- 1Department of Interdisciplinary Medicine, University of Bari, Bari, Italy
- 2Department of Economics, Management and Business Law, University of Bari, Bari, Italy
Background: In the age of digitalization and big data, personal health information is a key resource for health care and clinical research. This study aimed to analyze the determinants and describe the measurement of the willingness to disclose personal health information.
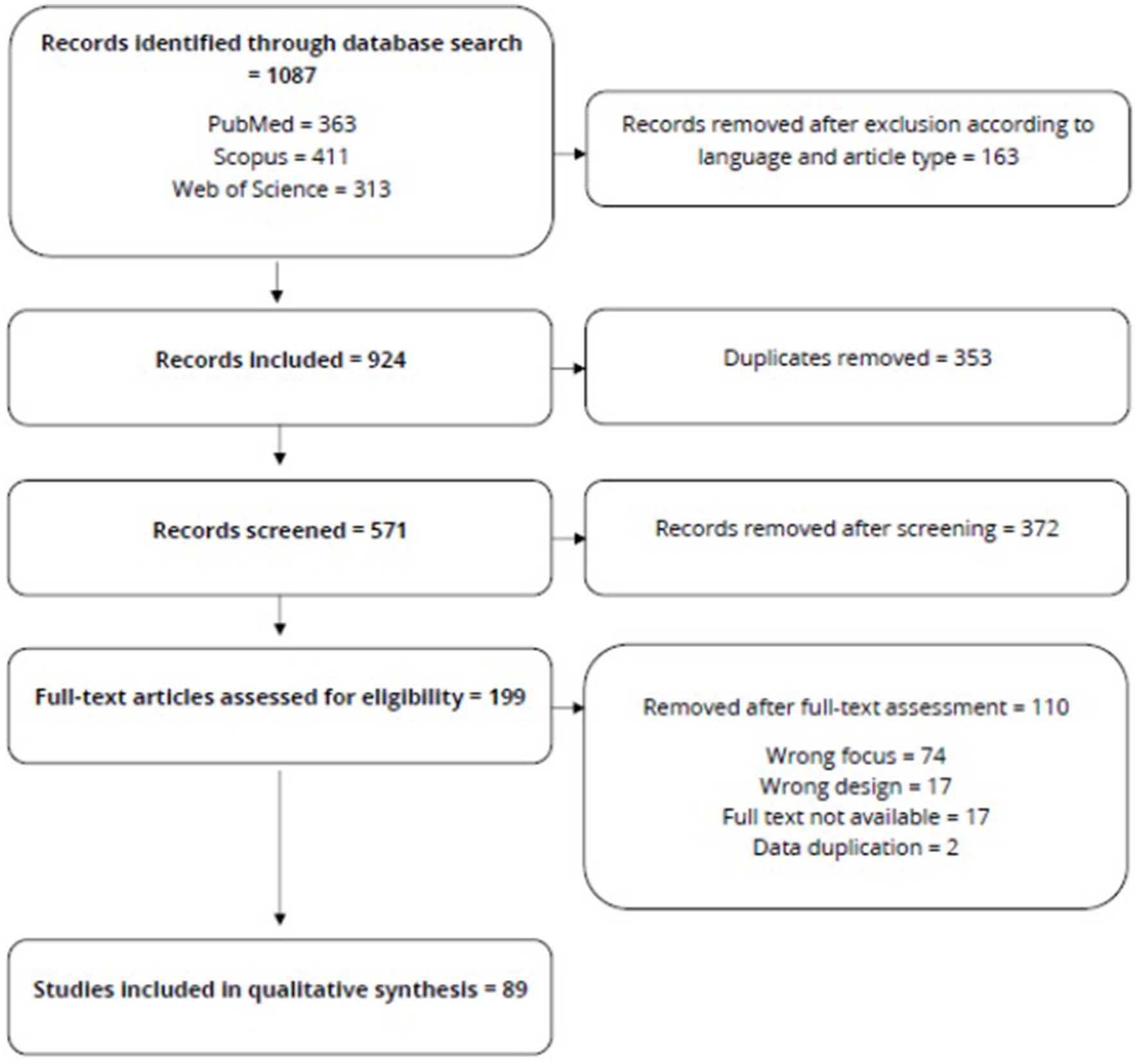
Methods: The study conducted a systematic review of articles assessing willingness to share personal health information as a primary or secondary outcome. The review followed the Preferred Reporting Items for Systematic Reviews and Meta-Analysis protocol. English and Italian peer-reviewed research articles were included with no restrictions for publication years. Findings were narratively synthesized.
Results: The search strategy found 1,087 papers, 89 of which passed the screening for title and abstract and the full-text assessment.
Conclusion: No validated measurement tool has been developed for willingness to share personal health information. The reviewed papers measured it through surveys, interviews, and questionnaires, which were mutually incomparable. The secondary use of data was the most important determinant of willingness to share, whereas clinical and socioeconomic variables had a slight effect. The main concern discouraging data sharing was privacy, although good data anonymization and the high perceived benefits of sharing may overcome this issue.
1. Introduction
The spread of information technologies has challenged assumptions about privacy and confidentiality, leading to feelings of discomfort, threat, and mistrust (1). This highlights the importance of personal data, which are defined as “any information relating to an identified or identifiable natural person,” according to Article 4 of the General Data Protection Regulation, a Regulation in EU law on data protection and privacy in the EU and the European Economic Area.
Studies have also highlighted the divergence between attitudes and behavior related to privacy, known as the “privacy paradox” (2–5). Evidence indicates that individuals are willing to share their personal information for relatively small rewards, which contrasts with the privacy concerns showed in polls and surveys (6). The paradox has been especially studied in the context of e-commerce and social media, as the understanding of privacy attitudes and behaviors has significant implications for the huge collectors of personal information (7).
Since the past decade, many countries have introduced digital health transformation (8, 9). This process proceeded with the progressive adoption of new technologies; development of telemedicine; and diffusion of wearable electronic devices, consumer-oriented apps, and services (10–14). A direct consequence of health digitalization is the availability of a variety of data, many of which can be considered personal data concerning health or personal health information (PHI) (15). Such complex and rich data may drive the development of high-performing big data and artificial intelligence (AI) systems in health care, which are also fundamental in producing new insights for clinical research (16, 17). For this reason, digital health and health-data management have become a priority, firmly embedded in EU policy and funding goals (18). However, even if PHI represents an inalienable resource, personal preference in disclosing such information may limit access to PHI (8, 19–25). During the coronavirus disease 2019 (COVID-19) pandemic, the usefulness of sharing PHI was observed: PHI has been fundamental for contact tracing, managing the vaccination campaign, and other public health interventions (26, 27). At the same time, many observers registered several risks to privacy triggered by the pandemic (28, 29).
Given the importance of PHI in the age of data-driven health care policy and clinical research, health sciences should elucidate the theoretical explanations of privacy attitudes and behaviors (30), which can help ensure ethical patient-centered policies and influence the development of health care practice. One of the key stages of this challenge in the health care context is the investigation of the personal willingness to share PHI. To the best of our knowledge, there are no validated tools to measure the willingness to share PHI. Thus, we conducted this systematic review to identify the tools that have been used to measure the willingness to share PHI and to investigate the clinical, demographic, and neuropsychological factors associated with such willingness.
2. Methods
This systematic review was conducted by following the Preferred Reporting Items for Systematic Review and Meta-Analyses (PRISMA) guidelines (31).
2.1. Search strategy
We used a systematic search strategy to conduct a two-step literature search. The first step, started on February 16, 2022, involved searching the Medline/PubMed, Web of Science, and Scopus databases using the following strings: (shar* OR disclos*) AND (personal OR electronic) AND (“health data” OR “health record” OR “health information”) AND (willing* OR desir* OR eager* OR disposit* OR inclinat*).
As a second step, two of the investigators included studies searched through the reference lists of included/excluded papers or relevant reviews with no limitation on the year of publication. The identified papers were then screened based on their titles and abstracts, and papers that passed the screening were assessed for eligibility by full-text reading. Discrepancies were resolved by consulting a third opinion or conducting Delphi rounds with all the authors when necessary. The review protocol was registered with PROSPERO (registration number: CRD42022341477).
2.2. Inclusion and exclusion criteria
Papers were included if the studies measured the willingness to share PHI. We excluded the articles written in languages other than English and Italian, reviews, case reports, and those whose full text could not be obtained even after contacting the corresponding author.
2.3. Data extraction
Titles and abstracts were independently screened by two reviewers in duplicate to determine whether the retrieved studies met the inclusion criteria outlined above. The full papers were obtained for studies that appeared to have met the inclusion criteria, or if screening of the title and abstract resulted in uncertainty. The full texts of all papers that passed the screening were independently assessed for eligibility by two reviewers. Discrepancies were resolved with a third reviewer or Delphi rounds, if required. We used a standardized form to extract data from the included studies to assist in study quality and evidence synthesis. Extracted information included the following: focus of the study, participant characteristics, measurement of willingness to share PHI, criteria used to validate the final judgment, and authors’ conclusions, as well as information required for the assessment of the risk of bias. Data extraction was performed by two reviewers independently and in duplicate. A third reviewer was consulted, if necessary.
2.4. Data charting
The aims and main results of the selected studies were briefly described. The study design was as follows: when the authors used a questionnaire with no open-ended questions, interviews were conducted using an open-ended questionnaire.
2.5. Quality assessment
Two independent reviewers performed a quality assessment for the systematic reviews of qualitative evidence to assess the quality of the selected studies. The quality assessment tool was drawn directly from Appendix D of Hawker et al. (32) The tool consisted of nine questions, each of which can be answered with “good,” “fair,” “poor,” or “very poor,” which we subsequently converted into a numerical score (from 1 to 4 points). Hence, every study received a score (from 9 to 36 points) that defined their overall quality grade: high quality, 30–36 points; medium quality, 24–29 points; and low quality, 9–24 points. The nine questions in the tool were as follows:
1. Abstract and title. Did they provide a clear description of the study? Good: structured abstract with full information and clear title. Fair: informative abstract. Poor: inadequate abstract. Very poor: no abstract.
2. Introduction and aims. Was there a good background section and a clear statement on the aims of the research? Good: full but concise background to discussion/study containing up-to-date literature review and highlighting gaps in knowledge; clear statement of aim and objectives, including research questions. Fair: background, literature review, and research questions outlined. Poor: some background but no aim/objectives/questions or aims/objectives but an inadequate background. Very poor: no mention of aims/objectives; no background or literature review.
3. Methods and data. Is the method appropriate and clearly explained? Good: method is appropriate and described clearly (e.g., questionnaires included); clear details of data collection and recording. Fair: method is appropriate; the description could be better. Poor: questionable whether the method is appropriate; the method is described inadequately, with little description of the data. Very poor: no mention of method and/or method inappropriate, and/or no details of data.
4. Sampling. Was the sampling strategy appropriate to address the aims? Good: details (age/sex/race/context) of who was studied, how they were recruited, and why this group was targeted; the sample size was justified for the study; response rates were shown and explained. Fair: sample size justified; most information is given but some are missing. Poor: sampling mentioned but with few descriptive details. Very poor: no sample details.
5. Data analysis. Was the description of the data analysis sufficiently rigorous? Good: clear description of how the analysis was carried out; description of how themes were derived and of respondent validation or triangulation. Fair: descriptive analysis. Poor: minimal details of the analysis. Very poor: no discussion of the analysis.
6. Ethics and bias. Were ethical issues addressed and was the necessary ethical approval gained? Was the relationship between researchers and participants adequately considered? Good: ethics: when necessary, issues of confidentiality, sensitivity, and consent were addressed; bias: the researcher was reflexive and/or aware of their own bias. Fair: lip service was paid to the above (i.e., these issues were acknowledged). Poor: brief mention of issues. Very poor: no mention of issues.
7. Results. Is there a clear statement about the findings? Good: findings are explicit, easy to understand, and in a logical progression; tables, if present, are explained in text; results relate directly to aims; sufficient data are presented to support the findings. Fair: findings mentioned but more explanation could be given; data presented relate directly to results. Poor: findings presented haphazardly, not explained, and do not progress logically from the results. Very poor: findings not mentioned or unrelated to aims.
8. Transferability or generalizability. Are the findings transferable (generalizable) to a wider population? Good: context and setting of the study are described sufficiently to allow comparison with other contexts and settings, plus a high score in sampling (Q4). Fair: some context and setting are described, but more is needed to replicate or compare the study with others. Poor: minimal description of contexts/settings. Very poor: no description of context/setting.
9. Implications and usefulness. How important are the findings to policy and practice? Good: contributes something new and/or different in terms of understanding/insight or perspective; suggests ideas for further research and implications for policy and/or practice. Fair: two of the above. Poor: only one of these. Very poor: none of the above.
3. Results
3.1. Search, screening, full text assessment
Our database search identified 1,087 studies. After applying the inclusion criteria (language and type of paper), the authors included 924 papers, 353 of which were duplicates. The authors screened 571 studies based on the titles and abstracts; we identified 199 papers eligible for full-text assessment. The 89 papers that passed the assessment were included in the data extraction Figure 1 depicts the flow of the paper selection process.
3.2. Quality assessment
The quality assessment is available in the Supplementary material. The mean overall quality score was 25.4/36 (range 13–36), corresponding to the medium quality rate. The lowest average scores were for the sampling (average of 2.2/4) and ethics and bias items (average of 2.2/4). The highest average scores were for the introduction/aims (average of 3.3/4) and data analysis items (average of 3.2/4).
3.3. Methods analysis
The charted data are available in the Supplementary material. Among the 89 selected papers, 66 presented the results of a survey, 22, interviews, and one, an analysis of patients’ preferences in informed consent acquisition. Nine papers presented hypothetical scenarios to the participants, and 13 invited them to join focus groups. The recruiters were authors in 51 cases, a market research company in 25 cases, and a public/non-profit organization in 13 cases. The recruiters used the in-person approach in 21 cases, email announcements/social media posts/posted fliers in 19 cases, and telephone calls or letters in six cases. Forty-six papers used qualitative content analysis, factorial analysis, structural equation models, cluster analysis, or inductive approach; 43 papers used only descriptive and inferential statistics. The studies required online participation in 47 cases, in-person sessions in 28 cases, telephone sessions in three cases, and mixed methods in the other cases.
4. Discussion
As almost all (88/89) of the selected papers investigated willingness to share PHI through surveys or interviews, it was not possible to summarize the results with a meta-analysis. About half of the selected papers employed qualitative analysis (46/89), and the rest (43/89) used only descriptive or inferential statistics. The overall quality of the studies ranged from high (36/36) to low (13/36); however, the average overall quality grades corresponded to medium (25.4/36).
Of the 89 selected papers published between 2006 and 2022, only two were published before 2009. This finding suggests that interest in PHI management increased along with the digitalization of health care and the more general diffusion of information technologies, which emerged in the past two decades (30). The years 2019, 2020, and 2022 registered high publication rates (13, 18, and 13, respectively), and more than half of the studies (56/89) were published between 2019 and 2022. As the search was completed in June 2022, we assumed that the publication rate in 2022 is largely underestimated.
The COVID-19 pandemic has aroused debate concerning PHI. Public health authorities recognized the need to carry out contact-tracing and personal restrictions, which entailed collecting and sharing personal data and PHI (e.g., personal localization, results of SARS-CoV-2 tests) through and between public organizations (17, 33, 34). Consequently, the management of PHI during the pandemic raised serious privacy concerns (35, 36). However, patients have been more comfortable sharing PHI during the COVID-19 pandemic, especially with care institutions and researchers (37). This may be linked to the burden of the pandemic, which redefined people’s perception of benefits.
Indeed, a vast amount of PHI has been necessary to cope with the pandemic while managing contact tracing and vaccination efforts. In the same period, researchers have also hypothesized the use of crowdsensing for research, which consists of collecting people’s location information via mobile sensing devices (38). Although this hypothesis seemed to threaten the right to personal privacy, many other forms of crowdsensing (e.g., real location information sent by mobile phones) had been used, even including for commercial purposes (39). The pandemic has also triggered efforts to increase health literacy, which positively influences the willingness to share PHI (40). Owing to the spread of COVID-19, many health providers adopted telemedicine, which allowed the delivery of health care services without any close contact (41, 42). Whether and how telemedicine may have provided a vast amount of digital PHI and influenced the likelihood of sharing PHI remain unclear and deserve a deeper analysis.
In general, increasingly digitalized health enables new far-reaching opportunities for the secondary use of PHI. Secondary uses may be categorized as for public health (e.g., public health surveillance), research, health care quality improvement [e.g., adoption of electronic health records (EHR)], and commercial (e.g., marketing, health insurance) purposes (43). Our results clearly showed that the secondary use of PHI represented one of the most important determinants of the willingness to share PHI.
People tend to be willing to share their PHI for research (44–52). However, previous results may reflect a sort of selection bias: responders who declare a good willingness to share PHI for research purposes are more likely to already be actively participating in research. In other words, we could not determine how willingness to participate in research could influence the willingness to share PHI for research, even if they seem to be mutually related. The only way to reduce the impact of this bias would be to increase sample representativeness. Given this limitation, the willingness to share PHI for research has been associated with sociodemographic features (white race, higher educational attainment, lower religiosity, health literacy), but also with the perception of more research benefits (15, 53–55). Biobanks and other large research projects have registered similar results (53, 56).
However, the type of disclosed information still determines the willingness to share for research. For example, a sample of 36,268 individuals from 22 countries showed a low willingness to share DNA data for research (57). This result seems to confirm the theory of “genetic exceptionalism,” according to which genetic data should be treated separately from other medical information (58). Meanwhile, in the same study, responders experienced with genetics and those who self-defined as “genetic exceptionalist” were much more willing than others to disclose genetic data for research (57). Moreover, a recent study demonstrated that disclosing genetic data is acceptable if anonymity is ensured (59).
Regarding health care quality improvement, an increasing number of countries are adopting EHR, a tool that is expected to enable safe and high-performing data exchange among health policy-makers, providers, and patients (60). Patients are willing to share their PHI using EHR, especially with providers involved in their care, and to facilitate health information exchange between them (61–68). Nevertheless, selecting the PHI to share with EHR makes patients more comfortable and increases their willingness to adopt EHR (69). Among older adults, EHR acceptance is positively influenced by a higher degree of multimorbidity, higher number of prescribed medications, higher number of hospital admissions, and living with a chronic illness, whereas a pessimistic attitude and lack of joy in life, as indicators of depressive mood, have a negative impact (70).
Meanwhile, commercial use is a strong determinant of unwillingness to share PHI (71–74). Nonetheless, researchers and health care organizations often need commercial partners to recruit samples and obtain suitable cloud servers or other technological infrastructures, especially while building big data (75). Users of health and fitness apps are also aware that these apps transmit user data to several third parties (76). For example, among the reviewed papers, the sample was recruited by a private research company in 25/89 cases. One major concern regarding third-party commercial use of PHI is the risk of discrimination (insurance and employment), especially related to the sharing of genomic data and mobile/wearable device data (59, 66). Insurance discrimination may act subtly; some United States insurance companies have started to move to interactive life insurance models by providing discounts to customers who share fitness data via monitoring devices (77). In this context, the fear of possible genetic insurance discrimination looms large in the public imagination, and empirical data suggest that this holds people back from undergoing testing (77).
Another issue relates to employees’ privacy being challenged in several ways. For example, during the pandemic, employers faced many burning questions on data protection, including the conditions under which they could process employees’ PHI to ensure health safety in the workplace (78). The risk of discrimination may be even more concrete while building AI into PHI databases, as AI predictive models can contain several layers of potential bias (79).
Another secondary use of PHI is peer-to-peer information exchange, which mainly regards patients with chronic or serious diseases. Independent of the secondary users of PHI, our findings demonstrated that the type of disease significantly influenced individuals’ perceptions of usefulness, accessibility, psychological risk, privacy concerns, stigma, and willingness to share PHI (80–82). For example, people living with HIV and adolescents with diabetes typically participate in peer-to-peer digital groups to improve their daily self-management (83, 84). Despite this, people living with HIV accept data sharing more willingly depending on the efforts expended to ensure the confidentiality of HIV-related data, as the stigma surrounding HIV prompts hesitancy in sharing PHI (85).
Many authors stated that both the general population and patients are more willing to share their non-psychiatric medical information than psychiatric information (13, 48, 52, 86, 87). Meanwhile, people with mental illness have shown more willingness to share PHI even when it entails disclosing their mental disease (50). Hence, even if the stigma surrounding psychiatric conditions may inhibit the willingness to share medical information, the benefits of sharing perceived by psychiatric patients can overcome their sense of uncertainty (88).
Patients with cancer are also more willing to share their inherited genetic information and other medical details than daily life or identity information (69, 89). The information-sharing preferences of patients with cancer or cancer survivors are driven mainly by the purpose of information reuse and type of data shared (90, 91). The likelihood of sharing PHI among cancer survivors may rely on the altruistic belief that the data could benefit others (91). A similar “altruism” might have also promoted participation in public health efforts during the COVID-19 pandemic (33). However, the influence of altruism on sharing PHI may also depend on stressful experiences, such as surviving cancer or living through the pandemic.
The influence of low socioeconomic status on willingness to share PHI showed some contradictory results. Green et al. observed that a low socioeconomic status may negatively influence the willingness to share PHI (92). Otherwise, several authors have indicated that low-income people largely support the sharing of PHI if doing so demonstrates benefits (93–96). The contradictory influence of low socioeconomic status may be indirectly due to the observed positive influence of health literacy and trust in health organizations, which in turn may be linked to socioeconomic status (34, 70).
The major concerns regarding PHI sharing are data misuse and data breach (48, 51, 53, 56, 69, 97). As such, strong underlying privacy views affect willingness to share PHI, and anonymization assumes a crucial role (98–107). Hence, trust in data security and awareness of data-storing systems can enhance participation in data sharing and research (108–114).
Finally, the observed reticence about sharing non-medical information (e.g., socioeconomic status) highlights the importance of shared data (12, 115). An increasing number of researchers and research institutions consider AI as an opportunity for future development in many human activities. However, it requires immense volumes of data (big data), represented by PHI in the health care context.
We found that although the willingness to share PHI seemed to meet the interest of the research community, the methods used to measure it varied, making outcomes mutually incomparable. This represents a significant limitation of studying such an issue. Given the importance of health data sharing, a standardized method to assess the willingness to share PHI and its determinants is necessary.
5. Conclusion
Despite the progressive digitalization of health care and the crucial role of health data in health care and research, until date, no validated measurement tool has been developed for willingness to share PHI. The reviewed papers measured such willingness through surveys, interviews, and questionnaires, which were mutually incomparable. The secondary use of PHI was the major determinant of the likelihood of sharing PHI, whereas clinical and socioeconomic variables had slight effects. Privacy was the main concern discouraging data sharing. However, good data anonymization and the high perceived benefits of sharing may overcome such concern. A better understanding of the phenomenon may drive the development of patient-centered digital health care and more ethical and effective clinical research.
Author contributions
MB and GM conceptualized the research goals and wrote the original draft. FC, CC, and SN conducted the investigation. DF, AM, and BS reviewed and edited the paper. AM and BS coordinated the research activity. All authors contributed to the article and approved the submitted version.
Funding
This work was supported by the Horizon Europe Seeds program (ID S16—CUP H91I21001610006).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2023.1213615/full#supplementary-material
References
1. Bietz, MJ, Bloss, CS, Calvert, S, Godino, JG, Gregory, J, Claffey, MP, et al. Opportunities and challenges in the use of personal health data for health research. J Am Med Inform Assoc. (2016) 23:e42–8. doi: 10.1093/jamia/ocv118
2. Gerber, N, Gerber, P, and Volkamer, M. Explaining the privacy paradox: a systematic review of literature investigating privacy attitude and behavior. Comput Secur. (2018) 77:226–61. doi: 10.1016/j.cose.2018.04.002
3. Carrascal, JP, Riederer, C, Erramilli, V, Cherubini, M, and De Oliveira, R. Your browsing behavior for a big mac: Economics of personal information online. In Proceedings of the 22nd international conference on world wide web. (2013). p. 189–200
4. Huberman, BA, Adar, E, and Fine, LR. Valuating privacy. IEEE Secur Priv. (2005) 3:22–5. doi: 10.1109/MSP.2005.137
5. Aguirre, E, Roggeveen, AL, Grewal, D, and Wetzels, M. The personalization-privacy paradox: implications for new media. J Consum Mark. (2016) 33:98–110. doi: 10.1108/JCM-06-2015-1458
6. Hoffmann, CP, Lutz, C, and Ranzini, G. Privacy cynicism: a new approach to the privacy paradox. Cyberpsychology J Psychosoc Res Cybersp. (2016):10. doi: 10.5817/CP2016-4-7
7. Kokolakis, S . Privacy attitudes and privacy behaviour: a review of current research on the privacy paradox phenomenon. Comput Secur. (2017) 64:122–34. doi: 10.1016/j.cose.2015.07.002
8. Krahe, M, Milligan, E, and Reilly, S. Personal health information in research: perceived risk, trustworthiness and opinions from patients attending a tertiary healthcare facility. J Biomed Inform. (2019) 95:103222. doi: 10.1016/j.jbi.2019.103222
9. Anderson, CL, and Agarwal, R. The digitization of healthcare: boundary risks, emotion, and consumer willingness to disclose personal health information. Inf Syst Res. (2011) 22:469–90. doi: 10.1287/isre.1100.0335
10. Cheung, C, Bietz, MJ, Patrick, K, and Bloss, CS. Privacy attitudes among early adopters of emerging health technologies. PLoS One. (2016) 11:e0166389. doi: 10.1371/journal.pone.0166389
11. Woldaregay, AZ, Henriksen, A, Issom, D-Z, Pfuhl, G, Sato, K, Richard, A, et al. User expectations and willingness to share self-collected health data. Stud Health Technol Inform. (2020) 270:894–8. doi: 10.3233/SHTI200290
12. Serrano, KJ, Yu, M, Riley, WT, Patel, V, Hughes, P, Marchesini, K, et al. Willingness to exchange health information via Mobile devices: findings from a population-based survey. Ann Fam Med. (2016) 14:34–40. doi: 10.1370/afm.1888
13. Bosanac, D, and Stevanovic, A. Trust in E-health system and willingness to share personal health data. Stud Health Technol Inform. (2022) 289:256–9. doi: 10.3233/SHTI210908
14. Atchariyachanvanich, K, Mitinunwong, N, Tamthong, B, and Sonehara, N. Determinants of personal health information disclosure: a case of mobile application. Int J Softw Innov. (2018) 6:31–43. doi: 10.4018/IJSI.2018010103
15. Belfrage, S, Helgesson, G, and Lynøe, N. Trust and digital privacy in healthcare: a cross-sectional descriptive study of trust and attitudes towards uses of electronic health data among the general public in Sweden. BMC Med Ethics. (2022) 23:19. doi: 10.1186/s12910-022-00758-z
16. Leff, DR, and Yang, GZ. Big data for precision medicine. Engineering. (2015) 1:277–9. doi: 10.15302/J-ENG-2015075
17. Garett, R, and Young, SD. Ethical views on sharing digital data for public health surveillance: Analysis of survey data among patients. Front Big Data. (2022) 5:871236. doi: 10.3389/fdata.2022.871236
18. European Commission . EU4Health programme 2021–2027—A vision for a healthier European Union. (2021). Available at: https://health.ec.europa.eu/funding/eu4health-programme-2021-2027-vision-healthier-european-union_en. Accessed November 26, 2022.
19. Karampela, M, Ouhbi, S, and Isomursu, M. Connected health user willingness to share personal health data: questionnaire study. J Med Internet Res. (2019) 21:e14537. doi: 10.2196/14537
20. Hah, H . Health consumers’ daily habit of internet banking use as a proxy for understanding health information sharing behavior: quasi-experimental approach. J Med Internet Res. (2020) 22:e15585. doi: 10.2196/15585
21. Tosoni, S, Voruganti, I, Lajkosz, K, Habal, F, Murphy, P, Wong, RKS, et al. The use of personal health information outside the circle of care: consent preferences of patients from an academic health care institution. BMC Med Ethics. (2021) 22:29. doi: 10.1186/s12910-021-00598-3
22. Grande, D, Mitra, N, Iyengar, R, Merchant, RM, Asch, DA, Sharma, M, et al. Consumer willingness to share personal digital information for health-related uses. JAMA Netw Open. (2022) 5:e2144787. doi: 10.1001/jamanetworkopen.2021.44787
23. Beesley, SJ, Powell, A, Groat, D, Butler, J, Hopkins, RO, Rozenblum, R, et al. Evaluating the balance between privacy and access in digital information sharing. Crit Care Med. (2022) 50:e109–16. doi: 10.1097/CCM.0000000000005234
24. Nunes Vilaza, G, Coyle, D, and Bardram, JE. Public attitudes to digital Health Research repositories: cross-sectional international survey. J Med Internet Res. (2021) 23:e31294. doi: 10.2196/31294
25. Whiddett, R, Hunter, I, Engelbrecht, J, and Handy, J. Patients’ attitudes towards sharing their health information. Int J Med Inform. (2006) 75:530–41. doi: 10.1016/j.ijmedinf.2005.08.009
26. Almeida B De ADoneda, D, Ichihara, MY, Barral-Netto, M, Matta, GC, Rabello, ET, et al. Personal data usage and privacy considerations in the COVID-19 global pandemic. Cien Saude Colet. (2020) 25:2487–92. doi: 10.1590/1413-81232020256.1.11792020,
27. Vergallo, GM, Zaami, S, and Marinelli, E. The COVID-19 pandemic and contact tracing technologies, between upholding the right to health and personal data protection. Eur Rev Med Pharmacol Sci. (2021) 25:2449–56. doi: 10.26355/eurrev_202103_25286
28. Ribeiro-Navarrete, S, Saura, JR, and Palacios-Marqués, D. Towards a new era of mass data collection: assessing pandemic surveillance technologies to preserve user privacy. Technol Forecast Soc Change. (2021) 167:120681. doi: 10.1016/j.techfore.2021.120681
29. Lenert, L, and McSwain, BY. Balancing health privacy, health information exchange, and research in the context of the COVID-19 pandemic. J Am Med Informatics Assoc. (2020) 27:963–6. doi: 10.1093/jamia/ocaa039
30. Alami, H, Gagnon, M-P, and Fortin, J-P. Digital health and the challenge of health systems transformation. mHealth. (2017) 3:31. doi: 10.21037/mhealth.2017.07.02
31. Liberati, A, Altman, DG, Tetzlaff, J, Mulrow, C, Gøtzsche, PC, Ioannidis, JPA, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol. (2009) 62:e1–e34. doi: 10.1016/j.jclinepi.2009.06.006
32. Hawker, S, Payne, S, Kerr, C, Hardey, M, and Powell, J. Appraising the evidence: reviewing disparate data systematically. Qual Health Res. (2002) 12:1284–99. doi: 10.1177/1049732302238251
33. Nong, P, Raj, M, Trinidad, MG, Rowe, Z, and Platt, J. Understanding racial differences in attitudes about public health efforts during COVID-19 using an explanatory mixed methods design. Soc Sci Med. (2021) 287:114379. doi: 10.1016/j.socscimed.2021.114379
34. Lee, CMY, Thomas, E, Norman, R, Wells, L, Shaw, T, Nesbitt, J, et al. Educational attainment and willingness to use technology for health and to share health information–the reimagining healthcare survey. Int J Med Inform. (2022) 164:104803. doi: 10.1016/j.ijmedinf.2022.104803
35. Gerke, S, Shachar, C, Chai, PR, and Cohen, IG. Regulatory, safety, and privacy concerns of home monitoring technologies during COVID-19. Nat Med. (2020) 26:1176–82. doi: 10.1038/s41591-020-0994-1
36. Chan, EY, and Saqib, NU. Privacy concerns can explain unwillingness to download and use contact tracing apps when COVID-19 concerns are high. Comput Human Behav. (2021) 119:106718. doi: 10.1016/j.chb.2021.106718
37. Tosoni, S, Voruganti, I, Lajkosz, K, Mustafa, S, Phillips, A, Kim, SJ, et al. Patient consent preferences on sharing personal health information during the COVID-19 pandemic: “the more informed we are, the more likely we are to help”. BMC Med Ethics. (2022) 23:53. doi: 10.1186/s12910-022-00790-z
38. Asif, H, Papakonstantinou, PA, Shiau, S, Singh, V, and Vaidya, J. Intelligent pandemic surveillance via privacy-preserving Crowdsensing. IEEE Intell Syst. (2022) 37:88–96. doi: 10.1109/mis.2022.3145691
39. Ma, D, Kong, D, Chen, X, Zhang, L, and Yuan, M. Robot location privacy protection based on Q-learning particle swarm optimization algorithm in mobile crowdsensing. Front Neurorobot. (2022) 16:981390. doi: 10.3389/fnbot.2022.981390
40. Świątkiewicz-Mośny, M, Prokop-Dorner, A, Ślusarczyk, M, Ożegalska-Łukasik, N, Piłat-Kobla, A, Zając, J, et al. When Peppa pig and Confucius meet, joining forces on the battlefield of health literacy-a qualitative analysis of COVID-19 educational materials for children and adolescents from China, the USA, and Europe. PLoS One. (2022) 17:e0278554. doi: 10.1371/journal.pone.0278554
41. Ferorelli, D, Moretti, L, Benevento, M, Mastrapasqua, M, Telegrafo, M, Solarino, B, et al. Digital health care, telemedicine, and medicolegal issues in orthopedics: a review. Int J Environ Res Public Health. (2022) 19:15653. doi: 10.3390/ijerph192315653
42. Ferorelli, D, Celentano, FE, Benevento, M, Dell’Erba, A, and Solarino, B. Destruction of telecommunications hinders access to healthcare: a crime against humanity? J Telemed Telecare. (2023) 29:72. doi: 10.1177/1357633X221103829
43. Grande, D, Mitra, N, Shah, A, Wan, F, and Asch, DA. Public preferences about secondary uses of electronic health information. JAMA Intern Med. (2013) 173:1798–806. doi: 10.1001/jamainternmed.2013.9166
44. Seltzer, E, Goldshear, J, Guntuku, SC, Grande, D, Asch, DA, Klinger, EV, et al. Patients’ willingness to share digital health and non-health data for research: a cross-sectional study. BMC Med Inform Decis Mak. (2019) 19:157. doi: 10.1186/s12911-019-0886-9
45. Grant, A, Ure, J, Nicolson, DJ, Hanley, J, Sheikh, A, McKinstry, B, et al. Acceptability and perceived barriers and facilitators to creating a national research register to enable’direct to patient’enrolment into research: the Scottish Health Research register (SHARE). BMC Health Serv Res. (2013) 13:1–15. doi: 10.1186/1472-6963-13-422
46. Kim, J, Kim, H, Bell, E, Bath, T, Paul, P, Pham, A, et al. Patient perspectives about decisions to share medical data and biospecimens for research. JAMA Netw Open. (2019) 2:e199550. doi: 10.1001/jamanetworkopen.2019.9550
47. Goodman, D, Johnson, CO, Bowen, D, Smith, M, Wenzel, L, and Edwards, K. De-identified genomic data sharing: the research participant perspective. J Community Genet. (2017) 8:173–81. doi: 10.1007/s12687-017-0300-1
48. Weng, C, Friedman, C, Rommel, CA, and Hurdle, JF. A two-site survey of medical center personnel’s willingness to share clinical data for research: implications for reproducible health NLP research. BMC Med Inform Decis Mak. (2019) 19:70. doi: 10.1186/s12911-019-0778-z
49. Weitzman, ER, Kaci, L, and Mandl, KD. Sharing medical data for health research: the early personal health record experience. J Med Internet Res. (2010) 12:e14. doi: 10.2196/jmir.1356
50. Kirkham, EJ, Lawrie, SM, Crompton, CJ, Iveson, MH, Jenkins, ND, Goerdten, J, et al. Experience of clinical services shapes attitudes to mental health data sharing: findings from a UK-wide survey. BMC Public Health. (2022) 22:357. doi: 10.1186/s12889-022-12694-z
51. Udesky, JO, Boronow, KE, Brown, P, Perovich, LJ, and Brody, JG. Perceived risks, benefits, and interest in participating in environmental health studies that share personal exposure data: a U.S. survey of prospective participants. J Empir Res Hum Res Ethics. (2020) 15:425–42. doi: 10.1177/1556264620903595
52. Soni, H, Grando, A, Aliste, MP, Murcko, A, Todd, M, Mukundan, M, et al. Perceptions and preferences about granular data sharing and privacy of behavioral health patients. Stud Health Technol Inform. (2019) 264:1361–5. doi: 10.3233/SHTI190449
53. Sanderson, SC, Brothers, KB, Mercaldo, ND, Clayton, EW, Antommaria, AHM, Aufox, SA, et al. Public attitudes toward consent and data sharing in biobank research: a large multi-site experimental survey in the US. Am J Hum Genet. (2017) 100:414–27. doi: 10.1016/j.ajhg.2017.01.021
54. Wagner, L, Frisch, M, Turner-Brown, L, Andrews, S, Edwards, A, Moultrie, R, et al. Preferences for the research use of electronic health records among young adults with fragile X syndrome or autism spectrum disorder. Disabil Health J. (2020) 13:100927. doi: 10.1016/j.dhjo.2020.100927
55. Hentschel, A, Hsiao, CJ, Chen, LY, Wright, L, Shaw, J, Du, X, et al. Perspectives of pregnant and breastfeeding women on participating in longitudinal mother-baby studies involving electronic health records: qualitative study. JMIR Pediatr Parent. (2021) 4:e23842. doi: 10.2196/23842
56. Brall, C, Berlin, C, Zwahlen, M, Ormond, KE, Egger, M, and Vayena, E. Public willingness to participate in personalized health research and biobanking: a large-scale Swiss survey. PLoS One. (2021) 16:e0249141. doi: 10.1371/journal.pone.0249141
57. Middleton, A, Milne, R, Almarri, MA, Anwer, S, Atutornu, J, Baranova, EE, et al. Global public perceptions of genomic data sharing: what shapes the willingness to donate DNA and health data? Am J Hum Genet. (2020) 107:743–52. doi: 10.1016/j.ajhg.2020.08.023
58. Evans, JP, and Burke, W. Genetic exceptionalism too much of a good thing? Genet Med. (2008) 10:500–1. doi: 10.1097/GIM.0b013e31817f280a
59. Vidgen, ME, Kaladharan, S, Malacova, E, Hurst, C, and Waddell, N. Sharing genomic data from clinical testing with researchers: public survey of expectations of clinical genomic data management in Queensland. Australia BMC Med Ethics. (2020) 21:119. doi: 10.1186/s12910-020-00563-6
60. Cherif, E, and Mzoughi, M. Electronic health record adopters: a typology based on patients’ privacy concerns and perceived benefits. Public Health. (2022) 207:46–53. doi: 10.1016/j.puhe.2022.03.010
61. Teixeira, PA, Gordon, P, Camhi, E, and Bakken, S. HIV patients’ willingness to share personal health information electronically. Patient Educ Couns. (2011) 84:e9–e12. doi: 10.1016/j.pec.2010.07.013
62. Jackman, K-MP, Hightow-Weidman, L, Poteat, T, Wirtz, AL, Kane, JC, and Baral, SD. Evaluating psychometric determinants of willingness to adopt sexual health patient portal services among black college students: a mixed-methods approach. J Am Coll Heal. (2021) 69:190–7. doi: 10.1080/07448481.2019.1660352
63. Hunter, IM, Whiddett, RJ, Norris, AC, McDonald, BW, and Waldon, JA. New Zealanders’ attitudes towards access to their electronic health records: preliminary results from a national study using vignettes. Health Informatics J. (2009) 15:212–28. doi: 10.1177/1460458209337435
64. Esmaeilzadeh, P, and Mirzaei, T. Comparison of consumers’ perspectives on different health information exchange (HIE) mechanisms: an experimental study. Int J Med Inform. (2018) 119:1–7. doi: 10.1016/j.ijmedinf.2018.08.007
65. Kim, KK, Sankar, P, Wilson, MD, and Haynes, SC. Factors affecting willingness to share electronic health data among California consumers. BMC Med Ethics. (2017) 18:25. doi: 10.1186/s12910-017-0185-x
66. Weitzman, ER, Kelemen, S, Kaci, L, and Mandl, KD. Willingness to share personal health record data for care improvement and public health: a survey of experienced personal health record users. BMC Med Inform Decis Mak. (2012) 12:39. doi: 10.1186/1472-6947-12-39
67. Yaraghi, N, Sharman, R, Gopal, R, Singh, R, and Ramesh, R. Drivers of information disclosure on health information exchange platforms: insights from an exploratory empirical study. J Am Med Inform Assoc. (2015) 22:1183–6. doi: 10.1093/jamia/ocv086
68. Al-Khalifa, M, Khatoon, S, Mahmood, A, and Fatima, I. Factors influencing patients’ attitudes to exchange electronic health information in Saudi Arabia: an exploratory study. Int J Adv Comput Sci Appl. (2016) 7:7. doi: 10.14569/IJACSA.2016.070827
69. Weis, A, Pohlmann, S, Poss-Doering, R, Strauss, B, Ullrich, C, Hofmann, H, et al. Caregivers’ role in using a personal electronic health record: a qualitative study of cancer patients and caregivers in Germany. BMC Med Inform Decis Mak. (2020) 20:158. doi: 10.1186/s12911-020-01172-4
70. Halmdienst, N, Pruckner, GJ, and Winter-Ebmer, R. Complexities of health and acceptance of electronic health records for the Austrian elderly population. Eur J Health Econ. (2022) 24:53–66. doi: 10.1007/s10198-022-01451-z
71. Kim, TK, and Choi, M. Older adults’ willingness to share their personal and health information when adopting healthcare technology and services. Int J Med Inform. (2019) 126:86–94. doi: 10.1016/j.ijmedinf.2019.03.010
72. Kim, KK, Joseph, JG, and Ohno-Machado, L. Comparison of consumers’ views on electronic data sharing for healthcare and research. J Am Med Inform Assoc. (2015) 22:821–30. doi: 10.1093/jamia/ocv014
73. Braunack-Mayer, A, Fabrianesi, B, Street, J, O’Shaughnessy, P, Carter, SM, Engelen, L, et al. Sharing government health data with the private sector: community attitudes survey. J Med Internet Res. (2021) 23:e24200. doi: 10.2196/24200
74. Kimura, M, Nakaya, JA, Watanabe, H, Shimizu, T, and Nakayasu, K. Survey aimed at general citizens of the US and Japan about their attitudes toward electronic medical data handling. Copyright: Creative Commons License. (2014) 11:4572–88. doi: 10.3390/ijerph110504572
75. Trinidad, MG, Platt, J, and Kardia, SLR. The public’s comfort with sharing health data with third-party commercial companies. Humanit Soc Sci Commun. (2020) 7:1–10. doi: 10.1057/s41599-020-00641-5
76. Challa, N, Yu, S, and Kunchakarra, S. Wary about wearables: potential for the exploitation of wearable health technology through employee discrimination and sales to third parties. Intersect Stanford J Sci Technol Soc. (2017):10.
77. Bélisle-Pipon, J-C, Vayena, E, Green, RC, and Cohen, IG. Genetic testing, insurance discrimination and medical research: what the United States can learn from peer countries. Nat Med. (2019) 25:1198–204. doi: 10.1038/s41591-019-0534-z
78. Suder, S . Processing employees’ personal data during the Covid-19 pandemic. Eur Labour Law J. (2021) 12:322–37. doi: 10.1177/2031952520978994
79. Murray, SG, Wachter, RM, and Cucina, RJ. Discrimination by artificial intelligence in a commercial electronic health record—a case study. Heal Aff Blog. (2020):10. doi: 10.1377/forefront.20200128.626576
80. Esmaeilzadeh, P, Mirzaei, T, and Dharanikota, S. The impact of data entry structures on perceptions of individuals with chronic mental disorders and physical diseases towards health information sharing. Int J Med Inform. (2020) 141:104157. doi: 10.1016/j.ijmedinf.2020.104157
81. Ernst, ME, Sandberg, DE, Keegan, C, Quint, EH, Lossie, AC, and Yashar, BM. The lived experience of MRKH: sharing health information with peers. J Pediatr Adolesc Gynecol. (2016) 29:154–8. doi: 10.1016/j.jpag.2015.09.009
82. Navarro-Millán, I, Zinski, A, Shurbaji, S, Johnson, B, Fraenkel, L, Willig, J, et al. Perspectives of rheumatoid arthritis patients on electronic communication and patient-reported outcome data collection: a qualitative study. Arthritis Care Res (Hoboken). (2019) 71:80–7. doi: 10.1002/acr.23580
83. Bussone, A, Kasadha, B, Stumpf, S, Durrant, AC, Tariq, S, Gibbs, J, et al. Trust, identity, privacy, and security considerations for designing a peer data sharing platform between people living with HIV. Proc ACM Human-Computer Interact. (2020) 4:1–27. doi: 10.1145/3415244
84. Vaala, SE, Lee, JM, Hood, KK, and Mulvaney, SA. Sharing and helping: predictors of adolescents’ willingness to share diabetes personal health information with peers. J Am Med Inform Assoc. (2018) 25:135–41. doi: 10.1093/jamia/ocx051
85. Maiorana, A, Steward, WT, Koester, KA, Pearson, C, Shade, SB, Chakravarty, D, et al. Trust, confidentiality, and the acceptability of sharing HIV-related patient data: lessons learned from a mixed methods study about health information exchanges. Implement Sci. (2012) 7:34. doi: 10.1186/1748-5908-7-34
86. Yu, E, Adams-Clark, A, Riehm, A, Franke, C, Susukida, R, Pinto, M, et al. Perspectives on illness-related stigma and electronically sharing psychiatric health information by people with multiple sclerosis. J Affect Disord. (2021) 282:840–5. doi: 10.1016/j.jad.2020.12.167
87. Soni, H, Grando, A, Murcko, A, Diaz, S, Mukundan, M, Idouraine, N, et al. State of the art and a mixed-method personalized approach to assess patient perceptions on medical record sharing and sensitivity. J Biomed Inform. (2020) 101:103338. doi: 10.1016/j.jbi.2019.103338
88. Matthews, EB, Savoy, M, Paranjape, A, Washington, D, Hackney, T, Galis, D, et al. Acceptability of health information exchange and patient portal use in depression care among underrepresented patients. J Gen Intern Med. (2022) 37:3947–55. doi: 10.1007/s11606-022-07427-2
89. Frost, J, Vermeulen, IE, and Beekers, N. Anonymity versus privacy: selective information sharing in online cancer communities. J Med Internet Res. (2014) 16:e126. doi: 10.2196/jmir.2684
90. Grande, D, Asch, DA, Wan, F, Bradbury, AR, Jagsi, R, and Mitra, N. Are patients with Cancer less willing to share their health information? Privacy, sensitivity, and social purpose. J Oncol Pract. (2015) 11:378–83. doi: 10.1200/JOP.2015.004820
91. Smith, TG, Dunn, ME, Levin, KY, Tsakraklides, SP, Mitchell, SA, van de Poll-Franse, LV, et al. Cancer survivor perspectives on sharing patient-generated health data with central cancer registries. Qual life Res an Int J Qual life Asp Treat care Rehabil. (2019) 28:2957–67. doi: 10.1007/s11136-019-02263-0
92. Green, BB, Anderson, ML, Ralston, JD, Catz, S, Fishman, PA, and Cook, AJ. Patient ability and willingness to participate in a web-based intervention to improve hypertension control. J Med Internet Res. (2011) 13:e1625. doi: 10.2196/jmir.1625
93. Patel, VN, Dhopeshwarkar, RV, Edwards, A, Barron, Y, Likourezos, A, Burd, L, et al. Low-income, ethnically diverse consumers’ perspective on health information exchange and personal health records. Inform Health Soc Care. (2011) 36:233–52. doi: 10.3109/17538157.2011.554930
94. Kitayama, K, Stockwell, MS, Vawdrey, DK, Peña, O, and Catallozzi, M. Parent perspectives on the design of a personal online pediatric immunization record. Clin Pediatr (Phila). (2014) 53:238–42. doi: 10.1177/0009922813506608
95. Lucero, RJ, Kearney, J, Cortes, Y, Arcia, A, Appelbaum, P, Fernández, RL, et al. Benefits and risks in secondary use of digitized clinical data: views of community members living in a predominantly ethnic minority urban neighborhood. AJOB Empir Bioeth. (2015) 6:12–22. doi: 10.1080/23294515.2014.949906
96. Bouras, A, Simoes, EJ, Boren, S, Hicks, L, Zachary, I, Buck, C, et al. Non-Hispanic white mothers’ willingness to share personal health data with researchers: survey results from an opt-in panel. J Particip Med. (2020) 12:e14062. doi: 10.2196/14062
97. Simon, SR, Evans, JS, Benjamin, A, Delano, D, and Bates, DW. Patients’ attitudes toward electronic health information exchange: qualitative study. J Med Internet Res. (2009) 11:e30. doi: 10.2196/jmir.1164
98. Haddow, G, Bruce, A, Sathanandam, S, and Wyatt, JC. “Nothing is really safe”: a focus group study on the processes of anonymizing and sharing of health data for research purposes. J Eval Clin Pract. (2011) 17:1140–6. doi: 10.1111/j.1365-2753.2010.01488.x
99. Valdez, AC, and Ziefle, M. The users’ perspective on the privacy-utility trade-offs in health recommender systems. Int J Hum Comput Stud. (2019) 121:108–21. doi: 10.1016/j.ijhcs.2018.04.003
100. Wu, B, Luo, P, Li, M, and Hu, X. The impact of health information privacy concerns on engagement and payment behaviors in online health communities. Front Psychol. (2022):13. doi: 10.3389/fpsyg.2022.861903
101. Li, T, and Slee, T. The effects of information privacy concerns on digitizing personal health records. J Assoc Inf Sci Technol. (2014) 65:1541–54. doi: 10.1002/asi.23068
102. Cherif, E, Bezaz, N, and Mzoughi, M. Do personal health concerns and trust in healthcare providers mitigate privacy concerns? Effects on patients’ intention to share personal health data on electronic health records. Soc Sci Med. (2021) 283:114146. doi: 10.1016/j.socscimed.2021.114146
103. Esmaeilzadeh, P, and Mirzaei, T. The potential of Blockchain Technology for Health Information Exchange: experimental study from patients’ perspectives. J Med Internet Res. (2019) 21:e14184. doi: 10.2196/14184
104. Milne, R, Morley, KI, Howard, H, Niemiec, E, Nicol, D, Critchley, C, et al. Trust in genomic data sharing among members of the general public in the UK, USA. Canada Australia Hum Genet. (2019) 138:1237–46. doi: 10.1007/s00439-019-02062-0
105. Middleton, A, Milne, R, Howard, H, Niemiec, E, Robarts, L, Critchley, C, et al. Members of the public in the USA, UK, Canada and Australia expressing genetic exceptionalism say they are more willing to donate genomic data. Eur J Hum Genet. (2020) 28:424–34. doi: 10.1038/s41431-019-0550-y
106. Medford-Davis, LN, Chang, L, and Rhodes, KV. Health information exchange: what do patients want? Health Informatics J. (2017) 23:268–78. doi: 10.1177/1460458216647190
107. Helou, S, Abou-Khalil, V, El Helou, E, and Kiyono, K. Factors related to personal health data sharing: data usefulness, sensitivity and anonymity. Stud Health Technol Inform. (2021) 281:1051–5. doi: 10.3233/SHTI210345
108. Lysaght, T, Ballantyne, A, Xafis, V, Ong, S, Schaefer, GO, Ling, JMT, et al. “Who is watching the watchdog?”: ethical perspectives of sharing health-related data for precision medicine in Singapore. BMC Med Ethics. (2020) 21:1–11. doi: 10.1186/s12910-020-00561-8
109. Bansal, G, and Gefen, D. The impact of personal dispositions on information sensitivity, privacy concern and trust in disclosing health information online. Decis Support Syst. (2010) 49:138–50. doi: 10.1016/j.dss.2010.01.010
110. Sun, S, Zhang, J, Zhu, Y, Jiang, M, and Chen, S. Exploring users’ willingness to disclose personal information in online healthcare communities: the role of satisfaction. Technol Forecast Soc Change. (2022) 178:121596. doi: 10.1016/j.techfore.2022.121596
111. Holm, S, Kristiansen, TB, and Ploug, T. Control, trust and the sharing of health information: the limits of trust. J Med Ethics. (2021) 47:e35–5. doi: 10.1136/medethics-2019-105887
112. Lu, C, Batista, D, Hamouda, H, and Lemieux, V. Consumers’ intentions to adopt blockchain-based personal health records and data sharing: focus group study. JMIR Form Res. (2020) 4:e21995. doi: 10.2196/21995
113. Khan, FA, Rahman, A, Alharbi, M, and Qawqzeh, YK. Awareness and willingness to use PHR: a roadmap towards cloud-dew architecture based PHR framework. Multimed Tools Appl. (2020) 79:8399–413. doi: 10.1007/s11042-018-6692-z
114. Juga, J, Juntunen, J, and Koivumäki, T. Willingness to share personal health information: impact of attitudes, trust and control. Rec Manag J. (2021) 31:48–59. doi: 10.1108/RMJ-02-2020-0005
Keywords: health data, personal health information, secondary data uses, privacy, data sharing
Citation: Benevento M, Mandarelli G, Carravetta F, Ferorelli D, Caterino C, Nicolì S, Massari A and Solarino B (2023) Measuring the willingness to share personal health information: a systematic review. Front. Public Health. 11:1213615. doi: 10.3389/fpubh.2023.1213615
Edited by:
Ahmed Shuhaiber, Zayed University, United Arab EmiratesReviewed by:
Paraskevi Papadopoulou, American College of Greece, GreeceJorge Calvillo-Arbizu, Sevilla University, Spain
Copyright © 2023 Benevento, Mandarelli, Carravetta, Ferorelli, Caterino, Nicolì, Massari and Solarino. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Marcello Benevento, bWFyY2VsbG8wODM1QGdtYWlsLmNvbQ==
†ORCID: Marcello Benevento https://orcid.org/0000-0002-4895-0182
 Marcello Benevento
Marcello Benevento Gabriele Mandarelli
Gabriele Mandarelli Francesco Carravetta
Francesco Carravetta Davide Ferorelli1
Davide Ferorelli1 Simona Nicolì
Simona Nicolì