
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health , 04 May 2023
Sec. Occupational Health and Safety
Volume 11 - 2023 | https://doi.org/10.3389/fpubh.2023.1169604
This article is part of the Research Topic Mental Health in Healthcare Workers and its Associations with Psychosocial Work Conditions View all 32 articles
A correction has been applied to this article in:
Corrigendum: “You knew you had to be there, it had to be done”: experiences of health professionals who faced the COVID-19 pandemic in one public hospital in Spain
Background: The purpose of the pilot study conducted by the authors was to assess occupational risk in selected areas of psychosocial risk factors among health professions in a pilot study. Medical staff working in the healthcare sector experience stress, job burnout and bullying on a daily basis. Monitoring occupational risks in the above areas provides an opportunity to take appropriate preventive measures.
Methods: The prospective online survey included 143 health care workers from various professional groups. Eighteen participants did not complete the survey, and the results of 125 participants were eventually included in the analysis. The study used health and safety questionnaires in the healthcare sector, which are not widely used as screening tools in Poland.
Results: The following statistical methods were performed in the study: the Mann-Whitney test, Kruskal-Wallis test, Dunn's test. In addition, multivariate analysis was performed. The results obtained in the study indicate that the questionnaires used in the study can be widely used by employers or occupational medicine as screening tools.
Conclusions: Our findings show that level of education attainment in healthcare is correlated with higher chance of experiencing stress and burnout. Among the surveyed professions, nurses reported a higher amount of stress and burnout. Paramedics reported the highest chance of being bullied at work. This can be explained by their nature of work which requires directly interacting with patients and their families. In addition, it should be noted that the tools used can be successfully applied in workplaces as elements of workplace ergonomics assessment in the context of cognitive ergonomics.
Ergonomic research indicates that there is a cause-and-effect relationship between workplace ergonomics and the ability of staff to work. It appears that there are few studies from the healthcare sector that address ergonomic aspects of stress, job burnout or bullying (1, 2).
Healthcare workers during their daily work can experience excessive physical and mental exhaustion. This is associated with adverse consequences including an increased risk of developing mental health conditions like anxiety and depression. Negative impacts of burnout on mental health of healthcare workers have been highlighted in recent studies and the importance of maintaining a balance between personal life and work has been discussed. Additionally, evidence shows improving workplace ergonomics can improve psychosocial working conditions and prevent burnout (3).
Ergonomics deals with matching the needs of a job with the capabilities of the worker and the work environment to ensure the most efficient workplace while reducing the risk of injury (4). In addition, it is emphasized that ergonomics is gaining increasing recognition as an integral part of the system for ensuring fitness for work in the medical professions as well (5). It is increasingly noted that among the risk factors in the workplace are psychosocial factors, which play a significant role in ensuring a safe workplace. Psychosocial factors fall into the area of cognitive ergonomics, which includes perception, memory, reasoning and motor responses. They are extremely important because they affect interactions between people and other elements of the human-environment system (6–8).
One predictor of mental health among medical personnel is occupational burnout syndrome, which was defined in the 1970s by psychoanalyst Freudenberger (9–11). Occupational burnout is included in the 11th Revision of the International Classification of Diseases (ICD-11) as an occupational phenomenon—although it is not classified as a medical condition. It is defined as a conceptualized syndrome resulting from chronic workplace stress that has not been effectively managed. It is characterized by three dimensions: feelings of energy depletion or exhaustion, increased mental distance from one's job or feelings of negativity or cynicism about one's work, and decreased professional effectiveness (12). The scale of professional burnout is enormous. The results of studies conducted for years in the US indicate that professional burnout can affect up to 51% of doctors (13). Among nurses, the scale of the phenomenon is even greater, as globally professional burnout is said to be 15–60%, and in developed countries 49–57% (14, 15). Occupational burnout is strongly influenced by long-lasting stress levels, which among the medical profession are also very high (16).
Both stress and job burnout can influence the occurrence of bullying. Bullying in the workplace is a destructive phenomenon and disrupts the sense of security (17). It turns out that the phenomenon of bullying among medical professions is most prevalent in the professional group of nurses. They experience both verbal and physical violence (18). Rates of physical violence against doctors and nurses are 16.2 per 1,000 and 21.9 per 1,000, respectively. In the European Union, 52% of health care workers have experienced some type of aggression at work (19).
A review of the literature indicates that both occupational stress and burnout and bullying are common in the health care system. It is therefore important to monitor risk factors in this area. The authors attempted to assess occupational risk, additionally during the burden of the COVID-19 pandemic, which may have been an additional aggravating factor.
The purpose of the study conducted by the authors was to assess occupational risk in selected areas of psychosocial risk factors among health professions in a pilot study.
The prospective survey was conducted from November 1, 2021, to December 31, 2021, during the COVID-19 pandemic. The survey was conducted in an online format, using the electronic survey platform www.webankieta.pl. The survey is consisted of two parts:
a) Socio-demographic information of participants.
b) Participants' assessments of psychosocial risk factors.
The psychosocial risk factors section goes over three major themes and ach theme is consisted of 15 questions which are adopted from the European Commission's guide to health and safety risks in the healthcare sector [Europejska (20); the English-language version of the manual with questionnaires for each dimension of psychosocial factors can be found at the link: https://www.ilo.org/dyn/travail/docs/1965/osh.pdf]:
a) Workplace stresses;
b) Work related burnout;
c) Bullying at workplace.
Surveys chose either “applicable” or “not applicable” in response to psychosocial risk factors' questions. We used the aggregated scores to asses the severity of psychosocial risks. The risk levels were defined as follows:
a) no risk (1–5 marked answers “applicable”)—the need to take action on individual elements.
b) increased risk (6–10 marked “applicable” answers)—structural and control analyses are recommended.
c) high risk (11–15 marked “applicable” answers)—need for urgent structural and control analyses.
The survey was distributed to medical staff at the Wroclaw University of Medical Sciences including physicians, dentists, nurses, midwives, paramedics, and physiotherapists. Potential participants received a link to the survey through their medical social media groups. Participation in the survey was voluntary and data was collected anonymously. Participants could withdraw anytime. An IP address filtering (a numerical identifier given to a network interface) was used to avoid collecting duplicate responses from a participants.
After data collection was completed, a database was prepared and used in the statistical analysis.
The inclusion criterion for this study was active practice of a medical profession at the time of the survey, i.e., November–December 2021, during the COVID-19 pandemic. The study targeted 143 potential participants and 18 of them did not complete the survey. Uncomplete results were excluded from statistical analysis.
The study was carried out in accordance with the tenets of the Declaration of Helsinki and guidelines of Good Clinical Practice (21). Written information about the study was provided as an introduction to the survey, with an emphasis on the voluntary and anonymous nature of participation and its guaranteed confidentiality. By answering the questionnaire, participants gave their consent to participate in the study. The research project was approved by the Independent Bioethics Committee at the Wroclaw Medical University (No. KB−613/2021).
Quantitative analysis was carried out by calculating the mean, standard deviation, median, and quartiles. Additionally, nominal variables were subjected to prevalence analysis based on the number and percentage of occurrences of each value. Comparison of the values of quantitative variables in the two groups was performed using the Mann-Whitney test. Comparison of the values of quantitative variables in three or more groups was performed using the Kruskal-Wallis test. When statistically significant differences were detected, post-hoc analysis was performed with Dunn's test to identify statistically significantly different groups. Multivariate analysis of the effect of multiple variables on a quantitative variable was performed using linear regression. The results are presented in the form of regression model parameter values with 95% confidence intervals. The analysis assumed a significance level of 0.05. So, all p-values below 0.05 were interpreted as indicating significant relationships. The analysis was performed in R software, version 4.2.2 (22).
The characteristics of the study group with detailed socio-demographic data are presented in Table 1. A general summary of the level of risk identified in the three areas studied is presented in Table 2. Based on the results of Table 2, it should be noted most of the participants reported a high risk in all three areas, experiencing stress, burnout syndromes, and bullying- 63.2, 65.6, and 50.4%, respectively. These results are very disturbing, considering that the average age of the respondents was 32.1 years (Me = 30), and more than half of the respondents (57.6%) described their length of service as between 1 and 5 years. These shows relatively young people, at the beginning of their careers, experiencing high levels of risk from the group of psychosocial factors.
After determining the overall level of risk, a detailed analysis of socio-demographic data in correlation with the studied areas of psychosocial factors was performed. Those socio-demographic parameters with statistically significant differences (p < 0.05) were analyzed in detail. Among others, the level of education was included in the analysis (Table 3), and it was revealed that the risk in the area of stress is significantly higher in those with a bachelor's or master's degree than in those with a high school education. In addition, the risk in the area of burnout is significantly higher in those with a bachelor's or master's degree than in those with a high school education. It should be noted that in the case of the correlation of stress and level of education, this applies mainly to the nurses. The reasons for such a correlation can be explained by the number of duties and managerial activities. Nurses with higher education very often have professional roles with greater responsibilities. Therefore, the risk of burnout among those healthcare workers may be higher. Interestingly, the risk in the area of stress is significantly higher among those with work experience of 6–10 years than other groups (Table 4). In contrast, the risk in the area of burnout is significantly lower among the group working 20–39 h/week than in the other groups (Table 5). It can conclude that standard working hours (i.e., about 40 h/week) are the most optimal, and that overtime/additional employment can result in job burnout. This is explained further in the following in the next analysis—in terms of risk in the area of stress, burnout, bullying, which is significantly higher among those who work in multiple positions (Table 6).
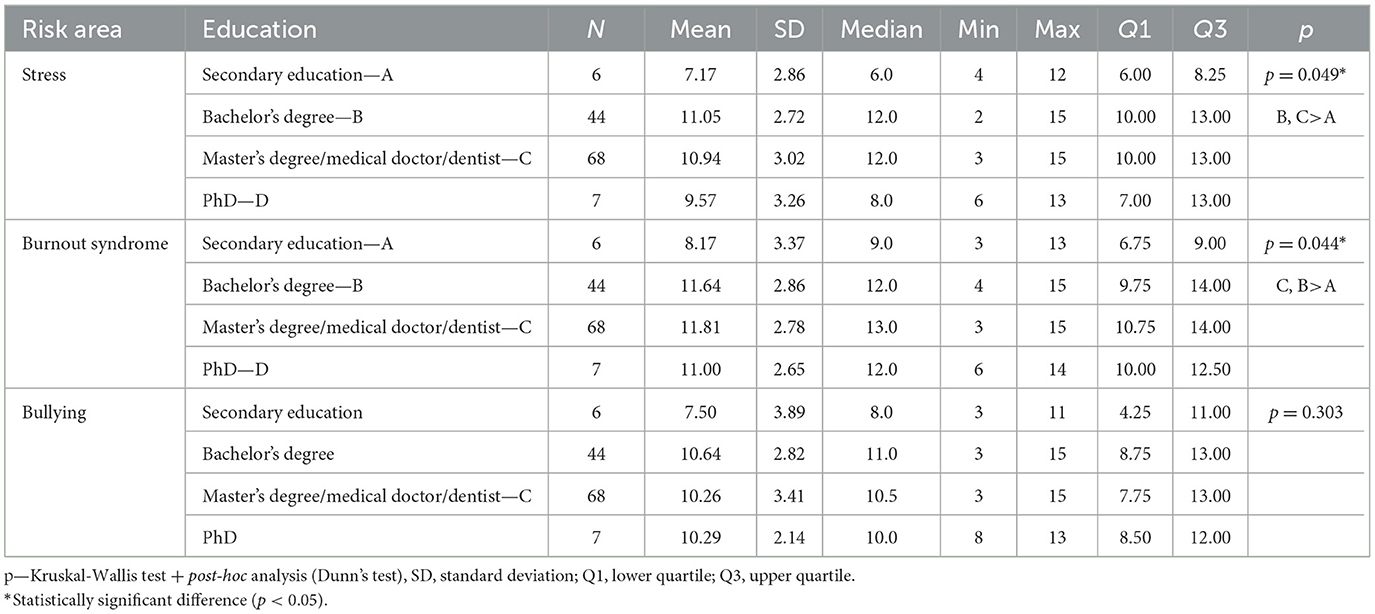
Table 3. Influence of education level on the incidence of stress risk, occupational burnout syndrome, and bullying.
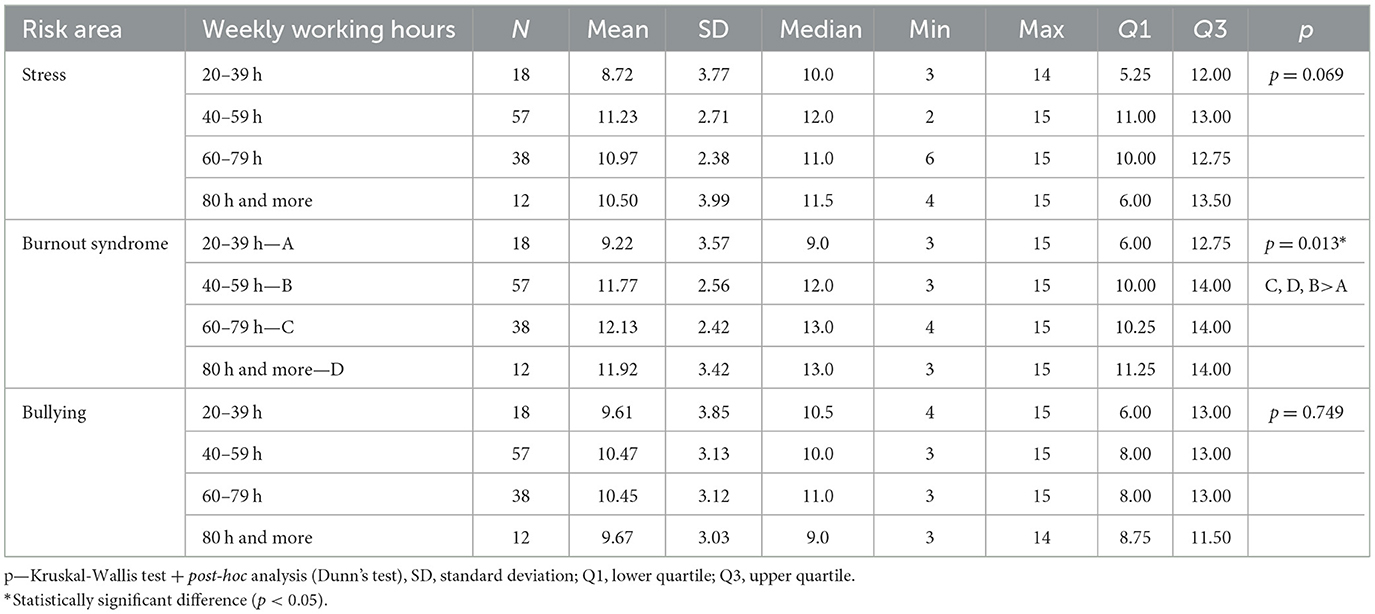
Table 5. The impact of weekly working hours on the incidence of stress risk, burnout syndrome, and bullying.
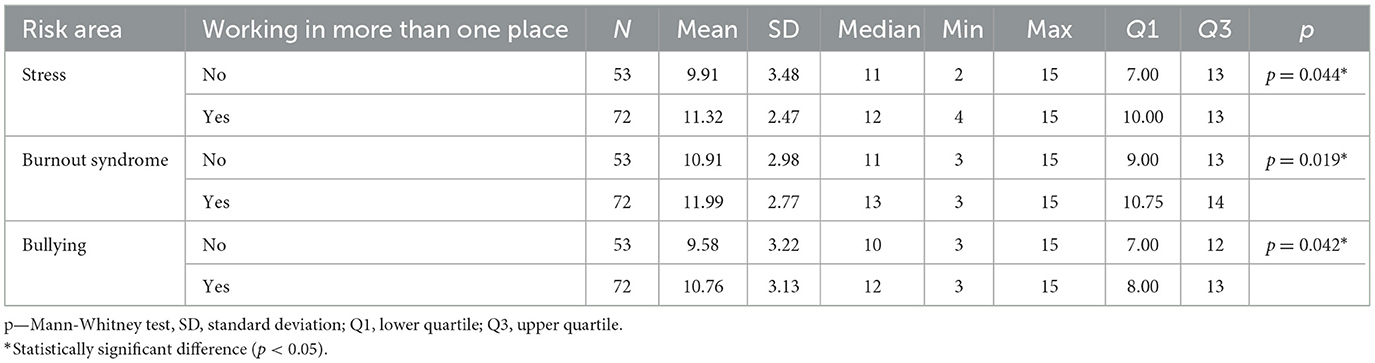
Table 6. The impact of working more than one job on the incidence of stress risk, burnout syndrome, and bullying.
In the areas discussed, the variable “gender” showed no statistically significant differences.
The next step was multivariate analyses. Included in these analyses were those variables that had a significant effect on a given risk area in the univariate analyses or were close to significance (i.e., had p < 0.1), as well as occupational group, which is the main variable in this analysis.
A multivariate linear regression model showed that significant (p > 0.05) independent predictors of risk in the area of stress are (Table 7):
a) Bachelor's degree: the regression parameter is 4.53, so it raises the risk by an average of 4.53 points relative to high school education.
b) Master's degree/doctor/dentist: The regression parameter is 4.91, so it raises the risk by an average of 4.91 points relative to secondary education.
c) Work experience of 6–10 years: the regression parameter is 3.17, so it raises the risk by an average of 3.17 points relative to < 1 year's experience.
d) Weekly working hours of 40–59 h: the regression parameter is 2.13, so it raises the risk by 2.13 points on average relative to working < 40 h/week.
e) Weekly working hours of 80 h or more: the regression parameter is 2.15, so it raises the risk by an average of 2.15 points relative to working < 40 h/week.
f) Working in more than one place: The regression parameter is 1.10, so it raises the risk by 1.10 points on average.
The correlations shown in the stress dimension that relate to educational level may be due to the fact that the vast majority of people have higher education. There are still nurses working in the health care system who have graduated from specialized schools—medical high schools. Medical personnel with master's degrees are more likely than those with bachelor's degrees to hold management positions, which further translates into higher stress levels. In turn, the weekly working hours—the greater, the higher the stress level is also a result of the fact that medical personnel often work in more than one place. Such behavior can determine a significant mental as well as physical burden. It should also be noted that the study was conducted during the pandemic period, when there was a shortage of staff, people worked beyond the norm to provide medical care to the needy.
In terms of burnout, a multivariate linear regression model showed that significant (p > 0.05) independent predictors of risk in this area are (Table 8):
a) Bachelor's degree: the regression parameter is 4.42, so it raises the risk by an average of 4.42 points relative to high school education.
b) Master's degree/doctor/dentist: The regression parameter is 5.05, so it raises the risk by an average of 5.05 points relative to secondary education.
c) Doctoral degree: The regression parameter is 3.59, so it raises the risk by an average of 3.59 points relative to secondary education.
d) Weekly working hours of 40–59 h: the regression parameter is 1.84, so it raises the risk by 1.84 points on average relative to working < 40 h/week.
e) Weekly working hours 60–79 h: The regression parameter is 2.21, so it raises the risk by an average of 2.21 points relative to working < 40 h/week.
f) Weekly working hours of 80 h or more: the regression parameter is 3.18, so it raises the risk by an average of 3.18 points relative to working < 40 h/week.
g) Place of employment other than a hospital: the regression parameter is −1.44, so it lowers the risk by an average of 1.44 points relative to hospital employment.
The problem of burnout among medical staff is widely studied. It is influenced by several factors: medics work too much (more than 40 h a week, in more than one place), we have a shortage of medical personnel (significant workload, rationing of care) and there is a lack of prevention in this area. Employers do not take measures to counteract professional burnout, and prc medicine does not give this problem the attention it deserves.
In terms of bullying, a multivariate linear regression model showed that significant (p > 0.05) independent predictors of risk in this area are (Table 9):
a) Practicing as a paramedic: The regression parameter is 2.11, so it raises the risk by an average of 2.11 points relative to the nursing/midwifery profession.
b) Working in more than one place: The regression parameter is 1.39, so it raises the risk by 1.39 points on average.
Experiencing violence by medical personnel, especially during a pandemic, was not unusual. It was related to fear of the SARS-CoV-2 virus, the consequences of COVID-19 disease or fear for the health of their loved ones. People in highly stressful situations behave irrationally which may be related to the results of the study. It should be noted that medical personnel very often experience violence—both psychological (such as verbal) and physical. Paramedics, are the people who are on the front line at accidents or in hospital emergency departments. They often have to deal with patients who are under the influence of psychoactive substances, which can potentiate aggressive behavior.
Medical staff are an essential part of the healthcare system, without them the provision of medical care is impossible. A safe and healthy workplace is critical to maintaining the mental health of healthcare workers. It is the resultant of ergonomic conditions and principles in the workplace. Ensuring the above is not possible without monitoring occupational risks in selected areas. The authors of the minor paper decided to focus on selected factors from the area of psychosocial factors, and the study was carried out during the period of increased tension, stress or fear caused by the COVID-19 pandemic.
The results revealed a significant problem likely associated with the absence of coping strategies for psychosocial risk factors. With respect to stress, burnout, and bullying, over half of respondents were in the high-risk group −63.2, 65.6, and 50.4% of respondents, respectively.
Our research shows that burnout is common amongst health care workers treating patients with COVID-19. Age, gender, category of employment and place of practice contribute to the level of employee burnout (23). The study found that medical staff with higher levels of educational attainment are more likely to suffer from burnout syndrome than those with high school education.
Sirilla (24) showed that the level of burnout recorded in oncology nurses was inversely proportional to the level of education—the higher the level of education, the lower the level of burnout. Grisales-Romero et al. (25) exhibited a similar relationship. Moreover, Lou et al. showed that during the COVID-19 pandemic, nurses experienced more stress than doctors (26).
Another factor which may increase the risk of stress or burnout is workload—in terms of hours. Second jobs can increase the risk to mental health. Stehman's work points out that working more than 40 h per week, being on call or working at night can greatly accelerate the burnout process (27).
Stress and burn-out can be linked to bullying, which can lead to verbal and physical abuse. The results of the multivariate analysis showed that practice in the paramedic profession and working in more than one location are associated with a higher risk of workplace bullying. Campo's study found that 46.6% of paramedics believe they have been verbally abused in the past year, and nearly 18% have reported being bullied which is a low percentage of total incidents (28).
European Agency for Safety and Health at Work (EU-OSHA) highlights psychosocial risks, which can result, for example, from poor work planning, poor work organization and management, and an unfavorable social work environment. Psychosocial hazards can lead to negative mental, physical and social effects, such as work-related stress, burnout or depression (29). The European Agency for Safety and Health at Work (EU-OSHA) has commissioned a Flash Eurobarometer survey in April 2022 to obtain more information on the state of OSH in post-pandemic workplaces, including psychosocial risk factors. EU-OSHA has commissioned a Flash Eurobarometer survey in April 2022 to obtain more information on the state of OSH in post-pandemic workplaces, including psychosocial risk factors. Respondents to the survey (46% of those surveyed) indicated that they are exposed to severe time pressure or work overload, with the experience of violence or verbal abuse from patients mentioned by 16% of respondents across the EU. Interestingly, employees from countries such as Finland, Malta, Sweden and Denmark were more likely than Poles to discuss their mental health with their employer. More than 4 in 10 respondents across the EU agree that their stress at work has increased as a result of the COVID-19 pandemic (30). The above findings correspond with the results obtained in this study. The pandemic has contributed to an increase in psychosocial burden among workers, including those in the healthcare sector.
Our findings show that level of education attainment in healthcare is correlated with higher chance of experiencing stress and burnout. Among the surveyed professions, nurses reported a higher amount of stress and burnout. Paramedics reported the highest chance of being bullied at work. This can be explained by their nature of work which requires directly interacting with patients and their families.
Considering the high rate of reported stress, burnout, and bullying among healthcare workers, it is important to increase awareness of the staff about psychosocial risk factors occupational risks. Considering the current shortage of human resources and increasing demand of aging population in west for healthcare related services, investing in educational programs for medical staff to make them familiar with strategies for managing occupational stress, burnout, and bullying can result in better less turnover of the staff, better mental health, and eventually better patient outcome. Additionally, investing in workplace management enhancement programs and improving ergonomics can prepare us for next potential pandemic and improve medical staff work satisfaction.
Practical implications for employers in the health care sector. A small pilot study has shown that questionnaires for assessing psychosocial risk factors in the areas of stress, occupational burnout and violence can be used in workplaces as screening tools for preventive measures against the mental health of health care workers. Based on the results obtained, corrective measures can be implemented in the areas of stress re-education, occupational burnout or violence prevention. Studies show that workplace ergonomics has a huge impact on the health of employees, and it is the employer's responsibility to provide safe working conditions. This is especially important at a time when the health care system is facing a major challenge—an increase in demand for medical care and a shortage of medical staff.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
ŁR and AK: conceptualization. ŁR: methodology, software, formal analysis, visualization, project administration, and supervision. ŁR and HS: validation. PG: investigation. ŁR and PG: resources. ŁR, IW, and HS: data curation and writing—original draft preparation. ŁR, AK, and HS: writing—review and editing. ŁR, IW, AK, and PG: funding acquisition. All authors contributed to the article and approved the submitted version.
This study was funded by internal resources: SUBZ.E260.23.023 and SUBZ.E060.23.037.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Haji L, arimi H, Valizadeh N. The effect of ergonomics on the occupational burnout, stress, and productivity of agricultural expert (the case of Kerman Province). Iran J Agric Econ Dev Res. (2022) 53:431–46. doi: 10.22059/ijaedr.2021.327963.669068
2. Batool Z, Younis MW, Yasir A, Rehman AU, Dilawar M, Yasin M, et al. Effects of safety pattern, cabin ergonomics, and sleep on work-related stress and burnout of city and transit bus drivers in Lahore, Pakistan. Ergonomics. (2022) 65:704–18. doi: 10.1080/00140139.2021.1983029
4. Edwards C, Fortingo N, Franklin E. Ergonomics: StatPearls Treasure Island (FL): StatPearls Publishing (2022).
5. Betsch D, Gjerde H, Lewis D, Tresidder R, Gupta RR. Ergonomics in the operating room: it doesn't hurt to think about it, but it may hurt not to! Can J Ophthalmol. (2020) 55(Suppl. 1):17–21. doi: 10.1016/j.jcjo.2020.04.004
6. Kedzior K. Introduction to human factors and ergonomics. Int J Occup Saf Ergon. (2018) 28:1980. doi: 10.1080/10803548.2018.1463724
7. Wilson JR. Fundamentals of systems ergonomics/human factors. Appl Ergon. (2014) 45:5–13. doi: 10.1016/j.apergo.2013.03.021
8. Dul J, Bruder R, Buckle P, Carayon P, Falzon P, Marras WS, et al. A strategy for human factors/ergonomics: developing the discipline and profession. Ergonomics. (2012) 55:377–95. doi: 10.1080/00140139.2012.661087
9. De Hert S. Burnout in Healthcare Workers: Prevalence, Impact and Preventative Strategies. Local Reg Anesth. (2020) 13:171–83.
10. Reith TP. Burnout in United States Healthcare Professionals: A Narrative Review. Cureus. (2018) 10:e3681. doi: 10.7759/cureus.3681
11. Galanis P, Vraka I, Fragkou D, Bilali A, Kaitelidou D. Nurses' burnout and associated risk factors during the COVID-19 pandemic: a systematic review and meta-analysis. J Adv Nurs. (2021) 77:3286–302. doi: 10.1111/jan.14839
12. WHO. Available online at: https://www.who.int/news/item/28-05-2019-burn-out-an-occupational-phenomenon-international-classification-of-diseases (accessed January 15, 2023).
13. Medscape Lifestyle Report 2017: Race Ethnicity Bias Burnout. (2017). Available online at: https://www.medscape.com/features/slideshow/lifestyle/2017/overview (accessed May 31, 2018).
14. Udho S, Kabunga A. Burnout and associated factors among hospital-based nurses in Northern Uganda: a cross-sectional survey. BioMed Res Int. (2022) 2022:8231564. doi: 10.1155/2022/8231564
15. Raudenská J, Steinerová V, Javurková A, Urits I, Kaye AD, Viswanath O, et al. Occupational burnout syndrome and post-traumatic stress among healthcare professionals during the novel coronavirus disease 2019 (COVID-19) pandemic. Best Pract Res Clin Anaesthesiol. (2020) 34:553–60. doi: 10.1016/j.bpa.2020.07.008
16. Walton M, Murray E, Christian MD. Mental health care for medical staff and affiliated healthcare workers during the COVID-19 pandemic. Eur Heart J Acute Cardiov Care. (2020) 9:241–7. doi: 10.1177/2048872620922795
17. Arnetz JE, Fitzpatrick L, Cotten SR, Jodoin C, Chang CD. Workplace bullying among nurses: developing a model for intervention. Violence Vict. (2019) 34:346–62. doi: 10.1891/0886-6708.VV-D-17-00211
18. Al-Qadi MM. Workplace violence in nursing: a concept analysis. J Occup Health. (2021) 63:e12226. doi: 10.1002/1348-9585.12226
19. Ariza-Montes A, Muniz NM, Montero-Simó MJ, Araque-Padilla RA. Workplace bullying among healthcare workers. Int J Environ Res Public Health. (2013) 10:3121–39. doi: 10.3390/ijerph10083121
20. Europejska K. Dyrekcja Generalna ds. Zatrudnienia, Spraw Społecznych i Właczenia Społecznego, Zagrozenia w zakresie bezpieczeństwa i higieny pracy w sektorze opieki zdrowotnej, Urzad Publikacji (2014). Available online at: https://data.europa.eu/doi/10.2767/78406 (accessed January 15, 2023).
21. World Medical Association. World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA (2013) 310:2191–4. doi: 10.1001/jama.2013.281053
22. R Core Team. R: A Language Environment for Statistical Computing. R Foundation for Statistical Computing, Vienna (2022). Available online at: https://www.R-project.org/ (accessed January 15, 2023).
23. Jalili M, Niroomand M, Hadavand F, Zeinali K, Fotouhi A. Burnout among healthcare professionals during COVID-19 pandemic: a cross-sectional study. Int Arch Occup Environ Health. (2021) 94:1345–52. doi: 10.1007/s00420-021-01695-x
24. Sirilla J. Moral distress in nurses providing direct care on inpatient oncology units. Clin J Oncol Nurs. (2014) 18(Suppl. 5):536–41. doi: 10.1188/14.CJON.536-541
25. Grisales-Romero H, Muñoz Y, Osorio D, Robles E. Síndrome de Burnout en el personal de enfermería de un hospital de referencia Ibagué, Colombia 2014. Enferm Glob. (2016) 41(Suppl. 1):244–57. doi: 10.6018/eglobal.15.1.212851
26. Lou NM, Montreuil T, Feldman LS, Fried GM. Nurses' and physicians' distress, burnout, and coping strategies during COVID-19: stress and impact on perceived performance and intentions to quit. J Cont Educ Health Prof . (2022) 42:e44–e52. doi: 10.1097/CEH.0000000000000365
27. Stehman CR, Testo Z, Gershaw RS, Kellogg AR. Burnout, drop out, suicide: physician loss in emergency medicine, part I. West J Emerg Med. (2019) 20:485–94. doi: 10.5811/westjem.2019.4.40970
28. Campo VR, Klijn TP. Verbal abuse and mobbing in pre-hospital care services in Chile. Rev Lat Am Enfermagem. (2018) 25:e2956. doi: 10.1590/1518-8345.2073.2956
29. Website of European Agency for Safety and Health at Work. Available online at: https://osha.europa.eu/pl/themes/psychosocial-risks-and-stress (accessed January 15, 2023).
Keywords: risk factors, medical staff, ergonomics, working condition, safety
Citation: Rypicz Ł, Witczak I, Gawłowski P, Salehi HP and Kołcz A (2023) Assessment of selected psychosocial risk factors: stress, job burnout, and bullying in the case of medical staff as part of workplace ergonomics during the COVID-19 pandemic—A prospective pilot study. Front. Public Health 11:1169604. doi: 10.3389/fpubh.2023.1169604
Received: 19 February 2023; Accepted: 11 April 2023;
Published: 04 May 2023.
Edited by:
Yong Shian Shawn Goh, National University of Singapore, SingaporeReviewed by:
Assis Kamu, Universiti Malaysia Sabah, MalaysiaCopyright © 2023 Rypicz, Witczak, Gawłowski, Salehi and Kołcz. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Łukasz Rypicz, bHVrYXN6LnJ5cGljekB1bXcuZWR1LnBs
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.