
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health , 16 June 2023
Sec. Aging and Public Health
Volume 11 - 2023 | https://doi.org/10.3389/fpubh.2023.1168792
 Xue-zhai Zeng1
Xue-zhai Zeng1 Ling-bing Meng1
Ling-bing Meng1 Na Jia1
Na Jia1 Jing Shi2
Jing Shi2 Chi Zhang3
Chi Zhang3 Ying-ying Li1
Ying-ying Li1 Xing Hu4
Xing Hu4 Jia-bin Hu4
Jia-bin Hu4 Jian-yi Li1
Jian-yi Li1 Di-shan Wu1
Di-shan Wu1 Hui Li1
Hui Li1 Xin Qi1
Xin Qi1 Hua Wang1
Hua Wang1 Qiu-xia Zhang5
Qiu-xia Zhang5 Juan Li6
Juan Li6 De-ping Liu1
*
De-ping Liu1
*Objective: Frailty increases adverse clinical outcomes in older patients with cardio-cerebral vascular disease (CCVD). The aim of this study was to investigate the prevalence of frailty and pre-frailty in older adults with CCVD in China and the factors associated with it.
Research design and methods: In this cross-sectional study, we used data from the fourth Sample Survey of Aged Population in Urban and Rural China. We used the frailty index for frailty and pre-frailty assessment, and the diagnosis of CCVD in older adults was self-reported.
Results: A total of 53,668 older patients with CCVD were enrolled in the study. The age-standardized prevalence of frailty and pre-frailty in older patients with CCVD was 22.6% (95% CI 22.3–23.0%) and 60.1% (95% CI 59.7–60.5%). Multinomial logistic regression analyses showed that being female, increasing age, rural residence, illiteracy, widowhood, ethnic minority, living alone, no health screening during the last year, hospitalization during the last year, difficult financial status, comorbid chronic conditions, and disability in activities of daily living were associated with frailty and pre-frailty in older patients with CCVD.
Conclusion: CCVD is strongly associated with frailty and pre-frailty in older Chinese people, and assessment of frailty should become routine in the management of older CCVD patients. Appropriate public health prevention strategies should be developed based on identified risk factors for frailty in older CCVD patients, which can help prevent, ameliorate or reverse the development of frailty in CCVD in the older population.
The seventh national population census in China conducted in 2020 showed that the population aged 60 or above was 264.02 million, representing 18.70%, up 5.44 percentage points from 2010, indicating that China has entered an aging society and the rate of aging is accelerating (1). With the advent of an aging population, the prevalence of cardio-cerebral vascular disease (CCVD) in China is on the rise, and the Cardiovascular Health and Diseases Report in China 2021 estimates that 330 million people have CCVD, and mortality from CCVD is the number one cause of death in both urban and rural areas, at 46.74% in rural areas and 44.26% in urban areas, it is higher than tumors and other diseases (2). CCVD imposes a heavy economic burden on the older adults and society, and has become a major public health problem. Frailty is a common geriatric syndrome, a clinical state that reflects heterogeneity between biological and chronological age due to a decrease in the physiological reserve and function of multiple systems resulting in a diminished ability of the organism to maintain homeostasis, an increased vulnerability of the organism and a diminished resistance to stress (3–6). Studies have shown a weighted prevalence of 11% (range 4–59%) for frailty in community-dwelling older adults (7). Frail older adults are at significantly increased risk for falls, disability, hospitalization, and death, and increase the burden on societal health care resources (3, 8, 9). Studies have shown that the prevalence of frailty in older adults with CCVD ranges from 10 to 60%, with a significant increase in adverse outcome events in older adults with frailty compared to those without frailty (10–13). In clinical practice, frail patients with CCVD require an individualized approach and optimized treatment decisions (14, 15). Early recognition of frailty is crucial to prevent the development of disability, dependence on others and a reduced quality of life (13). In order to reduce the burden of frailty in older patients with CCVD, corresponding public health policies are urgently needed, but the study of frailty in China started late, and there are few studies on the prevalence of frailty in older patients with CCVD. Our study aimed to analyze the prevalence of frailty and pre-frailty and related factors in older patients with CCVD in China, using data from the 4th Sample Survey of Aged Population in Urban and Rural China (SSAPUR) in 2015. The results of our study can provide valuable information for the prevention and treatment of frailty in older patients with CCVD.
In this cross-sectional study, we used data from the fourth SSAPUR, in which a total of 224,142 older adults aged 60 years or older from 31 provinces/municipalities/autonomous regions in mainland China participated from 1 August 2015 to 31 August 2015. The survey used a comprehensive sampling method with stratified, multi-stage, size-proportional probability sampling and an equal-probability sampling design at the final stage to ensure the representativeness of the national older population. The sample size was allocated according to the proportion of the older population in each provinces/municipalities/autonomous regions in mainland China, and 462 counties were finally selected. From each county, four towns were selected and from each town, four communities were selected. Finally, 30 older people were selected from each community using an equidistant sampling method. The data collected through household interviews and questionnaires provided valuable insights into the living conditions of older people. More detailed information on the survey design and sampling methods can be found in previous studies (16–18). We use the frailty index (FI) to assess the frailty status of older adults. Exclusion criteria for this study: 15,756 participants out of 224,142 older adults who participated in the fourth SSAPUR were excluded because less than 28/33 items were used to construct the FI, and 154,718 older adults without a history of CCVD were excluded out of the remaining 208,386 older adults. Inclusion criteria for this study: older adults with self-reported CCVD and ≥ 28/33 items used to construct FI, a total of 53,668 older patients with CCVD were enrolled in this study (Figure 1). The study protocol was approved by the National Bureau of Statistics (No. [2014] 87) and the Beijing Hospital Ethics Committee (2021BJYYEC-294-01). Written informed consent was provided by all participants.
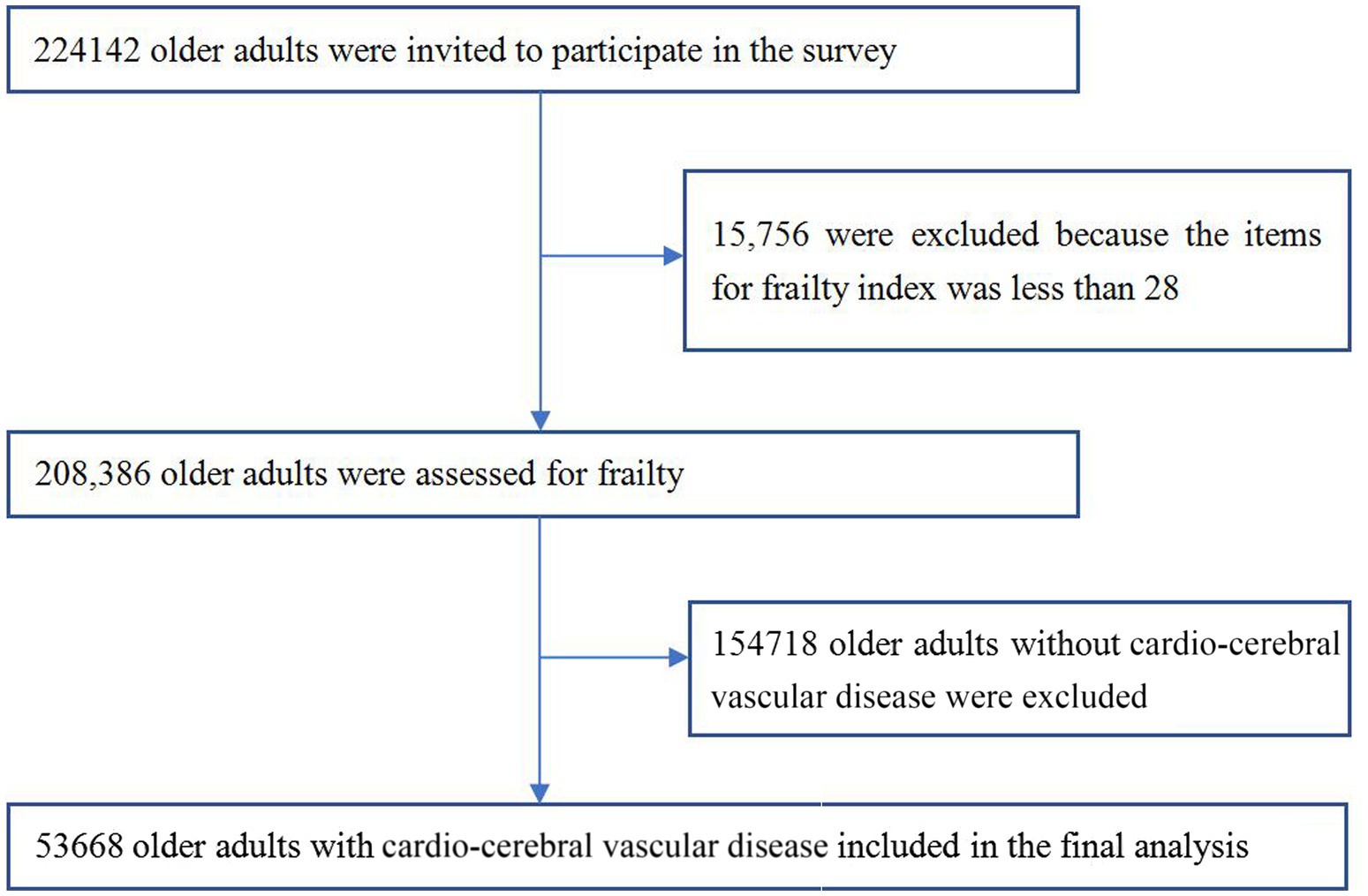
Figure 1. Flowchart of study participants on frailty and pre-frailty prevalence in older adults with cardio-cerebral vascular disease in China.
Demographic characteristics: age, sex, education, marital status, ethnicity, urban/rural, living alone, health screening during the last year, hospitalization during the last year, financial status, ease of reimbursement of medical expenses, disability in activities of daily living (ADL), co-morbid chronic diseases.
We selected 33 items from the questionnaire (at least 28/33 items per subject) to construct the FI according to the FI construct consensus (19). The exact construction method has been described in our previous study (16). We classified the FI into 3 levels: robust (FI < 0.12), pre-frailty (FI ≥ 0.12 and < 0.25), and frailty (FI ≥ 0.25).
The literature reports a 10–60% prevalence of frailty in patients with CCVD, and we used a 10% prevalence to calculate the sample size (10, 11, 13). We used PASS software (NCSS, Kaysville, UT, USA) to calculate the sample size and applied a design effect of 3 to account for a multi-stage cluster sampling design. The sample size was 10,671. Thus, our sample of over 50,000 participants in this study was adequate. Statistical analysis was performed using SPSS 24.0 (IBM Corporation, Armonk, NY, USA). Missing data were interpolated using the Markov Chain Monte Carlo (MCMC) multiple fill method. Age-adjusted prevalence of frailty and pre-frailty among older Chinese people with CCVD was calculated according to the weights established in our study. The significance of differences was assessed by Student’s t-test for continuous variables and by χ2-test for categorical variables. The Cochran-Armitage test was used to test for trends in the prevalence of covariates. Multinomial regression analyses were used to identify factors which were associated with frailty and pre-frailty, including age group, gender, ethnicity, place of residence, education level, marital status, living alone, health screening during the last year, hospitalization during the last year, financial status, ease of medical reimbursement, comorbid chronic conditions, and ADL disability. The level of statistical significance was defined as p less than 0.05.
A total of 53,668 self-reported patients with CCVD were included in our study, and the self-reported prevalence of CCVD among older adults was 25.8%, with a prevalence of 23.0% among men and 28.3% among women. The demographics and frailty risk factors by gender, urban/rural and ethnicity of older adults with CCVD are shown in Table 1.
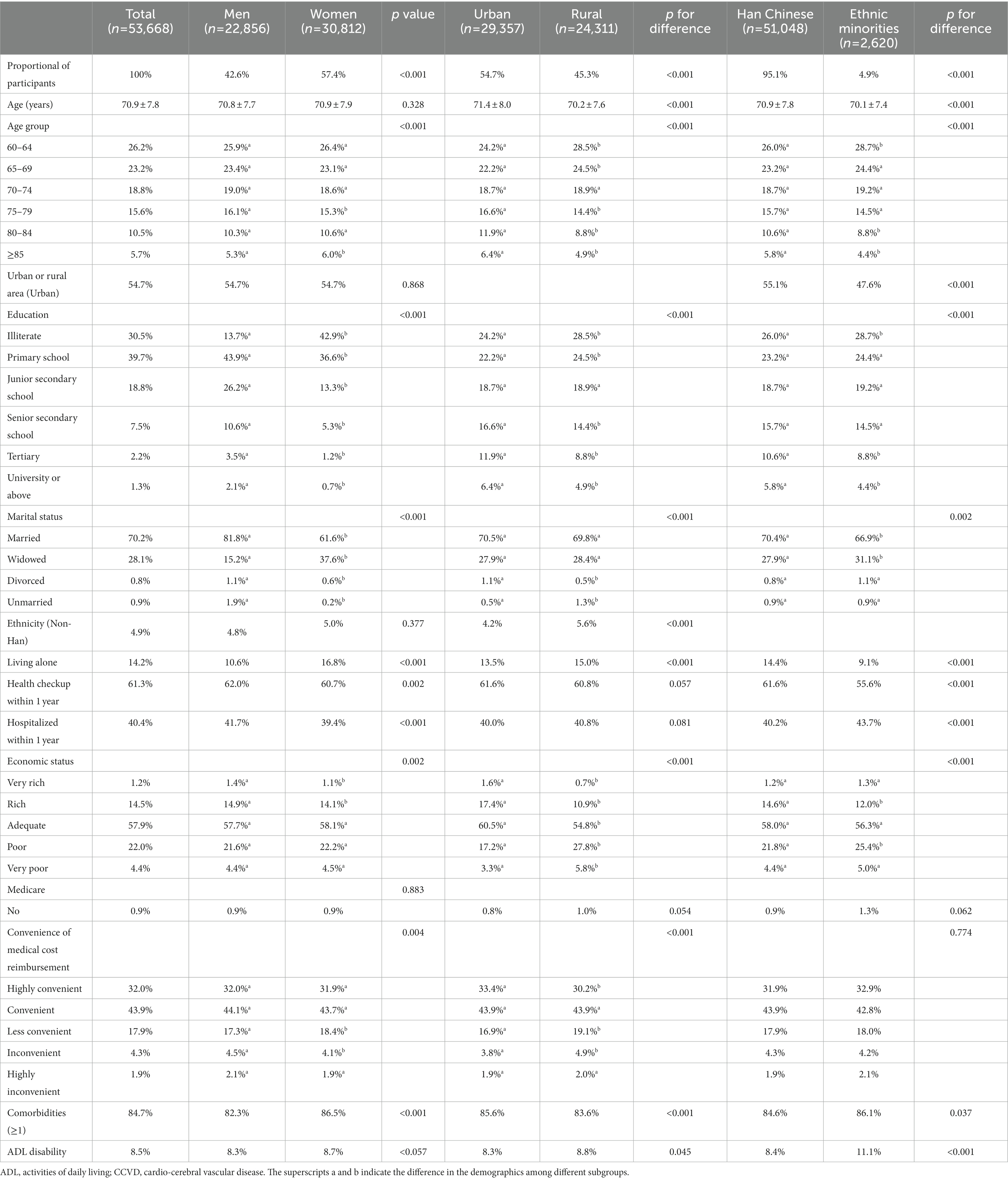
Table 1. Demographics of the Chinese adults aged 60 years or older with CCVD by gender, urban/rural, and ethnic groups in 2015.
The FI of older adults with CCVD was gamma distributed (statistical value = 0.094, p < 0.001). The FI of older adults with CCVD was 0.18 (0.11) (ranging from 0.04–0.67) and the FI for women was 0.19 (0.10) higher than the FI for men of 0.17 (0.10) (z = 17.495, p < 0.001).
The prevalence of frailty in older adults with CCVD increased with age, with a significant increase from 15.5% in the 60–64 age group to 42.1% in the ≥85 age group. Additionally, frailty was more prevalent in rural areas and among ethnic minorities. Frailty was mostly seen in older adults with CCVD who were illiterate, widowed, living alone, had not had a health screening during the last year, had been hospitalized during the last year, had financial difficulties, had difficulties in medical reimbursement, and had combined chronic diseases and ADL disabilities (See Table 2). Furthermore, the prevalence of frailty among older adults with CCVD was higher in northern China (24.0%) than in southern China (20.2%). The prevalence of frailty among older adults with CCVD in seven administrative regions of mainland China was highest in northwest China, followed by southwest China, then north China, then central, south, northeast and southeast China. The highest prevalence of frailty among older adults with CCVD in 31 provinces/municipalities/autonomous regions in mainland China was in Gansu Province (36.6%), while the lowest prevalence was in Fujian Province (14.9%) (Figure 2).
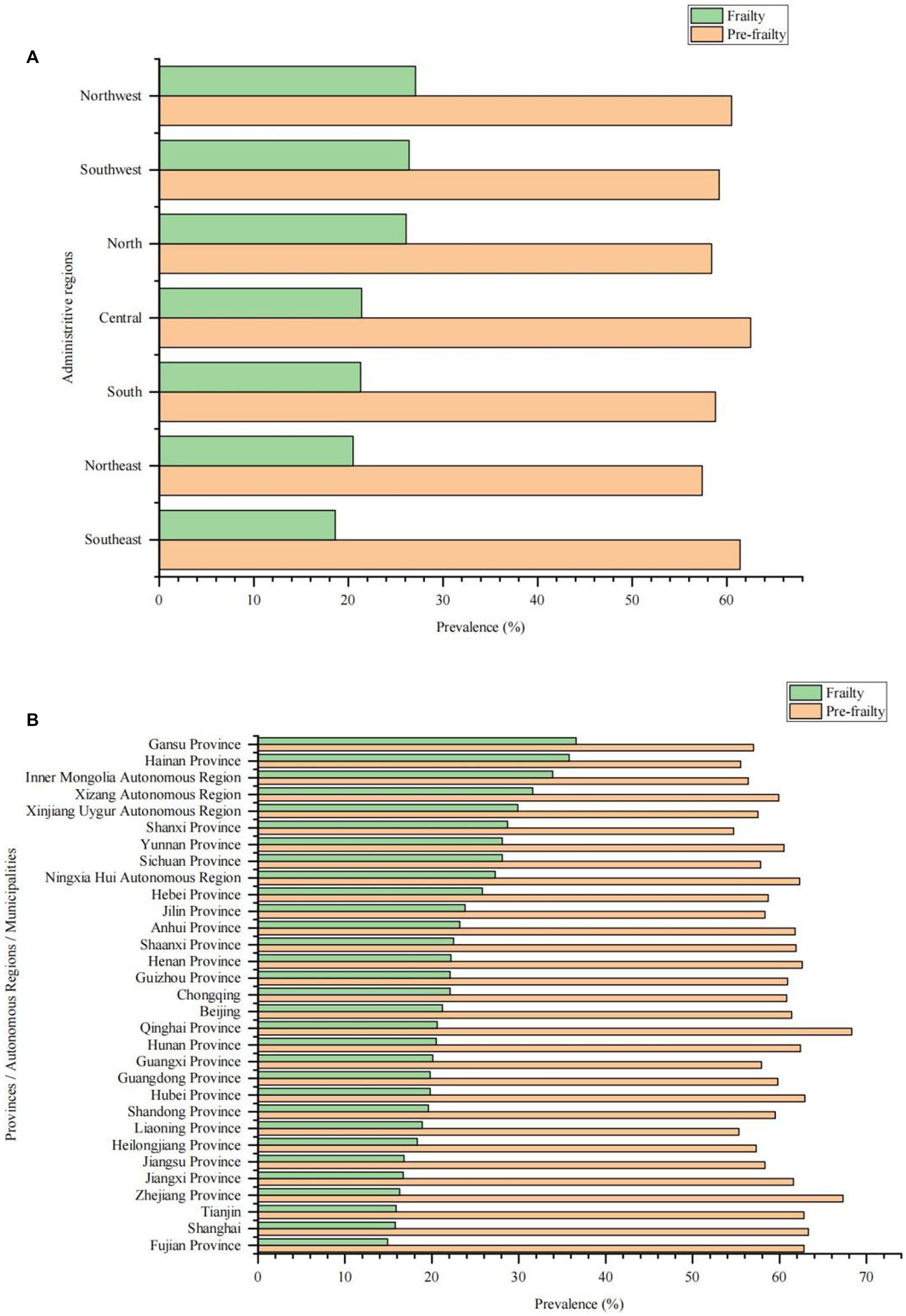
Figure 2. Prevalence of frailty and pre-frailty in older adults with cardio-cerebral vascular disease in different regions in China. (A) Prevalence of frailty and pre-frailty in older adults with cardio-cerebral vascular disease in different administrative regions. (B) Prevalence of frailty and pre-frailty in older adults with cardio-cerebral vascular disease in different provinces/autonomous regions/municipalities.
Multinomial regression analysis showed that being female, increasing age, living in a rural area, being widowhood, belonging to a ethnic minority, living alone, no having undergone health screening during the last year, experiencing hospitalization during the last year, facing economic hardship, comorbid chronic diseases, experiencing ADL disability were risk factors for frailty and pre-frailty in older adults with CCVD. On the other hand, having received education was a protective factor for frailty and pre-frailty in older adults with CCVD (Table 3).
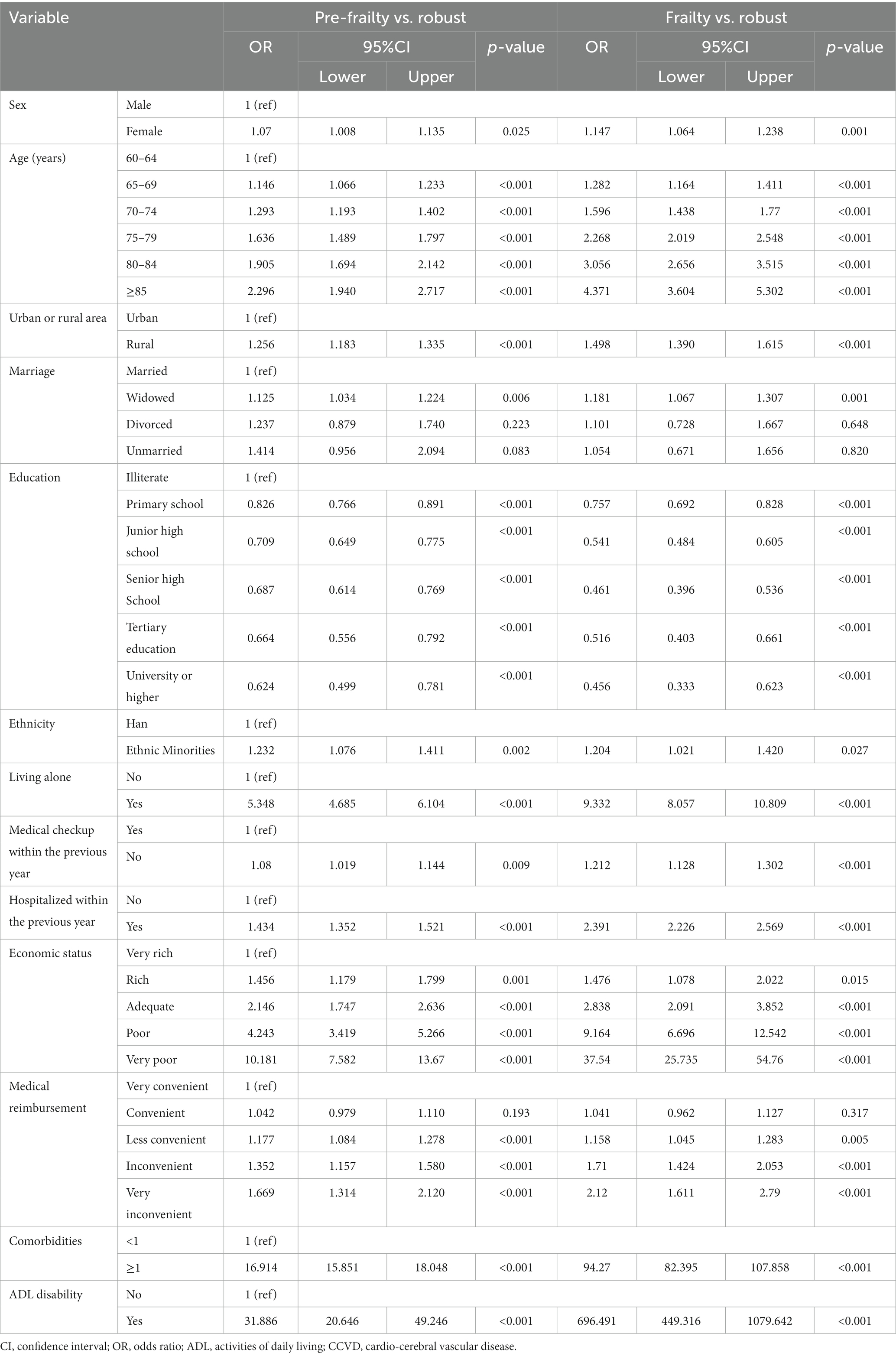
Table 3. Related factors associated with frailty and pre-frailty by multinomial logistic regression of older adults with CCVD.
Our large national sample study showed that the prevalence of self-reported CCVD among older adults in China was 25.8%, indicating a very high burden of CCVD among older adults. With the aging of the population, the burden of CCVD has shifted to older adults in the last two decades. The Cardiovascular Health and Diseases Report in China 2021 showed that the prevalence of CCVD in China is in a continuous rise, with about 330 million people currently suffering from CCVD, and the mortality rate of CCVD among Chinese urban and rural residents has also been on the rise in the last decade, with rural and urban CCVD accounting for 46.74 and 44.26% of causes of death, respectively, in 2019 (2). Population aging is the main driver of the increase in deaths from CCVD, with studies showing that 3.09 million residents died from CCVD in China in 2005, increasing to 4.58 million in 2020, representing a 48.06% increase in total mortality from CCVD in China compared to 2005 (20). CCVD has become the most important chronic non-communicable diseases that affect the health and longevity of older adults in China. Frailty is a prevalent age-dependent syndrome that is associated with adverse health outcomes. Studies have shown that CCVD is closely associated with frailty and that frailty has an impact on the immediate and long-term prognosis of patients with CCVD (11, 12). Therefore, studying the frailty status and risk factors of older Chinese patients with CCVD can help inform public health policy makers and promote healthy aging in older patients with CCVD.
Our study used a rigorous sampling design and quality control to accurately report the prevalence of frailty and pre-frailty among Chinese older adults with CCVD. Our study found a high age-standardized prevalence of frailty of 22.6% (95% CI 22.3–23.0%) and an age-standardized prevalence of pre-frailty of 60.1% (95% CI 59.7–60.5%) in older adults with CCVD. Studies have shown that the prevalence of frailty in patients with different degrees of CCVD ranges from 10 to 60%, relying on the definition of frailty and assessment tools used in each study (10, 11). In patients with CCVD, the prevalence of frailty was three times higher than in those without CCVD (21). In our study, the prevalence of frailty in older adults with CCVD was 4.6 times higher than in those without CCVD. Our study found a 61.2% prevalence of CCVD among frail older patients, significantly higher than the 17.4% prevalence of CCVD among robust older adults, and our study shows that cardiovascular disease is strongly associated with frailty in the older adults. Studies have shown a strong bidirectional association between CCVD and frailty (12, 22), with both disease processes having the same pathophysiological basis. Inflammatory senescence, a mild, asymptomatic, systemic, chronic inflammatory state, occurs with age and is characterized by an elevation of pro-inflammatory factors that act as molecular mediators and a decrease in factors that inhibit the inflammatory response. Chronic inflammation plays an important role in the pathophysiology of CCVD, and chronic inflammation also has direct or indirect effects on the musculoskeletal, endocrine, cardiovascular and hematological systems, leading to frailty occurrences (23, 24).
Our study found that that several factors, including being female, increased age, living in a rural area, being widowhood, belonging to a minority, not having undergone health screening during the last year, having been hospitalization during the last year, experiencing financial difficulties, facing inconvenient medical reimbursement, having comorbid chronic diseases, and experiencing ADL disability were risk factors for frailty and pre-frailty in older adults with CCVD, while having received education is a protective factor for frailty and pre-frailty in older adults with CCVD. The findings of our study are consistent with those of previous studies (4, 25–30). The risk factors for frailty in older patients with CCVD identified in our study could help to identify high-risk patients early and implement interventions to prevent or delay the onset of frailty in older patients with CCVD.
Our study found that older women with CCVD had higher rates in the ≥85-year-old age group, were widowed, lived alone, and had comorbid chronic diseases compared with older men with CCVD, Additionally, they had lower rates of good education, health screening during the last year, and financial well-being. These factors may partially explain the gender differences in frailty in older adults with CCVD. Furthermore, our study found that a higher proportion of older adults with CCVD in rural areas were unmarried, ethnic minorities, living alone, in difficult financial situations, experiencing ADL disability, facing inconvenient medical reimbursement, and less well educated compared to older adults with CCVD in urban areas. These factors may partially explain the urban–rural differences in frailty among older adults with CCVD. Additionally, our study found that compared with Han Chinese older adults with CCVD, ethnic minority older adults with CCVD had higher rates of illiteracy, widowhood, past 1-year hospitalization, financial hardship, ADL disability, comorbid chronic diseases, and lower rates of past 1-year health checkups. These differences in demographic characteristics and frailty risk factors may partially explain the ethnic differences in frailty among older adults with CCVD. Lastly, we also found that there were considerable regional differences in the prevalence of frailty among older adults with CCVD, with relatively high prevalence among older adults with CCVD in the less economically developed north-west and south-west regions, and relatively low prevalence in the economically developed coastal regions. These findings may help governments to formulate appropriate policies to prevent and ameliorate the frailty of older adults with CCVD.
Our study has several limitations that should be considered. Firstly, self-reported diagnostic information for CCVD may be subject to recall bias. Secondly, the study lacked information on the specific type, duration and extent of CCVD. Thirdly, smoking is an important risk factor for CCVD and this study did not assess the relationship between smoking and frailty in older patients with CCVD. Lastly, this study was a cross-sectional study and the causative relationship between the factors of interest and frailty in older patients with CCVD could not be determined.
In conclusion, the prevalence of frailty and pre-frailty in older cardiovascular patients is very high and frailty assessment should become routine in the management of older patients with CCVD, attention should be paid to early identification of risk factors for frailty in older patients with CCVD and timely interventions to prevent, delay or reverse the onset of frailty in older patients with CCVD.
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
The studies involving human participants were reviewed and approved by the National Bureau of Statistics (No. [2014] 87) and the Beijing Hospital Ethics Committee (2021BJYYEC-294-01). Written informed consent was provided by all participants. The patients/participants provided their written informed consent to participate in this study.
X-zZ and NJ wrote the various drafts of the manuscript. X-zZ, L-bM, and JS conducted the statistical analyses. CZ, Y-yL, J-bH, HL, XQ, HW, XH, D-sW, and J-yL participated in data interpretation. D-pL, Q-xZ, JL, and X-zZ conceived and designed this study. X-zZ, NJ, L-bM, CZ, Y-yL, J-bH, JS, HL, XQ, HW, XH, D-sW, J-yL, Q-xZ, JL, and D-pL were drafts of the manuscript for important scientific content. D-pL is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data, and the accuracy of the data analysis. All authors gave final approval of the version to be published.
The present study was funded by the National Key R&D Program of China (grant nos. 2020YFC2003000 and 2020YFC2003001). The study sponsors were not involved in the design of the study, the collection, analysis, and interpretation of data, writing the report, or the decision to submit the report for publication.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. National Bureau of Statistics. Main data of the seventh national population census . (2021). Available at: http://www.stats.gov.cn/tjsj/zxfb/202105/t20210510_1817176.html (Accessed January 6, 2022).
2. The Writing Committee of the Report on Cardiovascular Health and Diseases in China 2021 . Key points of report on cardiovascular health and diseases in China 2021. Chin J Cardiovasc Res. (2022) 20:577–96. doi: 10.3969/j.issn.1672-5301.2022.07.001
3. Hoogendijk, EO, Afilalo, J, Ensrud, KE, Kowal, P, Onder, G, and Fried, LP. Frailty: implications for clinical practice and public health. Lancet. (2019) 394:1365–75. doi: 10.1016/S0140-6736(19)31786-6
4. Rockwood, K, and Howlett, SE. Age-related deficit accumulation and the diseases of ageing. Mech Ageing Dev. (2019) 180:107–16. doi: 10.1016/j.mad.2019.04.005
5. Clegg, A, Young, J, Iliffe, S, Rikkert, MO, and Rockwood, K. Frailty in elderly people. Lancet. (2013) 381:752–62. doi: 10.1016/S0140-6736(12)62167-9
6. Fried, LP, Tangen, CM, Walston, J, Newman, AB, Hirsch, C, Gottdiener, J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci. (2001) 56:M146–57. doi: 10.1093/gerona/56.3.M146
7. Collard, RM, Boter, H, Schoevers, RA, and Oude Voshaar, RC. Prevalence of frailty in community-dwelling older persons: a systematic review. J Am Geriatr Soc. (2012) 60:1487–92. doi: 10.1111/j.1532-5415.2012.04054.x
8. Jin, HY, Liu, X, Xue, QL, Chen, S, and Wu, C. The association between frailty and healthcare expenditure among Chinese older adults. J Am Med Dir Assoc. (2020) 21:780–5. doi: 10.1016/j.jamda.2020.03.008
9. Han, L, Clegg, A, Doran, T, and Fraser, L. The impact of frailty on healthcare resource use: a longitudinal analysis using the clinical practice research Datalink in England. Age Ageing. (2019) 48:665–71. doi: 10.1093/ageing/afz088
10. Afilalo, J, Karunananthan, S, Eisenberg, MJ, Alexander, KP, and Bergman, H. Role of frailty in patients with cardiovascular disease. Am J Cardiol. (2009) 103:1616–21. doi: 10.1016/j.amjcard.2009.01.375
11. Afilalo, J, Alexander, KP, Mack, MJ, Maurer, MS, Green, P, Allen, LA, et al. Frailty assessment in the cardiovascular care of older adults. J Am Coll Cardiol. (2014) 63:747–62. doi: 10.1016/j.jacc.2013.09.070
12. Ijaz, N, Buta, B, Xue, QL, Mohess, DT, Bushan, A, Tran, H, et al. Interventions for frailty among older adults with cardiovascular disease: JACC state-of-the-art review. J Am Coll Cardiol. (2022) 79:482–503. doi: 10.1016/j.jacc.2021.11.029
13. Wleklik, M, Denfeld, Q, Lisiak, M, Czapla, M, Kaluzna-Oleksy, M, and Uchmanowicz, I. Frailty syndrome in older adults with cardiovascular diseases-what do we know and what requires further research? Int J Environ Res Public Health. (2022) 19:2234. doi: 10.3390/ijerph19042234
14. Pasieczna, AH, Szczepanowski, R, Sobecki, J, Katarzyniak, R, Uchmanowicz, I, Gobbens, RJJ, et al. Importance analysis of psychosociological variables in frailty syndrome in heart failure patients using machine learning approach. Sci Rep. (2023) 13:7782. doi: 10.1038/s41598-023-35037-3
15. Wleklik, M, Denfeld, Q, Czapla, M, Jankowska, E, Piepoli, MF, and Uchmanowicz, I. A patient with heart failure, who is frail: how does this affect therapeutic decisions? Cardiol J. (2023). doi: 10.5603/CJ.a2023.0027
16. Zeng, X, Jia, N, Meng, L, Shi, J, Li, Y, Hu, X, et al. A study on the prevalence and related factors of frailty and pre-frailty in the older population with diabetes in China: a national cross-sectional study. Front Public Health. (2022) 10:10. doi: 10.3389/fpubh.2022.996190
17. Meng, L, Xu, J, Li, J, Hu, J, Xu, H, Wu, D, et al. Self-reported prevalence and potential factors influencing cardio-cerebral vascular disease among the Chinese elderly: a national cross-sectional study. Front Cardiovasc Med. (2022) 9:979015. doi: 10.3389/fcvm.2022.979015
18. Dang, JW, Wei, YY, and Liu, NN. Survey report on the living conditions of China's urban and rural older persons. Beijing: Social Science Academic Press (2018).
19. Searle, SD, Mitnitski, A, Gahbauer, EA, Gill, TM, and Rockwood, K. A standard procedure for creating a frailty index. BMC Geriatr. (2008) 8:24. doi: 10.1186/1471-2318-8-24
20. Wang, W, Liu, Y, Liu, J, Yin, P, Wang, L, Qi, J, et al. Mortality and years of life lost of cardiovascular diseases in China, 2005-2020: empirical evidence from national mortality surveillance system. Int J Cardiol. (2021) 340:105–12. doi: 10.1016/j.ijcard.2021.08.034
21. von Haehling, S, Anker, SD, Doehner, W, Morley, JE, and Vellas, B. Frailty and heart disease. Int J Cardiol. (2013) 168:1745–7. doi: 10.1016/j.ijcard.2013.07.068
22. Damluji, AA, Chung, SE, Xue, QL, Hasan, RK, Moscucci, M, Forman, DE, et al. Frailty and cardiovascular outcomes in the National Health and aging trends study. Eur Heart J. (2021) 42:3856–65. doi: 10.1093/eurheartj/ehab468
23. Siti, HN, Kamisah, Y, and Kamsiah, J. The role of oxidative stress, antioxidants and vascular inflammation in cardiovascular disease (a review). Vasc Pharmacol. (2015) 71:40–56. doi: 10.1016/j.vph.2015.03.005
24. Wu, IC, Lin, CC, and Hsiung, CA. Emerging roles of frailty and inflammaging in risk assessment of age-related chronic diseases in older adults: the intersection between aging biology and personalized medicine. Biomedicine (Taipei). (2015) 5:1. doi: 10.7603/s40681-015-0001-1
25. Ma, L, Tang, Z, Zhang, L, Sun, F, Li, Y, and Chan, P. Prevalence of frailty and associated factors in the community-dwelling population of China. J Am Geriatr Soc. (2018) 66:559–64. doi: 10.1111/jgs.15214
26. Wu, C, Smit, E, Xue, QL, and Odden, MC. Prevalence and correlates of frailty among community-dwelling Chinese older adults: the China health and retirement longitudinal study. J Gerontol A Biol Sci Med Sci. (2017) 73:102–8. doi: 10.1093/gerona/glx098
27. Ge, L, Yap, CW, and Heng, BH. Associations of social isolation, social participation, and loneliness with frailty in older adults in Singapore: a panel data analysis. BMC Geriatr. (2022) 22:26. doi: 10.1186/s12877-021-02745-2
28. Li, Y, Xue, QL, Odden, MC, Chen, X, and Wu, C. Linking early life risk factors to frailty in old age: evidence from the China health and retirement longitudinal study. Age Ageing. (2020) 49:208–17. doi: 10.1093/ageing/afz160
29. Dugravot, A, Fayosse, A, Dumurgier, J, Bouillon, K, Rayana, TB, Schnitzler, A, et al. Social inequalities in multimorbidity, frailty, disability, and transitions to mortality: a 24-year follow-up of the Whitehall II cohort study. Lancet Public Health. (2020) 5:e42–50. doi: 10.1016/S2468-2667(19)30226-9
30. Hanlon, P, Nicholl, BI, Jani, BD, Lee, D, McQueenie, R, and Mair, FS. Frailty and pre-frailty in middle-aged and older adults and its association with multimorbidity and mortality: a prospective analysis of 493 737 UK biobank participants. Lancet Public Health. (2018) 3:e323–32. doi: 10.1016/S2468-2667(18)30091-4
Keywords: cardio-cerebral vascular disease, China, frailty, older adults, pre-frailty, prevalence
Citation: Zeng X-z, Meng L-b, Jia N, Shi J, Zhang C, Li Y-y, Hu X, Hu J-b, Li J-y, Wu D-s, Li H, Qi X, Wang H, Zhang Q-x, Li J and Liu D-p (2023) Prevalence of frailty and pre-frailty and related factors in older adults with cardio-cerebral vascular disease in China: a national cross-sectional study. Front. Public Health. 11:1168792. doi: 10.3389/fpubh.2023.1168792
Received: 18 February 2023; Accepted: 30 May 2023;
Published: 16 June 2023.
Edited by:
Giuseppe Caminiti, Università telematica San Raffaele, ItalyReviewed by:
Giuseppe Marazzi, IRCCS San Raffaele, ItalyCopyright © 2023 Zeng, Meng, Jia, Shi, Zhang, Li, Hu, Hu, Li, Wu, Li, Qi, Wang, Zhang, Li and Liu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: De-ping Liu, bGxpdWRlcGluZ0AyNjMubmV0
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.