- 1Biomedical Sciences Department, School of Pharmacy, Lebanese International, University, Beirut, Lebanon
- 2INSPECT-LB (Institut National de Santé Publique, d’Épidémiologie Clinique et de Toxicologie-Liban), Beirut, Lebanon
- 3Academic Quality Department, QU Health, Qatar University, Doha, Qatar
- 4Pharmaceutical Sciences Department, School of Pharmacy, Lebanese International, University, Beirut, Lebanon
- 5Pharmacy Practice Department, School of Pharmacy, Lebanese International, University, Beirut, Lebanon
- 6School of Education, Lebanese International University, Beirut, Lebanon
- 7Population Health Division, Gilbert and Rose-Marie Chagoury School of Medicine, Lebanese American University, Byblos, Lebanon
- 8Alice Ramez Chagoury School of Nursing, Lebanese American University, Byblos, Lebanon
- 9Lebanese Order of Pharmacists, Beirut, Lebanon
- 10Department of Epidemiology and Population Health, American University of Beirut, Beirut, Lebanon
- 11UMR U955 INSERM, Institut Mondor de Recherche Biomédicale, Université Paris-Est, Créteil, France
- 12École Doctorale Sciences de la Vie et de la Santé, Université Paris-Est, Créteil, France
Introduction: The COVID-19 pandemic has induced a global mental health crisis with variable consequences. This study aimed to assess the psychological impact of COVID-19 regarding anxiety, insomnia, depression, and response to trauma on pharmacists in Lebanon during COVID-19, and to identify factors contributing to psychological distress.
Methods: This was a cross-sectional study among pharmacists that involved the use of the 7-item Generalized Anxiety Disorder (GAD-7), 7-item Insomnia Severity Index (ISI), Patient Health Questionnaire 9-item depression module (PHQ-9), and Impact of Event Scale revised (IES-R) subscales. Descriptive statistical analyses were performed to determine the study distribution. The associations between the scores and the participants’ characteristics were assessed using the Chi-square test. Four binary logistic regression models were used to evaluate the association between the scores and the potential confounders, followed by four multivariable logistic regressions. An alpha of 0.05 was used to determine statistical significance.
Results: Participants comprised 311 pharmacists from all Lebanese districts, of whom 251 (80.7%) were females and 181 (58.2%) aged between 26 and 35 years. The majority of the participants were community pharmacists (n = 178, 57.2%). A considerable proportion of participants had symptoms of anxiety (n = 128, 41.2%), insomnia (n = 64, 20.6%), depression (n = 157, 50.5%), and subjective stress (n = 227, 78.8%). Higher anxiety (aOR: 1.73, 95% CI: 1.08; 2.78, p-value: 0.02), higher depression (aOR: 3.06, 95% CI: 1.73; 5.39, p-value: 0.001), and higher stress (aOR: 1.86, 95 percent CI: 1.11; 3.14, p-value: 0.02) scores were significantly associated with pharmacists who reported that their work involves contact with infected/suspected COVID-19 patients. Interestingly, pharmacists who expressed concern about contracting COVID-19 infection had significantly higher anxiety (aOR: 2.35, 95% CI: 1.40; 3.94, p-value: 0.001) and higher depression scores (aOR: 2.64, 95% CI: 1.49; 4.67, p-value: 0.001) respectively.
Conclusion: The preliminary results from pharmacists in Lebanon reflect increase in stress, burden, and frustration felt by pharmacists, creating a negative impact on their mental health and well-being during the global pandemic. As frontline healthcare workers, the role of pharmacists in the community should not be overlooked, and their mental health should be well investigated.
Introduction
On December 31, 2019, the first case of coronavirus disease 2019 (COVID-19), a severe infectious respiratory disease brought on by a new coronavirus (SARS-CoV-2), was reported in Wuhan, China (1). On March 11, 2020, the World Health Organization (WHO) formally designated it a global pandemic (2). Person-to-person transmission is via droplets released through coughing, sneezing, speaking, and contact with contaminated surfaces (3). In addition to raising concerns about global public health, COVID-19 also caused extraordinary disruptions to daily lives, with strong recommendations for social withdrawal, self-isolation, work interruptions, educational disruption, and travel limitations (4–7).
The COVID-19 pandemic has had detrimental psychological effects on healthcare workers who are on the front lines of treating infected patients (8). Personal and professional factors have contributed to fear, burnout, anxiety, depression, mental exhaustion, and insomnia among this population (4, 7). Some of the personal factors include a sense of fear, anxiety, and uncertainty, and a desire for appreciation, respect, and support, while work-related factors include unfamiliar responsibilities, insufficient resources, a lack of knowledge with personal protective equipment (PPE), and increased workloads (9).
Among the frontline healthcare workers are the pharmacists, who have been devotedly delivering essential services throughout the pandemic (10), and this has resulted in having them increasingly acknowledged as vital service providers around the world (11). This recognition stems from their ability to demonstrate that they are a dynamic workforce dedicated to public health and who can competently deliver a variety of services and products to meet current societal needs (12). During the lockdown, pharmacists were the most accessible healthcare members with whom patients could interact (13–16). They have actively participated in medical activities related to COVID-19 through utilizing their pharmacological expertise in screening, medication dispensing, as well as closely collaborating with other healthcare workers and governmental organizations to discover solutions and break down barriers (17, 18). Besides, they have played an essential role in community settings by raising public awareness related to health issues (19). As such, pharmacists are definitely frontline healthcare workers who are particularly positioned to provide care to a substantial segment of the population and have a high potential to contribute to the pandemic response.
While lockdown and staying at home regulations lingered, pharmacists continued working despite the numerous challenges. Hence, alongside this serious infectious public health event, the mental burden of pharmacists may be exacerbated by the rising number of confirmed and suspected cases, heavy workloads, negative emotions, exhaustion from PPE use, lack of certain medications, fear of spreading the disease to family, friends, and coworkers, as well as feelings of inadequate support (20, 21).
Due to the challenging conditions brought on by COVID-19, it has become crucial to evaluate the mental health of pharmacists who have been exposed to a variety of stress-related factors that have increased their stress levels, anxiety, depressive symptoms, and exacerbations of pre-existing mental disease (7, 20, 22, 23). In Lebanon, the COVID-19 pandemic, along with a severe economic downturn, has severely impacted an already struggling profession (24). The determination of the psychological impact of the COVID-19 regarding anxiety, insomnia, depression, and response to trauma on pharmacists in Lebanon during COVID-19, and the identification of characteristics that contribute to psychological distress, are warranted (25). Consequently, this study aimed to assess the psychological impact of COVID-19 regarding anxiety, insomnia, depression, and response to trauma on pharmacists in Lebanon during COVID-19, and to identify factors contributing to psychological distress.
Methods
Study design, setting, and participants
This was a cross-sectional study that involved pharmacists from all over Lebanon. Data were collected via an anonymous online questionnaire using Google Forms, over a period of 2 months during the COVID-19 outbreak from May 8 to July 5, 2020. A snowball sampling technique was used to collect data across the eight governorates (Mohafazat) of Lebanon and to target only Lebanese pharmacists who work in community, hospital, drug company, academic, and other settings.
Sample size calculation
The minimal sample size was calculated using CDC’s Epi-Info for population surveys. The population size was set 13,000, which is the number of pharmacists in Lebanon. The expected frequency was set at 75%, which is the previously reported frequency of community pharmacists who are familiar with the recommendations of the Lebanese Order of Pharmacists (26). Consequently, a minimum sample of 282 pharmacists was required to produce a 95% confidence level and an acceptable margin of error of 5%.
Data collection
The online questionnaire was developed in English language and piloted with 10 pharmacists to check for content and clarity. Amendments were then done and the final questionnaire was distributed forwarding its link to all pharmacists working in Lebanon. The study scope and purpose were explained at the beginning of the questionnaire, confirming that the survey was strictly confidential and conducted in compliance with the relevant data protection law. Participants were informed that their participation in the study is voluntary and they were assured that their responses would remain anonymous and confidential. They were requested to indicate through a mandatory selection box before beginning the survey that this was their first time doing so (ensuring 100% consent rate and preventing duplicate replies), and completion of the questionnaire until the end was considered as informed consent to participate.
Ethical approval
The Ethics and Research Committee of the School of Pharmacy at the Lebanese International approved the study protocol (protocol number: 2020RC-042-LIUSOP) and followed the Declaration of Helsinki Ethical Principles for Medical Research Involving Human Subjects. The procedures pertaining to the anonymity of the data and the information provided to the volunteers were anticipated and the nature of the elements to be collected did not carry the risk of disclosing weaknesses unknown to the volunteer and thereby causing unpredictable reactions.
Measurement tools
The questionnaire consisted of three sections. The first and second sections were concerned with the participants’ sociodemographic data and the pharmacists’ knowledge and concerns about COVID-19. In the following section, four validated scales that serve the purpose of the study in measuring the mental health status of the participants during the COVID-19 pandemic have been included. The 7-item Generalized Anxiety Disorder (GAD-7), 7-item Insomnia Severity Index (ISI), Patient Health Questionnaire 9-item depression module (PHQ-9), and Impact of Event Scale revised (IES-R) have been used to assess the psychological impact. The questionnaires were administered in English language because it is understood by the vast majority of Lebanese pharmacists who speak English. In fact, the OPL has adopted English as the language for their continuing education.
The 7-item insomnia severity index
The 7-ISI is a self-reporting instrument composed of 7 items that was used to assess the nature, severity, and impact of insomnia. Each item is rated on a 5-point Likert scale from 0 to 4 with a total score ranging from 0 to 28. The total score was calculated and interpreted as follows: normal with no insomnia (0–7), subthreshold (8–14), moderate (15–21), and severe (22–28) insomnia (27, 28). The Cronbach’s alpha among our sample was 0.886.
The patient health questionnaire 9-item depression module
Participants’ depressive symptoms during the COVID-19 pandemic were assessed using PHQ-9, which scores each of the nine Diagnostic and Statistical Manual of Mental Disorders, 4th edition (DSM-IV) criteria of depression on a scale ranging from “0″ (not at all) to “3″ (nearly every day). The total sum of the responses ranging from 0 to 27 suggests varying levels of depression: no/minimal depression (0–4), mild (5–9), moderate (10–14), moderately severe (15–19), and severe (20–27) (29). The Cronbach’s alpha among our sample was 0.868.
The 7-item generalized anxiety disorder scale
This 7-item self-rated tool was used to measure participants’ anxiety symptoms over the previous 2 weeks. Each item is assigned a score from “0″ (not at all) to “3″ (nearly every day). The total score of GAD-7 ranges from 0 to 21 and is grouped into four categories as follows: no/minimal anxiety (0–4), mild (5–9), moderate (10–14), and severe (15–21) (30). The Cronbach’s alpha among our sample was 0.930.
Impact of event scale revised
The IES-R has been utilized as a self-report measure to assess the level of symptomatic response to specific traumatic events as the COVID-19 pandemic as it was manifested in the previous 7 days. It consisted of a brief self-administered 22-item questionnaire, and for response, a five-point Likert scale was used. Scale scoring of IES-R included a total score (ranging from 0 to 88) that indicated the global subjective stress regarding COVID-19. Higher levels of distress are reflected by higher total (or subscale) scores. The total IES-R score was divided into: absence of PTSD in those with little or no symptoms (0–23), being at risk with several symptoms (24–32), and probable PTSD (≥33) (31). The Cronbach’s alpha among our sample was 0.960.
Statistical analysis
Descriptive statistics were performed to represent the participants’ characteristics, COVID-19 related information, the GAD-7 anxiety score, ISI insomnia severity score, PHQ-9 depression severity score, and IES-R global subjective stress score, and were expressed as percentages.
The GAD-7 anxiety score was expressed as “moderate and severe” versus “minimum and mild”; the insomnia severity index as “clinical insomnia (moderate and severe)” versus “no clinically significant insomnia and subthreshold insomnia”; the depression score as “moderate, moderately severe, and severe depression” versus “minimal and mild depression”; and the IES-R score as “little or no symptoms” versus “several symptoms” and “probable PTSD.” The bivariate associations between the scores and the participants’ characteristics were assessed using the Chi-square test for all variables or Fisher exact test (when >20% of the expected cell count were less than 5). Thereafter, four binary logistic regression models using the forward method were performed to preclude potential confounding. The dependent variables were the anxiety, insomnia, depression, and IES-R scores in the first, second, third, and fourth models, respectively. The participants’ characteristics having a p-value of less than 0.05 in the bivariate analysis were included as independent variables to account for them as potential confounding. The models were tested for adequacy in all the analysis. An alpha of 0.05 was used to determine statistical significance. All analyses were performed using the IBM’s Statistical Package for the Social Sciences (SPSS) version 22.0 (IBM, Inc., Chicago, IL).
Results
Demographic data of Lebanese pharmacists
A total of 311 Lebanese pharmacists participated in the study whose sociodemographic characteristics are shown in Table 1. The analyzed sample included participants from all Lebanese districts, of whom 251 (80.7%) were females and 181 (58.2%) aged between 26 and 35 years. As for the professional field, 57.2% work in community pharmacy, 6.1% work as hospital/clinical pharmacists, 14.8% in drug companies, 6.8% work in academia, 1% work in regulatory departments of pharmaceutical companies, and 14.1% in other pharmaceutical fields. Educational variables showed that 56.3% had a BPHARM degree and 43.7% had a BPHARM and postgraduate degrees (MS/PharmD/PhD). The majority (n = 112, 36%) belonged to the middle socioeconomic class with an average family income of more than 4,000,000 LBP per month.
Lifestyle changes during COVID-19 time
More than half of the participants stated that they drank at least 2 liters of water per day and were physically active during quarantine. However, the lifestyle of Lebanese pharmacists was affected during the pandemic, where alcohol intake was increased by 20% among alcohol consumers (51 [16.4%]). As for smoking, 23 (7.4%) were cigarette while 85 (27.3%) were waterpipe smokers respectively, and more than half of those reported increased smoking during the COVID-19 time. Caffeinated beverages were consumed by 271 (87.1%) and less than half (38%) increased their consumption during COVID-19. Energy drinks consumption was reported by 30 (9.6%), of whom 33.3% also had raised consumption during the pandemic, while alcohol consumption was reported by 51 (16.4%) and almost 20% increased their consumption during COVID-19.
Health and concerns about COVID-19, and results of the four mental health scales
Around half of the Lebanese pharmacists (n = 157, 50.5%) reported that they were in direct contact with infected/suspected COVID-19 patients during the pandemic period and 85 (27.3%) reported being frontline workers. Only 40 (12.9%) reported a history of chronic disease. The majority (n = 270, 86.8%) reported getting sufficient protection against COVID-19 infection during work and 196 (63%) reported that they were concerned about contracting COVID-19. A considerable proportion of participants had symptoms of anxiety (n = 128, 41.2%), insomnia (n = 64, 20.6%), depression (n = 157, 50.5%), and subjective stress (n = 227, 78.8%). Further details are shown in Table 2.
Scores of measurement and association of possible influence factors with anxiety, insomnia, depression, and stress during COVID-19 pandemic
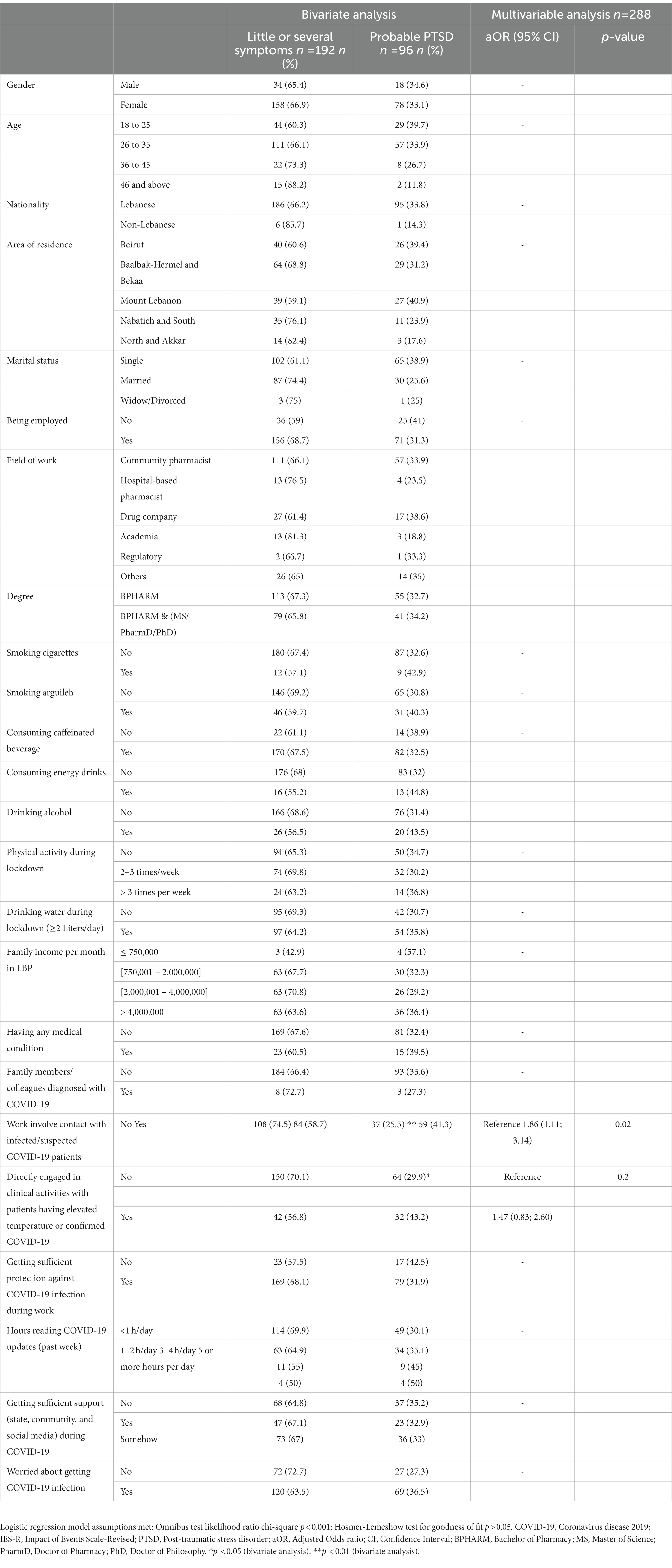
Numerous factors were shown to be significantly associated to anxiety, insomnia, depression, and stress among the pharmacists in Lebanon in the bivariate analysis. Tables 3–6 show the association of possible influence factors with GAD, insomnia, depression, and stress during COVID-19 pandemic.
Anxiety
Being married was significantly associated with lower anxiety levels as compared to single status (aOR: 0.51, 95% CI: 0.31; 0.83, p-value: 0.007). Interestingly, higher anxiety scores were significantly associated with pharmacists who expressed concern about contracting COVID-19 infection (aOR: 2.35, 95% CI: 1.40; 3.94, p-value: 0.001) and those who reported that their work involves contact with infected/suspected COVID-19 patients (aOR: 1.73, 95% CI: 1.08; 2.78, p-value: 0.02) respectively.
Insomnia
Higher rates of insomnia were associated with the presence of chronic medical disorders. Having a medical condition was significantly associated with greater scores for insomnia compared to those who did not have co-morbidities (aOR: 2.99, 95% CI: 1.45; 6.19, p-value: 0.003). On the other hand, being employed was significantly associated with lower levels of insomnia (aOR: 0.42, 95% CI: 0.22; 0.78, p-value: 0.006).
Depression
Interestingly, higher depression scores were significantly associated with pharmacists who expressed concern about contracting COVID-19 infection (aOR: 2.64, 95% CI: 1.49; 4.67, p-value: 0.001) and those who reported that their work involves contact with infected/suspected COVID-19 patients (aOR: 3.06, 95% CI: 1.73; 5.39, p-value: 0.001). Regarding variations to lifestyle, consuming energy drinks (aOR: 5.37, 95% CI: 1.81; 15.9, p-value: 0.002) was found to be significantly associated with higher depression scores. However, drinking more than 2 liters of water per day during lockdown (aOR: 0.52, 95% CI: 0.31; 0.88, p-value: 0.02) and receiving appropriate COVID-19 infection prevention at work (aOR: 0.28, 95% CI: 0.12; 0.64, p-value: 0.003) were protective factors towards depression. Similarly, being employed was significantly associated with lower depression scores (aOR: 0.35, 95% CI: 0.18; 0.69, p-value: 0.003).
Stress
Notably, pharmacists who stated that their work involves contact with COVID-19 patients who are infected or suspected of being infected, were substantially more likely to report greater stress levels (aOR: 1.86, 95% CI: 1.11; 3.14, p-value: 0.02).
Discussion
This study is among the very few ones addressing mental health in Lebanon during COVID-19 pandemic, and is the first to explore the effect of the pandemic on mental health of pharmacists. Most of the sociodemographic characteristics of the analyzed sample were aligned with previously published reports about pharmacists in Lebanon (32). Even though there aren’t many studies on this subject in this particular population, it was deemed suitable to compare and discuss the findings based on research on healthcare workers as well as general population surveys.
High levels of stress, insomnia, anxiety, and depression were observed among Lebanese pharmacists. A number of variables including poor pharmacists’ wages, which are typically not commensurate with their skills, as well as internal political upheaval and high inflation, could be to blame (33, 34). In fact, on November 19, 2020, Lebanon was ranked as the second-highest nation in terms of global inflation (Lebanon: 365%), only after Venezuela (2,133%). The pandemic, which exacerbated the burden on pharmacists’ mental health, made this situation much worse. This may eventually continue to reduce pharmacists’ productivity, performance, and optimism (34). The anxiety, insomnia, depression, and stress findings in this population are also in conformity with reported high prevalence among healthcare workers according to results of a systematic review and meta-analysis published in 2021 (35).
Our findings showed that throughout the pandemic, there was an increase in the respondents’ unhealthy behaviors. The rates of alcohol consumption, smoking, and caffeinated and energy drinks were increased and this was earlier reported among the Lebanese population during the pandemic (36), probably as a strategy to react to stressful situations, and has been reported elsewhere (37, 38). The increase in smoking and drinking alcohol during stressful experiences is actually consistent with the “coping effect” of tobacco versus psychological stress (39, 40).
Lower anxiety was noted among married individuals, which is consistent with a previous study by Lawal and colleagues, which reported better coping among married females (41). However, Tan and Colleagues reported that single people experience less of the negative effects of events, stress, anxiety, and depression than divorced, separated, or widowed individuals (42). On the other hand, those with chronic medical diseases were shown to experience high levels of mental health distress. This was in line with the findings of other studies that have documented COVID-19 fatalities in patients with comorbidities (43).
The current study is in line with an extensive body of evidence which indicated that consumption of energy drinks was increased (36, 44) and significantly associated with depression symptoms (45). Notable preventive factors against depression included appropriate COVID-19 protection at work and good hydration. To maintain better immune systems and reduce the risk of chronic illnesses and infectious diseases, drinking water is essential (46). Lack of access to PPE has been directly linked to psychological distress and depressive symptoms (47), although having enough PPE might lessen the potential negative effects of COVID exposure on mental health (48). Healthcare workers would feel safer with PPE as this relates to their own health, that of their patients, and that of their loved ones (48). Similarly, lower insomnia and depression scores were noted among employed pharmacists. This appears logical in a country with collapsed economy and the need for relative financial security through having a job.
As previously documented in a recent study among Portuguese pharmacists, increased anxiety and stress scores were reported with pharmacists who claimed that their profession entails contact with infected/suspected COVID-19 patients (49). Furthermore, anxiety and depression scores were much higher in pharmacists who showed fear about developing COVID-19 infection, possibly highlighting the severe and wide-ranging psychological effects that the pandemic can have on daily life (50). The increase in the number of patients seen, the amount of triage done, the bulk of COVID-19 information delivered, the vast medication shortages, and the amount of workplace harassment, may have all affected the mental health of Lebanese pharmacists in the studied sample.
Limitations
This study, which was based on an electronic survey, has several limitations. First of all, it is difficult to determine the temporal link between exposure and outcomes from the cross-sectional design of the study. Second, the snowball sampling technique may have been associated with a possible risk of selection bias, which may affect the generalizability of the current findings. However, it is believed that this risk is minimized as our sample included pharmacists from districts all over Lebanon, which can provide some generalizability to the current findings. Moreover, although a web-based survey is one of the most efficient ways to obtain quick data, especially if social interactions are prohibited (i.e., lockdown), it may be associated with another possible risk of selection bias as it may have excluded senior pharmacists with lesser digital literacy. Further research is still recommended to include a broader range of pharmacists and evaluate their mental health amid pandemics as COVID-19 and influenzae to confirm the current findings. However, recall bias may still arise as a consequence of self-reporting assessment methods. Nevertheless, it is believed that this bias is minimized as the survey utilized validated scales with good internal consistency and using the English language that is well understood by all Lebanese pharmacists. Finally, the current study applied generic validated scales rather than COVID-19 specific scales to assess mental health. Further studies are recommended to minimize the current biases.
Practical implications and future directions
The preliminary results from pharmacists in Lebanon reflect increase in stress, burden, and frustration felt by pharmacists, creating a negative impact on their mental health and well-being in the wake of the global pandemic. As frontline healthcare workers, the role of pharmacists in the community should not be overlooked, and their mental health should be well investigated. As we move towards a post-pandemic world, pertinent information about the mental health of pharmacists and associated factors should come up with essential recommendations on how to assist pharmacists in coping with anxiety, insomnia, depression, and stress occurring as collateral effects of COVID-19. With pharmacists being an integral segment of the healthcare system, their mental health and well-being is vital for proper health services. Accordingly, the impact of this study shall relate to pharmacists’ community role, and should help to purposefully interpret their ability to effectively serve their community.
Conclusion
During the COVID-19 pandemic, pharmacists played a crucial role in providing treatment on the front lines, but the increasing demand for their services also led to changes in their mental health. Throughout the pandemic, pharmacists have remained essential to the efficient provision of healthcare. The findings indicated that the COVID-19 pandemic and the ensuing lockdown had a significant negative influence on the mental health of Lebanese pharmacists. Therefore, it is as important for pharmacy professionals to put their own mental health first as it is for them to assist their patients. They must take the time to assess their own mental health for symptoms of burnout and general psychological strain in order to continue providing the best care for patients. It is important to keep in mind that stress is a typical response to a global infectious disease pandemic, however, it is crucial to prepare for stress and take the necessary actions to reduce its negative effects on the body and mind. A well-equipped workforce may be maintained by efforts towards a regular schedule, engaging in fun activities, asking for assistance from coworkers and family, and creating stress-reduction techniques. To make sure that enough resources and assistance are being offered, pharmacy managers should maintain frequent and regular communication with their staff. In light of the ongoing challenges brought on by COVID-19, it is imperative to treat the mental health of healthcare workers. The development of guidelines and solutions to enhance the safety of pharmacists and other healthcare workers during future pandemics and upcoming global outbreaks should be a top priority for pharmacy organizations.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The Ethics and Research Committee of the School of Pharmacy at the Lebanese International approved the study protocol (protocol number: 2020RC-042- LIUSOP) and followed the Declaration of Helsinki Ethical Principles for Medical Research Involving Human Subjects. The participants provided their written informed consent to participate in this study.
Author contributions
JS and DH: study conception and design. FSa, EB, and FSaa: acquisition of data. ZA, JS, MA, and FSaa: analysis and interpretation of results. MD, SY, and NM: investigation. MC, DH, and ZA: methodology. JS, SY, and DH: project administration. SY and JS: resources. ZA: software. DH and MA: visualization. JS, DH, and SY: writing original manuscript draft. SY, MR, DH, FSa, and MA: revision and editing it critically for important intellectual content. FSa and DH: validation. MR: supervision. All authors contributed to the article and approved the submitted version.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Zhou, P, Yang, XL, Wang, XG, Hu, B, Zhang, L, Zhang, W, et al. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. (2020) 579:270–3. doi: 10.1038/s41586-020-2012-7
2. Coronavirus Disease (COVID-19) (2022). Situation Reports [Internet]. Available at: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports [Accessed December 8, 2022].
3. Zhou, F, Yu, T, Du, R, Fan, G, Liu, Y, Liu, Z, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet Lond Engl. (2020) 395:1054–62. doi: 10.1016/S0140-6736(20)30566-3
4. Hall, H. The effect of the COVID-19 pandemic on healthcare workers’ mental health. JAAPA. (2020) 33:45–8. doi: 10.1097/01.JAA.0000669772.78848.8c
5. Sakr, F, Fahs, I, Dimassi, A, Younes, S, Mourad, N, Safwan, J, et al. Experiential pharmacy education in trying times: lessons learned from the COVID-19 pandemic. Pharm Educ. (2022) 22:823–34. doi: 10.46542/pe.2022.221.823834
6. Safwan, J, Cherfan, M, Dabbous, M, Hammoudi, D, Akiki, Z, Saade, F, et al. Faculty perceptions on online education in a school of pharmacy during the COVID-19 pandemic. Pharm Educ. (2022) 22:450–7. doi: 10.46542/pe.2022.221.450457
7. Luo, M, Guo, L, Yu, M, Jiang, W, and Wang, H. The psychological and mental impact of coronavirus disease 2019 (COVID-19) on medical staff and general public – a systematic review and meta-analysis. Psychiatry Res. (2020) 1:113190. doi: 10.1016/j.psychres.2020.113190
8. Banerjee, D, and Rai, M. Social isolation in Covid-19: the impact of loneliness. Int J Soc Psychiatry. (2020) 66:525–7. doi: 10.1177/0020764020922269
9. Lai, J, Ma, S, Wang, Y, Cai, Z, Hu, J, Wei, N, et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw Open. (2020) 3:e203976. doi: 10.1001/jamanetworkopen.2020.3976
10. Bukhari, N, Rasheed, H, Nayyer, B, and Babar, ZUD. Pharmacists at the frontline beating the COVID-19 pandemic. J Pharm Policy Pract. (2020) 13:8. doi: 10.1186/s40545-020-00210-w
11. Johnston, K, O’Reilly, CL, Cooper, G, and Mitchell, I. The burden of COVID-19 on pharmacists. J Am Pharm Assoc. (2021) 61:e61–4. doi: 10.1016/j.japh.2020.10.013
12. Al-Quteimat, OM, and Amer, AM. SARS-CoV-2 outbreak: how can pharmacists help? Res Soc Adm Pharm. (2021) 17:480–2. doi: 10.1016/j.sapharm.2020.03.018
13. Sabra, R, Safwan, J, Dabbous, M, Rida, A, Malaeb, D, Akel, M, et al. Assessment of knowledge, attitude and practice of Lebanese pharmacists in providing patient counseling on urinary tract infection and its treatment. Pharm Pract. (2022) 20:01–10. doi: 10.18549/PharmPract.2022.2.2653
14. Chahine, B, Cherfane, M, Sakr, F, Safwan, J, Dabbous, M, Akel, M, et al. Community pharmacists’ perceptions and role in the management of common dermatological problems in Lebanon: a cross-sectional study. Int J Pharm Pract. (2021) 29:573–9. doi: 10.1093/ijpp/riab056
15. Dabbous, MK, Moustafa, SM, Sakr, FR, Akel, MG, Safwan, JH, Cherfan, MM, et al. Knowledge, attitude and practice of Lebanese community pharmacists with regard to self-management of low back pain. Trop J Pharm Res. (2020) 19:873–8. doi: 10.4314/tjpr.v19i4.28
16. Sakr, F, Akiki, Z, Dabbous, M, Salameh, P, and Akel, M. The role of pharmacists in providing immunization to the general population: are Lebanese pharmacists ready for this role? Pharm Pract. (2022) 19:01–8. doi: 10.18549/PharmPract.2021.4.2565
17. Elbeddini, A, Prabaharan, T, Almasalkhi, S, and Tran, C. Pharmacists and COVID-19. J Pharm Policy Pract. (2020) 13:36. doi: 10.1186/s40545-020-00241-3
18. Ung, COL. Community pharmacist in public health emergencies: quick to action against the coronavirus 2019-nCoV outbreak. Res Soc Adm Pharm. (2020) 16:583–6. doi: 10.1016/j.sapharm.2020.02.003
19. Basheti, IA, Nassar, R, Barakat, M, Alqudah, R, Abufarha, R, Mukattash, TL, et al. Pharmacists’ readiness to deal with the coronavirus pandemic: assessing awareness and perception of roles. Res Soc Adm Pharm. (2021) 17:514–22. doi: 10.1016/j.sapharm.2020.04.020
20. Elbeddini, A, Wen, CX, Tayefehchamani, Y, and To, A. Mental health issues impacting pharmacists during COVID-19. J Pharm Policy Pract. (2020) 13:46. doi: 10.1186/s40545-020-00252-0
21. Chen, Q, Liang, M, Li, Y, Guo, J, Fei, D, Wang, L, et al. Mental health care for medical staff in China during the COVID-19 outbreak. Lancet Psychiatry. (2020) 7:e15–6. doi: 10.1016/S2215-0366(20)30078-X
22. Alameddine, M, Bou-Karroum, K, and Hijazi, MA. A national study on the resilience of community pharmacists in Lebanon: a cross-sectional survey. J Pharm Policy Pract. (2022) 15:8. doi: 10.1186/s40545-022-00406-2
23. Brooks, SK, Webster, RK, Smith, LE, Woodland, L, Wessely, S, Greenberg, N, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. (2020) 395:912–20. doi: 10.1016/S0140-6736(20)30460-8
24. Alameddine, M, Bou-Karroum, K, Kassas, S, and Hijazi, MA. A profession in danger: stakeholders’ perspectives on supporting the pharmacy profession in Lebanon. PLoS One. (2020) 15:e0242213. doi: 10.1371/journal.pone.0242213
25. Sakr, F, Haddad, C, Zeenny, RM, Sacre, H, Akel, M, Iskandar, K, et al. Work ethics and ethical attitudes among healthcare professionals: the role of leadership skills in determining ethics construct and professional behaviors. Healthcare. (2022) 10:1399. doi: 10.3390/healthcare10081399
26. Order of Pharmacist of Lebanon (2022). Drugs [Internet]. Available at: https://opl.org.lb/newsdetails.php?newsId=%20165 [Accessed December 7, 2022].
27. Morin, CM, Belleville, G, Bélanger, L, and Ivers, H. The insomnia severity index: psychometric indicators to detect insomnia cases and evaluate treatment response. Sleep. (2011) 34:601–8. doi: 10.1093/sleep/34.5.601
28. Bastien, CH, Vallières, A, and Morin, CM. Validation of the insomnia severity index as an outcome measure for insomnia research. Sleep Med. (2001) 2:297–307. doi: 10.1016/S1389-9457(00)00065-4
29. Pinto-Meza, A, Serrano-Blanco, A, Peñarrubia, MT, Blanco, E, and Haro, JM. Assessing depression in primary care with the PHQ-9: can it be carried out over the telephone? J Gen Intern Med. (2005) 20:738–42. doi: 10.1111/j.1525-1497.2005.0144.x
30. Ruiz, MA, Zamorano, E, García-Campayo, J, Pardo, A, Freire, O, and Rejas, J. Validity of the GAD-7 scale as an outcome measure of disability in patients with generalized anxiety disorders in primary care. J Affect Disord. (2011) 128:277–86. doi: 10.1016/j.jad.2010.07.010
31. Weiss, DS. (2022). Impact of Events Scale - Revised (IES-R): (567532010-001) [Internet]. American Psychological Association. Available at: http://www.crossref.org/deleted_DOI.html [Accessed July 17, 2022].
32. Hallit, S, Sacre, H, Hajj, A, Sili, G, Zeenny, RM, and Salameh, P. Projecting the future size of the Lebanese pharmacy workforce: forecasts until the year 2050. Int J Pharm Pract. (2019) 27:582–8. doi: 10.1111/ijpp.12564
33. Lebanon Inflation Rate 2022 Data - 2008-2021 Historical - July Forecast [Internet]. Available at: https://tradingeconomics.com/lebanon/inflation-cpi [Accessed July 19, 2022].
34. Tase, P. (2020). Prof. Steve Hanke on Lebanon’s current economic policies – interview [internet]. Eurasia Review. Available at: https://www.eurasiareview.com/03102020-prof-steve-hanke-on-lebanons-current-economic-policies-interview/ [Accessed July 19, 2022].
35. Hao, Q, Wang, D, Xie, M, Tang, Y, Dou, Y, Zhu, L, et al. Prevalence and risk factors of mental health problems among healthcare workers during the COVID-19 pandemic: a systematic review and meta-analysis. Front Psychiatry. (2021) 12:567381. doi: 10.3389/fpsyt.2021.567381
36. Younes, S, Safwan, J, Rahal, M, Hammoudi, D, Akiki, Z, and Akel, M. (2021). Effect of COVID-19 on mental health among the young population in Lebanon. L’Encéphale [Internet]. Available at: https://www.sciencedirect.com/science/article/pii/S0013700621001792 [Accessed July 19, 2022].
37. Kosendiak, A, Król, M, Ściskalska, M, and Kepinska, M. The changes in stress coping, alcohol use, cigarette smoking and physical activity during COVID-19 related lockdown in medical students in Poland. Int J Environ Res Public Health. (2021) 19:302. doi: 10.3390/ijerph19010302
38. Sidor, A, and Rzymski, P. Dietary choices and habits during COVID-19 lockdown: experience from Poland. Nutrients. (2020) 12:1657. doi: 10.3390/nu12061657
39. Assi, M, Onaissy, N, Sakr, F, Cherfan, M, Akiki, Z, Dabbous, M, et al. Smoking habits, attitudes and determinants among university aged population: comparison of pharmacy and non-pharmacy students from a private university in Lebanon. Pharm Educ. (2022) 22:523–32. doi: 10.46542/pe.2022.221.523532
40. Akel, M, Sakr, F, Fahs, I, Dimassi, A, Dabbous, M, Ehlinger, V, et al. Smoking behavior among adolescents: the Lebanese experience with cigarette smoking and Waterpipe use. Int J Environ Res Public Health. (2022) 19:5679. doi: 10.3390/ijerph19095679
41. Lawal, AM, Alhassan, EO, Mogaji, HO, Odoh, IM, and Essien, EA. Differential effect of gender, marital status, religion, ethnicity, education and employment status on mental health during COVID-19 lockdown in Nigeria. Psychol Health Med. (2022) 27:1–12. doi: 10.1080/13548506.2020.1865548
42. Tan, W, Hao, F, McIntyre, RS, Jiang, L, Jiang, X, Zhang, L, et al. Is returning to work during the COVID-19 pandemic stressful? A study on immediate mental health status and psychoneuroimmunity prevention measures of Chinese workforce. Brain Behav Immun. (2020) 87:84–92. doi: 10.1016/j.bbi.2020.04.055
43. Sayeed, A, Kundu, S, Al Banna, MH, Christopher, E, Hasan, MT, Begum, MR, et al. Mental health outcomes of adults with comorbidity and chronic diseases during the COVID-19 pandemic: a matched case-control study. Psychiatr Danub. (2020) 32:491–8. doi: 10.24869/psyd.2020.491
44. Mattioli, AV, and Sabatini, S. Changes in energy drink consumption during the COVID-19 quarantine. Clin Nutr Espen. (2021) 45:516–7. doi: 10.1016/j.clnesp.2021.06.034
45. Alamrawy, RG, Fadl, N, and Khaled, A. Psychiatric morbidity and dietary habits during COVID-19 pandemic: a cross-sectional study among Egyptian youth (14–24 years). Middle East Curr Psychiatry Ain Shams Univ. (2021) 28:6. doi: 10.1186/s43045-021-00085-w
46. Nutrition (2022). Nutrition advice for adults during the COVID-19 outbreak [Internet]. World Health Organization - Regional Office for the Eastern Mediterranean. Available at: http://www.emro.who.int/nutrition/covid-19/nutrition-advice-for-adults-during-the-covid-19-outbreak.html [Accessed November 21, 2022].
47. Mediavilla, R, Fernández-Jiménez, E, Martínez-Alés, G, Moreno-Küstner, B, Martínez-Morata, I, Jaramillo, F, et al. Role of access to personal protective equipment, treatment prioritization decisions, and changes in job functions on health workers’ mental health outcomes during the initial outbreak of the COVID-19 pandemic. J Affect Disord. (2021) 1:405–9. doi: 10.1016/j.jad.2021.08.059
48. Swaminathan, R, Mukundadura, BP, and Prasad, S. Impact of enhanced personal protective equipment on the physical and mental well-being of healthcare workers during COVID-19. Postgrad Med J. (2022) 98:231–3. doi: 10.1136/postgradmedj-2020-139150
49. Dos Santos, PM, da Silva, CR, Costa, D, and Torre, C. Burnout in the pharmaceutical activity: the impact of COVID-19. Front Psychol. (2021) 12:771462. doi: 10.3389/fpsyt.2021.771462
Keywords: COVID-19, frontline, Lebanon, pharmacists, mental health
Citation: Safwan J, Hammoudi Halat D, Akel M, Younes S, Rahal M, Mourad N, Akiki Z, Cherfane M, Saade F, Bouraad E, Dabbous M and Sakr F (2023) The impact of COVID-19 on the mental health of Lebanese pharmacists: A national cross-sectional study. Front. Public Health. 11:1156840. doi: 10.3389/fpubh.2023.1156840
Edited by:
Krystyna Kowalczuk, Medical University of Bialystok, PolandReviewed by:
Seockhoon Chung, University of Ulsan College of Meidicine, Republic of KoreaCaroline Pereira, University of São Paulo, Brazil
Ruhana Che Yusof, University of Malaya, Malaysia
Copyright © 2023 Safwan, Hammoudi Halat, Akel, Younes, Rahal, Mourad, Akiki, Cherfane, Saade, Bouraad, Dabbous and Sakr. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jihan Safwan, amloYW4uc2Fmd2FuQGxpdS5lZHUubGI=
 Jihan Safwan
Jihan Safwan Dalal Hammoudi Halat
Dalal Hammoudi Halat Marwan Akel
Marwan Akel Samar Younes
Samar Younes Mohamad Rahal
Mohamad Rahal Nisreen Mourad
Nisreen Mourad Zeina Akiki2
Zeina Akiki2 Michelle Cherfane
Michelle Cherfane Faraj Saade
Faraj Saade Etwal Bouraad
Etwal Bouraad Mariam Dabbous
Mariam Dabbous Fouad Sakr
Fouad Sakr