- 1Department of Preventive Medicine, Konyang University College of Medicine, Daejeon, Republic of Korea
- 2Department of Public Health and Welfare, The Graduate School, Konyang University, Daejeon, Republic of Korea
- 3Konyang University Myunggok Medical Research Institute, Daejeon, Republic of Korea
Background: Prior to COVID-19 pandemic, a yearly upward trajectory in the number of chlamydia infection cases was observed in South Korea. However, in response to the COVID-19 pandemic, Korea implemented several public health and social measures, which were shown to have an impact on the epidemiology of other infectious diseases. This study aimed to estimate the impact of the COVID-19 pandemic on the incidence and number of reported chlamydia infections in South Korea.
Methods: Using the monthly number of reported chlamydia infection data between 2017 and 2022, we compared the trends in the reported numbers, and the incidence rates (IR) of chlamydia infection stratified by demographic characteristics (sex, age group, and region) in the pre- and during COVID-19 pandemic period (January 2017–December 2019 and January 2020–December 2022).
Results: We observed an irregular downward trajectory in the number of chlamydia infection in the during-pandemic period. A 30% decrease in the total number of chlamydia infection was estimated in the during-pandemic compared to the pre-pandemic period, with the decrease greater among males (35%) than females (25%). In addition, there was a decrease in the cumulative incidence rate of the during COVID-19 pandemic period (IR: 0.43; 95% CI: 0.42–0.44) compared to the pre-pandemic period (IR: 0.60; 95% CI: 0.59–0.61).
Conclusions: We identified decrease in the number of chlamydia infection during COVID-19 pandemic which is likely due to underdiagnosis and underreporting for the infection. Therefore, strengthening surveillance for sexually transmitted infections including chlamydia is warranted for an effective and timely response in case of an unexpected rebound in the number of the infections.
Introduction
Chlamydia infection caused by Chlamydia trachomatis is a common sexually transmitted infection (STI) worldwide. Globally, ~50%−88% of chlamydia infection cases are asymptomatic (1). Due to the high rate of asymptomatic cases, systematic monitoring of chlamydia infections for high-risk populations, including sexually active young adults, has been recommended (2, 3). Furthermore, the monitoring of the infections provides us with a useful proxy for changes in sexual risk behaviors (4).
The first case of the newly discovered severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) in South Korea was reported on 20 January 2020 (5). And in an attempt to control the SARS-CoV-2, South Korea, implemented several public health and social measures (PHSMs), including social distancing, and wearing of face masks from 22 March 2020, which were crucial in mitigating the burden of the COVID-19 pandemic (6). The implementation of these PHSMs had considerable effects on the incidence and prevalence rates of other bacterial and viral infectious diseases (7, 8). In addition, these PHSMs reduced person-to-person interactions as well as the access and use of clinical services such as screening, and treatment for sexually transmitted infections (STIs) (9). The reported shift in various screening services including STI screening services, toward only symptomatic patients, could reduce the ability to identify asymptomatic chlamydia infections, hence a reduction in the overall reported number of cases (10).
There have been several concerns among clinicians and researchers in different countries regarding the spread of STIs during the COVID-19 pandemic and the possible long-term consequences of their underdiagnosis (11).
In 2019 before the importation of SARS-CoV-2 in South Korea, a total of 48,756 outpatient screening for chlamydia infection was done compared to 40,640 screenings in 2020 and 37,632 in 2021, implying a 16% and 23% decrease in 2020 and 2022, respectively (12).
Previous empirical literature in Europe (13, 14) and the United States (15) have demonstrated a decrease in the number of new cases of sexually transmitted infections including chlamydia infection during the early stages of the COVID-19 pandemic, and during the period when the PHSMs were implemented. In South Korea, a study reported an apparent decrease in the incidence of chlamydia infections during the early stages of the COVID-19 pandemic (16). However, the impact of COVID-19 on the trends of the reported number of chlamydia infection and incidence in the pre- vs. during-COVID-19 pandemic period in Korea is yet to be compared. Here, we compared the monthly number of reported chlamydia infection cases in the pre-COVID-19 period (January 2017–December 2019) with the number of monthly cases reported in the same period during-COVID-19 (January 2020–December 2022) by age, sex and regions in South Korea.
Materials and methods
Study data and variables
In South Korea, sentinel-based surveillance for chlamydia infection has been conducted since 2000 by the Korea Disease Control and Prevention Agency (KDCA) (17), an electronic database that collects data reported from healthcare professionals and laboratories in South Korea. This surveillance includes data from 587 sentinel sites located throughout the country (18). We collected the monthly number of chlamydia infection cases between January 2017 and December 2022, with a focus on the month of confirmation of the first COVID-19 case in South Korea (serving as the cut-off point of the pre vs. during-COVID-19 pandemic periods) and the first period of implementation of PHSMs (22 March, 2020 to 01 November, 2020). We divided the study period into two; the pre-pandemic (January 2017–December 2019) and the during-pandemic (January 2020–December 2022) periods.
In July 2017, due to system maintenance schedules according to the KCDA reports, no data inputs were made into the database. Therefore, we assumed the number of cases for the period of maintenance to be the average number of cases for June and August 2017. The collected data were stratified by sex, age group, and region of residence.
Data analysis
We assessed the impact of the COVID-19 pandemic and the implementation of the PHSMs on the number of reported chlamydia infection cases using two approaches. First, we compared chlamydia infection reported case monthly and yearly trends for the pre-COVID-19 pandemic period compared with the during-COVID-19 pandemic period and for each subgroup (sex, age group, and region). Second, using the pre-pandemic values as the baseline, we estimated the percentage changes in the absolute number of cases during the pandemic period. We examined significant differences in the changes between the pre-pandemic and during-pandemic values using the Chi-squared test. Using the 2021 population of South Korea as the standard population, we estimated the cumulative incidence rates of chlamydia and 95% confidence intervals (CI) for the pre-pandemic and during-pandemic period per 1,000. Then, we conducted stratified analyses by age group in years (<20, 20–29, 30–39, 40–49, and ≥50), sex (male, and female), and region. We classified the regions into two categories; in the Seoul Capital Area (SCA) which was made up of Seoul, Incheon, and Gyeonggi; and out of SCA which included all other cities.
All analyses were performed using R version 4.2.0 (R Foundation for Statistical Computing, Vienna, Austria), and the level of statistical significance was set at p < 0.05.
Results
A total of 31, 238 new chlamydia infection cases were reported in the pre-pandemic period while 22,186 new cases were reported in the during-pandemic period. There was a 28.9% decrease in the total number of chlamydia infection cases in the during-pandemic period compared to the pre-pandemic period. Stratifying by sex, compared to females (−24.9%), there was a significantly greater decrease in the number of chlamydia infection cases in males (−34.9%, P < 0.001). By age group, we identified a significant decrease in the number of reported cases among all groups, with the highest decrease in the age group 40–49 years (−41.9%, P < 0.001). By region, an almost equal magnitude of decrease was observed in the number of chlamydia infection cases in both the Seoul capital area region and out of the Seoul capital area region (respectively, −28.6% and −28.5 %, P < 0.001) (Table 1).
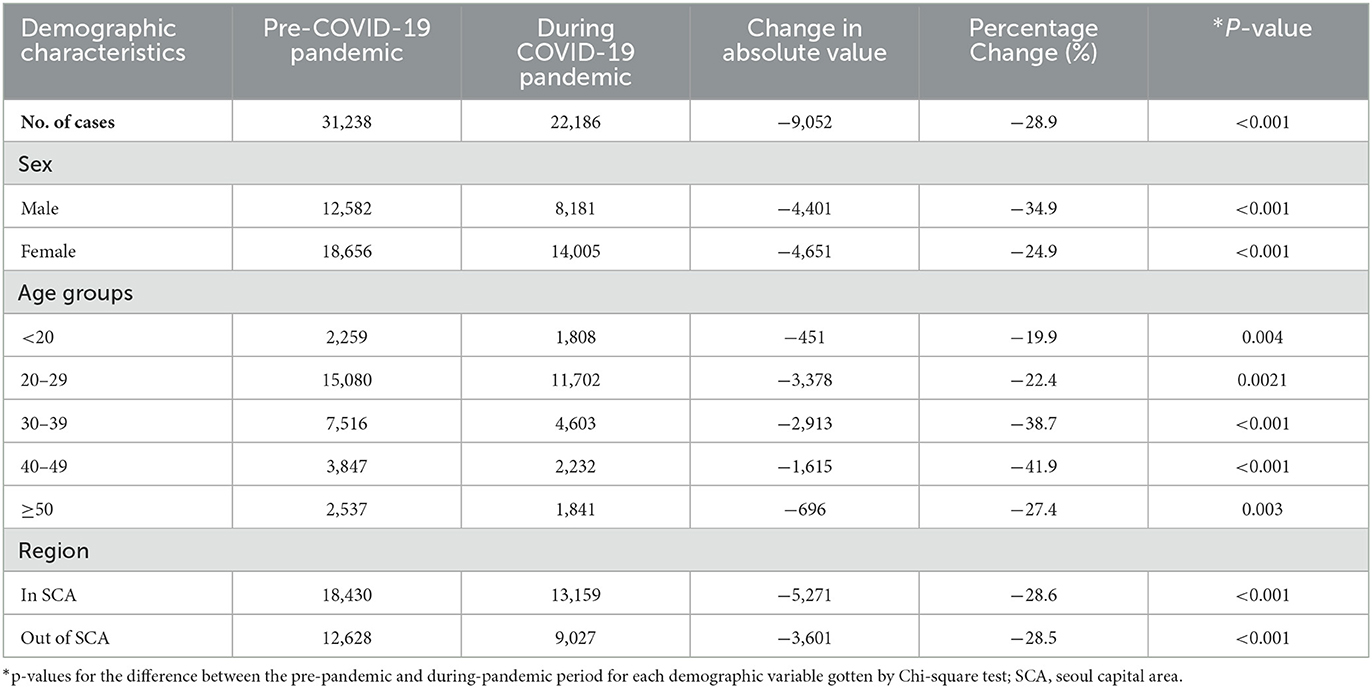
Table 1. Overall reported number of chlamydia infection cases during the pre-COVID-19 pandemic and during COVID-19 pandemic periods in South Korea.
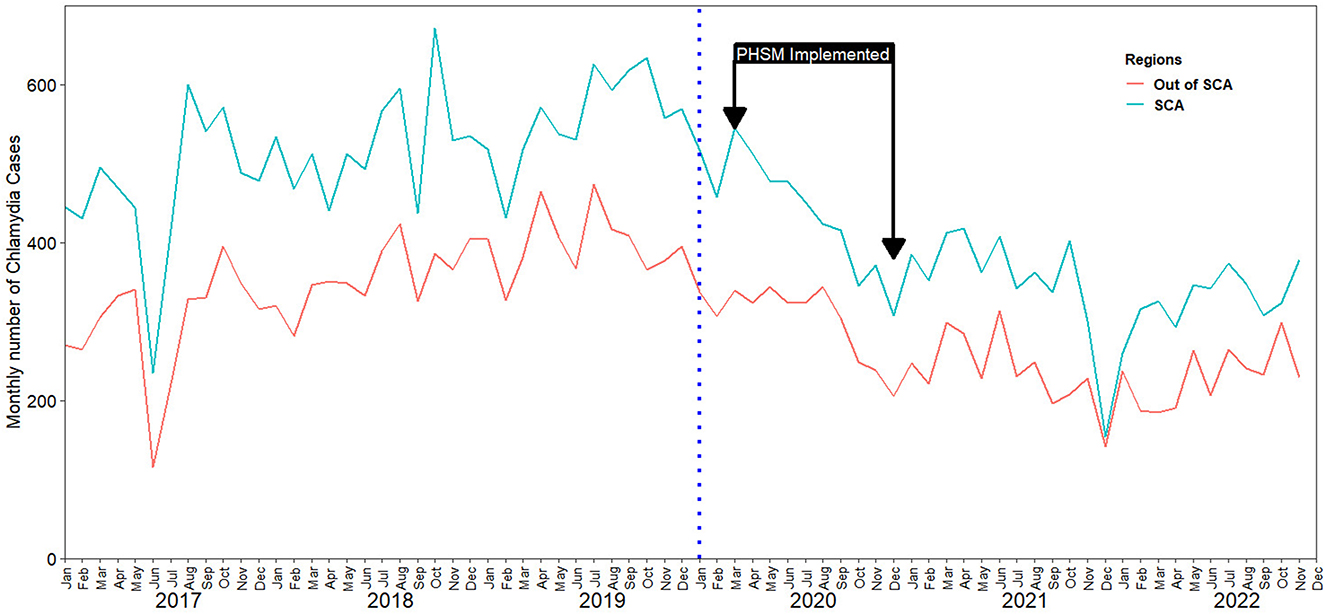
We identified the monthly number of chlamydia infection cases reported had an irregular upward trajectory between 2017 and 2019, while, a downward trajectory was observed between 2020 and 2022 (Figure 1, Supplementary Figure S1).
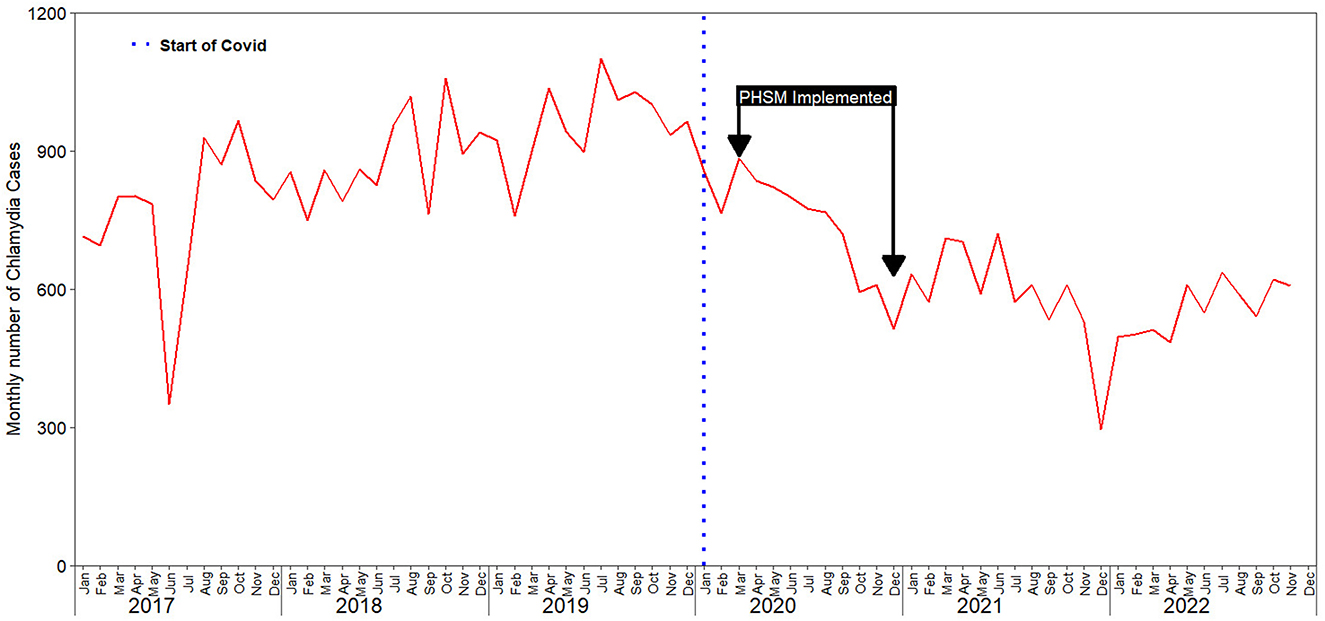
Figure 1. Impact of COVID-19 on chlamydia infection case reporting in South Korea: trends from 2017 to 2022.
Stratifying by sex, and age group an irregular downward trajectory was also observed in each subgroup, in the during-pandemic period (Figure 2). Similarly, we observed a downward trajectory in the during-pandemic period after stratification by region (Figure 3).
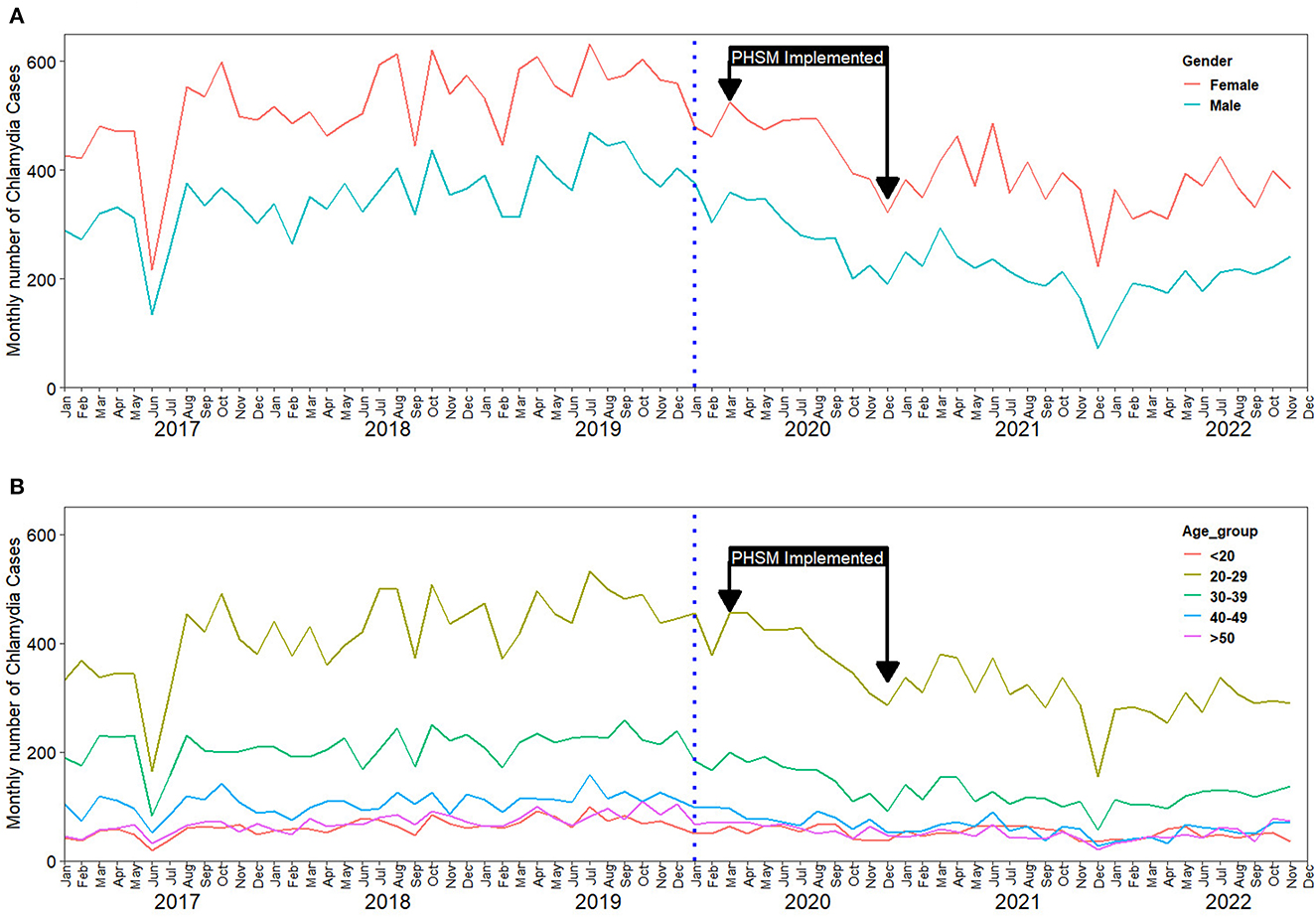
Figure 2. Impact of COVID-19 on chlamydia infection case reporting in South Korea: trends from 2017 to 2022; (A) Reported cases stratified by sex; (B) Reported cases stratified by age.
We also identified concurrent decreases in the during-pandemic chlamydia infection incidence rates in all subgroups in the during-pandemic period compared to the pre-pandemic period (Table 2).
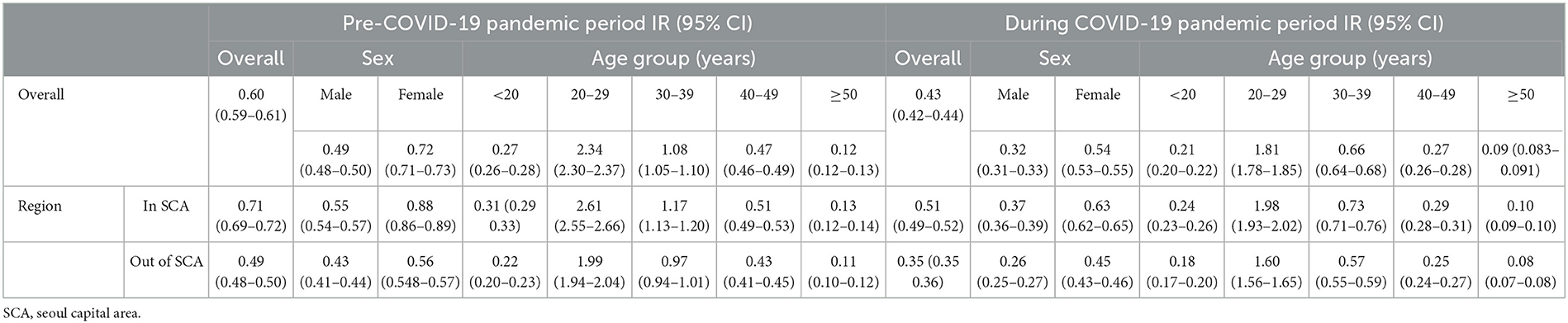
Table 2. Changes in Chlamydia infection incidence rates (IR) per 1,000 population for the pre-COVID-19 pandemic and during COVID-19 pandemic periods in Korea.
Discussion
We assessed the impact of the COVID-19 pandemic on the number of reported chlamydia infection cases and the incidence of chlamydia infection in Korea using national surveillance data. This assessment demonstrates the substantial impact of the COVID-19 pandemic on the chlamydia prevention program.
We observed a continuous downward trajectory in the number of reported chlamydia infection cases across all the years in the during-pandemic period. Similarly, there was a decrease in the cumulative incidence rate in the during-pandemic period compared to the pre-pandemic period. A similar trend was observed with other STIs (Supplementary material). This observed decreases in the pandemic period could be a result of behavioral changes as part of the stay-at-home mandates and also as a result of some barriers to patient care and preventive services that were directly or indirectly introduced as a result of the COVID-19 pandemic. During the COVID-19 pandemic, individuals were very reluctant to visit the doctor's office for medical consultation for fear of SARS-CoV-2 infection (19, 20). These changes in health-seeking behaviors could have impacted the screening of asymptomatic individuals. Moreover, the constant surveillance of STIs done by the local public health centers as well as associated primary health clinics may have been interrupted by COVID-19 control activities, limiting doctor's appointments and screening of potential cases. Our findings are similar to other studies that have also reported a decrease in the incidence and number of reported cases of chlamydia infection and other STIs in the pandemic period compared to the pre-pandemic period (21–24). However, our results are contrary to a study that reported an increase in chlamydia infection cases and other STIs during the COVID-19 pandemic (25, 26).
In this study, a sharper decrease in the overall trend was observed after the implementation of the PHSMs. During this period, the activities of the adult entertainment sectors (including nightclubs, bars, and other nighttime activities) were shut down. This may have reduced the number of STI screenings, as workers in the adult entertainment sector in South Korea are mandatorily screened for STIs every 3 months according to Korean Infectious Disease Control and Prevention act. However, due to the limited public health resources during COVID-19 pandemic, many workers was not likely screened for STIs by public health authorities. Our results are contrary to previous research that showed that PHSMs implemented during the early pandemic did not affect STIs (15, 27). This is likely due to the different level of use for public health resources for COVID-19 pandemic in different countries.
Our study also showed a sex, age group, and regional decrease in the trend of incidence and number of reported cases of chlamydia infection in the during-pandemic compared to the pre-pandemic period. Specifically, a significantly greater decrease was observed in males (−34.9%) compared to females and among those between 40 and 49 years old (−41.9%) compared to other age groups. This is in line with other studies in the literature which have shown that males are less likely to seek health care, especially for preventive care visits (28, 29). Therefore, this could be explained by underdiagnosis and underreporting given that there are concerns that chlamydia infections may be underdiagnosed in males and in middle age individuals (30). Underdiagnosis and underreporting of chlamydia infections may be due to decreased screening during the pandemic. Appropriate screening and medical consultations are recommended and health education and promotion activities aimed at sensitizing the public and healthcare providers are also needed.
There are some limitations to the present study. First, this study does not take into account the number of chlamydia tests that were conducted. Although the number of reported chlamydia infection cases decreased in the during-pandemic period, it is highly likely that many screening tests for the infection were not conducted. Furthermore, it is possible that the decrease in reported cases was not only due to the COVID-19 pandemic, but potentially due to policy changes around the fear of exposure to SARS-CoV-2 infection in a clinical setting.
Secondly, although several cofactors may exist between the COVID-19 pandemic and the incidence and number of reported chlamydia cases, this study could not assess the magnitude of the effect of each mediator, such as social restrictions, physical distancing, and hygiene measures.
In conclusion, our results suggest that the incidence and number of chlamydia infection cases decreased during the COVID-19 pandemic in South Korea. In pandemic and epidemic emergencies that involve behavioral restrictions, the promotion of healthcare-seeking behaviors among high-risk individuals for the sexually transmitted infections including chlamydia is encouraged.
Data availability statement
Publicly available datasets were analyzed in this study. This data can be found here: https://www.kdca.go.kr/npt/biz/npp/ist/simple/simplePdStatsMain.do.
Ethics statement
Ethical review or informed consent was not required because all data used in this study were anonymous and publicly available.
Author contributions
S-MH and SR conceived the study and sought funding. SR, AC, and J-HJ did the data collection, assimilation, and data analysis. SR and AC wrote the first draft of the manuscript. S-MH and AC critically reviewed and edited the manuscript. All authors contributed to the interpretation of the results, critical revision of the manuscript, and have given final approval of the version to be published.
Funding
This work is part of the project funded by the Myunggok Medical Research Center Konyang University, Daejeon, South Korea (# Myunggok 22-04). The sponsor of this study had no role in the study design, data collection, data analysis, data interpretation, or writing of this manuscript.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2023.1167321/full#supplementary-material
References
1. Keegan MB, Diedrich JT, Peipert JF. Chlamydia trachomatis infection: screening and management. J Clin Outcomes Manag. (2014) 21:30.
2. Skaletz-Rorowski A, Potthoff A, Nambiar S, Wach J, Kayser A, Kasper A, et al. Age specific evaluation of sexual behavior, STI knowledge and infection among asymptomatic adolescents and young adults. J Infect Public Health. (2020) 13:1112–7. doi: 10.1016/j.jiph.2020.04.005
3. Rondeau P, Valin N, Decré D, Girard PM, Lacombe K, Surgers L. Chlamydia trachomatis screening in urine among asymptomatic men attending an STI clinic in Paris: a cross-sectional study. BMC Infect Dis. (2019) 19:815. doi: 10.1186/s12879-018-3595-6
4. Choudhri Y, Miller J, Sandhu J, Leon A, Aho J. Chlamydia in Canada, 2010–2015. Can Commun Dis Rep. (2018) 44:49–54. doi: 10.14745/ccdr.v44i02a03
5. Kim HJ, Hwang HS, Choi YH, Song HY, Park JS, Yun CY, et al. The delay in confirming COVID-19 cases linked to a religious group in Korea. J Prev Med Public Health. (2020) 53:164–7. doi: 10.3961/jpmph.20.088
6. Ryu S, Ali ST, Jang C, Kim B, Cowling BJ. Effect of non-pharmaceutical interventions on transmission of severe acute respiratory syndrome coronavirus 2, South Korea, 2020. Emerg Infect Dis. (2020) 26:2406. doi: 10.3201/eid2610.201886
7. Achangwa C, Park H, Ryu S, Lee MS. Collateral impact of public health and social measures on respiratory virus activity during the COVID-19 pandemic 2020–2021. Viruses. (2022) 14:810. doi: 10.3390/v14051071
8. Ali ST, Lau YC, Shan S, Ryu S, Du Z, Wang L, et al. Prediction of upcoming global infection burden of influenza seasons after relaxation of public health and social measures during the COVID-19 pandemic: a modelling study. Lancet Glob Health. (2022) 10:e1612–22. doi: 10.1016/S2214-109X(22)00358-8
9. Apalla Z, Lallas A, Mastraftsi S, Giannoukos A, Noukari D, Goula M, et al. Impact of COVID-19 pandemic on STIs in Greece. Sex Transm Infect. (2021) 98:70. doi: 10.1136/sextrans-2021-054965
10. van Bergen JEAM, Hoenderboom BM, David S, Deug F, Heijne JCM, van Aar F, et al. Where to go to in chlamydia control? From infection control towards infectious disease control. Sex Transm Infect. (2021) 97:501. doi: 10.1136/sextrans-2021-054992
11. Barbee LA, Dombrowski JC, Hermann S, Werth BJ, Ramchandani M, Ocbamichael N, et al. “Sex in the time of COVID”: clinical guidelines for sexually transmitted disease management in an era of social distancing. Sex Transm Dis. (2020) 47:427–30. doi: 10.1097/OLQ.0000000000001194
12. Health Insurance Review & Assement Service. (2023). Statistics of Disease Sub-classification (Three-Stage Injury)|Healthcare Big Data Open System. Available online at: http://opendata.hira.or.kr/op/opc/olap3thDsInfo.do (accessed April 17, 2023).
13. Whitlock GG, Mcowan A, Nugent D. Gonorrhoea during COVID-19 in London, UK. Sex Transm Infect. (2021) 97:622–3. doi: 10.1136/sextrans-2020-054943
14. de Miguel Buckley R, Trigo E, de la Calle-Prieto F, Arsuaga M, Díaz-Menéndez M. Social distancing to combat COVID-19 led to a marked decrease in food-borne infections and sexually transmitted diseases in Spain. J Travel Med. (2021) 27:9626. doi: 10.1093/jtm/taaa134
15. Crane MA, Popovic A, Stolbach AI, Ghanem KG. Reporting of sexually transmitted infections during the COVID-19 pandemic. Sex Transm Infect. (2021) 97:101–2. doi: 10.1136/sextrans-2020-054805
16. Chang S, Ryu S, Kim D, Chun BC. Decrease in the incidence of chlamydia infection during the COVID-19 pandemic in South Korea. Sex Transm Infect. (2022) 98:155–155. doi: 10.1136/sextrans-2021-055074
17. Korea Disease Control and Prevention Agency. Infectious Disease Homepage. Sexually Transmitted Infectious Diseases-Sample Surveillance Infectious Diseases. (2023). Available online at: https://npt.kdca.go.kr/npt/biz/npp/iss/stisStatisticsMain.do (accessed April 17, 2023).
18. Korea Disease Control Prevention Agency. Infectious Disease Homepage. (2023). Available online at: https://npt.kdca.go.kr/npt/ (accessed April 17, 2023).
19. Lee YJ, Kim KO, Kim MC, Cho KB, Park KS, Jang BI. Perceptions and behaviors of patients with inflammatory bowel disease during the COVID-19 crisis. Gut Liver. (2022) 16:81–91. doi: 10.5009/gnl210064
20. Douglas M, Katikireddi SV, Taulbut M, McKee M, McCartney G. Mitigating the wider health effects of COVID-19 pandemic response. BMJ. (2020) 369:1002. doi: 10.1136/bmj.m1557
21. Ivarsson L, de Arriba Sánchez de. la Campa M, Elfving K, Yin H, Gullsby K, Stark L, et al. Changes in testing and incidence of Chlamydia trachomatis and Neisseria gonorrhoeae–the possible impact of the COVID-19 pandemic in the three Scandinavian countries. Infect Dis. (2022) 54:623–31. doi: 10.1080/23744235.2022.2071461
22. Saarentausta K, Ivarsson L, Jacobsson S, Herrmann B, Sundqvist M, Unemo M. Potential impact of the COVID-19 pandemic on the national and regional incidence, epidemiology and diagnostic testing of chlamydia and gonorrhoea in Sweden, 2020. APMIS. (2022) 130:34–42. doi: 10.1111/apm.13191
23. Tao J, Napoleon SC, Maynard MA, Almonte A, Silva E, Toma E, et al. Impact of the COVID-19 pandemic on sexually transmitted infection clinic visits. Sex Transm Dis. (2021) 48:5–7. doi: 10.1097/OLQ.0000000000001306
24. Johnson KA, Burghardt NO, Tang EC, Long P, Plotzker R, Gilson D, et al. Measuring the impact of the COVID-19 pandemic on sexually transmitted diseases public health surveillance and program operations in the state of California. Sex Transm Dis. (2021) 48:606–13. doi: 10.1097/OLQ.0000000000001441
25. Kanda N, Hashimoto H, Imai T, Yoshimoto H, Goda K, Mitsutake N, et al. Indirect impact of the COVID-19 pandemic on the incidence of non-COVID-19 infectious diseases: a region-wide, patient-based database study in Japan. Public Health. (2023) 214:20–4. doi: 10.1016/j.puhe.2022.10.018
26. Kuitunen I, Ponkilainen V. COVID-19-related nationwide lockdown did not reduce the reported diagnoses of Chlamydia trachomatis and Neisseria gonorrhoeae in Finland. Sex Transm Infect. (2021) 97:550–550. doi: 10.1136/sextrans-2020-054881
27. Lee KK, Lai CC, Chao CM, Tang HJ. Increase in sexually transmitted infection during the COVID-19 pandemic in Taiwan. J Eur Acad Dermatol Venereol. (2021) 35:e171–2. doi: 10.1111/jdv.17005
28. Pagaoa M, Grey J, Torrone E, Kreisel K, Stenger M, Weinstock H. Trends in nationally notifiable sexually transmitted disease case reports during the US COVID-19 pandemic, January to December 2020. Sex Transm Dis. (2021) 48:798–804. doi: 10.1097/OLQ.0000000000001506
29. Tao G, Dietz S, Hartnett KP, Jayanthi P, Gift TL. Impact of the COVID-19 pandemic on chlamydia and gonorrhea tests performed by a large national laboratory: United States, 2019 to 2020. Sex Transm Dis. (2022) 49:490–6. doi: 10.1097/OLQ.0000000000001638
30. Geba MC, Powers S, Williams B, Dort KR, Rogawski Mcquade ET, Mcmanus KA. A Missed Opportunity: Extragenital Screening for Gonorrhea and Chlamydia Sexually Transmitted Infections in People With HIV in a Southeastern Ryan White HIV/AIDS Program Clinic Setting. Oxford: Oxford University Press (2022). doi: 10.1093/ofid/ofac322
Keywords: chlamydia, surveillance, sexually transmitted infection (STI), sexually transmitted disease (STD), SARS-CoV-2, Korea
Citation: Chiara A, Ryu S, Jung J-H and Hwang S-M (2023) The impact of the COVID-19 pandemic on chlamydia infection in South Korea: a comparison between the pre-pandemic and during-pandemic periods. Front. Public Health 11:1167321. doi: 10.3389/fpubh.2023.1167321
Received: 16 February 2023; Accepted: 29 March 2023;
Published: 09 May 2023.
Edited by:
Creuza Rachel Vicente, Federal University of Espirito Santo, BrazilReviewed by:
Laura Huilaja, University of Oulu, FinlandAntonio C. R. Vallinoto, Federal University of Pará, Brazil
Copyright © 2023 Chiara, Ryu, Jung and Hwang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Se-Min Hwang, bmVvZnJldWQyQGRhdW0ubmV0
†These authors have contributed equally to this work
 Achangwa Chiara
Achangwa Chiara Sukhyun Ryu
Sukhyun Ryu Jae-Heon Jung1,3
Jae-Heon Jung1,3 Se-Min Hwang
Se-Min Hwang