- 1School of Medicine, Universidad de San Martín de Porres, Chiclayo, Peru
- 2Sociedad Científica San Fernando, Universidad Nacional Mayor de San Marcos, Lima, Peru
- 3Sociedad Científica Médico Estudiantil Continental, Universidad Continental, Huancayo, Peru
- 4Grupo Peruano de Investigación Epidemiológica, Unidad de Investigación para la Generación y Síntesis de Evidencias en Salud, Universidad San Ignacio de Loyola, Lima, Peru
- 5Carrera de Farmacia y Bioquímica, Facultad de Ciencias de la Salud, Universidad Científica del Sur, Lima, Peru
- 6Unidad de Investigación para la Generación y Síntesis de Evidencias en Salud, Universidad San Ignacio de Loyola, Lima, Peru
- 7OBEMET Centro de Obesidad y Salud Metabólica, Lima, Peru
Background: Sexually transmitted infections (STIs) are a serious public health problem worldwide, especially among reproductive-age women. The early sexual onset of sexual intercourse (EOSI) has been suggested as a risk factor, although there is no data at the national level.
Objective: To evaluate the association between EOSI and STIs in Peruvian women of childbearing age.
Methods: Analytical cross-sectional study with secondary data analyzes of the Peruvian Demographic and Family Health Survey 2018. The outcome was the presence of STIs in the last 12 months and the exposure variable was EOSI (age < 15 years at the time of their first sexual experience). To evaluate the association of interest, crude and adjusted prevalence ratios (aPRs) were calculated using generalized linear models with Poisson family and logarithmic link function.
Results: We analyzed data from 31,028 women of childbearing age. The 11.3% reported having STIs in the last 12 months and 20.2% of the participants had an EOSI. After adjusting for potential confounders, we found that EOSI was associated with STIs (aPR: 1.27; 95% CI: 1.08–1.50; p = 0.005). When conducting stratified analysis by area of residence and number of sexual partners, this association was maintained in women living in urban areas (aPR: 1.36; 95% CI: 1.11–1.66; p = 0.003) those who did not report having a history of multiple sexual partners (aPR: 1.27; 95% CI: 1.08–1.51; p = 0.005), and those in the middle (aPR: 1.42; 95% CI: 1.03–1.97; p = 0.034) and highest (aPR: 2.12; 95% CI: 1.33–3.39; p = 0.002) wealth quintiles.
Conclusion: Among reproductive-age women from Peru, EOSI was associated with STIs, especially in women living in urban areas, with no history of multiple sexual partners, and belonging to the middle to higher wealth index. The implementation of measures to prevent EOSI and fostering appropriate sexual health counseling for women with EOSI is advised.
1. Introduction
Sexually transmitted infections (STIs) represent a significant public health threat globally, primarily affecting family units, societal health, and individuals between the ages of 10–25 years (1–3). According to the World Health Organization (WHO), one million people contract an STI every day, predominantly chlamydia (127 million), gonorrhea (87 million), syphilis (6.3 million), trichomoniasis (156 million), and infections caused by hepatitis B virus, herpes simplex virus, human immunodeficiency virus (HIV), and human papillomavirus (HPV) (4). Notably, a strong association has also been observed between STIs and cancer (5–7), which also escalates healthcare costs (8, 9).
Evidence indicates that individuals exhibiting high-risk behaviors, such as frequent alcohol and tobacco use (10–12) drug use (13), engagement in unprotected sexual practices, or having multiple sexual partners (3, 14, 15) are at an increased risk of contracting STIs. Other contributing factors include exposure to sexual and physical violence (16), low socioeconomic status, low education level, rural place of origin, single marital status (12–15, 17), and early initiation of sexual activity (14, 18).
Early onset of sexual intercourse (EOSI) is defined as having a first sexual experience before the age of 15 years (18). Factors associated with EOSI reported in literature encompass substance use disorders (19–21), deficient family planning knowledge (21), inadequate family support (22), and a history of childhood abuse (23). This tends to amplify the occurrence of unwanted pregnancies, abortions, financial burdens, and STIs (10, 14, 16). In fact, studies conducted in Asia (14), Africa (24, 25), and America (26–30) have reported that young people with an EOSI are more likely to exhibit symptoms and receive an STI diagnosis during their lifetime. In Peru, (31) a study conducted in the province of Alto Huallaga (Huanuco, Peru) by Gomez et al. (27) found no statistically significant association between the age of first sexual intercourse (≤13 years) and STIs in their multivariable model. It should be noted that this study was restricted to a primary healthcare center’s population and solely included adolescents and young adults aged 18–24.
Globally, the average age of the onset of sexual activity is unknown, as most reports of sexual activity are more focused on selective groups (32–34). In Peru, it has been reported that half of the women between 25 and 49 years experienced their first sexual intercourse at 18.5 years (35). Furthermore, approximately 13% of women reported an STI or symptoms such as vaginal discharge or genital ulcers in 2017 (36). Therefore, despite the relevance and the potential connection between EOSI and STIs, there remains a lack of research in this area. Hence, this study aimed to evaluate the association between EOSI and STIs among reproductive-age women in Peru.
2. Materials and methods
2.1. Study design and data collection
We conducted an analytical cross-sectional study with secondary data analyzes. The study data were obtained from the Demographic and Family Health Survey (ENDES, Spanish acronym), which was carried out in 2018 (February to December) (35). ENDES, conducted annually by the National Institute of Statistics and Informatics (INEI, Spanish acronym), is a sample survey stratified by clusters representative at the national level that provides information on the health indicators of the Peruvian population. It comprises three questionnaires (Household, Individual women, and Health), and the data are collected in person by certified personnel. For this study, we used the Individual Questionnaire for Women, particularly the sections Medical Records; Reproduction; Birth History; Marriage; Knowledge and Attitude Regarding AIDS and Other STIs; HIV/AIDS; and Contraceptive Use. Additional information on the methodology of the survey can be found on the ENDES website.1
2.2. Sample population and context
The original ENDES 2018 data set included 39,745 women of childbearing age (15–49 years). This study excluded the data of 3,730 participants who had not yet commenced their sexual activityt, 174 participants who had their first sexual intercourse with their first partner and did not indicate their age at the time of the occurrence, and 4,813 participants with missing data for the variables of interest of this study. Finally, the analysis sample comprised 31,028 women aged 15–49 years who had already initiated their sexual activity. It is important to mention that our study only includes women, as complete information is only available for this population (i.e., there is no “Individual Men’s Questionnaire”).
2.3. Dependent variable
The main outcome of this study was the presence of STIs in the last 12 months. For its development, the RE758081 file of the ENDES 2018 microdata was considered, which included information on the knowledge, attitudes, opinions, and behaviors of women surveyed regarding STIs and AIDS. Variables with the codes V763A, V763B, and V763C were used to determine if the interviewee had any STI. The questiorans for the same were “In the last 12 months, have you been diagnosed with any STIs?0”; “During the last 12 months, have you had any sore or ulcer on your genitals?”; and “During the last 12 months, have you had any foul-smelling genital discharge or secretion?”. A new variable was created from these questions and dichotomized into Yes (when the participant answered yes to any of the questions) and No/Do Not Know.
2.4. Exposure
The primary independent variable whose association with the main outcome was evaluated in this study was the EOSI, which was constructed using data from the interviewee’s self-report of their age (in years) at the time of their first sexual experience. The cutoff age for the categorization of the study participants was set as below and equal to or above 15 years (22, 37–39).
2.5. Other variables
Other independent variables were also considered in the study, including age categories (15–19, 20–24, 25–29, 30–39; 40–49 years), marital status (unmarried; married/cohabiting), level of education (preschool/primary; secondary; professional/undergraduate/postgraduate), currently employed (yes; no), wealth index (very poor; poor; average; rich; very rich), region of origin (metropolitan Lima; rest of the coast; mountains; rainforest), area of residence (rural; urban), parity (childless; 1–2 children; >3 children), multiple sexual partners (yes [≥2 partners]; no [<2 partners]), and use of contraception (no contraception; condom; other).
2.6. Statistical analysis
The ENDES data were downloaded and filtered using the study variables as a reference. The statistical analysis of the data was performed by the Stata v16.0 statistical package (Stata Corporation, College Station, Texas, United States). The complex sample structure of the data was adjusted using the svy command, considering the sampling units, strata, and corresponding weighting factors for women of childbearing age. For univariate analysis, the categorical variables were summarized by absolute frequencies and weighted proportions, with a corresponding 95% confidence intervals (CI). The Chi-square test of independence along with Rao–Scott correction was used for comparing the independent variables and STI in the last 12 months.
To evaluate the association of interest, crude prevalence ratios and adjusted prevalence ratios (aPRs) were calculated using generalized linear models (GLMs) with Poisson family and logarithmic link function. The adjusted model followed an epidemiological approach and was adjusted for all the potentially confounding variables (age, marital status, level of education, wealth index, region of origin, residence, and use of contraception). All the estimates were reported with their corresponding 95% CIs, and p < 0.05 was considered significant.
Finally, interactions with the area of residence, multiple sexual partners, and wealth index were assessed using the adjusted Wald test (testparm command). Since the results were significant for these interactions, the final models were presented in a stratified manner.
2.7. Ethical aspects
The research protocol was reviewed and approved by the Institutional Review Board of the Universidad de San Martín de Porres (Record No. 991-2020-CIEI-FMH-USMP). This was an analytical study of the secondary database, which can be freely availed and accessed on the INEI website. This database is anonymous and does not reveal the identification of the participants.
This study offers both scientific and social benefits by addressing a gap in research regarding the association between early onset of sexual intercourse (EOSI) and sexually transmitted infections (STIs) among reproductive-age women in Peru. The findings can refine intervention strategies, enhance health policies, and guide future research to mitigate STI prevalence. Furthermore, the study aids in increasing awareness about STI risk factors, including EOSI, facilitating the development of targeted educational programs and community outreach efforts that promote safer sexual practices and ultimately improve public health and societal well-being.
3. Results
3.1. Sociodemographic characteristics of the study population
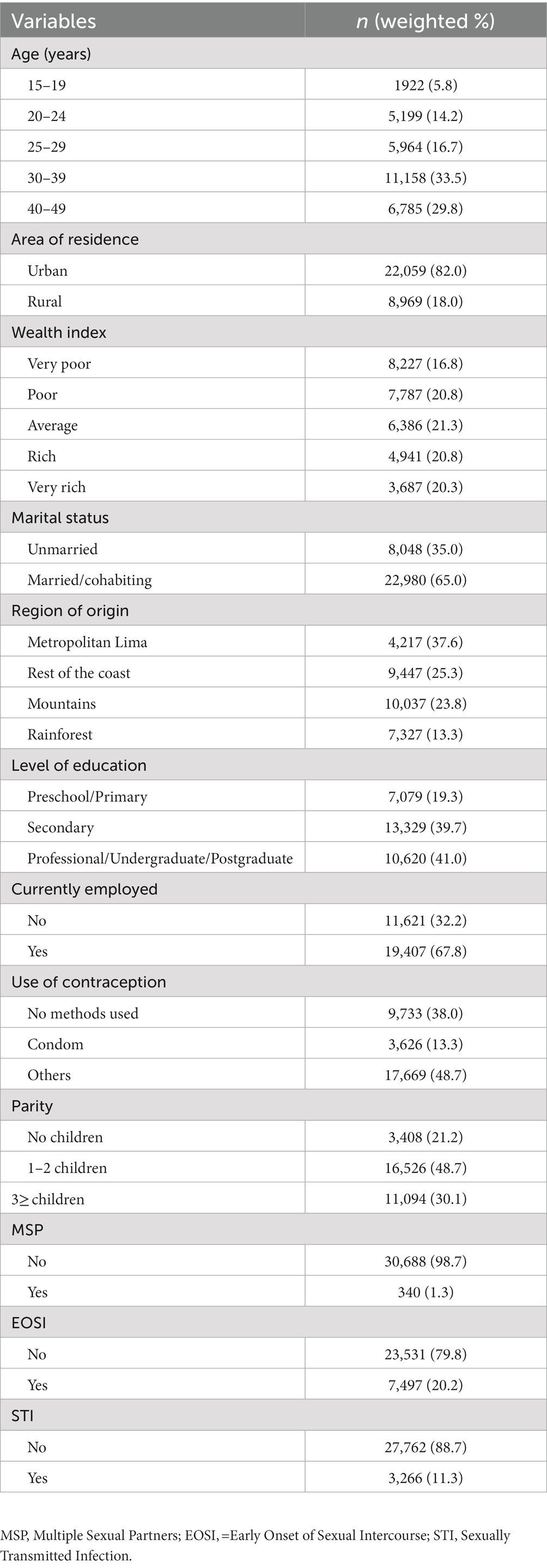
The study sample included 31,028 women of childbearing age, with majority of the participants in the 30–39 years age group (33.5%), followed by the 40–49 years age group (29.8%). In addition, 20.2% of the participants had an EOSI and 11.3% reported having STIs. The other sociodemographic variables are presented in Table 1.
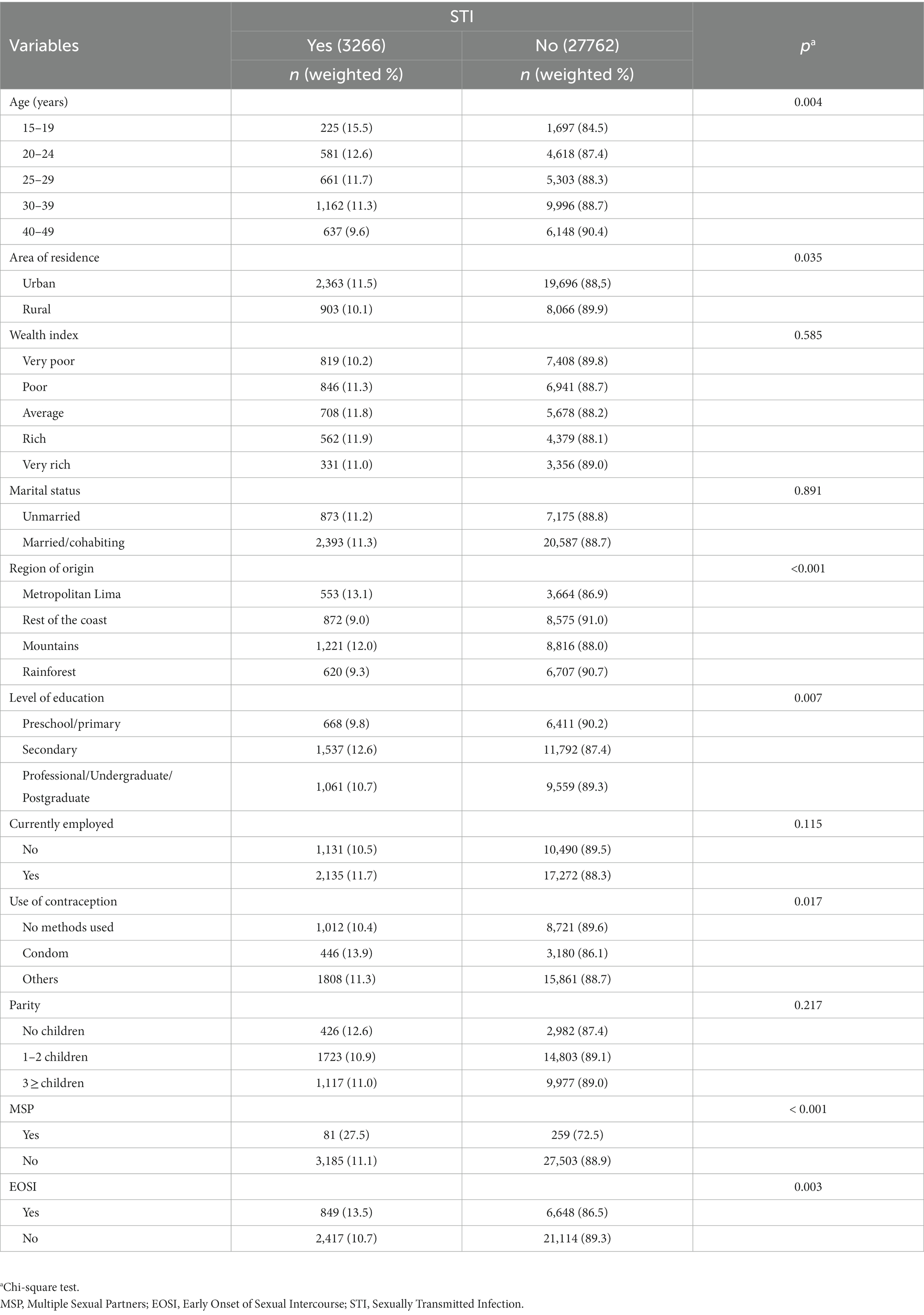
3.2. Characteristics of the study population according to their history of STIs
We found that the prevalence of STIs was significantly higher among women aged 15–19 years (p = 0.004), those living in urban areas (p = 0.035), those from metropolitan Lima (p < 0.001), those with secondary education (p = 0.007), those who had previously used condoms as a contraceptive method (p = 0.017), and those with a history of multiple sexual partners (p < 0.001). Regarding EOSI, 13.5% of the women in this category reported having an STI in recent months (p = 0.003) (Table 2).
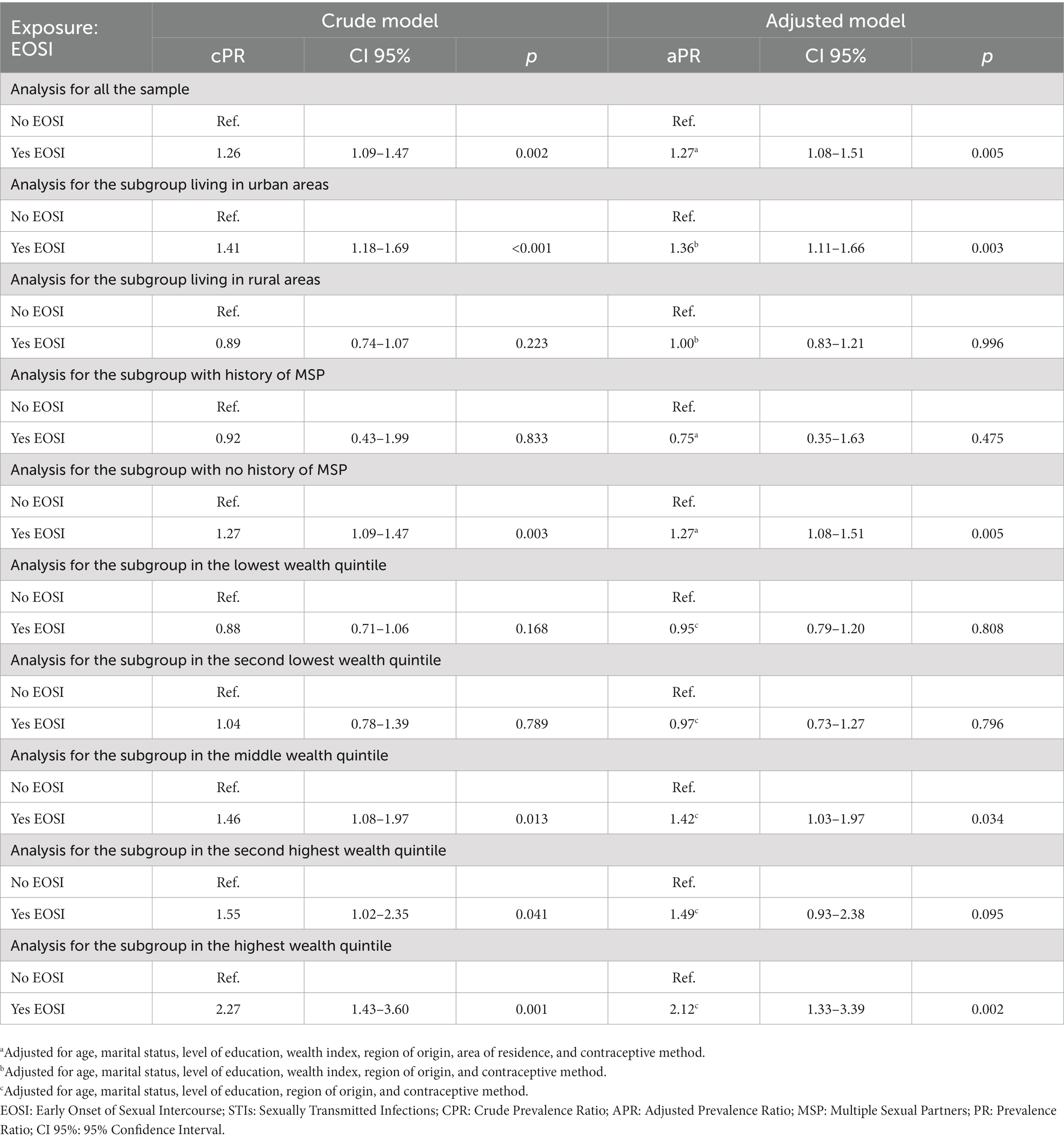
3.3. Association between the EOSI and STIs
Table 3 shows the crude and adjusted model for the association of interest. In all the sample, after adjustinf for potential confounders, the EOSI was found to be positively associated with STIs (aPR: 1.27; 95% CI: 1.08–1.50; p = 0.005). When conducting stratified analysis by area of residence, number of sexual partners and wealth index, this association was maintained in women living in urban areas (aPR: 1.36; 95% CI: 1.11–1.66; p = 0.003), those who did not report having a history of multiple sexual partners (aPR: 1.27; 95% CI: 1.08–1.51; p = 0.005), and those in the middle (aPR: 1.42; 95% CI: 1.03–1.97; p = 0.034) and highest (aPR: 2.12; 95% CI: 1.33–3.39; p = 0.002) wealth quintiles. The association was marginally statistically significant in the subgroup within the second highest wealth quintile (aPR: 1.49; 95% CI: 0.93–2.38; p = 0.095).
4. Discussion
4.1. Main findings
Using the data from more than 31,000 self-reports by Peruvian women of childbearing age who had already initiated their sexual activity, an association was found between the EOSI and the diagnosis or clinical symptoms of STIs in the last 12 months. Moreover, considering the area of residence, multiple sexual partners, and wealth index, an association between the EOSI and STIs was found only in women living in urban areas, those without a history of multiple sexual partners, those in the middle and highest wealth quintiles, and was marginally statistically significant in the subgroup within the second highest wealth quintile.
4.2. Comparison with other studies
Several studies have evaluated the association between the EOSI and STIs, early pregnancies, abortions, and long-term sexual consequences (40). However, to the best of our knowledge, no such studies have been conducted in Latin America, a region where the control of STIs is a persisting challenge (41). In this study, we determined that the EOSI increases the prevalence of STIs by 27% in women of childbearing age compared with those who report initiating sexual activities after the age of 15 years. Similarly, a longitudinal study in the United States of America (USA) (30) found that the EOSI was associated with lifelong STIs and during the last year in young women aged 24–34 years. Miller et al. (42) evaluated sexually active women between the ages of 15 and 44 years in the United States, and found that the prevalence of STIs (gonorrhea and chlamydia) was inversely proportional to the age of sexual activity initiation (13% STI prevalence at <15 years, 7% at 15–16 years, 5.3% at 17–18 years, and 3.4% at >19 years). In contrast, a study conducted in Spain (43) found no association between the EOSI and STIs in women between the ages of 18 and 70 years. However, the definition of the EOSI in the study was beginning sexual intercourse before the age of 18 years, whereas in this study, the EOSI is defined as the initiation of sexual activities before the age of 15 years.
An association between the EOSI and STIs were found in women with a history of having <2 sexual partners during the last 12 months. Similarly, in a sample of adults aged 15–49 years whose average number of sexual partners was <2 during their lifetime, the EOSI was observed to increase the STI odds in the last year (44) (OR: 1.41, 95% CI: 1.26–1.58). Additionally, the individuals with an EOSI who were sexually active with their partner during the last year were less likely to use a condom with their partner than those with a late onset of sexual intercourse. When evaluating the association between the EOSI and STIs according to the area of residence, this study identified the association only in the women living in urban areas. Similarly, Pinzon et al. (45) identified higher STI odds (specifically for syphilis) in Colombian adults living in an urban area, particularly in those who have been sexually active for a longer period than in those who had been sexually active for <20. Although a long period of sexual activity might suggest an EOSI, this is not accurate. The abovementioned study also included an urban population recently displaced from rural areas. In this study, a higher frequency of STIs was observed in the women living in urban areas than in rural areas. Similarly, there have been reports of a higher frequency of EOSI in sexually active Vietnamese women living in urban areas (15). Olakunle and Banougnin found a greater use of modern contraception that did not protect against STIs in Nigerian women aged between 14 and 24 years living in urban areas than in rural areas (46).
In our study, we found that EOSI was associated with STIs in women from the middle wealth quintile upwards. Socioeconomic status has been differently associated with both variables in the literature. A study conducted by Newbern et al. (47) reported that socioeconomic status was a weak to moderate indicator for STIs in American adolescents, while research in Uganda found that living in areas of higher socioeconomic status was associated with a higher risk of STIs (48). Regarding EOSI, the association reported in the literature is inverse, as evidenced in studies conducted in Africa, where young women belonging to higher wealth indexes had a lower risk of EOSI (49, 50).
4.3. Interpretation of the results
The EOSI has been associated with having multiple sexual partners, paying for sex, inconsistent use of contraception (44), group and/or casual sex (12), and depression (30). These also represent risk factors of STI transmission, thus supporting its association with the EOSI. An EOSI is hypothesized to cause the proportional increase of HIV cases in adolescent women aged 12–17 years in Peru during the last 5 years (51). Likewise, the increase of the EOSI in Peru (the prevalence of the EOSI was 5.1% in 2000 vs. 6.2% in 2009) (52) and its association with STIs in urban areas could explain the increase in STI cases in women and men from these areas (53). The migration of people from the rural to urban areas also poses a risk of increasing STI cases, with a higher STI risk reported in women migrating from rural to urban areas (54, 55).
Our study also demonstrated an association between the EOSI and STIs in women with <2 sexual partners during the last year, which might be accounted for by the inconsistent use of condoms, leading to a higher risk of STI transmission (55). Furthermore, it is important to highlight that several STIs are chronic and could be previously contracted by the women with an EOSI through transmission by the multiple sexual partners they might have had throughout their lives or prior to the year of evaluation (56), or due to their history of other sexually risky behaviors, such as casual or group sex (12). In addition, a cause of the EOSI in women is sexual abuse at an early age (57), wherein the sexual activities usually occurred without the use of condoms (58). Also, women with a history of sexual abuse at an early age show higher rates of sexual dysfunction (59), which could explain the lower number of sexual partners and chronic STIs.
The association between EOSI and STI was primarily evident in women belonging to a middle-to-high socioeconomic status, which may have several explanations. First, sexual patterns and practices may differ across various socioeconomic levels. For instance, in lower socioeconomic statuses, there is a higher prevalence of sexual relationships within stable and monogamous relationships (60), which could reduce the risk of STI. Second, literature has reported that women with a higher socioeconomic status exhibit increased behavior in seeking health care related to STIs (61). In this regard, limited access to medical care in lower socioeconomic levels could lead to reduced detection and reporting of STI.
4.4. Relevance in terms of public health
In 2020, the WHO estimated an incidence of 374 million STIs of bacterial origin (62). Concerning viral STIs, almost 20 million women and girls worldwide were living with HIV in 2020 (63), and almost 500 million people had a herpes infection in 2016 (62). It was estimated that 300 million women were infected with HPV, one of the causes of cervix cancer, the second most frequent type of cancer and the second most lethal among women of childbearing age worldwide (64). On the other hand, the age of beginning sexual activity lowers each year. In addition, the cost of STI treatments throughout people’s lives, according to the beginning of their sexual activity, is approximately calculated to be 16 billion dollars (65). In Peru, one out of five women reports having an EOSI. This study demonstrated an association between the EOSI and STIs in women of childbearing age compared with those who had a late onset of sexual intercourse. Hence, it is imperative to implement preventive measures for STIs in women who are yet to be sexually active and guide their decision-making process regarding this matter by providing them with the necessary tools (66). A few clinical trials of African students report on the relevance of the interventional roles played by schools, parents, communities, and the health system as a group in order to delay the age of sexual activity onset and increase women’s practice of using condoms (67). It is also essential to promote preventive behaviors in adolescents, such as regular attendance to health screenings (53), and to decrease risk factors such as alcohol use (68), smoking, peer pressure, and poor parental supervision (69). Moreover, interventional behavioral counseling (70) (in person or virtually) of sexually active women is recommended to promote safer sex practices; provide training in condom use, problem solving, communication about safer sex, and to assess the person’s risk of acquiring STIs.
4.5. Limitations
The present study is cross-sectional, which means establishing causal links between the variables of interest was not possible. Additionally, the STI variable focused on the last 12 months, not accounting for potential previous infections. Other factors associated with STIs, such as the characteristics of sexual partners (71), history of STIs (72), use of antiviral therapy (73), and mental health (74) were not included in this study due to the use of a secondary database. However, our study has strengths, including a large, nationally representative sample, and an analysis that considered area of residence, wealth index, and history of multiple sexual partners. We also adjusted for available confounding variables. Lastly, we did not conduct a mediation analysis because of the lack of certain variables in the database. For example, literature suggests that the use of illicit drugs prior to sexual activity could act as a mediator in the relationship between EOSI and STI (12). Therefore, we believe this should be analyzed in future studies.
5. Conclusion
Among Peruvian women aged 15 to 49 years who had initiated their sexual activity, 20% reported an EOSI. In this group, there was a notable association between EOSI and STIs. This association was particularly evident in urban women without a history of multiple sexual partners and in those belonging to a medium to high wealth index. It is recommended to implement measures to prevent EOSI and to provide targeted sexual health counseling for women reporting an EOSI.
Data availability statement
Publicly available datasets were analyzed in this study. This data can be found at: https://proyectos.inei.gob.pe/microdatos/.
Author contributions
JP-F and DA-V: conceptualization, investigation, and writing – original draft. MH: investigation and writing – original draft. SC-B: investigation, visualization, and writing – original draft. AL-V: investigation, visualization, writing – original draft, and writing – review and editing. CD-F: methodology, data curation, formal analysis, and writing – original draft. CT-H: conceptualization, methodology, formal analysis, writing – original draft, and supervision. All authors contributed to the article and approved the submitted version.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Footnotes
References
1. Álvarez Mesa, M, de la Torre, NL, and Domínguez, GJ. Las Infecciones de Transmisión Sexual: una revisión dirigida a la atención primaria de salud. Rev. Cuba. de Medicina Gen. Integral. (2014) 30:343–53.
2. Arefaynie, M, Yalew, M, Damtie, Y, and Kefale, B. Determinants of early sexual initiation among female youth in Ethiopia: a multilevel analysis of 2016 Ethiopian demographic and health survey. BMC Womens Health. (2020) 20:205. doi: 10.1186/s12905-020-01069-4
3. Urassa, W, Moshiro, C, Chalamilla, G, Mhalu, F, and Sandstrom, E. Risky sexual practices among youth attending a sexually transmitted infection clinic in Dar Es Salaam, Tanzania. BMC Infect Dis. (2008) 8:159. doi: 10.1186/1471-2334-8-159
4. WHO. Sexually transmitted infections (STIs) [internet]. Available at: https://www.who.int/news-room/fact-sheets/detail/sexually-transmitted-infections-(stis)
5. Caini, S, Gandini, S, Dudas, M, Bremer, V, Severi, E, and Gherasim, A. Sexually transmitted infections and prostate cancer risk: a systematic review and meta-analysis. Cancer Epidemiol. (2014) 38:329–38. doi: 10.1016/j.canep.2014.06.002
6. Durães, LC d, and Sousa, JB d. Anal cancer and sexually transmitted diseases: what is the correlation? Rev Col Bras Cir. (2010) 37:265–8. doi: 10.1590/s0100-69912010000400005
7. Frazier, EL, Sutton, MY, Tie, Y, McNaghten, AD, Blair, JM, and Skarbinski, J. Screening for cervical Cancer and sexually transmitted diseases among HIV-infected women. J Women's Health. (2016) 25:124–32. doi: 10.1089/jwh.2015.5368
8. Pearson, WS, Spicknall, IH, Cramer, R, and Jenkins, WD. Medicaid coverage of sexually transmitted disease service visits. Am J Prev Med. (2019) 57:51–6. doi: 10.1016/j.amepre.2019.02.019
9. Silverman, RA, Katz, DA, Levin, C, Bell, TR, Spellman, D, St John, L, et al. Sexually transmitted disease partner services costs, other resources, and strategies across jurisdictions to address unique epidemic characteristics and increased incidence. Sex Transm Dis. (2019) 46:493–501. doi: 10.1097/OLQ.0000000000001010
10. Jung, M. Risk factors of sexually transmitted infections among female sex workers in Republic of Korea. Infect Dis Poverty. (2019) 8:6. doi: 10.1186/s40249-019-0516-x
11. Rodríguez-Álvarez, MI, Gómez-Urquiza, JL, Husein-El Ahmed, H, Albendín-García, L, Gómez-Salgado, J, and Cañadas-De la Fuente, GA. Prevalence and risk factors of human papillomavirus in male patients: a systematic review and Meta-analysis. Int J Environ Res Public Health. (2018) 15:2210. doi: 10.3390/ijerph15102210
12. Wu, TL, Ting, TT, Chen, CY, Su, LW, and Chen, WJ. Early sexual initiation and risky sexual practices among alcohol- and tobacco-using young adults in Taiwan: mediation analysis of preceding-sex use of illicit drugs. BMC Public Health. (2020) 20:1647. doi: 10.1186/s12889-020-09777-0
13. Wendland, EM, Horvath, JDC, Kops, NL, Bessel, M, Caierão, J, Hohenberger, GF, et al. Sexual behavior across the transition to adulthood and sexually transmitted infections: findings from the national survey of human papillomavirus prevalence (POP-Brazil). Medicine (Baltimore). (2018) 97:e11758. doi: 10.1097/MD.0000000000011758
14. Ma, Q, Ono-Kihara, M, Cong, L, Xu, G, Pan, X, Zamani, S, et al. Early initiation of sexual activity: a risk factor for sexually transmitted diseases, HIV infection, and unwanted pregnancy among university students in China. BMC Public Health. (2009) 9:111. doi: 10.1186/1471-2458-9-111
15. Son, DT, Oh, J, Heo, J, Van Huy, N, Van Minh, H, Choi, S, et al. Early sexual initiation and multiple sexual partners among Vietnamese women: analysis from the multiple Indicator cluster survey, 2011. Glob Health Action. (2016) 9:29575. doi: 10.3402/gha.v9.29575
16. Nigatu, AM, Birhanu, AY, and Endehabtu, BF. Geographical variations of early age sexual initiation among reproductive-age women in Ethiopia: evidence from EDHS 2016. Arch Public Health. (2020) 78:28. doi: 10.1186/s13690-020-00411-4
17. Thorsteinsson, K, Ladelund, S, Storgaard, M, Rønsholt, FF, Johansen, IS, Pedersen, G, et al. Sexually transmitted infections and use of contraceptives in women living with HIV in Denmark – the SHADE cohort. BMC Infect Dis. (2016) 16:81. doi: 10.1186/s12879-016-1412-7
18. Uthman, OA. Geographical variations and contextual effects on age of initiation of sexual intercourse among women in Nigeria: a multilevel and spatial analysis. Int J Health Geogr. (2008) 7:27. doi: 10.1186/1476-072X-7-27
19. Peltzer, K, and Pengpid, S. Early sexual debut and associated factors among in-school adolescents in six Caribbean countries. West Indian Med J. (2015) 64:351–6. doi: 10.7727/wimj.2014.025
20. Roman Lay, AA, Fujimori, E, Simões Duarte, L, and Vilela Borges, AL. Prevalence and correlates of early sexual initiation among Brazilian adolescents. PLoS One. (2021) 16:e0260815. doi: 10.1371/journal.pone.0260815
21. Turi, E, Merga, BT, Fekadu, G, and Abajobir, AA. Why too soon? Early initiation of sexual intercourse among adolescent females in Ethiopia: evidence from 2016 Ethiopian demographic and health survey. Int J Women's Health. (2020) 12:269–75. doi: 10.2147/IJWH.S244621
22. Gazendam, N, Cleverley, K, King, N, Pickett, W, and Phillips, SP. Individual and social determinants of early sexual activity: a study of gender-based differences using the 2018 Canadian health behaviour in school-aged children study (HBSC). PLoS One. (2020) 15:e0238515. doi: 10.1371/journal.pone.0238515
23. Wang, ZY, Hu, M, Yu, TL, and Yang, J. The relationship between childhood maltreatment and risky sexual behaviors: a Meta-analysis. Int J Environ Res Public Health. (2019) 16:3666. doi: 10.3390/ijerph16193666
24. Abdul, R, Gerritsen, AAM, Mwangome, M, and Geubbels, E. Prevalence of self-reported symptoms of sexually transmitted infections, knowledge and sexual behaviour among youth in semi-rural Tanzania in the period of adolescent friendly health services strategy implementation. BMC Infect Dis. (2018) 18:229. doi: 10.1186/s12879-018-3138-1
25. Tilahun, M, and Ayele, G. Factors associated with age at first sexual initiation among youths in Gamo Gofa, south West Ethiopia: a cross sectional study. BMC Public Health. (2013) 13:622. doi: 10.1186/1471-2458-13-622
26. Epstein, M, Manhart, LE, Hill, KG, Bailey, JA, Hawkins, JD, Haggerty, KP, et al. Understanding the link between early sexual initiation and later sexually transmitted infection: test and replication in two longitudinal studies. J Adolesc Health. (2014) 54:435–441.e2. doi: 10.1016/j.jadohealth.2013.09.016
27. Gómez, AM, Speizer, IS, Reynolds, H, Murray, N, and Beauvais, H. Age differences at sexual debut and subsequent reproductive health: is there a link? Reprod Health. (2008) 5:8. doi: 10.1186/1742-4755-5-8
28. Kahn, NF, and Halpern, CT. Associations between patterns of sexual initiation, sexual partnering, and sexual health outcomes from adolescence to early adulthood. Arch Sex Behav. (2018) 47:1791–810. doi: 10.1007/s10508-018-1176-9
29. Tu, W, Batteiger, BE, Wiehe, S, Ofner, S, Van Der Pol, B, Katz, BP, et al. Time from first intercourse to first sexually transmitted infection diagnosis among adolescent women. Arch Pediatr Adolesc Med. (2009) 163:1106–11. doi: 10.1001/archpediatrics.2009.203
30. Vasilenko, SA, Kugler, KC, and Rice, CE. Timing of first sexual intercourse and Young adult health outcomes. J Adolesc Health. (2016) 59:291–7. doi: 10.1016/j.jadohealth.2016.04.019
31. Gómez, W, Damaso, B, Cortegana, C, Lahura, P, and Motta, J. Comportamientos sociales y sexuales asociados a las infecciones de transmisión sexual en jóvenes del Alto Huallaga. An Fac Med. (2008) 69:17–21. doi: 10.15381/anales.v69i1.1174
32. Freak-Poli, R, Kirkman, M, De Castro, LG, Direk, N, Franco, OH, and Tiemeier, H. Sexual activity and physical tenderness in older adults: cross-sectional prevalence and associated characteristics. J Sex Med. (2017) 14:918–27. doi: 10.1016/j.jsxm.2017.05.010
33. Jee, Y, and Lee, G. Prevalence of sexual experience among Korean adolescent: age-period-cohort analysis. Epidemiol Health. (2020) 42:e2020008. doi: 10.4178/epih.e2020008
34. Yan, R, Yu, J, Tanimoto, T, Ozaki, A, Lu, X, Che, B, et al. The relationship between sexual activity and sexual attitudes among breast cancer survivors in China. Cancer Med. (2020) 9:3425–36. doi: 10.1002/cam4.2874
35. INEI. Instituto Nacional de Estadística e Informática. Encuesta Demográfica y de Salud Familiar 2018 - Nacional y Regional. Lima, Perú: INEI. (2018). Available at: https://www.inei.gob.pe/media/MenuRecursivo/publicaciones_digitales/Est/Lib1656/index1.html
36. INEI. Instituto Nacional de Estadística e Informática. Encuesta Demográfica y de Salud Familiar Encuesta Demográfica y de Salud Familiar 2017 - Nacional y Departamental. Lima, Perú: INEI. (2017). Available at: https://www.inei.gob.pe/media/MenuRecursivo/publicaciones_digitales/Est/Lib1525/
37. Madkour, AS, Farhat, T, Halpern, CT, Godeau, E, and Gabhainn, SN. Early adolescent sexual initiation as a problem behavior: a comparative study of five nations. J Adolesc Health. (2010) 47:389–98. doi: 10.1016/j.jadohealth.2010.02.008
38. Spriggs, AL, and Halpern, CT. Sexual debut timing and depressive symptoms in emerging adulthood. J Youth Adolesc. (2008) 37:1085–96. doi: 10.1007/s10964-008-9303-x
39. Jamieson, LK, and Wade, TJ. Early age of first sexual intercourse and depressive symptomatology among adolescents. J Sex Res. (2011) 48:450–60. doi: 10.1080/00224499.2010.509892
40. Heywood, W, Patrick, K, Smith, AMA, and Pitts, MK. Associations between early first sexual intercourse and later sexual and reproductive outcomes: a systematic review of population-based data. Arch Sex Behav. (2015) 44:531–69. doi: 10.1007/s10508-014-0374-3
41. Garcia, PJ, Benzaken, AS, and Galban, E. STI management and control in Latin America: where do we stand and where do we go from here? Sex Transm Infect. (2011) 87:ii7–9. doi: 10.1136/sextrans-2011-050177
42. Miller, HG, Cain, VS, Rogers, SM, Gribble, JN, and Turner, CF. Correlates of sexually transmitted bacterial infections among U.S. women in 1995. Fam Plan Perspect. (1999) 31:4–23. doi: 10.2307/2991550
43. Sanjose, S, Cortés, X, Méndez, C, Puig-Tintore, L, Torné, A, Roura, E, et al. Age at sexual initiation and number of sexual partners in the female Spanish population: results from the AFRODITA survey. Eur J Obstet Gynecol Reprod Biol. (2008) 140:234–40. doi: 10.1016/j.ejogrb.2008.04.005
44. Shrestha, R, Karki, P, and Copenhaver, M. Early sexual debut: a risk factor for STIs/HIV acquisition among a nationally representative sample of adults in Nepal. J Community Health. (2016) 41:70–7. doi: 10.1007/s10900-015-0065-6
45. Pinzón Fernández, MV, Mueses Marín, HF, and Galindo, QJ. Factores sociodemográficos, conocimientos y comportamientos relacionados con sífilis y VIH en población desplazada de Colombia. Rev cub salud pública. (2013) 39:474–88.
46. Olakunle, AA, and Banougnin, BH. Timing between age at first sexual intercourse and age at first use of contraception among adolescents and young adults in Niger: what role do education and place of residence play? Gates Open Res. (2019) 3:1463. doi: 10.12688/gatesopenres.12972.1
47. Newbern, EC, Miller, WC, Schoenbach, VJ, and Kaufman, JS. Family socioeconomic status and self-reported sexually transmitted diseases among black and white american adolescents. Sex Transm Dis. (2004) 31:533–41. doi: 10.1097/01.olq.0000137898.17919.35
48. Anguzu, G, Flynn, A, Musaazi, J, Kasirye, R, Atuhaire, LK, Kiragga, AN, et al. Relationship between socioeconomic status and risk of sexually transmitted infections in Uganda: multilevel analysis of a nationally representative survey. Int J STD AIDS. (2019) 30:284–91. doi: 10.1177/0956462418804115
49. Hailegebreal, S, Gilano, G, Seboka, BT, Sidelil, H, Awol, SM, Haile, Y, et al. Prevalence and associated factors of early sexual initiation among female youth in East Africa: further analysis of recent demographic and health survey. BMC Womens Health. (2022) 22:304. doi: 10.1186/s12905-022-01895-8
50. Ferede, TA, Muluneh, AG, Wagnew, A, and Walle, AD. Prevalence and associated factors of early sexual initiation among youth female in sub-Saharan Africa: a multilevel analysis of recent demographic and health surveys. BMC Womens Health. (2023) 23:147. doi: 10.1186/s12905-023-02298-z
51. de Salud, Ministerio, Centro Nacional de Epidemiología, Prevención y Control de Enfermedades. Boletín VIH. In: Situación epidemiológica del VIH-Sida en el Perú [Internet]. Perú: MINSA; CDC. (2021). Available at: https://www.dge.gob.pe/epipublic/uploads/vih-sida/vih-sida_20219_30_081256.pdf
52. INEI. Instituto Nacional de Estadística e Informática. Los estudiantes y su comportamiento reproductivo [Internet]. Lima, Perú: INEI (2015).
53. Young, H, Burke, L, and Nic, GS. Sexual intercourse, age of initiation and contraception among adolescents in Ireland: findings from the health behaviour in school-aged children (HBSC) Ireland study. BMC Public Health. (2018) 18:362. doi: 10.1186/s12889-018-5217-z
54. Zou, X, Chow, EP, Zhao, P, Xu, Y, Ling, L, and Zhang, L. Rural-to-urban migrants are at high risk of sexually transmitted and viral hepatitis infections in China: a systematic review and meta-analysis. BMC Infect Dis. (2014) 14:490. doi: 10.1186/1471-2334-14-490
55. Osuafor, GN, Maputle, S, Ayiga, N, and Mturi, AJ. Condom use among married and cohabiting women and its implications for HIV infection in Mahikeng. South Africa J Pop Res. (2018) 35:41–65. doi: 10.1007/s12546-017-9195-2
56. Olesen, TB, Jensen, KE, Nygård, M, Tryggvadottir, L, Sparén, P, Hansen, BT, et al. Young age at first intercourse and risk-taking behaviours--a study of nearly 65 000 women in four Nordic countries. Eur J Pub Health. (2012) 22:220–4. doi: 10.1093/eurpub/ckr055
57. Keetile, M, and Rakgoasi, SD. Factors associated with first heterosexual sex; sexual coercion and sexual risk behaviors among adolescents in Botswana. Sex Res Soc Policy. (2021) 18:261–70. doi: 10.1007/s13178-020-00454-w
58. O’Neal, EN, Decker, SH, Spohn, C, and Tellis, K. Condom use during sexual assault. J Forensic Legal Med. (2013) 20:605–9. doi: 10.1016/j.jflm.2013.03.023
59. Pulverman, CS, Kilimnik, CD, and Meston, CM. The impact of childhood sexual abuse on Women’s sexual health: a comprehensive review. Sex Med Rev. (2018) 6:188–200. doi: 10.1016/j.sxmr.2017.12.002
60. Karney, BR. Socioeconomic status and intimate relationships. Annu Rev Psychol. (2021) 72:391–414. doi: 10.1146/annurev-psych-051920-013658
61. Handebo, S. Sexually transmitted infections related care-seeking behavior and associated factors among reproductive age women in Ethiopia: further analysis of the 2016 demographic and health survey. BMC Womens Health. (2020) 20:274. doi: 10.1186/s12905-020-01145-9
62. James, C, Harfouche, M, Welton, NJ, Turner, KM, Abu-Raddad, LJ, Gottlieb, SL, et al. Herpes simplex virus: global infection prevalence and incidence estimates, 2016. Bull World Health Organ. (2020) 98:315–29. doi: 10.2471/BLT.19.237149
63. UNAIDS. Joint United Nations Programme on HIV and AIDS. Global HIV statistics [internet]. Fact sheets 2022. Geneva: UNAIDS. (2022). Available at: https://www.unaids.org/sites/default/files/media_asset/UNAIDS_FactSheet_en.pdf
64. International Agency for Research on Cancer. Cancer today [internet]. Available at: http://gco.iarc.fr/today/home
65. Chesson, HW, Spicknall, IH, Bingham, A, Brisson, M, Eppink, ST, Farnham, PG, et al. The estimated direct lifetime medical costs of sexually transmitted infections acquired in the United States in 2018. Sex Transm Dis. (2021) 48:215–21. doi: 10.1097/OLQ.0000000000001380
66. Shangase, N, Kharsany, ABM, Ntombela, NP, Pettifor, A, and McKinnon, LR. A systematic review of randomized controlled trials of school based interventions on sexual risk behaviors and sexually transmitted infections among Young adolescents in sub-Saharan Africa. AIDS Behav. (2021) 25:3669–86. doi: 10.1007/s10461-021-03242-8
67. Mmbaga, EJ, Kajula, L, Aarø, LE, Kilonzo, M, Wubs, AG, Eggers, SM, et al. Effect of the PREPARE intervention on sexual initiation and condom use among adolescents aged 12–14: a cluster randomised controlled trial in Dar Es Salaam, Tanzania. BMC Public Health. (2017) 17:322. doi: 10.1186/s12889-017-4245-4
68. Furlanetto, MF, Ghedin, DM, Gonçalves, TR, and Marin, AH. Individual and contextual factors associated with sexual initiation among adolescents. Psicol Reflex Crit. (2019) 32:25. doi: 10.1186/s41155-019-0138-z
69. Kassahun, EA, Gelagay, AA, Muche, AA, Dessie, AA, and Kassie, BA. Factors associated with early sexual initiation among preparatory and high school youths in Woldia town, Northeast Ethiopia: a cross-sectional study. BMC Public Health. (2019) 19:378. doi: 10.1186/s12889-019-6682-8
70. US Preventive Services Task Force. Behavioral counseling interventions to prevent sexually transmitted infections: US preventive services task force recommendation statement. JAMA. (2020) 324:674–81. doi: 10.1001/jama.2020.13095
71. Ford, K, and Lepkowski, JM. Characteristics of sexual partners and STD infection among American adolescents. Int J STD AIDS. (2004) 15:260–5. doi: 10.1258/095646204773557802
72. Aguirrebengoa, OA, Garcia, MV, Sanchez, MR, D’Elia, G, Méndez, BC, Arrancudiaga, MA, et al. Risk factors associated with sexually transmitted infections and HIV among adolescents in a reference clinic in Madrid. PLoS One. (2020) 15:e0228998. doi: 10.1371/journal.pone.0228998
73. Ong, JJ, Baggaley, RC, Wi, TE, Tucker, JD, Fu, H, Smith, MK, et al. Global epidemiologic characteristics of sexually transmitted infections among individuals using Preexposure prophylaxis for the prevention of HIV infection: a systematic review and Meta-analysis. JAMA Netw Open. (2019) 2:e1917134. doi: 10.1001/jamanetworkopen.2019.17134
Keywords: sexual behavior, health risk behaviors, sexually transmitted diseases, women’s health, Peru
Citation: Perez-Fernandez J, Arroyo-Velasco DO, Huaman MR, Chavez-Bustamante SG, Llamo-Vilcherrez AP, Delgado-Flores CJ and Toro-Huamanchumo CJ (2023) Association between early sexual initiation and sexually transmitted infections among Peruvian reproductive-age women. Front. Public Health. 11:1191722. doi: 10.3389/fpubh.2023.1191722
Edited by:
Mulong Du, Nanjing Medical University, ChinaReviewed by:
Junyi Xin, Nanjing Medical University, ChinaTadesse Nigussie, Mizan Tepi University, Ethiopia
Copyright © 2023 Perez-Fernandez, Arroyo-Velasco, Huaman, Chavez-Bustamante, Llamo-Vilcherrez, Delgado-Flores and Toro-Huamanchumo. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Carlos J. Toro-Huamanchumo, dG9ybzI5OTNAaG90bWFpbC5jb20=
 Jhosuny Perez-Fernandez1
Jhosuny Perez-Fernandez1 Sarai G. Chavez-Bustamante
Sarai G. Chavez-Bustamante Carlos J. Toro-Huamanchumo
Carlos J. Toro-Huamanchumo