- 1Department of Microbiology, School of Life Sciences, JSS Academy of Higher Education and Research, Mysuru, Karnataka, India
- 2Department of Microbiology, JSS Medical College and Hospital, JSS Academy of Higher Education and Research, Mysuru, Karnataka, India
Introduction: Candida is one of the rising primary causes of infections connected with health care. However, their distribution and susceptibility patterns vary widely amongst different regions.
Method: The study was carried out to retrospectively analyze the distribution of Candida in various clinical samples, their species types and susceptibility, in a tertiary care hospital, in India for 4 years using the Vitek-2 database.
Results: Candida infection was identified in 751 clinical samples, and the major source of infection was found to be urine samples accounting for about 58.32%. A total of 18 different Candida species were recorded. Non-albicans Candida (NAC) 73.64% (n = 553) predominated Candida albicans 26.36% (n = 198). Candida tropicalis was found to be identified at a higher frequency followed by C. albicans, Candida glabrata and Candida parapsilosis. Candida tropicalis was the only species which were recovered from bile; Candida pelliculosa was recorded merely from blood and Candida lipolytica from urine and blood and not in any other samples. In vaginal swabs, C. albicans accounted for 63.64% (n = 14) compared to NAC 36.36% (n = 8). The susceptibility test revealed that 75.44% (n = 559) isolates were susceptible and 24.56% (n = 182) were resistant to one or more drugs tested. Major resistance was exhibited to flucytosine by C. tropicalis 77.46% (n = 55) compared to C. albicans 11.27% (n = 8). Apart from C. albicans, NAC-C. tropicalis, C. glabrata and Candida krusei showed resistance to echinocandins, and Candida haemulonii to amphotericin-B.
Conclusion: The knowledge of the incidence, resistance and emergence of different species might guide clinicians to select an appropriate antifungal therapy and plan effective strategies to control invasive and systemic Candida infections.
1. Introduction
Candida has been documented as the most common fungi associated with nosocomial infections due to their invasive interventions and indwelling nature in prosthetic devices (1). Also, they are the most common opportunistic infections in patients with immunocompromised conditions and those with impaired physiological and cellular barriers (2). Their dimorphic nature, adherence to host tissues/medical devices, invasive character, biofilm formation and secretion of extracellular hydrolytic enzymes have swapped the commensal character to pathogenic. Additionally, the factors such as profuse usage of wide-spectrum antibiotics, and corticosteroids, expanded use of antifungal drugs, and geographical difference in the epidemiology have increased their occurrence rate, distribution, and diversity frequency (3–8).
Among Candida species, Candida albicans is recorded as the most prevalent species, but its prevalence varies considerably depending on geographical regions; and a shift to non-albicans Candida (NAC) has been observed globally (9, 10). NAC have emerged as clinically interested pathogens and are exhibiting a high degree of resistance to the azole group of antifungals compared to C. albicans (11–13).
The rise of superbug Candida infections auris with increased morbidity and mortality in different parts of the continent is challenging the diagnosis methods and treatments (14). Candida is known to cause infections in cutaneous, mucosal, and deep-seated organs. Various species have been isolated from multiple clinical sites. The increased incidence of candidiasis, the surge of NAC, and the change in susceptibility patterns have emphasized the need to monitor laboratory data and select the appropriate antifungal for therapy (14–17). The knowledge of epidemiological surveillance on species distribution and their emerging resistance to antifungal agents can be the guide for effective management and antifungal stewardship.
The study aimed to retrospectively analyse the data on Candida species diversity, their distribution in different clinical samples and susceptibility profile in a tertiary care hospital, in Karnataka, India. Though individual institution data does not represent the total population, surveillance on species distribution and antifungal susceptibility test (AST) of a particular geographical area improve clinical decisions.
2. Materials and methods
A retrospective analysis was carried out to understand the distribution of Candida species in different clinical samples and their drug susceptibility pattern from the Department of Microbiology database of an 1800-bed tertiary care hospital in Mysuru, Karnataka, India, for 4 years. The database included patient identifiers, hospital wards/outpatient services/departments, sample collection date, specimen type, body site of isolation and results of speciation and AST pattern.
The samples were processed as per the standard microbiological procedures. The isolates were identified to the species level, and AST patterns were determined using the Vitek 2 system (BioMerieux, France). The AST panel included the antifungals such as amphotericin B, 5 flucytosine, caspofungin, micafungin, fluconazole, and voriconazole. The susceptibility results were concordant with CLSI and EUCAST Methodologies and were interpreted as sensitive (S), intermediate (I) and resistant (R) (18, 19).
The clinical samples received by the laboratory for routine analysis were processed as per the standard protocols. Therefore, the study did not require oversight by the institutional ethics committee because of its descriptive nature.
2.1. Statistical analysis
Descriptive analysis was carried out to analyse the distribution of C. albicans and NAC, in different clinical samples and susceptibility to antifungal drugs year-wise. The Mann–Whitney U-test and Pearson’s Chi-square Test were used to compare the differences and find the association between variables. The Mann–Whitney U-test with a 5% significance level and Pearson’s Chi-square Test with a p-value <0.05 was significant. Statistical analysis was performed using SPSS 20.0 program.
3. Results
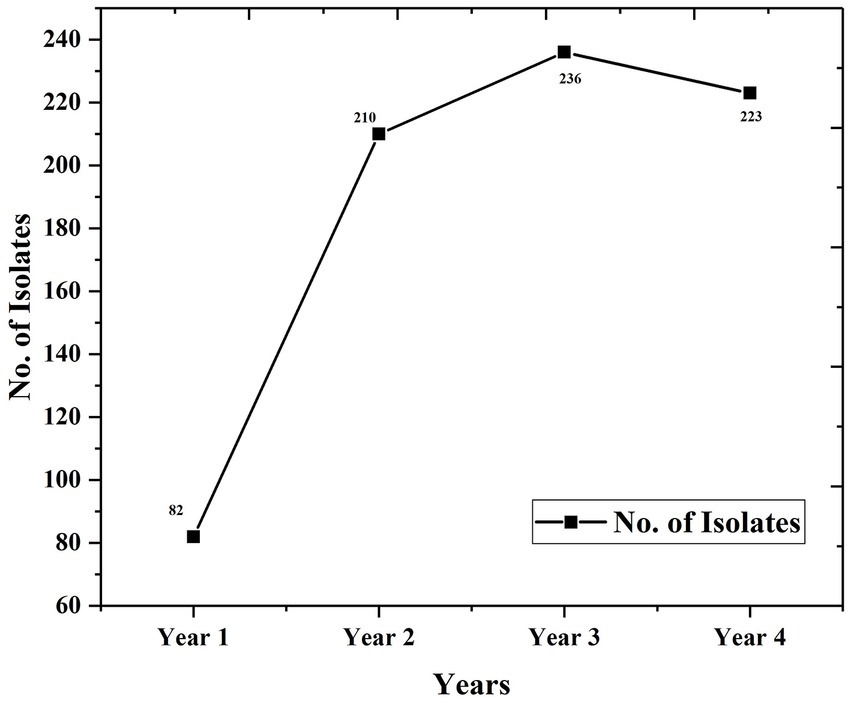
Analysis of the database revealed that 751 Candida isolates were recovered from different clinical samples over 4 years. The occurrence level had increased successively over the years except for last year (Figure 1).
The clinical samples processed include sputum, endotracheal (ET) secretions, tracheal aspirates, broncho-alveolar lavages (BAL), urine, stool, vaginal swabs (VS), cerebrospinal spinal fluid (CSF), pleural fluid (PF), ascitic fluid (AF), blood, bile, ear, nail, pus from post-surgical wounds, and catheter tips.
3.1. Candida species isolated from clinical samples
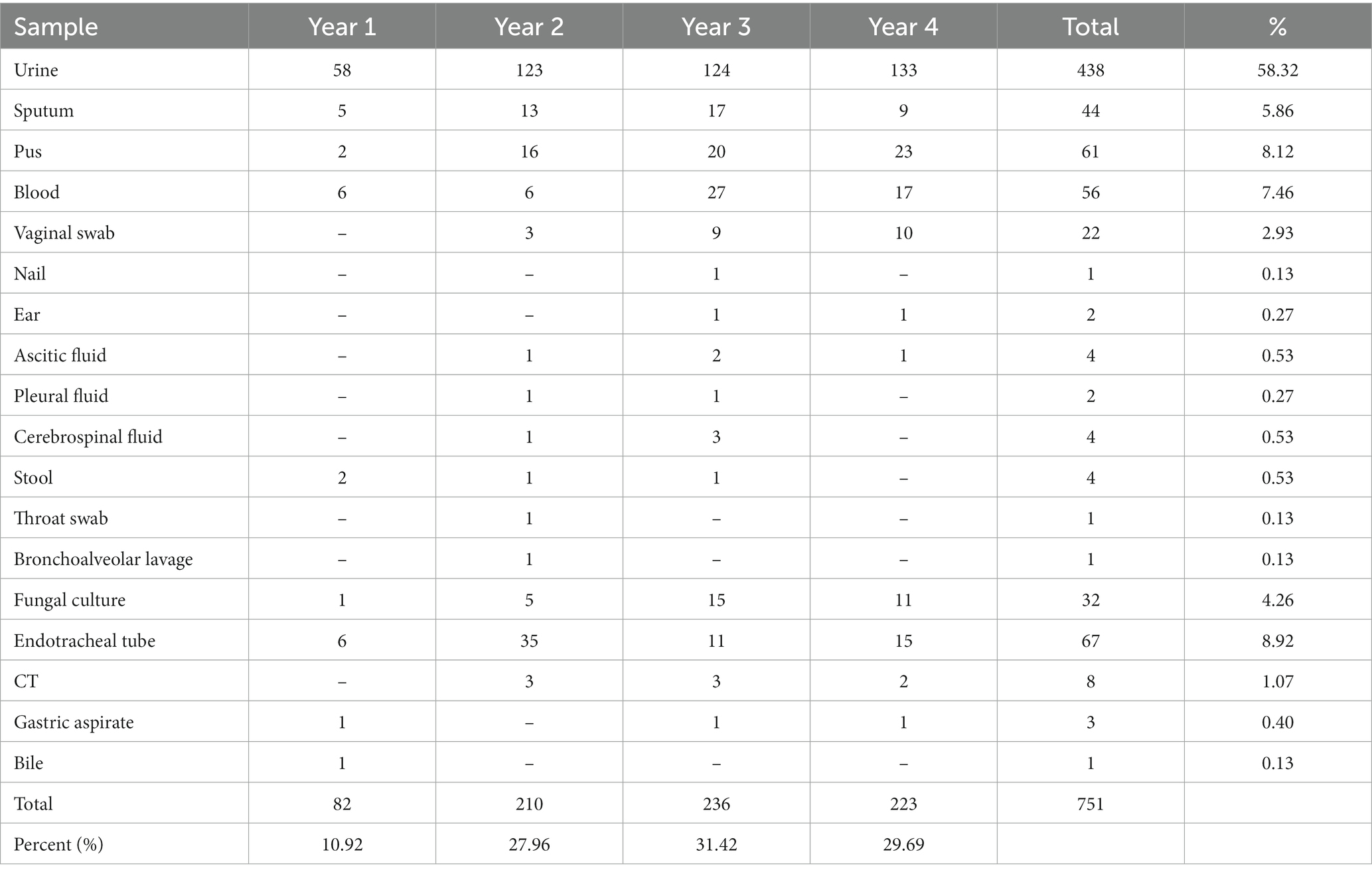
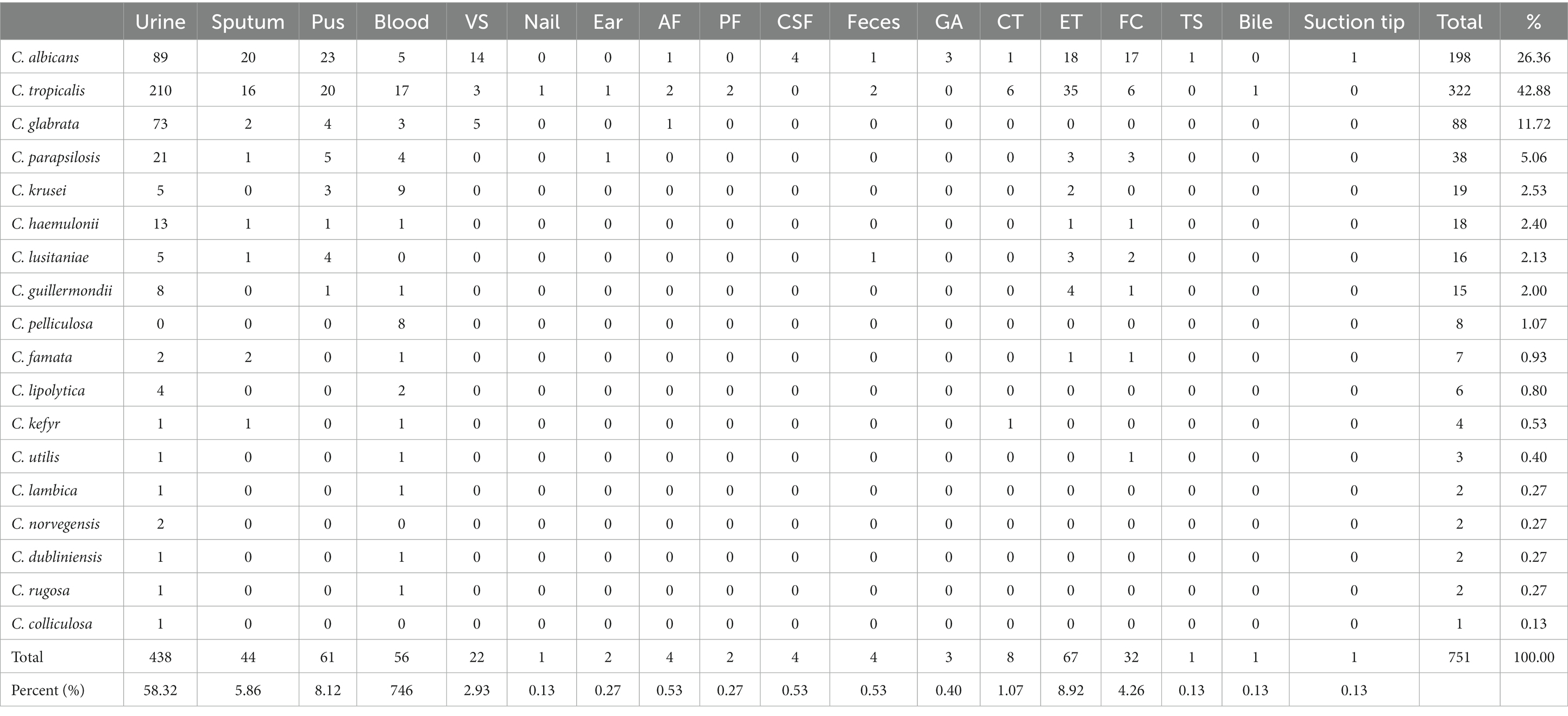
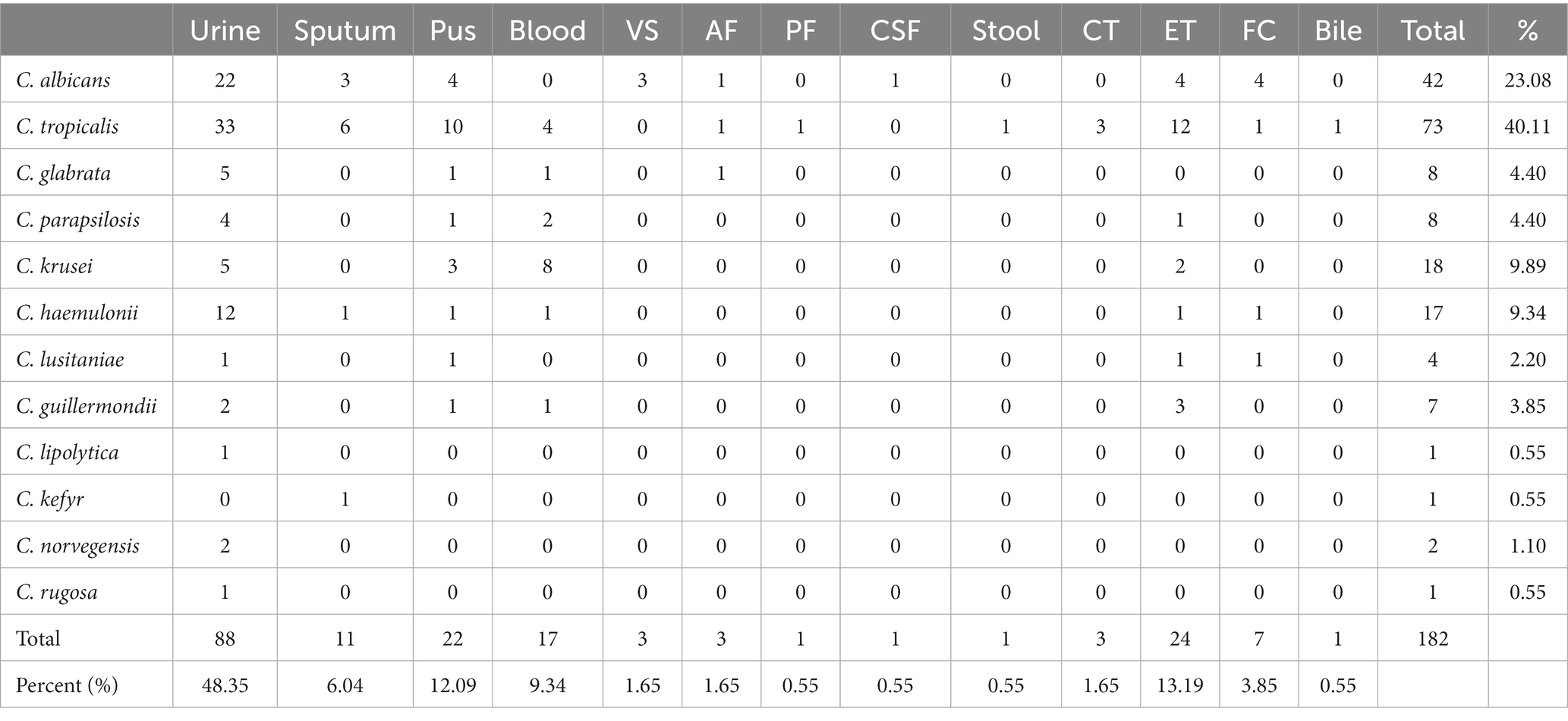
Table 1 represents the source of the samples from which Candida was isolated during the study period. Of all the samples, urine alone contributed 58.42%, followed by ET (8.92%), pus (8.12%), blood (7.46%), sputum (5.86%), and other samples were < 3%. Table 2 details the distribution of Candida species in different clinical samples. It was observed that over the years, there was an increase in the incidence and emergence of different NAC species (Figure 2). A total of 18 different types of Candida species were isolated from 751 isolates. NAC (n = 553, 73.64%) predominated over C. albicans (n = 198, 26.36%).
The distribution frequency of C. albicans over NAC by the Manne Whitney U-test revealed that NAC had the highest mean and sum rank compared to C. albicans. The test showed an asymptotic significance (2-tailed) value of p and concluded that NAC was statistically significantly higher than the C. albicans (p = 0.021 at a 5% significance level).
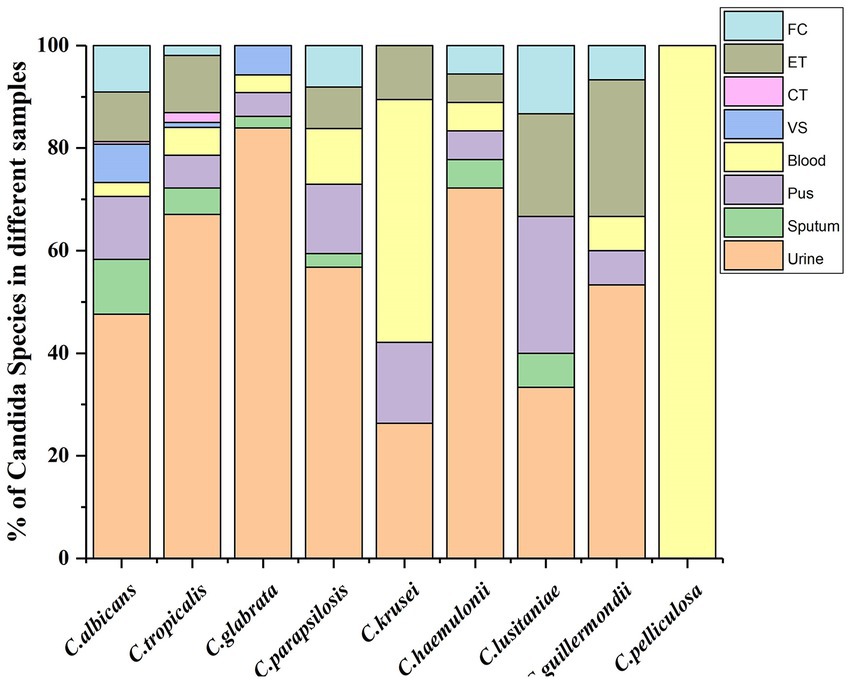
Among NAC, Candida tropicalis was the most frequently isolated (n = 322, 42.88%) species followed by Candida glabrata (n = 88, 11.72%), Candida parapsilosis (n = 38, 5.06%), Candida krusei (n = 19, 2.53%), Candida haemulonii (n = 18, 2.4%), Candida lusitaniae (n = 16, 2.13%), Candida guillermondii (n = 15, 2.0%). Figure 3 graphically represents the Candida species which were recovered at a higher rate (>1%) from different clinical specimens.
Out of 58.32% of Urine samples, C. tropicalis accounted to be 210 (46.2%), followed by C. albicans 89 (19.58%), C. glabrata 73 (16.06%), and C. parapsilosis 21 (4.62%). Except for Candida pelliculosa, all 17 Candida were recovered from urine samples. Candida tropicalis was isolated from all specimens except CSF, TS, and GA. It was the only species recovered from bile. Apart from C. lusitaniae, Candida norvegensis, and Candida colliculosa, all other species resulted in candidemia. Candida krusei and C. pelliculosa were frequently isolated from blood in concurrence with C. albicans and C. tropicalis; C. lipolytica was recovered only from urine and blood, whereas C. pelliculosa only from blood. Among 22 vaginal swabs processed, C. albicans accounted for 14 (63.64%), followed by C. glabarata 5 (22.7%) and C. tropicalis 3 (13.6%).
3.2. Antifungal susceptibility pattern
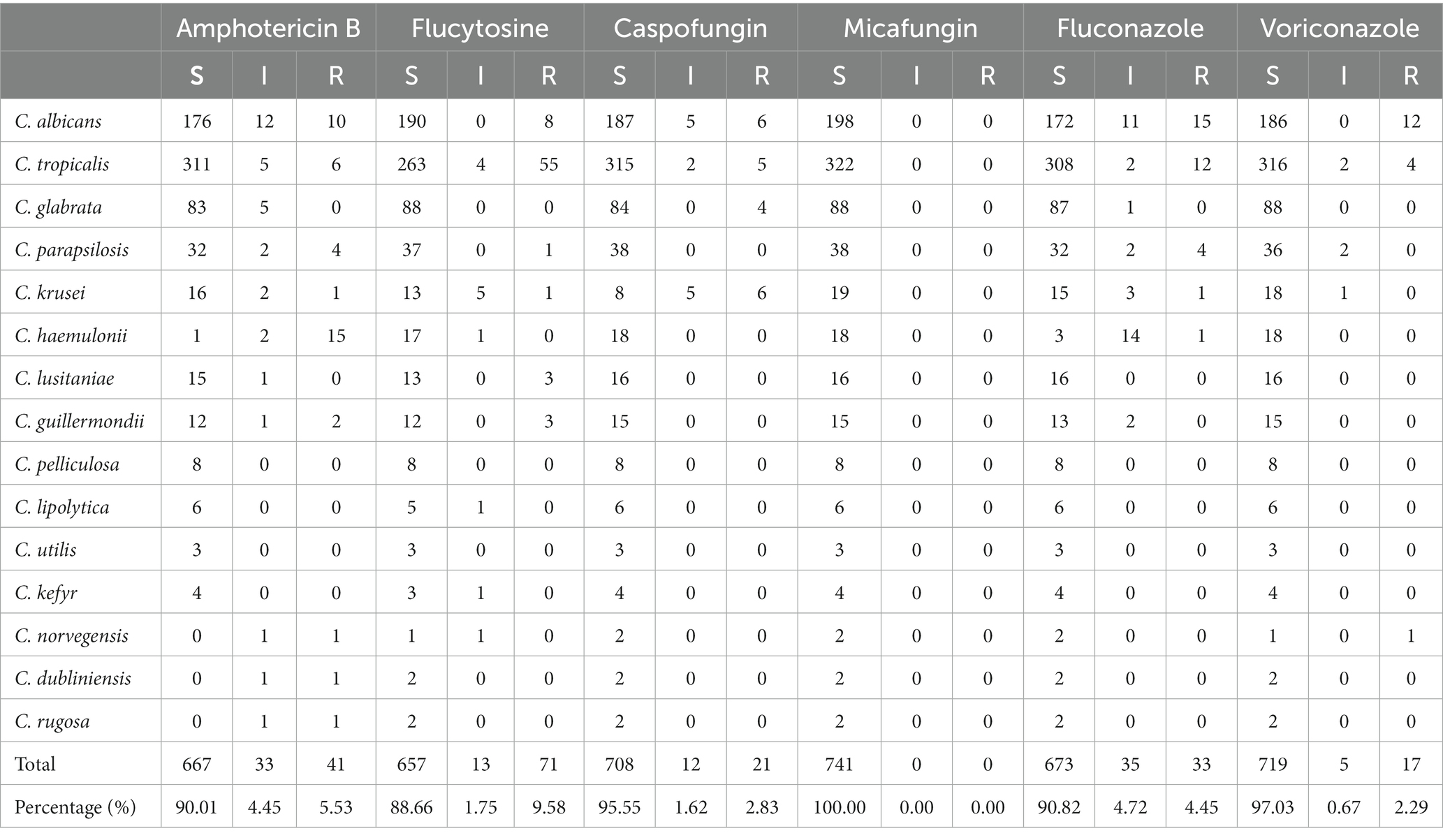
Drug susceptibility was carried out for all 751 isolates, but the susceptibility profile was available only for 741 isolates in VITEK with no interpretation for Candida famata (7), Candida lambica (2) and C. colliculosa (1). Among the 741 isolates, 182 (24.56%) showed resistance to one or more drugs tested, and 559 (75.44%) were susceptible to all drugs—Table 3. Both albicans and NAC showed increased resistance to drugs successively. Out of 198\u00B0 C. albicans, 156 (78.79%) were sensitive to all antifungals tested, and 42 (21.21%) were resistant to at least one drug—Figures 4, 5. Amongst 553 NAC, 403 (72.88%) were sensitive to all antifungals, and 140 (25.32%) showed resistance to at least one drug. The maximum number of resistant Candida species were isolated from urine samples 88/438, followed by ET 24/67, pus 22/61, blood 17/56, and sputum 11/44—Tables 3, 4.
Of the 182 resistant isolates, 140 (76.92%) NAC and 42 (23.08%) C. albicans showed resistance to at least one drug. Among NAC, three species that commonly exhibited resistance were C. tropicalis 73 (40.11%), C. krusei 18 (9.89%) and C. haemulonii 17 (9.34%). The Mann–Whitney U-test revealed a significant difference (p = 0.028 at 5% significance) in the resistance profile of albicans over NAC.
In vitro susceptibility pattern of Candida species to six antifungals—amphotericin B, caspofungin, flucytosine, fluconazole, micafungin, and voriconazole has been tabulated in Table 4. For echinocandins such as micafungin-all 741 isolates were susceptible. For caspofungin—maximum resistance was observed by C. krusei 6 (31.57%), followed by C. glabrata 4 (4.55%), C. albicans 6 (3.03%) and C. tropicalis 5 (1.55%). For azoles such as voriconazole—12 (6.06%) C. albicans and 4 (1.24%) C. tropicalis exhibited resistance; for fluconazole—15 (7.58%) C. albicans, 12 (3.73%) C. tropicalis, 4 (10.52%) C. parapsilosis, 1 (5.56%) C. haemulonii and 1 (5.2%) C. krusei showed resistance. Maximum resistance to flucytosine was observed by C. tropicalis 55 (20.91%), C. albicans 8 (4.21%), C. lusitaniae 3 (23.08%) and C. guillermondii 3 (25%). Of all the antifungals tested, Candida species were susceptible to micafungin and resistant to flucytosine. Sensitivity to other drugs was in the following order:—voriconazole, caspofungin, fluconazole, and amphotericin B. About 15 (83.3%) of C. haemulonii were resistant to amphotericin B. C. pelliculosa, C. utilis, and C. dubliniensis were found sensitive to all drugs.
On comparison of albicans and NAC resistance to all six drugs by the Pearson chi-square test, the value of p appeared to be less than 0.05(p = 0 < 0.001). Thus, there lies a statistical significance between the organism and the drugs. The drugs and organism association revealed a significant difference at a 5% level (value of p 0 < 0.001).
4. Discussion
Nosocomial invasive fungal infections are increasing at a higher frequency (20). The present study infers that NAC predominates C. albicans. C. tropicalis being the most common species reported, revealed a significant epidemiological shift compared to our previous study from 2010 to 2014 (16). The increased ratio of NAC over C. albicans reflected the rise in the incidence of NAC, but the reason for this switchover is unknown. Overall, candiduria was recorded in 58.32%, whereas candidemia was observed in 7.46%. Esmailzadeh et al. (21) and Zakhem et al. (22) reported an increased frequency of NAC compared to C. albicans in candiduria and candidemia conditions. Kato et al. (23) and Shenoy et al. (24) reported the prevalence of both albicans and NAC in bile. Among NAC, C. glabrata was recorded in both of their studies individually. Studies from Marak (25) and Ballal et al. (26) revealed the presence of only NAC in bile which is in line with our study. In a study by Baghdadi et al. 2016, C. albicans was the most common species isolated from endotracheal tubes accounting for 35.7%. Among NAC, C. glabrata, C. parapsilosis, C. tropicalis, and C. krusei were recorded (27). A retrospective analysis of epidemiology for candidemia has reported that central venous catheters and endotracheal intubation as the most common risk factors associated with mortality and highlights the significance of considering the possibility of invasive Candida infection in patients (28). From vaginal swabs C. albicans 63.64% was the predominant species isolated followed by C. glabrata and C. tropicalis. Studies have shown that elevated levels of estrogen have a direct impact on growth of Candida and its adherence to vaginal epithelium suggests an increased incidence of vaginal candidiasis in women. Studying hormone-sensing pathways help in explaining gender bias-associated infections. C. albicans is recorded as the predominant colonizer in the female reproductive tract and a major cause of genital thrush (29). The shift in the frequency from albicans to NAC such as C. glabrata, C. parapsilosis, C. tropicalis may be due to increased use of the counter drugs, a short-course of antifungal therapy, and long-term use of azoles (30). NAC has not only overtaken the albicans in uncontrolled distribution but has also evolved in exhibiting drug resistance to azole, polyene and echinocandins drugs which are alarming the situation. Data insights show that C. tropicalis parallels C. albicans in demonstrating resistance to azole and flucytosine drugs. Increased flucytosine resistance indicates indiscriminate usage of the drug. Apart from C. albicans, NAC such as C. tropicalis, C. glabrata, and C. krusei have evolved in exhibiting resistance toward echinocandins. C. haemulonii has demonstrated resistance to amphotericin B, which is the mainstay of systemic antifungal therapy (31). For micafungin, all isolates were found to be sensitive.
The limitations of the present study are no other tests were carried out for species confirmation. Also, the data was from a single institution and cannot be extrapolated to other hospitals.
In summary, it is a study which statistically infers the body sites affected by different species of Candida and their antifungal resistance patterns. Each species varies in susceptibility level to the distinct group of antifungal agents. The emergence of new species, indiscriminate usage of drugs and rising drug resistance have worsened the situation. Therefore, continuous surveillance, epidemiology, and clinical investigation studies performed locally from each hospital can provide a database to monitor Candidemia infections. The antibiogram profile could guide clinicians to choose appropriate drugs for the emerging Candida species and plan effective strategies to control invasive and systemic Candida infections.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
This is an observational study. JSS Academy of Higher Education & Research Ethics Committee has confirmed that no ethical approval is required.
Author contributions
US and MS contributed to the study’s conception and design. Material preparation, data collection and analysis were performed by US and MS. The first draft of the manuscript was written by US. All authors contributed to the article and approved the submitted version.
Acknowledgments
The authors acknowledge the support and infrastructure offered by the JSS Academy of Higher Education and Research (JSSAHER), Mysuru, India.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Sikora, A, and Zahra, F. Nosocomial Infections. [Updated 2023 Jan 23]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available at: https://www.ncbi.nlm.nih.gov/books/NBK559312/
2. Badiee, P, and Hashemizadeh, Z. Opportunistic invasive fungal infections: diagnosis & clinical management. Indian J Med Res. (2014) 139:195–204.
3. Viudes, A, Pemán, J, Cantón, E, Úbeda, P, López-Ribot, J, and Gobernado, M. Candidemia at a tertiary-care hospital: epidemiology, treatment, clinical outcome and risk factors for death. Eur J Clin Microbiol Infect Dis. (2002) 21:767–74. doi: 10.1007/s10096-002-0822-1
4. Pfaller, MA, and Diekema, DJ. Epidemiology of invasive candidiasis: a persistent public health problem. Clin Microbiol Rev. (2007) 20:133–63. doi: 10.1128/CMR.00029-06
5. Mohandas, V, and Ballal, M. Distribution of Candida species in different clinical samples and their virulence: biofilm formation, proteinase and phospholipase production: a study on hospitalized patients in southern India. J Global Infect Dis. (2011) 3:4–8. doi: 10.4103/0974-777X.77288
6. Sardi, JCO, Scorzoni, L, Bernardi, T, Fusco-Almeida, AM, and Mendes Giannini, MJS. Candida species: current epidemiology, pathogenicity, biofilm formation, natural antifungal products and new therapeutic options. J Med Microbiol. (2013) 62:10–24. doi: 10.1099/jmm.0.045054-0
7. Abi-Said, D, Anaissie, E, Uzun, O, Raad, I, Pinzcowski, H, and Vartivarian, S. The epidemiology of hematogenous candidiasis caused by different Candida species. Clin Infect Dis. (1997) 24:1122–8. doi: 10.1086/513663
8. Pappas, PG, Lionakis, MS, Arendrup, MC, and Ostrosky-Zeichner, L. Kullberg BJ (2018) invasive candidiasis. Nat Rev Dis Primers. (2018) 4:18026. doi: 10.1038/nrdp.2018.26
9. Guo, LN, Yu, SY, Xiao, M, Yang, CX, Bao, CM, Yu, YH, et al. Species distribution and antifungal susceptibility of invasive candidiasis: a 2016-2017 multicenter surveillance study in Beijing. China Infect Drug Resist. (2020) 13:2443–52. doi: 10.2147/IDR.S255843
10. Guo, F, Yang, Y, Kang, Y, Zang, B, Cui, W, Qin, B, et al. Invasive candidiasis in intensive care units in China: a multicentre prospective observational study. J Antimicrob Chemother. (2013) 68:1660–8. doi: 10.1093/jac/dkt083
11. Samra, Z, Bishara, J, Ashkenazi, S, Pitlik, S, Weinberger, M, Lapidoth, M, et al. Changing distribution of Candida species isolated from sterile and nonsterile sites in Israel. Eur J Clin Microbiol Infect Dis. (2002) 21:542–5. doi: 10.1007/s10096-002-0764-7
12. Sanglard, D, and Odds, FC. Resistance of Candida species to antifungal agents: molecular mechanisms and clinical consequences. Lancet Infect Dis. (2002) 2:73–85. doi: 10.1016/s1473-3099(02)00181-0
13. Cortegiani, A, Misseri, G, Fasciana, T, Giammanco, A, Giarratano, A, and Chowdhary, A. Epidemiology, clinical characteristics, resistance, and treatment of infections by Candida auris. J Intensive Care. (2018) 6:69. doi: 10.1186/s40560-018-0342-4
14. Eggimann, P, Garbino, J, and Pittet, D. 2003. Epidemiology of Candida species infections in critically ill non-immunosuppressed patients. Lancet Infect Dis. (2003) 3:685–702. doi: 10.1016/s1473-3099(03)00801-6
15. Sanguinetti, M, Porta, R, Sali, M, La Sorda, M, Pecorini, G, Fadda, G, et al. Evaluation of VITEK 2 and RapID yeast plus systems for yeast species identification: experience at a large clinical microbiology laboratory. J Clin Microbiol. (2007) 45:1343–6. doi: 10.1128/JCM.02469-06
16. Shivaswamy, U, and Neelambike, SM. A study of candidiasis in HIV reactive patients in a tertiary care hospital, Mysore—South India. Indian J Dermatol Venereol Leprol. (2014) 80:278. doi: 10.4103/0378-6323.132271
17. Deorukhkar, SC, Saini, S, and Mathew, S. Non-albicans Candida infection: an emerging threat. Interdiscip Perspect Infect Dis. (2014) 2014:615958. doi: 10.1155/2014/615958
18. M27-A3 reference method for broth dilution antifungal susceptibility testing of yeasts; approved standard-third edition (2008) (cited 2020 Dec 4). Available from: www.clsi.org.
19. Wayne, PA. Clinical and laboratory standards institute (CLSI): reference method for broth dilution antifungal susceptibility testing of filamentous fungi (2008) 28(16). Available at: https://clsi.org/media/1897/m27ed4_sample.pdf
20. Perlroth, J, Choi, B, and Spellberg, B. Nosocomial fungal infections: epidemiology, diagnosis, and treatment. Med Mycol. (2007) 45:321–46. doi: 10.1080/13693780701218689
21. Esmailzadeh, A, Zarrinfar, H, Fata, AM, and Sen, T. High prevalence of Candiduria due to non-Albicans Candida species among diabetic patients: a matter of concern? J Clin Lab Anal. (2018) 32:1–5. doi: 10.1002/jcla.22343
22. Zakhem, A, Istambouli, R, Alkozah, M, Gharamti, A, Tfaily, M, Jabbour, J, et al. (2021). “Predominance of Candida Glabrata among non-Albicans Candida species in a 16-year study of Candidemia at a tertiary Care Center in Lebanon.” Pathogens 10: 1–10, doi: 10.3390/pathogens10010082
23. Kato, H, Iizawa, Y, Nakamura, K, Gyoten, K, Hayasaki, A, Fujii, T, et al. The critical role of biliary candidiasis in development of surgical site infections after Pancreatoduodenectomy: results of prospective study using a selective culture medium for Candida species. Biomed Res Int. (2018) 2018:5939724–8. doi: 10.1155/2018/5939724
24. Shenoy, SM, Shalini, S, Gopal, S, Tantry, B, Baliga, S, and Jain, A. Clinicomicrobiological analysis of patients with cholangitis. Indian J Med Microbiol. (2014) 32:157–60. doi: 10.4103/0255-0857.129802
25. Marak, MB. Dhanashree B antifungal susceptibility and biofilm production of candida spp. isolated from clinical samples. Int. J Microbiol. (2018) 2018:7495218. doi: 10.1155/2018/7495218
26. Ballal, M, Shenoy, PA, Rodrigues, GS, Devadas, SM, and Shetty, V. Bangera SR biliary tract infections and their microbiological Spectrum-a study from coastal region of southern India. Infection. (2019) 23:253–8. doi: 10.22354/in.v23i3.789
27. Baghdadi, E, Khodavaisy, S, Rezaie, S, Abolghasem, S, Kiasat, N, Salehi, Z, et al. Antifungal susceptibility patterns of Candida species recovered from endotracheal tube in an intensive care unit. Adv Med. (2016) 2016:1–6. doi: 10.1155/2016/9242031
28. Zhang, X-B, Yu, S-J, Yu, J-X, Gong, Y-L, Feng, W, and Sun, F-J. Retrospective analysis of epidemiology and prognostic factors for candidemia at a hospital in China, 2000-2009. Jpn J Infect Dis. (2012) 65:510–5. doi: 10.7883/yoken.65.510
29. Krishnasamy, L, Krishnakumar, S, Santharam, P, and Saikumar, C. Isolation and identification of Candida species in patients with Vulvovaginal candidiasis. J Pure Appl Microbiol. (2018) 12:2269–73. doi: 10.22207/JPAM.12.4.67
30. Kumwenda, P, Cottier, F, Hendry, A, Kneafsey, D, Keevan, B, Gallagher, H, et al. Estrogen promotes innate immune evasion of Candida Albicans through inactivation of the alternative complement system. Cell Rep. (2022) 38:110183. doi: 10.1016/j.celrep.2021.110183
Keywords: Candida albicans, non-albicans Candida, species distribution, antifungal susceptibility, retrospective-analysis
Citation: S U and Sumana MN (2023) Retrospective analysis on distribution and antifungal susceptibility profile of Candida in clinical samples: a study from Southern India. Front. Public Health. 11:1160841. doi: 10.3389/fpubh.2023.1160841
Edited by:
Pooja Vijayaraghavan, Amity University Uttar Pradesh, IndiaReviewed by:
Jata Shankar, Jaypee University of Information Technology, IndiaGuanzhao Liang, Chinese Academy of Medical Sciences and Peking Union Medical College, China
Copyright © 2023 S and Sumana. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: M. N. Sumana, bW5zdW1hbmExMkBnbWFpbC5jb20=
 Umamaheshwari S.
Umamaheshwari S. M. N. Sumana
M. N. Sumana