- 1School of Public Health, Hubei University of Medicine, Shiyan, China,
- 2Center of Health Administration and Development Studies, Hubei University of Medicine, Shiyan, China
Background: The high multimorbidity and lower socioeconomic status (SES) of older adults, can lead to catastrophic health expenditures (CHEs) for older adults’ households. However, whether widowed older adults will bear such a financial burden has yet to be explored. The aim of this study was to investigate the influence of multimorbidity patterns and SES on CHE in Chinese widowed older adults.
Methods: Data was obtained from the 2018 China Health and Retirement Longitudinal Study (CHARLS). This is a cross-sectional study. A total of 1,721 widowed participants aged 60 years and older were enrolled in the study. Latent class analysis was performed based on 14 self-reported chronic diseases to identify multimorbidity patterns. The logistic model and Tobit model were used to analyze the influence of multimorbidity patterns and SES on the incidence and intensity of CHE, respectively.
Results: About 36.72% of widowed older adults generated CHE. The incidence and intensity of CHE were significantly higher in the cardiovascular class and multisystem class than in the minimal disease class in multimorbidity patterns (cardiovascular class, multisystem class, and minimal disease class). Among SES-related indicators (education, occupation and household per capita income), respondents with a middle school and above education level were more likely to generate CHE compared to those who were illiterate. Respondents who were in the unemployed group were more likely to generate CHE compared to agricultural workers. In addition, respondents aged 70–79 years old, geographically located in the east, having other medical insurance, or having fewer family members are more likely to generate CHE and have higher CHE intensity.
Conclusion: Widowed older adults are at high risk for CHE, especially those in the cardiovascular and multisystem disease classes, and those with low SES. Several mainstream health insurances do not provide significant relief. In addition, attention should be paid to the high-risk characteristics associated with CHE. It is necessary to carry out the popularization of chronic disease knowledge, improve the medical insurance system and medical service level, and provide more policy preferences and social support to widowed older adults.
Introduction
Catastrophic health expenditure (CHE) is generally defined as a household’s health expenditure as a percentage of total expenditure or income level reaching a threshold that has a catastrophic impact on the family’s financial situation and quality of life (1–3). The occurrence of CHE continues to increase worldwide. It has been demonstrated that the occurrence of CHE increased significantly in the 133 countries surveyed during the decade 2000 to 2010, regardless of which criteria was used to define CHE (4). This trend is much more pronounced in low- and middle-income countries, where health spending is growing at about 6% a year, 2% more than in high-income countries (5). Medical insurance systems in some low-income countries have achieved good results, such as China’s almost universal coverage (6), but due to the limited capital pool, it is difficult to fully protect the actual interests of the insured (7, 8). Studies have proved that the incidence of CHE in Chinese families is 13.9% (9) higher than some other countries, such as South Korea (10), Nepaland (11), and Bhutan (12). The proportion of OOP health expenditure in China’s total health expenditure is higher than the normal range defined by the WHO (13). It remains an important issue for China’s health authorities to provide more effective financial risk protection to its residents (14).
Multimorbidity refers to the occurrence of two or more chronic diseases in an individual at the same time (15), and it can share the same or different causes (16, 17), and has a significant negative impact on the health status, quality of life, and health expenditure of patients (18–21). Patients with multimorbidity have higher health expenditure than non-multimorbidity patients in developed countries, and already affect more than 60% of older adults (22, 23). Developing countries are not any exception. For example, nearly 70% of older adults in China suffer from multi-morbidity (24), and the medical complex service conditions required to treat multi-morbidity are a great challenge for the health care system (25, 26). Patients with different patterns of multimorbidity may have different care practices and health expenditures. Some scholars have used cluster analysis to cluster the information of chronic diseases of individuals (17, 27, 28), being aimed at better identify the potential categories of observed variables and conduct research on cognitive function, related outcomes, and related factors.
Contextual factors such as the physical characteristics of the environment, the sociocultural characteristics of the community and the accessibility of related services have some influence on health expenditure (29). When patients are under these adverse conditions, they may need to bear a greater risk of adverse health outcomes (30). Due to their lower socioeconomic status (SES), they have a lower economic level, and their money on medical and health services is likely to occupy a large proportion of their total household expenditure, thus generating CHE. In addition, the occurrence of CHE is associated with unequal socioeconomic status (e.g., employment, education, income), and subjects with CHE are more likely to be taken those with lower socioeconomic status (31, 32). Some SES factors, such as household income per capita, have been declared to have a significant impact on household CHE for older adults patients with chronic diseases. Equity in policies that reduce the incidence of CHE must be promoted by addressing socioeconomic factors that impact healthcare outcomes for older adults (33). The fairness of medical insurance design in China needs to be improved. For example, applying for the protection of the Medical Assistance program requires patients to have a certain level of health knowledge and be able to successfully fill out complex application forms, which disadvantage people of lower socioeconomic status (34, 35). It is therefore imperative to clarify differences in the equity of Medicare benefits and access to quality health services among patients of different socioeconomic status.
China holds the largest older adults population in the world (36). While the aging of the population is deepening, the widowed rate of older adults is also increasing. Depending upon the results of China’s seventh census, the number of older adults in China has reached 264 million, accounting for 18.70 percent of the total population. The number of widowed older adults has risen to 50 million, accounting for 18.9 percent of the total older adults population, an increase of nearly 2.6 million compared with 2010. The loss of a spouse is known as one of the most stressful events in human life (37), and its negative impact often involves the health status, economic level, quality of life and other aspects of the widowed person (38–41). Therefore, more attention should be paid to the economic burden of disease in widowed older adults, aiming to improve their quality of life in later life.
In this study, we aimed to evaluate multimorbidity patterns and the impact of SES on the incidence and intensity of CHE in widowed older adults in China. This is a cross-sectional study. The main challenge of this study is to identify the comorbidity pattern of widowed older adults in China and explore the influencing factors of CHE in widowed older adults. The main value and significance of this study is to provide a theoretical basis for the formulation of programs to alleviate the economic burden of diseases of widowed older adults, improve the quality of medical and health services, and perfect the medical insurance system, so as to promote the realization of healthy aging.
Methods
Data source
Data were obtained from the China Health and Retirement Longitudinal Study (CHARLS), a nationally representative longitudinal survey of Chinese adults aged 45 years and above (42). The baseline survey of CHARLS was undertaken in 2011, followed by four waves of surveys in 2013, 2015, and 2018. Electronic mapping software (GIS) was used to construct village-level sampling frame by mapping method, and multi-stage probability proportional to size (PPS) sampling was used. The survey covered 150 county-level units and 450 community-village level units in 28 provinces (autonomous regions and municipalities directly under the Central Government). The purpose of this study was to obtain relevant data on Chinese residents aged 45 and older, such as socio-demographic characteristics, family information, health status, medical insurance, work status, and medical service utilization of the respondents. CHARLS has received ethics approval from the Biomedical Ethics Review Board of Peking University (IRB0000105IRB 00001052–11015).
In this study, we used the data of CHARLS 2018, the fourth wave of its survey data, with a total of 19,816 respondents. Participants who met the required criteria (age 60 years and above, marital status as widowed, and complete information on chronic diseases and CHE related information) were included in the study, and 1,721 participants were finally included.
Measurement of catastrophic health expenditure (dependent variable)
The dependent variables in this study were the incidence and intensity of CHE. Build on previous research (31, 43–45), we measured CHE as out-of-pocket (OOP) medical expenses equal to or exceeding 40% of the family’s ability to pay (CTP). We included annual non-food household consumption expenditure as a measure of household ability to pay (CTP) to avoid measurement biases that may be missed by poor households (31, 46).
Annual household health expenditure was regarded as out-of-pocket (OOP) medical expenditure. We used pooled binary variables to determine the presence or absence of CHE in a participant’s household:
Among them, represents annual household health expenditure. The represents annual non-food household consumption expenditures, with z being 40% of the disaster threshold.
The strength of CHE indicates the extent to which OOP payments affect family life (47). It is expressed as CTP’s OOP payment proportion minus the threshold, calculated as follows:
Among them, represents the annual health expenditure cost of household i. is the non-food expenditure of household i and z is the catastrophe threshold of 40%.
Identification of multimorbidity patterns (independent variable)
The CHARLS 2018 survey collected information on whether participants had been diagnosed with any of the following 14 chronic conditions: hypertension, dyslipidemia, diabetes, cancer or malignant tumor, chronic lung disease, liver disease, heart disease, stroke, kidney disease, stomach and other digestive disease, emotional and psychiatric problems, memory-related disease, arthritis or rheumatism, and asthma. All the diseases were treated as dichotomous variables. LCA was used to identify multimorbidity patterns and to identify the category to which participants belonged.
SES indicators (independent variable)
SES measures used to represent the individual level include: education, occupation, and household per capita income. It has been shown that a higher level of education of an individual is associated with a lower frequency of use of medical services but a greater willingness to pay for medical services when needed (48, 49). Since the age of the subjects was not less than 60 years, we classified three levels of education: illiterate, primary school, middle school and above. The employment status and urban and rural residence of Chinese residents determine the type of medical insurance that individuals participate in. We categorized occupation types into four categories: agricultural work (at least 10 days of agricultural work in the past year and no other four categories of employment status were involved), non-agricultural work, retired (including early retirement, that is, people who quit before retirement age but enjoy the same benefits as normal retirement), and unemployed. Household per capita income is the average income of household members in the past 12 months.
Covariates
Covariates included in this study were: gender (male and female), age group (60–69 years, 70–79 years and ≥ 80 years), residence (urban and rural), geographic location (Northeast, East, central and West), type of health insurance [urban employee basic medical insurance (UEBMI), urban resident basic medical insurance (URBMI), new rural cooperative medical insurance (NRCMI), other MIs and no medical insurance (MI)], any financial support from family members or relatives and friends (yes or no), provision of any financial support to family members or relatives and friends (yes or no), difficulties in activities of daily living (ADL: eating, bathing, dressing, toileting, going to bed, and urinating; yes or no), and number of family members.
Introduction to logistic and Tobit model
Logistic regression model is one of the most important and widely used nonlinear statistical models to analyze dichotomous variables. In this model, the dependent variable is binary (y = 0 or y = 1), and the outcome variable has a nonlinear relationship with the independent variables. Tobit regression model is a kind of linear regression model, which is characterized by the truncation phenomenon of its dependent variable. Truncation means that some observations are not observed, that is, they are limited to a certain range of values. Tobit regression model can transform the truncated data into a probability model, and then perform statistical analysis on the truncated data.
Statistical analysis
Multimorbidity patterns as well as category affiliation of individuals were determined by performing LCA on chronic disease information from 1,721 participants. The use of LCA to identify case subclasses in multivariate categorical data can achieve excellent results (50). The statistical data and clinical significance of the various schemes were taken into account when selecting the best grouping of multimorbidity patterns.
Descriptive statistics were performed for each variable using the frequency distribution, and the differences between the two groups were compared using the chi-square test. Logistic regression model was used to analyze the influence of multimorbidity patterns and SES on the incidence of CHE. Tobit regression model was used to analyze the influence of multimorbidity patterns and SES on CHE intensity. CHE intensity was a continuous variable of no less than 0, and more than 60% of the participants had CHE intensity equal to 0, so the Tobit regression model applicable to the truncated data was utilized (51).
LCA was performed using Mplus version 8.3, and Stata version 16.0 was used for all statistical analyses. Two-sided p values of less than 0.05 were envisaged for indicate statistical significance.
Results
Sample characteristics
Of 1,721 participants, 73.39% were female. Most were in the 70–79 age group (39.45%), and more than four out of five (81.12%) lived in rural areas. About 6.16, 28.82, 28.82 and 36.20% of the subjects resided in northeastern, eastern, central and western China, respectively. Most participants (64.85%) were enrolled in NCRCMS. 89.77% received financial support from family members, and 50.49% provided financial support to family members. Nearly one-fifth (19.99%) of the subjects had difficulty in ADL. A total of 632 participants (36.72%) had CHE. The mean intensity of CHE was 0.108 with a standard deviation of 0.182 (Table 1).
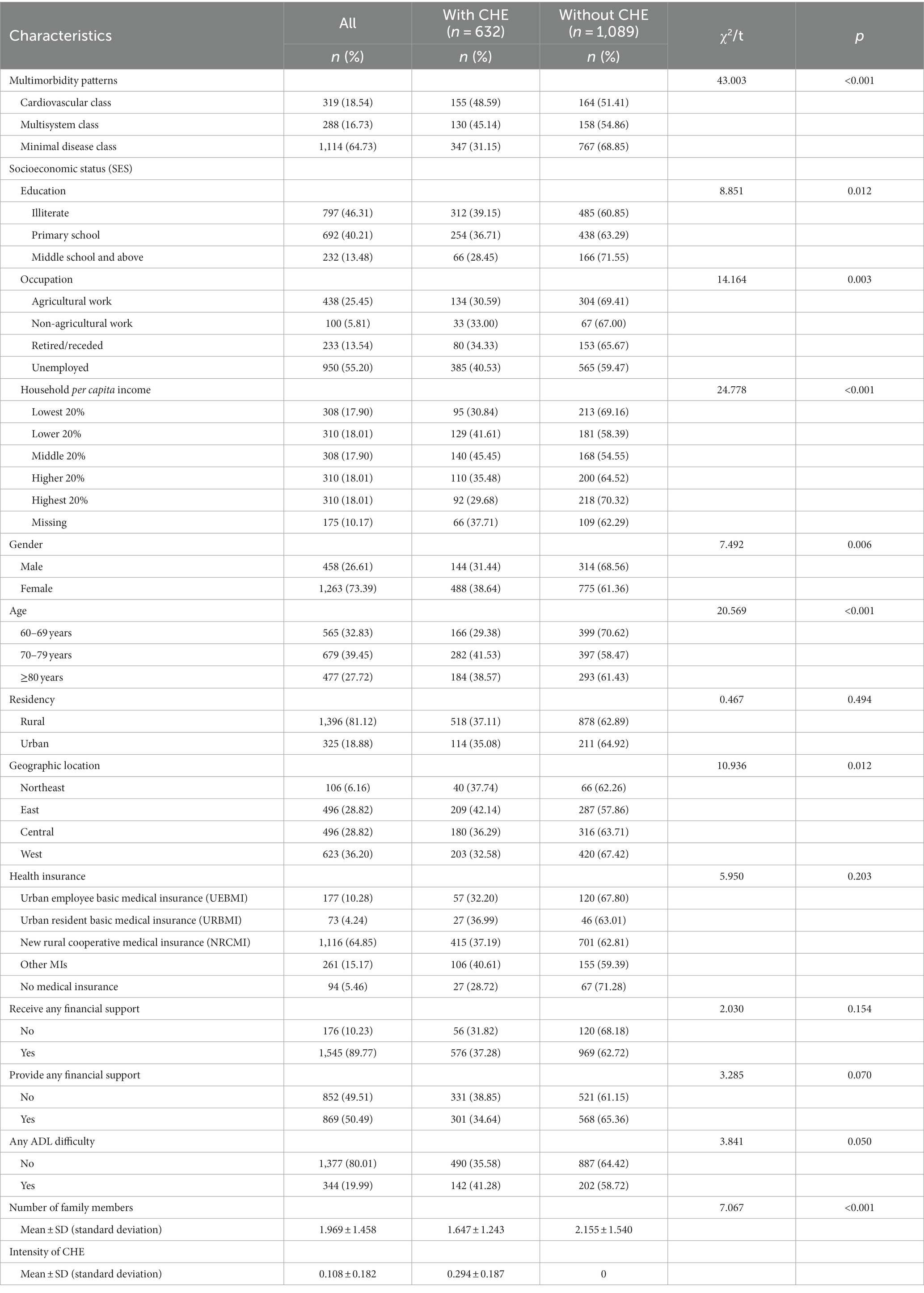
Table 1. Incidence of catastrophic health expenditure (CHE) by sociodemographic characteristics (n = 1,721).
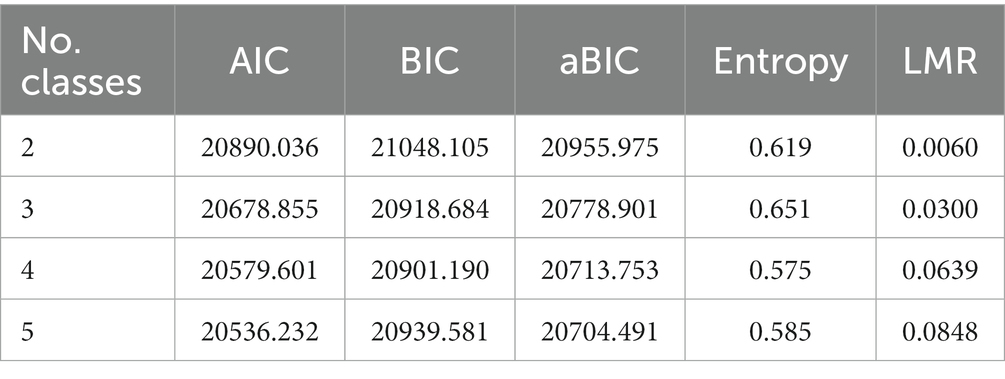
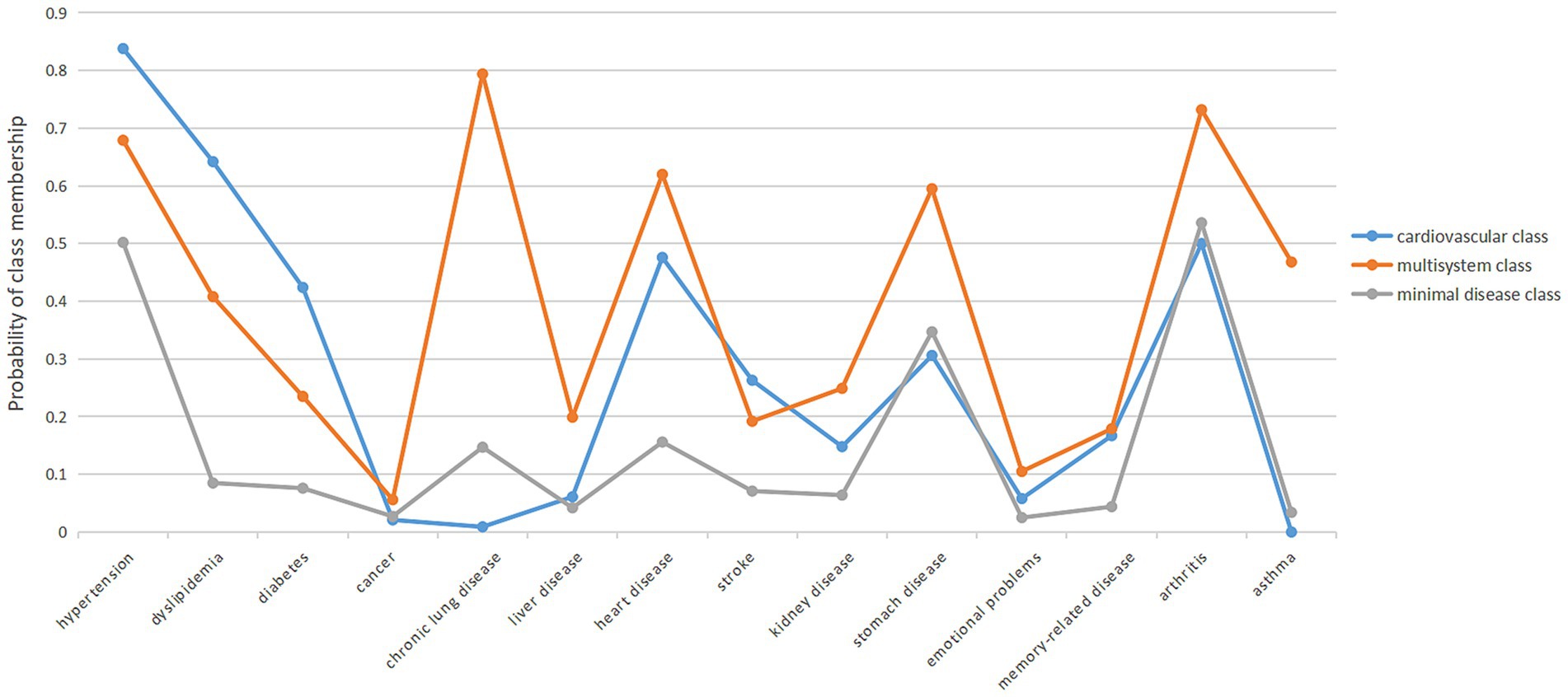
In identifying multimorbidity patterns, we examined class 2–5 models by LCA. The three-level model appeared to be the best-fitting model (Table 2) and showed the most reasonable clinical interpretability. Three patterns of multimorbidity were named cardiovascular class, multisystem class, and minimal disease class on the basis of the item-response probability as compared with the population average (Figure 1). The minimal disease class included relatively healthy participants with a low prevalence of 14 chronic diseases. The majority (64.73%) of the participants belonged to this pattern. The cardiovascular class includes individuals with a higher prevalence of hypertension, diabetes, heart attack, stroke, dyslipidemia, etc. About 18.54% of the participants were in the cardiovascular class. Participants in the multisystem class had a very high prevalence of 14 chronic conditions. Approximately 16.73% of the participants were in the multisystem class. In addition, the average number of chronic diseases in minimal disease class ranges is 1.781, the average number of chronic diseases in the cardiovascular class ranges is 4.282 and the average number of chronic diseases in the multisystem class ranges is 5.767.
Regarding the educational attainment of SES. Nearly half (46.31%) of the participants were illiterate. In terms of occupation type, more than half (55.20%) of the participants were unemployed. Participants who did not provide information on household income per capita were grouped into a single category. Whereas the others were divided into five equal groups from lowest to highest (Table 1).
Comparison of differences between the two groups
Gender (p = 0.006), age (p < 0.001), geographic location (p = 0.012), multimorbidity patterns (p < 0.001), education (p = 0.012), occupation (p = 0.003), household per capita income (p < 0.001) and number of family members (p < 0.001) were significant differences between the group with CHE and the group without CHE (Table 1). Among them, women have a higher incidence of CHE (38.64%). Participants with 70–79 years are more likely to develop CHE than other age groups (41.53%). Participants in the east are more likely to develop CHE than those in other regions (42.12%). Participants with fewer family members have a higher incidence of CHE. Participants in the cardiovascular disease group were more likely to develop CHE than those in other groups (48.59%). Illiterates were more likely to develop CHE than those with other levels of education (39.15%). Unemployed participants were more likely to develop CHE than those with other occupational types (40.53%). Participants with middle income were more likely to experience CHE than those with other incomes (45.45%).
Logistic regression results
We included the core independent variables, multimorbidity patterns and SES, in Model 1 and then further included all covariates in Model 2. The risk of CHE in the multi-system class and the cardiovascular class was significantly higher than that in the minimal disease class (p < 0.001). Specifically, subjects in the cardiovascular class were most likely to generate CHE (Model 1: OR = 2.134, 95% CI = 1.642–2.774; Model 2: OR = 2.025, 95%CI = 1.543–2.657), followed by multisystem class (Model 1: OR = 1.774, 95% CI = 1.355–2.323; Model 2: OR = 1.730, 95% CI = 1.308–2.290). In SES, education level of middle school and above was a protective factor for CHE (Model 1: OR = 0.621, 95% CI = 0.435–0.885; Model 2: OR = 0.669, 95% CI: 0.454–0.984), and unemployed occupation type presented a risk factor for CHE (Model 1: OR = 1.500, 95% CI = 1.170–1.923; Model 2: OR = 1.408, 95% CI: 1.075–1.844). In addition, the incidence of CHE was higher in participants aged 70 to 79 years, geographically located in the East, with other insurance type, or with a relatively small number of family members (p < 0.05, 0.01, or 0.001; Table 3).
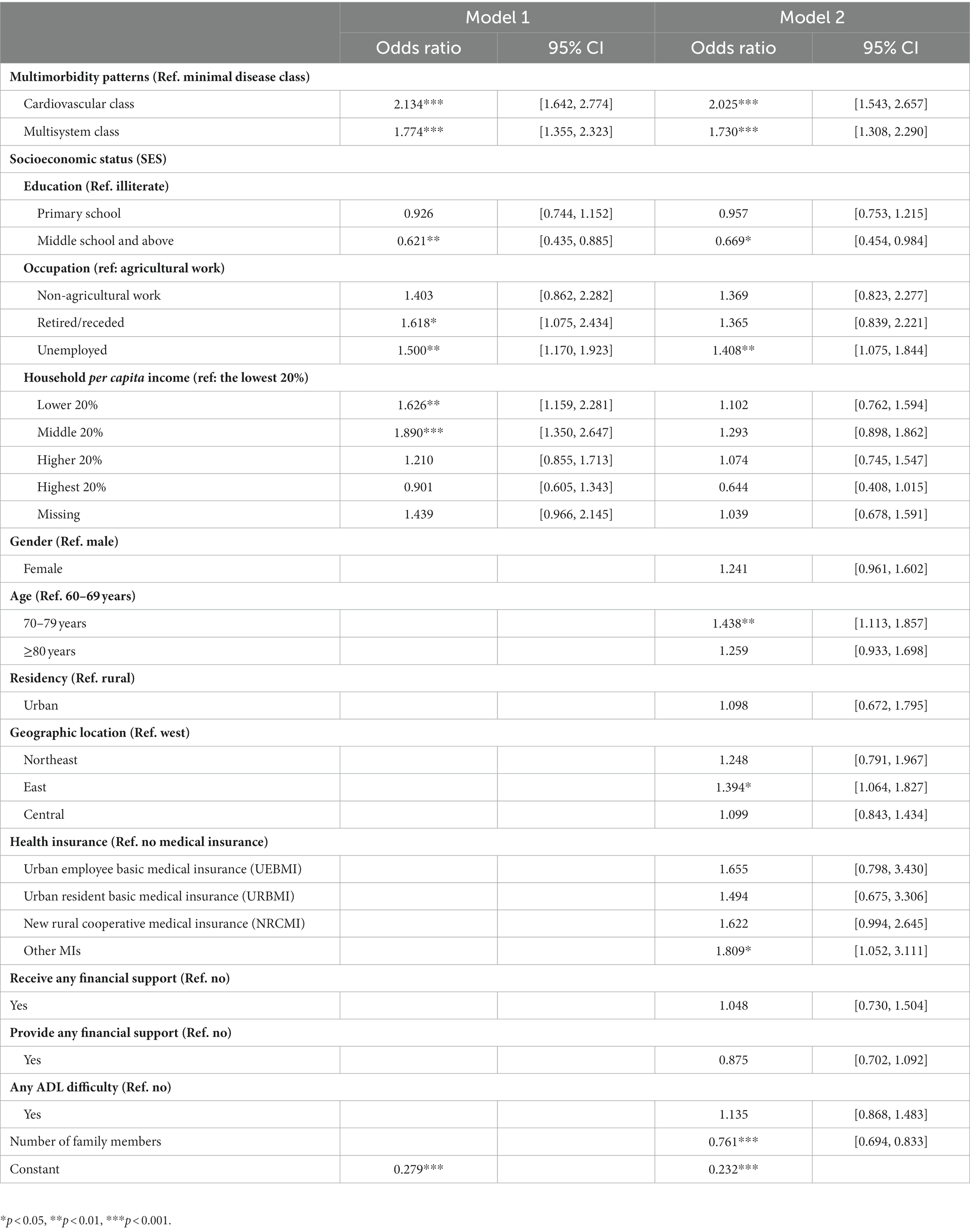
Table 3. Predictors of incidence of catastrophic health expenditure (CHE): results of logistic regression model.
Tobit regression results
Both Model 1 and Model 2 showed that the intensity of CHE of the cardiovascular class (Model 1: ME = 0.060, p < 0.001; Model 2: ME = 0.051, p < 0.001) and multi-system cluster (Model 1: ME = 0.057, p < 0.001; Model 2: ME = 0.053, p < 0.001) were significantly higher than that of the minimal disease group. In SES, Education level of middle school and above (Model 1: ME = −0.040, p < 0.01; Model 2: ME = −0.030, p < 0.05), and the unemployed (Model 1: ME = 0.031, p < 0.01; Model 2: ME = 0.024, p < 0.05) had a higher CHE intensity. In addition, CHE intensity was significantly higher among participants who aged 70–79 years, geographically located in the East, had UEBMI, NRCMI or other MIs, or who had a relatively small number of family members (p < 0.05, 0.01, or 0.001; Table 4).
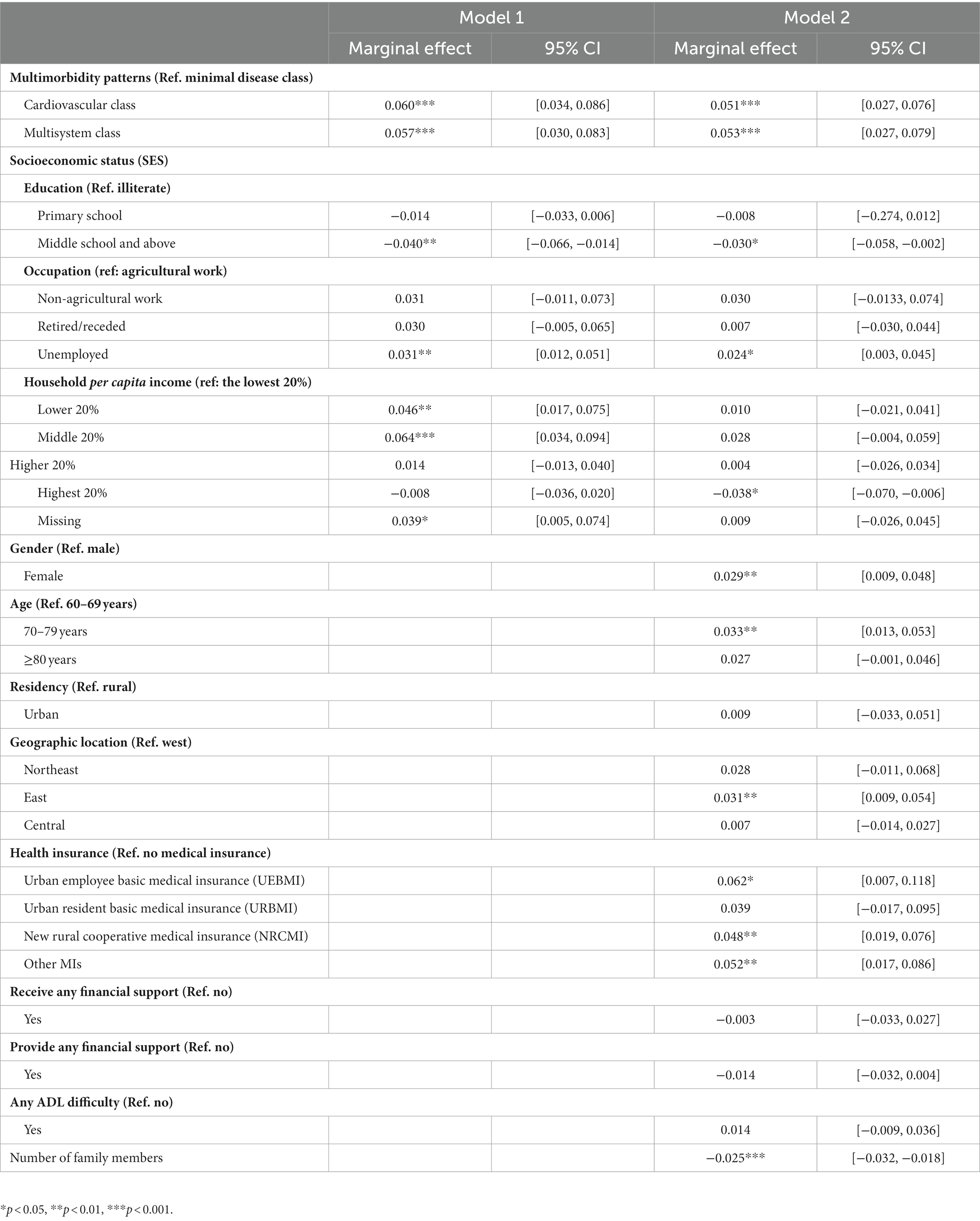
Table 4. Predictors of increasing the intensity of catastrophic health expenditure (CHE): results of Tobit regression model.
Additional information tables based on relevant results
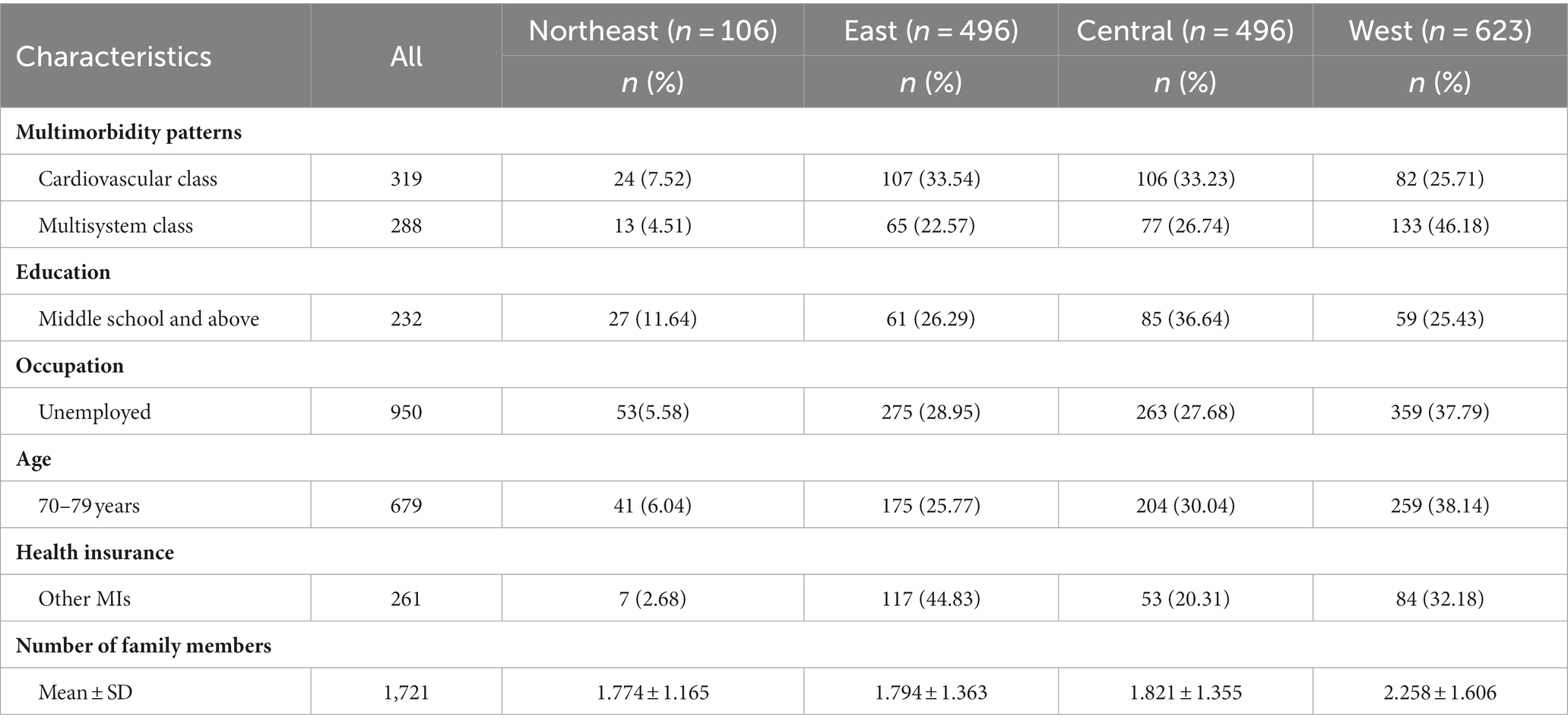
According to the logistic and Tobit regression results, we compared the characteristics of the target population with the regional characteristics. This statistical information serves to elucidate the relative position of the selected sample within the broader population spectrum, in order to provide some reference for the formulation of relevant policies (Table 5).
Discussion
This study used nationally representative CHARLS 2018 data to determine the incidence and intensity of CHE in widowed older adults in China, aiming to assess the status of multimorbidity patterns and SES influence on it. The results of this study have implications for clinical practice guidance and health policy formulation.
In this study, the incidence of CHE in widowed older adults was 36.72%, which was higher than 31.5% obtained by the study also using CHARLS 2018 data (52), and the intensity of CHE was 0.108, which was higher than the results of previous studies that did not fully focus on widowed older adults (53). This may be because the subjects of these two studies were older adults and adults, respectively, while this study narrowed the scope for older adults with widowed marital status. In addition, among the 1,721 participants in this study, 1,263 were female, accounting for about 73.39%, and 1,396 were rural residents, accounting for about 81.12%. China’s traditional family model, in which men outside the home, women inside, often still exists in these aging people, especially in rural areas (54). The death of the husband cuts off the main source of family income and reduces the economic level of widowed female older adults, which increases the possibility of CHE (39, 55–58). In addition, losing the care and companionship of a spouse is not conducive to physical and mental health, which may aggravate chronic diseases or lead to depression. In addition, China’s health resources tend to be in economically developed areas, and patients living in rural areas are therefore difficult to obtain the same level of health services (59). This may cause the deterioration of chronic diseases in rural patients with lower economic levels to be difficult to alleviate, thus making CHE occur through the continuous increase in health expenditure.
In this study, patterns of multimorbidity were identified from Chinese widowed older adults population, including the cardiovascular class, the multisystem class, and the minimal disease class. Among them, cardiovascular diseases are the biggest risk factors for CHE in subjects, followed by subjects with multi-system diseases, and they are also significant factors for the increase of CHE intensity. Studies have shown that the proportion of CHE in older adults with cardiovascular diseases in China exceeds that in developed countries, and the risk tolerance for medical payment is lower than the average level in China (60). Individuals with multiple chronic diseases are more apt to generate CHE (24). On the one hand, cardiovascular disease often requires long-term drug treatment and is a major contributor to the global economic burden of chronic diseases (61). In addition, cardiovascular diseases (such as hypertension, diabetes, and heart attacks) are associated with greater distress financing, leading households to be more inclined to borrow money or sell their property to be paid for related health costs (33, 62). On the other hand, expenditure on health care was positively correlated with the number of chronic diseases (33, 63–65), with participants in the multisystem class having higher expenditure on health care. Considering the economic level, mental status and other factors of widowed older adults, the families of patients in the cardiovascular class and the multisystem class are more likely to generate CHE and show higher CHE intensity values.
The present study found that the SES of widowed older adults people also affected the incidence and intensity of CHE in their families to some extent. There are related studies that also prove that CHE is related to SES (53, 66, 71). In this study, in terms of educational attainment, participants with middle school and above education had a lower probability of developing CHE. It may be because older adults with higher education level have stronger awareness of risk prevention, can effectively prevent the occurrence of chronic diseases (48), reduce their own economic burden of disease, and thus have a lower incidence of CHE. In terms of occupation type, CHE was more likely to occur in households of participants who were unemployed. It has been found that the families of unemployed older adults are more likely to generate CHE compared with agricultural workers, being consistent with the results of this study (67). The unemployed widowed older adults may have lost all economic sources. If there are no other family members in the family, the disease burden will bring significant negative effects on their economic level and quality of life, thus causing the occurrence of CHE. In terms of the number of family members, the higher the number, that is, the larger the household size, the lower the probability of CHE generation in older adults households. Similar studies have found that the family size of cancer patients is negatively correlated with the incidence of CHE (66), which is generally consistent with the results of this study. This may be due to the fact that more family members have more financial sources, daily care and spiritual support, and can effectively prevent and alleviate chronic diseases, so their incidence of CHE is lower.
This study showed that widowed older adults people aged 70–79 years, geographically located in the eastern region, and with other types of medical insurance were more likely to generate CHE, and the intensity of CHE is higher. There are regional differences in the allocation of medical and health resources in China, and the eastern regions with relatively developed economies have higher access to high-quality medical and health services (68). However, due to the low accessibility of medical and health services in other areas, it is therefore difficult to meet the medical service needs of patients, so that patients tend to produce a lower OOP medical expenditure (69, 70). China’s current medical insurance system has lowered the threshold for vulnerable groups to use medical and health services. However, it has not effectively alleviated the economic burden of disease of widowed older adults. When vulnerable groups can enter the threshold of medical and health services, OOP medical expenditure is generated. Even if this expenditure is relatively small, it has occupied a large proportion of the total family expenditure for them, which is likely to result in the occurrence of CHE and even produce high CHE intensity. It can be seen that China’s medical insurance system still have the shortcomings of insufficient policy protection in alleviating the economic burden of diseases in widowed older adults group.
Limitations and strengths
This study has certain limitations. First of all, the information on income, expenditure and chronic diseases in CHARLS data are self-reported, which may affect study results due to recall bias or undiagnosed chronic diseases. Second, the database used in this study did not include a large enough number of chronic diseases, which may affect the classification results of multimorbidity patterns. Third, the perspectives considered in this study are limited, and factors such as depression assessment and social capital can be incorporated into future studies. Fourth, this study utilized a cross-sectional design, and the conclusions are not causal.
This study also has certain strengths. First, LCA was used to identify the multimorbidity patterns of Chinese widowed older adults, which can provide a reference for the comprehensive treatment plan in clinical practice. Second, there are two indicators to measure CHE in this study, and logistic and Tobit regression are used to analyze the results separately, which makes the results robust. Thirdly, this study found out the characteristics of people who are more likely to develop CHE, which provides a basis for the government to formulate relevant plans to resist CHE risk.
Conclusion
According to nationally representative CHARLS 2018 data, we found that the incidence and intensity of CHE in widowed older adults were 36.72% and 0.108, respectively. Regarding multimorbidity patterns, we found that the incidence and intensity of CHE were higher in both the cardiovascular class and multisystem class than in the minimal disease class. Regarding SES, we found that the incidence and intensity of CHE were lower in the group with higher education level than in the illiterate group. The incidence and intensity of CHE were higher in unemployed than in agricultural workers. In addition, several mainstream medical insurance types did not effectively reduce the incidence and intensity of CHE, and those who chose other medical insurance had higher incidence and intensity of CHE than those who did not have medical insurance. Therefore, firstly, it is proposed to carry out the popularization of chronic disease knowledge on a large scale to prevent the occurrence of multimorbidity or slow down the deterioration of existing chronic diseases. Second, the amelioration and improvement of the medical insurance system and medical service institutions should increase the benefits to widowed older adults group, such as providing specific medical assistance plans for widowed older adults with cardiovascular diseases or multisystem diseases, and reasonably adjusting the detailed classification and payment scheme of the beneficiaries of medical insurance. Third, China’s health sector reform has achieved some results, but protecting vulnerable populations from health care-related poverty remains an ongoing challenge. Finally, relevant policies should also pay extra attention to groups of widowed older adults who have at least one of the following characteristics: the age range is 70–79 years, the geographical area belongs to the east, and the number of family members is small.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving human participants were reviewed and approved by the Biomedical Ethics Review Committee of Peking University (IRB0000105IRB00001052–11015). The patients/participants provided their written informed consent to participate in this study.
Author contributions
ZW conceived the idea, analyzed the data, and wrote the manuscript. ZZ provided advice on research methods and discussion of the manuscript. All authors contributed to the article and approved the submitted version.
Funding
The research was supported by supported by Key Research Center for Humanities and Social Sciences in Hubei Province (2022ZD002; Hubei university of Medicine) and Humanity and Social Science Youth Foundation of Ministry of Education of China (17YJCZH015).
Acknowledgments
The authors are sincerely grateful to the data source from China Health and Retirement Longitudinal Study (CHARLS).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Flores, G, Krishnakumar, J, O’Donnell, O, and van Doorslaer, E. Coping with health-care costs: implications for the measurement of catastrophic expenditures and poverty. Health Econ. (2008) 17:1393–412. doi: 10.1002/hec.1338
2. Duan, W, Zhang, W, Wu, C, Wang, Q, Yu, Y, Lin, H, et al. Extent and determinants of catastrophic health expenditure for tuberculosis care in Chongqing municipality, China: a cross-sectional study. BMJ Open. (2019) 9:e026638. doi: 10.1136/bmjopen-2018-026638
3. World Health Organization. Catastrophic health spending (and related indicators). (2022). Available at: https://www.who.int/data/gho/data/themes/topics/financial-protection/GHO/financial-protection.
4. Wagstaff, A, Flores, G, Hsu, J, Smitz, M-F, Chepynoga, K, Buisman, LR, et al. Progress on catastrophic health spending in 133 countries: a retrospective observational study. Lancet Glob Health. (2018) 6:e169–79. doi: 10.1016/S2214-109X(17)30429-1
5. WHO. Countries are spending more on health, but people are still paying too much out of their own pockets. (2019). Available at: https://www.who.int/news/item/20-02-2019-countries-are-spending-more-on-health-but-peopleare-still-paying-too-much-out-of-their-own-pockets (Accessed 2 September 2022).
6. Wei, S. Public health insurance and the labor market: evidence from China's urban resident basic medical insurance. Health Econ. (2020) 30:403–31. doi: 10.1002/HEC.4198
7. Liu, S, Coyte, PC, Fu, M, and Zhang, Q. Measurement and determinants of catastrophic health expenditure among elderly households in China using longitudinal data from the charls. Int J Equity Health. (2021) 20:62. doi: 10.1186/s12939-020-01336-8
8. Zhu, K, Zhang, L, Yuan, S, Zhang, X, and Zhang, Z. Health financing and integration ofurban and rural residents’ basic medical insurance systems in China. Int J Equity Health. (2017) 16:194. doi: 10.1186/s12939-017-0690-z
9. Wang, J, Tan, X, Qi, X, Zhang, X, Liu, H, Wang, K, et al. Minimizing the risk of catastrophic health expenditure in China: a multi-dimensional analysis of vulnerable groups. Front Public Health. (2021) 9:689809–9. doi: 10.3389/FPUBH.2021.689809
10. Jung, HW, Kwon, YD, and Noh, J-W. How public and private health insurance coverage mitigates catastrophic health expenditures in Republic of Korea. BMC Health Serv Res. (2022) 22:1042–2. doi: 10.1186/S12913-022-08405-4
11. Kumar, TA, and Raj, PA. National and provincial estimates of catastrophic health expenditure and its determinants in Nepal. J Nepal Health Res Counc. (2021) 18:741–6. doi: 10.33314/JNHRC.V18I4.2392
12. Jayendra, S, Milena, P, and Wim, G. Catastrophic health care expenditure and impoverishment in Bhutan. Health Policy Plan. (2022) 38:228–38. doi: 10.1093/HEAPOL/CZAC107
13. Ma, M, Li, Y, Wang, N, Wu, Q, Shan, L, Jiao, M, et al. Does the medical insurance system really achieved the effect of poverty alleviation for the middle-aged and elderly people in China? Characteristics ofvulnerable groups and failure links. BMC Public Health. (2020) 20:435. doi: 10.1186/s12889-020-08554-3
14. Di, Y, Yubraj, A, and Xiaoting, L. Social health insurance consolidation and urban-rural inequality in utilization and financial risk protection in China. Soc Sci Med. (2022) 308:115200–12. doi: 10.1016/J.SOCSCIMED.2022.115200
15. Van den Akker, M, Buntinx, F, and Knottnerus, JA. Comorbidity or multimorbidity: What’s in a name? A review of literature. Eur J Gen Pract. (1996) 2:65–70.
16. Olson, JE, Takahashi, PY, and Jennifer, M. Understanding the patterns of multimorbidity. Mayo Clin Proc. (2018) 93:824–5. doi: 10.1016/j.mayocp.2018.05.016
17. Zhang, Q, Han, X, Zhao, X, and Wang, Y. Multimorbidity patterns and associated factors in older Chinese: results from the China health and retirement longitudinal study. BMC Geriatr. (2022) 22:470–12. doi: 10.1186/S12877-022-03154-9
18. Garin, N, Olaya, B, Moneta, MV, Miret, M, Lobo, A, Ayuso-Mateos, JL, et al. Impact of multimorbidity on disability and quality of life in the spanish older population. PLoS One. (2014) 9:e111498. doi: 10.1371/journal.pone.0111498
19. Chen, H, Chen, Y, and Cui, B. The association of multimorbidity with healthcare expenditure among the elderly patients in Beijing, China. Arch Gerontol Geriatr Suppl. (2018) 79:32–8. doi: 10.1016/j.archger.2018.07.008
20. Gu, J, Chao, J, Chen, W, Xu, H, Zhang, R, He, T, et al. Multimorbidity and health-related quality of life among the community-dwelling elderly: a longitudinal study. Arch Gerontol Geriatr. (2018) 74:133–40. doi: 10.1016/j.archger.2017.10.019
21. Marengoni, A, Fratiglioni, L, and Onder, G. Improving public awareness of multimorbidity. J Am Med Dir Assoc. (2017) 18:372–3. doi: 10.1016/j.jamda.2017.01.010
22. Kingston, A, Robinson, L, Booth, H, Knapp, M, and Jagger, C, for the MODEM project. Projections of multi-morbidity in the older population in England to 2035: estimates from the population ageing and care simulation (PACSim) model. Age Ageing. (2018) 47:374–80. doi: 10.1093/ageing/afx201
23. Ofori-Asenso, R, Chin, KL, Curtis, AJ, Zomer, E, Zoungas, S, and Liew, D. Recent patterns of multimorbidity among older adults in high-income countries. Popul Health Manag. (2019) 22:127–37. doi: 10.1089/pop.2018.0069
24. Zhao, Q, Ji, J, Jiao, C, and Chang, J. Study on catastrophic health expenditure in families of chronic diseases patients. Health Econ Res. (2021) 2:7–10. doi: 10.14055/j.cnki.33-1056/f.2021.02.002
25. Wang, L, Si, L, Cocker, F, Palmer, AJ, and Sanderson, K. A systematic review of cost-of-illness studies of multimorbidity. Appl Health Econ Health Policy. (2018) 16:15–29. doi: 10.1007/s40258-017-0346-6
26. Cassell, A, Edwards, D, Harshfield, A, Rhodes, K, Brimicombe, J, Payne, R, et al. The epidemiology of multimorbidity in primary care: a retrospective cohort study. Br J Gen Pract. (2018) 68:e245–51. doi: 10.3399/bjgp18X695465
27. Nguyen, H, Chua, K-C, Dregan, A, Vitoratou, S, Bayes-Marin, I, Olaya, B, et al. Factors associated with multimorbidity patterns in older adults in England: findings from the English longitudinal study of aging (ELSA). J Aging Health. (2019) 32:1120–32. doi: 10.1177/0898264319891026
28. Bendayan, R, Zhu, Y, Federman, AD, and Dobson, RJB. Multimorbidity patterns and memory trajectories in older adults: evidence from the English longitudinal study of aging. J Gerontol A Biol Sci Med Sci. (2021) 76:867–75. doi: 10.1093/GERONA/GLAB009
29. Macintyre, S, Ellaway, A, and Cummins, S. Place effects on health: how can we conceptualise, operationalise and measure them? Soc Sci Med. (2002) 55:125–39. doi: 10.1016/S0277-9536(01)00214-3
30. Lantz, PM, Lynch, JW, House, JS, Lepkowski, JM, Mero, RP, Musick, MA, et al. Socioeconomic disparities in health change in a longitudinal study of US adults: the role of health-risk behaviors. Soc Sci Med. (2001) 53:29–40. doi: 10.1016/S0277-9536(00)00319-1
31. Zhonghua, W, Xiangjun, L, and Mingsheng, C. Catastrophic health expenditures and its inequality in elderly households with chronic disease patients in China. Int J Equity Health. (2015) 14:8. doi: 10.1186/s12939-015-0134-6
32. Mchenga, M, Chirwa, GC, and Chiwaula, LS. Impoverishing effects of catastrophic health expenditures in Malawi. Int J Equity Health. (2017) 16:25. doi: 10.1186/s12939-017-0515-0
33. Zhao, Y, Atun, R, Oldenburg, B, McPake, B, Tang, S, Mercer, SW, et al. Physical multimorbidity, health service use, and catastrophic health expenditure by socioeconomic groups in China: an analysis of population-based panel data. Lancet Glob Health. (2020) 8:e840–9. doi: 10.1016/S2214-109X(20)30127-3
34. Meng, Q, Fang, H, Liu, X, Yuan, B, and Xu, J. Consolidating the social health insurance schemes in China: towards an equitable and efficient health system. Lancet. (2015) 386:1484–92. doi: 10.1016/S0140-6736(15)00342-6
35. Sun, J, Deng, S, Xiong, X, and Tang, S. Equity in access to healthcare among the urban elderly in China: does health insurance matter? Int J Health Plann Manag. (2014) 29:e127–44. doi: 10.1002/hpm.2227
36. Chen, R, Xu, P, Song, P, Wang, M, and He, J. China has faster pace than Japan in population aging in next 25 years. Biosci Trends. (2019) 13:287–91. doi: 10.5582/bst.2019.01213
37. Holmes, TH, and Rahe, RH. The social readjustment rating scale. J Psychosom Res. (1967) 11:213–8. doi: 10.1016/0022-3999(67)90010-4
38. Lucas, RE, Clark, AE, Georgellis, Y, and Diener, E. Reexamining adaptation and the set point model of happiness: reactions to changes in marital status. J Pers Soc Psychol. (2003) 84:527–39. doi: 10.1037/0022-3514.84.3.527
39. Das, A. Spousal loss and health in late life. J Aging Health. (2013) 25:221–42. doi: 10.1177/0898264312464498
40. Kokou-Kpolou, CK, Adansikou, K, Park, S, Hajizadeh, S, Iorfa, SK, and Cénat, JM. Prolonged grief and posttraumatic growth among middle-aged and older widowed persons: a latent class analysis and testing for the role of social support. Death Stud. (2021) 46:1401–13. doi: 10.1080/07481187.2021.1978115
41. Yu, J, Kahana, E, Kahana, B, and Han, C. Depressive symptoms among elderly men and women who transition to widowhood: comparisons with long term married and long term widowed over a 10-year period. J Women Aging. (2019) 33:231–46. doi: 10.1080/08952841.2019.1685855
42. Zhao, YH, Hu, YS, Smith, JP, Strauss, J, and Yang, GH. Cohort profile: the China health and retirement longitudinal study (Charls). Int J Epidemiol. (2014) 43:61–8. doi: 10.1093/ije/dys203
43. Xu, Y, Zhou, Y, Pramono, A, Liu, Y, and Jia, C. A 25-year trend of catastrophic health expenditure and its inequality in China: evidence from longitudinal data. Risk Manage Healthc Policy. (2022) 15:969–81. doi: 10.21203/rs.3.rs-658127/v1
44. Vahedi, S, Rezapour, A, Khiavi, FF, Esmaeilzadeh, F, Javan-Noughabi, J, Almasiankia, A, et al. Decomposition of socioeconomic inequality in catastrophic health expenditure: an evidence from Iran. Clin Epidemiol Glob Health. (2020) 8:437–41. doi: 10.1016/j.cegh.2019.10.004
45. Si, Y, Zhou, Z, Su, M, Ma, M, Xu, Y, and Heitner, J. Catastrophic healthcare expenditure and its inequality for households with hypertension: evidence from the rural areas of Shaanxi Province in China. Int J Equity Health. (2017) 16:27. doi: 10.1186/s12939-016-0506-6
46. Wagstaff, A, and Doorslaer, E v. Catastrophe and impoverishment in paying for health care: with applications to Vietnam 1993-1998. Health Econ. (2003) 12:921–33. doi: 10.1002/hec.776
47. Saksena, P, Hsu, J, and Evans, DB. Financial risk protection and universal health coverage: evidence and measurement challenges. PLoS Med. (2014) 11:e1001701. doi: 10.1371/journal.pmed.1001701
48. Li, YN, Nong, DX, Wei, B, Feng, QM, and Luo, HY. The impact of predisposing, enabling, and need factors in utilization of health services among rural residents in Guangxi China. BMC Health Serv Res. (2016) 16:592. doi: 10.1186/s12913-016-1825-4
49. Pradhan, J, and Dwivedi, R. Do we provide affordable, accessible and administrable health care? An assessment of SES differential in out of pocket expenditure on delivery care in India. Sex Reprod Healthc. (2017) 11:69–78. doi: 10.1016/j.srhc.2016.10.006
50. Masyn, KE. Latent class analysis and finite mixture modeling In: TD Little, editor. The Oxford handbook of quantitative methods, Statistical analysis, vol. 2. Oxford: Oxford University Press (2013). 551–611.
52. Li, H, Chang, E, Zheng, W, Liu, B, Xu, J, Gu, W, et al. Multimorbidity and catastrophic health expenditure: evidence from the China health and retirement longitudinal study. Front Public Health. (2022) 10:1043189–9. doi: 10.3389/FPUBH.2022.1043189
53. Zhi, FX. The comparison of catastrophic health expenditure and its inequality between urban and rural households in China. Heal Econ Rev. (2022) 12:19. doi: 10.1186/S13561-022-00365-Z
54. Zhang, JN, and Shi, M. Research on influencing factors of rural labor transfer degree—based on the perspective of generation and gender differences. J Hebei Univ Econ Bus. (2022) 3:69–76. doi: 10.14178/j.cnki.issn1007-2101.20210416.004
55. Batista, MPP, Rebelo, JE, de Carvalho, RT, de Almeida, MHM, and Lancman, S. Widow's perception of their marital relationship and its influence on their restoration-oriented everyday occupations in the first six months after the death of the spouse: a thematic analysis. Aust Occup Ther J. (2019) 66:700–10. doi: 10.1111/1440-1630.12609
56. Bum, KY, and Hee, LS. Social network types and cognitive decline among older Korean adults: a longitudinal population-based study. Int J Geriatr Psychiatry. (2019) 34:1845–54. doi: 10.1002/gps.5200
57. Sommerlad, A, Ruegger, J, Singh-Manoux, A, Lewis, G, and Livingston, G. Marriage and risk of dementia: systematic review and meta-analysis of observational studies. J Neurol Neurosurg Psychiatry. (2017) 89:231–8. doi: 10.1136/jnnp-2017-316274
58. van der Houwen, K, Schut, H, van den Bout, J, Stroebe, M, and Stroebe, W. The efficacy of a brief internet-based self-help intervention for the bereaved. Behav Res Ther. (2010) 48:359–67. doi: 10.1016/j.brat.2009.12.009
59. Shen, S, and Hou, X. The integration goal of the fragmented social medical insurance system in China (in Chinese). Soc Sci Guangdong. (2012) 3:19–25. doi: 10.3969/j.issn.1000-114X.2012.03.002
60. Ma, M, Tian, W, Kang, J, Li, Y, Xia, Q, Wang, N, et al. Does the medical insurance system play a real role in reducing catastrophic economic burden in elderly patients with cardiovascular disease in China? Implication for accurately targeting vulnerable characteristics. Glob Health. (2021) 17:36–6. doi: 10.1186/S12992-021-00683-7
61. Mendoza-Herrera, K, Pedroza-Tobías, A, Hernández-Alcaraz, C, Ávila-Burgos, L, Aguilar-Salinas, CA, and Barquera, S. Attributable burden and expenditure of cardiovascular diseases and associated risk factors in Mexico and other selected mega-countries. Int J Environ Res Public Health. (2019) 16:4041–1. doi: 10.3390/ijerph16204041
62. Anshul, K, and Mohanty, SK. Disease-specific out-of-pocket and catastrophic health expenditure on hospitalization in India: do Indian households face distress health financing? PLoS One. (2018) 13:e0196106. doi: 10.1371/journal.pone.0196106
63. Picco, L, Achilla, E, Abdin, E, Chong, SA, Vaingankar, JA, McCrone, P, et al. Economic burden of multimorbidity among older adults: impact on healthcare and societal costs. BMC Health Serv Res. (2016) 16:173. doi: 10.1186/s12913-016-1421-7
64. McRae, I, Yen, L, Jeon, YH, Herath, PM, and Essue, B. Multimorbidity is associated with higher out-of-pocket spending: a study of older australians with multiple chronic conditions. Aust J Prim Health. (2013) 19:144–9. doi: 10.1071/PY12035
65. Bernardes, GM, Saulo, H, Fernandez, RN, Lima-Costa, MF, and Andrade, FB. Catastrophic health expenditure and multimorbidity among older adults in Brazil. Rev Saude Publica. (2020) 54:125. doi: 10.11606/s1518-8787.2020054002285
66. Deng, P, Fu, Y, Chen, M, and Si, L. Factors associated with health care utilization and catastrophic health expenditure among cancer patients in China: evidence from the China health and retirement longitudinal study. Front Public Health. (2022) 10:943271–1. doi: 10.3389/FPUBH.2022.943271
67. Chunyan, L, Belinda-Rose, Y, and Weiyan, J. Association of socioeconomic status with financial burden of disease among elderly patients with cardiovascular disease: evidence from the China health and retirement longitudinal survey. BMJ Open. (2018) 8:e018703. doi: 10.1136/bmjopen-2017-018703
68. Zhang, T, Xu, Y, Ren, J, Sun, L, and Liu, C. Inequality in the distribution of health resources and health services in China: hospitals versus primary care institutions. Int J Equity Health. (2017) 16:42. doi: 10.1186/s12939-017-0543-9
69. Towne, SD Jr, Liu, X, Li, R, Smith, ML, Maddock, JE, Tan, A, et al. Social and structural determinants of health inequities: socioeconomic, transportation-related, and provincial-level indicators of cost-related forgone hospital care in China. Int J Environ Res Public Health. (2021) 18:116113. doi: 10.3390/ijerph18116113
70. Zhang, X, Yang, S, and Zhang, X. Analysis of medical expenses of inpatients with diabetes: China’s eastern, central, and western regions (2013-2015). Public Health. (2020) 185:167–73. doi: 10.1016/j.puhe.2020.04.011
Keywords: catastrophic health expenditure, China, multimorbidity patterns, socioeconomic status, widowed older adults
Citation: Wang Z and Zeng Z (2023) Effects of multimorbidity patterns and socioeconomic status on catastrophic health expenditure of widowed older adults in China. Front. Public Health. 11:1188248. doi: 10.3389/fpubh.2023.1188248
Edited by:
Konstantinos Giannakou, European University Cyprus, CyprusReviewed by:
Maria Kyprianidou, European University Cyprus, CyprusSeyed Abolfazl Valizadeh, ETH Zurich, Switzerland
Hasan Yusefzadeh, Urmia University of Medical Sciences, Iran
Copyright © 2023 Wang and Zeng. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Zhi Zeng, emVuZ3poaUBoYm11LmVkdS5jbg==
 Zhen Wang
Zhen Wang Zhi Zeng1,2*
Zhi Zeng1,2*