- 1School of Nursing, Xinjiang Medical University, Urumqi, Xinjiang, China
- 2Breast Surgical Department, Oncology Center, The First Affiliated Hospital of Xinjiang Medical University, Urumqi, China
- 3School of Public Health, Xinjiang Medical University, Urumqi, Xinjiang, China
- 4Nursing Supervision Center, The First Affiliated Hospital of Xinjiang Medical University, Urumqi, China
- 5Intensive Care Unit (ICU), The First Affiliated Hospital of Xinjiang Medical University, Urumqi, China
Introduction: Patients with breast cancer (BC) after surgery are prone to negative physiological and psychosocial discomforts which cause the poor quality of life (QoL) among the patients. Therefore, how to improve the disease management ability of BC patients and to alleviate these cancer-related negative experience are particularly important. This study purpose to explore the potential effects of personalized care based on OPT model on the perceived control and the QoL among patients with BC, and to provide effective clinical nursing intervention for BC patients.
Methods: In this study, nonsynchronous controlled experiments were carried out on patients with BC, and the patients were randomly allocated to the control (n = 40) and intervention (n = 40) groups. The patients in the control group were given routine care; while the patients in the intervention group were given personalized care based on OPT model. The perceived control ability and QoL of the two groups were measured before and after the intervention.
Results: There were no significant differences in the total score of cancer experience and control efficacy of BC patients between the control group (61.15 ± 5.659, 41.80 ± 4.702) and the intervention group (60.58 ± 7.136, 42.15 ± 5.550) before intervention (p > 0.05). After the intervention, the total score of cancer experience in the intervention group (54.80 ± 8.519) was significantly lower than that in the control group (59.575 ± 7.331), with significant differences (p < 0.05). The total score of control efficacy in the intervention group (49.78 ± 6.466) was significantly higher than that in the control group (43.32 ± 6.219), with significant differences (p < 0.05). Compared with the control group, patients in intervention groups showed significant improvement in QoL after the intervention (p < 0.05).
Conclusion: Personalized care based on OPT model plays a significant role in improving the level of perceived control and the QoL among patients with BC.
Clinical Trial Registration: www.chictr.org.cn, ChiCTR2300069476.
Introduction
Breast cancer (BC) is the leading malignancy in women around the world with 2.3 million new cases per year (1). In recent years, the incidence of BC in China has been increasing year by year (2). Thus the treatment of BC is facing significant challenges. Breast cancer is characterized by four main different types (Luminal A, Luminal B, HER-2-positive and TNBC) based on their expressions in estrogen (ER), progesterone (PR), human epidermal growth factor receptor-2(HER-2) and Ki67. According to different types of BC patients, the treatment method is different (3). The main treatments of BC are surgery plus adjuvant treatment, such as chemotherapy, radiotherapy, endocrine therapy and hormone therapy (4, 5). With advances in cancer treatment and early disease detection, the survival rates of patients with BC have increased. The efficacy of BC treatment has improved over the years and now gradually becoming available in developing countries, whereas it is widely accessible in most developed nations (6). However, these treatments can also cause adverse effects, including pain, fatigue and sleep disorders (7–10). He (11) found that more than 84% of Chinese patients with BC who received chemotherapy experience these symptoms, such as fatigue, sleep disturbance, and depression. These symptoms can significantly exerts a negative impact on the course and effectiveness of the patient’s treatment, affecting cancer-related morbidity and mortality, as well as quality of life, especially in the period after surgery (12, 13).
Breasts are emphasized by the society as a symbol of femininity, motherhood and sexuality. Patients with BC after surgery are prone to negative psychology such as inferiority complex, anxiety, hopelessness, depression, reduced sexual attraction and suicide due to the absence of a body part (breast) and fear of death (9). Therefore, how to improve the disease management ability of BC patients and promote their adaptability to the disease is particularly important.
Perceived control is an individual’s subjective perception, feeling or belief in control (14, 15), as an individual’s ability to maintain or recover relatively stable psychological and physical functioning during or after exposure to significant stressful life events (16–18). Barez (19) suggest that perceived control could be used as an early predictor of psychological adjustment to illness. Low level of perceived control have been linked to a variety of symptoms: higher anxiety (20), greater panic disorder severity and greater obsessive–compulsive symptoms (21). High level of perceived control helps patients develop a positive attitude towards their health and cope with their illness, thus it is associated with enhancing the effectiveness of treatments and improving patients’ QoL (17). Perceived control is not a stable, and it is susceptible to change. The life-threatening nature of the cancer disease and the extensive treatment modalities with uncertain outcomes of the disease may challenge one’s perceived control (16). On the other hand, there are evidences that it is possible to increase the sense of control with appropriate guidance and intervention.
Many researchers have carried out a series of research work to improve the level of perceived control and the QoL of patients with BC, such as psychological education intervention (22–26), nursing self-care educational intervention (27) and Web/or telephone intervention (28–31), physical activities (11, 32–35), the appearance care (36), self-disclosure intervention (37), community based intervention (38). Although these projects have achieved satisfactory results, there are few comprehensive methods including postoperative physical, psychological and social rehabilitation.
OPT theoretical model (39): Outcome-Present state Test(OPT)model is a recurrent, nonlinear clinical reasoning model. It emphasizes that nurses must repeatedly compare the evaluation data of patients’ current state and expected outcome state, constantly reflect on the current situation and problems, outcomes and measures, so as to make the best individualized nursing intervention and serves (40, 41). This OPT model requires nurses to constantly reflect on the situation and problems, as well as the results of patients, in order to make the best personalized nursing decisions. The personalized care model (42–44) has a positive effect on the nurses’ caring ability, not only to help build great relationships between nurses and patients but also to enhance the patients’ satisfaction and level of perceived control, enable them to actively participate in healthy behaviors, and improve their QoL.
This study was conducted to develop and investigate the effects of the personalized nursing intervention on the perceived control and QoL of patients with BC. The novel personalized nursing interventions were developed based on OPT model which deeply implement the “patient-centered” as nursing service concept, break the conventional nursing inherent mode, emphasize the important role of patients’ needs in nursing service. In this study, the nursing model consists of specific interventions such as Supportive Care Intervention, Psychological Health Education, Chinese Medicine Foot Bath Combined with Massage and Progressive Muscle Relaxation Training. The BC patients were able to choose the appropriate nursing intervention under the guidance of the medical staff. We hypothesized that the nursing intervention model could significantly improve patients’ level of perceived control and QoL. This study provides a reference for clinical nursing of BC patients undergoing surgery and has significant application value.
Methods
Design
A randomized controlled trial design was used in the study. The protocol was reviewed and approved by the Human Research Ethics Committee of the First Affiliated Hospital of Xinjiang Medical University. The study flow diagram is illustrated in Figure 1.
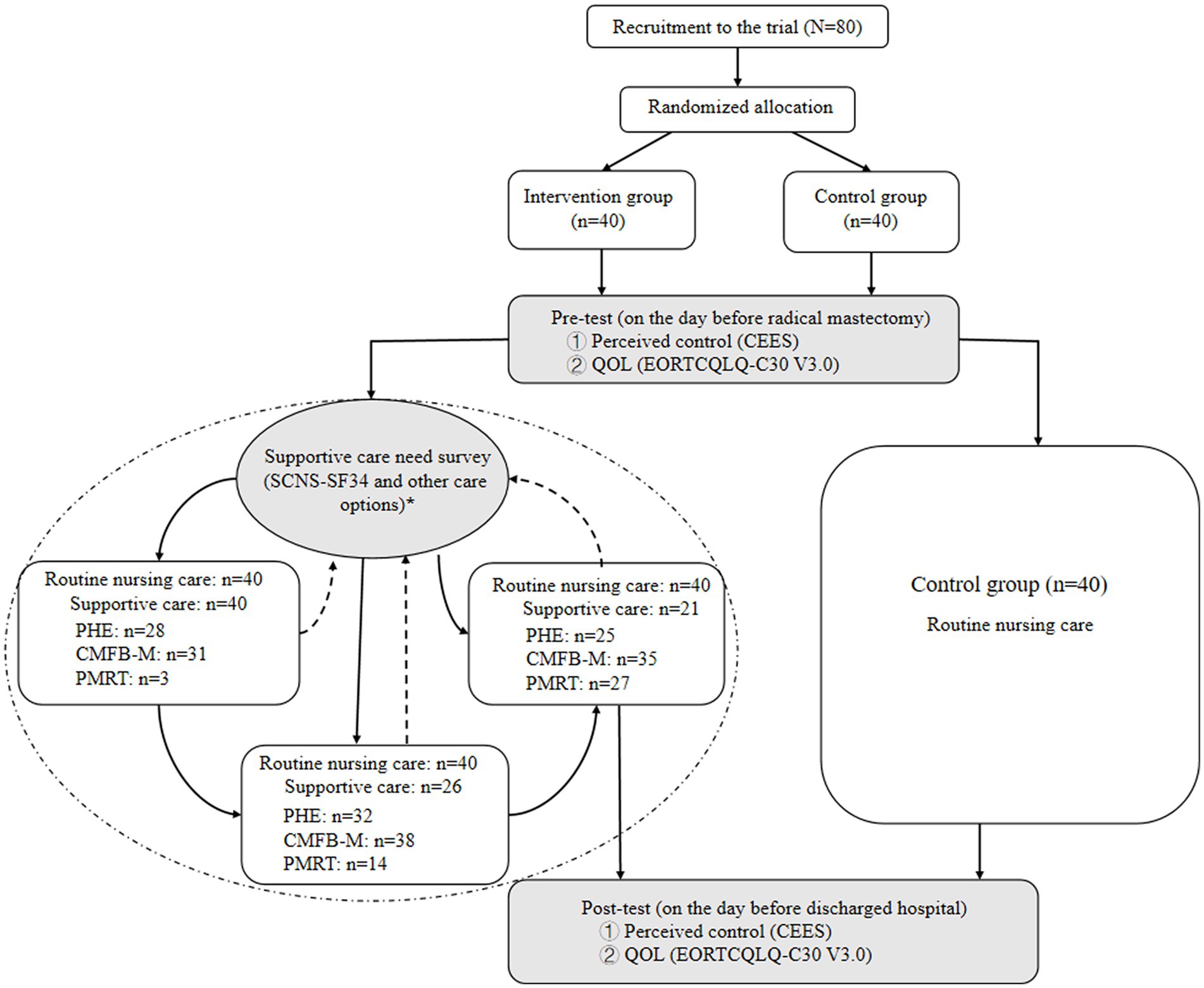
Figure 1. Flow chart of the personalized care program for patients with BC PHE: Psychological health education (afternoon 4 p.m.–6 p.m.Once every 3 days for 1 h) CMFB-M: Chinese medicine foot bath combined with massage (evening 21–22:30 for 30 min) PMRT: Progressive muscle relaxation training (early morning 8 a.m.–10 a.m for 30 min).
Setting
The trial was conducted in the breast surgical department of oncology center of the first affiliated hospital of Xinjiang Medical University, Urumqi, China.
Participants
In this study, information about the study was given and informed consent was obtained from all the patients who agreed to participate in the study. Forty hospitalized patients with BC between December 2020 and May 2021 were selected as the control group; 40 patients with BC between June 2021 and December 2021 were selected as the intervention group. Patient inclusion criteria: (1) All patients were diagnosed as breast invasive ductal carcinoma by surgical pathology, and received modified radical mastectomy for the first time; (2) Combined with chemotherapy, radiotherapy, targeted drug therapy, endocrine therapy, etc. (3) Normal cognitive function and ability to cooperate with the study; (4) 30 ≤ age ≤ 82 years old; (5) Informed consent was obtained from all patients. Patient exclusion criteria: (1) Patients with severe heart, brain, liver and kidney function diseases; (2) Other cancers such as cervical cancer; (3) Infectious diseases; (4) Limb dysfunction; (5) Mental diseases; (6) Pregnant or lactating women.
Statistical analysis and data analysis
The g-power 3.1 software was used for calculation, the t-test test method is selected, α is taken as 0.05, the effect value power is taken as 0.8, and the effect quantity D is 0.5. Using the bilateral test method, the sample size required for this study is 40 people in each group, and a total of 80 people.
The questionnaires were numbered in turn, and the data were recorded in Excel document after double check. After the data were checked again, they were imported into SPSS26.0 statistical software for data analysis. p < 0.05 means that the difference is statistically significant. (1) Patients’ general information, Supportive Care Need Survey Short-Form, (SCNS-SF34) (45), Cancer Experience and Efficacy Scale (CEES) (46), European Organization for Research and Treatment of Cancer Quality of Life Questionnaire Core 30 (EORTCQLQ-C30 V3.0) (47) scores were statistically described by frequency, percentage, c ± s. (2) Chi-square test or nonparametric Mann Whitney U-test were used to test the balance of general data of the two groups of subjects. (3) CEES, EORTCQLQ-C30 V3.0 were tested by normal distribution and ANOVA. (4) Repeated measurement analysis of variance was used to compare the intervention group and the control group in different intervention stages. The effect of two groups of nursing on CEES, EORTCQLQ-C30 V3.0 scores was discussed in detail.
Research tools
(1) General information questionnaire: designed by researchers according to research needs, mainly including demographic and sociological data: age, education level, marital status, nationality, medical payment method, disease related data, etc.; (2) Personalized nursing needs assessment questionnaire for BC patients: the OPT model was taken as the theoretical basis, supported by the literature, conversation with BC patients, and self-made assessment questionnaire; (3) Supportive care need survey short form (SCNS-SF34): this scale is developed from cancer patients needs questionnaire (CPNQ), which can comprehensively evaluate the needs of tumor patients in all aspects; (4) Cancer experience and efficacy scale (CEES): It is divided into two parts: cancer experience and control efficacy, a total of 6 dimensions and 29 items. Cancer experience includes personal experience, socio-economic and emotional experience; control efficacy includes personal, group and medical efficacy. Grade 1–5 scoring method is adopted. The higher the score of cancer experience, the more negative experience the patient has, and the higher the score of control efficiency, the better the patient can cope with the disease. CEES is suitable for domestic cancer patients; (5) European Organization for Research and Treatment of Cancer questionnaire (EORTC-QLQ-C30): There are 15 fields in total, including 5 functional fields (body, role, cognition, emotion and social function), 3 symptom fields (fatigue, pain, nausea and vomiting), 1 general health status/quality of life field and 6 single items (each as a field), a total of 30 items. The scoring method of items 1–28 is divided into four levels from “none, a little, equivalent and extraordinary”; Items 29 and 30 are divided into 7 grades, which are 1–7 points according to the patient’s answer.
Study design
Control group: the control group received routine nursing, the nursing content formulated by the Department, giving patients a comfortable environment, and routine admission education, diet guidance, medication guidance, activity guidance and discharge guidance during hospitalization.
Intervention group: patients in the intervention group were given routine care and personalized care based on OPT model during hospitalization. The personalized nursing services were selected by questionnaire survey among patients with BC, and the researchers formulated a personalized nursing intervention plan according to the assessment results of patients’ care needs. There are four nursing intervention including Supportive Care Intervention, Psychological Health Education (PHE), Chinese Medicine Foot Bath Bombined with Bassage (CMFB-M) and Progressive Muscle Relaxation Training (PMRT), etc. According to OPT theoretical model, a total of three sessions were provided in the program at lest during hospitalization. Each session, we provide personalized nursing services for patients according to their current nursing needs; Timely assess and understand patients’ satisfaction with nursing services, and constantly compare the current situation with the expected results to ensure the effectiveness of nursing services. The next session, patients are encouraged to choose the care method that is most suitable for them.
Supportive care intervention is according to the results of supportive care needs questionnaire (SCNS-SF34), provide targeted nursing services for patients.
PHE was delivered by a research team comprising three nurses and a psychologist. In this study, the psychoeducational intervention included psychoeducation on managing common symptoms in breast cancer patients and relaxation techniques. The general content of the psychoeducational intervention as follow: (1) Encourage personal introduction, expectations, and goals. Help patients find positive survival goals and build their confidence in life; (2) Encourage expression of feelings, thoughts, perceptions, anxieties and fears; (3) Provide accurate knowledge about BC and information about the common treatments; Pain control education; Provide nausea/vomiting and fatigue control education; Provide constipation and diarrhea control education; Sleep hygiene education; Coping improvement strategies; Problem-solving technique; Relaxation technique; Discuss communication skills.
CMFB-M was given to patients once a day for 30 min between 21:00 and 22:30 in the ward during hospitalization. The patients of this group were asked to sit on a chair with back support, then they immersed their feet in 40–45°C water of medicine prescription in electrical foot bath vessels for 20 min. The prescription mainly included Angelica sinensis, dried ginger and artemisia argyi leaves, etc. After that, patients receive massages focusing on the back, shoulder and arms for 10 min.
PMRT is the technique including continuous and systematic stretching and relaxing of the muscles until the whole body becomes relaxed (48). In this study, the patients were instructed how to contract and relax the 16 muscle groups on the third day after the surgery. Progressive muscle relaxation training was once a day, once in the early morning (8 a.m.10 a.m.) for 30 min per session until next survey. Progressive muscle relaxation training was conducted by the researchers in an orderly way and step by step according to the patients’ condition until the patients did the training freely and easily without uncomfortable feelings. Patients in the intervention group who chose this option attended and completed the training.
Results
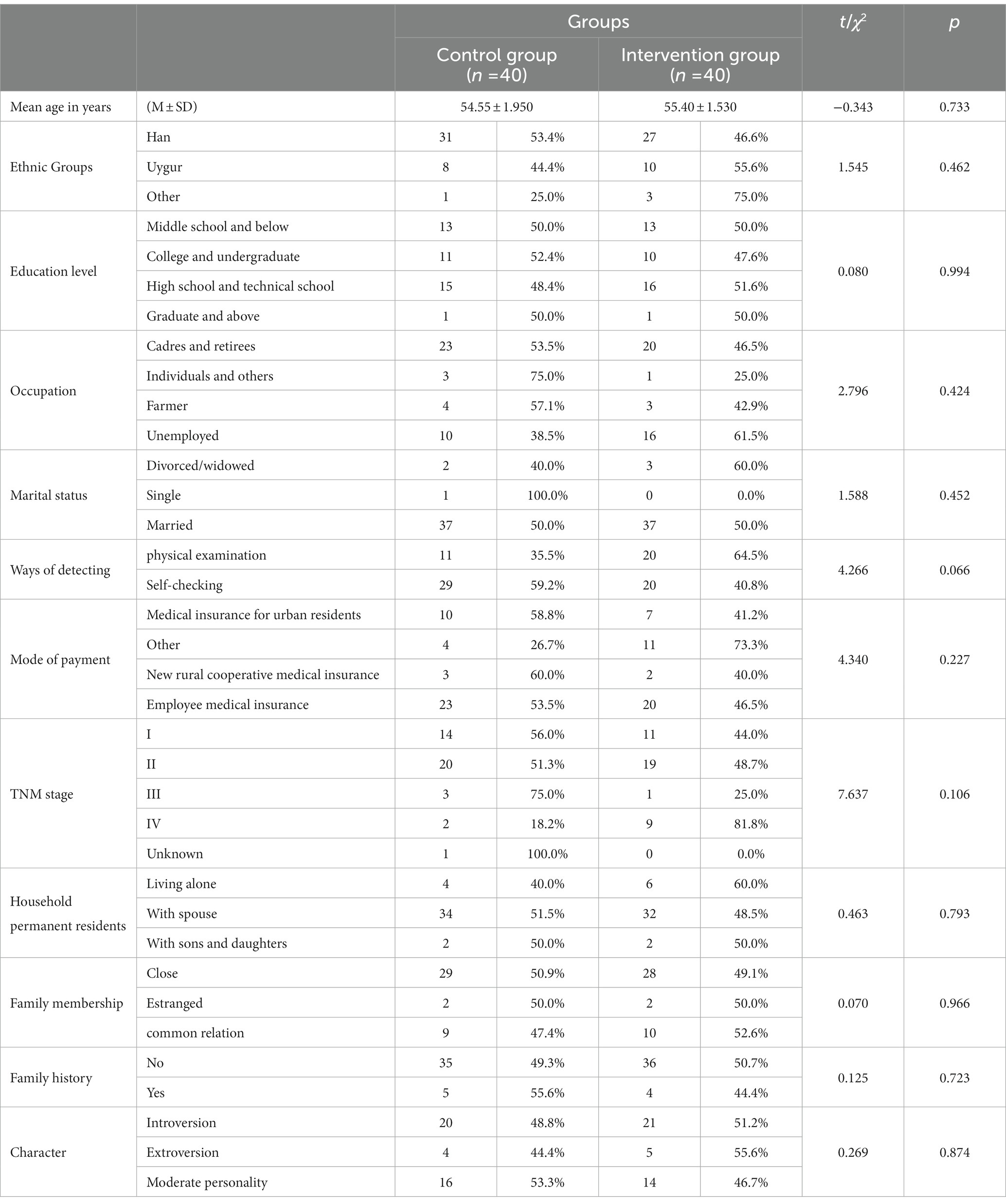
Comparison of general data and demographic characteristics of BC patients
The general data of BC patients in different groups were compared among groups in terms of demographic characteristics such as age, nationality, residential area, education level and marital status. According to the test results, There was no significant difference in general data between the two groups (p > 0.05). It means that the research results between the intervention group and the control group were comparable after intervention. See Table 1 for details.
Comparison of perceived control scores of different groups of BC patients before and after intervention
The results of this study showed that there were no significant differences in the total score of cancer experience and control efficacy of patients between the control group (61.15 ± 5.659, 41.80 ± 4.702) and the intervention group (60.58 ± 7.136, 42.15 ± 5.550) before treatment (p > 0.05). It means that the two groups of patients were in the same state before the intervention nursing. After the intervention, the total score of cancer experience in the intervention group (54.80 ± 8.519) was significantly lower than that in the control group (59.575 ± 7.331), with significant differences (p < 0.05). The total score of control efficacy in the intervention group (49.78 ± 6.466) was significantly higher than that in the control group (43.32 ± 6.219), with significant differences (p < 0.05). There were statistically significant differences in emotional experience, personal efficacy, collective efficacy, medical efficacy, total score of cancer experience and total score of control efficacy among different groups of BC patients (p < 0.05). See Table 2 for details.
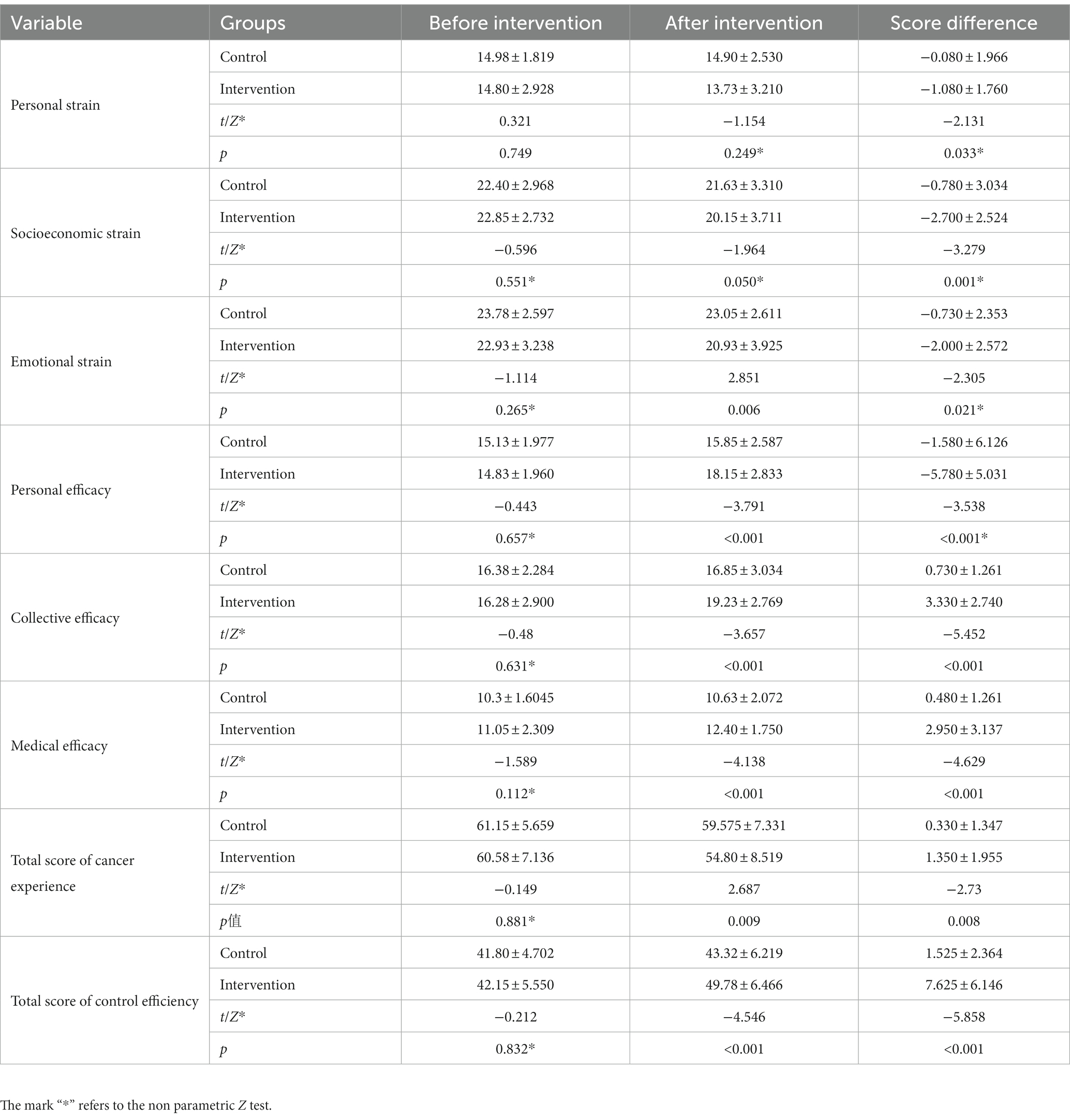
Table 2. Comparison of perceived control scores of breast cancer patients in different groups before and after intervention (n = 80).
Comparison of QoL scores of BC patients in different groups before and after intervention
Before the intervention, there was no significant difference in the scores of QoL, functional area and symptom area between the two groups, illustrating that the two groups of patients were in the same state, thus the data was comparable. There was no significant difference in the scores of QoL before (55.208 ± 12.184) and after (57.083 ± 13.549) the intervention in the control group (p > 0.05). There was significant difference in the scores of QoL before (54.583 ± 11.156) and after (61.458 ± 17.772) the intervention in the intervention group (p < 0.05). In the intervention group, the scores of the three dimensions of physical function (PF), role function (RF) and emotional function (EF) after the intervention were higher than those before the intervention, and the difference was statistically significant (p < 0.05). There were no statistically significant differences in the scores of other dimensions (p > 0.05). See Table 3 for details.
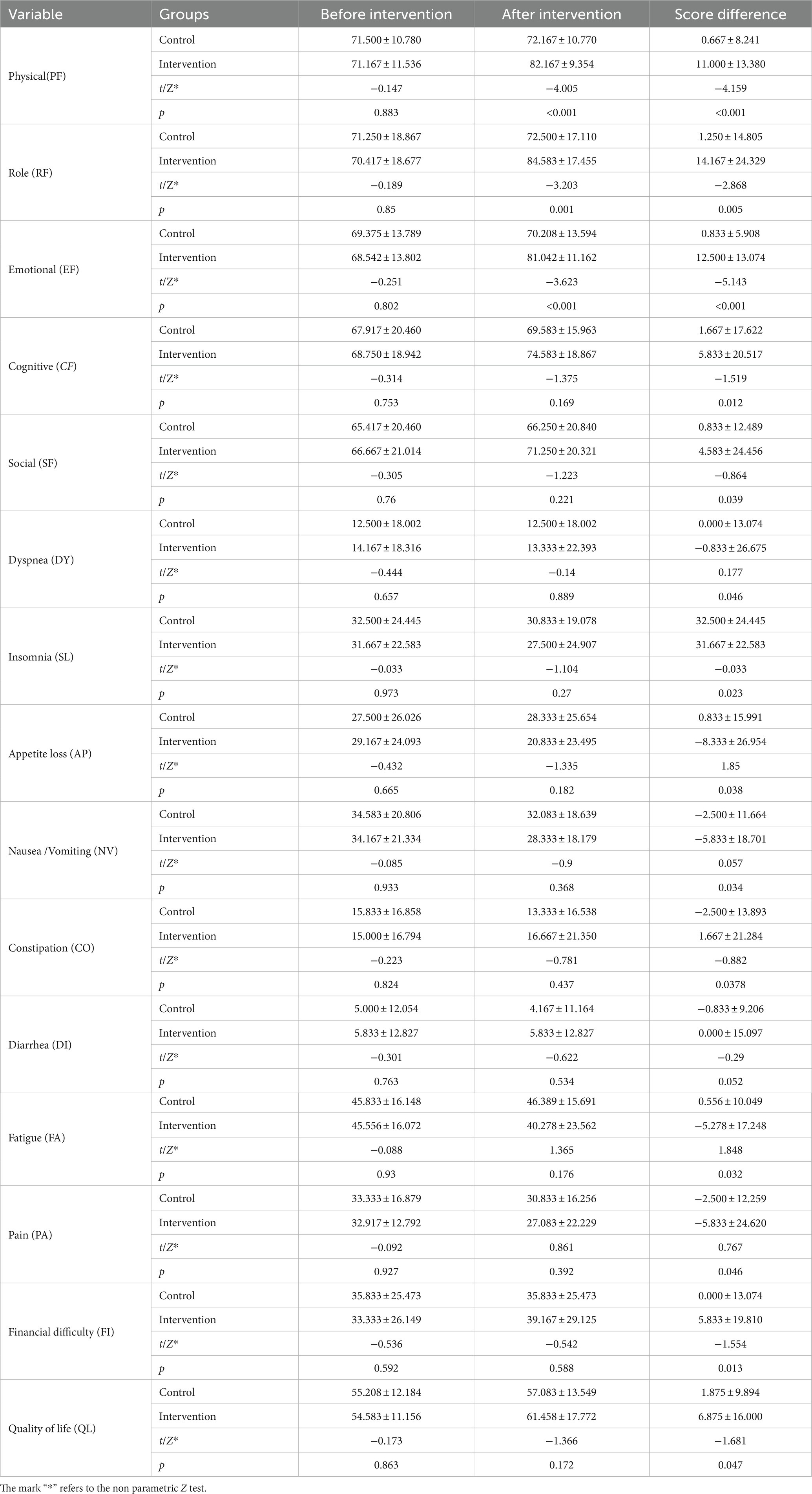
Table 3. Comparison of quality of life scores of breast cancer patients in different groups before and after intervention (n = 80).
Discussion
BC and its treatments are lead to a variety of physiological and psychological problems of patients, thus reducing the adaptability of patients to cancer, resulting in increased negative experience and reduced QoL (11). So how to improve patients’ cancer management ability and to alleviate these cancer-related negative experience are particularly important. Perceived control (49) refers to that individuals believe they have sufficient ability to deal with external adverse events and are full of confidence in the expected results. The subjective perception, feelings or beliefs generated by individual control can affect disease treatment. Perceived control can appropriately alleviate the negative experience of patients, increase the ability to confront diseases and improve their coping efficiency. Cancer patients with low perceived control are prone to cope with cancer passively, manifested in insufficient self-care, passive acceptance of health education, reluctance to participate in medical communication (50). Therefore, effective interventions should be given in time to improve their perceived control.
This study take the OPT model as the structural framework to construct the nursing intervention for BC patients during hospitalization, and target the satisfaction of the humanistic care needs of BC patients as the outcome goal. During hospitalization, the patients in the control group only received routine nursing, and the patients in the intervention group received routine nursing and personalized care based on the OPT model. In this study, firstly, researchers used the Personalized Care Support Evaluation questionnaire and the Patient Supportive Care Needs questionnaire to understand the nursing needs of BC patients. Secondly, data analysis was performed on the collected data and central problems were identified, and personalized nursing interventions were formulated and implemented to help patients correct bad habits and behaviors. Finally, the effectiveness and feasibility of nursing interventions in improving the perceived control level and QoL of BC patients were evaluated.
The results of this study showed that there were no significant differences in the scores of the cancer experience and control efficacy of BC patients between the control group and the intervention group before treatment (p > 0.05), it means indicating that the two groups of patients were in the same state before nursing. After treatment, cancer experience score in the intervention group was significantly lower than those in the control group, with significant differences (p < 0.05). The less the score of cancer experience, the less the negative experience of patients. The score of the control efficacy in the intervention group was significantly higher than those in the control group, with significant differences (p < 0.05). The higher the score of control efficacy, the better the patient could deal with the disease. There were statistically significant differences in the perceived control ability of two groups in six aspects (p < 0.05): Emotional experience, Personal efficacy, Collective efficacy, Medical efficacy, total score of cancer experience, total score of control efficacy, see Table 3 for details. The results demonstrated that personalized care based on the OPT model can improve the perceived control ability of BC patients. Because, the Supportive Care Intervention and PHE in the personalized care model presented patients with disease knowledge and daily guidance comprehensively, encouraged patients to actively express their views, made efforts to solve patients’ nursing needs, guided them to adjust their nursing plans and treatment goals according to personal economic conditions, physical conditions and social support, strengthened humanistic care, and encouraged them to participate in the process of making nursing plans and correct cognitive biases. In addition, the CMFB-M and the PMRT in the personalized care model make them comfortable and relieve stress, making them more confident. Therefore, after the intervention, the cancer experience was reduced, the cancer control efficiency was enhanced, and the overall perceived control ability was improved.
Quality of life is a person’s feeling of his position in the culture and value system, and it is a reflection of the collective concepts of health, psychological state, independence level, social relations and so on (51). According to the previous study about psychosocial consequences of cancer therapy (24), QoL is considered to be one of the important clinical outcomes, most of disease outcomes were assessed by QoL. The current medical model believes that the QoL can better reflect the treatment and rehabilitation status of patients. Medical workers should not only pay attention to the survival number of patients, but also the QoL of them (52). Van Dijck and others found (5, 53) that the QoL of patients with BC was significantly lower than normal women. Therefore, how to take effective intervention to improve the QoL of BC patients after surgery and improve their mood and expectancy level are great significance. Nurses can use good nursing intervention to give patients sufficient psychological comfort, and increase their confidence to overcome the disease, and improve the patients’ QoL.
The results of this study showed that there was no significant difference in the scores of QoL, functional areas and symptom areas between the two groups before the nursing (p > 0.05), it means that the two groups of patients were in the same state. After the intervention, there was no significant difference in the scores of QoL in the control group (p > 0.05). However, scores of physical function (PF), role function (RF) and emotional function (EF) of patients in the intervention group were higher than those before the intervention, and the difference was statistically significant (p < 0.05). Although there was no statistically significant difference in the scores of other (fatigue, insomnia, nausea and vomiting, pain and loss of appetite) dimensions (p > 0.05). The main reason was that the medicine the patients use in chemotherapy stages which has a different effect on patients such as allergy, nausea, vomiting, diarrhea, hair loss, abnormal of liver and kidney function. The scores of physical function (PF), role function (RF) and emotional function (EF) are higher than those before the intervention. See Table 3 for details. Hence, humanistic care based on OPT model can improve the QoL of patients. The reason may be that the intervention plans were formulated by the results of questionnaire survey and motivational interview with patients during the research process, and humanistic care was carried out for the weak cognitive areas and nursing needs of patients. According to the OPT theoretical model (39), it is emphasized that to make the best individualized nursing intervention, the medical staff must repeatedly compare the evaluation data of patients’ current state and expected outcome state. Patients were encouraged to participate in the formulation of nursing plans, and they were guided to review their reactions about adverse symptoms and negative emotions during the treatment. The patients were organized to exchange nursing effects and share experiences. Thus, effective interventions that are tailored to the individual condition have been established by continuous improvement. This tailored intervention effectively improved the perceived control of BC patients. Perceived control as a psychological variable plays an extraordinary role in individual life, reflected in cognitive, emotional and behavioral functions (54). Barez (19) found that improving patients’ perceived control ability would significantly reduce the burden of symptoms and achieve better clinical outcomes. Aburuz (50) also pointed out that enhanced perceived control can reduce complications and improve outcomes. Therefore, how to effectively increase the control efficacy and regulate the cancer experience are the key to improve the QoL of BC patients. In this process, the control efficacy of the patients played a significant role compared to cancer experience in the perceived control, and the patients can actively participate in decision-making process of treatment, and have a sense of control over treatment and physical discomfort, to take a more positive attitude to deal with discomfort. Therefore, medical staff should take effective interventions such as psychoeducational counselling which are more important than delivering simple information to improve perceived control, then patients have a clear understanding of the disease and are more willing to believe that they can overcome the disease. In this model, we adopted four different nursing interventions, and patients selectively received nursing interventions according to their own conditions. As a result, the all dimensions of QoL such as emotional dimension, functional dimension and physiological dimension of the patients in the intervention group were improved after the intervention. The results illustrated that the personalized care based on OPT model significantly improved patients’ level of perceived control and QoL.
The current study has three limitations. First, the cross-sectional design of this study is difficult to infer a time series between perceived control and QoL of hospitalized BC patients, and the long-term impact of the perceived control on QoL remains unclear. Second, the relatively small number of participants in this study (each group, N = 40) may lead to a large final deviation, future studies should expand the sample size. Third, we only used perceived control(CEES) and EORTC QLQ-C30 measures, future studies should also take multiple symptom-related measures.
Conclusion
In this study, the personalized care based on OPT model which was developed according to BC patients’ nursing needs and preferences significantly improved the level of perceived control and QoL among the patients with BC. In this model, we adopted four different nursing interventions, and patients selectively received nursing interventions according to their own conditions. There were significant differences in the total scores of cancer experience (60.58 ± 7.136, 54.80 ± 8.519, p < 0.05), control efficacy(42.15 ± 5.550, 49.78 ± 6.466, p < 0.05) and QoL (54.583 ± 11.156, 61.458 ± 17.772, p < 0.05) of BC patients in the intervention group before and after intervention. However, There were no significant differences in the total score of cancer experience (61.15 ± 5.659, 59.575 ± 7.331, p > 0.05), control efficacy(41.80 ± 4.702, 43.32 ± 6.219, p > 0.05) and QoL (55.208 ± 12.184, 57.083 ± 13.549, p > 0.05) of BC patients in the control group before and after nursing.
The results demonstrated the effectiveness and feasibility of the personalized nursing model. In the future research, implications of the study’s findings for health care providers, patients, and families would be valuable. The approach can be extended to the clinical nursing of other cancers, such as gastric cancer, lung cancer, and intestinal cancer. The study highlights that meeting the nursing needs of patients has to be taken as the central goal in clinical practice. The study suggest that health care professionals are encouraged to pay enough attention and understand the nursing needs of patients, help cancer patients effectively cope with the disease, reduce their cancer-related negative experience, and improve the patients’ quality of life. This study provided a reference for clinical nursing of BC patients undergoing surgery and has significant clinical practice value.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by the Human Research Ethics Committee of the First Affiliated Hospital of Xinjiang Medical University. The patients/participants provided their written informed consent to participate in this study.
Author contributions
RR: conceptualization, methodology, formal analysis, investigation, writing—original draft, and project administration. HW: data collection, methodology, visualization, investigation, project administration, and supervision. MN: methodology, formal analysis, writing, statistical analysis and data analysis, and validation. MM: data collection, methodology, visualization, investigation, and supervision. ZA: conceptualization, methodology, investigation, writing, and review and editing. MS: methodology, formal analysis, review and editing, and supervision. HS and XZ: data collection, data curation, data interpretation, and investigation. All authors contributed to the article and approved the submitted version.
Funding
This study was financially supported by Natural Science Foundation of Xinjiang Uygur Autonomous Region (no. 2020D01C168). We sincerely appreciate the support.
Acknowledgments
The authors gratefully thank the medical staff for their cooperation and all the patients for their contributions to the study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Ayala, N, Barchuk, S, Inurrigarro, G, Celano, C, Soriano-García, JL, Bolaños, P, et al. Status of breast cancer in Latin American: results of the breast cancer revealed initiative. Crit Rev Oncol Hematol. (2023) 181:103890. doi: 10.1016/j.critrevonc.2022.103890
2. Lu, H, Hou, L, and Liu, R. Application of "gesture analogy Method" in postoperative nursing care of patients with breast cancer. Asian J Surg. (2022) 45:629–30. doi: 10.1016/j.asjsur.2021.10.027
3. Löb, S, Linsmeier, E, Herbert, SL, Schlaiß, T, Kiesel, M, Wischhusen, J, et al. Prognostic effect of HER2 evolution from primary breast cancer to breast cancer metastases. J Cancer Res Clin Oncol. (2022). doi: 10.1007/s00432-022-04486-0
4. Modi, ND, Sorich, MJ, Rowland, A, Logan, JM, McKinnon, RA, Kichenadasse, G, et al. A literature review of treatment-specific clinical prediction models in patients with breast cancer. Crit Rev Oncol Hematol. (2020) 148:102908. doi: 10.1016/j.critrevonc.2020.102908
5. Kerr, AJ, Dodwell, D, McGale, P, Holt, F, Duane, F, Mannu, G, et al. Adjuvant and neoadjuvant breast cancer treatments: a systematic review of their effects on mortality. Cancer Treat Rev. (2022) 105:102375. doi: 10.1016/j.ctrv.2022.102375
6. Salisu, WJ, Mirlashari, J, Varaei, S, and Seylani, K. Limited access to care for persons with breast cancer in Africa: a systematic review. Eur J Oncol Nurs. (2021) 50:101867. doi: 10.1016/j.ejon.2020.101867
7. Cvetkovic, J, and Nenadovic, M. Depression in breast cancer patients. Psychiatry Res. (2016) 240:343–7. doi: 10.1016/j.psychres.2016.04.048
8. Ruiz-Casado, A, Álvarez-Bustos, A, de Pedro, CG, Méndez-Otero, M, and Romero-Elías, M. Cancer-related fatigue in breast cancer survivors: a review. Clin Breast Cancer. (2021) 21:10–25. doi: 10.1016/j.clbc.2020.07.011
9. Lundberg, PC, and Phoosuwan, N. Life situations of Swedish women after mastectomy due to breast cancer: a qualitative study. Eur J Oncol Nurs. (2022) 57:102116. doi: 10.1016/j.ejon.2022.102116
10. Verhoeff-Jahja, R, ter Kuile, MM, Weijl, NI, Oosterkamp, R, Cloos, M, Portielje, JEA, et al. Symptoms of anxiety but not depression before start of taxane-based chemotherapy are associated with peripheral neuropathy: a multicenter study in women with breast cancer. Support Care Cancer. (2022) 30:6947–53. doi: 10.1007/s00520-022-07093-4
11. He, X, Ng, MSN, Choi, KC, and So, WKW. Effects of a 16-week dance intervention on the symptom cluster of fatigue-sleep disturbance-depression and quality of life among patients with breast cancer undergoing adjuvant chemotherapy: a randomized controlled trial. Int J Nurs Stud. (2022) 133:104317. doi: 10.1016/j.ijnurstu.2022.104317
12. Chui, PL. Cancer- and chemotherapy-related symptoms and the use of complementary and alternative medicine. Asia Pac J Oncol Nurs. (2019) 6:4–6. doi: 10.4103/apjon.apjon_51_18
13. Oei, SL, Thronicke, A, Matthes, H, and Schad, F. Assessment of integrative non-pharmacological interventions and quality of life in breast cancer patients using real-world data. Breast Cancer. (2021) 28:608–17. doi: 10.1007/s12282-020-01193-x
14. Donovan, HS, Hartenbach, EM, and Method, MW. Patient-provider communication and perceived control for women experiencing multiple symptoms associated with ovarian cancer. Gynecol Oncol. (2005) 99:404–11. doi: 10.1016/j.ygyno.2005.06.062
15. Mansell, W. The perceptual control model of psychopathology. Curr Opin Psychol. (2021) 41:15–20. doi: 10.1016/j.copsyc.2021.01.008
16. Ranchor, AV, Wardle, J, Steptoe, A, Henselmans, I, Ormel, J, and Sanderman, R. The adaptive role of perceived control before and after cancer diagnosis: a prospective study. Soc Sci Med. (2010) 70:1825–31. doi: 10.1016/j.socscimed.2009.10.069
17. Bauml, J, Langer, CJ, Evans, T, Garland, SN, Desai, K, and Mao, JJ. Does perceived control predict complementary and alternative medicine (CAM) use among patients with lung cancer? A cross-sectional survey. Support Care Cancer. (2014) 22:2465–72. doi: 10.1007/s00520-014-2220-5
18. Brédart, A, Kop, JL, de Pauw, A, Caron, O, Fajac, A, Noguès, C, et al. Effect on perceived control and psychological distress of genetic knowledge in women with breast cancer receiving a BRCA1/2 test result. Breast. (2017) 31:121–7. doi: 10.1016/j.breast.2016.10.024
19. Barez, M, Blasco, T, Fernandez-Castro, J, and Viladrich, C. Perceived control and psychological distress in women with breast cancer: a longitudinal study. J Behav Med. (2009) 32:187–96. doi: 10.1007/s10865-008-9180-5
20. Gallagher, MW, Naragon-Gainey, K, and Brown, TA. Perceived control is a transdiagnostic predictor of cognitive-behavior therapy outcome for anxiety disorders. Cognit Ther Res. (2014) 38:10–22. doi: 10.1007/s10608-013-9587-3
21. de Waal, MW, Hegeman, JM, Gussekloo, J, Verhaak, PF, van der Mast, RC, and Comijs, HC. The effect of pain on presence and severity of depressive disorders in older persons: the role of perceived control as mediator. J Affect Disord. (2016) 197:239–44. doi: 10.1016/j.jad.2016.03.012
22. Weis, JB, Gschwendtner, K, Giesler, JM, Adams, L, and Wirtz, MA. Psychoeducational group intervention for breast cancer survivors: a non-randomized multi-center pilot study. Support Care Cancer. (2019) 28:3033–40. doi: 10.1007/s00520-019-05076-6
23. Beatty, L, Koczwara, B, Butow, P, Turner, J, Girgis, A, Schofield, P, et al. Development and usability testing of a web-based psychosocial intervention for women living with metastatic breast cancer: finding my way-advanced. J Cancer Surviv. (2021) 15:403–9. doi: 10.1007/s11764-021-01019-5
24. Lu, Q, Chen, L, Shin, LJ, Wang, C, Dawkins-Moultin, L, Chu, Q, et al. Improvement in quality of life and psychological well-being associated with a culturally based psychosocial intervention for Chinese American breast cancer survivors. Support Care Cancer. (2021) 29:4565–73. doi: 10.1007/s00520-020-05942-8
25. Al-Alawi, KS, Al-Azri, M, Al-Fahdi, A, and Chan, MF. Effect of psycho-educational intervention to reduce anxiety and depression at Postintervention and follow-up in women with breast cancer: a systematic review and meta-analysis. Semin Oncol Nurs. (2022) 38:151315. doi: 10.1016/j.soncn.2022.151315
26. Setyowibowo, H, Yudiana, W, Hunfeld, JAM, Iskandarsyah, A, Passchier, J, Arzomand, H, et al. Psychoeducation for breast cancer: a systematic review and meta-analysis. Breast. (2022) 62:36–51. doi: 10.1016/j.breast.2022.01.005
27. Bouya, S, Barahoie, Z, and Kiani, F. The effect of nursing self-care educational intervention on depression in women with breast cancer undergoing post-mastectomy chemotherapy: a quasi-experimental study. Int J Surg Open. (2021) 32:100333. doi: 10.1016/j.ijso.2021.100333
28. Torres-Vigil, I, Cohen, MZ, Million, RM, and Bruera, E. The role of empathic nursing telephone interventions with advanced cancer patients: a qualitative study. Eur J Oncol Nurs. (2021) 50:101863. doi: 10.1016/j.ejon.2020.101863
29. Li, J, Liu, Y, Jiang, J, Peng, X, and Hu, X. Effect of telehealth interventions on quality of life in cancer survivors: a systematic review and meta-analysis of randomized controlled trials. Int J Nurs Stud. (2021) 122:103970. doi: 10.1016/j.ijnurstu.2021.103970
30. Meneses, K, Pisu, M, Azuero, A, Benz, R, Su, X, and McNees, P. A telephone-based education and support intervention for rural breast cancer survivors: a randomized controlled trial comparing two implementation strategies in rural Florida. J Cancer Surviv. (2020) 14:494–503. doi: 10.1007/s11764-020-00866-y
31. Post, KE, and Flanagan, J. Web based survivorship interventions for women with breast cancer: an integrative review. Eur J Oncol Nurs. (2016) 25:90–9. doi: 10.1016/j.ejon.2016.10.004
32. Zagalaz-Anula, N, Mora-Rubio, MJ, Obrero-Gaitan, E, and Del-Pino-Casado, R. Recreational physical activity reduces breast cancer recurrence in female survivors of breast cancer: a meta-analysis. Eur J Oncol Nurs. (2022) 59:102162. doi: 10.1016/j.ejon.2022.102162
33. Shimizu, Y, Tsuji, K, Ochi, E, Okubo, R, Kuchiba, A, Shimazu, T, et al. Oncology care providers' awareness and practice related to physical activity promotion for breast cancer survivors and barriers and facilitators to such promotion: a nationwide cross-sectional web-based survey. Support Care Cancer. (2022) 30:3105–18. doi: 10.1007/s00520-021-06706-8
34. Gil-Herrero, L, Pollán, M, Martín, M, López-Tarruella, S, Castellanos, M, and Casla-Barrio, S. The importance of physical exercise in cardiovascular fitness in breast cancer survivors. A cross-sectional study: women in motion 2.0. Support Care Cancer. (2022) 30:6745–54. doi: 10.1007/s00520-022-06993-9
35. Coughlin, SS, Caplan, LS, and Williams, V. Home-based physical activity interventions for breast cancer patients receiving primary therapy: a systematic review. Breast Cancer Res Treat. (2019) 178:513–22. doi: 10.1007/s10549-019-05424-4
36. Zhu, M, Sun, S, Zhang, Y, Chen, L, He, H, Chen, J, et al. Effects of the appearance care on psychosocial outcomes for breast cancer: a systematic review and meta-analysis. Support Care Cancer. (2022) 30:8805–17. doi: 10.1007/s00520-022-07274-1
37. Zhang, MM, Chen, JJ, Zhang, T, Wang, QL, and Li, HP. Feasibility and effect of a guided self-disclosure intervention designed to facilitate benefit finding in breast cancer patients: a pilot study. Eur J Oncol Nurs. (2021) 50:101879. doi: 10.1016/j.ejon.2020.101879
38. Zeinomar, N, and Moslehi, R. The effectiveness of a community-based breast cancer education intervention in the New York state capital region. J Cancer Educ. (2013) 28:466–73. doi: 10.1007/s13187-013-0488-7
39. Daniel, P, and Pesut, J. OPT: transformation of nursing process for contemporary practice. Nurs Outlook. (1998) 46:29–36. doi: 10.1016/s0029-6554(98)90022-7
40. Jessee, MA. An update on clinical judgment in nursing and implications for education, practice, and regulation. J Nurs Regul. (2021) 12:50–60. doi: 10.1016/s2155-8256(21)00116-2
41. Georg, C, Welin, E, Jirwe, M, Karlgren, K, and Ulfvarson, J. Psychometric properties of the virtual patient version of the Lasater clinical judgment rubric. Nurse Educ Pract. (2019) 38:14–20. doi: 10.1016/j.nepr.2019.05.016
42. He, J, Hu, D-Y, Liu, Y-L, Wu, L-F, and Liu, L. Study of the effect of humanistic nursing care model wards in children caring Ward School on the nurses' caring ability. Chin Nurs Res. (2016) 3:45–7. doi: 10.1016/j.cnre.2016.04.001
43. Puhalla, S, Bhattacharya, S, and Davidson, NE. Hormonal therapy in breast cancer: a model disease for the personalization of cancer care. Mol Oncol. (2012) 6:222–36. doi: 10.1016/j.molonc.2012.02.003
44. Zhao, J. The power of small data for personalized cancer care. Asia Pac J Oncol Nurs. (2022) 9:100084. doi: 10.1016/j.apjon.2022.100084
45. Cossich, T, Schofield, P, and McLachlan, SA. Validation of the cancer needs questionnaire (CNQ) short-form version in an ambulatory cancer setting. Qual Life Res. (2004) 13:1225–33. doi: 10.1023/B:QURE.0000037496.94640.d9
46. Hou, WK. Intrapersonal and interpersonal dimensions of cancer perception: a confirmatory factor analysis of the cancer experience and efficacy scale (CEES). Support Care Cancer. (2010) 18:561–71. doi: 10.1007/s00520-009-0687-2
47. Aaronson, NK, Ahmedzai, S, Bergman, B, Bullinger, M, Cull, A, Duez, NJ, et al. The European Organization for Research and Treatment of cancer QLQ-C30: a quality-of-life instrument for use in international clinical trials in oncology. J Natl Cancer Inst. (1993) 85:365–76. doi: 10.1093/jnci/85.5.365
48. Lee, J, Dibble, SL, Pickett, M, and Luce, J. Chemotherapy-induced nausea/vomiting and functional status in women treated for breast cancer. Cancer Nurs. (2005) 28:249–255.
49. Molnar, DS, Flett, GL, and Hewitt, PL. Perfectionism and perceived control in posttraumatic stress disorder symptoms. Int J Ment Health Addict. (2021) 19:2204–18. doi: 10.1007/s11469-020-00315-y
50. AbuRuz, ME, and Al-Dweik, G. Depressive symptoms, perceived control and quality of life among patients undergoing coronary artery bypass graft: a prospective cohort study. BMC Nurs. (2022) 21:87. doi: 10.1186/s12912-022-00857-7
51. Shen, A, Qiang, W, Wang, Y, and Chen, Y. Quality of life among breast cancer survivors with triple negative breast cancer--role of hope, self-efficacy and social support. Eur J Oncol Nurs. (2020) 46:101771. doi: 10.1016/j.ejon.2020.101771
52. Riani Costa, LA, Barreto, RF, de Leandrini, SMM, Gurgel, ARB, de Sales, GT, Voltarelli, VA, et al. The influence of a supervised group exercise intervention combined with active lifestyle recommendations on breast cancer survivors' health, physical functioning, and quality of life indices: study protocol for a randomized and controlled trial. Trials. (2021) 22:934. doi: 10.1186/s13063-021-05843-z
53. van Dijck, S, Nelissen, P, Verbelen, H, Tjalma, W, and Gebruers, N. The effects of physical self-management on quality of life in breast cancer patients: a systematic review. Breast. (2016) 28:20–8. doi: 10.1016/j.breast.2016.04.010
Keywords: OPT model, personalized care, breast cancer, perceived control, quality of life
Citation: Rahman R, Mamat P, Wang H, Nurtai M, Mahsut M, Ahmat Z, Siyit M, Shang H and Zhang X (2023) Effect of personalized care based on OPT model on perceived control and quality of life among patients with breast cancer. Front. Public Health. 11:1149558. doi: 10.3389/fpubh.2023.1149558
Edited by:
Morteza Shamsizadeh, Hamadan University of Medical Sciences, IranReviewed by:
Laleh Abbasi, Islamic Azad University Tonekabon, IranFatemeh Tajik, Iran University of Medical Sciences, Iran
Roya Boodaghi Malidarre, Payame Noor University, Iran
Copyright © 2023 Rahman, Mamat, Wang, Nurtai, Mahsut, Ahmat, Siyit, Shang and Zhang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Rabigul Rahman, cmFiaWd1bHJhaG1hbkB4am11LmVkdS5jbg==; Haiyan Wang, MTA5MTk0MDE3OUBxcS5jb20=
 Rabigul Rahman
Rabigul Rahman Parida Mamat1
Parida Mamat1