- 1Department of Epidemiology and Biostatistics, School of Public Health, Kwame Nkrumah University of Science and Technology, Kumasi, Ghana
- 2Information, Monitoring and Evaluation Department, Ghana Health Service, Ho Polyclinic, Ho, Ghana
- 3Department of Mathematics and Acturial Science, KNUST, Kumasi, Ghana
- 4Department of Health Policy, Management and Economics, School of Public Health, Kwame Nkrumah University of Science and Technology, Kumasi, Ghana
- 5Department of Geography, Miami University, Oxford, OH, United States
- 6Department of Geography, Environment and Earth Sciences, University of Hull, Hull, United Kingdom
- 7Department of Agribusiness and Applied Economics, North Dakota State University, Fargo, ND, United States
- 8Department of Geography and Rural Development, Kwame Nkrumah University of Science and Technology, Kumasi, Ghana
- 9College of Public Health, Medical and Veterinary Sciences, James Cook University, Townsville, QLD, Australia
- 10Center for Social Research in Health, UNSW Sydney, Sydney, NSW, Australia
- 11Social Policy Research Centre, UNSW, Sydney, NSW, Australia
- 12Centre for Primary Health Care and Equity, UNSW, Sydney, NSW, Australia
Background: Adolescent use of substances and injury experiences such as head injury have become increasingly prevalent. However, information regarding their association and the potential pathways linking them remains limited. This study examined the association between substance use and injuries, emphasizing the mediating role of interpersonal violence among adolescents.
Methods: We employed a multi-country analysis of Global School-based Health Surveys of 122,945 in-school adolescents aged 11–18 from 29 countries. This study was a cross-sectional school-based, nationally representative study developed by the World Health Organization and the United States Centers for Disease Control and Prevention, other United Nations allies, and country-specific institutions. Random-effects meta-analysis was performed to estimate the overall prevalence of injury and substance use and the I-square (
Results: Prevalence of substance use and injuries were 33.6% (95%CI = 28.5, 38.6%) and 41.7% (95%CI = 37.3, 46.1%), respectively. Substance use (37.8% vs. 29.4%, p = 0.001) and injuries (47.3% vs. 36.4%, p = 0.001) were significantly higher among male adolescents than females, respectively. After adjustment, substance users had 40% higher odds of injuries. The path analysis showed a mediation effect of perpetration of and victimization by interpersonal violence on the association of substance use with injuries, with total positive effects of perpetration [β = 0.18; 95%CI = 0.16, 0.19; p = 0.001] and victimization on injuries [β = 0.22; 95%CI = 0.21, 0.24; p = 0.001]. In a further subgroup analysis, tobacco users were 3.98 times more likely to sustain a gunshot wound whiles marijuana users had 2.81 times higher odds of sustaining gunshot wounds. Cigarette smokers had 45% lower odds of sustaining cut/stab wounds. Alcohol users were 53% more likely to sustain concussion/head injury and two and half times more likely to sustain gunshot wound.
Conclusion: A significant association exists between substance use and severe injuries among adolescents, mediated by interpersonal violence exposure. Our findings may have utility in informing substance use and interpersonal violence control policies and interventions to address adolescent injuries.
Introduction
Substance use remains one of the adolescents’ main risk-taking lifestyle behaviours, potentially impacting their mental and physical health and well-being (1). Among adolescents, tobacco products and alcohol remain the most prevalent substances (2). These substances are primarily used before initiating illicit drugs such as marijuana (2). Specifically, regarding alcohol, more than a quarter of young people aged 15–19 years are current drinkers, which is estimated to affect 155 million adolescents worldwide (1, 3–5). Recent studies among adolescents found that 4.1% smoked cigarettes, 2% used forms of tobacco other than combustible cigarettes (eg. Tobacco products), and 38% used marijuana, respectively (5, 6).
Substance use increases public health issues, such as serious injuries (7). The prevalence of substance use-related injuries among adolescents is 42.2% in four southeast Asian countries (8) and 45.3% in sub-Saharan Africa [SSA] (9). Studies suggest that substance using adolescents are more likely to experience severe injuries (10, 11). For instance, a review of studies on injury risk associated with cannabis and cocaine use concluded that most intentional and general injuries were associated with the use of cannabis and cocaine (10). Research has found that persons who abused a wide range of licit and illicit substances were likelier to experience multiple injuries (12). Moreover, a significant association between traumatic brain injury (TBI) and substance use among young, incarcerated people have been reported (13).
Substance use and injuries are serious public health issues. However, there is a lack of knowledge regarding the potential pathways explaining the link between substance use and severe injuries among adolescents. Violence and aggression could link substance use to severe injuries (11). Inferring from preliminary evidence, interpersonal violence is mainly motivated by substance use (14), which could mediate substance use and serious injuries. Therefore, this study sought to explore the mediating effect of perpetration of and victimization by interpersonal violence on substance use and serious injuries. We hypothesized that perpetration of and victimization by interpersonal violence mediates the association between substance use and serious injuries.
Methods
Data source
This study used publicly available data from the Global School-based Student Health Survey (GSHS) among 29 countries and territories. The GSHS is a large and representative survey of students’ health behaviours and risk factors using a standardized two-stage probability sampling approach for participant selection. The survey was developed by the World Health Organization (WHO) and the US Centers for Disease Control and Prevention (CDC), and other United Nations (UN) allies and country-specific institutions (1, 15). The survey draws content from the CDC Youth Risk Behaviours Survey (YRBS), for which test–retest reliability has been established (16). Information, including the aims, methodology, and sampling procedure of the GSHS, is available at http://www.cdc.gov/gshs/. This study used the most recent data available in GSHS-participating countries and territories. Countries and territories with their most recent data released before 2015 were excluded from the analysis. Also, countries with recent datasets missing information on the variables of interest for the present study were excluded. By applying the inclusion and exclusion criteria, data from adolescents aged 11–18 years in 29 countries and territories were considered recent and eligible to be included in the analysis (see Table 1).
Data collection procedure
Data collection was conducted during a regular class period with the help of trained enumerators from local social work organizations and other research institutions. The GSHS questionnaire was close-ended, structured and developed in English but translated into the local language in each country. The questionnaire included multiple-choice questions. After informed consent was obtained from the students, parents, and school officials, the questionnaires were administered. The trained enumerators explained the aim of the study and the instructions in detail to the students before the questionnaires were distributed. In addition, the survey ensured that students’ privacy was protected through anonymous and voluntary participation. The study complied with the Declaration of Helsinki, and each country’s Institutional review boards or ethics committees reviewed and approved all GSHS surveys.
Assessment of substance use
The respondent’s substance use was assessed with single items for tobacco, marijuana, cigarette, and alcohol use. The items included “During the past 30 days, how many days did you smoke cigarettes?” (0 days, 1 or 2 days, 3 to 5 days, 6 to 9 days, 10 to 19 days, 20 to 29 days and all 30 days), “During the past 30 days, on how many days did you use any tobacco products other than cigarettes, such as country specific examples?” (0 days, 1 or 2 days, 3 to 5 days, 6 to 9 days, 10 to 19 days, 20 to 29 days and, all 30 days), “During the past 30 days, how many times have you used marijuana?” (1 = 0 times, 2 = 1 or 2 times, 3 = 3–9 times, 4 = 10–19 times and 5 = 20 or more times), and “During the past 30 days, how many days did you have at least one drink containing alcohol?” (0 days, 1 or 2 days, 3 to 5 days, 6 to 9 days, 10 to 19 days, 20 to 29 days and all 30 days). All variables were re-coded on a dichotomous scale (Yes or No, where 0 times/days were considered as No and at least 1 day/time was considered Yes) as in other existing GSHS studies (17–19). We created a composite variable, “substance use,” by assigning a score of “1” each for “Yes” responses to smoking cigarettes, other tobacco, marijuana, and alcohol. A “0” score was assigned if the response was “No”. The score for each participant was added with a possible total score of 0–4. Participants who scored ≥1 were considered substance users.
Assessment of serious injuries
The primary outcome of this study was a self-reported serious injury. This variable was assessed in response to the question, “During the past 12 months, how many times were you seriously injured?” The GSHS questionnaire defined serious injury as an injury that makes the respondent miss at least one full day of usual activities such as school, sports, or a job or requires treatment by a doctor or nurse. Response options to the question were 1 = 0 times; 2 = 1 time; 3 = 2 or 3 times; 4 = 3 or 4 times; 4 = 4 or 5 times; 5 = 6 or 7 times; 6 = 8 0r 9 times; 7 = 10 or 11 times; 8 = 12 or more times. For analytic purposes, the options were further categorized into 1 = 0 [No] and 2 to 12 or more times = 1 [Yes] for this study. The students whose response option was “0 times” showed that they had not sustained any serious injury, while the remaining response options meant that they had sustained one or more injuries in the 12 months preceding the survey (9, 20, 21). We dichotomized the variable to simplify the analysis by analyzing group differences rather than individual differences (22).
Assessment of interpersonal violence
Perpetration of and victimization by interpersonal violence were the mediating variables in this study. Perpetration of interpersonal violence was measured as “During the past 12 months, how many times were you in a physical fight?” and victimization by interpersonal violence was assessed as “During the past 12 months, how many times were you physically attacked?” The two variables had the same response options including 1 = 0 times; 2 = 1 time; 3 = 2 or 3 times; 4 = 4 or 5 times; 5 = 6 or 7 times; 6 = 8 or 9 times; 7 = 10 or 11 times; and 8 = 12 or more times. For simplification and analytic purposes, the responses were further categorized into “No” for those who responded “0 times,” with the remaining responses as “Yes” in both variables Previous studies have used perpetration of and victimization by interpersonal violence to measure interpersonal violence (20, 23, 24).
Statistical analysis
The “svyset” command in Stata was used for the statistical analyses to adjust the complex sampling design employed by the GSHS survey using the weight, primary sampling unit (PSU), and stratum variables. Descriptive statistics were used to analyze and describe respondents’ characteristics stratified by substance use status. The chi-square test of independence was used to determine the association between substance use and background characteristics. Country-specific prevalence of substance use and injury was summarised using proportions and 95% confidence intervals. To calculate the overall prevalence of injury and substance use, we performed random-effects meta-analysis in stata. We investigated the between-country heterogeneity using the I-square ( statistic and the high heterogeneity ( >95%) was used to justify the random-effect modelling. Bivariate and multivariable logistic regression models were used to assess the influence of substance use on injuries, adjusting for other risk factors of injury. Odds ratios and 95% confidence intervals were reported. Variables with a value of p of 0.05 or less were considered statistically significant in the multivariable analysis. A path analysis using the structural equation model examined the potential mediation effect of perpetration of and victimization by interpersonal violence on the association between substance use and injury. Direct and indirect effects were tested, and the decomposition of total, direct, and indirect effects were specified (25). A sub-group analysis was also conducted to determine the associations between substance types and forms of injuries. This analysis employed a multinomial logistic regression analysis, with injury types as the outcome variable and substance types (tobacco, cigarette, marijuana, and alcohol) as the explanatory variables. Broken bone/dislocated joint was considered the base outcome, while concussion/head injury, gunshot wound, bad burn, and poison were the other outcomes used for the multinomial regression analysis. The data were analyzed from multiple countries jointly, and a country variable was included in the regression models to account for the joint analysis derived from multiple surveys.
Results
Background characteristics of the respondents by substance use
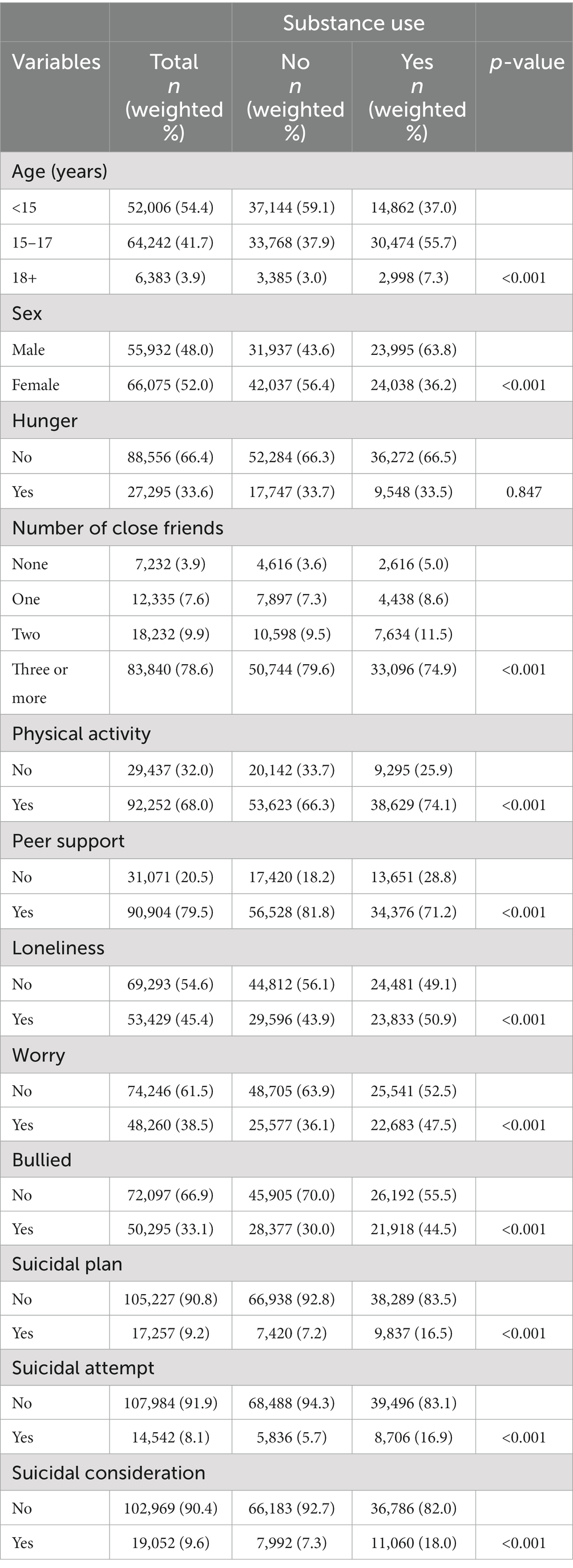
Table 2 shows the background characteristics of the respondents by substance use. In general, the majority of respondents were below the age of 15. Females constituted a higher proportion at 52.0%. The majority of the respondents (78.6%) reported having three or more close friends. A significant percentage, 68.0%, engaged in physical activity, while 79.5% received support from peers. Approximately 45.4% experienced feelings of loneliness. Around one-third of respondents reported being bullied, 9.2% had a suicidal plan, 8.1% had attempted suicide, and roughly 9.6% had contemplated suicide. Aside from hunger, all other background characteristics (age, sex, number of close friends, physical activity, peer support, loneliness, worry, bullying, suicidal plan, suicidal attempt, and suicidal consideration) were significantly associated with substance use.
Prevalence of substance use and injuries
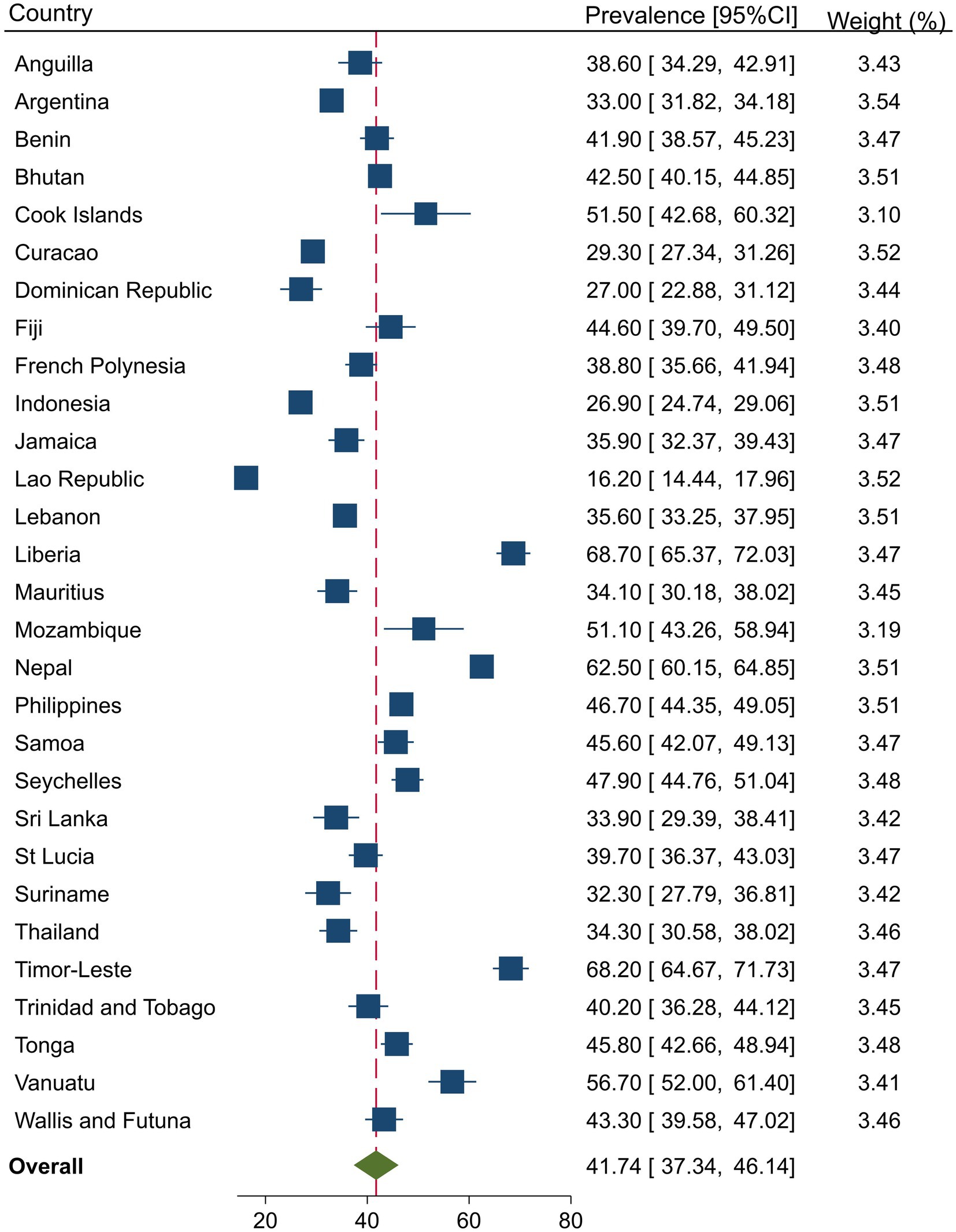
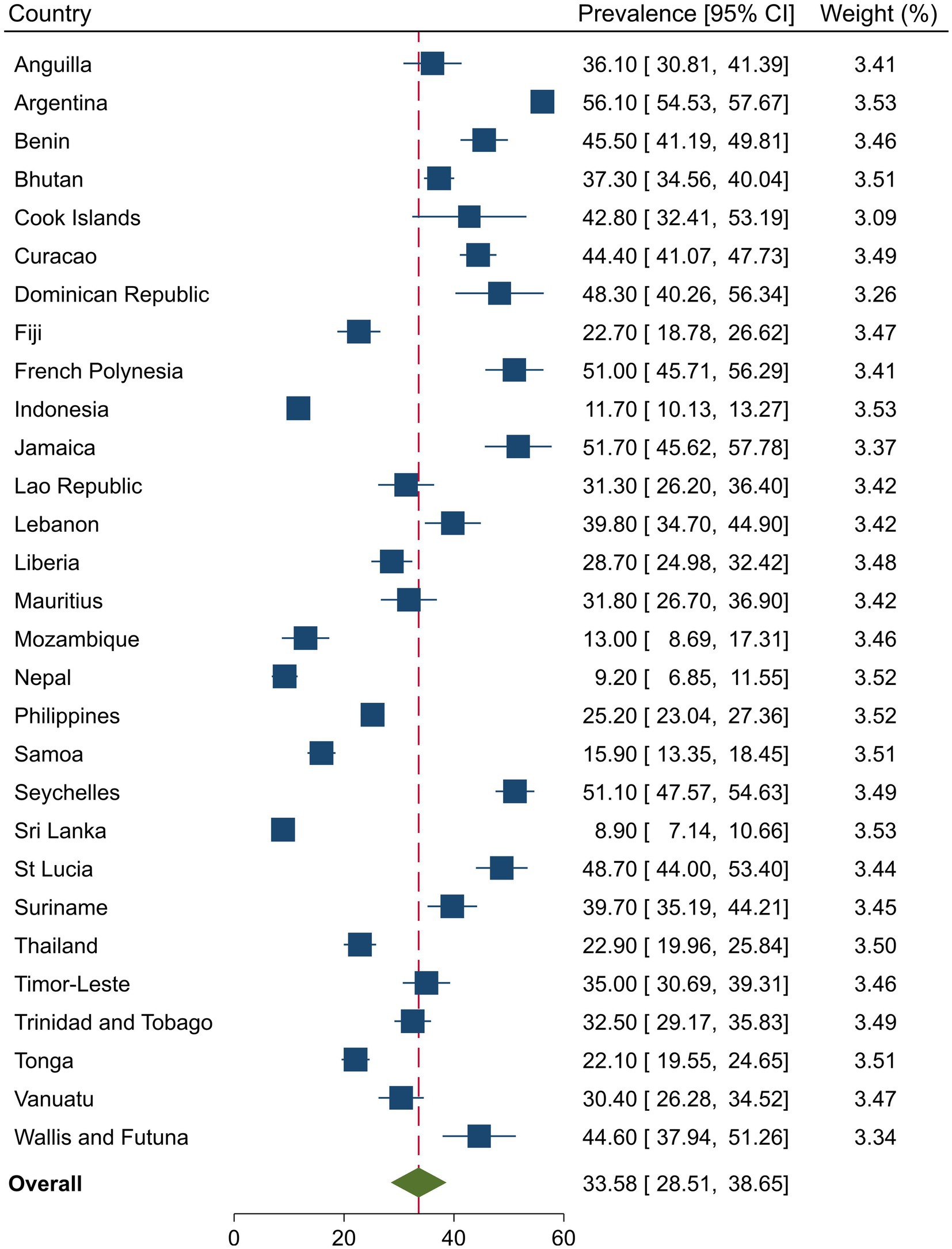
Figures 1, 2 present the country-specific prevalence of injuries and substance use, respectively. Overall, the injury prevalence was 41.7% (95%CI = 37.3, 46.1) among in-school adolescents and was significantly higher in males than females (47.3% vs. 36.4%, p = 0.001), respectively. The overall pooled prevalence of substance use was 33.6 (95%CI = 28.5, 38.6). Substance use was significantly higher among males than females (37.8% vs. 29.4%, p = 0.001), respectively.
Influence of substance use on injuries and other risk factors associated with injuries
Table 3 shows the influence of substance use on injuries among in-school adolescents. It also presents other risk factors associated with injuries. When unadjusted, the odds of injuries were 94% higher among in-school adolescents who used substances than their counterparts who did not use substances [OR = 1.94, 95%CI = 1.80, 2.09]. When the effect of substance use on injuries was adjusted for all other variables, the odds of injuries were 40% higher among in-school adolescents who used substances [AOR = 1.40, 95%CI = 1.31, 1.49].
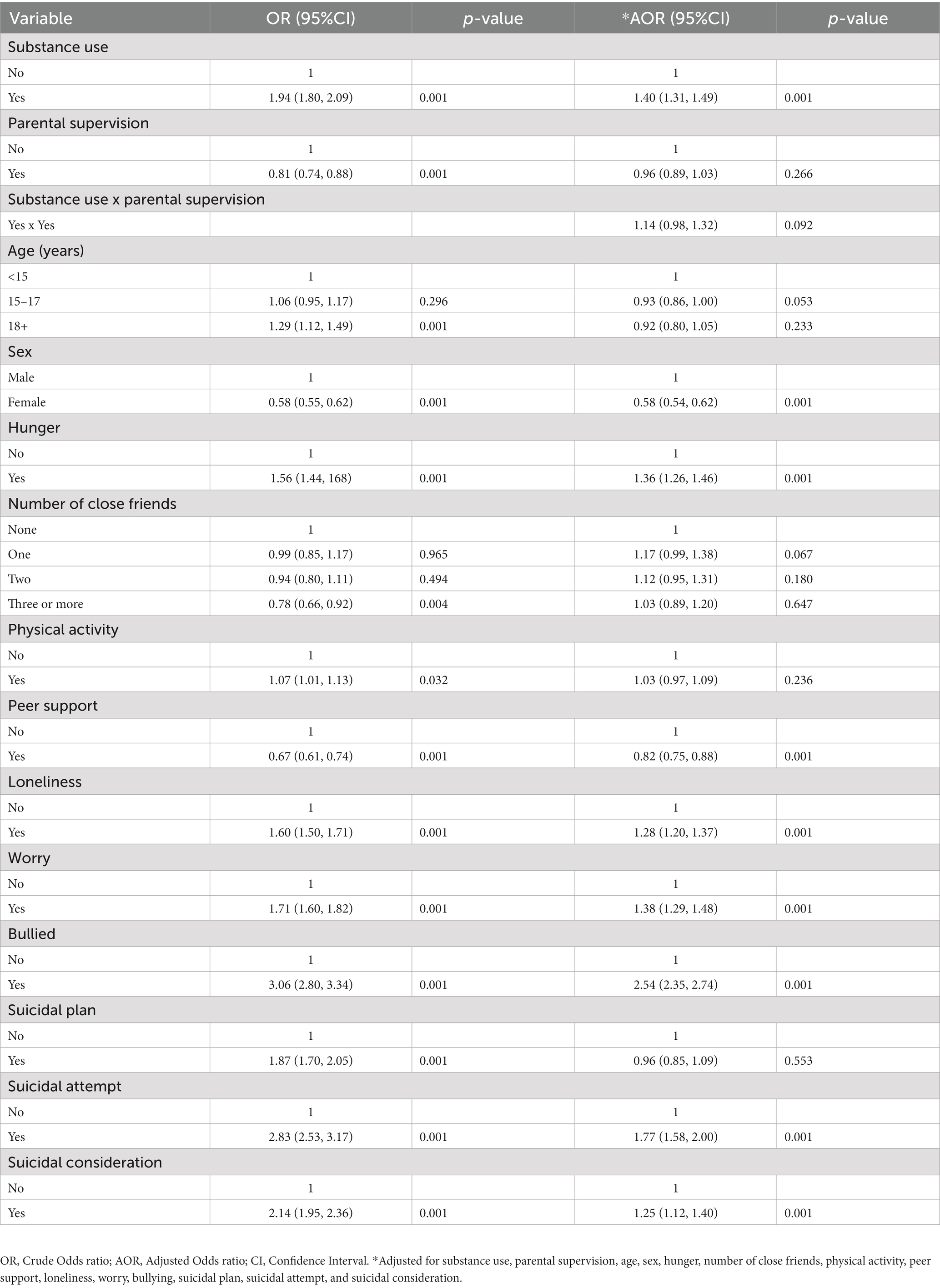
Table 3. Logistic regression analysis showing the association of substance use and risk factors with adolescents’ serious injuries.
Mediation effect of perpetration of and victimization by interpersonal violence on the association between substance use and injuries
Figure 3 presents a path analysis showing how perpetration of and victimization by interpersonal violence potentially mediates the effect of substance use on injuries. It revealed a positive direct effect of substance use on injuries [β = 0.10; 95%CI = 0.09, 0.11; p = 0.001]. Decomposition of the effects revealed a positive indirect effect of substance use on injuries running through perpetration of and victimization by interpersonal violence [β = 0.06; 95%CI = 0.05, 0.07; p = 0.001] with a total positive effect of both perpetration [β = 0.18; 95%CI = 0.16, 0.19; p = 0.001] and victimization on injuries [β = 0.22; 95%CI = 0.21, 0.24; p = 0.001]. This finding indicates a significant mediation effect of perpetration of and victimization by interpersonal violence on the association between substance use and injuries.
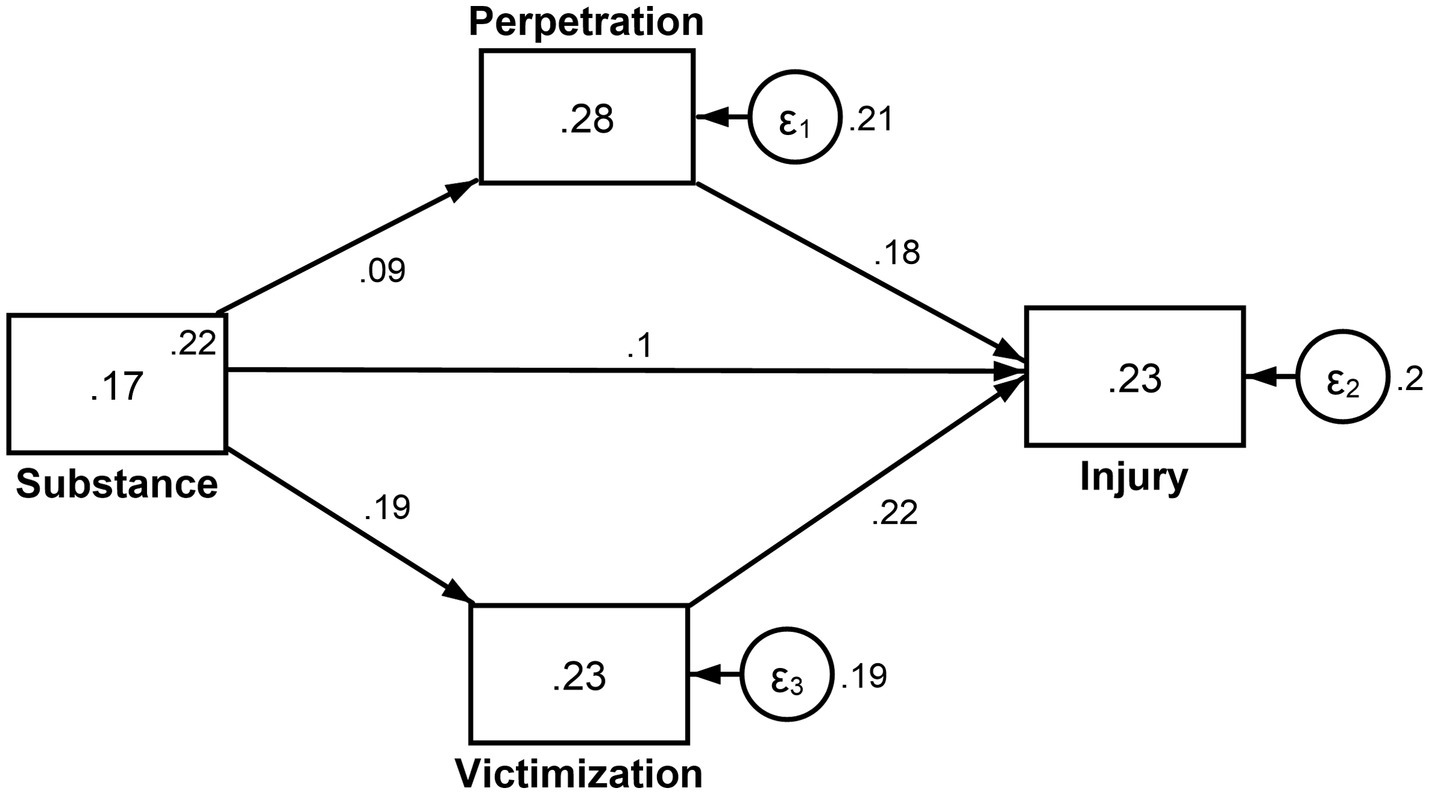
Figure 3. Mediation effect of perpetration of and victimization by interpersonal violence on the association between substance use and injuries.
Associations between substance types (tobacco, cigarette, alcohol, and marijuana) and forms of injuries
Table 4 presents a subgroup analysis showing the association between substance types and forms of injuries using multinomial logistic regression analysis. Compared to adolescents who do not use tobacco, those who used tobacco were 3.98 times more likely to sustain gunshot wound [OR = 3.98, 95%CI = 2.05, 7.75] rather than broken bone/dislocated joint. Also, compared to those who did not use cigarettes, adolescents who smoked cigarettes had 45% lower odds of sustaining a cut/stab wound rather than a broken bone/dislocated joint [OR = 0.55, 95%CI = 0.44, 0.68]. Moreover, compared to non-smokers of marijuana, adolescents who smoked marijuana had 2.81 higher odds of sustaining a gunshot wound [OR = 2.81, 95%CI = 1.29, 6.10] rather than broken bone/dislocated joint. Also, compared to non-users of alcohol, alcohol users were 25% less likely to sustain cut/stab wound [OR = 0.75, 95%CI = 0.62, 0.91], 53% more likely to sustain concussion/head injury [OR = 1.53, 95%CI = 1.19, 1.97], and two and half times more likely to sustain gunshot wound [OR = 2.50, 95%CI = 1.52, 4.12] rather than broken bone/dislocated joint.
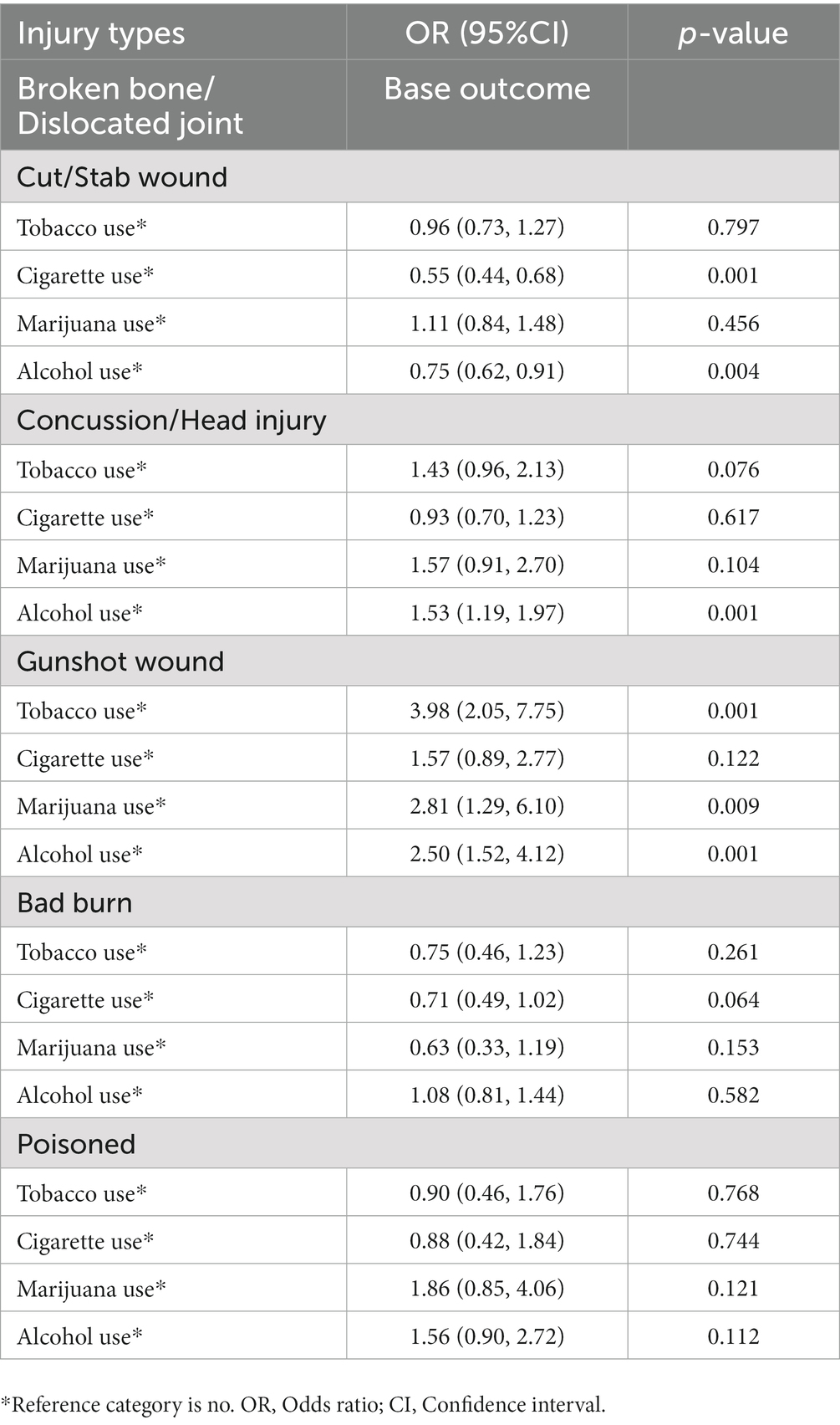
Table 4. Multinomial logistic regression analysis of the associations between substance types (tobacco, cigarette, alcohol, and marijuana) and forms of injuries.
Discussion
To the best of our knowledge, this is the first study examining the mediation effect of both perpetration of and victimization by interpersonal violence on the association between substance use and severe injuries among adolescents from multiple countries. Even though the present study is distinct on this critical topic, previous studies have examined the direct relationships between substance use and serious injuries (26, 27). For example, Guvendeger Doksat et al. (26) reported a strong association between substance use, such as cannabis and cocaine, and non-suicidal self-injury. Van den Ban et al. have also revealed that severe injuries associated with hospital admissions among children and adolescents are twice as high in substance users (27). The current study extends the previously published literature by estimating the mediating role of perpetration of and victimization by interpersonal violence in the global context.
Although the exact mechanisms linking substance use to severe injuries are unclear, several plausible mechanisms and hypotheses have been proposed to account for the observed relationship between substance use and severe injuries among adolescents (10, 13). Our findings suggest that the involvement in interpersonal violence as a perpetrator and/or a victim mediates the connection between substance use and injury among in-school adolescents. Several reasons may explain why perpetration of and victimization by interpersonal violence could be a potential pathway linking substance use and severe injuries among adolescents. Existing evidence suggests that substance use may trigger violent and aggressive behaviours, such as physical attacks and fights which may lead to injuries (28, 29). Consequently, violent and aggressive adolescents may be entangled with other stressful and psychologically detached circumstances, potentially leading to severe injuries (30). The study further explains that correlates of substance use, such as low self-esteem, depression, and anxiety, could influence adolescents to engage in violent and aggressive behaviours, possibly leading to injuries (30). Thus, our findings support earlier evidence suggesting that substance use increases the likelihood of interpersonal violence, thereby intensifying the occurrence of injuries among adolescents. Dynamic strategic approaches involving all stakeholders, such as encouraging parental involvement in school activities, providing more creative, sports, and recreational activities centers for school-going adolescents, and improving on monitoring system in school to control substance use rates, are essential to tackle violent and aggressive behaviours in schools to address serious injuries further. The present study’s findings indicate that the double burden of substance use and interpersonal violence could negatively affect adolescents, which calls for attention both within and outside the school environment.
Lastly, the subgroup analysis yielded noteworthy results, indicating that certain substances, namely tobacco, marijuana, and cigarettes, exhibited statistically significant associations with specific types of injuries, including head injuries and gunshot wounds. For instance, our findings showed that tobacco users had a 3.98 times higher likelihood of sustaining a gunshot wound. Similarly, marijuana users had 2.81 times higher odds of sustaining gunshot wounds, and alcohol users had 1.53 and 2.50 times higher odds of sustaining head injury and gunshot wounds, respectively, underscoring the substantial impact of substance use on the severity of serious injuries. Previous studies have reported similar effects of marijuana and substance use on head injuries (31–33). These findings hold significant implications for public health, policy, and practice. They also emphasize the need for further clinical research to deepen our understanding of the relationship between substance use and injury occurrence, particularly among adolescents.
There are specific strengths and limitations to the present study. Our sample used nationally representative datasets with large sample sizes across several countries and territories, increasing the study findings’ generalizability. Despite these strengths, our results should be interpreted in the context of the following limitations. Although we adjusted for most known potential confounders, it is still possible that residual confounding may exist that impact or explain the results. Also, there is a potential timeframe imbalance between the measures. However, this may not be a methodological concern in a cross-sectional study design like the present study. Moreover, this cross-sectional study cannot infer causal relationships and implications from the association between substance use and serious injuries.
Conclusion
This multi-context study among in-school paediatric populations has provided evidence showing a statistically significant association between substance use and serious injuries, which is mediated by perpetration of and victimization by interpersonal violence. Our results may have utility in informing future public health or substance use and interpersonal violence control policies and interventions, as well as strategies within and outside the school environment to address adolescent substance use and interpersonal violence.
Data availability statement
Publicly available datasets were analyzed in this study. This data can be found here: http://www.cdc.gov/gshs/.
Ethics statement
Ethical review and approval was not required for the study on human participants in accordance with the local legislation and institutional requirements. Written informed consent to participate in this study was provided by the participants’ legal guardian/next of kin.
Author contributions
BA and PP had full access to all of the data in the study and took responsibility for the integrity of the data, the accuracy of the data analysis, acquisition, and analysis, or interpretation of data. PP: concept of design. BA: statistical analysis. BA, MA, SA-A, RO, SN, LM, AA, EO, CA, and PP: drafting of the manuscript and critical revision of the manuscript for important intellectual content. PP and CA: supervision. All authors contributed to the article and approved the submitted version.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Author disclaimer
The findings and conclusions of this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
References
1. World Health Organization. (2021). Fact sheet: adolescent and young adult health. Available at: https://www.who.int/news-room/fact-sheets/detail/adolescents-health-risks-and-solutions (Accessed September 20, 2022).
2. Degenhardt, L, Stockings, E, Patton, G, Hall, WD, and Lynskey, M. The increasing global health priority of substance use in young people. Lancet Psychiatry. (2016) 3:251–64. doi: 10.1016/S2215-0366(15)00508-8
3. NIDA. (2021). NIH-funded study finds overall rate of drug use among 10–14 year-olds remained stable during the 2020 COVID-19 pandemic. Available at: https://nida.nih.gov/news-events/news-releases/2021/08/nih-funded-study-finds-overall-rate-of-drug-use-among-10-14-year-olds-remained-stable-during-the-2020-covid-19-pandemic (Accessed September 19, 2022).
4. Ma, C, Xi, B, Li, Z, Wu, H, Zhao, M, Liang, Y, et al. Prevalence and trends in tobacco use among adolescents aged 13–15 years in 143 countries, 1999–2018: findings from the global youth tobacco surveys. Lancet Child Adolesc Health. (2021) 5:245–55. doi: 10.1016/S2352-4642(20)30390-4
5. Levy, S. (2022). Drug and substance use in adolescents. Available at: https://www.msdmanuals.com/professional/pediatrics/problems-in-adolescents/drug-and-substance-use-in-adolescents (Accessed September 19, 2022).
6. Johnston, LD, Miech, RA, Patrick, ME, O'Malley, PM, Schulenberg, JE, and Bachman, JG. (2021). Monitoring the future National Survey Results on drug use 1975–2021: 2021 overview, key findings on adolescent drug use. Institute for Social Research. Available at: https://eric.ed.gov/?id=ED611736.
7. Simatwa, EMW, Odhong, SO, Juma, SLA, and Choka, GM. Substance abuse among public secondary school students: prevalence, strategies and challenges for public secondary school managers in Kenya: a case study of Kisumu east Sub County. Educ Res. (2014) 5:315–30. doi: 10.14303/er.2014.226
8. Peltzer, K, and Pengpid, S. Injury and social correlates among in-school adolescents in four southeast Asian countries. Int J Environ Res Public Health. (2012) 9:2851–62. doi: 10.3390/ijerph9082851
9. Aboagye, RG, Mireku, DO, Nsiah, JJ, Ahinkorah, BO, Frimpong, JB, Hagan, JE, et al. Prevalence and psychosocial factors associated with serious injuries among in-school adolescents in eight sub-Saharan African countries. BMC Public Health. (2022) 22:853–8. doi: 10.1186/s12889-022-13198-6
10. Macdonald, S, Anglin-Bodrug, K, Mann, RE, Erickson, P, Hathaway, A, Chipman, M, et al. Injury risk associated with cannabis and cocaine use. Drug Alcohol Depend. (2003) 72:99–115. doi: 10.1016/S0376-8716(03)00202-3
11. Davies, RC, Williams, WH, Hinder, D, Burgess, CN, and Mounce, LT. Self-reported traumatic brain injury and post-concussion symptoms in incarcerated youth. J Head Trauma Rehabil. (2012) 27:E21–7. doi: 10.1097/HTR.0b013e31825360da
12. Vitale, S, and Van de Mheen, D. Illicit drug use and injuries: a review of emergency room studies. Drug Alcohol Depend. (2006) 82:1–9. doi: 10.1016/j.drugalcdep.2005.08.017
13. Moore, E, Indig, D, and Haysom, L. Traumatic brain injury, mental health, substance use, and offending among incarcerated young people. J Head Trauma Rehabil. (2014) 29:239–47. doi: 10.1097/HTR.0b013e31828f9876
14. Madan, A, Beech, DJ, and Flint, L. Drugs, guns, and kids: the association between substance use and injury caused by interpersonal violence. J Pediatr Surg. (2001) 36:440–2. doi: 10.1053/jpsu.2001.21599
15. Pfledderer, CD, Burns, RD, and Brusseau, TA. School environment, physical activity, and sleep as predictors of suicidal ideation in adolescents: evidence from a national survey. J Adolesc. (2019) 74:83–90. doi: 10.1016/j.adolescence.2019.05.008
16. Brener, ND, Collins, JL, Kann, L, Warren, CW, and Williams, BI. Reliability of the youth risk behavior survey questionnaire. Am J Epidemiol. (1995) 141:575–80. doi: 10.1093/oxfordjournals.aje.a117473
17. Pengpid, S, and Peltzer, K. Prevalence, demographic and psychosocial correlates for school truancy among students aged 13–15 in the Association of Southeast Asian Nations (ASEAN) member states. J Child Adolesc Ment Health. (2017) 29:197–203. doi: 10.2989/17280583.2017.1377716
18. Pengpid, S, and Peltzer, K. Parental involvement and health risk behaviours among school-going adolescents in six African countries. J Psychol Afr. (2018) 28:212–7. doi: 10.1080/14330237.2017.1409481
19. Asante, KO, Kugbey, N, Osafo, J, Quarshie, EN, and Sarfo, JO. The prevalence and correlates of suicidal behaviours (ideation, plan and attempt) among adolescents in senior high schools in Ghana. SSM Popul Health. (2017) 3:427–34. doi: 10.1016/j.ssmph.2017.05.005
20. Aboagye, RG, Seidu, AA, Bosoka, SA, Hagan, JE Jr, and Ahinkorah, BO. Prevalence and correlates of unintentional injuries among in-school adolescents in Ghana. Int J Environ Res Public Health. (2021) 18:6800. doi: 10.3390/ijerph18136800
21. Pengpid, S, and Peltzer, K. High prevalence of unintentional injuries and socio-psychological correlates among school-going adolescents in Timor-Leste. Int J Adolesc Med Health. (2021) 33:253–9. doi: 10.1515/ijamh-2019-0069
22. MacCallum, RC, Zhang, S, Preacher, KJ, and Rucker, DD. On the practice of dichotomization of quantitative variables. Psychol Methods. (2002) 7:19–40. doi: 10.1037/1082-989X.7.1.19
23. Senanayake, SJ, Gunawardena, S, Wickramasinghe, S, Wickramasinghe, C, Gunawardena, NS, Lokubalasooriya, A, et al. Prevalence and correlates of interpersonal violence among in-school adolescents in Sri Lanka: results from the 2016 Sri Lankan global school-based health survey. Asia Pac J Public Health. (2019) 31:147–56. doi: 10.1177/1010539519825600
24. Peltzer, K, Pengpid, S, and Apidechkul, T. Heavy internet use and its associations with health risk and health-promoting behaviours among Thai university students. Int J Adolesc Med Health. (2014) 26:187–94. doi: 10.1515/ijamh-2013-0508
25. Fairchild, AJ, and MacKinnon, DP. A general model for testing mediation and moderation effects. Prev Sci. (2009) 10:87–99. doi: 10.1007/s11121-008-0109-6
26. Guvendeger Doksat, N, Zahmacioglu, O, Ciftci Demirci, A, Kocaman, GM, and Erdogan, A. Association of suicide attempts and non-suicidal self-injury behaviors with substance use and family characteristics among children and adolescents seeking treatment for substance use disorder. Subst Use Misuse. (2017) 52:604–13. doi: 10.1080/10826084.2016.1245745
27. van den Ban, E, Souverein, P, Meijer, W, Van Engeland, H, Swaab, H, Egberts, T, et al. Association between ADHD drug use and injuries among children and adolescents. Eur Child Adolesc Psychiatry. (2014) 23:95–102. doi: 10.1007/s00787-013-0432-8
28. Barkin, SL, Smith, KS, and DuRant, RH. Social skills and attitudes associated with substance use behaviors among young adolescents. J Adolesc Health. (2002) 30:448–54. doi: 10.1016/S1054-139X(01)00405-0
29. DuRant, RH, Altman, D, Wolfson, M, Barkin, S, Kreiter, S, and Krowchuk, D. Exposure to violence and victimization, depression, substance use, and the use of violence by young adolescents. J Pediatr. (2000) 137:707–13. doi: 10.1067/mpd.2000.109146
30. Litwiller, BJ, and Brausch, AM. Cyber bullying and physical bullying in adolescent suicide: the role of violent behavior and substance use. J Youth Adolesc. (2013) 42:675–84. doi: 10.1007/s10964-013-9925-5
31. Baiden, P, Morgan, MA, and Logan, MW. Sports-and physical activity-related concussions, binge drinking and marijuana use among adolescents: the mediating role of depression and suicidal ideation. Subst Use Misuse. (2022) 57:504–15. doi: 10.1080/10826084.2021.2019779
32. Andelic, N, Jerstad, T, Sigurdardottir, S, Schanke, AK, Sandvik, L, and Roe, C. Effects of acute substance use and pre-injury substance abuse on traumatic brain injury severity in adults admitted to a trauma Centre. J Trauma Manag Outcomes. (2010) 4:1–2. doi: 10.1186/1752-2897-4-6
33. Olson-Madden, JH, Brenner, LA, Corrigan, JD, Emrick, CD, and Britton, PC. Substance use and mild traumatic brain injury risk reduction and prevention: a novel model for treatment. Rehabil Res Pract. (2012) 2012:1–6. doi: 10.1155/2012/174579
Keywords: substance use, interpersonal violence, serious injuries, mediation, adolescents
Citation: Adjei BN, Afetor M, Ansong-Aggrey S, Okwei R, Nachibi SU, Munkaila L, Arimiyaw AW, Osei Bonsu E, Adu C and Peprah P (2023) Substance use and adolescent injuries: a multi-country analysis of the association and mediating effect of interpersonal violence among 122,945 in-school paediatric populations in 29 countries. Front. Public Health. 11:1193711. doi: 10.3389/fpubh.2023.1193711
Edited by:
Jingwen Hu, University of Michigan, United StatesReviewed by:
Jason Randall, University of Alberta, CanadaRobert J. Wellman, Department of Population & Quantitative Health Sciences, United States
Copyright © 2023 Adjei, Afetor, Ansong-Aggrey, Okwei, Nachibi, Munkaila, Arimiyaw, Osei Bonsu, Adu and Peprah. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Benjamin Noble Adjei, YmVubm9ibGVhZGplaUBnbWFpbC5jb20=
 Benjamin Noble Adjei
Benjamin Noble Adjei Maxwell Afetor2,3
Maxwell Afetor2,3 Reforce Okwei
Reforce Okwei Emmanuel Osei Bonsu
Emmanuel Osei Bonsu