
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
REVIEW article
Front. Public Health, 18 July 2023
Sec. Life-Course Epidemiology and Social Inequalities in Health
Volume 11 - 2023 | https://doi.org/10.3389/fpubh.2023.1183284
This article is part of the Research TopicInsights in Gender, Sex and Sexualities: 2022View all 14 articles
Gender identity and sexual orientation are determinants of health that can contribute to health inequities. In the 2SLGBTQIA+ community, belonging to a sexual and/or gender minority group leads to a higher risk of negative health outcomes such as depression, anxiety, and cancer, as well as maladaptive behaviors leading to poorer health outcomes such as substance abuse and risky sexual behavior. Empirical evidence suggests that inequities in terms of accessibility to health care, quality of care, inclusivity, and satisfaction of care, are pervasive and entrenched in the health care system. A better understanding of the current Canadian health care context for individuals of the 2SLGBTQIA+ community is imperative to inform public policy and develop sensitive public health interventions to make meaningful headway in reducing inequity. Our search strategy was Canadian-centric and aimed at highlighting the current state of 2SLGBTQIA+ health inequities in Canada. Discrimination, patient care and access to care, education and training of health care professionals, and crucial changes at the systemic and infrastructure levels have been identified as main themes in the literature. Furthermore, we describe health care-related disparities in the 2SLGBTQIA+ community, and present available resources and guidelines that can guide healthcare providers in narrowing the gap in inequities. Herein, the lack of training for both clinical and non-clinical staff has been identified as the most critical issue influencing health care systems. Researchers, educators, and practitioners should invest in health care professional training and future research should evaluate the effectiveness of interventions on staff attitudinal changes toward the 2SLGBTQIA+ community and the impact on patient outcomes.
The determinants of health encompass personal, social, economic, and environmental factors that determine health, such as income and social status, employment and working conditions, education and literacy, childhood experiences, access to health services, racism, culture, biology and genetic endowment, age, sexual orientation, and gender identity (1, 2). Certain health determinants can contribute to health inequities by inciting discriminatory and/or intolerant behaviors. The acronym 2SLGBTQIA+ (Two-Spirit, Lesbian, Gay, Bisexual, Transgender/Trans, Queer/Questioning, Intersexual, Asexual/Aromantic/Agender and all others) is used to describe sexual and gender minorities (3). Individuals of sexual and/or gender minority are often faced with higher rates of adverse health outcomes when compared to the general population; this includes suicide, anxiety, cancer, obesity, and arthritis (4). They are also more likely to engage in harmful health behaviors, such as substance use and risky sexual conduct (4).
2SLGBTQIA+ health disparities can be explained by minority stress theory (5) which postulates that high levels of chronic stress brought on by enacted and/or anticipated stigmatization and discrimination, as well as internalized cis-hetero-normativity (i.e., the presumption that all individuals are inherently cis-gendered and heterosexual) are detrimental to health (6–9). This chronic stress directly impacts physical and psychosocial health and drives avoidance behaviors that impact health. The health of 2SLGBTQIA+ individuals has often been compromised by stigmatization, discrimination, a lack of visibility, and a lack of cultural competency in the health care system (10–21). In addition, the notion of intersectionality explains how 2SLGBTQIA+ individuals may be confronted with multiple interlinked forms of discrimination like cis-hetero-normativity, agism, ableism and racism, that when combined, increase vulnerability to health inequities and lead to inferior clinical outcomes (22–25). In other words, the health equity gap widens increasingly.
Importantly, these risk factors are modifiable when proper action is taken to address them. This involves adequate education for health care professionals (HCP) in matters of 2SLGBTQIA+ specific health needs, cultural competency, and implicit bias training, as well as resolving systemic discrimination and lack of inclusivity within the health care system. The main goal of this review is to present succinct and up-to-date information on the current state of 2SLGBTQIA+ health inequities in Canada. Specific objectives were to (i) present known factors associated with health disparities in the 2SLGBTQIA+ community and (ii) identify existing resources that can be used by Canadian health care institutions to address inequities and therefore, ameliorate the health outcomes of the 2SLGBTQIA+ community. Discrimination, patient care, and access to care, education and training of HCP, and crucial changes at the systemic and infrastructure levels have been identified as main themes in the literature. They will be discussed throughout this review.
Access to quality health care is a fundamental right that is not always extended to the 2SLGBTQIA+ community because of individual and systemic discrimination. Discriminatory attitudes from HCP are a major problem in the health care system (26–29). Notably, refusal to administer treatment and medication and delaying treatments for 2SLGBTQIA+ individuals are striking examples of individual discrimination by HCP (15, 17, 30–36). Contrastingly to these reports of misconduct, studies have demonstrated an increase in explicitly positive attitudes toward the 2SLGBTQIA+ community from nursing staff and physicians over time (12–14, 37–39). However, despite this rise in explicit positive attitudes, patients remain victims of stigma, discrimination and are denied their civil and human rights (11, 40). It is thus important to distinguish between implicit and explicit biases; even when HCP are committed to providing equal care, this can be undermined by implicit biases operating unconsciously (41–46). These psychological biases are described as the nonconscious or implicit prejudice and stereotypes health care providers hold without knowing it. Even when HCP are committed to providing equitable care, some evidence supports that implicit biases can impact health care providers’ judgment and behavior when interacting with patients from the 2SLGBTQIA+ community (40).
Discrimination is also found at the systemic level, in forms, processes, language used, medical records, and the physical environment, exacerbating the discriminatory experience within the health care system (4, 47, 48). This leads to delayed treatment, which inevitably has a damaging impact on health (13, 14, 30–33, 36, 49–53). Furthermore, general apprehension and being cognizant of the negative impact that divulgation may have on health leads to non-disclosure of sexual orientation and/or gender identity. Although non-disclosure protects patients from prejudice short term, it has a detrimental impact on health long term, more specifically, on patient care, health, and satisfaction of care (10, 15, 36, 50, 52, 54, 55). Hence, patients are put in a lose-lose situation created by an inequitable health care system that ultimately contributes to health disparities. Stigma and discrimination also lead to unfair access to social and material resources auxiliary to good health like employment, income, housing, education and health care (56). For example, the Trans PULSE Project (a community-based research project that investigated the impact of social exclusion and discrimination on the health of 2SLGBTQIA+ people in Ontario, Canada) found that 40 and 45% of the transgender population surveyed had low-income and un-met health needs, respectively, and bisexual folks experienced food insecurities at double the rate of their heterosexual counterparts (57). These disparities are further exacerbated by race, socio-economic status, gender, and sexual orientation through an intersectional lens (24). These findings can be explained by the intersectionality theory, where the intersection of social health determinants have a compounding impact on health (25). As shown in Figure 1, this theory is often used to correct for health determinants that would otherwise be analyzed separately to assess their direct impact on health instead of looking at how they interact together. In reality, various determinants interact together and compound the impact on an individual’s health. Many studies in this review have illustrated this phenomenon in the 2SLGBTQIA+ community in Canada, where sexual or gender minority status will have an influence on other health determinants directly or indirectly and ultimately impact health.
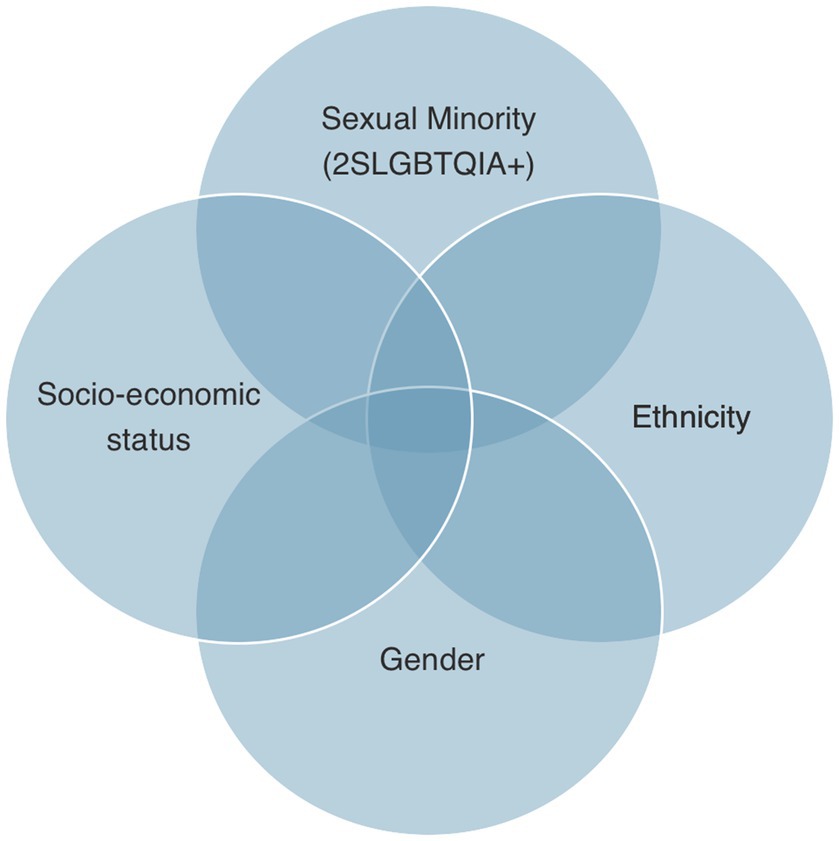
Figure 1. The intersectionality of social determinants of health to illustrate the compounding impact on health disparities.
The minority stress framework posits that 2SLGBTQIA+ individuals are subject to stressors that have a pernicious effect on physical and psychosocial health (58, 59). Notably, the 2SLGBTQIA+ community disproportionately experiences stigmatization and discrimination which can lead to mental illness (e.g., increased risk of depression, suicidal ideation, anxiety), as well as maladaptive behaviors such as substance abuse and risky sexual behavior that may lead to higher rates of HIV and sexually transmitted infections (54, 60–66). Often, these risk factors are overlooked by clinicians, making it difficult to properly treat patients (67, 68).
In the United States, half of the people diagnosed with HIV are gay and bisexual men (60, 69); these figures are roughly the same in Canada (4). In addition, men who have sex with men are at higher risk of developing anal and genital cancers (70, 71). Lesbian and bisexual women tend to have more binge eating behaviors to deal with social isolation and other pressures related to minority stress (72). This partly explains why lesbian and bisexual women are more likely to be overweight and suffer from obesity, which increases their risk of cardiovascular disease and arthritis compared to the general population (4, 48, 54, 69, 73, 74). Once again illustrating how these increased health risks could be mitigated by reducing the harm associated with minority stress (72). In addition, they also tend to avoid screening for breast cancer, cervical cancer, and sexually transmitted infections due to feelings of distress associated with medical visits (11, 54, 60, 69). Lower screening rates could potentially lead to an increased risk of cancer diagnoses in this population (75, 76) and the development of advanced metastatic disease. Studies suggest that screening tests performed in a comfortable and safe environment make for a positive experience and could potentially remedy the lack of screening (77–80). Positive feelings resulted from sensitive health care providers acknowledging patients’ vulnerability and considering the physical discomfort they may feel while simultaneously affirming their identities. Avoiding the use of gendered or binary language in screening, especially for many cancers is of note, for example, employing the use of “chest” or “upper body” instead of “breast” (48, 81). Simply naming the organ involved instead of referring to female/male reproductive cancer or other body parts is also consequential. Furthermore, health care providers may need to provide education about the need for cervical cancer screening for lesbian women, trans and non-binary people (48). Historically, there has been a misconception that lesbians did not need cervical cancer screening, and some health care providers and community members may still erroneously believe this to be true (48). Therefore, grassroots education for HCP is needed and many Canadian resources and guidelines are available online to this end, these promote preventive care, early diagnosis, and effective management (48). Specialized 2SLGBTQIA+ clinical groups focused specifically on the management of health conditions or the prevention and/or management of behavioral risk factors for chronic diseases have also been shown to be effective in improving care (82–90). A summary of evidence on the prevalence of health conditions can be found in Table 1.
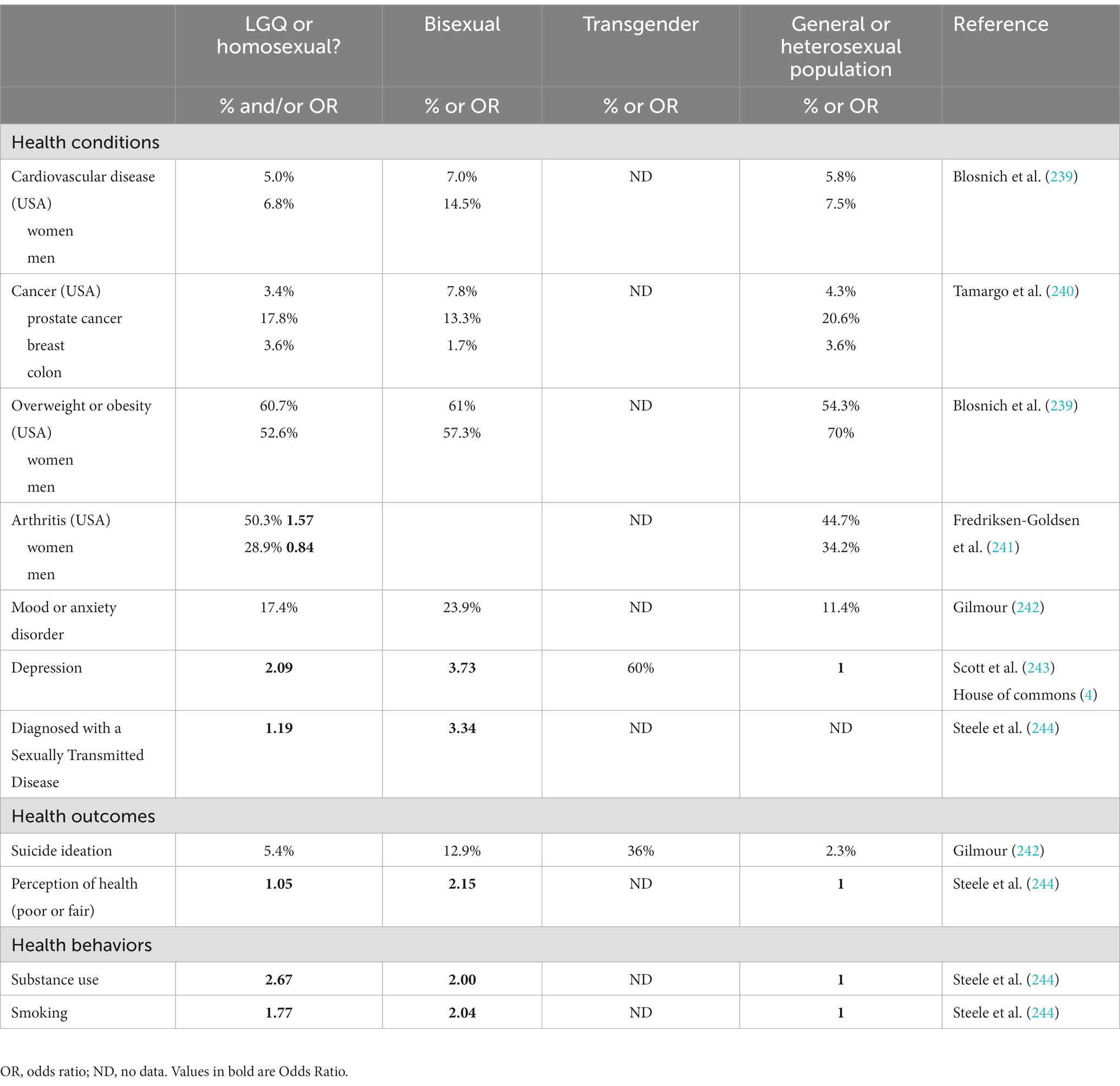
Table 1. A summary of evidence on the prevalence of health conditions, outcomes, and behaviors among individuals from the LGBQ community and transgender individuals in comparison to the general adult population in Canada or the United-States of America (USA).
The transgender (trans) community is among the most neglected and underserved populations in the 2SLGBTQIA+ community. Marginalization, discrimination, lack of HCP experience and knowledge, inadequate services, and structural barriers are causal factors (91–96). Canadian studies have shown that more than half of trans participants have had negative experiences within the health care system, one-third have not been helped, and long wait times have been observed (97–101). In addition, trans women are more likely than trans men to go without medical treatment (102). Transgender individuals have seen their treatments delayed and have been subject to physical and verbal violence at a more alarming rate (32, 49, 103).
Trans people may decide to transition socially, transition medically, or not transition. Social transition refers to the cosmetic, social, and legal changes of transition, such as changing one’s appearance and name. A medical transition may involve hormone therapy and/or surgical procedures. Primary care needs are largely related to medically supervised transition and access to and control of hormone administration and dosing (104). Importantly, transition in many cases is essential, non-elective, and mitigates the risks of suicide and psychological distress prevalent in this population (99, 105–112). As an example, a cross-sectional study of a large Australian cohort found that 57% of transgender individuals were diagnosed with depression and 39% with anxiety (113). In addition to discrimination, the lack of trans-specific medical training has been identified as a major barrier to providing health care to this population (92–94, 114–118). In fact, only one-third of medical schools in Canada and the United States provide education on hormone therapy and surgical transition (119). In a national survey, only 10% of medical students felt they were prepared to care for trans patients (118). In Canada, primary care HCP serve the transgender population; however, the number of clinicians with the necessary skill set to support this population adequately remains low. As a result, patients are placed on waiting lists or are required to travel great distances, and incur costs related to travel and medical procedures to receive adequate health care (100). In addition, general practitioners often refer patients to specialists, such as endocrinologists, often by lack of experience and because they presume the patients will be in better hands. This approach can be interpreted as an unwillingness on the part of the HCP to provide care to the patient and can also increase wait time (93). Incidentally, the great majority (80%) of endocrinologists have not received trans-specific training (120). Another financial barrier is the consultation with a private HCP (psychologists, psychotherapists, or social workers). This step is mandatory for the patient to obtain a letter recommending gender affirmation surgery and is not always straightforward (4). Instead, the Canadian Professional Association for Transgender Health now recommends that informed consent be promoted for a more effective and timely service (121). Prompt access to treatment could greatly reduce the distress felt by this at-risk population (4).
Current curricula do not provide the knowledge required to care for trans people adequately. To fill the knowledge gap in Canada, organizations such as TransCare BC, Rainbow Health Ontario and the Canadian Professional Association for Transgender Health have put together conferences and workshops specifically tailored to providing primary care to trans people (122). Indeed, Canadian primary care guidelines from Ontario and British Columbia are available online for clinicians (98, 123–125). Another example of online continuing education is the Ontario Ministry of Health and Long-Term Care funded program, Trans Health Connection, which provides HCP with training on cultural competency and clinical care for the trans population (98). Finally, excellent guidelines are also freely available from the Registered Nurses’ Association of Ontario (48). Of note, much of the Canadian health care literature comes from the Ontario Trans PULSE study and may not be generalizable to the broader Canadian context due to provincial differences in health care services, such as health care coverage and access to surgeries (122). In Canada, the health system is publicly financed; most health expenditures are financed through the general tax revenues of the federal, provincial, and territorial governments. While the federal government has a role in setting national standards for funding, streamlining data collection and research as well as regulating prescription drugs, Canadian provinces and territories are responsible for financing as well as administrating their own tax-funded and universal hospital and medical care plans (126). This could explain inter-province variability in service delivery and accessibility for the 2SLGBTQIA+ community. Notably, Ontario has the highest number of health programs that target the 2SLGBTQIA+ community (29.5%). That proportion is higher than the programs available across the country, and especially in comparison to the Atlantic provinces. That means, in addition to the variations in logistics between provinces, there are also important variations in programs available to provide health care to individuals from the 2SLGBTQIA+ community. In 2019, an environmental scan of programs in Canada revealed these substantial variations as illustrated in Table 2 (57).
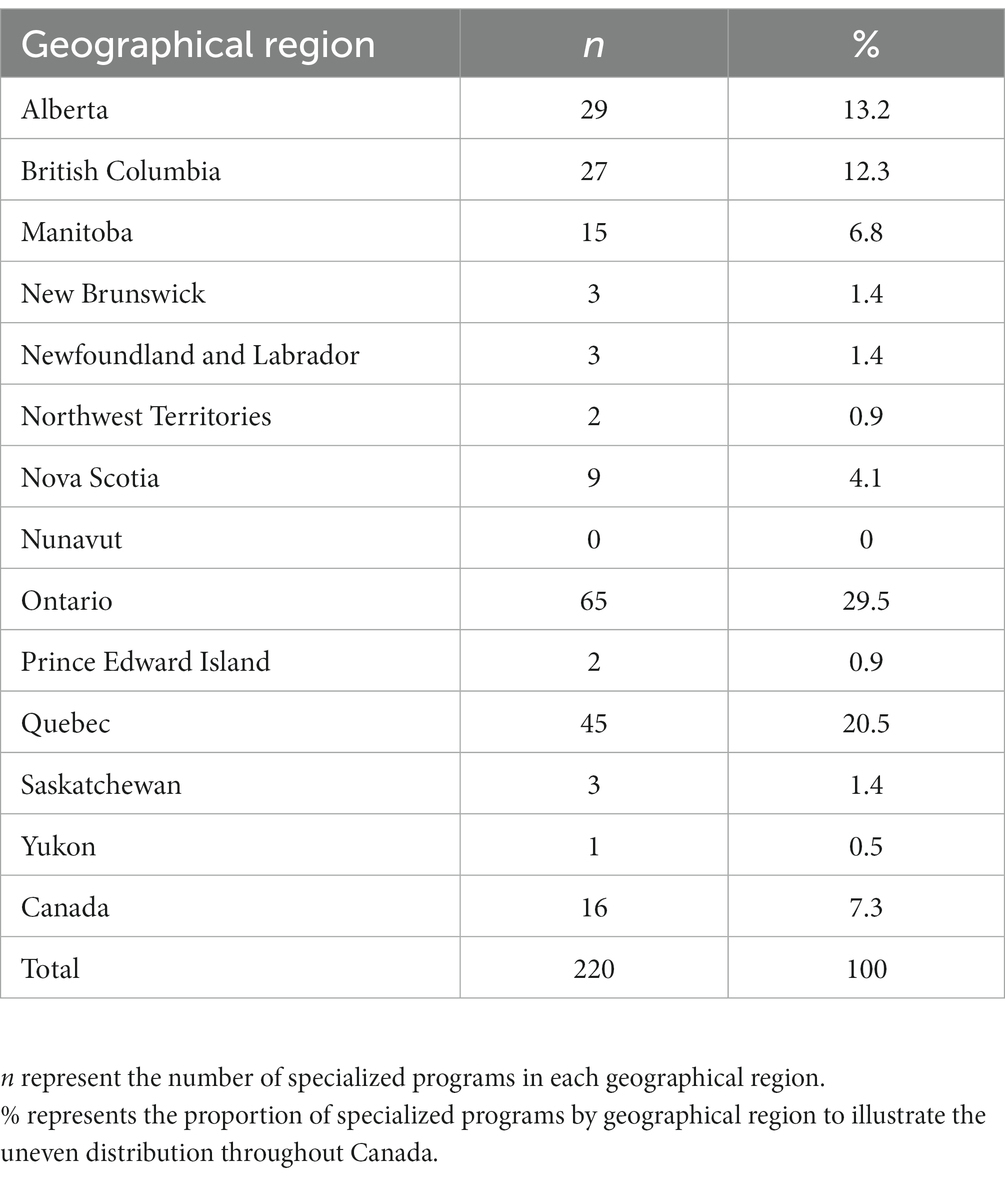
Table 2. Environmental scan of programs targeting sexual and gender minority populations in Canada (2019).
We use the designation ‘Indigenous’ in the present document to describe individuals and groups who identify as descendants of civilizations that predate colonization in Canada. Although there is no universal definition that has been accepted to describe this extremely diverse group of peoples, we employ this terminology because it is understood that individuals and communities will be supported in self-defining what it means to them (127).
Colonization and racism are intertwined and have resulted in deep-rooted and continuing stigma against Indigenous peoples, which have a demonstrably negative impact on health and well-being (128, 129). Racist ideologies have pervaded education, housing, food securities and employment, societal systems and institutions including child welfare, the criminal justice system and, notably, health care (127). The most egregious barrier to health care for Indigenous peoples remains attitudinal and systemic racism (130). Indeed, research shows that racism is so prevalent that Indigenous peoples strategize around anticipated racism before visiting health care facilities or avoid them altogether (131–133). Past horrific assimilationist practices, namely residential schools, the Sixties Scoop, and contemporary child welfare, have also resulted in deep-rooted intergenerational trauma negatively affecting well-being and health (134, 135).
Two-Spirit is a contemporary umbrella term to describe Indigenous peoples with both masculine and feminine spirits outside of the Western colonialist framework (136, 137). Although a unifying term, many Indigenous tribes have their own words, definitions, and cultural understanding of what this means to them; western categories do not accurately reflect the ontologies of gender and sexuality for Indigenous peoples. Oral histories show that Two-Spirit peoples held important roles within Indigenous spirituality and were honored and respected. They were indeed vital to the collective well-being and survival of their tribes, contributing to the maintenance of Indigenous legal, cultural, and spiritual systems (135). Indigenous peoples belonging to the 2SLGBTQIA+ are particularly vulnerable to health inequities due to intersectional forms of discrimination and invisibility within the health care system (138, 139). Consequently, the experiences of Two-Spirit peoples are unique. There is however a scarcity of literature that look exclusively at the health and health inequities of Canadian Two-Spirit peoples (138). And so, the Canadian House of Common’s Standing Committee on Health has called for increased research and programing for the community. It is particularly important for HCP and health care institutions to work toward reconciliation and decolonization to ameliorate existing inequities (140) and acknowledge the Calls to Action and Calls for Justice. Notably, the resiliency of Indigenous peoples has allowed them to survive and flourish in the face of horrendous colonial oppression, demonstrating collective strength and fortitude. There is much to learn here for the betterment of health and health care, not only for Two-Spirit peoples but for the broader LGBTQIA+ community. Understanding the historical, contemporary, and emergent issues faced by Indigenous and Two-Spirit peoples must be a Canadian priority (135).
HCP have reported a lack of curricula geared toward the 2SLGBTQIA+ community (119, 141–145), and HCP who have not been trained appropriately feel that their lack of training negatively affect their ability to care for patients (19, 146, 147). Notably, a survey conducted at the University of Ottawa found that 41% of medical students witnessed anti-2SLGBTQIA+ attitudes within the education system (148). Given the lack of ingrained 2SLGBTQIA+ cultural competency and sensitivity, when in an uncomfortable situation with a member of the community, HCP tend to disconnect from patients which could be perceived as heterosexism by consulting patients (10, 146). This real or perceived disconnect between patients and HCP negatively impacts the consultation and treatments (41, 42). However, when education and training are available, these positively influence comfort levels and diminish anxiety in students and health care providers (149–152). It would thus be imperative to normalise and require HCP to be trained in matters of cultural competency, and the specific health care needs of 2SLGBTQIA+ individuals (19, 141, 145–147, 153–155). Nevertheless, despite overt efforts to deliver equity of care and with no remaining explicit prejudices, discrimination is still common and can be explained by the resilience of unconscious, implicit biases (41, 42, 149, 156–170). Implicit biases are not as easily modifiable as explicit biases because they are firmly entrenched beliefs; thus, for significant change to occur, dedication on the part of the learner is required as well as a strong educational support. Because measures of implicit biases are more strongly associated with real-world behaviors than explicit biases (171, 172), the former should be the focus of educational practices. Furthermore, with less time and limited information processing capacity, providers’ decisions are increasingly governed by implicit stereotypes and biases (173, 174). Moving beyond cultural competency and including training on implicit biases is thus undeniably important (41, 42, 158, 159).
Educating HCP on implicit bias as well as culturally competent care such as 2SLGBTQIA+ social issues and health should be integrated into curricula, in continuing education and in all learning and teaching opportunities when health assessment, health promotion and disease prevention are addressed (43, 44, 175). These themes should not only be promoted but integrated into multimodal learning strategies, experiential learning (e.g., case studies, role-playing, simulation) as well as reflective practice to better prepare HCP to meet the health care needs of 2SLGBTQIA+ patients (60, 147, 176). Moreover, because HCP have generally not had proper training, health care authorities should include and require training for all new employees and offer opportunities for continued education (142, 165, 177). Interventions geared toward training programs have been highlighted, show good promise, and are briefly summarized in four points:
(i) A good first step could be to evaluate the inclusivity of programs/institutions using tools such as the Health care Equality Index (HEI) benchmark (178). Although certification is only available in the United States, they offer numerous learning resources and a scoring system methodology online that could be reproduced for use in Canada (179).
(ii) Include implicit bias training in teaching programs, such as case scenarios used by the Gay and Lesbian medical Association and Fenway Institute (180). Practicing self-reflection and awareness through journaling, self-assessment, deconstructing existing beliefs and analyzing social issues affecting the lives of the 2SLGBTQIA+ community have been shown to be effective tools (181, 182). Programs incorporating bias training should also evaluate their efficacy with tests such as the Implicit Association Test (IAT) (183).
(iii) A training program focused on cultural competency, the inclusion of 2SLGBTQIA+ perspectives and patient-centered care has been shown to be efficacious (46). The trainings found in the literature use a range of effective learning strategies to increase cultural competence, such as lectures, readings, videos, interviews, or presentations by people from the community (intergroup contact), and group discussions. Of these strategies, intergroup contact, i.e., the inclusion of 2SLGBTQIA+ perspectives in training institutions, is most effective in promoting more tolerant attitudes toward this population (46). In these training programs, a variety of topics were covered, including sexual orientation, gender identity, sexual history, 2SLGBTQIA+ terminology, disclosure of orientation and gender identity, discrimination and bias, the impact of discrimination on health, factors affecting patient access and medical care, myths and stereotypes, medical care for transgender people, and legal concerns. Even more importantly, repetition of relevant trainings was a strategy that increased the long-term comfort level of HCP (46).
(iv). The inclusion of cultural safety in teaching programs has been proposed (47, 48). Cultural safety moves away from a focus on cultural differences (cultural competence) to a view of the health system environment as a site of change (184), that involves understanding the history, safety needs, power imbalances (oppression), and the influence of staff values and beliefs on service delivery (185, 186). Research has identified several key components in cultural safety interventions (47), these include provider self-reflection, addressing bias and discrimination, and patient-centered care such as building authentic relationships with patients, power sharing, validation of patient autonomy/intuition, and meaningful training for HCP (127, 184, 187, 188).
There is presently no national standard for health care education in Canada (189). Although several focus points and potential solutions have been highlighted here, no Canadian guidelines or resources exist to transform the current lack of 2SLBGTQIA+ curricula. Data-backed interventions and evaluation of their efficacy are urgently needed for nation-wide implementation.
Cis normativity, the concept of two distinct and opposing genders (women and men), and heteronormativity are profoundly embedded in our society and are reflected in our physical environment. Western Euro-Christian cultural beliefs about gender are being challenged and we must address the inadequacies of our environment to meet the needs of all people, regardless of their gender and sexual orientation. To create a supportive environment, HCP must first assess their own belief systems, cultural norms, and biases to increase their cultural sensitivity, and develop better relationships with 2SLGBTQIA+ patients and gain their trust (Supplementary Table S1) (190).
Creating an open and safe space in all levels of the health care system is essential. In addition, waiting rooms, bathrooms, common areas, and patient care spaces should promote inclusion and support of 2SLGBTQIA+ patients and families through the display of a non-discrimination policy, pro-2SLGBTQIA+ symbols, magazines, posters, information, decorations, or images depicting 2SLGBTQIA+ families (77, 191–198). For instance, bathrooms are an integral and necessary part of our daily lives (199). Gender-neutral bathrooms should be available, and people should also be able to use bathrooms that conform to their gender identity (48, 200). It is therefore recommended to provide gender-neutral and gender-specific toilets and most importantly, to have educated staff who can defend the rights of their users in case of discrimination (Supplementary Table S1) (48). Of note, experts have warned against signage in unsafe spaces, for instance, where employees have not been properly trained to deal with 2SLGBTQIA+ patients or instances of discrimination (48). Visibility can only happen in safe spaces; hence, it is important to have adequate training, and anti-discrimination policies that address instances of discrimination and promote accountability (201, 202).
To open the lines of communication between patients and HCP, electronic medical forms and records should be inclusive and allow for disclosure of sexual orientation and gender and contain neutral language that allows the patient to openly self-identify without presumption (54, 93, 200). At a minimum, all medical forms, processes, language/terminology, and records should include the individual’s chosen name, pronouns, gender identity, sex assigned at birth and sexual orientation (Supplementary Table S1). Assuming a patient’s pronouns based on appearance is harmful because a stereotype regarding gender expression is implicitly reinforced. In fact, this disclosure of the information is of great importance and will have a positive impact on the patient’s health and will make the patient feel comfortable and safe, if done properly (10, 15, 36, 54, 192, 193, 195, 203–205). It is also good practice for HCP to declare their own pronouns before asking the patient to share theirs (206), all the while maintaining privacy when information is shared (194, 207–209). It is important to be non-judgmental and comfortable when asking questions about gender, sex, sexuality, and sexual activity (77, 194, 208).
Moreover, the broader political environment can influence the success of institutional initiatives for change (210), such as bathroom inclusivity and gender neutrality in medical forms and in communication. Organizational cultures influence the acceptability of discriminatory and stigmatizing practices and how HCP interact with patients (Supplementary Table S1). Injurious practices can become embedded in the culture of health care organizations and be reinforced by clinical and non-clinical staff. This can manifest itself in stigmatizing language, assumptions, lack of confidentiality, and denying care or access to treatment. Thus, structural change needs to be accompanied with proper training of staff, accountability, and well cemented inclusive organizational culture.
The drivers of discrimination and stigma impacting 2SLGBTQIA+ health must be addressed at the organizational level on an evidentiary basis (47, 184, 211–215). Interventions should target multiple levels simultaneously, such as creating inclusive physical environments, enhancing workforce diversity, policy changes, practice changes, with education of both clinical and nonclinical staff being the bedrock of change (202, 212, 216–218). A better understanding of health disparities unique to each individual group within the community, notably the trans and bisexual community, and considering intersectionality will be crucial to better tailor service delivery. This will require national data collection and funding large scale research projects geared toward understanding the 2SLGBTQIA+ health care experience. The latter could include descriptive studies of patient journey as well as the development and validation of educational programs tackling implicit bias. Lack of data, lack of national educational programs and guidelines, and the scarce investment in change are presently hindering or impeding forward movement. The lack of national guidelines and best practices are reflected in inter-province variability in terms of programs offered for the health and well-being of sex and gender minorities, with a particularly deplorable amount offered in the Maritime provinces as compared to Ontario. Realistically, overall change will take some time. It is thus important to aim at firstly armoring the 2SLGBTQIA+ community with tools to navigate the health care system. Reducing the impact of stigma on well-being can be achieved through psychoeducation programs at the individual level (219–221); which could help members of the community better navigate and cope with an imperfect health care system. These interventions can also take place in a group setting and include cognitive and behavioral components, such as cognitive-behavioral therapy, and aim to change internalized discriminatory and stigmatizing beliefs, improve coping skills, promote autonomy, and enhance social support (219–225).
To address gender related health inequalities in the past, the World Health Organization and the United Nations stressed the importance of transforming all areas of the health sector to integrate the gender perspective (226–228). This integral change was to encompass actions on policy, research, including interventions at the individual level (training/education). However, more than 20 years of research reveals that gender inequities remain embedded in health systems, and unconscious gender bias and sexism still have a pernicious impact on patient care (229–231). Over the years, institutions have seldom invested in education/training, data collection, changes in workplace culture, and human resource management to make sex and gender equality goals and standards an integral part of their governance (232). Sex and gender inclusivity had become an idea that has engrossed many institutions and governments at the expense of substantial actions to remedy health inequities (232–234). Lack of awareness and capacity in policy making, underfunding, bureaucratization, lack of evidence, and lack of patient participation in decision making are noted as pitfalls (235). A close parallel can be drawn between the struggle for gender inclusion in medicine and the inclusion of the 2SLGBTQIA+ community. Indeed, this could present an opportunity to learn from the mistakes of the past, move forward and avoid making the same missteps in addressing the health inequality of the 2SLGBTQIA+ community. Investing in diligent and exhaustive research-backed interventions at the organizational level could avoid such a misuse of resources and precious time (233, 235).
It is also important to highlight that gender inequities do not only have an impact on the 2SLGBTQIA+ community but is also endemic to the cis-gender and heterosexual population. Restrictive gender norms maintain a hierarchical system in which dominant forms of masculinity are favored. A gender system is created that not only undermines the health and human rights of girls and women, but also promotes the marginalization and discrimination of all those who transgress restrictive gender norms, including boys and men (230, 236–238). Ultimately, both face the same misogynistic and gendered barriers, therefore, the inclusion of the 2SLGBTQIA+ community in health care stretches its reach beyond this to all who are subjugated.
2SLGBTQIA+ inequities in the Canadian Health care system need to be corrected. Systemic discrimination, patient care and access to care need to be addressed through large scale national education and training programs with research and data collection being the linchpin of all forward movement and progress, all of which will require significant investment.
A literature review was performed using PubMed, Embase, and CINAHL. A broad subset of keywords relating to Canadian health care for sexual and gender minorities were used and Canadian articles were prioritized. Canadian grey literature such as federal and provincial government reports, health care authorities and other community-based communications were included in our search.
DC reviewed the literature and wrote the manuscript under the supervision of NB. CJ contributed to the writing and editing of the manuscript. NB wrote sections, edited, and corrected the manuscript. All authors reviewed, provided feedback, and approved the final version of the manuscript.
We would like to thank Isabelle Wallace, a registered nurse from the Madawaska Maliseet First Nation in New Brunswick, who kindly reviewed the section on Two-Spirit peoples. Her input has been crucial in accurately and respectfully describing Two-Spirit peoples’ culture.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2023.1183284/full#supplementary-material
1. Manandhar, M, Hawkes, S, Buse, K, Nosrati, E, and Magar, V. Gender, health and the 2030 agenda for sustainable development. Bull World Health Organ. (2018) 96:644–53. doi: 10.2471/BLT.18.211607
2. Social determinants of health and health inequalities – Government of Canada. Health science, research, and data (2020). Available at: https://www.canada.ca/en/public-health/services/health-promotion/population-health/what-determines-health.html (Accessed April 26, 2022).
3. Gouvernement du Canada. LGBTQ2 terminology-glossary and commons acronyms (2020). Available at: https://women-gender-equality.canada.ca/en/free-to-be-me/lgbtq2-glossary.html (Accessed April 13, 2022).
4. Casey, B. (2019). The health of LGBTQIA2 communities in Canada. Report of the standing committee on health – 42nd parliament, 1st session. Available at: https://www.ourcommons.ca/Content/Committee/421/HESA/Reports/RP10574595/hesarp28/hesarp28-e.pdf (Accessed January 4, 2023).
5. Dentato, MP. The minority stress perspective. Psychology and AIDS Exchange Newsletter. Available at: https://www.apa.org/pi/aids/resources/exchange/2012/04/minority-stress. (2012) (Accessed May 13, 2022)
6. Meyer, IH. Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: conceptual issues and research evidence. Psychol Bull. (2003) 129:674–97. doi: 10.1037/0033-2909.129.5.674
7. Pollitt, AM, Mernitz, SE, Russell, ST, Curran, MA, and Toomey, RB. Heteronormativity in the lives of lesbian, gay, bisexual, and queer Young people. J Homosex. (2021) 68:522–44. doi: 10.1080/00918369.2019.1656032
8. Rich, AJ, Salway, T, Scheim, A, and Poteat, T. Sexual minority stress theory: remembering and honoring the work of Virginia Brooks. LGBT Health. (2020) 7:124–7. doi: 10.1089/lgbt.2019.0223
9. Hatzenbuehler, ML, and Pachankis, JE. Stigma and minority stress as social determinants of health among lesbian, gay, bisexual, and transgender youth: research evidence and clinical implications. Pediatr Clin N Am. (2016) 63:985–97. doi: 10.1016/j.pcl.2016.07.003
10. Baker, K, and Beagan, B. Making assumptions, making space: an anthropological critique of cultural competency and its relevance to queer patients. Med Anthropol Q. (2014) 28:578–98. doi: 10.1111/maq.12129
11. Institute of Medicine. The health of lesbian, gay, bisexual, and transgender people: building a foundation for better understanding. Washington, DC: National Academies Press (2011).
12. Blackwell, CW. Belief in the free choice model of homosexuality: a correlate of homophobia in registered nurses. J LGBT Health Res. (2007) 3:31–40. doi: 10.1080/15574090802093117
13. Klotzbaugh, R, and Spencer, G. Magnet nurse administrator attitudes and opportunities: toward improving lesbian, gay, bisexual, or transgender-specific healthcare. J Nurs Adm. (2014) 44:481–6. doi: 10.1097/NNA.0000000000000103
14. Röndahl, G, Innala, S, and Carlsson, M. Nursing staff and nursing students' emotions towards homosexual patients and their wish to refrain from nursing, if the option existed. Scand J Caring Sci. (2004) 18:19–26. doi: 10.1111/j.1471-6712.2004.00263.x
15. Ayhan, CHB, Bilgin, H, Uluman, OT, Sukut, O, Yilmaz, S, and Buzlu, S. A systematic review of the discrimination against sexual and gender minority in health Care settings. Int J Health Serv. (2020) 50:44–61. doi: 10.1177/0020731419885093
16. Bockting, WO, Miner, MH, Swinburne Romine, RE, Hamilton, A, and Coleman, E. Stigma, mental health, and resilience in an online sample of the US transgender population. Am J Public Health. (2013) 103:943–51. doi: 10.2105/AJPH.2013.301241
17. Bradford, J, Reisner, SL, Honnold, JA, and Xavier, J. Experiences of transgender-related discrimination and implications for health: results from the Virginia transgender health initiative study. Am J Public Health. (2013) 103:1820–9. doi: 10.2105/AJPH.2012.300796
18. Clements-Nolle, K, Marx, R, and Katz, M. Attempted suicide among transgender persons: the influence of gender-based discrimination and victimization. J Homosex. (2006) 51:53–69. doi: 10.1300/J082v51n03_04
19. Abdessamad, HM, Yudin, MH, Tarasoff, LA, Radford, KD, and Ross, LE. Attitudes and knowledge among obstetrician-gynecologists regarding lesbian patients and their health. J Womens Health. (2013) 22:85–93. doi: 10.1089/jwh.2012.3718
20. Jabson, JM, Mitchell, JW, and Doty, B. Associations between non-discrimination and training policies and physicians' attitudes and knowledge about sexual and gender minority patients: a comparison of physicians from two hospitals. BMC Public Health. (2016) 16:256. doi: 10.1186/s12889-016-2927-y
21. Berliant, M, Odorizzi, S, and Leppard, J. Out of the closet and into the waiting room: improving care of 2SLGBTQIA+ patients in the emergency department. CJEM. (2021) 23:733–6. doi: 10.1007/s43678-021-00202-y
22. Eckstrand, KL, Eliason, J, St Cloud, T, and Potter, J. The priority of intersectionality in academic medicine. Acad Med. (2016) 91:904–7. doi: 10.1097/ACM.0000000000001231
23. Hsieh, N, and Ruther, M. Sexual minority health and health risk factors: intersection effects of gender, race, and sexual identity. Am J Prev Med. (2016) 50:746–55. doi: 10.1016/j.amepre.2015.11.016
24. Veenstra, G. Race, gender, class, and sexual orientation: intersecting axes of inequality and self-rated health in Canada. Int J Equity Health. (2011) 10:3. doi: 10.1186/1475-9276-10-3
25. Bauer, GR. Incorporating intersectionality theory into population health research methodology: challenges and the potential to advance health equity. Soc Sci Med. (2014) 110:10–7. doi: 10.1016/j.socscimed.2014.03.022
26. Karakaya, S, and Kutlu, FY. LGBT individuals' opinions about their health care experiences: a qualitative research study. J Nurs Manag. (2021) 29:24–31. doi: 10.1111/jonm.13199
27. Logie, CH, Lys, CL, Dias, L, Schott, N, Zouboules, MR, MacNeill, N, et al. Automatic assumption of your gender, sexuality and sexual practices is also discrimination: exploring sexual healthcare experiences and recommendations among sexually and gender diverse persons in Arctic Canada. Health Soc Care Community. (2019) 27:1204–13. doi: 10.1111/hsc.12757
28. McCann, E, and Brown, M. Education and practice developments: addressing the psychosocial concerns and support needs of LGBT+ people. Nurse Educ Today. (2019) 82:15–20. doi: 10.1016/j.nedt.2019.08.008
29. Khan, A, Plummer, D, Hussain, R, and Minichiello, V. Does physician bias affect the quality of care they deliver? Evidence in the care of sexually transmitted infections. Sex Transm Infect. (2008) 84:150–1. doi: 10.1136/sti.2007.028050
30. Johnson, MJ, Jackson, NC, Arnette, JK, and Koffman, SD. Gay and lesbian perceptions of discrimination in retirement care facilities. J Homosex. (2005) 49:83–102. doi: 10.1300/J082v49n02_05
31. Kass, NE, Faden, RR, Fox, R, and Dudley, J. Homosexual and bisexual men's perceptions of discrimination in health services. Am J Public Health. (1992) 82:1277–9. doi: 10.2105/AJPH.82.9.1277
32. Kattari, SK, Walls, NE, Whitfield, DL, and Langenderfer-Magruder, L. Racial and ethnic differences in experiences of discrimination in accessing health services among transgender people in the United States. Int J Transgend. (2015) 16:68–79. doi: 10.1080/15532739.2015.1064336
33. Li, CC, Matthews, AK, Aranda, F, Patel, C, and Patel, M. Predictors and consequences of negative patient-provider interactions among a sample of African American sexual minority women. LGBT Health. (2015) 2:140–6. doi: 10.1089/lgbt.2014.0127
34. Reisner, SL, Pardo, ST, Gamarel, KE, Hughto, JMW, Pardee, DJ, and Keo-Meier, CL. Substance use to cope with Stigma in healthcare among U.S. female-to-male Trans masculine adults. LGBT. Health. (2015) 2:324–32. doi: 10.1089/lgbt.2015.0001
35. Risher, K, Adams, D, Sithole, B, Ketende, S, Kennedy, C, Mnisi, Z, et al. Sexual stigma and discrimination as barriers to seeking appropriate healthcare among men who have sex with men in Swaziland. J Int AIDS Soc. (2013) 16:18715. doi: 10.7448/IAS.16.3.18715
36. Steele, LS, Tinmouth, JM, and Lu, A. Regular health care use by lesbians: a path analysis of predictive factors. Fam Pract. (2006) 23:631–6. doi: 10.1093/fampra/cml030
37. Yen, CF, Pan, SM, Hou, SY, Liu, HC, Wu, SJ, Yang, WC, et al. Attitudes toward gay men and lesbians and related factors among nurses in southern Taiwan. Public Health. (2007) 121:73–9. doi: 10.1016/j.puhe.2006.08.013
38. Hou, SY, Pan, SM, Ko, NY, Liu, HC, Wu, SJ, Yang, WC, et al. Correlates of attitudes toward homosexuality and intention to care for homosexual people among psychiatric nurses in southern Taiwan. Kaohsiung J Med Sci. (2006) 22:390–7. doi: 10.1016/S1607-551X(09)70328-6
39. Smith, DM, and Mathews, WC. Physicians' attitudes toward homosexuality and HIV: survey of a California medical society- revisited (PATHH-II). J Homosex. (2007) 52:1–9. doi: 10.1300/J082v52n03_01
40. Flores, A.R. Social acceptance of LGBTI people in 175 countries and locations (2021). Available at: https://williamsinstitute.law.ucla.edu/publications/global-acceptance-index-lgbt/ (Accessed March 23, 2022).
41. Zestcott, CA, Blair, IV, and Stone, J. Examining the presence, consequences, and reduction of implicit Bias in health care: a narrative review. Group Process Intergroup Relat. (2016) 19:528–42. doi: 10.1177/1368430216642029
42. van Ryn, M, and Saha, S. Exploring unconscious bias in disparities research and medical education. JAMA. (2011) 306:995–6. doi: 10.1001/jama.2011.1275
43. Bellack, JP. Unconscious Bias: an obstacle to cultural competence. J Nurs Educ. (2015) 54:S63–4. doi: 10.3928/01484834-20150814-12
44. Blair, IV, Steiner, JF, and Havranek, EP. Unconscious (implicit) bias and health disparities: where do we go from here? Perm J. (2011) 15:71–8. doi: 10.7812/TPP/11.979
45. National LGBT Health Education Center. Learning to address implicit bias towards LGBTQ patients: case scenarios. Boston, MA: Fenway (2018).
46. Morris, M, Cooper, RL, Ramesh, A, Tabatabai, M, Arcury, TA, Shinn, M, et al. Training to reduce LGBTQ-related bias among medical, nursing, and dental students and providers: a systematic review. BMC Med Educ. (2019) 19:325. doi: 10.1186/s12909-019-1727-3
47. Stigma, Addressing (2019). Towards a more inclusive health system. The chief public health Officer's report on the state of public health in Canada. Available at: https://www.canada.ca/content/dam/phac-aspc/documents/corporate/publications/chief-public-health-officer-reports-state-public-health-canada/addressing-stigma-what-we-heard/stigma-eng.pdf (Accessed April 24, 2022).
48. Promoting 2SLGBTQI+ Health Equity (2021). Registered Nurses' Association of Ontario. Available at: https://rnao.ca/sites/rnao-ca/files/bpg/2SLGBTQI_BPG_FIINAL_WEB_2.0.pdf (Accessed April 24, 2022).
49. Shires, DA, and Jaffee, K. Factors associated with health care discrimination experiences among a national sample of female-to-male transgender individuals. Health Soc Work. (2015) 40:134–41. doi: 10.1093/hsw/hlv025
50. Smith, EM, Johnson, SR, and Guenther, SM. Health care attitudes and experiences during gynecologic care among lesbians and bisexuals. Am J Public Health. (1985) 75:1085–7. doi: 10.2105/AJPH.75.9.1085
51. Lee, RS, Melhado, TV, Chacko, KM, White, KJ, Huebschmann, AG, and Crane, LA. The dilemma of disclosure: patient perspectives on gay and lesbian providers. J Gen Intern Med. (2008) 23:142–7. doi: 10.1007/s11606-007-0461-4
52. Mosack, KE, Brouwer, AM, and Petroll, AE. Sexual identity, identity disclosure, and health care experiences: is there evidence for differential homophobia in primary care practice? Womens Health Issues. (2013) 23:e341–6. doi: 10.1016/j.whi.2013.07.004
53. Shetty, G, Sanchez, JA, Lancaster, JM, Wilson, LE, Quinn, GP, and Schabath, MB. Oncology healthcare providers' knowledge, attitudes, and practice behaviors regarding LGBT health. Patient Educ Couns. (2016) 99:1676–84. doi: 10.1016/j.pec.2016.05.004
54. Johnson, MJ, and Nemeth, LS. Addressing health disparities of lesbian and bisexual women: a grounded theory study. Womens Health Issues. (2014) 24:635–40. doi: 10.1016/j.whi.2014.08.003
55. Whitehead, J, Shaver, J, and Stephenson, R. Outness, Stigma, and primary health care utilization among rural LGBT populations. PLoS One. (2016) 11:e0146139. doi: 10.1371/journal.pone.0146139
56. Hatzenbuehler, ML, Phelan, JC, and Link, BG. Stigma as a fundamental cause of population health inequalities. Am J Public Health. (2013) 103:813–21. doi: 10.2105/AJPH.2012.301069
57. Higgins, R, Hansen, B, Jackson, BE, Shaw, A, and Lachowsky, NJ. Programs and interventions promoting health equity in LGBTQ2+ populations in Canada through action on social determinants of health. Health Promot Chronic Dis Prev Can. (2021) 41:431–5. doi: 10.24095/hpcdp.41.12.04
58. Delozier, AM, Kamody, RC, Rodgers, S, and Chen, D. Health disparities in transgender and gender expansive adolescents: a topical review from a minority stress framework. J Pediatr Psychol. (2020) 45:842–7. doi: 10.1093/jpepsy/jsaa040
59. Lick, DJ, Durso, LE, and Johnson, KL. Minority stress and physical health among sexual minorities. Perspect Psychol Sci. (2013) 8:521–48. doi: 10.1177/1745691613497965
60. Daniel, H, and Butkus, R, Health and Public Policy Committee of the American College of Physicians. Lesbian, gay, bisexual, and transgender health disparities: executive summary of a policy position paper from the American College of Physicians. Ann Intern Med. (2015) 163:135–7. doi: 10.7326/M14-2482
61. Reisner, SL, Greytak, EA, Parsons, JT, and Ybarra, ML. Gender minority social stress in adolescence: disparities in adolescent bullying and substance use by gender identity. J Sex Res. (2015) 52:243–56. doi: 10.1080/00224499.2014.886321
62. Russell, ST, Ryan, C, Toomey, RB, Diaz, RM, and Sanchez, J. Lesbian, gay, bisexual, and transgender adolescent school victimization: implications for young adult health and adjustment. J Sch Health. (2011) 81:223–30. doi: 10.1111/j.1746-1561.2011.00583.x
63. Reisner, SL, White, JM, Bradford, JB, and Mimiaga, MJ. Transgender health disparities: comparing full cohort and nested matched-pair study designs in a community health center. LGBT Health. (2014) 1:177–84. doi: 10.1089/lgbt.2014.0009
64. Norman, RE, Byambaa, M, de, R, Butchart, A, Scott, J, and Vos, T. The long-term health consequences of child physical abuse, emotional abuse, and neglect: a systematic review and meta-analysis. PLoS Med. (2012) 9:e1001349. doi: 10.1371/journal.pmed.1001349
65. Rhoades, H, Rusow, JA, Bond, D, Lanteigne, A, Fulginiti, A, and Goldbach, JT. Homelessness, mental health and suicidality among LGBTQ youth accessing crisis services. Child Psychiatry Hum Dev. (2018) 49:643–51. doi: 10.1007/s10578-018-0780-1
66. Roberts, AL, Austin, SB, Corliss, HL, Vandermorris, AK, and Koenen, KC. Pervasive trauma exposure among US sexual orientation minority adults and risk of posttraumatic stress disorder. Am J Public Health. (2010) 100:2433–41. doi: 10.2105/AJPH.2009.168971
67. Rowe, D, Ng, YC, O'Keefe, L, and Crawford, D. Providers' attitudes and knowledge of lesbian, gay, bisexual, and transgender health. Fed Pract. (2017) 34:28–34.
68. Mule, NJ, Ross, LE, Deeprose, B, Jackson, BE, Daley, A, Travers, A, et al. Promoting LGBT health and wellbeing through inclusive policy development. Int J Equity Health. (2009) 8:18. doi: 10.1186/1475-9276-8-18
69. Fredriksen-Goldsen, KI, Simoni, JM, Kim, HJ, Lehavot, K, Walters, KL, Yang, J, et al. The health equity promotion model: reconceptualization of lesbian, gay, bisexual, and transgender (LGBT) health disparities. Am J Orthopsychiatry. (2014) 84:653–63. doi: 10.1037/ort0000030
70. Johnson, LG, Madeleine, MM, Newcomer, LM, Schwartz, SM, and Daling, JR. Anal cancer incidence and survival: the surveillance, epidemiology, and end results experience, 1973-2000. Cancer. (2004) 101:281–8. doi: 10.1002/cncr.20364
71. Cranston, RD, Murphy, R, Weiss, RE, da Costa, M, Palefsky, J, Shoptaw, S, et al. Anal human papillomavirus infection in a street-based sample of drug using HIV-positive men. Int J Std AIDS. (2012) 23:195–200. doi: 10.1258/ijsa.2011.011169
72. Mason, TB, and Lewis, RJ. Minority stress and binge eating among lesbian and bisexual women. J Homosex. (2015) 62:971–92. doi: 10.1080/00918369.2015.1008285
73. Caceres, BA, Brody, A, and Chyun, D. Recommendations for cardiovascular disease research with lesbian, gay and bisexual adults. J Clin Nurs. (2016) 25:3728–42. doi: 10.1111/jocn.13415
74. Caceres, BA, Brody, A, Luscombe, RE, Primiano, JE, Marusca, P, Sitts, EM, et al. A systematic review of cardiovascular disease in sexual minorities. Am J Public Health. (2017) 107:e13–21. doi: 10.2105/AJPH.2016.303630
75. Diamant, AL, and Wold, C. Sexual orientation and variation in physical and mental health status among women. J Womens Health. (2003) 12:41–9.
76. Lee, R. Health care problems of lesbian, gay, bisexual, and transgender patients. West J Med. (2000) 172:403–8. doi: 10.1136/ewjm.172.6.403
77. Agénor, M, Bailey, Z, Krieger, N, Austin, SB, and Gottlieb, BR. Exploring the cervical Cancer screening experiences of black lesbian, bisexual, and queer women: the role of patient-provider communication. Women Health. (2015) 55:717–36. doi: 10.1080/03630242.2015.1039182
78. Connolly, D, Hughes, X, and Berner, A. Barriers and facilitators to cervical cancer screening among transgender men and non-binary people with a cervix: a systematic narrative review. Prev Med. (2020) 135:106071. doi: 10.1016/j.ypmed.2020.106071
79. Peitzmeier, SM, Agénor, M, Bernstein, IM, McDowell, M, Alizaga, NM, Reisner, SL, et al. "it can promote an existential crisis": factors influencing pap test acceptability and utilization among Transmasculine individuals. Qual Health Res. (2017) 27:2138–49. doi: 10.1177/1049732317725513
80. Johnson, M, Wakefield, C, and Garthe, K. Qualitative socioecological factors of cervical cancer screening use among transgender men. Prev Med Rep. (2020) 17:101052. doi: 10.1016/j.pmedr.2020.101052
81. Trans Care, BC. Gender Inclusive Language: Clinical settings with new clients. Trans Care BC Provincial Health Services Authority. Available at: http://www.phsa.ca/transcarebc/Documents/HealthProf/Gender_Inclusive_Language_Clinical.pdf (Accessed April, 2022).
82. Capistrant, BD, Torres, B, Merengwa, E, West, WG, Mitteldorf, D, and Rosser, BRS. Caregiving and social support for gay and bisexual men with prostate cancer. Psychooncology. (2016) 25:1329–36. doi: 10.1002/pon.4249
83. Batist, E, Brown, B, Scheibe, A, Baral, SD, and Bekker, LG. Outcomes of a community-based HIV-prevention pilot programme for township men who have sex with men in Cape Town, South Africa. J Int AIDS Soc. (2013) 16:18754. doi: 10.7448/IAS.16.4.18754
84. Barry, MC, Threats, M, Blackburn, NA, LeGrand, S, Dong, W, Pulley, DV, et al. Stay strong! Keep ya head up! Move on! It gets better!!!!: resilience processes in the healthMpowerment online intervention of young black gay, bisexual and other men who have sex with men. AIDS Care. (2018) 30:S27–38. doi: 10.1080/09540121.2018.1510106
85. Cruess, DG, Burnham, KE, Finitsis, DJ, Goshe, BM, Strainge, L, Kalichman, M, et al. A randomized clinical trial of a brief internet-based group intervention to reduce sexual transmission risk behavior among HIV-positive gay and bisexual men. Ann Behav Med. (2018) 52:116–29. doi: 10.1093/abm/kax031
86. Hidalgo, MA, Kuhns, LM, Hotton, AL, Johnson, AK, Mustanski, B, and Garofalo, R. The MyPEEPS randomized controlled trial: a pilot of preliminary efficacy, feasibility, and acceptability of a group-level, HIV risk reduction intervention for young men who have sex with men. Arch Sex Behav. (2015) 44:475–85. doi: 10.1007/s10508-014-0347-6
87. Logie, CH, Lacombe-Duncan, A, Weaver, J, Navia, D, and Este, D. A pilot study of a group-based HIV and STI prevention intervention for lesbian, bisexual, queer, and other women who have sex with women in Canada. AIDS Patient Care STDs. (2015) 29:321–8. doi: 10.1089/apc.2014.0355
88. Heckman, BD, Lovejoy, TI, Heckman, TG, Anderson, T, Grimes, T, Sutton, M, et al. The moderating role of sexual identity in group teletherapy for adults aging with HIV. Behav Med. (2014) 40:134–42. doi: 10.1080/08964289.2014.925417
89. Eliason, MJ, Dibble, SL, Gordon, R, and Soliz, GB. The last drag: an evaluation of an LGBT-specific smoking intervention. J Homosex. (2012) 59:864–78. doi: 10.1080/00918369.2012.694770
90. McElroy, JA, Haynes, SG, Eliason, MJ, Wood, SF, Gilbert, T, Barker, LT, et al. Healthy weight in lesbian and bisexual women aged 40 and older: an effective intervention in 10 cities using tailored approaches. Womens Health Issues. (2016) 26:S18–35. doi: 10.1016/j.whi.2016.05.002
91. Alegria, CA. Transgender identity and health care: implications for psychosocial and physical evaluation. J Am Acad Nurse Pract. (2011) 23:175–82. doi: 10.1111/j.1745-7599.2010.00595.x
92. Roberts, TK, and Fantz, CR. Barriers to quality health care for the transgender population. Clin Biochem. (2014) 47:983–7. doi: 10.1016/j.clinbiochem.2014.02.009
93. Bauer, GR, Hammond, R, Travers, R, Kaay, M, Hohenadel, KM, and Boyce, M. I don't think this is theoretical; this is our lives: how erasure impacts health care for transgender people. J Assoc Nurses AIDS Care. (2009) 20:348–61. doi: 10.1016/j.jana.2009.07.004
94. Snelgrove, JW, Jasudavisius, AM, Rowe, BW, Head, EM, and Bauer, GR. completely out-at-sea with two-gender medicine: a qualitative analysis of physician-side barriers to providing healthcare for transgender patients. BMC Health Serv Res. (2012) 12:110. doi: 10.1186/1472-6963-12-110
95. Carlström, R, Ek, S, and Gabrielsson, S. Treat me with respect: transgender persons' experiences of encounters with healthcare staff. Scand J Caring Sci. (2021) 35:600–7. doi: 10.1111/scs.12876
96. Samuels, EA, Tape, C, Garber, N, Bowman, S, and Choo, EK. Sometimes you feel like the freak show: a qualitative assessment of emergency care experiences among transgender and gender-nonconforming patients. Ann Emerg Med. (2018) 71:170–182.e1. doi: 10.1016/j.annemergmed.2017.05.002
97. Gahagan, J, and Subirana-Malaret, M. Improving pathways to primary health care among LGBTQ populations and health care providers: key findings from Nova Scotia, Canada. Int J Equity Health. (2018) 17:76. doi: 10.1186/s12939-018-0786-0
98. Giblon, R, and Bauer, GR. Health care availability, quality, and unmet need: a comparison of transgender and cisgender residents of Ontario, Canada. BMC Health Serv Res. (2017) 17:283. doi: 10.1186/s12913-017-2226-z
99. Ross, KAE, Law, MP, and Bell, A. Exploring healthcare experiences of transgender individuals. Transgend Health. (2016) 1:238–49. doi: 10.1089/trgh.2016.0021
100. Rotondi, NK, Bauer, GR, Scanlon, K, Kaay, M, Travers, R, and Travers, A. Nonprescribed hormone use and self-performed surgeries: do-it-yourself transitions in transgender communities in Ontario. Canada Am J Public Health. (2013) 103:1830–6. doi: 10.2105/AJPH.2013.301348
101. Vermeir, E, Jackson, LA, and Marshall, EG. Barriers to primary and emergency healthcare for trans adults. Cult Health Sex. (2018) 20:232–46. doi: 10.1080/13691058.2017.1338757
102. Scheim, AI, and Bauer, GR. Sex and gender diversity among transgender persons in Ontario, Canada: results from a respondent-driven sampling survey. J Sex Res. (2015) 52:1–14. doi: 10.1080/00224499.2014.893553
103. Mayer, KH, Bradford, JB, Makadon, HJ, Stall, R, Goldhammer, H, and Landers, S. Sexual and gender minority health: what we know and what needs to be done. Am J Public Health. (2008) 98:989–95. doi: 10.2105/AJPH.2007.127811
104. Sanchez, NF, Sanchez, JP, and Danoff, A. Health care utilization, barriers to care, and hormone usage among male-to-female transgender persons in new York City. Am J Public Health. (2009) 99:713–9. doi: 10.2105/AJPH.2007.132035
105. Russell, ST, Pollitt, AM, Li, G, and Grossman, AH. Chosen name use is linked to reduced depressive symptoms, suicidal ideation, and suicidal behavior among transgender youth. J Adolesc Health. (2018) 63:503–5. doi: 10.1016/j.jadohealth.2018.02.003
106. Green, AE, DeChants, JP, Price, MN, and Davis, CK. Association of Gender-Affirming Hormone Therapy with Depression, thoughts of suicide, and attempted suicide among transgender and nonbinary youth. J Adolesc Health. (2022) 70:643–9. doi: 10.1016/j.jadohealth.2021.10.036
107. Achille, C, Taggart, T, Eaton, NR, Osipoff, J, Tafuri, K, Lane, A, et al. Longitudinal impact of gender-affirming endocrine intervention on the mental health and well-being of transgender youths: preliminary results. Int J Pediatr Endocrinol. (2020) 2020:8. doi: 10.1186/s13633-020-00078-2
108. Turban, JL, King, D, Carswell, JM, and Keuroghlian, AS. Pubertal suppression for transgender youth and risk of suicidal ideation. Pediatrics. (2020) 145:1–8. doi: 10.1542/peds.2019-1725
109. Goldenberg, T, Jadwin-Cakmak, L, Popoff, E, Reisner, SL, Campbell, BA, and Harper, GW. Stigma, gender affirmation, and primary healthcare use among black transgender youth. J Adolesc Health. (2019) 65:483–90. doi: 10.1016/j.jadohealth.2019.04.029
110. Durwood, L, McLaughlin, KA, and Olson, KR. Mental health and self-worth in socially transitioned transgender youth. J Am Acad Child Adolesc Psychiatry. (2017) 56:116–123.e2. doi: 10.1016/j.jaac.2016.10.016
111. Olson, KR, Durwood, L, DeMeules, M, and McLaughlin, KA. Mental health of transgender children who are supported in their identities. Pediatrics. (2016) 137:e20153223. doi: 10.1542/peds.2015-3223
112. Veale, JF, Peter, T, Travers, R, and Saewyc, EM. Enacted Stigma, mental health, and protective factors among transgender youth in Canada. Transgend Health. (2017) 2:207–16. doi: 10.1089/trgh.2017.0031
113. Hyde, Z, Doherty, M, Tilley, P, McCaul, K, Rooney, R, and Jancey, J. The first Australian national trans mental health study: summary of results. Curtin University: School of Public Health (2014).
114. Cruz, TM. Assessing access to care for transgender and gender nonconforming people: a consideration of diversity in combating discrimination. Soc Sci Med. (2014) 110:65–73. doi: 10.1016/j.socscimed.2014.03.032
115. Gardner, IH, and Safer, JD. Progress on the road to better medical care for transgender patients. Curr Opin Endocrinol Diabetes Obes. (2013) 20:553–8. doi: 10.1097/01.med.0000436188.95351.4d
116. Sanchez, NF, Rabatin, J, Sanchez, JP, Hubbard, S, and Kalet, A. Medical students' ability to care for lesbian, gay, bisexual, and transgendered patients. Fam Med. (2006) 38:21–7.
117. White, W, Brenman, S, Paradis, E, Goldsmith, ES, Lunn, MR, Obedin-Maliver, J, et al. Lesbian, gay, bisexual, and transgender patient care: medical students’ preparedness and comfort. Teach Learn Med. (2015) 27:254–63. doi: 10.1080/10401334.2015.1044656
118. Chan, B, Skocylas, R, and Safer, JD. Gaps in transgender medicine content identified among Canadian medical school curricula. Transgend Health. (2016) 1:142–50. doi: 10.1089/trgh.2016.0010
119. Obedin-Maliver, J, Goldsmith, ES, Stewart, L, White, W, Tran, E, Brenman, S, et al. Lesbian, gay, bisexual, and transgender-related content in undergraduate medical education. JAMA. (2011) 306:971–7. doi: 10.1001/jama.2011.1255
120. Irwig, MS. Transgender Care by endocrinologists in the United States. Endocr Pract. (2016) 22:832–6. doi: 10.4158/EP151185.OR
121. Association professionnelle canadienne pour la santé transgenre, Mémoire présenté au Comité permanent de la santé, mai (2019). Available at: https://www.noscommunes.ca/Content/Committee/421/HESA/Brief/BR10482210/br-external/CanadianProfessionalAssociationForTransgenderHealth-1-10057296-f.pdf.
122. Ziegler, E, Valaitis, R, Carter, N, Risdon, C, and Yost, J. Primary Care for Transgender Individuals: a review of the literature reflecting a Canadian perspective. SAGE Open. (2020) 10:215824402096282. doi: 10.1177/2158244020962824
123. Dahl, M., Feldman, J., Goldburg, J., and Jaberi, A. (2015). Endocrine therapy for transgender adults in British Columbia: suggested guidelines. Available at: http://www.phsa.ca/transcarebc/Documents/HealthProf/BC-Trans-Adult-Endocrine-Guidelines-2015.pdf.
124. Rainbow Health Ontario. Guidelines and protocols for hormone therapy and primary healthcare for trans clients. 2nd ed. Rainbow Health Ontario (2015).
125. Ziegler, E, Valaitis, R, Yost, J, Carter, N, and Risdon, C. Primary care is primary care: use of normalization process theory to explore the implementation of primary care services for transgender individuals in Ontario. PLoS One. (2019) 14:e0215873. doi: 10.1371/journal.pone.0215873
126. Marchildon, GP, Allin, S, and Merkur, S. Canada: health system review. Health Syst Transit. (2020) 22:i–194.
127. Allan, B, and Smylie, J. First peoples, second class treatment: the role of racism in the health and well-being of indigenous peoples in Canada. The Wellesley Institute. (2015). Available at: https://www.wellesleyinstitute.com/wp-content/uploads/2015/02/Summary-First-Peoples-Second-Class-Treatment-Final.pdf) Accessed April 24, 2022
128. National Collaborating Centre for Aboriginal Health. Understanding racism. Prince George, BC: National Collaborating Centre for Aboriginal Health (2013).
129. Firestone, M, Smylie, J, Maracle, S, Spiller, M, and O’Campo, P. Unmasking health determinants and health outcomes for urban first nations using respondent-driven sampling. BMJ Open. (2014) 4:e004978. doi: 10.1136/bmjopen-2014-004978
130. Paradies, Y. Colonisation, racism and indigenous health. J Popul Res. (2016) 33:83–96. doi: 10.1007/s12546-016-9159-y
131. Kurtz, DLM, Nyberg, JC, Van Den Tillaart, S, and Mills, B, Okanagan Urban Aboriginal Health Research Collective (OUAHRC). Silencing of voice: an act of structural violence: urban aboriginal women speak out about their experiences with health care. J Aborig Health. (2008) 4:53–63. doi: 10.18357/ijih41200812315
132. Tang, SY, and Browne, AJ. 'Race' matters: racialization and egalitarian discourses involving aboriginal people in the Canadian health care context. Ethn Health. (2008) 13:109–27. doi: 10.1080/13557850701830307
133. Browne, AJ, Smye, VL, Rodney, P, Tang, SY, Mussell, B, and O'Neil, J. Access to primary care from the perspective of aboriginal patients at an urban emergency department. Qual Health Res. (2011) 21:333–48. doi: 10.1177/1049732310385824
134. Brave Heart, MY. The historical trauma response among natives and its relationship with substance abuse: a Lakota illustration. J Psychoactive Drugs. (2003) 35:7–13. doi: 10.1080/02791072.2003.10399988
135. Hunt, S. An introduction to the health of two-spirit people: historical, contemporary, and emergent issues. Prince George, BC: National Collaborating Centre for Aboriginal Health (2016).
136. OUTSaskatoon. (2020). Two Spirit. Available at: https://www.outsaskatoon. (Accessed June 14, 2023)ca/two_spirit1.
137. Robinson, M. Two-Spirit and bisexual people: different umbrella, same rain. J Bisexuality. (2017) 17:7–29. doi: 10.1080/15299716.2016.1261266
138. Dykhuizen, M, Marshall, K, Loewen Walker, R, and Saddleback, J. Holistic health of two Spirit people in Canada: a call for nursing action. J Holist Nurs. (2022) 40:383–96. doi: 10.1177/08980101211072645
139. Scheim, AI, Jackson, R, James, L, Sharp Dopler, T, Pyne, J, and Bauer, GR. Barriers to well-being for aboriginal gender-diverse people: results from the Trans PULSE project in Ontario, Canada. Ethn Inequal Health Soc Care. (2013) 6:108–20. doi: 10.1108/EIHSC-08-2013-0010
140. House of Commons Standing Committee on Health. The health of LGBTQIA2 communities in Canada. Ottawa, ON: Parliament of Canada (2019).
141. Sekoni, AO, Gale, NK, Manga-Atangana, B, Bhadhuri, A, and Jolly, K. The effects of educational curricula and training on LGBT-specific health issues for healthcare students and professionals: a mixed-method systematic review. J Int AIDS Soc. (2017) 20:21624. doi: 10.7448/IAS.20.1.21624
142. Carabez, R, Mankovitz, A, Pellegrini, M, Eliason, M, Ciano, M, and Scott, M. Never in all my years…: Nurses' education about LGBT health. J Prof Nurs. (2015) 31:323–9. doi: 10.1016/j.profnurs.2015.01.003
143. Honigberg, MC, Eshel, N, Luskin, MR, Shaykevich, S, Lipsitz, SR, and Katz, JT. Curricular time, patient exposure, and comfort caring for lesbian, gay, bisexual, and transgender patients among recent medical graduates. LGBT Health. (2017) 4:237–9. doi: 10.1089/lgbt.2017.0029
144. Parameshwaran, V, Cockbain, BC, Hillyard, M, and Price, JR. Is the lack of specific lesbian, gay, bisexual, transgender and queer/questioning (LGBTQ) health Care education in medical school a cause for concern? Evidence from a survey of knowledge and practice among UK medical students. J Homosex. (2017) 64:367–81. doi: 10.1080/00918369.2016.1190218
145. Kitts, RL. Barriers to optimal care between physicians and lesbian, gay, bisexual, transgender, and questioning adolescent patients. J Homosex. (2010) 57:730–47. doi: 10.1080/00918369.2010.485872
146. Hinchliff, S, Gott, M, and Galena, E. I daresay I might find it embarrassing: general practitioners' perspectives on discussing sexual health issues with lesbian and gay patients. Health Soc Care Community. (2005) 13:345–53. doi: 10.1111/j.1365-2524.2005.00566.x
147. Stott, DB. The training needs of general practitioners in the exploration of sexual health matters and providing sexual healthcare to lesbian, gay and bisexual patients. Med Teach. (2013) 35:752–9. doi: 10.3109/0142159X.2013.801943
148. Nama, N, MacPherson, P, Sampson, M, and McMillan, H. Medical students’ perception of lesbian, gay, bisexual, and transgender (LGBT) discrimination in their learning environment and their self-reported comfort level for caring for LGBT patients: a survey study. Med Educ Online. (2017) 22:1368850. doi: 10.1080/10872981.2017.1368850
149. Carabez, R, Pellegrini, M, Mankovitz, A, Eliason, MJ, and Dariotis, WM. Nursing students' perceptions of their knowledge of lesbian, gay, bisexual, and transgender issues: effectiveness of a multi-purpose assignment in a public health nursing class. J Nurs Educ. (2015) 54:50–3. doi: 10.3928/01484834-20141228-03
150. Dixon-Woods, M, Regan, J, Robertson, N, Young, B, Cordle, C, and Tobin, M. Teaching and learning about human sexuality in undergraduate medical education. Med Educ. (2002) 36:432–40. doi: 10.1046/j.1365-2923.2002.01198.x
151. Rosen, R, Kountz, D, Post-Zwicker, T, Leiblum, S, and Wiegel, M. Sexual communication skills in residency training: the Robert Wood Johnson model. J Sex Med. (2006) 3:37–46. doi: 10.1111/j.1743-6109.2005.00135.x
152. Reygan, FC, and D'Alton, P. A pilot training programme for health and social care professionals providing oncological and palliative care to lesbian, gay and bisexual patients in Ireland. Psychooncology. (2013) 22:1050–4. doi: 10.1002/pon.3103
153. Dunjić-Kostić, B, Pantović, M, Vuković, V, Randjelović, D, Totić-Poznanović, S, Damjanović, A, et al. Knowledge: a possible tool in shaping medical professionals’ attitudes towards homosexuality. Psychiatr Danub. (2012) 24:143–51.
154. Sawning, S, Steinbock, S, Croley, R, Combs, R, Shaw, A, and Ganzel, T. A first step in addressing medical education curriculum gaps in lesbian-, gay-, bisexual-, and transgender-related content: the University of Louisville Lesbian, gay, bisexual, and transgender health certificate program. Educ Health (Abingdon). (2017) 30:108–14. doi: 10.4103/efh.EfH_78_16
155. Neville, S, and Henrickson, M. Perceptions of lesbian, gay and bisexual people of primary healthcare services. J Adv Nurs. (2006) 55:407–15. doi: 10.1111/j.1365-2648.2006.03944.x
156. Sabin, JA, Riskind, RG, and Nosek, BA. Health Care Providers' implicit and explicit attitudes toward lesbian women and gay men. Am J Public Health. (2015) 105:1831–41. doi: 10.2105/AJPH.2015.302631
157. Burke, SE, Dovidio, JF, Przedworski, JM, Hardeman, RR, Perry, SP, Phelan, SM, et al. Do contact and empathy mitigate Bias against gay and lesbian people among heterosexual first-year medical students? A report from the medical student CHANGE study. Acad Med. (2015) 90:645–51. doi: 10.1097/ACM.0000000000000661
158. Wilson, TD, and Brekke, N. Mental contamination and mental correction: unwanted influences on judgments and evaluations. Psychol Bull. (1994) 116:117–42. doi: 10.1037/0033-2909.116.1.117
159. Greenwald, AG, and Banaji, MR. Implicit social cognition: attitudes, self-esteem, and stereotypes. Psychol Rev. (1995) 102:4–27. doi: 10.1037/0033-295X.102.1.4
160. Bristol, S, Kostelec, T, and MacDonald, R. Improving emergency health care workers' knowledge, competency, and attitudes toward lesbian, gay, bisexual, and transgender patients through interdisciplinary cultural competency training. J Emerg Nurs. (2018) 44:632–9. doi: 10.1016/j.jen.2018.03.013
161. du Mont, J, Saad, M, Kosa, SD, Kia, H, and Macdonald, S. Providing trans-affirming care for sexual assault survivors: an evaluation of a novel curriculum for forensic nurses. Nurse Educ Today. (2020) 93:104541. doi: 10.1016/j.nedt.2020.104541
162. Maruca, AT, Diaz, DA, Stockmann, C, and Gonzalez, L. Using simulation with nursing students to promote affirmative practice toward the lesbian, gay, bisexual, and transgender population: a multisite study. Nurs Educ Perspect. (2018) 39:225–9. doi: 10.1097/01.NEP.0000000000000302
163. Vance, SR, Deutsch, MB, Rosenthal, SM, and Buckelew, SM. Enhancing pediatric trainees' and Students' knowledge in providing care to transgender youth. J Adolesc Health. (2017) 60:425–30. doi: 10.1016/j.jadohealth.2016.11.020
164. Wyckoff, ED. LGBT cultural competence of acute care nurses. J Nurses Prof Dev. (2019) 35:125–31. doi: 10.1097/NND.0000000000000524
165. Medina-Martínez, J, Saus-Ortega, C, Sánchez-Lorente, MM, Sosa-Palanca, EM, García-Martínez, P, and Mármol-López, MI. Health inequities in LGBT people and nursing interventions to reduce them: a systematic review. Int J Environ Res Public Health. (2021) 18:1–16. doi: 10.3390/ijerph182211801
166. Eriksson, SE, and Safer, JD. Evidence-based curricular content improves student knowledge and changes attitudes towards transgender medicine. Endocr Pract. (2016) 22:837–41. doi: 10.4158/EP151141.OR
167. Strong, KL, and Folse, VN. Assessing undergraduate nursing students’ knowledge, attitudes, and cultural competence in caring for lesbian, gay, bisexual, and transgender patients. J Nurs Educ. (2015) 54:45–9. doi: 10.3928/01484834-20141224-07
168. Thomas, DD, and Safer, JD. A simple intervention raised resident-physician willingness to assist transgender patients seeking hormone therapy. Endocr Pract. (2015) 21:1134–42. doi: 10.4158/EP15777.OR
169. Johnson, K, Rullo, J, and Faubion, S. Student-initiated sexual health selective as a curricular tool. Sex Med. (2015) 3:118–27. doi: 10.1002/sm2.57
170. Hardacker, CT, Rubinstein, B, Hotton, A, and Houlberg, M. Adding silver to the rainbow: the development of the nurses' health education about LGBT elders (HEALE) cultural competency curriculum. J Nurs Manag. (2014) 22:257–66. doi: 10.1111/jonm.12125
171. Greenwald, AG, Poehlman, TA, Uhlmann, EL, and Banaji, MR. Understanding and using the implicit association test: III. Meta-analysis of predictive validity. J Pers Soc Psychol. (2009) 97:17–41. doi: 10.1037/a0015575
172. Greenwald, AG, Banaji, MR, and Nosek, BA. Statistically small effects of the implicit association test can have societally large effects. J Pers Soc Psychol. (2015) 108:553–61. doi: 10.1037/pspa0000016
173. Blair, IV, Havranek, EP, Price, DW, Hanratty, R, Fairclough, DL, Farley, T, et al. Assessment of biases against Latinos and African Americans among primary care providers and community members. Am J Public Health. (2013) 103:92–8. doi: 10.2105/AJPH.2012.300812
174. Rowniak, SR. Factors related to homophobia among nursing students. J Homosex. (2015) 62:1228–40. doi: 10.1080/00918369.2015.1037135
175. Cornelius, JB, Enweana, I, Alston, CK, and Baldwin, DM. Examination of lesbian, gay, bisexual, and transgender health care content in North Carolina schools of nursing. J Nurs Educ. (2017) 56:223–6. doi: 10.3928/01484834-20170323-06
176. Society for Adolescent Health and Medicine. Recommendations for promoting the health and well-being of lesbian, gay, bisexual, and transgender adolescents: a position paper of the Society for Adolescent Health and Medicine. J Adolesc Health. (2013) 52:506–10. doi: 10.1016/j.jadohealth.2013.01.015
177. Aleshire, ME, Ashford, K, Fallin-Bennett, A, and Hatcher, J. Primary Care Providers’ attitudes related to LGBTQ people: a narrative literature review. Health Promot Pract. (2019) 20:173–87. doi: 10.1177/1524839918778835
178. Human Rights Campaign Foundation Healthcare equality index. (2022). Available at: https://www.hrc.org/resources/healthcare-equality-index (Accessed April 23, 2022).
179. National LGBTQIA+ health education center (a program of the Fenway institute). (2023). Available at: https://www.lgbtqiahealtheducation.org (Accessed April 13, 2022).
180. National LGBT Health Education Center. Learning to address implicit bias towards LGBTQ patients: case scenarios. Boston, MA: Fenway Institute (2018).
181. Vinjamuri, M. Using reflection and dialogue to prepare social work students for practice with LGBT populations: an emerging pedagogical model. J Gay Lesbian Soc Serv. (2017) 29:144–66. doi: 10.1080/10538720.2017.1295896
182. Rivers, B, and Swank, JM. LGBT ally training and counselor competency: a mixed-methods study. J LGBT Issues Couns. (2017) 11:18–35. doi: 10.1080/15538605.2017.1273162
183. Greenwald, AG, McGhee, DE, and Schwartz, JL. Measuring individual differences in implicit cognition: the implicit association test. J Pers Soc Psychol. (1998) 74:1464–80. doi: 10.1037/0022-3514.74.6.1464
184. Browne, AJ, Varcoe, C, Lavoie, J, Smye, V, Wong, ST, Krause, M, et al. Enhancing health care equity with indigenous populations: evidence-based strategies from an ethnographic study. BMC Health Serv Res. (2016) 16:544. doi: 10.1186/s12913-016-1707-9
185. Crameri, P, Barrett, C, Latham, JR, and Whyte, C. It is more than sex and clothes: culturally safe services for older lesbian, gay, bisexual, transgender and intersex people. Australas J Ageing. (2015) 34:21–5. doi: 10.1111/ajag.12270
186. McEldowney, R, and Connor, MJ. Cultural safety as an ethic of care: a praxiological process. J Transcult Nurs. (2011) 22:342–9. doi: 10.1177/1043659611414139
187. Berg, K, McLane, P, Eshkakogan, N, Mantha, J, Lee, T, Crowshoe, C, et al. Perspectives on indigenous cultural competency and safety in Canadian hospital emergency departments: a scoping review. Int Emerg Nurs. (2019) 43:133–40. doi: 10.1016/j.ienj.2019.01.004
188. Brooks-Cleator, L, Phillipps, B, and Giles, A. Culturally safe health initiatives for indigenous peoples in Canada: a scoping review. Can J Nurs Res. (2018) 50:202–13. doi: 10.1177/0844562118770334
189. Schreiber, M, Ahmad, T, Scott, M, Imrie, K, and Razack, S. The case for a Canadian standard for 2SLGBTQIA+ medical education. CMAJ. (2021) 193:E562–5. doi: 10.1503/cmaj.202642
190. Coren, JS, Coren, CM, Pagliaro, SN, and Weiss, LB. Assessing your office for care of lesbian, gay, bisexual, and transgender patients. Health Care Manag. (2011) 30:66–70. doi: 10.1097/HCM.0b013e3182078bcd
191. McClain, Z, Hawkins, LA, and Yehia, BR. Creating welcoming spaces for lesbian, gay, bisexual, and transgender (LGBT) patients: an evaluation of the health Care environment. J Homosex. (2016) 63:387–93. doi: 10.1080/00918369.2016.1124694
192. Ross, KA, and Castle Bell, G. A culture-centered approach to improving healthy trans-patient-practitioner communication: recommendations for practitioners communicating withTrans individuals. Health Commun. (2017) 32:730–40. doi: 10.1080/10410236.2016.1172286
193. German, D, Kodadek, L, Shields, R, Peterson, S, Snyder, C, Schneider, E, et al. Implementing sexual orientation and gender identity data collection in emergency departments: patient and staff perspectives. LGBT Health. (2016) 3:416–23. doi: 10.1089/lgbt.2016.0069
194. Stover, CM, Hare, P, and Johnson, M. Healthcare experiences of lesbian, gay, and bisexual college students: recommendations for the clinical nurse specialist. Clin Nurse Spec. (2014) 28:349–57. doi: 10.1097/NUR.0000000000000081
195. Brooks, H, Llewellyn, CD, Nadarzynski, T, Pelloso, FC, de Souza Guilherme, F, Pollard, A, et al. Sexual orientation disclosure in health care: a systematic review. Br J Gen Pract. (2018) 68:e187–96. doi: 10.3399/bjgp18X694841
196. Maragh-Bass, AC, Torain, M, Adler, R, Ranjit, A, Schneider, E, Shields, RY, et al. Is it okay to ask: transgender patient perspectives on sexual orientation and gender identity collection in healthcare. Acad Emerg Med. (2017) 24:655–67. doi: 10.1111/acem.13182
197. Guss, CE, Woolverton, GA, Borus, J, Austin, SB, Reisner, SL, and Katz-Wise, SL. Transgender Adolescents' experiences in primary care: a qualitative study. J Adolesc Health. (2019) 65:344–9. doi: 10.1016/j.jadohealth.2019.03.009
198. Dodge, B, Schnarrs, PW, Goncalves, G, Malebranche, D, Martinez, O, Reece, M, et al. The significance of privacy and trust in providing health-related services to behaviorally bisexual men in the United States. AIDS Educ Prev. (2012) 24:242–56. doi: 10.1521/aeap.2012.24.3.242
199. Herman, J. L. (2013). Gendered restrooms and minority stress: the public regulation of gender and its impact on transgender People’s lives. Available at: https://williamsinstitute.law.ucla.edu/publications/gendered-restrooms-minority-stress/ (Accessed March 28, 2022).
200. Lim, FA, Brown, DV, and Justin Kim, SM. Addressing health care disparities in the lesbian, gay, bisexual, and transgender population: a review of best practices. Am J Nurs. (2014) 114:24–34. doi: 10.1097/01.NAJ.0000450423.89759.36
201. Sullivan, KM. Acceptance in the domestic environment: the experience of senior housing for lesbian, gay, bisexual, and transgender seniors. J Gerontol Soc Work. (2014) 57:235–50. doi: 10.1080/01634372.2013.867002
202. McCalman, J, Jongen, C, and Bainbridge, R. Organisational systems’ approaches to improving cultural competence in healthcare: a systematic scoping review of the literature. Int J Equity Health. (2017) 16:78. doi: 10.1186/s12939-017-0571-5
203. Thompson, HM. Patient perspectives on gender identity data collection in electronic health records: an analysis of disclosure, privacy, and access to Care. Transgend Health. (2016) 1:205–15. doi: 10.1089/trgh.2016.0007
204. Bjarnadottir, RI, Bockting, W, and Dowding, DW. Patient perspectives on answering questions about sexual orientation and gender identity: an integrative review. J Clin Nurs. (2017) 26:1814–33. doi: 10.1111/jocn.13612
205. Brown, C, Frohard-Dourlent, H, Wood, BA, Saewyc, E, Eisenberg, ME, and Porta, CM. It makes such a difference: an examination of how LGBTQ youth talk about personal gender pronouns. J Am Assoc Nurse Pract. (2020) 32:70–80. doi: 10.1097/JXX.0000000000000217
206. Foster, Haidn. Gender pronouns: a Provider’s guide to referring to transgender patients. Pride in Practice Published February 11, 2019. Available at: https://www.prideinpractice.org/articles/transgender-pronouns-guide/ (Accessed April 25, 2022).
207. Rounds, KE, McGrath, BB, and Walsh, E. Perspectives on provider behaviors: a qualitative study of sexual and gender minorities regarding quality of care. Contemp Nurse. (2013) 44:99–110.
208. Rucker, AJ, Murray, A, Gaul, Z, Sutton, MY, and Wilson, PA. The role of patient-provider sexual health communication in understanding the uptake of HIV prevention services among black men who have sex with men. Cult Health Sex. (2018) 20:761–71. doi: 10.1080/13691058.2017.1375156
209. Lisy, K, Peters, MDJ, Schofield, P, and Jefford, M. Experiences and unmet needs of lesbian, gay, and bisexual people with cancer care: a systematic review and meta-synthesis. Psychooncology. (2018) 27:1480–9. doi: 10.1002/pon.4674
210. On behalf of the EQUIP Research TeamLavoie, JG, Varcoe, C, Wathen, CN, Ford-Gilboe, M, and Browne, AJ. Sentinels of inequity: examining policy requirements for equity-oriented primary healthcare. BMC Health Serv Res. (2018) 18:705. doi: 10.1186/s12913-018-3501-3
211. Butler, M, McCreedy, E, Schwer, N, Burgess, D, Call, K, Przedworski, J, et al. Improving Cultural Competence to Reduce Health Disparities [Internet]. Rockville (MD): Agency for Healthcare Research and Quality (US). (Comparative Effectiveness Reviews, No. 170.) (2016). Available at: https://www.ncbi.nlm.nih.gov/books/NBK361126/
212. Knaak, S, Mantler, E, and Szeto, A. Mental illness-related stigma in healthcare: barriers to access and care and evidence-based solutions. Healthc Manage Forum. (2017) 30:111–6. doi: 10.1177/0840470416679413
213. Clifford, A, McCalman, J, Bainbridge, R, and Tsey, K. Interventions to improve cultural competency in health care for indigenous peoples of Australia, New Zealand, Canada and the USA: a systematic review. Int J Qual Health Care. (2015) 27:89–98. doi: 10.1093/intqhc/mzv010
214. Truong, M, Paradies, Y, and Priest, N. Interventions to improve cultural competency in healthcare: a systematic review of reviews. BMC Health Serv Res. (2014) 14:99. doi: 10.1186/1472-6963-14-99
215. Browne, AJ, Varcoe, C, Ford-Gilboe, M, Nadine Wathen, C, Smye, V, Jackson, BE, et al. Disruption as opportunity: impacts of an organizational health equity intervention in primary care clinics. Int J Equity Health. (2018) 17:154. doi: 10.1186/s12939-018-0820-2
216. Nyblade, L, Stockton, MA, Giger, K, Bond, V, Ekstrand, ML, Lean, RM, et al. Stigma in health facilities: why it matters and how we can change it. BMC Med. (2019) 17:25. doi: 10.1186/s12916-019-1256-2
217. Ungar, T, Knaak, S, and Szeto, AC. Theoretical and practical considerations for combating mental illness Stigma in health Care. Community Ment Health J. (2016) 52:262–71. doi: 10.1007/s10597-015-9910-4
218. Celik, H, Lagro-Janssen, TALM, Widdershoven, GGAM, and Abma, TA. Bringing gender sensitivity into healthcare practice: a systematic review. Patient Educ Couns. (2011) 84:143–9. doi: 10.1016/j.pec.2010.07.016
219. Mittal, D, Sullivan, G, Chekuri, L, Allee, E, and Corrigan, PW. Empirical studies of self-Stigma reduction strategies: a critical review of the literature. Psychiatr Serv. (2012) 63:974–81. doi: 10.1176/appi.ps.201100459
220. Büchter, RB, and Messer, M. Interventions for reducing self-stigma in people with mental illnesses: a systematic review of randomized controlled trials. Ger Med Sci. (2017) 15:Doc07. doi: 10.3205/000248
221. Ma, PHX, Chan, ZCY, and Loke, AY. Self-Stigma reduction interventions for people living with HIV/AIDS and their families: a systematic review. AIDS Behav. (2019) 23:707–41. doi: 10.1007/s10461-018-2304-1
222. Tsang, HW, Ching, SC, Tang, KH, Lam, HT, Law, PYY, and Wan, CN. Therapeutic intervention for internalized stigma of severe mental illness: a systematic review and meta-analysis. Schizophr Res. (2016) 173:45–53. doi: 10.1016/j.schres.2016.02.013
223. Livingston, JD, Milne, T, Fang, ML, and Amari, E. The effectiveness of interventions for reducing stigma related to substance use disorders: a systematic review. Addiction. (2012) 107:39–50. doi: 10.1111/j.1360-0443.2011.03601.x
224. Chaudoir, SR, Wang, K, and Pachankis, JE. What reduces sexual minority stress? A review of the intervention "toolkit". J Soc Issues. (2017) 73:586–617. doi: 10.1111/josi.12233
225. Thornicroft, G, Mehta, N, Clement, S, Evans-Lacko, S, Doherty, M, Rose, D, et al. Evidence for effective interventions to reduce mental-health-related stigma and discrimination. Lancet. (2016) 387:1123–32. doi: 10.1016/S0140-6736(15)00298-6
226. Vlassoff, C, and Garcia Moreno, C. Placing gender at the Centre of Health Programming: challenges and limitations. Soc Sci Med. (2002) 54:1713–23. doi: 10.1016/S0277-9536(01)00339-2
227. World Health Organisation. (2007). Sixtieth world health assembly, Geneva, 14–23 may 2007: Summary Records of Committees: Reports of committees. World Health Organization. Available at: https://apps.who.int/iris/handle/10665/22640 (Accessed April 12, 2022).
228. Report of the fourth world conference on women (Beijing, 4–15 September 1995). United Nations, and platform for action plan 2000. United Nations publication No. 96.IV.13 (1995). Available at: https://www.un.org/womenwatch/daw/beijing/pdf/Beijing%20full%20report%20E.pdf (Accessed April 12, 2022).
229. Payne, S. Beijing fifteen years on: the persistence of barriers to gender mainstreaming in health policy. Soc Polit. (2011) 18:515–42. doi: 10.1093/sp/jxr019
230. Hay, K, McDougal, L, Percival, V, Henry, S, Klugman, J, Wurie, H, et al. Disrupting gender norms in health systems: making the case for change. Lancet. (2019) 393:2535–49. doi: 10.1016/S0140-6736(19)30648-8
231. Morgan, R, George, A, Ssali, S, Hawkins, K, Molyneux, S, and Theobald, S. How to do (or not to do)… gender analysis in health systems research. Health Policy Plan. (2016) 31:1069–78. doi: 10.1093/heapol/czw037
232. Gupta, GR, Oomman, N, Grown, C, Conn, K, Hawkes, S, Shawar, YR, et al. Gender equality and gender norms: framing the opportunities for health. Lancet. (2019) 393:2550–62. doi: 10.1016/S0140-6736(19)30651-8
233. Brouwers, R. Revisiting gender mainstreaming in international development: goodbye to an illusionary strategy, ISS working paper—General series 556. The Hague: International Institute of Social Studies of Erasmus University Rotterdam (2013).
234. Ravindran, TK, and Kelkar-Khambete, A. Gender mainstreaming in health: looking back, looking forward. Glob Public Health. (2008) 3:121–42.
235. Crespí-Lloréns, N, Hernández-Aguado, I, and Chilet-Rosell, E. Have policies tackled gender inequalities in health? A scoping review. Int J Environ Res Public Health. (2021) 18:1–12. doi: 10.3390/ijerph18010327
236. Weber, AM, Cislaghi, B, Meausoone, V, Abdalla, S, Mejía-Guevara, I, Loftus, P, et al. Gender norms and health: insights from global survey data. Lancet. (2019) 393:2455–68. doi: 10.1016/S0140-6736(19)30765-2
237. Heise, L, Greene, ME, Opper, N, Stavropoulou, M, Harper, C, Nascimento, M, et al. Gender inequality and restrictive gender norms: framing the challenges to health. Lancet. (2019) 393:2440–54. doi: 10.1016/S0140-6736(19)30652-X
238. Heymann, J, Levy, JK, Bose, B, Ríos-Salas, V, Mekonen, Y, Swaminathan, H, et al. Improving health with programmatic, legal, and policy approaches to reduce gender inequality and change restrictive gender norms. Lancet. (2019) 393:2522–34. doi: 10.1016/S0140-6736(19)30656-7
239. Blosnich, JR, Farmer, GW, Lee, JG, Silenzio, VM, and Bowen, DJ. Health inequalities among sexual minority adults: evidence from ten U.S. states. Am J Prev Med, 2014. (2010) 46:337–49. doi: 10.1016/j.amepre.2013.11.010
240. Tamargo, CL, Quinn, GP, Sanchez, JA, and Schabath, MB. Cancer and the LGBTQ population: quantitative and qualitative results from an oncology Providers' survey on knowledge, attitudes, and practice behaviors. J Clin Med. (2017) 6:1–13. doi: 10.3390/jcm6100093
241. Fredriksen-Goldsen, KI, Kim, HJ, Shui, C, and Bryan, AEB. Chronic health conditions and key health indicators among lesbian, gay, and bisexual older US adults, 2013–2014. Am J Public Health. (2017) 107:1332–8. doi: 10.2105/AJPH.2017.303922
242. Gilmour, H. Sexual orientation and complete mental health. Health Rep. (2019) 30:3–10. doi: 10.25318/82-003-x201901100001-eng
243. Scott, RL, Lasiuk, G, and Norris, CM. Sexual orientation and depression in Canada. Can J Public Health. (2017) 107:e545–9. doi: 10.17269/cjph.107.5506
Keywords: 2SLGBTQIA+ , health care, Canada, health inequities, determinants of health, gender, sexual minority
Citation: Comeau D, Johnson C and Bouhamdani N (2023) Review of current 2SLGBTQIA+ inequities in the Canadian health care system. Front. Public Health 11:1183284. doi: 10.3389/fpubh.2023.1183284
Received: 09 March 2023; Accepted: 03 July 2023;
Published: 18 July 2023.
Edited by:
Kath Woodward, The Open University, United KingdomReviewed by:
Sarah Ashley Job, University of Central Florida, United StatesCopyright © 2023 Comeau, Johnson and Bouhamdani. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Nadia Bouhamdani, bmFkaWEuYm91aGFtZGFuaUB2aXRhbGl0ZW5iLmNh
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.