- 1Shenzhen Bao'an District Central Hospital, Shenzhen, China
- 2School of Public Health, Guangdong Pharmaceutical University, Guangzhou, China
- 3Guangdong Provincial Engineering Research Center of Public Health Detection and Assessment, Guangdong Pharmaceutical University, Guangzhou, China
Background: Due to the outbreak of Coronavirus Disease 2019, there has been a significant impact on the mental health of parents. However, no detailed study on the mental health status of parents has been conducted to date.
Methods: This study was a cross-sectional used a whole-group random sampling method to conduct an online questionnaire survey with 102,883 parents in Guangdong Province, China, April 25, 2020 and May 14, 2020. Anxiety was assessed by using the Generalized Anxiety Disorder tool (GAD-7). Potential factors of anxiety were estimated using univariate analysis and multivariate logistic regression analysis by SPSS 22.0 statistical software.
Results: Among the total 94,705 parents who have completed the questionnaire survey (92.05% response rate). The incidence of anxiety was 23.77%. Parents' anxiety symptoms are more likely to be caused by female family roles, higher levels of education, unemployed or jobless employment status, children not being an only child, and children having negative attitudes toward online courses.
Conclusions: Our research shows that most parents experienced mild anxiety during the Coronavirus Disease 2019 epidemic. Our findings provide strong evidence for investigating and focusing on the mental health of this population during the COVID-19 epidemic. Therefore, governments and healthcare departments at all levels should actively provide psychological counseling services to relieve their anxiety symptoms.
1. Introduction
Since December 2019, COVID-19 – a cluster of acute respiratory illness with unknown causes (1) has spread rapidly in China and whole world, causing a serious damage to human life and health. The World Health Organization declared the coronavirus disease 2019 is a pandemic on March 11, 2020 (2), and the world entered a state of emergency. The COVID-19 not only brings people in China and other parts of the world the risk of death due to virus infection, but also brings unbearable psychological pressure (3, 4). In 2017, data from the Global Burden of Disease Study showed that the global prevalence of anxiety disorders was 3,721,764 cases per 100,000 people, ranking first among mental disorders (5). The sudden COVID-19 pandemic and the home isolation measures adopted by the government can be regarded as a kind of social isolation to some extent. It is understood that in the absence of interpersonal communication, anxiety disorders are more likely to occur and worsen (6). In an early study about investigating immediate psychological response during COVID-19 epidemic among general population in China reported that 53.8% of participants rated the psychological impact of the outbreak as moderate or severe (7). During COVID-19 pandemic, home isolation measures led to the physical and social isolation of parents, who suffered not only from work and financial problems, but also from the stresses of family life. Concerns about the health of family and friends and planning for the future in this new and uncertain situation. Especially with the delayed start of school for students nationwide and “stop classes without stopping” to carry out online classes for home learning, parents of students must supervise their children's learning, tutor homework and communicate with their teachers in a timely manner to ensure their children's normal learning status, in addition to protecting themselves and their families, resuming work and production pressure. All of these factors can lead to elevated levels of parental stress and accompanying symptoms of anxiety. Hence, a timely understanding of anxiety status is urgently needed.
At present, there is evidences that infectious diseases are associated with mental health problems in general population (8, 9), medical personnel (10, 11), patients, children and the elderly (12–14). However, no detailed study on the mental health status of parents of students has been conducted to date. Therefore, by understanding the anxiety level of Chinese students' parents during the COVID-19 epidemic and its influencing factors, our study is hereby carried out a cross-sectional study to provide a certain reference for relevant departments to carry out psychological intervention and guidance to the masses.
2. Materials and methods
2.1. Data collection
The anxiety level and related factors of the parents of students during the epidemic were evaluated by a cross-sectional survey. We used the online-based program “questionnaire star” as the survey vehicle and the education system as the backbone, the link to the questionnaire was sent to school heads in various cities in Guangdong Province. Participants voluntarily scans the QR code or clicks on the relevant link to fill in, and the survey respondent's informed consent is by default obtained. The questionnaire is equipped with mandatory questions and jump questions to ensure the completeness and logic of the answers. After the questionnaire is submitted, the researcher conducts manual screening, and deletes the answer sheets with obvious errors and “questionnaire response time ≤4 min” to ensure the authenticity and validity of the data obtained. The same IP address can only be answered once. The study was approved by the Medical Ethics Review Board of the School of Public Health, Guangdong Pharmaceutical University (IRB 2023–001), and complied with the Declaration of Helsinki guidelines. A total of 102,883 questionnaires from parents of students were collected anonymously from April 25, 2020 to May 14, 2020. 94705 questionnaires were available, the effective rate of the questionnaire was 92.05%.
2.2. Survey instrument
The content of the questionnaire includes general demographic characteristics and the Generalized Anxiety Disorder-7 (GAD-7). General information includes parental role, age, education level, employment status, per capita monthly household income, grade level of the child, access to internet classes, meals and exercise, etc. GAD-7 is an effective tool to identify cases of generalized anxiety disorder (15) and has good reliability and validity in previous studies on anxiety (16, 17). The Cronbach's alpha coefficient for the GAD-7 was 0.92. It has been recommended by the Psychiatric Branch of the Chinese Medical Association and the American Psychiatric Association. GAD-7 can be used to screen, diagnose and evaluate the severity of anxiety disorders, as well as social phobia, post–traumatic stress disorder and panic disorder (18). It takes less than 3 min to complete and easy to score (19). The GAD-7 measures the frequency of symptoms in 7 areas, according to the scoring criteria (20), including “not at all”, “a few days”, “more than a week” and “almost every day”, the corresponding scores are 0, 1, 2, and 3. The total score ranges from 0 to 21 points, the higher the total score, the higher the degree of anxiety disorder. Among them, a total score of 0 to 4 as no GAD, 5 to 9 as mild GAD, 10 to 14 as moderate GAD, and 15 to 21 as severe GAD. The Cronbach's alpha coefficient in the present study is 0.92.
2.3. Statistical analyses
Categorical variables were expressed as frequencies and percentages. Univariate analyses were conducted using the Kruskal–Wallis H-test. Independent correlations between anxiety symptoms and independent variables were assessed using multivariate logistic regression analysis. Model calibration was evaluated using the Hosmer-Lemeshow goodness-of-fit statistic. Statistical analyses were performed using SPSS 22.0 and a two-sided P < 0.05 was considered a statistically significant difference.
3. Results
3.1. Characteristics of the participants
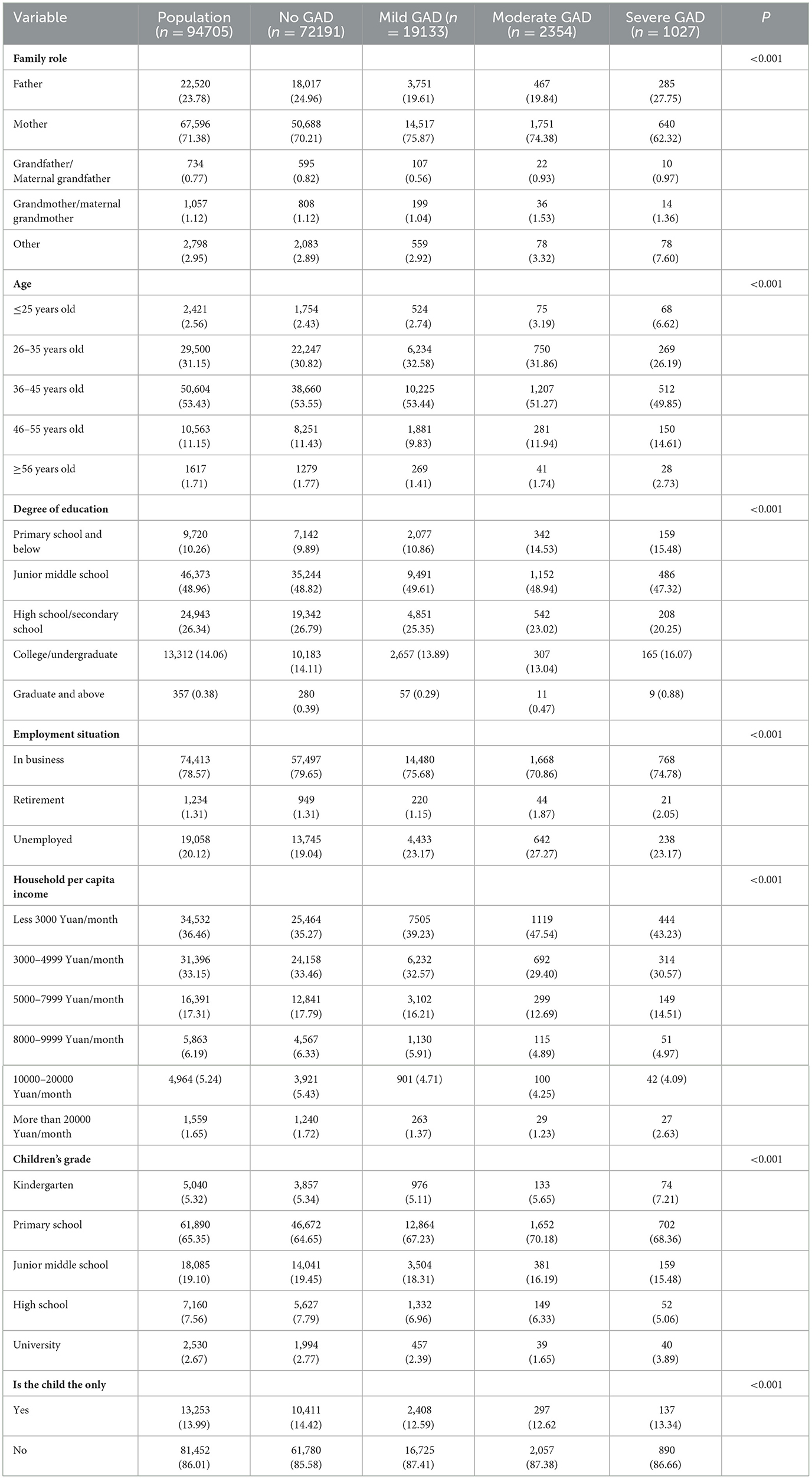
Table 1 shows the characteristics of the participants. Of 94,705 parents, 22,514 parents experienced anxiety disorders during the outbreak. The majority of participants were between the ages of 36–45 years. The participants were mainly mothers 67,596 (71.38%), most parents had junior high school education or above 84,985 (89.74%), the majority of parents were employed 74,413 (78.57%), the per capita monthly household income was mainly below 3,000/month 34,532 (36.46%), nearly half of the children were in primary school 61,890 (65.35%) and not the majority of children are in primary school 61,890 (65.35%) and are not only children 81,452 (86.01%).
3.2. Univariate analysis of potential factors related to symptoms of anxiety among parents during the COVID-19 epidemic
The overall prevalence of anxiety symptoms was 23.77%. Of these, 72,191 (76.23%) had no anxiety symptoms (0–4); 19,133 (20.21%) had mild anxiety symptoms (5–9); 23,54 (2.49%) had moderate anxiety symptoms (10–14); and 1,027 (1.07%) had severe anxiety symptoms (15–21). Table 1 shows that family role, age, education, employment status, monthly income per capita, grade level of the child, and whether or not the child is an only child are all potential factors related to anxiety symptoms (P < 0.001).
3.2.1. Relationship between family and self COVID-19 infection status and anxiety symptoms
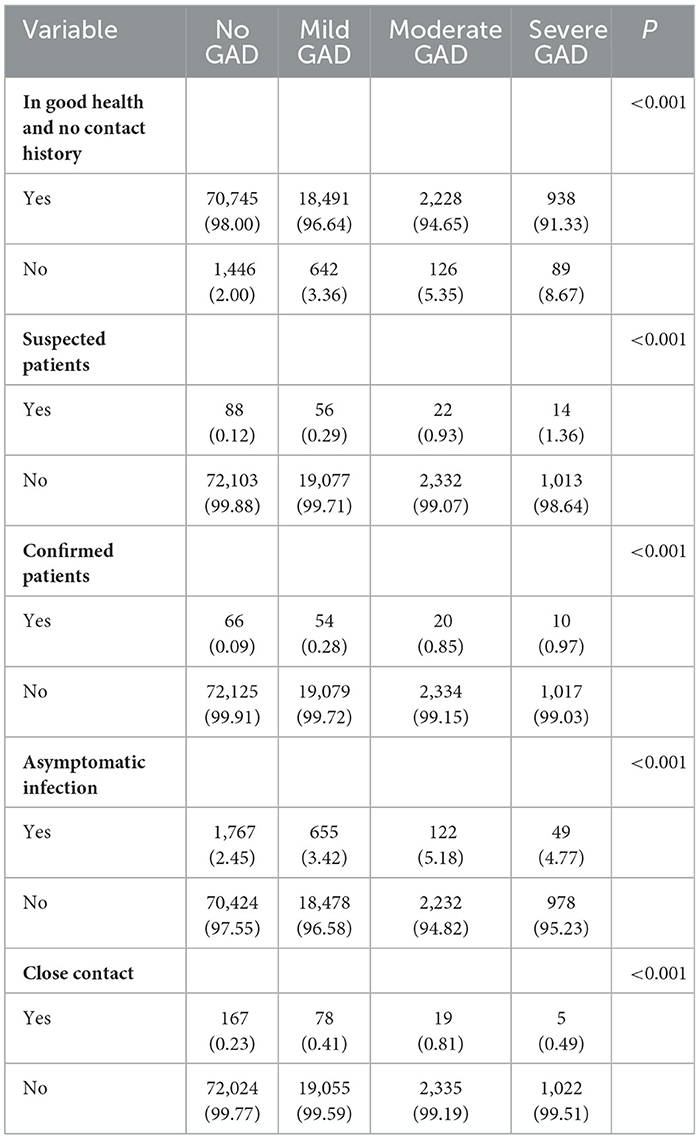
As the survey was conducted during a period of home isolation for outbreak prevention and control, it was particularly important to understand the impact of parents' own and their families' physical health on anxiety. Table 2 presents that participants who are in good health and have no history of exposure are less likely to experience anxiety (76.56% had no anxiety symptoms). The level of anxiety was higher in cases with confirmed patients than in other cases (P < 0.001).
3.2.2. Relationship between children's access to internet classes, meals, exercise, and anxiety symptoms
Both children's and parents' attitudes toward Internet classes were influential factors in anxiety symptoms. Those with “strongly dislike” (0.53% had no anxiety symptoms) and “doesn't matter” (11.22% had no anxiety symptoms) attitudes had higher levels of anxiety than the rest of the group (Table 3).
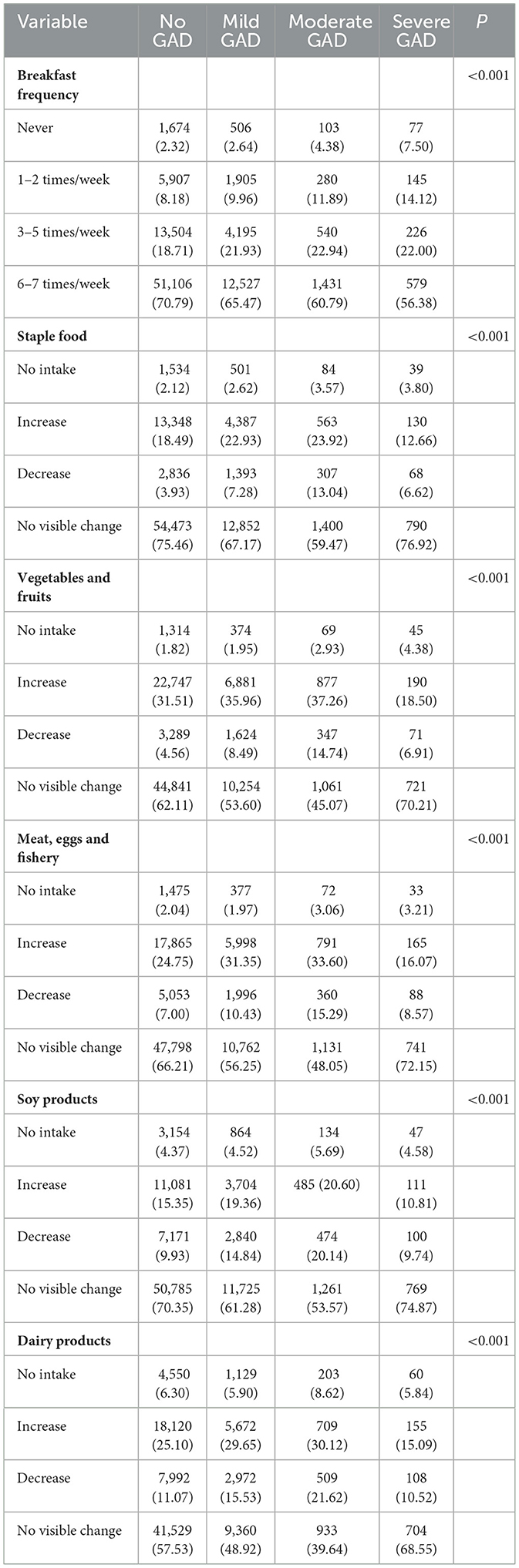
The frequency of breakfast “6–7 times/week” (70.79% had no anxiety symptoms) and the option “no significant change” (75.46%, 62.11%, 66.21%, 70.35%, 57.53% had no anxiety symptoms) had the lowest number of anxieties, while the options “never eat breakfast” (2.32% had no anxiety symptoms) and “no intake” (2.12%,1.81%,2.04%,4.37%,6.30% had no anxiety symptoms) were both more anxious than the other cases (Table 4).
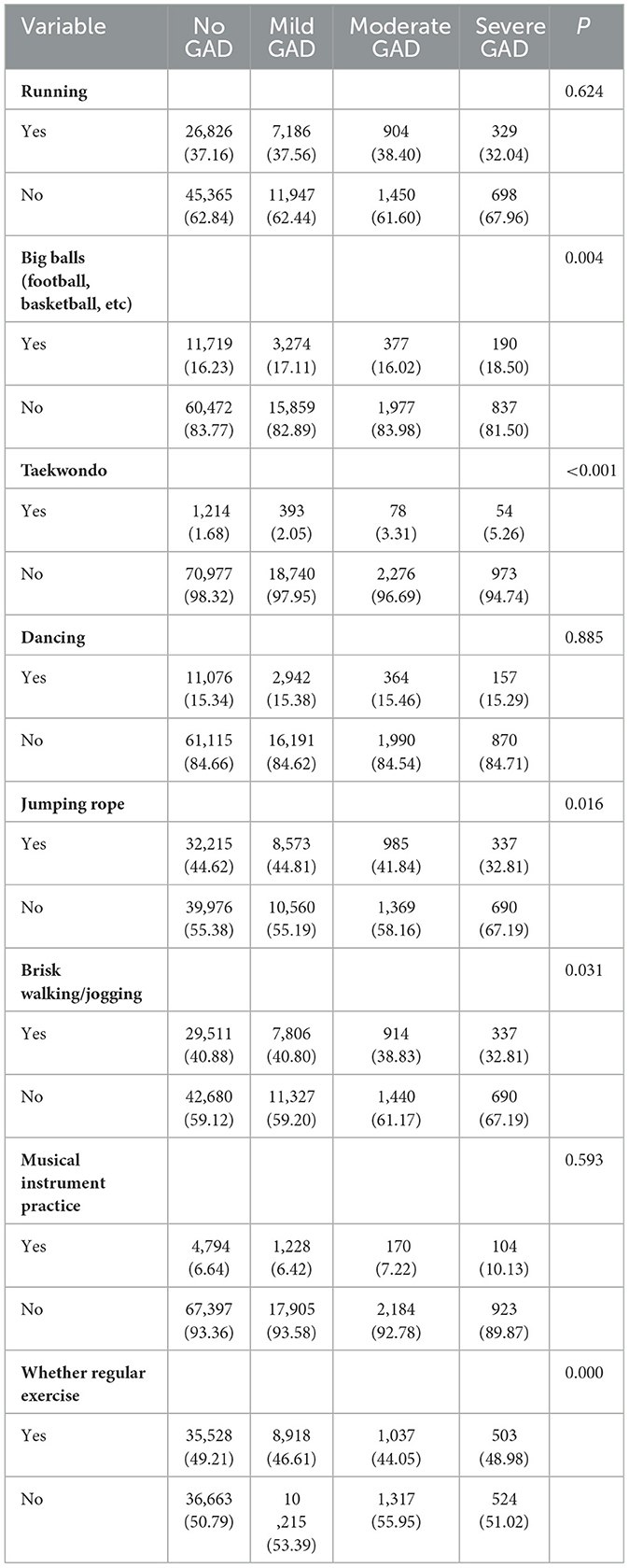
In terms of the children exercise profile, big balls (football, basketball, etc.), taekwondo, skipping rope, brisk walking/jogging, and whether or not the exercise was regular were all potential factors on anxiety symptoms, while running, dancing, and practicing musical instruments were not potential factors in anxiety symptoms. Choosing Taekwondo (1.68% had no anxiety symptoms) as a form of exercise is associated with higher levels of anxiety than other sports (Table 5).
3.3. Multivariate logistic regression analysis of factors significantly associated with anxiety symptoms among parents during the COVID-19 epidemic
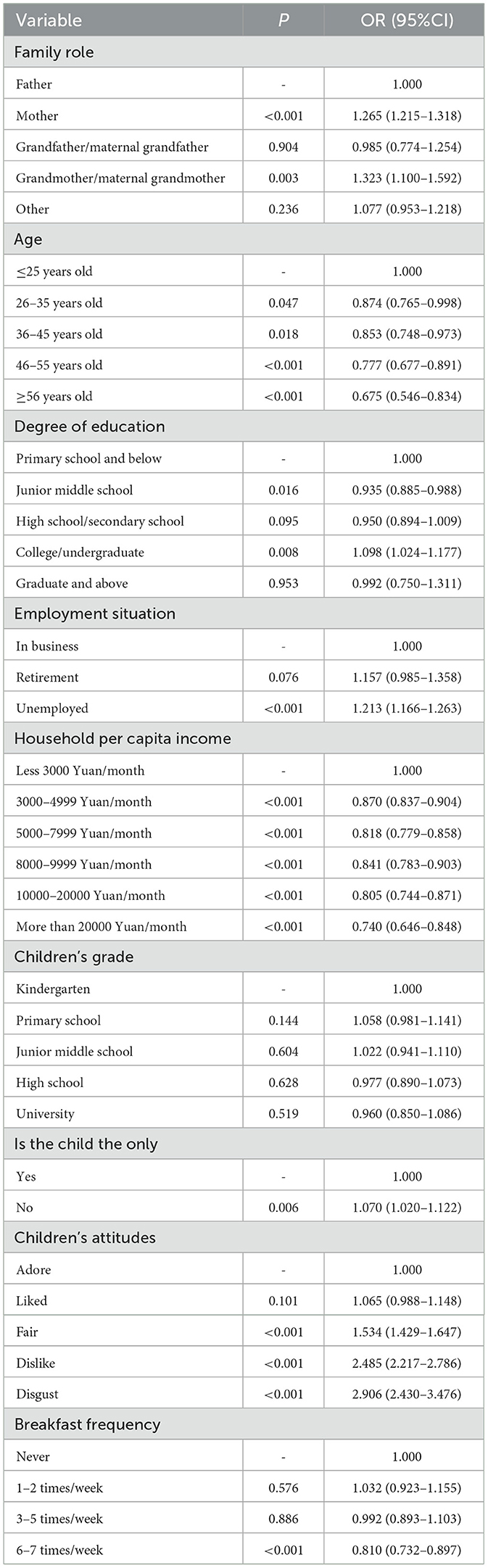
In multiple logistic regression analysis, mother (OR = 1.265, 95% CI: 1.215–1.318) and (maternal) grandmother (OR = 1.323, 95% CI: 1.100–1.592), college/bachelor's degree (OR = 1.098, 95% CI: 1.024–1.177), unemployed or jobless (OR = 1.213, 95% CI: 1.166–1.263), child not an only child (OR = 1.070, 95% CI: 1.020–1.122), child's attitude toward online classes was fair (OR = 1.534, 95% CI: 1.429–1.647), disgusted (OR = 2.485, 95% CI: 2.217–2.786), very averse (OR = 2.906, 95% CI: 2.430–3.476) were more likely to show symptoms of anxiety.
Age: 26–35 years (OR = 0.874, 95% CI: 0.765–0.998), 36–45 years (OR = 0.853, 95% CI: 0.748–0.973), 46–55 years (OR = 0.777, 95% CI: 0.677–0.891), ≥56 years (OR = 0.675, 95% CI. 0.546–0.834), lower secondary education (OR = 0.935, 95% CI: 0.885–0.988), per capita monthly income: 3000–4999/month (OR = 0.870, 95% CI: 0.837–0.904), 5000–7999/month (OR = 0.818, 95% CI: 0.779- 0.858), 8000–9999 /month (OR = 0.841, 95% CI: 0.783–0.903), 10,000–20,000 /month (OR = 0.805, 95% CI: 0.744–0.871), 20,000 or more/month (OR = 0.740, 95% CI: 0.646–0.848), children's breakfast frequency 6–7 times/week (OR = 0.810,95%CI: 0.732–0.897) had a significant protective effect against parents developing symptoms of anxiety. See in Table 6.
4. Discussion
During COVID-19 pandemic, there was widespread concern about the mental health status of health care workers, children, older people and so on. There is little research on parental mental health issues. Parents, as the backbone of society and families, are under more pressure than usual. On the one hand, some families are under increased financial pressure due to economic changes and rising unemployment. On the other hand, home isolation measures has led to parents working at home while caring for and educating their children, and the double pressure has brought about a surge in anxiety among parents. Our study shows that the number of people with anxiety accounted for 23.77% of the total number of people. The mood of anxious people is mainly mild anxiety, which is similar to the survey results of Sun et al. (21). Parents with multiple children are more likely to be anxious and have higher levels of anxiety. This phenomenon is likely due to parents have more to worry about as they juggle their daily work and life while tutoring or supervising multiple children online. For students with negative attitudes toward online classes, the level of parental anxiety is even higher. Students usually receive information passively and lack active communication in online classes, and over time they may lose interest in online courses (22, 23). Parents are generally very concerned about their children's academic performance, and their children's negative attitudes toward online classes can add to their concerns.
In terms of meals, the more frequently children eat breakfast, the lower the anxiety of parents. This may be due to the fact that both parents and children are confined to their home during home isolation, and the prolonged periods of confinement make people prone to emotional instability. The regularity of children's eating habits will ease the irritability of parents. Isolation at home enables parents to supervise and feed their children, showing healthier eating habits (24). Our study found children's intake of all types of food did not change much compared to usual during the epidemic. These findings were consistent with a cross-sectional study in the China, which showed that 65% of participants did not change their eating habits during the epidemic (25) This study was conducted during the recovery period of the epidemic when people's lives were gradually returning to normal compared to the outbreak period, and dietary patterns were likely to be consistent with usual.
In addition to the influencing factors brought by children, parents' own conditions can also cause anxiety. In the family, mothers and grandmothers have relatively high levels of anxiety. It was said to be due to a heightened sensitivity of females to the threat (26), the result has implications for the identification of risk groups and interventions. Also anxiety may be related to estrogen levels, with studies showing a significant increase in anxiety levels during the first menstrual period and in post-menopausal women (27) It has been shown that circulating estradiol increases abruptly from prepubertal to adult levels during the sexual developmental phase, and therefore the risk of anxiety symptoms was significantly increased at the first menstrual period (28, 29). Among the influencing factors of age, parents of young students are more likely to have anxiety, which is similar to previous studies on age and anxiety (29–31). Older parents will have some financial means (some savings) even in the face of the epidemic, while younger parents will generally have less financial means than older ones (32). On the other hand, young people rely more on getting news about the epidemic from the Internet, and they receive more negative news than parents of older students. This may lead to anxiety about their future and concerns about their family and children. At this time, parents of students should maintain an objective and rational attitude in the face of numerous reports, and adjust their personal mentality.
There are signs that the increase in the number of patients and suspected cases, as well as the increase in the number of provinces and countries affected by the epidemic, has triggered public concerns about being infected in this epidemic. (33). The results of present study show that parents' anxiety about the epidemic is related to whether they and their family members are infected with the new crown pneumonia virus.
Research by Hinz et al. (34) also suggest that anxiety is related to unemployment and low income. As expected, the unemployed parents are more likely to have anxiety (35). The lower the income level, the higher their anxiety. Studies have shown that low-income households are more likely to experience financial hardship (e.g. loss of employment or pay cuts) (36). Income sources are suspended, and prices of epidemic prevention materials and daily necessities have risen during the epidemic. Income and expenditure are a huge challenge. Parents with relatively high incomes and stable employment have sufficient savings and resources to cope with the economic crisis brought about by the epidemic, while parents with low monthly household incomes will have more worries about their own and their families' future. On the other hand, the negative emotions of low-income parents may also affect their children, causing children from low-income families to show some degree of anxiety (37). These results suggest that financial support and psychological support are effective ways to alleviate anxiety during the epidemic.
At this particular time, anxiety is just as worrying as the virus. It is even more important for parents to adapt themselves and their children physically and mentally to protect themselves from the epidemic. There are several suggestions for this: First, relax and be optimistic. When you feel down, you can talk with your family and exercise together to relieve anxiety. Second, keep a regular schedule and healthy. During home isolation, it is also necessary to maintain regular work and rest, set an example, cultivate children's good living habits, and create a healthy and positive family atmosphere, which is more conducive to the removal of anxiety. Thirdly, the relevant authorities can help people through this difficult time by providing rent relief, reducing taxes and fees, stabilizing employment and granting temporary subsidies.
The limitations of this study is that the sample comes from Guangdong Province, but the distribution is uneven, and it cannot yet better represent the national situation; In addition, the collection of questionnaire is obtained through the student group contacting parentsand the results only represent a part of the population. In the future, researchers will expand representation of population and increase the sample size in all cities across the country, if possible, further to carry out cohort studies, and conduct research on the anxiety intervention of Chinese residents.
5. Conclusions
This study analyzed the anxiety level and related factors of the parents of students during the epidemic, and found that 23.77% of the parents had anxiety symptoms. Although the degree of anxiety of parents is mild, but the long-term lack of interpersonal communication is very likely to increase the degree of anxiety. Therefore, during the period of coronavirus disease 2019, governments and healthcare departments at all levels should actively provide psychological counseling services to relieve their anxiety symptoms.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by the Medical Ethics Review Board of the School of Public Health, Guangdong Pharmaceutical University. Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
Author contributions
XZ, JH, YL, and DZ were involved in setting up the study and data collection. SZ, YL, and QC contributed to the data analysis. XZ drafted the manuscript. All authors approved the final version of the paper.
Funding
This study was funded by the Medical Science and Technology Foundation of Guangdong Province [Grant No. 2019GCZX012 (QC)].
Acknowledgments
We thank all the parents who took part in this study. We are grateful for your contribution.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Wuhan Municipal Health Commission. Report of Novel Coronavirus-Infected Pneumonia in China. (2020). Available online at: http://wjw.wuhan.gov.cn/front/web/showDetail/2020012009077 (accessed January 20, 2020).
2. WHO. Coronavirus Disease (COVID-19) Situation Report-136. (2020). Available online at: https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200604-covid19-sitrep-136.pdf?sfvrsn=fd36550b_2 (accessed June 4, 2020).
3. Xiao C. A novel approach of consultation on 2019 novel coronavirus (COVID-19)-related psychological and mental problems: structured letter therapy. Psychiatry Investig. (2020) 17:175–6. doi: 10.30773/pi.2020.0047
4. Duan L, Zhu G. Psychological interventions for people affected by the COVID-19 epidemic. Lancet Psychiatry. (2020) 7:300–2. doi: 10.1016/S2215-0366(20)30073-0
5. GBD 2017 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. (2018) 392:1789–858. doi: 10.1016/S0140-6736(18)32279-7
6. Kmietowicz Z. Rules on isolation rooms for suspected covid-19 casesin GP surgeries to be relaxed. BMJ. (2020) 368:m707. doi: 10.1136/bmj.m707
7. Wang C, Pan R, Wan X, Tan Y, Xu L, Ho CS, et al. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int J Environ Res Public Health. (2020) 17:1729. doi: 10.3390/ijerph17051729
8. Taha S, Matheson K, Cronin T, Anisman H. Intolerance of uncertainty, appraisals, coping, and anxiety: the case of the 2009 H1N1 pandemic. Br J Health Psychol. (2014) 19:592–605. doi: 10.1111/bjhp.12058
9. Cowling BJ, Ng DM, Ip DK, Liao Q, Lam WW, Wu JT, et al. Community psychological and behavioral responses through the first wave of the 2009 influenza A(H1N1) pandemic in Hong Kong. J Infect Dis. (2010) 202:867–76. doi: 10.1086/655811
10. Bai Y, Lin CC, Lin CY, Chen JY, Chue CM, Chou P. (2004). Survey of stress reactions among health care workers involved with the SARS outbreak. Psychiatr Serv. (2004) 55:1055–7. doi: 10.1176/appi.ps.55.9.1055
11. Lee SM, Kang WS, Cho AR, Kim T, Park JK. Psychological impact of the 2015 MERS outbreak on hospital workers and quarantined hemodialysis patients. Compr Psychiatry. (2018) 87:123–7. doi: 10.1016/j.comppsych.2018.10.003
12. Chen Q, Liang M, Li Y, Guo J, Fei D, Wang L, et al. Mental health care for medical staff in China during the COVID-19 outbreak. Lancet Psychiatry. (2020) 7:e15–6. doi: 10.1016/S2215-0366(20)30078-X
13. Yang Y, Li W, Zhang Q, Zhang L, Cheung T, Xiang YT. Mental health services for older adults in China during the COVID-19 outbreak. Lancet Psychiatry. (2020) 7:e19. doi: 10.1016/S2215-0366(20)30079-1
14. Li SW, Wang Y, Yang YY, Lei XM, Yang YF. Analysis of influencing factors of anxiety and emotional disorders in children and adolescents during home isolation during the epidemic of novel coronavirus pneumonia. Chin J Child Health. (2020) 28:1–9. doi: 10.11852/zgetbjzz2020-0169
15. Spitzer RL, Kroenke K, Williams JB, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. (2006) 166:1092–7. doi: 10.1001/archinte.166.10.1092
16. Toussaint A, Hüsing P, Gumz A, Wingenfeld K, Härter M, Schramm E, et al. Sensitivity to change and minimal clinically important difference of the 7-item generalized anxiety disorder questionnaire (GAD- 7). J Affect Disord. (2020) 265:395–401. doi: 10.1016/j.jad.2020.01.032
17. Wei L, Shi L, Cao J. Analysis of the psychological status of primary medical workers in Shanghai during the new coronavirus pneumonia epidemic. J Tongji Univ. (2020) 41:155–60. doi: 10.16118/j.1008-0392.2020.02.003
18. Moreno E, Muñoz-Navarro R, Medrano LA, González-Blanch C, Ruiz-Rodríguez P, Limonero JT, et al. Factorial invariance of a computerized version of the GAD-7 across various demographic groups and over time in primary care patients. J Affect Disord. (2019) 252:114–21. doi: 10.1016/j.jad.2019.04.032
19. Budikayanti A, Larasari A, Malik K, Syeban Z, Indrawati LA, Octaviana F. Screening of generalized anxiety disorder in patients with epilepsy: using a valid and reliable indonesian version of generalized anxiety disorder-7 (GAD-7). Neurol Res Int. (2019). doi: 10.1155/2019/5902610
20. Schalet BD, Cook KF, Choi SW, Cella D. Establishing a common metric for self-reported anxiety: linking the MASQ, PANAS, and GAD-7 to PROMIS Anxiety. J Anxiety Disord. (2014) 28:88–96. doi: 10.1016/j.janxdis.2013.11.006
21. Sun M, Li S, Yue H, Li X, Li W, Xu S. Analysis of my country's netizens' anxiety and its influencing factors during the new crown pneumonia epidemic. World Sci Technol Modernization Trad Chin Med. (2020) 22:686–91. doi: 10.11842/wst.20200301003
22. Cui S, Zhang C, Wang S, Zhang X, Wang L, Zhang L, et al. Experiences and attitudes of elementary school students and their parents toward online learning in china during the COVID-19 pandemic: questionnaire study. J Med Internet Res. (2021) 23:e24496. doi: 10.2196/24496
23. Zhao Y, Guo Y, Xiao Y, Zhu R, Sun W, Huang W, et al. The effects of online homeschooling on children, parents, and teachers of grades 1-9 during the COVID-19 pandemic. Med Sci Monit. (2020) 26:e925591. doi: 10.12659/MSM.925591
24. Teixeira MT, Vitorino RS, da Silva JH, Raposo LM, Aquino LA, Ribas SA. Eating habits of children and adolescents during the COVID-19 pandemic: the impact of social isolation. J Hum Nutr Diet. (2021) 34:670–8. doi: 10.1111/jhn.12901
25. Yang GY, Lin XL, Fang AP, Zhu HL. Eating habits and lifestyles during the initial stage of the COVID-19 lockdown in china: a cross-sectional study. Nutrients. (2021) 13:970. doi: 10.3390/nu13030970
26. Burani K, Nelson BD. Gender differences in anxiety: The mediating role of sensitivity to unpredictable threat. Int J Psychophysiol. (2020) 153:127–34. doi: 10.1016/j.ijpsycho.2020.05.001
27. Stanikova D, Luck T, Pabst A, Bae YJ, Hinz A, Glaesmer H, et al. Associations between anxiety, body mass index, and sex hormones in women. Front Psychiatry. (2019) 10:479. doi: 10.3389/fpsyt.2019.00479
28. Borrow AP, Handa RJ. Estrogen receptors modulation of anxiety-like behavior. Vitam Horm. (2017) 103:27–52. doi: 10.1016/bs.vh.2016.08.004
29. Zhang B, Xiong S, Xu Y. The relationship between mobile phone use and anxiety and depression: a meta-analysis. Chin J Clin Psychology. (2019) 27:1144–50. doi: 10.16128/j.cnki.1005-3611.2019.06.014
30. Luo X, Han J, Fan W. Health information and health anxiety in the internet era. Inf Doc Serv. (2019) 40:76–86. doi: 10.12154/j.qbzlgz.2019.02.010
31. Yang L, Zhang Y, Xu Y, Zheng J, Lin C. Survey on the psychological stress of community residents in response to the novel coronavirus pneumonia epidemic. Nurs Res. (2020) 34:1140–5. doi: 10.12102/j.issn.1009-6493.2020.07.009
32. Hall LR, Sanchez K, da Graca B, Bennett MM, Powers M, Warren AM. Income differences and COVID-19: impact on daily life and mental health. Popul Health Manag. (2022) 25:384–91. doi: 10.1089/pop.2021.0214
33. Bao Y, Sun Y, Meng S, Shi J, Lu L. 2019-nCoV epidemic: address mental health care to empower society. Lancet. (2020) 395:e37–8. doi: 10.1016/S0140-6736(20)30309-3
34. Hinz A, Klein AM, Brähler E, Glaesmer H, Luck T, et al. Psychometric evaluation of the Generalized Anxiety Disorder Screener GAD-7, based on a large German general population sample. J Affect Disord. (2017) 210:338–44. doi: 10.1016/j.jad.2016.12.012
35. Peng L, Zhang J, Li M, Li P, Zhang Y, Zuo X, et al. Negative life events and mental health of Chinese medical students: the effect of resilience, personality and social support. Psychiatry Res. (2012) 196:138–41. doi: 10.1016/j.psychres.2011.12.006
36. Wolfson JA, Leung CW. Food insecurity and COVID-19: disparities in early effects for US adults. Nutrients. (2020) 12:1648. doi: 10.3390/nu12061648
Keywords: parents, anxiety, GAD-7, coronavirus disease 2019, influencing factors
Citation: Han J, Zhang X, Zhang S, Li Y, Zhang D and Chen Q (2023) Analysis of the anxiety level and influencing factors during the coronavirus disease 2019 epidemic among the parents of students in China. Front. Public Health 11:1143836. doi: 10.3389/fpubh.2023.1143836
Received: 13 January 2023; Accepted: 21 February 2023;
Published: 09 March 2023.
Edited by:
Valerio Dell'Oste, University of Pisa, ItalyReviewed by:
Wenning Fu, Huazhong University of Science and Technology, ChinaLi Zou, Zhongnan Hospital, Wuhan University, China
Copyright © 2023 Han, Zhang, Zhang, Li, Zhang and Chen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Qingsong Chen, cWluZ3NvbmdjaGVuQGFsaXl1bi5jb20=
†These authors have contributed equally to this work
 Jing Han1†
Jing Han1† Qingsong Chen
Qingsong Chen