- 1Department of Environmental and Occupational Health and Safety, Institute of Public Health, College of Medicine and Health Sciences, University of Gondar, Gondar, Ethiopia
- 2Amhara Regional Health Beauro, Wogera Primary Hospital, Northwest, Ethiopia
- 3Department of Epidemiology and Biostatistics, Institute of Public Health, College of Medicine and Health Sciences, University of Gondar, Gondar, Ethiopia
- 4Department of Public Health, College of Health Sciences, Debre Tabor University, Debre Tabor, Ethiopia
Background: Risk identification, as well as the prevention and management of diseases associated with pregnancy or other conditions that may occur concurrently, is the essential component of ANC.
Method: The observational follow-up and cross-sectional studies on the effect of antenatal care on low birth weight in Africa were conducted according to the Preferred Reporting Items for Systematic reviews and Meta-Analyses guidelines. Five computerized bibliographic databases: Google Scholar, PubMed, Scopus, Cochrane Library, and Hinari Direct were searched for published studies written in English till May 2022. The risk of bias assessment tools developed by the Joanna Briggs Institute for cross-sectional and observational follow-up research was used, and the caliber of each included study was assessed. Seven papers were included, with a total of 66,690 children participating in the study.
Results: Seven studies met the selection criteria. Prenatal care and low birth weight were linked in four of the seven studies included in the review. The pooled odd ratio for low birth weight in the random-effects model was 0.46 (95% CI: 0.39, 0.53). The pooled odds ratio for low birth weight was 0.21 (95% CI: 0.19, 0.22) and 0.21 (95% CI: 0.19, 0.22), respectively, among pregnant women who had no antenatal care follow-up and those who had antenatal care follow up.
Conclusion: Women who attended at least one antenatal care appointment were more likely than their counterparts to have a baby of normal weight. Interventions to reduce low birth weight in Africa should focus on providing adequate antenatal care and quality healthcare services to women with low socioeconomic status.
Background
The care provided to pregnant women and adolescent girls by skilled medical professionals throughout pregnancy is known as antenatal care (ANC). Risk identification, as well as the prevention and management of diseases associated with pregnancy or other conditions that may occur concurrently, is the essential component of ANC (1). Although it is widely accepted that ANC should be tailored to each patient, there is a lack of explicit definitions of the practices required to support normal pregnancy outcomes, particularly in developing countries where resources are frequently scarce. It is due to the lack of credible studies on the effects of antenatal care continuity, availability, and substance on pregnancy outcomes like low birth weight (LBW), postnatal morbidity, and mortality (2).
The World Health Organization (WHO) defines LBW as a baby’s weight of less than 2.5 kilograms. Over 20 million births are thought to have LBW each year, accounting for 15 to 20% of all babies born worldwide. Additionally, there are regional variations in the percentage of LBW, with South Asia having a 28 percent rate, Sub-Saharan Africa having a 13 percent rate, and Latin America having a 9 percent rate (3, 4). Twenty-two million babies were born in the world in 2013. Of these, 16% of babies had LBW, with 96% of births found in developing countries (5). A study in Nepal in 2011 found that the prevalence of LBW was 15.4% (6). It was found that LBW infants were more likely to pass away in the first year. Small-for-gestational-age birth (born before 37 weeks of pregnancy), intrauterine growth retardation, or a combination of the two can result in LBW (7). Neonatal mortality and low birth weight were found to be linked, indicating a serious public health issue. A thorough review of the literature up to 2011 and a meta-analysis revealed an odds ratio of 8.5 for neonatal mortality in full-term (37 gestational weeks) newborns weighing 2.5 kg (8). As revealed by a cohort study in Brazil between 2011 and 2012, LBW was one of the factors associated with neonatal mortality (9). Furthermore, asthma and hypertension were two morbidities linked to LBW (8, 10).
Recently published research suggested that ANC attendance was related to (11, 12). The WHO recommended that ANC visits throughout pregnancy time must be at least four; however, a new model unveiled in 2016 recommends that the minimum contact must be at least eight (13). There is compelling evidence that skipping ANC visits or skipping fewer visits than recommended increased the risk of LBW by four (13). This viewpoint was supported by the fact that ANC provides a channel for delivering a variety of therapies to pregnant women that improve maternal and fetal health outcomes (14).
In impoverished nations, the highest LBW cases were caused by intrauterine development retardation, while preterm delivery was like in wealthy countries (4, 15). Aside from the negative outcomes of increased neonatal morbidity and mortality, restricted growth and cognitive development, and a higher risk of chronic illness development later in life (16). LBW has been linked to an increased risk of non-communicable diseases such as diabetes and cardiovascular disease later in life (17, 18).
Low birth weight (LBW) was associated with at least five to eight missed ANC appointments, no ANC services during the first trimester, and a lack of availability of certain ANC supplies (11, 19). Aside from that, there is disagreement about how ANC therapies influence maternal and neonatal health outcomes (20, 21). To date, ANC alone has not been proven to improve birth outcomes but other healthcare programs reduce perinatal mortality (22) and newborn morality is also reduced when study models compared with ANC visits (23).
On the other hand, insufficient and no ANC had no impact on perinatal mortality (24), while improved ANC had no effect on perinatal or neonatal mortality (25). As a result, this systematic review and meta-analysis aimed to evaluate the effectiveness of ANC in reducing the rate of low birth weight (LBW) among children in Africa.
Methods and materials
Search strategy
A thorough search of the literature was employed using databases (PubMed, Scopus, the Cochrane Library, and Hinari Direct) and search engines such as Google Scholar. Scholars with extensive experience in systematic reviews conducted the initial search, and GTE independently screened titles, abstracts, and full texts. In the event of a disagreement, another reviewer was asked to settle it. The initial search terms were LBW, ANC (effect, prenatal care, antenatal care, infant, low birth weight, and low-birth-weight infant, and Africa).
In the search strategy, a combination of keywords related to LBW, terms related to study design (prevalence, epidemiology, cross-sectional study, observation follow-up study), and title, title/abstract, or medical subject heading was developed. Additionally, relevant literature was identified by searching the reference lists of full-text articles and grey literature on Google.
Eligibility criteria
We settled on the following criteria to incorporate studies in the review: (1) women who were delivering or labouring, had newborn babies, were pregnant women, or were postpartum women who had live births, (2) studies in analytical cross-sectional and observational follow-up study designs, (3) the study reported the outcomes of low birth weight, (4) the use of ANC was regarded as a factor or exposure for the outcomes, (5) the article was published in English, and (6) the study will be published? (Is it only published? (What about grey literature?)) until May 15, 2022.
Risk of bias assessment
The selection of the articles was based on the standardized critical appraisal instrument adapted from Hoy et al.’s risk of bias tool (26). The tool has 9 items, with a maximum score of nine and a minimum of zero. The overall risk of the bias has been leveled into three categories: 0–3 = low risk, 4–6 = moderate risk and 7–9 = high risk.
Data extraction and outcome of interest
The author extracts the data and compared the results. Discrepancies were resolved by discussion, or the six reviewers made the decision. The primary authors of the eligible studies were contacted through their email or phone for further clarification about the data. We extracted the following data from each study:
i. Author(s) and years of publication
ii. Study design (cross-sectional and observational follow-up)
iii. Country of the region and participants (mothers who give birth, pregnant women, all live births, and women born 5 years prior)
iv. Prevalence estimates reported stratified by the weight of the child and ANC
The primary outcomes were pooled of LBW prevalence, and the secondary outcome was identifying the effect of antenatal care on LBW and investigating.
Reliability
The second reviewer was blinded to the primary reviewer’s (GTE and DAA) decisions on article selection, data extraction, and risk of bias assessment. Any differences were solved through discussion; otherwise, another person was available to arbitrate any issues that remained unresolved.
Analysis of the data
The relevance of each study was assessed based on its topic, objectives, and methodology. An initial descriptive analysis of the studies has been employed. Heterogeneity between estimates was assessed using the I2 statistic; an I2 value of above 75% indicates considerable heterogeneity (27–29). Potential influences on the prevalence estimate were investigated using sensitivity analyses. Where studies allowed, we descriptively compared prevalence estimates by sex, first author’s last name, publication year, study design, site, sample size, study duration, study population, outcome, and comparison groups were all recorded for each study. The exposure variable was divided into two categories: “No ANC visit at all” and “One or more ANC visits. Quantitative papers were pooled in a statistical meta-analysis using the STATA version 14. Both odd ratios and heterogeneity were considered statistically significant if the value of p was less than 0.05. Egger’s test for small-study effects (p-value <0.05) was used to look into possible publication bias (30).
Outcome measurement
The WHO defines low birth weight as a weight of less than 2,500 g. But the length of the pregnancy and the rate of fetal growth affect the birth weight (31). When a newborn’s weight was less than 2,500 grams, LBW was considered (31, 32).
Patient and public involvement
There was no patient or public involvement in this study.
Result
The review processes
The initial database search generated 125 articles. After removing duplicates by title and abstract, 83 remained. All 83 articles were considered for the full-text review. Then, after the full text of 19 articles was reviewed, 12 articles were excluded (their outcomes were not directly related to our outcomes of interest), and seven articles were included for both the systematic review and meta-analysis (Figure 1).
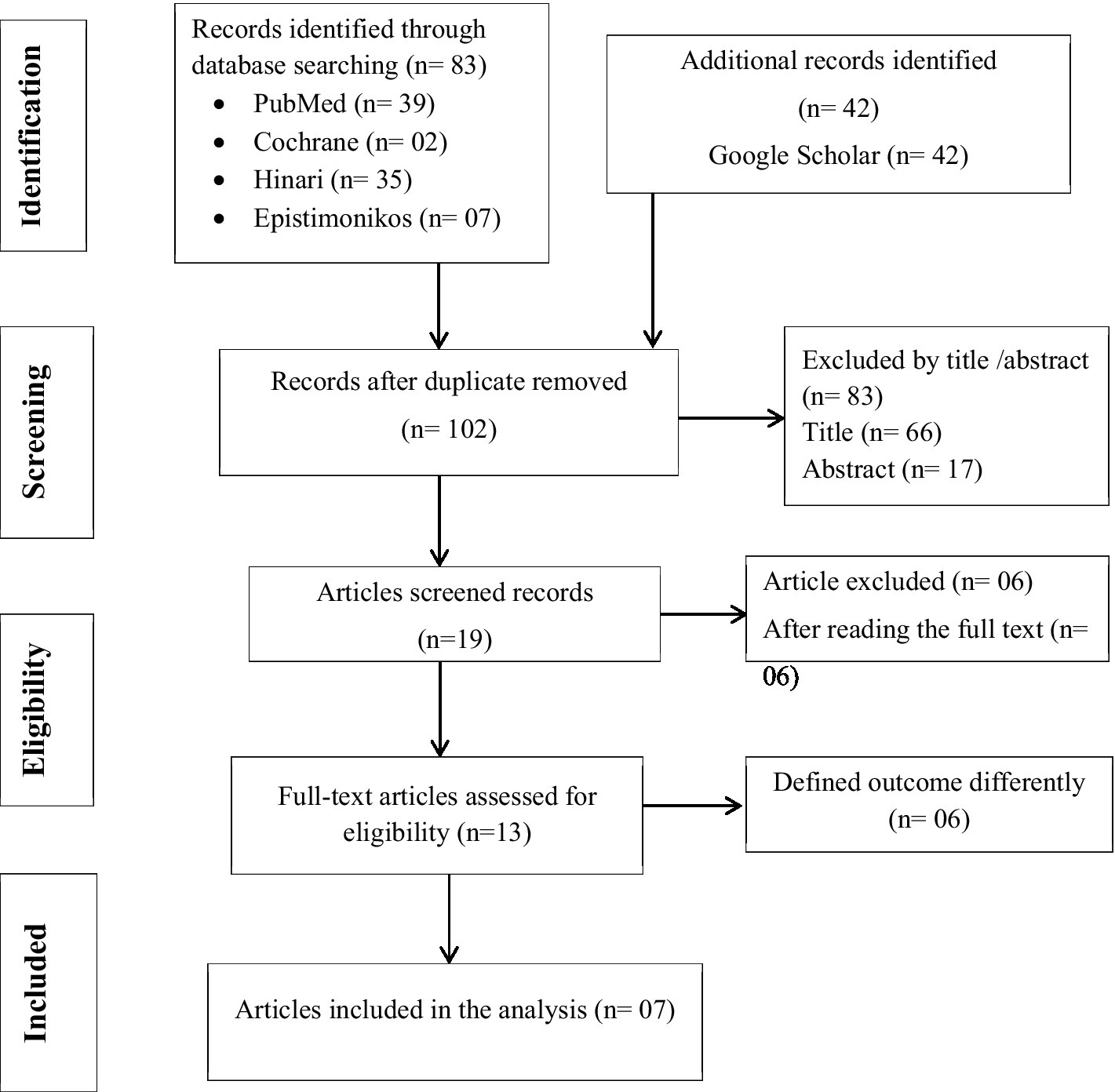
Figure 1. PRISMA flow chart for identifications of studies that were included in the systematic review and Meta-analysis in Africa.
Characteristics of the included studies
Table 1 lists the characteristics of the seven primary studies that were a part of this review. In diverse regions of Africa, four cross-sectional studies, one retrospective follow-up study, one case–control study, and one prospective cohort study were conducted.
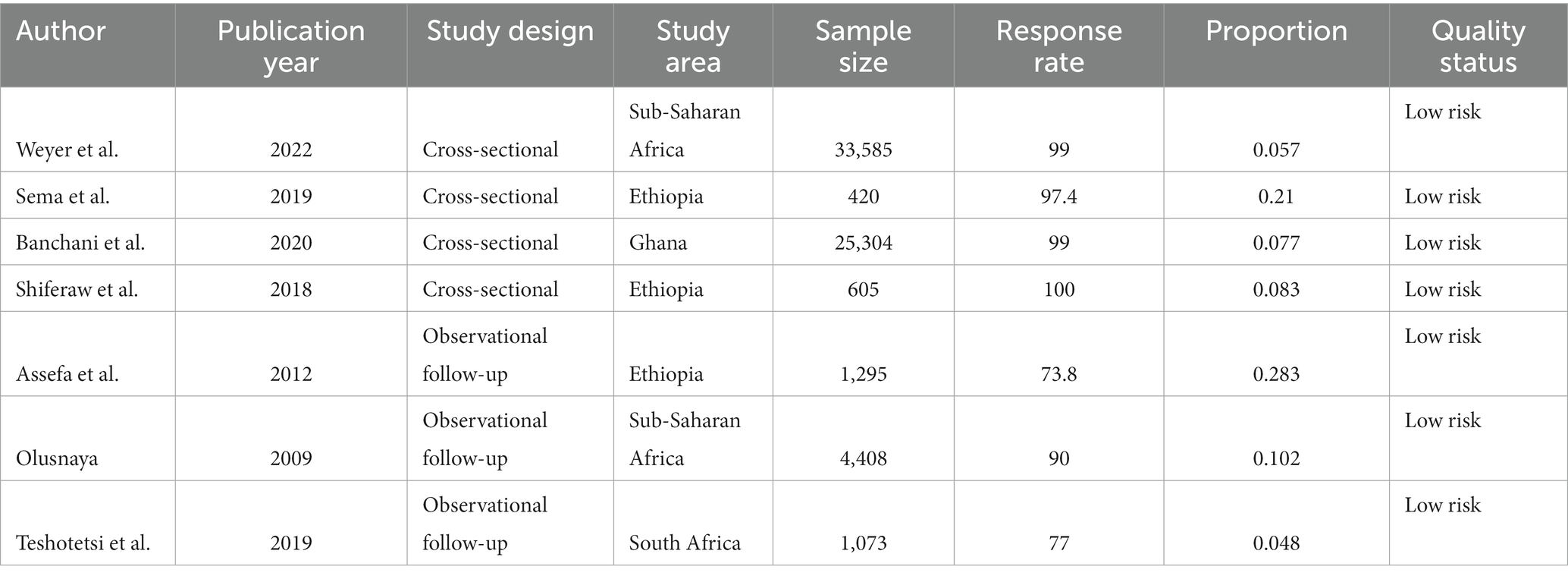
Table 1. Characteristics of the individual studies included in this systematic review and meta-analysis, 2022.
A total of seven studies with 66,690 participants were included. About a quarter (33.3%) of the studies were from Ethiopia (33–35), one from South Africa (36), and Sub-Saharan Africa contributed two studies each (15, 37), and one was from Ghana (38). All included studies were cross-sectional and observational and published between 2009 and 2022. The sample sizes ranged from 420 in Ethiopia to 33,585 in Sub-Saharan Africa. Africa had the lowest and highest rates of LBW, 4.8 and 21.3%, respectively. Except for two studies using data from the Demographic Health Survey (DHS), all the studies were done in healthcare settings.
Of the seven included studies, five of them were institution based, while the rest were demographic and health surveys. Five studies reported the effect of ANC on low birth weight, one anthropometric measurement, and the rest general LBW (Table 1). To diagnose LBW, The weight is compared with the baby’s gestational age and recorded in the medical record. The criteria of WHO were used (birth weight less than 2,500 grams (5 pounds, 8 ounces) is diagnosed as low birth weight). Babies weighing less than 1,500 grams (3 pounds, 5 ounces) at birth are considered to have very low birth weight (31, 32).
Meta-analysis
In the estimation of the pooled effect of ANC on LBW among ANC-attendant women in Africa, seven studies were used, and a total of 66,690 pregnant women and mothers who give birth were participants. The forest plot results of seven included studies showed that the overall pooled prevalence of LBW in Africa was 15% (95% CI: 0.14, 0.16). There is no heterogeneity, as evidenced by the I-squared (I2) statistics (Iʌ2 = 0.00%, p = .). Hence, a fixed-effect model was used to estimate the overall pooled effect size of ANC on LBW among ANC-attendant women in Africa (Figure 2).
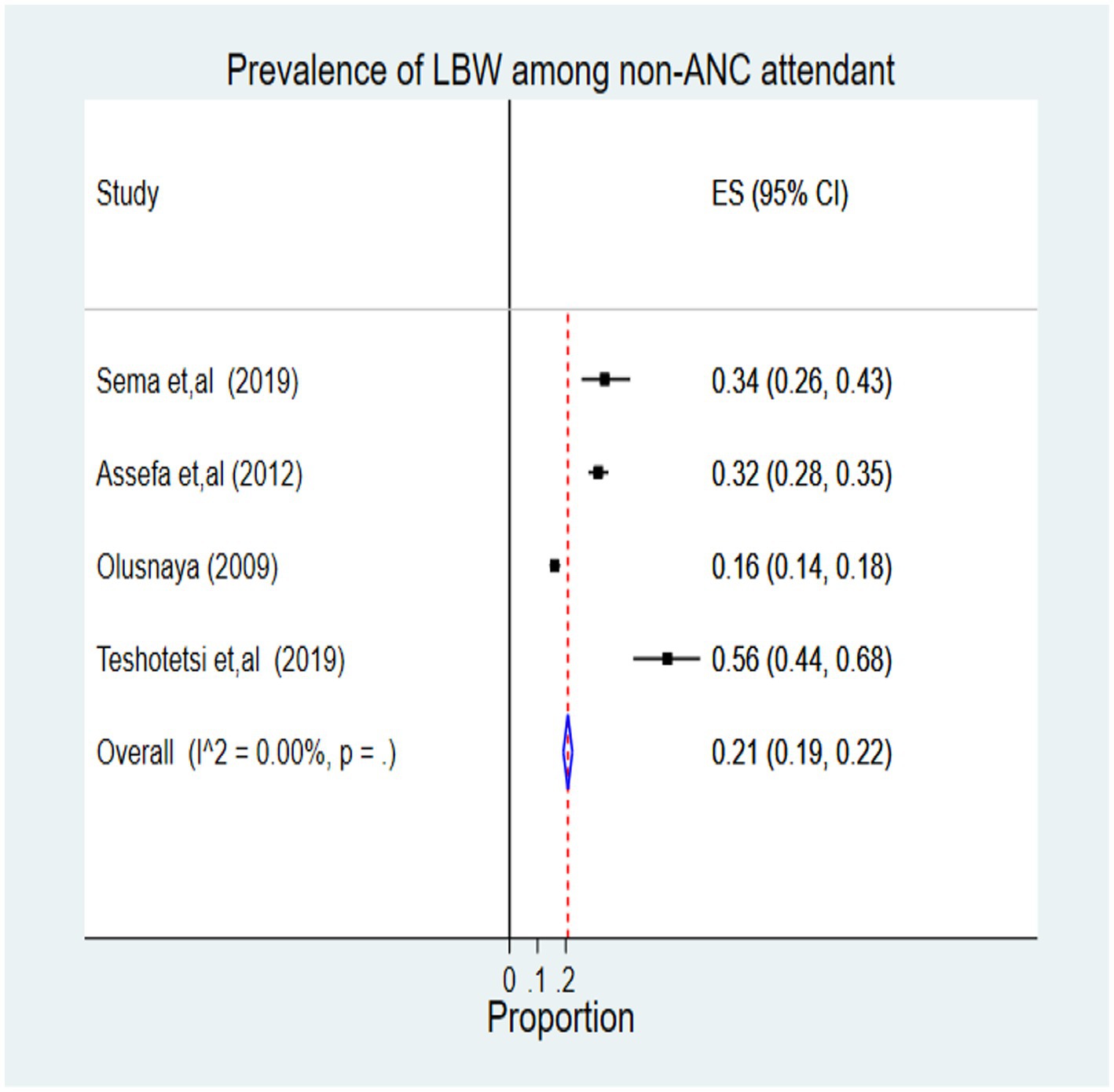
From this review, among non-ANC attendant women, 533 cases of LBW were identified among 2,348 newborn children, representing 21% (95% CI: 0.19, 0.22). According to the I2 statistics, heterogeneity is not an issue (Iʌ2 = 0.00%, p = 0.01) (Figure 3).
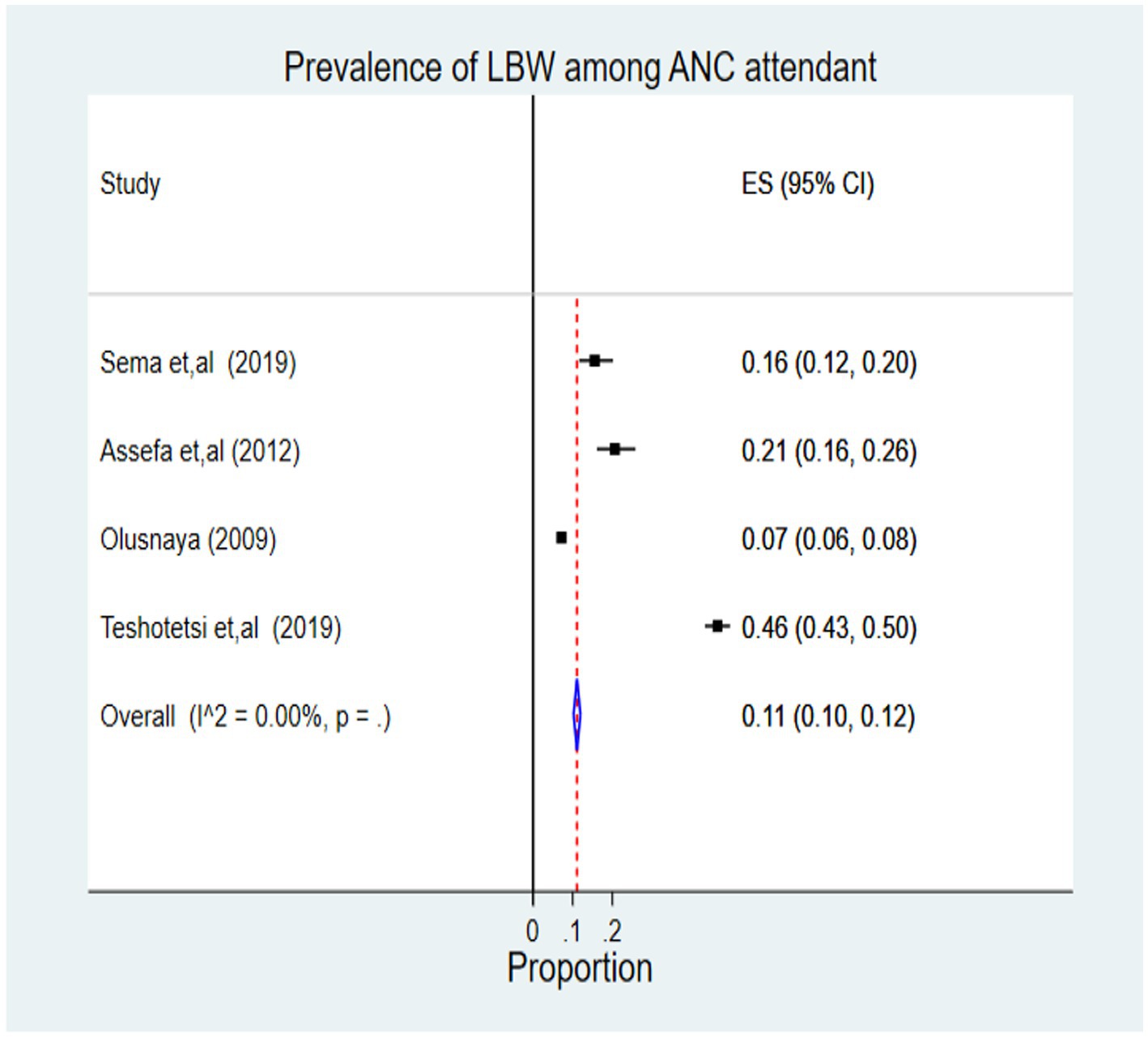
Four thousand four hundred nine newborns had 769 cases of LBW among ANC attendant mothers, which represents 11% (95% CI 0.10, 0.12). According to the I2 statistics, there was no heterogeneity problem (Iʌ2 = 0.00%, p = 0.01) (Figure 4).
Subgroup analysis by study design
A subgroup analysis was performed to determine the pooled prevalence of LBW in Africa based on the study design. The cross-sectional study had the greatest prevalence rate, at 21% (95% CI: 0.17, 0.25), and Figure 5 shows the I-squared statistics (Iʌ2 = 0.00%, p = .).
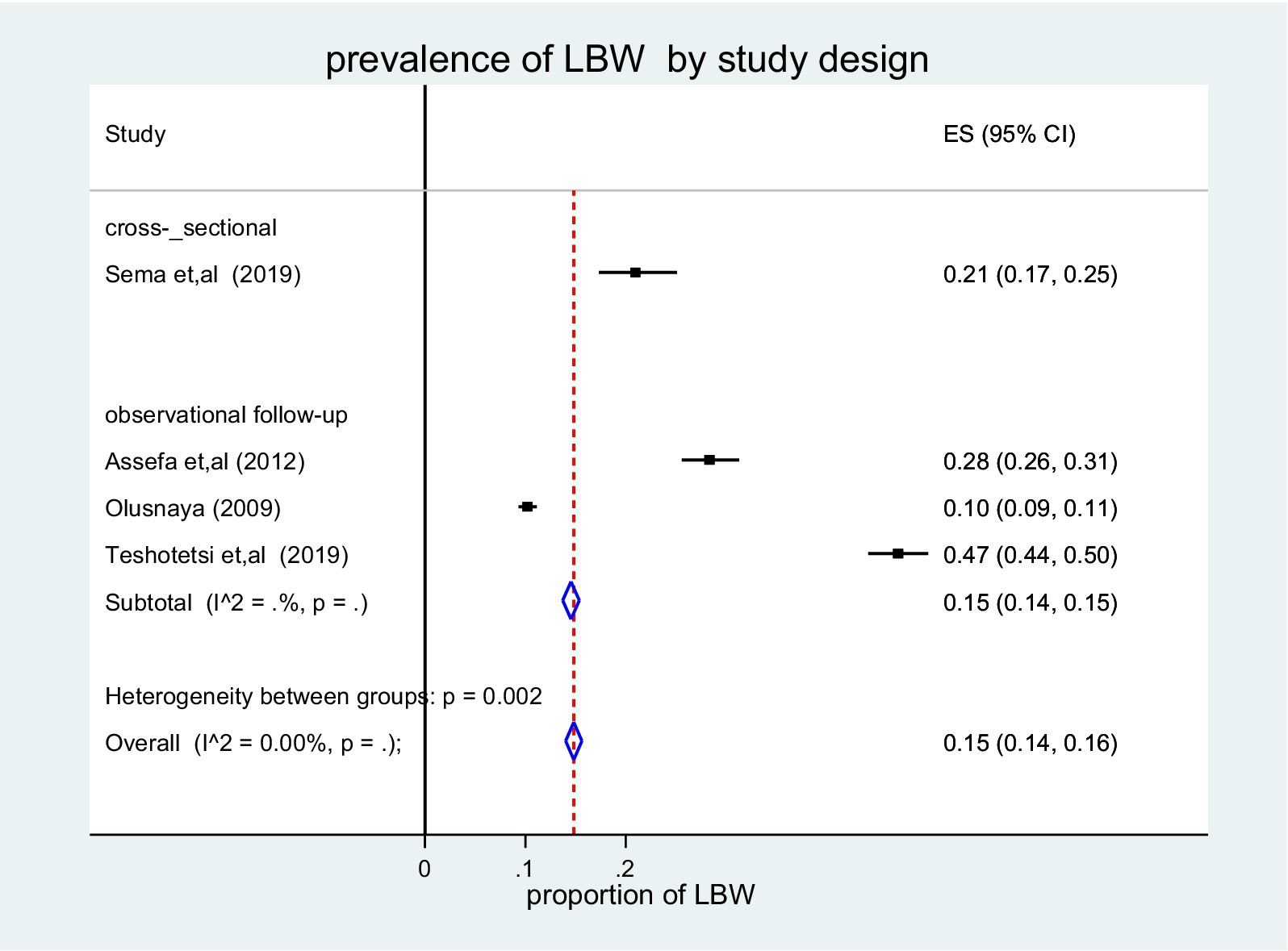
Figure 5. Forest plot of the pooled prevalence of LBW among children in Africa by study design, 2022.
The pooled effect size of ANC on low birth weight
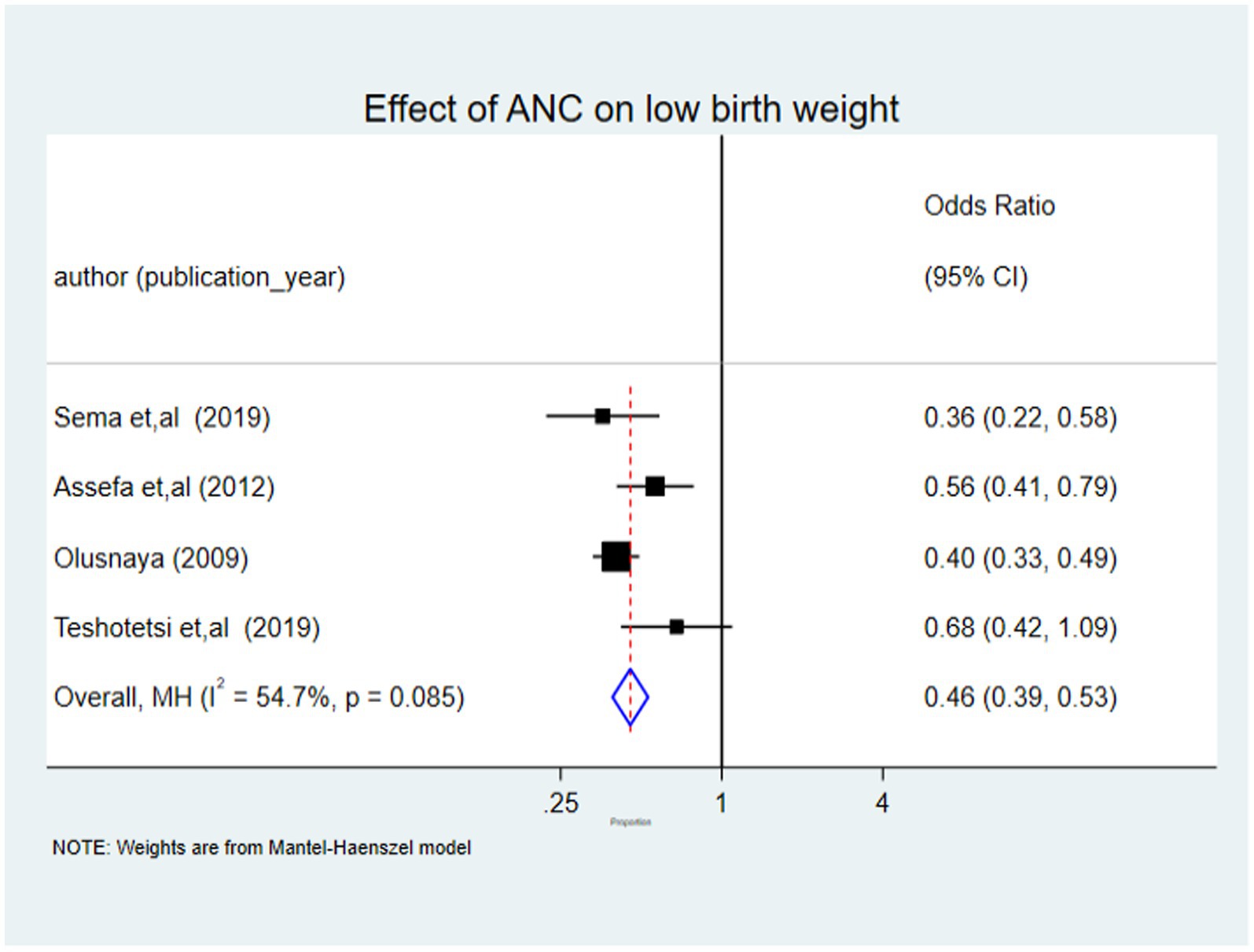
Four of the seven studies included in the analysis, each with at least one ANC visit, revealed statistically significant associations with LBW. There were 6,757 children involved in all four studies. Compared to neonates whose mothers received no ANC follow-up at all, the Mantel–Haenszel method by fixed effect model for children born to women who received at least one ANC follow-up was 0.46 (95% CI: 0.39, 0.53) with I-squared statistics of 54.7% (Iʌ2 = 54.7%, p = 0.000). According to this finding, using ANC services decrease the burden of LBW by 54% when compared to non-ANC attendants (Figure 6).
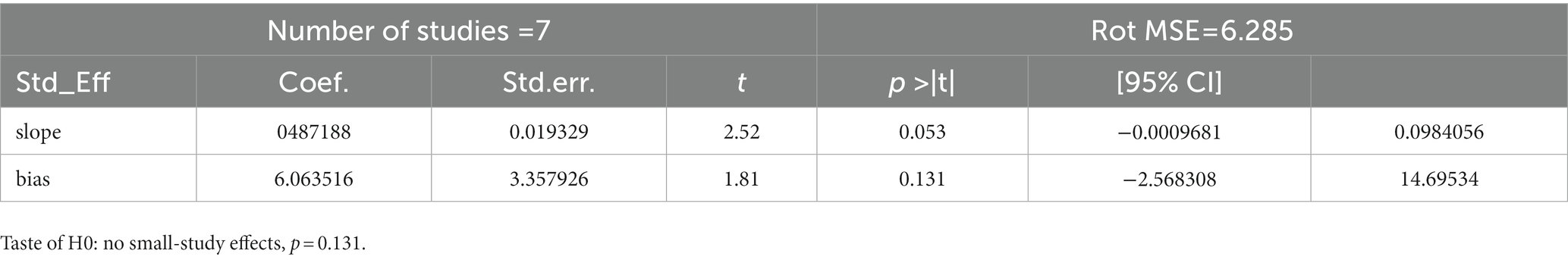
Small study effect
Utilizing a funnel plot and Egger test, it was determined whether a potential small study effect existed. The value of p for egger’s test was checked (p = 0.131), and there was no indication of publication bias since this funnel plot demonstrated an asymmetric distribution (Table 2).
Discussion
The purpose of this study was to determine the efficacy of targeted ANC in reducing LBW in newborns from African populations. Seven major studies testing ANC with a variety of groups, including pregnant women, labouring women, and postpartum moms, as well as their newborn children’s weight, were found to be eligible. The benefits of ANC delivered by skilled attendants for the health of babies have been documented throughout Africa. In LMICs, a variety of tactics and strategies have been used to improve the effectiveness of ANC. Most LMICs, including Africa, have adopted WHO’s focused ANC approach, which was created in the 1990s (39). In this meta-analysis, a total of 66,690 children were included to estimate the pooled effect size of ANC on low birth weight. The seven studies were conducted in different countries on the continent. All studies were conducted in a health institution setting, and among a total of 66,690 children, 533 and 769 low birth weight newborns were identified among non-ANC attendant and ANC attendant women, respectively. The risk of bias assessment was done for both cross-sectional and observational follow-up studies independently using JBI risk of bias assessment tools, and all studies had a low risk of bias.
The association between low birth weight and prenatal care utilization is clinically plausible and has been noted previously. A child’s birth weight is an important indicator of the child’s vulnerability to the risk of childhood illnesses and the chances of survival. Although, LBW is one of the main risk factors for infant morbidity and mortality
Different factors affect LBW among pregnant mothers. Risk factors for low birth weight include, for example, the location of the kitchen in the living room, an iron intake of less than 180 tablets, a weight gain of less than 6.53 kg during the second and third trimesters, comorbidity during pregnancy, attendance at ANC, and preterm birth (47, 48). Attendance of at least one ANC follow-up by pregnant women had a statistically significant effect on LBW. In this study, women who had at least one ANC visit with a qualified attendant in Africa had a 54 percent lower risk of LBW. The study’s main finding was that even limited ANC (as little as one visit) results in better newborn weight than no ANC, and encouraging pregnant women to seek ANC would have a significant impact on the LBW rate and would be an essential strategy to include in planning initiatives aimed at reducing LBW. This result is consistent with studies from other countries (49, 50), and other population-based birth registry results from the global network in Africa, India, Pakistan, and Guatemala (51). A study in Asia found that women who had ANC visits and delivered in a health institution had a lower risk of LBW (52).
Low birth weight (LBW) is related to the quality and sufficiency of prenatal care (ANC). Additionally, it is a result of intrauterine growth restriction or premature birth. Pregnant women receive a variety of services during ANC visits, including tetanus toxoid-diphtheria immunization and intermittent preventative therapy in pregnancy (IPTp), both of which are crucial for the health of the expectant mother and the unborn child (5, 15). A subgroup analysis and a thorough database search were both performed to determine whether any particular study level factor best described the results. The vast sample size of the analysis allowed it to identify the impact of ANC on LBW in Africa because the evaluation covered all research done in Africa. They were done in English and were cross-sectional and observational studies with inherent biases, the systematic review and meta-analysis were constrained. Articles based on the number of visits were excluded because they did not identify zero visits, making it impossible to pool the overall effect size of ANC for those studies.
Limitations of the study
The evaluation of this study covered all research done in Africa, and the large sample size of the analysis allowed it to identify the impact of ANC on LBW in Africa. However, the studies were cross-sectional and observational with inherent biases, and the systematic review and meta-analysis were limited. Articles based on the number of visits were excluded because they did not identify zero visits, making it impossible to pool the overall effect size of ANC for those studies.
Conclusion
The frequency and follow-up of prenatal care visits demonstrated a positive correlation with birth weight. Encouraging pregnant women to seek prenatal care, even when they are in their third trimester, can be beneficial. Furthermore, it is warranted to point out the necessity of enhancing communication, education, and information activities. A well-designed prospective follow-up study should be conducted to determine whether a minimal number of visits are required to increase birth weight.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
GTE and DAA were responsible for the inception of the idea and study. The authors participated from the inception of the study to the final manuscript’s writing, reviewing, and editing. AHT, MF, AN, AY, WA, and MTE were also involved in the article selection, statistical analysis, and writing and editing of the manuscript. All authors contributed to the article and approved the submitted version.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
ANC, Antenatal Care; CI, Confidence Interval; DHS, Demographic Health Survey; IUGR, Intrauterine Growth Restriction; JBI, Joanna Briggs Institute; LBW, Low Birth Weight; LMICS, Low-and-Middle-Income Countries; PICO, Population, Intervention, Comparison, Outcome; PRISMA, Preferred Reporting Items for Systematic Review and Meta-analysis statement; SSA, Sub-Saharan Africa; WHO, World Health Organization.
References
1. Coria-Soto, IL, Bobadilla, JL, and Notzon, F. The effectiveness of antenatal care in preventing intrauterine growth retardation and low birth weight due to preterm delivery. Int J Qual Health Care. (1996) 8:13–20. doi: 10.1093/intqhc/8.1.13
2. Fund UNCs, Fund WHOJUNCs, York WHON. Low birthweight: Country, Regional and Global Estimates. Geneva: World Health Organization (2004).
3. Shaheen, R, Roy, M, Anny, A, Shova, NY, and Hema, TJDSAHMJ. Prevalence of low birth weight in urban Dhaka and its association with maternal age and socioeconomic status. PLoS One. (2020) 2:162–6. doi: 10.2991/dsahmj.k.200905.001
4. Moreira, AIM, Sousa, PRM, and Sarno, FJE. Low birth weight and its associated factors. Einstein (São Paulo). (2018) 16:eAO4251. doi: 10.31744/einstein_journal/2018AO4251
5. Acharya, D, Singh, JK, Kadel, R, Yoo, S-J, Park, J-H, Lee, K, et al. Maternal factors and utilization of the antenatal care services during pregnancy associated with low birth weight in rural Nepal: analyses of the antenatal care and birth weight records of the MATRI-SUMAN trial. Int J Environ Res Public Health. (2018) 15:2450. doi: 10.3390/ijerph15112450
6. Singh, U, Ueranantasun, A, and Kuning, MJBP. Factors associated with low birth weight in Nepal using multiple imputation. BMC Pregnancy Childbirth. (2017) 17:1–10. doi: 10.1186/s12884-017-1252-5
7. Lawn JECousens, S, and Zupan, J, Lancet Neonatal Survival Steering Team. 4 million neonatal deaths: when? Where? Why? Int J Environ Res Public Health. (2005) 365:891–900. doi: 10.1016/S0140-6736(05)71048-5
8. Malin, G, Morris, R, Riley, R, Teune, M, and Kjbaijoo, K. when is birthweight at term abnormally low? A systematic review and meta-analysis of the association and predictive ability of current birthweight standards for neonatal outcomes. BJOG. (2014) 121:515–26. doi: 10.1111/1471-0528.12517
9. Lansky, S, Friche, AA d L, Silva, AAM d, Campos, D, Bittencourt, SD d A, Carvalho, ML d, et al. Pesquisa Nascer no Brasil: perfil da mortalidade neonatal e avaliação da assistência à gestante e ao recém-nascido. Cad Saude Publica. (2014) 30:S192–207. doi: 10.1590/0102-311X00133213
10. Mu, M, Wang, S-F, Sheng, J, Zhao, Y, Li, H-Z, Hu, C-L, et al. Birth weight and subsequent blood pressure: a meta-analysis. Arch Cardiovasc Dis. (2012) 105:99–113. doi: 10.1016/j.acvd.2011.10.006
11. Zhou, H, Wang, A, Huang, X, Guo, S, Yang, Y, Martin, K, et al. Quality antenatal care protects against low birth weight in 42 poor counties of Western China. PLoS One. (2019) 14:e0210393. doi: 10.1371/journal.pone.0210393
12. Tafere, TE, Afework, MF, and AWJRH, Y. Providers adherence to essential contents of antenatal care services increases birth weight in Bahir Dar City Administration, north West Ethiopia: a prospective follow up study. Reprod Health. (2018) 15:1–8. doi: 10.1186/s12978-018-0610-8
13. Lattof, SR, Moran, AC, Kidula, N, Moller, A-B, Jayathilaka, CA, Diaz, T, et al. Implementation of the new WHO antenatal care model for a positive pregnancy experience: a monitoring framework. BMJ Glob Health. (2020) 5:e002605. doi: 10.1136/bmjgh-2020-002605
14. Asundep, NN, Carson, AP, Turpin, CA, Tameru, B, Agidi, AT, Zhang, K, et al. Determinants of access to antenatal care and birth outcomes in Kumasi. Ghana. (2013) 3:279–88. doi: 10.1016/j.jegh.2013.09.004
15. Weyori, AE, Seidu, A-A, Aboagye, RG, Holmes, FA, Okyere, J, Okyere, J, et al. Antenatal care attendance and low birth weight of institutional births in sub-Saharan Africa. BMC Pregnancy Childbirth. (2022) 22:1–8. doi: 10.1186/s12884-022-04576-4
16. Chen, W, Srinivasan, SR, Yao, L, Li, S, Dasmahapatra, P, Fernandez, C, et al. Low birth weight is associated with higher blood pressure variability from childhood to young adulthood: the Bogalusa heart study. Am J Epidemiol. (2012) 176:S99–S105. doi: 10.1093/aje/kws298
17. Ediriweera, DS, Dilina, N, Perera, U, Flores, F, and Samita, SJBPH. Risk of low birth weight on adulthood hypertension-evidence from a tertiary care hospital in a south Asian country, Sri Lanka: a retrospective cohort study. BMC Public Health. (2017) 17:1–6. doi: 10.1186/s12889-017-4268-x
18. Ba, L, Bertrais, S, Czernichow, P, and Leger, JJP. School difficulties in 20-year-olds who were born small for gestational age at term in a regional cohort study. BMC Public Health. (2001) 108:111–5. doi: 10.1542/peds.108.1.111
19. Tayebi, T, Hamzehgardeshi, Z, Ahmad Shirvani, M, Dayhimi, M, and Danesh, M. Relationship between revised graduated index (R-GINDEX) of prenatal care utilization & preterm labor and low birth weight. Glob J Health Sci. (2014) 6:131–7. doi: 10.5539/gjhs.v6n3p131
20. Adam, T, Lim, SS, Mehta, S, Bhutta, ZA, Fogstad, H, Mathai, M, et al. Cost effectiveness analysis of strategies for maternal and neonatal health in developing countries. BMJ. (2005) 331:1107. doi: 10.1136/bmj.331.7525.1107
21. Carroli, G, Villar, J, Piaggio, G, Khan-Neelofur, D, Gülmezoglu, M, Mugford, M, et al. WHO systematic review of randomised controlled trials of routine antenatal care. Lancet. (2001) 357:1565–70. doi: 10.1016/S0140-6736(00)04723-1
22. Rumbold, AR, and Cunningham, JJM. Journal ch. A review of the impact of antenatal care for Australian indigenous women and attempts to strengthen these services. Lancet. (2008) 12:83–100. doi: 10.1007/s10995-007-0216-1
23. Dowswell, T, Carroli, G, Duley, L, Gates, S, Gülmezoglu, AM, Khan-Neelofur, D, et al. Alternative versus standard packages of antenatal care for low-risk pregnancy. Cochrane Database Syst Rev. (2015) 2015:CD000934. doi: 10.1002/14651858.CD000934.pub3
24. Tuladhar, H, and NJNJOO, D. Impact of antenatal care on maternal and perinatal utcome: a study at Nepal medical college teaching hospital. Nepal J Obstet Gynecol. (2011) 6:37–43. doi: 10.3126/njog.v6i2.6755
25. Pasha, O, McClure, EM, Wright, LL, Saleem, S, Goudar, SS, Chomba, E, et al. A combined community-and facility-based approach to improve pregnancy outcomes in low-resource settings: a global network cluster randomized trial. BMC Med. (2013) 11:1–12. doi: 10.1186/1741-7015-11-215
26. Hoy, D, Brooks, P, Woolf, A, Blyth, F, March, L, Bain, C, et al. Assessing risk of bias in prevalence studies: modification of an existing tool and evidence of interrater agreement. J Clin Epidemiol. (2012) 65:934–9. doi: 10.1016/j.jclinepi.2011.11.014
27. Higgins, JP, and Green, S. Cochrane handbook for systematic reviews of interventions. Chichester, England; Hoboken. NJ: Wiley-Blackwell (2008).
28. Higgins, JP, Thompson, SG, Deeks, JJ, and Altman, DGJB. Measuring inconsistency in meta-analyses. BMJ. (2003) 327:557–60. doi: 10.1136/bmj.327.7414.557
29. Cumpston, M, Li, T, Page, MJ, Chandler, J, Welch, VA, Higgins, JP, et al. Updated guidance for trusted systematic reviews: a new edition of the Cochrane handbook for systematic reviews of interventions. Cochrane Database Syst Rev. (2019) 10:14651858. doi: 10.1002/14651858.ED000142
30. Egger, M, Smith, GD, Schneider, M, and Minder, CJB. Bias in meta-analysis detected by a simple, graphical test. BMJ. (1997) 315:629–34. doi: 10.1136/bmj.315.7109.629
31. Kramer, MS. Determinants of low birth weight: methodological assessment and meta-analysis. Bull World Health Organ. (1987) 65:663–737.
32. Egata, AD, and Bafa, TA. Predictors of low birth weight in newborn delivered in public Hospital of Gurage Zone, southern Ethiopia: a case-control study. Food Sci Nutr. (2019) 10:428–38. doi: 10.4236/fns.2019.104032
33. Sema, A, Tesfaye, F, Belay, Y, Amsalu, B, Bekele, D, and Desalew, AJ. Associated factors with low birth weight in Dire Dawa City, Eastern Ethiopia: a cross-sectional study. Biomed Res Int. (2019) 2019:2965094. doi: 10.1155/2019/2965094
34. Assefa, N, Berhane, Y, and Worku, A. Wealth status, mid upper arm circumference (MUAC) and antenatal care (ANC) are determinants for low birth weight in Kersa, Ethiopia. PLoS One. (2012) 7:e39957. doi: 10.1371/journal.pone.0039957
35. Shiferaw, CB, Yallew, WW, and Tiruneh, GT. Maternal anthropometric measurements do not have effect on birth weight of term, single, and live births in Addis Ababa City, Ethiopia. J Pregnancy. (2018) 2018:1982134. doi: 10.1155/2018/1982134
36. Tshotetsi, L, Dzikiti, L, Hajison, P, and SJPO, F. Maternal factors contributing to low birth weight deliveries in Tshwane District, South Africa. PLoS One. (2019) 14:e0213058. doi: 10.1371/journal.pone.0213058
37. Olusanya, BO, and Ofovwe, GEJM. Predictors of preterm births and low birthweight in an inner-city hospital in sub-Saharan Africa. Matern Child Health J. (2010) 14:978–86. doi: 10.1007/s10995-009-0528-4
38. Banchani, E, and Tenkorang, EY. Determinants of low birth weight in Ghana: does quality of antenatal care matter? Matern Child Health J. (2020) 24:668–77. doi: 10.1007/s10995-020-02895-6
39. Haddad, SM, Souza, RT, Cecatti, JG, Barreix, M, Tamrat, T, Footitt, C, et al. Building a digital tool for the adoption of the World Health Organization’s antenatal care recommendations: methodological intersection of evidence, clinical logic, and digital technology. J Med Internet Res. (2020) 22:e16355. doi: 10.2196/16355
40. Fonseca, J, Silva, A, Rocha, P, Batista, R, Thomaz, E, Lamy-Filho, F, et al. Racial inequality in perinatal outcomes in two Brazilian birth cohorts. Braz J Med Biol Res. (2021) 54:e10120. doi: 10.1590/1414-431x202010120
41. MJAJOPH, K. The adequacy of prenatal care utilization index: its US distribution and association with low birthweight. Eur J Obstet Gynecol Reprod Biol. (1994) 84:1486–9. doi: 10.2105/AJPH.84.9.1486
42. Ahmed, FU, and Das, AM. Beneficial effects. Three ANC visits might be the divergent point in lowering low birth weight babies. Bangladesh Integration (Tokyo Japan). (1992):50–3.
43. De Bernabé, JV, Soriano, T, Albaladejo, R, Juarranz, M, MAE, C, Martinez, D, et al. Risk factors for low birth weight: a review. Eur J Obstet Gynecol Reprod Biol. (2004) 116:3–15. doi: 10.1016/j.ejogrb.2004.03.007
44. Nahar, N, Afroza, S, and Hossain, MJBMRCB. Incidence of low birth weight in three selected communities of Bangladesh. Bangladesh Med Res Counc Bull. (1998) 24:49–54.
45. Vahdaninia, M, Tavafian, SS, and AJBP, M. Correlates of low birth weight in term pregnancies: a retrospective study from Iran. BMC Pregnancy Childbirth. (2008) 8:1–5. doi: 10.1186/1471-2393-8-12
46. Dubois, L, and Girard, MJPI. Determinants of birthweight inequalities: population-based study. Pediatr Int. (2006) 48:470–8. doi: 10.1111/j.1442-200X.2006.02256.x
47. Kc, A, Basel, PL, and SJPO, S. Low birth weight and its associated risk factors: health facility-based case-control study. PLoS One. (2020) 15:e0234907. doi: 10.1371/journal.pone.0234907
48. Desta, SA, Damte, A, and TJIJOP, H. Maternal factors associated with low birth weight in public hospitals of Mekelle city, Ethiopia: a case-control study. Ital J Pediatr. (2020) 46:1–9. doi: 10.1186/s13052-020-00890-9
49. Engmann, C, Matendo, R, Kinoshita, R, Ditekemena, J, Moore, J, Goldenberg, RL, et al. Stillbirth and early neonatal mortality in rural Central Africa. Int J Gynaecol Obstet. (2009) 105:112–7. doi: 10.1016/j.ijgo.2008.12.012
50. Gogia, S, and HJJOP, S. Home-based neonatal care by community health workers for preventing mortality in neonates in low-and middle-income countries: a systematic review. J Perinatol. (2016) 36:S55–73. doi: 10.1038/jp.2016.33
51. Saleem, S, Tikmani, SS, McClure, EM, Moore, JL, Azam, SI, Dhaded, SM, et al. Trends and determinants of stillbirth in developing countries: results from the global Network’s population-based birth registry. Reprod Health. (2018) 15:100–30. doi: 10.1186/s12978-018-0526-3
Keywords: antenatal care, low birth weight, Africa, public health, institutional births
Citation: Engdaw GT, Tesfaye AH, Feleke M, Negash A, Yeshiwas A, Addis W, Angaw DA and Engidaw MT (2023) Effect of antenatal care on low birth weight: a systematic review and meta-analysis in Africa, 2022. Front. Public Health. 11:1158809. doi: 10.3389/fpubh.2023.1158809
Edited by:
Amir Almasi-Hashiani, Arak University of Medical Sciences, IranReviewed by:
Richard Derman, Thomas Jefferson University, United StatesJakyoung Lee, Ajou University, Republic of Korea
Copyright © 2023 Engdaw, Tesfaye, Feleke, Negash, Yeshiwas, Addis, Angaw and Engidaw. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Garedew Tadege Engdaw, Z2FyZWRld3RhZGkyN0BnbWFpbC5jb20=
†ORCID: Garedew Tadege Engdaw, https://orcid.org/0000-0002-7311-3079
 Garedew Tadege Engdaw1*†
Garedew Tadege Engdaw1*†