- 1Department of Obstetrics and Gynaecology, Erasmus University Medical Centre, Rotterdam, Netherlands
- 2Department of Health Services Management & Organisation, Erasmus School of Health Policy & Management, Erasmus University Rotterdam, Rotterdam, Netherlands
- 3Department of Nephrology, University Medical Centre Groningen, Groningen, Netherlands
Introduction: In recent years, Value-Based Healthcare (VBHC) has been gaining traction, particularly in hospitals. A core VBHC element is patient value, i.e., what matters most to the patient and at what cost can this be delivered. This interpretation of value implies patient engagement in patient–doctor communication. Although patient engagement in direct care in the VBHC setting is well described, patient engagement at the organizational level of improving care has hardly been studied. This systematic review maps current knowledge regarding the intensity and impact of patient engagement in VBHC initiatives. We focus on the organizational level of a continuous patient engagement model.
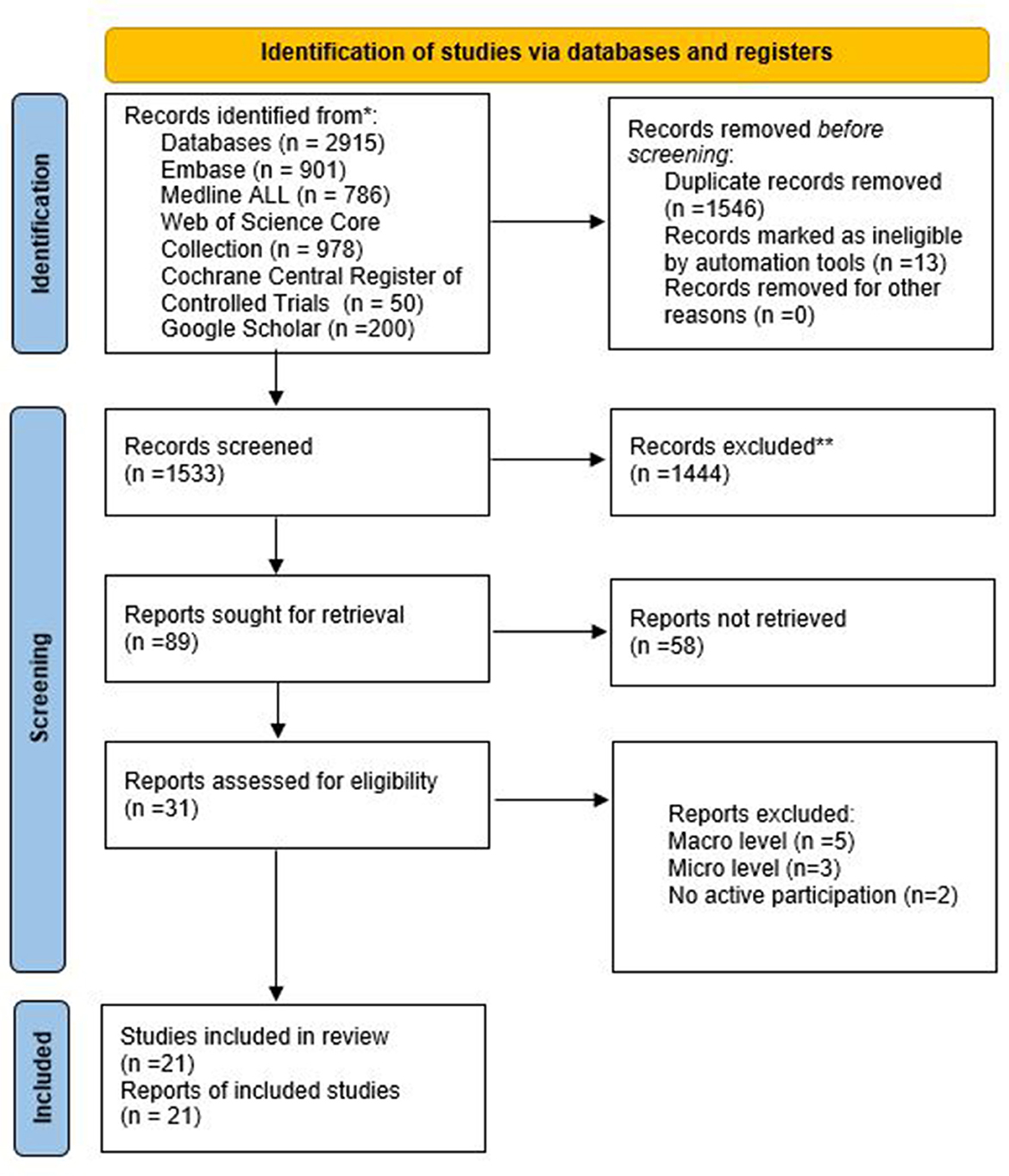
Methods: We performed a systematic review following PRISMA guidelines using five electronic databases. The search strategy yielded 1,546 records, of which 21 studies were eligible for inclusion. Search terms were VBHC and patient engagement, or similar keywords, and we included only empirical studies in hospitals or transmural settings at the organizational level.
Results: We found that consultation, using either questionnaires or interviews by researchers, is the most common method to involve patients in VBHC. Higher levels of patient engagement, such as advisory roles, co-design, or collaborative teams are rare. We found no examples of the highest level of patient engagement such as patients co-leading care improvement committees.
Conclusion: This study included 21 articles, the majority of which were observational, resulting in a limited quality of evidence. Our review shows that patient engagement at the organizational level in VBHC initiatives still relies on low engagement tools such as questionnaires and interviews. Higher-level engagement tools such as advisory roles and collaborative teams are rarely used. Higher-level engagement offers opportunities to improve healthcare and care pathways through co-design with the people being served. We urge VBHC initiatives to embrace all levels of patient engagement to ensure that patient values find their way to the heart of these initiatives.
1. Introduction
The concept of value-based healthcare (VBHC) was introduced in 2006 by Porter and Teisberg (1), as a response to the ever increasing and from a societal point of view unsustainable costs of healthcare, a problem that was especially, but not exclusively, present for decades in the US that had the highest costs of care in the world and one of the lowest health indicators (2). In the second half of the 20th century different strategies were pursued to tackle costs varying from fee-for-service payment systems, negotiating prices by both government and private insurers and the introduction of health maintenance organizations (HMOs) for employees. The strategies resulted in a variety of external accountability tools, physicians who feel over controlled and consumer groups (patients) who feel helpless (3). The irony of these approaches was that the system was volume driven, with physicians overproducing thus earning more money and insurers tried to cut both prices and volume in order to control costs. Both mechanisms were not in the interest of patients and people with sickness and diseases. Over the decades new insights were developed that resulted in a growing interest in the concept of value in healthcare. Rather than just focusing on output or lowering costs as isolated management tools, healthcare providers should focus on creating value for patients. Porter and Teisberg introduced the definition of value of any healthcare service as the outcome relative to all the costs incurred to achieve that outcome. They argued that, by following this path, a patient-centered, high quality and affordable healthcare delivery system could be realized. In Europe, EXPH on behalf of the European Commission has defined value broader and introduced four distinct elements of VBHC: personal value (to the patient), technical value (technical achievement), allocative value (distribution of resources), and societal value (contribution to social participation) (4). In this review we limit ourselves to the more narrow definition of VBHC as introduced by Porter and Teisberg (1).
Value for patients is one of the key elements of value-based healthcare (5, 6). To create patient value, in addition to good medical practice, a clear understanding is needed of which outcomes matter most to patients (5, 7). To this end, the use of patient-centered sets of outcome standards is promoted by the International Consortium for Health Outcomes Measurement (ICHOM). Patient Reported Outcome Measures (PROMs) are increasingly used in the consultation room to measure patient-valued outcomes of clinical practice (7–10). In essence, PROMs are questionnaires on a range of health and quality-of-life related issues that are reported by patients themselves and discussed with their doctor.
A second key element of VBHC is the focus on the full cycle of care and the introduction of integrated practice units (IPUs) where care is organized around the needs of patients alongside specialized medical interventions (1, 11). To optimize, from a patient's perspective, the full cycle of care, involving patients in designing patient-centered care pathways can be helpful (12–14). The possibilities and constraints of involving patients in improving health services has been widely studied, including topics such as quality improvement, patient safety, protocol adherence, patient satisfaction, service innovation, and the effectiveness of patient involvement (15–20).
Three frameworks of patient involvement are frequently used (12): Arnstein's (21) ladder of participation, Bate and Robert's (22) continuum of patient involvement and Carman et al.'s (23) continuum of patient engagement. All these frameworks have different angles: Arnstein's (24), a model from the 1960s, focuses on power distribution between actors such as patients and doctors and ignores the value of knowledge diversity. Bate and Robert present a continuum with the most advanced form being experience-based co-design (EBCD) of a care pathway (22). Carman et al. (23) provide a descriptive framework involving three different levels, each along a continuum of patient engagement: the direct care level, the organizational level, and the policy level. On each level, they define a continuum of engagement ranging from consultation through involvement to partnership and shared leadership.
The aim of our study is to present an overview of empirical findings regarding patient engagement in a VBHC context on the organizational level of hospitals. We have chosen to use Carman et al. (23) framework for patient engagement since this makes an explicit distinction between the direct care, the organizational, and the policy levels. The direct-care level is well described in the current VBHC literature and includes outcome measurements, shared decision-making, and costs (8, 21, 22). The policy level concerns societal issues related to healthcare and is only loosely linked to day-to-day clinical practice. Consequently, this study focuses on the organizational level, covering the hospital unit through to designing the full cycle of care, which is hardly described from the perspective of patient engagement (3, 23).
2. Methods
This systematic review is conducted and reported following the protocol of Prisma Guidelines for systematic reviews (25). Details are provided in Supplementary material 1. In addition, the authors are trained researchers and the team is highly experienced in conducting systematic reviews. The review was not registered.
2.1. Search strategy
The search strategy was developed in collaboration with an expert librarian from the Erasmus University Medical Centre, Rotterdam, Netherlands. Five databases were searched on 14-01-2022: Embase, Medline ALL, Web of Science Core Collection, Cochrane Central Register of Controlled Trials, and Google Scholar. The search strategy followed PICO to formulate the definitions of the research question. (1) P (patient/ population), patients in a hospital or transmural setting, (2) I (intervention), value-based healthcare, (3) O (outcomes), patient engagement on an organizational level of hospitals. The C (comparator) is not applicable in this study. The search strategy consisted of the two major elements of this systematic review, patient participation and value-based healthcare, plus their plural forms. Supplementary material 2 provides the full search string. Duplications of any articles were excluded. References were cross-checked and added if not already included. Seven clearly relevant papers were identified in advance of this to check that the search strategy correctly retrieved them.
2.2. Selection process
In advance of the full selection process, five articles were independently screened by two researchers (MV&WS) by title and abstract to check for agreement on inclusion and exclusion criteria. The results were discussed by the two researchers and the results of the screening by these two researchers were fully agreed by both. We made the choice to use Rayyan as a tool to streamline the process. Herewith, both researchers independently screened the titles and abstracts of the papers identified in the search. After both researchers (MV & WS) had screened these articles, they were uploaded in one overview. There was discussion about articles when there was a discrepancy between the two researchers. Consensus was found between the two researchers and these articles proceeded to full text screening. The reasons for excluding a research paper during the next stage, full text screening, were recorded and inconsistent screening outcomes were discussed by the two researchers. Six articles where there was no consensus were reviewed by two other researchers (AF & KA) with four being included and two rejected.
2.3. Eligibility criteria
The eligibility criteria were applied in two phases: title and abstract screening and full text screening. In the first phase (title and abstract screening), the criteria for excluding the studies were “mentioned value-based healthcare as a research topic but no patient engagement or vice versa”, “setting other than a hospital environment or transmural”, “research papers prior to 2006”, “not written in English”, “not peer reviewed”, “not empirical research”, and “conference paper”. We did not include papers published prior to 2006 because Porter and Teisberg (1) introduced the concept of value-based healthcare in 2006. In the second phase (full text screening), patient engagement and value-based healthcare were further explored. The primary outcomes were the level of patient engagement on an organizational level and the integration of the VBHC elements in practice. Patient engagement was defined as active participation by patients in the study described in the research paper. Based on the framework by Carman et al. we investigated the level of patient engagement from an organizational unit (meso-level) perspective. Carman et al.'s model presents a continuum of engagement, whereby consultation, involvement and partnership, and shared leadership are used to define the level of patient engagement from low to high (23). The criteria for excluding the initially identified studies were “direct care (micro-level) in a hospital setting”, “macro-level care in a hospital setting”. This research was aimed at synthesizing the information from the studies that developed new knowledge about patient engagement from an organizational-unit perspective in a value-based healthcare context which was the focus of our study. An integrative approach has been chosen in this systematic review, since the ways in which patients participate in both qualitative and quantitative data can be investigated.
2.4. Data extraction and analysis
Data extraction consisted of three steps of thematic analysis and these were carried out independently by two researchers (MV & WS). Atlas.ti, version 22 was used to facilitate this process. First, the generic characteristics of a study were examined in terms of authors' names, the year of publication, country, medical specialties involved, study design, and number of patients involved. Second, the context of the study in terms of the field of value-based healthcare was examined. We looked for the presence, or absence, of the elements of value-based healthcare proposed by Porter and Teisberg (1): value, outcomes, and costs, and how these were used in the practical design of the study. Finally, to examine the context of patient engagement, we inductively analyzed how patients were involved, what level of patient engagement was apparent based on the model of Carman et al. which patient engagement outcomes were reported and to what extent the participation of patients contributed to the results of the study.
Due to the focus of the research question, a narrative approach has been chosen for displaying and presenting the data in tables. As a result, a meta-analysis was not undertaken and the results were analyzed descriptively and thematic. This was necessary given the studies' heterogeneity for study designs, participants, objectives and results.
2.5. Quality assessment
The mixed methods appraisal tool (MMAT) (26) was used to assess the quality and risk of bias in the 21 studies included. The MMAT was developed for systematic reviews that combine qualitative, quantitative, and/or mixed studies (27, 28). Moreover, the MMAT was developed for the appraisal stage of systematic reviews and facilitates the appraisal of empirical studies including observational studies. MMAT facilitates the appraisal of five research categories: qualitative research, randomized controlled trials, non-randomized studies, quantitative descriptive studies, and mixed methods studies. Following the quality criteria as described in the MMAT user guide, two researchers (MV & WS) have both independently of each other assessed each study and after discussion, the scores were decided together. The qualitative (n = 5), quantitative (n = 9), and mixed-methods (n = 7) studies were subjected to their own screening categorization that involves a set of five unique criteria. For each criteria, a “yes” response was scored “1” and a “no” or “can't tell” scored “0”. An overall score of “5” means that all the quality criteria are met; a score of “0” that none of the quality criteria are met (26). We converted this to the score “5” is high, score “4” and “3” is medium, and “2”, “1” and “0” is low.
3. Results
The search strategy yielded a total of 2,915 articles across the five databases. A total of 1,533 articles remained after removing duplicates. A total of 21 articles remained after the title and abstract, followed by full text, screening. Further details can be found in Figure 1 above.
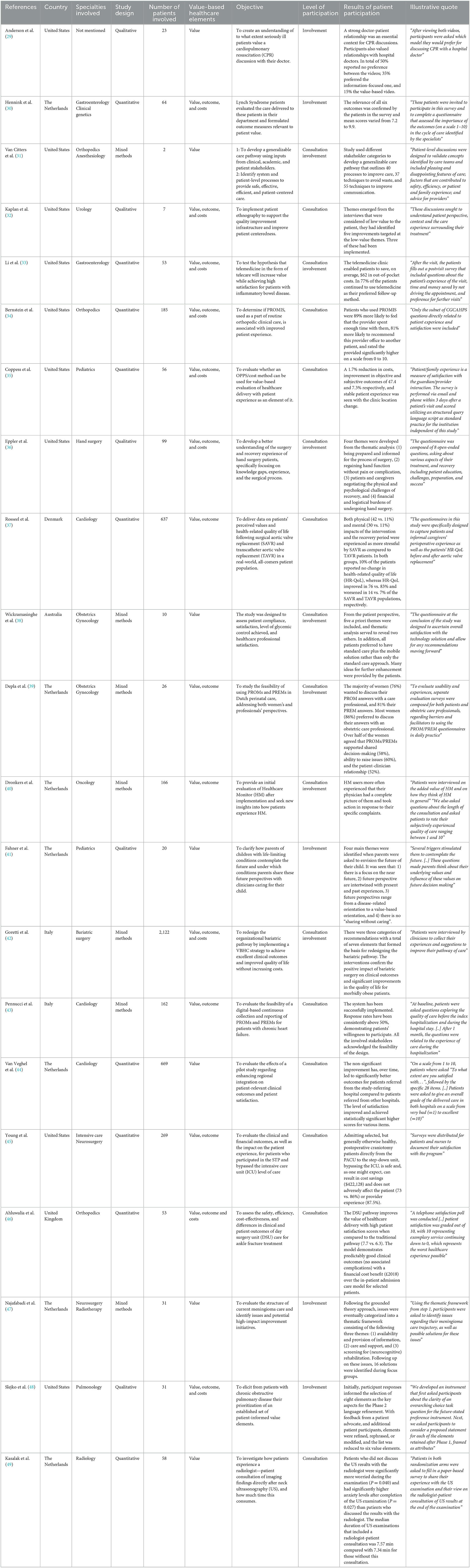
A schematic representation of all results of the 21 studies is provided in Table 1 below.
3.1. General characteristics
The studies were all published between 2013 and 2022. Nine studies were conducted in the United States (29, 31–36, 45, 48), seven studies in The Netherlands (30, 39–41, 44, 47, 49), two in Italy (42, 43), one in Australia (38), one in Denmark (37), and one in the United Kingdom (46). Nine studies had a quantitative design (30, 33–35, 37, 44–46, 49); seven studies a mixed methods design (31, 38–40, 42, 43, 47) and five a qualitative design (29, 32, 36, 41, 48). In total, 4,743 participants were involved in the 21 studies, ranging from 2 patients (31) to 2,122 patients (42). All 21 studies were conducted in hospitals: 14 studies in a single hospital (29, 30, 33–35, 37, 40–43, 46–49), five studies in multiple hospitals (31, 36, 38, 44, 45), one in a single hospital and in patients' homes (32), and one in multiple hospitals and at home (39).
3.2. Quality assessment
The quality assessment resulted in classifications of “high” (13 studies), “medium” (8 studies), with none categorized as “low”. Consequently, no studies were excluded on the basis of the MMAT. Overall, the quantitative studies tended to achieve higher quality scores than the mixed methods and qualitative studies. A detailed overview and the explanations of the scores of the quality assessment are provided in Supplementary material 3.
3.3. Patient participation in a value-based healthcare context
3.3.1. Value-based healthcare context
Nine studies discussed value, outcome, and costs in relation to each other (30, 32–36, 42, 46, 48) of which six investigated the costs from an organizational perspective (30, 32, 34, 35, 42, 46) and three from a patient perspective (33, 36, 48). Five other studies discussed both value and outcomes but not costs (37, 39, 40, 43, 45), three of which investigated patient-reported outcomes (39, 40, 43) and two studies clinical outcomes (37, 45). Seven studies discussed only value (29, 31, 38, 41, 44, 47, 49). In these articles, the focus on value was not linked to outcomes and costs, but more on patient value in terms of what patients consider important.
3.4. Levels of patient engagement
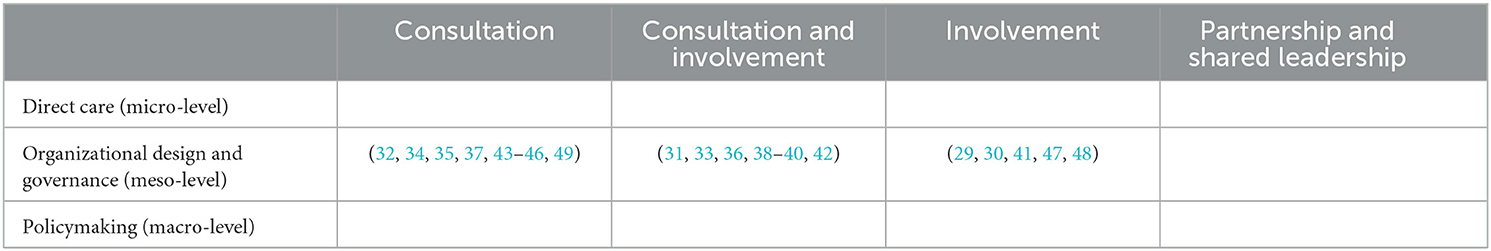
Nine studies indicated only the level of consultation (32, 34, 35, 37, 43–46, 49), and five the level of involvement (29, 30, 41, 47, 48). In addition, seven studies included both these aspects of patient engagement (31, 33, 36, 38–40, 42). None of the studies reported patient engagement at the “partnership and shared leadership” level. A schematic representation is provided in Table 2 below.
The findings in the reviewed papers, insofar as they relate to the levels of patient engagement that emerged from the thematic analysis, in terms of level of engagement, type of studies and their modalities, data collection methods, role of patients related to the level of patient engagement, outcomes patient engagement and results of patient engagement reported are included in three different tables. The details for each level are discussed below.
3.5. Consultation
For the nine studies (32, 34, 35, 37, 43–46, 49) that were limited to the consultation level of patient engagement (23), we investigated how the level of engagement “consultation” was implemented in practice. Further details can be found in Table 3 below.
3.5.1. Type of studies and their modalities
Eight of nine studies have an observational study design (32, 34, 35, 37, 43–46) of which four are cohort studies (32, 43, 44, 46), and four cross-control studies (34, 35, 37, 45). One study has a randomized study design, which is a prospective randomized study (49).
3.5.2. Data collection methods
Seven of nine studies used either a questionnaire or a survey (34, 35, 37, 43–45, 49). In one study the questionnaire or survey was combined with a workshop (43). One study relied completely on interviews for collecting data (32), and another used a telephone satisfaction poll (46).
3.5.3. Outcomes of patient engagement
Based on the role of patients, one or two outcomes were reported. Five of nine studies reported two outcomes in their article (32, 34, 37, 43, 49) and four studies one outcome (35, 44–46). Five studies reported patient satisfaction as outcome of patient engagement (34, 35, 44–46), five studies patient experience (32, 34, 37, 43, 49), two studies quality of care (32, 43), one study patient perspective (49) and one study patient health- related quality of life.
3.5.4. Results of patient participation reported
Six of nine studies show that the role of patients and their input is substantial used in the results and conclusion of the study (32, 34, 37, 43, 44, 49), two studies show that the results were included as part of more results (35, 46) and one study shows that is used minimally in the results (45). In the studies which the results were included as part of more results, one study focuses either on financial and clinical outcomes (46) and one either on financial outcomes (35). In the study which the results were minimally used focused heavily on financial and clinical outcomes (45).
3.6. Consultation and involvement
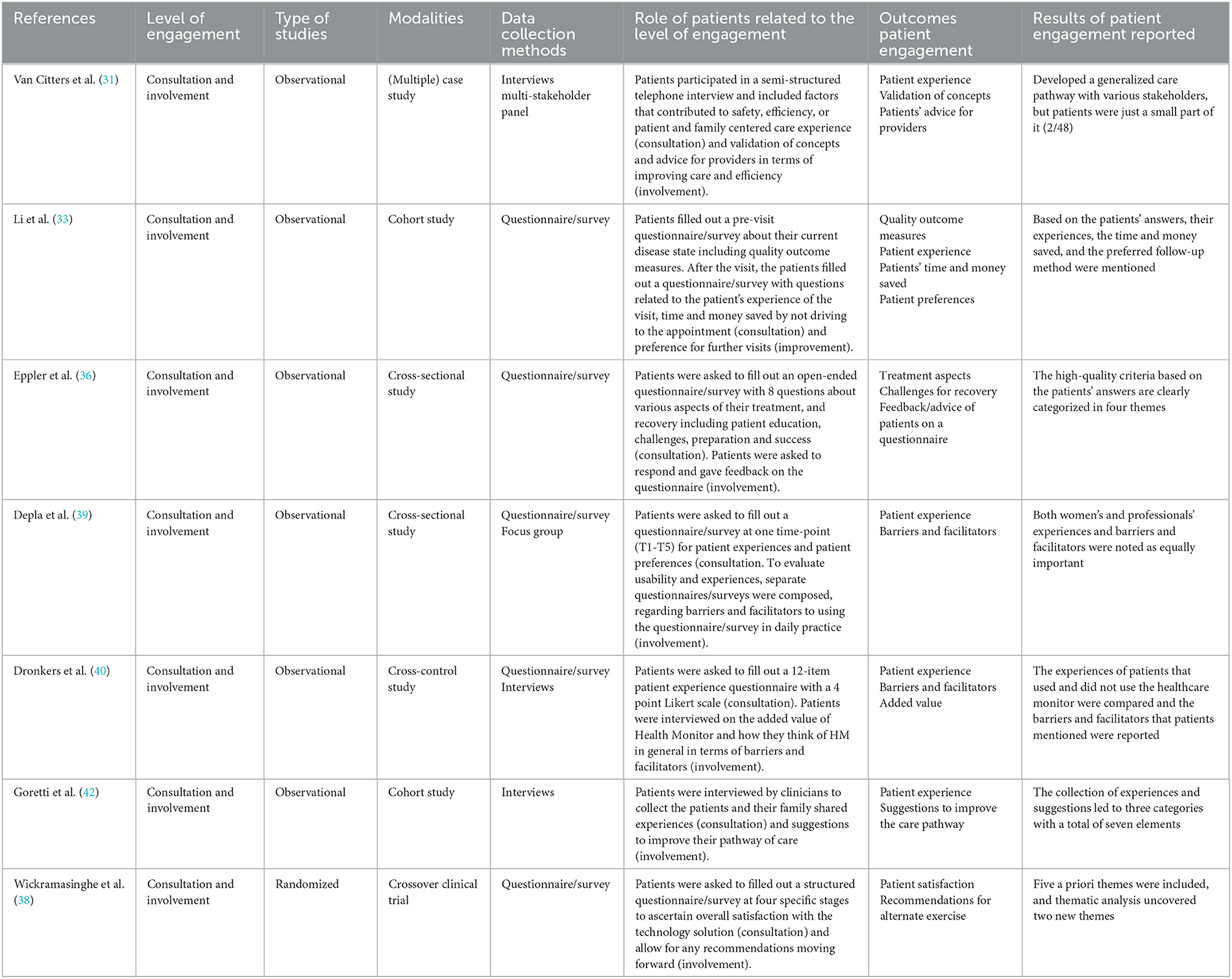
Seven studies addressed the level of consultation and involvement (31, 33, 36, 38–40, 42). Further details can be found in Table 4 below.
3.6.1. Type of studies and their modalities
Six of seven studies have an observational design (31, 33, 36, 39, 40, 42), of which two are cohort studies (33, 42), two are cross-sectional studies (36, 39), one a cross-control study (40), and one a multiple case study (31). One of seven studies has a randomized design, which is a cross-over clinical trial (38).
3.6.2. Data collection methods
Five of the seven studies used a questionnaire or survey (33, 36, 38–40), one in combination with interviews (40). In one study, interviews were the only data collection method used (42) and in one study interviews were combined with a multi-stakeholder panel (31).
3.6.3. Outcomes of patient engagement
All seven studies reported the outcomes of both levels consultation and involvement. Three of seven studies reported three outcomes (31, 36, 40), three reported two outcomes (38, 39, 42) and one study reported four outcomes (33). At the level of consultation five studies reported patient experience as outcome of patient engagement (31, 33, 39, 40, 42), one study patient satisfaction (38), one study quality outcome measures and time and money saved (33), and one study treatment aspects and challenges for recovery (36). At the level of involvement two studies patient's advice as outcome of patient engagement (31, 36), two studies barriers and facilitators (39, 40), one study validation of concepts (31), one study preferences for further visits (33), one study added value of a healthcare monitor (40), one study suggestions to improve the care pathway (42), and one study recommendations for alternate exercise (38).
3.6.4. Results reported
Six of seven studies show that the role of patients and their input is substantial used in the results and conclusion of the study (33, 36, 38–40, 42), and one study shows that it is used minimally (31). In the study which the results were minimally used there were just two patients that participated in a total of 48 participants (31). In the other six studies there were different results reported. One study mentioned patients' experiences, time and money saved and the preferred follow-up method (33), one study mentioned the high-quality criteria based on patients' answers (36), another study mentioned the patient and professional experiences and barriers and facilitators as equally important (39), another study mentioned the experiences and barriers and facilitators of two groups of patients (40), another study mentioned the experiences and suggestions which led to three categories with a total of seven elements to improve their pathway of care (42) and one study mentioned two new themes based on the thematic analysis with patients (38).
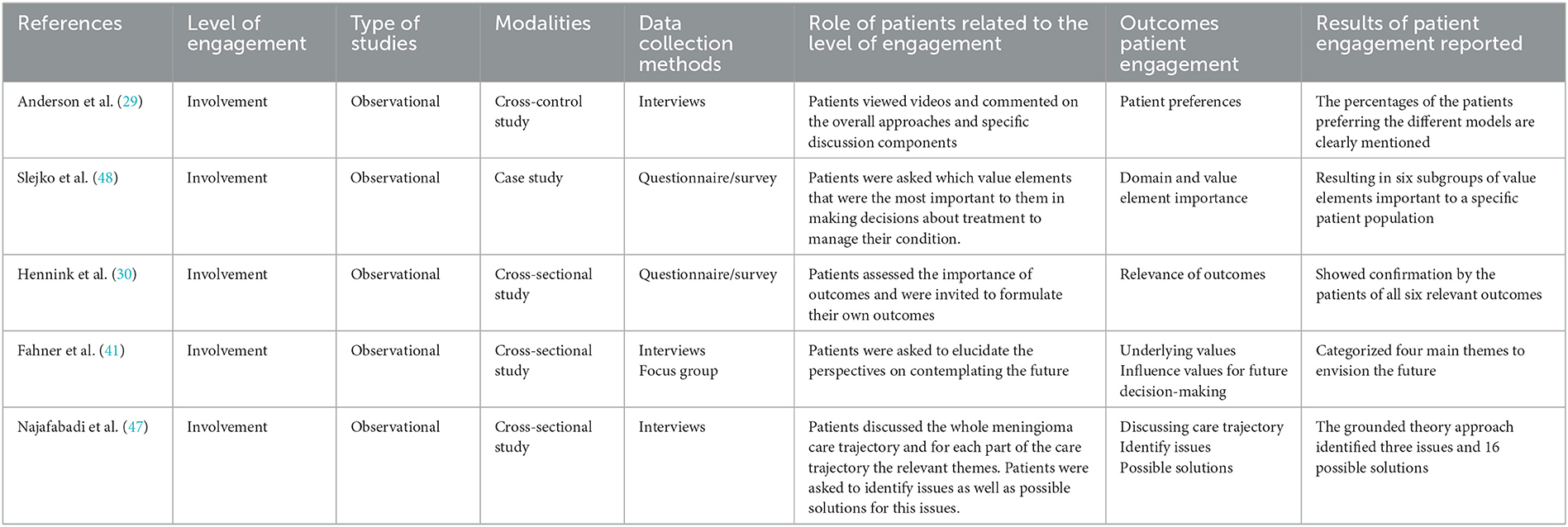
3.7. Involvement
Five studies addressed the involvement level (29, 30, 41, 47, 48). Further details can be found in Table 5 below.
3.7.1. Type of studies and their modalities
All five studies have an observational design (29, 30, 41, 47, 48), of which three are cross-sectional studies (30, 41, 47), one cross-control study (29), and one case study (48).
3.7.2. Data collection methods
Two studies used questionnaires (30, 48), two studies interviews (29, 47), and one study used interviews in combination with a focus group (41). The data collection methods in the five studies have led to different roles of patients in relation to the level “involvement” of patient engagement.
3.7.3. Outcomes of patient engagement
All studies reported one outcome and there are different outcomes reported. One study focused on patient preferences (29), one on domain and value importance (48), one on the relevance of outcomes (30), one on the underlying values and influence of values for future decision-making (41), and one on discussing the care trajectory, the issues related to the care trajectory and the possible solutions for these issues (47).
3.7.4. Results reported
All studies show that the role of patients and their input is substantial used in the results and conclusion of the study. One study mentioned the preferences of patients clearly (29), one study mentioned six different subgroups important to the specific patient population (48), another study provided confirmation by the patients of all six relevant outcomes (30), another categorized four main themes to envision the future (41), and one study identified, on the basis of a grounded theory approach, three issues and sixteen solutions for these issues (47).
4. Discussion
To the best of our knowledge, this is the first systematic review that investigates the communication between patients and healthcare providers at the organizational level of hospitals and throughout the full cycle of care in a VBHC setting. We found that it was most commonly interviews and questionnaires, that can be seen as examples of low-level engagement, that were deployed to engage patients in designing new care pathways and quality improvement projects. Higher-level engagement tools, such as focus groups, co-design experience, collaborative teams, advisory committees, and joint decision-making, are rarely used to improve healthcare in hospitals. This is remarkable in value-driven care approaches that claim to take patient-centeredness and creating patient value as the starting point.
This low level of patient engagement in VBHC is also illustrated by the roadmap for implementing VBHC that has recently been presented by an expert working group from nine large European University Hospitals (50). The roadmap does not pay any attention to patient engagement beyond the advice to develop patient-reported outcome measures (PROMs) and patient-reported experience measures (PREMs) to measure outcomes and experiences. Our conclusion that higher levels of patient engagement should be pursued is supported by the work of Berwick (3). Today, according to Berwick, we are in an era where there is great emphasis on mandatory measurements and a clash between professional autonomy and these tools for external accountability. Berwick emphasizes the importance of “hearing the voices of the people served” in what he envisions as a new era for medicine and healthcare. The expected benefits of this new era are reduced mutual distrust among by actors in the field, a greatly reduced administrative burden for all, and, by incorporating healthcare users of and their families in co-design activities, improved services.
VBHC research that focuses on the level of direct care demonstrates that patient-reported outcome measures are increasingly used in the consulting room to discuss treatment and outcome preferences between doctors and patients. PROMs could also be used to improve healthcare quality and result in higher levels of patient engagement such as shared decision-making (24–29, 31–33). However, we found that higher-level engagement is not yet current practice in VBHC initiatives at the organizational level. Furthermore, our review shows that the organization of the care process and improvements to care pathways are hardly influenced by patient engagement. Only one paper reported the implementation of an improved care process that was a result of patient engagement (32). The possibilities to improve care pathways by using high-level patient engagement strategies extend to experienced-based co-design, involving patient advocates in the organization of care and in influencing patient organizations (12, 16, 51–55). However, we also recognize the risk of tokenistic patient engagement (12, 16). Tokenistic engagement may demotivate patients to participate. To avoid this pitfall, the importance of “creating a receptive context” is stressed, along with open communication, honesty, and trust between doctors, patients, and other participants (12, 56).
Furthermore, the results of our systematic review at the organizational level show that, although low levels of patient engagement do inform healthcare providers about the values held by patients, once this input has been made by patients and their family members, they are no longer involved in improving healthcare services. Patients and families are rarely involved in collaborative thinking about ways to improve healthcare, even though the literature suggests that higher levels of patient engagement can increase the likelihood of improving care processes (12, 16, 52, 53, 57). To determine what is of value to patients, in other words what matters most to patients, patients have to be engaged in the development of healthcare services (52). To summarize, we believe that higher levels of patient engagement at the organizational level (e.g., involvement in redesigning care processes) can be of tremendous value when implementing VBHC.
4.1. Strengths and limitations
A strength of our study is that it focuses on organizational-level patient engagement in a VBHC setting, a field that to the best of our knowledge has not previously been addressed in a systematic review. This is a developing and relevant field because both VBHC and patient engagement are of growing importance in improving healthcare and in the ongoing shift from volume-driven to value-driven healthcare delivery. In addition, VBHC initially focuses on the needs of patients at the direct care level, whereby this systematic review shows that there are already 21 papers at the organizational level of patient engagement in a VBHC context.
There are five limitations in this study. First, we specifically included empirical research in the VBHC field that involved any form of patient engagement. By only including current research related to hospital care, we did not include primary care or chronic care for the elderly in nursing homes. The motivation for limiting ourselves to research involving hospitals was prompted by the fact that VBHC always aims to improve the full cycle of care, and so hospitals are always an element in this. Second, as a result of our 21 included articles, 19 papers were observational and two randomized. Due to this, there may be a limited level of evidence, however, this study shows that the observational articles contain a relatively large number of cohort and cross-control studies that are in the highest levels of observational studies (58). Third, due to the choice of MMAT as quality assessment tool, we did not analyze inconsistency and publication bias, which could be important items for assessing the quality of the studies. Fourth, we only included peer-reviewed publications, which may mean that we have overlooked relevant VBHC initiatives. Finally, the perspective of this study is limited to the definition of VBHC as introduced by Porter on patient and organizational level. Although Porter's definition may have evolved over time, especially in Europe, allocative and societal value play hardly a role in his definition.
5. Conclusion
This study included 21 articles, the majority of which were observational, resulting in a limited quality of evidence. Our main contribution is highlighting that extensive patient engagement, as a valuable approach to improving healthcare at the organizational level in a VBHC setting, is rarely used. Current engagement tools between care providers and patients rarely go beyond the communication level of interviews and questionnaires. While this form of communication may be of value to care providers seeking to improve healthcare, it ignores the possibilities of higher-level engagement such as co-design and collaboration. Higher-level engagement would provide an opportunity to improve healthcare and care pathways through co-production with the people being served. We would urge VBHC initiatives to embrace all levels of patient engagement to ensure that patient values find their way to the heart of these initiatives.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
MV and WS: involved in the conceptualization of the study, development of the search strategy, screened all papers (first screener), formal analysis, and original draft and editing. MJ: involved in the resources, review, editing, and supervision. AF: involved in the conceptualization of the study, screened a subset of the articles (second screener), resources, review, editing, and supervision. KA: involved in the conceptualization of the study, development of the search strategy, screened a subset of the articles (second screener), resources, review, editing, and supervision. All authors approved the final version of the manuscript.
Acknowledgments
The authors wish to thank W. M. Bramer from the Erasmus MC Medical Library for developing and updating the search strategies.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2023.1144027/full#supplementary-material
References
1. Porter ME, Teisberg EO. Redefining Health Care: Creating Value-Based Competition on Results. Bostan, MA: Harvard Business Press. (2006).
2. Hogle LF. Accounting for accountable care: Value-based population health management. Soc Stud Sci. (2019) 49:556–82. doi: 10.1177/0306312719840429
3. Berwick DM. Era 3 for Medicine and Health Care. JAMA. (2016) 315:1329–30. doi: 10.1001/jama.2016.1509
4. European Commission Directorate-General for Health Food Safety. (2019). Opinion on assessing the impact of digital transformation of health services. Publications Office. Available online at: https://data.europa.eu/doi/10.2875/644722 (accessed March 21, 2023).
5. Porter ME. What is value in health care? N Engl J Med. (2010) 363:2477–81. doi: 10.1056/NEJMp1011024
6. Nilsson K Bååthe F Andersson AE Wikström E Sandoff M. Experiences from implementing value-based healthcare at a Swedish University Hospital - an longitudinal interview study. BMC Health Serv Res. (2017) 17:169. doi: 10.1186/s12913-017-2104-8
7. Damman OC, Verbiest MEA, Vonk SI, Berendse HW, Bloem BR, de Bruijne MC, et al. Using PROMs during routine medical consultations: The perspectives of people with Parkinson's disease and their health professionals. Health Expect. (2019) 22:939–51. doi: 10.1111/hex.12899
8. Lapin BR, Honomichl R, Thompson N, Rose S, Abelson A, Deal C, et al. Patient-reported experience with patient-reported outcome measures in adult patients seen in rheumatology clinics. Qual Life Res. (2021) 30:1073–82. doi: 10.1007/s11136-020-02692-2
9. Bausewein C, Simon ST, Benalia H, Downing J, Mwangi-Powell FN, Daveson BA, et al. Implementing patient reported outcome measures (PROMs) in palliative care–users' cry for help. Health Qual Life Outcomes. (2011) 9:27. doi: 10.1186/1477-7525-9-27
10. van der Willik EM, van Zwet EW, Hoekstra T, van Ittersum FJ, Hemmelder MH, Zoccali C, et al. Funnel plots of patient-reported outcomes to evaluate health-care quality: Basic principles, pitfalls and considerations. Nephrology (Carlton). (2021) 26:95–104. doi: 10.1111/nep.13761
11. Steinmann G, Delnoij D, van de Bovenkamp H, Groote R, Ahaus K. Expert consensus on moving towards a value-based healthcare system in the Netherlands: a Delphi study. BMJ Open. (2021) 11:e043367. doi: 10.1136/bmjopen-2020-043367
12. Bombard Y, Baker GR, Orlando E, Fancott C, Bhatia P, Casalino S, et al. Engaging patients to improve quality of care: a systematic review. Implement Sci. (2018) 13:98. doi: 10.1186/s13012-018-0784-z
13. Palumbo R. Contextualizing co-production of health care: a systematic literature review. Int J Public Sector Manag. (2016) 29:72–90. doi: 10.1108/IJPSM-07-2015-0125
14. Gedney N, Sipma W, Søndergaard H. Innovations in dialysis: the user's perspective. Nat Rev Nephrol. (2020) 16:544–5. doi: 10.1038/s41581-020-0292-7
15. Domecq JP, Prutsky G, Elraiyah T, Wang Z, Nabhan M, Shippee N, et al. Patient engagement in research: a systematic review. BMC Health Serv Res. (2014) 14:89. doi: 10.1186/1472-6963-14-89
16. Bellows M, Kovacs Burns K, Jackson K, Surgeoner B, Gallivan J. Meaningful and effective patient engagement: what matters most to stakeholders. Patient Exper J. (2015) 2:18–28. doi: 10.35680/2372-0247.1069
17. Graham I, Filippatos G, Atar D, Vardas PE, Pinto FJ, Fitzsimons D. Patient engagement. Eur Heart J. (2017) 38:3114–5. doi: 10.1093/eurheartj/ehx600
18. Boudes M, Robinson P, Bertelsen N, Brooke N, Hoos A, Boutin M, et al. What do stakeholders expect from patient engagement: Are these expectations being met? Health Expect. (2018) 21:1035–45. doi: 10.1111/hex.12797
19. Anderson NN, Dong K, Baker GR, Moody L, Scane K, Urquhart R, et al. Impacts of patient and family engagement in hospital planning and improvement: qualitative interviews with patient/family advisors and hospital staff. BMC Health Serv Res. (2022) 22:360. doi: 10.1186/s12913-022-07747-3
20. Van der Voorden M, Ahaus K, Franx A. Explaining the negative effects of patient participation in patient safety: an exploratory qualitative study in an academic tertiary healthcare centre in the Netherlands. BMJ Open. (2023) 13:e063175. doi: 10.1136/bmjopen-2022-063175
21. Arnstein SR A ladder of citizen participation. J Am Inst Plann. (1969) 35:216–24. doi: 10.1080/01944366908977225
22. Bate P, Robert G. Experience-based design: from redesigning the system around the patient to co-designing services with the patient. Qual Saf Health Care. (2006) 15:307–10. doi: 10.1136/qshc.2005.016527
23. Carman KL, Dardess P, Maurer M, Sofaer S, Adams K, Bechtel C, et al. Patient and family engagement: a framework for understanding the elements and developing interventions and policies. Health Aff (Millwood). (2013) 32:223–31. doi: 10.1377/hlthaff.2012.1133
24. Tritter JQ, McCallum A. The snakes and ladders of user involvement: Moving beyond Arnstein. Health Policy. (2006) 76:156–68. doi: 10.1016/j.healthpol.2005.05.008
25. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. Int J Surg. (2021) 88:105906. doi: 10.1016/j.ijsu.2021.105906
26. Hong QN, Fàbregues S, Bartlett G, Boardman F, Cargo M, Dagenais P, et al. The Mixed Methods Appraisal Tool (MMAT) version 2018 for information professionals and researchers. Educ. Inf. (2018) 34:285–91. doi: 10.3233/EFI-180221
27. Heyvaert M, Maes B, Onghena P. Mixed methods research synthesis: definition, framework, and potential. Qual Quant. (2013) 47:659–76. doi: 10.1007/s11135-011-9538-6
28. Pluye P, Hong QN. Combining the power of stories and the power of numbers: mixed methods research and mixed studies reviews. Annu Rev Public Health. (2014) 35:29–45. doi: 10.1146/annurev-publhealth-032013-182440
29. Anderson WG, Cimino JW, Lo B. Seriously ill hospitalized patients' perspectives on the benefits and harms of two models of hospital CPR discussions. Patient Educ Couns. (2013) 93:633–40. doi: 10.1016/j.pec.2013.08.003
30. Hennink SD, Hofland N, Gopie JP, van der Kaa C, de Koning K, Nielsen M, et al. Value-based healthcare in Lynch syndrome. Fam Cancer. (2013) 12:347–54. doi: 10.1007/s10689-013-9655-6
31. Van Citters AD, Fahlman C, Goldmann DA, Lieberman JR, Koenig KM, DiGioia AM, et al. Developing a pathway for high-value, patient-centered total joint arthroplasty. Clin Orthop Relat Res. (2014) 472:1619–35. doi: 10.1007/s11999-013-3398-4
32. Kaplan AL, Klein MP, Tan HJ, Setlur NP, Agarwal N, Steinberg K, et al. Use of patient ethnography to support quality improvement in benign prostatic hyperplasia. Healthc (Amst). (2014) 2:263–7. doi: 10.1016/j.hjdsi.2014.10.004
33. Li SX, Thompson KD, Peterson T, Huneven S, Carmichael J, Glazer FJ, et al. Delivering high value inflammatory bowel disease care through telemedicine visits. Inflamm Bowel Dis. (2017) 23:1678–81. doi: 10.1097/MIB.0000000000001210
34. Bernstein DN, Fear K, Mesfin A, Hammert WC, Mitten DJ, Rubery PT, et al. Patient-reported outcomes use during orthopaedic surgery clinic visits improves the patient experience. Musculoskeletal Care. (2019) 17:120–5. doi: 10.1002/msc.1379
35. Coppess S, Soares J, Frogner BK, DeMarre K, Faherty A, Hoang J, et al. A pilot study assessing clinic value in pediatric pharyngeal dysphagia: The OPPS/cost method. Laryngoscope. (2019) 129:1527–32. doi: 10.1002/lary.27552
36. Eppler SL, Kakar S, Sheikholeslami N, Sun B, Pennell H, Kamal RN. Defining quality in hand surgery from the patient's perspective: a qualitative analysis. J Hand Surg Am. (2019) 44:311–320.e4. doi: 10.1016/j.jhsa.2018.06.007
37. Rosseel L, Bieliauskas G, Brodersen BB, Olsen PS, Søndergaard L, De Backer O. Patients and informal caregivers' experience of surgical and transcatheter aortic valve replacement: Real-world data contributing to establish value-based medicine in Denmark. Clin Cardiol. (2019) 42:444–51. doi: 10.1002/clc.23166
38. Wickramasinghe N, John B, George J, Vogel D. Achieving value-based care in chronic disease management: intervention study. JMIR Diabetes. (2019) 4:e10368. doi: 10.2196/10368
39. Depla AL, Ernst-Smelt HE, Poels M, Crombag NM, Franx A, Bekker MN, et al. feasibility study of implementing a patient-centered outcome set for pregnancy and childbirth. Health Sci Rep. (2020) 3:e168. doi: 10.1002/hsr2.168
40. Dronkers EAC, Baatenburg de Jong RJ, van der Poel EF, Sewnaik A, Offerman MPJ. Keys to successful implementation of routine symptom monitoring in head and neck oncology with “Healthcare Monitor” and patients' perspectives of quality of care. Head Neck. (2020) 42:3590–600. doi: 10.1002/hed.26425
41. Fahner JC, Thölking TW, Rietjens JAC, van der Heide A, van Delden JJM, Kars MC. Towards advance care planning in pediatrics: a qualitative study on envisioning the future as parents of a seriously ill child. Eur J Pediatr. (2020) 179:1461–8. doi: 10.1007/s00431-020-03627-2
42. Goretti G, Marinari GM, Vanni E, Ferrari C. Value-Based Healthcare and Enhanced Recovery After Surgery Implementation in a High-Volume Bariatric Center in Italy. Obes Surg. (2020) 30:2519–27. doi: 10.1007/s11695-020-04464-w
43. Pennucci F, De Rosis S, Passino C. Piloting a web-based systematic collection and reporting of patient-reported outcome measures and patient-reported experience measures in chronic heart failure. BMJ Open. (2020) 10:e037754. doi: 10.1136/bmjopen-2020-037754
44. van Veghel D, Soliman-Hamad M, Schulz DN, Cost B, Simmers TA, Dekker LRC. Improving clinical outcomes and patient satisfaction among patients with coronary artery disease: an example of enhancing regional integration between a cardiac centre and a referring hospital. BMC Health Serv Res. (2020) 20:494. doi: 10.1186/s12913-020-05352-w
45. Young JS, Chan AK, Viner JA, Sankaran S, Chan AY, Imershein S, et al. A Safe Transitions Pathway for post-craniotomy neurological surgery patients: high-value care that bypasses the intensive care unit. J Neurosurg. (2020) 134:1386–91. doi: 10.3171/2020.3.JNS192133
46. Ahluwalia R, Cook J, Raheman F, Karuppaiah K, Colegate-Stone T, Tavakkolizadeh A, et al. Improving the efficiency of ankle fracture care through home care and day-surgery units: Delivering safe surgery on a value-based healthcare model. Surgeon. (2021) 19:e95–e102. doi: 10.1016/j.surge.2020.08.004
47. Najafabadi AHZ, van de Mortel JPM, Lobatto DJ, Brandsma DR, Peul WC, Biermasz N, et al. Unmet needs and recommendations to improve meningioma care through patient, partner, and health care provider input: a mixed-method study. Neurooncol Pract. (2020) 7:239–48. doi: 10.1093/nop/npz055
48. Slejko JF, Hong YD, Sullivan JL, Reed RM, dosReis S. Prioritization and refinement of patient-informed value elements as attributes for chronic obstructive pulmonary disease treatment preferences. Patient. (2021) 14:569–79. doi: 10.1007/s40271-021-00495-2
49. Kasalak Ö, Yakar D, Dierckx RAJO, Kwee TC. Radiologist-patient consultation of imaging findings after neck ultrasonography: An opportunity to practice value-based radiology. Clin Imaging. (2022) 81:87–91. doi: 10.1016/j.clinimag.2021.09.022
50. Cossio-Gil Y, Omara M, Watson C, Casey J, Chakhunashvili A, Miguel MG-S, et al. The Roadmap for Implementing Value-Based Healthcare in European University Hospitals-Consensus Report and Recommendations. Value Health. (2022) 25:1148–56. doi: 10.1016/j.jval.2021.11.1355
51. Diaby V, Ali AA, Montero AJ. Value assessment frameworks in the United States: A call for patient engagement. Pharmacoecon Open. (2019) 3:1–3. doi: 10.1007/s41669-018-0094-z
52. Laurance J, Henderson S, Howitt PJ, Matar M, Kuwari HA, Edgman-Levitan S, et al. Patient engagement: four case studies that highlight the potential for improved health outcomes and reduced costs. Health Aff (Millwood). (2014) 33:1627–34. doi: 10.1377/hlthaff.2014.0375
53. Bergerum C, Thor J, Josefsson K, Wolmesjö M. How might patient involvement in healthcare quality improvement efforts work-A realist literature review. Health Expect. (2019) 22:952–64. doi: 10.1111/hex.12900
54. Green T, Bonner A, Teleni L, Bradford N, Purtell L, Douglas C, et al. Use and reporting of experience-based codesign studies in the healthcare setting: a systematic review. BMJ Qual Saf. (2020) 29:64–76. doi: 10.1136/bmjqs-2019-009570
55. Palmer VJ, Weavell W, Callander R, Piper D, Richard L, Maher L, et al. The Participatory Zeitgeist: an explanatory theoretical model of change in an era of coproduction and codesign in healthcare improvement. Med Humanit. (2019) 45:247–57. doi: 10.1136/medhum-2017-011398
56. Haywood K, Lyddiatt A, Brace-McDonnell SJ, Staniszewska S, Salek S. Establishing the values for patient engagement (PE) in health-related quality of life (HRQoL) research: an international, multiple-stakeholder perspective. Qual Life Res. (2017) 26:1393–404. doi: 10.1007/s11136-016-1465-5
57. Coulter A, Locock L, Ziebland S, Calabrese J. Collecting data on patient experience is not enough: they must be used to improve care. BMJ. (2014) 348:g2225. doi: 10.1136/bmj.g2225
Keywords: value-based healthcare (VBHC), patient engagement, quality improvement, patient perspective, co-design, co-production, communication
Citation: van der Voorden M, Sipma WS, de Jong MFC, Franx A and Ahaus KCTB (2023) The immaturity of patient engagement in value-based healthcare—A systematic review. Front. Public Health 11:1144027. doi: 10.3389/fpubh.2023.1144027
Received: 13 January 2023; Accepted: 10 April 2023;
Published: 11 May 2023.
Edited by:
Mora Claramita, Gadjah Mada University, IndonesiaReviewed by:
Elena Vlahu-Gjorgievska, University of Wollongong, AustraliaPedro Ruiz-Lopez, Research Institute Hospital 12 de Octubre, Spain
Copyright © 2023 van der Voorden, Sipma, de Jong, Franx and Ahaus. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Michael van der Voorden, bS52YW5kZXJ2b29yZGVuQGVyYXNtdXNtYy5ubA==
†These authors have contributed equally to this work and share first authorship
 Michael van der Voorden
Michael van der Voorden Wim S. Sipma
Wim S. Sipma Margriet F. C. de Jong3
Margriet F. C. de Jong3 Kees C. T. B. Ahaus
Kees C. T. B. Ahaus