- 1National Centre for Mental Health Promotion, Riyadh, Saudi Arabia
- 2Saudi Food and Drug Authority, Riyadh, Saudi Arabia
- 3Informed Decision-Making for Research and Studies, Riyadh, Saudi Arabia
- 4College of medicine, Alfaisal University, Riyadh, Saudi Arabia
Background: Mental health disorders, such as major depressive disorder (MDD) and generalized anxiety disorder (GAD), represent a significant public health concern in Saudi Arabia. This study aims to provide a recent mental health screening prevalence, including anxiety and depression screening in the general public and to explore the associated risk factors.
Methods: A cross-sectional study was conducted, employing a phone interview survey with 6,015 participants, using a quota sampling strategy to ensure equal representation of both sexes and administrative regions. The study assessed the prevalence of MDD and GAD risk and examined demographic, socioeconomic, and lifestyle factors associated with these mental health disorders.
Results: The national prevalence of people at risk of MDD and GAD were found to be 12.7 and 12.4%, respectively. Low diagnosis and treatment rates were observed, with only 1.5 and 0.5% of participants currently diagnosed and treated for depression and anxiety, respectively. Risk factors for MDD and GAD included female sex, lower education and income levels, smoking, and waterpipe use. Protective factors included physical activity, participation in volunteering activities and the practice of daily hobbies in the last 30 days.
Conclusion: The relatively high prevalence of MDD and GAD risk and low diagnosis and treatment rates in Saudi Arabia emphasize the need for increased mental health promotion, early detection, and treatment accessibility. The study highlights the importance of addressing modifiable risk factors and fostering protective factors through targeted interventions. Future research should focus on longitudinal associations, potential mediators and moderators, and the development of culturally appropriate and evidence-based interventions to enhance mental health outcomes in the region.
1. Introduction
The importance of national screening for mental health cannot be overstated. Mental health issues, particularly depression and anxiety, have become increasingly prevalent in recent years, posing a significant public health concern (1). Early identification and timely intervention have been shown to improve treatment outcomes and reduce the burden of mental health disorders on individuals, families, and society as a whole (2).
National screening programs can help identify individuals at risk for mental health disorders and facilitate their access to appropriate care. In addition, such programs can provide valuable data for researchers and policymakers, allowing them to better understand the prevalence, risk factors, and demographic characteristics of mental health disorders, and to design targeted interventions to address these issues (3). Furthermore, national screening programs can contribute to reducing the stigma associated with mental health disorders, as they underscore the importance of mental health as a public health priority (4).
Despite the increasing recognition of the importance of mental health, many individuals with depression and anxiety remain undiagnosed and untreated. According to the World Health Organization (5), the global prevalence of depression is estimated to be approximately 4.4% and anxiety disorders at about 3.6%. However, it has been estimated that up to 50% of individuals with these conditions do not receive a formal diagnosis or treatment (6).
There are several reasons for this high rate of undiagnosed mental health disorders. First, depression and anxiety symptoms can be non-specific and easily overlooked, particularly in primary care settings (7). Second, stigma and lack of awareness surrounding mental health can prevent individuals from seeking help (8). Finally, limited access to mental health care services, particularly in low-and middle-income countries, can further exacerbate the problem (9).
Saudi Arabia, like many other countries, faces significant challenges in addressing the mental health needs of its population (10, 11). A recent large national screening using the Patient health questionnaire-9 (PHQ-9) and the Generalized Anxiety Disorder 7 (GAD-7) in 2020 showed that the prevalence of Major Depressive Disorders (MDD) is at 13.8% while Generalized Anxiety Disorders were at 11.8% (12).
Several risk factors have been identified for depression and anxiety in Saudi Arabia, including female gender, low income, low educational level, unemployment, and chronic health conditions (12, 13). Furthermore, social factors such as marital status, family structure, and social support can also play a significant role in the development and maintenance of mental health disorders (12, 13).
Given the high prevalence of risk of MDD and GAD in Saudi Arabia and the associated burden on individuals and society, it is crucial to collect recent and frequent national statistics on these mental health disorders. Regularly updated data on the prevalence, risk factors, and demographic characteristics of depression and anxiety can help inform the development and implementation of targeted interventions and policies (1, 12).
Moreover, such data can contribute to raising awareness about mental health issues and combating the stigma associated with these disorders (4). Furthermore, accurate and up-to-date statistics can facilitate international comparisons and enable researchers to better understand the global context of mental health disorders, thereby informing global mental health initiatives and strategies (3).
In conclusion, the importance of national screening for mental health, particularly for depression and anxiety, cannot be overstated. Such programs can help identify individuals at risk, facilitate access to appropriate care, and provide valuable data for researchers, policymakers, and mental health advocates (14). In the context of Saudi Arabia, there is a pressing need for recent and frequent national statistics to inform targeted interventions and policies, reduce stigma, and contribute to the global understanding of mental health issues. Prior research on creating a national mental health screening surveillance system in Saudi Arabia took place in 2020, amid the COVID-19 pandemic. The system underwent testing in four phases, producing consistent and valid results (12, 14, 15). To maintain ongoing mental health monitoring, the National Center for Mental Health Promotion (NCMH) launched an annual program in 2022, utilizing the knowledge and infrastructure established during the 2020 surveillance system. Additionally, the 2020 surveillance system primarily concentrated on epidemic-related factors, such as national lockdowns and social distancing measures. While the new program plans to consider current and future large-scale events, its primary focus lies in addressing demographic and preventive factors, with long-term continuity.
Thus, this study aims to provide a recent mental health screening prevalence, including anxiety and depression screening in the general public and to explore the associated risk factors.
2. Materials and methods
2.1. Design
This study is a cross-sectional, nationwide mental health screening carried out through computer-aided telephonic interviews, in October–November 2022. The data collectors, who were skilled in conducting telephone interview research, underwent two training sessions to familiarize themselves with the interview manual before conducting the interviews. In this national survey we adopted the same methodology of the Saudi Arabia Mental Health Surveillance System (MHSS) (12, 14) which showed high quality and validity and will allow for comparison with historical data (15). Data collection and management were executed through the ZDataCloud research data collection system for enhanced organization and efficiency (16).
2.2. Participants and recruitment
Saudi Arabia residents, adults aged 18 and above were enlisted using a randomly generated phone number list, encompassing all 13 administrative regions of Saudi Arabia. Individuals were reached via telephone up to three attempts. In case of non-response, an alternative potential participant with a comparable demographic background (age, gender, area) was approached. The data collectors sought verbal consent from participants and recorded it in the consent field of the data collection system. If a participant did not give consent, an alternative individual with a similar demographic background (age, gender, area) was approached instead.
2.3. Sample size
The SMHNS employed a proportional quota sampling method to attain a balanced distribution of participants, stratified according to age, gender, and region within and among the 13 administrative divisions of Saudi Arabia. Two age categories were formed based on the Saudi median adult age of 36 years (one category consisted of individuals aged 18 to 36 years, while the other comprised those aged 37 years and above). This resulted in a quota of 52 for this national survey, which contributed to enhancing the sample’s diversity and minimizing the likelihood of nonprobability sampling bias.
Based on the desired depth of sub-analysis, we determined the sample size, which involved comparing age and sex groups across regions with a medium effect size of roughly 0.26, 80% power, and a 95% confidence level (17). Consequently, each quota was recommended to have 115 participants, resulting in a total of 460 individuals per region and an overall sum of 5,980 participants as a total sample. Upon fulfilling the quota sample, participants with comparable attributes were not allowed to partake in the research.
2.4. Data collection
The quota sampling technique is an automated procedure, as it is managed automatically by the ZDataCloud data collection system without human intervention, which also reduces sampling bias (16). As the data collection system closed the quotas after achieving only the targeted sample and as a group of phone call attempts was happening concurrently, on some occasions, more than one participant could pass the eligibility process at the same time, increasing the sample size above the target for some of the quotas. Thus, a slightly larger sample size maybe recruited for some quotas. Since the research utilized automated electronic data collection and management, no missing values were present; additionally the ZDataCloud incorporates a data integrity verification feature to deter data collectors from inputting incorrect information.
2.5. Study variables
The study comprises multiple sections, including demographic data, health lifestyle and behavior, and psychological well-being screening. During the data compilation phase, demographic factors including age, sex, administrative area, educational achievement, income level, and marital status were collected. Furthermore, details regarding other health-related variables, existing depression or anxiety diagnosis, obesity, physical activity, practicing hobbies, volunteering, and smoking habits, were also acquired.
In this study, the primary instrument employed for screening mental health was the Patient Health Questionnaire (PHQ-9) (18–20). The choice of PHQ-9 over other depression assessment methods was based on several factors (1): its validation across different age categories, such as adolescents, adults, and older individuals (12, 21) (2); its consistent performance irrespective of administration mode (e.g., self-reported by patients, administered in person or via phone by interviewers, or through touch-screen devices) (21, 22) (3); its proven validity and reliability for depression screening in a Saudi sample (12, 23). Additionally, the PHQ-9 has been employed in numerous global assessments and monitoring systems for mental health evaluation, such as the CDC’s utilization in the United States for the Behavioral Risk Factor Surveillance System and the National Health and Nutrition Examination Survey; this also enables international comparisons (24).
Finally, the Generalized Anxiety Disorder-7 (GAD-7) was employed to screen for anxiety levels, exhibiting strong validity and reliability across multiple studies (15, 25). Furthermore, GAD-7 has proven its validity in screenings of general populations, inclusive of Arabic speakers within the Saudi community (15, 26, 27).
2.6. Outcome measures and variables transformation
In order to measure the occurrence of risk of depression within our sample, we applied a score exceeding 10, which demonstrated the most favorable balance between sensitivity, 0.89 (95% CI 0.75 to 0.96), and specificity, 0.89 (95% CI 0.79 to 0.94), based on the combined findings from 10 studies (12, 28).
Regarding the GAD-7, the collective sensitivity and specificity values seemed to be satisfactory at a threshold of 8 [sensitivity: 0.83 (95% CI 0.71–0.91), specificity: 0.84 (95% CI 0.70–0.92)], while cut-off scores ranging from 7 to 10 also exhibited comparable combined sensitivity/specificity estimates (29). Moreover, in relation to the GAD-7 anxiety metric, a score of 10 or higher presented the ideal cut-off point in both the literature and prior research conducted on Saudi demographics (25, 26).
The study also adhered to the World Health Organization’s (WHO) global recommendations for adult physical activity (ages 18–64), which include (1): 75 min of vigorous intensity physical activity (VIPA) per week, or (2) 150 min of moderate intensity physical activity (MIPA) per week (30). Based on the self-reported information gathered from participants through interview questionnaires (e.g., exercise duration, frequency, and intensity per week), two distinct outcome variables were established to determine if the guidelines were met: an adequate level of physical activity (ALPA) (consisting of a minimum of 150 min of MIPA weekly and/or at least 75 min of VIPA weekly) and a suboptimal level of physical activity (LLPA) (falling below 150 min of MIPA and/or 75 min of VIPA).
Other variables were presented as obtained with no transformation processes.
2.7. Statistical analysis
The prevalence was reported as proportion of the overall sample. For quantitative variables with a normal distribution, means and standard deviations (SD) are provided, while medians and ranges are used when appropriate. Qualitative variables are displayed as percentages and confidence intervals (CIs) and are compared using Pearson’s chi-square test. Multivariate regression analysis (logistic regression) was used to investigate risk factors related to the susceptibility of Major Depressive Disorder (MDD) or Generalized Anxiety Disorder (GAD).
3. Results
3.1. Demographics
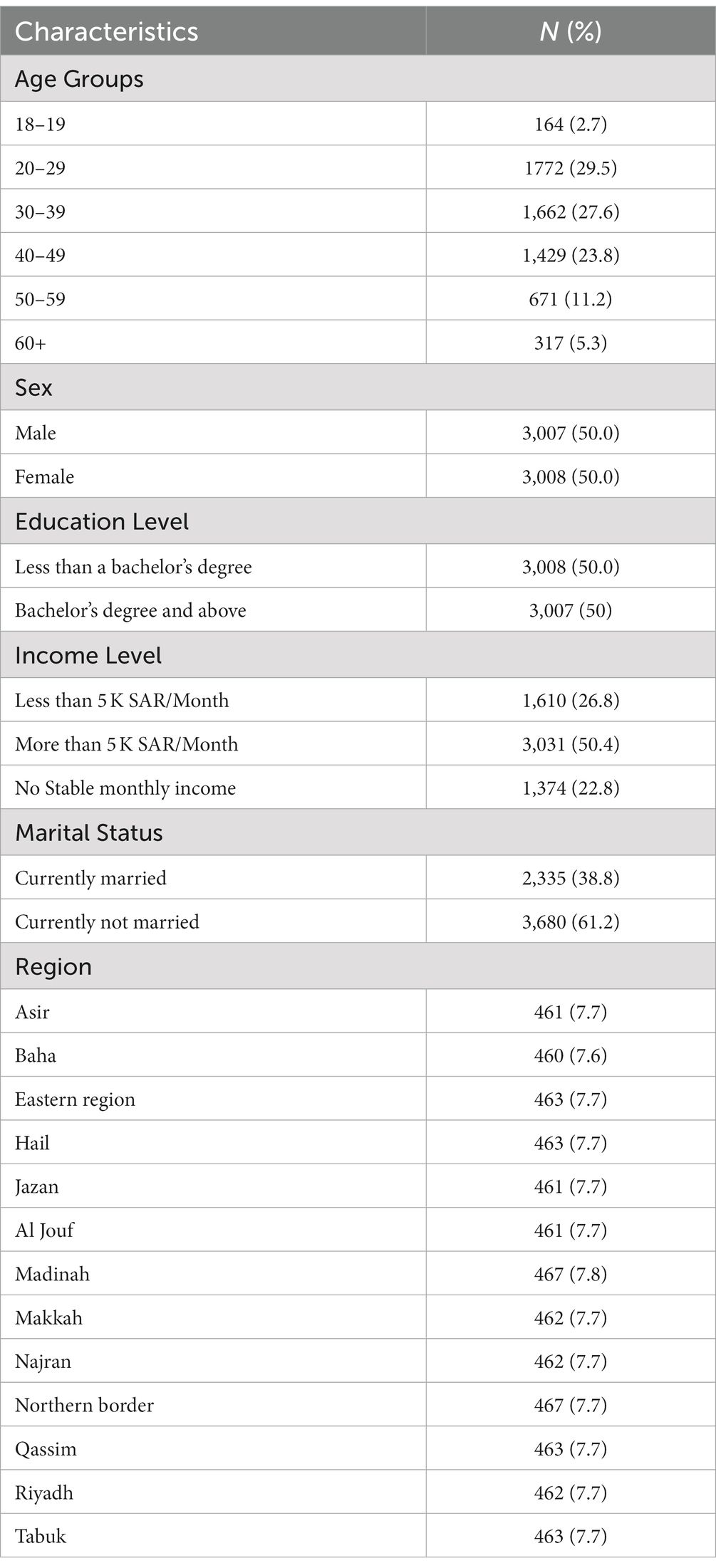
Of the 9,248 potential participants contacted, 6,015 from the 13 administrative regions of Saudi Arabia completed the phone interview, with a response rate of 65.04%, including those who did not answer on 3 occasions. Out of the total participants as planned in the quota sampling, 50% were female. The mean age was 36.45 (SD 12.45; range: 18–90). Table 1 shows the demographic distribution of the sample.
3.2. Mental health risks and associated variables
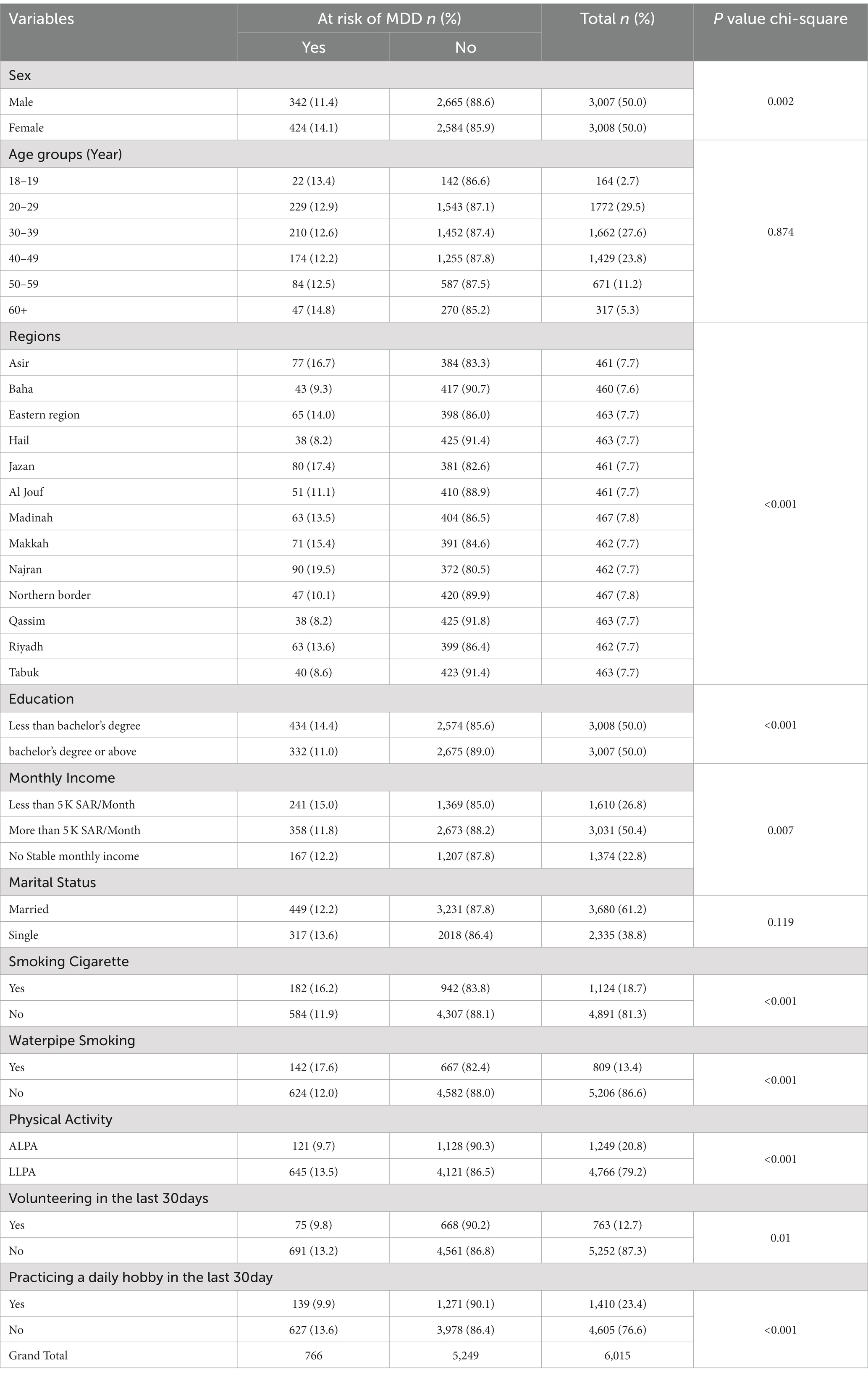
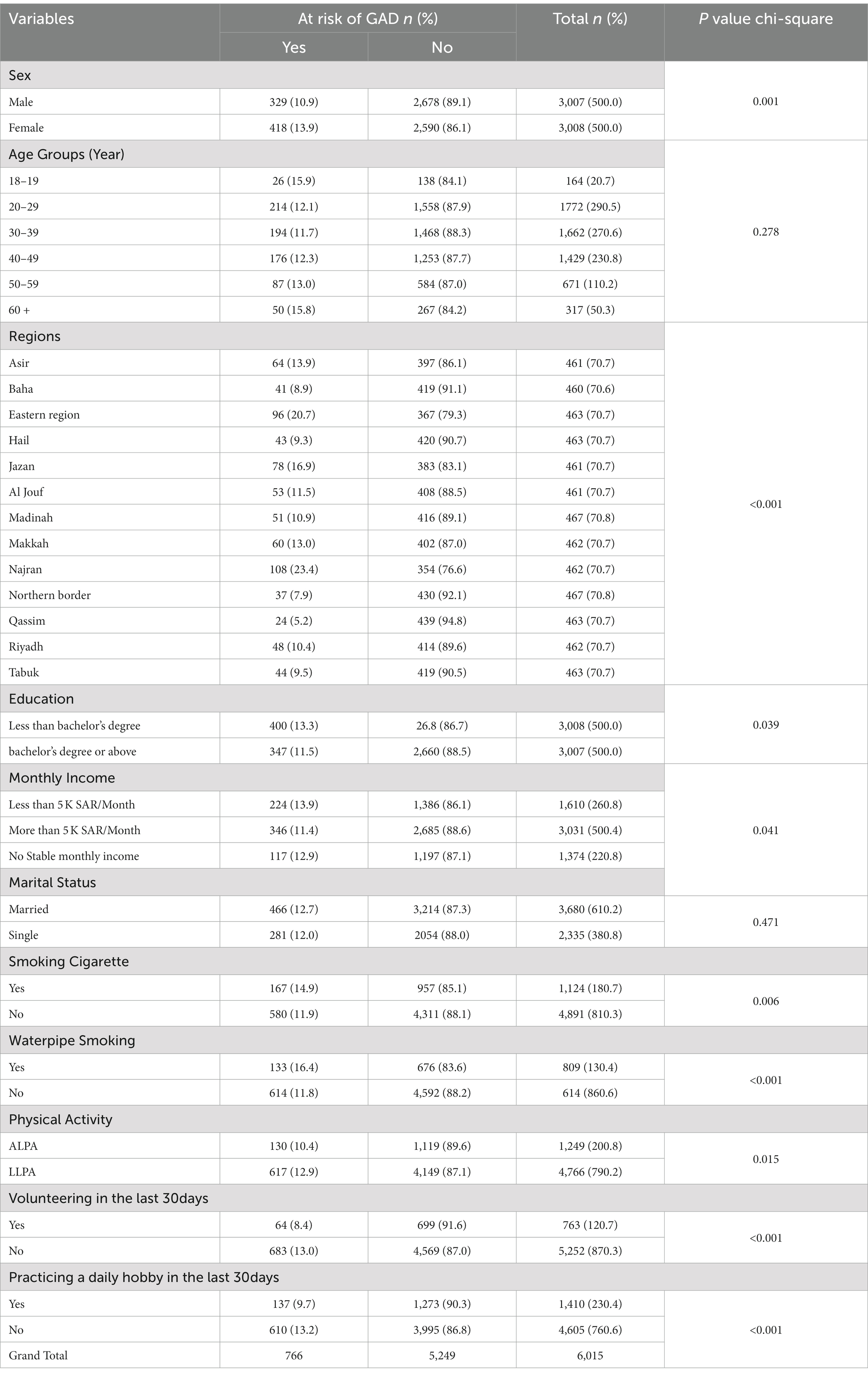
The sample prevalence of people at risk of MDD (PHQ-9—Cut-Off above 10) was 12.7%. The national prevalence of people at risk of GAD (GAD-7—Cut-Off above 10) was 12.4%.
Table 2 shows the association between risk of MDD and all other variables. Overall, the following variables were significantly associated with risk of MDD (sex, region, education, monthly income, smoking cigarette, waterpipe smoking, physical activity, volunteering in the last 30 days, and practicing a daily hobby in the last 30 day).
Table 3 shows the association between risk of GAD and all other variables. Overall, the following variables were significantly associated with risk of GAD (sex, region, education, monthly income, smoking cigarette, waterpipe smoking, physical activity, volunteering in the last 30 days, and practicing a daily hobby in the last 30 day).
Only 93 (1.5%) participants are currently diagnosed with depression and on-treatment, and only 32 (0.5%) participants are currently diagnosed with anxiety and on-treatment.
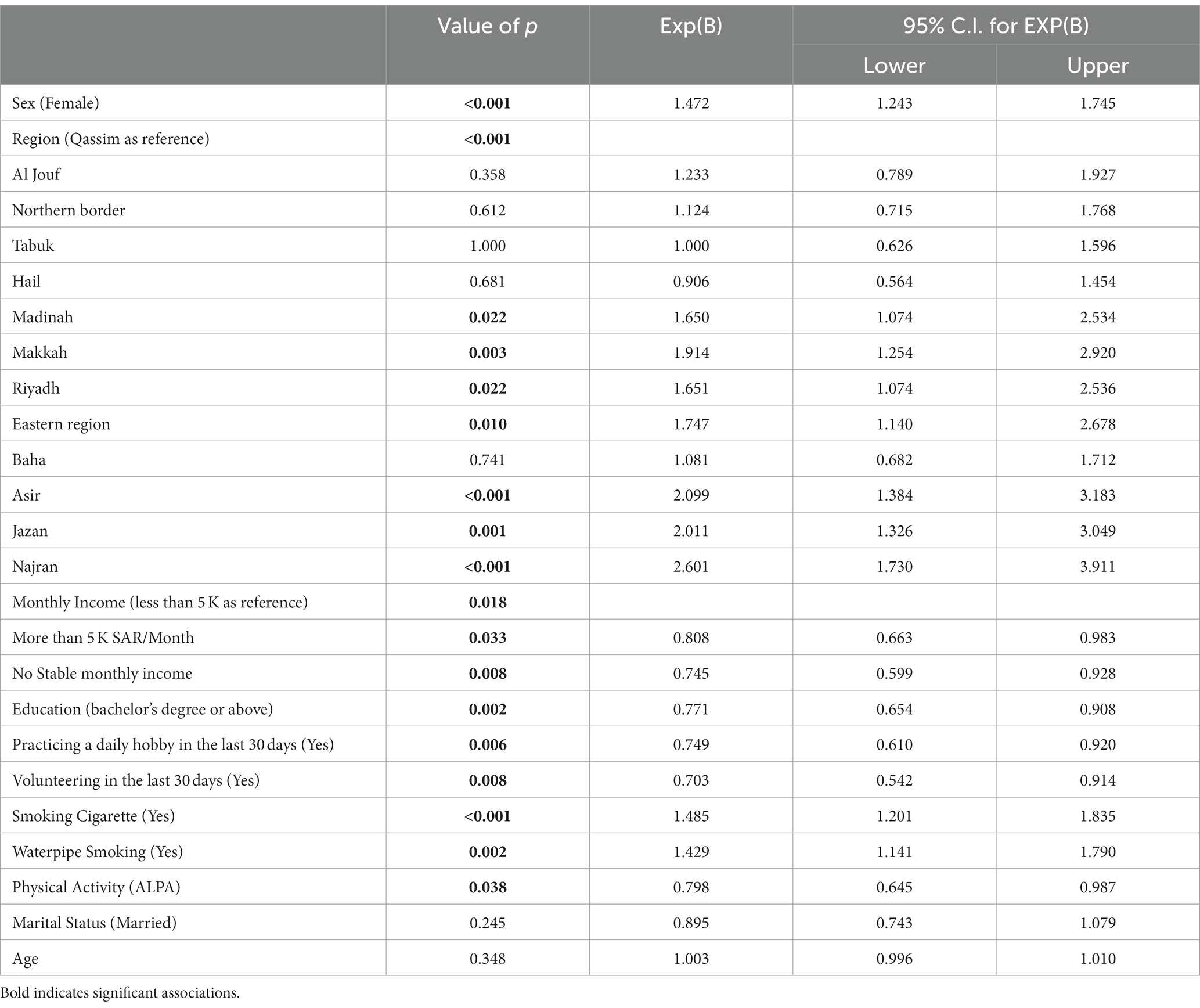
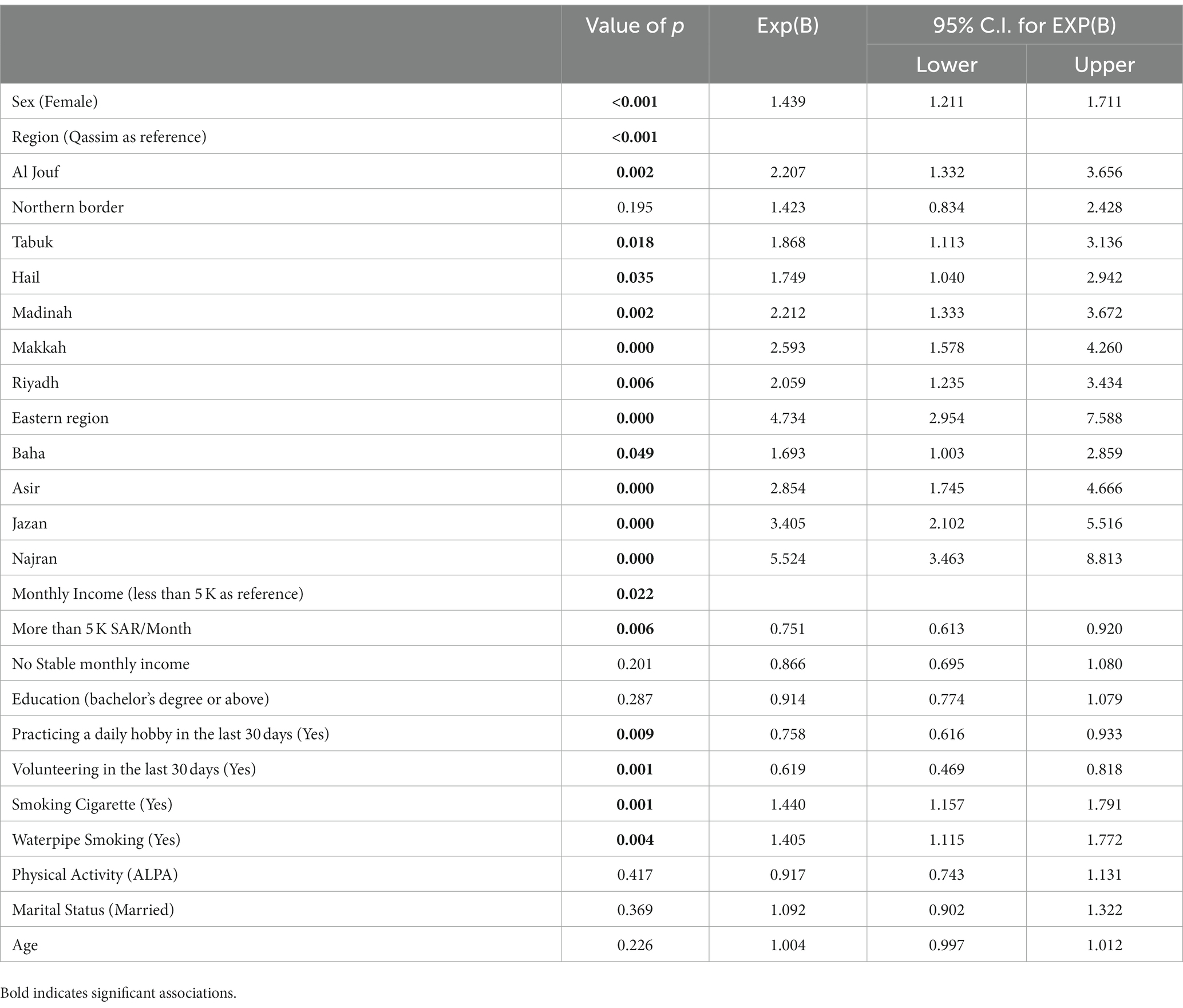
Finally, logistic regression model was preformed including all the variables to further explore which of the variables are more likely to be associated with risk of MDD and GAD. As shown in Table 4, Sex, Region, Monthly Income, Education, practicing a daily hobby in the last 30 days, volunteering in the last 30 days, smoking cigarette, waterpipe smoking, and physical activity were significantly associated with MDD risk.
On the other hand, as shown in Table 5, sex, region, monthly income, practicing a daily hobby in the last 30 days, volunteering in the last 30 days, smoking cigarette, and waterpipe smoking, were significantly associated with MDD risk.
4. Discussion
In this cross-sectional study, we achieved a response rate of 65.04% among the 6,015 participants, which is considered satisfactory for a phone interview survey (31). The quota sampling strategy employed in this study ensured an equal representation of both sexes, with 50% of the participants being female. The mean age of participants was 36.45, similar to the general population in Saudi Arabia (32).
The sample prevalence of people at risk of MDD and GAD were found to be 12.7 and 12.4% respectively, which is consistent with previous studies conducted in Saudi Arabia and overall lower than many other countries (12). Although this study results were similar to the results of the 2020 MHSS which were conducted during the COVID-19 epidemic, with the lack of more historical data we could not determine why the results are similar, thus, with the continuity of this national screening program over the coming years more understanding of mental health indicators could be generated. It is important to note that only a small proportion of participants were currently diagnosed and on treatment for depression (1.5%) and anxiety (0.5%), which highlights the potential underdiagnosis and undertreatment of mental health disorders in this population. This assumption is supported by the global prevalence of depression in 5% of adults, with 4% in men and 6% in women (33). Furthermore, a national screening study conducted in 2010 revealed that the 12-month prevalence of any DSM-IV/CIDI disorder is 20.2%, with anxiety disorders are the most common type of disorder, with a lifetime prevalence of 12.3%, followed by mood disorders at 6.8% (34).
Our findings show that sex, region, education, monthly income, smoking cigarette, waterpipe smoking, physical activity, volunteering in the last 30 days, and practicing a daily hobby in the last 30 days were significantly associated with the risk of MDD and GAD. These results are in line with previous research that identified similar factors as predictors of mental health disorders (12, 35, 36).
In our study, females showed a higher risk for both MDD and GAD, which is consistent with previous literature (12, 37). Due to the limited number of prior studies examining regional differences in mental health prevalence, pinpointing a logical explanation proves challenging. However, potential reasons for these disparities may include variations in access to mental health services, cultural factors, socioeconomic differences, or it could be that regional classification is simply a random grouping variable with no real association to mental health (38). Moreover, there is limited information in the literature available on the association between region or city and mental health indicators such as depression or anxiety prevalence. However, existing studies do suggest that regional differences may exist in mental health prevalence (38). The social gradient, which is the relationship between social and economic factors and health outcomes, impacts both the risk of disorder and access to services, ultimately influencing mental health outcomes (38).
The association between lower education and income levels with increased risk of MDD and GAD has been well-documented (39, 40).
Smoking, waterpipe use, and physical inactivity were also significantly associated with increased risk of MDD and GAD, which is consistent with the literature (12, 41, 42). Interestingly, our study discovered a potential link between engaging in volunteer work or pursuing a daily hobby within the past 30 days and a reduced likelihood of being at risk for Major Depressive Disorder (MDD) and Generalized Anxiety Disorder (GAD). Although this cross-sectional study cannot establish causality, the results may suggest that involvement in such activities could provide behavioral activation and protective effects on mental health. Alternatively, individuals with MDD or GAD might be less able to participate in volunteer work, daily hobbies, or physical activities due to the impact of their mental condition (43–46).
Our findings contribute to the growing body of evidence on mental health risks in Saudi Arabia and the Middle East. The high prevalence of MDD and GAD risk, coupled with low diagnosis and treatment rates, calls for increased efforts in mental health promotion, early detection, and treatment accessibility. Additionally, our study highlights the importance of addressing modifiable risk factors such as smoking, physical inactivity, and socioeconomic disparities through targeted interventions. Nonetheless, it is worth noting that in 2019, Saudi Arabia established the NCMH to spearhead mental health promotion and prevention initiatives. In 2021, over 3,500 pages of mental health awareness content were published by NCMH, targeting prevention programs in schools, universities, and workplaces. Collaboration with educational institutions led to conferences, lectures, and teacher training sessions (47, 48). University programs included mental health promotion groups, student support centers, and over 650 awareness activities (47, 48). Workplace initiatives involved mental health first aid training, awareness sessions, and mental health ambassadors (47, 48). Four digital mental health platforms, including NCMH’s Qareboon app, provided thousands of free consultations (47, 48). NCMH also conducted workshops for mental health professionals, focusing on policies, regulations, disaster response, and specialized skills (47, 48).
Future research should explore longitudinal associations between these factors and mental health outcomes, as well as potential mediators and moderators of these relationships. In addition, there is a need for more comprehensive assessments of mental health disorders and their determinants in the region, which will inform the development and implementation of culturally appropriate and evidence-based interventions.
Limitations of the study include the cross-sectional design, which prevents the establishment of causal relationships between variables. Additionally, the use of self-report measures may introduce response bias. Although our study utilized quota sampling, which can be associated with selection bias risks, it was chosen over random probability sampling due to its previously proven consistency and sensitivity to mental health screening in Saudi Arabia and lower costs (15). Furthermore, employing a proportionally large sample and 52 quotas helps mitigate selection bias (31, 49, 50). Currently, in Saudi Arabia, generating a random national-level sample is only feasible through household surveys, which also have limitations caused by cultural factors. Additionally, the utilization of the ZDataCloud research data collection and governance system improved the quota sampling process by eliminating human selection bias. This enhancement as shown in the results led to a well-balanced sample across the 52 quotas, ensuring a more accurate representation of the targeted population. Nonetheless, the study provides valuable insights into the mental health risks and associated variables in the Saudi Arabian population, contributing to the development of effective mental health interventions and policies.
5. Conclusion
In conclusion, this cross-sectional study reveals a significant prevalence of individuals at risk for MDD and GAD in Saudi Arabia, and potential underdiagnosis and undertreatment of these mental health disorders. Our findings confirm the association of various factors such as sex, region, education, income, smoking, physical activity, and engagement in hobbies or volunteering with the risk of MDD and GAD. These results underline the need for targeted interventions addressing modifiable risk factors and promoting mental health awareness and treatment accessibility in Saudi Arabia. Future research should investigate longitudinal associations and comprehensive assessments of mental health disorders to inform culturally appropriate, evidence-based interventions. Despite the study’s limitations, it offers valuable insights for developing effective mental health policies and strategies in Saudi Arabia and the Middle East.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by Sharik Association for Health Research’s ethics committee (Approval no. 04–2022). The patients/participants provided their written informed consent to participate in this study.
Author contributions
NA and NB participated in the conceptual design and formulation of the research questions. All authors participated in the development and review of the manuscript.
Funding
This study was funded by the National Center for Mental Health Promotion.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Kessler, RC, Aguilar-Gaxiola, S, Alonso, J, Chatterji, S, Lee, S, Ormel, J, et al. The global burden of mental disorders: an update from the WHO world mental health (WMH) surveys. Epidemiol Psychiatr Sci. (2009) 18:23–33. doi: 10.1017/S1121189X00001421
2. Vigo, D, Thornicroft, G, and Atun, R. Estimating the true global burden of mental illness. Lancet Psychiatry. (2016) 3:171–8. doi: 10.1016/S2215-0366(15)00505-2
3. Thornicroft, G, Chatterji, S, Evans-Lacko, S, Gruber, M, Sampson, N, Aguilar-Gaxiola, S, et al. Undertreatment of people with major depressive disorder in 21 countries. Br J Psychiatry. (2017) 210:119–24. doi: 10.1192/bjp.bp.116.188078
4. Henderson, C, Evans-Lacko, S, and Thornicroft, G. Mental illness stigma, help seeking, and public health programs. Public Health. (2013) 103:777–780. doi: 10.2105/AJPH.2012.301056
5. WHO. Depression and other common mental disorders: global health estimates. Geneva: World Health Organization (2017) Available at: https://apps.who.int/iris/handle/10665/254610.
6. Kohn, R, Saxena, S, Levav, I, and Saraceno, B. The treatment gap in mental health care. Bull World Health Organ. (2004) 82:858–66.
7. Mitchell, AJ, Vaze, A, and Rao, S. Clinical diagnosis of depression in primary care: a meta-analysis. Lancet. (2009) 374:609–19. doi: 10.1016/S0140-6736(09)60879-5
8. Clement, S, Schauman, O, Graham, T, Maggioni, F, Evans-Lacko, S, Bezborodovs, N, et al. What is the impact of mental health-related stigma on help-seeking? A systematic review of quantitative and qualitative studies. Psychol Med. (2015) 45:11–27. doi: 10.1017/S0033291714000129
9. Patel, V, Saxena, S, Lund, C, Thornicroft, G, Baingana, F, Bolton, P, et al. The lancet commission on global mental health and sustainable development. Lancet. (2018) 392:1553–98. doi: 10.1016/S0140-6736(18)31612-X
10. Qureshi, NA, Al-Habeeb, AA, and Koenig, HG. Mental health system in Saudi Arabia: an overview. Neuropsychiatr Dis Treat. (2013) 9:1121–35. doi: 10.2147/NDT.S48782
11. Carlisle, J. Mental health law in Saudi Arabia. BJPsych Int. (2018) 15:17–9. doi: 10.1192/bji.2017.10
12. BinDhim, NF, Althumiri, NA, Basyouni, MH, Alageel, AA, Alghnam, S, Al-Qunaibet, AM, et al. Saudi Arabia mental health surveillance system (MHSS): mental health trends amid COVID-19 and comparison with pre-COVID-19 trends. Eur J Psychotraumatol. (2021) 12:1875642. doi: 10.1080/20008198.2021.1875642
13. Al-Qadhi, W, Ur Rahman, S, Ferwana, MS, and Abdulmajeed, IA. Adult depression screening in Saudi primary care: prevalence, instrument and cost. BMC Psychiatry. (2014) 14:1–9. doi: 10.1186/1471-244X-14-190
14. BinDhim, NF, Althumiri, NA, Basyouni, MH, Alageel, AA, Alghnam, S, Al-Qunaibet, AM, et al. A mental health surveillance system for the general population during the COVID-19 pandemic: protocol for a multiwave cross-sectional survey study. JMIR Res Protoc. (2020) 9:e23748. doi: 10.2196/23748
15. Althumiri, NA, Basyouni, MH, and BinDhim, NF. Consistency and sensitivity evaluation of the Saudi Arabia mental health surveillance system (MHSS): hypothesis generation and testing. JMIR Form Res. (2022) 6:e23965. doi: 10.2196/23965
16. ZDataCloud. (n.d.). Available at: https://zdatacloud.com/.
17. Cohen, J. Statistical power analysis for the behavioral sciences. Cambridge, MA: Academic press (2013).
18. Becker, S, Al Zaid, K, and Al, FE. Screening for somatization and depression in Saudi Arabia: a validation study of the PHQ in primary care. Int J Psychiatry Med. (2002) 32:271–83. doi: 10.2190/XTDD-8L18-P9E0-JYRV
19. Kroenke, K, and Spitzer, RL. The PHQ-9: a new depression diagnostic and severity measure. Slack Incorporated Thorofare, New Jersey (2002). 509–515.
20. Kroenke, K, Spitzer, RL, and Williams, JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. (2001) 16:606–13. doi: 10.1046/j.1525-1497.2001.016009606.x
21. BinDhim, NF, Alanazi, EM, Aljadhey, H, Basyouni, MH, Kowalski, SR, Pont, LG, et al. Does a mobile phone depression-screening app motivate mobile phone users with high depressive symptoms to seek a health care professional’s help? J Med Internet Res. (2016) 18:e156. doi: 10.2196/jmir.5726
22. Fann, JR, Berry, DL, Wolpin, S, Austin-Seymour, M, Bush, N, Halpenny, B, et al. Depression screening using the patient health Questionnaire-9 administered on a touch screen computer. Psycho-oncology: journal of the psychological, social and behavioral dimensions of. Cancer. (2009) 18:14–22. doi: 10.1002/pon.1368
23. AlHadi, AN, AlAteeq, DA, Al-Sharif, E, Bawazeer, HM, Alanazi, H, AlShomrani, AT, et al. An arabic translation, reliability, and validation of patient health questionnaire in a Saudi sample. Ann General Psychiatry. (2017) 16:1–9. doi: 10.1186/s12991-017-0155-1
24. Reeves, WC, Pratt, LA, Thompson, W, Ahluwalia, IB, Dhingra, SS, McKnight-Eily, LR, et al. Mental illness surveillance among adults in the United States. MMWR Suppl. (2011) 60:1–29.
25. Spitzer, RL, Kroenke, K, Williams, JB, and Löwe, B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. (2006) 166:1092–7. doi: 10.1001/archinte.166.10.1092
26. Alosaimi, FD, Al-Sultan, OA, Alghamdi, QA, Almohaimeed, IK, and Alqannas, SI. Gender-specific differences in depression and anxiety symptoms and help-seeking behavior among gastroenterology patients in Riyadh, Saudi Arabia. Neuroscience. (2014) 19:203–9.
27. Sawaya, H, Atoui, M, Hamadeh, A, Zeinoun, P, and Nahas, Z. Adaptation and initial validation of the patient health questionnaire–9 (PHQ-9) and the generalized anxiety disorder–7 questionnaire (GAD-7) in an Arabic speaking Lebanese psychiatric outpatient sample. Psychiatry Res. (2016) 239:245–52. doi: 10.1016/j.psychres.2016.03.030
28. Manea, L, Gilbody, S, and McMillan, D. Optimal cut-off score for diagnosing depression with the patient health questionnaire (PHQ-9): a meta-analysis. CMAJ. (2012) 184:E191–6. doi: 10.1503/cmaj.110829
29. Plummer, F, Manea, L, Trepel, D, and McMillan, D. Screening for anxiety disorders with the GAD-7 and GAD-2: a systematic review and diagnostic metaanalysis. Gen Hosp Psychiatry. (2016) 39:24–31. doi: 10.1016/j.genhosppsych.2015.11.005
30. World Health Organization. Physical activity and adults. Geneva: World Health Organization (n.d.).
31. Groves, RM, Fowler, FJ, Couper, MP, Lepkowski, JM, Singer, E, and Tourangeau, R. Survey methodology. New York: John Wiley & Sons (2011).
32. Desa, U World population prospects 2019: Highlights. New York, US: United Nations Department for Economic and Social Affairs pp. 11–125. (2019).
33. WHO. Depressive disorder (depression). (2023) Available at: https://www.who.int/news-room/fact-sheets/detail/depression.
34. Altwaijri, YA, Al-Habeeb, A, Al-Subaie, AS, Bilal, L, Al-Desouki, M, Shahab, MK, et al. Twelve-month prevalence and severity of mental disorders in the Saudi National Mental Health Survey. Int J Methods Psychiatr Res. (2020) 29:e1831. doi: 10.1002/mpr.1831
35. Investigators, EM, Alonso, J, Angermeyer, M, Bernert, S, Bruffaerts, R, Brugha, T, et al. Prevalence of mental disorders in Europe: results from the European study of the epidemiology of mental disorders (ESEMeD) project. Acta Psychiatr Scand. (2004) 109:21–7. doi: 10.1111/j.1600-0047.2004.00327.x
36. Kessler, RC, Berglund, P, Demler, O, Jin, R, Merikangas, KR, and Walters, EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. (2005) 62:593–602. doi: 10.1001/archpsyc.62.6.593
37. Seedat, S, Scott, KM, Angermeyer, MC, Berglund, P, Bromet, EJ, Brugha, TS, et al. Cross-national associations between gender and mental disorders in the World Health Organization world mental health surveys. Arch Gen Psychiatry. (2009) 66:785–95. doi: 10.1001/archgenpsychiatry.2009.36
38. Alegría, M, NeMoyer, A, Falgàs Bagué, I, Wang, Y, and Alvarez, K. Social determinants of mental health: where we are and where we need to go. Curr Psychiatry Rep. (2018) 20:1–13. doi: 10.1007/s11920-018-0969-9
39. Lorant, V, Deliège, D, Eaton, W, Robert, A, Philippot, P, and Ansseau, M. Socioeconomic inequalities in depression: a meta-analysis. Am J Epidemiol. (2003) 157:98–112. doi: 10.1093/aje/kwf182
40. Patel, V, Flisher, AJ, Hetrick, S, and McGorry, P. Mental health of young people: a global public-health challenge. Lancet. (2007) 369:1302–13. doi: 10.1016/S0140-6736(07)60368-7
41. Steptoe, A, Shankar, A, Demakakos, P, and Wardle, J. Social isolation, loneliness, and all-cause mortality in older men and women. Proc Natl Acad Sci. (2013) 110:5797–801. doi: 10.1073/pnas.1219686110
42. Al-Hejji, Z, Al-Khudhair, M, Al-Musaileem, M, and Al-Eithan, M. Prevalence and associated risk factors of antenatal depression among women attending antenatal clinics in primary health care centers in the Ministry of Health in Al-Ahsa City, Saudi Arabia. J Fam Med Prim Care. (2019) 8:3900–7. doi: 10.4103/jfmpc.jfmpc_724_19
43. Musick, MA, and Wilson, J. Volunteering and depression: the role of psychological and social resources in different age groups. Soc Sci Med. (2003) 56:259–69. doi: 10.1016/S0277-9536(02)00025-4
44. Cohen, S. Social relationships and health. Am Psychol. (2004) 59:676–84. doi: 10.1037/0003-066X.59.8.676
45. Jack McDermott DON. Evidence insights: volunteering and mental health. (2021) Available at: https://www.volunteeringaustralia.org/wp-content/uploads/Evidence-Insights-Volunteering-and-mental-health-Final.pdf.
46. Ekers, D, Webster, L, Van Straten, A, Cuijpers, P, Richards, D, and Gilbody, S. Behavioural activation for depression; an update of meta-analysis of effectiveness and sub group analysis. PLoS One. (2014) 9:e100100. doi: 10.1371/journal.pone.0100100
47. NCMH. About the National Center for mental health promotion. (2020) Available at: https://ncmh.org.sa/view/16/3th.
49. Marsh, C, and Scarbrough, E. Testing 9 hypotheses about quota sampling. J Mark Res Soc. (1990) 32:485–506.
50. The Methodologists. Quota sampling: reducing Bias and outperforming random sampling. (2023) Available at: https://methodologists.net/Quota-Sampling:-Reducing-Bias-and-Outperforming-Random-Sampling.
Keywords: mental health, depression, anxiety, screening, Saudi Arabia
Citation: Alhabeeb AA, Al-Duraihem RA, Alasmary S, Alkhamaali Z, Althumiri NA and BinDhim NF (2023) National screening for anxiety and depression in Saudi Arabia 2022. Front. Public Health 11:1213851. doi: 10.3389/fpubh.2023.1213851
Edited by:
Anu Molarius, Region Värmland Kommunalförbund, SwedenReviewed by:
Aulia Iskandarsyah, Padjadjaran University, IndonesiaFredrik Granström, Linköping University, Sweden
Copyright © 2023 Alhabeeb, Al-Duraihem, Alasmary, Alkhamaali, Althumiri and BinDhim. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Nora A. Althumiri, bm9yYUBhbHRodW1pcmkubmV0
 Abdulhameed Abdullah Alhabeeb1
Abdulhameed Abdullah Alhabeeb1 Nora A. Althumiri
Nora A. Althumiri Nasser F. BinDhim
Nasser F. BinDhim