-makers), groups, and organizations (see Figure 1) (36). Studies have used this framework to analyze health policy issues in contexts as diverse as Kenya (39), Cambodia (40), and the Eastern Mediterranean regions (37).
3. Results
3.1. Exercise as a treatment for NCDs
Physical exercise is increasingly recognized as of importance in the primary medical care of at least 35 chronic diseases. Exercise not only reduces the risk of developing new chronic NCDs, but also decreases the progression of many existing chronic noncommunicable conditions while improving quality of life (41, 42). Specifically, the significance of exercise intervention as the first-line treatment for several chronic NCDs has been investigated extensively during the past two decades (26). Exercise may induce modifications in gene expression, and affect cardiovascular risk, musculoskeletal function, pulmonary function, hyperinsulinemia, sensitivity to insulin, oxygen consumption, fasting plasma/blood glucose intolerance, body fats, cholesterol, blood pressure, dosage of antidiabetic medications, immunity, sleep quality, self-satisfaction, and consequently general health and fitness. Furthermore, exercise can also improve aerobic capacity, and the mental health of patients (7, 17, 33, 34, 43).
Not everything is known, of course, and there remains important work to be done to explore the different types and dosage of exercise that are suitable for exercise prescription following specific diagnoses and conditions for NCD patient populations. A 2008 American College of Sports Medicine (ACSM) report noted, for example, that Moderate to Vigorous Physical Activity (MVPA) reduced breast and colon cancer risk. In 2018, the ACSM report was expanded to include more types of cancers whose risk was reduced by MVPA. These included endometrial, esophageal, kidney, lung, stomach, and bladder cancers (7, 41). Engagement in regular exercise activity is not only feasible and safe for cancer patients but also improves the tolerance for treatment, facilitates recovery, reduces the length of hospital stays, slows progression, and reduces risks associated with recurrence, readmission, and mortality (44).
3.2. Exercise intervention guidelines and education for NCD patients
The ‘Health Care Providers Action Guide’ was developed by the ACSM. It outlines six basic steps for working with health care providers and patients to facilitate and manage medical referrals, including assessment of the physical activity levels of patients, determination of patients’ readiness to change, prescription of exercise for patients, provision of patients’ physical activity referrals, and promotion of exercise in clinics (45). Several resources have also been developed, including exercise implementation tools, handouts, and patient reports. Examples such as physical activity algorithms with an initial assessment by a nurse or clinician, link into exercise prescription and patient education, concluding with suggested readings to encourage patients to change behavior from inactive to active (46). Adaptation of the physical activity algorithm into clinical practice allows for an opportunity to increase patients’ participation in their own health outcomes using a prescribed exercise routine. Similar forms of guidance have been developed by ACSM and other organizations: examples include ACSM guidelines on using exercise for cancer survivors (47); the Enhanced Recovery After Surgery (ERAS) programme (48); and the Pulmonary rehabilitation exercise prescription in chronic obstructive pulmonary disease guidelines etc. (49).
Exercise education and consultation are further relevant factors for patients with NCDs. The identification of patient intervention capacity and suitability can be achieved by considering the various contraindications and constraints, preferences, barriers and facilitators for exercise, and the potential benefits relevant to them, whether those be physiological, psychosocial or economic (50). Further steps, aims and objectives of exercise need to be prioritized according to the most valuable outcome for the patients (e.g., symptom management, improving mood, minimizing a decline in cardiorespiratory fitness, reversing loss of muscle mass, survival etc.). Therefore, it is essential to provide the patients with information relating to the exercise components that are necessary for achieving specific goals. It is worth noting here that some may prioritize long-term exercise benefits over short-term goals, physiological over psychosocial or functional benefits, and that the goals and priorities for many will likely change over time (50). The flexibility of exercise education and consultation are particularly important when patient exercise preferences fail to align with achieving their desired goals (50). Physical exercise education and consultation are facilitators for NCDs patients to participate in exercise programmes. The skills and knowledge developed by patient education and exercise guidelines may provide confidence and competence in minimizing adverse reactions to related individual medical situations, such as the fear of hypoglycemia. Additionally, health professional training and improving community engagement is also essential in exercise prescription support following discharge, based on the physician’s guidance (51).
3.3. Multidisciplinary team care
The scope of exercise prescription practice is dynamic and can be responsive to the needs of patients and society. The ideal condition is for health services to provide adequate recognition and support for interdisciplinary intervention through proper legislation and policies (52). Unstructured referral from physicians deprives patients of medical services such as diagnosis, health promotion, and complication prevention (53). The most significant considerations for implying multidisciplinary team care are cost and convenience (54). In primary care, physicians, nurses, physiotherapists, and other health professionals working together in a medical services team is an effective strategy to achieve multidisciplinary health service goals. Furthermore, at the primary health care level, organizing people-centered integrated health services that are safe for patients and of assured quality with effective referral networks between basic health care and hospital care is essential (53, 55, 56). Multidisciplinary practice can be aided by standardized procedures, policies, and regulations. Furthermore, the organizational structure of service delivery and clinical responsibilities suggests that it can be responsive to the needs of patients and communities rather than practitioner-led delivery (53).
Health clubs and personal trainers are traditional outlets for the promotion of physical activity and exercise regimens, and physicians are not depending on these partnerships to promote physical activity to their patients in a sufficient manner (54). Not only is inter-hospital collaboration required, collaboration between physicians and community practitioners is an important link for patients with NCDs after they leave the clinic or are discharged from the hospital (54). Fostering multisectoral public and commercial partnerships that bring together government and society to promote health policies is vital to address concerns such as financing, accessibility, efficiency, and the quality of health care (57).
3.4. Barriers to exercise prescription implementation
From a patient perspective, common reasons for non-adherence to exercise prescription include physical and psychosocial factors such as patient missed sessions, dropouts because of wellness problems, hospital readmissions, disease progressions, adverse skeletal events, or a paucity of interest, motivation, knowledge and/or confidence (24, 44, 51, 58). From an institutional and physician perspective, major barriers for service integration are related to limited funding, lack of a detailed implementation plan, limited availability of suitable programmes, and low organizational buy-in (lack of public funding and resources). In addition, the physicians’ characteristics of lacking exercise science educational backgrounds, related knowledge, and specific professional qualifications have also been noted as detrimental (24, 32, 44, 51, 58). Furthermore, in real work situations the lack of time for counselling, workload pressures, and extra work concerns, would all disrupt clinic efficiency and have been identified as related issues contributing to barriers for providing exercise prescription to patients (58). Some accessibility barriers related to location, cost and exercise schedules coinciding with treatment days have also been identified. In addition, political and economic context arrangements, such as minimal structured reimbursement policies; and barriers related to collaboration and leadership with stakeholder and other actor groups in social context are also issues that cannot be ignored (58).
3.5. Related examples
Among the documented international examples of effective uses of exercise in the prevention and treatment of NCDs are the following three initiatives:
• Singapore has adapted a systematic approach for integrating exercise as medicine into the disease and management pathway. This resulted in the design of an Exercise as Medicine template, and progressively incorporated the Physical Activity Vital Sign (PAVS) structure into electronic case notes in numerous departments at Changi General Hospital. The mainstay of Exercise is Medicine (funded in 2007 by the American College of Sports Medicine) in the Singapore development is to train physicians in the prescription of exercise (22).
• Another example is the implementation of tailored exercise interventions for women following breast cancer diagnosis in Brisbane, Australia. A supervised exercise intervention led to significant improvements in fitness parameters and significant decreases in breast cancer health care utilization (32) This provided a cost-effective treatment compared to usual care with eight-year follow-up (59).
• A further example comes from the Jewish General Hospital, Montreal, Quebec. During the operation of a Rehabilitation and Exercise Oncology model of care (ActivOnco), patients were encouraged to participate in exercise based on individual goals and preferences in a group environment or individual setting (60). Most of the referrals (71%) came from members of the multidisciplinary team, including nutritionists, nurse coordinators, social workers, and treating oncologists (60). The programme benefited from easy access to medical records, and interaction with medical teams providing constant updates on the treatment and medical status for patients and patients’ families (50).
3.6. Health policy analysis
Health policy design comprises a set of decisions, plans and actions taken within a society to achieve a specific healthcare goal, or a set of actions taken by an agency or organization at the national, regional or local levels of government to promote public health (36). Based on the evidence discussed above we can reasonably claim that NCDs patients would be greatly advantaged by a healthcare system shift in conceptualization toward an exercise health promotion initiative, including re-orientation of the general practice environment and collaboration with exercise professionals in inpatient and outpatient provision. At a societal level, healthcare support includes developing practical infrastructure, equipment base and peer networks; and improvements in the confidence of patients for exercise interventions, making them more receptive to exercise prescription. The following table outlines the health policy-making analysis for implementation of exercise prescription in regard to NCDs (See Table 1).
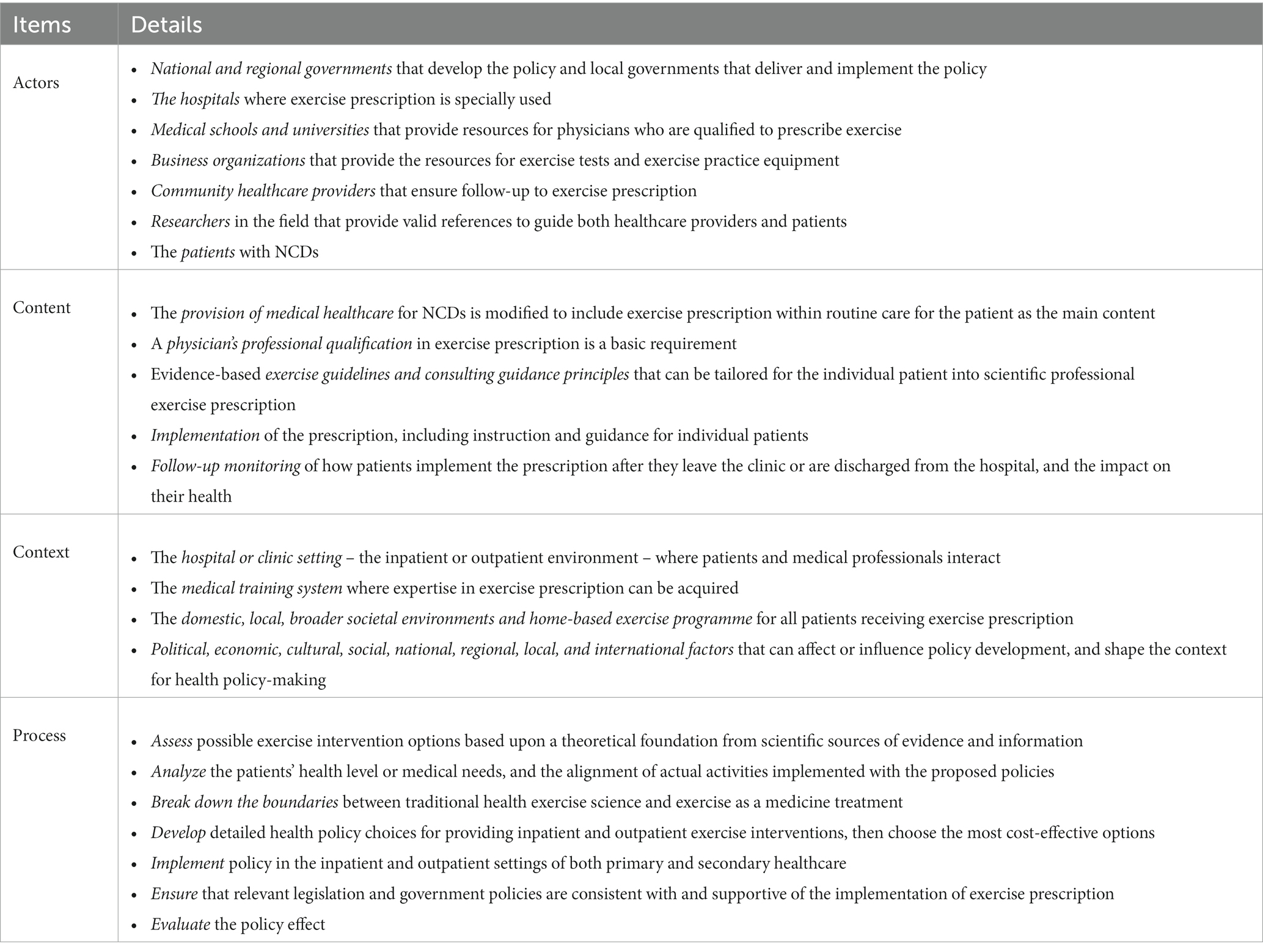
Table. 1. The health policy-making analysis for implementation of exercise prescription into the noncommunicable diseases medical provision based on the health triangular policy framework.
4. Discussion
4.1. Applying a formal exercise prescription curriculum in the physician training system
There is evidence that providing effective exercise guidance for patients can help increase physical activity levels and decrease disease rates, thereby reducing the financial burden on governments (28). However, exercise prescription or physical activity advice for patients with NCDs are not included in the academic curriculum of most medical professionals (30, 61, 62). A previous survey outlined a lack of formal undergraduate medical education knowledge related to the medical benefits of exercise and physical activity in 1975. Subsequent surveys since 1975 have demonstrated little improvement (30). For example, most US medical students do not have the competence, skills, or confidence to counsel patients on exercise prescription following graduation (30). It is essential that newly qualified physicians are aware of the role that exercise as medicine can play in treating and preventing disease. A more recent study reported that exercise guidelines and exercise prescription education programmes provide the tools and knowledge to assess properly patients’ activity levels and offer individualized recommendations, while also increasing practitioner confidence to engage in exercise prescription (28).
Physicians may lack knowledge and confidence to prescribe exercise as medicine because of the paucity of detailed instruction in medical schools (63). Training and education for physicians on the benefits of different modes of exercise prescription, and how to structure exercise intervention to each patient’s needs, can empower them with confidence and knowledge (28). Conceptualization and implementation of an exercise prescription medical education course is needed to provide health care staff with the ability to assess, counsel, and refer patients for physical activity and exercise. This development is crucial to prevent and treat chronic noncommunicable diseases and is required urgently (22). Exercise prescription training needs to be integrated into most of phases of medical education, and can be facilitated in medical schools, residency programmes, credentialing processes and continuing education requirements (30). The development and implementation of professional standards must include performance and ethics, standards of conduct, and core clinical skills. They need to be established under a standards development framework in which all aspects are evidence-based, benchmarked against international standards such as those of the American College of Sports Medicine, and consistent with the needs of patients and practitioners (61). Assessment of the quality of education and training programmes is also required, to ensure they give clinical exercise physiology graduates the skills and knowledge to practice safely and competently. A university curricula programme accreditation framework should be developed based on current national health service provision models (61). There may also be a need to include specialized mandatory courses and conduct an evaluation of exercise prescription within the physicians’ final examination for the degree.
There is also a requirement to develop physicians’ communication skills to enable them to guide patients in the behavioral change scenarios of exercise adaptation and maintenance in daily life. Furthermore, physicians need to be encouraged to engage with community physical activity/exercise resources, which is consistent with the evolution of patient-centered care (30). When medical students graduate, they should be able to demonstrate proficiency in the prescription of exercise and assessment; and should also be knowledgeable about the principles of exercise counselling and behavioral strategies related to patients’ personal health (30). Additionally, developing collaborations between medical schools/universities and healthcare institutions not only provides more exercise medicine practical information, but also provides internship opportunities.
There is a programme available in the US called Exercise is Medicine Greenville (EIMG). This is the first partnership engaging a medical school, a health care system, and a community organization combining resources collectively to educate physicians on the clinical benefits of exercise (22). Several universities have now successfully incorporated sports and exercise medicine into their medical curriculum in places as diverse as Colombia, South Carolina, the United Kingdom, and Iran. These curricula have included a focus on exercise medicine and how to successfully prescribe exercise for patients (30, 64–67). This extensive system needs further development, consolidation, expansion, and exploration as a model of best practice.
4.2. Guarantee adequate exercise medicine resources
The installation of an exercise prescription facility within existing NCDs medical care provision settings may require slight infrastructural adjustment to ensure the availability of suitable spaces, and any necessary equipment, to provide instruction in different forms of exercise. There will also be a need for the hiring of experienced exercise science specialists, and medical staff who possess exercise prescription skills. A concerted effort is required to identify and develop the correct implementation strategies to stimulate a cultural shift and debate in the host organization (44).
Exercise testing is necessary when health/fitness and clinical exercise professionals are concerned about individuals’ risk, or when they require additional information to design exercise prescription (68). An 18-year cross-sectional study provided data on the safety of clinical Chinese population-based exercise testing, and was expressed as the number of adverse events per 10,000 tests (using 95% confidence intervals). These results suggested that clinical exercise testing was safe and that the low incidence of adverse events recorded might be due to the overall changes in clinical practice over time (69). In real practice, the clinical exercise test would need to meet three important aspects: address patients’ needs, be time efficient, and be cost-effective. NCDs patients should be screened using a health risk appraisal questionnaire or a self-reported medical history (including patients and family health history, comorbidities, additional chronic diseases and related treatments, and physical activity and exercise history). An example would be the modified American Heart Association/ACSM Health/Fitness Facility Preparticipation Screening Questionnaire (41) for the presence of risk factors for various cardiovascular, pulmonary, renal, and metabolic diseases as well as other conditions such as pregnancy and orthopedic injury that require special attention when developing exercise prescription. Further medical evaluation measures, including blood pressure, heart rate and some anthropometric indicators should also be conducted to determine any health issues that contribute to risks of morbidity and/or mortality. Physical activity assessment needs to be incorporated into standard medical examination routines during clinical visiting and as part of the treatment plan (22). This recommendation should be considered not only for patients at high risk of exercise-related complications; regular exercise testing should be recommended for all patients prior to participating in a light- to moderate-intensity exercise programme (68). Evidence-based, specific, and valid measures of physical status would aid physicians in examination and discussion of exercise prescription with patients (70).
Technology-based support, such as mobile-technology, wearable devices, texts, and emails, improves compliance among patients and has been validated previously (31, 71–73). Suggestions to design and develop special software/applications to enhance exercise prescription adherence are gaining momentum. Digital support tools can be used for the purpose of including information such as the patient’s medication history, illness, and physical fitness levels; follow-ups using remote monitoring after outpatient’s service or discharge should be attractive to many healthcare systems and providers. Using these methodologies, patients can live at home and by using multiple intelligent devices communicate with the physician to access supervision and instructions. This communication helps with follow-up over the next weeks or months to monitor compliance with exercise prescription and provide encouragement. This method can also expand the opportunities for increased accuracy and acceptance of exercise intervention. Remote consultation is also featured by consistency and regularity, low cost and acceptability to the patient’s family. In addition to the digital health system mentioned previously, the workflows for exercise prescription will need to be compatible with existing workflows and working procedures to limit burdens and increase efficiency (24).
Community exercise resources are another important component for effective exercise continuation in compliance with physician’s instructions following discharge. Health providers and physicians will often wish to refer patients to community resources to integrate exercise into their daily lives. These include the use of self-directed resources, such as public sports facilities, bike-sharing programmes, and the use of local parks (22). Aligning community and healthcare partners to provide a clinic-to-community model may be beneficial for implementing exercise as a core prevention strategy for assisting patients who are at risk for NCDs, to regress, reverse, and minimise the progression of disease (74).
4.3. Effective evaluation for exercise prescription implementation
For general practitioners and fitness related personnel, focusing on the theoretical study and practical operation of exercise interventions for NCDs needs to be re-evaluated. The potential way to ensure the quality of exercise prescription is the development of an exercise prescription credential to recognize qualified and certified fitness professionals who work with patients referred from health care providers (22). This includes medical practice, health care knowledge, NCDs prevention and treatment, exercise rehabilitation, and scientific exercise understanding. Follow-up evaluation after the implementation of the policy should not be ignored, and investigations and surveys should be conducted to further determine the effectiveness of exercise prescription implementation, as well as patients’ confidence levels and intervention effects.
4.4. Including exercise prescription into medical insurance programmes
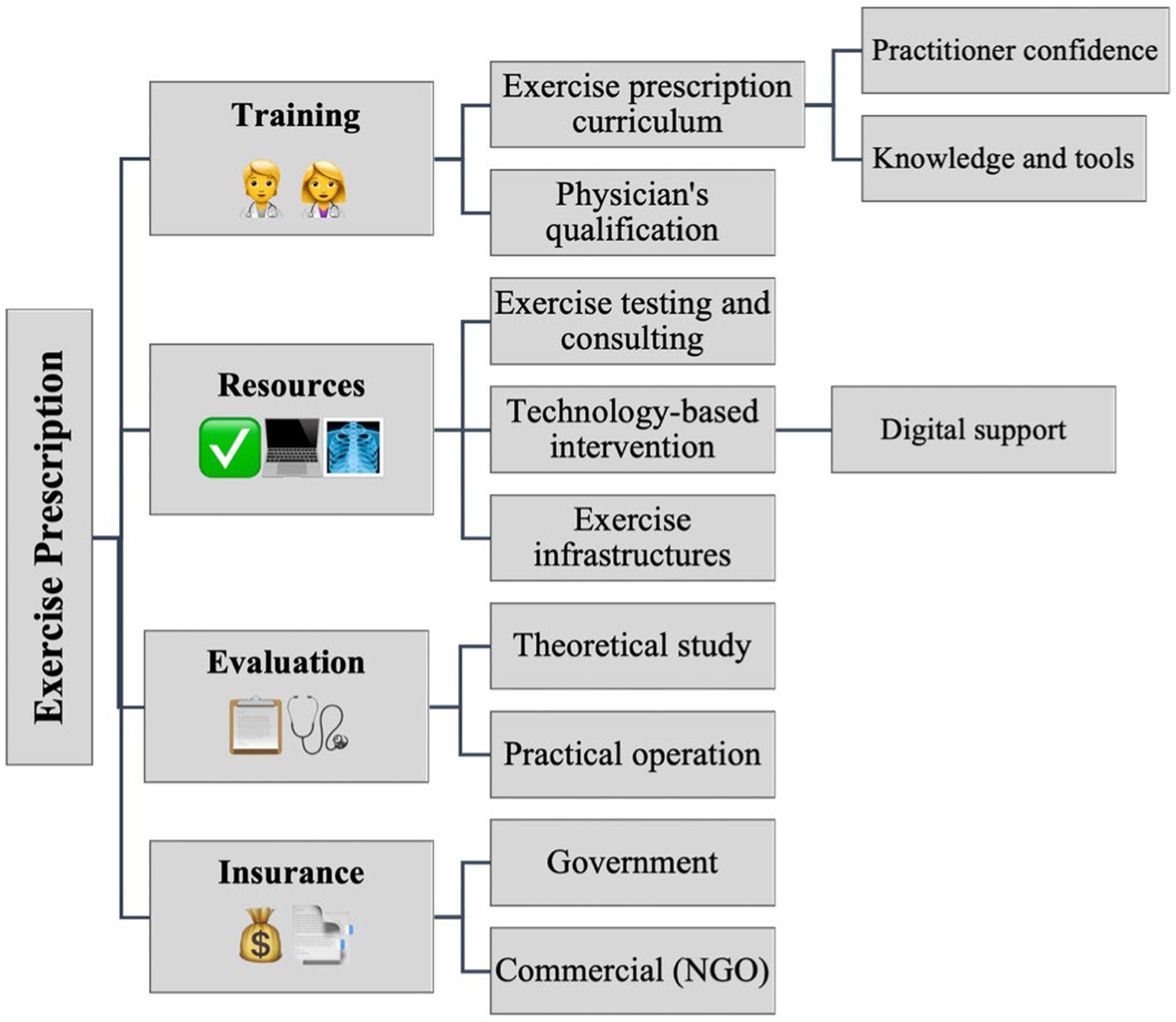
Achieving universal health coverage (UHC) is a sub-target of the Sustainable Development Goals (SDGs) (36). The acceptance and coverage of government universal medical insurance and commercial insurers to include exercise prescription in the claim for reimbursement is the cornerstone of long-term development of exercise prescription. Medical insurance system support is essential for physicians and patients to adhere to exercise prescription. If medical insurance policies generally provide more reimbursement for inpatient care, this incentivizes patients to use hospital resources for even minor health conditions, and therefore inhibits healthcare treatment from primary clinics (75). The government’s healthcare policy could support the treatment of most NCDs in outpatient settings. This would provide savings in medical resources and medical expenses and improve the health level of the entire population in the long term. In addition, this provision would increase the treatment capacities of related hospitals and healthcare establishments. For example, outpatient medical body checks/tests related to patient symptoms and physical exercise ability, should be part of every physician’s exercise prescription, and follow-up exercise medical assistance should be reimbursed as usual. The implementation of exercise prescription in clinical provision would reduce the expenditure of drugs, intravenous infusion therapy and inpatient care. On the other hand, it also indirectly reduces the expenses of inpatient medical reimbursement and provides a virtuous healthy cycle. Nevertheless, medical insurance policies should set a limited coverage for exercise prescription in primary health care/clinic provision, by means of setting a maximum limit for total reimbursement, to avoid over-use of medical services. Figure 2 provides a general outline of the suggestions of implementation of exercise prescription.
5. Conclusion
Based on the available evidence, exercise is a powerful intervention to prevent and manage NCDs, improve patients’ life quality and mitigate the effects of chronic diseases, and lower mortality rates. Exercise prescription is a non-pharmaceutical health intervention and should be promoted in combination with traditional medical support. Individual patients will be at different stages of readiness to participate in exercise, and each will present with different unique health and environmental challenges, so the individual prescription of exercise recommendation is necessary and beneficial. This review summaries the evidence and suggestions for implementing exercise prescription into the NCDs medical healthcare provision. The information provided here also identifies barriers that need to be overcome for success in implementation of the health policy-making process. There is a paucity of studies documenting the process of exercise as medicine in different and varied healthcare settings. This gap creates difficulties for providers, in the selection and choice of appropriate strategies at organizational levels that recognize the factors enabling the adaption and development of new working methods. Healthcare professionals also need to be aware that prescribing exercise as medicine in one particular setting may not be applicable and beneficial in the same way when implemented elsewhere. Medical practitioners need to select and modify appropriate and useful strategies at each organizational level, recognizing the combination of factors that enable development and adoption of new working practices.
Inserting exercise prescription into the healthcare system would improve population health status and healthy lifestyles. We have attempted to link the literature to the structure of the specific policy-making process, bridging the gap from theory to practical implication suggestions. Following the scientific policy-making process and suggestions, we need to keep the general alignment between policy and practice to ensure long-term success, effective implementation, and delivery. The suggestions outlined in this study need combined efforts from the medical profession, governments, and policymakers to facilitate practice into reality in the healthcare arena.
Author contributions
DT performed writing-original draft, conceptualization, and data interpretation. DT and JSB performed the literature searches and contributed to the screening process and selection of included studies. DT, RA-S, GIA, and JSB performed writing-review and editing, verification. ZP, YDG, YG, AC, RS, YS, and RX provided critical feedback on the protocol. YDG performed project administration. All authors contributed to the article and approved the submitted version.
Funding
This work was supported by the Research Academy of Medicine Combining Sports, Ningbo (No.2023001), the Project of NINGBO Leading Medical & Health Discipline (No.2022-F15, No.2022-F22). GIA was supported by the National Institute of Diabetes, Digestive, and Kidney Diseases of the National Institutes of Health under a mentored research scientist development award (K01DK129441).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Hosseinpoor, AR, Bergen, N, Kunst, A, Harper, S, Guthold, R, Rekve, D, et al. Socioeconomic inequalities in risk factors for non communicable diseases in low-income and middle-income countries: results from the world health survey. BMC Public Health. (2012) 12:912. doi: 10.1186/1471-2458-12-912
2. Hills, AP, Misra, A, Gill, JMR, Byrne, NM, Soares, MJ, Ramachandran, A, et al. Public health and health systems: implications for the prevention and management of type 2 diabetes in South Asia. Lancet Diabetes Endocrinol. (2018) 6:992–1002. doi: 10.1016/S2213-8587(18)30203-1
3. Bennett, JE, Stevens, GA, Mathers, CD, Bonita, R, Rehm, J, Kruk, ME, et al. NCD countdown 2030: worldwide trends in non-communicable disease mortality and progress towards sustainable development goal target 3.4. Lancet. (2018) 392:1072–88. doi: 10.1016/S0140-6736(18)31992-5
4. WHO . Noncommunicable diseases. (2022). Available at:: https://www.who.int/news-room/fact-sheets/detail/noncommunicable-diseases.
5. Marten, R, Mikkelsen, B, Shao, R, Dal Zennaro, L, Berdzuli, N, Fernando, T, et al. Committing to implementation research for health systems to manage and control non-communicable diseases. Lancet Glob Health. (2021) 9:e108–9. doi: 10.1016/S2214-109X(20)30485-X
6. Kaldor, JC, Thow, AM, and Schönfeldt, H. Using regulation to limit salt intake and prevent non-communicable diseases: lessons from South Africa’s experience. Public Health Nutr. (2019) 22:1316–25. doi: 10.1017/S1368980018003166
7. Pedersen, BK . The physiology of optimizing health with a focus on exercise as medicine. Annu Rev Physiol. (2019) 81:607–27. doi: 10.1146/annurev-physiol-020518-114339
8. Duff-Brown B . Non-communicable disease could cost global economy $47 trillion by 2030. (2017), Available at: https://globalhealthsciences.ucsf.edu/news/non-communicable-disease-could-cost-global-economy-47-trillion-2030#:~:text=Non-communicable%20Disease%20Could%20Cost%20Global%20Economy%20%2447%20Trillion%20by%202030,-By%20Beth%20Duff.
9. David Watkins, HR . NCD countdown 2030: efficient pathways and strategic investments to accelerate progress towards the sustainable development goal target 3.4 in low-income and middle-income countries. Lancet. (2022) 399:1266–78. doi: 10.1016/S0140-6736(21)02347-3
10. Tao, D, Gao, Y, Li, F, Liang, W, Jiao, J, Huang, W, et al. Physical education provision in schools. A role for dance. Phys Act Health. (2022) 6:38–41. doi: 10.5334/paah.137
11. Sun, Y, Gao, Y, Yu, S, Wang, A, Ou, X, Tao, D, et al. Promoting physical activity among workers: a review of literature and future directions on developing theory-based interventions. Int J Environ Res Public Health. (2022) 19:13594. doi: 10.3390/ijerph192013594
12. Yu, S, Gao, Y, Wang, A, Sun, Y, Wang, J, Kwok, HHM, et al. Effectiveness of an adapted physical activity intervention for weight management in adolescents with intellectual disability: a randomized controlled trial. Pediatr Obes. (2022) 17:e12882. doi: 10.1111/IJPO.12882
13. Baker, JS, Cole, A, Tao, D, Li, F, Liang, W, Jiao, J, et al. The preventive role of exercise on the physiological, psychological, and psychophysiological parameters of coronavirus 2 (SARS-CoV-2): a mini review. J Risk Financ Manag. (2021) 14:476. doi: 10.3390/jrfm14100476
14. Dan, T, Yeheng, H, Alistair, C, Roger, AS, Rashmi, S, Yang, G, et al. The benefits of heart rate variability (HRV) in the assessment of health and exercise performance. Imag J Clin Med Sci. (2022) 9:011–4. doi: 10.17352/2455-8702.000136
15. Scott, JM, Zabor, EC, Schwitzer, E, Koelwyn, GJ, Adams, SC, Nilsen, TS, et al. Efficacy of exercise therapy on cardiorespiratory fitness in patients with Cancer: a systematic review and Meta-analysis. J Clin Oncol. (2018) 36:2297–305. doi: 10.1200/JCO.2017.77.5809
16. Bekhet, AH, Abdallah, AR, Ismail, HM, Genena, DM, Osman, NA, el Khatib, A, et al. Benefits of aerobic exercise for breast cancer survivors: a systematic review of randomized controlled trials. Asian Pac J Cancer Prev. (2019) 20:3197–209. doi: 10.31557/APJCP.2019.20.11.3197
17. Shawahna, R, Batta, A, Jomaah, M, and Abdelhaq, I. Exercise as a complementary medicine intervention in type 2 diabetes mellitus: a systematic review with narrative and qualitative synthesis of evidence. Diabetes Metab Syndr. (2021) 15:273–86. doi: 10.1016/j.dsx.2021.01.008
18. O'Donoghue, G, Blake, C, Cunningham, C, Lennon, O, and Perrotta, C. What exercise prescription is optimal to improve body composition and cardiorespiratory fitness in adults living with obesity? A network meta-analysis. Obes Rev. (2021) 22:e13137. doi: 10.1111/obr.13137
19. Tao, D, Gao, Y, Cole, A, Baker, JS, Gu, Y, Supriya, R, et al. The physiological and psychological benefits of dance and its effects on children and adolescents: a systematic review. Front Physiol. (2022) 13:1–13. doi: 10.3389/fphys.2022.925958
20. Chéour, S, Chéour, C, Gendreau, T, Bouazizi, M, Singh, KP, Saeidi, A, et al. Remediation of cognitive and motor functions in Tunisian elderly patients with mild Alzheimer’s disease: implications of music therapy and/or physical rehabilitation. Front Aging Neurosci. (2023) 15:1216052. doi: 10.3389/FNAGI.2023.1216052
21. Tao, D, Supriya, R, Gao, Y, Li, F, Liang, W, Jiao, J, et al. Dementia and dance: medication or movement? Phys Act Health. (2021) 5:250–4. doi: 10.5334/paah.138
22. Thompson, WR, Sallis, R, Joy, E, Jaworski, CA, Stuhr, RM, and Trilk, JL. Exercise Is Medicine. Am J Lifestyle Med. (2020) 14:511–23. doi: 10.1177/1559827620912192
23. Sallis, R . Exercise is medicine: a call to action for physicians to assess and prescribe exercise. Physic Sportsmed. (2015) 43:22–6. doi: 10.1080/00913847.2015.1001938
24. O’Regan, A, Pollock, M, D’Sa, S, and Niranjan, V. ABC of prescribing exercise as medicine: a narrative review of the experiences of general practitioners and patients. BMJ Open Sport Exerc Med. (2021) 7:e001050. doi: 10.1136/bmjsem-2021-001050
25. Tao, D, Awan-Scully, R, Cole, A, Gao, Y, Ash, GI, Gu, Y, et al. Integration of exercise prescription into medical provision as a treatment for non-communicable diseases: a scoping review. Front Public Health. (2023) 11:1126244. doi: 10.3389/fpubh.2023.1126244
26. Pedersen, BK, and Saltin, B. Exercise as medicine - evidence for prescribing exercise as therapy in 26 different chronic diseases. Scand J Med Sci Sports. (2015) 25:1–72. doi: 10.1111/sms.12581
27. WHO . Physical activity. (2022). Available at: https://www.who.int/news-room/fact-sheets/detail/physical-activity.
28. Kyei-Frimpong, J, Blood-Siegfried, J, Wijetilaka, R, and Gendler, A. Exercise as medicine: providing practitioner guidance on exercise prescription. Prev Med Rep. (2021) 22:101323. doi: 10.1016/j.pmedr.2021.101323
29. Barnes, PM, and Schoenborn, CA. Trends in adults receiving a recommendation for exercise or other physical activity from a physician or other health professional. NCHS Data Brief. (2012):1–8.
30. Trilk, JL, and Phillips, EM. Incorporating “exercise is medicine” into the university of South Carolina school of medicine Greenville and Greenville health system. Br J Sports Med. (2014) 48:165–7. doi: 10.1136/bjsports-2013-093157
31. Ash, GI, Stults-Kolehmainen, M, Busa, MA, Gregory, R, Garber, CE, and Liu, J. Establishing a Global Standard for Wearable Devices in Sport and Fitness: Perspectives from the New England Chapter of the American College of Sports Medicine Members. Curr Sports Med Rep. (2020) 19:45–9. doi: 10.1249/JSR.0000000000000680
32. Wonders, KY, Schmitz, K, Wise, R, and Hale, R. Cost-savings analysis of an individualized exercise oncology program in early-stage breast Cancer survivors: a randomized clinical control trial. JCO Oncol Pract. (2022) 18:e1170–80. doi: 10.1200/OP.21.00690
33. Gronek, P, Wielinski, D, Cyganski, P, Rynkiewicz, A, Zając, A, Maszczyk, A, et al. A review of exercise as medicine in cardiovascular disease: pathology and mechanism. Aging Dis. (2020) 11:327–40. doi: 10.14336/AD.2019.0516
34. Kruse, NT, and Scheuermann, BW. Cardiovascular responses to skeletal muscle stretching: “stretching” the truth or a new exercise paradigm for cardiovascular medicine? Sports Med. (2017) 47:2507–20. doi: 10.1007/s40279-017-0768-1
35. Reibling, N, Ariaans, M, and Wendt, C. Worlds of healthcare: a healthcare system typology of OECD countries. Health Policy. (2019) 123:611–20. doi: 10.1016/j.healthpol.2019.05.001
36. O'Brien, GL, Sinnott, SJ, Walshe, V, Mulcahy, M, and Byrne, S. Health policy triangle framework: narrative review of the recent literature. Health Policy Open. (2020) 1:100016. doi: 10.1016/j.hpopen.2020.100016
37. Behzadifar, M, Ghanbari, MK, Ravaghi, H, Bakhtiari, A, Shahabi, S, Doshmangir, L, et al. Health policy analysis in eastern Mediterranean region using a health policy triangle framework: historical and ethical insights from a systematic review. J Prev Med Hyg. (2022) 63:E351–73. doi: 10.15167/2421-4248/jpmh2022.63.2.2450
38. Molete, M, Stewart, A, Bosire, E, and Igumbor, J. The policy implementation gap of school oral health programmes in Tshwane, South Africa: a qualitative case study. BMC Health Serv Res. (2020) 20:338. doi: 10.1186/s12913-020-05122-8
39. Shiroya, V, Neuhann, F, Müller, O, and Deckert, A. Challenges in policy reforms for non-communicable diseases: the case of diabetes in Kenya. Glob Health Action. (2019) 12:1611243. doi: 10.1080/16549716.2019.1611243
40. Khim, K, Ir, P, and Annear, PL. Factors driving changes in the design, implementation, and scaling-up of the contracting of health services in rural Cambodia, 1997–2015. Health Syst Reform. (2017) 3:105–16. doi: 10.1080/23288604.2017.1291217
41. Thompson, PD, Baggish, AL, Franklin, B, Jaworski, C, and Riebe, D. American College of Sports Medicine expert consensus statement to update recommendations for screening, staffing, and emergency policies to prevent cardiovascular events at health fitness facilities. Curr Sports Med Rep. (2020) 19:223–31. doi: 10.1249/JSR.0000000000000721
42. Rustler, V, Hagerty, M, Daeggelmann, J, Marjerrison, S, Bloch, W, and Baumann, FT. Exercise interventions for patients with pediatric cancer during inpatient acute care: a systematic review of literature. Pediatr Blood Cancer. (2017) 64:1–5. doi: 10.1002/pbc.26567
43. Tao, D, Gao, Y, Li, F, et al. Physical inactivity, COVID-19, and the future of Global Health. Is Dancing the Solution? J Phys Act Res. (2021) 7:7–9. doi: 10.12691/jpar-7-1-2
44. Ezenwankwo, EF, Nnate, DA, Usoro, GD, Onyeso, CP, Anieto, IB, Ibeneme, SC, et al. A scoping review examining the integration of exercise services in clinical oncology settings. BMC Health Serv Res. (2022) 22:236. doi: 10.1186/s12913-022-07598-y
45. Exercise is Medicine . Health care providers action guide. American College of Sports Medicine , Available at: https://www.exerciseismedicine.org/eim-in-action/health-care/health-care-providers/provider-action-guide/
46. Austin, A, Damani, S, and Bevers, T. Clinical approach for patient-centered physical activity assessment and interventions. Clin J Oncol Nurs. (2016) 20:S2–7. doi: 10.1188/16.CJON.S2.3-7
47. Schmitz, KH, Courneya, KS, Matthews, C, Demark-Wahnefried, W, Galvão, DA, Pinto, BM, et al. American college of sports medicine roundtable on exercise guidelines for cancer survivors. Med Sci Sports Exerc. (2010) 42:1409–26. doi: 10.1249/MSS.0b013e3181e0c112
48. Scott, MJ, Baldini, G, Fearon, KCH, Feldheiser, A, Feldman, LS, Gan, TJ, et al. Enhanced recovery after surgery (ERAS) for gastrointestinal surgery, part 1: pathophysiological considerations. Acta Anaesthesiol Scand. (2015) 59:1212–31. doi: 10.1111/aas.12601
49. Garvey, C, Bayles, MP, Hamm, LF, Hill, K, Holland, A, Limberg, TM, et al. Pulmonary rehabilitation exercise prescription in chronic obstructive pulmonary disease: review of selected guidelines: an official statement from the American association of cardiovascular and pulmonary rehabilitation. J Cardiopulm Rehabil Prev. (2016) 36:75–83. doi: 10.1097/HCR.0000000000000171
50. Hayes, SC, Newton, RU, Spence, RR, and Galvão, DA. The exercise and sports science Australia position statement: exercise medicine in cancer management. J Sci Med Sport. (2019) 22:1175–99. doi: 10.1016/j.jsams.2019.05.003
51. Brennan, MC, Brown, JA, Ntoumanis, N, and Leslie, GD. Barriers and facilitators of physical activity participation in adults living with type 1 diabetes: a systematic scoping review. Appl Physiol Nutr Metab. (2021) 46:95–107. doi: 10.1139/apnm-2020-0461
52. Interdisciplinary Chronic Disease Collaboration . The research to health policy cycle: a tool for better management of chronic noncommunicable diseases. J Nephrol. (2008) 21:621–31.
53. Okasheh, R, Al-Yahya, E, Al-Khlaifat, L, et al. Advancing cardiorespiratory physiotherapy practice in a developing country: surveying and benchmarking. Rehabil Res Pract. (2019) 2019:1–13. doi: 10.1155/2019/7682952
54. Pojednic, R, Bantham, A, Arnstein, F, Kennedy, MA, and Phillips, E. Bridging the gap between clinicians and fitness professionals: a challenge to implementing exercise as medicine. BMJ Open Sport Exerc Med. (2018) 4:1–6. doi: 10.1136/bmjsem-2018-000369
55. Chattranukulchai, P, Thongtang, N, Ophascharoensuk, V, Muengtaweepongsa, S, Angkurawaranon, C, Chalom, K, et al. An implementation framework for telemedicine to address noncommunicable diseases in Thailand. Asia Pac J Public Health. (2021) 33:968–71. doi: 10.1177/10105395211008754
56. Otu, AA, Effa, EE, Onwusaka, O, Omoyele, C, Arakelyan, S, Okuzu, O, et al. MHealth guideline training for non-communicable diseases in primary care facilities in Nigeria: a mixed methods pilot study. BMJ Open. (2022) 12:e060304. doi: 10.1136/bmjopen-2021-060304
57. Castillo-Carandang, NT, Buenaventura, RD, Chia, YC, do van, D, Lee, C, Duong, NL, et al. Moving towards optimized noncommunicable disease management in the asean region: recommendations from a review and multidisciplinary expert panel. Risk Manag Health Policy. (2020) 13:803–19. doi: 10.2147/RMHP.S256165
58. Kennedy, MA, Bayes, S, Newton, RU, Zissiadis, Y, Spry, NA, Taaffe, DR, et al. Implementation barriers to integrating exercise as medicine in oncology: an ecological scoping review. J Cancer Surviv. (2021) 16:865–81. doi: 10.1007/s11764-021-01080-0
59. Gordon, LG, Eakin, EG, Spence, RR, Pyke, C, Bashford, J, Saunders, C, et al. Cost-effectiveness analysis from a randomized controlled trial of tailored exercise prescription for women with breast cancer with 8-year follow-up. Int J Environ Res Public Health. (2020) 17:1–13. doi: 10.3390/ijerph17228608
60. Dalzell, MA, Smirnow, N, Sateren, W, Sintharaphone, A, Ibrahim, M, Mastroianni, L, et al. Rehabilitation and exercise oncology program: translating research into a model of care. Curr Oncol. (2017) 24:e191–8. doi: 10.3747/co.24.3498
61. Jones, H, George, KP, Scott, A, Buckley, JP, Watson, PM, Oxborough, DL, et al. Charter to establish clinical exercise physiology as a recognised allied health profession in the UK: a call to action. BMJ Open Sport Exerc Med. (2021) 7:e001158. doi: 10.1136/bmjsem-2021-001158
62. Pandya, T, and Marino, K. Embedding sports and exercise medicine into the medical curriculum; a call for inclusion. BMC Med Educ. (2018) 18:306. doi: 10.1186/s12909-018-1422-9
63. Cardinal, BJ, Park, EA, Kim, MS, and Cardinal, MK. If exercise is medicine, where is exercise in medicine? Review of U.S. medical education curricula for physical activity-related content. J Phys Act Health. (2015) 12:1336–43. doi: 10.1123/jpah.2014-0316
64. Noormohammadpour, P, Halabchi, F, Mazaheri, R, Mansournia, MA, Alizadeh, Z, Seif Barghi, T, et al. Designing and implementing a curriculum for sports and exercise medicine elective course for undergraduate medical students of Tehran University of Medical Sciences. Br J Sports Med. (2019) 53:601–4. doi: 10.1136/bjsports-2018-099462
65. Tovar, G, López, G, Ibáñez, M, et al. Institutionalized physical activity curriculum benefits of medical students in Colombia. Educ Health. (2016) 29:203–9.
66. Gates, AB . Training tomorrow’s doctors, in exercise medicine, for tomorrow’s patients. Br J Sports Med. (2015) 49:207–8. doi: 10.1136/bjsports-2014-094442
67. Morrissey, D, Nutt, JL, Mehdian, R, and Maffulli, N. The intercalated BSc in sports and exercise medicine at Barts and the London School of Medicine and Dentistry. Muscles Ligaments Tendons J. (2013) 3:190–5.
68. Thompson, PD, Arena, R, Riebe, D, and Pescatello, LS, American College of Sports Medicine. ACSM’s new preparticipation health screening recommendations from ACSM’s guidelines for exercise testing and prescription, ninth edition. Curr Sports Med Rep. (2013) 12:215–7. doi: 10.1249/JSR.0b013e31829a68cf
69. Dun, Y, Olson, TP, Ripley-Gonzalez, JW, Xie, K, Zhang, W, Cai, Y, et al. Safety of exercise testing in the clinical Chinese population. Front Cardiovasc Med. (2021) 8:8682. doi: 10.3389/fcvm.2021.638682
70. Lu, KD, Cooper, D, Dubrowski, R, Barwick, M, and Radom-Aizik, S. Exploration of barriers and facilitators to implementing best practice in exercise medicine in primary pediatric care-pediatrician perspectives. Pediatr Exerc Sci. (2021) 33:162–9. doi: 10.1123/pes.2020-0214
71. Paley, CA, and Johnson, MI. Abdominal obesity and metabolic syndrome: exercise as medicine? BMC Sports Sci Med Rehabil. (2018) 10:7. doi: 10.1186/s13102-018-0097-1
72. Liu, J, Spakowicz, DJ, Ash, GI, Hoyd, R, Ahluwalia, R, Zhang, A, et al. Bayesian structural time series for biomedical sensor data: a flexible modeling framework for evaluating interventions. PLoS Comput Biol. (2021) 17:1–21. doi: 10.1371/journal.pcbi.1009303
73. Ash, GI, Griggs, S, Nally, LM, Stults-Kolehmainen, M, Jeon, S, Brandt, C, et al. Evaluation of web-based and in-person methods to recruit adults with type 1 diabetes for a mobile exercise intervention: prospective observational study. JMIR Diab. (2021) 6:1–17. doi: 10.2196/28309
74. Porter, RR, McClelland, P, Ewing, A, Sonka, V, and Trilk, JL. Design and implementation of a clinic-to-community, physical activity health promotion model for healthcare providers. Prev Med Rep. (2022) 26:101697. doi: 10.1016/j.pmedr.2022.101697
Keywords: exercise prescription, health policy, noncommunicable diseases, medical provision, health policy triangle framework
Citation: Tao D, Awan-Scully R, Ash GI, Gu Y, Pei Z, Gao Y, Cole A, Supriya R, Sun Y, Xu R and Baker JS (2023) Health policy considerations for combining exercise prescription into noncommunicable diseases treatment: a narrative literature review. Front. Public Health. 11:1219676. doi: 10.3389/fpubh.2023.1219676
Edited by:
Yanfang Su, University of Washington, United StatesReviewed by:
Basil H. Aboul-Enein, University of London, United KingdomChidiebele Ojukwu, University of Nigeria, Nsukka, Nigeria
Copyright © 2023 Tao, Awan-Scully, Ash, Gu, Pei, Gao, Cole, Supriya, Sun, Xu and Baker. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Roger Awan-Scully, YXdhbnNjdWxseUBoa2J1LmVkdS5oaw==
 Dan Tao
Dan Tao Roger Awan-Scully3*
Roger Awan-Scully3* Garrett I. Ash
Garrett I. Ash Yaodong Gu
Yaodong Gu Zhong Pei
Zhong Pei Yang Gao
Yang Gao Alistair Cole
Alistair Cole Rashmi Supriya
Rashmi Supriya Yan Sun
Yan Sun Rui Xu
Rui Xu