
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
BRIEF RESEARCH REPORT article
Front. Public Health , 20 June 2023
Sec. Public Health Policy
Volume 11 - 2023 | https://doi.org/10.3389/fpubh.2023.1186429
This article is part of the Research Topic Fighting Against Vaccine Hesitancy: An Emerging Challenge for Public Health View all 26 articles
 Serena Barello1,2,3
Serena Barello1,2,3 Marta Acampora1,2*
Marta Acampora1,2* Michele Paleologo1,2
Michele Paleologo1,2 Lorenzo Palamenghi1,2,4
Lorenzo Palamenghi1,2,4 Guendalina Graffigna1,2,4
Guendalina Graffigna1,2,4Vaccine hesitancy became a more and more important issue during the COVID-19 pandemic. Due to the emergence of new variants, many international health agencies have already begun administering booster doses of the vaccine in response to these threats. Studies have emphasized the effectiveness of different types of incentive-based strategies to increase vaccination behaviors. The purpose of the present study was to identify the correlation between different types of incentives (legal or financial) with people’s intentions to get a COVID-19 booster vaccine. We conducted a cross-sectional study between 29 January 2022 and 03 February 2022. An online quantitative survey was carried out in Italy. One thousand and twenty-two Italian adults were recruited by a professional panel provider. Descriptive statistics were computed for the five variables concerning the incentives (monetary, tax, fee, health certification, travel) toward vaccination. A general linear model (GLM) was then computed to compare the scores of the five different variables within the subjects. The general linear model showed a significant within-subjects main effect. Post-hoc comparisons showed that among the financial incentive, the monetary reward is rated lower than all the others. Tax and fees both resulted lower than both the legal incentives. Finally, COVID-19 health certification and travel did not result significantly different from each other. This study offers an important contribution to public policy literature and to policymakers in their efforts to explain and steer booster vaccination acceptance while facing an ongoing pandemic.
Vaccine hesitancy, has become an increasingly important issue during the COVID-19 pandemic, to the extent that it was identified in 2019 by the World Health Organisation (1) as a major threat to global health. Due to the emergence of new variants, many international health agencies have already begun administering booster doses of the vaccine in response to these threats.
If vaccine acceptance has been a problem since the beginning of the pandemic, the administration of future booster shots could increase the hesitancy phenomenon, as studies have shown (2–8). As of 21st, July 2022 (at the time of writing this manuscript), only 107 million fully vaccinated people worldwide have received an additional vaccine dose or a booster dose, the highest level of protection against the virus.
Given these figures, the phenomenon of vaccine hesitancy will continue to be a serious threat to the end of the COVID-19 pandemic and for this reason it is necessary to investigate the mechanisms underlying this phenomenon by taking opportunity of large-scale vaccination due to the recent health emergency as a field of study.
Low vaccination intentions have been linked to people’s lack of trust in the safety of vaccines, complacency (seeing vaccination as largely unnecessary), calculativeness (carefully weighing risks and benefits), obstacles to vaccination, and low collective responsibility (e.g., unwillingness to get vaccinated to protect others) perceptions, according to previous research involving healthcare workers and the general population (9–12). Researchers have suggested a range of interventions, from informational campaigns to mandatory vaccination, for addressing these vaccine antecedents and boosting vaccination intentions (13–15). Offering incentives for vaccination could increase vaccination intentions in the same way that incentives have been demonstrated to encourage other healthy habits, such as keeping a healthier diet, stopping smoking, or doing physical exercise (16–18).
The literature (19–22) on this topic has emphasized the effectiveness of different types of incentive-based strategies to increase vaccination behaviours. Several studies (23–26) have shown how incentive-based strategies based on financial remuneration (e.g., monetary, bonus) in different countries have increased the acceptance of vaccines. Other studies (27–32) have also shown that the use of legal incentives linked to providing freedoms (e.g., the possibility to travel, the possibility to participate in public activities) are effective in promoting vaccination campaigns. However, vaccine hesitancy persists among certain population segments, necessitating further research into effective strategies for addressing this issue (33).
In this scenario, it is crucial to understand the effective approaches that can motivate the hesitant population to receive uptake doses of the COVID-19 vaccine, leveraging this health emergency as a field of study to gain a deeper understanding of vaccine hesitancy as a whole. Indeed, despite certain unique aspects related to COVID-19 (15), being against vaccine remains a significant barrier to COVID-19 vaccination (34). Therefore, effective strategies in this specific context may also prove effective in the future, presenting an opportunity to bridge the gap between scientific potential and citizen behavior.
Based on these premises, the purpose of the present study was to identify the correlation between different types of incentives (legal or financial) with people’s intentions to get a COVID-19 booster vaccine.
One thousand and twenty-two Italian adults were recruited by a professional panel provider (Norstat Italia Srl) by employing a stratified sampling. After providing their informed consent, the participants were asked to fill an online survey (using a CAWI methodology). The survey included questions regarding the participants’ sociodemographic status (gender, age, monthly family wage, level of education); one question regarding their COVID-19 vaccinal status, namely whether they did the booster dose, scheduled it, or did not do it nor scheduled it; and five questions regarding their intention to do an additional anti-COVID-19 vaccinal dose if an incentive were provided. Incentives were either financial (monetary, tax relief, or a fee in case of non-compliance), or legal (COVID-19 health certification, or freedom to travel). Participants were asked to rate their agreement on a 6 steps Likert scale (1 = strongly disagree, 6 = strongly agree).
Participants that did not do, nor scheduled the booster dose were excluded from the sample; the same goes for participants who refused to answer the question regarding their monthly wage.
First, frequencies were calculated for the sociodemographic characteristics of the sample. Descriptive statistics (mean, standard deviation, skewness and kurtosis) were computed for the five variables concerning the incentives towards vaccination. The scores for the five variables were also transformed in z-scores and screened for outliers (z ≥ |3|).
A general linear model (GLM) was then computed to compare the scores of the five different variables within the subjects. Gender, wage (coded as above and below the median of 1800€/month), and education (coded as no high school degree, high school degree, and university degree) were also included in the model as between-subjects variables. Interactions with the within-subject variable were also included in the model, but no interactions between the between-subject variables were computed. Mauchly’s test of sphericity was computed to verify the assumption of sphericity, and the appropriate correction was then applied to correct for the violated sphericity, depending on the resulting ε: Greenhouse–Geisser correction for <0.75 (35), and Huynh–Feldt correction for ε > 0.75 (36). Partial eta-squared (ηp2) was calculated as effect size for the F-tests. Post-hoc analyses were calculated, using the Holm-Bonferroni correction (37), to inspect pairwise differences between the different levels of the within-subject dependent variable in the overall sample, and -where an interaction resulted significant in the different levels of the independent variables; Cohen’s d was calculated as effect size for these comparisons.
All the analyses were run using JASP software v0.16.
This study has been performed in accordance with the Declaration of Helsinki and has been approved by an independent ethics commission of the Department of Psychology of Università Cattolica del Sacro Cuore in Milan (CERPS).
Two hundred and thirty-five participants were removed as they indicated that they did not do the recommended vaccination cycle, nor did they schedule it. Further 113 participants were removed as they showed missing data on the question regarding wage. The overall remaining sample was N = 674. The average age in the sample was 48 (SD = 13, range between 20 and 72). Table 1 shows the descriptive statistics of the sample: gender, geographical area of residence, education level, and family monthly wage. Descriptive statistics of the values of the intention of the sample to do an additional dose under the five different incentive type conditions (monetary, tax, fee, health certification and travel) were also conducted. As shown in Table 2, the results show that legal incentives are more endorsed than financial incentives by respondents. The screening of the outliers based on the z-scores showed that no outliers were present in the sample.
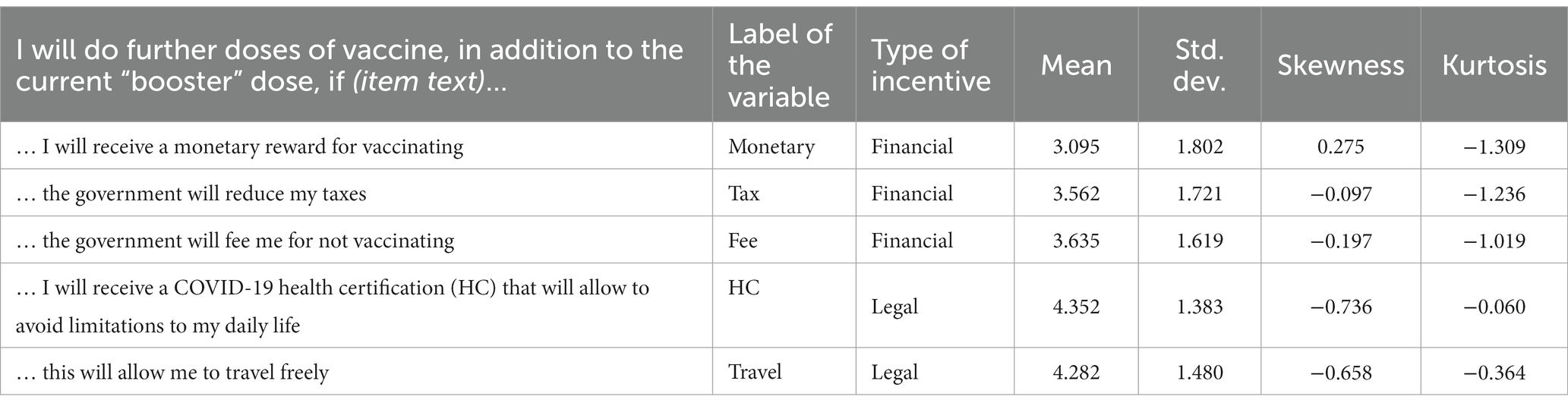
Table 2. Descriptive statistics of the values of the intention to do an additional dose under the five different conditions.
Mauchly’s test of sphericity resulted significant [χ2(9) = 326.230; p < 0.001; ε = 0.805]: Huyn–Feldt correction was then applied for the subsequent analyses.
The general linear model showed a significant within-subjects main effect [F(3.220, 2154.115) = 117.115; p < 0.001; ηp2 = 0.149]. Post-hoc comparisons (see Table 3) show that among the financial incentive, the monetary reward is rated lower than all the others with p < 0.001. Tax and Fee did not result significantly different from each other (with p = 0.396), but both resulted lower than both the legal incentives (i.e., health certification and travel) with p < 0.001. Finally, HC and Travel did not result significantly different from each other (with p = 0.307).
Additionally, a between-subjects main effect of the gender variable resulted significant [F(1, 669) = 8.647; p = 0.003; ηp2 = 0.013], with males having an overall mean of 0.283 (95% CI, 0.094, 0.472) above females. No significant main effect for wage (p = 0.971) and education (p = 0.637) emerged from analyses.
Finally, a marginally significant interaction gender × incentives resulted from analyses [F(3.220, 2154.115) = 4.368; p = 0.004; ηp2 = 0.006]. The post-hoc analyses (see Table 4) showed that there is a significant difference in the mean of the monetary incentive between the male and the female group, with males having a higher mean answer than female with p < 0.001. No other comparison resulted significant.
A marginally significant effect was also noted in the wage × incentives interaction [F(3.220, 2154.115) = 3.866; p = 0.007; ηp2 = 0.006]; however, post-hoc analyses showed no particular differences of interest of the dependent variables between the groups of people with higher or lower wages.
In this study, we investigated the effects of legal and financial incentives on COVID-19 booster dose vaccination intentions. Our results indicated that incentives are a suitable mean to motivate citizens to increase their willingness to get vaccinated even in the case of booster doses. Furthermore, we discovered that both types of incentives significantly relate with peoples’ willingness to vaccinate against COVID-19. However, for our sample, legal incentives—and in particular the introduction of vaccination health certificates required to access specific venues and being allowed to travel—were reported as the most effective incentive to boost vaccination intentions as indicated by other studies (25, 38, 39).
Our results are also in line with other studies that reported positive impacts of financial incentives on booster vaccination (23, 40, 41). Indeed, while vaccination mandates seem to be more likely to increase primary vaccination, incentives could be implemented to sustain booster uptake (42).
Indeed, as showed by other studies on the role of ethnicity in modifying the relationship between incentives and health behaviour change (43, 44), it is possible that for various populations and cultural backgrounds, the observed impacts of financial and legal incentives would differ. Thus, caution should be used when interpreting our findings. Additionally, several research advice considering the varying effects of rewards on persons with various motivations. According to the psychological literature, a person’s motivation levels may influence how they are influenced by the outside rewards that are given to them to increase their desire to carry out the requested behaviours (45–47). Evidence demonstrates that while typically highly motivated individuals are less influenced by external incentives (48), highly motivated individuals can occasionally be more susceptible to financial incentives than other individuals (49).
This study has some limitations, and results should be interpreted and used with caution. Firstly, the measures used in this study were self-reported and might be subject to reporting bias. In addition, the current study adopted a series of measures that were not validated—even if internal consistency was adequate. Second, as an observational cross-sectional study, causal relationships could not be inferred. Finally, there are indeed some socio-demographic variables that were not considered in this paper, and that is worth discussing. Despite its limitations, this study offers an important contribution to public policy literature and to policy makers in their efforts to explain and steer booster vaccination acceptance while facing an ongoing pandemic. Future research should explore the effects of other monetary and non-monetary types of incentives, as well as the interaction effect of incentive type and valence. Moreover other studies should estimate the impact of compulsory vaccine in acceptance rate and vaccine coverage (50, 51).
Based on results of this study, policymakers should consider incorporating common incentives into their vaccination promotion campaign, providing monetary incentives, and issuing health certifications—which permit access to public spaces and cultural events. Moreover, the social and cultural context of the intended vaccination target should be considered while designing these incentives.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by an independent ethics commission of the Department of Psychology of Università Cattolica del Sacro Cuore in Milan (CERPS). The patients/participants provided their written informed consent to participate in this study.
SB contributed to the conception and design of the study, methodology, and writing original draft. LP performed the statistical analysis. MA contributed to the methodology and preparation writing original draft. MP contributed to the methodology and data curation. GG supervised the research project and contributed to the writing, reviewing, and editing the manuscript. All authors contributed to the article and approved the submitted version.
This study was conducted within the CRAFT project, funded by Fondazione Cariplo and Regione Lombardia. The authors declare that the funders had no role in the study design, in interpretation of the results or in the decision to publish the results.
The authors wish to thank the study participants for their contribution to the research.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Thangaraju, P, and Venkatesan, S. Dünya Sağlık Örgütünün 2019’da küresel sağlığa tehdit ettiğini belirttiği on tehditten biri: Antimikrobiyal direnç. Cukurova Med J. (2019) 44:1150–1. doi: 10.17826/cumj.514157
2. Yadete, T, Batra, K, Netski, DM, Antonio, S, Patros, MJ, and Bester, JC. Assessing acceptability of COVID-19 vaccine booster dose among adult Americans: a cross-sectional study. Vaccine. (2021) 9:1424. doi: 10.3390/vaccines9121424
3. Hu, T, Li, L, Lin, C, Yang, Z, Chow, C, Lu, Z, et al. An analysis of the willingness to the COVID-19 vaccine booster shots among urban employees: evidence from a megacity H in eastern China. Int J Environ Res Public Health. (2022) 19:2300. doi: 10.3390/ijerph19042300
4. Klugar, M, Riad, A, Mohanan, L, and Pokorná, A. COVID-19 vaccine booster hesitancy (VBH) of healthcare workers in Czechia: national cross-sectional study. Vaccine. (2021) 9:1437. doi: 10.3390/vaccines9121437
5. Koh, SWC, Tan, HM, Lee, WH, Mathews, J, and Young, D. COVID-19 vaccine booster hesitancy among healthcare workers: a retrospective observational study in Singapore. Vaccine. (2022) 10:464. doi: 10.3390/vaccines10030464
6. Paul, E, and Fancourt, D. Predictors of uncertainty and unwillingness to receive the COVID-19 booster vaccine: an observational study of 22,139 fully vaccinated adults in the UK. Lancet Reg Health Eur. (2022) 14:100317. doi: 10.1016/j.lanepe.2022.100317
7. Qin, C, Wang, R, Tao, L, Liu, M, and Liu, J. Association between risk perception and acceptance for a booster dose of COVID-19 vaccine to children among child caregivers in China. Front Public Health. (2022) 10:834572. doi: 10.3389/fpubh.2022.834572
8. Wu, JH-C, Langford, B, Ha, R, Garber, G, Daneman, N, Johnstone, J, et al. Defining appropriate antibiotic prescribing in primary care: A modified Delphi panel approach. J Assoc Med Microbiol Infect Dis Can. (2020) 5:61–9. doi: 10.3138/jammi.2019-0023
9. Betsch, C, Schmid, P, Heinemeier, D, Korn, L, Holtmann, C, and Böhm, R. Beyond confidence: development of a measure assessing the 5C psychological antecedents of vaccination. PLoS One. (2018) 13:e0208601. doi: 10.1371/journal.pone.0208601
10. Falcon, M, Rodríguez-Blázquez, C, Romay-Barja, M, Ayala, A, Burgos, A, De Tena-Dávila, MJ, et al. COVID-19 vaccine hesitancy in Spain and associated factors. Front Public Health. (2023) 11:1129079. doi: 10.3389/fpubh.2023.1129079
11. Tomietto, M, Simonetti, V, Comparcini, D, Stefanizzi, P, and Cicolini, G. A large cross-sectional survey of COVID-19 vaccination willingness amongst healthcare students and professionals: reveals generational patterns. J Adv Nurs. (2022) 78:2894–903. doi: 10.1111/jan.15222
12. Barello, S, Maiorino, G, Palamenghi, L, Torri, C, Acampora, M, Gagliardi, L, et al. Exploring the motivational roots of getting vaccinated against COVID-19 in a population of vaccinated pediatric healthcare professionals: evidence from an Italian cross-sectional study. Vaccine. (2022) 10:467. doi: 10.3390/vaccines10030467
13. Betsch, C, Böhm, R, and Chapman, GB. Using behavioral insights to increase vaccination policy effectiveness. Policy Insights Behav Brain Sci. (2015) 2:61–73. doi: 10.1177/2372732215600716
14. Dubé, E, Gagnon, D, and MacDonald, NE. Strategies intended to address vaccine hesitancy: review of published reviews. Vaccine. (2015) 33:4191–203. doi: 10.1016/j.vaccine.2015.04.041
15. Singh, P, Dhalaria, P, Kashyap, S, Soni, GK, Nandi, P, Ghosh, S, et al. Strategies to overcome vaccine hesitancy: a systematic review. Syst Rev. (2022) 11:78. doi: 10.1186/s13643-022-01941-4
16. Notley, C, Gentry, S, Livingstone-Banks, J, Bauld, L, Perera, R, and Hartmann-Boyce, J. Incentives for smoking cessation. Cochrane Database Syst Rev. (2019) 7:CD004307. doi: 10.1002/14651858.CD004307.pub6
17. Wall, J, Mhurchu, CN, Blakely, T, Rodgers, A, and Wilton, J. Effectiveness of monetary incentives in modifying dietary behavior: a review of randomized, controlled trials. Nutr Rev. (2006) 64:518–31. doi: 10.1111/j.1753-4887.2006.tb00185.x
18. Laiou, E, Rapti, I, Schwarzer, R, Fleig, L, Cianferotti, L, Ngo, J, et al. Review: nudge interventions to promote healthy diets and physical activity. Food Policy. (2021) 102:102103. doi: 10.1016/j.foodpol.2021.102103
19. Lau, D, Hu, J, Majumdar, SR, Storie, DA, Rees, SE, and Johnson, JA. Interventions to improve influenza and pneumococcal vaccination rates among community-dwelling adults: a systematic review and Meta-analysis. Ann Fam Med. (2012) 10:538–46. doi: 10.1370/afm.1405
20. Weaver, T, Metrebian, N, Hellier, J, Pilling, S, Charles, V, Little, N, et al. Use of contingency management incentives to improve completion of hepatitis B vaccination in people undergoing treatment for heroin dependence: a cluster randomised trial. Lancet. (2014) 384:153–63. doi: 10.1016/S0140-6736(14)60196-3
21. Savulescu, J, Pugh, J, and Wilkinson, D. Balancing incentives and disincentives for vaccination in a pandemic. Nat Med. (2021) 27:1500–3. doi: 10.1038/s41591-021-01466-8
22. Rockliffe, L, Stearns, S, and Forster, AS. A qualitative exploration of using financial incentives to improve vaccination uptake via consent form return in female adolescents in London. PLoS One. (2020) 15:e0237805. doi: 10.1371/journal.pone.0237805
23. Iyer, G, Nandur, V, and Soberman, D. Vaccine hesitancy and monetary incentives. Humanit Soc Sci Commun. (2022) 9:81. doi: 10.1057/s41599-022-01074-y
24. Seal, K. A randomized controlled trial of monetary incentives vs. outreach to enhance adherence to the hepatitis B vaccine series among injection drug users. Drug Alcohol Depend. (2003) 71:127–31. doi: 10.1016/S0376-8716(03)00074-7
25. Klüver, H, Hartmann, F, Humphreys, M, Geissler, F, and Giesecke, J. Incentives can spur COVID-19 vaccination uptake. Proc Natl Acad Sci U S A. (2021) 118:e2109543118. doi: 10.1073/pnas.2109543118
26. Munzert, S, Selb, P, Gohdes, A, Stoetzer, LF, and Lowe, W. Tracking and promoting the usage of a COVID-19 contact tracing app. Nat Hum Behav. (2021) 5:247–55. doi: 10.1038/s41562-020-01044-x
27. Wilf-Miron, R, Myers, V, and Saban, M. Incentivizing vaccination uptake: the “green pass” proposal in Israel. JAMA. (2021) 325:1503–4. doi: 10.1001/jama.2021.4300
28. Eshun-Wilson, I, Mody, A, Tram, KH, Bradley, C, Sheve, A, Fox, B, Thompson, V, and Geng, E. H.. Preferences for COVID-19 vaccine distribution strategies in the US: A discrete choice survey. PLoS One. (2021) 16:e0256394. doi: 10.1101/2021.05.19.21257355
29. Shmueli, L. The role of incentives in deciding to receive the available COVID-19 vaccine in Israel. Vaccine. (2022) 10:77. doi: 10.3390/vaccines10010077
30. Barello, S, Paleologo, M, Palamenghi, L, Acampora, M, and Graffigna, G. Public perceptions of harms and benefit of COVID-19 immunity certificate: a cross-sectional study in the Italian setting. Vaccine. (2022) 10:1501. doi: 10.3390/vaccines10091501
31. Barello, S, Acampora, M, Paleologo, M, Schiavone, L, Anderson, G, and Graffigna, G. Public views on the COVID-19 immunity certificate: a scoping review. Health Expect. (2022) 25:2645–57. doi: 10.1111/hex.13589
32. Lamiani, G, Barello, S, Browning, DM, Vegni, E, and Meyer, EC. Uncovering and validating clinicians’ experiential knowledge when facing difficult conversations: a cross-cultural perspective. Patient Educ Couns. (2012) 87:307–12. doi: 10.1016/j.pec.2011.11.012
33. Bussink-Voorend, D, Hautvast, JLA, Vandeberg, L, Visser, O, and Hulscher, MEJL. A systematic literature review to clarify the concept of vaccine hesitancy. Nat Hum Behav. (2022) 6:1634–48. doi: 10.1038/s41562-022-01431-6
34. Wiysonge, CS, Ndwandwe, D, Ryan, J, Jaca, A, Batouré, O, Anya, B-PM, et al. Vaccine hesitancy in the era of COVID-19: could lessons from the past help in divining the future? Hum Vaccin Immunother. (2021) 18:1–3. doi: 10.1080/21645515.2021.1893062
36. Huynh, H, and Feldt, LS. Estimation of the box correction for degrees of freedom from sample data in randomized block and split-plot designs. J Educ Stat. (2023) 1:69–82. doi: 10.3102/10769986001001069
38. Mills, MC, and Rüttenauer, T. The effect of mandatory COVID-19 certificates on vaccine uptake: synthetic-control modelling of six countries. Lancet Public Health. (2022) 7:e15–22. doi: 10.1016/S2468-2667(21)00273-5
39. Oliu-Barton, M, Pradelski, BSR, Woloszko, N, Guetta-Jeanrenaud, L, Aghion, P, Artus, P, et al. The effect of COVID certificates on vaccine uptake, health outcomes, and the economy. Nat Commun. (2022) 13:3942. doi: 10.1038/s41467-022-31394-1
40. Campos-Mercade, P, Meier, AN, Schneider, FH, Meier, S, Pope, D, and Wengström, E. Monetary incentives increase COVID-19 vaccinations. Science. (2021) 374:879–82. doi: 10.1126/science.abm0475
41. Robertson, E, Reeve, KS, Niedzwiedz, CL, Moore, J, Blake, M, Green, M, et al. Predictors of COVID-19 vaccine hesitancy in the UK household longitudinal study. Brain Behav Immun. (2021) 94:41–50. doi: 10.1016/j.bbi.2021.03.008
42. Sprengholz, P, Henkel, L, Böhm, R, and Betsch, C. Different interventions for different vaccinations? Effects of psychological factors and health policies on COVID-19 primary and booster vaccine uptake. PsyArXiv22. [Epub ahead of preprint], doi: 10.31234/osf.io/xsh48
43. Chaturvedi, N. Ethnicity as an epidemiological determinant— crudely racist or crucially important. Int J Epidemiol. (2001) 30:925–7. doi: 10.1093/ije/30.5.925
44. Egede, LE. Financial incentives to improve glycemic control in African American adults with type 2 diabetes: a pilot randomized controlled trial. BMC Health Serv Res. (2021) 21:1–9. doi: 10.1186/s12913-020-06029-0
45. Frey, BS, and Oberholzer-Gee, F. The cost of Price incentives: an empirical analysis of motivation crowding-out. Am Econ Rev. (1997) 87:746–55.
46. Frey, BS, and Jegen, R. Motivation crowding theory: a survey of empirical evidence. SSRN J. (2000). doi: 10.2139/ssrn.203330
47. Lohmann, J, Houlfort, N, and De Allegri, M. Crowding out or no crowding out? A self-determination theory approach to health worker motivation in performance-based financing. Soc Sci Med. (2016) 169:1–8. doi: 10.1016/j.socscimed.2016.09.006
48. Underhill, K. When extrinsic incentives displace intrinsic motivation: designing legal carrots and sticks to confront the challenge of motivational crowding-out. Yale J Regul. (2016) 33:69.
49. Silvi, M, and Padilla, E. Pro-environmental behavior: social norms, intrinsic motivation and external conditions. Environ Policy Gov. (2021) 31:619–32. doi: 10.1002/eet.1960
50. Kuznetsova, L, Diago-Navarro, E, Mathu, R, and Trilla, A. Effectiveness of COVID-19 vaccination mandates and incentives in Europe. Vaccine. (2022) 10:1714. doi: 10.3390/vaccines10101714
Keywords: booster vaccination, COVID-19 vaccine, monetary incentive, legal incentives, vaccination intention, public health policy
Citation: Barello S, Acampora M, Paleologo M, Palamenghi L and Graffigna G (2023) Providing freedom or financial remuneration? A cross-sectional study on the role of monetary and legal incentives on COVID-19 further booster vaccination intention in the Italian context. Front. Public Health. 11:1186429. doi: 10.3389/fpubh.2023.1186429
Received: 14 March 2023; Accepted: 06 June 2023;
Published: 20 June 2023.
Edited by:
Pasquale Stefanizzi, University of Bari Aldo Moro, ItalyReviewed by:
Nami Mohammadian Khonsari, Alborz University of Medical Sciences, IranCopyright © 2023 Barello, Acampora, Paleologo, Palamenghi and Graffigna. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Marta Acampora, bWFydGEuYWNhbXBvcmFAdW5pY2F0dC5pdA==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.