- 1Department of Epidemiology and Biostatistics, School of Public Health, Tianjin Medical University, Tianjin, China
- 2Department of Pulmonary and Critical Care Medicine, Center of Respiratory Medicine, China-Japan Friendship Hospital, National Clinical Research Center for Respiratory Diseases, Beijing, China
- 3Clinical Pharmacology Department, Zhejiang Hisun Pharmaceutical Co., Ltd., Taizhou, Zhejiang, China
- 4Department of Epidemiology and Preventive Medicine, School of Public Health and Preventive Medicine, Monash University, Melbourne, VIC, Australia
- 5Department of Endocrinology, Tianjin Hospital, Tianjin, China
- 6Thoracic Clinical College, Tianjin Medical University, Tianjin, China
- 7Cardiovascular Institute, Tianjin Chest Hospital, Tianjin, China
- 8Chinese PLA Center for Disease Control and Prevention, Beijing, China
Objectives: Exposure to air pollution has been linked to an increased risk of premature mortality. However, the acute effects of air pollution on the risk of non-accidental mortality have not been extensively researched in developing countries, and the findings thus far have been inconsistent. Therefore, this study aimed to examine the association between short-term exposure to six pollutants (PM2.5, PM10, SO2, NO2, O3, and CO) and non-accidental mortality in Beijing, China.
Methods: Daily data on non-accidental deaths were gathered from 1 January 2017 to 31 December 2018. Air pollution data for the same period were collected from 35 fixed-site air quality monitoring stations in Beijing. Generalized additive models (GAM) based on Poisson regression were used to investigate the association between non-accidental mortality in emergency department visits and the daily average levels of air pollutants.
Results: There were 8,676 non-accidental deaths recorded during 2017–2018. After sensitivity analysis, short-term exposure to air pollutants, particularly gaseous pollutants, was linked to non-accidental mortality. Specifically, for every 10 μg/m3 increase (5 μg/m3 in SO2, 0.5 mg/m3 in CO) of SO2 (lag 04), NO2 (lag 04), O3 (lag 05), and CO (lag 04), the relative risk (RR) values were 1.054 (95% CI: 1.009, 1.100), 1.038 (95% CI: 1.013, 1.063), 1.032 (95% CI: 1.011, 1.054), and 1.034 (95% CI: 1.004, 1.066), respectively. In terms of causes of death, short-term exposure to NO2, SO2, and O3 increased the risk of circulatory mortality. Further stratified analysis revealed that the stronger associations were presented in females for O3 while in males for CO. People aged 65 and over were strongly associated with ambient air pollution.
Conclusions: Our study showed that ambient air pollutants were associated with non-accidental mortality. Our findings suggested that efforts to control gaseous pollution should be stepped up, and vulnerable groups should be the focus of health protection education.
1. Introduction
With urbanization and modernization, China has become one of the countries suffering from the most serious air pollution (1, 2). Air pollution has become the fourth leading cause of mortality in China, and it has been related to an increased chance of premature death due to heart disease, stroke, and lung cancer (3–5). The severity of air pollution in China is evident from the frequent occurrence of haze events in recent years, which has raised significant concern (6). Since the beginning of 2013, the incidence and extent of haze have quickly grown with 75% of cities and 8 million people suffering from haze pollution in China, which presents a significant challenge to public health (7).
In response, China has implemented policies such as the Air Pollution Prevention and Control Action Plan (APPCAP) to enhance air quality and lessen the harmful impacts of pollution on human health (8). However, the air quality in Beijing remains critical, with average pollutant concentrations exceeding the World Health Organization's (WHO) targets (9). Recently, a growing number of epidemiological studies have been done in China to gain a comprehensive understanding of the short-term impacts of air pollution on non-accidental mortality (10, 11). Air pollution in China is complexly characterized by high levels of PM2.5 and O3 (12). A recent meta-analysis in China confirmed that short-term exposure to O3 was associated with an elevated risk of cardiovascular mortality (13). Significant links were found between short-term coarse particulate matter exposure and daily non-accidental mortality in a nationwide analysis of 272 Chinese cities (14). However, the findings on gaseous pollutants (SO2 and NO2) were not entirely consistent across several studies. For instance, the time-series study conducted in Hefei City showed SO2 was linked with non-accidental mortality (15), while studies in Northern China and the Pearl River Delta region reported no association between SO2 and mortality (16, 17). Furthermore, the studies from Hong Kong and Taipei City reported a significant increase in respiratory disease mortality associated with short-term NO2 exposure (18, 19), while another study conducted in Beijing reported a positive but non-significant association (20). It is noteworthy that very few studies have analyzed directly the association between non-accidental deaths and short-term exposure to air pollutants, where both particulate matter and gaseous pollutants are involved (21, 22). Therefore, it is necessary to conduct more research to better understand the relationship between air pollution and non-accidental mortality in China.
Previous studies have predominantly relied on hospitalization data as the primary data source to investigate the association between air pollution and non-accidental mortality, with limited utilization of emergency department data (23, 24). The study has the advantage of providing the evidence of the association between air pollutants (particulate matter and gaseous pollutants) and emergency non-accidental mortality in Beijing. First of all, emergency data provides faster feedback because emergency services typically respond immediately and record relevant data. This allows us to observe acute health events and mortality cases related to air pollution more promptly. Secondly, since emergency services are accessible to the public and people are more likely to seek emergency assistance during acute conditions, these data can cover a broader range of age groups and populations. Some studies have shown that it is significant to examine emergency department data specifically, as it represents more immediate, acute impacts and may identify vulnerability in specific populations (25, 26). Finally, emergency department data can avoid the interference of cross-regional visits when compared with hospitalization data, and brings the advantage of exposure assessment (27).
As the capital of China, Beijing is situated in northern China, with high population density, high levels of industrialization, long heating hours, and high air pollution levels (28). Therefore, it becomes very important to develop related preventive strategies to protect public health, especially sensitive populations, by estimating the acute health impacts of air pollution. This study performed a time-series analysis to investigate the short-term effects of six air pollutants (PM2.5, PM10, SO2, NO2, O3, and CO) on non-accidental mortality in Beijing and to explore the populations vulnerable to adverse effects of pollutant exposure.
2. Materials and methods
2.1. Data collection
The death data during 2017–2018 including the gender, age, and causes of death were collected from Beijing Red Cross Emergency Medical Center, which excluded accidental deaths. Causes of death were classified according to the International Classification of Diseases (ICD-10; non-accidental death: A00-R99, neoplasms disease death: C00–D48, respiratory system disease death: J00-J98, circulatory system disease death: I00–I99). Then, we stratified the non-accidental deaths by sex (male and female), age (< 65 and ≥65 years). This study was approved by the Ethics Committees of Tianjin Medical University (No. TMUhMEC 2021009).
The Chinese National Environmental Monitoring Center provided air pollution data during 2017–2018 through their online platform. For all measurements, they were made in accordance with China's National Air Quality Control standards (GB3095-2012). The 24-h average daily concentrations were calculated from the average of 35 fixed-site air quality–monitoring stations, with an average of one monitoring station per 468.9 km2. The 24-h average concentrations of six air pollutants including PM2.5, PM10, CO, SO2, NO2, and O3 were used for further analysis. For adjustment in the analysis, we also extracted the daily average temperature and relative humidity from the China Meteorological Science Data Sharing Service System (http://data.cma.cn/) between 1 January 2017 and 31 December 2018.
2.2. Statistical analysis
A time-series design was used in the research to investigate the relationship between short-term exposure to air pollutants and non-accidental mortality in emergency department visits. Descriptive analysis was used for daily non-accidental deaths, air pollutants (PM2.5, PM10, SO2, NO2, O3, and CO), and meteorological variables (daily average temperature and relative humidity). We investigated the collinearity between air pollutants and meteorological variables using Spearman correlation analysis. Non-accidental mortality in emergency department visits is a low-chance occurrence in this research, with the distribution roughly following the Poisson distribution. Thus, the assessment of the relationship between the daily non-accidental deaths in the emergency department visits and the daily average concentrations of air pollutants was performed by generalized additive models (GAM) based on Poisson regression. The formulation of this study is as follows:
E(Yt) represents the expected number of non-accidental deaths in emergency department visits at day t; α stands for the model intercept and β indicates the log-relative risk (RR) of daily non-accidental mortality associated with a unit increase of pollutant concentrations (Zt); ns shows the natural cubic spline smooth function and df is its degree of freedom. The ns (time, df1) is utilized to consider seasonality and long-term trends. The 12 degrees of freedom per year for the time variable were chosen based on the Akaike information criterion (AIC) minimization and previous research (29). Daily average temperature and relative humidity were included as covariates in the formula. By referring to previous literature (30–32), we chose 6 df for daily average temperature and 3 df for daily average humidity to account for the possible non-linear confounding effects of meteorological variables. The day of the week (DOW) is controlled as a binary variable.
We separately incorporated the air pollutants into the GAM for exploring the relationship between air pollution and daily non-accidental mortality. To explore the potentially delayed effects, we used single lag exposure (lag 0-lag 5) and cumulative lag exposure (lag 01-lag 05). The concentration of pollutant on that day was considered as lag 0, and the concentration of pollutant on the previous 5th day was considered as lag 5. The 6-day moving average pollutant concentration for the current and prior 5 days was recorded as lag 05. We also conducted stratified analyses by age and sex. The Z-test was utilized to compare the differences in groups with the following formula:
As an example of sex-stratified analysis, β1 and β2 are the effect estimates for males and females, while SE1 and SE2 are standard errors.
Sensitivity analyses were performed in this study to ensure the stability of the results. Firstly, we used alternative df to control the time trend (10–14), temperature (2–7), and relative humidity (2–7) in single-pollutant models. Secondly, two-pollutant models and multi-pollutant models were used to check the confounding effect on non-accidental mortality from co-pollutants. The pollutants with Spearman correlation values >0.60 were not included in models simultaneously to prevent multicollinearity (33). Since temperature has been found to have prolonged health effects in previous studies (34, 35), we also controlled the potential lagged effects of temperature (up to 28 days). Finally, exposure-response (E-R) curves between non-accidental mortality and six air pollutants were plotted based on GAM.
The results were presented as the estimated RR with the corresponding 95% confidence interval (CI) of non-accidental mortality in emergency department visits for every 10 μg/m3 (PM2.5, PM10, NO2, and O3), 5 μg/m3 (SO2) or 0.5 mg/m3 (CO) increase in ambient air pollutants. In this study, statistical tests were using two-tailed tests, and P-values < 0.05 were considered to be statistically significant. R (version 4.1.3) “mgcv” and “splines” packages (R Development Core Team, Vienna, Austria) were used for statistical analysis.
3. Results
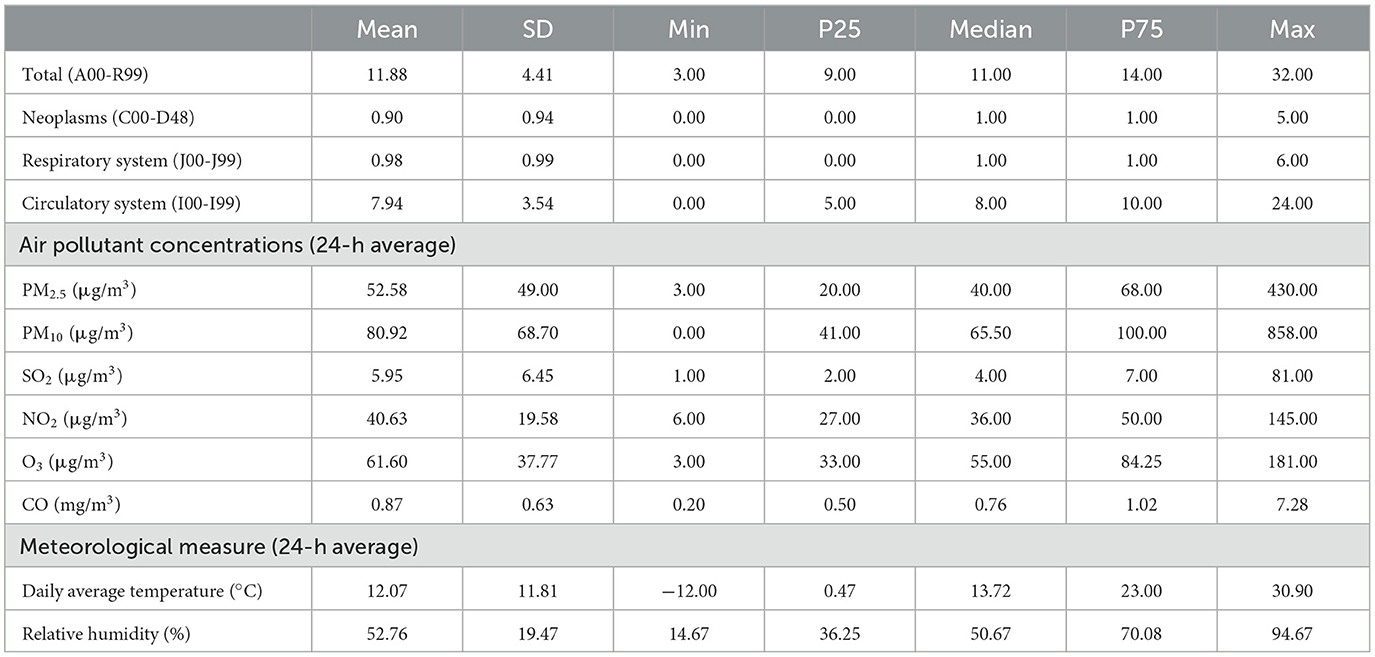
The total number of non-accidental deaths was 8,676 during 2017–2018, of which 58.37% were males, 77.11% were older than 65 years of age, and 66.83% died from circulatory diseases (Supplementary Table 1). As shown in Table 1, the 24-h average concentrations were 52.58 μg/m3 for PM2.5, 80.92 μg/m3 for PM10, 5.95 μg/m3 for SO2, 40.63 μg/m3 for NO2, 0.87 mg/m3 for CO, and 61.60 μg/m3 for O3.
The Spearman correlation analysis results showed there were strong correlations among the air pollutants (Supplementary Table 2). It is worth noting that PM2.5 was highly correlated with CO (r = 0.85), and PM10 (r = 0.78). O3 was negatively correlated with SO2, NO2, and CO, respectively (P < 0.01). The overall trend in non-accidental deaths from emergency department visits was U-shaped, and higher in winter (Figure 1). SO2, NO2, and O3 showed seasonal fluctuations over time with a stable overall trend.
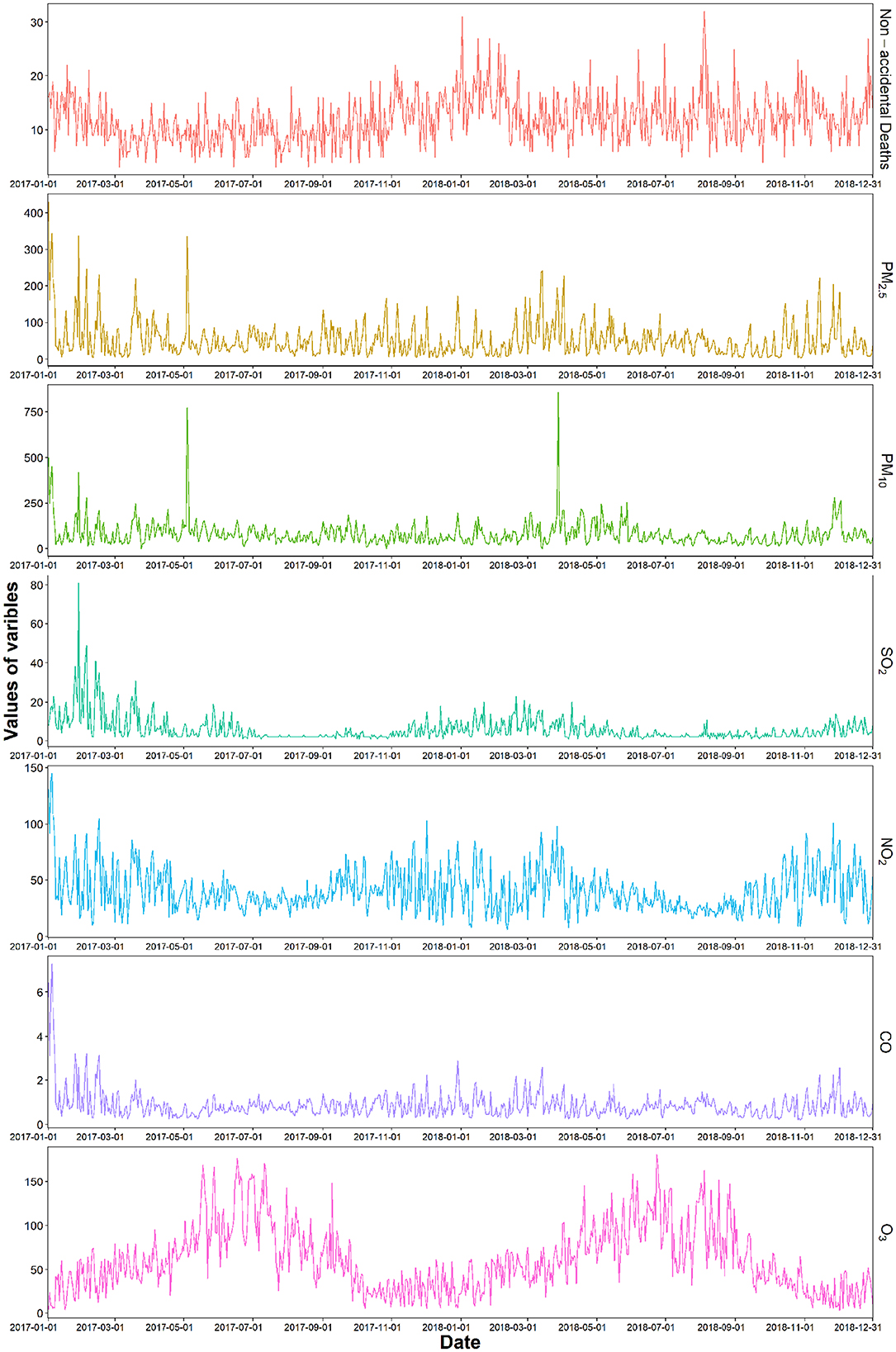
Figure 1. Time series of air pollutants and non-accidental mortality in emergency department visits from 2017 to 2018.
The estimated RRs with 95% CIs for non-accidental mortality in single-pollutant models linked to a unit increment of air pollutant concentrations are shown in Table 2. After adjusting for time-trended, daily average temperature, relative humidity, and day of week, there were significant positive relationships between air pollution and non-accidental mortality. Significant associations between exposure to air pollutants (PM2.5, SO2, NO2, and CO) and non-accidental mortality for emergency department visits could be observed at lag 3 days (lag 4 and lag 5 for O3) in single-day lagged models. In contrast to single-day lags, larger effect estimates were observed in multi-day lags. The strongest effects observed for a unit increase in short-term exposure were 1.008 (95% CI: 1.001, 1.016) for PM2.5 at lag 04, 1.007 (95% CI: 1.001, 1.013) for PM10 at lag 05, 1.054 (95% CI: 1.009, 1.100) for SO2 at lag 04, 1.038 (95% CI: 1.013, 1.063) for NO2 at lag 04, 1.032 (95% CI: 1.011, 1.054) for O3 at lag 05, 1.034 (95% CI: 1.004, 1.066) for CO at lag 04.
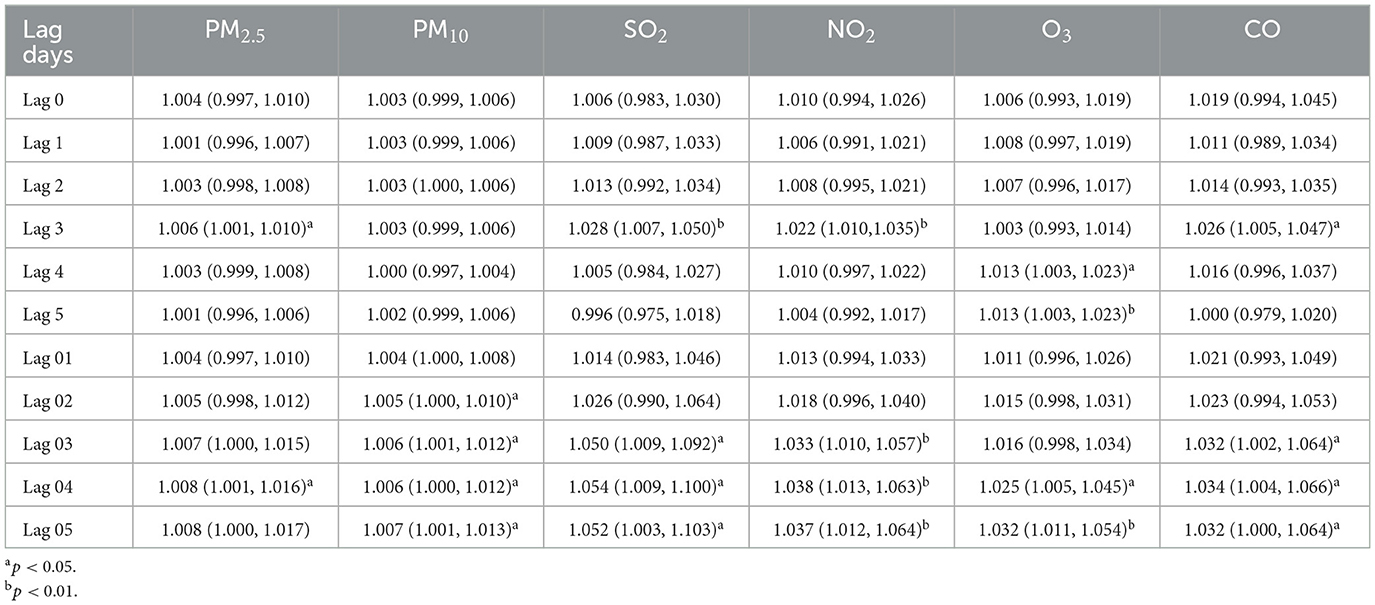
Table 2. The estimated RRs with 95% CIs of non-accidental mortality in emergency department visits per 10 μg/m3 increase in air pollutants (5 μg/m3 in SO2, 0.5 mg/m3 in CO) in single-pollutant models at different lag days.
Figure 2 shows the relationship between air pollution and cause-specific mortality in different lag models. We found that these pollutants (PM2.5 and CO) only have significant positive associations with neoplasms disease mortality at lag 3, the RRs were 1.021 (95% CI: 1.005, 1.038) for PM2.5 and 1.080 (95% CI: 1.003, 1.163) for CO. Meanwhile, SO2 (lag 3, lag 03, and lag 04) and O3 (lag 2, lag 02, lag 04, and lag 05) were only associated with circulatory disease mortality, the RRs were 1.057 (95% CI: 1.002, 1.114) for SO2 (lag 04) and 1.034 (95% CI: 1.009, 1.061) for O3 (lag 05). Short-term exposure to NO2 had the significant impact on circulatory disease mortality in cumulative lag models and the RR was 1.044 (95% CI: 1.014, 1.075) in lag 04. The detailed results were shown in Supplementary Table 3.
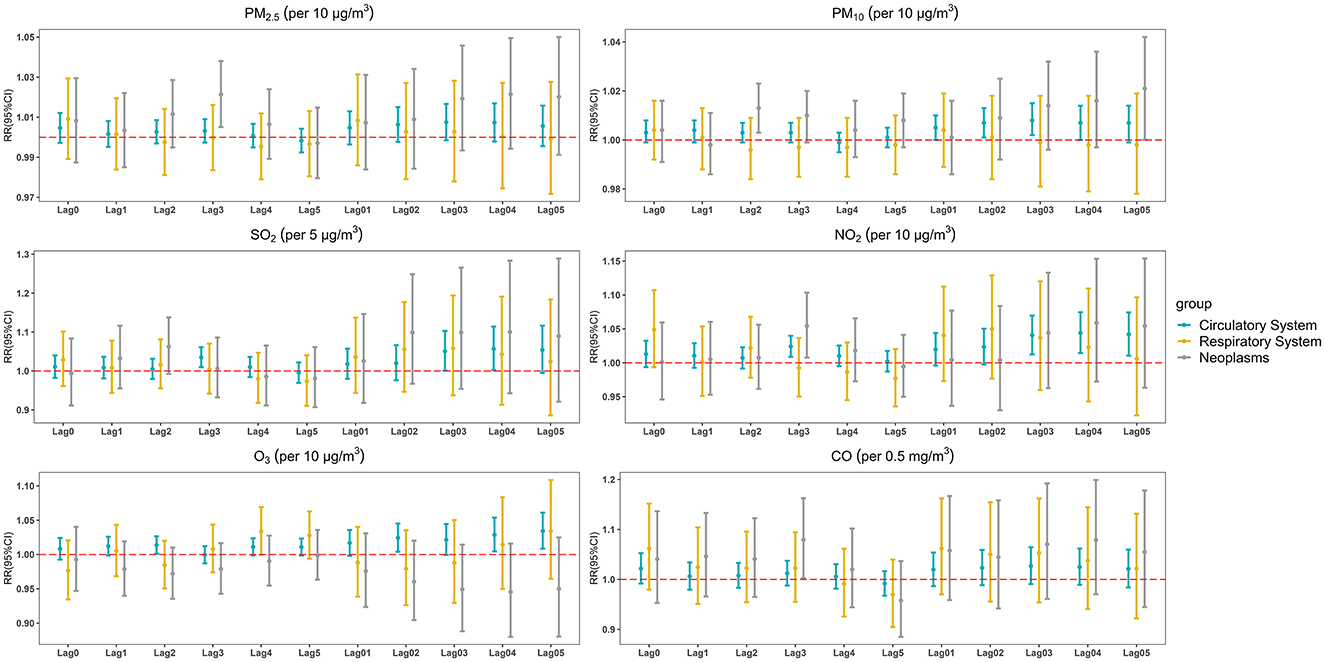
Figure 2. The estimated RRs with 95% CIs of cause-specific mortality associated with a 10 μg/m3 increase in air pollutant concentrations (5 μg/m3 in SO2, 0.5 mg/m3 in CO) at different lag days.
The results of the sex-specific analyses in different lag models are shown in Figure 3. Short-term exposure to CO and NO2 had the significant impact on males, and the RR values were 1.052 (95% CI: 1.020, 1.086) for NO2 at lag 04 and 1.067 (95% CI: 1.026, 1.110) for CO at lag 04 (the sex modification was statistically significant for CO). Meanwhile, the correlation between O3 and daily non-accidental deaths in emergency department visits was significantly positive in females, and the RR was 1.053 (95% CI: 1.019, 1.087) at lag 05 (the sex modification was statistically significant). The detailed results of stratified analyses by sex were in Supplementary Table 4.
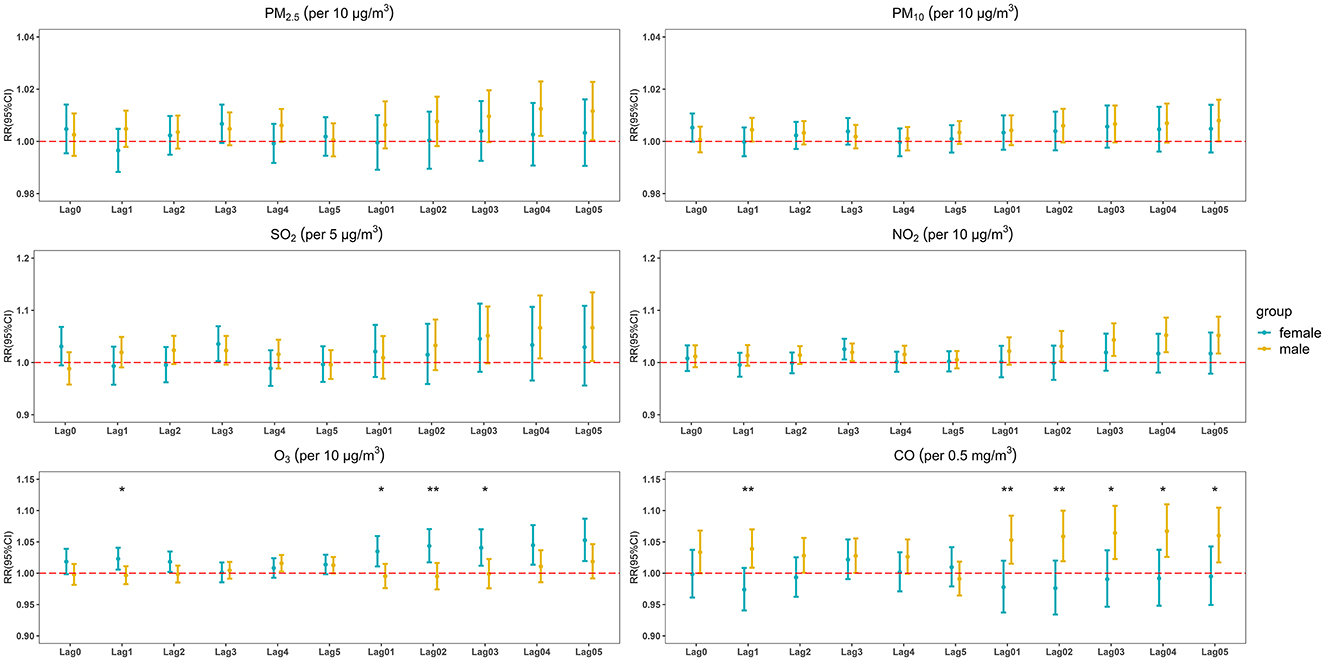
Figure 3. The estimated RRs with 95% CIs of daily non-accidental deaths in emergency department visits associated with a 10 μg/m3 increase in air pollutant concentrations (5 μg/m3 in SO2, 0.5 mg/m3 in CO) in sex-stratified analysis at different lag days (statistically significant for between-group difference *p < 0.05; **p < 0.01).
The outcomes of the stratified analysis by age in different lag models are shown in Figure 4. Short-term exposure to the four air pollutants (PM10, SO2, NO2, and O3) had significant effects on people aged 65 years and older (the age modification was not statistically significant). The strongest effects observed in response to a unit increase in exposure were 1.008 (95% CI: 1.002, 1.014) for PM10 at lag 03, 1.062 (95% CI: 1.007, 1.121) for SO2 at lag 05, 1.040 (95% CI: 1.012, 1.068) for NO2 at lag 04, 1.030 (95% CI: 1.006, 1.054) for O3 at lag 05. Detailed outcomes of the age-specific stratified analysis are shown in Supplementary Table 5.

Figure 4. The estimated RRs with 95% CIs of non-accidental mortality in emergency department visits associated with a 10 μg/m3 increase in air pollutant concentrations (5 μg/m3 in SO2, 0.5 mg/m3 in CO) in age-stratified analysis at different lag days (statistically significant for between-group difference *p < 0.05).
In sensitivity analysis, our findings were robust by adjusting the dfs to control for long-time trends (10–14 df per year), temperature (2–7 df), and relative humidity (2–7 df ; Supplementary Tables 6–8). After controlling for other pollutants, the short-term effects of air pollutants on non-accidental mortality in co-pollutant models are shown in Table 3 and Supplementary Table 9. The lag periods used in models were determined based on the maximum lag effect between non-accidental mortality and air pollution in single-pollutant models (lag 05 for PM10 and O3, lag 04 for other air pollutants). After adjusting for other pollutants in two-pollutant models, the positive associations between air pollutants and daily non-accidental deaths from emergency department visits remained significant, which demonstrated the relative robustness of the estimated effects. After adjusting for temperature of longer lag days (up to 28 days), the effect estimates changed slightly (Supplementary Table 10).
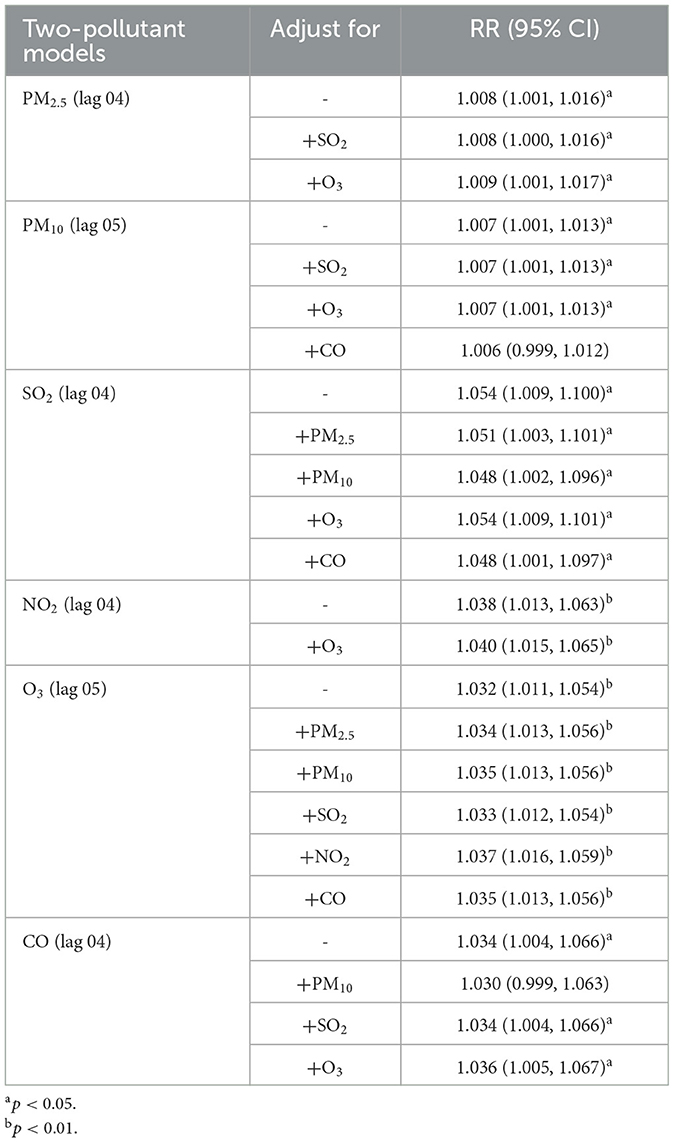
Table 3. The estimated RRs with 95% CIs for daily non-accidental deaths in emergency department visits associated with a 10 μg/m3 increment in air pollutant concentrations (5 μg/m3 in SO2, 0.5 mg/m3 in CO) in two-pollutant models.
Figure 5 shows the E-R association between air pollutant levels (lag 05 for PM10 and O3, lag 04 for other air pollutants) and non-accidental mortality in emergency department visits. An approximate linear effect of NO2 was found for non-accidental mortality. Non-accidental morbidity monotonously increased with the concentrations of NO2. Meanwhile, the E-R curve for O3 was U-shaped and it showed potential risk within the concentration of < 30 or > 75 μg/m3.

Figure 5. The exposure-response (E-R) curves for the association between six air pollutants and non-accidental mortality.
4. Discussion
So far as we know, there are few studies examining the short-term effects of gaseous pollutants and particulate matter on non-accidental mortality based on data from emergency department visits in Beijing. Our data were obtained through the biggest emergency center in Beijing, which could more reasonably and accurately reflect the acute health effects from ambient pollution (26). Short-term exposure to air pollutants, especially gaseous pollutants, was demonstrated to have a positive relationship with non-accidental mortality. Meanwhile, short-term exposure to NO2, SO2, and O3 increased the risk of circulatory mortality. Additionally, stronger associations were presented in females for O3 while in males for CO. People aged 65 and over are strongly associated with ambient air pollution.
Gaseous pollutants had greater effects on non-accidental mortality than particulate matter in this study. In previous studies, such results were also found (31, 36). This may be related to a variety of factors including residents' awareness of self-protection, exposure levels, biological mechanisms, and population susceptibility. Gaseous pollutants are more likely to cause acute diseases, such as acute myocardial infarction, acute respiratory infections, and ischemic heart disease (37–39). Some studies have demonstrated that long-term exposure (e.g., several years) to particulate matter increases the risk of mortality to an even larger extent than exposure over a few days (40, 41). It has been shown that long-term exposure to PM2.5 is related to accelerated coronary artery calcification or increased the risk to plaque rupture (42). One study concluded that people had less awareness of protection against ozone when compared to particulate matter (43). The E-R associations of gaseous pollutant concentrations with non-accidental mortality were positive. It was interesting to note that the E-R curve for O3 was U-shaped, which showed a potential risk in the concentration range of < 30 or >75 μg/m3. Similar results were found in a study conducted in Delhi, India (44). This could be related to seasonal fluctuations in O3, with higher concentrations in summer. Synergy effects between temperature and O3 for non-accidental mortality are also biologically plausible (45, 46). The State Council of China issued the APCAP in 2013, but the annual average concentrations of NO2 and O3 in China have not changed significantly (47). This study indicates that emission control efforts for gaseous pollutants and people's awareness of protection should be strengthened in the future.
The relationship between short-term exposure to ambient gaseous pollution and non-accidental deaths has been extensively explored in developed countries. Similar to our research results, several previous meta-analyses based on North America and Europe investigated the relationship between ambient ozone and non-accidental mortality which demonstrated a statistically significant risk effect for non-accidental mortality (48, 49). There was a high positive association between most air pollutants (PM2.5, SO2, NO2, and CO) and daily mortality from diabetes in a study conducted in Montreal, Quebec, Canada (50). Similar outcomes related to non-accidental mortality have been discussed in China. A study conducted in Hefei, an inland city in China, showed that per 10 μg/m3 increment in SO2 (lag 03) and NO2 (lag 01) were significantly associated with 4.93% (95% CI: 1.94, 8.00), 2.11% (95% CI: 1.18, 3.05) increase of daily non-accidental deaths (15). Similar to our findings, a study exploring the acute effects of SO2 and NO2 on mortality found non-accidental mortality in Beijing raised 0.60% (95% CI: 0.26, 0.95) for every 10 μg/m3 increase in daily NO2 concentration (20). Meanwhile, a meta-analysis of the acute effects of ambient ozone on mortality in Chinese cities showed that the percent change for non-accidental mortality was 0.42% (95% CI: 0.32, 0.52) with an increase of 10 μg/m3 in the maximum 8-h average concentration of O3 (51). Variations in effect estimates are caused by many factors, including variation across the populations, various analysis strategy, and issues related to data quality and measurement error (50).
For cause-specific mortality, there was a significant association between short-term exposure to NO2, SO2 and O3 on circulatory disease mortality. The relationships of increased NO2, SO2, and O3 with increased cardiovascular mortality were also observed in exist evidence (51–54). The biological mechanisms contributing to the link of NO2, SO2, and O3 to circulatory disease mortality pathologies may involve complex processes. Increase in oxidant stress appears to be a broadly applicable mechanism, regardless of the type of pollutants that contributes to the adverse effects of air pollution. NO2, SO2, and O3 induce oxidative stress, thereby triggering inflammatory responses and gene activation, potentially leading to endothelial dysfunction, atherothrombotic alterations, metabolic dysregulation, and the development of cardiometabolic diseases (55–58). Researches have shown that O3 can lead to an imbalance in heart rate variability and an increased sensitivity to myocardial calcium load, which can trigger vascular and cardiac injury, ultimately manifesting as cardiovascular disease (59, 60). SO2 can reduce the permeability of red blood cells and lead to organ shortages, while short-term exposure to it can lead to a decreased in cardiac vagal control measures (61). NO2 is considered a proxy for traffic-related pollutants and is often found in conjunction with traffic noise, which is also associated with adverse cardiovascular health outcomes (62).
In stratified analysis, the effect estimates for CO were consistently higher in males, while the effect estimates for O3 were consistently higher in females. The sex modification was statistically significant for CO and O3. Several studies showed that males were more sensitive to air pollutants (32, 43, 63). The smoking rate for males is significantly higher than for females in China. Even after quitting smoking, impaired lung function may not recover to normal quickly, and may have synergistic effects with air pollution (64). Meanwhile, some studies have suggested that the increased susceptibility of females to the adverse effects of O3, which could be related to differential regulation of the lung immune response (65). The reasons for gender vulnerability to air pollution were not clear and need further investigation. In the stratified analyses by age, the association between short-term exposure to air pollutants and non-accidental deaths seemed to be evident in older people. Several foreign studies have also reported increased susceptibility in older people (66, 67). Studies confirm that certain physiological regulatory functions diminish with age, which may lead to an increased health risk associated with those older than 65 years (68). Some studies have indicated that current air quality guidelines are designed to protect the general population but not enough to protect older people (69). Therefore, we call for more studies to investigate the susceptibility of older people to air pollutant concentrations in different countries or different regions with the aim of determining whether this finding can be generalized across different climatic and air pollution characteristics.
Several limitations exist within this study that should be considered. First, we use data on air pollution from the average of fixed-site air quality–monitoring stations to represent exposure at the individual level, which can lead to exposure misclassification. Secondly, this study fails to control for social and demographic factors (e.g., education level and socioeconomic status) which could influence the demographic composition and mortality (70, 71). Thirdly, this is an ecological research limiting causal inference. This needs to be addressed by further toxicological or epidemiological studies. Finally, it was a single-center study with limited study time. Therefore, we encourage further large-scale studies, especially in developing countries.
5. Conclusion
Our findings demonstrated that short-term exposure to ambient pollutants, especially gaseous pollutants, increased the risk of non-accidental mortality in emergency department visits to Beijing. Additionally, stronger associations were presented in females for O3 while in males for CO. People aged 65 and over are strongly associated with ambient air pollution. The study provides health authorities with critical information on the acute adverse effects of air pollution, which will contribute to the development of protective measures in China.
Data availability statement
The data that support the findings of this study are available from the corresponding authors, upon reasonable request.
Author contributions
SW and YZ: conceptualization, formal analysis, and writing—original draft preparation. XL: software and writing—review and editing. JZ: methodology. NZ: validation and visualization. YG: validation. JC, YLi, and YLy: data curation. ZC: writing—original draft preparation. CL: project administration. JG: software and funding acquisition. WZ: methodology and resources. JM: investigation, resources, and supervision. All authors contributed to the article and approved the submitted version.
Funding
This work was supported by the Key Project of Scientific and Technological Support Plan of Tianjin in 2020 (No. 20YFZCSY00820).
Conflict of interest
XL was employed by Clinical Pharmacology Department, Zhejiang Hisun Pharmaceutical Co., Ltd.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2023.1208514/full#supplementary-material
Abbreviations
GAM, Generalized additive model; E-R, Exposure-response; RR, Relative risk; CI, Confidence interval; AIC, Akaike information criterion.
References
1. Chen Z, Wang JN, Ma GX, Zhang YS. China tackles the health effects of air pollution. Lancet. (2013) 382:1959–60. doi: 10.1016/S0140-6736(13)62064-4
2. Cai J, Peng C, Yu S, Pei Y, Liu N, Wu Y, et al. Association between PM(2.5) exposure and all-cause, non-accidental, accidental, different respiratory diseases, sex and age mortality in Shenzhen, China. Int J Environ Res Public Health. (2019) 16:30401. doi: 10.3390/ijerph16030401
3. Collaborators GBDRF. Global burden of 87 risk factors in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. (2020) 396:1223–49. doi: 10.1016/S0140-6736(20)30752-2
4. Zhou M, Wang H, Zeng X, Yin P, Zhu J, Chen W, et al. Mortality, morbidity, and risk factors in China and its provinces, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. (2019) 394:1145–58. doi: 10.1016/S0140-6736(19)30427-1
5. Yang G, Wang Y, Zeng Y, Gao GF, Liang X, Zhou M, et al. Rapid health transition in China, 1990-2010: findings from the Global Burden of Disease Study 2010. Lancet. (2013) 381:1987–2015. doi: 10.1016/S0140-6736(13)61097-1
6. Yang BY, Liu Y, Hu LW, Zeng XW, Dong GH. Urgency to assess the health impact of ambient air pollution in China. Adv Exp Med Biol. (2017) 1017:1–6. doi: 10.1007/978-981-10-5657-4_1
7. Yang D, Yang X, Deng F, Guo X. Ambient air pollution and biomarkers of health effect. Adv Exp Med Biol. (2017) 1017:59–102. doi: 10.1007/978-981-10-5657-4_4
8. Maji KJ, Li VO, Lam JC. Effects of China's current Air Pollution Prevention and Control Action Plan on air pollution patterns, health risks and mortalities in Beijing 2014-2018. Chemosphere. (2020) 260:127572. doi: 10.1016/j.chemosphere.2020.127572
9. Liang L, Cai Y, Lyu B, Zhang D, Chu S, Jing H, et al. Air pollution and hospitalization of patients with idiopathic pulmonary fibrosis in Beijing: a time-series study. Respir Res. (2022) 23:81. doi: 10.1186/s12931-022-01998-8
10. Lin H, Wang X, Liu T, Li X, Xiao J, Zeng W, et al. Air pollution and mortality in China. Adv Exp Med Biol. (2017) 1017:103–21. doi: 10.1007/978-981-10-5657-4_5
11. Yin P, Chen R, Wang L, Meng X, Liu C, Niu Y, et al. Ambient ozone pollution and daily mortality: a nationwide study in 272 Chinese cities. Environ Health Perspect. (2017) 125:117006. doi: 10.1289/EHP1849
12. Ren L, Yang W, Bai Z. Characteristics of major air pollutants in China. Adv Exp Med Biol. (2017) 1017:7–26. doi: 10.1007/978-981-10-5657-4_2
13. Guo X, Su W, Wang H, Li N, Song Q, Liang Q, et al. Short-term exposure to ambient ozone and cardiovascular mortality in China: a systematic review and meta-analysis. Int J Environ Health Res. (2022) 2022:1–18. doi: 10.1080/09603123.2022.2066070
14. Chen R, Yin P, Meng X, Wang L, Liu C, Niu Y, et al. Associations between coarse particulate matter air pollution and cause-specific mortality: a nationwide analysis in 272 Chinese cities. Environ Health Perspect. (2019) 127:17008. doi: 10.1289/EHP2711
15. Deng J, Hu X, Xiao C, Pan F. The association between gaseous pollutants and non-accidental mortality: a time series study. Environ Geochem Health. (2021) 43:2887–97. doi: 10.1007/s10653-020-00800-2
16. Lu X, Yao T, Fung JCH, Lin C. Estimation of health and economic costs of air pollution over the Pearl River Delta region in China. Sci Total Environ. (2016) 566–7:134–43. doi: 10.1016/j.scitotenv.2016.05.060
17. Chen X, Zhang LW, Huang JJ, Song FJ, Zhang LP, Qian ZM, et al. Long-term exposure to urban air pollution and lung cancer mortality: a 12-year cohort study in Northern China. Sci Total Environ. (2016) 571:855–61. doi: 10.1016/j.scitotenv.2016.07.064
18. Wong TW, Tam WS, Yu TS, Wong AH. Associations between daily mortalities from respiratory and cardiovascular diseases and air pollution in Hong Kong, China. Occup Environ Med. (2002) 59:30–5. doi: 10.1136/oem.59.1.30
19. Yang CY, Chang CC, Chuang HY, Tsai SS, Wu TN, Ho CK. Relationship between air pollution and daily mortality in a subtropical city: Taipei, Taiwan. Environ Int. (2004) 30:519–23. doi: 10.1016/j.envint.2003.10.006
20. Zeng Q, Li G, Zhang L, Tian L, Pan X. Acute effects of SO2 and NO2 on mortality in the six cities of China. Zhonghua Yu Fang Yi Xue Za Zhi. (2015) 49:1085–91. doi: 10.3760/cma.j.issn.0253-9624.2015.12.013
21. Shang Y, Sun Z, Cao J, Wang X, Zhong L, Bi X, et al. Systematic review of Chinese studies of short-term exposure to air pollution and daily mortality. Environ Int. (2013) 54:100–11. doi: 10.1016/j.envint.2013.01.010
22. Li W, Pei L, Li A, Luo K, Cao Y, Li R, et al. Spatial variation in the effects of air pollution on cardiovascular mortality in Beijing, China. Environ Sci Pollut Res Int. (2019) 26:2501–11. doi: 10.1007/s11356-018-3725-0
23. Khorsandi B, Farzad K, Tahriri H, Maknoon R. Association between short-term exposure to air pollution and COVID-19 hospital admission/mortality during warm seasons. Environ Monit Assess. (2021) 193:426. doi: 10.1007/s10661-021-09210-y
24. Bravo MA, Son J, de Freitas CU, Gouveia N, Bell ML. Air pollution and mortality in Sao Paulo, Brazil: effects of multiple pollutants and analysis of susceptible populations. J Expo Sci Environ Epidemiol. (2016) 26:150–61. doi: 10.1038/jes.2014.90
25. Garcia TC, Bernstein AB, Bush MA. Emergency department visitors and visits: who used the emergency room in 2007? NCHS Data Brief. (2010) 2010:1–8. doi: 10.1037/e665452010-001
26. Basu R, Pearson D, Malig B, Broadwin R, Green R. The effect of high ambient temperature on emergency room visits. Epidemiology. (2012) 23:813–20. doi: 10.1097/EDE.0b013e31826b7f97
27. Fu Y, Zhang W, Li Y, Li H, Deng F, Ma Q. Association and interaction of O(3) and NO(2) with emergency room visits for respiratory diseases in Beijing, China: a time-series study. BMC Public Health. (2022) 22:2265. doi: 10.1186/s12889-022-14473-2
28. Wang K, Tian H, Hua S, Zhu C, Gao J, Xue Y, et al. A comprehensive emission inventory of multiple air pollutants from iron and steel industry in China: temporal trends and spatial variation characteristics. Sci Total Environ. (2016) 559:7–14. doi: 10.1016/j.scitotenv.2016.03.125
29. Chen R, Yin P, Wang L, Liu C, Niu Y, Wang W, et al. Association between ambient temperature and mortality risk and burden: time series study in 272 main Chinese cities. Br Med J. (2018) 363:k4306. doi: 10.1136/bmj.k4306
30. Yang C, Chen A, Chen R, Qi Y, Ye J, Li S, et al. Acute effect of ambient air pollution on heart failure in Guangzhou, China. Int J Cardiol. (2014) 177:436–41. doi: 10.1016/j.ijcard.2014.09.003
31. Li D, Ji A, Lin Z, Liu J, Tan C, Huang X, et al. Short-term ambient air pollution exposure and adult primary insomnia outpatient visits in Chongqing, China: a time-series analysis. Environ Res. (2022) 212:113188. doi: 10.1016/j.envres.2022.113188
32. Ma C, Jung CR, Nakayama SF, Tabuchi T, Nishihama Y, Kudo H, et al. Short-term association of air pollution with lung cancer mortality in Osaka, Japan. Environ Res. (2023) 224:115503. doi: 10.1016/j.envres.2023.115503
33. Wang Z, Peng J, Liu P, Duan Y, Huang S, Wen Y, et al. Association between short-term exposure to air pollution and ischemic stroke onset: a time-stratified case-crossover analysis using a distributed lag nonlinear model in Shenzhen, China. Environ Health. (2020) 19:1. doi: 10.1186/s12940-019-0557-4
34. Ma W, Wang L, Lin H, Liu T, Zhang Y, Rutherford S, et al. The temperature-mortality relationship in China: an analysis from 66 Chinese communities. Environ Res. (2015) 137:72–7. doi: 10.1016/j.envres.2014.11.016
35. Wang L, Zhang F, Pilot E, Yu J, Nie C, Holdaway J, et al. Taking action on air pollution control in the Beijing-Tianjin-Hebei (BTH) region: progress, challenges and opportunities. Int J Environ Res Public Health. (2018) 2018:15. doi: 10.3390/ijerph15020306
36. Qu Y, Pan Y, Niu H, He Y, Li M, Li L, et al. Short-term effects of fine particulate matter on non-accidental and circulatory diseases mortality: a time series study among the elder in Changchun. PLoS ONE. (2018) 13:e0209793. doi: 10.1371/journal.pone.0209793
37. Lin H, An Q, Luo C, Pun VC, Chan CS, Tian L. Gaseous air pollution and acute myocardial infarction mortality in Hong Kong: a time-stratified case-crossover study. Atmos Environ. (2013) 76:68–73. doi: 10.1016/j.atmosenv.2012.08.043
38. Zhang C, Ding R, Xiao C, Xu Y, Cheng H, Zhu F, et al. Association between air pollution and cardiovascular mortality in Hefei, China: a time-series analysis. Environ Pollut. (2017) 229:790–7. doi: 10.1016/j.envpol.2017.06.022
39. Xu H, Wang X, Tian Y, Tian J, Zeng Y, Guo Y, et al. Short-term exposure to gaseous air pollutants and daily hospitalizations for acute upper and lower respiratory infections among children from 25 cities in China. Environ Res. (2022) 212:113493. doi: 10.1016/j.envres.2022.113493
40. Brook RD, Rajagopalan S, Pope CA 3rd, Brook JR, Bhatnagar A, Diez-Roux AV, et al. Particulate matter air pollution and cardiovascular disease: an update to the scientific statement from the American Heart Association. Circulation. (2010) 121:2331–78. doi: 10.1161/CIR.0b013e3181dbece1
41. Pope CA 3rd, Dockery DW. Health effects of fine particulate air pollution: lines that connect. J Air Waste Manag Assoc. (2006) 56:709–42. doi: 10.1080/10473289.2006.10464485
42. Liang F, Liu F, Huang K, Yang X, Li J, Xiao Q, et al. Long-term exposure to fine particulate matter and cardiovascular disease in China. J Am Coll Cardiol. (2020) 75:707–17. doi: 10.1016/j.jacc.2019.12.031
43. Wang N, Mengersen K, Tong S, Kimlin M, Zhou M, Wang L, et al. Short-term association between ambient air pollution and lung cancer mortality. Environ Res. (2019) 179:108748. doi: 10.1016/j.envres.2019.108748
44. Collart P, Dramaix M, Leveque A, Mercier G, Coppieters Y. Concentration-response curve and cumulative effects between ozone and daily mortality: an analysis in Wallonia, Belgium. Int J Environ Health Res. (2018) 28:147–58. doi: 10.1080/09603123.2018.1453050
45. Pascal M, Wagner V, Chatignoux E, Falq G, Corso M, Blanchard M, et al. Ozone and short-term mortality in nine French cities: influence of tem perature and season. Atmos Environ. (2012) 62:566–72. doi: 10.1016/j.atmosenv.2012.09.009
46. Basu R. High ambient temperature and mortality: a review of epidemiologic stud ies from 2001 to 2008. Environ Health. (2009) 8:40. doi: 10.1186/1476-069X-8-40
47. Huang J, Pan X, Guo X, Li G. Health impact of China's Air Pollution Prevention and Control Action Plan: an analysis of national air quality monitoring and mortality data. Lancet Planet Health. (2018) 2:e313–e23. doi: 10.1016/S2542-5196(18)30141-4
48. Bell ML, Dominici F, Samet JM. A meta-analysis of time-series studies of ozone and mortality with comparison to the national morbidity, mortality, and air pollution study. Epidemiology. (2005) 16:436–45. doi: 10.1097/01.ede.0000165817.40152.85
49. Levy JI, Chemerynski SM, Sarnat JA. Ozone exposure and mortality: an empiric bayes metaregression analysis. Epidemiology. (2005) 16:458–68. doi: 10.1097/01.ede.0000165820.08301.b3
50. Goldberg MS, Burnett RT, Yale JF, Valois MF, Brook JR. Associations between ambient air pollution and daily mortality among persons with diabetes and cardiovascular disease. Environ Res. (2006) 100:255–67. doi: 10.1016/j.envres.2005.04.007
51. Yan M, Liu Z, Liu X, Duan H, Li T. Meta-analysis of the Chinese studies of the association between ambient ozone and mortality. Chemosphere. (2013) 93:899–905. doi: 10.1016/j.chemosphere.2013.05.040
52. Abdolahnejad A, Jafari N, Mohammadi A, Miri M, Hajizadeh Y. Mortality and morbidity due to exposure to ambient NO(2), SO(2), and O(3) in Isfahan in 2013-2014. Int J Prev Med. (2018) 9:11. doi: 10.4103/ijpvm.IJPVM_387_16
53. Orellano P, Reynoso J, Quaranta N, Bardach A, Ciapponi A. Short-term exposure to particulate matter (PM(10) and PM(25)), nitrogen dioxide (NO(2)), and ozone (O(3)) and all-cause and cause-specific mortality: systematic review and meta-analysis. Environ Int. (2020) 142:105876. doi: 10.1016/j.envint.2020.105876
54. Dehbi HM, Blangiardo M, Gulliver J, Fecht D, de Hoogh K, Al-Kanaani Z, et al. Air pollution and cardiovascular mortality with over 25years follow-up: a combined analysis of two British cohorts. Environ Int. (2017) 99:275–81. doi: 10.1016/j.envint.2016.12.004
55. Munzel T, Sorensen M, Gori T, Schmidt FP, Rao X, Brook FR, et al. Environmental stressors and cardio-metabolic disease: part II-mechanistic insights. Eur Heart J. (2017) 38:557–64. doi: 10.1093/eurheartj/ehw294
56. Munzel T, Hahad O, Sorensen M, Lelieveld J, Duerr GD, Nieuwenhuijsen M, et al. Environmental risk factors and cardiovascular diseases: a comprehensive expert review. Cardiovasc Res. (2022) 118:2880–902. doi: 10.1093/cvr/cvab316
57. Routledge HC, Manney S, Harrison RM, Ayres JG, Townend JN. Effect of inhaled sulphur dioxide and carbon particles on heart rate variability and markers of inflammation and coagulation in human subjects. Heart. (2006) 92:220–7. doi: 10.1136/hrt.2004.051672
58. Krishna MT, Springall DR, Frew AJ, Polak JM, Holgate ST. Mediators of inflammation in response to air pollution: a focus on ozone and nitrogen dioxide. J R Coll Physicians Lond. (1996) 30:61–6.
59. Kodavanti UP, Thomas R, Ledbetter AD, Schladweiler MC, Shannahan JH, Wallenborn JG, et al. Vascular and cardiac impairments in rats inhaling ozone and diesel exhaust particles. Environ Health Perspect. (2011) 119:312–8. doi: 10.1289/ehp.1002386
60. Farraj AK, Walsh L, Haykal-Coates N, Malik F, McGee J, Winsett D, et al. Cardiac effects of seasonal ambient particulate matter and ozone co-exposure in rats. Part Fibre Toxicol. (2015) 12:12. doi: 10.1186/s12989-015-0087-3
61. Liu H, Zhai S, Kong Y, Wang Z, Song G, Song H, et al. Synergistic effects of gaseous pollutants on hospital admissions for cardiovascular disease in Liuzhou, China. Environ Sci Pollut Res Int. (2022) 29:9841–51. doi: 10.1007/s11356-021-16334-8
62. Yang BY, Guo Y, Markevych I, Qian ZM, Bloom MS, Heinrich J, et al. Association of long-term exposure to ambient air pollutants with risk factors for cardiovascular disease in China. J Am Med Assoc Netw Open. (2019) 2:e190318. doi: 10.1001/jamanetworkopen.2019.0318
63. Ma Y, Zhao Y, Yang S, Zhou J, Xin J, Wang S, et al. Short-term effects of ambient air pollution on emergency room admissions due to cardiovascular causes in Beijing, China. Environ Pollut. (2017) 230:974–80. doi: 10.1016/j.envpol.2017.06.104
64. Willemse BW, Postma DS, Timens W, ten Hacken NH. The impact of smoking cessation on respiratory symptoms, lung function, airway hyperresponsiveness and inflammation. Eur Respir J. (2004) 23:464–76. doi: 10.1183/09031936.04.00012704
65. Cabello N, Mishra V, Sinha U, DiAngelo SL, Chroneos ZC, Ekpa NA, et al. Sex differences in the expression of lung inflammatory mediators in response to ozone. Am J Physiol Lung Cell Mol Physiol. (2015) 309:L1150–63. doi: 10.1152/ajplung.00018.2015
66. Gouveia N, Fletcher T. Time series analysis of air pollution and mortality: effects by cause, age and socioeconomic status. J Epidemiol Community Health. (2000) 54:750–5. doi: 10.1136/jech.54.10.750
67. Spix C, Anderson HR, Schwartz J, Vigotti MA, LeTertre A, Vonk JM, et al. Short-term effects of air pollution on hospital admissions of respiratory diseases in Europe: a quantitative summary of APHEA study results. Air Pollut Health. (1998) 53:54–64. doi: 10.1080/00039899809605689
68. Xie J, Teng J, Fan Y, Xie R, Shen A. The short-term effects of air pollutants on hospitalizations for respiratory disease in Hefei, China. Int J Biometeorol. (2019) 63:315–26. doi: 10.1007/s00484-018-01665-y
69. Cakmak S, Dales RE, Vidal CB. Air pollution and mortality in Chile: susceptibility among the elderly. Environ Health Perspect. (2007) 115:524–7. doi: 10.1289/ehp.9567
70. Zhu G, Zhu Y, Wang Z, Meng W, Wang X, Feng J, et al. The association between ambient temperature and mortality of the coronavirus disease 2019 (COVID-19) in Wuhan, China: a time-series analysis. BMC Public Health. (2021) 21:117. doi: 10.1186/s12889-020-10131-7
Keywords: non-accidental mortality, air pollution, short-term exposure, gaseous pollutant, time-series study
Citation: Wang S, Zhang Y, Li X, Zhao J, Zhang N, Guo Y, Chen J, Liu Y, Cui Z, Lyu Y, Gao J, Li C, Zhang W and Ma J (2023) Effect of short-term exposure to ambient air pollutants on non-accidental mortality in emergency department visits: a time-series study. Front. Public Health 11:1208514. doi: 10.3389/fpubh.2023.1208514
Received: 19 April 2023; Accepted: 05 June 2023;
Published: 30 June 2023.
Edited by:
Tongjian Cai, Army Medical University, ChinaReviewed by:
Wanzhou Wang, Peking University, ChinaZilong Zhang, Sun Yat-sen University, China
Xinlei Deng, National Institute of Environmental Health Sciences (NIH), United States
Copyright © 2023 Wang, Zhang, Li, Zhao, Zhang, Guo, Chen, Liu, Cui, Lyu, Gao, Li, Zhang and Ma. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Wenyi Zhang, end5MDQxOUAxMjYuY29t; Jun Ma, anVubWFAdG11LmVkdS5jb20=
†These authors have contributed equally to this work
 Siting Wang
Siting Wang Yongming Zhang
Yongming Zhang Xia Li
Xia Li Jinhua Zhao
Jinhua Zhao Naijian Zhang
Naijian Zhang Yuming Guo
Yuming Guo Jiageng Chen
Jiageng Chen Yuanyuan Liu
Yuanyuan Liu Zhuang Cui
Zhuang Cui Yuanjun Lyu
Yuanjun Lyu Jing Gao
Jing Gao Changping Li
Changping Li Wenyi Zhang
Wenyi Zhang Jun Ma
Jun Ma