
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health, 09 May 2023
Sec. Infectious Diseases: Epidemiology and Prevention
Volume 11 - 2023 | https://doi.org/10.3389/fpubh.2023.1153136
This article is part of the Research TopicRe-emergence of neglected tropical diseases amid the COVID-19 pandemic: Epidemiology, transmission, mitigation strategies, and recent advances in chemotherapy and vaccinesView all 13 articles
 Sarya Swed1*†
Sarya Swed1*† Hidar Alibrahim1
Hidar Alibrahim1 Haidara Bohsas1
Haidara Bohsas1 Nagham Jawish2
Nagham Jawish2 Mohammed Amir Rais3
Mohammed Amir Rais3 Mohamad Nour Nasif1
Mohamad Nour Nasif1 Wael Hafez4,5
Wael Hafez4,5 Bisher Sawaf6
Bisher Sawaf6 Ahmed Abdelrahman7
Ahmed Abdelrahman7 Sherihan Fathey8
Sherihan Fathey8 Ismail Atef Ismail Ahmed Ibrahim9
Ismail Atef Ismail Ahmed Ibrahim9 Sondos Hussein Ahmad Almashaqbeh10
Sondos Hussein Ahmad Almashaqbeh10 Razan Mohammad Yousef Aljawarneh11
Razan Mohammad Yousef Aljawarneh11 Amine Rakab12
Amine Rakab12 Emad Hassan Hassan EL-Shafei13
Emad Hassan Hassan EL-Shafei13 Rene Hurlemann14,15,16
Rene Hurlemann14,15,16 Mohamed E. G. Elsayed14,17*† and Data Collection Group
Mohamed E. G. Elsayed14,17*† and Data Collection GroupBackground: The aim of this study was to explore potential healthcare workers' (HCWs) concerns about the monkeypox virus in order to create practical solutions to manage this disease.
Methods: Online cross-sectional research was conducted in 11 Arabic countries (Egypt, Saudi Arabia, Yemen, Syria, Libya, Algeria, Tunisia, Iraq, Palestine, Jordan, and Sudan) from 2 August 2022 to 28 December 2022.
Results: Approximately 82% of respondents felt the need to acquire further information. The acceptability of the vaccine against monkeypox has been indicated by more than half of the participants (54.5%). Furthermore, we state that 45% of the participants are knowledgeable about the monkeypox virus, and 53.1% of the participants have never been affected with COVID-19 before are more worried about COVID-19 than about monkeypox. Participants diagnosed with COVID-19 were 0.63 times less likely to worry about monkeypox than those who were not diagnosed with COVID-19. A greater willingness to get the monkeypox vaccination was seen among the age group 21–30 years (42.4%) compared to the other age groups.
Conclusion: Most healthcare professionals have a moderate knowledge of the monkeypox virus. Furthermore, they demonstrated a low willingness to get the vaccination against the monkeypox virus.
Health experts are worried about the emergence of a new epidemic caused by the monkeypox virus, and they believe monkeypox virus may pose a new threat to human health when the world seems to be in the late stages of the coronavirus disease 2019 (COVID-19) pandemic (1, 2). Monkeypox virus is a DNA virus with two strands that belong to the genus Orthopoxvirus, which also contains variola, cowpox (CPX), and vaccinia viruses (3, 4). Since the Democratic Republic of the Congo (DRC) reported the first human cases of monkeypox in 1970, the disease has spread to other parts of Africa and, more recently, instances of spread of monkeypox outside of Africa have been reported (5). According to the World Health Organization (WHO), there have been more than 13,069 instances of monkeypox worldwide, as on 18 July 2022, with 80% of these cases occurring in the European Union (6). Sexual transmission of infections or diseases has been identified as a major factor associated with greater spreading of the current epidemic, particularly among males who have been identified as homosexual or bisexual (7). Moreover, the virus may get spread by sharing beds or clothes and through direct exposure to infected sores, scabs, or bodily fluids. While the symptoms of monkeypox are comparable with those of smallpox, the lesser extent of severity of the symptoms of monkeypox such as fever, rash, and lymphadenopathy characterize the clinical condition (8, 9). On the contrary, it is characterized by many complications, the most important of which are secondary bacterial infections, keratitis that threatens vision, encephalitis, and pneumonitis. As of late May 2022, many cases of monkeypox have been discovered in various countries in the Middle East (10).
As a result of the extraordinary success achieved by the World Health Organization (WHO) in smallpox eradication 40 years ago, smallpox vaccination is no longer used, with about 70% of the population worldwide have not been vaccinated. The smallpox vaccine is delineated as a prevention method for the monkeypox virus as well since it is effective against orthopoxvirus infections; however, most cases of monkeypox infection have occurred in non-vaccinated individuals (11). Healthcare workers are at high risk of contracting infectious diseases like the monkeypox virus. That increased risk stems from close contact between infected patients and healthcare staff, especially when personal protective equipment is unavailable. The third generation of the smallpox vaccine has shown high efficacy in healthcare workers (12): however, healthcare workers may decline vaccination because of emotional and personal considerations rather than scientific knowledge of this particular situation, and if they are affected by vaccine hesitancy, they may convey this attitude to the patients they care for (13). Healthcare workers must deal with the growing number of human monkeypox virus cases worldwide through early detection, management, and prevention. According to the WHO statement, one of the reasons for the resurgence of the infection was poor knowledge of monkeypox among healthcare workers (10). Before the monkeypox virus spreads further, it is necessary to renovate healthcare facilities and prepare for future epidemics, particularly in low-income countries with limited healthcare system resources (14). During the current COVID-19 pandemic, low- and middle-income courtiers have more reasons to worry about monkeypox virus due to their lower socioeconomic level and limited access to healthcare.
Consequently, they must prepare to cope with another outbreak (15). In Syria, the outbreak of COVID-19 has been a major challenge added to the country's inhabitants who were also affected by the catastrophic effects of warfare (16). A previous study from Jordan revealed that healthcare workers had limited knowledge of the monkeypox virus and confirmed that practitioners lacked confidence in their abilities to diagnose and treat infected patients (17). The monkeypox virus has been a source of rising worry among scientists for various circumstances, including the fact that the disease does not have a definitive treatment or vaccine until now, and the current treatment management depends on improving symptoms and preventing complications. Furthermore, after the monkeypox outbreak in many countries, concerns about the possibility of virus phenotype changing by different mutations have increased (18). The objective of this study is to assess the concerns of healthcare workers in the Arabic countries about the monkeypox virus and the factors associated with good knowledge, in addition to examining vaccine advocacy among them.
An online cross-sectional study was conducted from 2 August 2022 to 28 December 2022 to assess worries and concerns among HCWs toward the monkeypox virus and the factors associated with good knowledge, as well as to examine monkeypox virus vaccine advocacy among them. The inclusion criteria were healthcare workers, such as physicians, nurses, pharmacists, and undergraduate medical students, from the Arabic countries. The countries involved in this study were Egypt, Saudi Arabia, Yemen, Syria, Libya, Algeria, Tunisia, Iraq, Palestine, Jordan, and Sudan. All participants were informed of the aim of the study, the work team identity, their right to withdraw from the study, and the confidentiality of their personal information. The questionnaire was developed based on a previous cross-sectional study conducted in the Arabic country, Saudi Arabia, which included validated scales (19). Furthermore, a professional translator translated the survey from English into Arabic to ensure the total comprehension of the questions. We performed convenience and snowball sampling strategies to perform a professional and non-biased data collection process as possible. We collected the data by creating a Google Forms survey and sending it to respondents through social media platforms such as Facebook, WhatsApp, and Telegram. Fourteen collaborators from each investigated Arabic country in our study were responsible for the data-gathering process. In addition, there was a lead collaborator in each involved study as a local investigator to monitor the data collection and investigate if there were any random, multi-auto, or illogical responses on the online questions, and to check the current job of each respondent to avoid including any person from non-medical staff.
The minimal sample size was computed by interrupting a single proportion of the population formula [n = [(Zα/2)2 × P(1 – P)]/d2], with a 95% of confidence level (CI); Zα/2 = 1.96; a 5% margin of error; P, the proportion of healthcare workers who were more concerned about Monkeypox disease compared to COVID-19 (35.7%); and the proportion of healthcare workers who accepted the vaccination (67.7%) (19). According to the formula, a sample size of 385 was required. The study questionnaire was sent to 3,902 participants through the Google Forms; however, 46 of them refused to participate, bringing the total number of responses to 3,856.
The questionnaire consists of 44 questions divided into five sections. The first section contains information about the participants' sociodemographic variables; the second evaluates HCWs' knowledge of the monkeypox virus and their sources of information; the third examines the perceptions and concerns of healthcare workers about the monkeypox virus; the fourth addresses questions regarding knowledge of HCWs monkeypox infection; and the final section of the questionnaire includes questions adapted from the Generalized Anxiety Disorder-7 (GAD-7) to assess HCWs anxiety about the monkeypox virus.
To identify about the participants' demographic characteristics, such as their age, country of origin, gender, marital status, place of residence, chronic disease, number of family members, economic status, and educational background (including whether they are physicians, nurses, pharmacists, or medical students and their academic year), 14 questions were included in the questionnaire. Furthermore, there were questions about the participants' working hospital type (primary, secondary, or tertiary healthcare centers). The respondents' years of experience and their workplace within the hospital if they work in the hospital pharmacy, intensive care units, isolation departments, or elsewhere were included as additional information. The last question of this section asked the respondents if they had ever been diagnosed with COVID-19.
This section consists of four questions about participants' awareness of the monkeypox virus, including whether the respondents had visited a monkeypox-endemic country (West or Central Africa, Europe, North America, the UAE, and Australia). Also, participants were asked to evaluate their current awareness of the monkeypox disease (low, high, or moderate), and they were asked how informed they were about monkeypox disease (international health websites, social media platforms, or scientific journals) and whether they needed to read more about monkeypox after participating in the survey.
This section contains eight questions designed to measure the concerns and perceptions of healthcare workers regarding the monkeypox virus. Respondents were asked if they were concerned on whether the monkeypox virus will cause a global pandemic like COVID-19 and whether they believe that the monkeypox infection causes a more severe disease than monkeypox. In addition, they were asked to identify the cause of their monkeypox worries (such as their fear of being affected by the disease, concerns about developing another worldwide pandemic, or worries about national lockdown). Respondents were questioned on their acceptance of vaccination and their perceptions of which category should first get the monkeypox vaccine (older adult, children, college students, etc.).
Regarding assessing HCWs' knowledge of the monkeypox virus, we adopted questionnaire items from a study about knowledge of human monkeypox among students in various Jordanian health schools (20). In this section, with 11 questions about monkeypox, participants were asked: “is monkeypox common in the Middle East?” “is monkeypox common in Western and Central Africa?” “is there a global epidemic of human monkeypox?” “is monkeypox caused by a virus or another pathogen?” and “is spreading the disease from person to person a risk?” Participants were also asked “whether human monkeypox could be treated with antibiotics?” “whether diarrhea is one of the signs or symptoms of human monkeypox?” “whether pustules are one of the signs or symptoms of infection?” “whether skin rash is one of the signs or symptoms of human monkeypox?” “whether monkeypox has similar signs and symptoms to smallpox?” and “whether vaccination is available to prevent human monkeypox?” The possible answers to each knowledge item were “yes,” “no,” and “I do not know”). Correct replies were given a score of 1, wrong responses were assigned a score of −1, and “I do not know” was given a score of 0. These scores represented the participants' monkeypox knowledge score (MPX K-score). An adequate degree of knowledge was determined as a score of 70% correct replies or above as we depended on the published studies.
This scale contains seven items that measure participants' GAD regarding the monkeypox virus (20, 21). Participants were asked to rate how often they had felt symptoms such as worry, concern, restlessness, impatience, and dread over the past 2 weeks. We assigned values from 0 to 3 for the four frequency levels of never, sometimes, often, and very frequently. There were four levels of severity determined by the GAD7 score: minimum (1–4), mild (5–9), moderate (10–14), and severe (0–14). (15–21).
To make sure the survey questions were clear before launching the online survey on social media platforms, we sent the questions to 45 randomly selected Arabic healthcare providers from specific countries. Then we modified the survey depending on the feedback and suggested adjustments. Although we have used the scales from a published study of an Arabic country, we ran a pilot study in which we sent the questionnaire to 50 volunteers, who were healthcare providers from those countries involved in our study to confirm the reliability of the used scales, for which we determined the Cronbach's α to each involved scale. Then, we confirmed that the scales we used in our cross-sectional study had high internal consistency levels (Cronbach's α was above 7.0).
The Syrian Ethical Society for Scientific Research at Aleppo University, Syria provided the ethical approval for conducting the study (IRB: SA-1087). In addition, we ordered at least one printed ethical approval from the clinical and educational institutions (Hospitals and Medical Colleges) of the lead collaborators from each investigated country of our study. The first question in the online survey was about the respondent's acceptance to complete the survey. We also ensured that all methods in our online cross-sectional were according to the Declaration of Helsinki developed by World Medical Association (WMA). The survey takes 5–12 min to complete, and for security purposes, all data is saved in an online database.
The data were examined using the Statistical Package for the Social Sciences (IBM SPSS V. 28.0). Statistical significance was defined as a p-value of ≤ 0.05. The quantitative data were given with a mean and standard deviation, while the categorical data were presented with frequency and percentages. After validating the data and distribution that were non-parametric using the Shapiro–Wilk test, we used the Kruskal–Wallis test to compare how much each subgroup differed from others in terms of their awareness of monkeypox, desiring to vaccinate themselves against monkeypox, and worrying toward the new pandemic that will arise due to monkeypox. Finally, using the cutoff points from the Saudi Arabian research (22), we conducted a binary logistic regression to calculate the odds ratios (ORs) between the dependent variables (awareness of monkeypox and desire to vaccinate themselves against monkeypox) and independent variables (sociodemographic factors) for having an appropriate awareness of monkeypox and a desire to vaccinate themselves against monkeypox.
The questionnaire was distributed to 3,902 participants; however, 46 among the participants declined to participate, resulting in a final sample size of 3,856. Most of the participants were aged between 21 and 30 years (78%), and more than half of the sampling participants (56.3%) were of females. Participants residing in the city comprised 82.3%, and most of the participants (50.2%) had a moderate financial condition. Students involved in the study were 50.1%, while practitioners involved in the study remained 30.7%. The majority (63.6%) of participants were employed by the hospital's central wards, while 16.5% worked in the outpatient department, and 12.1% were employed by the hospital's pharmacy or laboratory (Table 1).
Participants with previous diagnoses of COVID-19 comprised 35.7%; however, 8.8% of participants were concerned that monkeypox might generate an epidemic like COVID-19, whereas 43.5% of participants were uncertain about the severity of monkeypox compared to smallpox. Respondents concerned more about monkeypox than about COVID-19 were 18.1%, and 82.3% of the respondents felt that they needed to learn more about it after reading the survey. More than half of the participants (54.5%) have expressed acceptance of the vaccination against monkeypox. Participants reported social media (58.1%), websites of the WHO/Centers for Disease Control and Prevention (CDC) (31.1%), and the Internet (30.2%) as a source of information about monkeypox (Table 2).
We found that 61.7% of participants were concerned about being infected themselves or their family, while 54.6% were worried about the number of monkeypox cases increasing to the level that might force a national lockdown. Less than half of the participants reported being anxious about the sickness progressing to the level of a global pandemic (45.9%) (Table 3).
Approximately half of the participants (55%) were unaware of the monkeypox virus (Figure 1), and 23.8% of respondents believe that the monkeypox virus is expected in the Arabic countries. In comparison, 35.3% of respondents do not know whether there is a global epidemic of monkeypox. Regarding the resemblance of symptoms between monkeypox and smallpox, 58.4% of participants thought the symptoms were similar, while 23.3% of participants agreed that antibiotics might be used to treat monkeypox. Only 27.1% of respondents believe that monkeypox immunization is available (Table 4).
Our results show that females were more concerned about COVID-19 (44.6%) than monkeypox (11.7%), as well as participants who had not been diagnosed with COVID-19 were concerned more about COVID-19 (53.1%) than about monkeypox (11.2%). Among respondents who felt that monkeypox symptoms are like smallpox, 10.8% were more concerned about monkeypox than about COVID-19. Among anxious individuals, 18.4% are more concerned about COVID-19 than about monkeypox virus. Notably 7 out of 15 predictor factors were significantly linked with greater worry from monkeypox than from COVID-19 (p < 0.05). Participants with more than 5 years of work experience were less likely to be concerned more about monkeypox than about COVID-19 (OR = 0.59; 95% CI: 0.374–0.931), comparable to those with < 5 years of work experience. Participants diagnosed with COVID-19 were less likely to worry about monkeypox (OR = 0.63; 95% CI: 500–807) than those without. A higher likelihood of worrying about monkeypox than COVID-19 was anticipated among participants who worried more about monkeypox causing a widespread epidemic like COVID-19 (OR = 2.87; 95% CI:
1.962–4.212). Concern about monkeypox was expected to be higher than COVID-19 (OR = 4.47; 95% CI: 2.852–7.020) among participants who believed that monkeypox produces more severe symptoms than smallpox (Table 5).
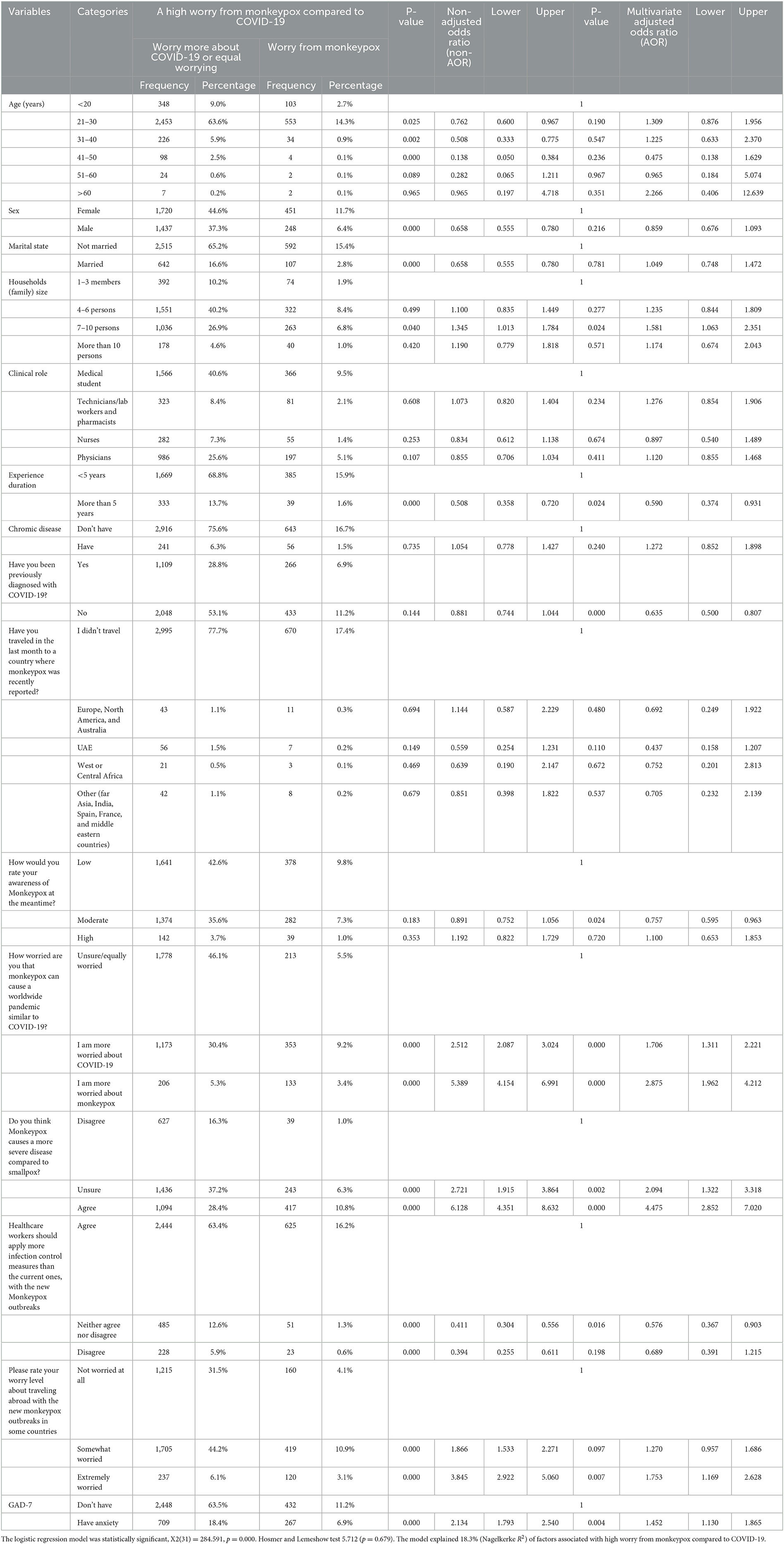
Table 5. Multivariate binary logistic regression analysis of the HCWs' odds ratios of high worry from monkeypox compared to COVID-19.
Our analysis shows that 29.4% of females, 42.4% of participants aged between 21 and 30 years, 32.9% of participants diagnosed with COVID-19, and 46.6% of participants with < 5 years of experience accepted receiving the vaccine. However, 13.7% of participants with good economic status, 3.6% of participants aged between 31 and 40 years, and 35.3% of participants who were not anxious about monkeypox refused to receive the vaccine.
Notably, 7 of the 15 predictor factors were statistically associated with HCWs' support for immunizations against monkeypox (p < 0.05). Male MHWs were more likely to accept immunization against monkeypox (OR = 1.3; 95% CI: 1.168–1.668) than female MHWs. Participants aged between 21 and 30 years were 2.36 times more likely to receive the vaccine than those aged under 20. Participants who were not diagnosed with COVID-19 infection have a lower probability of accepting the vaccine than participants who were diagnosed with COVID-19 infection (OR = 0.64). Regarding the GAD-7 scale, anxious participants were more likely to endorse immunizations against monkeypox (OR = 1.48) than those without anxiety (Table 6).
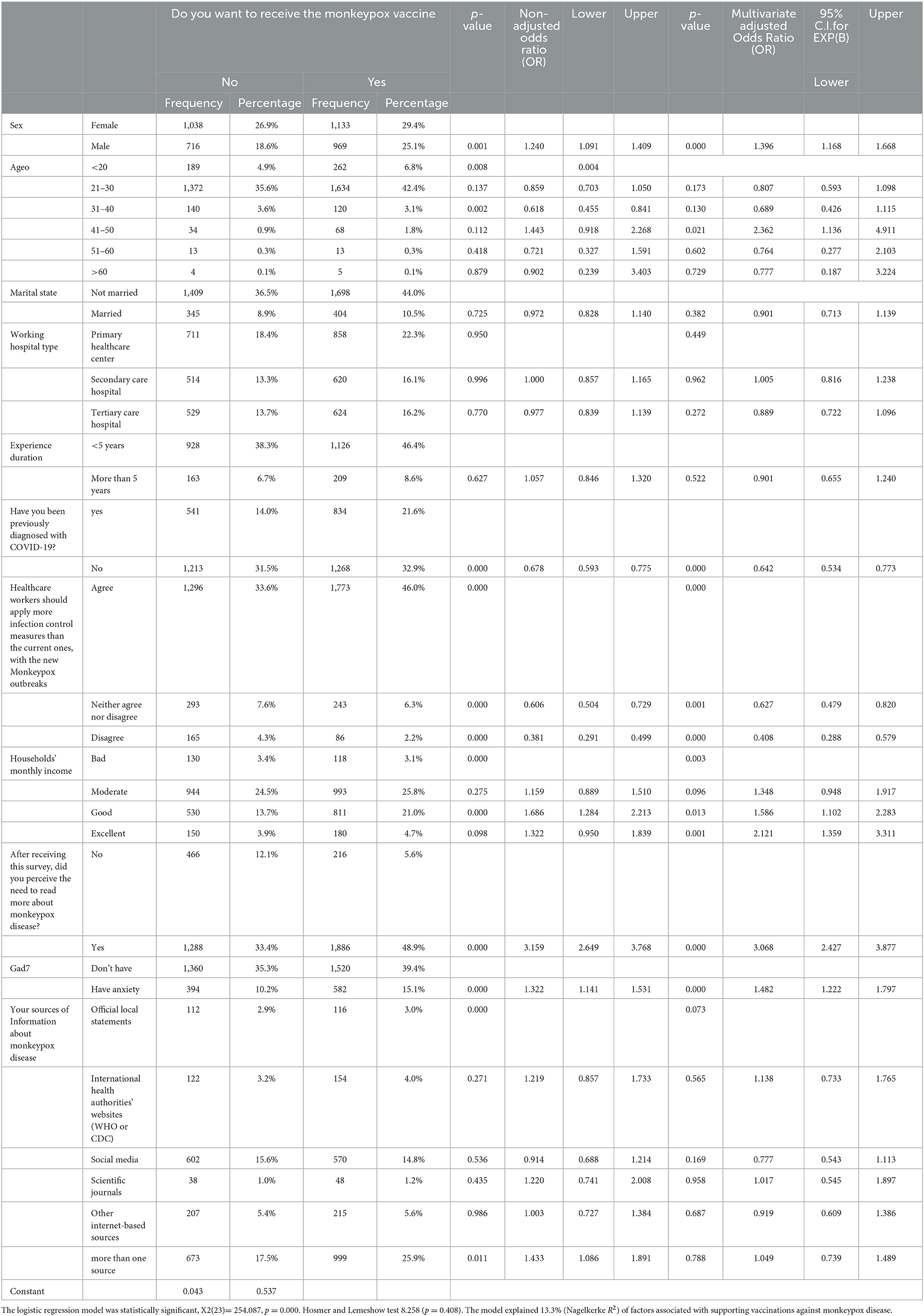
Table 6. Multivariate binary logistic regression analysis of the HCWs' odds ratios of supporting vaccinations against monkeypox disease.
Regarding adherence to monkeypox disease control measures, participants who showed no adherence were 53.7% of females, 73.1% of participants aged between 21 and 30 years, 38.9% of participants worried more about COVID-19, and 23.6% of respondents had anxiety about monkeypox. In comparison, participants revealed adherence to control measures were 4.9% of participants aged between 31 and 40 years, 4.8% of participants who do not have anxiety about monkeypox, and 5.9% of participants with < 5 years of experience.
Notably, five of the 14 predictor factors were substantially linked to HCWs' probability of backing more stringent infection control measures against monkeypox (p < 0.05). Females have shown greater adherence to disease control measures than males (OR = 1.67). Participants with anxiety were more likely to adhere to disease control measures than that of the participants without anxiety (OR = 1.79). Participants worried more about COVID-19 have a greater probability of disease control measures adherence (OR = 1.64) compared to participants who expressed equal concern about both illnesses (Table 7).
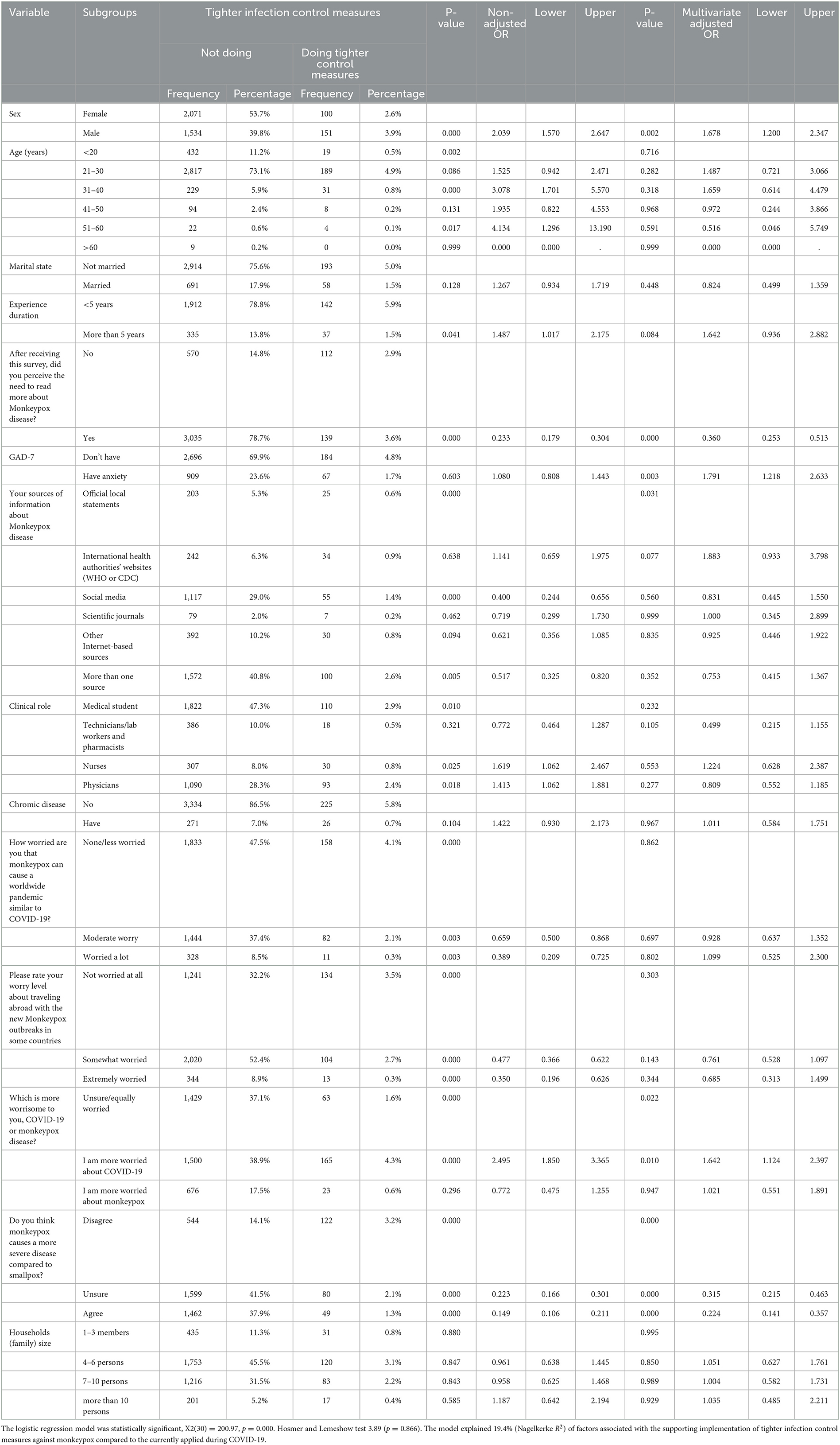
Table 7. Multivariate binary logistic regression analysis of the HCWs' odds of supporting the implementation of tighter infection control measures against monkeypox compared to the currently applied during COVID-19.
Good knowledge about the monkeypox virus was shown by 25.4% of females and 34.8% of individuals aged 21–30 years. However, only 21.3% of medical students and 7.7% of clinicians with more than 5 years of experience show adequate knowledge of monkeypox. Only 22.2% of the participants agreed that monkeypox develops a more severe illness than smallpox, and 27.6% of respondents who agreed to receive the monkeypox vaccination had good knowledge of monkeypox. Only 12.1% of individuals with anxiety disorders have a good knowledge of monkeypox. In a multivariate logistic regression analysis, we found that family size, study year, participants' ratings of their awareness of monkeypox, participants' worry that monkeypox will cause a pandemic like COVID-19, and whether healthcare workers should apply more infection control measures were all significantly associated with HCWs' odds ratios of knowing about monkeypox (p < 0.05). Participants concerned about monkeypox developing a similar pandemic like COVID-19 have greater knowledge than participants who did not concern about monkeypox (OR = 1.82). Respondents who disagreed that HCWs should adhere more to the disease control methods were less likely to be knowledgeable about monkeypox than participants who agreed that HCWs should adhere more to the disease control methods (OR= 0.38) (Table 8).
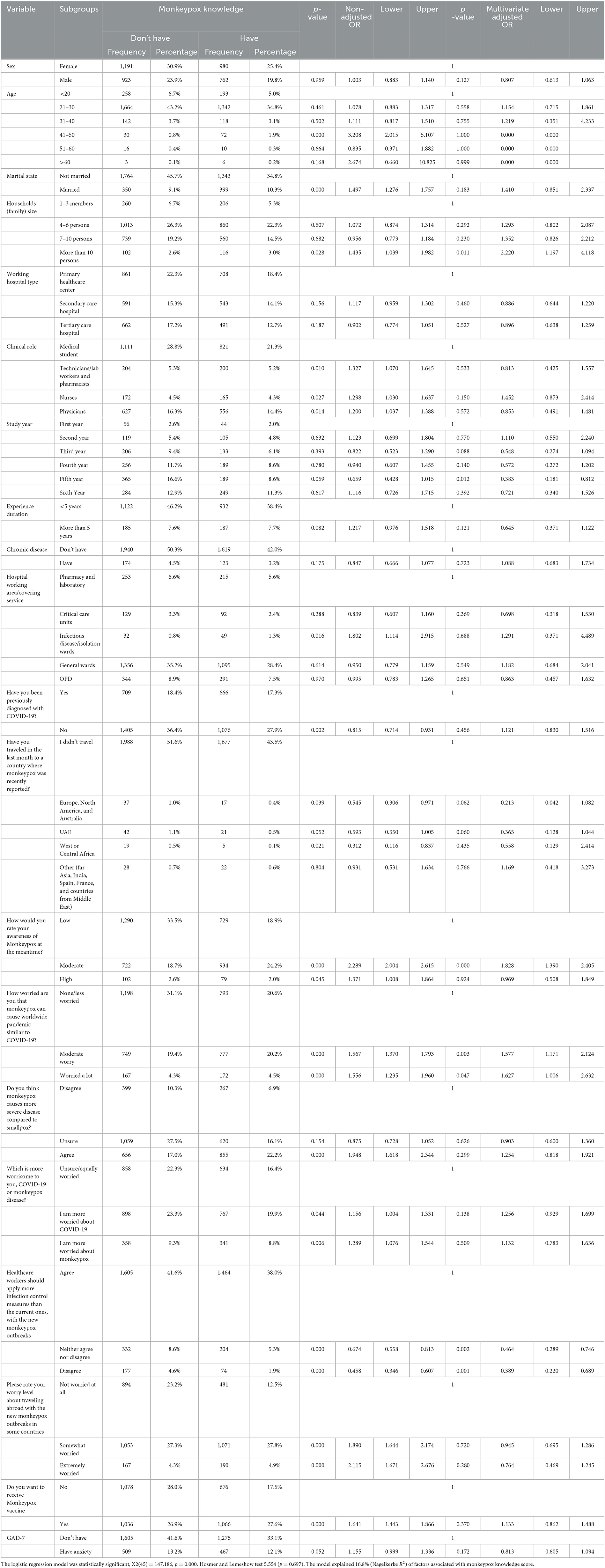
Table 8. Multivariate binary logistic regression analysis of the HCWs' odds ratios of monkeypox knowledge score.
Monkeypox is an infectious disease caused by orthopoxvirus characterized by a rash that may be isolated, preceded, or accompanied by fever or lymph nodes (23). Since 14 May 2022, confirmed cases of the virus have been reported or confirmed in several countries in Europe and North America, and the situation is evolving rapidly. In the UK, 16 cases of infection have been detected (as of 17 May 2022). Except for the first infected person, returning from Nigeria, all appear to have been infected in the UK, according to the local health safety agency (24). For fear of a possible new pandemic, health authorities worldwide have boosted their efforts to ensure the control of its spread by studying the means of transmission and early clinical signs. During the current increase of the reported infected cases of monkeypox, the knowledge, concern, and perception of the available vaccines are concerning factors, especially among healthcare providers and medical staff persons (25). Our study was conducted in the Middle East and North Africa (MENA) region with a final sample size of 3,856 participants, of which 1,375 had a history of COVID-19 diagnosis. Results reported that about 9% of participants considered that monkeypox might generate as an epidemic and a tremendous burden on human health scenario might occur like COVID-19, while 51.6% had no worries about monkeypox. These findings are similar to a Saudi Arabian study where only 25.3% of the study population were very worried, and 48.7% had no or less worries about a further monkeypox pandemic (22). Also, for almost the quarter, 18.1% of participants were concerned more about monkeypox than about COVID-19. These findings are also concomitant with another Saudi Arabian study published in August 2022 carried out by Mohamad et al. among the general population, where results reported a higher worry (62%) about COVID-19 than monkeypox (26). Concerning HCWs' sources of worries toward monkeypox disease, the majority (61.7%) of participants were concerned about being infected themselves or their relatives, and slightly more than half (54%) were afraid of a possible future lockdown. Similarly, these findings are concomitant with results found in a Saudi Arabian study by Temsah et al. (26).
About monkeypox knowledge level, slightly more than half (55%) of the participants were unaware of the monkeypox virus and had no sufficient information about it, and 58.4% of respondents could not make a difference between monkeypox and smallpox symptoms. Also, only 27.1% of participants reported positively that monkeypox immunization is already available. Knowledge findings were concomitant overall with Indonesian research conducted by Harapan et al., where monkeypox knowledge level was evaluated as low at 63.5% and insufficient among 432 general practitioners (27).
Male HCWs in the MENA region were less predicted to worry about monkeypox than female HCWs (6.4 and 11.7%, respectively), which was also reported toward COVID-19 worries. This was similarly found in a Saudi Arabian study by Ajman et al. (22). In addition, results reported that participants diagnosed with COVID-19 were less likely to worry about monkeypox (OR = 0.63 times) than those who had not been infected with COVID-19 virus. Findings also reported higher acceptance for the monkeypox vaccine by participants who had not been diagnosed with COVID-19 (n = 1,268, 32.9%) than those had been diagnosed with previous COVID-19. This incomprehensible and unpredictable finding could only be justified by a drop in healthcare workers' confidence level in vaccine protection after COVID-19 infection following administration of vaccines. This should be adjusted and corrected as approved vaccines have proven to be effective in preventing fatal complications of COVID-19 infection, reducing the number of people hospitalized and admitted to the intensive care unit, and reducing the number of infections without preventing it (28).
The knowledge of monkeypox infection, attitude toward its possible spread among healthcare practitioners in the MENA region, and vaccine advocacy must be improved urgently. This will prevent a possible pandemic because a good knowledge of the symptoms, confidence in diagnosis, modes of transmission, physiopathology, and comorbidities will help to avoid the maximum number of cases. Also, in case of a further pandemic, it will pave way to control the situation efficiently and professionally, based on the previous COVID-19 experience (15). These human monkeypox concerns among Arabic healthcare professionals can be corrected and improved through several approaches and by multiple means such as (29–32) (a) continuing medical education and scientific improvement on the infection process, which makes it less contagious than COVID-19 and, therefore, same rapid spread and a sudden pandemic scenario like COVID-19 are not expected; (b) more data about available vaccines and their efficiency—currently, only two vaccines, ACAM2000 vaccine and JYNNEOS, known as Imvanex, are available, and (c) involvement in research of international monkeypox network and patients' sensitivity and education on preventive measures.
To examine the present degree of opinions of healthcare professionals concerning the characteristics of the monkeypox epidemic, next to COVID-19, our international cross-sectional survey includes a large sample size from various countries in the Arabic region. Additionally, we utilized scales that were getting better with its effectiveness, developed by Arabic scholars. We checked their validity to ensure if the questions they were using accurately represented the subject being investigated. Nevertheless, even though cross-sectional research may be carried out in a short amount of time and at no cost, the research needs to consider the specific and valid causal link and the generality of monkeypox. In addition, concerning the online cross-sectional research, it is difficult to get answers from those who do not have surplus time for attempting the questionnaire, those who do not have Internet access and a mobile phone, or those who are having trouble completing the survey due to technical challenges. This is particularly the case in connection with older adult individuals who are not familiar with the use of mobile phones.
Our results showed that healthcare professionals in the Arabic countries seemed to be less concerned about the monkeypox virus compared with their concern about the COVID-19 virus. Moderate knowledge of the monkeypox virus was noticed, and less tendency to receive vaccination against the monkeypox virus was also noticed. Furthermore, negative attitudes toward the monkeypox virus protection methods were observed. As a result, we recommend further regulations for the medical staff and precautionary measures. Furthermore, adequate awareness programs should be implemented for medical staff to teach them about the risks of monkeypox infection.
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding authors.
The Syrian Ethical Society for Scientific Research at Aleppo University, Syria, provided the ethical approval for conducting the study (IRB: SA-1087). In addition we ordered at least one printed ethical approval from the lead collaborator from each inquired country in our study that was given by the clinical, and educational institutions (Hospitals, Medical Colleges). To confirm that participating in our study was voluntary, the first question in the online survey was about the respondent's acceptance to complete the survey.
SS: study conception and design. HA, HB, NJ, MR, MN, WH, BS, AA, and SF: writing and reviewing the manuscript. MN and SS: formal analysis. IA, SA, and RY: draft manuscript. AR and ME: interpretation of results and revising. All authors reviewed the results and approved the final version of the manuscript.
1. Albaraa Daradkeh, Faculty of Medicine, Alexandria University, Alexandria, Egypt (ZWxiYXJhYS5tYWhtb3VkMTkwMUBhbGV4bWVkLmVkdS5lZw==).
2. Zuhair Antakly, Resident Doctor at Aleppo University Hospital, Department of Oncology (WnVoYWlyYW50YWtseUBnbWFpbC5jb20=).
3. Mirna Maged Armanyos, Faculty of Medicine, Alexandria University, Egypt (mirnam.armanios@icloud.com).
4. Ajmal J. Alsufyani, Faculty of Medicine, Sana'a University, Sana'a, Yemen (YWptYWxhbHN1ZnluaUBnbWFpbC5jb20=).
5. Salsabeel Abdulbaki Ghalib Al_hanani: Faculty of Medicine, Sana'a University, Sana'a, Yemen (c2Fsc2FiZWVsYWxoYW5hbmlAZ21haWwuY29t).
6. Moyasar Awad Idris Abubakr, House Officer, Gadarif Teaching Hospital, Surgical Department Gadarif, Sudan (bWF5YXNhcmF3YWRAZ21haWwuY29t).
7. Hadeil Ali Abdelsalam Alhashmi, Faculty of Medicine, Altinbaş University, Istanbul, Turkey (SGFkZWlsYWxoYXNobWlAZ21haWwuY29t).
8. Jarjees Abduljabar Sulaiman, University of Duhok, College of Medicine (amFyamVzYWJkdWxqYWJhckBnbWFpbC5jb20=).
9. Hadeel Fuad Alwan Al-sharjabi, Faculty of Medicine, Sana'a University, Sana'a, Yemen (aGFkZWVsZnVhZGFsc2hhcmphYmk4OUBnbWFpbC5jb20=).
10. Nidaa T Alhumaidi, Faculty of Pharmacy, Taif University, Taif, Saudi Arabia (nidaa.t.alhumidi@icloud.com).
11. Monzir Ahmed Hassan Osman, Department of General Surgery, Ibrahim Malik teaching hospital, Khartoum, Sudan (bW9uemlyYWhtZWQ5N0BnbWFpbC5jb20=).
12. Mohamed Basyouni Helal, Faculty of Medicine, Menoufia University, Menoufia, Egypt (bW9oYW1lZGJhc3lvdW5pNDE2ODQzQGdtYWlsLmNvbQ==).
13. Abdulghani A Al-Aswadi, Faculty of Medicine, Sana'a University, Sana'a, Yemen (YWJkdWxnaGFuaWFsYXN3YWRpMUBnbWFpbC5jb20=).
14. Amna Elaagib, MBBS, Almughtaribeen University, Khartoum, Sudan (YW1uYWVsYWFnaWJAZ21haWwuY29t).
15. Amatalkhaleq Hussein Hamoud Azzam, University of Sana'a, Faculty of Medicine and Health Science, Sana'a, Yemen (YW1hdGFsa2hhbGVxYXp6YW1AZ21haWwuY29t).
16. Alshaymaa Mortada Ali Eltohry, Faculty of Medicine, Ain Shams University, Egypt (YWxzaGF5bWFhYWxpNjJAZ21haWwuY29t).
17. Wesal Mohammed Ahmed Abdelkaream Ishag, Faculty of Medicine, University of Gezira (d2VzYWw5MnNvbGFAZ21haWwuY29t).
18. Lyn Ahmad, Faculty of Medicine, Damascus University, Damascus, Syria (bHlucm9zNjJAZ21haWwuY29t).
19. Safiya Mohammed Al-Haddi, Thamar University, Faculty of Medicine, Yemen (U2FmZmltb2hhbW1lZDk3OUBnbWFpbC5jb20=).
20. Ebrahim Ahmed Shaddad, Faculty of Medicine, Sana'a University, Sana'a, Yemen (ebrahimshaddad.es@gmail.com).
21. Mawahib Hajhamed El Sheikh Mergani, Faculty of Medicine, Ahfad University for Women, Khartoum, Sudan (bWF3YWhpYmhhamhhbWVkQGdtYWlsLmNvbQ==).
22. Hossam Tharwat Ali, Qena Faculty of Medicine, South Valley University, Qena, Egypt (aG9zc2FtdGhhcndhdGFsaUBnbWFpbC5jb20=).
23. Hadeel Shayef Ahmed Aljalal, Faculty of Medicine, Sana'a University, Sana'a, Yemen (aGFkZWVsc2hheWVmQGdtYWlsLmNvbQ==).
24. Ashjan Nasser Abdurabu Bamarhool, MBBS, Ibn Sina National College, Jeddah, Saudi Arabia (dG9hc2wyMjJAZ21haWwuY29t).
25. Manal Jamal Qasim Al-Dhaheri, Faculty of Medicine, Sana'a University, Sana'a, Yemen (bWFuYWxkaGFoZXJpOTdAZ21haWwuY29t).
26. Suhaib Hassan Mohammed Yousif, MBBS, Almughtaribeen University, Khartoum, Sudan (c29oYWliYWxyb21lMTJAZ21haWwuY29t).
27. Waheeb Ali Al-Garadi, Faculty of Medicine, Thamar University, Thamar City, Yemen (V2FoZWViOTk5NDRAZ21haWwuY29t).
28. Raghad Sameer Qazzaz, MD, Faculty of Medicine, Mutah University, Karak, Jordan (cmFnaGFkc2FtZWVyNzZAZ21haWwuY29t).
29. Nora Ra'ed Abdullah Atiah, Sana'a University, Faculty of Medicine and Health Sciences, Sana'a, Yemen (YXRpYWhub3JhMTFAZ21haWwuY29t).
30. Dua Hassan, Faculty of Medicine, Sana'a University, Sana'a, Yemen (ZG9jdG9yZHVhYTMzMUBnbWFpbC5jb20=).
31. Ali Haj Yehia, Faculty of Medicine, Damascus University, Damascus, Syria (YWxpaGFqeWVoaWE0NUBnbWFpbC5jb20=).
32. Tahany A. Qashwa, Faculty of Medicine, Sana'a University, Sana'a, Yemen (dGFoYW55YWhtZWQyMDgwQGdtYWlsLmNvbQ==).
33. Imen Achouri, Department of Physical Education and Sports Science, Higher Institute of Sport and Physical Education of Sfax, University of Sfax, Tunisia (aW1lbmFjaG91cmkyMDIxQGdtYWlsLmNvbQ==).
34. Aseela Reyadh Abdu Mokbel Alhammadi, Faculty of Medicin, Sana'a University, Sana'a, Yemen (YXNlZWxhYWxoYW1tYWRpNzhAZ21haWwuY29t).
35. Lana Sheet, Faculty of Medicine, Aleppo University, Aleppo, Syria (TGFuYXNoZWl0dDNAZ21haWwuY29t).
36. Wehba Hraiz, Faculty of Medicine, Damascus University, Damascus, Syria (aHJhaXp3ZWhiYUBnbWFpbC5jb20=).
37. Mohammed Ahmed Salah Mohammed Ahmed Elgak, University of Kassala, Faculty of Medicine, Sudan (Mohammedahmed6218@gmail).
38. Sarah Alawi Almaqdi, Faculty of Medicine, Hadramout University, Hadramout, Yemen (c2FyYWhhbGF3aTUwNUBnbWFpbC5jb20=).
39. Hashem Tehsib Ali, Faculty of Medicine, Al-Furat University, Deir ez-Zor, Syria (aGFzaGVtYWJ1YXJpOThAZ21haWwuY29t).
40. Kareem Fathy Mohamed, Rheumatology Resident, Faculty of Medicine, Al-Azhar University Hospital, New Damietta (S2ZhdGh5NjM4QGdtYWlsLmNvbQ==).
BS was employed by Hamad Medical Corporation.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2023.1153136/full#supplementary-material
1. Rizk JG, Lippi G, Henry BM, Forthal DN, Rizk Y. Prevention and treatment of monkeypox. Drugs. (2022) 82:957–63. doi: 10.1007/s40265-022-01742-y
2. Shapo L, Puca E. What could drive the re-emergence of infectious diseases in a post-Covid19 era? Travel Med Infect Dis. (2023) 52:102546. doi: 10.1016/j.tmaid.2023.102546
3. Realegeno S, Puschnik AS, Kumar A, Goldsmith C, Burgado J, Sambhara S, et al. Monkeypox virus host factor screen using haploid cells identifies essential role of GARP complex in extracellular virus formation. J Virol. (2017) 91. doi: 10.1128/JVI.00011-17
4. Farasani. Monkeypox virus: future role in human population. J Infect Public Health. (2022) 15:1270–5. doi: 10.1016/j.jiph.2022.10.002
5. Bunge EM, Hoet B, Chen L, Lienert F, Weidenthaler H, Baer LR, et al. The changing epidemiology of human monkeypox-A potential threat? A systematic review. PLoS Negl Trop Dis. (2022) 16. doi: 10.1371/journal.pntd.0010141
6. WHO, (2022). Global Health Monkeypox. Available online at: https://github.com/globaldothealth/monkeypox (accessed May 19, 2022).
7. Sah R, Abdelaal A, Reda A, Katamesh BE, Manirambona E, Abdelmonem H, et al. Monkeypox and its possible sexual transmission: where are we now with its evidence? Pathogens. (2022) 11:924. doi: 10.20944/preprints202207.0314.v1
8. Adler H, Gould S, Hine P, Snell LB, Wong W, Houlihan CF, et al. Clinical features and management of human monkeypox: a retrospective observational study in the UK. Lancet Infect Dis. (2022) 22:1153–62. doi: 10.1016/S1473-3099(22)00228-6
9. Hasan S, Saeed S. Monkeypox disease: an emerging public health concern in the shadow of COVID-19 pandemic: an update. Trop Med Infect Dis. (2022) 7:283. doi: 10.3390/tropicalmed7100283
11. Simpson K, et al. Human monkeypox - After 40 years, an unintended consequence of smallpox eradication. Vaccine. (2020) 38:5077–81. doi: 10.1016/j.vaccine.2020.04.062
12. Petersen BW, Kabamba J, McCollum AM, Lushima RS, Wemakoy EO, Tamfum J-JM, et al. Vaccinating against monkeypox in the Democratic Republic of the Congo. Antiviral Res. (2019) 162:171–7. doi: 10.1016/j.antiviral.2018.11.004
13. Riccò M, Ferraro P, Camisa V, Satta E, Zaniboni A, Ranzieri S, et al. When a neglected tropical disease goes global: knowledge, attitudes and practices of Italian physicians towards monkeypox, preliminary results. Trop Med Infect Dis. (2022) 7. doi: 10.3390/tropicalmed7070135
14. Idris I, Adesola RO. Current efforts and challenges facing responses to Monkeypox in United Kingdom. Biomed J. (2022). doi: 10.1016/j.bj.2022.07.007
15. Taseen S, Nasir F, Abbas M, Altaf M, Asghar MS, Tahir MJ. Post-pandemic world at the mercy of monkeypox virus outbreak: Time to worry or not? J Med Virol. (2022). doi: 10.1002/jmv.27948
16. Swed S, Alibrahim H, Sawaf B, Alzabibi MA, Shibani M, Sakkour R. COVID-19, war and poverty in Syria. Ann Med Surg. (2022) 75:103382. doi: 10.1016/j.amsu.2022.103382
17. Sallam M, Al-Mahzoum K, Al-Tammemi AB, Alkurtas M, Mirzaei F, Kareem N, et al. Assessing healthcare workers' knowledge and their confidence in the diagnosis and management of human monkeypox: a cross-sectional study in a middle eastern country. Healthcare. (2022) 10. doi: 10.3390/healthcare10091722
18. Farahat RA, Abdelaal A, Shah J, Ghozy S, Sah R, Bonilla-Aldana DK, et al. Monkeypox outbreaks during COVID-19 pandemic: are we looking at an independent phenomenon or an overlapping pandemic? Ann Clin Microbiol Antimicrob. (2022) 21:26. doi: 10.1186/s12941-022-00518-2
19. Sallam M, Al-Mahzoum K, Dardas LA, Al-Tammemi AB, Al-Majali L, Al-Naimat H, et al. Knowledge of human monkeypox and its relation to conspiracy beliefs among students in jordanian health schools: filling the knowledge gap on emerging zoonotic viruses. Medicina. (2022) 58, 924. doi: 10.3390/medicina58070924
20. Spitzer RL, Kroenke K, Williams JB, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. (2006) 166:1092–7. doi: 10.1001/archinte.166.10.1092
21. AlHadi AN, AlAteeq DA, Al-Sharif E, Bawazeer HM, Alanazi H, AlShomrani AT, et al. An arabic translation, reliability, and validation of patient health questionnaire in a saudi sample. Ann Gen Psychiatry. (2017) 16:32. doi: 10.1186/s12991-017-0155-1
22. Ajman F, Alenezi S, Alhasan K, Saddik B, Alhaboob A, Altawil ES, et al. Healthcare workers' worries and monkeypox vaccine advocacy during the first month of the WHO monkeypox alert: cross-sectional survey in Saudi Arabia. Vaccines. (2022) 10:28. doi: 10.3390/vaccines10091408
23. Moore MJ, Rathish B, Zahra F. Monkeypox. In: StatPearls. Treasure Island, FL: StatPearls Publishing Copyright © 2022, StatPearls Publishing LLC. (2022).
24. Di Gennaro F, Veronese N, Marotta C, Shin JI, Koyanagi A, Silenzi A, et al. Human monkeypox: a comprehensive narrative review and analysis of the public health implications. Microorganisms. (2022) 10:1633. doi: 10.3390/microorganisms10081633
25. Ajmera KM, Goyal L, Pandit T, Pandit R. Monkeypox - An emerging pandemic. IDCases. (2022) 29:e01587. doi: 10.1016/j.idcr.2022.e01587
26. Temsah M-H, Aljamaan F, Alenezi S, Alhasan K, Saddik B, Al-Barag A, et al. Monkeypox caused less worry than COVID-19 among the general population during the first month of the WHO Monkeypox alert: experience from Saudi Arabia. Travel Med Infect Dis. (2022) 49:102426. doi: 10.1016/j.tmaid.2022.102426
27. Harapan H, Setiawan AM, Yufika A, Anwar S, Wahyuni S, Asrizal FW, et al. Knowledge of human monkeypox viral infection among general practitioners: a cross-sectional study in Indonesia. Pathog Glob Health. (2020) 114:68–75. doi: 10.1080/20477724.2020.1743037
28. Xing K, Tu XY, Liu M, Liang ZW, Chen JN, Li JJ, et al. Efficacy and safety of COVID-19 vaccines: a systematic review. Zhongguo Dang Dai Er Ke Za Zhi. (2021) 23:221–8. doi: 10.7499/j.issn.1008-8830.2101133
29. Goyal L, Ajmera K, Pandit R, Pandit T. Prevention and treatment of monkeypox: a step-by-step guide for healthcare professionals and general population. Cureus. (2022) 14:e28230. doi: 10.7759/cureus.28230
30. Rao AK, Petersen BW, Whitehill F, Razeq JH, Isaacs SN, Merchlinsky MJ, et al. Use of JYNNEOS (smallpox and monkeypox vaccine, live, nonreplicating) for preexposure vaccination of persons at risk for occupational exposure to orthopoxviruses: recommendations of the advisory committee on immunization practices - United States, 2022. MMWR Morb Mortal Wkly Rep. (2022) 71:734–42. doi: 10.15585/mmwr.mm7122e1
31. Poland GA, Kennedy RB, Tosh PK. Prevention of monkeypox with vaccines: a rapid review. Lancet Infect Dis. (2022) 22:e349–58. doi: 10.1016/S1473-3099(22)00574-6
Keywords: monkeypox, COVID-19, anxiety, vaccination, multi-national cross-sectional study
Citation: Swed S, Alibrahim H, Bohsas H, Jawish N, Rais MA, Nasif MN, Hafez W, Sawaf B, Abdelrahman A, Fathey S, Atef Ismail Ahmed Ibrahim I, Almashaqbeh SHA, Yousef Aljawarneh RM, Rakab A, EL-Shafei EHH, Hurlemann R, Elsayed MEG and Data Collection Group (2023) A multinational cross-sectional study on the awareness and concerns of healthcare providers toward monkeypox and the promotion of the monkeypox vaccination. Front. Public Health 11:1153136. doi: 10.3389/fpubh.2023.1153136
Received: 28 January 2023; Accepted: 29 March 2023;
Published: 09 May 2023.
Edited by:
Veronique Seidel, University of Strathclyde, United KingdomReviewed by:
Muruganandam Nagarajan, Regional Medical Research Centre (ICMR), IndiaCopyright © 2023 Swed, Alibrahim, Bohsas, Jawish, Rais, Nasif, Hafez, Sawaf, Abdelrahman, Fathey, Atef Ismail Ahmed Ibrahim, Almashaqbeh, Yousef Aljawarneh, Rakab, EL-Shafei, Hurlemann, Elsayed and Data Collection Group. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Sarya Swed, c2FyeWFzd2VkMUBnbWFpbC5jb20=; Mohamed E. G. Elsayed, bW9oYW1lZC5lbHNheWVkQG1laW4uZ214; bW9oYW1lZC5lbHNheWVkMUB1bmktb2xkZW5idXJnLmRl
†ORCID: Sarya Swed orcid.org/0000-0002-9983-2020
Mohamed E. G. Elsayed orcid.org/0000-0002-0011-7837
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.