- 1Montclair State University, Montclair, NJ, United States
- 2Dr. Hari Singh Gour University, Sagar, Madhya Pradesh, India
Background: A large number of systematic reviews have been published that synthesized various determinants of COVID-19 vaccination intention (CVI). However, they reported inconsistent evidence. Therefore, we conducted a meta-review (systematic review of systematic reviews) to provide a comprehensive synthesis of factors influencing CVI.
Methods: This meta-review was conducted in accordance with PRISMA guidelines. PubMed, Scopus, Web of Science, and CINAHL were searched for systematic reviews published from 2020 to 2022 that examined the determinants of CVI. AMSTAR-2 critical appraisal tool was used to ensure the quality of included reviews, and ROBIS tool was used to evaluate the risk of bias.
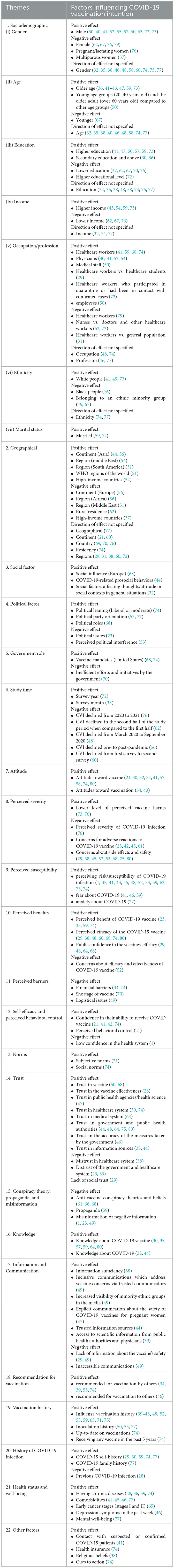
Results: Globally, the average rate of COVID-19 vaccination intention was 56.97%. We identified 21 main determinants of CVI: socio-demographic, geographical location, social, political, government role, study timeline, attitude, perceived severity, perceived susceptibility, perceived benefits, perceived barriers, self-efficacy and perceived behavioral control, norms, trust, conspiracy theory/propaganda/misinformation, knowledge, information and communication, vaccination recommendation, vaccination history, history of COVID-19 infection, and health status and well-being.
Conclusions: These results suggest that COVID-19 vaccination intention is a complex process and is affected by numerous multidimensional factors. Therefore, integrated communication strategies and multifaceted interventions may be effective for improving vaccination intention against COVID-19.
1. Introduction
Several pandemics have been recorded in history, but the emergence of SARS-CoV-2 in the latter part of 2019 is one of the deadliest public health crises in our living memory (1). On January 30, 2020, the World Health Organization (WHO) declared it a Public Health Emergency of International Concern (PHEIC). This declaration was made in response to the rapid spread of the virus beyond China. Various restriction measures were imposed throughout the world to restrain the spread of the virus. As it was a novel Coronavirus, efforts were made to discover its treatment and invent vaccines to combat its challenges. Several vaccines were developed, and as of May 9, 2023, more than 13 billion vaccine doses have been administered. As per WHO Coronavirus Dashboard (2) on May 9, 2023, globally, more than 765 million confirmed cases and 6.9 million deaths were reported. On May 4, 2023, in the fifteenth meeting of the International Health Regulations (2005) Emergency Committee of WHO, it was declared that the ongoing COVID-19 pandemics now an established and ongoing health issue that no longer constitutes a PHEIC. The Committee highlighted the decreasing trend of hospitalization and death due to COVID-19 and the high levels of population immunity to SARS-CoV-2. WHO also emphasized that the virus remains a global health threat as it continues to spread and its new variants are expected to continue to emerge (3).
However, a significant proportion of the world's population is still unvaccinated, posing a continuous public health concern. Some populations, especially women, single, young adults, patients, and healthcare workers, are still hesitant to get primary series or boosters (4–7). Likewise, increasing vaccination rates, especially booster vaccination among specific groups, such as children, was an immense obstacle in some countries, such as Jordan (8), Croatia (9), and China (10). Therefore, to manage COVID-19 and control its new variants, continuous efforts should be made by governments and international health agencies to overcome misperceptions about the virus. Furthermore, in light of the WHO's recent PHEIC declaration for COVID-19 and declining confirmed cases and deaths, vaccination promotion campaigns should not only focus on highlighting the benefits of vaccines and the severity and susceptibility of the virus but also identify the factors that influence public's continuous support for COVID-19 vaccination.
In this study, COVID vaccination intention (CVI) refers to the willingness to be vaccinated, vaccine acceptability including desirability, vaccine demand, and positive attitudes toward the given vaccine, which is contrasted to vaccine hesitancy, the delay or refusal to be vaccinated (11). There are numerous barriers to vaccination campaigns, even when the vaccines are freely accessible or affordable. Some barriers reported by previous studies include psychological (12, 13), socio-economic (14–17), and demographic (18–20).
Numerous systematic reviews, scoping reviews, rapid reviews, and meta-analyses have been published from different parts of the world with the coverage of diverse populations and regions on vaccination intention. However, they reported inconsistent findings with regard to the drivers influencing vaccination acceptance and vaccination intention rates (4, 21–23). Hence, the objective of this meta-review (systematic review of systematic reviews) is to provide a comprehensive overview of existing evidence on factors influencing the COVID-19 vaccination intention published by different types of review and to offer some avenues for future research. More specifically, the present study contributes literature in several ways. First, to our knowledge, this is the first study to systematically map and synthesize key findings of the systematic reviews and identify major factors driving COVID-19 vaccination acceptance. Secondly, this meta-review included different types of reviews including systematic reviews with meta-analyses, scoping reviews, rapid reviews, and systematic review with no meta-analyses for a broader and a holistic understanding about vaccination intention and its determinants reported around the globe. Thirdly, this meta-review provides directions for future research. Finally, this will report an overall global vaccination intention rate and vaccine acceptance across geographic locations.
2. Methodology
A meta-review requires a critical appraisal of the methodological quality of systematic reviews and meta-analyses. For this review, the guidelines of Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) were followed (24, 25). ROBIS (Risk of Bias in Systematic Reviews) tool (26) was used to assess the bias in the search, selection, data extraction, and synthesis. AMSTAR-2 critical appraisal tool (27) was used to ensure the methodological quality of systematic reviews included in this meta-review. In this study, the term ‘systematic reviews' refers to different types of reviews, including systematic reviews with or without meta-analyses, scoping reviews, mapping reviews, literature reviews, and rapid reviews.
2.1. Search strategy
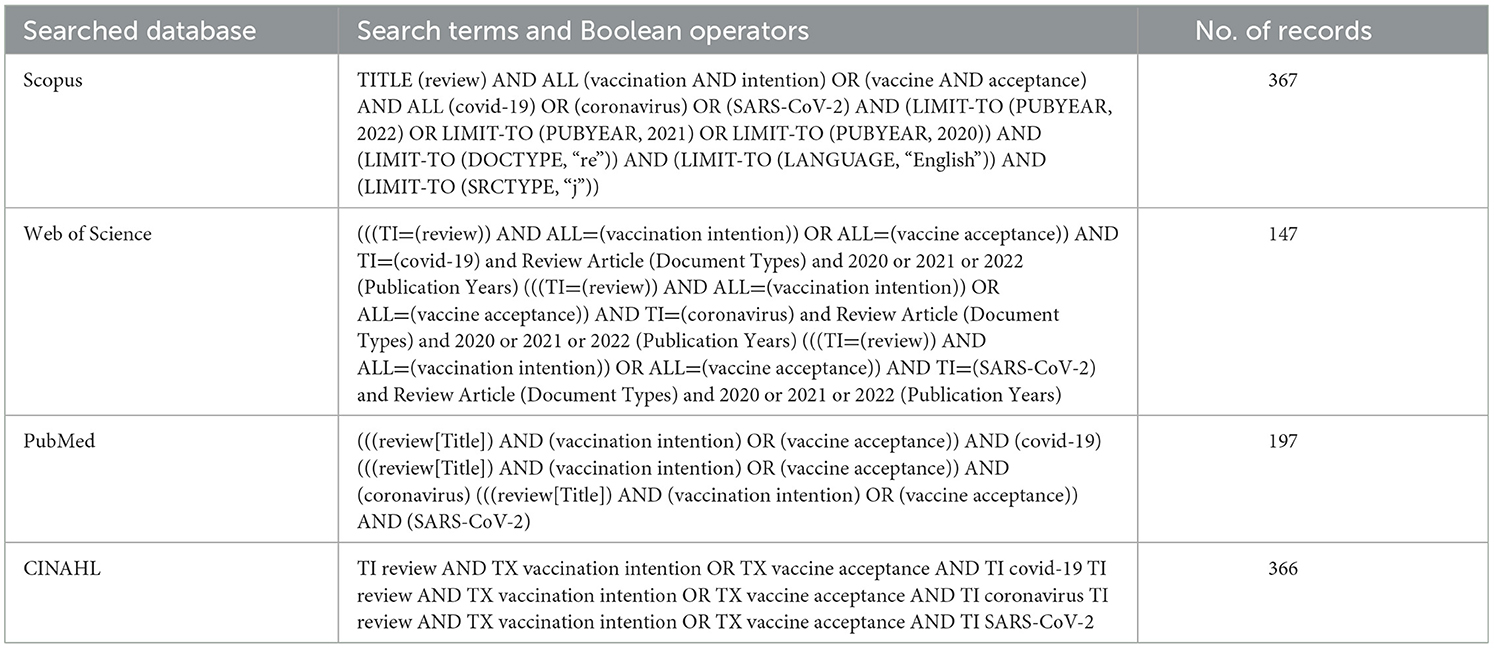
We conducted a comprehensive search of published literature from four databases (PubMed, Web of Science, CINAHL, and Scopus) using various keywords, such as “review”, “vaccination intention”, and “COVID-19”, “coronavirus”, or “SARS-CoV-2”. The combinations of search terms and Boolean operators that were used to locate studies in each database are presented in Table 1.
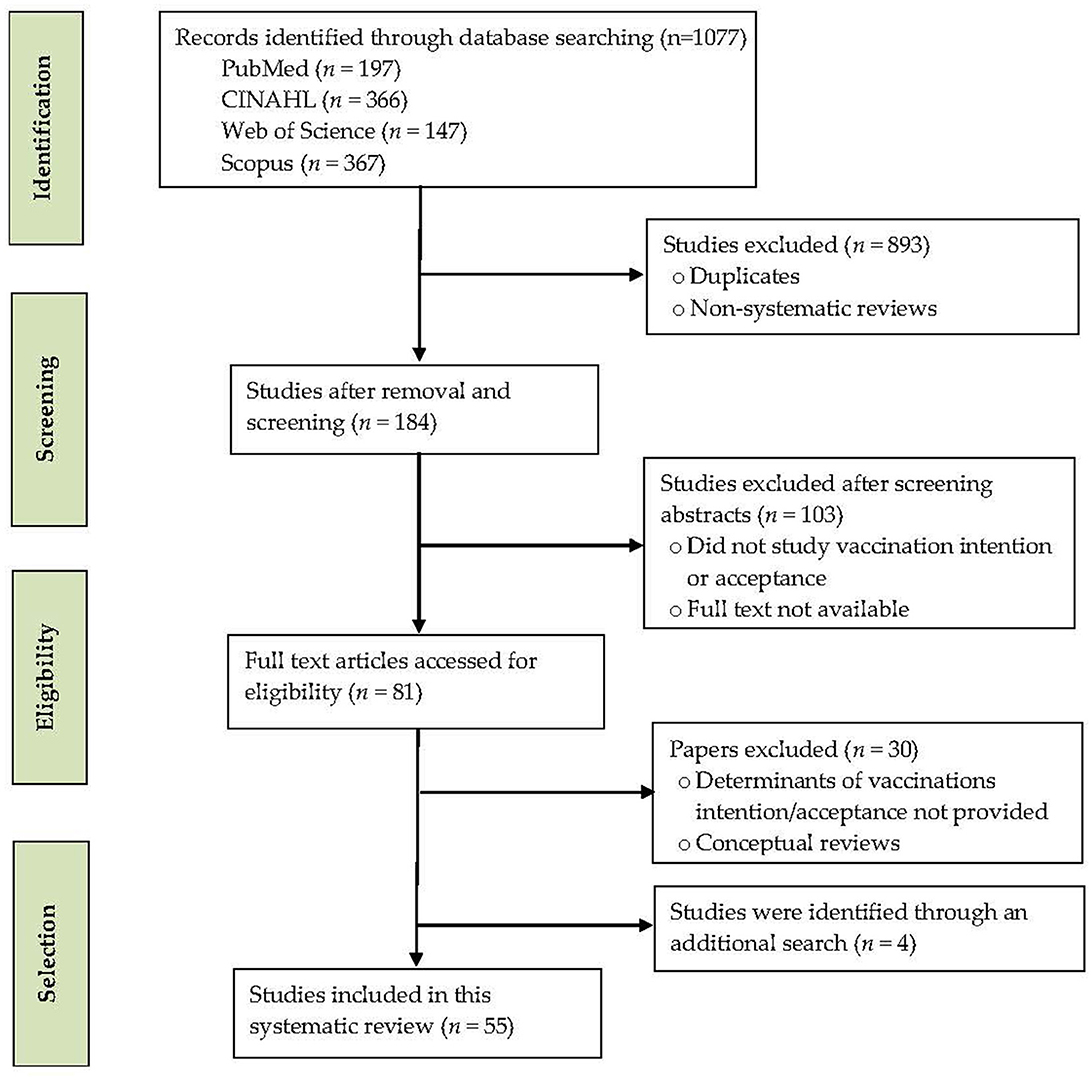
To demonstrate the study selection process, the number of records identified, screened, and excluded, and the reasons for exclusion, a PRISMA flow diagram is drawn (Figure 1). A total of 1077 records were retrieved from the databases. Of them, 893 records were removed for duplicates, non-systematic reviews, and non-peer-reviewed reviews. A total of 103 records were excluded after screening the abstracts that were irrelevant or did not study vaccination intention and its determinants. The remaining 81 full-text systematic reviews were further assessed for eligibility. Furthermore, four eligible systematic reviews were identified through an additional search. Fifty-five full-length reviews published from January 2020 to December 2022 were retrieved for this meta-review.
2.2. Inclusion and exclusion criteria
The following inclusion and exclusion criteria were used to identify relevant systematic reviews.
2.2.1. Inclusion criteria
I. Systematic reviews that reported the predictors of CVI.
II. Systematic reviews published in peer-reviewed journals.
III. Systematic reviews published in English.
2.2.2. Exclusion criteria
I. Systematic reviews that reported the determinants of COVID-19 vaccine hesitancy.
II. Qualitative/narrative reviews.
III. Non-systematic reviews.
IV. Non-peer-reviewed systematic reviews.
Two researchers independently screened the titles and abstracts of the identified systematic reviews. Full-text systematic reviews were obtained whose titles and abstracts met inclusion criteria. All full-text systematic reviews were then evaluated to confirm if they reported necessary information or statistics on vaccination intention with respect to COVID-19.
2.3. Risk of bias
To ensure the methodological quality and risk of bias, ROBIS tool was used as per the guidelines of Whiting et al. (26). To evaluate the level of bias present in a systematic review and to assess specific concerns about potential biases in the search, selection, data extraction, and synthesis, ratings were used to judge the overall risk of bias. The signaling questions were answered as “yes”, “probably yes”, “probably no”, “no”, or “no information”. The subsequent level of concern about bias associated with each domain was then judged as “low”, “high”, or “unclear”. If the answers to all signaling questions for a domain were “yes” or “probably yes”, the level of concern was judged as low. If any signaling question was answered “no” or “probably no”, then a bias existed. Two researchers independently used the ROBIS tool to perform risk of bias and to identify eligible systematic reviews to be included in the present meta-review. Any disagreements were resolved through discussion or a decision made by an expert, a third umpire. Similarly, the selection of databases or digital libraries was also decided with consensus.
2.4. Critical appraisal of included reviews
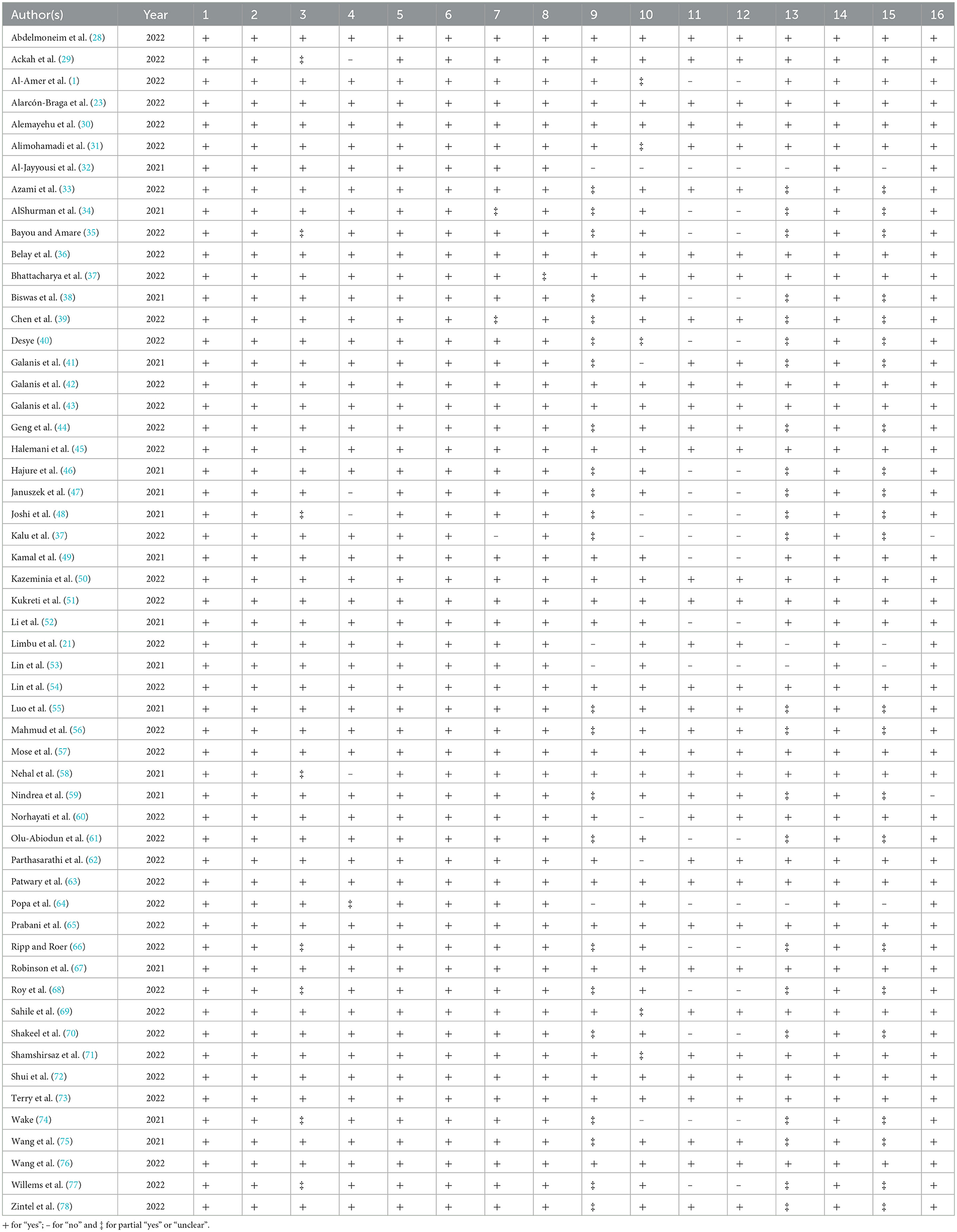
A critical appraisal of included reviews was conducted using the tool AMSTAR-2 (27) and displayed in Table 2. It was noticed that a few reviews did not meet some criteria. However, most studies complied with a large number of criteria. All the included reviews fulfilled some criteria, such as 1, 2, 5, 6, and 14. They were marked by a + sign or “yes”. Criterion 1 is about the components of PICO (population, intervention, control group, and outcome), whether the included reviews have details of PICO or not. We found that all reviews met this criterion. Similarly, all the reviews also complied with criteria 2, 5, 6, and 14. Criterion 6 is about unbiased data extraction, and we found that data extraction of all included reviews was unbiased; similarly, criterion 14 (the discussion of heterogeneity) was observed in the results.
The highest number of negative responses, i.e., “no” or—sign, was recorded for criteria 11 and 12. Out of 55 reviews included in the present study, approximately one-third, i.e., 20 reviews, did not perform a meta-analysis. These reviews also did not comply with criterion 12. Partial “yes” or “unclear” or ‡ sign was also recorded. The highest responses were recorded for criteria 9, 13, and 15. Five out of 55 reviews did not meet criterion 4 (29, 47, 48, 58, 64). These reviews were based on a search of a single database; the remaining searched two or more databases.
Overall, we found that the vast majority of the reviews satisfied most of the necessary AMSTAR-2 criteria. However, in many cases, not meeting the criteria was due to the fact that there was no mention of the element in the review or it was not stated explicitly enough for the reader to comprehend. There are several reasons for this, such as publishing guidelines of the specific journal, word limitation, different standards of different journals, and the requirement topic chosen for review.
2.5. Data extraction and analysis
Data extraction was also performed by the same two researchers independently. The main information that were extracted from studies included author's name, publication year, type of systematic review, vaccination intention rate (%), searched databases, study objective, participants (study population), number of studies included, and determinants of CVI. IBM SPSS Statistics 27 was used to analyze the data.
3. Results
3.1. Description of included systematic reviews
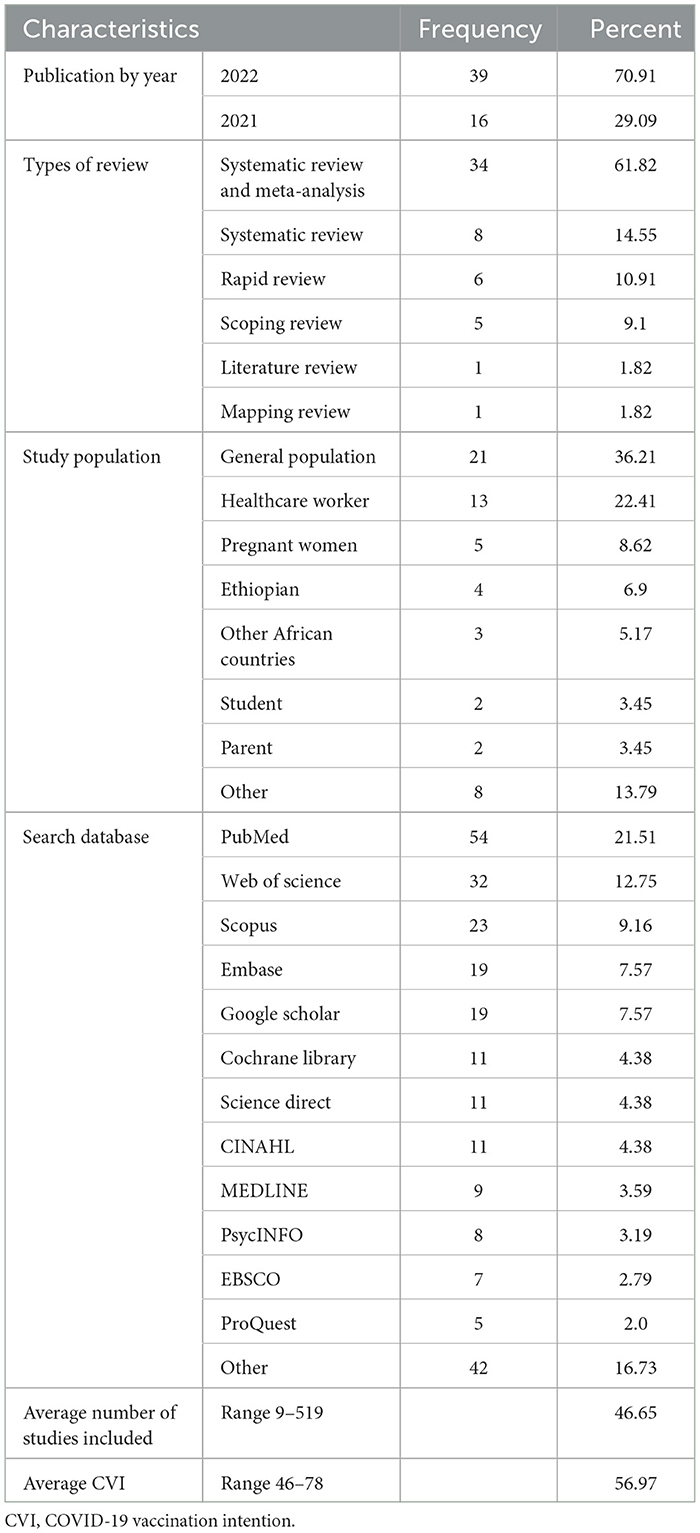
As presented in Tables 3, 4, the majority of the systematic reviews (70.91%) included in this meta-review were published in 2022, and the remaining were published in 2021. Most reviews (61.82%) were systematic reviews with meta-analyses, followed by systematic reviews with no meta-analyses, rapid reviews, scoping reviews, literature reviews, and mapping reviews. The most frequently searched database was PubMed (54/55), followed by Web of Science (32/55), Scopus (23/55), Embase (19/55), Google Scholar (19/55), Cochrane Library (11/55), Science Direct (11/55), CINAHL (11/55), MEDLINE (9/55), PsycINFO (8/55), and EBSCO (7/55). Twenty-one reviews focused on the general adult population, healthcare workers (13/55), and pregnant women (5/55). The studies included in this meta-review consisted of 2,519 studies conducted across the globe, with an average study of 46.65 (standard deviation = 72.4), ranging from 9 (47) to 519 (76). The systematic review and meta-analysis included the highest average number of studies (50), followed by scoping review (44), systematic review (35), and rapid review (34).
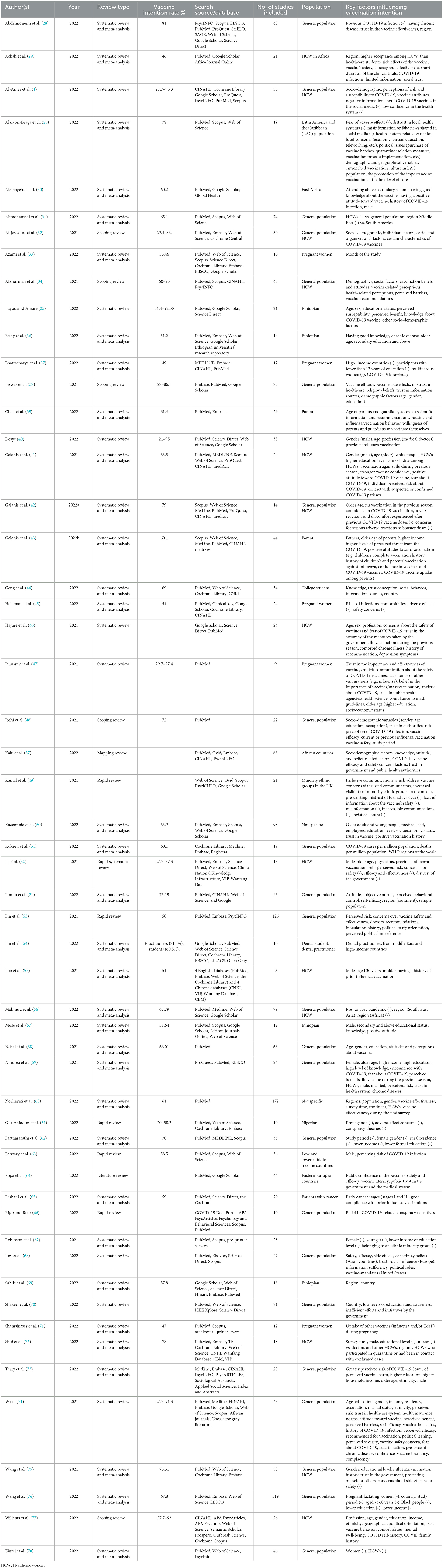
Table 4. Characteristics of included reviews and factors influencing COVID-19 vaccination intention.
Table 4 presents vaccination intention rates reported by the included reviews. The average rate of COVID-19 vaccination intention was 56.97% (SD = 20.05), ranging from 46% (29) to 78% (23). The highest average vaccination intention rate was reported by systematic reviews with meta-analyses (62.53%), followed by rapid reviews (54.25%). Vaccination acceptance rate differed by population type (F(4, 24) = 3.845, p ≤ 0.05). Average vaccination intention rate was highest among general populations (68.36%), followed by healthcare workers (64.8%) and parents (60.75%). Vaccine acceptance was lowest among pregnant women (50.87%).
3.2. Factors influencing COVID-19 vaccination intention
3.2.1. Socio-demographic
Table 5 shows that the most frequent socio-demographic predictors of CVI were gender, age, education, income, occupation, ethnicity, and marital status. Gender predicted CVI in almost one-half of the included reviews (27/55). Several reviews indicated that males were more likely to accept COVID vaccines than females (30, 40, 41, 52, 55, 57, 60, 63, 72, 73). Other reviews reported that women were less willing to get vaccinated against COVID-19 (37, 62, 67, 76, 79). Similarly, Wang et al. (76) reported that pregnant/lactating women have the lowest vaccination intention.
Several reviews reported that older people were more likely to accept COVID vaccines (36, 41–43, 47, 52, 59, 73). On the other hand, younger individuals were less likely to get vaccinated against COVDI-19 (67). However, Kazeminia et al. (50) revealed mixed findings; young age groups (20–40 years old) and the older adult population (over 60 years old) demonstrated more CVI than other age groups.
Twenty-one reviews reported education attainment as a significant predictor of CVI, but findings are inconclusive. A higher level of educational attainment was positively associated with a higher level of CVI in eight reviews (30, 36, 41, 47, 50, 57, 59, 73). Conversely, a lower level of education was negatively associated with CVI in five studies (37, 62, 67, 70, 76). On the contrary, Shui et al. (72) reported the opposite in which the willingness of healthcare workers to vaccinate against COVID-19 declined with higher levels of education.
Ethnicity was a significant predictor of CVI in six reviews. For example, a higher level of COVID-19 vaccine acceptance was found in White people (41, 49, 73). Conversely, Black people (76) and minorities (67) demonstrated lower CVI. Similarly, a study showed that ethnic minorities had significantly lower vaccine uptake compared to White British groups (49).
In regard to marital status, married individuals were more likely to accept COVID vaccines (59, 74). When it comes to income, higher income was positively associated with a higher level of CVI (43, 54, 59, 73). On the other hand, people with lower incomes had lower vaccine acceptance (62, 67, 76).
Contradictory evidence was reported on the association between occupation and CVI. For example, eleven reviews reported that healthcare workers such as dental practitioners (54) were more likely to accept COVID vaccines (29, 40, 41, 50, 52, 59, 60, 72, 74). However, two reviews found the opposite (31, 79). Therefore, the impact of occupation on healthcare workers' intentions to get vaccinated has not yet been confirmed (55).
3.2.2. Geographical factors
Geographical factors such as region, country, continent, and residency were found to be associated with CVI, but the findings are mixed. For example, a higher COVID-19 vaccine acceptance rate was reported in South-East Asia (44, 56), the Middle East (54), high-income countries (54), South America (31), and WHO regions of the world (51). On the contrary, other studies reported lower COVID-19 vaccine acceptance in high-income countries (37), Europe (44), Africa (56), the Middle East (31), and rural areas (62).
3.2.3. Social factor
Roy et al. (68) highlighted the role of social influence on CVI. The authors revealed that opinions from friends, family, and social networks significantly affected CVI, especially in Europe and the United States. Geng et al. (44) found that COVID-19-related prosocial behaviors (e.g., donating resources and providing help to those affected by COVID-19) were positively associated with increased CVI. Social factors that affected people's thoughts or attitudes in social contexts in general situations (e.g., social density, prosocial concern, communication and media, social solidarity) positively impacted vaccination intention against COVID-19 (34).
3.2.4. Political factor
Major political factors that influenced CVI included political leaning (being moderate or liberal) (74), political party orientation (54, 77), and political roles (68). Other factors that had negative associations with CVI were political issues (i.e., purchase of vaccine batches, quarantine isolation measures, vaccination process implementation) (23) and perceived political interference (53).
3.2.5. Government role
Vaccine mandates in the United States (68) and believing in mandatory COVID-19 vaccination (74) were significant determinants of COVID-19 vaccine acceptance. However, inefficient efforts and initiatives by the government had an adverse effect on CVI (70).
3.2.6. Study timeline
Vaccination intentions varied by survey time (72). For example, most reviews reported that the average COVID-19 acceptance rate declined over time. In addition, the acceptance rate declined in the second survey period compared to the first survey period (60), in the second half of the study period when compared to the first half (62), from March 2020 (86%) to September 2020 (72%) (48) and from pre-pandemic period to post-pandemic period (56). Furthermore, the acceptance rate declined globally from December 2020 to late 2021 (76). On the contrary, one study reported that the pooled acceptance rate of COVID-19 vaccine among healthcare workers in China was higher in 2021 than in 2020 (72).
3.2.7. Attitude
Attitudes toward vaccines (21, 30, 32, 34, 41, 57, 58, 74, 80) and attitudes toward vaccination (34, 43) were positively associated with CVI. Moreover, the attitude had a significant influence in Asia, Europe, and Oceania, especially among adults, parents, and patients (21).
3.2.8. Perceived severity
Several studies identified the perceived severity of COVID-19 infection (74), concerns for adverse reactions to COVID-19 vaccine (23, 41, 45, 61), and concerns about side effects and safety of COVID vaccines (29, 38, 45, 52, 53, 68, 75, 80) as the common predictors of COVID-19 vaccine acceptance. In addition, Halemani et al. (45) stated that adverse effects were the top indicators for rejecting the COVID vaccine. On the other hand, a lower level of perceived vaccine harms (73, 74) was positively related to CVI.
3.2.9. Perceived susceptibility
The association between perceived susceptibility (perceived risk of contracting COVID-19) and CVI was reported in 17 studies. Perceiving susceptibility to COVID-19 infection (1, 35, 41, 43, 45, 48, 52, 53, 59, 63, 73, 74), fear about COVID-19 (41, 46, 59) and anxiety about COVID-19 (47) were key drivers of CVI. In addition, the risks of infections were one of the main reasons for accepting the COVID vaccine in pregnant women (45).
3.2.10. Perceived benefits
Our study also shows that the perceived benefit of the COVID-19 vaccine (35, 59, 74, 75), perceived efficacy of the COVID-19 vaccine (29, 38, 47, 48, 60, 68, 74, 80), and public confidence in the vaccines' efficacy (29, 48, 64, 68) positively influenced CVI. Similarly, Januszek et al. (47) found the perceived effectiveness of the vaccine as a strong factor co-existing with the acceptance of the COVID-19 vaccination during pregnancy. On the other hand, concerns about the efficacy and effectiveness of the COVID-19 vaccine negatively impacted CVI in healthcare workers (52).
3.2.11. Perceived barriers
A few reviews reported that perceived vaccination barriers such as shortage of vaccines (79), logistical issues (49), and financial barriers (34, 74) significantly impaired vaccination intention against COVID-19.
3.2.12. Self-efficacy and perceived behavioral control
People's confidence in their ability to receive the COVID-19 vaccine (21, 41, 42, 74) influenced COVID-19 vaccine acceptance. For example, low confidence in the health system reduced CVI (1). In a systematic review and meta-analysis, perceived behavioral control (i.e., whether the ability to get the vaccine is within an individual's control) was found as one of the dominant drivers of vaccination intention, especially among African patients (21).
3.2.13. Norms
Limbu et al. (21) showed that subjective norms (i.e., the perception that a family member would support them in having a COVID-19 vaccination) had a dominant effect on CVI in Asia and Oceania, especially among parents and patients. Another study found social norms (i.e., whether valued others support getting a vaccine) as an influential predictor of behavioral intention to vaccinate against COVID-19 (72).
3.2.14. Trust
Numerous reviews reported trust as a crucial determinant of CVI. Trust-related factors that affected CVI included trust in the vaccine (50, 68), trust in the vaccine effectiveness (28), trust in public health agencies/health science (47), trust in healthcare system (59, 74), trust in medical system (64), trust in government and public health authorities (44, 48, 64, 75, 80), trust in the accuracy of the measures taken by the government (46), and trust in information sources (38, 44). On the contrary, people's mistrust of the healthcare system (38) and distrust of the government and healthcare system (23, 53) decreased CVI. A low acceptance of the COVID-19 vaccine was impacted by the lack of social trust (i.e., insufficient trust in the vaccine's source, lack of trust from the manufacturers, and lack of trust from governments) (29).
3.2.15. Conspiracy theory, propaganda, and misinformation
Some studies found that anti-vaccine conspiracy theories and beliefs (61, 66, 68), propaganda (61), and misinformation or negative information (1, 23, 49) significantly impaired people's intentions to get vaccinated against COVID-19.
3.2.16. Knowledge
A higher level of knowledge about COVID-19 vaccines was positively associated with a higher level of vaccination intention (30, 35, 57, 59, 64, 80). Likewise, knowledge about COVID-19 significantly increased people's vaccination intentions (32, 44).
3.2.17. Information and communication
Information- and communication-related factors such as information sufficiency (68), inclusive communications which address vaccine concerns via trusted communicators (49), increased visibility of minority ethnic groups in the media (49), explicit communication about the safety of COVID-19 vaccines for pregnant women (47), trusted information sources (44), and access to scientific information from public health authorities and physicians (39) were strong drivers of CVI. On the contrary, lack of information about the vaccine's safety (29, 49) and inaccessible communications (49) were significant barriers to CVI.
3.2.18. Recommendation for vaccination
Some reviews indicated that people's vaccination intentions were influenced by the recommendations from public health authorities and physicians (34, 39, 53, 74). In addition, people's tendencies to recommend vaccination to others were positively associated with CVI (46).
3.2.19. Vaccination history
Past vaccine behavior was one of the most powerful predictors of the willingness to be vaccinated against COVID-19 (77). Inoculation history (50, 53), including influenza vaccination history (39–43, 46, 48, 52, 55, 59, 65, 71, 75), up-to-date vaccinations (74), and receiving any vaccine in the past 5 years (74) were positively associated with a higher level of CVI.
3.2.20. History COVID-19 infection
Some reviews reported that prior COVID-19 infection (29, 30, 59, 74, 77) and family history of COVID-19 infection (77) were significant determinants of CVI. Conversely, one study showed that previous COVID-19 infection was associated with a lower intention to have the booster dose (28).
3.2.21. Health status and well-being
Individuals with chronic diseases (28, 36, 59, 74), such as comorbidities (41, 45, 46, 77) and early cancer stages (65), were more likely to get vaccinated against COVID-19. Similarly, mental well-being was positively associated with increased CVI (77). However, one study reported that depression symptoms strengthened the willingness to get vaccinated (46).
3.2.22. Other factors
Other common determinants affecting vaccination intention included health insurance (74), religious beliefs (38), and cues to action (74).
4. Discussion
Mass vaccination is the most successful and cost-effective public health intervention to overcome a pandemic like COVID-19, as it has significantly contributed to improving global health by reducing mortality caused due to many infectious diseases (81, 82). However, despite the availability of vaccines and the mass global drive for vaccination, many people remain hesitant to be vaccinated, are less inclined to receive booster shots, or are even less likely to vaccinate their offspring (21). As a result, several countries, including some African countries, have low vaccination rates or yet to achieve herd immunity (81). There are several barriers to achieving the desired goal of vaccination coverage. According to Alam et al. (83), to achieve a higher coverage of the vaccines and to attain herd immunity, it is essential to elicit a positive attitude toward COVID-19 vaccines amongst individuals and populations. Furthermore, it is imperative to identify the causes of refusal/hesitancy and accordingly develop appropriate interventions. Hence, this meta-review was carried out to provide a comprehensive understanding of the factors influencing COVID-19 vaccination intention. The results of this study will be helpful to the agencies involved in vaccination and the prevention and control of pandemics around the globe.
This meta-review found a moderate COVID-19 vaccination acceptance rate of 56.97% globally. Vaccine acceptance was higher among healthcare workers, parents, and seniors, but some populations, such as young people and women, were more hesitant to receive primary series or booster doses. These results indicate that there is a need to improve vaccine coverage among specific populations (76). Thus, targeted communication and intervention approaches can be used to increase vaccine uptake among such populations.
We identified twenty-one main clusters of predictors that influenced COVID-19 vaccination acceptance, including socio-demographic, geographical, political, attitude, perception, norm, trust, knowledge, and vaccine-related factors. These results indicate that COVID-19 vaccination acceptance is a complex process and is affected by numerous multifaceted factors.
The most frequent socio-demographic predictors of vaccine acceptance were gender, age, education, income, and occupation. All systematic reviews that synthesized evidence on gender effect concluded that females were more likely to be vaccine-hesitant. In terms of age, younger individuals were associated with being less likely to intend to vaccinate. In addition, several studies reported that ethnic minorities and individuals with a lower level of income and education had a lower level of intention to get vaccinated against COVID-19. Thus, these results clearly suggest that it is important to understand why different socio-demographic groups, such as females, young individuals, and low-income populations, demonstrate lower intentions to vaccinate against COVID-19 and develop targeted information campaigns and interventions that could enhance their vaccination intentions (62, 67). However, such campaigns should focus on improving awareness of the efficacy of COVID-19 vaccines (36).
Results also show that COVID-19 vaccine acceptance varies by geographic location. This variability was evident in different countries and regions of the world. However, the evidence is contradictory and inconclusive. For example, some reviews reported higher vaccine acceptance rates in South-East Asia, the Middle East, high-income countries, South America, and WHO regions of the world (31, 44, 51, 54, 56). On the contrary, other reviews reported lower vaccine acceptance in high-income countries, Europe, Africa, the Middle East, and rural areas (31, 37, 44, 56, 62). More research is needed to shed light on regional disparities in COVID-19 vaccine acceptance (56). Moreover, reasons for not accepting COVID-19 vaccines should be investigated across different geographic locations (region, country, residency), and targeted measures should be taken into account to improve COVID-19 vaccine acceptance according to their local contexts (76).
Our results show that social factors were influential drivers of individuals' vaccination willingness. Opinions provided by friends, family, and social networks had significant effects on vaccine acceptance. In addition, COVID-19-related prosocial behaviors (e.g., donating resources and providing help to those affected by COVID-19) and social factors that affected people's thoughts or attitudes in social contexts in general situations (e.g., social density, prosocial concern, communication and media, social solidarity) positively impacted vaccination acceptance. Moreover, recommendations from public health authorities and healthcare providers influenced people's vaccination intentions. Moreover, individuals' vaccination intentions were influenced by the recommendations from public health authorities and healthcare providers. Thus, effective vaccination communication strategies may include encouragement from loved ones and trusted figures, such as family, friends, physicians and religious leaders (84).
The decision to accept COVID-19 vaccination was also influenced by political factors (e.g., political leaning, political roles, political interference) and government roles (e.g., vaccine mandates, government initiatives). Hence, government institutions should implement strategies that help to eliminate political barriers. In addition, COVID-19 vaccine mandates for healthcare workers and other vulnerable populations (e.g., older adult and co-morbid individuals) and information dissemination and recommendations from trusted government officials and political leaders can be effective strategies in improving vaccination acceptance (68).
Individual factors, such as attitudes (e.g., attitudes toward vaccination and vaccines), perceptions, and beliefs, were dominant predictors of CVI. An effective attitude change strategy for COVID-19 vaccine uptake will benefit from focusing on populations with negative attitudes, especially among adults, parents, and patients in Asian, European, and Oceania countries (21). The results of the present study show that the most frequently demonstrated perceptions and beliefs that impacted vaccination intentions were perceived severity, perceived susceptibility, perceived benefits, perceived barriers, self-efficacy, and perceived behavioral control. Therefore, future public awareness and educational campaigns aimed at promoting COVID-19 vaccines should focus on these factors and consider using psychological theories such as the health belief model and theory of planned behavior as conceptual frameworks for designing stimuli and effective interventions (4, 21, 85). Such campaigns should highlight the potential risk of contracting COVID-19/risks of infections, the advantage of COVID-19 vaccines, and the efficacy of the COVID-19 vaccines. More importantly, further data and information on the safety and efficacy of vaccines should be provided with transparency (52). To enhance public confidence and uptake of COVID vaccines, addressing people's vaccine-related concerns, such as side effects and adverse reactions, is essential. It is also vital to address vaccination barriers, such as concerns associated with accessibility and cost of vaccines. However, integrated global efforts are required to overcome such barriers (56).
Numerous reviews included in our study reported distrust (e.g., lack of trust in vaccines, public health agencies, healthcare system, medical system, and information sources) and anti-vaccine conspiracy theories/beliefs (e.g., misinformation or negative information) as significant determinants of vaccination intention. Governments and other stakeholders engaged in the production, promotion, and distribution of vaccines should strengthen their credibility and convey trusted information through credible sources, focusing on transparency and restoring trust in health authorities. The spread of misinformation regarding vaccination and conspiracy theories should be taken very seriously and counterbalanced by targeted interventions and communication campaigns (53, 70, 77).
Some studies showed that a higher level of knowledge about COVID-19 vaccines and information- and communication-related factors (e.g., information sufficiency, inclusive communications, explicit communication about vaccine safety, and access to scientific information from public health authorities and healthcare providers) were strong drivers of vaccine acceptance. On the contrary, lack of information about the vaccine's safety and inaccessible communications were significant barriers. Therefore, governments and healthcare providers have to pay more attention to individuals and populations with lower levels of knowledge and implement policies to elevate their awareness about vaccination and vaccines through targeted education programs that are designed to increase their self-efficacy (21).
History of previous vaccination against COVID-19 or influenza was one of the most prevalent predictors of the willingness to be vaccinated against COVID-19. Moreover, a family history of COVID-19 infection was associated with a higher intention to have additional doses. Individuals with poor health (e.g., chronic diseases, comorbidities) were more likely to get vaccinated against COVID-19. Thus, these factors should be taken into account when developing interventions aimed at decreasing COVID-19 vaccine hesitancy.
This meta-review has several limitations; thus, the significance of these findings should be interpreted with caution. For example, we searched only four databases to locate systematic reviews; thus, some relevant studies might have been overlooked. In addition, systematic reviews included in this meta-review varied in terms of study populations and countries, which might have contributed to their inconsistent findings. Finally, we excluded non-English systematic reviews, which may limit the scope and validity of our results or may present publication bias.
This meta-review identified several important areas for future research: (1) several studies included in this review reported mixed findings, which warrants future research. Further studies are needed to shed light on inconclusive evidence, especially in regard to the role of gender, education, occupation, and geographic location; (2) a micro-level study should be conducted to understand minute cultural issues of COVID-19 vaccine hesitancy and acceptance; (3) this meta-review shows that vaccine acceptance was found lower among young individuals and women, hence future primary studies could investigate the reasons for their unwillingness to get vaccinated; (4) social and mass media have a pivotal role in promoting or making rumors against vaccines. Thus, future studies should explore deeper insights into the role of social media as a promoter or a barrier to vaccination campaigns; and (5) future research is needed to examine the impact of social capital (bonding, bridging, and linking) and a reference group (a person or group of people that significantly influences an individual's behavior) in influencing vaccination intention.
5. Conclusion
This meta-review reveals that there are wide disparities in vaccine acceptance across the globe, and several factors (e.g., psychological, demographic, geographical, political, and social) affect individuals' decision to accept a COVID-19 vaccine. A holistic educational approach to improve confidence in COVID-19 vaccines and multifaceted interventions may be effective for improving vaccination intention against COVID-19. However, a country- and population-specific strategy at amicro-level is required for a successful mass vaccination drive and manage the COVID-19.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
All authors listed have made a substantial, direct, and intellectual contribution to the work and approved it for publication.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Al-Amer R, Maneze D, Everett B, Montayre J, Villarosa AR, Dwekat E, et al. COVID-19 vaccination intention in the first year of the pandemic: a systematic review. J Clin Nurs. (2022) 31:62–86. doi: 10.1111/jocn.15951
2. World Health Organization. Coronavirus (COVID-19) Dashboard. Available online at: https://covid19.who.int/ (accessed January 18, 2023).
3. World Health Organization. Statement on the fifteenth meeting of the IHR (2005) Emergency Committee on the COVID-19 pandemic. (2023). Available online at: https://www.who.int/news/item/05-05-2023-statement-on-the-fifteenth-meeting-of-the-international-health-regulations-(2005)-emergency-committee-regarding-the-coronavirus-disease-(covid-19)-pandemic (accessed May 14, 2023).
4. Limbu YB, Gautam RK, Pham L. The health belief model applied to COVID-19 vaccine hesitancy: a systematic review. Vaccines. (2022) 10:973. doi: 10.3390/vaccines10060973
5. Ratzan S, Schneider EC, Hatch H, Cacchione J. Missing the Point — How Primary Care Can Overcome Covid-19 Vaccine “Hesitancy”. N Engl J Med. (2021) 384:e100. doi: 10.1056/NEJMp2106137
6. Limbu YB, Huhmann BA. Why some people are hesitant to receive COVID-19 boosters: a systematic review. Trop Med Infect Dis. (2023) 8:159. doi: 10.3390/tropicalmed8030159
7. Umakanthan S, Lawrence S. Predictors of COVID-19 vaccine hesitancy in Germany: a cross-sectional, population-based study. Postgrad Med J. (2022) 98:756–64. doi: 10.1136/postgradmedj-2021-141365
8. Al-Qerem W, Al Bawab AQ, Hammad A, Ling J, Alasmari F. Willingness of the Jordanian population to receive a COVID-19 booster dose: a cross-sectional study. Vaccines. (2022) 10:410. doi: 10.3390/vaccines10030410
9. De Giorgio A, Kuvačić G, Maleš D, Vecchio I, Tornali C, Ishac W, et al. Willingness to receive COVID-19 booster vaccine: associations between green-pass, social media information, Anti-Vax beliefs, and emotional balance. Vaccines. (2022) 10:481. doi: 10.3390/vaccines10030481
10. Zhou M, Liu L, Gu SY, Peng XQ, Zhang C, Wu QF, Xu XP, You H. Behavioral intention and its predictors toward COVID-19 booster vaccination among chinese parents: applying two behavioral theories. Int J Environ Res Public Health. (2022) 19:7520. doi: 10.3390/ijerph19127520
11. Gates A, Gates M, Rahman S, Guitard S, MacGregor T, Pillay J, et al. A systematic review of factors that influence the acceptability of vaccines among Canadians. Vaccine. (2021) 39:222–36. doi: 10.1016/j.vaccine.2020.10.038
12. Murphy J, Vallières F, Bentall RP, Shevlin M, McBride O, Hartman TK, et al. Psychological characteristics associated with COVID-19 vaccine hesitancy and resistance in Ireland and the United Kingdom. Nat Commun. (2021) 12:29. doi: 10.1038/s41467-020-20226-9
13. Barello S, Palamenghi L, Graffigna G. Looking inside the ‘black box' of vaccine hesitancy: unlocking the effect of psychological attitudes and beliefs on COVID-19 vaccine acceptance and implications for public health communication. Psychol Med. (2023) 53:1120–1. doi: 10.1017/S003329172100101X
14. Chadwick A, Kaiser J, Vaccari C, Freeman D, Lambe S, Loe BS, et al. Online social endorsement and Covid-19 vaccine hesitancy in the United Kingdom. Soc Media Soc. (2021) 7:205630512110088. doi: 10.1177/20563051211008817
15. Allington D, McAndrew S, Moxham-Hall V, Duffy B. Coronavirus conspiracy suspicions, general vaccine attitudes, trust and coronavirus information source as predictors of vaccine hesitancy among UK residents during the COVID-19 pandemic. Psychol Med. (2021) 1:1–2. doi: 10.1017/S0033291721001434
16. Soares P, Rocha JV, Moniz M, Gama A, Laires PA, Pedro AR, et al. Factors associated with COVID-19 vaccine hesitancy. Vaccines. (2021) 9:300. doi: 10.3390/vaccines9030300
17. Guzman-Holst A, DeAntonio R, Prado-Cohrs D, Juliao P. Barriers to vaccination in Latin America: a systematic literature review. Vaccine. (2020) 38:470–81. doi: 10.1016/j.vaccine.2019.10.088
18. Al-Mohaithef M, Padhi BK. Determinants of COVID-19 vaccine acceptance in Saudi Arabia: a web-based national survey. J Multidiscip Healthc. (2020) 13:1657–63. doi: 10.2147/JMDH.S276771
19. Wang J, Jing R, Lai X, Zhang H, Lyu Y, Knoll MD, et al. Acceptance of COVID-19 vaccination during the COVID-19 pandemic in China. Vaccines. (2020) 8:482. doi: 10.3390/vaccines8030482
20. Fisher KA, Bloomstone SJ, Walder J, Crawford S, Fouayzi H, Mazor KM. Attitudes toward a potential SARS-CoV-2 vaccine: a survey of US adults. Ann Intern Med. (2020) 173:964–73. doi: 10.7326/M20-3569
21. Limbu YB, Gautam RK, Zhou W. Predicting vaccination intention against COVID-19 using theory of planned behavior: a systematic review and meta-analysis. Vaccines. (2022) 10:2026. doi: 10.3390/vaccines10122026
22. Cascini F, Pantovic A, Al-Ajlouni YA, Failla G, Puleo V, Melnyk A, et al. Social media and attitudes towards a COVID-19 vaccination: a systematic review of the literature. eClinicalMedicine. (2022) 48:101454. doi: 10.1016/j.eclinm.2022.101454
23. Alarcón-Braga EA, Hernandez-Bustamante EA, Salazar-Valdivia FE, Valdez-Cornejo VA, Mosquera-Rojas MD, Ulloque-Badaracco JR, et al. Acceptance towards COVID-19 vaccination in Latin America and the Caribbean: a systematic review and meta-analysis. Travel Med Infect Dis. (2022) 49:102369. doi: 10.1016/j.tmaid.2022.102369
24. Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JPA, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med. (2009) 6:e1000100. doi: 10.1371/journal.pmed.1000100
25. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. Updating guidance for reporting systematic reviews: development of the PRISMA 2020 statement. J Clin Epidemiol. (2021) 134:103–12. doi: 10.1016/j.jclinepi.2021.02.003
26. Whiting P, Savović J, Higgins JPT, Caldwell DM, Reeves BC, Shea B, et al. A new tool to assess risk of bias in systematic reviews was developed. J Clin Epidemiol. (2016) 69:225–34. doi: 10.1016/j.jclinepi.2015.06.005
27. Shea BJ, Reeves BC, Wells G, Thuku M, Hamel C, Moran J, et al. AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ. (2017) 358:j4008. doi: 10.1136/bmj.j4008
28. Abdelmoneim SA, Sallam M, Hafez DM, Elrewany E, Mousli HM, Hammad EM, et al. COVID-19 vaccine booster dose acceptance: systematic review and meta-analysis. Trop Med Infect Dis. (2022) 7:298. doi: 10.3390/tropicalmed7100298
29. Ackah M, Ameyaw L, Gazali Salifu M, Afi Asubonteng DP, Osei Yeboah C, Narkotey Annor E, et al. COVID-19 vaccine acceptance among health care workers in Africa: A systematic review and meta-analysis. PLoS ONE. (2022) 17:e0268711. doi: 10.1371/journal.pone.0268711
30. Alemayehu A, Demissie A, Yusuf M, Gemechu Lencha A, Oljira L. Covid-19 vaccine acceptance and determinant factors among general public in East Africa: a systematic review and meta-analysis. Health Serv Res Manag Epidemiol. (2022) 9:233339282211062. doi: 10.1177/23333928221106269
31. Alimohamadi Y, Hosamirudsari H, Hesari E, Sepandi M. Global COVID-19 vaccine acceptance rate: a systematic review and meta-analysis. J Public Health. (2022) 1–13. doi: 10.1007/s10389-022-01757-5
32. Al-Jayyousi GF, Sherbash MAM, Ali LAM, El-Heneidy A, Alhussaini NWZ, Elhassan MEA, et al. Factors influencing public attitudes towards COVID-19 vaccination: a scoping review informed by the socio-ecological model. Vaccines. (2021) 9:548. doi: 10.3390/vaccines9060548
33. Azami M, Nasirkandy MP, Esmaeili Gouvarchin Ghaleh H, Ranjbar R. COVID-19 vaccine acceptance among pregnant women worldwide: a systematic review and meta-analysis. PLoS ONE. (2022) 17:e0272273. doi: 10.1371/journal.pone.0272273
34. AlShurman BA, Khan AF, Mac C, Majeed M, Butt ZA. What demographic, social, and contextual factors influence the intention to use COVID-19 vaccines: a scoping review. Int J Environ Res Public Health. (2021) 18:9342. doi: 10.3390/ijerph18179342
35. Bayou FD, Amare SN. Acceptance of COVID-19 vaccine and its associated factors among Ethiopian population: a systematic review. Patient Prefer Adherence. (2022) 16:1093–103. doi: 10.2147/PPA.S360174
36. Belay GM, Alemu TG, Techane MA, Wubneh CA, Assimamaw NT, Tamir TT, et al. COVID-19 vaccine acceptance rate and its predictors in Ethiopia: a systematic review and meta-analysis. Hum Vaccines Immunother. (2022) 18:2114699. doi: 10.1080/21645515.2022.2114699
37. Bhattacharya O, Siddiquea BN, Shetty A, Afroz A, Billah B. COVID-19 vaccine hesitancy among pregnant women: a systematic review and meta-analysis. BMJ Open. (2022) 12:e061477. doi: 10.1136/bmjopen-2022-061477
38. Biswas MdR, Alzubaidi MS, Shah U, Abd-Alrazaq AA, Shah Z. A scoping review to find out worldwide COVID-19 vaccine hesitancy and its underlying determinants. Vaccines. (2021) 9:1243. doi: 10.3390/vaccines9111243
39. Chen F, He Y, Shi Y. Parents' and guardians' willingness to vaccinate their children against COVID-19: a systematic review and meta-analysis. Vaccines. (2022) 10:179. doi: 10.3390/vaccines10020179
40. Desye B. Prevalence and determinants of COVID-19 vaccine acceptance among healthcare workers: a systematic review. Front Public Health. (2022) 10:941206. doi: 10.3389/fpubh.2022.941206
41. Galanis P, Vraka I, Fragkou D, Bilali A, Kaitelidou D. Intention of healthcare workers to accept COVID-19 vaccination and related factors: A systematic review and meta-analysis. Asian Pac J Trop Med. (2021) 14:543. doi: 10.4103/1995-7645.332808
42. Galanis P, Vraka I, Katsiroumpa A, Siskou O, Konstantakopoulou O, Katsoulas T, et al. First COVID-19 booster dose in the general population: a systematic review and meta-analysis of willingness and its predictors. Vaccines. (2022) 10:1097. doi: 10.3390/vaccines10071097
43. Galanis P, Vraka I, Siskou O, Konstantakopoulou O, Katsiroumpa A, Kaitelidou D. Willingness, refusal and influential factors of parents to vaccinate their children against the COVID-19: a systematic review and meta-analysis. Prev Med. (2022) 157:106994. doi: 10.1016/j.ypmed.2022.106994
44. Geng H, Cao K, Zhang J, Wu K, Wang G, Liu C. Attitudes of COVID-19 vaccination among college students: a systematic review and meta-analysis of willingness, associated determinants, and reasons for hesitancy. Hum Vaccines Immunother. (2022) 18:2054260. doi: 10.1080/21645515.2022.2054260
45. Halemani K, Dhiraaj S, Latha T, Mishra P, Issac A. The prevalence of COVID vaccine acceptance among pregnant women: a systematic review and meta-analysis. Clin Epidemiol Glob Health. (2022) 17:101144. doi: 10.1016/j.cegh.2022.101144
46. Hajure M, Tariku M, Bekele F, Abdu Z, Dule A, Mohammedhussein M, et al. Attitude towards COVID-19 vaccination among healthcare workers: a systematic review. Infect Drug Resist. (2021) 14:3883–97. doi: 10.2147/IDR.S332792
47. Januszek SM, Faryniak-Zuzak A, Barnaś E, Łoziński T, Góra T, Siwiec N, et al. The approach of pregnant women to vaccination based on a COVID-19 systematic review. Medicina. (2021) 57:977. doi: 10.3390/medicina57090977
48. Joshi A, Kaur M, Kaur R, Grover A, Nash D, El-Mohandes A. Predictors of COVID-19 vaccine acceptance, intention, and hesitancy: a scoping review. Front Public Health. (2021) 9:698111. doi: 10.3389/fpubh.2021.698111
49. Kamal A, Hodson A, Pearce JM. A rapid systematic review of factors influencing COVID-19 vaccination uptake in minority ethnic groups in the UK. Vaccines. (2021) 9:1121. doi: 10.3390/vaccines9101121
50. Kazeminia M, Afshar ZM, Rajati M, Saeedi A, Rajati F. Evaluation of the acceptance rate of Covid-19 vaccine and its associated factors: a systematic review and meta-analysis. J Prev. (2022) 43:421–67. doi: 10.1007/s10935-022-00684-1
51. Kukreti S, Rifai A, Lin C-Y, Ko W-C, Chen P-L, Strong C, et al. Willingness to obtain COVID-19 vaccination in general population: a systematic review and meta-analysis. J Glob Health. (2022) 12:50. doi: 10.7189/jogh.12.05006
52. Li M, Luo Y, Watson R, Zheng Y, Ren J, Tang J, Chen Y. Healthcare workers' (HCWs) attitudes and related factors towards COVID-19 vaccination: a rapid systematic review. Postgrad Med J. (2021) postgradmedj-2021-140195. doi: 10.1136/postgradmedj-2021-140195
53. Lin C, Tu P, Beitsch LM. Confidence and receptivity for COVID-19 vaccines: a rapid systematic review. Vaccines. (2020) 9:16. doi: 10.3390/vaccines9010016
54. Lin GSS, Lee HY, Leong JZ, Sulaiman MM, Loo WF, Tan WW. COVID-19 vaccination acceptance among dental students and dental practitioners: a systematic review and meta-analysis. PLoS ONE. (2022) 17:e0267354. doi: 10.1371/journal.pone.0267354
55. Luo C, Yang Y, Liu Y, Zheng D, Shao L, Jin J, et al. Intention to COVID-19 vaccination and associated factors among health care workers: a systematic review and meta-analysis of cross-sectional studies. Am J Infect Control. (2021) 49:1295–304. doi: 10.1016/j.ajic.2021.06.020
56. Mahmud S, Mohsin M, Hossain S, Islam MM, Muyeed A. The acceptance of COVID-19 vaccine at early stage of development and approval: a global systematic review and meta-analysis. Heliyon. (2022) 8:e10728. doi: 10.1016/j.heliyon.2022.e10728
57. Mose A, Wasie A, Shitu S, Haile K, Timerga A, Melis T, et al. Determinants of COVID-19 vaccine acceptance in Ethiopia: a systematic review and meta-analysis. PLoS One. (2022) 17:e0269273. doi: 10.1371/journal.pone.0269273
58. Nehal KR, Steendam LM, Campos Ponce M, van der Hoeven M, Smit GSA. Worldwide vaccination willingness for COVID-19: a systematic review and meta-analysis. Vaccines. (2021) 9:1071. doi: 10.3390/vaccines9101071
59. Nindrea RD, Usman E, Katar Y, Sari NP. Acceptance of COVID-19 vaccination and correlated variables among global populations: a systematic review and meta-analysis. Clin Epidemiol Glob Health. (2021) 12:100899. doi: 10.1016/j.cegh.2021.100899
60. Norhayati MN, Che Yusof R, Azman YM. Systematic review and meta-analysis of COVID-19 vaccination acceptance. Front Med. (2022) 8:783982. doi: 10.3389/fmed.2021.783982
61. Olu-Abiodun O, Abiodun O, Okafor N. COVID-19 vaccination in Nigeria: a rapid review of vaccine acceptance rate and the associated factors. PLoS ONE. (2022) 17:e0267691. doi: 10.1371/journal.pone.0267691
62. Parthasarathi A, Puvvada RK, Basappa S, Krishna MT, Mahesh PA. Global intention of the general public to undergo COVID-19 vaccination: time trends and risk factors for vaccine refusal, a systematic review and meta-analysis. Wellcome Open Res. (2022) 7:17. doi: 10.12688/wellcomeopenres.17517.1
63. Patwary MM, Alam MA, Bardhan M, Disha AS, Haque MdZ, Billah SM, et al. COVID-19 vaccine acceptance among low- and lower-middle-income countries: a rapid systematic review and meta-analysis. Vaccines. (2022) 10:427. doi: 10.3390/vaccines10030427
64. Popa AD, Enache AI, Popa IV, Antoniu SA, Dragomir RA, Burlacu A. Determinants of the hesitancy toward COVID-19 vaccination in Eastern European countries and the relationship with health and vaccine literacy: a literature review. Vaccines. (2022) 10:672. doi: 10.3390/vaccines10050672
65. Prabani KIP, Weerasekara I, Damayanthi HDWT. COVID-19 vaccine acceptance and hesitancy among patients with cancer: a systematic review and meta-analysis. Public Health. (2022) 212:66–75. doi: 10.1016/j.puhe.2022.09.001
66. Ripp T, Röer JP. Systematic review on the association of COVID-19-related conspiracy belief with infection-preventive behavior and vaccination willingness. BMC Psychol. (2022) 10:66. doi: 10.1186/s40359-022-00771-2
67. Robinson E, Jones A, Lesser I, Daly M. International estimates of intended uptake and refusal of COVID-19 vaccines: a rapid systematic review and meta-analysis of large nationally representative samples. Vaccine. (2021) 39:2024–34. doi: 10.1016/j.vaccine.2021.02.005
68. Roy DN, Biswas M, Islam E, Azam MdS. Potential factors influencing COVID-19 vaccine acceptance and hesitancy: a systematic review. PLoS ONE. (2022) 17:e0265496. doi: 10.1371/journal.pone.0265496
69. Sahile AT, Gizaw GD, Mgutshini T, Gebremariam ZM, Bekele GE. COVID-19 vaccine acceptance level in Ethiopia: a systematic review and meta-analysis. Can J Infect Dis Med Microbiol. (2022) 2022:1–7. doi: 10.1155/2022/2313367
70. Shakeel CS, Mujeeb AA, Mirza MS, Chaudhry B, Khan SJ. Global COVID-19 vaccine acceptance: a systematic review of associated social and behavioral factors. Vaccines. (2022) 10:110. doi: 10.3390/vaccines10010110
71. Shamshirsaz AA, Hessami K, Morain S, Afshar Y, Nassr AA, Arian SE, et al. Intention to receive COVID-19 vaccine during pregnancy: a systematic review and meta-analysis. Am J Perinatol. (2022) 39:492–500. doi: 10.1055/a-1674-6120
72. Shui X, Wang F, Li L, Liang Q. COVID-19 vaccine acceptance among healthcare workers in China: a systematic review and meta-analysis. PLoS ONE. (2022) 17:e0273112. doi: 10.1371/journal.pone.0273112
73. Terry E, Cartledge S, Damery S, Greenfield S. Factors associated with COVID-19 vaccine intentions during the COVID-19 pandemic; a systematic review and meta-analysis of cross-sectional studies. BMC Public Health. (2022) 22:1667. doi: 10.1186/s12889-022-14029-4
74. Wake AD. The willingness to receive COVID-19 vaccine and its associated factors: “Vaccination Refusal Could Prolong the War of This Pandemic” – a systematic review. Risk Manag Healthc Policy. (2021) 14:2609–23. doi: 10.2147/RMHP.S311074
75. Wang Q, Yang L, Jin H, Lin L. Vaccination against COVID-19: a systematic review and meta-analysis of acceptability and its predictors. Prev Med. (2021) 150:106694. doi: 10.1016/j.ypmed.2021.106694
76. Wang Q, Hu S, Du F, Zang S, Xing Y, Qu Z, et al. Mapping global acceptance and uptake of COVID-19 vaccination: a systematic review and meta-analysis. Commun Med. (2022) 2:113. doi: 10.1038/s43856-022-00177-6
77. Willems LD, Dyzel V, Sterkenburg PS. COVID-19 Vaccination intentions amongst healthcare workers: a scoping review. Int J Environ Res Public Health. (2022) 19:10192. doi: 10.3390/ijerph191610192
78. Zintel S, Flock C, Arbogast AL, Forster A, von Wagner C, Sieverding M. Gender differences in the intention to get vaccinated against COVID-19: a systematic review and meta-analysis. J Public Health. (2022). doi: 10.1007/s10389-021-01677-w
79. Guidry JPD, Laestadius LI, Vraga EK, Miller CA, Perrin PB, Burton CW, et al. Willingness to get the COVID-19 vaccine with and without emergency use authorization. Am J Infect Control. (2021) 49:137–42. doi: 10.1016/j.ajic.2020.11.018
80. Kalu ME, Oyinlola O, Ibekaku MC, Adandom II, Iwuagwu AO, Ezulike CJ, et al. Mapping review on the uptake of the COVID-19 vaccine among adults in Africa using the 5As vaccine taxonomy. Am J Trop Med Hyg. (2022) 106:1688–97. doi: 10.4269/ajtmh.21-0515
81. Idris IO, Ayeni GO, Adebisi YA. Why many African countries may not achieve the 2022 COVID-19 vaccination coverage target. Trop Med Health. (2022) 50:15. doi: 10.1186/s41182-022-00407-6
82. Centers for Disease Control and Prevention (CDC). COVID Data Tracker. US Department of Health and Human Services: Atlanta, GA, USA, 2022. Available online at: https://covid.cdc.gov/covid-data-tracker (accessed February 10, 2022).
83. Alam Md M, Melhim LKB, Ahmad MT, Jemmali M. Public attitude towards COVID-19 vaccination: validation of COVID-vaccination attitude scale (C-VAS). J Multidiscip Healthc. (2022) 15:941–54. doi: 10.2147/JMDH.S353594
84. Hostler TJ, Wood C, Armitage CJ. The influence of emotional cues on prospective memory: a systematic review with meta-analyses. Cogn Emot. (2018) 32:1578–96. doi: 10.1080/02699931.2017.1423280
Keywords: COVID-19, vaccination intention, meta-review, systematic review of systematic reviews, COVID-19 vaccine
Citation: Limbu YB and Gautam RK (2023) The determinants of COVID-19 vaccination intention: a meta-review. Front. Public Health 11:1162861. doi: 10.3389/fpubh.2023.1162861
Received: 10 February 2023; Accepted: 23 May 2023;
Published: 12 June 2023.
Edited by:
Francesco Paolo Bianchi, University of Bari Aldo Moro, ItalyReviewed by:
Srikanth Umakanthan, The University of the West Indies St. Augustine, Trinidad and TobagoSusanta Kumar Ghosh, National Institute of Malaria Research (ICMR), India
Copyright © 2023 Limbu and Gautam. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yam B. Limbu, bGltYnV5QG1vbnRjbGFpci5lZHU=
 Yam B. Limbu
Yam B. Limbu Rajesh K. Gautam
Rajesh K. Gautam