
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Public Health , 08 March 2023
Sec. Aging and Public Health
Volume 11 - 2023 | https://doi.org/10.3389/fpubh.2023.1142456
This article is part of the Research Topic Reviews in Behavioral and Lifestyle Interventions for Healthy Aging: 2022 View all 6 articles
Background: Depression, an increasing global crisis, has affected many people's daily life, especially for older adults. Horticultural therapy has been widely used in non-pharmacological treatment for patients with depression, with a body of studies demonstrating its therapeutic effects. However, a lack of systematic reviews and meta-analyses makes it difficult to get a holistic picture of this research field.
Objectives: We aimed to evaluate the reliability of the previous studies and the effectiveness of horticultural therapy (including the intervention of environmental settings, activities, and duration) on older adults with depression.
Methods: This systematic review was conducted under the Preferred Reporting Items for Systematic Review and Meta-Analysis Protocols (PRISMA) guidelines. We searched relevant studies in multiple databases, and the original search was finished on 25 September 2022. We included studies using randomized controlled trials (RCTs) or quasi-experimental designs.
Results: We yielded a total of 7,366 studies and finally included 13 which involved 698 aged people with depression. Results from meta-analysis indicated significant effects of horticultural therapy on reducing depressive symptoms for the older adults. Besides, we found different outcomes among various horticultural interventions (such as environmental setting, activities, and duration). Depression reduction was more effective in care-providing settings than in community settings; participatory activities were more effective in reducing depression than observational activities; intervention of 4–8 weeks might represent the optimal course of treatment compared to interventions more than 8 weeks in duration.
Conclusion: We came up with a comprehensive set of recommendations based on the meta-analysis: aged people in care-providing settings with depression could get the most benefit from horticultural therapy by participating in participatory activities for 4–8 weeks.
Systematic review registration: https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42022363134, identifier CRD42022363134.
Population aging has become a severe societal problem worldwide and accordingly the older adults' overall quality of life should be given adequate attention (1). World Health Organization defined health as a state of complete physical, mental, and social wellbeing, thus mental health and wellbeing are as important as, if not more important than, physical health (2). The older adults are more likely to experience various types of psychosocial stress due to reduced social contact, living alone, and health concerns, all of which exacerbate their emotions of loneliness and helplessness, increasing the possibility of depression (3). According to the report named Depression: A Global Crisis released by the United Nations (4), depression was ranked as the third leading cause of the global burden of disease in 2004 and will move into the first place by 2030. Around 3.7–34.8% of the older adults in the general population suffered from depression up to 2019 (5).
Depression in the twilight life was an affect-related disease marked by considerable and persistent depression, as well as changes in mind, behavior, and somatic symptoms, normally with long-lasting effects and a high relapse rate (6, 7). Depression might cause great suffering for both patients and caregivers, and lead to impaired functioning in patients' daily life. The major effects of depression included physical and psychological discomfort, worsening of pre-existing diseases, cognitive impairment, greater financial loads on families, and increased suicide rates (8, 9). For aged people, depression was a common cause of morbidity and disability and was commonly associated with Alzheimer's disease (8, 10–13). Depression in the aged made up a significant proportion of national health care budgets and there is a strong need for low-cost and effective strategies to treat depression in aged people.
Pharmacological interventions have been considered the primary treatment for depression for a long time (14, 15). However, medication may have side effects, such as increased risks of cardiovascular disease and metabolic syndrome (16). As a result, non-pharmacological methods–using physical and non-chemical methods rather than medications, are becoming increasingly popular in the treatment for aged people with depression (17, 18). Non-pharmacological treatments are significantly more cost-effective and feasible, and they have been increasingly employed as a first-line treatment before pharmacological treatment (19–22).
Horticultural therapy was regularly adopted as a non-pharmacological treatment for depression (23–28). Horticultural therapy is defined as the participation in horticultural activities facilitated by registered horticultural therapists to achieve specific goals within an established treatment, rehabilitation, or vocational plan (29). In recent decades, researchers and health practitioners have come to realize the potential health benefits derived from these activities, and empirical evidence for the effectiveness of horticulture therapy on the older adults with depression has received increasing attention (30–32). Previous systematic reviews have supported the effectiveness of horticultural therapy on various populations involving healthy people (33), patients with dementia (34), peoples with schizophrenia (35), people with depressive symptoms (36), etc. When participating in horticultural activities, older adults could improve their quality of life by changing monotonous life patterns, diverting attention from harmful emotions (such as anxiety, sadness) and illness, enhancing self-confidence and self-esteem, and preventing depression (37–40). It is also worth noting that the horticultural interventions of environmental settings, activities, and duration have significant impacts on the outcomes of depression-reduction effects (41–43).
Overall, studies have done abundant work on unveiling the depression-reduction effects of horticultural therapy. However, it is difficult for researchers to obtain a holistic picture of this topic due to the lack of a systematic review on the older adults with depression (measured or/and clinical confirmed) and the best dose of a “prescription pill”–the interventions of horticultural therapy, including the environmental settings, activities, and duration. Meta-analysis is a fundamental approach for evidence-based medical research which helps to resolve inconsistencies among studies by aggregating their results, in order to draw the most definitive conclusions from a statistical perspective (44). Therefore, we utilized meta-analysis to measure the effectiveness of horticulture therapy on aged people suffering from depression. We aim to evaluate existing studies, provide a comprehensive understanding of the effects of horticultural therapy on older adults with depression, and provide suggestions and inspirations for future research.
This systematic review was conducted under the Preferred Reporting Items for Systematic Review and Meta-Analysis (PRISMA) guidelines (45), which are presented in Supplementary Table 1. This study protocol was registered in the International Prospective Register of Systematic Reviews (PROSPERO) with registration number CRD42022363134. We searched relevant studies in several databases including PubMed, Embase, The Cochrane Library, Medline, CINAHL, PsycINFO, Web of Science, Scopus, ProQuest, and four Chinese databases–China National Knowledge Infrastructure (CNKI), Wanfang Data, VIP Data, and Chinese BioMedical Literature Database (CBM), with restrictions on the published year from database inception to 25 September 2022. We used the following common keywords: “aged/ elderly/‘old people'/older”, “Melancholia*/‘Depressive Disorder'/depress*”, and “horticult*/garden*/farm*”, and the Supplementary Tables 2–14 listed full search strings applicable to all 13 databases. The search strategy for Chinese databases was as follows: “(SU=‘老人 (old people)' OR SU=‘老 年(aged)' OR SU=‘老龄(older)' OR SU=‘长者(older adults)')AND (SU=‘抑郁(depression)' OR SU=‘忧郁(depressive symptoms)') AND (SU=‘花园(garden)' OR SU=‘园艺(horticulture)' OR SU=‘农(farm)').”
We included studies by the following criteria: (i) Population: older adults aged 60 or above with measured or clinically confirmed depression; (ii) Intervention: horticultural therapy; (iii) Comparison: conventional work training and other non-pharmacological treatments; (iiii) Outcomes: the score of depression; (iiiii) Study design: randomized controlled trials (RCTs) and quasi-experimental studies. Literature of which the original research data is missing or the full text is unavailable, duplicate publications of research data or literature, literature not in English or Chinese, and conference papers or dissertations were excluded.
All studies were imported into EndNote X9. We screened the titles and abstracts to exclude irrelevant literature, followed by a full-text assessment. The data extracts included: author, year of publication, country, age, gender, sample size, environmental settings (confined care-providing settings such as nursing homes, health center and hospital/unconfined community settings), performer, intervention method (activities, frequency, duration), follow-up, and outcome indicators, as well as mean and standard deviation (SD) score of depression. Other test parameters (e.g., Confidence Interval (CI), p and F) were used to calculate SD when it was not available. We also contacted the authors when an effect size could not be calculated. Two investigators screened the literature and extracted information independently, and a third investigator was involved when there were disagreements.
The Cochrane Collaboration's risk of bias tool (46) was used to evaluate the risk of bias in the included RCT studies. The risk of bias assessment consisted of seven essential sources of bias: random sequence generation, allocation concealment, blinding of subjects and investigators, blinding of outcome assessors, incomplete outcome data, selective reporting of results and bias from other sources, with the expressions “low risk,” “high risk” and “unclear” representing the outcomes of the assessment.
The Joanna Briggs Institute (JBI) Critical appraisal tool were used to evaluate the risk of bias in the included quasi-experimental studies. The quality assessment consisted of nine items, covering causality of study variables, baseline, control, measurement of outcome indicators, and data analysis, with the expressions “Yes,” “No,” “Unclear” and “Not applicable” representing the outcomes of the assessment. Two investigators independently assessed all included studies, and when disagreements arose, two investigators discussed with each other or referred to the third investigator for consultation.
RevMan 5.3 software and Stata version 15.1 software were used for data processing, analyzing, and graphical plotting. The effect sizes were determined using standardized mean differences (SMDs) because the data included were continuous data measured on different scales. The results were aggregated with 95% CIs. The I2 test was used to assess the heterogeneity of intervention effects among studies, with 25, 50, and 75% being considered as low, moderate, and high degrees of heterogeneity respectively. We used the random-effects model when there was substantial between-study heterogeneity (I2 > 50%); otherwise a fixed effects model was used. If heterogeneity differences were too large, then subgroup analyses based on the study design and sensitivity analyses were performed to explore potential sources of heterogeneity and evaluate the robustness of the results. Furthermore, the funnel plot (if there were sufficient studies) and Egger's test (p > 0.05 (two-tailed) indicates no publication bias) were performed to assess the risk of publication bias.
The literature screening process and results are presented in Figure 1 according to the PRISMA flow diagram (47). We yielded a total of 7,366 articles; we eliminated 2,794 articles due to duplication, 4.503 due to irrelevant titles and abstracts, and 57 articles due to the failure to meet the criteria or unavailable full text (e.g., not people aged 60 or above, not people with depression, or not horticultural therapy). Twelve articles reporting 13 studies were finally included in this meta-analysis since two studies were from the same article (48). Six of which were RCTs and seven were quasi-experimental studies.
We included a total of 13 studies that were published between 2010 and 2022, involving 698 older people with depression. Supplementary Table 15 shows the details of these studies. A majority of studies were performed in China (n = 6), followed by Japan (n = 3), Korea (n = 3) and Poland (n = 1). Most retrieved studies (n = 8; 61.5%) used the 15-item Geriatric Depression Scale (GDS-15), with remaining five studies using the 30-item Geriatric Depression Scale (GDS-30). The levels of depression were mild to moderate, with no aged people suffering from major depression in the reported studies.
The studies involved in the final analysis varied greatly in sample size. For example, Chu et al. (37) recruited 150 participants, and Wang and Jiang (49) recruited 126 participants, with six studies including < 30 participants. Nine studies had both male and female participants, while study from McCaffrey et al. (50) did not describe the gender composition of the participants, and studies from Kim (48) and Szczepanska et al. (51) had only female participants. All of the aged people involved in the studies had normal cognitive function, except for Kim (48). Some studies also included specific groups of people who, in addition to the depression they exhibited, may also have mild dementia (48), or memory problem (12). Ten studies involved interventions of horticultural therapy that were guided by professionals such as researchers (37, 50, 52–54), therapist (51), horticultural therapist (48, 55), and experts (12), while three studies did not mention any information about the performer (49, 56, 57).
Regarding the environmental settings, four studies were conducted in community (12, 50, 54, 56), three in nursing home (37, 55, 57), four in special care facilities (48, 51, 52), and one in hospital (49). Almost all studies were conducted in realistic environment, with two studies conducted using Virtual-Reality (VR) technology (51, 53). Seven studies were quasi-experimental studies, of which five were before-after design and two used a parallel design. Six RCTs were also parallel-designed studies. For parallel-designed studies, three studies adopted art therapy (50), sports care (49) and a blank (52), respectively as control, while the other two studies adopted leisure or education activities or usual care as a control. In terms of horticultural therapy, 11 studies selected participatory activities such as planting and harvest, and two involved observational activities such as walking in the green areas (50, 54). The course of treatment–duration of interventions ranged from 4 weeks (51) to 36 weeks (54), with each session lasting ~90 min on average (ranging from 20 to 120 minutes). The frequency of the interventions mainly included activities on daily, weekly, and monthly bases (12, 49, 54).
Figures 2, 3 shows the evaluations of the risk of bias in six RCTs. Most of the studies were assessed as low-risk, with some studies having a loss to follow-up bias. One study mentioned “random” but did not explain the specific method they adopted, and the remaining studies described how the random sequence was generated, i.e., computer randomization. Five studies used central random assignment or sealed opaque envelopes, while others did not describe the concealment of allocation. Two studies were blinded to subjects. Three studies were blinded to the outcome measures. Only one study had incomplete outcome data, but the number and reasons for loss to follow-up bias were similar in the control and experimental groups. Selective bias was not found in all studies, and there was no other bias. Table 1 shows the detailed results of the risk of bias in seven quasi-experimental studies. In general, no risk of bias was found in the quasi-experimental studies included, according to the JBI critical appraisal checklist.
The retrieved studies used the GDS-15 and the GDS-30 to measure the depression-reduction effects, and SMD was used because of the non-uniform standard. We used the random-effects model, accounting for diversity in horticultural interventions across studies (58). As shown in Figure 4, a significantly positive difference was found in the impact of horticultural therapy [SMD = −1.62, 95% CI (−2.56, −0.69), p = 0.0007], though with high heterogeneity detected in the pooled analysis (p < 0.00001, I2 = 97%). A sensitivity analysis was performed by removing the study included one by one and a significant decreased heterogeneity (I2 = 88%) was detected after removing the study from Chu et al. (37) [SMD = −0.69, 95% CI (−1.19, −0.19), p = 0.007]. Nevertheless, this analysis still suggested that horticultural therapy positively reduced depression for the older adults, indicating a robust effect.
Subgroup analysis was conducted according to the interventions of horticultural therapy including environmental settings, activities, and duration, to analyze the heterogeneity within the subgroups.
We divided the intervention settings into care-providing settings and community settings based on the well-accepted ways of aged care around the world (59, 60). SMD was used because of the non-uniform standard. We used the random-effects model because of the existence of substantial heterogeneity (p < 0.00001, I2 = 97%). In Figure 5, the depression-reduction effects were significant in care-providing settings [SMD = −2.14, 95% CI (−3.55, −0.74), p = 0.003] while not found in community settings [SMD = −0.70, 95% CI (−1.67, 0.26), p = 0.15]. We removed all the studies one by one and no changes were detected in sensitivity analyses.
The majority of the horticultural activities included planting and walking, and we categorized them into participatory and observational types according to previous studies (61, 62). SMD was used as well because of the non-uniform standard. We used the random-effects model because of the existence of substantial heterogeneity (p < 0.00001, I2 = 97%). Figure 6 demonstrates significant effects of horticultural therapy in the participatory activities [SMD = −1.76, 95% CI (−2.84, −0.68), p = 0.001] on the score of GDS, whereas the outcomes were not significant in the observational activities [SMD = −1.01, 95% CI (−3.15, 1.13), p = 0.36]. We removed all the studies one by one and the result became opposite in sensitivity analyses when removing the study from McCaffrey et al. (50) [SMD = 2.09, 95% CI [−2.64, −1.54], p < 0.00001) in observational activities.
We divided the intervention duration into 4–8 weeks and more than 8 weeks, due to the majority of the included studies and previous studies being 8 weeks. We used the random-effects model because of the existence of substantial heterogeneity (p < 0.00001, I2 = 97%), with SMD used. As shown in Figure 7, the result indicated significant effects of horticultural therapy in the duration of 8 weeks and below [SMD = −3.40, 95% CI (−6.36, −0.44), p = 0.02] and significant differences were detected in sensitivity analyses when removing the study from Jiang et al. (55) [SMD = −4.17, 95% CI (−8.65, 0.31), p = 0.07]. No difference was found between experimental group and control group in the duration of more than 8 weeks [SMD = −0.67, 95% CI (−1.47, 0.13), p = 0.10] and the result became opposite in sensitivity analyses when removing the study from Lin et al. (53) [SMD = −0.91, 95% CI (−1.61, −0.21), p = 0.01].
The funnel plot shows that the included studies are mainly clustered at the top and sparsely distributed at the bottom (Figure 8). They have symmetrical trends and are evenly dispersed on both sides, suggesting there was no publication bias. The conclusion was further supported by Egger's test, which found no evidence of publication bias (p = 0.062).
This study provided a quantitative synthesis of the evidence supporting the positive effects of horticulture therapy on older adults people with depression. Previous research has shown that horticultural therapy could improve participants' emotions (63), reduce their stress level (64, 65), build confidence and self-esteem (66, 67), and improve their motor skills. During the activities, patients were willing to discuss and share their positive experiences with peers, which could strengthen their social interaction skills and increase their sense of community (68). This study provides a comprehensive prospect over the non-pharmacological prescription–horticultural therapy for aged people with depression, and we have identified several important attributes of horticultural therapy from subgroup analysis.
Environmental settings could have essential impacts on effective treatment, in consistence with prior findings (69–72). Our results supported the therapeutic effects of horticultural activities in care-providing settings rather than those in community settings. We supposed that the reasons could be as follows: (i) Patients in care-providing settings might have a stronger desire to be cured compared to patients in community settings, which positively support their recovery from depression. (ii) The care-providing environments include a variety of specialized care environments such as hospitals and nursing homes, and featured a more professional medical and nursing team compared to communities. Thus, horticultural therapy was more likely to be long-termed and regular in care-providing settings.
The therapeutic effect to a large extent depends on the healing design for the environment and the degree of proximity to nature. Therefore, we appeal for more studies characterizing the healing environment in a clear and detailed way to shed light on the quantitative impact of the environment on healing outcomes.
The effectiveness of horticulture therapy was also influenced by the types of activities. We found that participatory activities were more beneficial in reducing depression than observational activities. People involved in participatory activities were more physically engaged than those in observational activities (73), which could strengthen their body functions and improve their physical condition. Simultaneously, participating in horticulture activities allowed individuals to enjoy their horticultural task meanwhile removed their negative emotions (74). Furthermore, aged people with depression may experience a variety of tactile sensations such as the temperature, hardness, and texture of different plants in participatory activities, which may stimulate the intuitive and motor parts of the cerebral cortex, resulting in a sense of comfort and enjoyment (75–77).
Our findings also suggest that when one study (50) on the efficiency of horticultural therapy in observational activities was excluded, the results turned out to be the contrary. This shows that the current evidence of the effectiveness of observational activities is not robust. The results of this test represent more of an indication than evidence, though many studies have shown that simply being exposed to nature could have a long-lasting and deep impact on health, both physically and psychologically (78–82). Moreover, given the limited studies on the observational activities, more well-designed studies are needed to evaluate the effectiveness.
Studies reported in this review varied in the duration and frequency of horticultural therapy. According to our results, the optimal intervention for older adults with depression was identified to be 4–8 weeks (basically once each week). The probable explanation might be that participants can completely participate in the life cycle of a certain plant. A longer intervention period, on the other hand, may result in aesthetic fatigue and a loss of novelty, with little or no improvement in outcomes. Meanwhile, the results became opposite when removing one study (55) in the effectiveness of 4–8 weeks duration and another (53) in the effectiveness of more than 8 weeks duration. This demonstrates that more well-designed studies of duration are required to evaluate the effectiveness as the current evidence about the effectiveness in duration is not robust. According to the included studies, a single horticulture activity lasted mostly 1–2 h. As Hayashi pointed out, horticultural activities longer than 2 h did not have a positive effect on mood (83). Though previous studies showed that even short-time exercise in gardens provided instantaneous benefits on health, such as reductions in the symptoms of depression and anxiety (65, 83, 84).
We came up with a “prescription pill” of horticultural therapy in the aged people with depression according to our study (as shown in Figure 9).
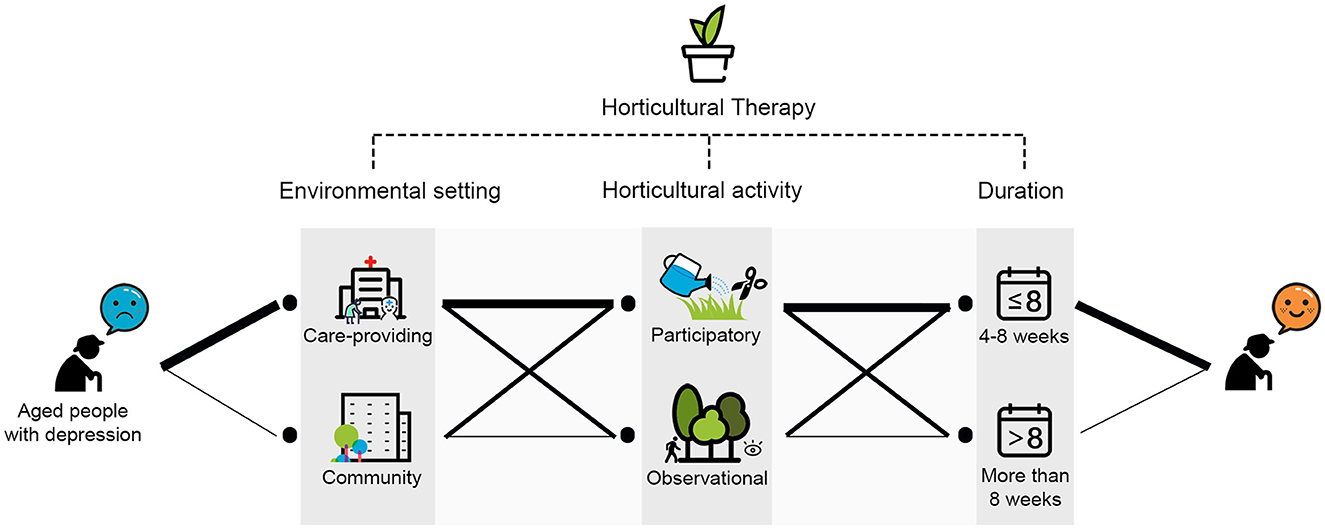
Figure 9. The “prescription pill” of horticultural therapy in the aged people with depression. (Note: thicker lines indicate better therapeutic effect).
However, there are some limitations. We only included articles written in English or Chinese, which might result in articles published in other languages not being included in our analysis. And we only classified environmental settings into care-providing and community settings instead of more specific environmental subgroups given the wide range of environments (communities, hospitals, nursing homes, homeless living facility, care centrals and long-term care facilities). Gender of participants and the performers of horticultural therapy (such as researchers, nursing staff, or horticultural therapists) might also influence the outcomes of horticultural therapy on depression reduction in the aged. Therefore, future studies should pay more attention on these issues.
Our analysis supported the notion that horticultural therapy could improve symptoms in aged people with depression. We also looked into the effectiveness of different interventions of horticultural therapy (including the types of environmental settings, activities, and duration) and then came up with a comprehensive set of recommendations. In terms of the environment settings, care-providing settings were demonstrated to produce higher therapeutic effects. Participatory activities produced greater outcomes than observational activities. In terms of the duration of the interventions, a course of 4–8 weeks of horticultural therapy had better outcomes. Furthermore, future research on horticultural therapy and depression is in high need, and more rigorously designed studies are needed to shed light on which type of environment settings and horticultural interventions leads to improved depression outcomes.
Overall, our results demonstrated that horticultural therapy plays an effective role in promoting the wellbeing of older adults with depression. We also developed a comprehensive framework for future conduct of horticulture therapy (in a methodical and professional manner) based on our subgroup analysis. This research serves as a reference for the planning and implementation of horticultural activities as well as the design of healing gardens. We hope the application of horticultural therapy could help lower national financial expenditures on public health care and bring new ideas and approaches to promote public health. We call on future studies to include additional outcome indicators (such as quality of life, social function) and study designs (such as cross-section study) to demonstrate the efficacy of horticultural therapy for various dimensions of depression, and other diseases as well as groups of people.
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
MX and FX contributed to conception and design of the study. MX, SL, and JL organized the database. MX performed the statistical analysis and wrote the first draft of the manuscript. SL and JL wrote sections of the manuscript. All authors contributed to manuscript revision, read, and approved the submitted version.
This study was supported by the Beijing Municipal Science and Technology Commission (project no. Z201100008020004).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2023.1142456/full#supplementary-material
1. Chan HY, Ho RCM, Mahendran R, Ng KS, Tam WWS, Rawtaer I, et al. Effects of horticultural therapy on elderly' health: protocol of a randomized controlled trial. BMC Geriatr. (2017) 17:192. doi: 10.1186/s12877-017-0588-z
2. United Nations. Constitution of the World Health Organization. (1948). Available online at: https://www.who.int/about/governance/constitution (accessed December 22, 2022).
3. United Nations. Mental Health of Older Adults. (2017). Available online at: https://www.who.int/news-room/fact-sheets/detail/mental-health-of-older-adults (accessed December 29, 2021).
4. United Nations. Depression: A Global Crisis. (2012). Available online at: https://tai.ee/sites/default/files/2021-03/138062227459_Depression_A_Global_Crisis_2012.pdf (accessed December 22, 2022).
5. Cui L, Ding D, Chen J, Wang M, He F, Yu S. Factors affecting the evolution of Chinese elderly depression: a cross-sectional study. BMC Geriatr. (2022) 22:109. doi: 10.1186/s12877-021-02675-z
6. Bruce DF. Depression in Older Adults. WebMD. (2020). Available from: https://www.webmd.com/depression/guide/depression-elderly (accessed December 22, 2021).
7. Fiske A, Wetherell JL, Gatz M. Depression in older adults. Annu Rev Clin Psychol. (2009) 5:363–89. doi: 10.1146/annurev.clinpsy.032408.153621
8. Friedhoff AJ. Diagnosis and treatment of depression in late life. JAMA. (1992) 268:1018. doi: 10.1001/jama.1992.03490080092032
9. Orsolini L, Latini R, Pompili M, Serafini G, Volpe U, Vellante F, et al. Understanding the complex of suicide in depression: from research to clinics. Psychiatry Investig. (2020) 17:207–21. doi: 10.30773/pi.2019.0171
10. Beekman ATF, Copeland J, Prince MJ. Review of community prevalence of depression in later life. Br J Psychiatry. (1999) 174:307–11. doi: 10.1192/bjp.174.4.307
11. Djernes JK. Prevalence and predictors of depression in populations of elderly: a review. Acta Psychiatr Scand. (2006) 113:372–87. doi: 10.1111/j.1600-0447.2006.00770.x
12. Makizako H, Tsutsumimoto K, Doi T, Makino K, Nakakubo S, Liu-Ambrose T, et al. Exercise and horticultural programs for older adults with depressive symptoms and memory problems: a randomized controlled trial. J Clin Med. (2020) 9:99. doi: 10.3390/jcm9010099
13. Makizako H, Tsutsumimoto K, Doi T, Hotta R, Nakakubo S, Liu-Ambrose T, et al. Effects of exercise and horticultural intervention on the brain and mental health in older adults with depressive symptoms and memory problems: study protocol for a randomized controlled trial [UMIN000018547]. Trials. (2015) 16:499. doi: 10.1186/s13063-015-1032-3
14. Huang Y, Meng X, Zhang Z, Zhang G, Wu F. Cognitive function predicts treatment response of inpatients with major depressive disorder. J China Med Univ. (2021) 50:439–43. doi: 10.12007/j.issn.0258-4646.2021.05.011
15. Wang T, Li Y, Wang J. Clinical effect of citalopram in elderly chronic heart failure patients with depression. Chin J Geriatric Heart Brain Vessel Dis. (2021) 23:172–5. doi: 10.3969/j.issn.1009-0126.2021.02.016
16. Qu W, Gu SS. New progress in treatment of depression. J Third Milit Med Univ. (2014) 36:1113–7. doi: 10.16016/j.1000-5404.2014.11.022
17. Olazarán J, Reisberg B, Clare L, Cruz I, Peña-Casanova J, Del Ser T, et al. Nonpharmacological therapies in Alzheimer's disease: a systematic review of efficacy. Dement Geriatr Cogn Disord. (2010) 30:161–78. doi: 10.1159/000316119
18. Tuunainen A, Kripke DF, Endo T. Light therapy for non-seasonal depression. Cochrane Database Syst Rev. (2004) 2:CD004050. doi: 10.1002/14651858.CD004050.pub2
19. Akram M. Alternative Medicine - Update. (2021) [cited 2021 Dec 29]. Available online at: https://www.intechopen.com/books/9445 (accessed December 29, 2021).
20. Herguedas AJU. Non-Pharmacological Interventions in Preventive, Rehabilitative Restorative Medicine. Alternative Medicine - Update. IntechOpen (2020). Available online at: https://www.intechopen.com/chapters/73680 (accessed November 16, 2021).
21. Noriega RB, Camporro SN, Rodríguez AMI. Nursing and no drug for the management of insomnia treatment. Enf Global. (2019) 18:512–32. doi: 10.6018/eglobal.18.2.322311
22. Plácido R, Mebazaa A. Nonpharmacological management of acute heart failure. Rev Esp Cardiol. (2015) 68:794–802. doi: 10.1016/j.rec.2015.05.006
23. Detweiler MB, Self JA, Lane S, Spencer L, Lutgens B, Kim DY, et al. Horticultural therapy: a pilot study on modulating cortisol levels and indices of substance craving, posttraumatic stress disorder, depression, and quality of life in veterans. Altern Ther Health Med. (2015) 21:36–41.
24. Hoseinpoor Najjar A, Foroozandeh E, Asadi Gharneh HA. Horticulture therapy effects on memory and psychological symptoms of depressed male outpatients. Iranian Rehab J. (2018) 16:147–54. doi: 10.32598/irj.16.2.147
25. Kim HK, Na SS, Kim HH. Effects of horticultural therapy programs on depression and self-esteem in released-convicts. J People Plants Environ. (2017) 20:143–8. doi: 10.11628/ksppe.2017.20.2.143
26. Kim KH, Park SA. Horticultural therapy program for middle-aged women's depression, anxiety, and self-identify. Complement Ther Med. (2018) 39:154–9. doi: 10.1016/j.ctim.2018.06.008
27. Korah T, Morrison D, Mason D, Diehl ER, Bussing R. Therapeutic horticulture as a therapeutic intervention in patients receiving electroconvulsive therapy (ECT) treatment for major depressive disorder. Cureus. (2021) 13:e17363. doi: 10.7759/cureus.17363
28. Maeong HJ, Gang M, Oh HJ. The effects of five sensory horticulture therapy on perceived stress and heart rate variability in adults with depression. J Korea Converg Soc. (2019) 10:517–23. doi: 10.15207/JKCS.2019.10.12.517
29. American Horticultural Therapy Association. Definitions Positions. (1997). Available online at: https://www.ahta.org/ahta-definitions-and-positions (accessed December 29, 2021).
30. Clatworthy J, Hinds JM, Camic P. Gardening as a mental health intervention: a review. Mental Health Rev J. (2013) 18:214–25. doi: 10.1108/MHRJ-02-2013-0007
31. Genter C, Roberts A, Richardson J, Sheaff M. The contribution of allotment gardening to health and wellbeing: a systematic review of the literature. Br J Occup Therapy. (2015) 78:593–605. doi: 10.1177/0308022615599408
32. Wang D, MacMillan T. The benefits of gardening for older adults: a systematic review of the literature. Act Adapt Aging. (2013) 37:153–81. doi: 10.1080/01924788.2013.784942
33. Spano G, D'Este M, Giannico V, Carrus G, Elia M, Lafortezza R, et al. Are community gardening and horticultural interventions beneficial for psychosocial well-being? A meta-analysis. Int J Environ Res Public Health. (2020) 17:3584. doi: 10.3390/ijerph17103584
34. Lu LC, Lan SH, Hsieh YP, Yen YY, Chen JC, Lan SJ. Horticultural therapy in patients with dementia: a systematic review and meta-analysis. Am J Alzheimers Dis Other Demen. (2020) 35:1–11. doi: 10.1177/1533317519883498
35. Lu S, Zhao Y, Liu J, Xu F, Wang Z. Effectiveness of horticultural therapy in people with schizophrenia: a systematic review and meta-analysis. Int J Environ Res Public Health. (2021) 18:964. doi: 10.3390/ijerph18030964
36. Zhang YW, Wang J, Fang TH. The effect of horticultural therapy on depressive symptoms among the elderly: A systematic review and meta-analysis. Front Public Health. (2022) 10:953363. doi: 10.3389/fpubh.2022.953363
37. Chu HY, Chen MF, Tsai CC, Chan HS, Wu TL. Efficacy of a horticultural activity program for reducing depression and loneliness in older residents of nursing homes in Taiwan. Geriatric Nurs. (2019) 40:386–91. doi: 10.1016/j.gerinurse.2018.12.012
38. Gagliardi C, Piccinini F. The use of nature – based activities for the well-being of older people: an integrative literature review. Arch Gerontol Geriatr. (2019) 83:315–27. doi: 10.1016/j.archger.2019.05.012
39. Hawkins J, Mercer J, Thirlaway K, Clayton DA. “Doing” gardening and “being” at the allotment site: exploring the benefits of allotment gardening for stress reduction and healthy aging. Ecopsychology. (2013) 5:110–25. doi: 10.1089/eco.2012.0084
40. Tu PC, Cheng WC, Hou PC, Chang YS. Effects of types of horticultural activity on the physical and mental state of elderly individuals. Int J Environ Res Public Health. (2020) 17:5225. doi: 10.3390/ijerph17145225
41. Kim D. The effects of a recollection-based occupational therapy program of Alzheimer's disease: a randomized controlled trial. Occup Ther Int. (2020) 2020:e6305727. doi: 10.1155/2020/6305727
42. Okura M, Ogita M, Yamamoto M, Nakai T, Numata T, Arai H. The relationship of community activities with cognitive impairment and depressive mood independent of mobility disorder in Japanese older adults. Arch Gerontol Geriatr. (2017) 70:54–61. doi: 10.1016/j.archger.2016.12.010
43. Wu YT, Prina AM, Jones A, Matthews FE, Brayne C. MRC CFAS older people, the natural environment and common mental disorders: cross-sectional results from the cognitive function and ageing study. BMJ Open. (2015) 5:e007936. doi: 10.1136/bmjopen-2015-007936
44. Impellizzeri FM, Bizzini M. Systematic review and meta-analysis: a primer. Int J Sports Phys Ther. (2012) 7:493–503.
45. Moher D, Liberati A, Tetzlaff J, Altman DG, Group TP. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. (2009) 6:e1000097. doi: 10.1371/journal.pmed.1000097
46. Higgins JPT, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, et al. The cochrane collaboration's tool for assessing risk of bias in randomised trials. BMJ. (2011) 343:d5928. doi: 10.1136/bmj.d5928
47. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. (2021) 372:n71. doi: 10.1136/bmj.n71
48. Kim Y, Jo HS, Park CS, Kang K. Comparing the effectiveness of the frequency and duration of the horticultural therapy program on elderly women with mild cognitive impairment and mild dementia. J People Plant Environ. (2020) 23:35–46. doi: 10.11628/ksppe.2020.23.1.35
49. Wang Z, Jiang D. Nursing effect of horticultural therapy combined with sports nursing intervention in elderly patients with depression and its effect on aggressive behavior. Chin Foreign Med Res. (2020) 18:101–3. doi: 10.14033/j.cnki.cfmr.2020.14.040
50. McCaffrey R, Liehr P, Gregersen T, Nishioka R. Garden walking and art therapy for depression in older adults: a pilot study. Res Gerontol Nurs. (2011) 4:237–42. doi: 10.3928/19404921-20110201-01
51. Szczepańska-Gieracha J, Cieślik B, Serweta A, Klajs K. Virtual therapeutic garden: a promising method supporting the treatment of depressive symptoms in late-life: a randomized pilot study. J Clin Med. (2021) 10:1942. doi: 10.3390/jcm10091942
52. Kim Y, Lee SH, Park CS, Bae H, Kim YJ, Huh MR. A horticultural therapy program focusing on gardening activities to promote psychological, emotional and social health of the elderly living in a homeless living facility for a long time: a pilot study. J People Plants Environ. (2020) 23:565–76. doi: 10.11628/ksppe.2020.23.5.565
53. Lin TY, Huang CM, Hsu HP, Liao JY, Cheng VYW, Wang SW, et al. Effects of a combination of three-dimensional virtual reality and hands-on horticultural therapy on institutionalized older adults' physical and mental health: quasi-experimental design. J Med Internet Res. (2020) 22:e19002. doi: 10.2196/19002
54. McCaffrey R, Hanson C, McCaffrey W. Garden walking for depression: a research report. Holist Nurs Pract. (2010) 24:252–9. doi: 10.1097/HNP.0b013e3181f1acd7
55. Jiang N, Hu H, Xie L, Qiu Y. Intervention study of horticultural therapy on depression in the elderly with mild to moderate cognitive disease. J Yueyang Vocat Tech College. (2022) 37:74–9. doi: 10.13947/j.cnki.yyzyxb.2022.04.018
56. Yun GW. Exploration on the effect of horticultural therapy in improving the symptoms of senile depression J Anhui Agric Sci. (2016) 44:272–4. doi: 10.13989/j.cnki.0517-6611.2016.17.089
57. Chen YM, Ji JY. Effects of horticultural therapy on psychosocial health in older nursing home residents: a preliminary study. J Nurs Res. (2015) 23:167–71. doi: 10.1097/jnr.0000000000000063
58. Borenstein M, Hedges LV, Higgins JPT, Rothstein HR. A basic introduction to fixed-effect and random-effects models for meta-analysis. Res Synth Methods. (2010) 1:97–111. doi: 10.1002/jrsm.12
59. Kane RL. Medical care for the elderly in other western countries: lessons for the United States a general policy perspective. Home Health Care Serv Q. (1986) 7:307–15. doi: 10.1300/J027v07n03_37
60. Ting GHY, Woo J. Effects elder care: is legislation of family responsibility the solution? Asian J Gerontol Psychiatry. (2009) 4:72–5.
61. Lindemuth AL. Beyond the bars: landscapes for health and healing in corrections. In:Tidball KG, Krasny ME, , editors. Greening in the Red Zone: Disaster, Resilience and Community Greening. Dordrecht: Springer Netherlands (2014). p. 361–74.
62. Zhao Y, Liu Y, Wang Z. Effectiveness of horticultural therapy in people with dementia: A quantitative systematic review. J Clin Nurs. (2022) 31:1983–97. doi: 10.1111/jocn.15204
63. Kwon YH, Song MO, Kim CN. Effects of horticulture therapy on depression and stress in patient of hospice unit. J Korea Acad Indust Coop Soc. (2011) 12:4394–402. doi: 10.5762/KAIS.2011.12.10.4394
64. Cheng VYW, Huang CM, Liao JY, Hsu HP, Wang SW, Huang SF, et al. Combination of 3-dimensional virtual reality and hands-on aromatherapy in improving institutionalized older adults' psychological health: quasi-experimental study. J Med Internet Res. (2020) 22:e17096. doi: 10.2196/17096
65. Van Den Berg AE, Custers MHG. Gardening promotes neuroendocrine and affective restoration from stress. J Health Psychol. (2011) 16:3–11. doi: 10.1177/1359105310365577
66. Blair D, Giesecke CC, Sherman S. A dietary, social and economic evaluation of the Philadelphia urban gardening project. J Nutr Educ. (1991) 23:161–7. doi: 10.1016/S0022-3182(12)81191-5
67. Kong JH, Yun SY, Choi BJ. The effects of reminiscence-based horticultural therapy on institutionalized demented elders' self-esteem and quality of life. J Korean Soc People Plants Environ. (2015) 18:305–9. doi: 10.11628/ksppe.2015.18.4.305
68. Wu J, Xiao M, Zhao Q, Tian J, Luo Q, Xiao L, et al. Effects of horticultural therapy on quality of life and social function in patients with depression. Chin Nurs Manag. (2018) 18:48–51. doi: 10.3969/j.issn.1672-1756.2018.01.013
69. Asano F. Healing at a hospital garden: interaction of physical and non-physical aspects. Acta Hortic. (2008) 775:13–22. doi: 10.17660/ActaHortic.2008.775.1
70. Cervinka R, Röderer K, Hämmerle I. Evaluation of hospital gardens and implications for design: benefits from environmental psychology for architecture and landscape planning. J Archit Plann Res. (2014) 31:43–56.
71. Huxmann N. The garden as setting for horticultural therapy. Acta Horticulturae. (2016) 1121:39–46. doi: 10.17660/ActaHortic.2016.1121.7
72. Pasha S, Shepley M. Research note: physical activity in pediatric healing gardens. Landsc Urban Plan. (2013) 118:53–8. doi: 10.1016/j.landurbplan.2013.05.005
73. Xiu M, Li S. A preliminary study of the influence of horticultural operation activities on the physical and mental health of the elderly. Chin Landscape Architect. (2006) 22:46–9. doi: 10.3969/j.issn.1000-6664.2006.06.010
74. Koay WI, Dillon D. Community gardening: stress, well-being, and resilience potentials. Int J Environ Res Public Health. (2020) 17:6740. doi: 10.3390/ijerph17186740
75. Lo SKL, Lam WYY, Kwan RYC, Tse MMY, Lau JKH, Lai CKY. Effects of horticultural therapy: perspectives of frail and pre-frail older nursing home residents. Nursing Open. (2019) 6:1230–6. doi: 10.1002/nop2.323
76. Ferrini F. Horticultural therapy and its effect on people's health. Adv Hort Sci. (2003) 17:77–87. Available online at: https://www.jstor.org/stable/42882222 (accessed February 22, 2023).
77. Townsend M. Feel blue? Touch green! participation in forest/woodland management as a treatment for depression. Urban Forest Urban Green. (2006) 5:111–20. doi: 10.1016/j.ufug.2006.02.001
78. Beyer KMM, Kaltenbach A, Szabo A, Bogar S, Nieto FJ, Malecki KM. Exposure to neighborhood green space and mental health: evidence from the survey of the health of Wisconsin. Int J Environ Res Public Health. (2014) 11:3453–72. doi: 10.3390/ijerph110303453
79. Cox DTC, Shanahan DF, Hudson HL, Fuller RA, Anderson K, Hancock S, et al. Doses of nearby nature simultaneously associated with multiple health benefits. Int J Environ Res Public Health. (2017) 14:E172. doi: 10.3390/ijerph14020172
80. Dean JH, Shanahan DF, Bush R, Gaston KJ, Lin BB, Barber E, et al. Is nature relatedness associated with better mental and physical health? Int J Environ Res Public Health. (2018) 15:E1371. doi: 10.3390/ijerph15071371
81. Jakstis K, Fischer LK. Urban nature and public health: how nature exposure and sociocultural background relate to depression risk. Int J Environ Res Public Health. (2021) 18:9689. doi: 10.3390/ijerph18189689
82. Kotera Y, Lyons M, Vione KC, Norton B. Effect of nature walks on depression and anxiety: a systematic review. Sustainability. (2021) 13:4015. doi: 10.3390/su13074015
83. Hayashi N, Wada T, Hirai H, Miyake T, Matsuura Y, Shimizu N, et al. The effects of horticultural activity in a community garden on mood changes. Environ Control Biol. (2008) 46:233–40. doi: 10.2525/ecb.46.233
Keywords: horticultural therapy, aged people, depression, meta-analysis, systematic review
Citation: Xu M, Lu S, Liu J and Xu F (2023) Effectiveness of horticultural therapy in aged people with depression: A systematic review and meta-analysis. Front. Public Health 11:1142456. doi: 10.3389/fpubh.2023.1142456
Received: 11 January 2023; Accepted: 09 February 2023;
Published: 08 March 2023.
Edited by:
Lei Feng, National University of Singapore, SingaporeReviewed by:
Chongxian Chen, South China Agricultural University, ChinaCopyright © 2023 Xu, Lu, Liu and Xu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Feng Xu, Y2N4ZmNuQHNpbmEuY29t
†These authors share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.