
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Public Health , 27 March 2023
Sec. Children and Health
Volume 11 - 2023 | https://doi.org/10.3389/fpubh.2023.1152321
This article is part of the Research Topic The Impact of Smart Screen Technologies and Accompanied Apps on Young Children Learning and Developmental Outcomes - Volume 2 View all 9 articles
 Shanshan Geng1†
Shanshan Geng1† Weijie Wang1†
Weijie Wang1† Liping Huang1†
Liping Huang1† Jinhong Xie1
Jinhong Xie1 Gareth J. Williams2
Gareth J. Williams2 Charlie Baker3
Charlie Baker3 Wenchong Du3*
Wenchong Du3* Jing Hua1,4*
Jing Hua1,4*Introduction: Excessive screen exposure (ESE) is a growing global public health concern. This study aims to investigate the potential association between ESE and suspected developmental coordination disorder (DCD) in Chinese pre-schoolers, with or without siblings.
Method: A retrospective cohort study was conducted, involving 126,433 children from 551 cities in China. The Little Developmental Coordination Disorder Questionnaire (LDCDQ) was employed to evaluate motor impairment in children, while parents provided information on their children’s screen time in the past year. A mixed and multi-level logistic regression model was used to analyze the associations of all screen exposure measurements from the past year with LDCDQ scores and the risk of suspected DCD.
Results: The prevalence of excessive screen exposure was 67.6% (>1 h per day) and 28.9% (>2 h per day) in Chinese pre-schoolers. One hour’s increase in weekday daily screen time, weekend daily screen time, and screen time before sleep in the past year was associated with a decreased total score of the LDCDQ (β were −0.690, −0.398, and −1.587, p < 0.001) and an increased risk of suspected DCD by 15.3%, 9.1%, and 46.8% when adjusting for the child, family and maternal health characteristics. Excessive screen exposure decreased the total LDCDQ scores by 1.335 (>1 vs. ≤1 h) and 1.162 (>2 vs. ≤2 h) and increased risks of suspected DCD by 44.0% (>1 vs. ≤1 h) and 31.1% (>2 vs. ≤2 h) with statistical significance (each p < 0.05). The stratified analysis showed that the association between screen time and LDCDQ score was stronger in children without siblings than in those with siblings.
Conclusion: The risk of suspected DCD was highest for screen time exposure before bed compared with average weekday and weekend exposures. Parents should be advised to prevent their children from using electronic screens unsupervised, especially in one-child families.
Evidence suggests that excessive screen exposure (ESE) time in early childhood is associated with child development and health (1–4). The COVID-19 pandemic has triggered a marked increase in sedentary behavior, notably excessive screen time among children, with potential long-term implications for their developmental outcomes (5). Several studies had documented that screen time in young children can be longer than 2 h per day at 30 months old in the United Kingdom (6), the United States (7), and India (8), and children at 18 and 30 months old were reported to watch more than 4 h of TV per day in a Japanese study (9). Reports also suggested that the screen exposure time varied from 21% to 98% in middle-income countries, and 10% to 93.7% in high-income countries, respectively (10).
Screen exposure time normally includes time spent watching TV, or using a smartphone, a computer, or a tablet. According to the previous literature, two standards were commonly used to define ESE, and daily screen time exceeding 1 h (9, 11–13) or 2 h (14–17) per day is generally considered excessive. ESE has been linked to delayed development of language (11, 18), negative psychosocial development, and cognitive and socioemotional development (19). Research has indicated that preschool children who engage in screen time exceeding 2 h per day display increased emotion dysregulation, diminished prosocial behavior (20, 21), elevated inattention, and hyperactivity (22, 23). Moreover, recent studies have increasingly reported associations between ESE and developmental disorders, such as Autism Spectrum Disorder (ASD) and Attention-Deficit/Hyperactivity Disorder (24–26). However, no study has examined the effects of screen time and ESE on developmental coordination disorder (DCD), a neurodevelopmental disorder which affects child motor and coordination function and occurs in 5%–6% of children (27).
In the present study, we conducted a national retrospective cohort study in preschoolers aged 3–5 years old in China, aiming to investigate the association between screen exposure time during weekdays, weekends, and before sleep in the past year with motor development and the risk of DCD. We also explored the effects of excessive screen exposure time on DCD using two cut-off standards of screen exposure (>1 h per day) (9, 11–13, 28) and >2 h per day (14–17). Additionally, the role of sibling presence in the association between screen time and suspected DCD was also examined.
Data on motor development was extracted from the Chinese National Cohort of Motor Development (CNCMD) (29). Stratified cluster sampling was used to ensure that the study participants were representative of the Chinese population. The China 2018–2019 National Census was used for stratification by geographic region, age, sex, and socioeconomic status (SES). Nurseries were invited to participate in the study. Class teachers at the nurseries which agreed to participate distributed notifications to parents to complete an online questionnaire, and researchers’ contact details were provided so parents or teachers could make contact if they had queries about the study. An online questionnaire system was used in the study for data collection.
Data were collected from 1st April 2018 to 3rd December 2019, and 188,814 pre-schoolers from 2,403 mainstream nurseries in 551 cities of China were recruited in total. A total of 129,278 children were included in the analysis of the current study (Figure 1). Informed consent has been obtained from all participants. The study was approved by the ethics committee of Shanghai First Maternity and Infant Hospital (KS18156).
Following the same measurement used in previous studies (1–4), parents were asked to provide the average time in a day in the past year their child spent watching TV, using a smartphone or computer or other tablets with a screen by answering three questions: (1). Consider the typical situation in the past whole year, how many minutes on a weekday does your child usually spend watching TV, using a smartphone, a computer, or a tablet? (2). Consider the typical situation in the past whole year, how many minutes on a weekend day does your child usually spend watching TV, using a smartphone, a computer, or a tablet? and (3). Consider the typical situation in the past whole year, how many minutes does your child usually spend watching TV, using a smartphone, a computer, or a tablet before sleep? Weekday daily screen time, weekend screen time, and screen time before sleep was also converted into hours. According to the previous literature (30, 31), the average daily time in hours a child spent in screen exposure (daily screen time) was weighted with 5/7 given to weekday screen time and 2/7 given to weekend screen time. Additionally, ESE was defined as daily screen time exceeding one (9, 11–13) and two (14–17) hours per day.
The motor performance of children was assessed using the Little Developmental Coordination Disorder Questionnaire (LDCDQ), which was developed as a screening tool for motor coordination difficulties in 3- and 4-year-old children (32) and can also be extended for use with children up to 5 years (33). The LDCDQ consists of 15 questions divided into three sub-categories: control during movement/gross motor, fine motor skills, and general coordination. Each category contains five items; for each item, parents are asked to compare the performance of their child with that of children of the same age and sex and to rate their performance on a 5-point Likert scale, with 1 = not at all relevant to my child and 5 = extremely relevant to my child. Each sub-category has a maximum score of 25. Scores are summed to give a maximum total score of 75, with higher scores indicating a higher level of motor proficiency. The LDCDQ has been demonstrated to be a valid and reliable measurement in Chinese children (34). Per previous recommendations (33, 35), we used the age- and sex-specific norms of the LDCDQ and cut-off scores based on a national sample in China to indicate suspected impairments of motor coordination (“suspected DCD” with LDCDQ ≤ 15 percentile; “probably not DCD” with LDCDQ > 15 percentile).
A wide range of child personal, family, and maternal health characteristics as potential confounders (which might be related to both screen exposure and DCD), and adjust for in the analysis (Table A1). BMI is computed by children’s height and weight [BMI = weight (kg)/height(m)] (36). Family structures were grouped into three categories: single-parent family, nuclear family, and families with more than two generations in the same household. Maternal age were grouped into three categories: “<30,” “30–34,” and “>34” years (37). Other Maternal complications were defined according to the International Classification of Diseases-Revision 10 (ICD-10), i.e., if the mother had one of the following maternal complications: vaginal bleeding during pregnancy, risk of miscarriage, use of antibiotics, use of fertility drugs, intrauterine distress, or fetal asphyxia. The daily physical activity was divided into two categories by different time duration: low level (<180 min) and high level (≥180 min) according to the National Association of Sport and Physical Education (NASPE) guidelines of the United States for preschool-aged children (aged 3–5 years).
A mixed model utilizing a random intercept (we hypothesized that there was no interaction between nursery types and the total LDCDQ scores) was used to investigate the associations of screen time with the total score and sub-scores of LDCDQ. A multi-level logistic regression model was used to determine the strength of association for different gestational ages associated with poor motor performance (“suspected DCD” was defined as LDCDQ ≤ 15th percentile; “probably not DCD” was defined as LDCDQ > 15th percentile). The nurseries as primary sampling units and other potential confounders (child personal, family, and maternal health characteristics as described above) were all considered in these models. All covariates as mentioned earlier were controlled for in the analysis. In stratified analysis, the above associations of screen time with suspected DCD in one-child and multi-child families were compared using the Z test. Analyses were carried out using LMER, GLMER procedures using R version 4.0.1. and p < 0.05 was denoted as statistically significant.
Of the 129,278 children included in the final analysis, the weekday daily screen time, the weekend daily screen time, and the screen time before sleep were 1.275, 2.584, and 0.515 h, with a standard deviation of 0.948, 1.847, and 0.506, respectively. A total of 86,728 children (67.1%) had more than 1 h of daily screen time, and 37,362 children (28.9%) had more than 2 h of daily screen exposure. The mean of the total score of LDCDQ, and the sub-scores in motor control, writing/fine motor, and general coordination were 67.817, 22.907, 22.716, and 22.194, with a standard deviation of 8.927, 3.102, 3.154, and 3.218, respectively. Per total LDCDQ scores, 19,969 children (15.447%) were defined as suspected DCD and 109,309 children (84.553%) were defined as probably not DCD The child, family characteristics and maternal health during pregnancy in the study population were shown in Table 1.

Table 1. The child, family characteristics and maternal health during pregnancy in the study population (n = 129,278).
The results showed that 1 h’s increase in weekday daily screen time, weekend daily screen time, and screen time before sleep was associated with a decreased total score of the LDCDQ (β were −0.690, −0.398, and −1.587, p < 0.001) when adjusting for physical activity and family, maternal and child’s characteristics. One hour’s increase in weekday daily screen time, weekend daily screen time, and screen time before sleep was associated with all three sub-scores of the LDCDQ: the sub-score of motor control (adjusted β = −0.179, −0.101, and −0.480, each p < 0.001), writing/fine motor (adjusted β = −0.265, −0.151, and −0.583, each p < 0.001), and general coordination (adjusted β = −0.246, −0.147, and −0.526, each p < 0.001) when adjusting for all the covariates.
ESE in the past year was also associated with a decreased total score of the LDCDQ, sub-score of motor control, writing/fine motor, and general coordination (>1 h: adjusted β = −1.335, −0.345, −0.534, and −0.457; >2 h: adjusted β = −1.162, −0.278, −0.453. and −0.432, each p < 0.001). The crude and adjusted β and 95% CI were shown in Table 2.
One hour’s increase in weekday daily screen time, weekend daily screen time, and screen time before sleep in the past year was associated with an increased risk of suspected DCD by 15.3%, 9.1%, and 46.8% when adjusting for physical activity and family, maternal and child’s characteristics. ESE increased the risk of suspected DCD by 44.0% (>1 vs. ≤1 h) and 31.1% (>2 vs. ≤2 h) when adjusting for the same covariates. The crude and adjusted OR and 95%CI were shown in Table 3.
The stratified analysis showed that the statistically significant associations of screen time with the LDCDQ scores and suspected DCD remained in both one-child and multi-child families (Figures 2, 3). However, the association between prolonged screen time (weekday, before sleep) and the LDCDQ scores (total score, motor control, and general coordination) in one-child families were stronger than those in multi-child families with statistical significance (each p < 0.05).

Figure 2. Distribution of 551 participant cities from 31 provinces/municipalities/autonomous regions in mainland China.
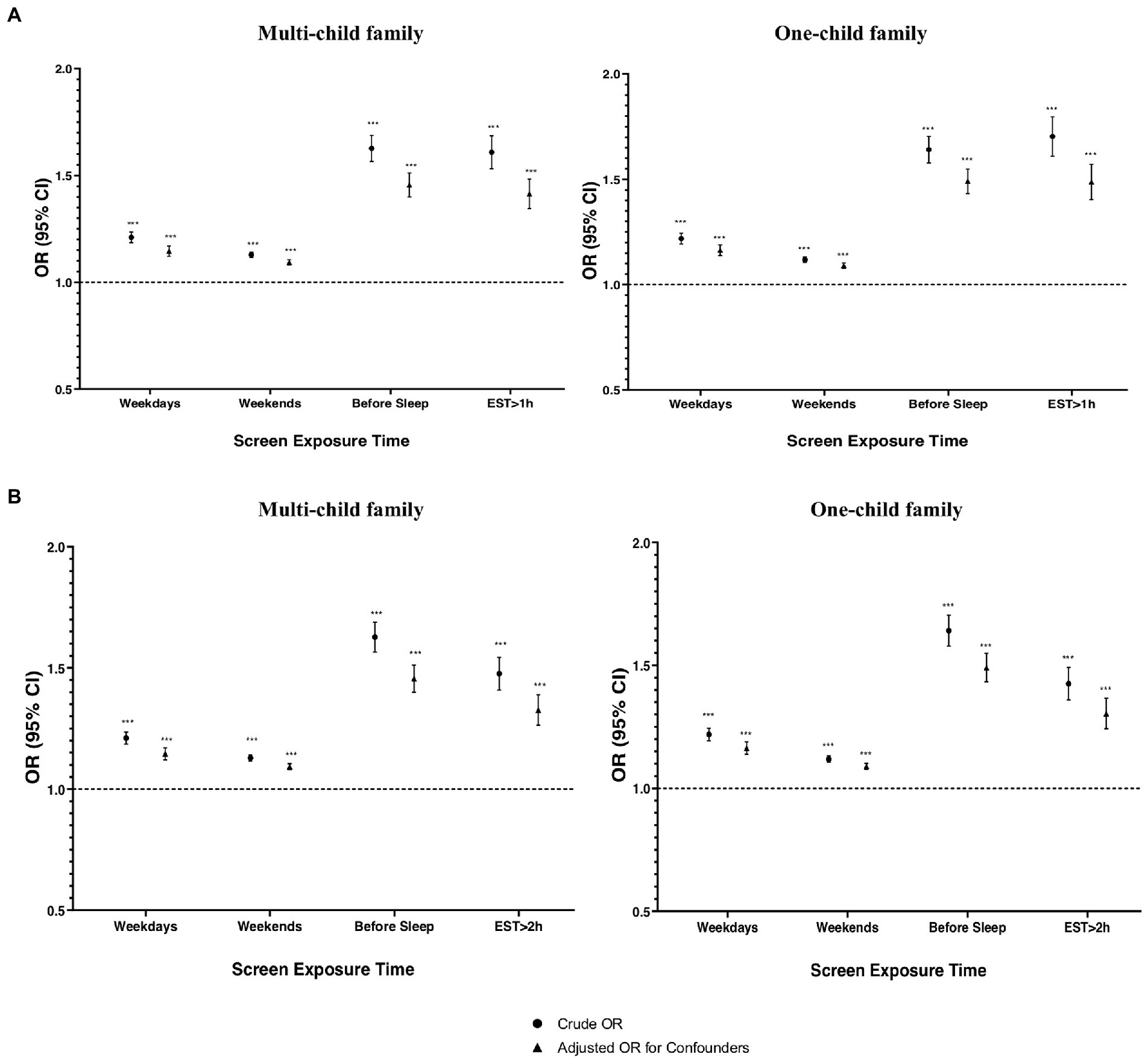
Figure 3. The association between screen time and suspected DCD in multi child and one-child family when adjusting or not adjusting for child and family characteristics and maternal health during pregnancy (n = 129,278). (A) Excessive screen exposure is defined as more than 1 h per day. (B) Excessive screen exposure is defined as more than 2 h per day.
The associations of screen time and ESE with the total score of LDCDQ (Figure A1) and risk of suspected DCD (Figure A2) remained robust before and after adjusting for the covariates. The strengths of these results did not change significantly when adjusting for the covariates, respectively (Figures A1, A2).
The present study examined the association between screen time and DCD, using a large nationally representative sample. There were significant associations between all measurements of screen exposure time in the past year with motor impairment measurements and the risk of DCD. The strongest association was found for screen exposure time before sleep when compared to weekday daily screen time and weekend daily screen time. Additionally, the association between screen exposure time and the risk of DCD was stronger in children without siblings than in those with siblings.
We found that longer weekday and weekend daily screen time in the past year was associated with negatively affected motor performance including gross motor, fine motor, and balance when adjusting for a wide range of confounding factors including physical activities. Previous studies have reported associations between screen time and fundamental motor skills (38, 39), and associations between prolonged screen exposure time and both decreased physical activity engagement and fine and gross motor performances. Additionally, screen exposure time has been reported to negatively relate to attention-related patterns generated by (EEG) in preschool children (40). While complicated and distinct, there are specific relationships between motor performance and cognitive processes (41), due to the close connections between brain development and motor abilities (42), which are consequential for early childhood development. With neuroscientific evidence having linked ESE to the delayed development of cognitive processes (43, 44), we can infer that ESE may also affect motor development.
Our results also suggested an association between prolonged screen exposure time on weekdays and weekends in the past year and increased risk of DCD. Increased screen exposure time has previously been associated with lower microstructural integrity of brain white matter tracts in preschool-aged children (45). Children with DCD also showed significant brain differences in motor and sensorimotor white matter pathways when compared with controls (46, 47). Furthermore, evidence suggested that higher screen exposure is independently associated with lower serum Brain-derived neurotrophic factor (BDNF) levels (48). The BDNF genotype regulates both the inhibitory and excitatory circuits in the human primary motor cortex which mostly relate to motor controls (49). Therefore, ESE might lead to a higher risk of motor impairments through the change in the microstructural integrity of the brain. It should be noted that the association we found between ESE and the risk of DCD was stronger using the WHO recommendation (>1 h per day) compared to exceeding 2 h per day. Exceeding 1 h of screen time in a day increased the vulnerability in physical health and well-being, social competence, and communication skills among other domains of developmental health (50). Using 1 h as the excessive screen exposure daily cut-off standard showed a higher prediction power compared to 2 h. Our study provides new evidence to support that one-hour maximum screen time per day is an optimal recommendation for pre-schoolers.
One of our important findings is that the screen time before sleep had the strongest association between the LDCDQ score and the risk of suspected DCD, compared to weekday and weekend daily screen time. One possible explanation is the effect of screen exposure on melatonin. Exposure to blue light from backlit electronic screens has been found to inhibit melatonin production (51). Melatonin has been found to improve motor coordination in ethanol-hungover mice (52), and treatment with melatonin could promote motor performance in nocturnal animals (53). Additionally, prolonged screen exposure was associated with later bedtimes and shorter sleep duration in pre-schoolers (4), which can also lead to circadian discrepancy (54) and decreased motor performance during the day (55).
With the relaxation of China’s one-child policy in 2016, there has been sustained interest in the role of siblings in a multi-child dynamic on child development. A stronger association between prolonged screen time and motor competence was found in one-child families in the current study compared to multi-child families. Previous studies found that being the only child in a family is a risk factor for DCD and motor development delay (56, 57), and suggested the positive influence of the presence of a sibling on motor development. Studies suggest that older siblings can provide good role models that younger children can imitate (58), which can then, therefore, help to decrease the time needed by parents to teach basic motor skills to the younger ones. The presence of siblings in the family context is especially influential for motor development after 24 months of age because siblings provide cooperative activities such as play and challenges that improve cognitive, social, emotional, and physical development (59), which may also moderate the negative influence of screen exposure.
There are several strengths to this study, one is the size and cross-sectoral nature of the sample. This was the first study based on a large nationally representative sample and is also one of the few that examined the sibling effect of screen exposure on a neurodevelopmental disorder. Limitations of the current study included that self-reported information on childhood adversities may produce a differential recall bias and result in an inaccurate estimation of total and direct effects. However, the majority of parents do not have awareness of motor impairment or DCD (60) and children with DCD are rarely diagnosed in China (61). Therefore, the two groups with parents of children with and without suspected DCD in the current study were less likely to have different recalling accuracy when providing the information of their children, and misclassification of the two groups is unlikely to be different. Therefore, the possibility of differential recall bias can be considered minimal in the current study. Moreover, it is often insufficient to control for confounding factors in a retrospective study. However, we included a wide range of confounders to adjust for in the analysis in the current study, although some potential confounders such as the presence of another child in the family with a physical or neurodevelopmental delay could also be controlled for because it could also affect the motor development of children. It should also be noticed that although we asked the parents to recall the general screen exposure time on a typical day in the past year, the current study was a retrospective cohort study, and our research results cannot support any causal relationship among variables. Additionally, we did not use a validated scale to assess screen exposure in our study. Further research with a longitudinal design using a scaled measurement might be needed to explain the mechanisms linking screen exposure and DCD.
Digital devices have been used more widely by young children to receive information, and parents should be advised to prevent their children from using the screen excessively which can affect their normal neurodevelopment. Limiting screen time exposure could form an integral part of child healthcare, which can be achieved by the combined participation of parents, guardians, and healthcare professionals. Future studies should focus on effective practices to reduce screen time in children.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The study was approved by the Ethics Committee of Shanghai First Maternity and Infant Hospital (KS18156). Written informed consent to participate in this study was provided by the participants’ legal guardian/next of kin.
WD and JH: integrity of the data, accuracy of the data analysis, and concept and design. SG and JH: drafting of the manuscript. SG, WW, LH, and JX: acquisition, analysis, and interpretation of data. JH, WD, GW, and CB: critical revision of the manuscript for important intellectual content. SG, JH, and WD: administrative, technical, or material support and obtained funding. All authors contributed to the article and approved the submitted version.
This study was supported by the National Natural Science Foundation of China (81673179), the Science and Technology Commission of Shanghai Municipality (21DZ2202000 and 19140903100), Shanghai Municipal Health Commission (2020YJZX0213), and Shanghai Pudong New Area Health Commission (PW2020D-11).
We are grateful to the class teachers in all participating kindergartens for distributing the notification to parents to complete the online questionnaire.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2023.1152321/full#supplementary-material
1. Kushima, M, Kojima, R, Shinohara, R, Horiuchi, S, Otawa, S, Ooka, T, et al. Association between screen time exposure in children at 1 year of age and autism Spectrum disorder at 3 years of age: the Japan environment and Children’s study. JAMA Pediatr. (2022) 176:384–91. doi: 10.1001/jamapediatrics.2021.5778
2. Vaidyanathan, S, Manohar, H, Chandrasekaran, V, and Kandasamy, P. Screen time exposure in preschool children with ADHD: a cross-sectional exploratory study from South India. Indian J Psychol Med. (2021) 43:125–9. doi: 10.1177/0253717620939782
3. Sari, BA, Taner, HA, and Kaya, ZT. Screen media exposure in pre-school children in Turkey: the relation with temperament and the role of parental attitudes. Turk J Pediatr. (2021) 63:818–31. doi: 10.24953/turkjped.2021.05.010
4. Hiltunen, P, Leppanen, MH, Ray, C, Maatta, S, Vepsalainen, H, Koivusilta, L, et al. Relationship between screen time and sleep among Finnish preschool children: results from the DAGIS study. Sleep Med. (2021) 77:75–81. doi: 10.1016/j.sleep.2020.11.008
5. Musa, S, Elyamani, R, and Dergaa, I. COVID-19 and screen-based sedentary behaviour: systematic review of digital screen time and metabolic syndrome in adolescents. PLoS One. (2022) 17:e0265560. doi: 10.1371/journal.pone.0265560
6. Barber, SE, Kelly, B, Collings, PJ, Nagy, L, Bywater, T, and Wright, J. Prevalence, trajectories, and determinants of television viewing time in an ethnically diverse sample of young children from the UK. Int J Behav Nutr Phys Act. (2017) 14:88. doi: 10.1186/s12966-017-0541-8
7. Rideout, V, and Robb, MB. The common sense census: Media use by kids age zero to eight. (2020) San Francisco, CA: Common Sense Media.
8. Shah, RR, Fahey, NM, Soni, AV, Phatak, AG, and Nimbalkar, SM. Screen time usage among preschoolers aged 2-6 in rural Western India: a cross-sectional study. J Fam Med Prim Care. (2019) 8:1999–2002. doi: 10.4103/jfmpc.jfmpc_206_19
9. Cheng, S, Maeda, T, Yoichi, S, Yamagata, Z, and Tomiwa, K. Early television exposure and children’s behavioral and social outcomes at age 30 months. J Epidemiol. (2010) 20:S482–9. doi: 10.2188/jea.je20090179
10. Kaur, N, Gupta, M, Malhi, P, and Grover, S. Screen time in under-five children. Indian Pediatr. (2019) 56:773–88. doi: 10.1007/s13312-019-1638-8
11. Byeon, H, and Hong, S. Relationship between television viewing and language delay in toddlers: evidence from a Korea national cross-sectional survey. PLoS One. (2015) 10:e0120663. doi: 10.1371/journal.pone.0120663
12. Carson, V, Spence, JC, Cutumisu, N, and Cargill, L. Association between neighborhood socioeconomic status and screen time among pre-school children: a cross-sectional study. BMC Public Health. (2010) 10:367. doi: 10.1186/1471-2458-10-367
13. Emond, JA, Tantum, LK, Gilbert-Diamond, D, Kim, SJ, Lansigan, RK, and Neelon, SB. Household chaos and screen media use among preschool-aged children: a cross-sectional study. BMC Public Health. (2018) 18:1210. doi: 10.1186/s12889-018-6113-2
14. Kourlaba, G, Kondaki, K, Liarigkovinos, T, and Manios, Y. Factors associated with television viewing time in toddlers and preschoolers in Greece: the GENESIS study. J Public Health. (2009) 31:222–30. doi: 10.1093/pubmed/fdp011
15. Wu, CS, Fowler, C, Lam, WY, Wong, HT, Wong, CH, and Yuen, LA. Parenting approaches and digital technology use of preschool age children in a Chinese community. Ital J Pediatr. (2014) 40:44. doi: 10.1186/1824-7288-40-44
16. Downing, KL, Hinkley, T, Salmon, J, Hnatiuk, JA, and Hesketh, KD. Do the correlates of screen time and sedentary time differ in preschool children? BMC Public Health. (2017) 17:285. doi: 10.1186/s12889-017-4195-x
17. Jago, R, Stamatakis, E, Gama, A, Carvalhal, IM, Nogueira, H, Rosado, V, et al. Parent and child screen-viewing time and home media environment. Am J Prev Med. (2012) 43:150–8. doi: 10.1016/j.amepre.2012.04.012
18. Lin, LY, Cherng, RJ, Chen, YJ, Chen, YJ, and Yang, HM. Effects of television exposure on developmental skills among young children. Infant Behav Dev. (2015) 38:20–6. doi: 10.1016/j.infbeh.2014.12.005
19. Pagani, LS, Fitzpatrick, C, Barnett, TA, and Dubow, E. Prospective associations between early childhood television exposure and academic, psychosocial, and physical well-being by middle childhood. Arch Pediatr Adolesc Med. (2010) 164:425–31. doi: 10.1001/archpediatrics.2010.50
20. Stiglic, N, and Viner, RM. Effects of screentime on the health and well-being of children and adolescents: a systematic review of reviews. BMJ Open. (2019) 9:e023191. doi: 10.1136/bmjopen-2018-023191
21. Domingues-Montanari, S. Clinical and psychological effects of excessive screen time on children. J Paediatr Child Health. (2017) 53:333–8. doi: 10.1111/jpc.13462
22. Landhuis, CE, Poulton, R, Welch, D, and Hancox, RJ. Does childhood television viewing lead to attention problems in adolescence? Results from a prospective longitudinal study. Pediatrics. (2007) 120:532–7. doi: 10.1542/peds.2007-0978
23. Wu, X, Tao, S, Rutayisire, E, Chen, Y, Huang, K, and Tao, F. The relationship between screen time, nighttime sleep duration, and behavioural problems in preschool children in China. Eur Child Adolesc Psychiatry. (2017) 26:541–8. doi: 10.1007/s00787-016-0912-8
24. Hill, MM, Gangi, D, Miller, M, Rafi, SM, and Ozonoff, S. Screen time in 36-month-olds at increased likelihood for ASD and ADHD. Infant Behav Dev. (2020) 61:101484. doi: 10.1016/j.infbeh.2020.101484
25. Tandon, PS, Sasser, T, Gonzalez, ES, Whitlock, KB, Christakis, DA, and Stein, MA. Physical activity, screen time, and sleep in children with ADHD. J Phys Act Health. (2019) 16:416–22. doi: 10.1123/jpah.2018-0215
26. Tamana, SK, Ezeugwu, V, Chikuma, J, Lefebvre, DL, Azad, MB, Moraes, TJ, et al. Screen-time is associated with inattention problems in preschoolers: results from the CHILD birth cohort study. PLoS One. (2019) 14:e0213995. doi: 10.1371/journal.pone.0213995
27. Blank, R, Barnett, AL, Cairney, J, Green, D, Kirby, A, Polatajko, H, et al. International clinical practice recommendations on the definition, diagnosis, assessment, intervention, and psychosocial aspects of developmental coordination disorder. Dev Med Child Neurol. (2019) 61:242–85. doi: 10.1111/dmcn.14132
28. McCarthy, M. Cut children’s screen time to less than two hours a day, US pediatricians say. BMJ. (2013) 347:f6573. doi: 10.1136/bmj.f6573
29. Hua, J, Barnett, AL, Williams, GJ, Dai, X, Sun, Y, Li, H, et al. Association of Gestational age at birth with subsequent suspected developmental coordination disorder in early childhood in China. JAMA Netw Open. (2021) 4:e2137581. doi: 10.1001/jamanetworkopen.2021.37581
30. Doherty, M, Santiago-Torres, M, Cui, Y, Schoeller, D, LaRowe, T, Adams, A, et al. The association between screen time and weight status in Hispanic children. BAOJ Obes Weight Loss Manag. (2015) 1:001. Epub 2015 Sep 4.
31. Pedersen, J, Rasmussen, MG, Olesen, LG, Klakk, H, Kristensen, PL, and Grontved, A. Recreational screen media use in Danish school-aged children and the role of parental education, family structures, and household screen media rules. Prev Med. (2022) 155:106908. doi: 10.1016/j.ypmed.2021.106908
32. Rihtman, T, Wilson, BN, and Parush, S. Development of the little developmental coordination disorder questionnaire for preschoolers and preliminary evidence of its psychometric properties in Israel. Res Dev Disabil. (2011) 32:1378–87. doi: 10.1016/j.ridd.2010.12.040
33. Cantell, M, Houwen, S, and Schoemaker, M. Age-related validity and reliability of the Dutch little developmental coordination disorder questionnaire (LDCDQ-NL). Res Dev Disabil. (2019) 84:28–35. doi: 10.1016/j.ridd.2018.02.010
34. Geng, S, Dai, X, Wang, T, Cui, W, and Hua, J. The preliminary study on the reliability and validity of the Chinese version of the little developmental coordination disorder questionnaire [journal article]. J Clin Pediatr. (2020) 38:921–4. doi: 10.3969/j.issn.1000-3606.2020.12.010
35. Wilson, BN, Creighton, D, Crawford, SG, Heath, JA, Semple, L, Tan, B, et al. Psychometric properties of the Canadian little developmental coordination disorder questionnaire for preschool children. Phys Occup Ther Pediatr. (2015) 35:116–31. doi: 10.3109/01942638.2014.980928
36. Consultation WHOE. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. (2004) 363:157–63. doi: 10.1016/S0140-6736(03)15268-3
37. Teng, X, Shane, MI, and Pan, S. The changing situation about maternal age, risk factors and pregnancy outcomes after the two-child policy: a retrospective cohort study. Ann Palliat Med. (2020) 9:824–34. doi: 10.21037/apm.2020.04.27
38. Webster, EK, Martin, CK, and Staiano, AE. Fundamental motor skills, screen-time, and physical activity in preschoolers. J Sport Health Sci. (2019) 8:114–21. doi: 10.1016/j.jshs.2018.11.006
39. Martins, CML, Bandeira, PFR, Lemos, N, Bezerra, TA, Clark, CCT, Mota, J, et al. A network perspective on the relationship between screen time, executive function, and fundamental motor skills among preschoolers. Int J Environ Res Public Health. (2020) 17:8861. doi: 10.3390/ijerph17238861
40. Zivan, M, Bar, S, Jing, X, Hutton, J, Farah, R, and Horowitz-Kraus, T. Screen-exposure and altered brain activation related to attention in preschool children: an EEG study. Trends Neurosci Educ. (2019) 17:100117. doi: 10.1016/j.tine.2019.100117
41. Stockel, T, and Hughes, CM. The relation between measures of cognitive and motor functioning in 5- to 6-year-old children. Psychol Res. (2016) 80:543–54. doi: 10.1007/s00426-015-0662-0
42. Diamond, A. Close interrelation of motor development and cognitive development and of the cerebellum and prefrontal cortex. Child Dev. (2000) 71:44–56. doi: 10.1111/1467-8624.00117
43. Supanitayanon, S, Trairatvorakul, P, and Chonchaiya, W. Screen media exposure in the first 2 years of life and preschool cognitive development: a longitudinal study. Pediatr Res. (2020) 88:894–902. doi: 10.1038/s41390-020-0831-8
44. John, JJ, Joseph, R, David, A, Bejoy, A, George, KV, and George, L. Association of screen time with parent-reported cognitive delay in preschool children of Kerala, India. BMC Pediatr. (2021) 21:73. doi: 10.1186/s12887-021-02545-y
45. Hutton, JS, Dudley, J, Horowitz-Kraus, T, DeWitt, T, and Holland, SK. Associations between screen-based media use and brain white matter integrity in preschool-aged children. JAMA Pediatr. (2020) 174:e193869. doi: 10.1001/jamapediatrics.2019.3869
46. Brown-Lum, M, Izadi-Najafabadi, S, Oberlander, TF, Rauscher, A, and Zwicker, JG. Differences in white matter microstructure among children with developmental coordination disorder. JAMA Netw Open. (2020) 3:e201184. doi: 10.1001/jamanetworkopen.2020.1184
47. Izadi-Najafabadi, S, and Zwicker, JG. White matter changes with rehabilitation in children with developmental coordination disorder: a randomized controlled trial. Front Hum Neurosci. (2021) 15:673003. doi: 10.3389/fnhum.2021.673003
48. Goldfield, GS, Cameron, JD, Sigal, RJ, Kenny, GP, Holcik, M, Prud’homme, D, et al. Screen time is independently associated with serum brain-derived neurotrophic factor (BDNF) in youth with obesity. Appl Physiol Nutr Metab. (2021) 46:1083–90. doi: 10.1139/apnm-2020-0756
49. Sasaki, R, Otsuru, N, Miyaguchi, S, Kojima, S, Watanabe, H, Ohno, K, et al. Influence of brain-derived Neurotrophic factor genotype on short-latency afferent inhibition and motor cortex metabolites. Brain Sci. (2021) 11:395. doi: 10.3390/brainsci11030395
50. Glascoe, FP, Gellasch, P, and Chen, V. When do clinicians decide to screen children for mental health-behavioral-developmental delays/disorders: is it time to reconsider policy recommendations? J Pediatr. (2019) 206:248–55. doi: 10.1016/j.jpeds.2018.08.084
51. Cajochen, C, Frey, S, Anders, D, Spati, J, Bues, M, Pross, A, et al. Evening exposure to a light-emitting diodes (LED)-backlit computer screen affects circadian physiology and cognitive performance. J Appl Physiol. (2011) 110:1432–8. doi: 10.1152/japplphysiol.00165.2011
52. Karadayian, AG, Bustamante, J, Czerniczyniec, A, Cutrera, RA, and Lores-Arnaiz, S. Effect of melatonin on motor performance and brain cortex mitochondrial function during ethanol hangover. Neuroscience. (2014) 269:281–9. doi: 10.1016/j.neuroscience.2014.03.062
53. Poulos, SG, and Borlongan, CV. Artificial lighting conditions and melatonin alter motor performance in adult rats. Neurosci Lett. (2000) 280:33–6. doi: 10.1016/s0304-3940(99)00997-0
54. Lan, QY, Chan, KC, Yu, KN, Chan, NY, Wing, YK, Li, AM, et al. Sleep duration in preschool children and impact of screen time. Sleep Med. (2020) 76:48–54. doi: 10.1016/j.sleep.2020.09.024
55. Gradisar, M, Wolfson, AR, Harvey, AG, Hale, L, Rosenberg, R, and Czeisler, CA. The sleep and technology use of Americans: findings from the National Sleep Foundation’s 2011 sleep in America poll. J Clin Sleep Med. (2013) 9:1291–9. eng. doi: 10.5664/jcsm.3272
56. Du, W, Ke, L, Wang, Y, Hua, J, Duan, W, and Barnett, AL. The prenatal, postnatal, neonatal, and family environmental risk factors for developmental coordination disorder: a study with a national representative sample. Res Dev Disabil. (2020) 104:103699. doi: 10.1016/j.ridd.2020.103699
57. Dai, X, Williams, G, Lin, S, Baker, C, Wu, M, Du, W, et al. The sibling effect on neurodevelopment of preschoolers under China’s newly relaxed child policy: a national retrospective cohort study. Front Psychol. (2022) 13:988622. doi: 10.3389/fpsyg.2022.988622
58. Franca, TLB, Medeiros, WR, Souza, NL, Longo, E, Pereira, SA, Franca, TBO, et al. Growth and development of children with microcephaly associated with congenital Zika virus syndrome in Brazil. Int J Environ Res Public Health. (1990) 15:1990. doi: 10.3390/ijerph15091990
59. Rebelo, M, Serrano, J, Duarte-Mendes, P, Paulo, R, and Marinho, DA. Effect of siblings and type of delivery on the development of motor skills in the first 48 months of life. Int J Environ Res Public Health. (2020) 17:3864. doi: 10.3390/ijerph17113864
60. Hunt, J, Zwicker, JG, Godecke, E, and Raynor, A. Awareness and knowledge of developmental coordination disorder: a survey of caregivers, teachers, allied health professionals and medical professionals in Australia. Child Care Health Dev. (2021) 47:174–83. doi: 10.1111/cch.12824
Keywords: excessive screen exposure, screen time before sleep, suspected DCD, one-child family, preschoolers
Citation: Geng S, Wang W, Huang L, Xie J, Williams GJ, Baker C, Du W and Hua J (2023) Association between screen time and suspected developmental coordination disorder in preschoolers: A national population-based study in China. Front. Public Health. 11:1152321. doi: 10.3389/fpubh.2023.1152321
Received: 27 January 2023; Accepted: 09 March 2023;
Published: 27 March 2023.
Edited by:
Stamatios Papadakis, University of Crete, GreeceReviewed by:
Ricardo Adrian Nugraha, Airlangga University, IndonesiaCopyright © 2023 Geng, Wang, Huang, Xie, Williams, Baker, Du and Hua. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Wenchong Du, dml2aWVubmUuZHVAbnR1LmFjLnVr; Jing Hua, amluZ2h1YUB0b25namkuZWR1LmNu
†These authors have contributed equally to this work and share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.